Radiologic Evaluation of Intracranial Tumors Todd Gourdin MIV

- Slides: 45
Radiologic Evaluation of Intracranial Tumors Todd Gourdin M-IV Radiology Final Presentation August 2, 2007
Available Modalities 1)X-ray 2)CT 3)MRI 4)Nuclear Medicine
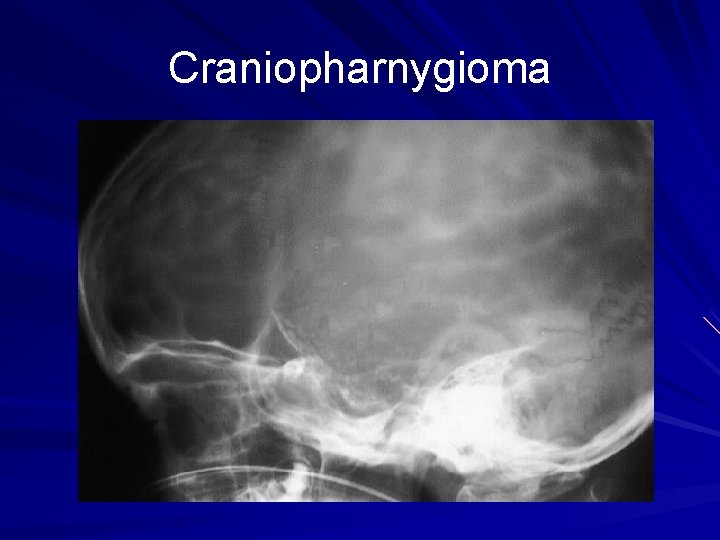
X-ray - Primarily of historical interest since the onset of CT in 1974. - Was useful for detecting increased intracranial pressure and intracranial calcifications.

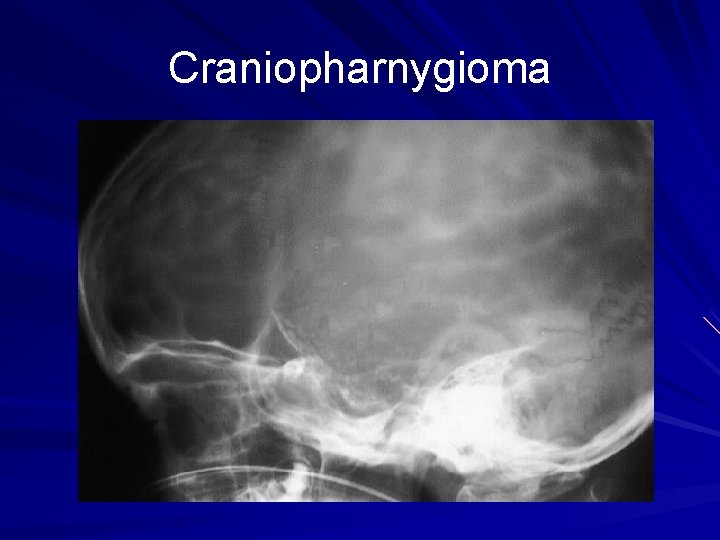
Craniopharnygioma
CT - Most intracranial neoplasms are visible on CT - Tumors may be hypodense, isodense, or hyperdense on a noncontrast CT depending on tumor histology and location
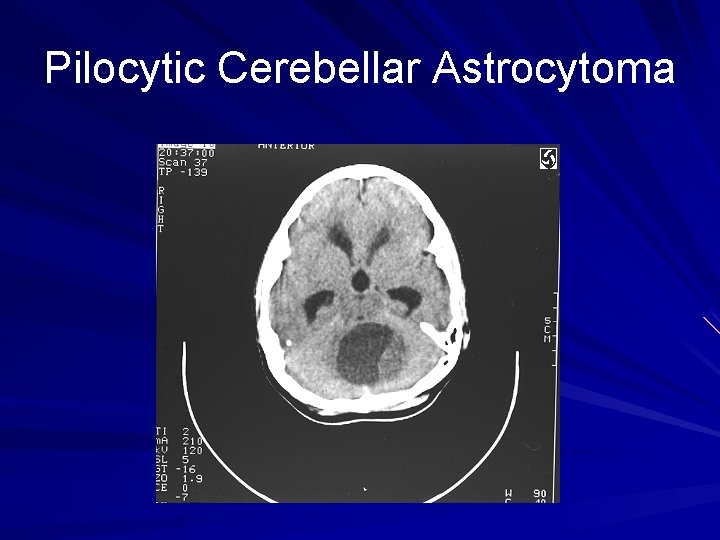
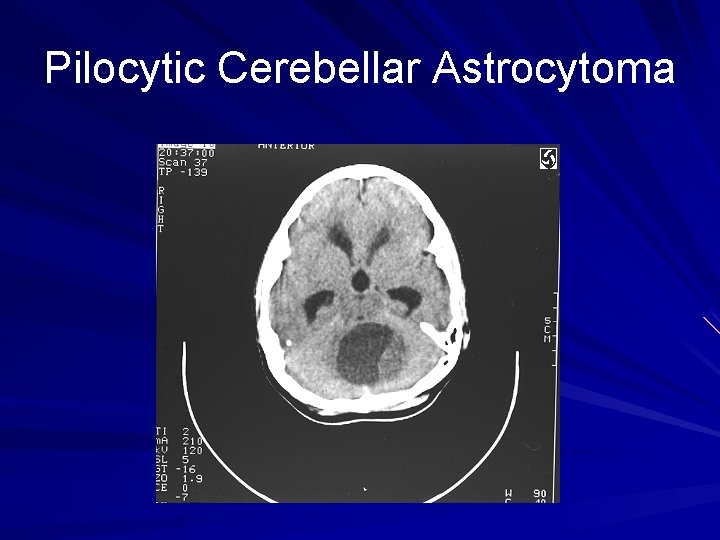
Pilocytic Cerebellar Astrocytoma
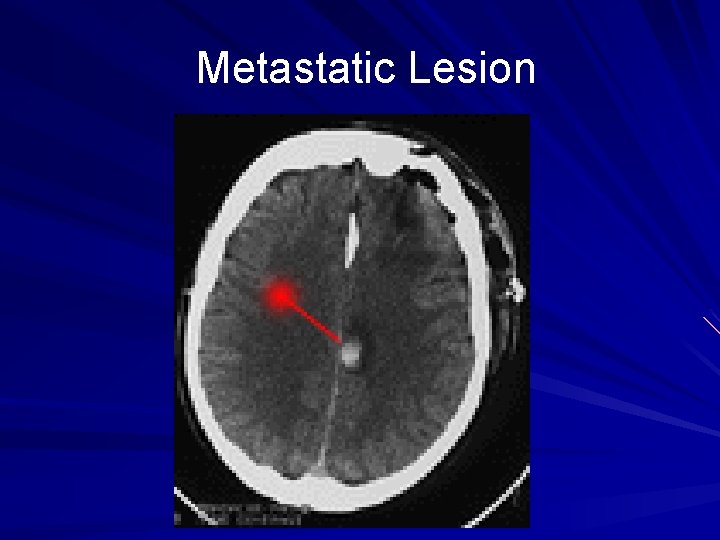
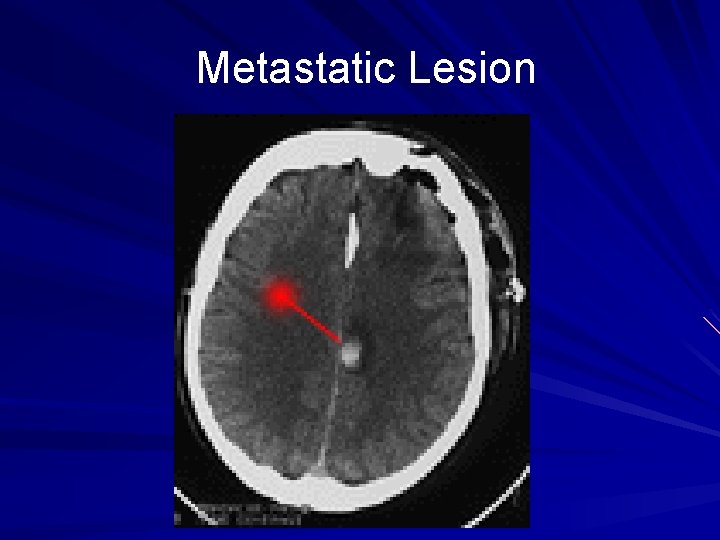
Metastatic Lesion
- Small tumors or isodense tumors may be missed on noncontrast CT but highlight after contrast administration - Meningiomas and Neuromas enhance strongly with contrast while low-grade gliomas and epidermoid tumors do not enhance.
