PostConcussion Headaches Charles Clarke MD Assistant Professor of


- Slides: 31
Post-Concussion Headaches Charles Clarke, MD Assistant Professor of Neurology Vanderbilt Williamson Neurology
History of Concussion • Initially brought to the interest of the medical community by Dr. Joseph Babinski. Due to blast injuries of WWI soldiers. • Now appropriately at the forefront of popular culture due to prominent athletes being concussed and its relationship to chronic traumatic encephalopathy.
Definitions of Concussion • The latin meaning for concuss literally means to “shake violently” or “dash [strike] together” • Clinically, though it is a “syndrome of neurocognitive and behavioral dysfunction due to alteration in brain physiology due to a mechanical injury. ” • Often used synonymously with mild TBI • Mild TBI is a GCS of 13 -15
Objectives • Discuss the epidemiology of post-concussion headaches • Discuss the evaluation of post-concussion headaches. • Explain the management of post-concussion headaches.
Epidemiology • There is a widely variable incidence of postconcussion headaches between 25%-78% of patients with mild TBI. • Post-concussion headaches are unexpectedly more prevalent, greater in severity, and greater in duration after mild TBI than more severe TBI.
Headache Type • Post-traumatic headaches according to the International Headache Society (HIS) can be classified as migraine and/or tension headaches most commonly. • Other headache types include: occipital neuralgia, vascular dissections, trigeminal neuralgia, low CSF pressure headaches, hemicranias continua, etc. • Many patients with have more than one headache type.
Tension Headache • Typically this pain is a dull pressure or sensation of tightness. • This is classically described as band-like wrapping around the head, but can be located essentially anywhere. • Patient is able to remain active typically • No other associated symptoms • Can be acute or chronic
Tension Headache Treatment • NSAIDS are the mainstay of acute tension headache treatment, butalbital/caffeine/APAP preparations can be used as well in moderation. • Tricyclic antidepressants are often used for prevention of chronic tension headaches. • Due to short acting pain medication use co-morbid medication overuse headache or rebound headache is commonly associated with this.
Rebound Headache • Highest risk ▫ Opiods ▫ Butalbital compounds ▫ ASA/acetaminophen/caffeine combos • Lower risk ▫ -triptans/ergots ▫ NSAIDS
Rebound Headache • Paramount in treatment is the withdrawal of the offending medication for at least 2 weeks ▫ Taper opiods or use clonidine patch ▫ Butalbital withdraw 100 mg of butalbital = 30 mg of phenobarb OR 30 mg phenobarb BID x 2 wks then 15 mg BID x 2 wks ▫ You can abruptly stop other offending medications
Rebound Headache • Use a bridge therapy ▫ Long acting NSAIDS ▫ Tizanidine ▫ Steroids • 2 weeks of treatment with naproxen and tizanidine has been shown to be helpful for headache management during the withdrawal period. • Start prophylactic medication for primary headache condition
Migraine • In general there is a cumulative lifetime prevalence of ▫ 43% in women ▫ 18% in men • Estrogen’s role in migraine is thought to be due to it increasing NO synthase activity.
