Postconcussion syndrome The term Postconcussion syndrome or postconcussional













- Slides: 28



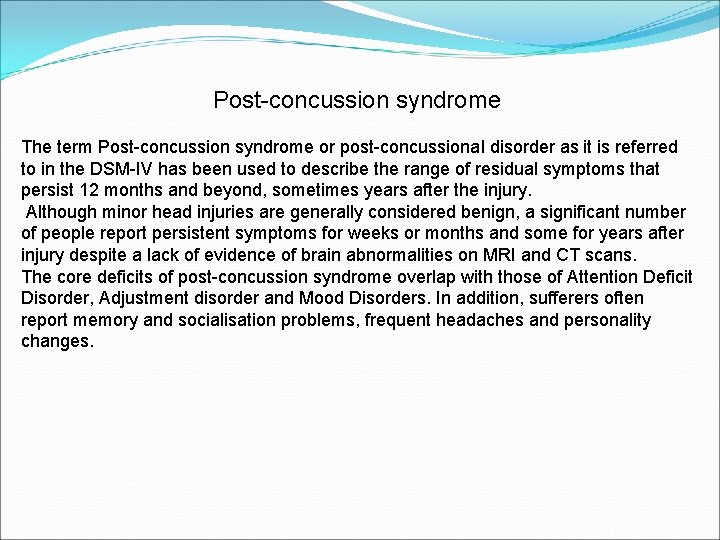
Post-concussion syndrome The term Post-concussion syndrome or post-concussional disorder as it is referred to in the DSM-IV has been used to describe the range of residual symptoms that persist 12 months and beyond, sometimes years after the injury. Although minor head injuries are generally considered benign, a significant number of people report persistent symptoms for weeks or months and some for years after injury despite a lack of evidence of brain abnormalities on MRI and CT scans. The core deficits of post-concussion syndrome overlap with those of Attention Deficit Disorder, Adjustment disorder and Mood Disorders. In addition, sufferers often report memory and socialisation problems, frequent headaches and personality changes.

The cluster of symptoms reported by these patients is referred to as the Post-concussion syndrome. The following are amongst the most commonly reported symptoms of postconcussion syndrome Attention deficits, difficulty sustaining mental effort. Fatigue and tiredness Impulsivity, irritability Low frustration threshold Temper outbursts and changes in mood Learning and memory problems Impaired planning and problem solving Inflexibility, concrete thinking Lack of initiative Dissociation between thought and action Communication difficulties Socially inappropriate behavior Self centeredness and lack of insight Poor self awareness Impaired balance Headaches and Dizziness Personality Changes
גופניות למחלות נפשית קומורבידיות Adjustment Disorder Psychiatric Disorder due to medical condition The following features suggest a medical origin to psychiatric symptoms: Known underlying medical condition Atypical presentation of a specific psychiatric diagnosis Absence of personal and family history of psychiatric illnesses Treatment resistance or unusual response to treatment Sudden onset of mental symptoms Abnormal vital signs Waxing and waning mental status