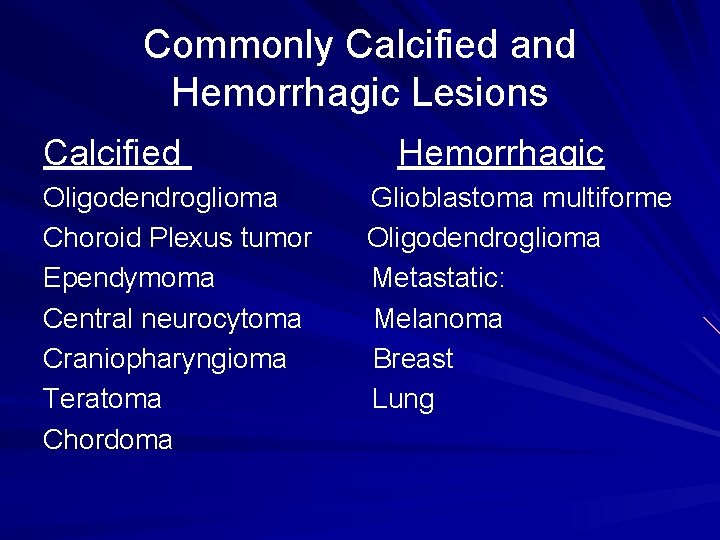
Why not MRI them all? ? ? - MRI is generally preferable to CT for evaluating intracranial neoplasms - CT is preferred for visualizing tumor calcification or intratumor hemorrhage.
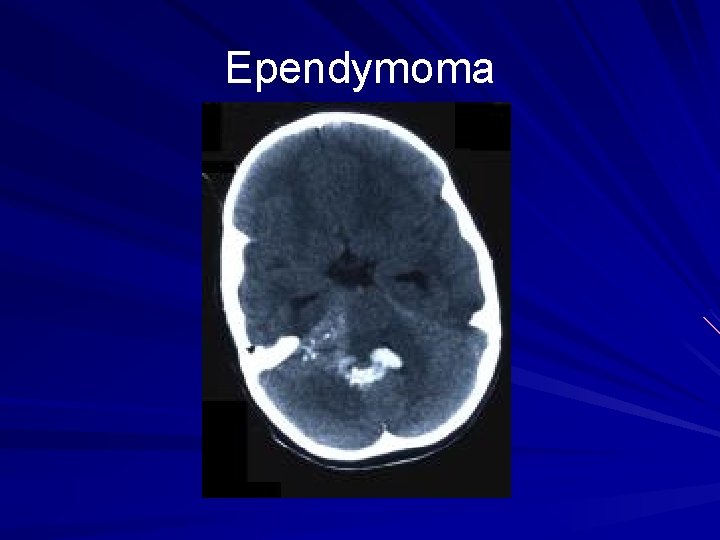
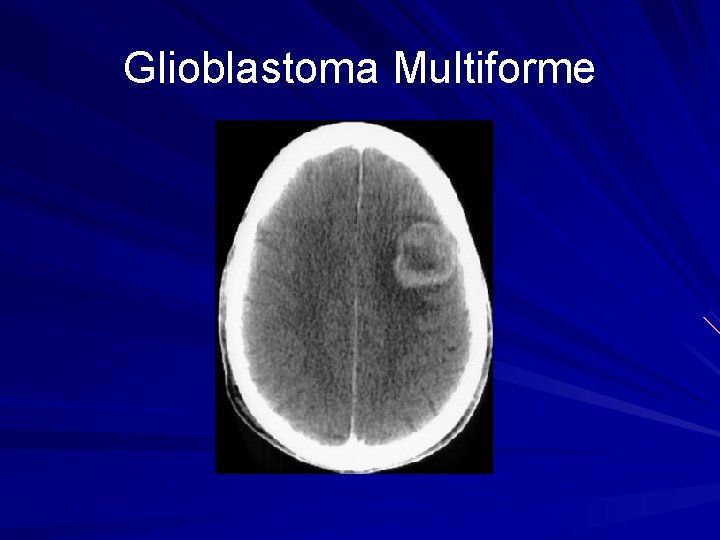
Commonly Calcified and Hemorrhagic Lesions Calcified Oligodendroglioma Choroid Plexus tumor Ependymoma Central neurocytoma Craniopharyngioma Teratoma Chordoma Hemorrhagic Glioblastoma multiforme Oligodendroglioma Metastatic: Melanoma Breast Lung
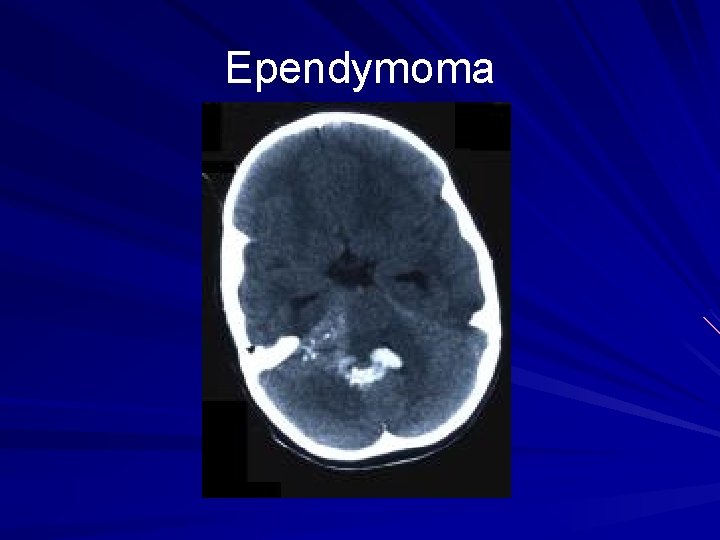
Ependymoma
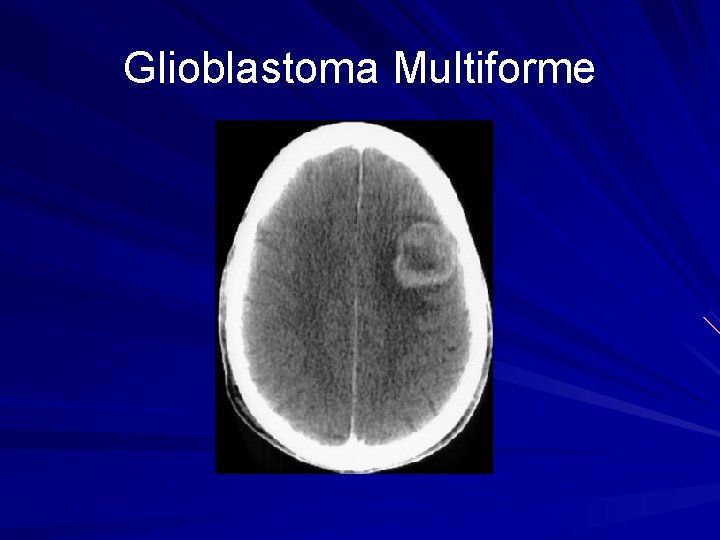
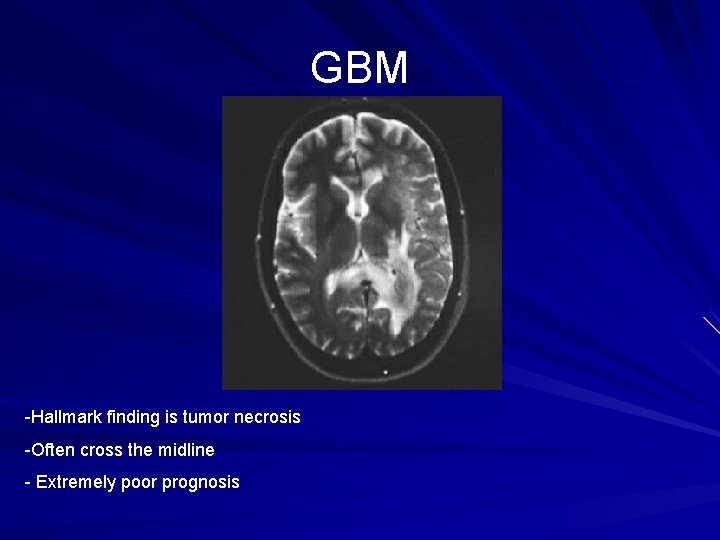
Glioblastoma Multiforme
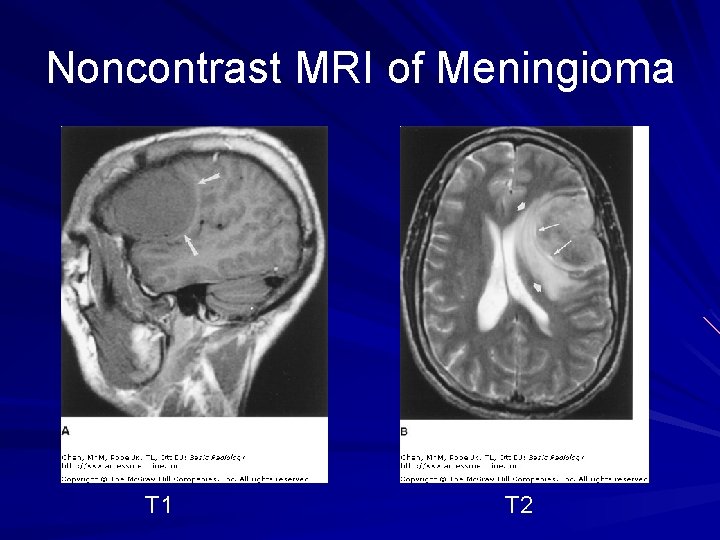
MRI - Usually the preferred method of imaging intracranial tumors due to better soft-tissue contrast - MRI exploits increased water content of many neoplasms. This water content shows up as increased signal on T 2 weighted images and decreased signal on T 1 Images.
