Medical Nutrition Therapy for Anemia Anemia Definition deficiency
- Slides: 42
Medical Nutrition Therapy for Anemia
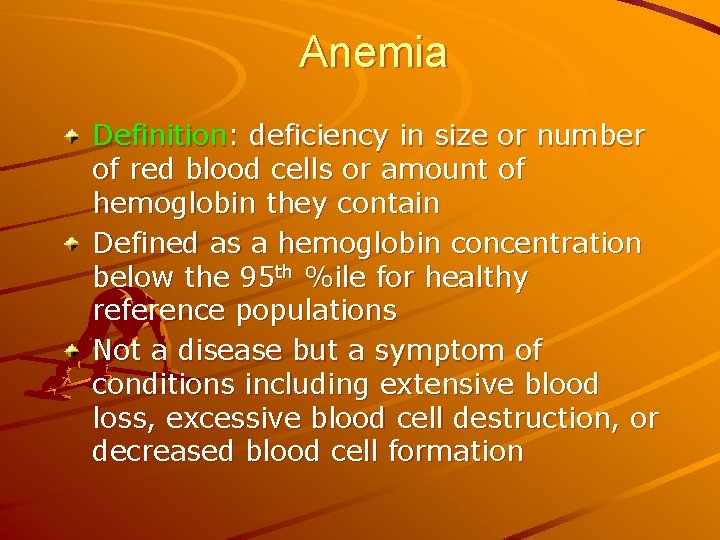
Anemia Definition: deficiency in size or number of red blood cells or amount of hemoglobin they contain Defined as a hemoglobin concentration below the 95 th %ile for healthy reference populations Not a disease but a symptom of conditions including extensive blood loss, excessive blood cell destruction, or decreased blood cell formation
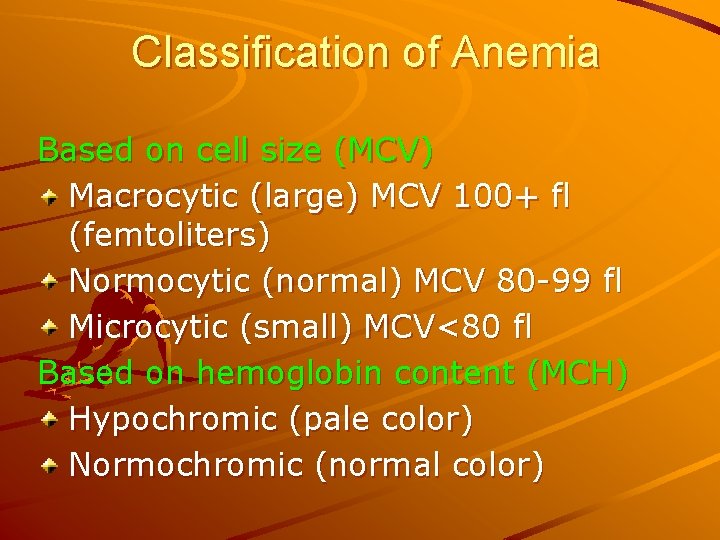
Classification of Anemia Based on cell size (MCV) Macrocytic (large) MCV 100+ fl (femtoliters) Normocytic (normal) MCV 80 -99 fl Microcytic (small) MCV<80 fl Based on hemoglobin content (MCH) Hypochromic (pale color) Normochromic (normal color)
Iron Deficiency Anemia Characterized by the production of small (microcytic) erythrocytes and a diminished level of circulating hemoglobin Last stage of iron deficiency Represents the end point of a long period of iron deprivation
Causes of Iron Deficiency Anemia Inadequate ingestion Inadequate absorption Defects in release from Inadequate utilization Increased blood loss or Increased requirement stores excretion
Stages of Iron Deficiency Stage 1: moderate depletion of iron stores; no dysfunction Stage 2: Severe depletion of iron stores; no dysfunction Stage 3: Iron deficiency Stage 4: Iron deficiency (dysfunction and anemia)
