PreOperative Anemia Lessons from Surgery with Application to


- Slides: 42
Pre-Operative Anemia: Lessons from Surgery with Application to PCI? Kathrine P Frey, MD Blood Management Medical Director Fairview Southdale Hospital Edina, MN Kathrine Frey, MD kfrey 2@fairview. org 952 -4122700 1
Credentials and Conflicts of Interest • Pathologist (AP/CP/Transfusion Medicine) and Director of Patient Blood Management, Fairview Southdale Hospital • Chief Medical Officer, Patient Readiness Institute, outsourced peri-surgical blood management program for hospitals. Kathrine Frey, MD kfrey 2@fairview. org 952412 -2700 2
Disclaimer No off-label use of medications or commercial products will be discussed in this presentation. Kathrine Frey, MD kfrey 2@fairview. org 952412 -2700 3
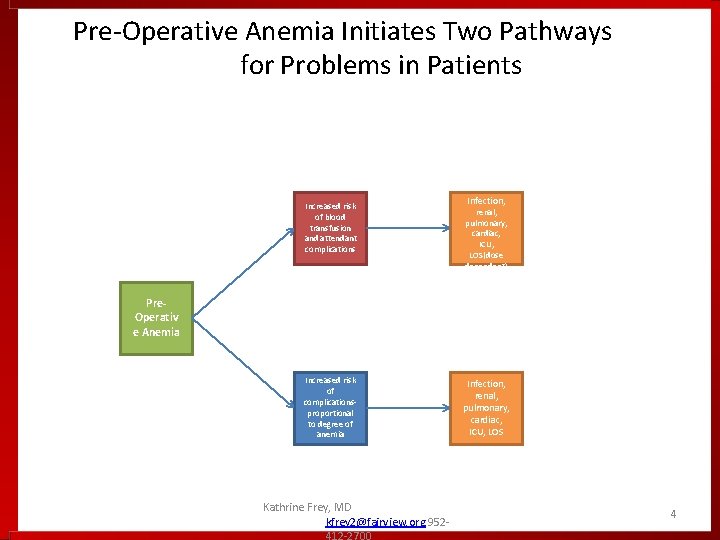
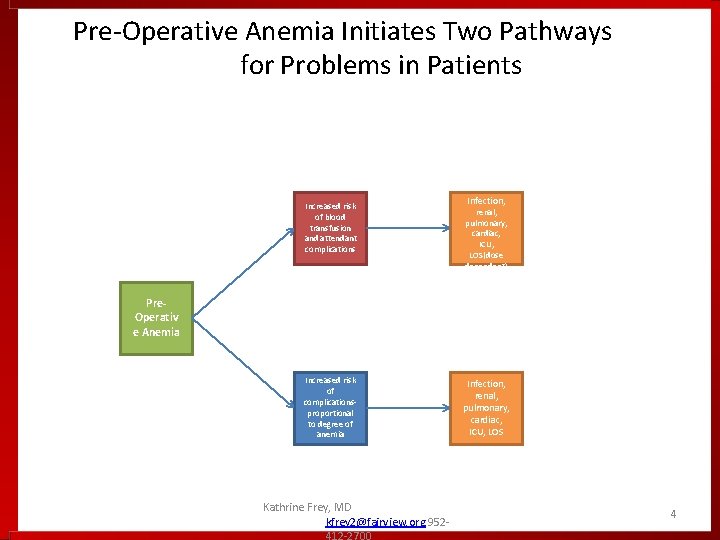
Pre-Operative Anemia Initiates Two Pathways for Problems in Patients Increased risk of blood transfusion and attendant complications Infection, renal, pulmonary, cardiac, ICU, LOS(dose dependent) Pre. Operativ e Anemia Increased risk of complicationsproportional to degree of anemia Kathrine Frey, MD kfrey 2@fairview. org 952412 -2700 Infection, renal, pulmonary, cardiac, ICU, LOS 4
5
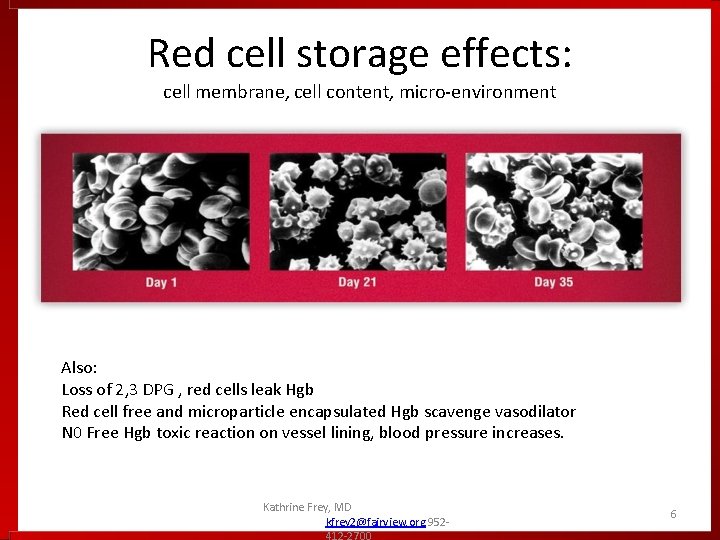
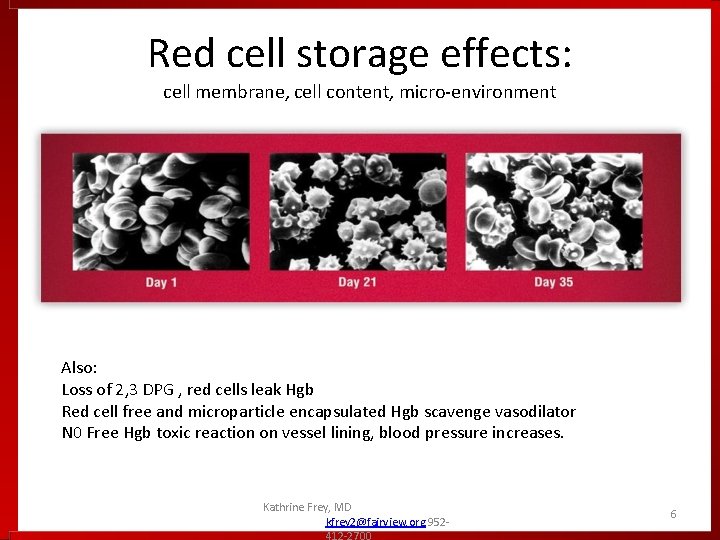
Red cell storage effects: cell membrane, cell content, micro-environment Also: Loss of 2, 3 DPG , red cells leak Hgb Red cell free and microparticle encapsulated Hgb scavenge vasodilator N 0 Free Hgb toxic reaction on vessel lining, blood pressure increases. Kathrine Frey, MD kfrey 2@fairview. org 952412 -2700 6
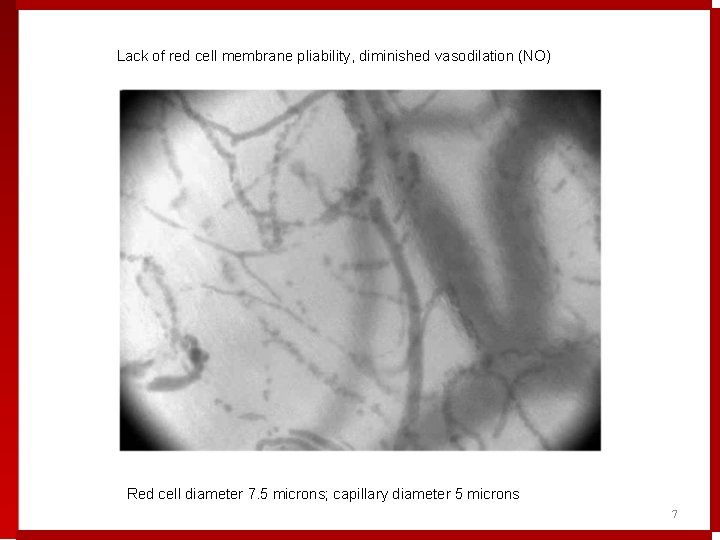
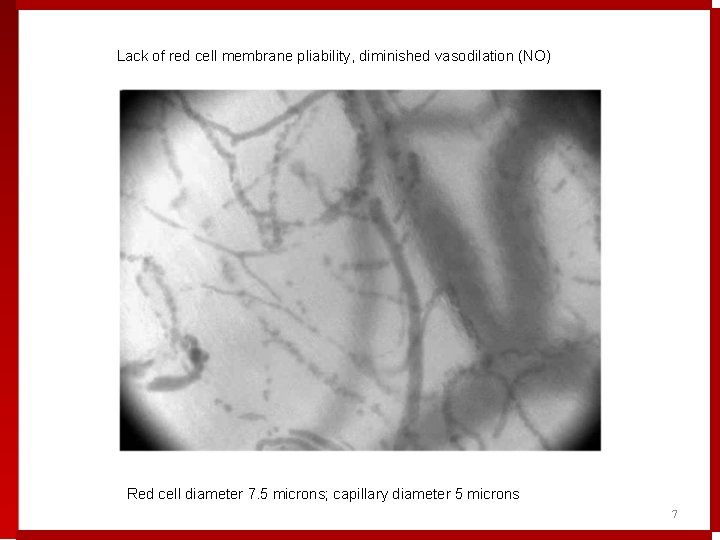
Lack of red cell membrane pliability, diminished vasodilation (NO) Red cell diameter 7. 5 microns; capillary diameter 5 microns 7
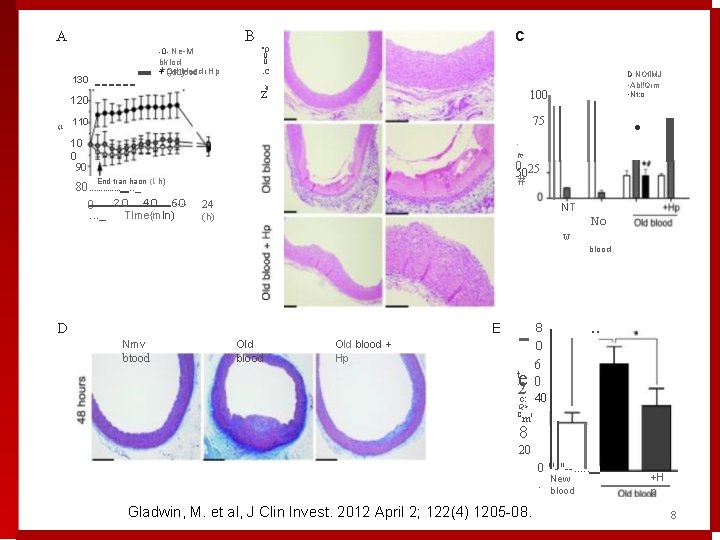
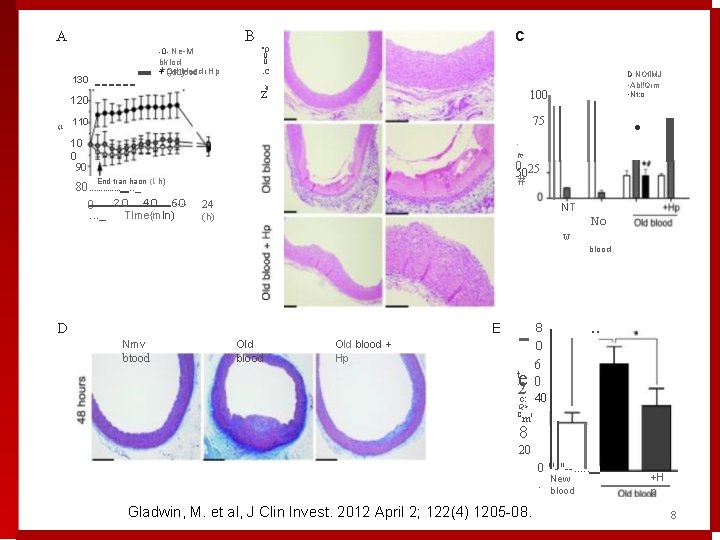