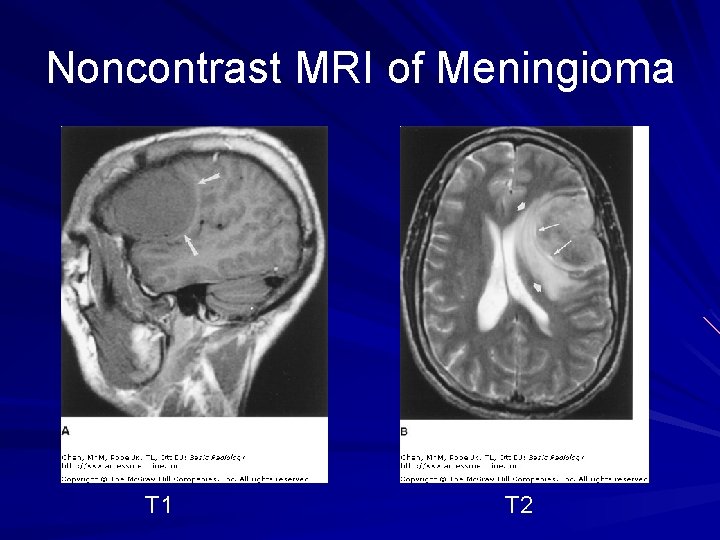
Noncontrast MRI of Meningioma T 1 T 2
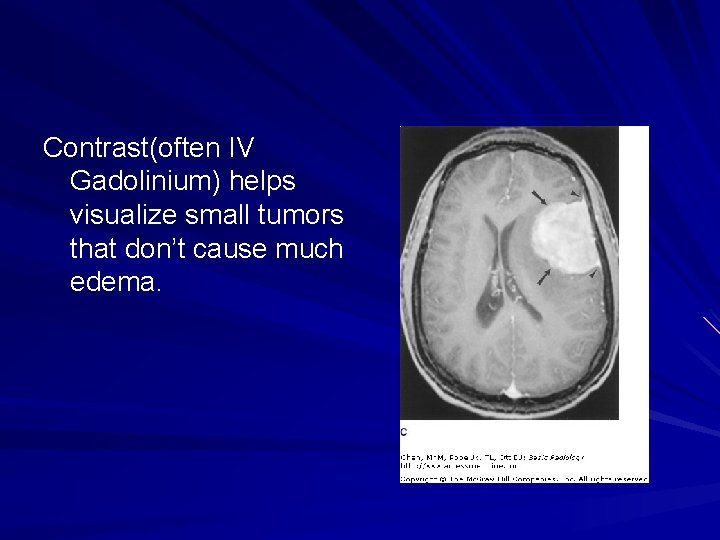
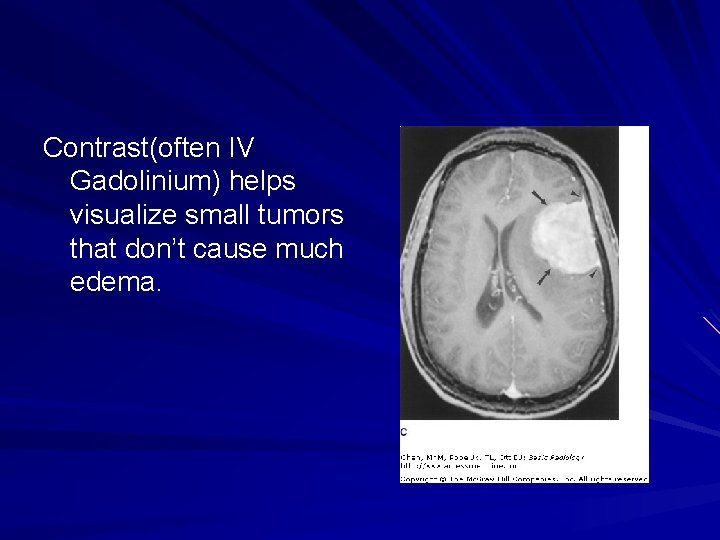
Contrast(often IV Gadolinium) helps visualize small tumors that don’t cause much edema.
Advanced MRI Techniques “This stuff is complicated!!!!”
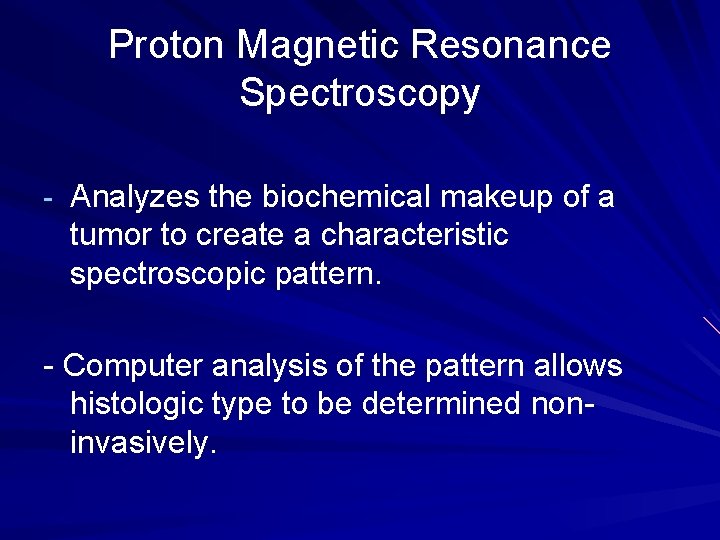
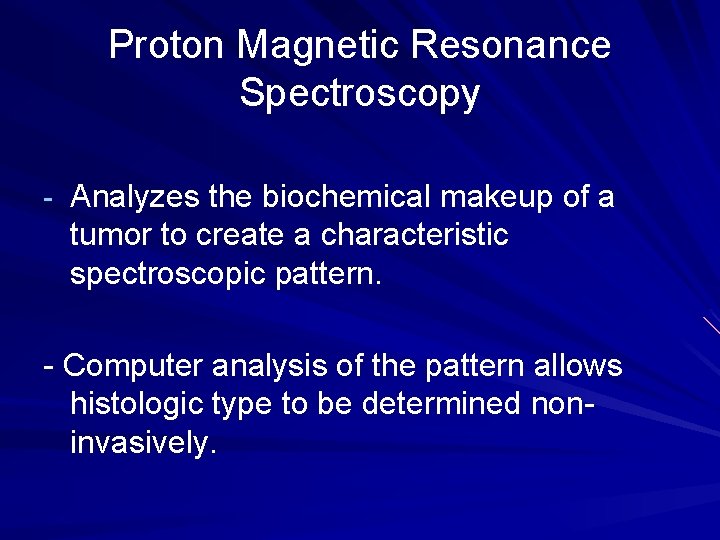
Proton Magnetic Resonance Spectroscopy - Analyzes the biochemical makeup of a tumor to create a characteristic spectroscopic pattern. - Computer analysis of the pattern allows histologic type to be determined noninvasively.
