WHE 2008 Anemia When Iron Deficiency is the





- Slides: 55

WHE 2008 Anemia (When Iron Deficiency is the Cause) By: Dr. ABDULLAH T. AL-MOHAMADI DEMONESTRATOR King Abdulaziz University Hospital Jeddah, K. S. A.
WHE 2008 Today’s Agenda ● Definition of Anemia ● Magnitude of the problem and its impact ● Prevalence ● Functions of iron ● Normal iron cycle ● Causes of iron deficiency anemia ● Factors that modify iron absorption ● Symptoms ● Signs ● Stages of iron deficiency ● Diagnosis ● Prevention ● Treatment failure ● Recommendations
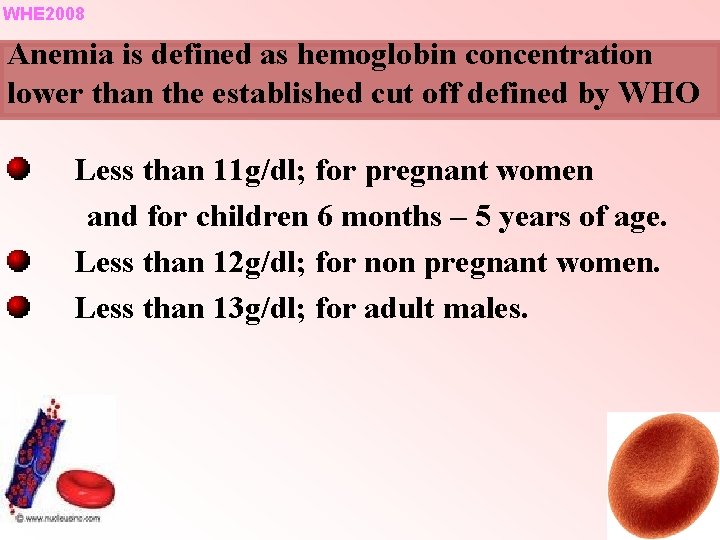
WHE 2008 Anemia is defined as hemoglobin concentration lower than the established cut off defined by WHO Less than 11 g/dl; for pregnant women and for children 6 months – 5 years of age. Less than 12 g/dl; for non pregnant women. Less than 13 g/dl; for adult males.
WHE 2008 Most Common Nutritional Disorder in the World Has negative effects on work capacity and physical labor. Diminishes motor, mental and growth development in infants and children. Might cause low birth weight and preterm delivery or even maternal and fetal death *Haas and Brownlie, 2001*
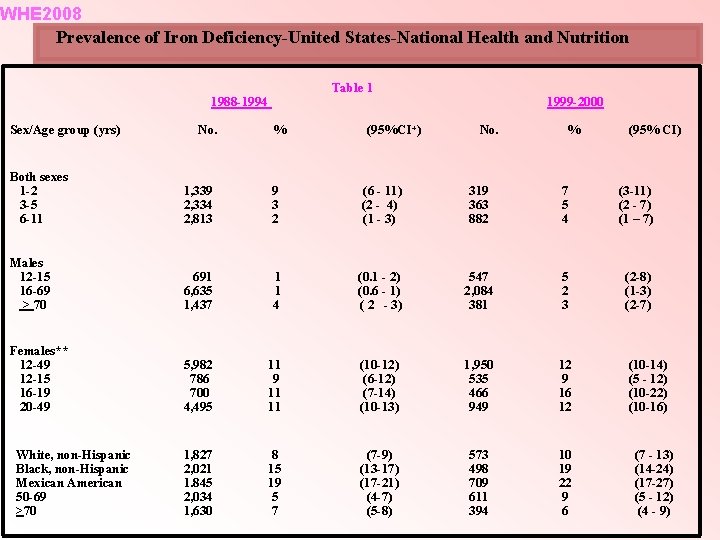
WHE 2008 Magnitude of the Problem It is common in developing countries. Prevalence was observed in the United States among certain population such as toddlers and females of childbearing age. (●) (Table -1 -) Iron deficiency anemia has a prevalence of 2 -5% among adult men and post-menopausal women in the developed word. * (●) looker et al, Prevalence of iron deficiency in the United States. JAMA, 1997. (*) WHO. Iron deficiency anemia. Assessment, prevention and control. A Guide for Program Managers Geneva. 2001.
