Quality HospitalAcquired Conditions Tatyan Clarke MD FACS Assistant


- Slides: 40
Quality & Hospital-Acquired Conditions Tatyan Clarke, MD, FACS Assistant Professor, General, Minimally-Invasive & Bariatric Surgery Patricia Heys, BS Director of Infection Prevention & Control Sally Hinkle, DNP, MPA, RN Director of Performance Improvement & Clinical Value Jonathan Shinefeld, RN Perioperative Performance Improvement Manager
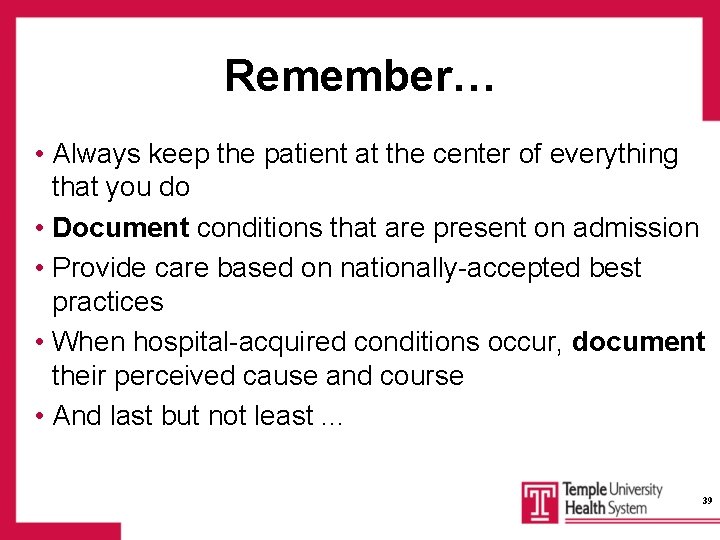
Institute of Medicine: Six Aims for Improving Health Care Quality • Safe Care Avoiding injuries to patients • Effective Care Providing care based on scientific knowledge • Patient-Centered Care Providing respectful & responsive care that ensures that patient values guide clinical decisions • Timely Care Reducing waits for both patients & providers of care • Efficient Care Avoiding waste • Equitable Care Providing consistent quality of care
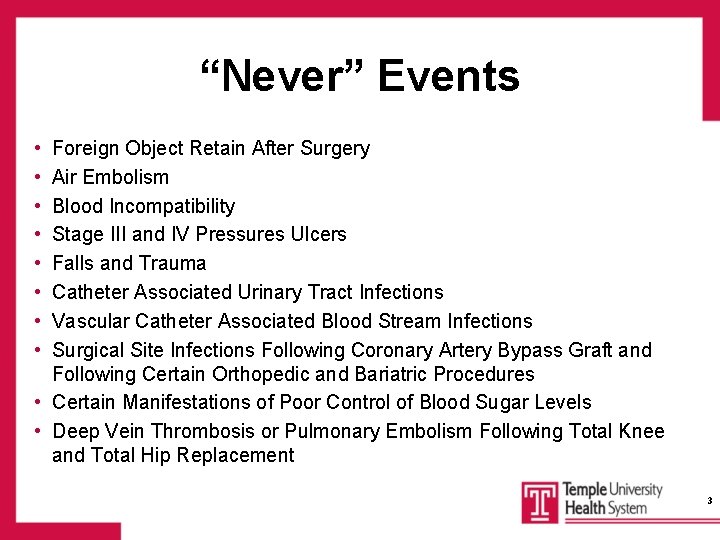
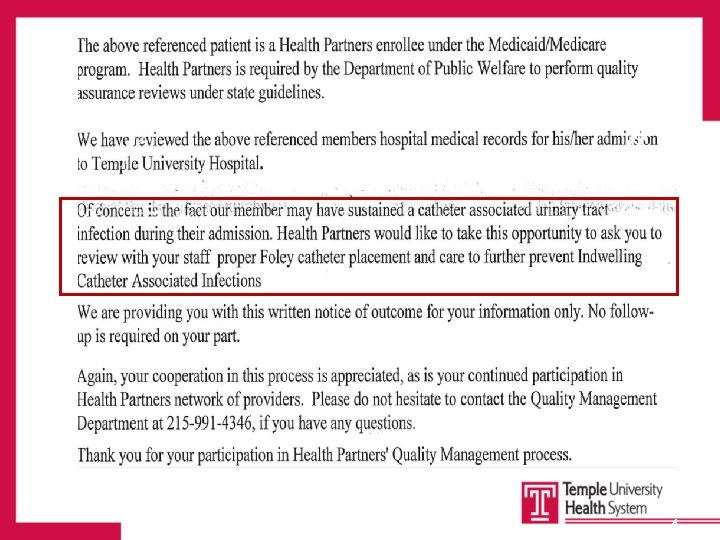
“Never” Events • • Foreign Object Retain After Surgery Air Embolism Blood Incompatibility Stage III and IV Pressures Ulcers Falls and Trauma Catheter Associated Urinary Tract Infections Vascular Catheter Associated Blood Stream Infections Surgical Site Infections Following Coronary Artery Bypass Graft and Following Certain Orthopedic and Bariatric Procedures • Certain Manifestations of Poor Control of Blood Sugar Levels • Deep Vein Thrombosis or Pulmonary Embolism Following Total Knee and Total Hip Replacement 3
ACT 52 In the Commonwealth of Pennsylvania, patients must be notified in writing of all hospitalacquired conditions 4
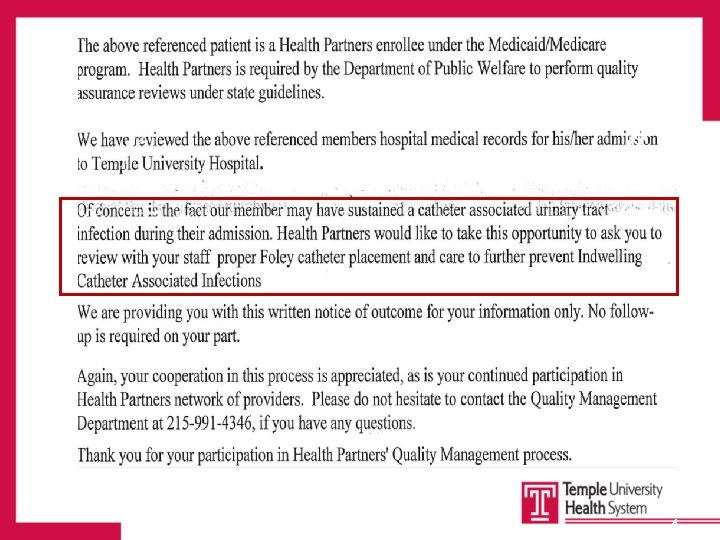
4
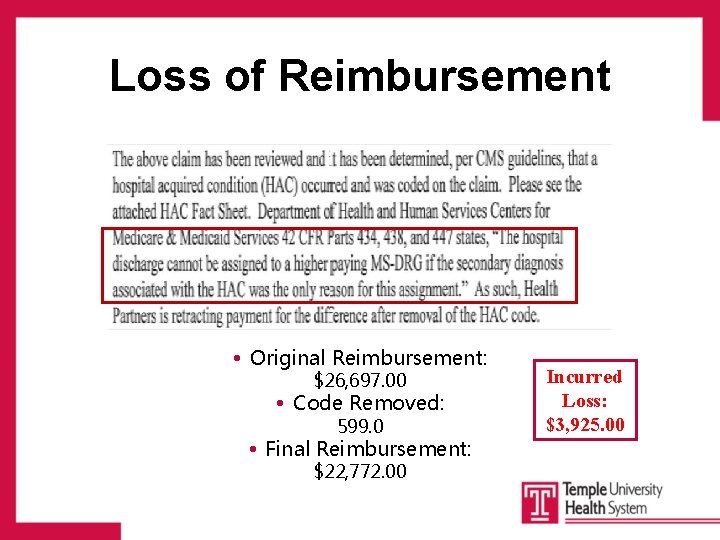
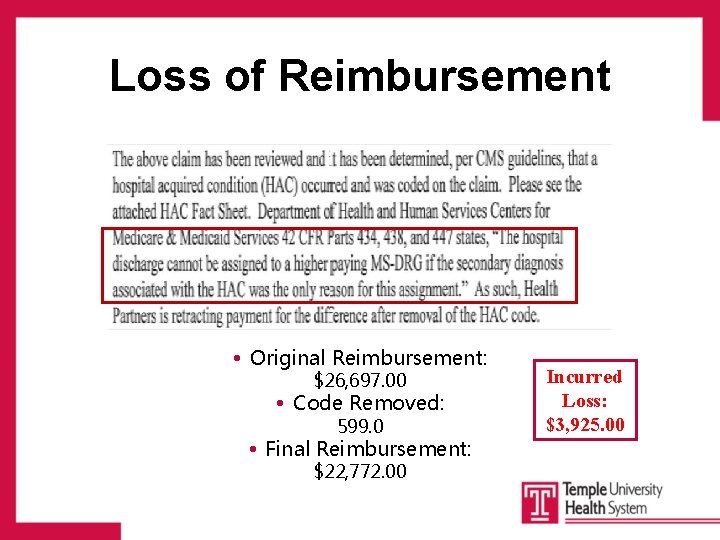
Loss of Reimbursement • Original Reimbursement: $26, 697. 00 • Code Removed: 599. 0 • Final Reimbursement: $22, 772. 00 4 Incurred Loss: $3, 925. 00