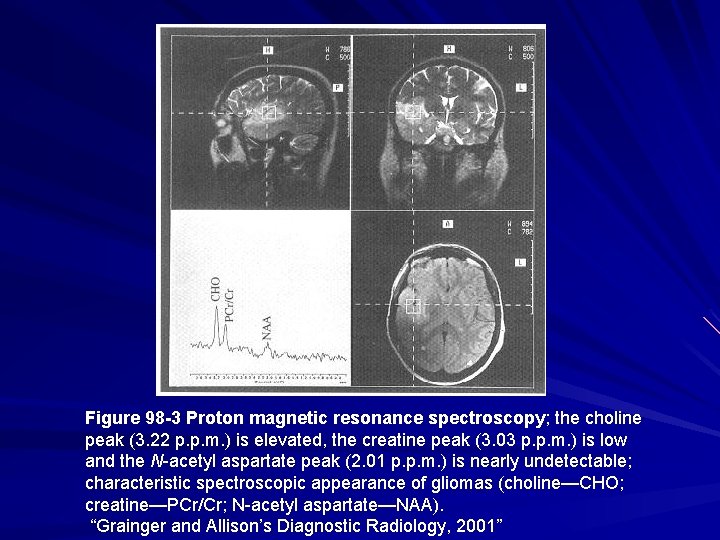
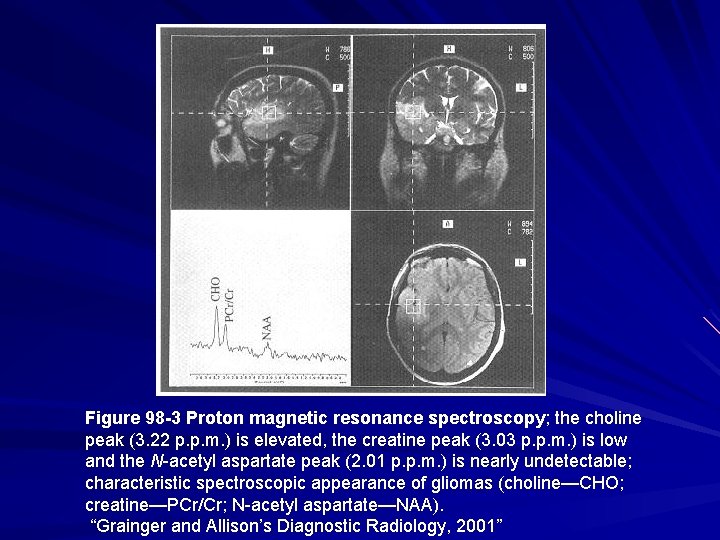
Figure 98 -3 Proton magnetic resonance spectroscopy; the choline peak (3. 22 p. p. m. ) is elevated, the creatine peak (3. 03 p. p. m. ) is low and the N-acetyl aspartate peak (2. 01 p. p. m. ) is nearly undetectable; characteristic spectroscopic appearance of gliomas (choline—CHO; creatine—PCr/Cr; N-acetyl aspartate—NAA). “Grainger and Allison’s Diagnostic Radiology, 2001”
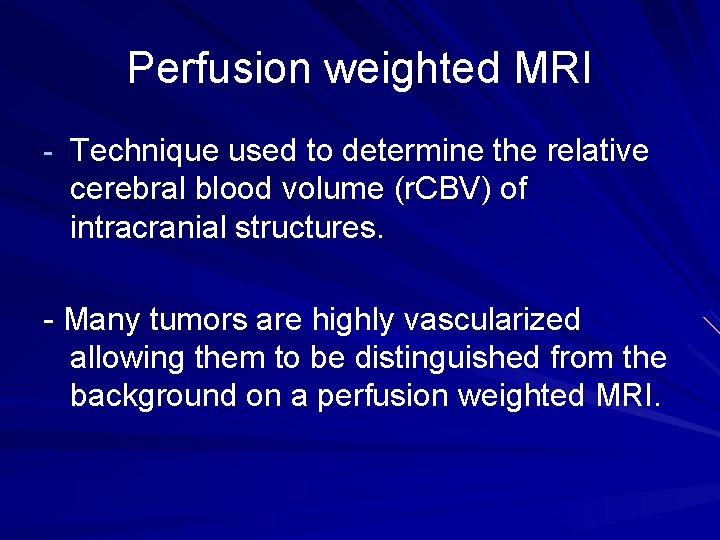
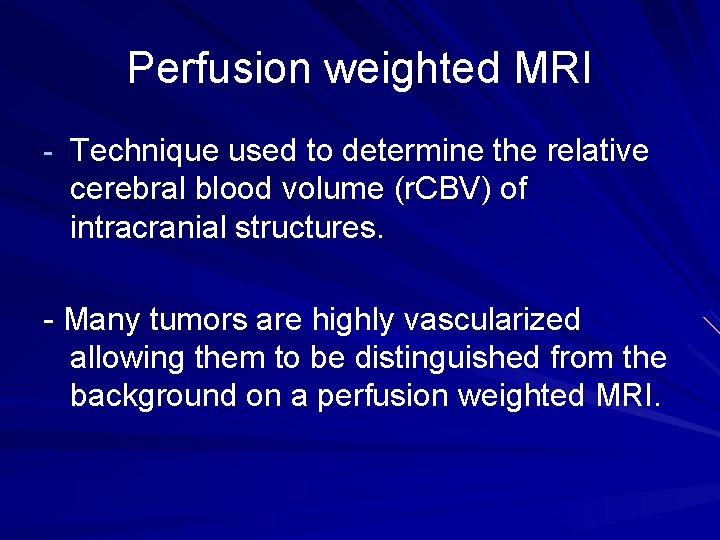
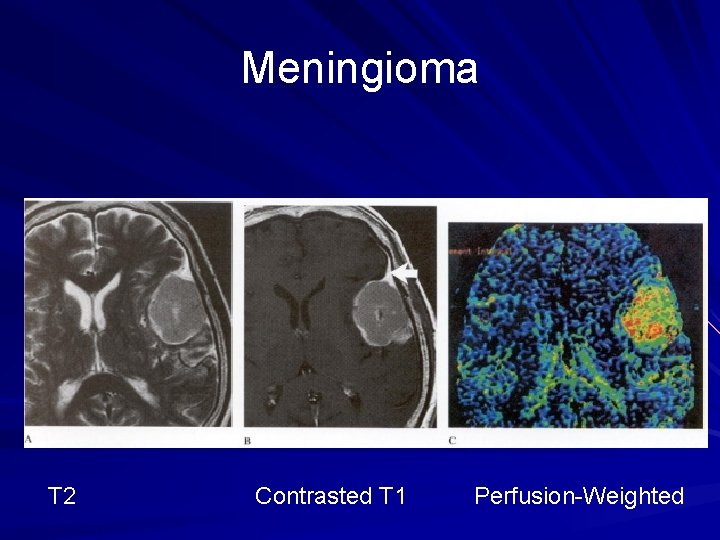
Perfusion weighted MRI - Technique used to determine the relative cerebral blood volume (r. CBV) of intracranial structures. - Many tumors are highly vascularized allowing them to be distinguished from the background on a perfusion weighted MRI.
