Radiation Sources in Radiotherapy Accidents in Radiotherapy IAEA
























- Slides: 58
Radiation Sources in Radiotherapy Accidents in Radiotherapy IAEA International Atomic Energy Agency Day 7 – Lecture 6
Objective To become familiar with the contributing factors that can led to unwanted exposure in radiotherapy. To be aware of investigation of accidents; case studies of accidental exposures in radiotherapy and lessons learned. Role of the Regulatory Body in case of accidents and emergencies in radiotherapy. IAEA 2

Contents • • • Potential for accidents in radiotherapy. Deviation from the prescribed dose. Potential exposures in external beam therapy. Potential exposures in brachytherapy. Case examples and lessons learned from accidental exposures in radiotherapy. • Role of the Regulatory Body. IAEA

Potential for accidents in radiotherapy Radiotherapy is unique from the point of view of radiation safety because: • it is the only use of radiation sources in which very high radiation doses are given deliberately to the human body. • not only the tumour, but also normal tissue receives radiation doses comparable to the tumour dose. IAEA 4

Potential for accidents in radiotherapy (cont) Potential Exposure “Prospective exposure that is not expected to be delivered with certainty but that may result from an anticipated operational occurrence, accident at a source or owing to an event or sequence of events of a probabilistic nature, including equipment failures and operating errors. ” [GSR Part 3 Definitions] IAEA

Deviations from the prescribed dose: • may involve severe or even fatal consequences; • require prompt investigation by licensees in the event of an accidental patient exposure. IAEA 6
Accidental Medical Exposure “Any medical treatment delivered to the wrong individual or the wrong tissue of the patient, or using the wrong radiopharmaceutical, or with an activity, a dose or dose fractionation differing substantially from (over or under) the values prescribed by the radiological medical practitioner, or that could lead to unduly severe secondary affects” “Any failure of medical radiological equipment, software failure or system failure, or accident error, mishap or other unusual occurrence with the potential for subjecting the patient to a medical exposure that is significantly different from what was intended. ” [GSR Part 3 Requirement 41. 3. 179] IAEA 7

Causes of accidents For external beam therapy, accidents may be related to: • equipment design; • beam calibration; • maintenance; • treatment planning; • dose calculation; • treatment simulation; • treatment setup and delivery. IAEA 8
Examples – Equipment Design An operator of a linear accelerator selected x-ray mode and then quickly changed to electron mode. The machine was unable to complete the first request (to operate in x-ray mode) and subsequently operated with “hybrid” instructions. The same accident occurred in 6 different hospitals and 2 patients died due to doses ranging from 160 -180 Gy Contributing factors • The software controlled linear accelerators were not tested for the conditions that occurred in practice at the hospitals. IAEA 9
Examples – Equipment Design (cont) An operator of a linear accelerator selected x-ray mode and then quickly changed to electron mode. The machine was unable to complete the first request (to operate in x-ray mode) and subsequently operated with “hybrid” instructions. The same accident occurred in 6 different hospitals and 2 patients died due to doses ranging from 160 -180 Gy. Contributing factors (cont) • The manufacturer took too long to identify the problem and to disseminate the information. By then the 6 hospitals had experienced the same failure and 2 patients had died from their radiation exposure. IAEA 10
Examples – Beam Calibration Accidents due to mistakes in properly determining the radiation dose rate have led to patient over-exposure, in some cases by as much as 60%. Other reported accidents have concerned misinterpretation of a calibration certificate and an atmospheric pressure correction factor; incorrect use of a plane-parallel ionization chamber; inadequate briefing of a replacement medical physicist. Contributing factors • Lack of understanding of beam calibration procedures, calibration certificates, conversion factors and dosimetry instruments. IAEA 11

Examples – Beam Calibration (cont) Contributing factors (cont) • Lack of training and expertise in radiotherapy physics; • Lack of redundant and independent determination of absorbed dose (mistakes were not detected); • Lack of formal procedures for communication and information exchange with new personnel. IAEA 12
Examples – Beam Calibration (cont) In one case verification of a 60 Co teletherapy beam had not been undertaken for 22 months. Contributing factors • The physicist responsible was fully engaged with a new linear accelerator and “ignored” the 60 Co unit. • Management did not review staffing needs when the new accelerator was installed. IAEA 13
Examples – Maintenance problems Incorrect adjustment of the electron energy of a linear accelerator resulted in 27 patients being over exposed. Doses were between 3 and 10 times greater than intended, causing several deaths. Contributing factors • A repair was made by a maintenance technician who did not understand the accelerator circuitry nor the consequences of incorrectly adjusting the electron energy (i. e. insufficient or incorrect training and experience). • The repair was not communicated to the medical physicist and patient treatments resumed without beam verification. IAEA 14