Hospital-Acquired Conditions The Centers for Medicare and Medicaid Services (CMS) identified several types of medical occurrences that: • Are Preventable • Are high-cost or high-volume • Result in additional costs to CMS Among these are cases referred to as “Never Events” 7
Hospital-Acquired Conditions: The Future • The list of “Never” Events is expected to grow significantly each year • The major shift is payment for outcomes versus process – Mortality – PSI 90 – Infections 8
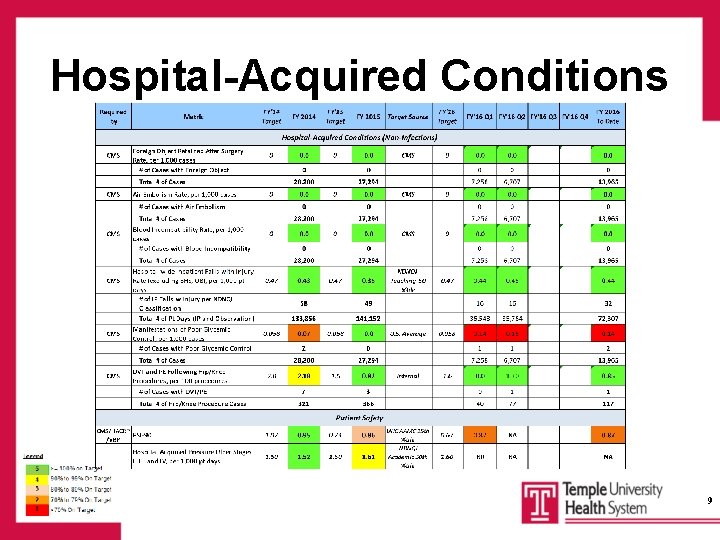
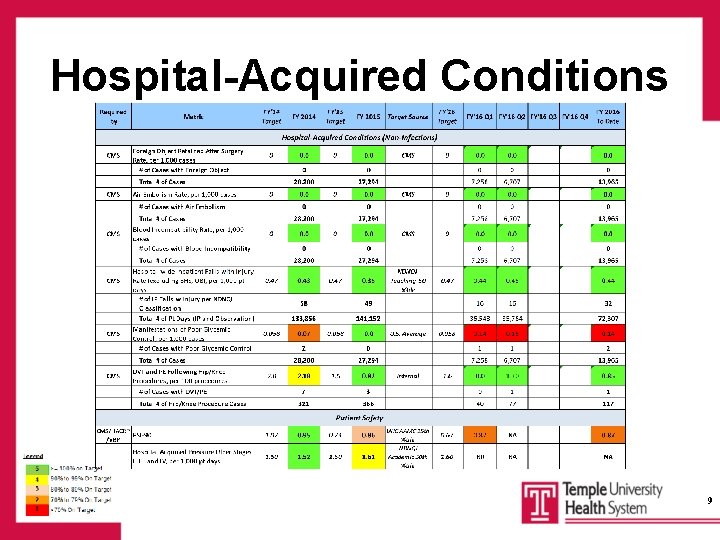
Hospital-Acquired Conditions 9
Core Measures & Best Practice • Set of best-practice standards proven to decrease morbidity, mortality, and readmission rates • Process indicators tied to clinical outcomes & improved quality • Mandated by Centers for Medicare & Medicaid Services (CMS) & The Joint Commission (TJC) • Links healthcare provider performance practices to facility reimbursement 10
2016 Reported Core Measures • Emergency Department • Hospital Based Inpatient Psychiatric Services • Immunization • Perinatal Care • Sepsis Bundle (New 2016 Measure) • Stroke • Venous Thromboembolism (VTE) 11
2016 SEP-1 Measure Severe Sepsis/Septic Shock : SEP-1 To be completed within 3 hours: • Serum Lactate • Blood cultures before initial antibiotic administration • Administration of broad-spectrum antibiotics • Administration of 30 m. L/kg crystalloid for hypotension or lactate ≥ 4 mmol/L To be completed within 6 hours: • Repeat lactate for elevated initial lactate (Lactate>2) • For hypotension that does not respond to initial fluid administration, administration of vasopressors to maintain MAP >65 mm. Hg • Repeat volume status and tissue perfusion reassessment if hypotension persists after fluid admin 12