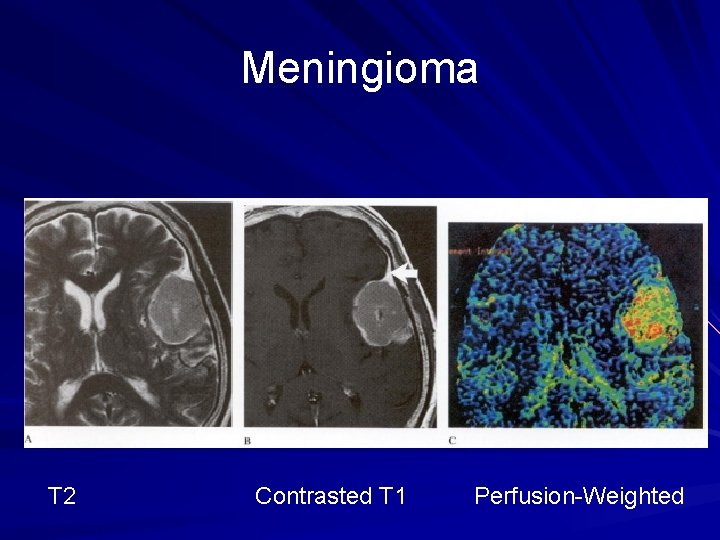
Meningioma T 2 Contrasted T 1 Perfusion-Weighted
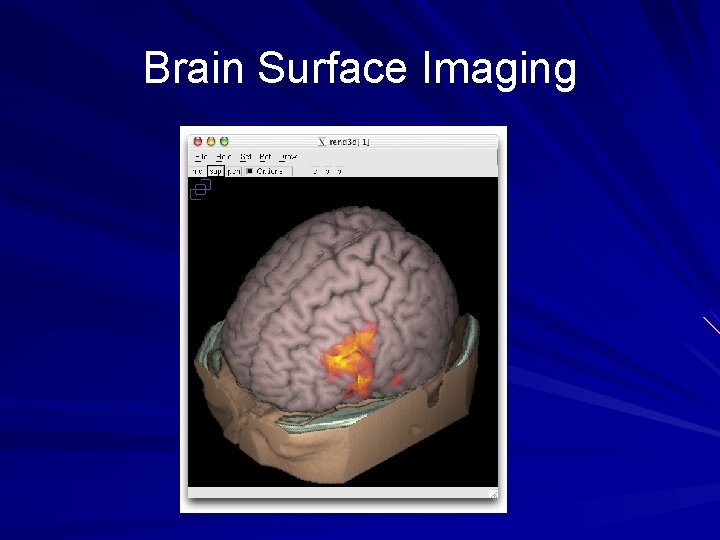
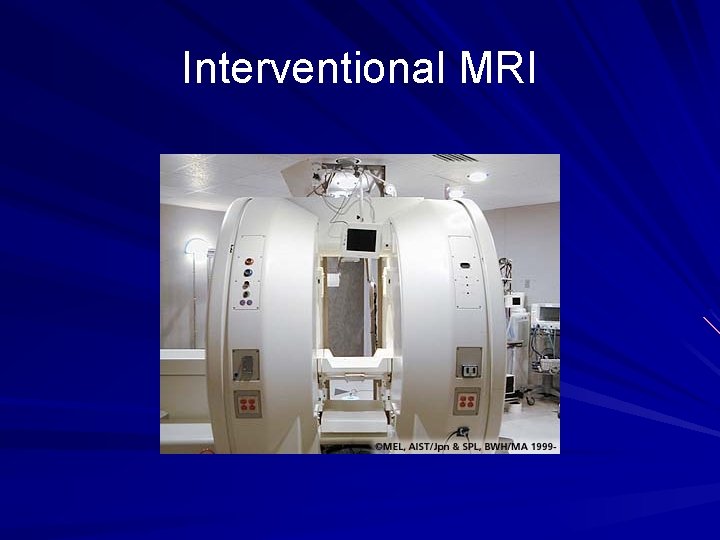
MRI-guided Surgery - A variety of techniques have been developed to incorporate MRI into the surgical process for intracranial tumor resection: MRI guided stereotactic biopsy Brain surface imaging Interventional MRI
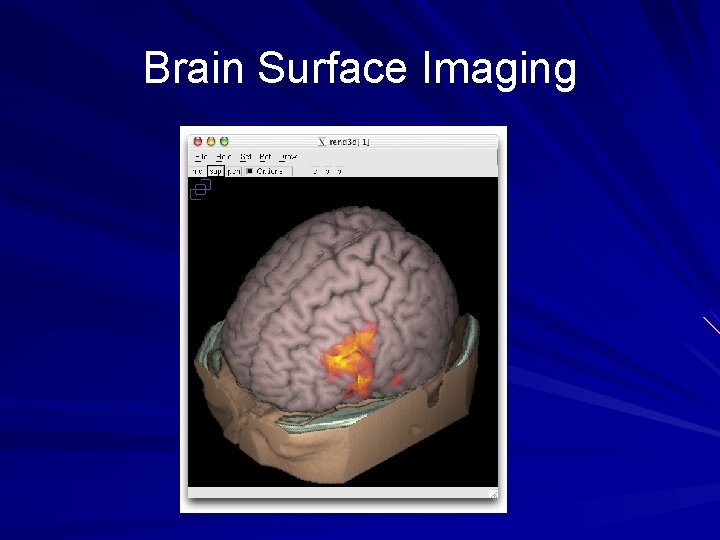
Brain Surface Imaging
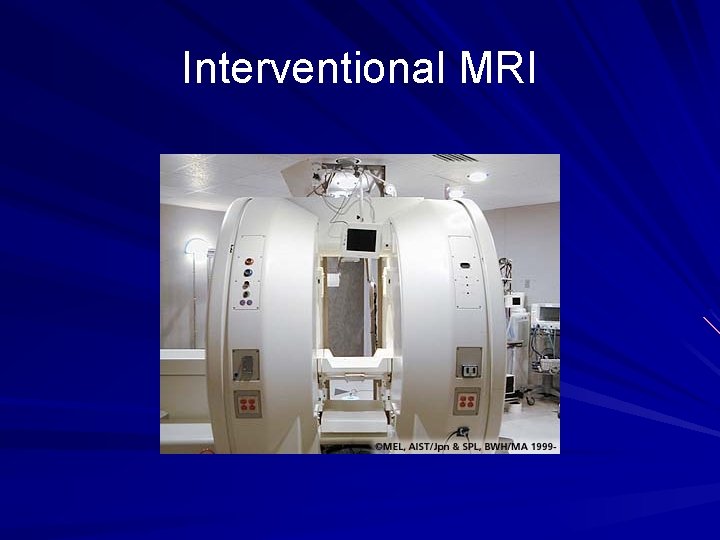
Interventional MRI
Nuclear Medicine SPECT(Single Photon Emission Computed Tomography) - Gamma rays emitted during radionuclide decay are detected by a gamma camera that rotates about the patient’s head - The radionuclides must cross the bloodbrain barrier
Radionuclides preferentially taken up by intracranial neoplasms include: 201 TI Chloride 99 m Tc MIBI 123 I a-methyl tyrosine 111 In octreotide - Can be used for example in distinguishing between benign lesions, low-grade gliomas, and high-grade gliomas
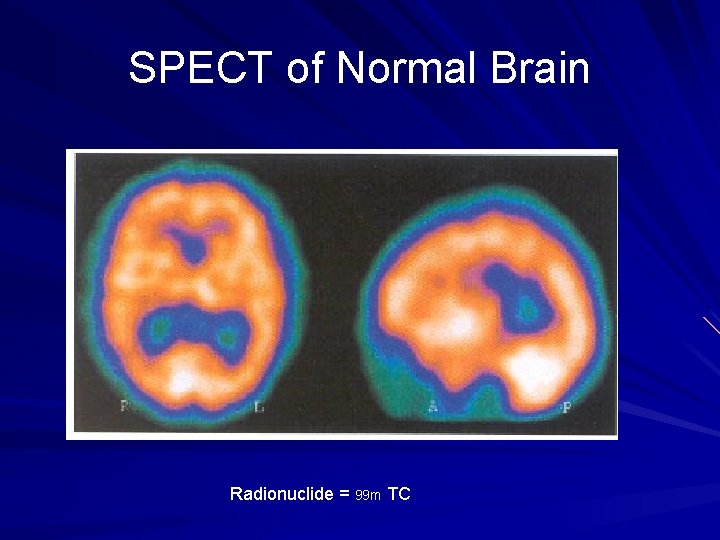
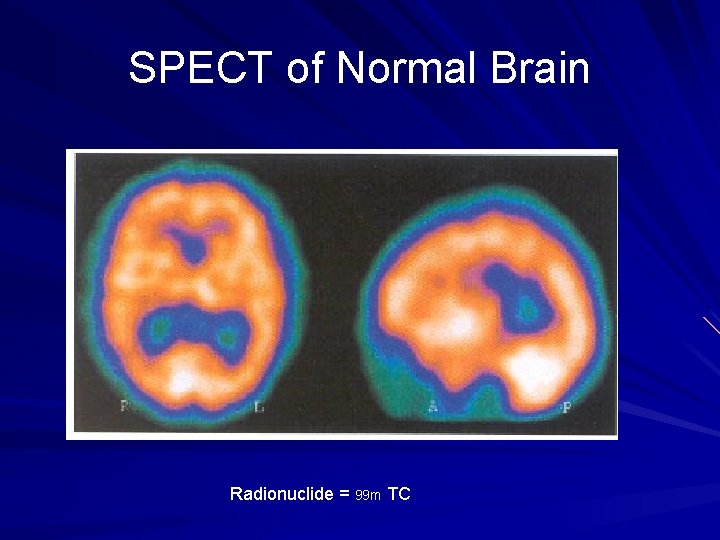
SPECT of Normal Brain Radionuclide = 99 m TC
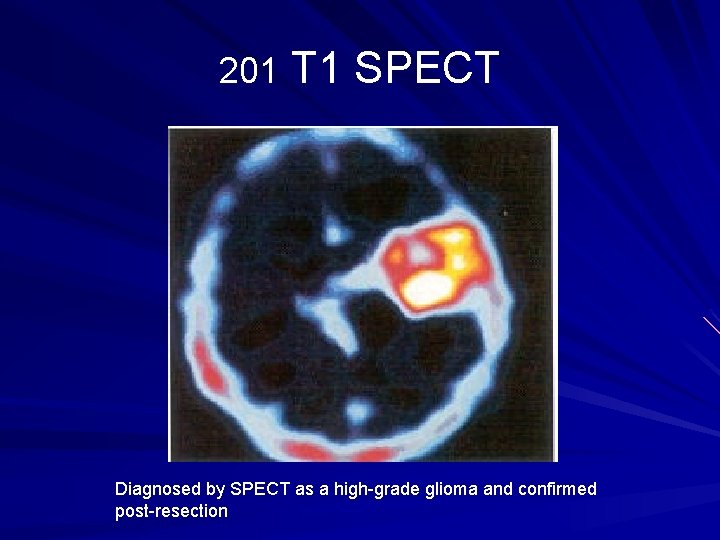
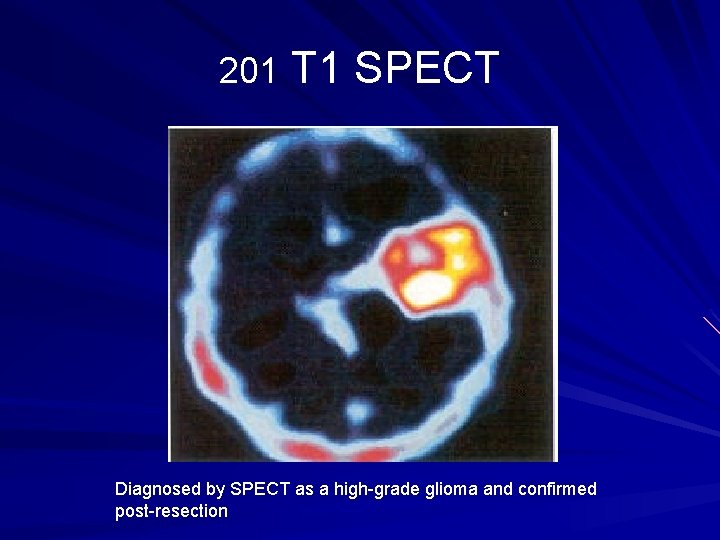
201 T 1 SPECT Diagnosed by SPECT as a high-grade glioma and confirmed post-resection
PET(Positron Emission Tomography) - Similar to SPECT but the radioisotopes used decay to produce positrons - These positrons quickly combine with an adjacent electron to produce two gamma rays that travel in opposite directions. Detection of these gamma rays allows calculation of their exact point of origin. - Can evaluate different brain processes depending on the radioisotope selected