Tests for Iron Deficiency Serum iron: poor indicator, highly variable day to day and during the day Ferritin - most sensitive—chief storage form of iron; directly proportional to iron stored in cells
Tests for Iron Deficiency Zinc protoporphyrin/heme ratio (ZPPH) protoporphyrin binds iron to form heme or zinc to form zinc protoporphyrin In the presence of iron deficiency, ratio will rise (iron deficiency defined as ratio>1: 12, 000) Not affected by hematocrit or other causes of anemia; specific to iron deficiency
Tests for Iron Deficiency • • • Total iron binding capacity (TIBC)— capacity of transferrin to bind iron Transferrin—globulin that binds/transports Fe from gut wall to tissues Percent saturation of transferrin (calculate by dividing serum iron by the TIBC) • • TIBC increases in iron deficiency As stored iron falls, saturation of transferrin decreases
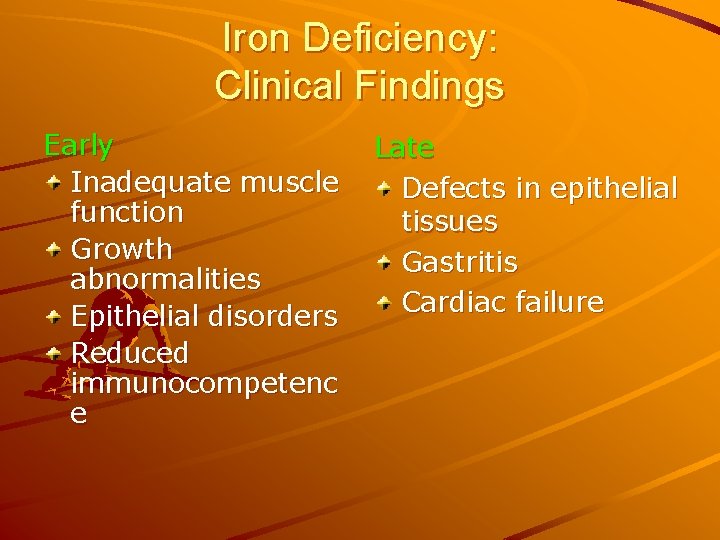
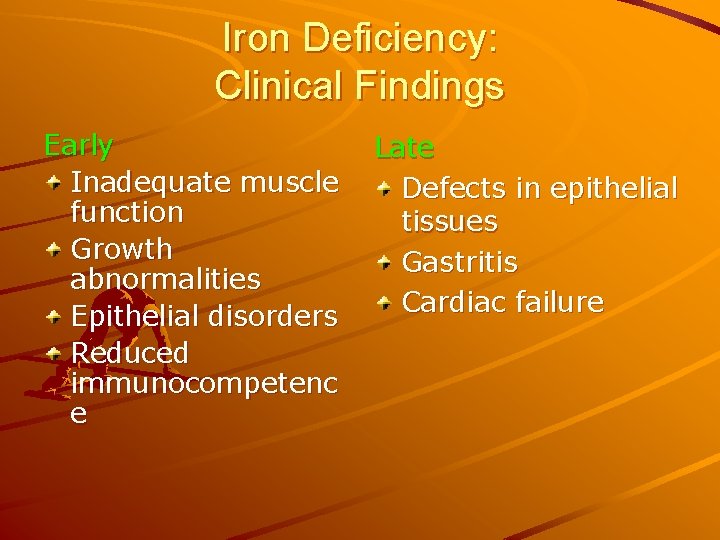
Iron Deficiency: Clinical Findings Early Inadequate muscle function Growth abnormalities Epithelial disorders Reduced immunocompetenc e Late Defects in epithelial tissues Gastritis Cardiac failure
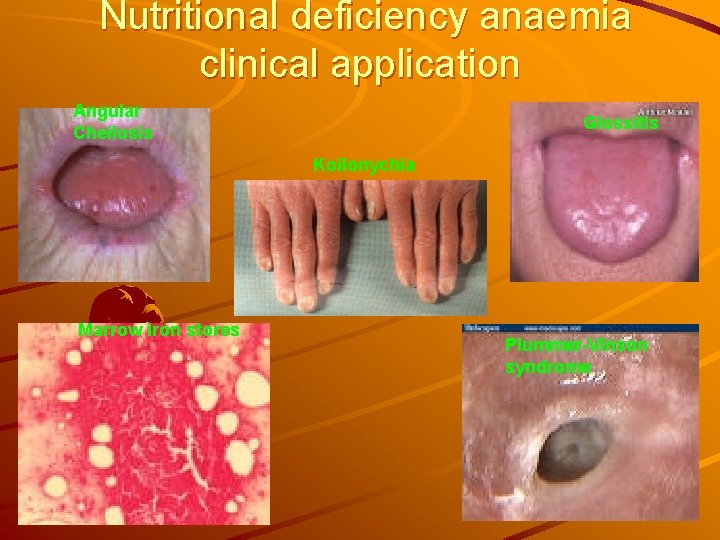
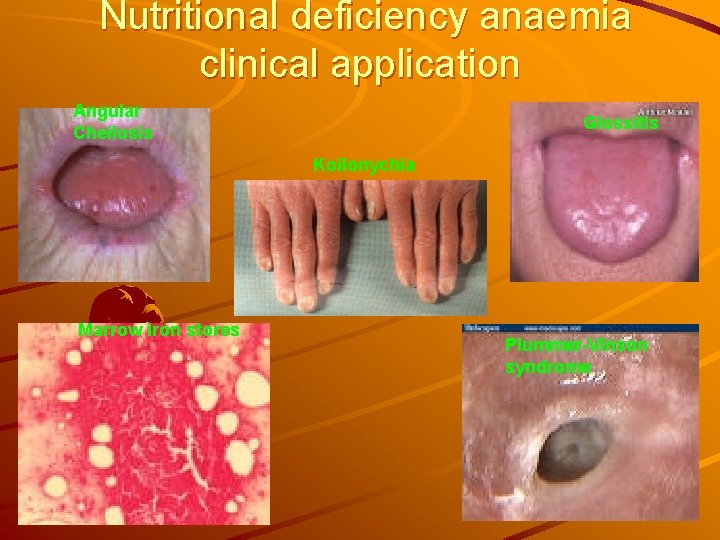
Nutritional deficiency anaemia clinical application Angular Cheilosis Glossitis Koilonychia Marrow iron stores Plummer-Vinson syndrome
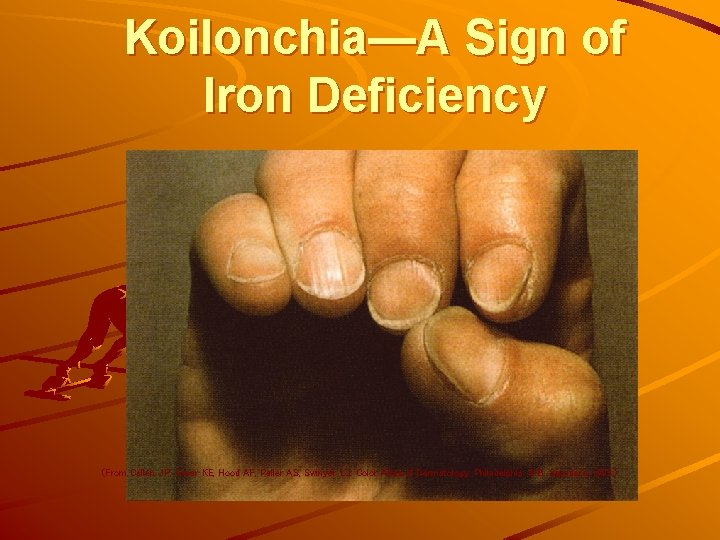
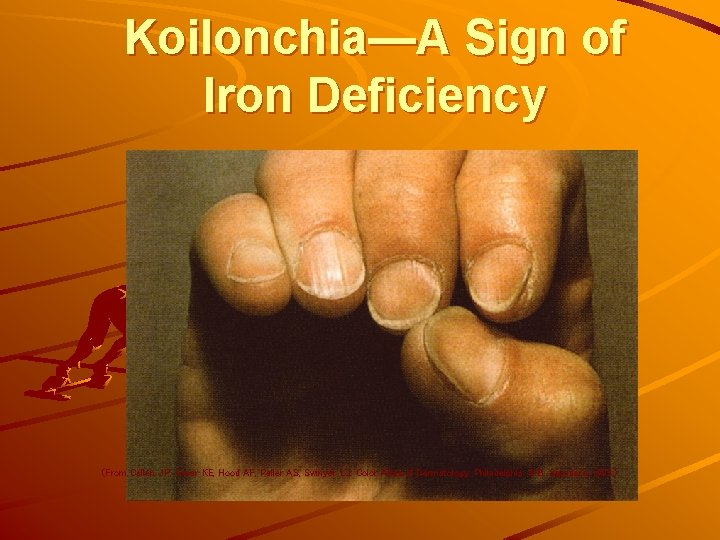
