Nuclear medicine Essential idea Nuclear radiation whilst dangerous
- Slides: 27
Nuclear medicine Essential idea Nuclear radiation, whilst dangerous owing to its ability to damage cells and cause mutations, can also be used to both diagnose and cure diseases.
Nuclear medicine • Uses radionuclides: unstable nucleii that spontaneously decay emitting radiation (energy and particles) to form more stable nucleii. • Radionuclides can be natural or produced by bombarding nucleii with subatomic particles. • How are these nuclides used?
Radiotherapy • Use of ionizing radiation as emitted by radionuclides to treat diseases (radiotherapy) such as cancer by destroying the cancer cells. • Also used to diagnose a disease by providing detailed information in the form of images (nuclear imaging) about internal organs affected by the disease. • Radioisotopes or radionuclides have an unstable nucleus that decays spontaneously into a more stable form by emitting radiation either in the form of subatomic particles or energy.
Radiotherapy can be … • Internal: radionuclides are placed in the human body to target a particular cancerous tissue or group of receptors. Internal radionuclides are administered orally as a solid or as a liquid (e. g. I-131), as an implant or injected in the case of some liquid radionuclides. • External: radiation source remains outside the human body and the beams of radiation (beta or gamma rays, photons or neutrons) target specific cancerous tissues in the body. A commonly used radionuclide for this approach is Co-60.
Effect of nuclear radiation on cells Removes electrons from atoms in biological molecules converting them into ions (ionizing radiation) that form reactive radicals (H and OH ) that interfere with physiological processes. This causes genetic damage which can lead to cell death, mutations and cancer because: o Break structure of DNA. o Changes to the structure of the DNA within the genes of cells (genetic damage) (mutations). o A reduced ability of cells to repair DNA damage. o Limited growth and regeneration of the cells/tissue.