Migraine • Most often a lateralized, moderate to severe, throbbing head pain • Associated with additional features such as nausea, vomiting, photophobia, phonophobia, and/or aura • Can be episodic or chronic
Migraine • Where does the pain originate? ▫ Trigeminovascular system: dura, arteries, venous sinuses, CNs, cranial musculoskeletal components, and nasal sinuses. • What causes aura? ▫ Cortical spreading depression of depolarization partially under the influence of NO

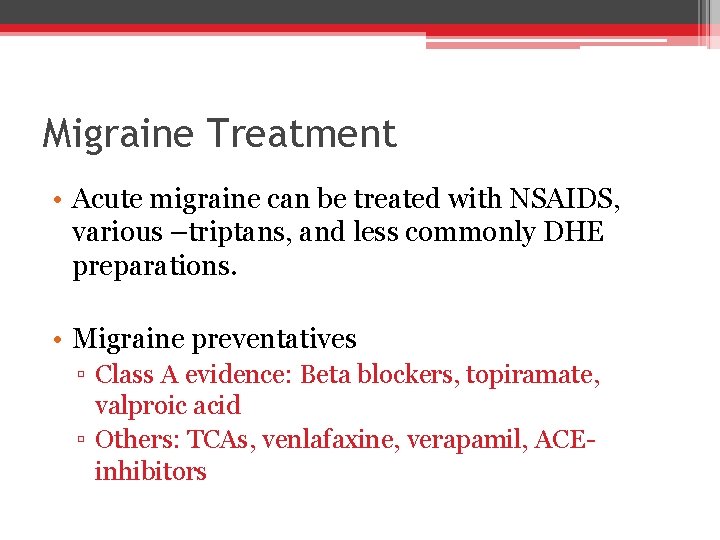
Migraine Treatment • Acute migraine can be treated with NSAIDS, various –triptans, and less commonly DHE preparations. • Migraine preventatives ▫ Class A evidence: Beta blockers, topiramate, valproic acid ▫ Others: TCAs, venlafaxine, verapamil, ACEinhibitors
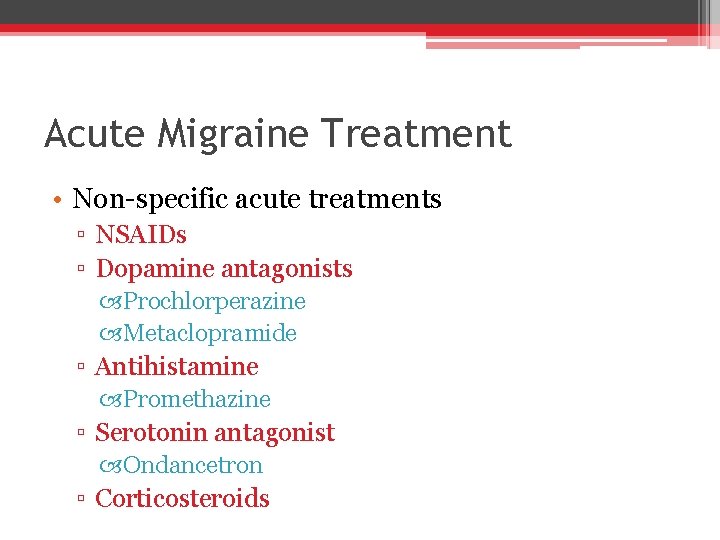
Acute Migraine Treatment • Non-specific acute treatments ▫ NSAIDs ▫ Dopamine antagonists Prochlorperazine Metaclopramide ▫ Antihistamine Promethazine ▫ Serotonin antagonist Ondancetron ▫ Corticosteroids
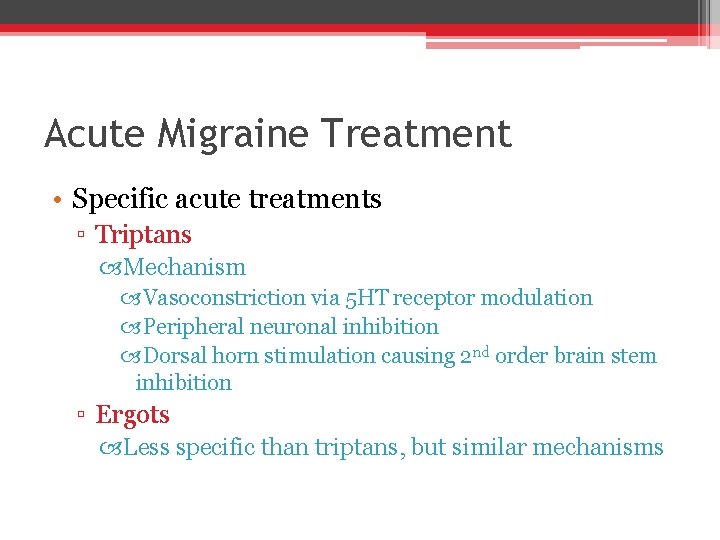
Acute Migraine Treatment • Specific acute treatments ▫ Triptans Mechanism Vasoconstriction via 5 HT receptor modulation Peripheral neuronal inhibition Dorsal horn stimulation causing 2 nd order brain stem inhibition ▫ Ergots Less specific than triptans, but similar mechanisms
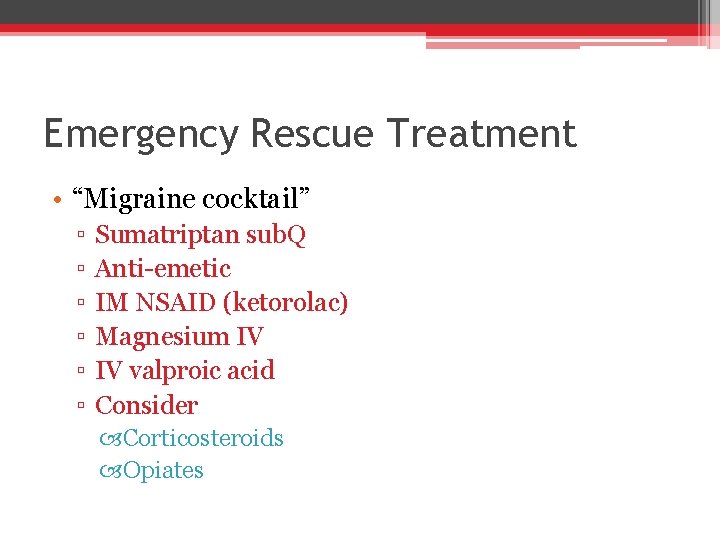
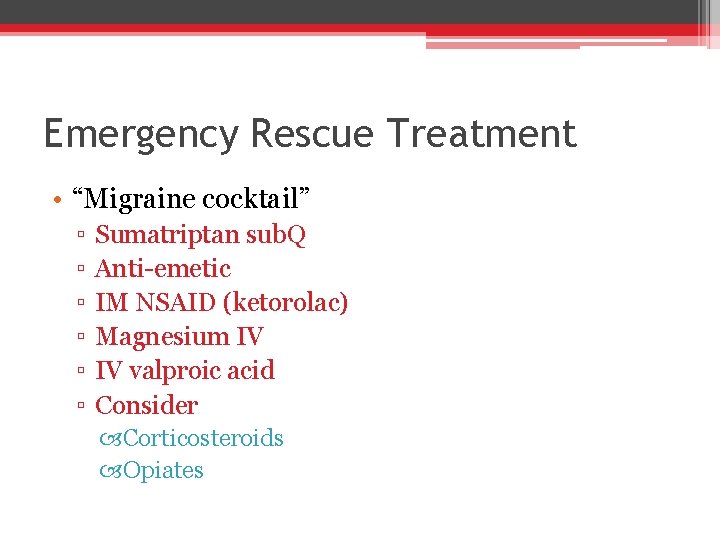
Emergency Rescue Treatment • “Migraine cocktail” ▫ ▫ ▫ Sumatriptan sub. Q Anti-emetic IM NSAID (ketorolac) Magnesium IV IV valproic acid Consider Corticosteroids Opiates