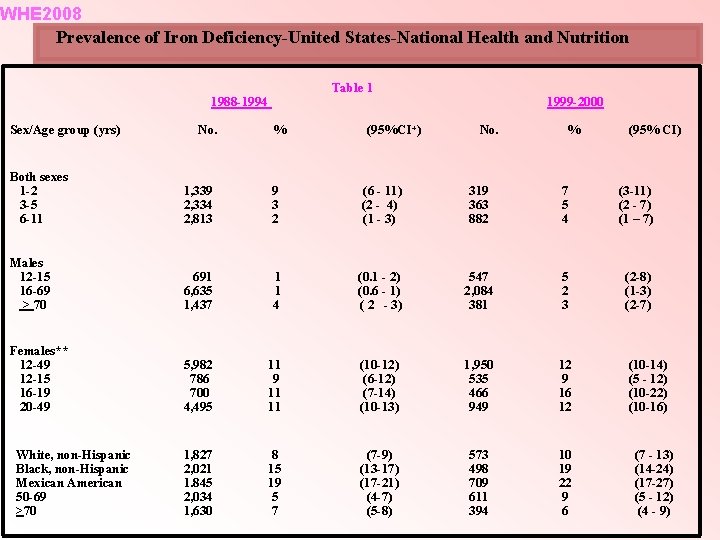
WHE 2008 Prevalence of Iron Deficiency-United States-National Health and Nutrition Table 1 1988 -1994 Sex/Age group (yrs) No. % (95%CI+) 1999 -2000 No. % (95% CI) Both sexes 1 -2 3 -5 6 -11 1, 339 2, 334 2, 813 9 3 2 (6 - 11) (2 - 4) (1 - 3) 319 363 882 7 5 4 (3 -11) (2 - 7) (1 – 7) Males 12 -15 16 -69 > 70 691 6, 635 1, 437 1 1 4 (0. 1 - 2) (0. 6 - 1) ( 2 - 3) 547 2, 084 381 5 2 3 (2 -8) (1 -3) (2 -7) Females** 12 -49 12 -15 16 -19 20 -49 5, 982 786 700 4, 495 11 9 11 11 (10 -12) (6 -12) (7 -14) (10 -13) 1, 950 535 466 949 12 9 16 12 (10 -14) (5 - 12) (10 -22) (10 -16) 1, 827 2, 021 1. 845 2, 034 1, 630 8 15 19 5 7 (7 -9) (13 -17) (17 -21) (4 -7) (5 -8) 573 498 709 611 394 10 19 22 9 6 White, non-Hispanic Black, non-Hispanic Mexican American 50 -69 >70 (7 - 13) (14 -24) (17 -27) (5 - 12) (4 - 9)
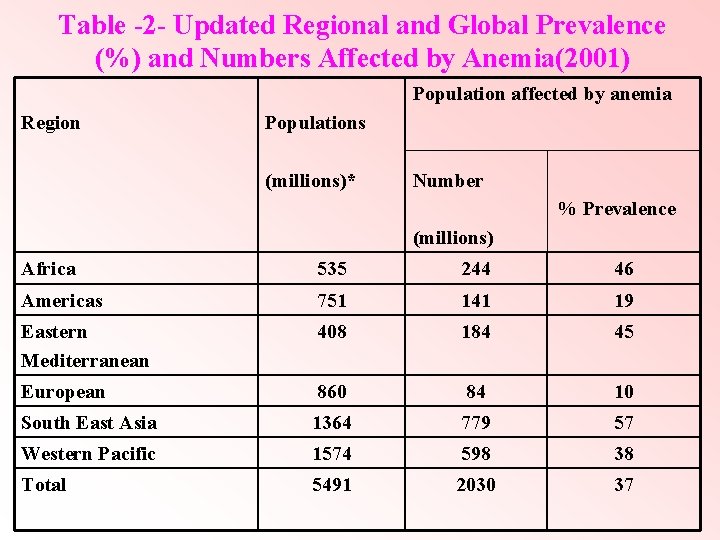
WHE 2008 World Health Organization (WHO) Estimates that most preschool children and pregnant women in developing countries are iron deficient. * (Table 2) (*) WHO report, Iron deficiency anemia. Assessment, Prevention and Control. A Guide for Program Managers. Geneva. 2001.
