Radiation Sources in Nuclear Medicine Accidents in Nuclear
- Slides: 32
Radiation Sources in Nuclear Medicine Accidents in Nuclear Medicine IAEA International Atomic Energy Agency Day 7 – Lecture 8
Objective To understand the consequences of accidents in nuclear medicine. IAEA 2
Contents • Deviation from prescribed dose; • Accidental medical exposure; • Case studies and lessons learned. IAEA 3
Accident An accident is “any unintended event, including operating errors, equipment failures or other mishaps, the consequences or potential consequences of which are not negligible from the point of view of protection and safety. ” [GSR Part 3 Definitions] IAEA 4
Accidental Medical Exposure In the event of an accident: “Registrants and licensees shall promptly investigate any of the following unintended or accidental medical exposures: (a) any therapeutic treatment delivered to either the wrong patient or the wrong tissue, or using the wrong pharmaceutical, or with a dose or dose fractionation differing substantially from the values prescribed by the medical practitioner or which may lead to undue acute secondary effects; ” [GSR Part 3 Requirement 41. 3. 179] IAEA 5
Accidental Medical Exposure (cont) In the event of an accident the licensee shall take action to: • estimate the dose received; • take measures to prevent a reoccurrence; • notify the Regulatory Body; • inform the patient and their doctor. IAEA 6
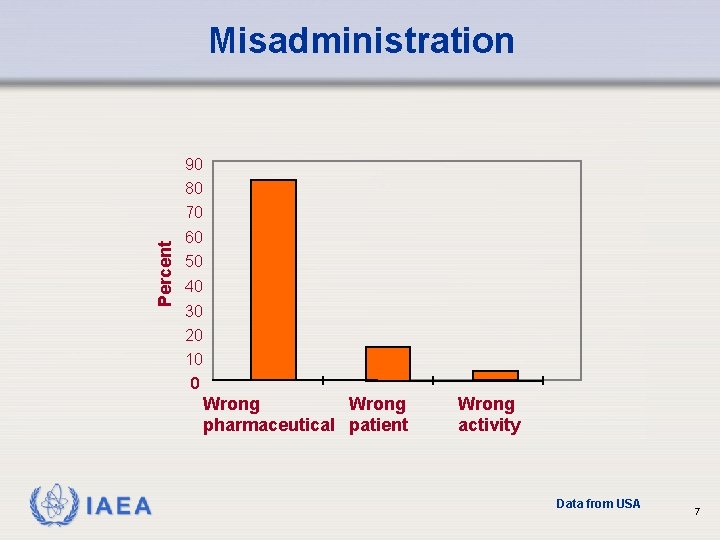
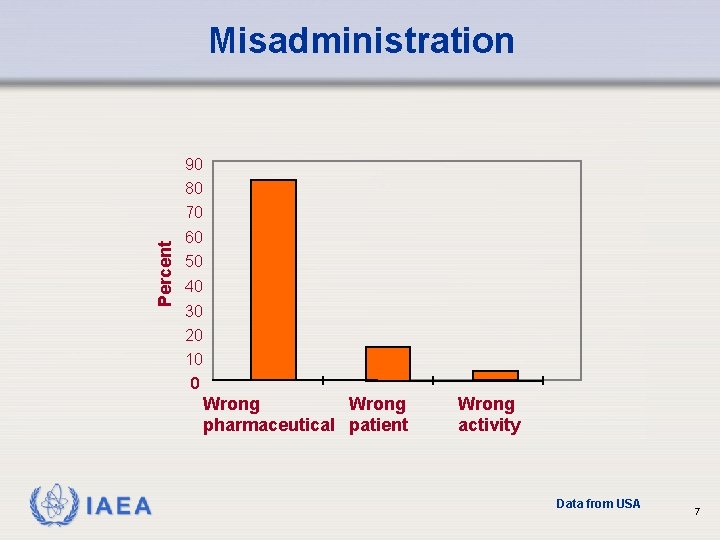
Misadministration 90 80 Percent 70 60 50 40 30 20 10 0 Wrong pharmaceutical patient IAEA Wrong activity Data from USA 7
Misadministration – Wrong Radiopharmaceutical • wrong patient; • wrong route of administration; • wrong activity: IAEA q therapy >10% from prescribed activity. q diagnosis > 50% from prescribed activity. 8