Effect on cancerous cells Same effect as described in previous slide but cancerous cells are affected more by radiation than normal cells so targeted radiotherapy (internal or external) is on obvious choice for the treatment of cancer.
Side effects Ionizing radiation also affects normal cells but some cells more than others in particular cells that divide rapidly such as hair follicle cells, sex cells and cells in the skin causing more damage to the DNA and reducing growth. Some side effects: hair loss, damage to skin and nails, nausea, fatigue and sterility. Issue: ionizing radiation can be used for diagnosis and treatment of cancer but can also cause it!!
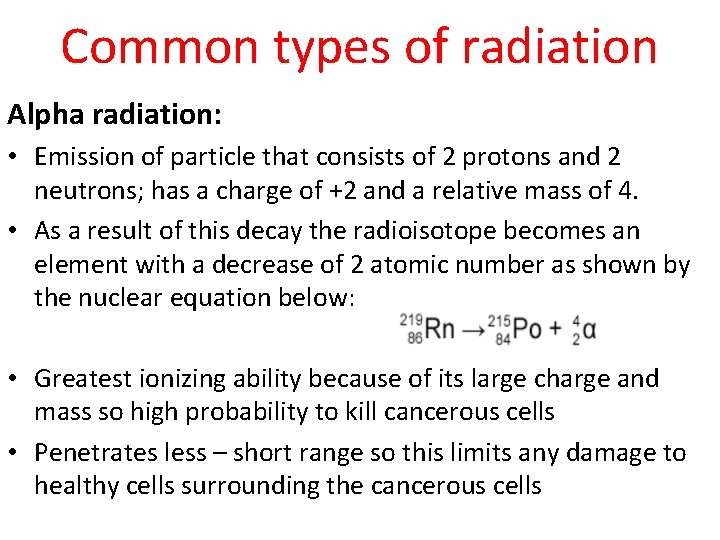
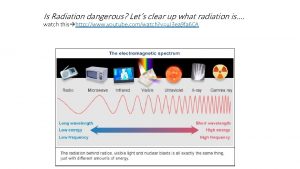
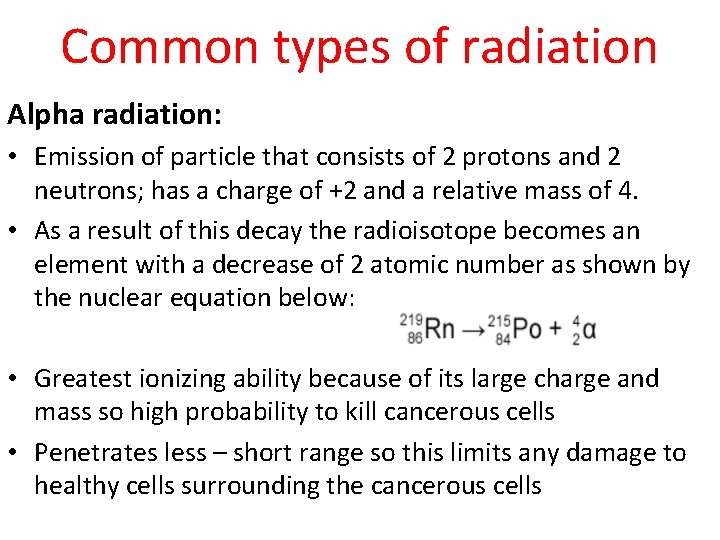
Common types of radiation Alpha radiation: • Emission of particle that consists of 2 protons and 2 neutrons; has a charge of +2 and a relative mass of 4. • As a result of this decay the radioisotope becomes an element with a decrease of 2 atomic number as shown by the nuclear equation below: • Greatest ionizing ability because of its large charge and mass so high probability to kill cancerous cells • Penetrates less – short range so this limits any damage to healthy cells surrounding the cancerous cells
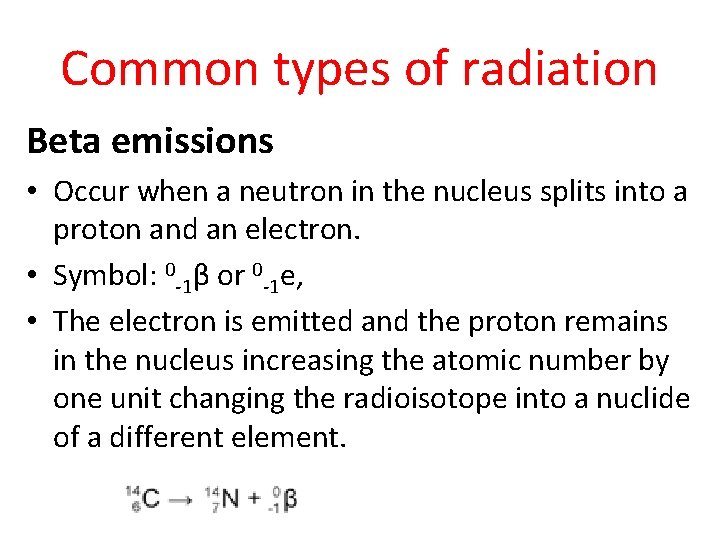
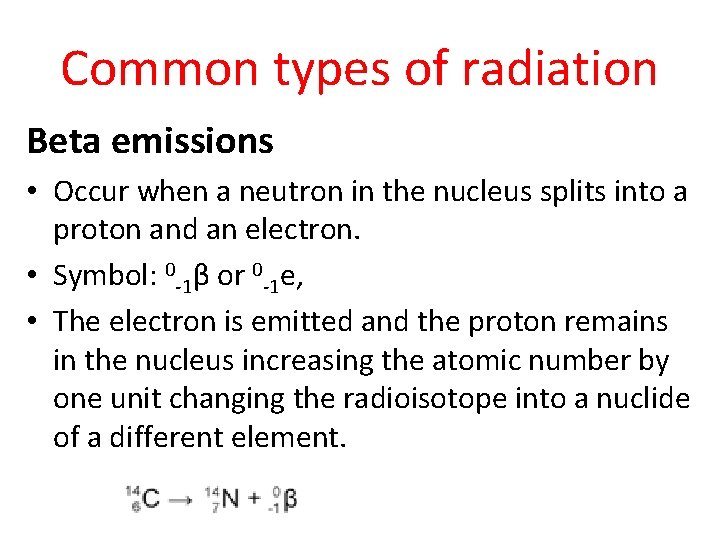
Common types of radiation Beta emissions • Occur when a neutron in the nucleus splits into a proton and an electron. • Symbol: 0 -1β or 0 -1 e, • The electron is emitted and the proton remains in the nucleus increasing the atomic number by one unit changing the radioisotope into a nuclide of a different element.