Examples – Maintenance problems (cont) Contributing factors (cont) • It was possible to operate the machine with the energy selector disabled. • Conflicting displays and signals on the control panel were misinterpreted (the energy selector indicated a different energy to the instrument on the control panel). IAEA 15
Examples – Maintenance problems (cont) Operation of a linear accelerator in “physics” mode for treatments resulted in one death. Contributing factors Repeated, intermittent and unresolved equipment faults were interrupting treatments. The radiation oncologist took a decision to operate the accelerator in “physics” mode which bypassed safety interlocks. IAEA 16
Examples – Treatment planning Accident relating to the commissioning of the Treatment Planning System (TPS) leading to wrong doses to many patients. • A distance correction was applied manually but the TPS already had the data in the computer plan. This error resulted in underexposure of over 1000 patients by as much as 30%. • Other accidents were related to entering incorrect data into the TPS computer. Contributing factors • Insufficient understanding of the TPS (no staff training on the new equipment for treatment planning); IAEA 17
Examples – Treatment planning (cont) Contributing factors (cont) • Lack of an independent check of the dose planning (either by manual calculations to selected points or by measurement on a phantom, or by “in vivo” dosimetry); • Lack of formal commissioning of the TPS (no test before using the TPS for treating patients). IAEA 18
Examples – Treatment Simulation Anatomical error with identification of the patient’s left and right sides interchanged. Contributing factors • the treatment was simulated in an unusual position; • there was no check of the anatomical site relative to the check film. IAEA 19
Examples – Treatment set up and delivery Treatment of the wrong patient, wrong site, giving the wrong treatment, applying the wrong treatment schedule. Contributing factors • Lack of procedures for proper identification of the patient, the anatomical site or the treatment schedule; • procedures not followed rigorously. IAEA 20

Causes of accidents Brachytherapy accidents may be related to: • Equipment design; • Source order and delivery; • Source calibration and acceptance; • Source preparation for the treatment; • Treatment planning and dose calculation; • Source removal. IAEA 21
Examples – Equipment Design and testing Sources were dislodged from the drive mechanism of a high dose rate (HDR) remote after loading device and remained in the patient. The patient died from the radiation dose. Contributing factors • The HDR device apparently was not adequately tested for conditions such as a source train jammed in the catheter or a kinked catheter. IAEA 22
Examples – Equipment Design and testing (cont) Contributing factors (cont) • Conflicting signals - the HDR device indicator was showing “source shielded” while an area monitor indicated the presence of radiation. The wrong signal was accepted. • The external radiation monitor had a history of malfunctions and was not trusted. • A portable survey instrument was not used to confirm the return of the sources to the HDR device after the treatment. IAEA 23

Examples – Source orders, delivery, etc Different units of activity were used by the hospital (m. Ci) and the manufacturer (mg-Ra-equivalent). This led to a patient receiving a radiation dose 74% greater than prescribed. In three cases, patients received less than the prescribed dose due to the use of sources without a check on the source activity. Contributing factors • Different activity units were used by the hospital and manufacturer; • Insufficient check of documents (order and delivery); • A source calibration check was not undertaken before use (source strength determination). IAEA 24

Examples – Treatment planning Errors in treatment time calculations ranged from - 59% to + 49%. Contributing factors • Copies of an obsolete form were still available for clinical use; • Records did not include the treatment distance relevant to the treatment time calculations; • Miscommunication between the radiation oncologist, physicist and others (a treatment plan was modified but an unmodified plan was used); • Lack of independent verification of treatment time calculations. IAEA 25
Examples – Source preparation • Wrong sources were used resulting, in one instance, of treatment with less than 50% of the prescribed dose; • In one case the manufacturer delivered a source with essentially no activity; • Two 192 Ir sources were lost; • A leaking 125 I source was re-used; • Sources withdrawn from clinical use were used with incompatible applicators. IAEA 26