Misadministration – Wrong Patient • A therapy dose of 350 MBq 131 I was administered to patient A instead of patient B. Patient A had been prescribed 500 MBq 99 m. Tc for a bone scan. The 99 m. Tc was administered to A and the patient seated in the waiting room. • Patient B, who was scheduled for the 131 I treatment arrived later, completed an interview and was seated in the waiting room. The technologist prepared the 131 I and called patient B but patient A responded. • The technologist explained the treatment, scheduled a follow-up appointment and administered the activity. The patient then questioned the procedure and it became clear that the wrong patient had received the 131 I. IAEA 9
Misadministration – Wrong Patient (cont) • Patient A was immediately informed of the error and his stomach was pumped, retrieving about 1/3 rd the activity. The patient was administered perchlorate and Lugol’s solution to block further uptake by the thyroid. • The misadministration resulted in an absorbed dose to the thyroid of the wrong patient (A) of about 8 Gy. Initiating event: A patient responded to another patient’s name. Contributing factor: Hospital protocol for identification of patients was not followed IAEA 10
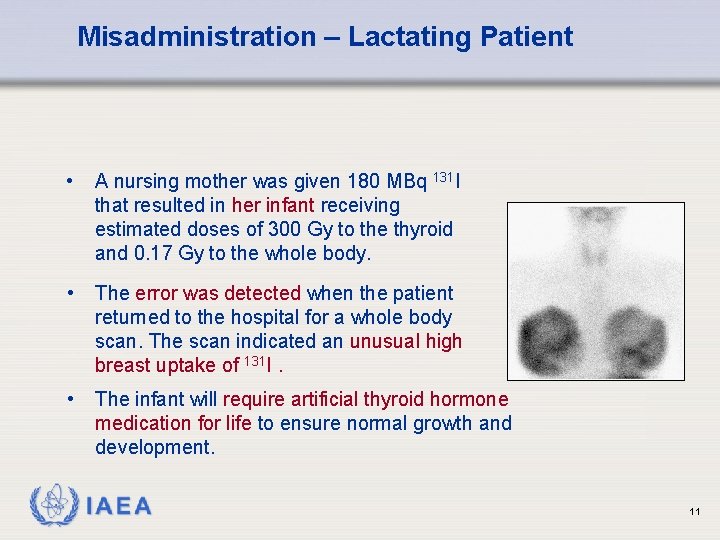
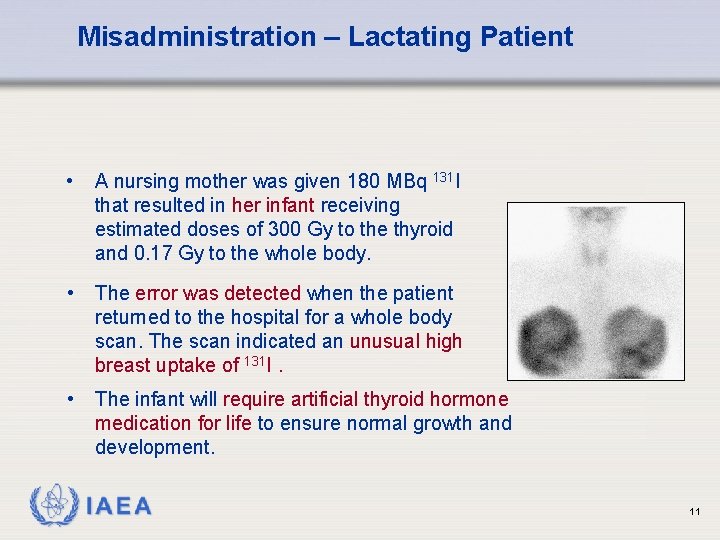
Misadministration – Lactating Patient • A nursing mother was given 180 MBq 131 I that resulted in her infant receiving estimated doses of 300 Gy to the thyroid and 0. 17 Gy to the whole body. • The error was detected when the patient returned to the hospital for a whole body scan. The scan indicated an unusual high breast uptake of 131 I. • The infant will require artificial thyroid hormone medication for life to ensure normal growth and development. IAEA 11
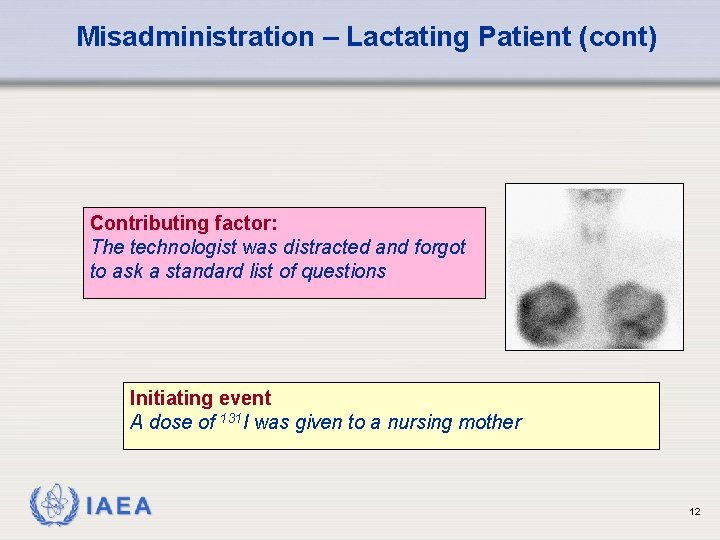
Misadministration – Lactating Patient (cont) Contributing factor: The technologist was distracted and forgot to ask a standard list of questions Initiating event A dose of 131 I was given to a nursing mother IAEA 12
Misadministration – Pregnant Patient A 43 year old female patient was scheduled for a thyroid scan. • • • She called the department in the morning and told the technologist that she was trying to get pregnant but there was no evidence at the moment that she was. The technologist misunderstood the patient and she was persuaded to undertake the examination. Later, it appeared that the patient was in the very early stages of pregnancy and subsequently had a miscarriage. IAEA 13