Migraine Prevention • Best data (Level A) ▫ Beta blockers (propranolol, timolol, and metoprolol) ▫ Valproic acid ▫ Topiramate • Next best (Level B) ▫ Amitriptyline ▫ Venlafaxine
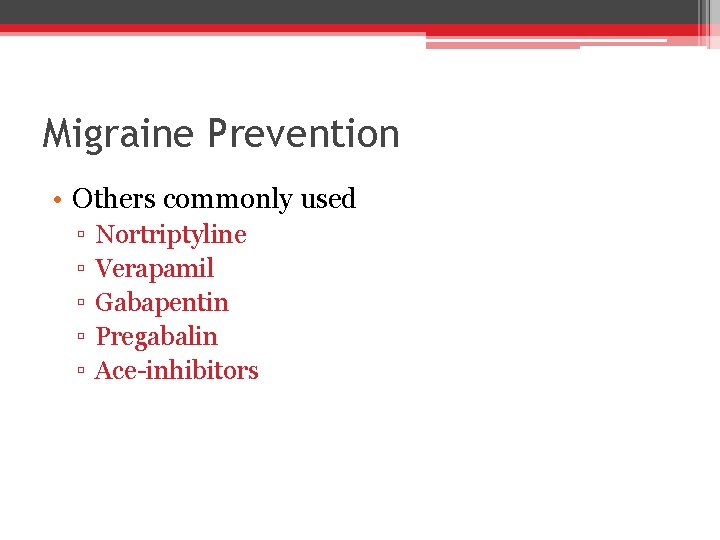
Migraine Prevention • Others commonly used ▫ ▫ ▫ Nortriptyline Verapamil Gabapentin Pregabalin Ace-inhibitors
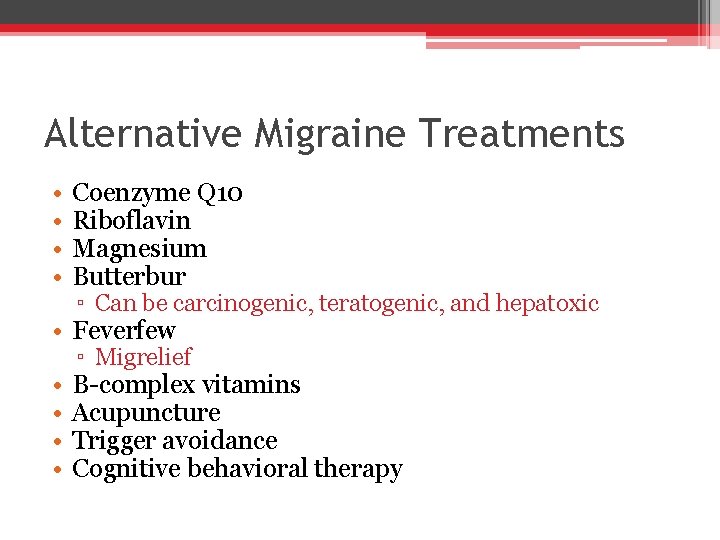
Alternative Migraine Treatments • • Coenzyme Q 10 Riboflavin Magnesium Butterbur ▫ Can be carcinogenic, teratogenic, and hepatoxic • Feverfew • • ▫ Migrelief B-complex vitamins Acupuncture Trigger avoidance Cognitive behavioral therapy
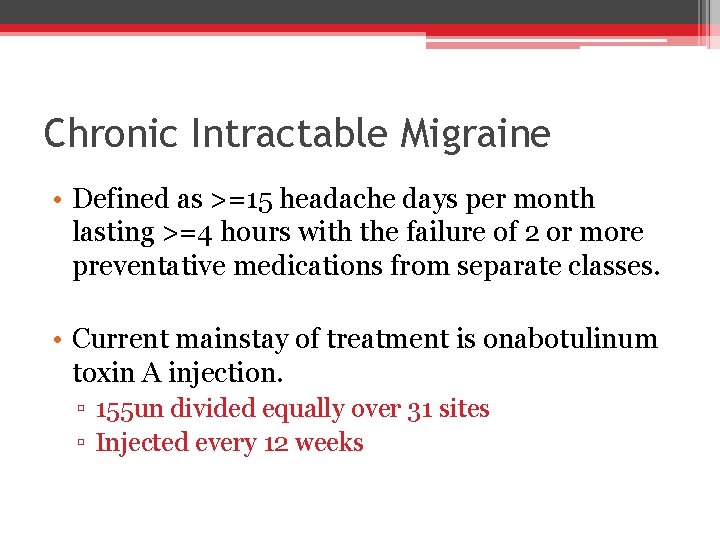
Chronic Intractable Migraine • Defined as >=15 headache days per month lasting >=4 hours with the failure of 2 or more preventative medications from separate classes. • Current mainstay of treatment is onabotulinum toxin A injection. ▫ 155 un divided equally over 31 sites ▫ Injected every 12 weeks
Hemicrania Continua • The location is frontal, retro-orbital, or temporal • Pain is widely variable in severity and nature, but is usually unrelenting • Often associated with cranial autonomic symptoms • Response to indomethacin is required by strict diagnostic definition
Hemicrania Continua Treatment • Indomethacin is the mainstay of treatment ▫ Dosing 25 -75 mg every 8 hours is typical (doses up to 200 mg per day are used) ▫ Often limited by GI side effects ▫ Other oral alternatives: COX-2 inhibitors, topiramate, verapamil, melatonin, and gabapentin ▫ Rare invasive treatments include onabotulinum toxin A injection, vagus nerve stimulation, and occipital nerve stimulation