Koilonchia—A Sign of Iron Deficiency (From Callen JP, Greer KE, Hood AF, Paller AS, Swinyer LJ. Color Atlas of Dermatology. Philadelphia: W. B. Saunders, 1993. )
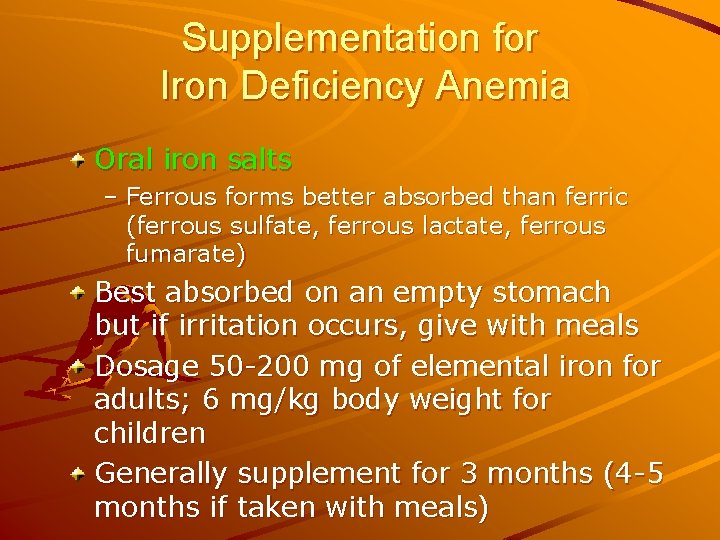
Supplementation for Iron Deficiency Anemia Oral iron salts – Ferrous forms better absorbed than ferric (ferrous sulfate, ferrous lactate, ferrous fumarate) Best absorbed on an empty stomach but if irritation occurs, give with meals Dosage 50 -200 mg of elemental iron for adults; 6 mg/kg body weight for children Generally supplement for 3 months (4 -5 months if taken with meals)
Nutritional Management of Iron. Deficiency Anemia Increase absorbable iron in the diet Include vitamin C at every meal Include meat, fish or poultry at every meal Decrease tea and coffee consumption
Restoring Iron Levels Factors to consider: Bioavailability of iron—the lower the Fe stores, the greater the rate of absorption Vitamin C—binds iron to form a readily absorbed complex Heme sources (meat, poultry, fish)— about 15% absorbable Nonheme iron (grains, vegetables, eggs)—about 3% to 8% absorbable
Supplementation for Iron Deficiency Anemia If patient fails to respond May not be taking supplements May not be absorbing iron (celiac disease, steatorrhea, hemodialysis) May be bleeding May need IV iron dextran (can cause allergic reactions)
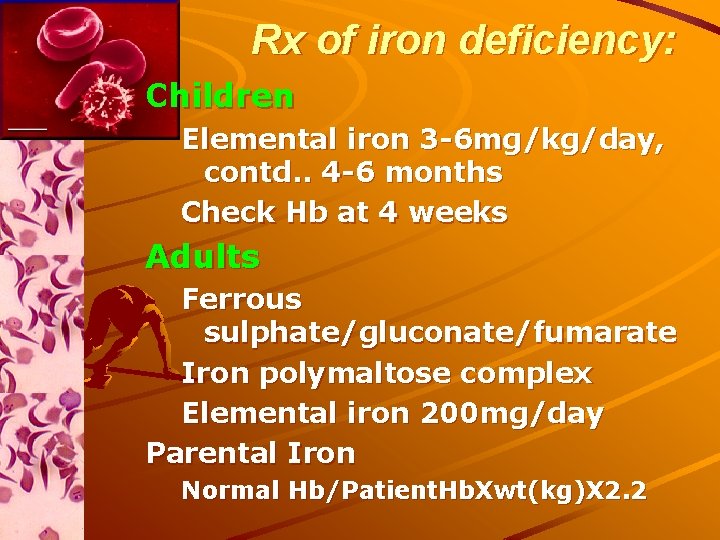
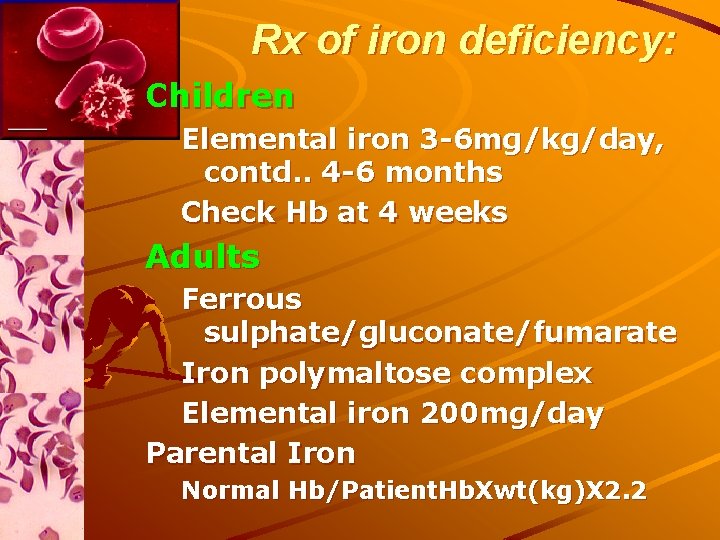