A 130 120 /; l ------- c B 0 Ne M "O bklod + blood I Hp + Od ()dtljood . c 0 0 Q) z D NOfl. MJ • Abl!Qrm • Nt: o 100 75 110 10 0 90 • · ft! 0 25 50 # End tran haon (1 h) 80. . . . _ . . . 20 40 60 0. . . _ Tlme{mln) 24 NT (h) No w D E Nmv btood Old blood + Hp 8 0 t 6 0 c: 40 e 2 Q> C l blood . . m 8 20 0 "'-"--. . . New blood Gladwin, M. et al, J Clin Invest. 2012 April 2; 122(4) 1205 08. +H p 8
-What % of red cell use is believed to be avoidable -What % of red cells in the US are given to CV patients? • • 20% 30% 40% 50% Kathrine Frey, MD kfrey 2@fairview. org 952412 -2700 9
Best interest for patient having non emergent high blood loss surgery is: • An adequate red cell mass prior to surgery • Understanding of red cell regeneration capability (or not) • A peri-operative plan for safe transfusion avoidance or minimization Kathrine Frey, MD 952 -412 -2700 10
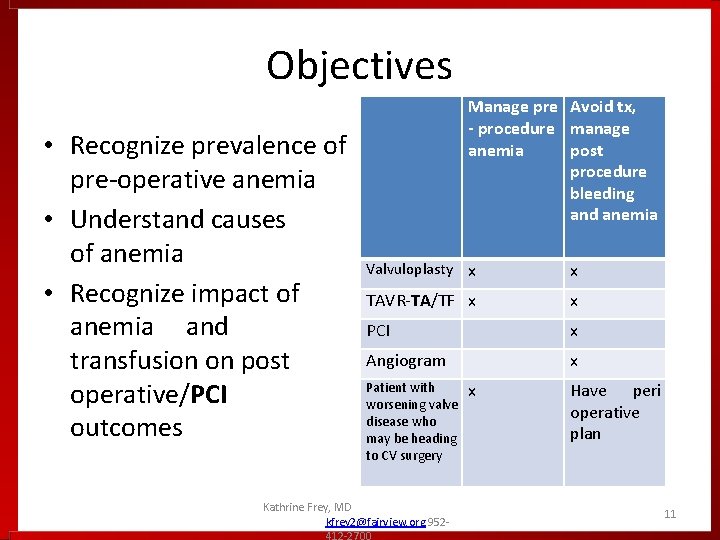
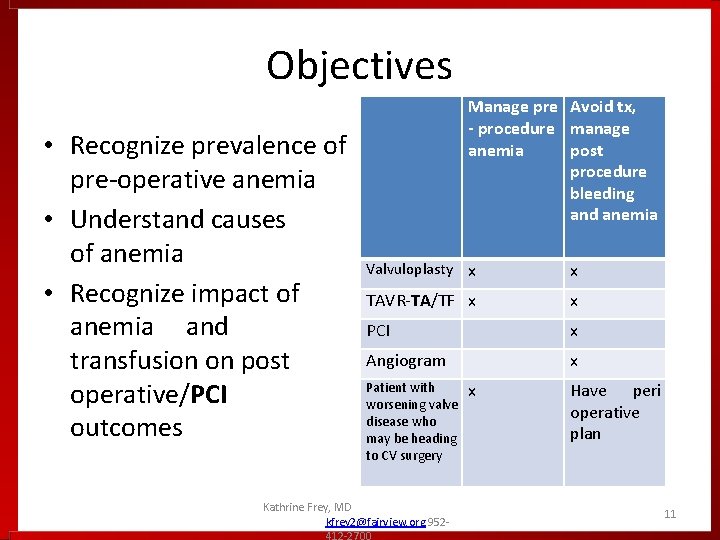
Objectives • Recognize prevalence of pre-operative anemia • Understand causes of anemia • Recognize impact of anemia and transfusion on post operative/PCI outcomes Manage pre Avoid tx, - procedure manage anemia post procedure bleeding and anemia Valvuloplasty x x TAVR-TA/TF x x PCI x Angiogram x Patient with worsening valve disease who may be heading to CV surgery Kathrine Frey, MD kfrey 2@fairview. org 952412 -2700 x Have peri operative plan 11
Anemia • WHO definition- Hgb < 12 g/d. L (f, pre - menopausal), < 13 g/d. L (m) • 20% of world population, iron deficiency most common cause • CV Surgery patients overall 40%, CABG @ 20 - 30 %, Valve replacement 50 -65% Kathrine Frey, MD kfrey 2@fairview. org 952412 -2700 12
Anemia in High Blood Loss Surgery Patients: overall 40 +%, CABG @ 20 -30%, Valve replacement 50 -65% • Women disadvantaged by lower Hgb cutoff in addition to lower body mass, red cell mass and blood volume • STS recommends minimum Hgb 12. 9 for males and females prior to non-emergent CV surgery. Kathrine Frey, MD kfrey 2@fairview. org 952412 -2700 13
Other risks for patients • Transfusion variability: often 3 or > fold difference in surgeons doing same CV procedure ( can be 5 -95% of patients) • Suggested that elective first time CV surgery patients receive RBCs < 10% of the time, other components <1% of the time • Modifications needed- manage anemia, address transfusion appropriateness Kathrine Frey, MD kfrey 2@fairview. org 952412 -2700 14