Examples – Source preparation (cont) Contributing factors • Personnel handling sources and applicators lacked proper training; • Source activity was not verified; • Failure to properly audit the inventory of radiation sources; • Source leakage was not detected during preparation. A similar incident in another hospital had not triggered a check action; • Sources withdrawn from clinical use were re-used by mistake. IAEA 27
Examples – Delivery of treatment • a resident physician did not implant all prescribed sources; • a wrong patient was treated; • a source ribbon was dislodged from the catheter and was taped by a nurse on the face of the patient; • sources became displaced; • sources were removed by the patient; • a source that did not match the applicator was loose and fell out of the applicator. IAEA 28
Examples – Delivery of treatment (cont) Contributing factors • untrained physician working without supervision; • nurses without appropriate training were caring for brachytherapy patients; • no written safety procedures; • poor communication of instructions that were not understood. IAEA 29
Examples – Source removal • Sources lost due to lack of appropriate checks after removal. Contributing factors • Sources were not accounted for after removal; • The patient, their clothes, the room and waste from the treatment room were not monitored. IAEA 30

Lessons learned Studies have shown that most accidents could have been prevented by consistent application of the Requirements 34 – 42 (3. 144 – 3. 184) of the GSR Part 3. IAEA 31

Accidents in radiotherapy Human error resulting in a therapeutic treatment delivered: • to the wrong patient • to the wrong treatment site • with a substantially different dose, or dose fraction, to that prescribed by the medical practitioner Equipment malfunction IAEA 32

The Panama accident This accident, investigated by the IAEA, occurred at a facility that provided radiotherapy for cancer patients. • In keeping with common practice, the facility used blocks of shielding material to modify the shape of the radiation beams to protect normal tissue, including critical structures, during treatment. IAEA 33
The Panama accident (cont) • A computerized treatment planning system (TPS) was used to calculate the dose distribution and determine treatment times. • The TPS allows a maximum of four shielding blocks per field to be taken into account when calculating treatment times and dose distributions. • The data for each shielding block should have been entered into the TPS separately. IAEA 34
The Panama accident (cont) • In August 2000, to satisfy the request of a radiation oncologist to include five blocks in the field, the method for digitizing the shielding blocks was changed. • It was found that it was possible to enter data into the TPS for multiple shielding blocks together, as if they were a single block, thereby apparently overcoming the limitation of four blocks per field. IAEA 35

The Panama accident (cont) • Although the TPS accepted entry of the data for multiple shielding blocks as if they were a single block, the computer output indicated a treatment time substantially longer than it should have been. • The result was that patients received a proportionately higher dose than that prescribed. • The modified treatment protocol was used for 28 patients, treated between August 2000 and March 2001 for prostate cancer and cancer of the cervix. IAEA 36
The Panama accident (cont) • In November 2000, a radiation oncologist started to observe unusually prolonged diarrhoea in some patients. In December 2000, the effect was observed in other patients. • The Department’s physicists reviewed the treatment plans but did not find any anomaly. • The computer outputs (dose distribution and treatment time) calculations were not checked. IAEA 37
The Panama accident (cont) The outcome at 30 May 2000 • 8 of the 28 patients dead. q 5 deaths - radiation related. q 2 deaths - unknown if radiation related. q 1 death due to metastatic cancer. • 20 patients surviving. IAEA

The Panama accident (cont) • “Additional radiation effects will become apparent in the affected patients over the next months and years and, given the radiation doses received, the morbidity and mortality can be expected to increase. ” • “Most of the surviving patients already have serious medical problems related mainly to bowel and bladder overexposure. Most of the untoward bowel and bladder effects cannot be remedied. ” IAEA Investigation of an Accidental Exposure of Radiotherapy Patients in Panama IAEA Vienna 2001 39
The Panama accident (cont) Compliance with legislation The radiotherapy department of the facility applied for authorization in 1997 but this had not been granted by the time of the accidental exposure, pending the resolution of several outstanding issues. Records showed that the Regulatory Body had issued a number of reminders to the department since 1997: • requesting information, principally the manuals of procedures for radiation protection and quality assurance. IAEA 40
The Panama accident (cont) Compliance with legislation (cont) • A number of brachytherapy sources from the facility were found to be in use in a different hospital without authorization; • An incident had occurred in which a cobalt therapy source had not returned to the ‘OFF’ (shielded) position, risking excessive radiation exposure of staff and patients. No radiation oncologist was present at the hospital at the time. The Regulatory Body sent a letter to the facility reminding it of its obligation to have at least one radiation oncologist always present when patients are being treated. IAEA 41