Rx of iron deficiency: Children Elemental iron 3 -6 mg/kg/day, contd. . 4 -6 months Check Hb at 4 weeks Adults Ferrous sulphate/gluconate/fumarate Iron polymaltose complex Elemental iron 200 mg/day Parental Iron Normal Hb/Patient. Hb. Xwt(kg)X 2. 2
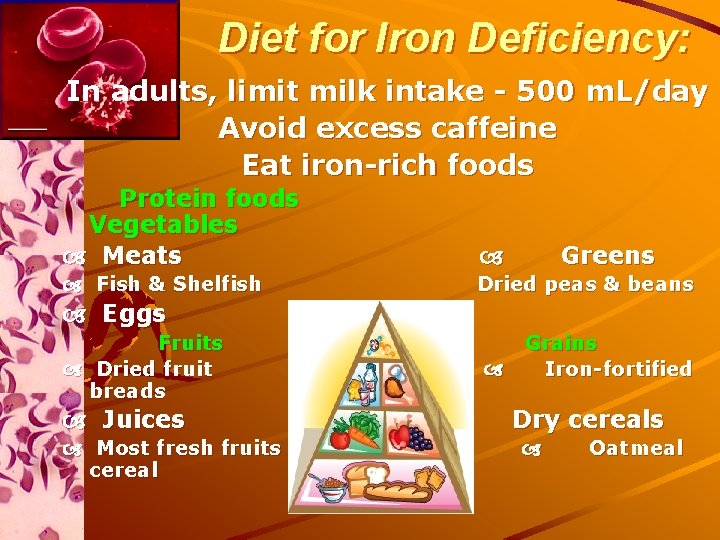
Diet for Iron Deficiency: In adults, limit milk intake - 500 m. L/day Avoid excess caffeine Eat iron-rich foods Protein foods Vegetables Meats Fish & Shelfish Dried peas & beans Greens Eggs Fruits Dried fruit breads Juices Most fresh fruits cereal Grains Iron-fortified Dry cereals Oatmeal
Disorders Associated with Iron Toxicity Thalassemias Sideroblastic anemias Chronic hemolytic anemia Aplastic anemia Ineffective erythropoiesis Transfusional iron overload Alcoholic cirrhosis
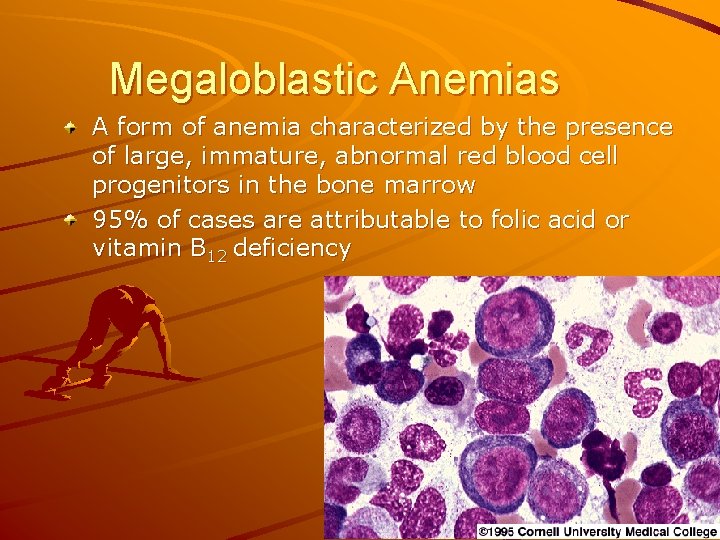
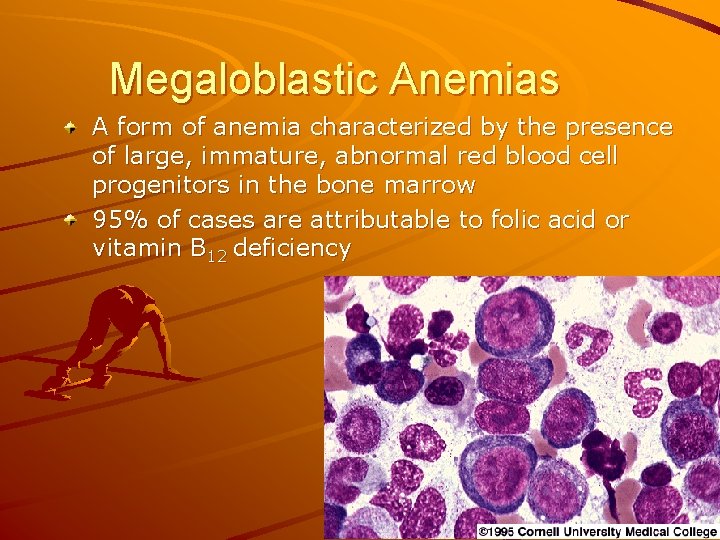
Megaloblastic Anemias A form of anemia characterized by the presence of large, immature, abnormal red blood cell progenitors in the bone marrow 95% of cases are attributable to folic acid or vitamin B 12 deficiency
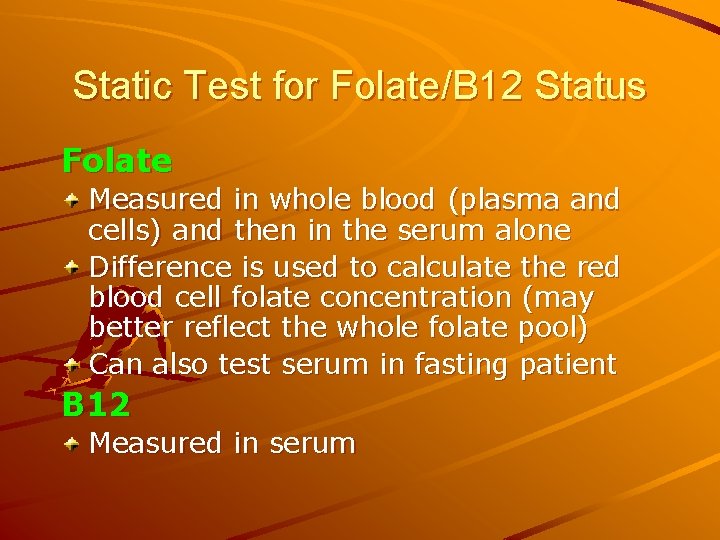
Static Test for Folate/B 12 Status Folate Measured in whole blood (plasma and cells) and then in the serum alone Difference is used to calculate the red blood cell folate concentration (may better reflect the whole folate pool) Can also test serum in fasting patient B 12 Measured in serum