Misadministration – Pregnant Patient (cont) Contributing factor • Communication failure. • Inappropriate local rules. Initiating event Examination of a pregnant woman. IAEA 14
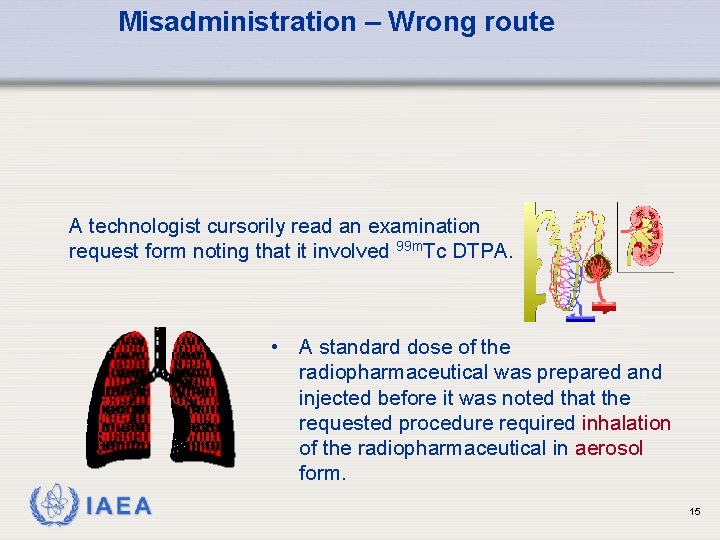
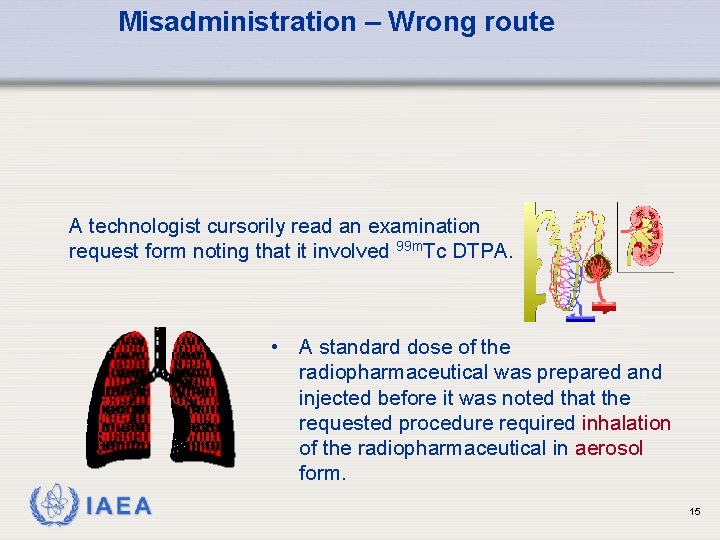
Misadministration – Wrong route A technologist cursorily read an examination request form noting that it involved 99 m. Tc DTPA. • A standard dose of the radiopharmaceutical was prepared and injected before it was noted that the requested procedure required inhalation of the radiopharmaceutical in aerosol form. IAEA 15
Misadministration – Wrong route (cont) Initiating event Wrong route of administration Contributing factor Failed to carefully read the request form IAEA 16
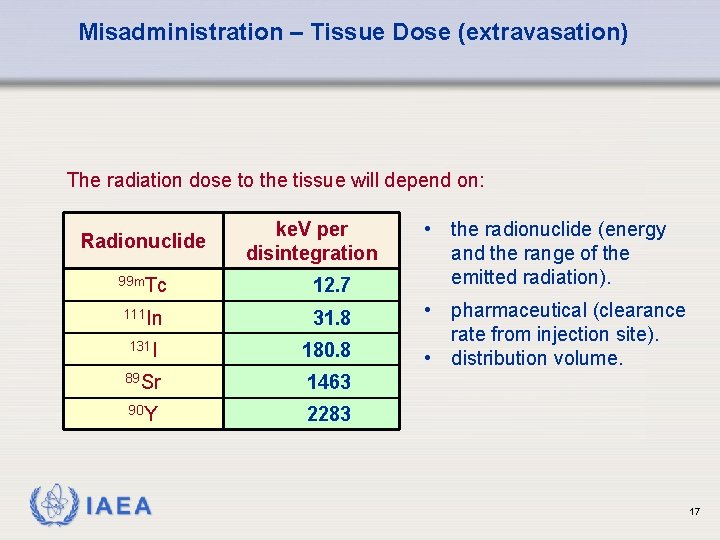
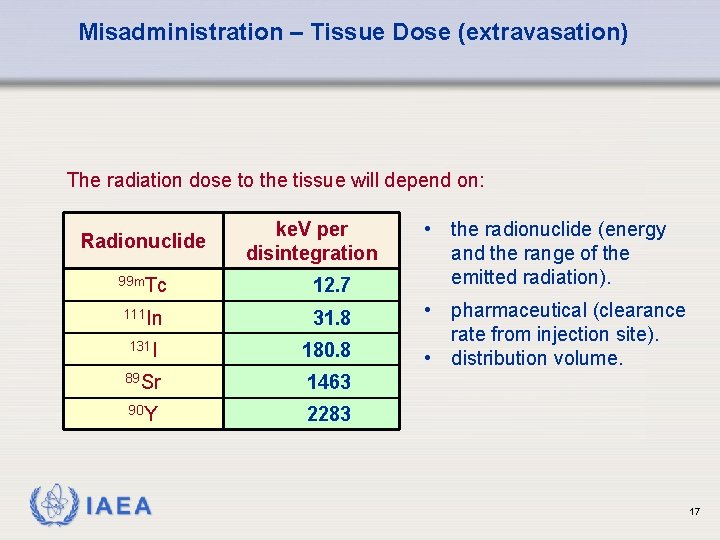
Misadministration – Tissue Dose (extravasation) The radiation dose to the tissue will depend on: Radionuclide ke. V per disintegration 99 m. Tc 12. 7 111 In 31. 8 131 I 180. 8 89 Sr 1463 90 Y 2283 IAEA • the radionuclide (energy and the range of the emitted radiation). • pharmaceutical (clearance rate from injection site). • distribution volume. 17
Misadministration – Wrong Activity A patient was to be administered 259 MBq 131 I. • The radiopharmaceutical was in two 130 MBq capsules and was so indicated on the vial label. • Previous doses at the hospital had been administered in the form of one 259 MBq capsule. • When the vial was inverted one of the two capsules fell out and the technologist assumed this was the entire dose. • Much later the other capsule was detected. The patient received only 50% of the prescribed activity. IAEA 18
Misadministration – Wrong Activity (cont) Contributing factor • Absence of cross check of the vial label with respect to both activity and number of capsules. • No measurement of the activity before treatment. Initiating event One of two capsules remained stuck in the vial IAEA 19
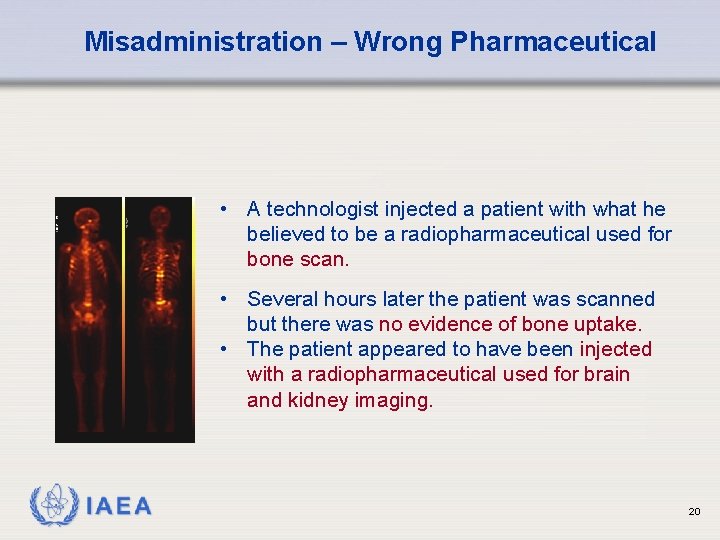