Pre-op Anemia: A Big, Bad, Modifiable Problem • Addressable • Awareness not enough, “modifiable” requires new “doing” (eval and treatment) • “Doing”- not by surgeon or surgery service, surgeon directed, patient and surgeoncentric, process could be activated by Cardiologist? • Current process problem, patients get to PCD for pre-op check close to time of surgery Kathrine Frey, MD kfrey 2@fairview. org 952412 -2700 15

Understand causes and diagnosis of anemia Kathrine Frey, MD kfrey 2@fairview. org 952412 -2700 16
Anemia • Decreased Production of RBCs or Hgb • Heme: Iron deficiency (absolute lack of Fe, or inaccessible Fe) • Globin chains: Vitamin B 12, folate • Red cells: Erythropoietin (renal insufficiency) • Marrow Failure: Chronic Disease, medications • Increased Red Cell Destruction • Blood loss (GI, GU) Hemolysis (intra and extravascular) Kathrine Frey, MD kfrey 2@fairview. org 952412 -2700 17
Pre-Surgical Anemia Causes • Iron deficiency (30%)- poor diet, blood loss, impaired absorption • Anemia of Chronic Disease ( impaired absorption, RE blockade) (25%) • Chronic Kidney Disease (15 -20%) • B 12 deficiency • Folate deficiency • Medication related ( inhibited erythropoiesis and/or anticoagulant-associated bleeding) • Blood loss- Recent Invasive Procedure ( ex. Angiogram can have 1 -2 gm or > Hgb loss into soft tissues ) • Unexplained Anemia of the elderly (UAE) MULTIFACTORIAL (ex. CKD + IDA + Medication components) Kathrine Frey, MD kfrey 2@fairview. org 952412 -2700 18
Iron Deficiency- Anemia is Late Stage • Iron depletion: near absent storage iron, no anemia, asymptomatic • Iron deficiency without anemia-stored and blood borne iron below normal, can be asymptomatic or symptomatic (fatigue) • Iron deficiency anemia- initially normocytic, as severity increased, microcytic… Kathrine Frey, MD kfrey 2@fairview. org 952 -4122700 19