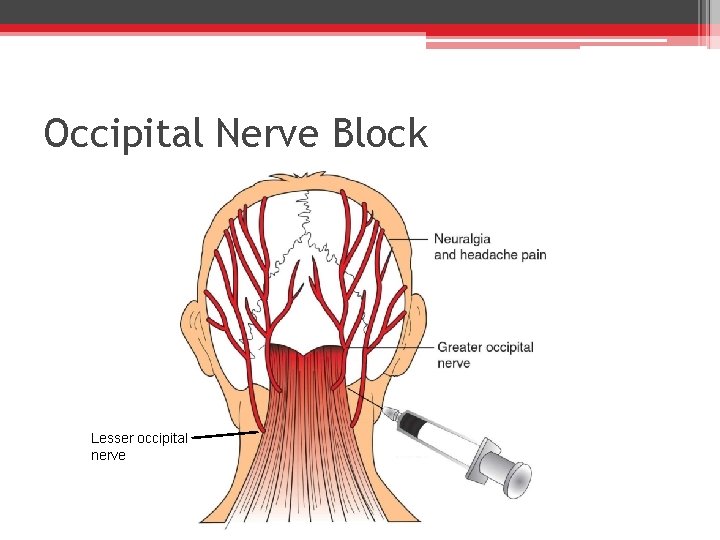
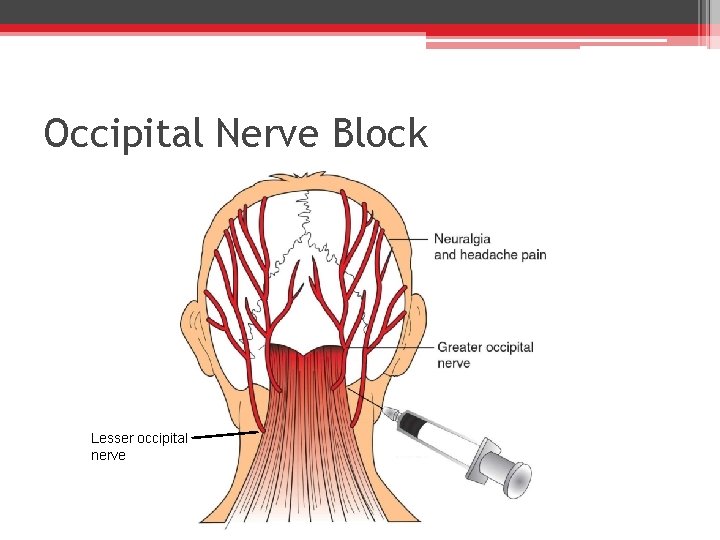
Occipital Neuralgia • Occipital head pain or dysesthesias that are caused by irritation or damage to the occipital or upper cervical nerves. • Greater occipital nerve originates from the 2 nd cervical nerve and perforates the semispinalis capitus and trapezius muscles. • Can be unilateral or bilateral
Occipital Neuralgia • Diagnosis ▫ ▫ Paroxyms of pain in the correct distribution Dysesthesia or allodynia to the area Occipital tender points Pain improved by occipital nerve block
Occipital Neuralgia • Conservative management ▫ Heat or cold compresses • Occipital nerve block • Medical management ▫ TCAs, Carbemazepine, or gabapentin • Rarely, occipital nerve stimulation
Occipital Nerve Block Lesser occipital nerve
Other Associated Head Pain • Trigeminal neuralgia • Low pressure headache • Traumatic vascular dissections • Cluster headaches
References Bendtsen L, et al. EFNS guideline on the treatment of tension-type headache—report of an EFNS task force. European Journal of Neurology 2010: 17(11): 1318 -1325. Goadsby P, Lipton R, and Ferrari M. Migraine—current understanding and treatment. New England Journal of Medicine 2002 346(4): 257 -270. Handel T and Kaplan R. Occipital Neuralgia. Essential of physical medicine and rehabilitation. Lippincott Williams and Wilkins, Philadelphia, PA 2002. 