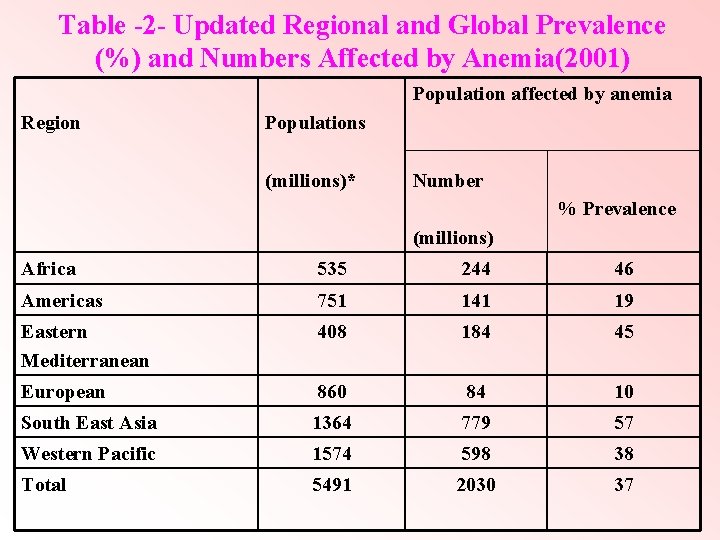
Table -2 - Updated Regional and Global Prevalence (%) and Numbers Affected by Anemia(2001) Population affected by anemia Region Populations (millions)* Number % Prevalence (millions) Africa 535 244 46 Americas 751 141 19 Eastern Mediterranean 408 184 45 European 860 84 10 South East Asia 1364 779 57 Western Pacific 1574 598 38 Total 5491 2030 37
WHE 2008 Magnitude of the Problem: cont. The prevalence of anemia in developing countries is three to four times higher than that for developed countries. Prevalence of anemia in the Gulf region ranged from 15 -48% in women childbearing age mostly attributed to iron deficiency(●)
WHE 2008 Magnitude of the Problem: cont. In Saudi Arabia the overall country prevalence of anemia was 30 -56%(●) Cross sectional study, conducted in Riyadh among school girls showed that IDA prevalence was 40. 5% among female adolescents (16 -18) years old. * Verster A, Pols J. Anemia in Mediterranean region “ 1995” (*) Al-Shehris. Health Profile of Saudi adoloscent Schoolgirls. “ 1996 “ (*) Joharah, M. Al-Quaiz. Iron deficiency anemia. A study of Risk factors. Saudi Med J 2001. (●)
WHE 2008 WHO/UNICEF jointly adopted nutritional goals, aiming to control iron deficiency by the turn of the century. (●) WHO, UNICEF, INACG. Guidelines for use of iron supplements to prevent and treat iron deficiency anemia, 1998
