Congenital and Acquired Hemolytic Anemias Rachael Grace MD
- Slides: 56
Congenital and Acquired Hemolytic Anemias Rachael Grace, MD, MMSc
Disclosures • Agios Pharmaceuticals: Research funding, Scientific advisor Copyright © 2019 by ASPHO
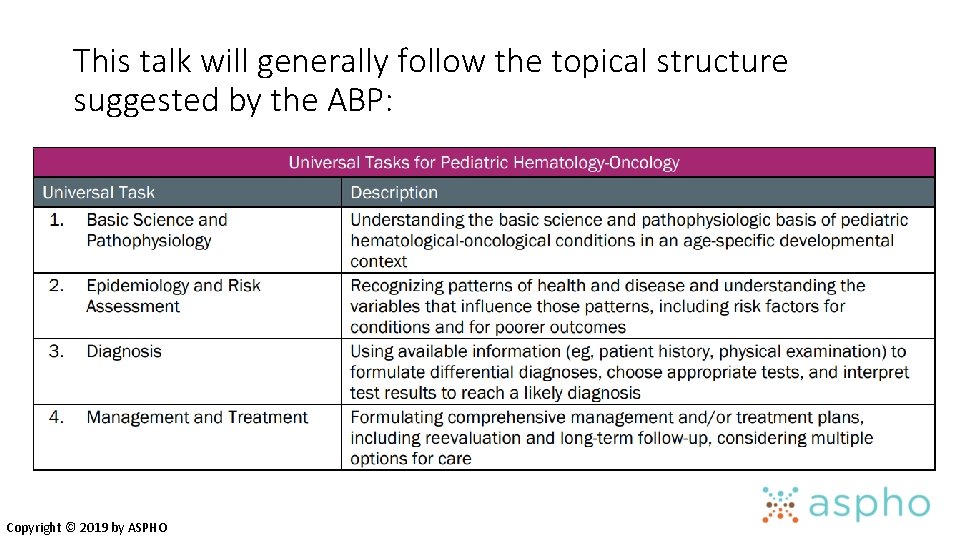
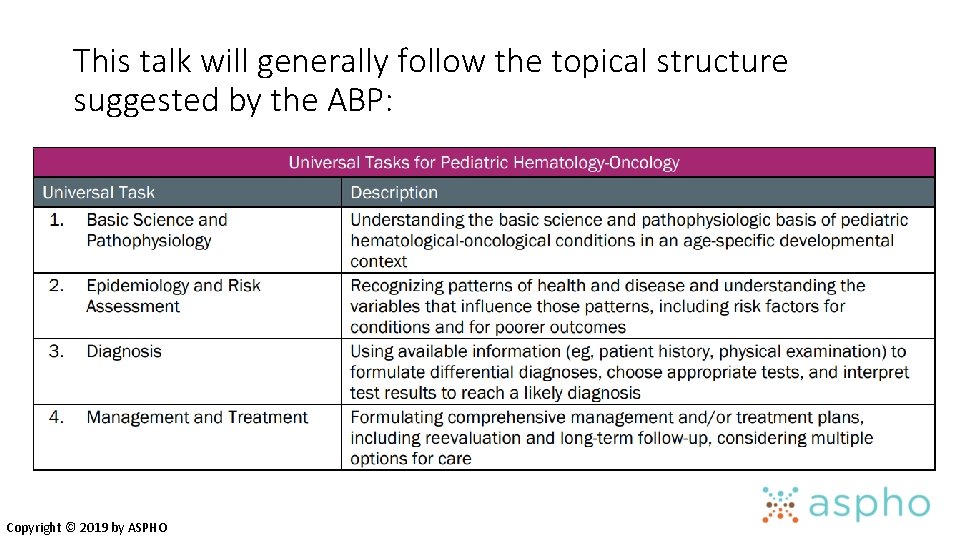
This talk will generally follow the topical structure suggested by the ABP: Copyright © 2019 by ASPHO
Hemolytic Anemia • General Features: Symptoms, Management, Differential Diagnosis • Membranopathies (Cytoskeleton) • Cation Permeability Defects (Ion Channel) • Unstable Hemoglobins • Enzymopathies • Methemoglobinemia • Antibody/Complement-Mediated • Microangiopathic Hemolytic Anemias (Fragmentation) • Other Hemolytic Anemias Copyright © 2019 by ASPHO
General Features Copyright © 2019 by ASPHO
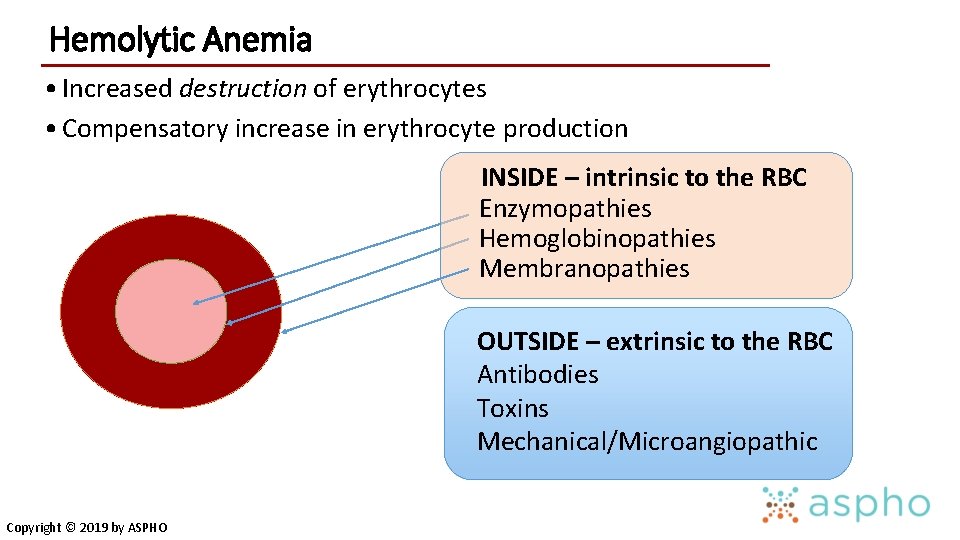
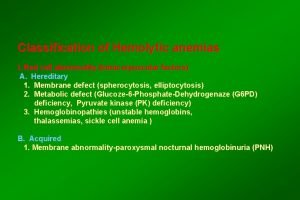
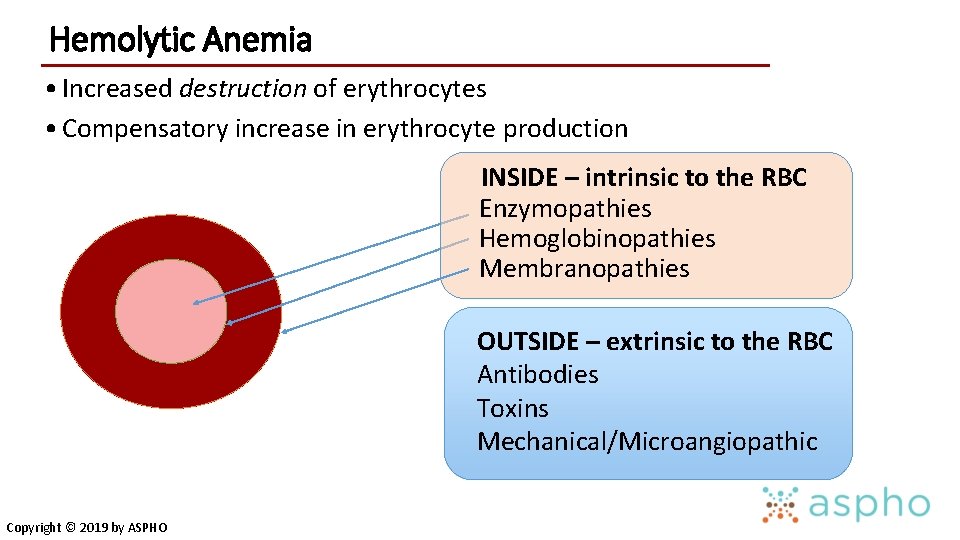
Hemolytic Anemia • Increased destruction of erythrocytes • Compensatory increase in erythrocyte production INSIDE – intrinsic to the RBC Enzymopathies Hemoglobinopathies Membranopathies OUTSIDE – extrinsic to the RBC Antibodies Toxins Mechanical/Microangiopathic Copyright © 2019 by ASPHO
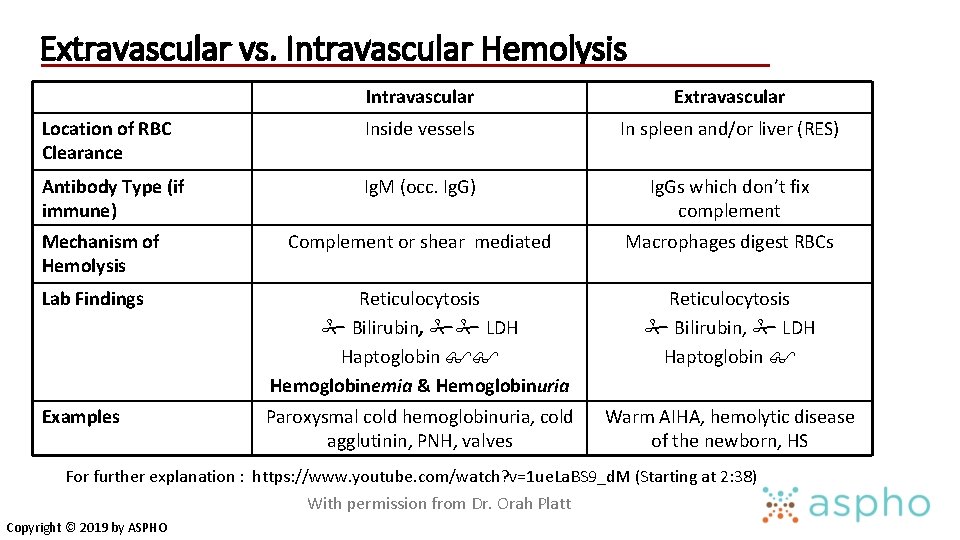
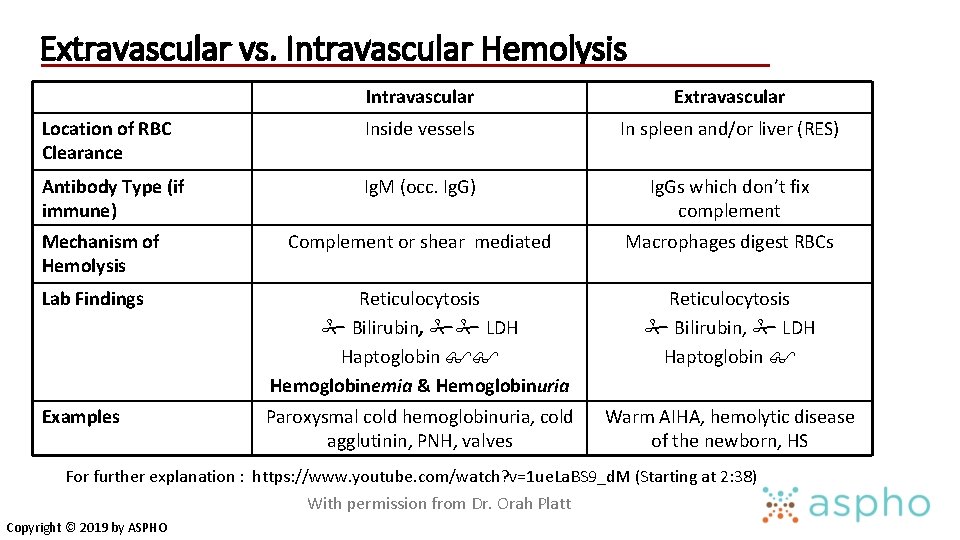
Extravascular vs. Intravascular Hemolysis Intravascular Extravascular Location of RBC Clearance Inside vessels In spleen and/or liver (RES) Antibody Type (if immune) Ig. M (occ. Ig. G) Ig. Gs which don’t fix complement Complement or shear mediated Macrophages digest RBCs Lab Findings Reticulocytosis Bilirubin, LDH Haptoglobin Hemoglobinemia & Hemoglobinuria Reticulocytosis Bilirubin, LDH Haptoglobin Examples Paroxysmal cold hemoglobinuria, cold agglutinin, PNH, valves Warm AIHA, hemolytic disease of the newborn, HS Mechanism of Hemolysis For further explanation : https: //www. youtube. com/watch? v=1 ue. La. BS 9_d. M (Starting at 2: 38) With permission from Dr. Orah Platt Copyright © 2019 by ASPHO
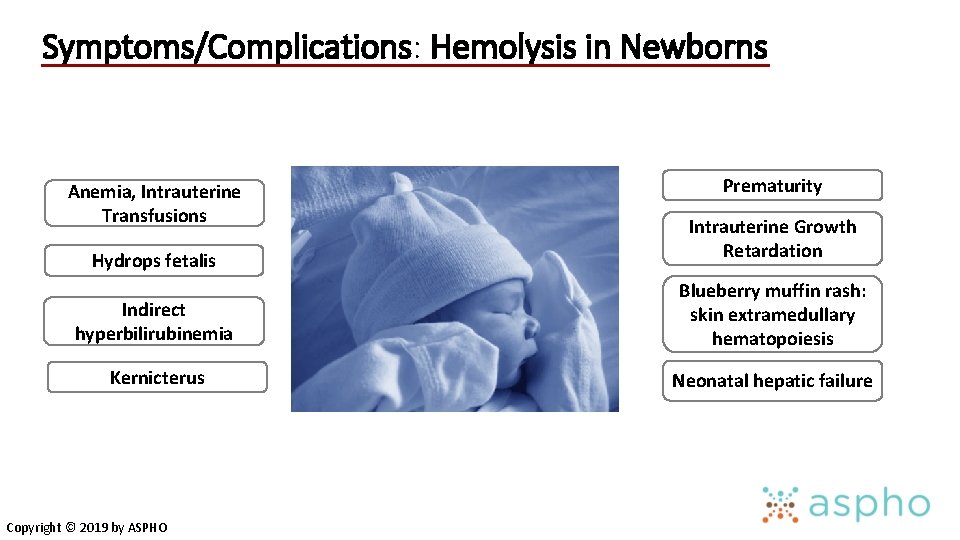
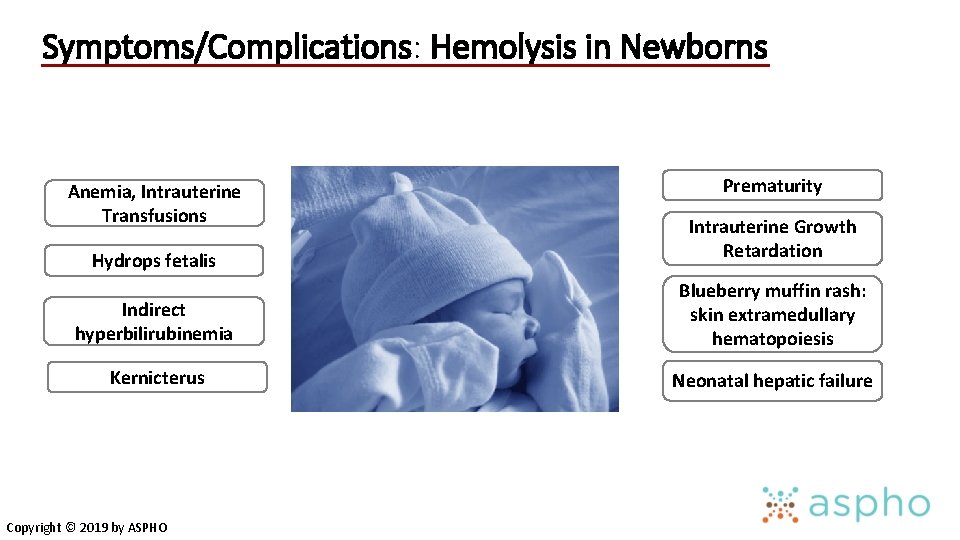
Symptoms/Complications: Hemolysis in Newborns Anemia, Intrauterine Transfusions Prematurity Hydrops fetalis Intrauterine Growth Retardation Indirect hyperbilirubinemia Blueberry muffin rash: skin extramedullary hematopoiesis Kernicterus Neonatal hepatic failure Copyright © 2019 by ASPHO
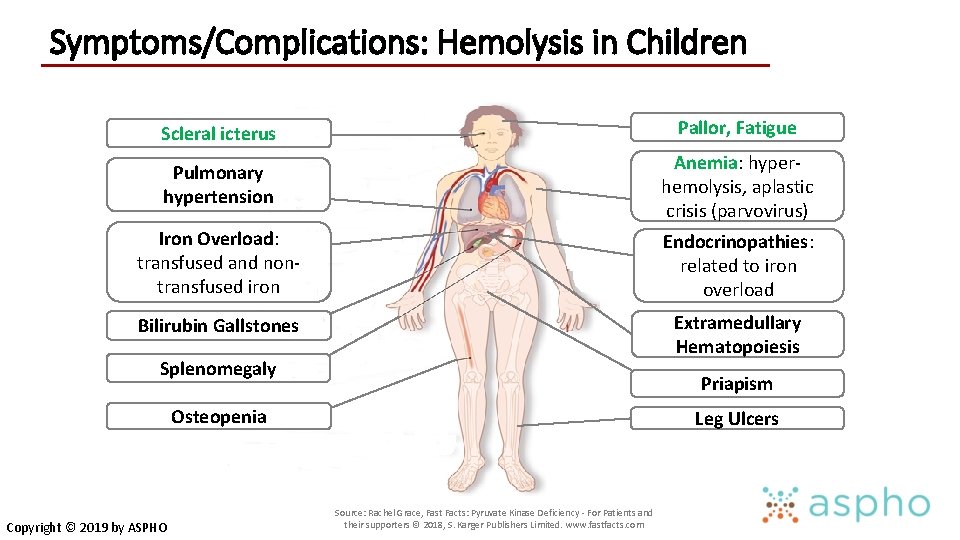
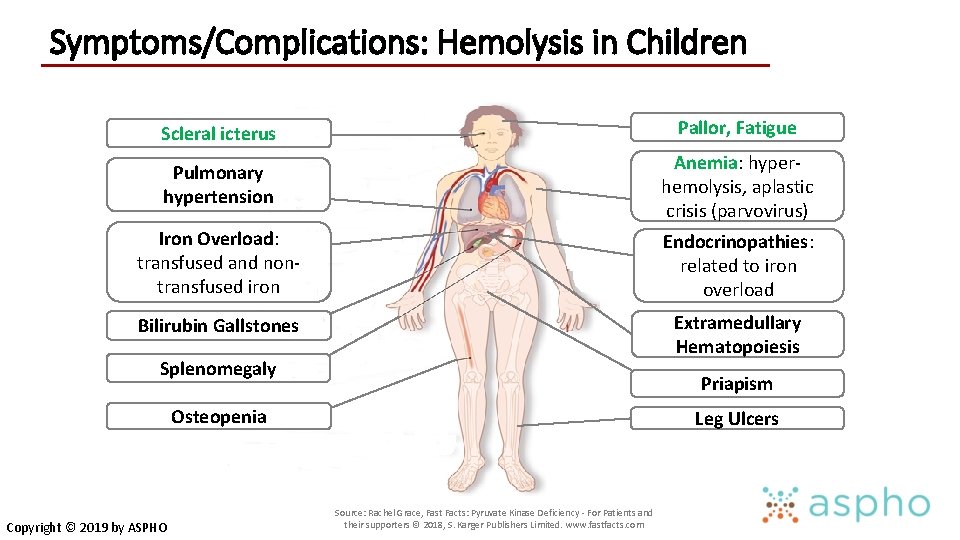