Mental disorder affecting medical condition (e. g. , an Axis I disorder such as major depressive disorder delaying recovery from a myocardial infarction, depressive symptoms delaying recovery from surgery; anxiety exacerbating asthma) Personality traits or coping style affecting medical condition (e. g. , pathological denial of the need for surgery in a patient with cancer, hostile, pressured behavior contributing to cardiovascular disease) Maladaptive health behaviors affecting medical condition (e. g. , lack of exercise, unsafe sex, overeating) Stress-related physiological response affecting general medical condition (e. g. , stress-related exacerbations of ulcer, hypertension, arrhythmia, or tension headache) Other unspecified psychological factors affecting medical condition (e. g. , interpersonal, cultural, or religious factors)
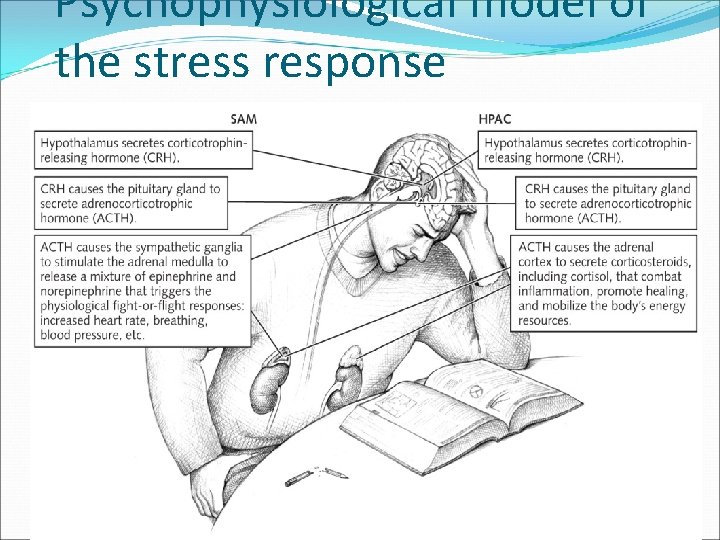
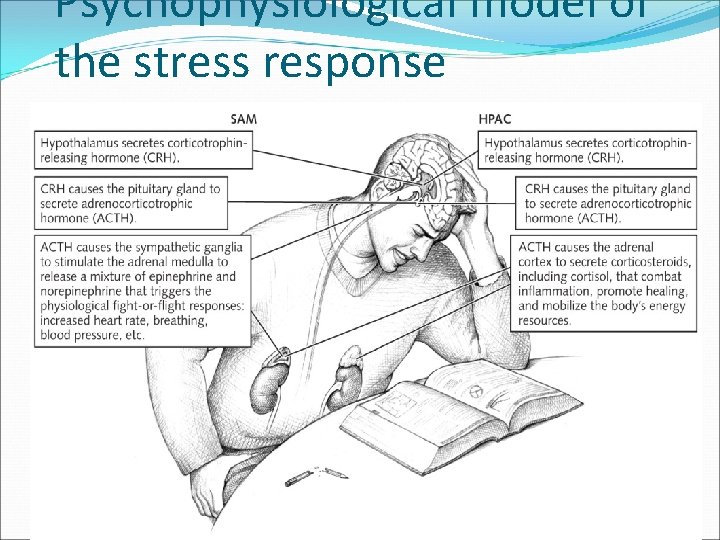
Psychophysiological model of the stress response
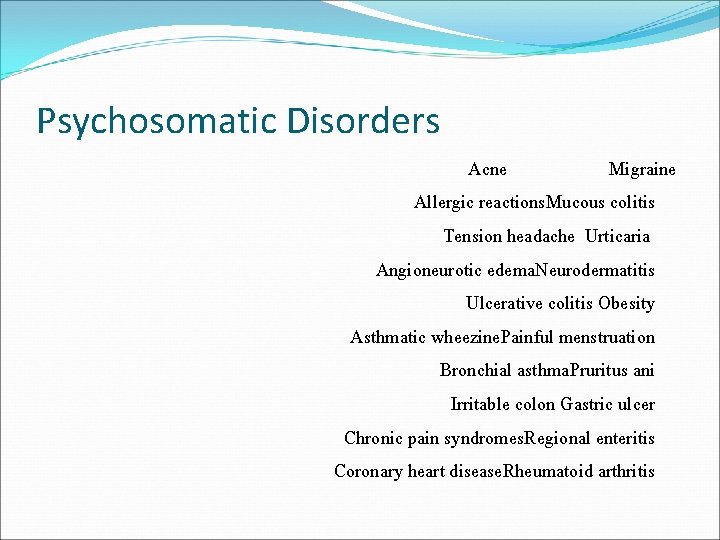
Psychosomatic Disorders Acne Migraine Allergic reactions. Mucous colitis Tension headache Urticaria Angioneurotic edema. Neurodermatitis Ulcerative colitis Obesity Asthmatic wheezine. Painful menstruation Bronchial asthma. Pruritus ani Irritable colon Gastric ulcer Chronic pain syndromes. Regional enteritis Coronary heart disease. Rheumatoid arthritis
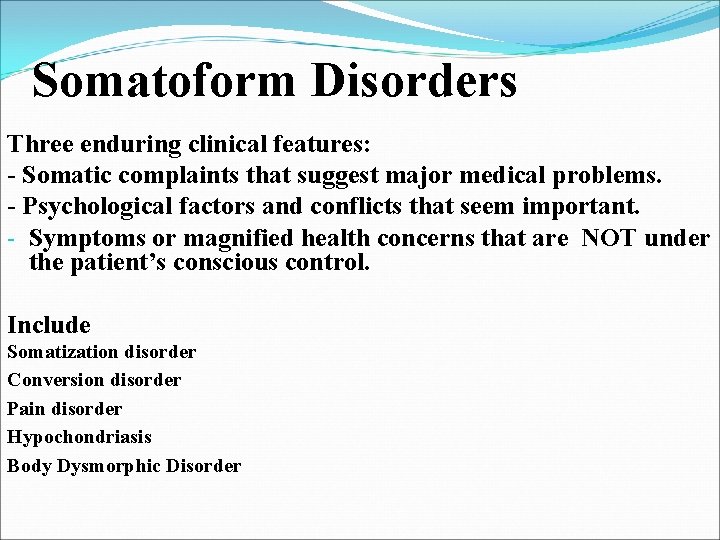
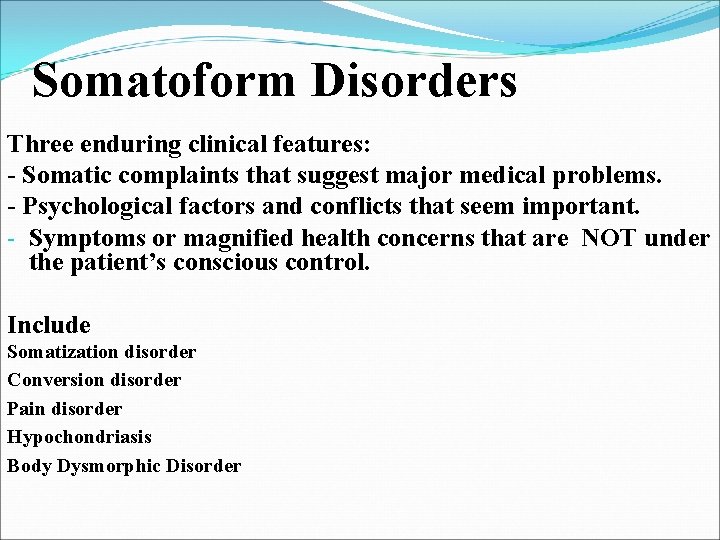
Somatoform Disorders Three enduring clinical features: - Somatic complaints that suggest major medical problems. - Psychological factors and conflicts that seem important. - Symptoms or magnified health concerns that are NOT under the patient’s conscious control. Include Somatization disorder Conversion disorder Pain disorder Hypochondriasis Body Dysmorphic Disorder
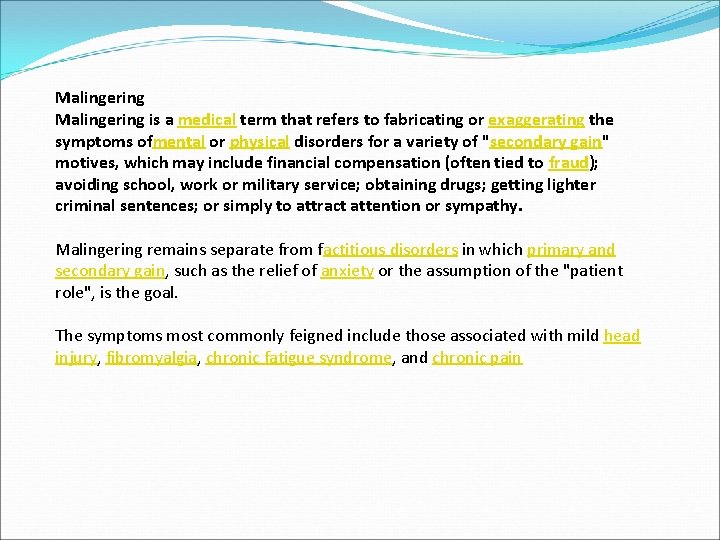
Malingering is a medical term that refers to fabricating or exaggerating the symptoms ofmental or physical disorders for a variety of "secondary gain" motives, which may include financial compensation (often tied to fraud); avoiding school, work or military service; obtaining drugs; getting lighter criminal sentences; or simply to attract attention or sympathy. Malingering remains separate from factitious disorders in which primary and secondary gain, such as the relief of anxiety or the assumption of the "patient role", is the goal. The symptoms most commonly feigned include those associated with mild head injury, fibromyalgia, chronic fatigue syndrome, and chronic pain