WHE 2008 Recent report from WHO indicates that the prevalence of anemia has not changed much over the years, (It is a persisting public health problem).
WHE 2008 Iron and Functions Iron, is one of the most common elements constituting about 5% of the earth crust. Essential for all living organisms. It has several vital functions in the body.
WHE 2008 Iron and Functions: cont. Storage and carrier of oxygen to tissue by red blood cell hemoglobin or to muscles by myoglobin Some important enzymes contain iron like that catalyze the redox reaction required for the generation of energy eg. Cytochrome.
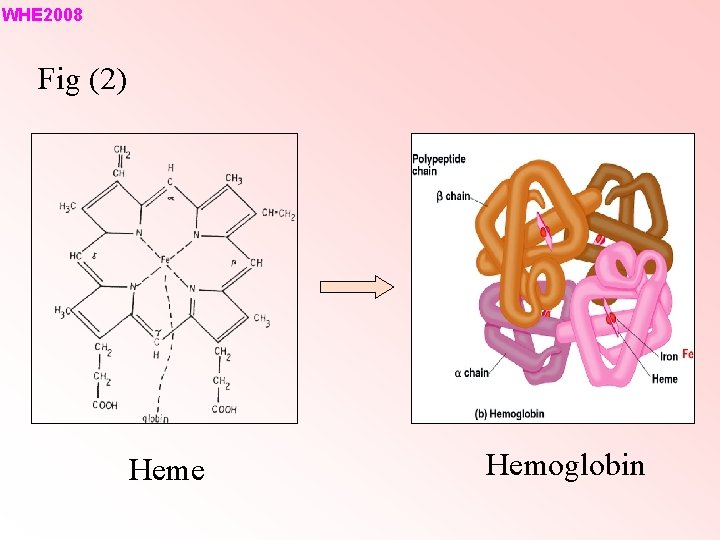
WHE 2008 Fig (2) Heme Hemoglobin
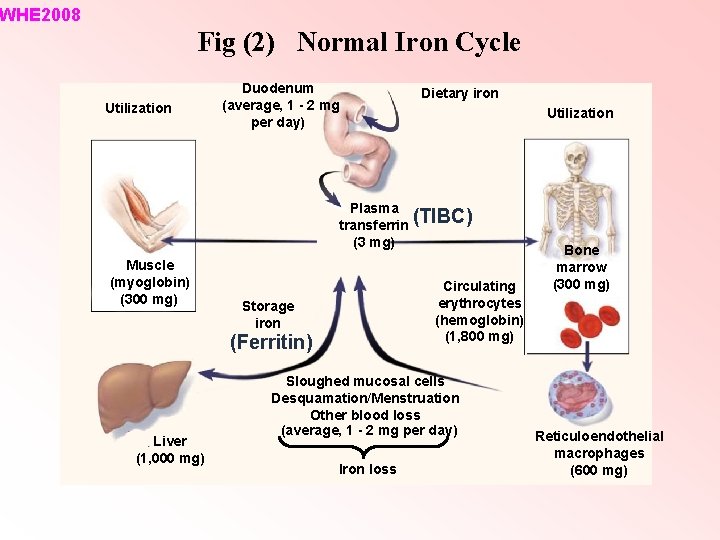
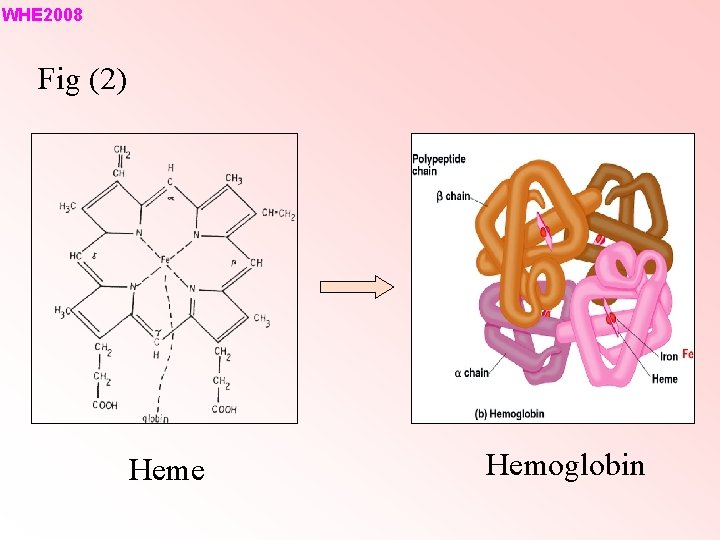
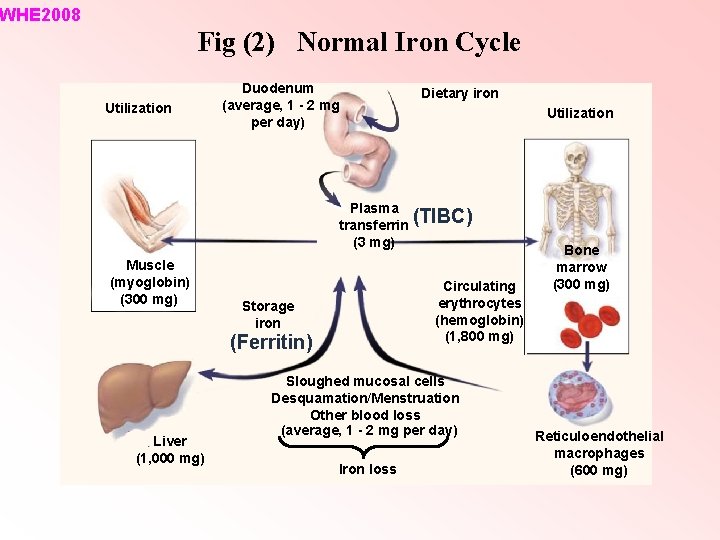
WHE 2008 Fig (2) Normal Iron Cycle Utilization Duodenum (average, 1 - 2 mg per day) Dietary iron Utilization Plasma (TIBC) transferrin (3 mg) Muscle (myoglobin) (300 mg) Circulating erythrocytes (hemoglobin) (1, 800 mg) Storage iron (Ferritin) Liver (1, 000 mg) Sloughed mucosal cells Desquamation/Menstruation Other blood loss (average, 1 - 2 mg per day) Iron loss Bone marrow (300 mg) Reticuloendothelial macrophages (600 mg)
WHE 2008 Causes of Iron Deficiency Anemia ü Blood loss Menorrhagia is one of the most frequent causes of iron deficiency and should always be suspected as the cause in women during reproductive life. (*)Query Specific points in the menstrual history (*) The use of intra-uterine devices (IUCD).