Radionuclides useful for PET analysis of intracranial tumors include: Fluorodeoxyglucose C methionine F a-methyl tyrosine
Advantages of PET over SPECT: - Can be used to quantify emission - Better resolution Disadvantages of PET: - Cost - Limited availability - Need for a cyclotron(particle accelerator)
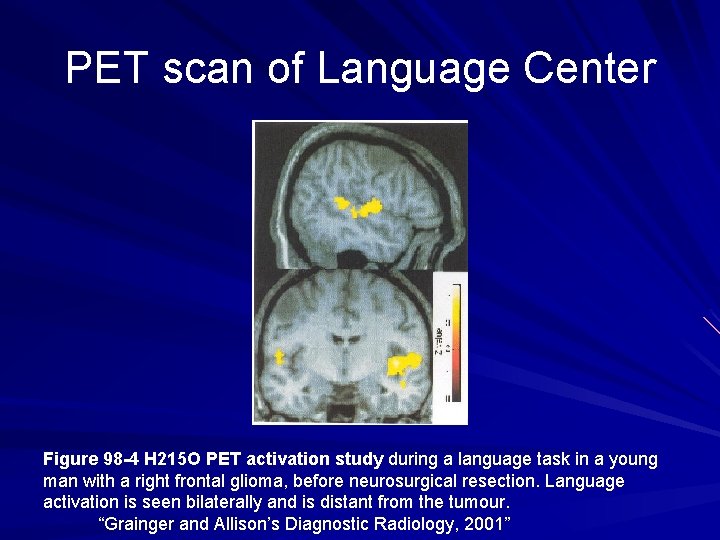
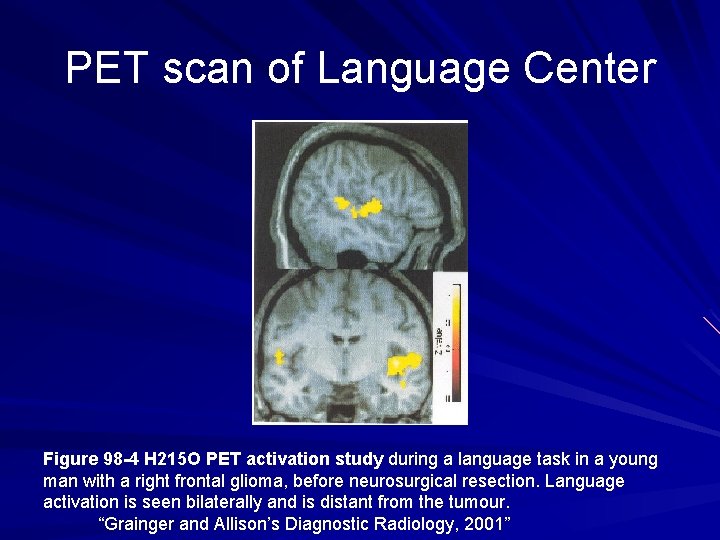
PET scan of Language Center Figure 98 -4 H 215 O PET activation study during a language task in a young man with a right frontal glioma, before neurosurgical resection. Language activation is seen bilaterally and is distant from the tumour. “Grainger and Allison’s Diagnostic Radiology, 2001”
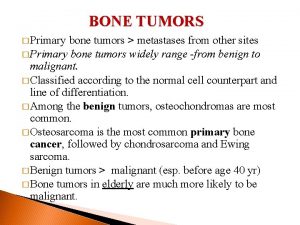
Classification of Intracranial Neoplasms 1)Neuroepithelial Origin – astrocytoma, oligodendroglioma, ependymoma, mixed glioma, choroid plexus tumor, neuronal tumor, pineal tumor. -Gliomas(astrocytomas, oligodendroglioma, ependymoma) = approximately 50% of primary brain tumors -Graded from 1 -4 based on severity -Grade 4 = Glioblastoma Multiforme – most common primary intracranial neoplasm
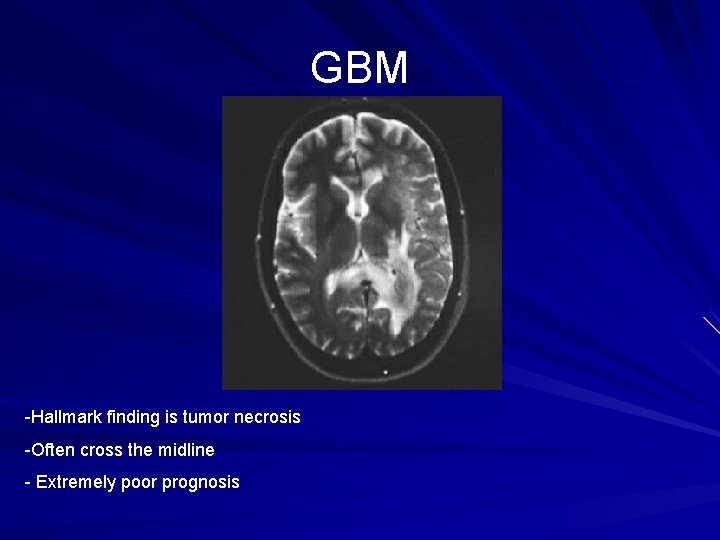
GBM -Hallmark finding is tumor necrosis -Often cross the midline - Extremely poor prognosis
2)Tumors of Nerve Sheath – Schwannoma, Neurofibroma - These are cranial nerve sheath tumors that show marked enhancement with IV contrast
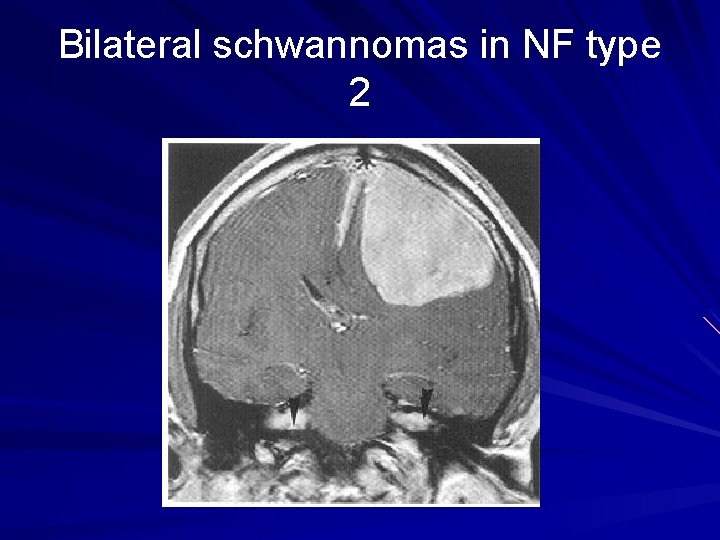
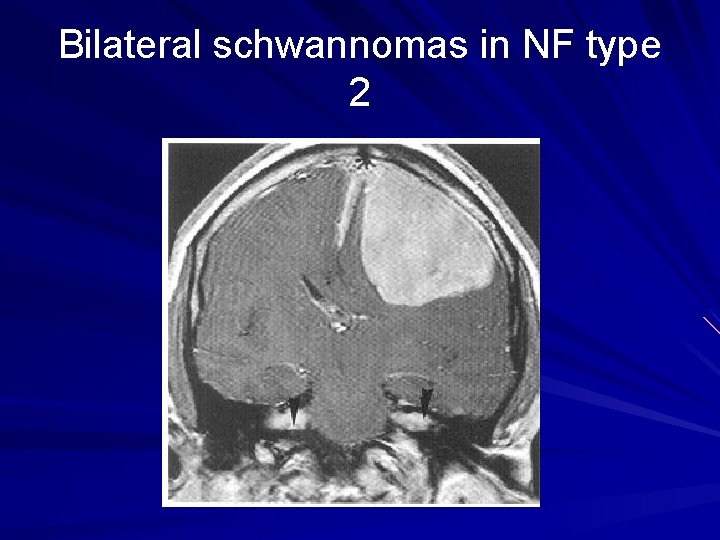
Bilateral schwannomas in NF type 2
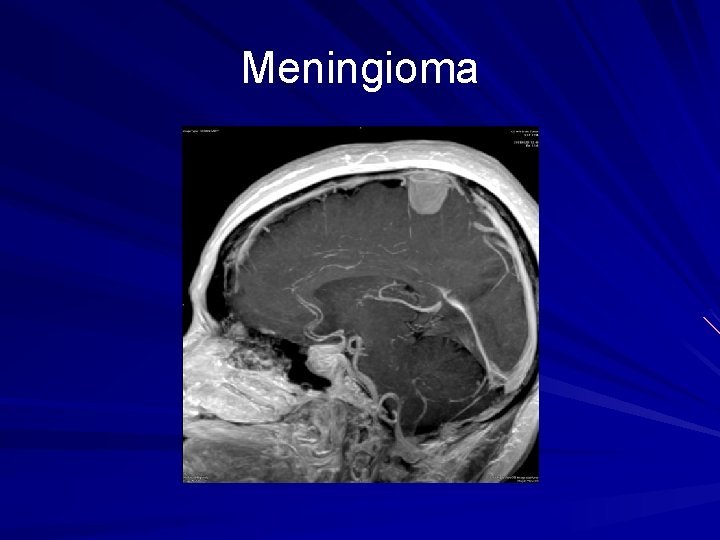
3)Meningeal tumors – meningioma - Originate from “arachnoid cell rests” in the dura matter - Commonly arise from parasagittal region, cerebral convexities, sphenoid ridge, and olfactory groove - Often contain calcifications and enhance well with IV contrast - Represents approximately 15% of primary intracranial tumors