2016 SEP-1 Measure: Needs • Consistent physician documentation (coding) – Severe Sepsis – Septic Shock • Consistent staff documentation of time elements – Support time sensitive measure for 3 hour and 6 hour bundles • Consistent nursing documentation: Dates/Times – Fluid administration with end times – Blood culture draws • Consistent ordering of repeat lactate if initial >2 • Sepsis Care opportunities: – Transition of Care (ED→Floor/ICU; Floor→ICU) 13
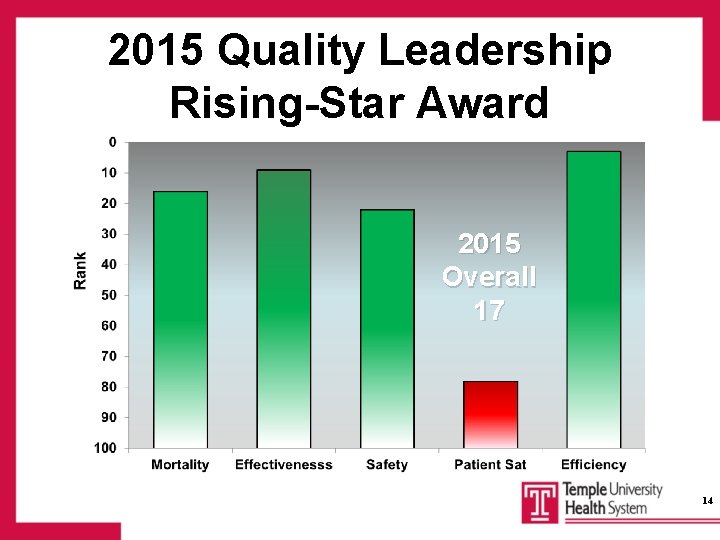
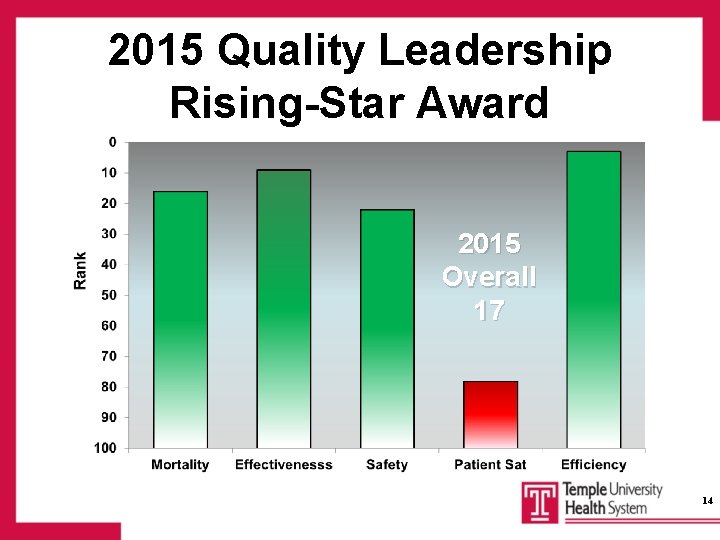
2015 Quality Leadership Rising-Star Award 2015 Overall 17 14
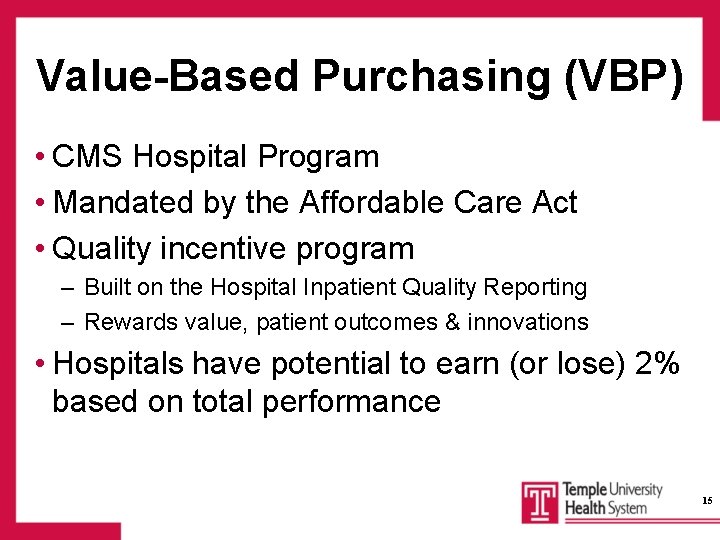
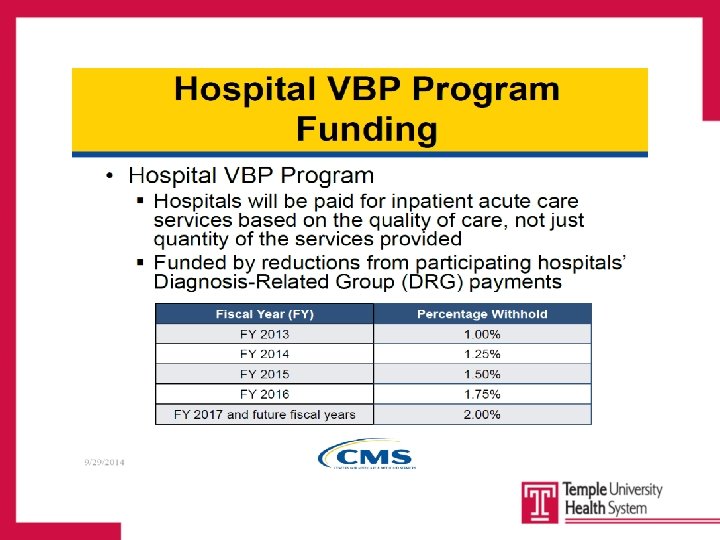
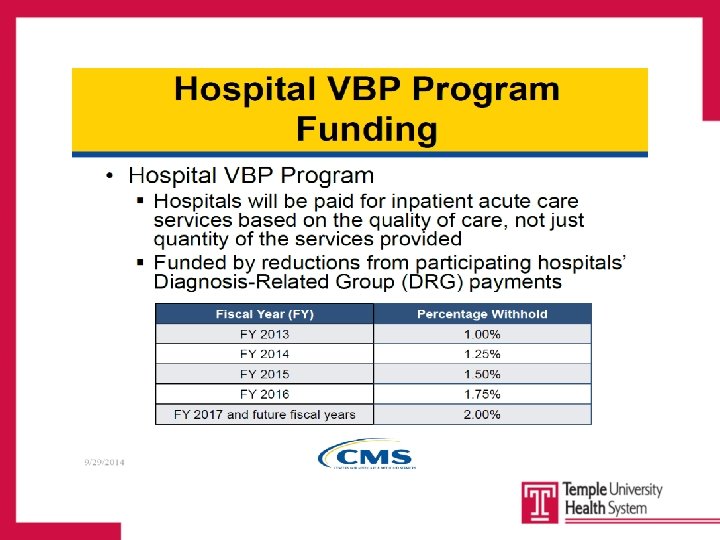
Value-Based Purchasing (VBP) • CMS Hospital Program • Mandated by the Affordable Care Act • Quality incentive program – Built on the Hospital Inpatient Quality Reporting – Rewards value, patient outcomes & innovations • Hospitals have potential to earn (or lose) 2% based on total performance 15
4 4
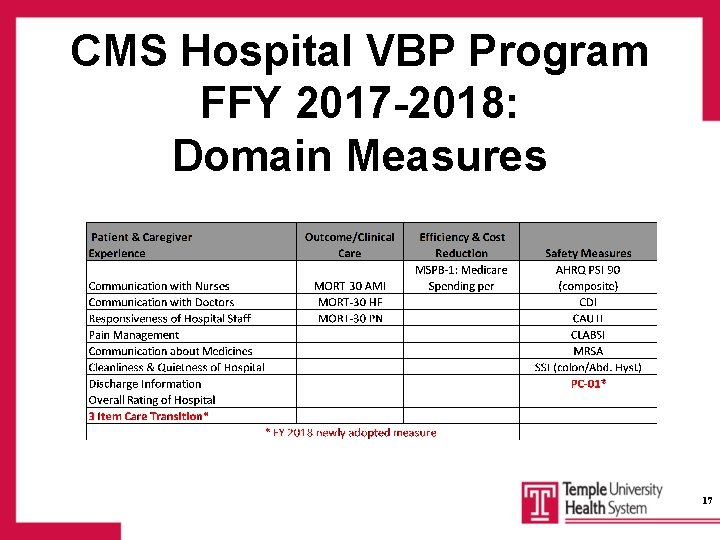
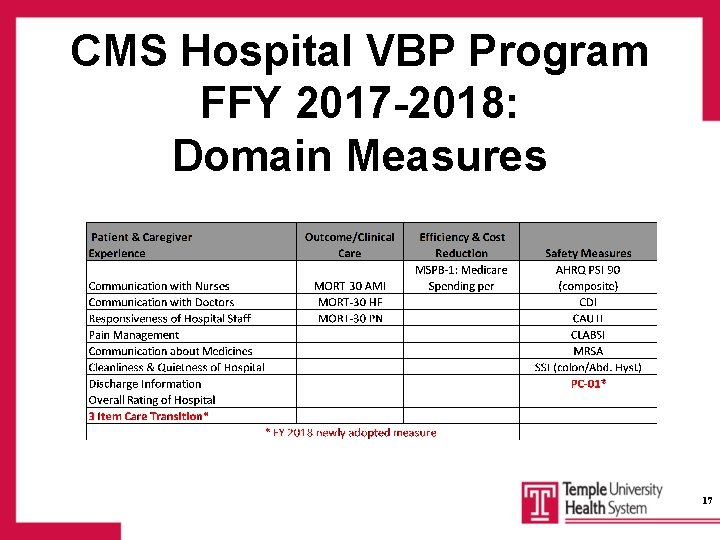
CMS Hospital VBP Program FFY 2017 -2018: Domain Measures 17
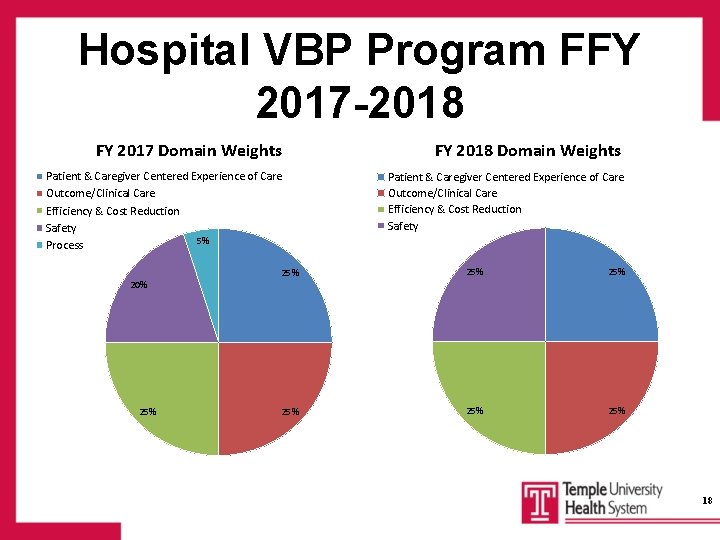
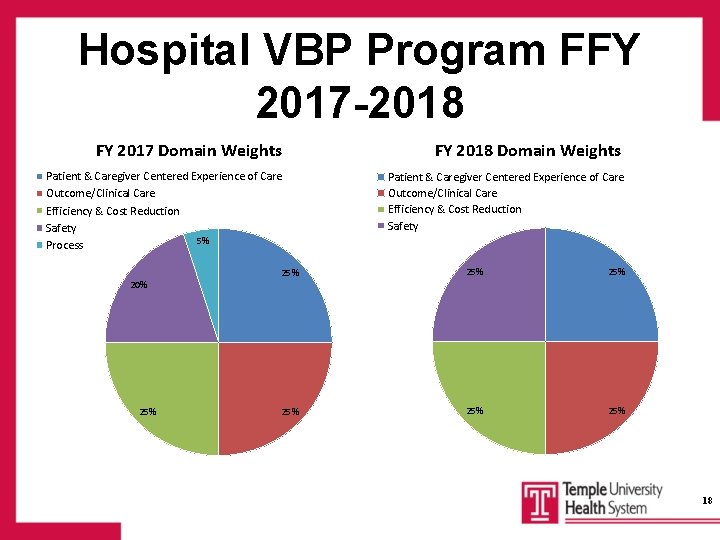
Hospital VBP Program FFY 2017 -2018 FY 2017 Domain Weights FY 2018 Domain Weights Patient & Caregiver Centered Experience of Care Outcome/Clinical Care Efficiency & Cost Reduction Safety 5% Process Patient & Caregiver Centered Experience of Care Outcome/Clinical Care Efficiency & Cost Reduction Safety 25% 25% 25% 20% 25% 18

Care Resources Ethics Consult Inpatient Hospice __________________________________________ Palliative Care 19
Care Resources: Ethics Consult • Request may be initiated by the patient, family member, hospital staff, or employee • Common reasons for consults include: – Questions about decision making – Conflicting recommendations for plan of care – Distress regarding current course of care • Requires a consult request and/or contact Risk Management – 215 -707 -8219 – After hours/weekend call Risk Management 215 -707 -4545 20