Symptoms/Complications: Hemolysis in Children Scleral icterus Pallor, Fatigue Pulmonary hypertension Anemia: hyperhemolysis, aplastic crisis (parvovirus) Iron Overload: transfused and nontransfused iron Endocrinopathies: related to iron overload Bilirubin Gallstones Extramedullary Hematopoiesis Splenomegaly Priapism Osteopenia Copyright © 2019 by ASPHO Leg Ulcers Source: Rachel Grace, Fast Facts: Pyruvate Kinase Deficiency - For Patients and their supporters © 2018, S. Karger Publishers Limited. www. fastfacts. com
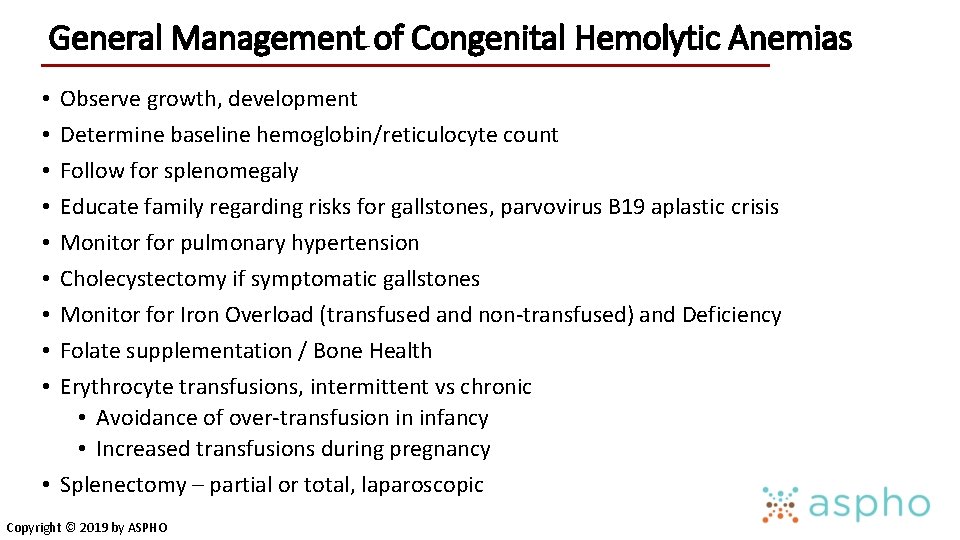
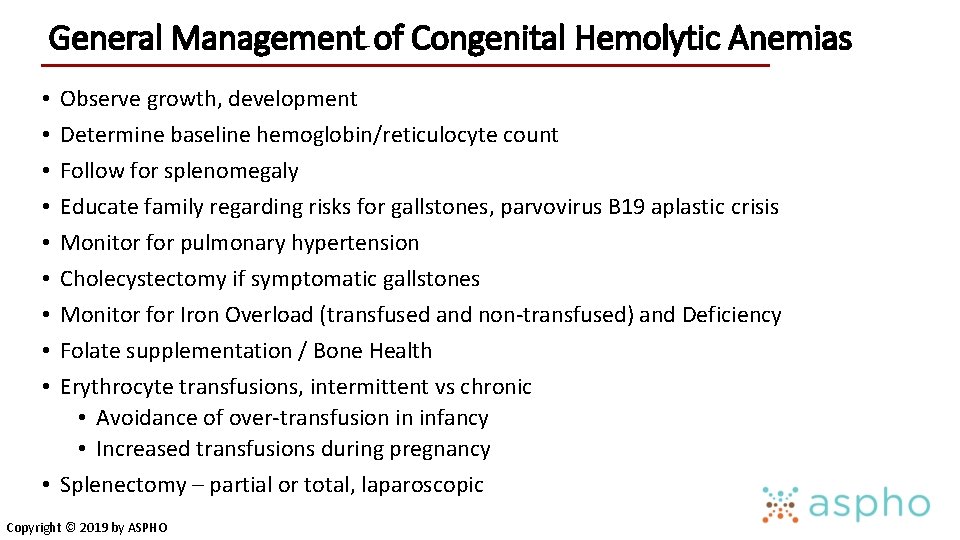
General Management of Congenital Hemolytic Anemias Observe growth, development Determine baseline hemoglobin/reticulocyte count Follow for splenomegaly Educate family regarding risks for gallstones, parvovirus B 19 aplastic crisis Monitor for pulmonary hypertension Cholecystectomy if symptomatic gallstones Monitor for Iron Overload (transfused and non-transfused) and Deficiency Folate supplementation / Bone Health Erythrocyte transfusions, intermittent vs chronic • Avoidance of over-transfusion in infancy • Increased transfusions during pregnancy • Splenectomy – partial or total, laparoscopic • • • Copyright © 2019 by ASPHO
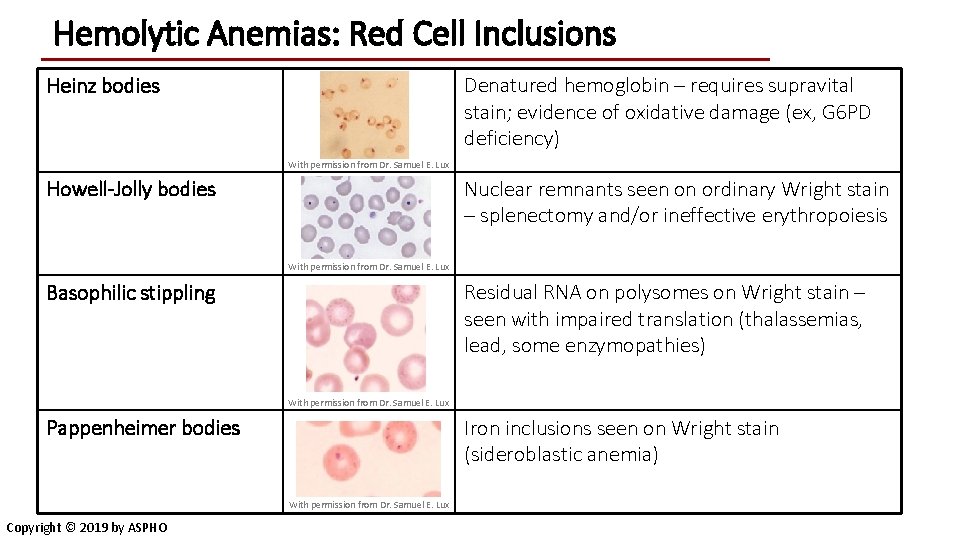
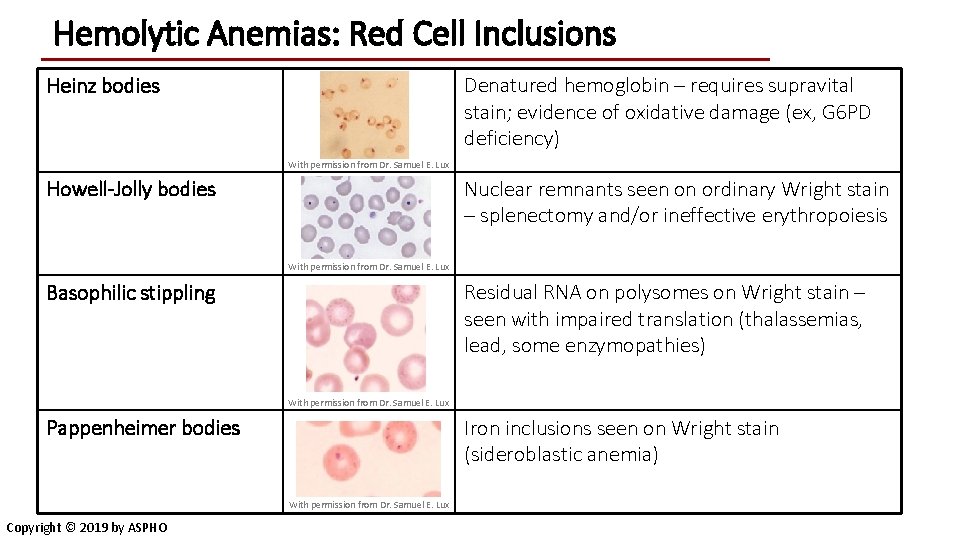
Hemolytic Anemias: Red Cell Inclusions Heinz bodies Denatured hemoglobin – requires supravital stain; evidence of oxidative damage (ex, G 6 PD deficiency) With permission from Dr. Samuel E. Lux Howell-Jolly bodies Nuclear remnants seen on ordinary Wright stain – splenectomy and/or ineffective erythropoiesis With permission from Dr. Samuel E. Lux Basophilic stippling Residual RNA on polysomes on Wright stain – seen with impaired translation (thalassemias, lead, some enzymopathies) With permission from Dr. Samuel E. Lux Pappenheimer bodies Iron inclusions seen on Wright stain (sideroblastic anemia) With permission from Dr. Samuel E. Lux Copyright © 2019 by ASPHO
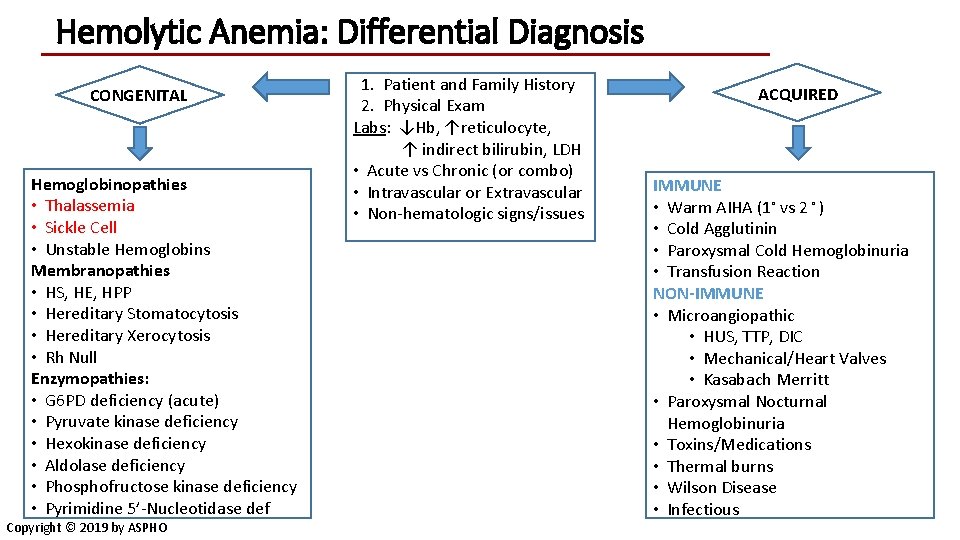
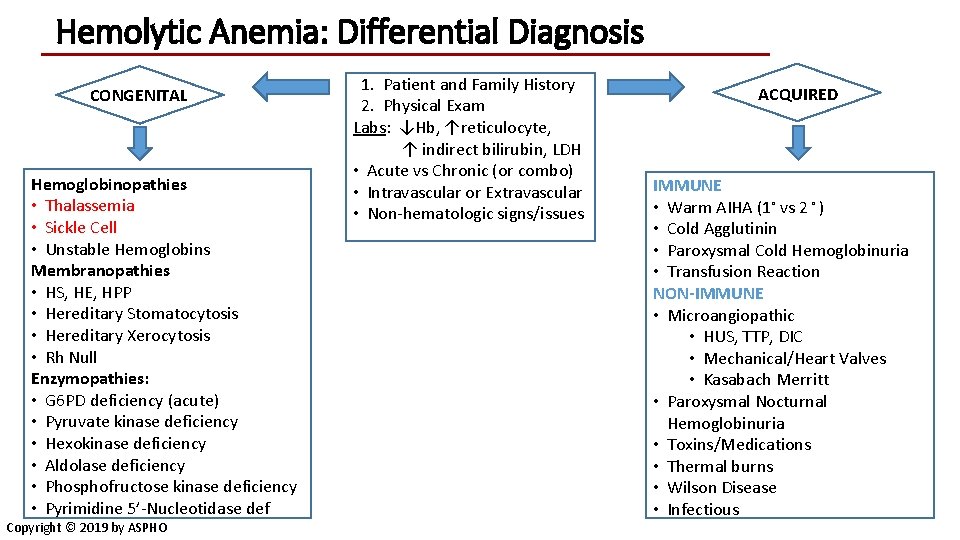
Hemolytic Anemia: Differential Diagnosis CONGENITAL Hemoglobinopathies • Thalassemia • Sickle Cell • Unstable Hemoglobins Membranopathies • HS, HE, HPP • Hereditary Stomatocytosis • Hereditary Xerocytosis • Rh Null Enzymopathies: • G 6 PD deficiency (acute) • Pyruvate kinase deficiency • Hexokinase deficiency • Aldolase deficiency • Phosphofructose kinase deficiency • Pyrimidine 5’-Nucleotidase def Copyright © 2019 by ASPHO 1. Patient and Family History 2. Physical Exam Labs: ↓Hb, ↑reticulocyte, ↑ indirect bilirubin, LDH • Acute vs Chronic (or combo) • Intravascular or Extravascular • Non-hematologic signs/issues ACQUIRED IMMUNE • Warm AIHA (1◦ vs 2 ◦ ) • Cold Agglutinin • Paroxysmal Cold Hemoglobinuria • Transfusion Reaction NON-IMMUNE • Microangiopathic • HUS, TTP, DIC • Mechanical/Heart Valves • Kasabach Merritt • Paroxysmal Nocturnal Hemoglobinuria • Toxins/Medications • Thermal burns • Wilson Disease • Infectious
Red Cell Membrane Disorders Copyright © 2019 by ASPHO
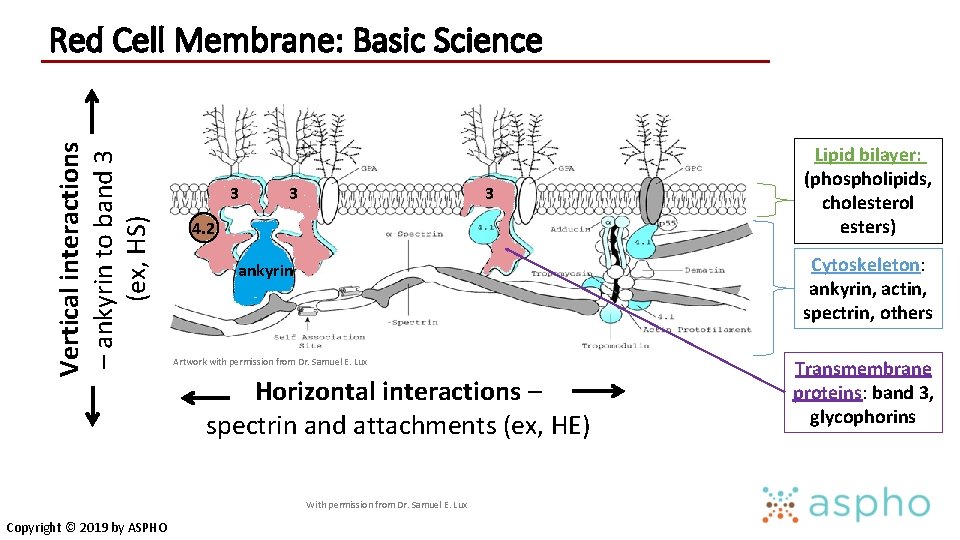
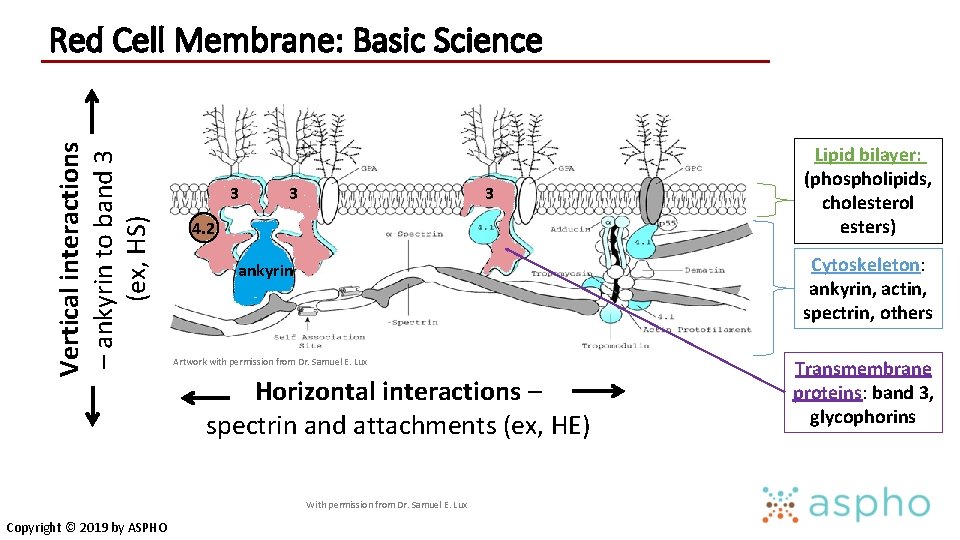
Vertical interactions – ankyrin to band 3 (ex, HS) Red Cell Membrane: Basic Science 3 3 3 4. 2 Cytoskeleton: ankyrin, actin, spectrin, others ankyrin Artwork with permission from Dr. Samuel E. Lux Horizontal interactions – spectrin and attachments (ex, HE) With permission from Dr. Samuel E. Lux Copyright © 2019 by ASPHO Lipid bilayer: (phospholipids, cholesterol esters) Transmembrane proteins: band 3, glycophorins
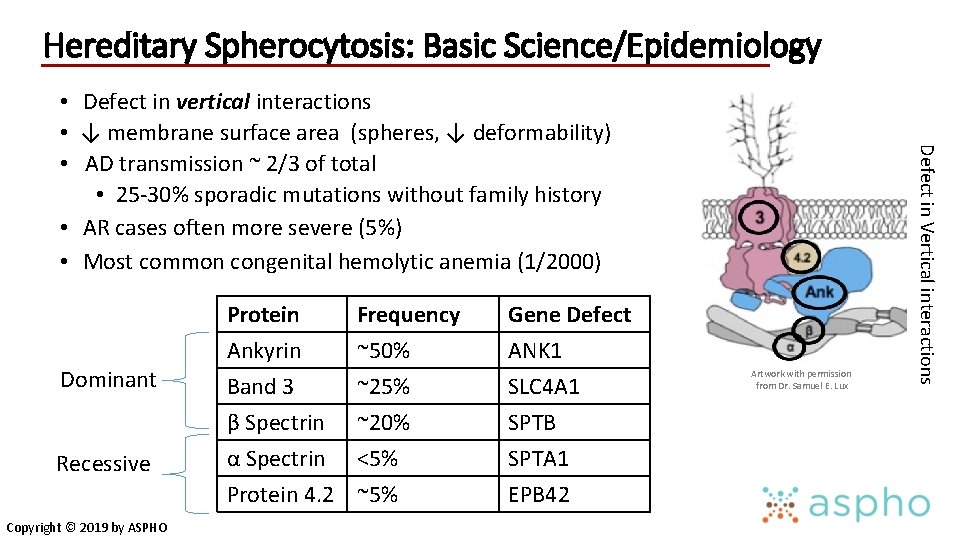
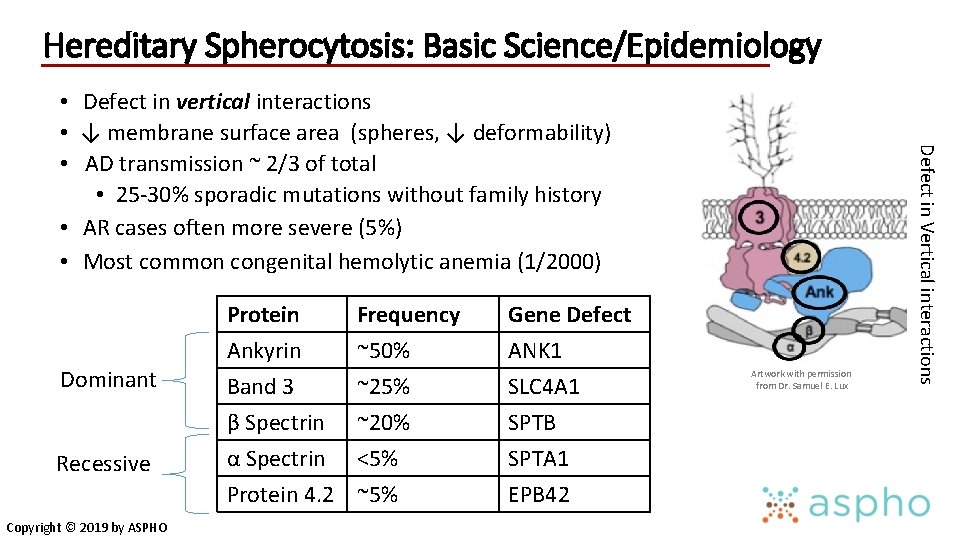
Hereditary Spherocytosis: Basic Science/Epidemiology Dominant Recessive Copyright © 2019 by ASPHO Protein Ankyrin Band 3 β Spectrin Frequency ~50% ~25% ~20% α Spectrin <5% Protein 4. 2 ~5% Gene Defect ANK 1 SLC 4 A 1 SPTB SPTA 1 EPB 42 Artwork with permission from Dr. Samuel E. Lux Defect in Vertical interactions • Defect in vertical interactions • ↓ membrane surface area (spheres, ↓ deformability) • AD transmission ~ 2/3 of total • 25 -30% sporadic mutations without family history • AR cases often more severe (5%) • Most common congenital hemolytic anemia (1/2000)
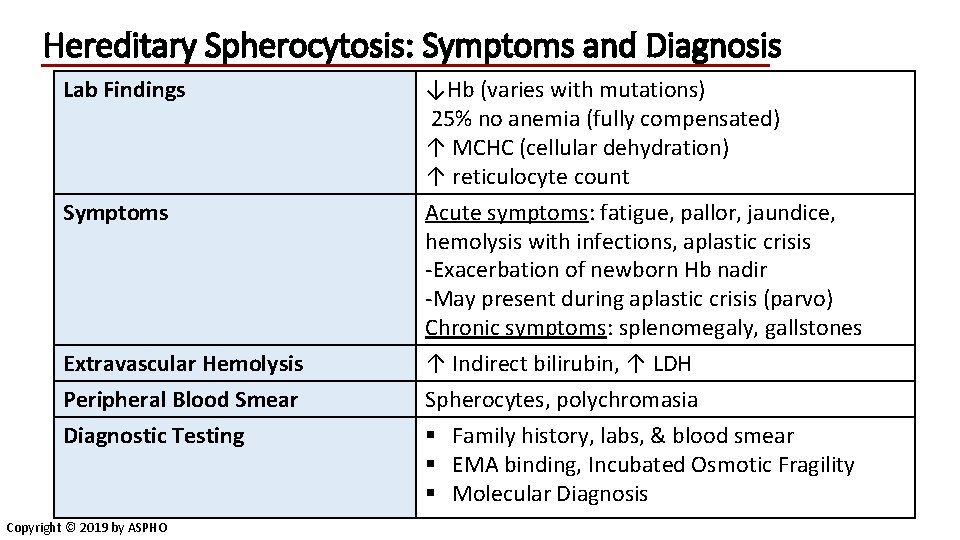
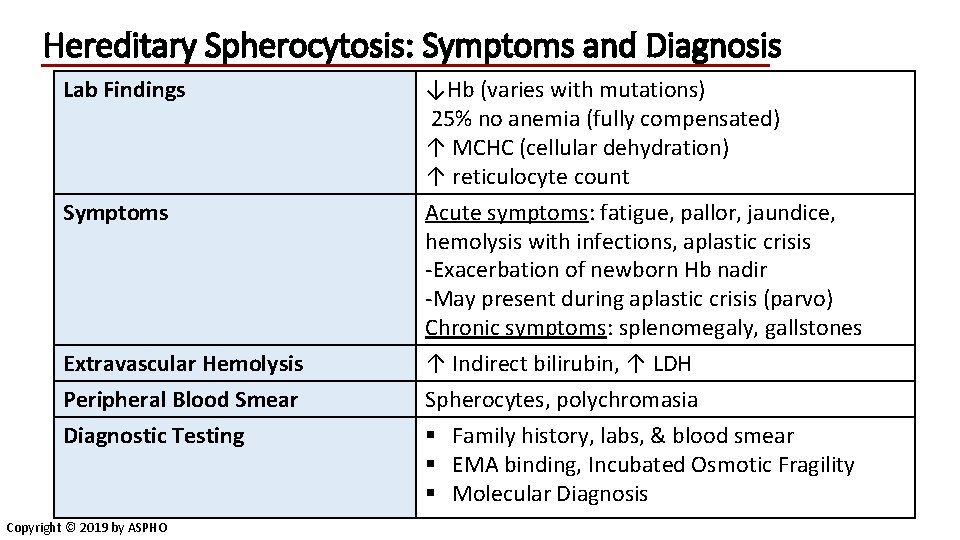
Hereditary Spherocytosis: Symptoms and Diagnosis Lab Findings Symptoms Extravascular Hemolysis Peripheral Blood Smear Diagnostic Testing Copyright © 2019 by ASPHO ↓Hb (varies with mutations) 25% no anemia (fully compensated) ↑ MCHC (cellular dehydration) ↑ reticulocyte count Acute symptoms: fatigue, pallor, jaundice, hemolysis with infections, aplastic crisis -Exacerbation of newborn Hb nadir -May present during aplastic crisis (parvo) Chronic symptoms: splenomegaly, gallstones ↑ Indirect bilirubin, ↑ LDH Spherocytes, polychromasia § Family history, labs, & blood smear § EMA binding, Incubated Osmotic Fragility § Molecular Diagnosis
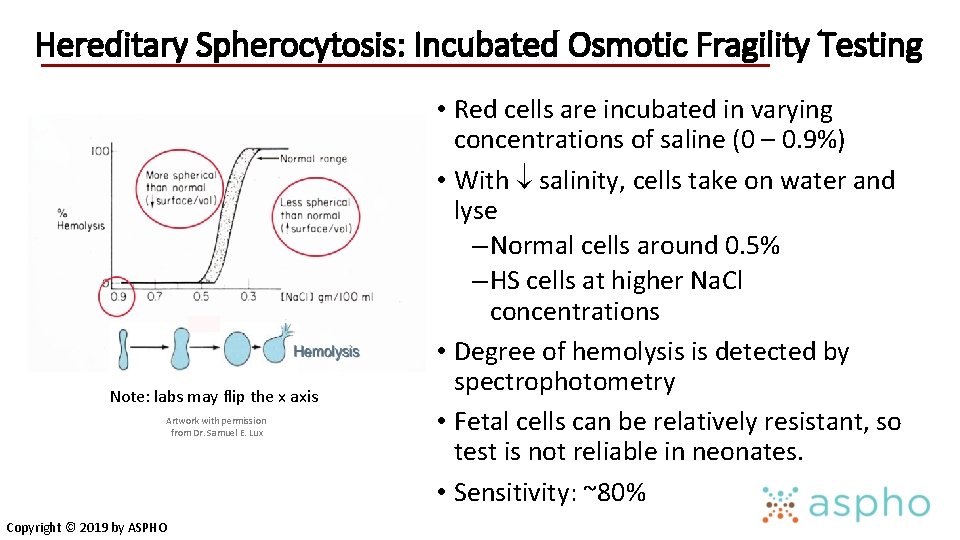
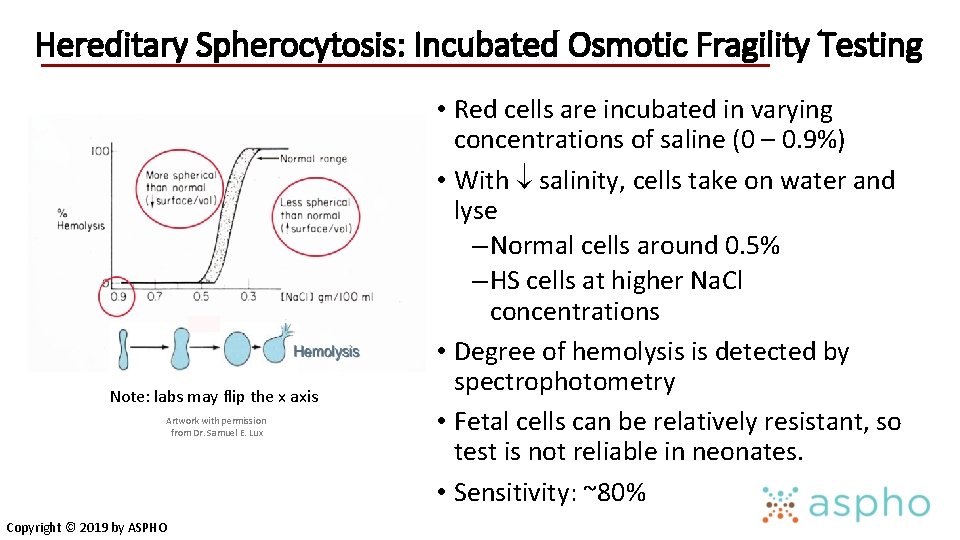