Functional Tests for Macrocytic Anemias Homocysteine: Folate and B 12 are needed to convert homocysteine to methionine; high homocysteine may mean deficiencies of folate, B 12 or B 6 Methylmalonic acid measurements can be used along with homocysteine to distinguish between B 12 and folate deficiencies Schilling test: radiolabeled cobalamin is used to test for B 12 malabsorption
Pernicious Anemia A macrocytic, megaloblastic anemia caused by a deficiency of vitamin B 12. Usually secondary to lack of intrinsic factor (IF) May be caused by strict vegan diet Also can be caused by ↓gastric acid secretion, gastric atrophy, H-pylori, gastrectomy, disorders of the small intestine (celiac disease, regional enteritis, resections), drugs that inhibit B 12 absorption including neomycin, alcohol, colchicine, metformin, pancreatic disease
Symptoms of Pernicious Anemia Paresthesia (especially numbness and tingling in hands and feet) Poor muscular coordination Impaired memory and hallucinations Damage can be permanent
Vitamin B 12 Depletion Stage I—early negative vitamin B 12 balance Stage II—vitamin B 12 depletion Stage III—damaged metabolism: vitamin B 12 deficient erythropoiesis Stage IV—clinical damage including vitamin B 12 anemia Pernicious anemia—numbness in hands and feet; poor muscular coordination; poor memory; hallucinations
Causes of Vitamin B 12 Deficiency Inadequate ingestion Inadequate absorption Inadequate utilization Increased requirement Increased excretion Increased destruction by antioxidants