Care Resources: Inpatient Hospice • Attending physician determines that the patient is appropriate for hospice care and is too unstable to be transferred to another facility. • Requires a hospice care order. • Requires a call to VNA/Hospice of Philadelphia – 215 -581 -204) to request a hospice evaluation – Hospice nurse evaluates the patient, explains the benefits – Hospice election form must be signed 21
Care Resources: Palliative Care Service • Mission is to provide specialized medical care for patients with serious/chronic illness – Focus: relief of the symptoms, pain, & stress of a serious illness – Goal: improvement of quality of life for both the patient & family • Palliative Care Consult: Interdisciplinary consult – Team includes physicians, nurse practitioners, social workers & chaplains – Requires an order-call 215 -581 -2057 • Compass Program- Outpatient Office referral for inhome advance care-planning & goal-setting by trained Palliative Care Social Worker 22
Advance Directives • Patient Self-Determination Act (CMS/TJC) • Requirements: – Health Care Institutions must maintain AD Policies & Procedures – Health Care Institutions must provide AD information to patients • TUH AD Information Booklet – Living Will – Durable Power of Attorney for Health Care – Surrogate Decision-maker 23
Areas of Focus →Identification and documentation of conditions “Present on Admission” →Properly document to distinguish between “Present on Admission” and “Hospital-Acquired” conditions Prevent “Never”Events from occurring → 24
Present on Admission (POA) • Deficit Reduction Act of 2005 mandated that POA indicators be reported for all diagnoses submitted on Medicare inpatient acute care claims (10/2007) • Differentiates conditions present at the time of admission from those conditions that develop during the inpatient admission • Billable • Influences Case Mix Index (CMI) • Must be clearly documented 25