Iron Matters: Beyond Anemia • Iron deplete and deficient patients will have difficulty making new red cells to replenish surgical and in hospital blood loss • Good to know who these patients are so iron stores can be replenished, pre and post OP. • Iron important in 200 + in vivo chemical reactions, including in muscle in ATP production • Iron deplete and deficient, anemic and non anemic CHF patients have improved function (LVEF, 6 min walk) and QOL when iron levels restored. Kathrine Frey, MD kfrey 2@fairview. org 952412 -2700 20
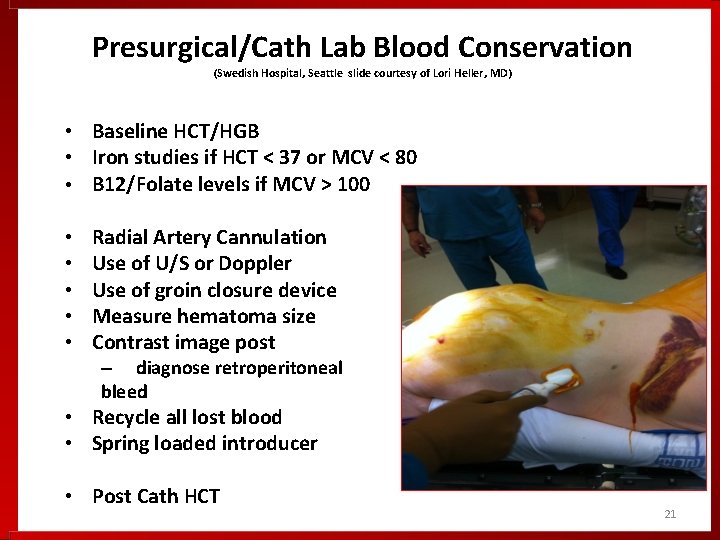
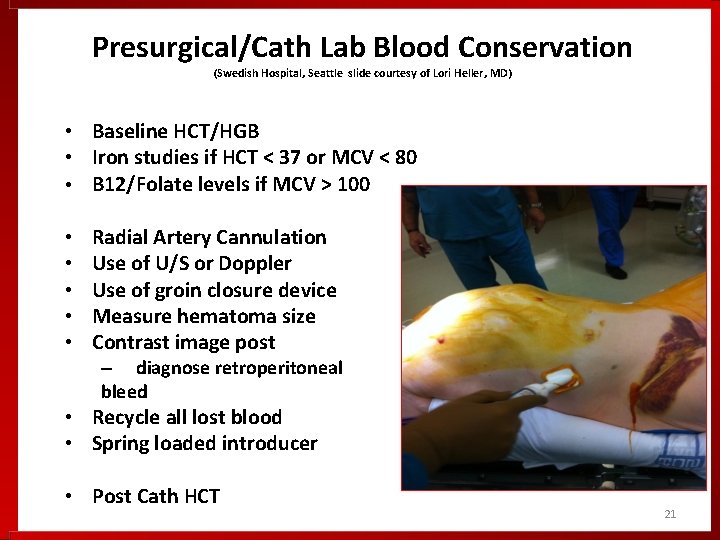
Presurgical/Cath Lab Blood Conservation (Swedish Hospital, Seattle slide courtesy of Lori Heller, MD) • Baseline HCT/HGB • Iron studies if HCT < 37 or MCV < 80 • B 12/Folate levels if MCV > 100 • • • Radial Artery Cannulation Use of U/S or Doppler Use of groin closure device Measure hematoma size Contrast image post – diagnose retroperitoneal bleed • Recycle all lost blood • Spring loaded introducer • Post Cath HCT 21
Mehta SR, Jolly SS, Cairns J, et al. Effects of Radial Versus Femoral Artery Access in Patients With Acute Coronary Syndromes With or Without ST- Segment Elevation. Journal of the American College of Cardiology. 2012 • RIVAL trial, multinational, prospective, femoral vs radial access in 7021 patients with ACS (STEMI and non-STEMI) • Reduced vascular access complications in radial group • STEMI patients with radial PCI had 40% decrease in composite morbidity and mortality and 61% decrease in all cause mortality. Kathrine Frey, MD kfrey 2@fairview. org 952412 -2700 22
Iron Deficiency in CV Surgery Patients Preoperative iron deficiency increases transfusion requirements and fatigue in cardiac surgery patients: a prospective observational study. Piednoir, P. et al, Eur J Anesthiol 28(11) 798 -801. • Iron deficiency searched for in anemic and non-anemic patients • 100 consecutive patients, iron studies done day of surgery, 37 with iron deficiency • IDA patients WITHOUT anemia received more blood than iron replete non-anemic patients Kathrine Frey, MD kfrey 2@fairview. org 952412 -2700 23
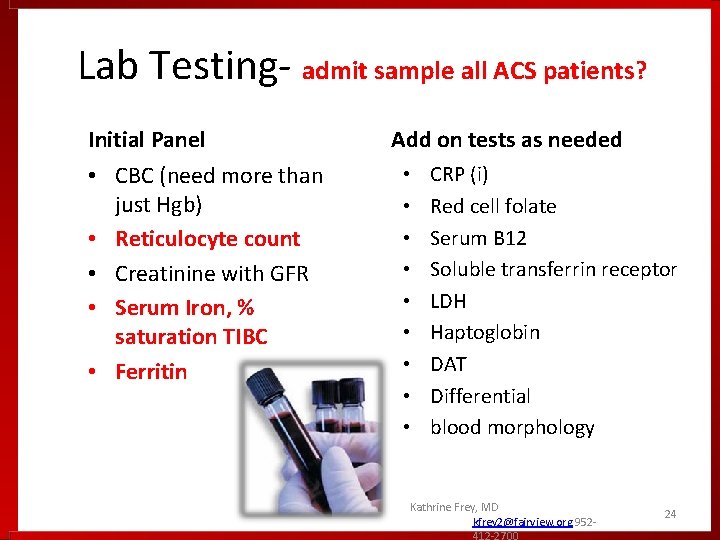
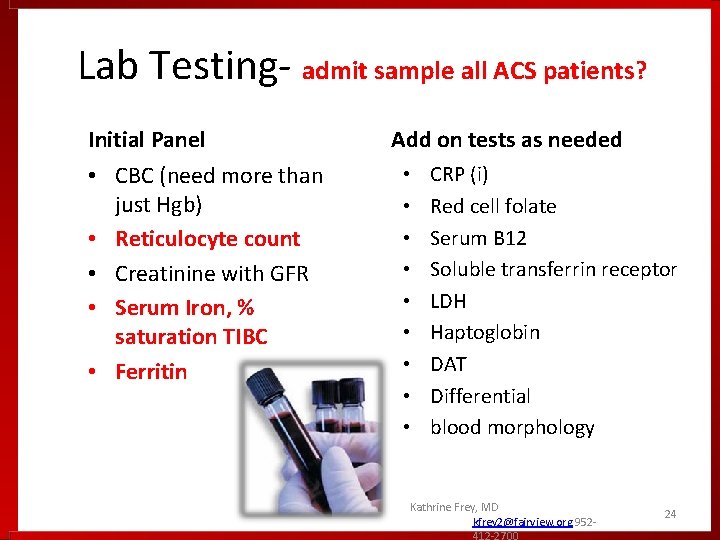