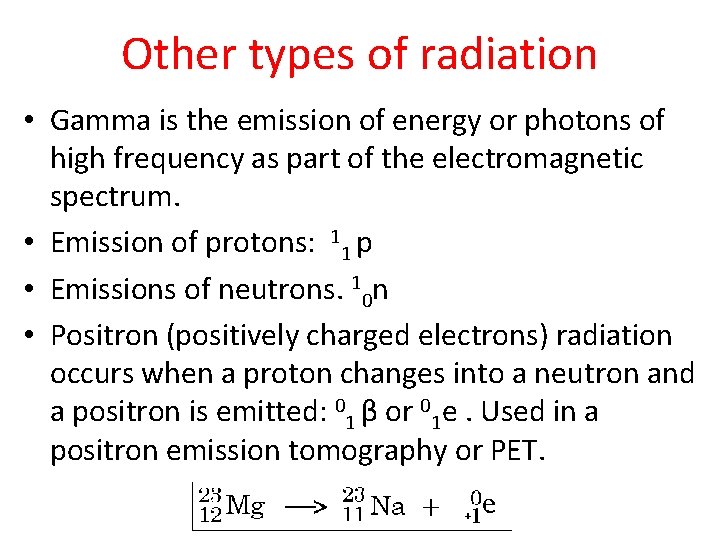
Other types of radiation • Gamma is the emission of energy or photons of high frequency as part of the electromagnetic spectrum. • Emission of protons: 11 p • Emissions of neutrons. 10 n • Positron (positively charged electrons) radiation occurs when a proton changes into a neutron and a positron is emitted: 01 β or 01 e. Used in a positron emission tomography or PET.
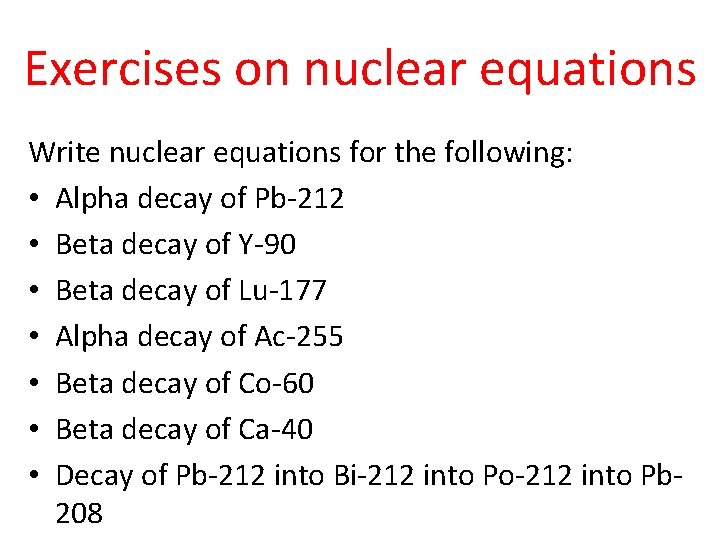
Exercises on nuclear equations Write nuclear equations for the following: • Alpha decay of Pb-212 • Beta decay of Y-90 • Beta decay of Lu-177 • Alpha decay of Ac-255 • Beta decay of Co-60 • Beta decay of Ca-40 • Decay of Pb-212 into Bi-212 into Po-212 into Pb 208
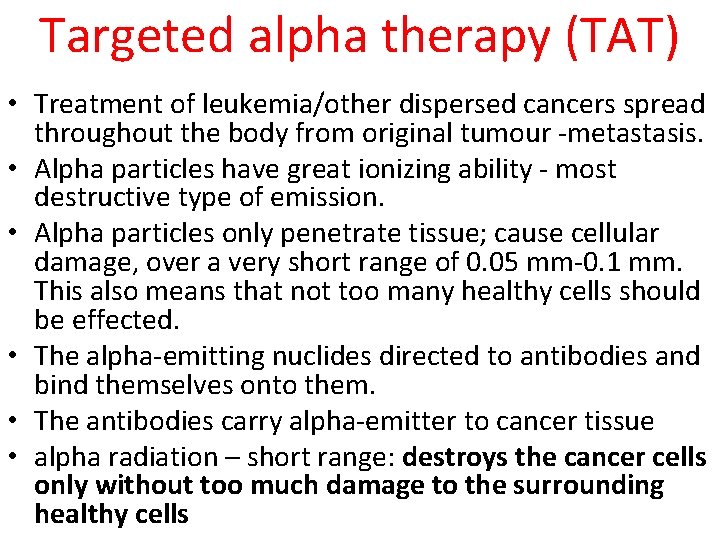
Targeted alpha therapy (TAT) • Treatment of leukemia/other dispersed cancers spread throughout the body from original tumour -metastasis. • Alpha particles have great ionizing ability - most destructive type of emission. • Alpha particles only penetrate tissue; cause cellular damage, over a very short range of 0. 05 mm-0. 1 mm. This also means that not too many healthy cells should be effected. • The alpha-emitting nuclides directed to antibodies and bind themselves onto them. • The antibodies carry alpha-emitter to cancer tissue • alpha radiation – short range: destroys the cancer cells only without too much damage to the surrounding healthy cells