Treatment of B 12 Deficiency Before 1926 was incurable; until 1948 was treated with liver extract Now treatment consists of injection of 100 mcg of vitamin B 12 once per week until resolved, then as often as necessary Also can use very large oral doses or nasal gel MNT: high protein diet (1. 5 g/kg) with meat, liver, eggs, milk products, green leafy vegetables
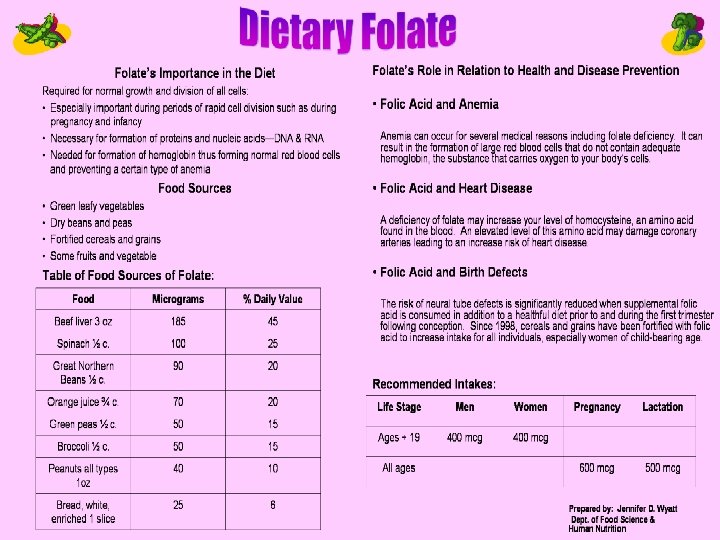
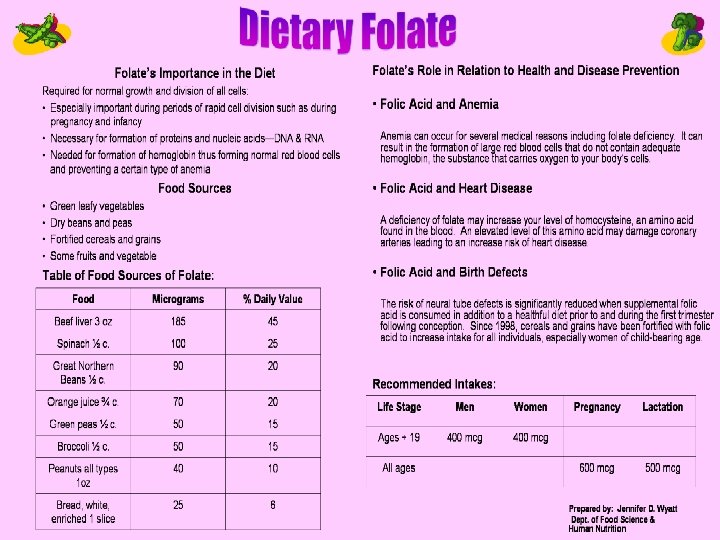
Folic Acid Deficiency Tropical sprue; pregnancy; infants born to deficient mothers Alcoholics People taking medications chronically that affect folic acid absorption Malabsorption syndromes
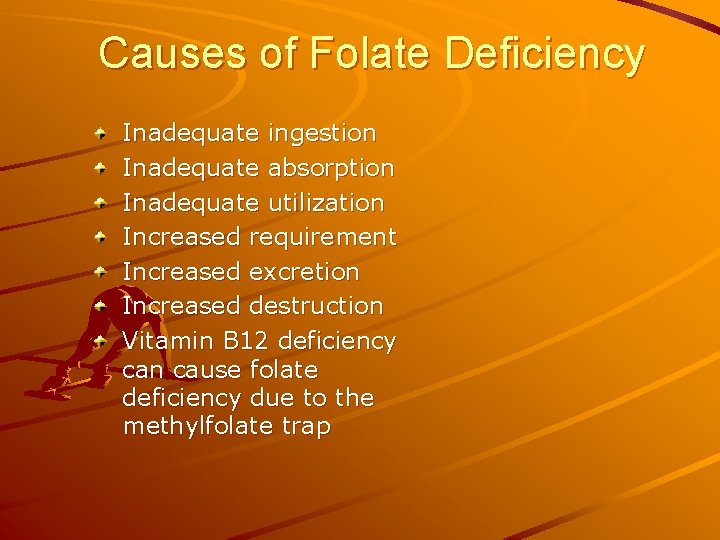
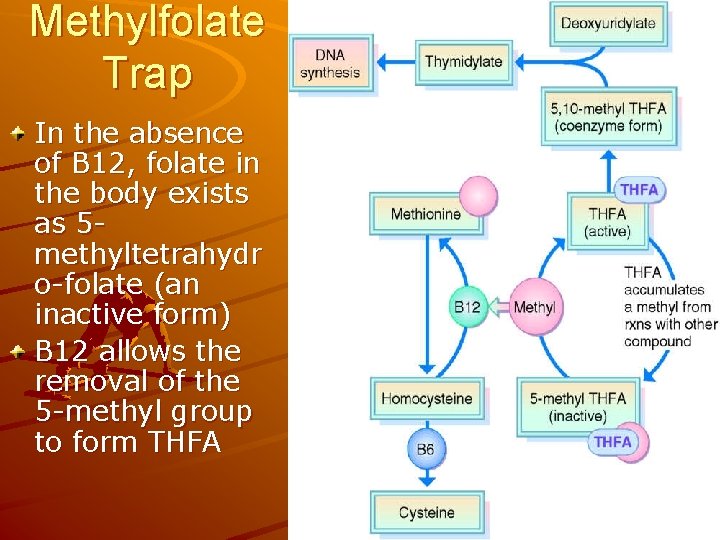
Causes of Folate Deficiency Inadequate ingestion Inadequate absorption Inadequate utilization Increased requirement Increased excretion Increased destruction Vitamin B 12 deficiency can cause folate deficiency due to the methylfolate trap
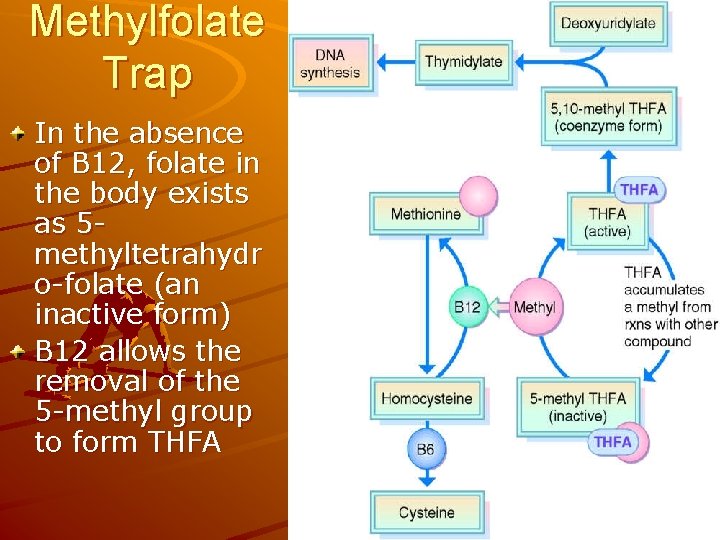
Methylfolate Trap In the absence of B 12, folate in the body exists as 5 methyltetrahydr o-folate (an inactive form) B 12 allows the removal of the 5 -methyl group to form THFA
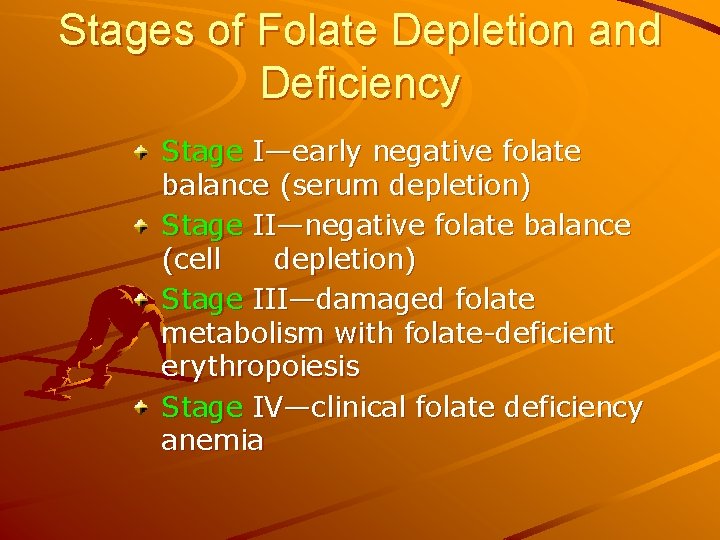
Stages of Folate Depletion and Deficiency Stage I—early negative folate balance (serum depletion) Stage II—negative folate balance (cell depletion) Stage III—damaged folate metabolism with folate-deficient erythropoiesis Stage IV—clinical folate deficiency anemia
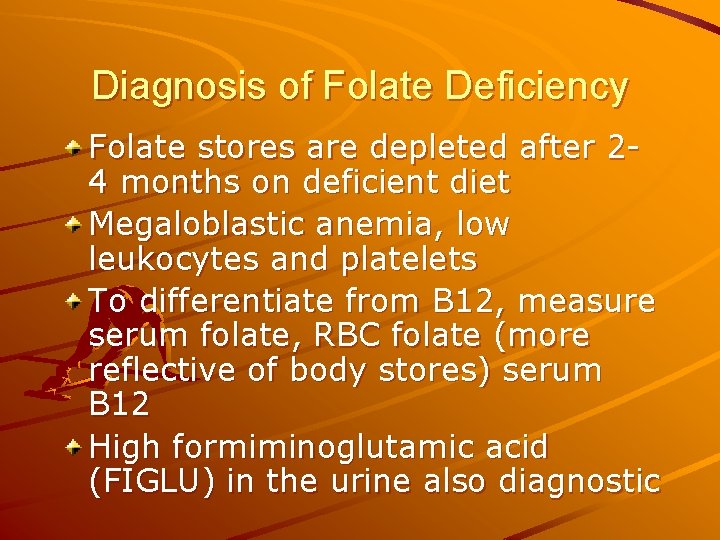