Lab Testing- admit sample all ACS patients? Initial Panel • CBC (need more than just Hgb) • Reticulocyte count • Creatinine with GFR • Serum Iron, % saturation TIBC • Ferritin Add on tests as needed • • • CRP (i) Red cell folate Serum B 12 Soluble transferrin receptor LDH Haptoglobin DAT Differential blood morphology Kathrine Frey, MD kfrey 2@fairview. org 952412 -2700 24
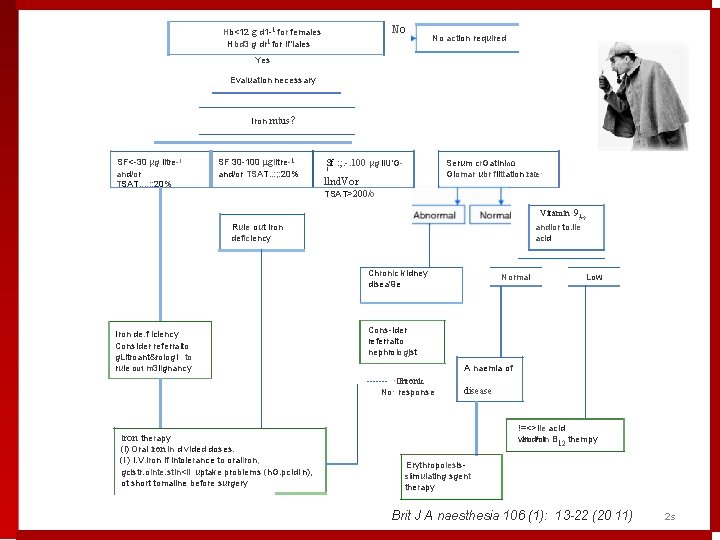
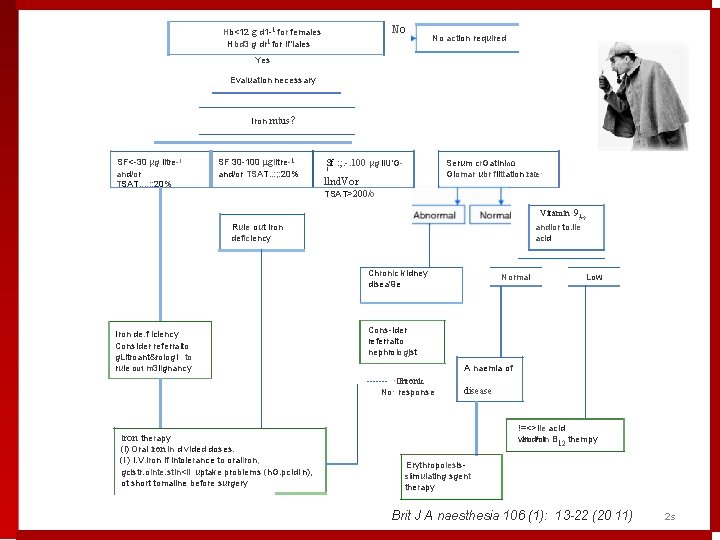
No Hb<12 g d 1 1 for females Hbd 3 g dr 1 for ll"lales No action required Yes Evaluation necessary Iron mtus? SF< 30 µg litre 1 and/or TSAT. . : : 20% SF 30 100 µglitre 1 and/or TSAT. . : ; : 20% Sf : ; . -. 100 µg li. U'G Serum cr. Gatinin. Q Glomar ubr filttation rate· 1 llnd. Vor TSAT>200/o Vitamin 9: <? 1 Rule out iron deficiency andlor to. lie acid Chronic kidney disea'9 e Iron de. f iciency Consider referralto g. Litroant&rologi to rule out m 3 lignancy Low Cons ider referralto nephrologjst A naemia of ------- ·Ghronic No· response Iron therapy (i) Oral iron in d vided doses. (i ) I. V. iron if intolerance to oraliron, gcistr. ointe. stin<ll uptake problems (h. G. pcidi n), ot short tomaline before surgery Normal disease !=<>lie acid. and/or B 12 thempy viro. min Erythropoiesis slimulating sgent therapy Brit J A naesthesia 106 (1): 13 -22 (20 11) 2 s
Impact of Pre-Operative Anemia and Transfusion on Post-Operative Outcomes Kathrine Frey, MD kfrey 2@fairview. org 952412 -2700 26
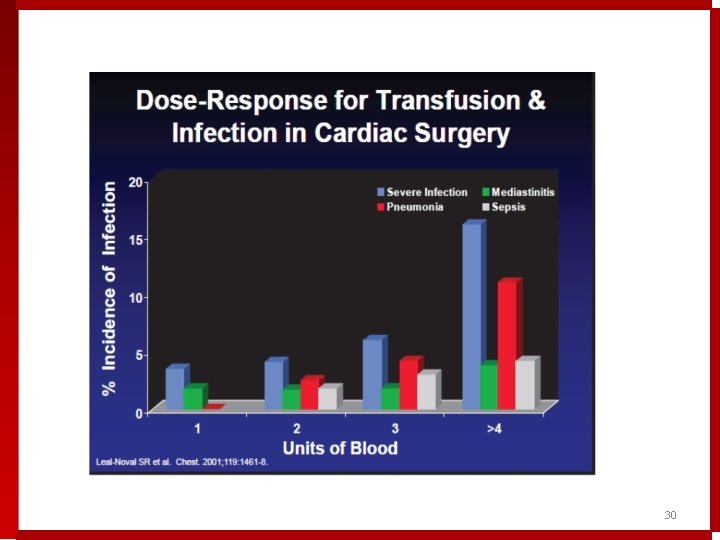
Effect of Preoperative Anemia for CV Patients • Pre-Surgical anemia alone is associated with increased morbidity and mortality • Pre-Surgical anemia is the strongest predictor of need for blood transfusion • Blood Transfusion is also associated with increased morbidity and mortality in a dose dependent manner Kathrine Frey, MD kfrey 2@fairview. org 952412 -2700 27
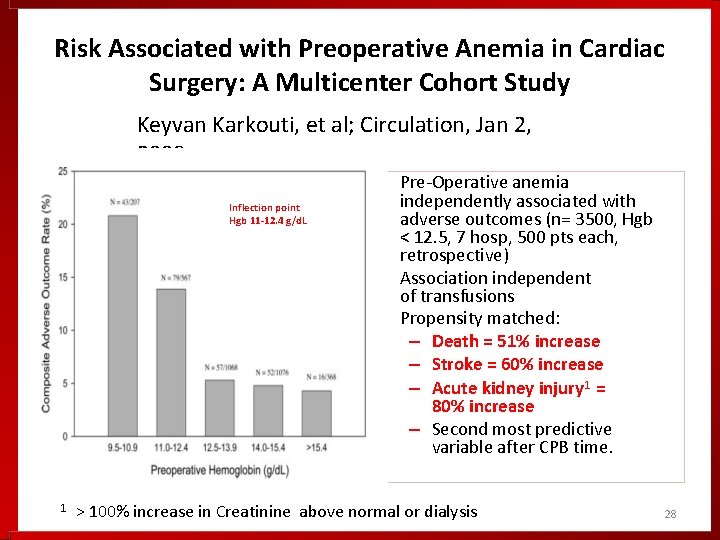
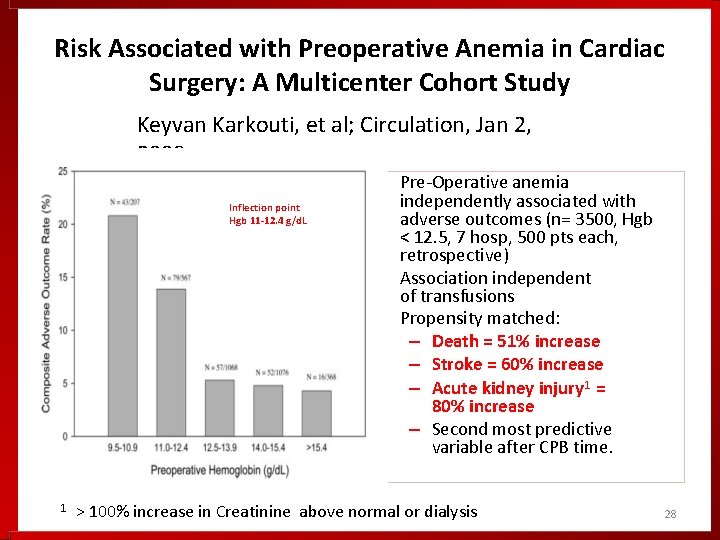