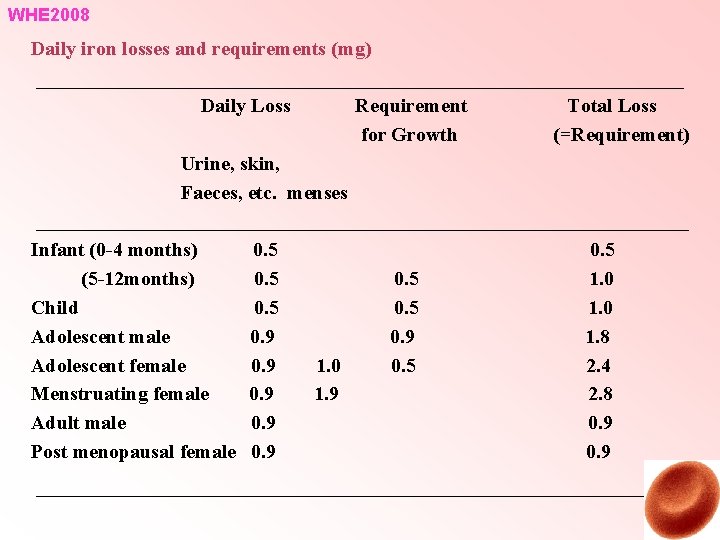
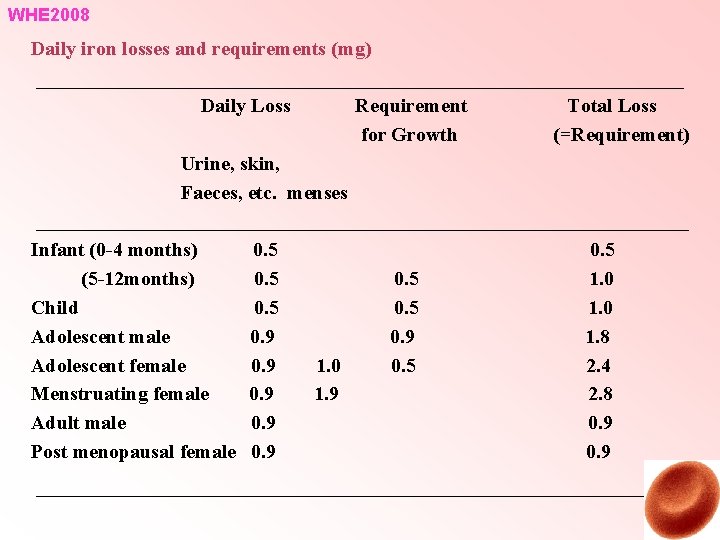
WHE 2008 Daily iron losses and requirements (mg) Daily Loss Requirement for Growth Total Loss (=Requirement) Urine, skin, Faeces, etc. menses Infant (0 -4 months) (5 -12 months) Child Adolescent male Adolescent female Menstruating female Adult male Post menopausal female 0. 5 0. 9 0. 9 1. 0 1. 9 0. 5 0. 9 0. 5 1. 0 1. 8 2. 4 2. 8 0. 9
WHE 2008 Causes of iron deficiency anemia: cont ü Losses can increase with colorectal cancer, polyps, diverticular disease, excessive use of certain medication, Hook worm infestation and frequent blood donation. (●) Common cause of referral to gastroenterologist. (●) Blood loss from the (GI) tract is the commonest cause of iron deficiency anemia in adult men and post-menopausal women ü Most common cause of Iron Deficiency Anemia, in America and North America
WHE 2008 Causes of Iron Deficiency Anemia : cont ü high physiological requirement such as in infancy, early childhood, puberty and Pregnancy: Blood in the body expands until it is about 50% or more Most women start pregnancy without sufficient iron store Increase demand for iron particularly in the second and third trimesters
WHE 2008 Pregnancy: cont. ● Higher risk with morning sickness ● Two or more pregnancies close together ● Pregnancy with more than one baby ● Iron poor diet or if prior pregnancy menstrual flow was heavy.
WHE 2008 Causes of Iron Deficiency Anemia cont ■ Diet ● Rarely is the sole cause of iron deficiency. ● Vegetarians are more likely to develop iron deficiency anemia. ● Various food can influence the absorption of dietary iron. Vit. C can increase the absorbtion of iron. Tea, coffee and cocoa drinking especially with food reduce the absorbtion of dietary iron.