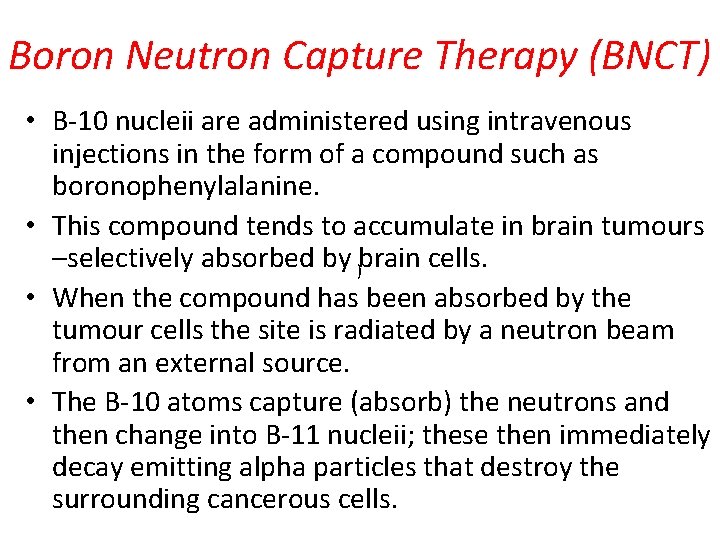
Boron Neutron Capture Therapy (BNCT) • B-10 nucleii are administered using intravenous injections in the form of a compound such as boronophenylalanine. • This compound tends to accumulate in brain tumours –selectively absorbed by )brain cells. • When the compound has been absorbed by the tumour cells the site is radiated by a neutron beam from an external source. • The B-10 atoms capture (absorb) the neutrons and then change into B-11 nucleii; these then immediately decay emitting alpha particles that destroy the surrounding cancerous cells.
BNCT Write a nuclear equation for: o The neutron capture of B-10 o Alpha-decay of B-11
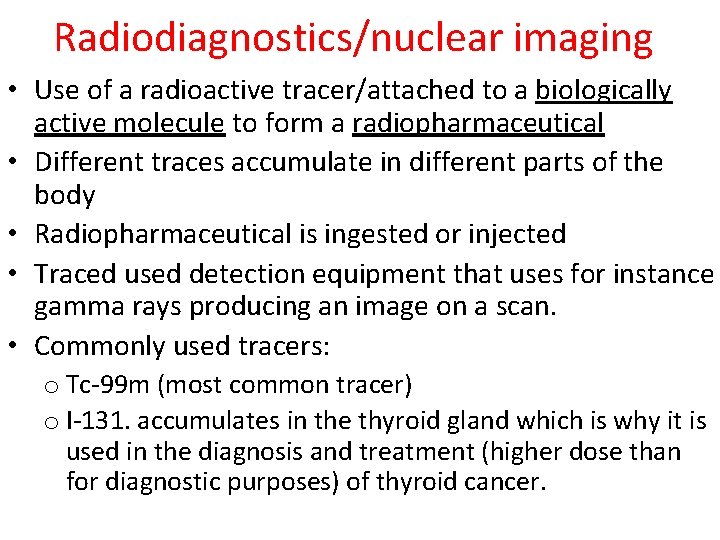
Radiodiagnostics/nuclear imaging • Use of a radioactive tracer/attached to a biologically active molecule to form a radiopharmaceutical • Different traces accumulate in different parts of the body • Radiopharmaceutical is ingested or injected • Traced used detection equipment that uses for instance gamma rays producing an image on a scan. • Commonly used tracers: o Tc-99 m (most common tracer) o I-131. accumulates in the thyroid gland which is why it is used in the diagnosis and treatment (higher dose than for diagnostic purposes) of thyroid cancer.