38. Headache Classification Committee of the International Headache Society. The International Classification of Headache Disorders, 3 rd Edition. Cephalgia 2013; (33): 629. Headache Classification Committee of the International Headache Society. The International Classification of Headache Disorders, 2 nd edition. Cephalgia 2004; (24) 9 -160. Krymchantowski, A and Moreira, P. Outpatient detoxification in chronic migraine: comparison of strategies. Cephalagia. 2003; 23(10): 982 -993. Lance, J and Goadsby, P. Cranial neuralgias and central causes of facial pain. Mechanisms and management of headache, Elsevier Butterworth Heinemann, Philadelphia, PA 2005. 333. Langlois, etal. The epidemiology and impact of traumatic brain injury: A brief overview. Journal of head trauma rehabilitation 2006; 21 (5): 375– 378. Mc. Crory, etal. Consensus statement on concussion and sport: The fourth international converts on concussion in sport. November 2012. British Journal of Sports Medicine. 2013; 47 (5): 252 - 258. Preiss-Farzanegan, etal. The relationship between gender and postconcussion symptoms after sport related mild traumatic brain injury. Physical medicine rehabilitation 2009; 1 (1934– 1482): 245– 253. Prins, etal. Repeated mild traumatic brain injury: Mechanisms of cerebral vulnerability. Journal of nerve trauma 2013; 30 to (1): 30– 38. Schneider, etal. The effects of rest and treatment following sport related concussion: A systematic review of the literature. British Journal of Sports Medicine. 2013; 47 (5): 304– 307. Silberstien S. Practice parameter: evidence based guidelines for migraine headache. American Academy of Neurology 2000; 55(6): 754 -762.