Case Study • What conditions were present at the time of admission? • Were there any infections that resulted from the care delivered during the inpatient admission? 424
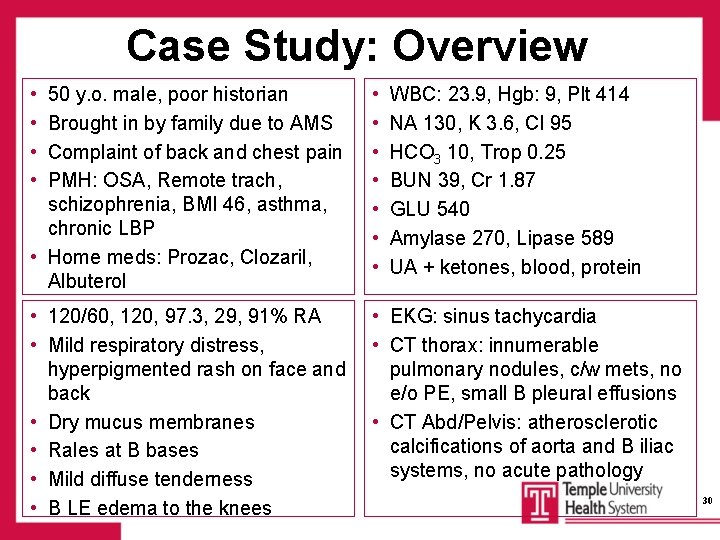
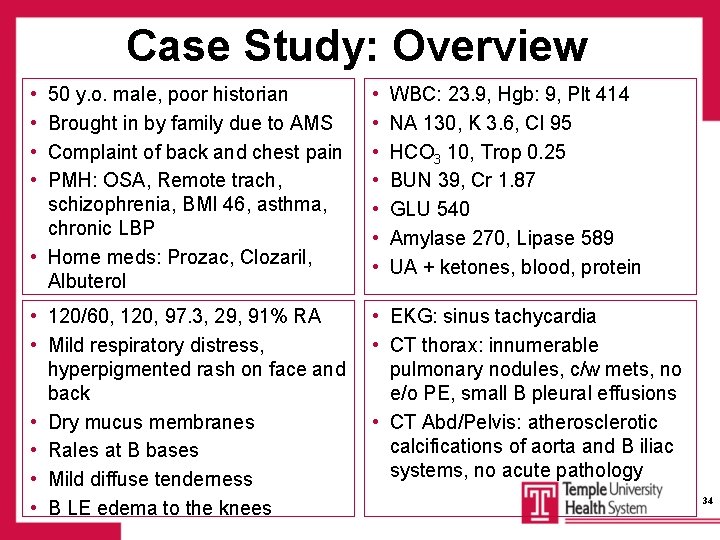
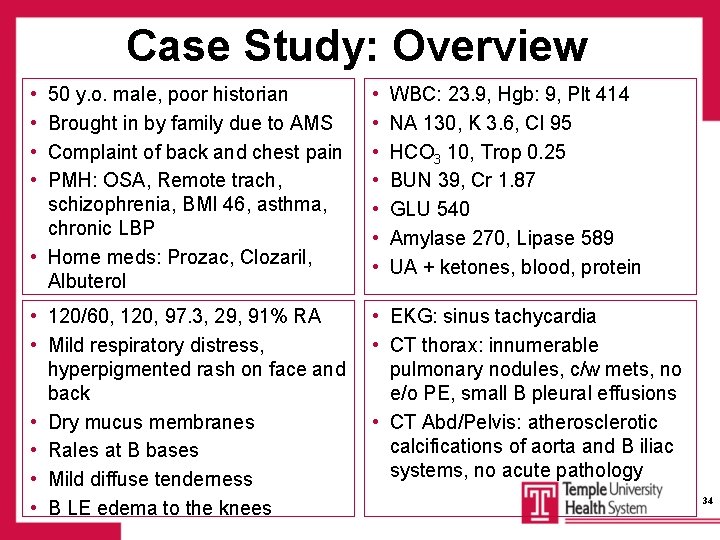
Case Study: History • 50 y. o. male, poor historian • Brought in by family due to AMS • Complained of back and chest pain • PMH: OSA, Remote trach, schizophrenia, BMI 46, asthma, chronic LBP • Home meds: Prozac, Clozaril, Albuterol 27
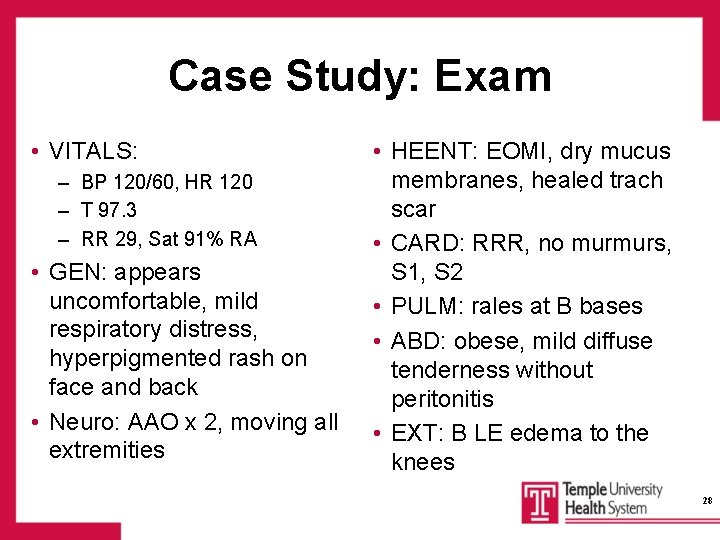
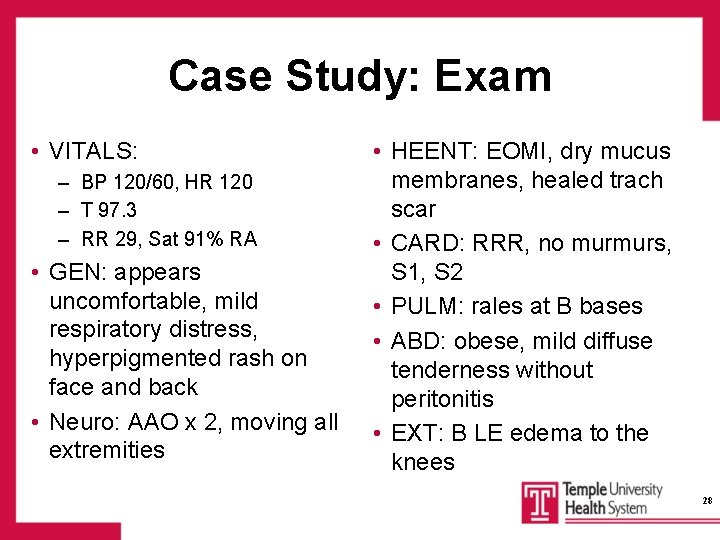
Case Study: Exam • VITALS: – BP 120/60, HR 120 – T 97. 3 – RR 29, Sat 91% RA • GEN: appears uncomfortable, mild respiratory distress, hyperpigmented rash on face and back • Neuro: AAO x 2, moving all extremities • HEENT: EOMI, dry mucus membranes, healed trach scar • CARD: RRR, no murmurs, S 1, S 2 • PULM: rales at B bases • ABD: obese, mild diffuse tenderness without peritonitis • EXT: B LE edema to the knees 28
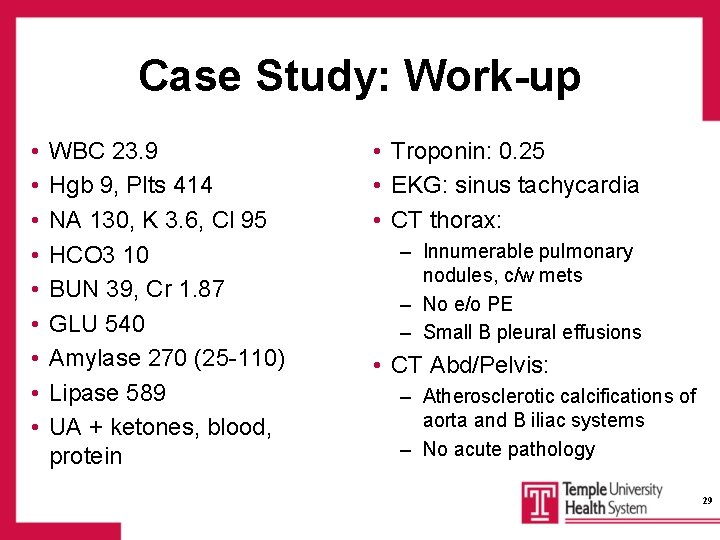
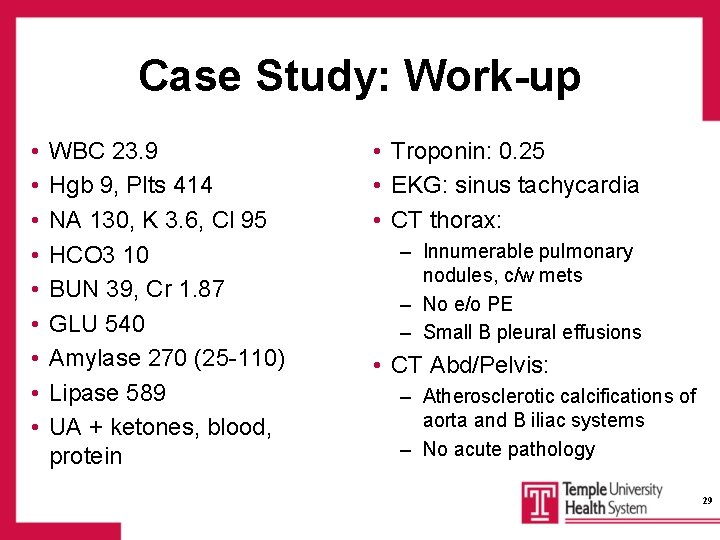
Case Study: Work-up • • • WBC 23. 9 Hgb 9, Plts 414 NA 130, K 3. 6, Cl 95 HCO 3 10 BUN 39, Cr 1. 87 GLU 540 Amylase 270 (25 -110) Lipase 589 UA + ketones, blood, protein • Troponin: 0. 25 • EKG: sinus tachycardia • CT thorax: – Innumerable pulmonary nodules, c/w mets – No e/o PE – Small B pleural effusions • CT Abd/Pelvis: – Atherosclerotic calcifications of aorta and B iliac systems – No acute pathology 29
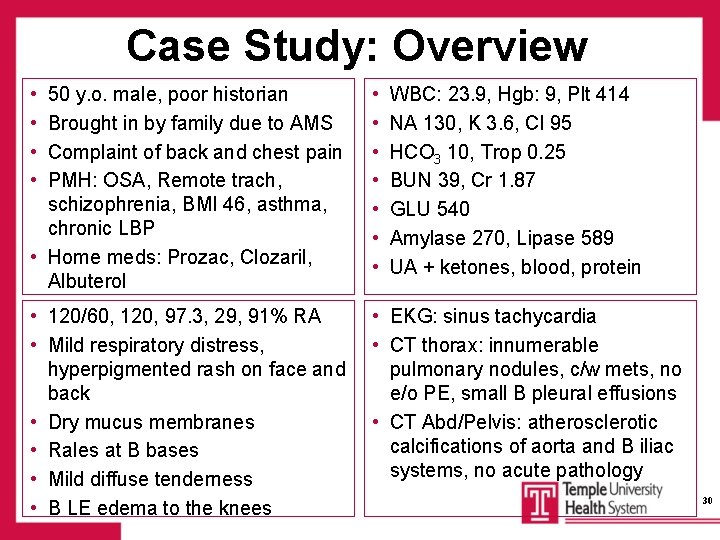