The Panama accident (cont) The event was triggered by: • the search for a way to overcome the limitation to four shielding blocks. Contributory factors • Several different ways of digitizing the shielding blocks were accepted by the computer; • There was no warning on the computer screen when the blocks were digitized in an unacceptable way i. e. in a way different to that prescribed in the manual; IAEA 42

The Panama accident (cont) • When blocks were digitized incorrectly, the TPS produced a diagram which was the same as that produced when data were entered correctly, thereby giving the impression that the calculated results were correct. • The modified protocol was used without a verification test i. e. without a manual calculation of the treatment time for comparison with the computer calculated treatment time, or a simulation of treatment by irradiating a water phantom and measuring the dose delivered. • Although the treatment times were about twice those required for correct treatment, the error went unnoticed. IAEA 43
Not an isolated event • More than 90 cases of accidental exposures in radiotherapy have been documented. • Accidents have occurred in both brachytherapy and external beam radiotherapy. • Accidents occur in both developed and developing countries IAEA 44
Consequences in practice If the dose: • is too low - reduction of tumor control probability. There is no second chance! • is too high – risk of acute complications and late complications. There is less likelihood that an accident will occur where a country has a functioning regulatory system. However, these countries may be over-represented in accident summaries possibly because all (? ) accidents are actually reported. IAEA 45

Lessons learned “Registrants and licensees shall promptly investigate any of the following unintended or accidental medical exposures: (a) any therapeutic treatment delivered to either the wrong patient or the wrong tissue, or using the wrong pharmaceutical, or with a dose or dose fractionation differing substantially from the values prescribed by the medical practitioner or which may lead to undue acute secondary effects; ” [GSR Part 3 Requirement 41. 3. 179] IAEA 46

Lessons learned from the Panama accident • Treatment planning is a critical aspect of treatments. • Written procedures are required. • New procedures must be tested - including documentation. • Computer calculations should be verified manually. • Treatment planning software should include: q an instruction manual; q on-screen warnings; q fool-proof tests. IAEA 47
Lessons learned from the Panama accident (cont) • Ongoing communication with the treatment device manufacturer is important for both service and staff training. • Radiotherapy facilities must be appropriately resourced (staffing, equipment etc) in keeping with the patient workload. • The licensee, responsible medical practitioner, RPO and senior staff must encourage a strong safety culture in all personnel through appropriate supervision and interaction. • Directions from the Regulatory Body must be complied with promptly. IAEA 48
Investigation of accidents • Minor accidents should be investigated by the licensee and the results, along with the corrective actions, reported to the Regulatory Body. • The Regulatory Body should prescribe the types of accidents and incidents that must be reported. • For more serious, or potentially serious accidents and emergencies, an independent investigation by the Regulatory Body (and sometimes also by other government authorities) should be conducted in addition to the investigation conducted by the user. IAEA 49
Investigation of accidents (cont) • Determine the root causes and contributing factors. • Assess the consequences in terms of exposure and the likelihood of exposure of: q exposure of patient, staff (or public) • Identify corrective actions. • Derive the lessons to be learned and the significance of the findings for other radiotherapy facilities. IAEA 50

What action should the Regulatory Body take in response to a lost radioactive source? If a therapy radioactive source is no longer on-site and no longer under the licensee’s control (through poor inventory control, improper transfer or disposal, theft etc) and that loss is confirmed, the Regulatory Body should immediately inform government and initiate the appropriate emergency response plan. Consider the need for wider national and international notification IAEA 51
What action should the Regulatory Body take in response to a reported accident or incident? Determine if an inspection is necessary to obtain first-hand information of the cause of the accident or incident. The licensee’s report should be reviewed (in collaboration with other authorities and government agencies, if appropriate to the circumstances) IAEA 52
What action should the Regulatory Body take in response to a reported accident or incident? Determine how similar accidents or incidents can be best avoided in future and recommend corrective measures. Determine what enforcement action, if any, may be appropriate IAEA Accidents and Incidents 53
What action should the Regulatory Body take in response to a reported accident or incident? Particularly in cases where injury (or the perceived risk of injury) may lead to litigation, determine the potential health outcomes, responsibility and liability (under the radiation safety legislation) for the accident or incident. IAEA 54