Hereditary Spherocytosis: Incubated Osmotic Fragility Testing Note: labs may flip the x axis Artwork with permission from Dr. Samuel E. Lux Copyright © 2019 by ASPHO • Red cells are incubated in varying concentrations of saline (0 – 0. 9%) • With salinity, cells take on water and lyse – Normal cells around 0. 5% – HS cells at higher Na. Cl concentrations • Degree of hemolysis is detected by spectrophotometry • Fetal cells can be relatively resistant, so test is not reliable in neonates. • Sensitivity: ~80%
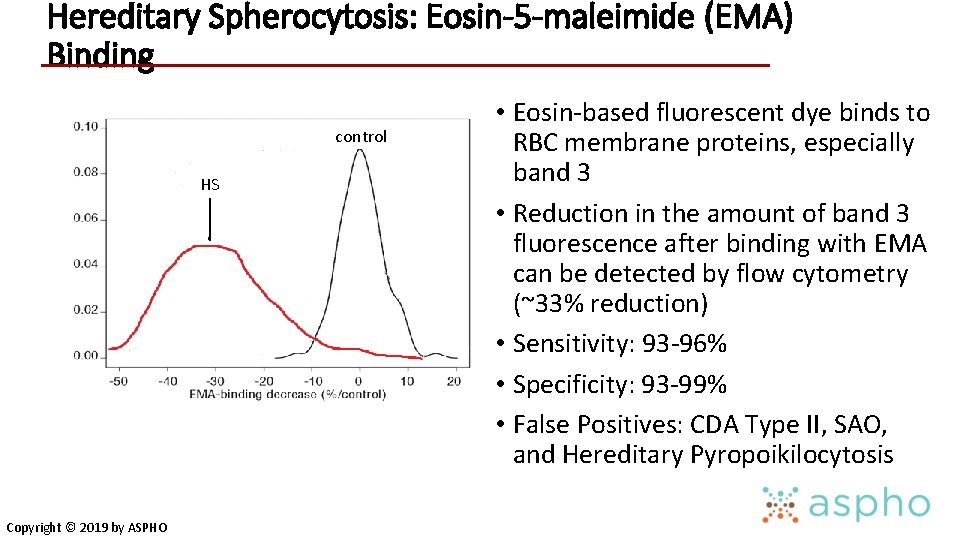
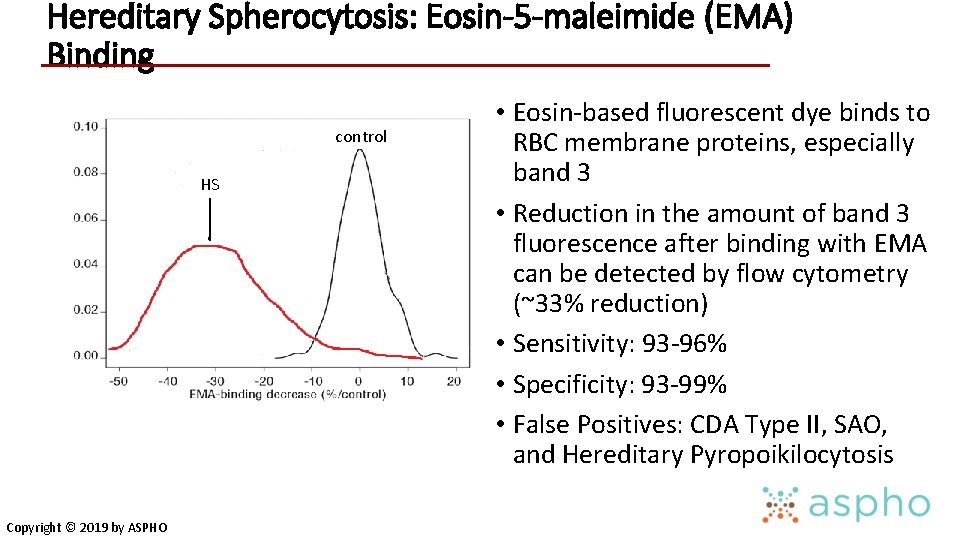
Hereditary Spherocytosis: Eosin-5 -maleimide (EMA) Binding control HS Copyright © 2019 by ASPHO • Eosin-based fluorescent dye binds to RBC membrane proteins, especially band 3 • Reduction in the amount of band 3 fluorescence after binding with EMA can be detected by flow cytometry (~33% reduction) • Sensitivity: 93 -96% • Specificity: 93 -99% • False Positives: CDA Type II, SAO, and Hereditary Pyropoikilocytosis
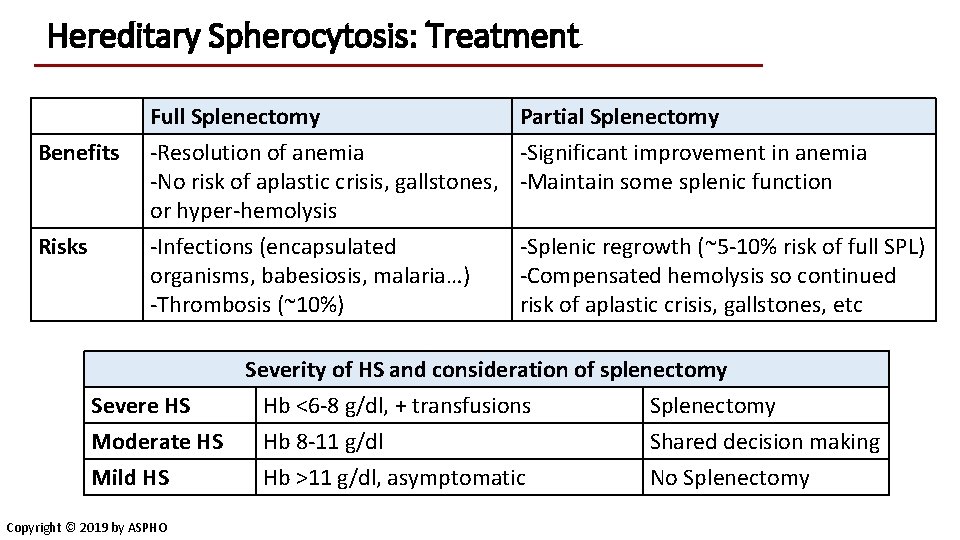
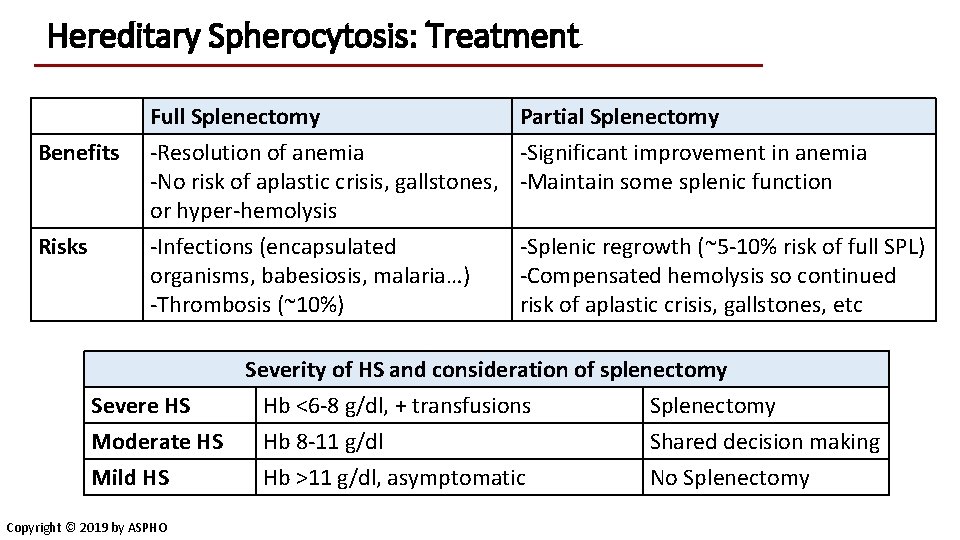
Hereditary Spherocytosis: Treatment Benefits Risks Full Splenectomy Partial Splenectomy -Resolution of anemia -Significant improvement in anemia -No risk of aplastic crisis, gallstones, -Maintain some splenic function or hyper-hemolysis -Infections (encapsulated organisms, babesiosis, malaria…) -Thrombosis (~10%) -Splenic regrowth (~5 -10% risk of full SPL) -Compensated hemolysis so continued risk of aplastic crisis, gallstones, etc Severity of HS and consideration of splenectomy Severe HS Hb <6 -8 g/dl, + transfusions Splenectomy Moderate HS Hb 8 -11 g/dl Shared decision making Mild HS Hb >11 g/dl, asymptomatic No Splenectomy Copyright © 2019 by ASPHO
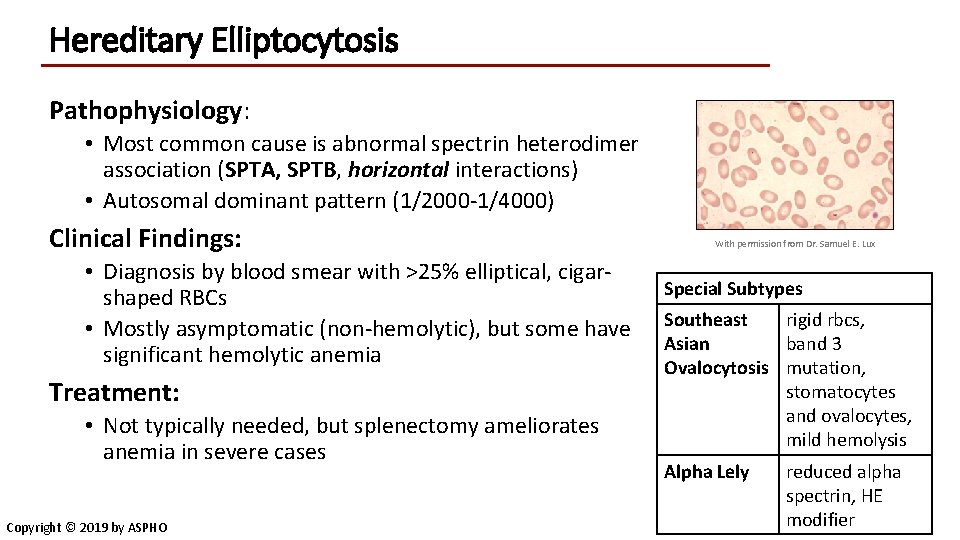
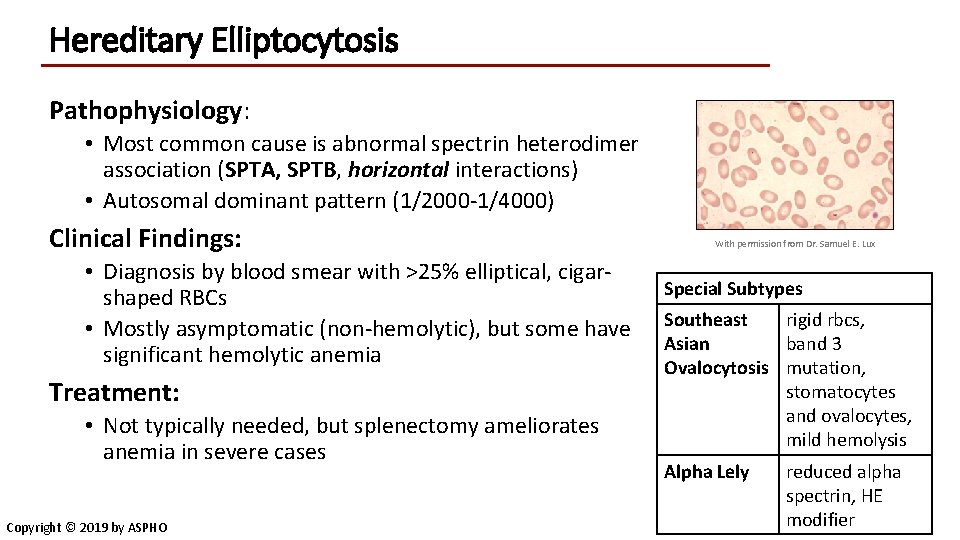
Hereditary Elliptocytosis Pathophysiology: • Most common cause is abnormal spectrin heterodimer association (SPTA, SPTB, horizontal interactions) • Autosomal dominant pattern (1/2000 -1/4000) Clinical Findings: • Diagnosis by blood smear with >25% elliptical, cigarshaped RBCs • Mostly asymptomatic (non-hemolytic), but some have significant hemolytic anemia Treatment: • Not typically needed, but splenectomy ameliorates anemia in severe cases Copyright © 2019 by ASPHO With permission from Dr. Samuel E. Lux Special Subtypes Southeast rigid rbcs, Asian band 3 Ovalocytosis mutation, stomatocytes and ovalocytes, mild hemolysis Alpha Lely reduced alpha spectrin, HE modifier
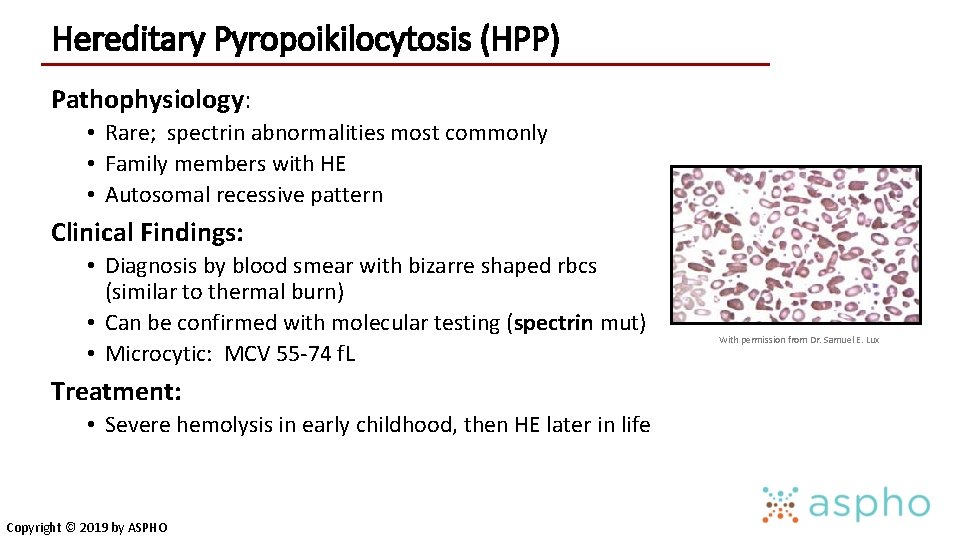