Misadministration – Wrong Pharmaceutical • A technologist injected a patient with what he believed to be a radiopharmaceutical used for bone scan. • Several hours later the patient was scanned but there was no evidence of bone uptake. • The patient appeared to have been injected with a radiopharmaceutical used for brain and kidney imaging. IAEA 20
Misadministration – Wrong Pharmaceutical (cont) Initiating event Wrong radiopharmaceutical Contributing factor Improper labeling of the radiopharmaceutical (syringe) IAEA 21
Misadministration Consequences • Non-justified exposure • Increased radiation risks • Delayed diagnosis • Increased costs • Increased workload • Reduced confidence IAEA 22
Misadministration counter measures Immediately use all available means to minimize any adverse effects, such as: • • expeditious removal of orally administered radiopharmaceuticals by emesis, gastric lavage, laxatives or enemas. accelerated excretion of intravenously administered radiopharmaceuticals by hydration, diuresis, etc. removal of urine by catheterization from patients who cannot void spontaneously. when appropriate, use of blocking agents to diminish the absorbed dose to the thyroid gland, salivary glands and stomach. IAEA 23
Misadministration causes • Communication problems. • • • Busy environment, distraction. Unknown local rules. No training in emergency situations. Not clearly defined responsibilities. No efficient Quality Assurance. IAEA 24
Avoiding Accidents and Misadministrations • Safety culture. • Safety assessment to define critical procedures and emergency situations. • Reporting system (When? Where? Why? ). • Education and training: q initial; q continuing. IAEA 25
Investigating accidental medical exposures • Inform the responsible nuclear medicine physician. • • • Inform the patient and the referring physician. Calculate the dose. Indicate the corrective measures to be taken. Implement those measures. Submit report to the licensee’s Radiation Protection Committee and to the Regulatory Body. IAEA 26
Lessons Learned • Communication errors. • Errors in patient identification. • Using the wrong radiopharmaceutical or the wrong activity. • Calibration errors and/or maintenance failure. Studies have shown that most accidents could have been prevented by consistent application of the Requirements 34 – 42 (3. 144 – 3. 184) of the GSR Part 3. IAEA 27