What action should the Regulatory Body take in response to a reported accident or incident? Disseminate the findings of the investigation to all relevant clients, organizations and professional associations. IAEA 55

References • IAEA Human Health Series No. 14 Planning National Radiotherapy Services. IAEA, Vienna 2010 • Setting Up a Radiotherapy Programme: Clinical, Medical Physics, Radiation Protection and Safety Aspects. IAEA, Vienna 2008 • IAEA-TECDOC-1040 Design and implementation of a radiotherapy programme: Clinical, medical physics, radiation protection and safety aspects IAEA 56

References (cont) • Medical Handling of Accidentally Exposed Individuals. IAEA Safety Series No. 88 • Event No. 8: “Calibration error after a source change in a 60 Co unit. ” • Event No. 20: “Design error in accelerator control software. ” • Event No. 70: “Inadequate implantation and loss of sources. ” IAEA 57
References (cont) • Radiation Protection and Safety of Radiation Sources: International Basic Safety Standards. Generic Safety Requirements. GSR Part 3 (Interim) Vienna (2011) • IAEA Safety Guide: Radiological Protection for Medical Exposure to Ionizing Radiation (Safety Standards Series No. RS-G-1. 5, 2002) IAEA 58
 Radiotherapy
Radiotherapy Pterigiums
Pterigiums Mayneord factor equation
Mayneord factor equation Radiotherapy
Radiotherapy Ssd and sad technique in radiotherapy
Ssd and sad technique in radiotherapy Siemens radiotherapy
Siemens radiotherapy Sújb
Sújb Ionizing radiation sources
Ionizing radiation sources Natural sources of radiation
Natural sources of radiation Print and web sources
Print and web sources Imp of water resources
Imp of water resources Nuclear wastes
Nuclear wastes Iaea
Iaea Iaea
Iaea Iaea livechart
Iaea livechart Gsr part 7
Gsr part 7 Iaea
Iaea Iaea gsr part 2
Iaea gsr part 2 Steel scrap
Steel scrap Iaea gsr part 4
Iaea gsr part 4 Pcmf
Pcmf Pcmf
Pcmf Stefano monti iaea
Stefano monti iaea Ssr5
Ssr5 Iaea
Iaea Rtc protective film
Rtc protective film Film badge dosimeter
Film badge dosimeter Iaea
Iaea Saris iaea
Saris iaea Iaea
Iaea An investigation of the therac-25 accidents
An investigation of the therac-25 accidents Industrial radiography accidents
Industrial radiography accidents Accidents sportifs statistiques
Accidents sportifs statistiques Momentum conservation law
Momentum conservation law Accidents & disasters
Accidents & disasters Av accidents
Av accidents Take away any liquid near your working area true or false
Take away any liquid near your working area true or false Chapter 20 preventing kitchen accidents
Chapter 20 preventing kitchen accidents Accidents in construction industry
Accidents in construction industry Scissor aerial work platform
Scissor aerial work platform Texte argumentatif sur les accidents de la route
Texte argumentatif sur les accidents de la route An insurance company checks police records on 582 accidents
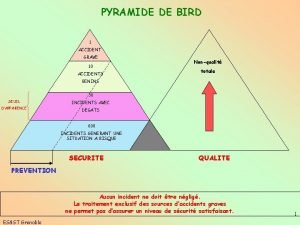
An insurance company checks police records on 582 accidents Diagramme de bird
Diagramme de bird Industrial radiography accidents
Industrial radiography accidents Chapter 14 promotion of safety
Chapter 14 promotion of safety Desinències verbals
Desinències verbals Accidents/illness of family members
Accidents/illness of family members Kitchen safety choking
Kitchen safety choking Looked but failed to see
Looked but failed to see Statistiques accidents du travail d'origine électrique
Statistiques accidents du travail d'origine électrique What is theatre safety
What is theatre safety Preventing kitchen accidents worksheet
Preventing kitchen accidents worksheet Goal freedom alertness theory
Goal freedom alertness theory Accidents & disasters
Accidents & disasters Chapter 13:2 preventing accidents and injuries
Chapter 13:2 preventing accidents and injuries Chapter 5 defensive driving
Chapter 5 defensive driving Adaptive radiation
Adaptive radiation Examples of radiation
Examples of radiation Example of radiation
Example of radiation