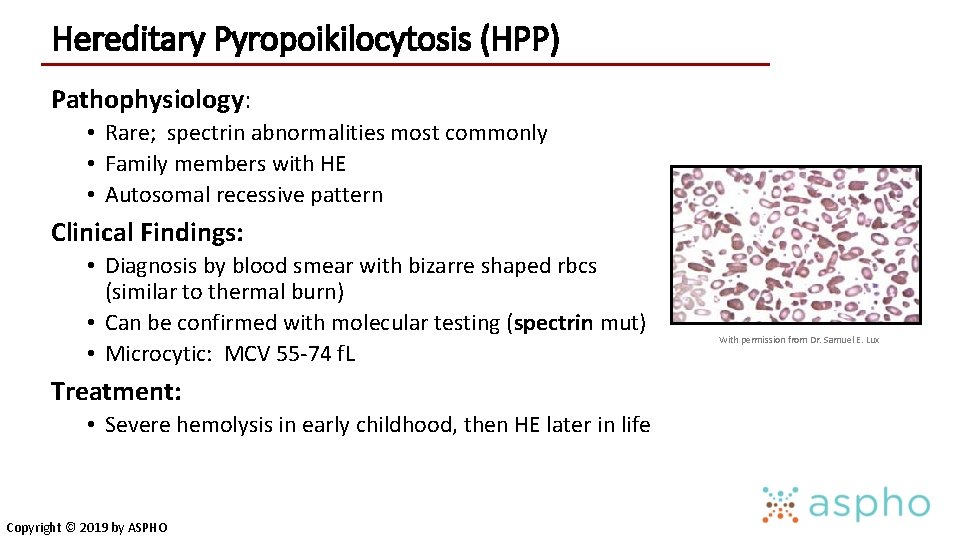
Hereditary Pyropoikilocytosis (HPP) Pathophysiology: • Rare; spectrin abnormalities most commonly • Family members with HE • Autosomal recessive pattern Clinical Findings: • Diagnosis by blood smear with bizarre shaped rbcs (similar to thermal burn) • Can be confirmed with molecular testing (spectrin mut) • Microcytic: MCV 55 -74 f. L Treatment: • Severe hemolysis in early childhood, then HE later in life Copyright © 2019 by ASPHO With permission from Dr. Samuel E. Lux
Cation Permeability Defects (Ion Channel) Copyright © 2019 by ASPHO
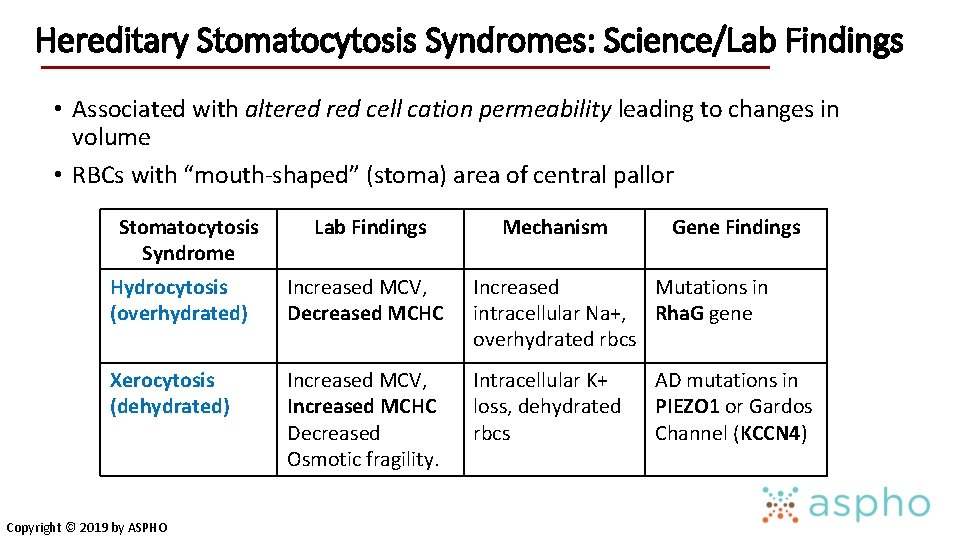
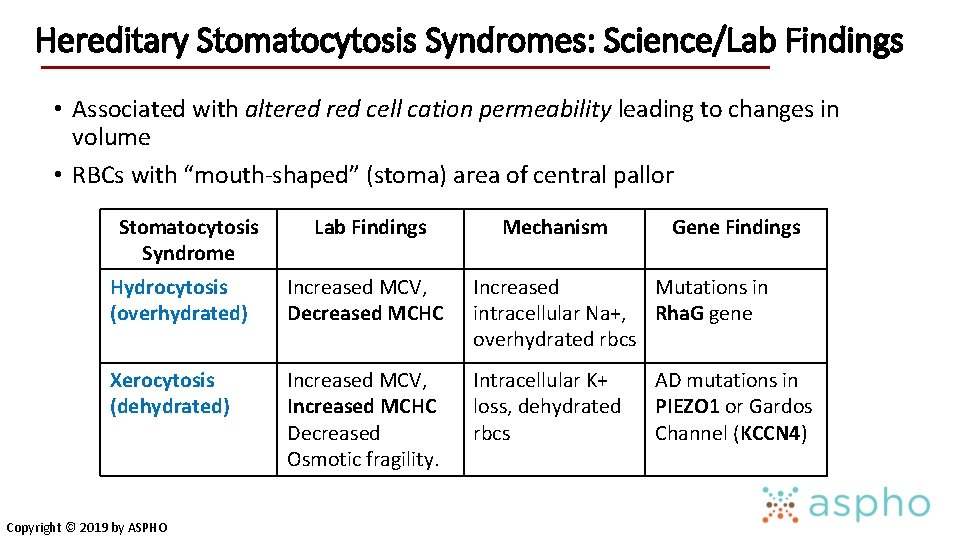
Hereditary Stomatocytosis Syndromes: Science/Lab Findings • Associated with altered cell cation permeability leading to changes in volume • RBCs with “mouth-shaped” (stoma) area of central pallor Stomatocytosis Syndrome Lab Findings Mechanism Gene Findings Hydrocytosis (overhydrated) Increased MCV, Decreased MCHC Increased Mutations in intracellular Na+, Rha. G gene overhydrated rbcs Xerocytosis (dehydrated) Increased MCV, Increased MCHC Decreased Osmotic fragility. Intracellular K+ loss, dehydrated rbcs Copyright © 2019 by ASPHO AD mutations in PIEZO 1 or Gardos Channel (KCCN 4)
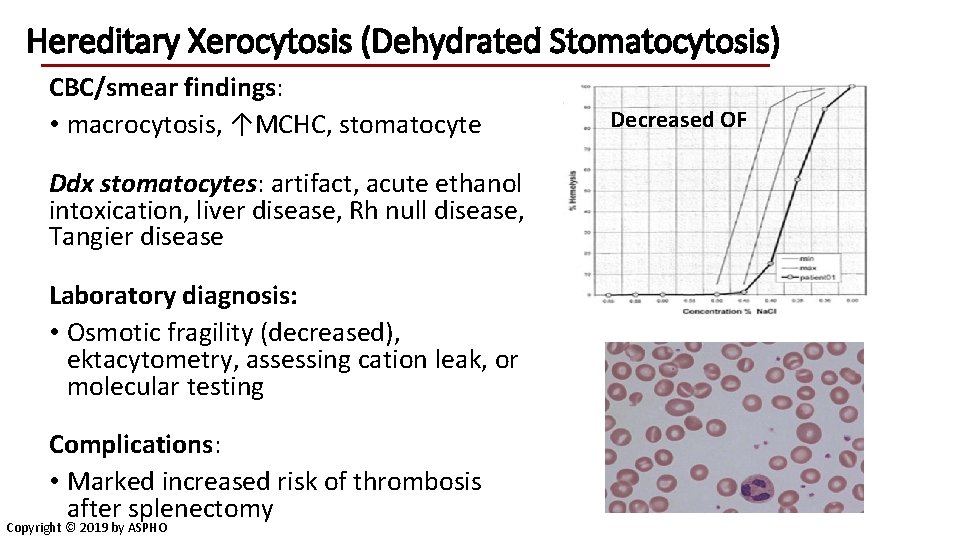
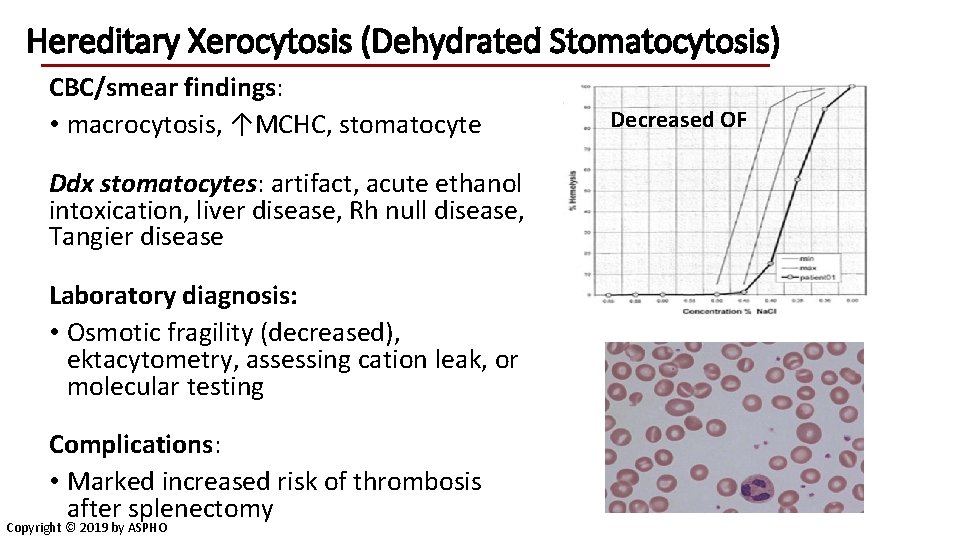
Hereditary Xerocytosis (Dehydrated Stomatocytosis) CBC/smear findings: • macrocytosis, ↑MCHC, stomatocyte Ddx stomatocytes: artifact, acute ethanol intoxication, liver disease, Rh null disease, Tangier disease Laboratory diagnosis: • Osmotic fragility (decreased), ektacytometry, assessing cation leak, or molecular testing Complications: • Marked increased risk of thrombosis after splenectomy Copyright © 2019 by ASPHO Decreased OF
Unstable Hemoglobins (all other hemoglobinopathies covered in other lectures) Copyright © 2019 by ASPHO
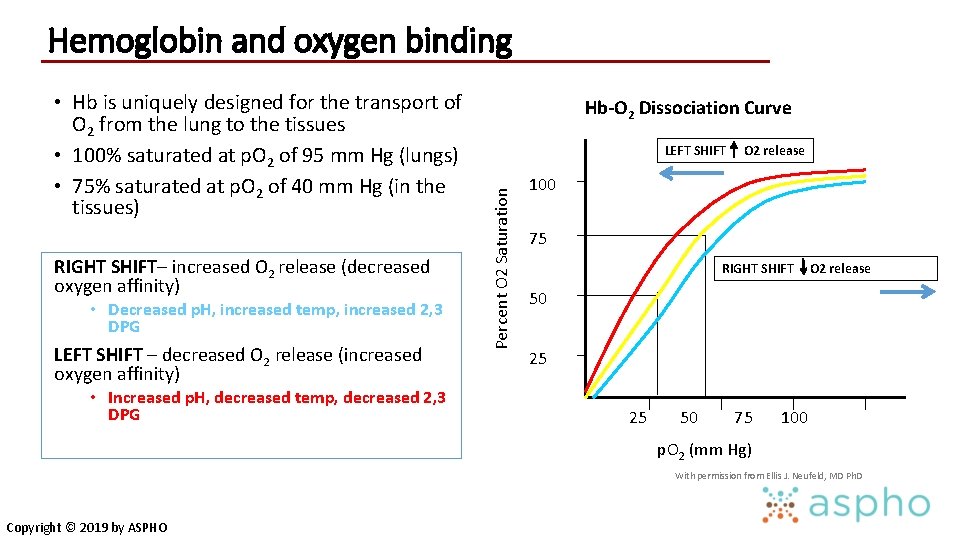
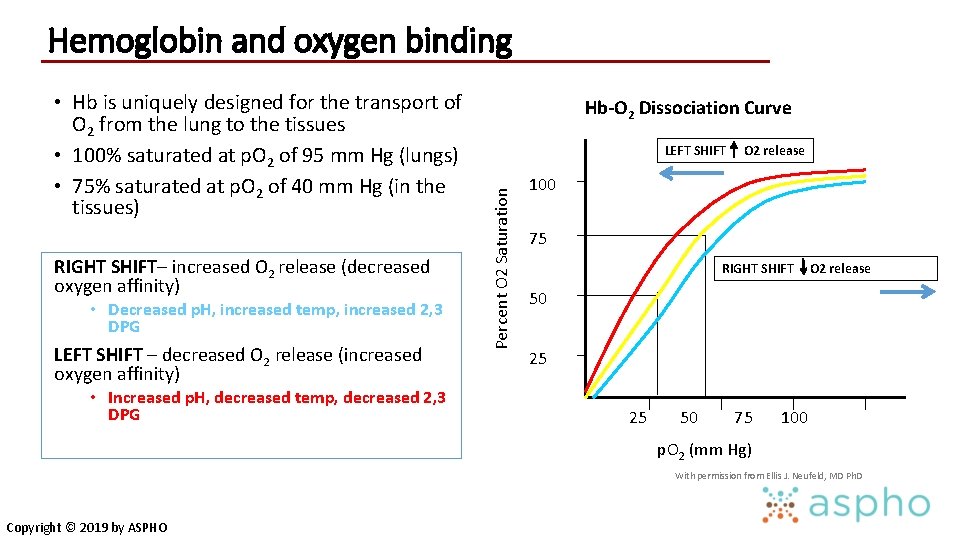
Hemoglobin and oxygen binding RIGHT SHIFT– increased O 2 release (decreased oxygen affinity) • Decreased p. H, increased temp, increased 2, 3 DPG LEFT SHIFT – decreased O 2 release (increased oxygen affinity) • Increased p. H, decreased temp, decreased 2, 3 DPG Hb-O 2 Dissociation Curve LEFT SHIFT Percent O 2 Saturation • Hb is uniquely designed for the transport of O 2 from the lung to the tissues • 100% saturated at p. O 2 of 95 mm Hg (lungs) • 75% saturated at p. O 2 of 40 mm Hg (in the tissues) O 2 release 100 75 RIGHT SHIFT O 2 release 50 25 25 50 75 100 p. O 2 (mm Hg) With permission from Ellis J. Neufeld, MD Ph. D Copyright © 2019 by ASPHO