Accidents and Lessons Learned - Example An 87 year old patient was administered 7. 4 GBq 131 I to relieve esophageal compression caused by metastatic thyroid carcinoma. • • • About 34 hours after receiving the dose, the patient had a cardiopulmonary arrest and died. Attempts at resuscitation were made in the patient’s room by 16 staff members. The efforts included insertion of a pacemaker. Contaminated blood and urine were spilled and no surveys of the clothing of those present were done. The highest dose recorded was 0. 3 m. Gy for one nurse. Even though the contamination was extensive, subsequent thyroid uptake measurements showed no uptakes by involved staff. IAEA 28
Accidents and Lessons Learned – Example (cont) Initiating event Heart failure of patient shortly after iodine therapy Contributing factor • Contingency procedures for emergency situations involving radionuclides were not available. • Monitoring instruments and decontamination equipment were not available. No simulation exercises had been performed. IAEA 29
Medical Emergency Contact the RPO for specific instructions. Medical personnel should proceed with emergency care while attempting to take precautions against spread of contamination but: • avoid direct contact with the patient’s mouth, • all members of the emergency team should wear impermeable protective gloves. Medical personnel shall be informed and trained in procedures for dealing with a radioactive patient. IAEA 30
Medical Emergency (cont) Radiation protection considerations should not prevent or delay life -saving operations in the event surgery on the patient is required. However, the following precautions should be observed: • Notify the operating room staff. • Modify operating procedures under the supervision of RPO to minimize exposure and spread of contamination. • Protective equipment may be used as long as efficiency and speed is not affected. • Rotation of personnel may be necessary if the surgical procedure is lengthy. The RPO should monitor individual doses to members of the staff. IAEA 31