Diagnosis of Folate Deficiency Folate stores are depleted after 24 months on deficient diet Megaloblastic anemia, low leukocytes and platelets To differentiate from B 12, measure serum folate, RBC folate (more reflective of body stores) serum B 12 High formiminoglutamic acid (FIGLU) in the urine also diagnostic
Other Nutritional Anemias Copper deficiency anemia Anemia of protein-energy malnutrition Sideroblastic (pyridoxine-responsive) anemia Vitamin E–responsive (hemolytic) anemia
Copper Deficiency Copper is required for mobilization of iron from storage sites In copper deficient state, result is low serum iron and hemoglobin, even when iron stores are normal Copper is widespread in foods and needed in tiny amounts Sometimes occurs in infants fed deficient formula or cow’s milk, adults and children with malabsorption or on TPN without copper Diagnosis is important, since more iron won’t help and may interfere with copper absorption
Sideroblastic Anemia Microcytic, hypochromic form Inherited defect of heme synthesis enzyme High serum and tissue iron levels Buildup of immature sideroblasts— hence the name B 6 is essential—must replace 25 to 100 times the RDA; may need lifelong replacement Pyridoxine-responsive anemia, distinguished from anemia caused by pyridoxine deficiency
Hemolytic Anemia Oxidative damage to cells—lysis occurs Vitamin E is an antioxidant that seems to be protective. This anemia can occur in newborns, especially preemies.