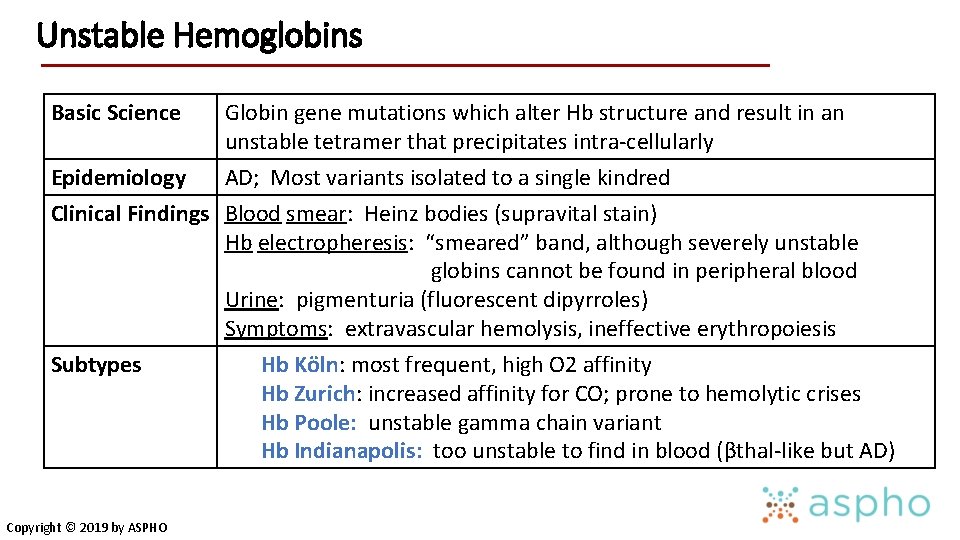
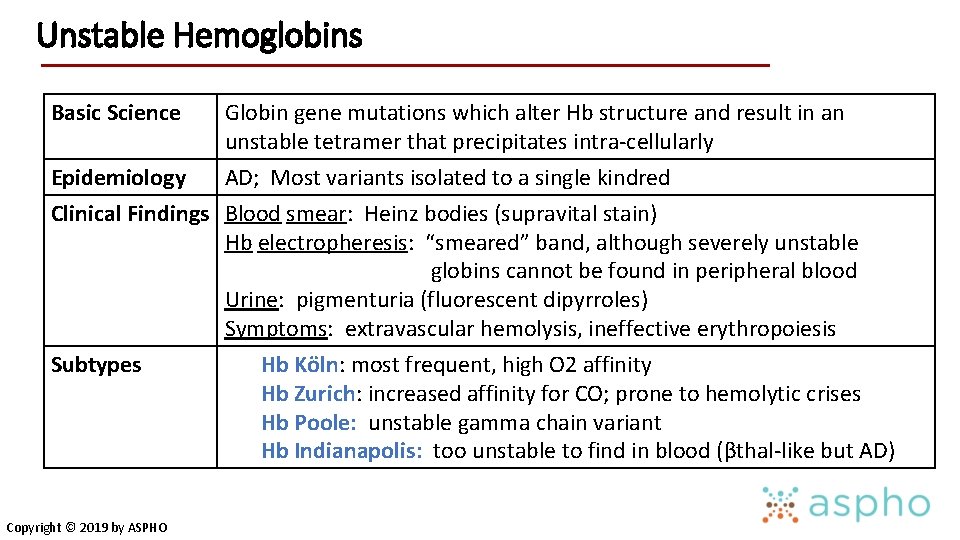
Unstable Hemoglobins Basic Science Globin gene mutations which alter Hb structure and result in an unstable tetramer that precipitates intra-cellularly Epidemiology AD; Most variants isolated to a single kindred Clinical Findings Blood smear: Heinz bodies (supravital stain) Hb electropheresis: “smeared” band, although severely unstable globins cannot be found in peripheral blood Urine: pigmenturia (fluorescent dipyrroles) Symptoms: extravascular hemolysis, ineffective erythropoiesis Subtypes Hb Köln: most frequent, high O 2 affinity Hb Zurich: increased affinity for CO; prone to hemolytic crises Hb Poole: unstable gamma chain variant Hb Indianapolis: too unstable to find in blood (βthal-like but AD) Copyright © 2019 by ASPHO
Enzymopathies Copyright © 2019 by ASPHO
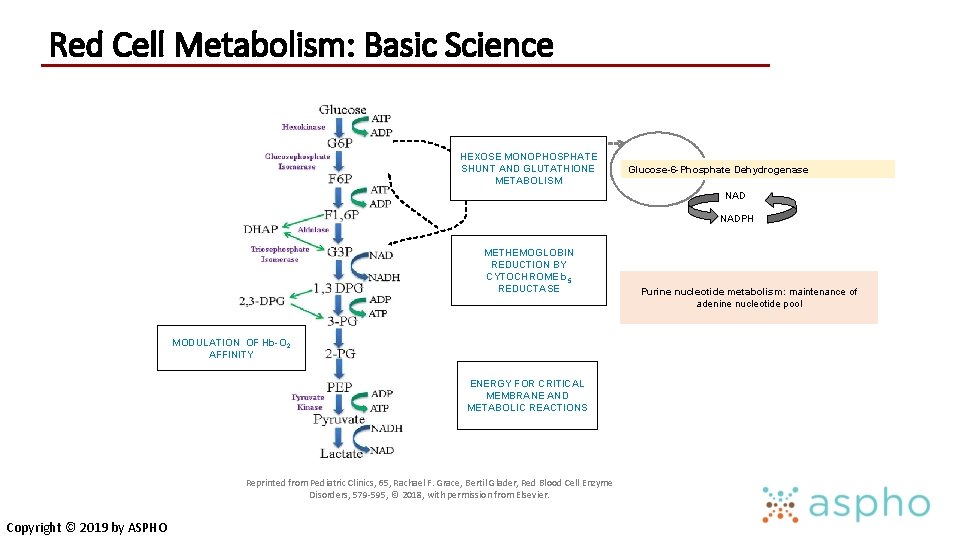
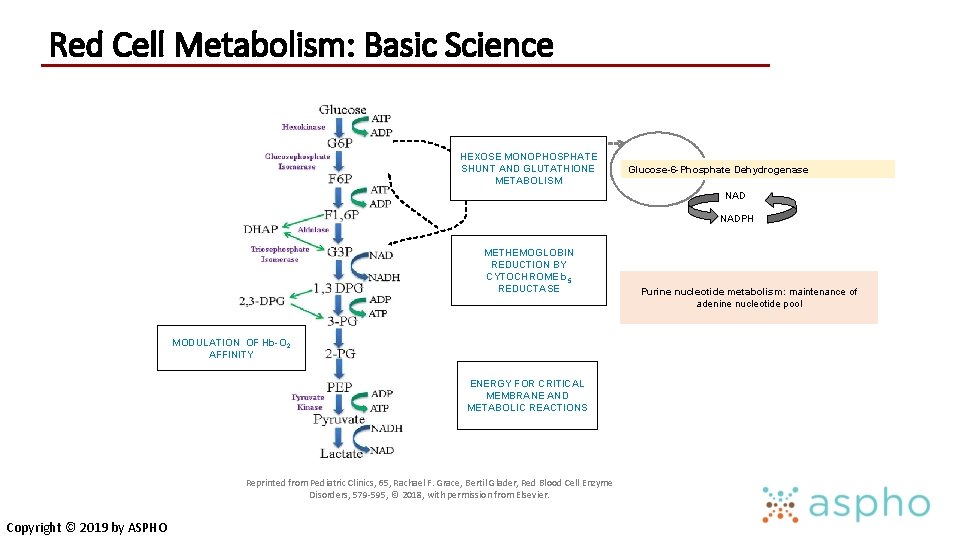
Red Cell Metabolism: Basic Science HEXOSE MONOPHOSPHATE SHUNT AND GLUTATHIONE METABOLISM Glucose-6 -Phosphate Dehydrogenase NADPH METHEMOGLOBIN REDUCTION BY CYTOCHROME b 5 REDUCTASE MODULATION OF Hb-O 2 AFFINITY ENERGY FOR CRITICAL MEMBRANE AND METABOLIC REACTIONS Reprinted from Pediatric Clinics, 65, Rachael F. Grace, Bertil Glader, Red Blood Cell Enzyme Disorders, 579 -595, © 2018, with permission from Elsevier. Copyright © 2019 by ASPHO Purine nucleotide metabolism: maintenance of adenine nucleotide pool
RBC Enzyme Disorders: Pathophysiology • RBC enzymes are important for: • Energy production through glycolysis and the Hexose monophosphate shunt (pyruvate kinase deficiency) • Maintaining cation gradient • Protecting from oxidative damage (G 6 PD deficiency) • Production of 2, 3 DPG • Maintenance of ferrous 2+ heme iron (methemoglobinemia) • Nucleotide salvage (pyrimidine 5’ nucleotidase: basophilic stippling) • Abnormalities result in diverse phenotypes, both hematologic and nonhematologic Copyright © 2019 by ASPHO
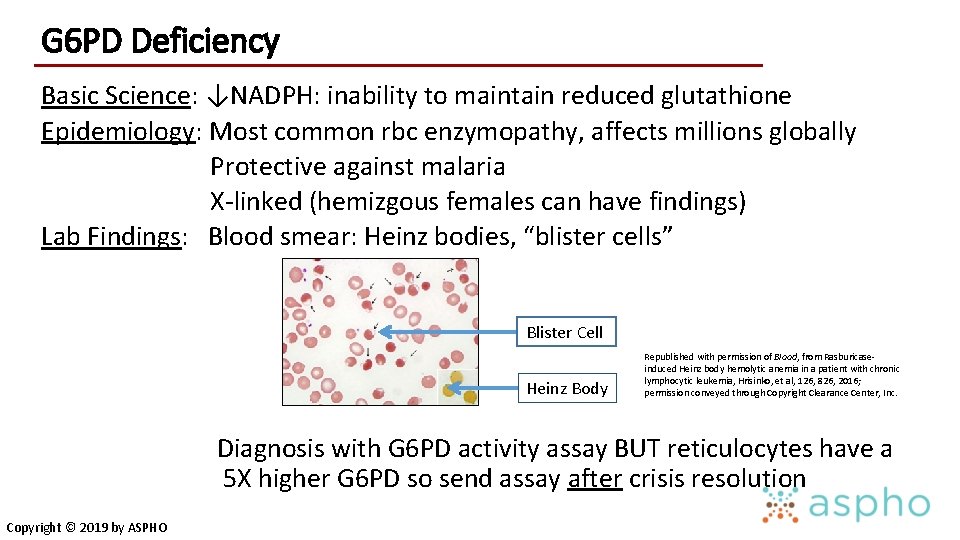
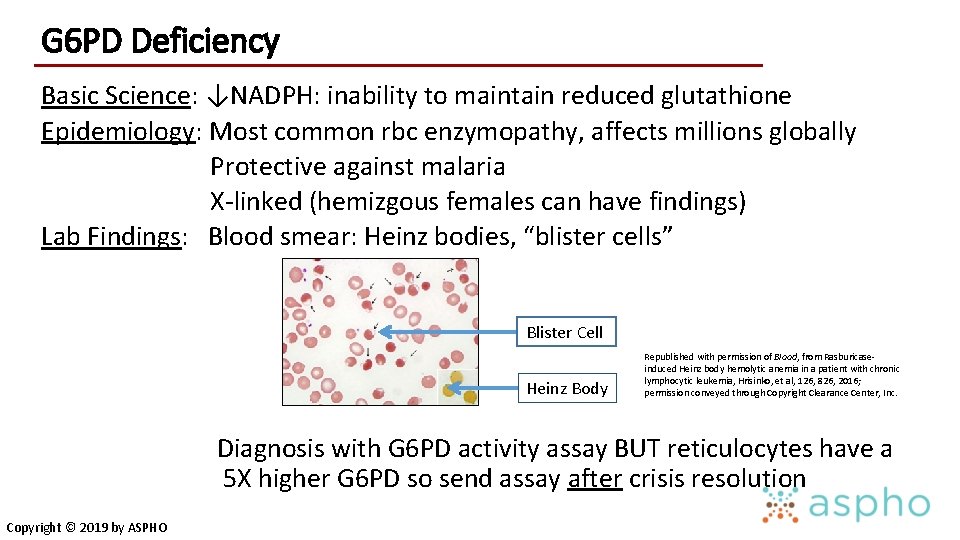
G 6 PD Deficiency Basic Science: ↓NADPH: inability to maintain reduced glutathione Epidemiology: Most common rbc enzymopathy, affects millions globally Protective against malaria X-linked (hemizgous females can have findings) Lab Findings: Blood smear: Heinz bodies, “blister cells” Blister Cell Heinz Body Republished with permission of Blood, from Rasburicaseinduced Heinz body hemolytic anemia in a patient with chronic lymphocytic leukemia, Hrisinko, et al, 126, 826, 2016; permission conveyed through Copyright Clearance Center, Inc. Diagnosis with G 6 PD activity assay BUT reticulocytes have a 5 X higher G 6 PD so send assay after crisis resolution Copyright © 2019 by ASPHO