 Apsasia
Apsasia Promotion from assistant to associate professor
Promotion from assistant to associate professor Cuhk assistant professor salary
Cuhk assistant professor salary Baudelaire corrispondenze
Baudelaire corrispondenze Charles manson charles luther manson
Charles manson charles luther manson Alex clarke naked
Alex clarke naked Nucleo intermedio
Nucleo intermedio Dr nick clarke
Dr nick clarke Situational crime prevention definition
Situational crime prevention definition Renata clarke fao
Renata clarke fao Rob clarke art
Rob clarke art Dr allison clarke
Dr allison clarke Reference frame theory
Reference frame theory Miracle on st david's day gillian clarke
Miracle on st david's day gillian clarke Dr tatyan clarke
Dr tatyan clarke Clarke's analysis of drugs and poisons
Clarke's analysis of drugs and poisons Sonji clarke
Sonji clarke Catherine clarke psychologist
Catherine clarke psychologist Ryan clarke drugs
Ryan clarke drugs Todd clarke albuquerque
Todd clarke albuquerque Clarke
Clarke Griff by austin c clarke summary
Griff by austin c clarke summary Dr randolph clarke
Dr randolph clarke Alan turing julius mathison turing
Alan turing julius mathison turing Shrove tuesday significato
Shrove tuesday significato Pinire
Pinire Who won the battle of kettle creek
Who won the battle of kettle creek Clarke
Clarke Shaune clarke
Shaune clarke Woofound
Woofound Tr rubrospinalis
Tr rubrospinalis What is citation
What is citation