Risk Associated with Preoperative Anemia in Cardiac Surgery: A Multicenter Cohort Study Keyvan Karkouti, et al; Circulation, Jan 2, 2008 • Inflection point Hgb 11 -12. 4 g/d. L • • 1 Pre-Operative anemia independently associated with adverse outcomes (n= 3500, Hgb < 12. 5, 7 hosp, 500 pts each, retrospective) Association independent of transfusions Propensity matched: – Death = 51% increase – Stroke = 60% increase – Acute kidney injury 1 = 80% increase – Second most predictive variable after CPB time. > 100% increase in Creatinine above normal or dialysis 28
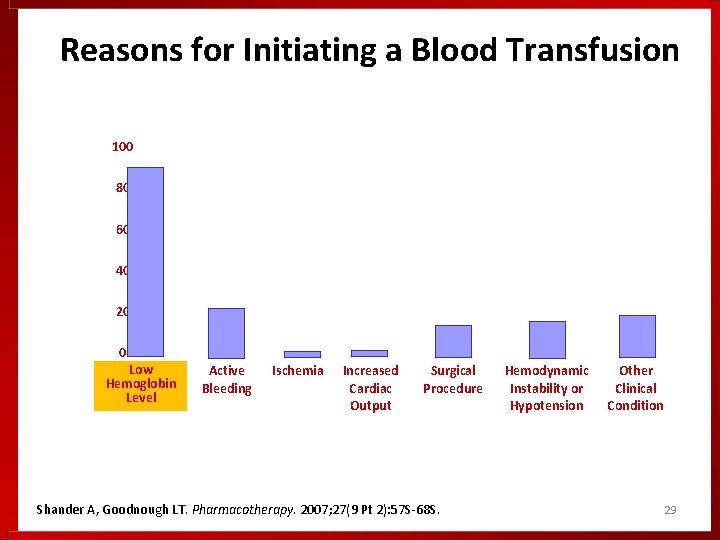
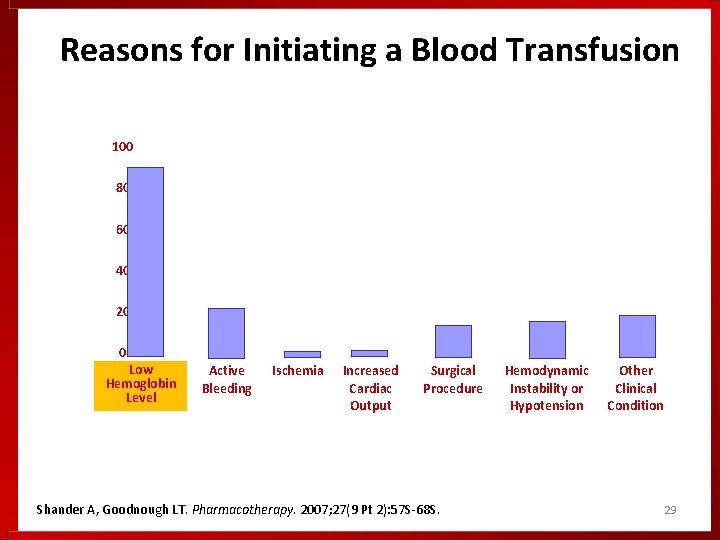
Reasons for Initiating a Blood Transfusion 100 80 60 40 20 0 Low Hemoglobin Level Active Bleeding Ischemia Increased Cardiac Output Surgical Procedure Shander A, Goodnough LT. Pharmacotherapy. 2007; 27(9 Pt 2): 57 S-68 S. Hemodynamic Instability or Hypotension Other Clinical Condition 29
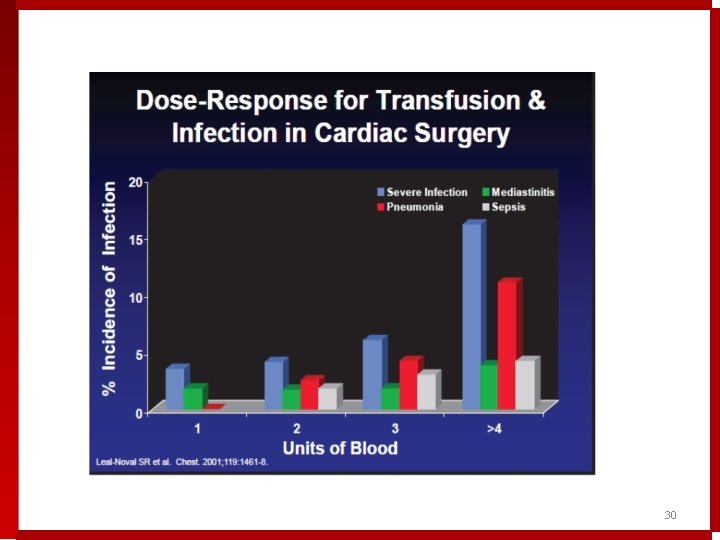
30
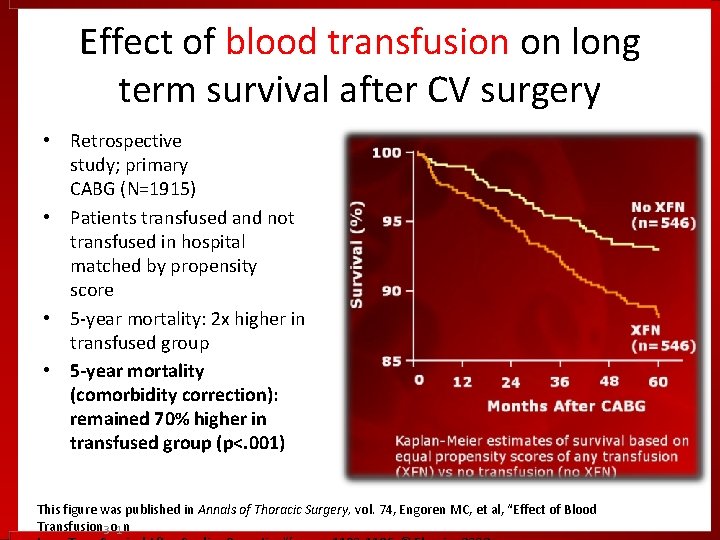
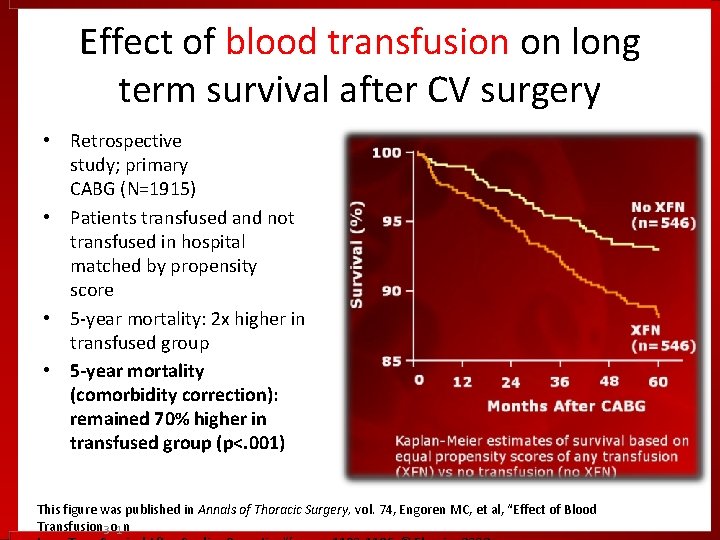
Effect of blood transfusion on long term survival after CV surgery • Retrospective study; primary CABG (N=1915) • Patients transfused and not transfused in hospital matched by propensity score • 5 -year mortality: 2 x higher in transfused group • 5 -year mortality (comorbidity correction): remained 70% higher in transfused group (p<. 001) This figure was published in Annals of Thoracic Surgery, vol. 74, Engoren MC, et al, “Effect of Blood Transfusion 3 o 1 n
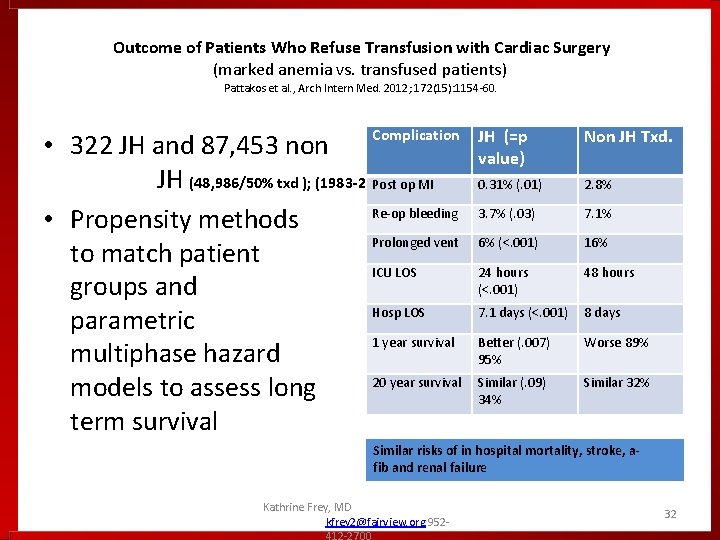
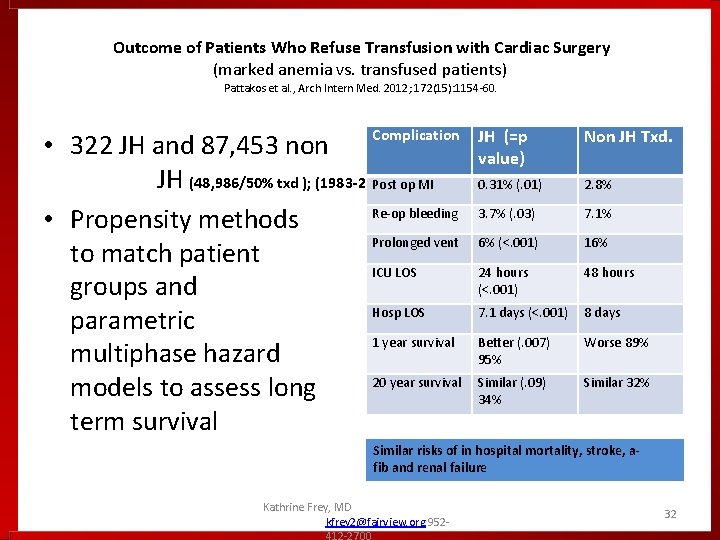
Outcome of Patients Who Refuse Transfusion with Cardiac Surgery (marked anemia vs. transfused patients) Pattakos et al. , Arch Intern Med. 2012; 172(15): 1154 -60. Complication • 322 JH and 87, 453 non JH (48, 986/50% txd ); (1983 -2011 Post op MI Re-op bleeding • Propensity methods Prolonged vent to match patient ICU LOS groups and Hosp LOS parametric 1 year survival multiphase hazard 20 year survival models to assess long term survival ) JH (=p value) Non JH Txd. 0. 31% (. 01) 2. 8% 3. 7% (. 03) 7. 1% 6% (<. 001) 16% 24 hours (<. 001) 48 hours 7. 1 days (<. 001) 8 days Better (. 007) 95% Worse 89% Similar (. 09) 34% Similar 32% Similar risks of in hospital mortality, stroke, afib and renal failure Kathrine Frey, MD kfrey 2@fairview. org 952412 -2700 32