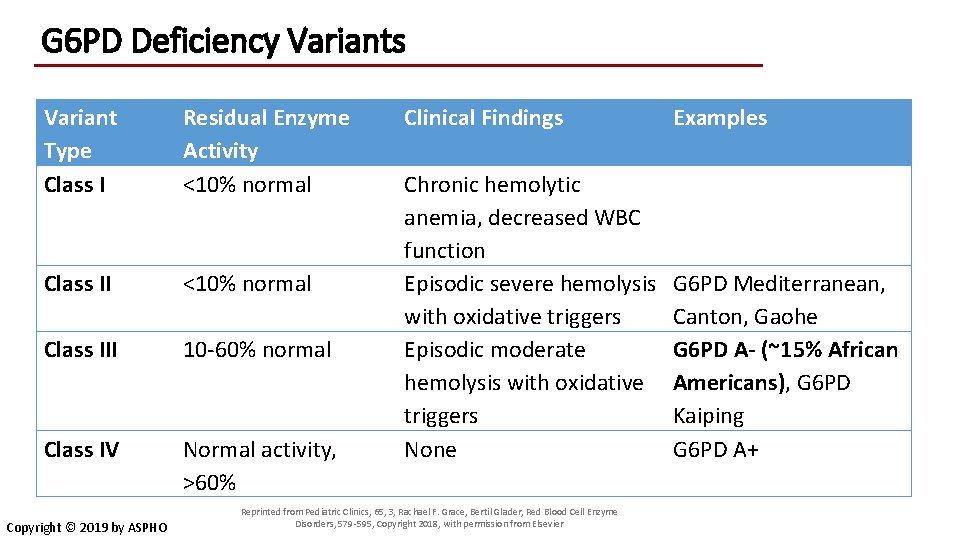
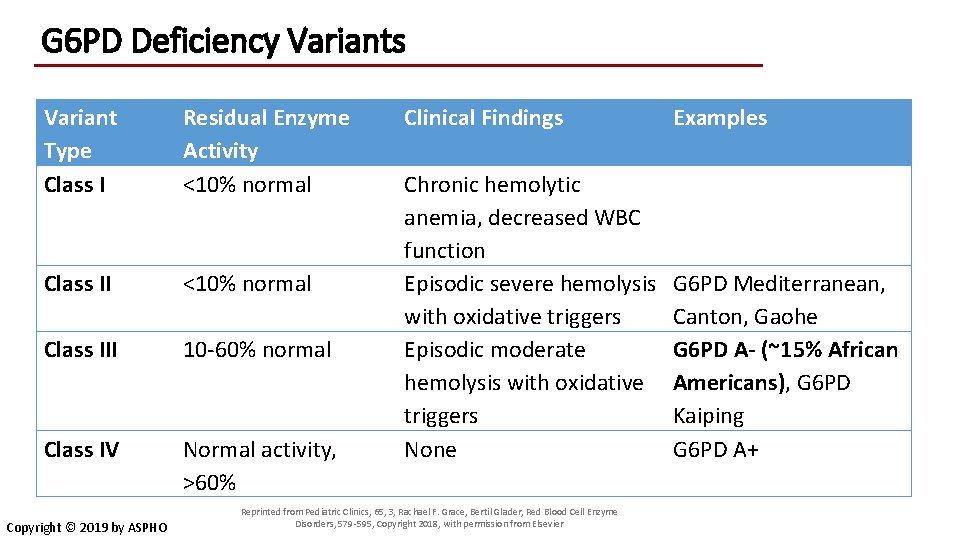
G 6 PD Deficiency Variants Variant Type Class I Residual Enzyme Activity <10% normal Class III 10 -60% normal Class IV Normal activity, >60% Copyright © 2019 by ASPHO Clinical Findings Examples Chronic hemolytic anemia, decreased WBC function Episodic severe hemolysis with oxidative triggers Episodic moderate hemolysis with oxidative triggers None G 6 PD Mediterranean, Canton, Gaohe G 6 PD A- (~15% African Americans), G 6 PD Kaiping G 6 PD A+ Reprinted from Pediatric Clinics, 65, 3, Rachael F. Grace, Bertil Glader, Red Blood Cell Enzyme Disorders, 579 -595, Copyright 2018, with permission from Elsevier
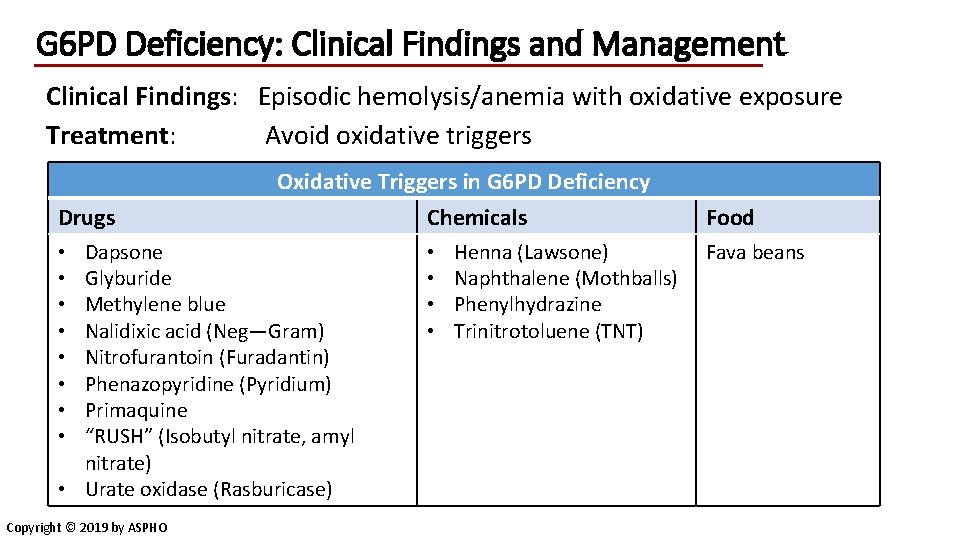
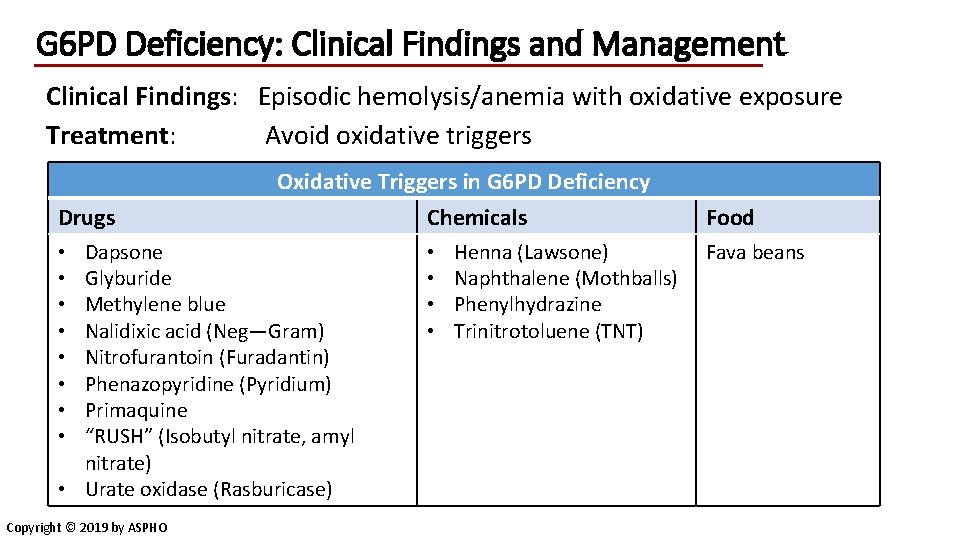
G 6 PD Deficiency: Clinical Findings and Management Clinical Findings: Episodic hemolysis/anemia with oxidative exposure Treatment: Avoid oxidative triggers Drugs Oxidative Triggers in G 6 PD Deficiency Chemicals Dapsone Glyburide Methylene blue Nalidixic acid (Neg—Gram) Nitrofurantoin (Furadantin) Phenazopyridine (Pyridium) Primaquine “RUSH” (Isobutyl nitrate, amyl nitrate) • Urate oxidase (Rasburicase) • • Copyright © 2019 by ASPHO • • Henna (Lawsone) Naphthalene (Mothballs) Phenylhydrazine Trinitrotoluene (TNT) Food Fava beans
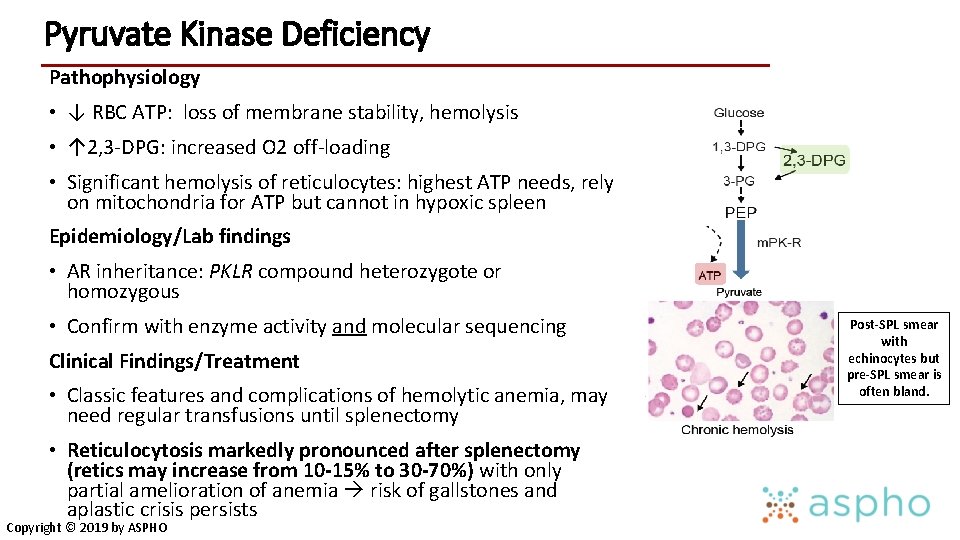
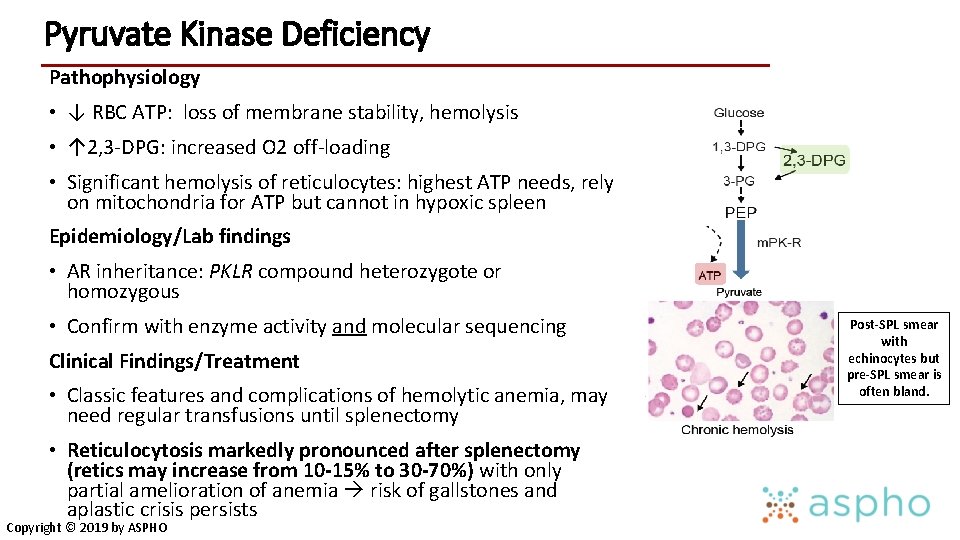
Pyruvate Kinase Deficiency Pathophysiology • ↓ RBC ATP: loss of membrane stability, hemolysis • ↑ 2, 3 -DPG: increased O 2 off-loading • Significant hemolysis of reticulocytes: highest ATP needs, rely on mitochondria for ATP but cannot in hypoxic spleen Epidemiology/Lab findings • AR inheritance: PKLR compound heterozygote or homozygous • Confirm with enzyme activity and molecular sequencing Clinical Findings/Treatment • Classic features and complications of hemolytic anemia, may need regular transfusions until splenectomy • Reticulocytosis markedly pronounced after splenectomy (retics may increase from 10 -15% to 30 -70%) with only partial amelioration of anemia risk of gallstones and aplastic crisis persists Copyright © 2019 by ASPHO Post-SPL smear with echinocytes but pre-SPL smear is often bland.