References • Manual on Radiation Protection in Hospitals and General Practice, Volume 4, Nuclear Medicine. IAEA/WHO. • Manual on therapeutic use of Iodine-131. Practical Radiation Safety Guide, IAEA 32
 Ionizing radiation sources
Ionizing radiation sources Ionizing radiation sources
Ionizing radiation sources Nuclear energy
Nuclear energy Nuclear radiation
Nuclear radiation Nuclear fission radiation
Nuclear fission radiation Types of radiation
Types of radiation What is nuclear radiation
What is nuclear radiation Print and web sources
Print and web sources Water resources importance
Water resources importance Mt sinai nuclear medicine
Mt sinai nuclear medicine Nuclear medicine information system
Nuclear medicine information system Filtered back projection
Filtered back projection Septal penetration artifact
Septal penetration artifact Case study conclusion
Case study conclusion Nuclear medicine lectures
Nuclear medicine lectures Lifestyle medicine
Lifestyle medicine Intranet
Intranet Ples phantom
Ples phantom Lesson 15 nuclear quest nuclear reactions
Lesson 15 nuclear quest nuclear reactions Fisión nuclear vs fision nuclear
Fisión nuclear vs fision nuclear Chapter 20 preventing kitchen accidents
Chapter 20 preventing kitchen accidents Accidents in construction industry
Accidents in construction industry Scissor aerial work platform
Scissor aerial work platform Av accidents
Av accidents Texte argumentatif sur les accidents de la route
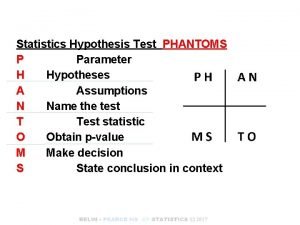
Texte argumentatif sur les accidents de la route Phantoms in statistics
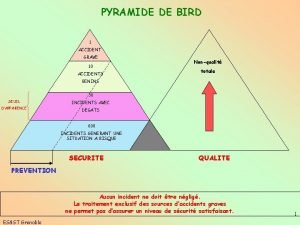
Phantoms in statistics Pyramide de bird exemple
Pyramide de bird exemple Chapter 14:1 using body mechanics
Chapter 14:1 using body mechanics Desinències verbals
Desinències verbals Industrial radiography accidents
Industrial radiography accidents 7 types of kitchen accidents
7 types of kitchen accidents Looked but failed to see
Looked but failed to see Statistiques accidents du travail d'origine électrique
Statistiques accidents du travail d'origine électrique