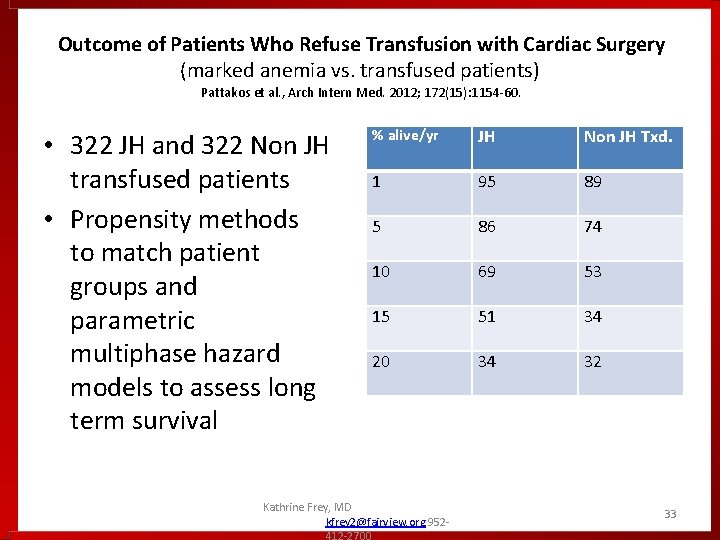
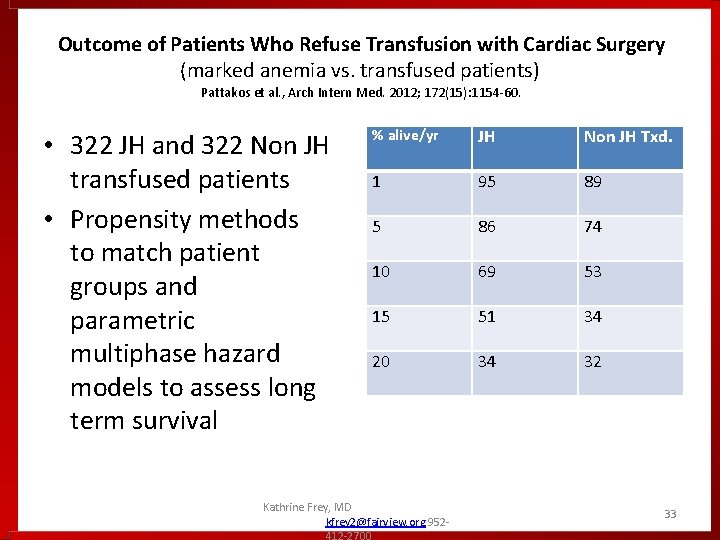
Outcome of Patients Who Refuse Transfusion with Cardiac Surgery (marked anemia vs. transfused patients) Pattakos et al. , Arch Intern Med. 2012; 172(15): 1154 -60. • 322 JH and 322 Non JH transfused patients • Propensity methods to match patient groups and parametric multiphase hazard models to assess long term survival % alive/yr JH Non JH Txd. 1 95 89 5 86 74 10 69 53 15 51 34 20 34 32 Kathrine Frey, MD kfrey 2@fairview. org 952412 -2700 33
• Blood Transfusion and PCI Kathrine Frey, MD kfrey 2@fairview. org 952412 -2700 34
Doyle BJ, Rihal CS, Gastineau D a, Holmes DR. Bleeding, blood transfusion, and increased mortality after percutaneous coronary intervention: implications for contemporary practice. Journal of the American College of Cardiology. 2009; 53(22): 2019 – 27. • 90, 000 patient study • Bleeding complications requiring blood transfusion had 350% increase in mortality • This greater than the risk of death from a MI during the procedure Kathrine Frey, MD kfrey 2@fairview. org 952412 -2700 35
Ergelen M, Uyarel H, Altay S, et al. Prognostic impact of red blood cell transfusion in patients undergoing primary angioplasty for ST elevation myocardial infarction. Coronary artery disease. 2012; . • 2600 STEMI patients undergoing PCI concluded that blood transfusion independently increased in-hospital mortality, long term morbidity and length of stay • Both of these studies emphasized that the best strategy is primary prevention to reduce bleeding complications to avoid transfusion in PCI patients. Kathrine Frey, MD kfrey 2@fairview. org 952412 -2700 36
• On anemia treatment and improved patient outcomes Kathrine Frey, MD kfrey 2@fairview. org 952412 -2700 37
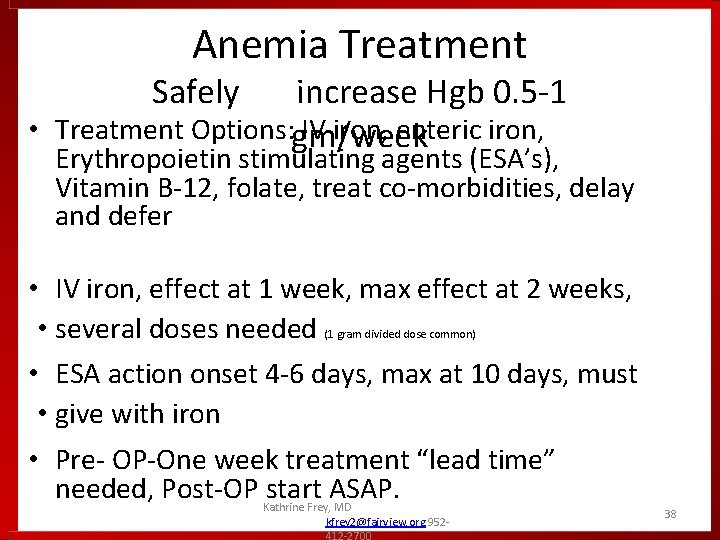
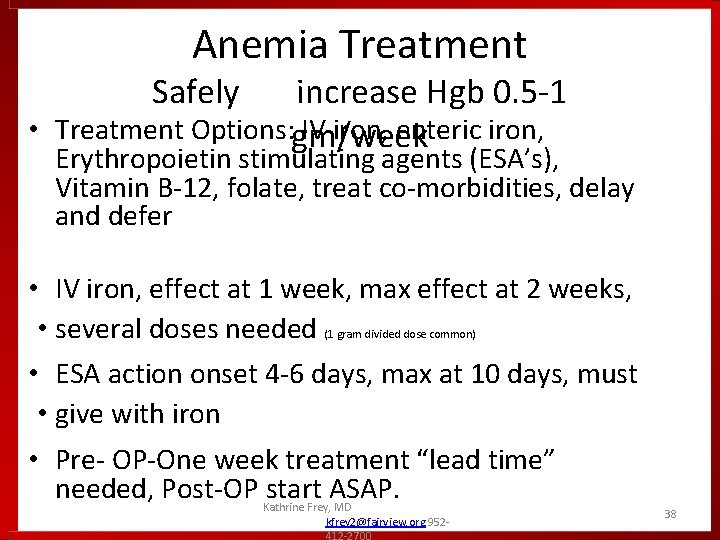