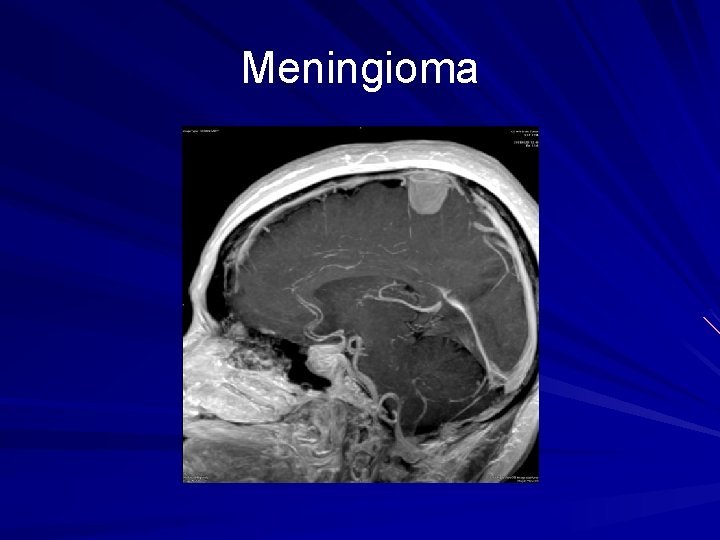
Meningioma
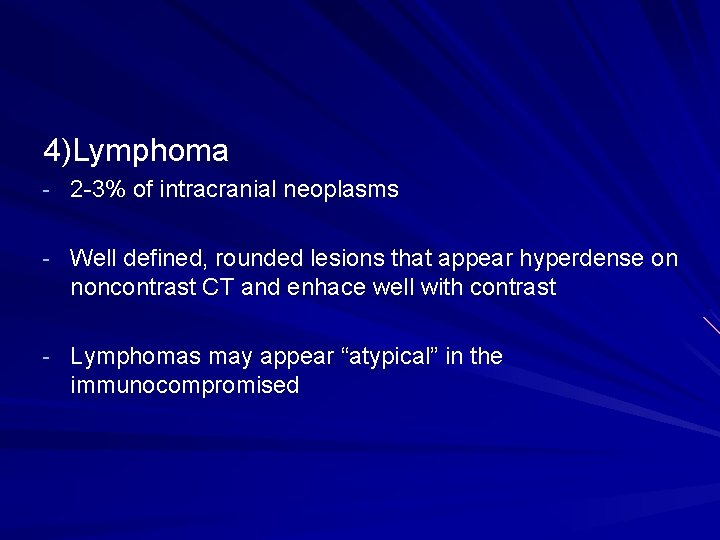
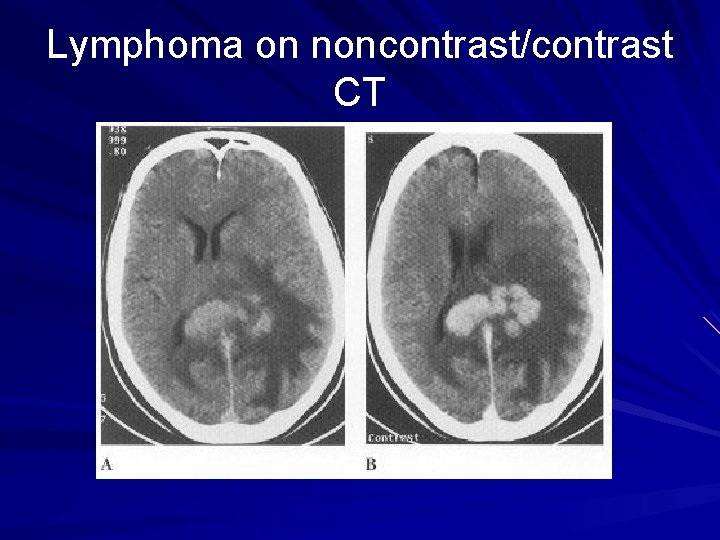
4)Lymphoma - 2 -3% of intracranial neoplasms - Well defined, rounded lesions that appear hyperdense on noncontrast CT and enhace well with contrast - Lymphomas may appear “atypical” in the immunocompromised
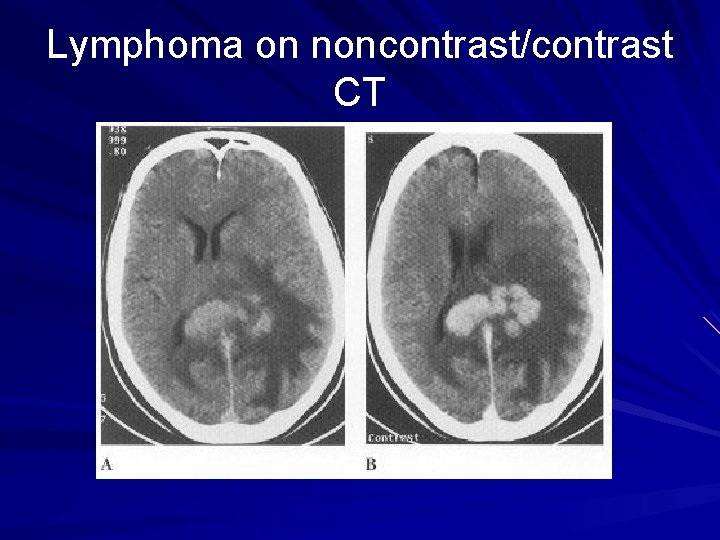
Lymphoma on noncontrast/contrast CT
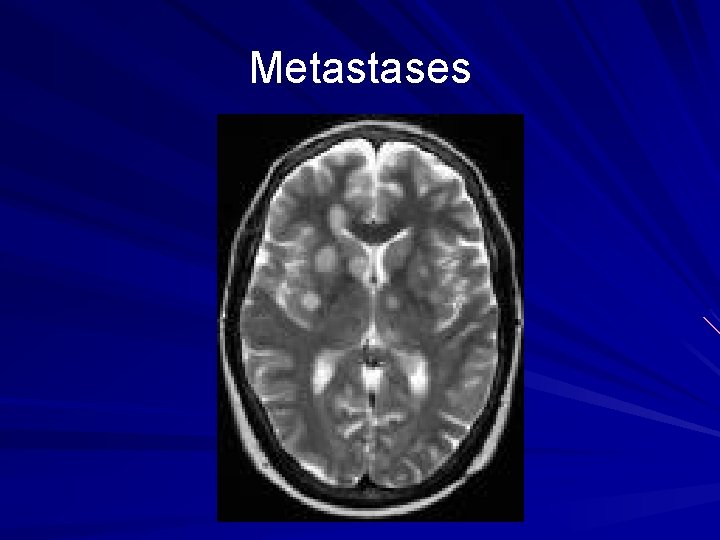
5)Metastasis - Usually multiple lesions which help distinguish them from supratentorial gliomas - Often found at grey/white matter junction
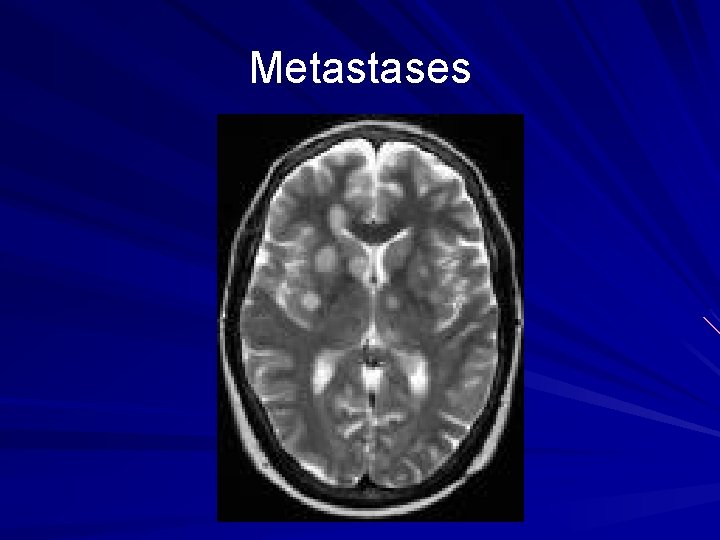
Metastases
6)Additional classes include: germ cell tumors, dermoid/epidermoid cysts, sellar/pituitary tumors,
Some famous people who have suffered from a brain tumor
References Harvard University Dept. of Radiology www. brighamrad. harvard. edu LSU Dept. of Radiology www. medschool. lsuhsc. edu University of South Carolina Dept. of Radiology www. radiology. med. sc. edu Grainger and Allison’s Diagnostic Radiology: A Textbook of Medical Imaging, 4 th ed. 2001 Churchill Livinstone Inc. , 2001.
 Response evaluation criteria in solid tumors (recist)
Response evaluation criteria in solid tumors (recist) Miv uc davis
Miv uc davis El camino radiology
El camino radiology Pharmacology and venipuncture in radiology pdf
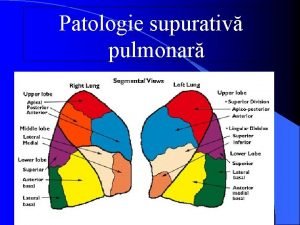
Pharmacology and venipuncture in radiology pdf Segmente pulmonare
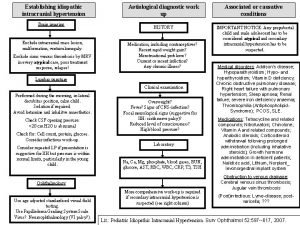
Segmente pulmonare Increased intracranial pressure ati
Increased intracranial pressure ati Cushing's triad vitals