Case Study: Overview • • 50 y. o. male, poor historian Brought in by family due to AMS Complaint of back and chest pain PMH: OSA, Remote trach, schizophrenia, BMI 46, asthma, chronic LBP • Home meds: Prozac, Clozaril, Albuterol • • 120/60, 120, 97. 3, 29, 91% RA • Mild respiratory distress, hyperpigmented rash on face and back • Dry mucus membranes • Rales at B bases • Mild diffuse tenderness • B LE edema to the knees • EKG: sinus tachycardia • CT thorax: innumerable pulmonary nodules, c/w mets, no e/o PE, small B pleural effusions • CT Abd/Pelvis: atherosclerotic calcifications of aorta and B iliac systems, no acute pathology WBC: 23. 9, Hgb: 9, Plt 414 NA 130, K 3. 6, Cl 95 HCO 3 10, Trop 0. 25 BUN 39, Cr 1. 87 GLU 540 Amylase 270, Lipase 589 UA + ketones, blood, protein 30
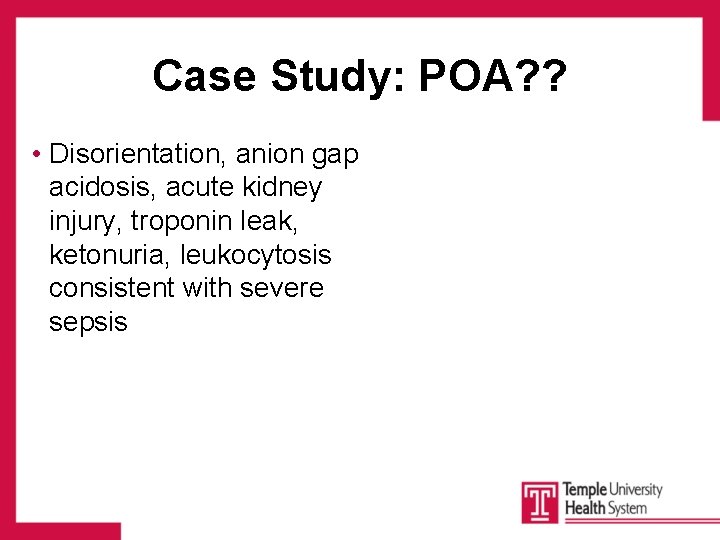
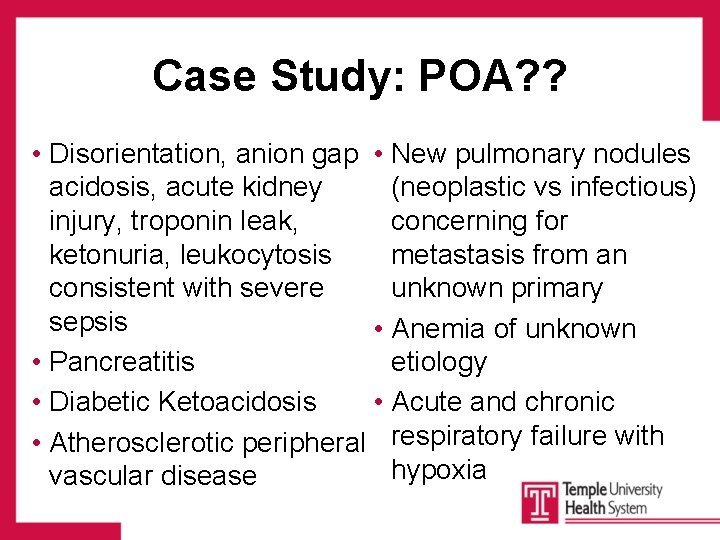
Case Study: POA? ? • Disorientation, anion gap acidosis, acute kidney injury, troponin leak, ketonuria, leukocytosis consistent with severe sepsis
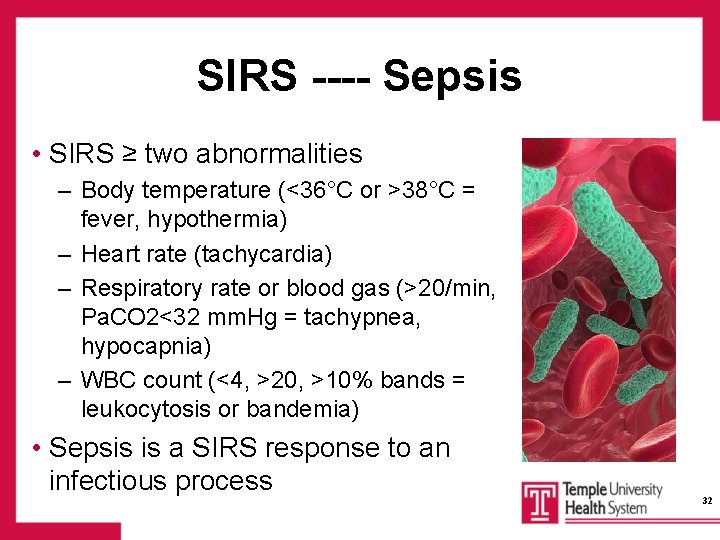
SIRS ---- Sepsis • SIRS ≥ two abnormalities – Body temperature (<36°C or >38°C = fever, hypothermia) – Heart rate (tachycardia) – Respiratory rate or blood gas (>20/min, Pa. CO 2<32 mm. Hg = tachypnea, hypocapnia) – WBC count (<4, >20, >10% bands = leukocytosis or bandemia) • Sepsis is a SIRS response to an infectious process 32
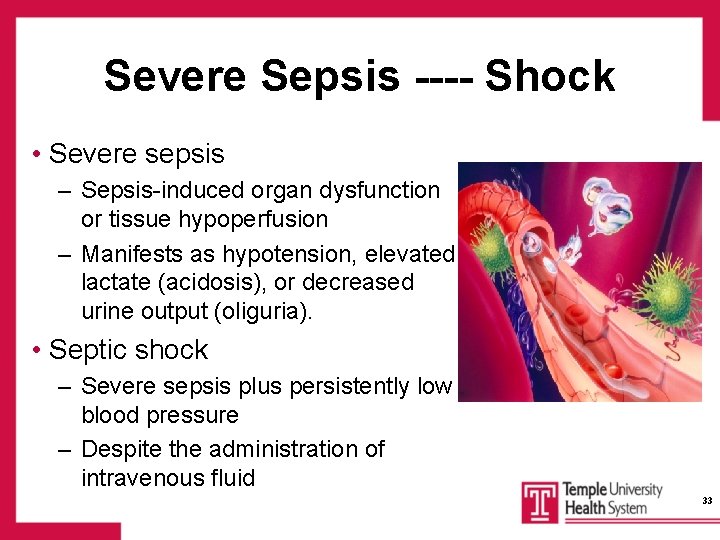
Severe Sepsis ---- Shock • Severe sepsis – Sepsis-induced organ dysfunction or tissue hypoperfusion – Manifests as hypotension, elevated lactate (acidosis), or decreased urine output (oliguria). • Septic shock – Severe sepsis plus persistently low blood pressure – Despite the administration of intravenous fluid 33
Case Study: Overview • • 50 y. o. male, poor historian Brought in by family due to AMS Complaint of back and chest pain PMH: OSA, Remote trach, schizophrenia, BMI 46, asthma, chronic LBP • Home meds: Prozac, Clozaril, Albuterol • • 120/60, 120, 97. 