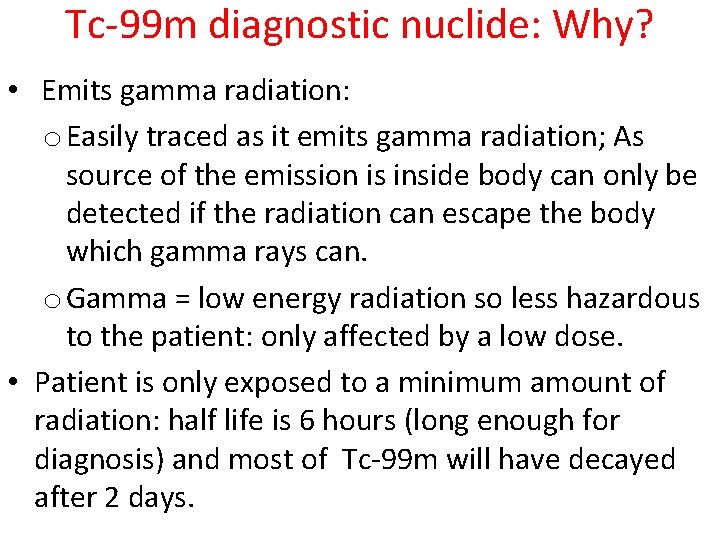
Tc-99 m diagnostic nuclide: Why? • Emits gamma radiation: o Easily traced as it emits gamma radiation; As source of the emission is inside body can only be detected if the radiation can escape the body which gamma rays can. o Gamma = low energy radiation so less hazardous to the patient: only affected by a low dose. • Patient is only exposed to a minimum amount of radiation: half life is 6 hours (long enough for diagnosis) and most of Tc-99 m will have decayed after 2 days.
Tc-99 m diagnostic nuclide: Why? • Artificially produced; m=metastable • Emission of low energy electrons. • Versatile nuclide and easily administered: o Can be used to diagnose and treat cancer in different organs and tissues as it can bind onto a number of different biological carrier. Each type of tissue has its own biologically active molecule that accumulates there. o Can easily be administered to specific areas in the body.
Lu-177 diagnostic nuclide: Why? • Emits strong beta radiation • Also emits gamma radiation that can be detected outside the body and can therefore be used for imaging of small tumours • Also used for TAT
Y-90 diagnostic nuclide: Why? • Emits beta radiation • Short half life of 64 hours
Activity or rate of decay Rate of decay is the number of nuclides that decay or emit radiation per second. The unit is Bequerel or Bq. One Bq means 1 nuclide decays per second.
Half life, t 1/2 • Time it takes for : o Half the initial amount or concentration of a radionuclide to decay. o Activity or rate of decay to half • Dependent on nature of nuclide (decay constant) • Half life remains constant • Independent of : o Concentration or starting amount of nuclide o Temperature o Pressure
Half life, t 1/2 • The longer the half-life, the more slowly a radionuclide decays, the lower its activity (inverse relationship between half life and activity), the lower the dose of radiation emitted. • As radioactive decay only involves 1 reacting species it follows first order reaction kinetics i. e. rate = k[N].
Decay constant, λ • Radioactive decay follows first order reaction kinetics as expressed by the following rate law: rate of decay = k[N] N= radionuclide • The rate law expression can be converted into the following expression that links the half life to the rate constant which is now called a decay constant • Expression: t 1/2 = ln 2/λ (t 1/2 = 0. 693/λ) (In data booklet!!)
Decay constant The expression λ = ln 2/ t 1/2 also indicates that: • Decay constant is also independent of: o concentration or starting amount of the nuclide o Temperature o Pressure • Dependent on t 1/2 which depends on the nature of radionuclide • Decay constant remains constant throughout the decay process. • Has unit time-1
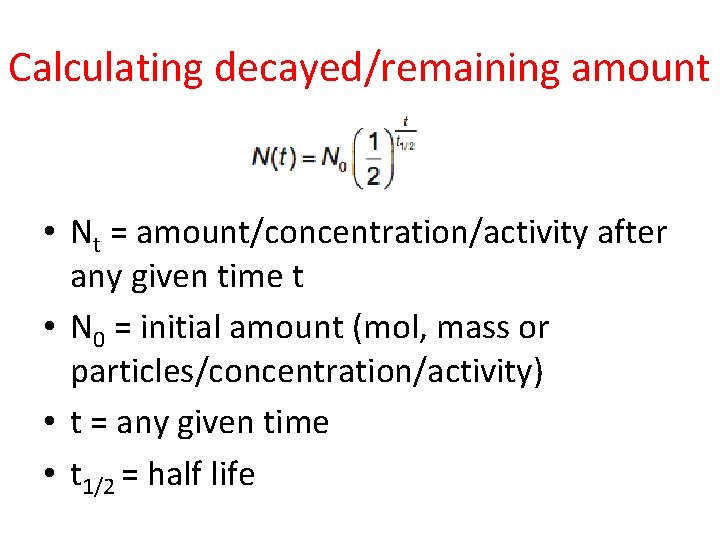
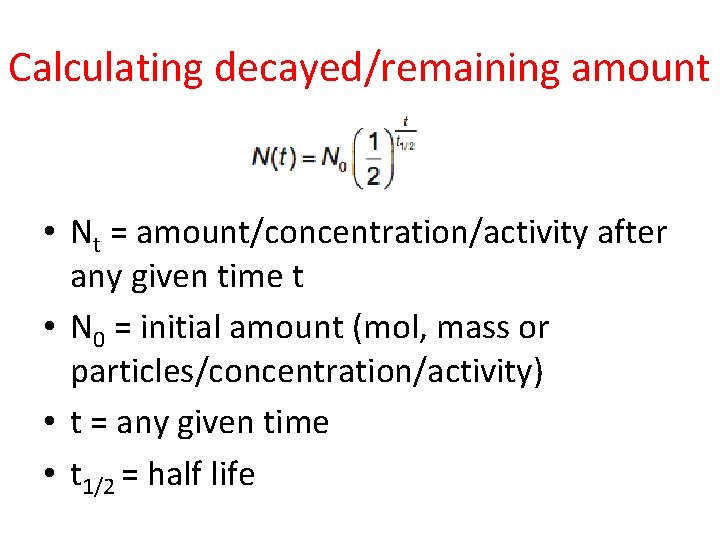