WHE 2008 Causes of Iron Deficiency Anemia: cont. ● * Calcium intake can inhibit iron absorption. A cross sectional study among girls and young women in 6 European countries showed that dietary calcium intake had a consistent inverse association with iron store. * Van de Vijver Lp. L et al. Calcium intake is weakly but consistently negatively associated with iron status in girls and women in six Eusropean countries. J Nut 1999.
WHE 2008 Causes of Iron Deficiency Anemia: cont. Malabsorbtion ■ Hypo-or achlorohydria, H. Pylori colonisation ■ Coeliac disease ■ Gastrectomy, Gut resection and Gastric bypass surgeries and others.
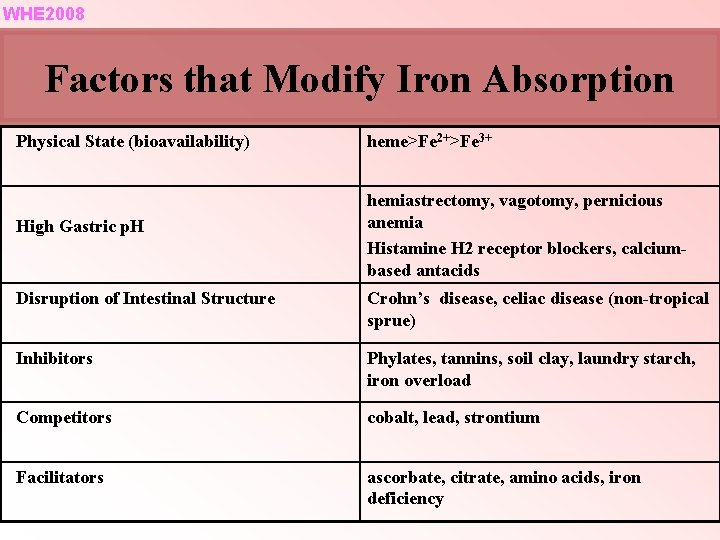
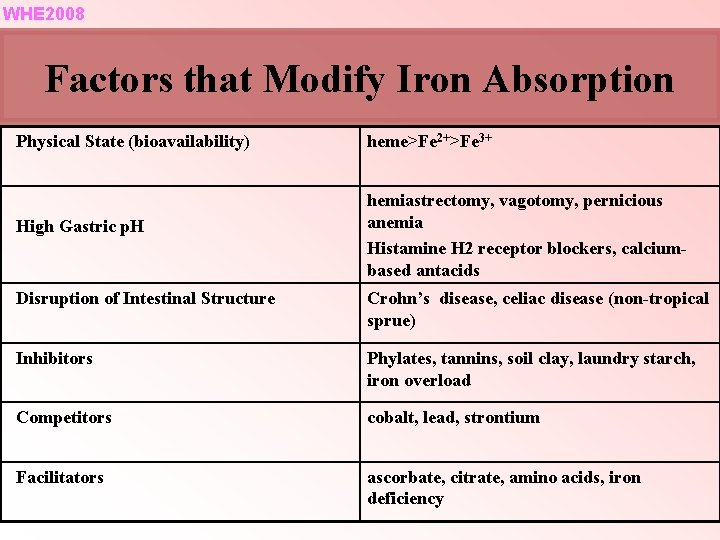
WHE 2008 Factors that Modify Iron Absorption Physical State (bioavailability) heme>Fe 2+>Fe 3+ High Gastric p. H hemiastrectomy, vagotomy, pernicious anemia Histamine H 2 receptor blockers, calciumbased antacids Disruption of Intestinal Structure Crohn’s disease, celiac disease (non-tropical sprue) Inhibitors Phylates, tannins, soil clay, laundry starch, iron overload Competitors cobalt, lead, strontium Facilitators ascorbate, citrate, amino acids, iron deficiency
WHE 2008 ● Iron deficiency develops after gastric bypass for several reasons: (●) Intolerance for red meat (●) Diminished gastric acid secretion (●) Exclusion of the duodenum from the alimentary tract
WHE 2008 ■ In a case control study of risk factors for IDA among Saudi women of childbearing age (87 patients and 203 controls) ● Poor dietary habits ● Menorrhagia ● History of ingestion of NSAID or antacids were the most important risk factors. J M. Al—Quaiz-Iron deficiency anemia, A Study of risk factors Saudi Med J. 2001
WHE 2008 Symptoms ■ ■ Seldom appear before Hb <10 g/dl. Tiredness, palpitation, lack of stamina, shortness of breath, dizziness, headache, irritability, depression and excessive hair loss. ■ soreness and burning of the tongue and a sensation that the tongue feels swollen. ■ Vertigo, tinnitus, tendency to faint, anginal pain, gastrointestinal discomfort, loss of appetite or perversion of the appetite (pica)
WHE 2008 Cont. Pica ● Occurs variably in patients with iron deficiency ● Precise pathophysiology of the syndrome is unknown ● Patients consume unusual items eg. laundry starch, ice, soil clay ● Clay and starch can bind iron in the GIT, exacerbating the deficiency.