Cushing's triad vitals Cushing reaction
Cushing reaction Intracranial teratoma
Intracranial teratoma How does meningitis cause increased intracranial pressure
How does meningitis cause increased intracranial pressure Intracranial hypertension
Intracranial hypertension Mosby
Mosby Adhesive arachnoiditis
Adhesive arachnoiditis Cushing's triad vitals
Cushing's triad vitals Neuropathey
Neuropathey Intracranial hypotension radiopedia
Intracranial hypotension radiopedia Intracranial mass
Intracranial mass Intracranial regulation nursing
Intracranial regulation nursing Decreased intracranial adaptive capacity nursing diagnosis
Decreased intracranial adaptive capacity nursing diagnosis Ameloblastoma rtg
Ameloblastoma rtg Mobile phone brain tumour
Mobile phone brain tumour Odontogenic tumors classification
Odontogenic tumors classification Exocrine tumors of pancreas
Exocrine tumors of pancreas Codman üçgeni
Codman üçgeni Thyroid tumors
Thyroid tumors Acromely
Acromely Teratoma
Teratoma Enneking staging
Enneking staging How many bones
How many bones Classification of tumors
Classification of tumors Paresthiasis
Paresthiasis Cervical ectropion
Cervical ectropion Odontogenic tumors
Odontogenic tumors Anterior ramus of spinal cord
Anterior ramus of spinal cord Classification of tumors
Classification of tumors Prostate adenocarcinoma perineural invasion
Prostate adenocarcinoma perineural invasion Malignant and benign tumors
Malignant and benign tumors Todd snide
Todd snide Todd tannenbaum
Todd tannenbaum Examen de la marcha
Examen de la marcha Dr todd baron
Dr todd baron Connor durrell
Connor durrell Vikram shakkottai
Vikram shakkottai Dr wilcox orthopedic
Dr wilcox orthopedic Todd sosna
Todd sosna Fast analytics
Fast analytics