Calculating decayed/remaining amount • Nt = amount/concentration/activity after any given time t • N 0 = initial amount (mol, mass or particles/concentration/activity) • t = any given time • t 1/2 = half life
Medical considerations • Long half life means low value for decay constant and low value for activity. • Nuclides used in diagnosis or therapy should have shorter half lives so they do not remain radioactive for too long but not too short either as otherwise patient will receive high dose of radiation. • Long half life is also not ideal as often nuclides remain in the body for a while and will make patient be exposed to radiation for a longer period of time.
MRI • Magnetic resonance imaging. • MRI uses the same principles as NMR as the scans use very powerful magnets to detect not just H-1 but also C -13, Na-23, He-3 and P-31 nuclei and also use low frequency radio waves that are not ionizing therefore no known impact on human tissue – non-invasive. • Protons in different tissues absorb radiowaves of different frequencies e. g. cancerous tissue; computers identify the type of tissue a proton is in. • The radiowaves absorbed by the nuclei are detected and used by computers to identify the type of tissue the proton is in and produce 2 D or 3 D images of internal organs or body parts.
 Text jackie
Text jackie What is nuclear radiation
What is nuclear radiation Nuclear radiation
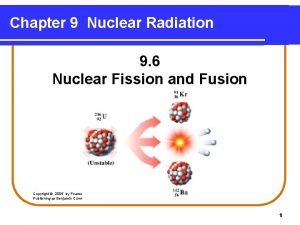
Nuclear radiation Nuclear fission radiation
Nuclear fission radiation Types of radiation
Types of radiation Plamatic acid
Plamatic acid Case study conclusion
Case study conclusion Venus in medical terms
Venus in medical terms Edge packing
Edge packing Lifestyle medicine
Lifestyle medicine Mt sinai nuclear medicine
Mt sinai nuclear medicine Filtered back projection
Filtered back projection Diaphragm
Diaphragm Nuclear medicine information system
Nuclear medicine information system Nuclear medicine lectures
Nuclear medicine lectures Lesson 15 nuclear quest nuclear reactions
Lesson 15 nuclear quest nuclear reactions Fisión nuclear vs fision nuclear
Fisión nuclear vs fision nuclear Mitosis and cell cycle terminology
Mitosis and cell cycle terminology What is an example of a theme statement
What is an example of a theme statement Irrelevant sentences in paragraphs
Irrelevant sentences in paragraphs Homiletical idea
Homiletical idea Stated and implied main idea examples
Stated and implied main idea examples What is controlling idea
What is controlling idea Kepentingan penanda organisasi
Kepentingan penanda organisasi What is the difference between topic and theme
What is the difference between topic and theme Phylogenetisches artkonzept
Phylogenetisches artkonzept Nan-f--app8 -site:youtube.com
Nan-f--app8 -site:youtube.com Weighbridge radiation detector
Weighbridge radiation detector