3, 29, 91% RA • Mild respiratory distress, hyperpigmented rash on face and back • Dry mucus membranes • Rales at B bases • Mild diffuse tenderness • B LE edema to the knees • EKG: sinus tachycardia • CT thorax: innumerable pulmonary nodules, c/w mets, no e/o PE, small B pleural effusions • CT Abd/Pelvis: atherosclerotic calcifications of aorta and B iliac systems, no acute pathology WBC: 23. 9, Hgb: 9, Plt 414 NA 130, K 3. 6, Cl 95 HCO 3 10, Trop 0. 25 BUN 39, Cr 1. 87 GLU 540 Amylase 270, Lipase 589 UA + ketones, blood, protein 34
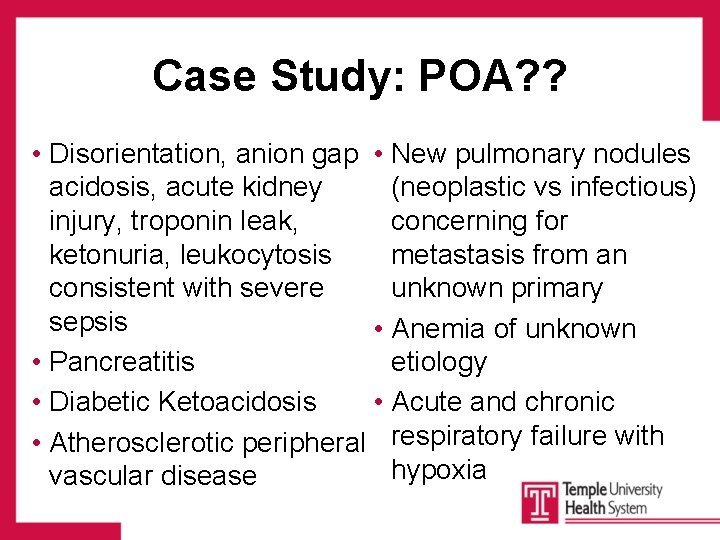
Case Study: POA? ? • Disorientation, anion gap • New pulmonary nodules acidosis, acute kidney (neoplastic vs infectious) injury, troponin leak, concerning for ketonuria, leukocytosis metastasis from an consistent with severe unknown primary sepsis • Anemia of unknown • Pancreatitis etiology • Diabetic Ketoacidosis • Acute and chronic • Atherosclerotic peripheral respiratory failure with hypoxia vascular disease
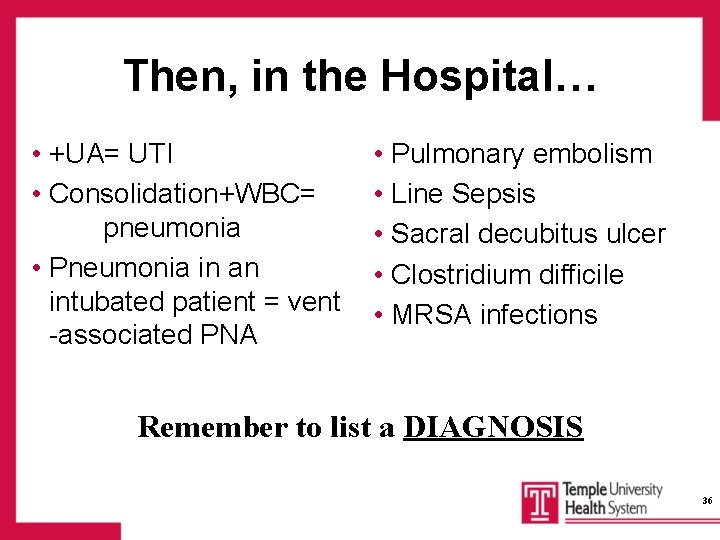
Then, in the Hospital… • +UA= UTI • Consolidation+WBC= pneumonia • Pneumonia in an intubated patient = vent -associated PNA • Pulmonary embolism • Line Sepsis • Sacral decubitus ulcer • Clostridium difficile • MRSA infections Remember to list a DIAGNOSIS 36
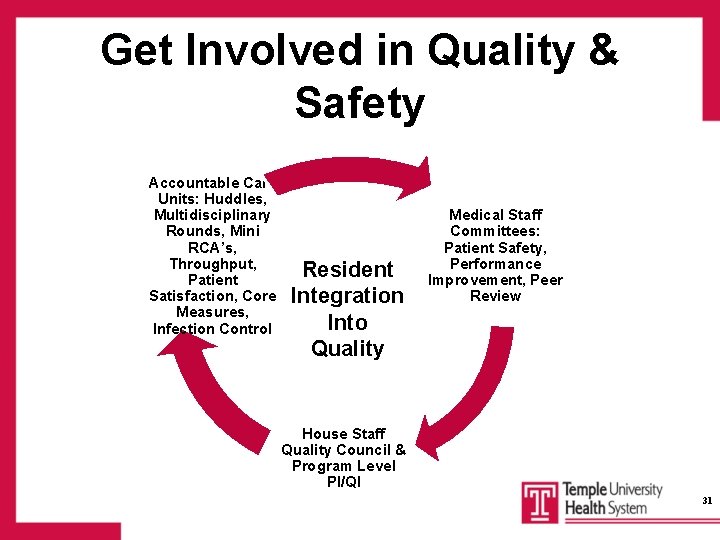
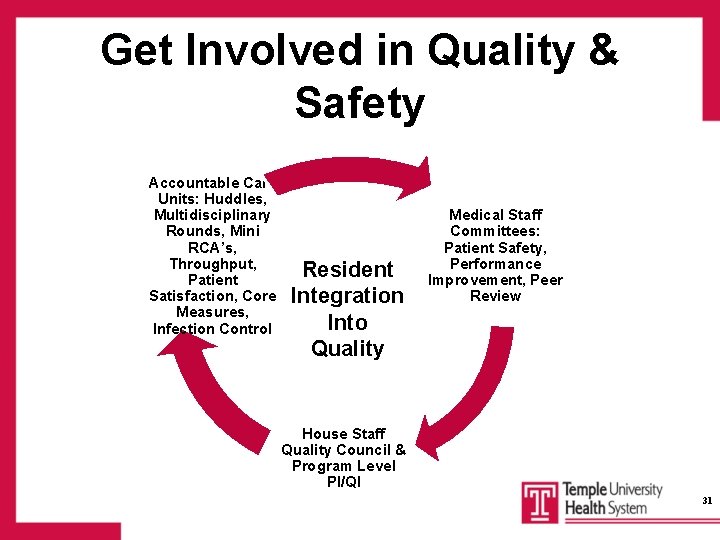
Get Involved in Quality & Safety Accountable Care Units: Huddles, Multidisciplinary Rounds, Mini RCA’s, Throughput, Patient Satisfaction, Core Measures, Infection Control Resident Integration Into Quality Medical Staff Committees: Patient Safety, Performance Improvement, Peer Review House Staff Quality Council & Program Level PI/QI 31
Centers for Medicare & Medicaid Services The focus in Health Care Quality: Getting the right care to the right patient – every time 32