WHE 2008 Physical Examination ■ ■ Pallor Dryness or roughness of the skin, or it may be more transparent and thinner than normal. ■ Brittle, soft and flattened or spoon shaped koilonychia ■ Lips are often dry and cracked and the surface may become uneven. ■ Painful, moist cracks at the angles of the mouth occurs in about 15%.

WHE 2008 Cont. ■ ■ 50% of patients suffer smooth, glossy, reddening of the tongue vesicles or erosions develop. The hair may be brittle, splitting at the ends with marked thinning. Cold intolerance develops in one fifth of patients 5 – 20% of patients with long standing iron deficiency anemia develop dysphagia.

WHE 2008 Stages of Iron Deficiency ● prelatent iron deficiency occurs when stores are depleted without a change in hematocrit or serum iron levels. This stage of iron deficiency is rarely detected. ● latent iron deficiency occurs when the serum iron drops and the TIBC increases without a change in the hematocrit. This stage is occasionally detected by a routine check of the transferrin saturation. ● frank iron deficiency anemia is associated with erythrocyte microcytosis and hypochromia. Iron deficiency attracts medical attention most commonly at this stage.
WHE 2008 Diagnosis of Iron Deficiency very vague ■ symptoms such as fatigue and tiredness may be attributed to overwork or disregarded completely. ● Complete blood count~Hb level * documents severity of microcytic hypochromic indices ( MCV, MCHC) and red cell distribution width. ● Platelets may be normal. Increased or reduced in rare cases. ● The WBC count is usually within reference range.
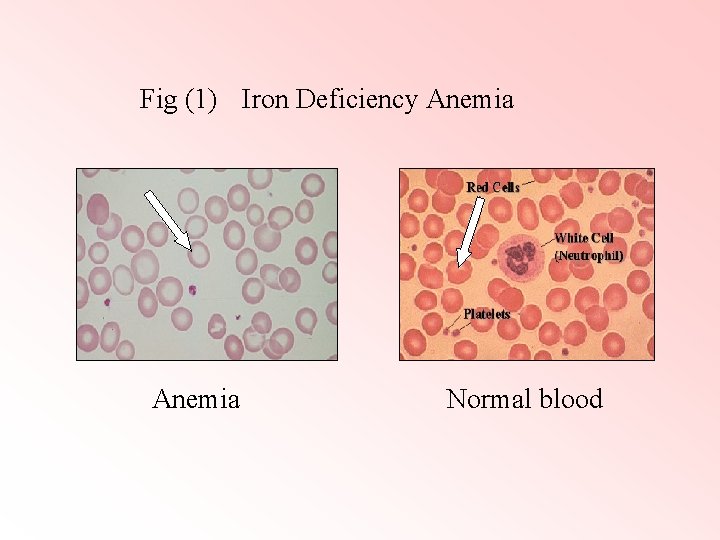
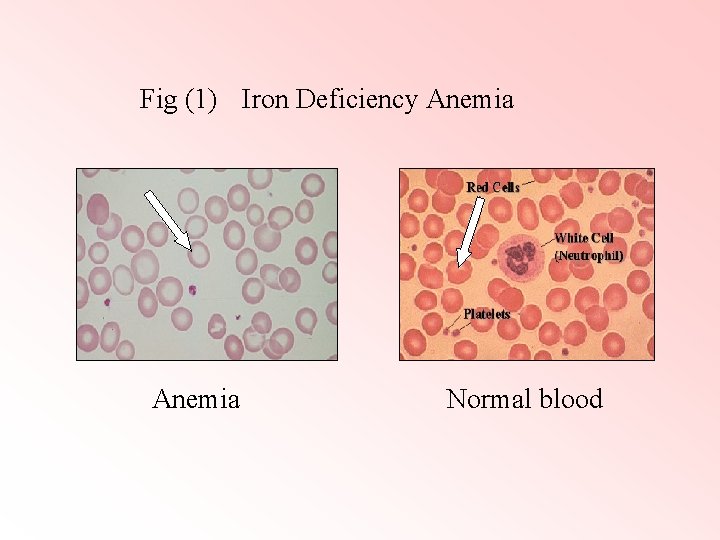
Fig (1) Iron Deficiency Anemia Normal blood
WHE 2008 Diagnosis of Iron Deficiency: cont. ● Assessment of body iron profile (serum iron, total iron-binding capacity (TIBC) and ferritin) low SF is diagnostic of iron deficiency. ● The serum transferrin receptor assay is a relatively new approach to measuring iron status at the cellular level.