Anemia Treatment Safely increase Hgb 0. 5 -1 • Treatment Options: gm/week IV iron, enteric iron, Erythropoietin stimulating agents (ESA’s), Vitamin B-12, folate, treat co-morbidities, delay and defer • IV iron, effect at 1 week, max effect at 2 weeks, • several doses needed • ESA action onset 4 -6 days, max at 10 days, must • give with iron (1 gram divided dose common) • Pre- OP-One week treatment “lead time” needed, Post-OP start ASAP. Kathrine Frey, MD kfrey 2@fairview. org 952412 -2700 38
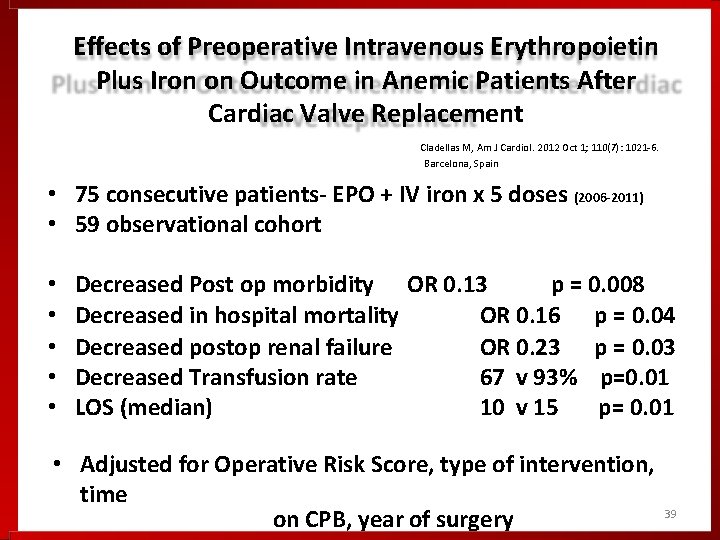
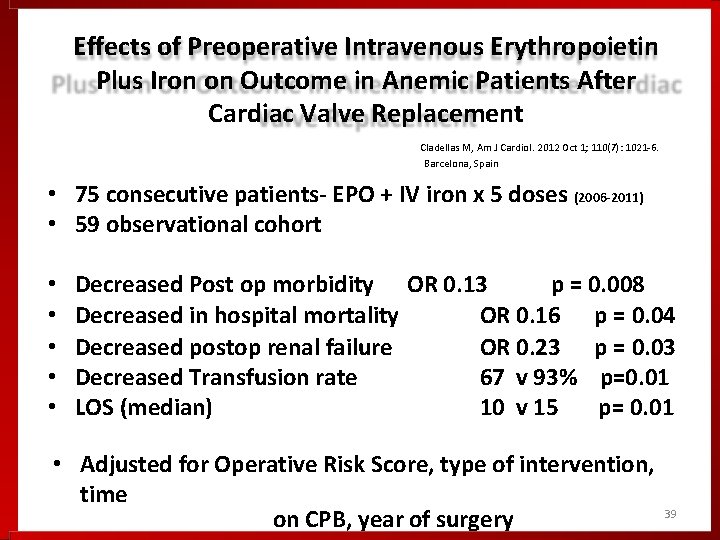
Effects of Preoperative Intravenous Erythropoietin Plus Iron on Outcome in Anemic Patients After Cardiac Valve Replacement Cladellas M, Am J Cardiol. 2012 Oct 1; 110(7): 1021 -6. Barcelona, Spain • 75 consecutive patients- EPO + IV iron x 5 doses (2006 -2011) • 59 observational cohort • • • Decreased Post op morbidity OR 0. 13 p = 0. 008 Decreased in hospital mortality OR 0. 16 p = 0. 04 Decreased postop renal failure OR 0. 23 p = 0. 03 Decreased Transfusion rate 67 v 93% p=0. 01 LOS (median) 10 v 15 p= 0. 01 • Adjusted for Operative Risk Score, type of intervention, time on CPB, year of surgery 39
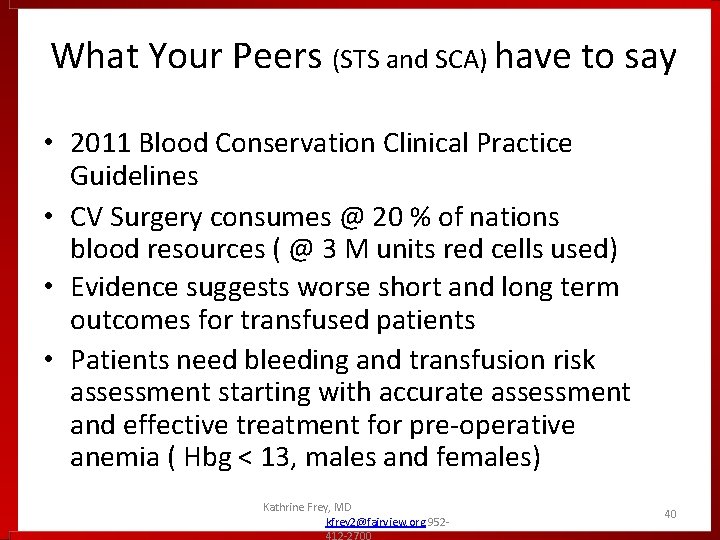
What Your Peers (STS and SCA) have to say • 2011 Blood Conservation Clinical Practice Guidelines • CV Surgery consumes @ 20 % of nations blood resources ( @ 3 M units red cells used) • Evidence suggests worse short and long term outcomes for transfused patients • Patients need bleeding and transfusion risk assessment starting with accurate assessment and effective treatment for pre-operative anemia ( Hbg < 13, males and females) Kathrine Frey, MD kfrey 2@fairview. org 952412 -2700 40
What I hoped to have you “see” • There is a Need for Pre-Op “Blood Health” check (clearance) for non-emergent patients ( 3 weeks to surgery) • Includes: 1) patient’s red cell mass maximized and 2) patient has ability or plan to make new red cells after blood is lost • Blood Health Preparedness akin to dental exam clearance for valve or PFT need for lobectomy patients- don’t go to surgery without it. Kathrine Frey, MD kfrey 2@fairview. org 952412 -2700 41

• Transfusion no longer an acceptable part of medical care, now considered an UNDESIRABLE EVENT. Kathrine Frey, MD kfrey 2@fairview. org 952412 -2700 42