Remember… • Always keep the patient at the center of everything that you do • Document conditions that are present on admission • Provide care based on nationally-accepted best practices • When hospital-acquired conditions occur, document their perceived cause and course • And last but not least. . . 39

WASH YOUR HANDS! 40
 Dr tatyan clarke
Dr tatyan clarke Just facs
Just facs Facs vizsgálat
Facs vizsgálat Hemorrhagic shock classification
Hemorrhagic shock classification Bu facs core
Bu facs core Just facs kitchen safety
Just facs kitchen safety Facs
Facs Fluorescence-activated cell sorting (facs)
Fluorescence-activated cell sorting (facs) Facs
Facs Firas mussa md
Firas mussa md Facs recipes
Facs recipes Chapter 1 food affects life
Chapter 1 food affects life Dr allison clarke
Dr allison clarke Reference frame theory
Reference frame theory Dr nick clarke
Dr nick clarke St david's day poem
St david's day poem Nucleo intermedio mediale
Nucleo intermedio mediale Renata clarke fao
Renata clarke fao Catherine clarke psychologist
Catherine clarke psychologist Ryan clarke drugs
Ryan clarke drugs Todd clarke albuquerque
Todd clarke albuquerque Sonji clarke
Sonji clarke Clarke
Clarke Griff by austin c clarke summary
Griff by austin c clarke summary Alan turing joan clarke
Alan turing joan clarke Clarke's analysis of drugs and poisons
Clarke's analysis of drugs and poisons Shrove tuesday significato
Shrove tuesday significato Pinire
Pinire What was the importance of the battle of kettle creek
What was the importance of the battle of kettle creek Dr randolph clarke
Dr randolph clarke Woofound
Woofound Citation clarke click
Citation clarke click Sarah clarke solicitor
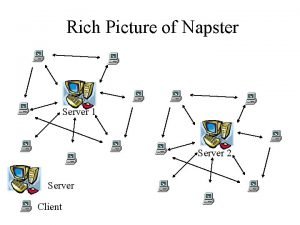
Sarah clarke solicitor Ian clarke freenet
Ian clarke freenet Clarke
Clarke Alex clarke naked
Alex clarke naked Shaune clarke
Shaune clarke Tr.corticospinalis
Tr.corticospinalis Ron clarke 1992
Ron clarke 1992 Rob weapon art
Rob weapon art Quality metrics pmp
Quality metrics pmp