Detection Some features at presentation which are unusual in genuine cases include: Dramatic or atypical presentation Vague and inconsistent details, although possibly plausible on the surface Long medical record with multiple admissions at various hospitals in different cities Knowledge of textbook descriptions of illness Symptoms and signs that do not conform to an identifiable medical or mental disorder An unusual grasp of medical terminology Employment in a medically related field Presentation in the emergency department during times when obtaining old medical records is hampered or when experienced staff are less likely to be present (e. g. , holidays, late Friday afternoons)

Acceptance, with equanimity, of the discomfort and risk of diagnostic procedures Acceptance, with equanimity, of the discomfort and risk of surgery Substance abuse, especially of prescribed analgesics and sedatives Symptoms or behaviors only present when the patient knows he is being observed Controlling, hostile, angry, disruptive, or attention-seeking behavior during hospitalization Reporting of wild psychological symptoms, and silly wrong answers on questionnaires, not likely in patients with similar but real conditions. Fluctuating clinical course, including rapid development of complications or a new pathology if the initial workup findings prove negative Coinciding indigence or homelessness of the patient, with impending cold weather and a need for indoor lodgings.

Three tests commonly used to determine malingering are: Computerized Assessment of Response Bias (CARB) Minnesota Multiphasic Personality Inventory (MMPI) (see Validity scales) The Test of Memory Malingering (TOMM)