Non-nutritional Anemias Sports anemia (hypochromic microcytic transient anemia) Anemia of pregnancy: dilutional Anemia of inflammation, infection, or malignancy (anemia of chronic disease) Sickle cell anemia Thalassemias
Sports Anemia Transient—usually in athletes who are runners; from compression of RBCs in feet until they burst, releasing hemoglobin Check lab values Counsel about a proper diet
Sickle Cell Anemia Protein-energy malnutrition common; may have poor intake and increased energy needs Be careful not to overdo iron in diet or supplements; iron stores are often high due to frequent transfusions; avoid iron rich foods, alcohol, and ascorbic acid which enhance iron absorption Promote foods high in copper, zinc and folate as needs are increased due to constant replacement of erythrocytes Zinc supplements may be useful
Thalassemia Severe inherited anemia affecting mostly people of Mediterranean extraction Defective globin formation in hemoglobin leads to increased blood volume, splenomegaly, bone marrow expansion, facial deformities, osteomalacia, bone changes Iron buildup due to transfusions requires chelation therapy to remove excess iron
Medical and Nutritional Management of Anemia It is important to be familiar with the etiology and treatment of nutritional and non-nutritional anemias Many non-nutritional anemias have nutritional implications It is critical to DIAGNOSE before treating anemias with nutritional or non-nutritional therapies
 Medical nutrition therapy for stroke
Medical nutrition therapy for stroke Medical nutrition therapy for hypertension
Medical nutrition therapy for hypertension Small bowel obstruction medical nutrition therapy
Small bowel obstruction medical nutrition therapy Minerals are inorganic elements that the body
Minerals are inorganic elements that the body Anemiam
Anemiam What is severe iron deficiency
What is severe iron deficiency Low iron symptoms
Low iron symptoms Iron deficiency anemia smear
Iron deficiency anemia smear Retikulocyte
Retikulocyte Pernicious anemia symptoms
Pernicious anemia symptoms Serum ferritin in iron deficiency anemia
Serum ferritin in iron deficiency anemia Symptoms of anemia in pregnancy
Symptoms of anemia in pregnancy Dietary iron
Dietary iron Indication of anemia
Indication of anemia Crew cut x ray
Crew cut x ray Losmosis
Losmosis Nutrition deficiency
Nutrition deficiency Nutrition deficiency
Nutrition deficiency Koilonchia
Koilonchia Nutrition deficiency
Nutrition deficiency Megaloblastic anemia vs pernicious anemia
Megaloblastic anemia vs pernicious anemia Macrocytic anemia causes
Macrocytic anemia causes Pseudocholinesterase deficiency
Pseudocholinesterase deficiency Nutrition and diet therapy nursing
Nutrition and diet therapy nursing Both psychoanalysis and humanistic therapy stress
Both psychoanalysis and humanistic therapy stress Bioness integrated therapy system price
Bioness integrated therapy system price What are the major humanistic therapies
What are the major humanistic therapies Medical family therapy
Medical family therapy Iso 22301 utbildning
Iso 22301 utbildning Typiska novell drag
Typiska novell drag Nationell inriktning för artificiell intelligens
Nationell inriktning för artificiell intelligens Ekologiskt fotavtryck
Ekologiskt fotavtryck Varför kallas perioden 1918-1939 för mellankrigstiden?
Varför kallas perioden 1918-1939 för mellankrigstiden? En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Adressändring ideell förening
Adressändring ideell förening Tidbok för yrkesförare
Tidbok för yrkesförare Anatomi organ reproduksi
Anatomi organ reproduksi Densitet vatten
Densitet vatten Datorkunskap för nybörjare
Datorkunskap för nybörjare Boverket ka
Boverket ka Hur skriver man en tes
Hur skriver man en tes Autokratiskt ledarskap
Autokratiskt ledarskap Nyckelkompetenser för livslångt lärande
Nyckelkompetenser för livslångt lärande