WHE 2008 Cont. ü Search for the underlying cause. Upper and lower GI investigations should be considered in all post-menopausal female and all male patients , unless there is a history of significant overt non-GI blood loss (Grade B evidence). Celiac disease serology if positive, should be confirmed by small bowel biopsy. (●) BSG Guidelines in Gastroentrology for the Management of iron deficiency anemia, May 2005.
WHE 2008 Prevention of Iron Deficiency Evidence are accumulating , strongly suggest a relationship between iron deficiency and brain development. IQ of school children and attention deficit disorder. Functional defects affecting learning and behavior cannot be reversed by giving iron later on.
WHE 2008 ● WHO strategies. (1) Food education. (2) Iron supplementation ~giving iron tablets to certain target group such as pregnant women and pre-school children. (3) Iron fortification of certain foods.
WHE 2008 Several Factors Determine the Feasibility and Effectiveness of Different Strategies (1) Health infrastructure. (2) Economy. (3) Access to iron fortification. (4) Food education.
WHE 2008 Treatment of Iron Deficiency (1) Blood transfusion should be reserved for patients with or at risk of cardiovascular instability. (2) Food education (3) Treatment of the underlying cause. (4) Correction of the deficiency by therapy with inorganic iron. Keep iron supplements highly capped and away from children’s reach.
WHE 2008 Treatment of Iron Deficiency: cont. Types of inorganic iron: (1) Ferrous sulphate (2) Ferrous gluconate (3) Ferrous fumarate
WHE 2008 Treatment of Iron Deficiency: cont. 200 mg ferrous sulphate – 63 mg iron 300 mg ferrous gluconate or ferrous fumarate - 35 mg iron Simultaneous intake of ascorbic acid will enhance the iron absorption. ü 2 -3 times /day , 3 -6 months to correct the deficit.
WHE 2008 Treatment of Iron Deficiency: cont. Side effects related to amount of iron epigastric pain and nausea diarrhea, constipation rarely skin eruptions
WHE 2008 Parentral Therapy - unnecessary lack of compliance because of side effects malabsorbtion late pregnancy when hemorrhage is likely to continue
Parentral Therapy: cont Intravenous preparation , Iron dextran (Imferon) Intramascular preparation , Iron sorbitol (jectofer) Sodium ferric gluconate (ferrlecit) sucrose (venofer)
WHE 2008 Parentral Therapy: cont. Side effects (1) systemic anaphylaxix (0. 6 -0. 7%) (2) local inflammation, phlebitis
WHE 2008 Poor Response to Therapy (●) Non compliance (●) On-going blood loss, infection or occult malignancy. (●) Incorrect diagnosis ~thalassemia trait. Anemia of chronic disorder. (●) Other nutritional deficiencies~B 12 and or folate.
WHE 2008 Recommendations: I ■ Educational programs to improve public awareness of this problem and it’s causes “greater food availability does not necessarily equal better nutrition and health status”. ■ Physician education is needed to ensure a greater awareness of iron deficiency and the testing needed to establish diagnosis as well as underlying causes. ■ Screening for iron deficiency in high risk groups in our community. ■ Healthy dietary habits
WHE 2008 Recommendations: II ■ Preventive dose of iron tablet for women presenting with heavy period. ■ Encouraging mothers to breast feed their infants and to include iron-enriched food in the diet of infants and young children. ■ Prescription of NSIAD or antiacid should be carried out with causion. ■ Future research is needed to evaluate dietary iron adequacy in Saudi diet.
WHE 2008 Conclusions ● Iron deficiency anemia has remained a widespread public health problem. ● One in five women and about half of all pregnant women are iron deficient according to the last Mayo Clinic report. ● Simple and easily treatable health problem under diagnosed ~undertreated problem. ● Primary health care specialist should advocate a fight against an old enemy.