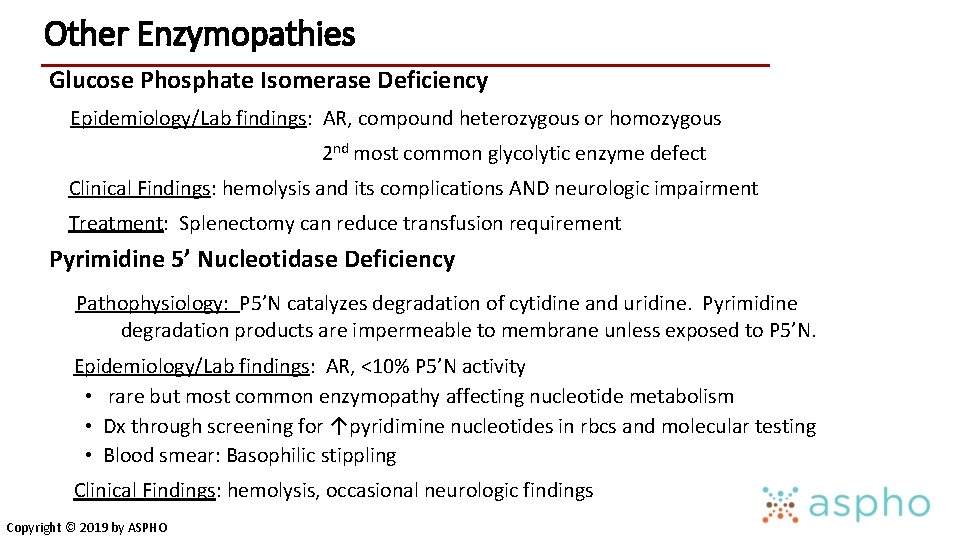
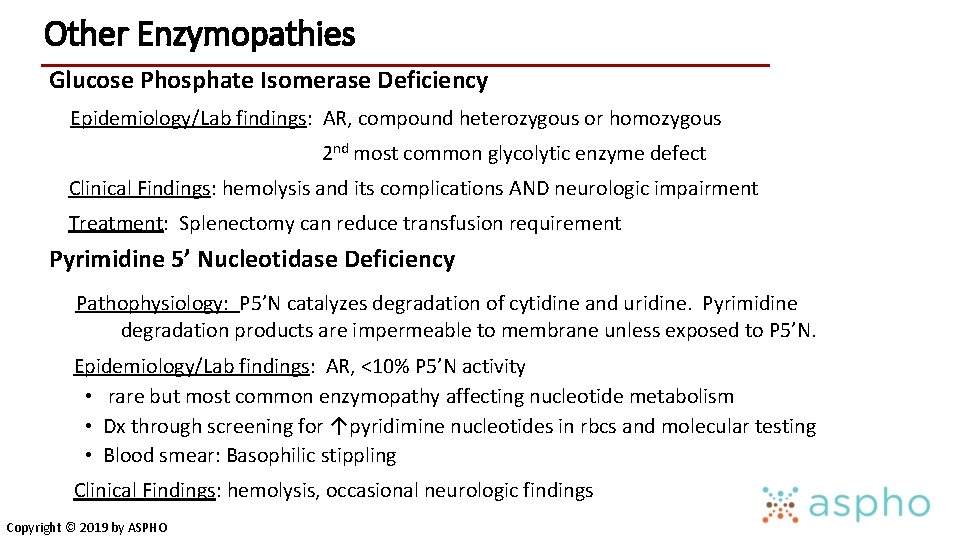
Other Enzymopathies Glucose Phosphate Isomerase Deficiency Epidemiology/Lab findings: AR, compound heterozygous or homozygous 2 nd most common glycolytic enzyme defect Clinical Findings: hemolysis and its complications AND neurologic impairment Treatment: Splenectomy can reduce transfusion requirement Pyrimidine 5’ Nucleotidase Deficiency Pathophysiology: P 5’N catalyzes degradation of cytidine and uridine. Pyrimidine degradation products are impermeable to membrane unless exposed to P 5’N. Epidemiology/Lab findings: AR, <10% P 5’N activity • rare but most common enzymopathy affecting nucleotide metabolism • Dx through screening for ↑pyridimine nucleotides in rbcs and molecular testing • Blood smear: Basophilic stippling Clinical Findings: hemolysis, occasional neurologic findings Copyright © 2019 by ASPHO
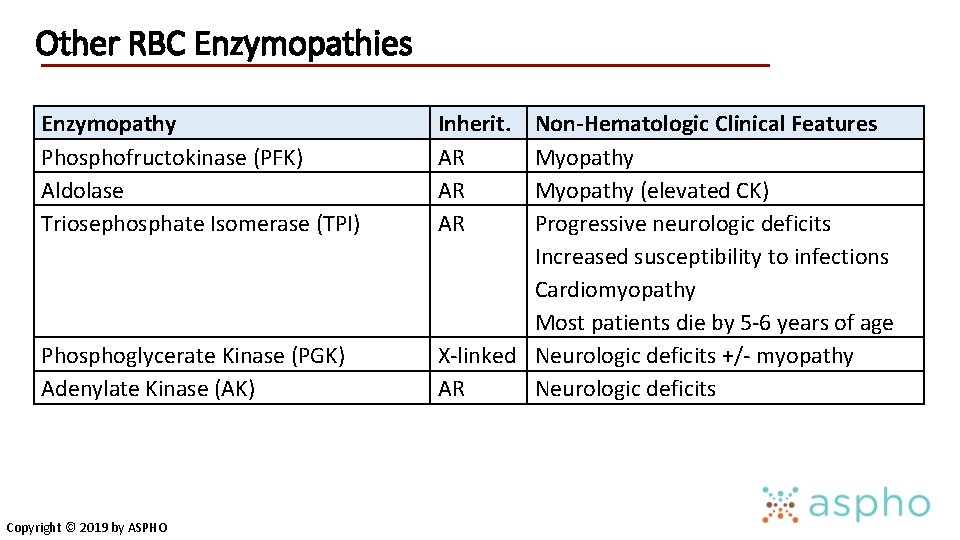
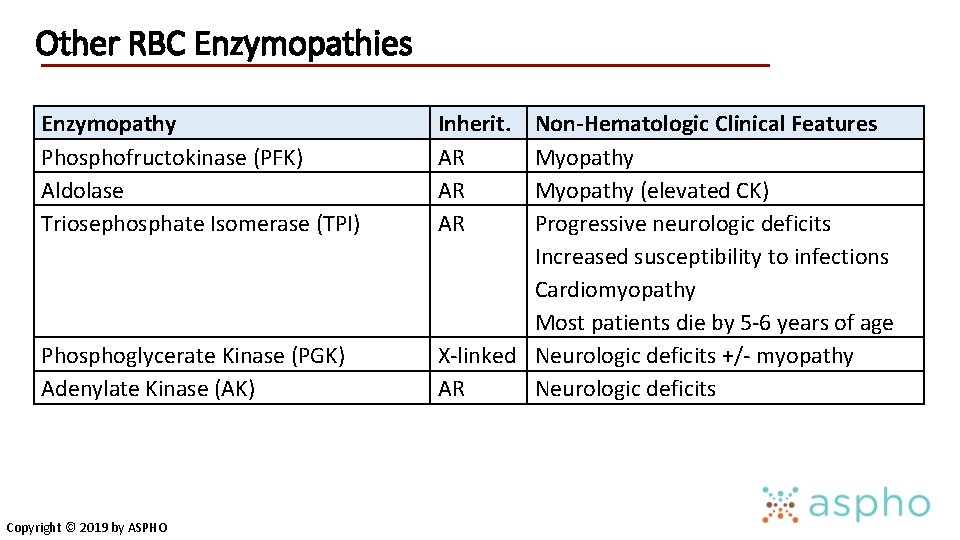
Other RBC Enzymopathies Enzymopathy Phosphofructokinase (PFK) Aldolase Triosephosphate Isomerase (TPI) Phosphoglycerate Kinase (PGK) Adenylate Kinase (AK) Copyright © 2019 by ASPHO Inherit. AR AR AR Non-Hematologic Clinical Features Myopathy (elevated CK) Progressive neurologic deficits Increased susceptibility to infections Cardiomyopathy Most patients die by 5 -6 years of age X-linked Neurologic deficits +/- myopathy AR Neurologic deficits
Methemoglobinemia Copyright © 2019 by ASPHO
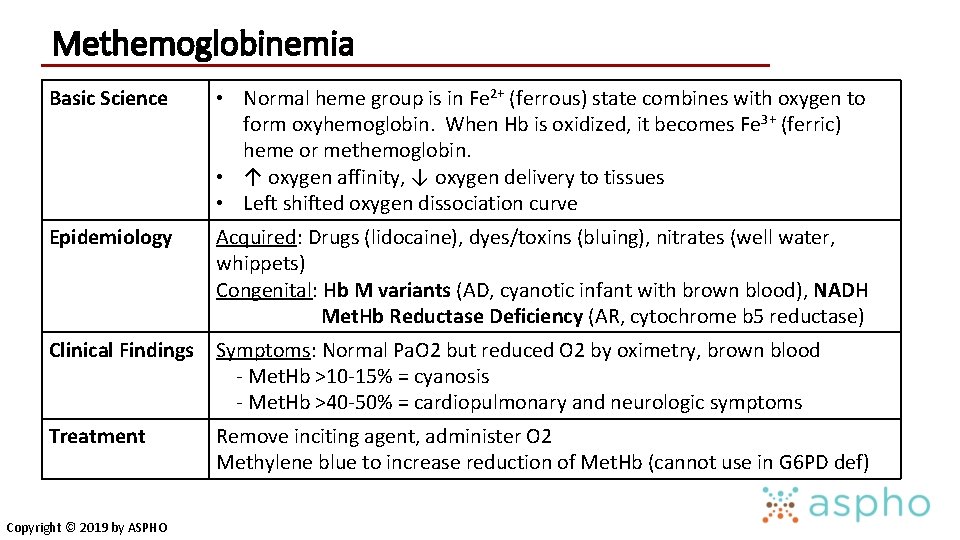
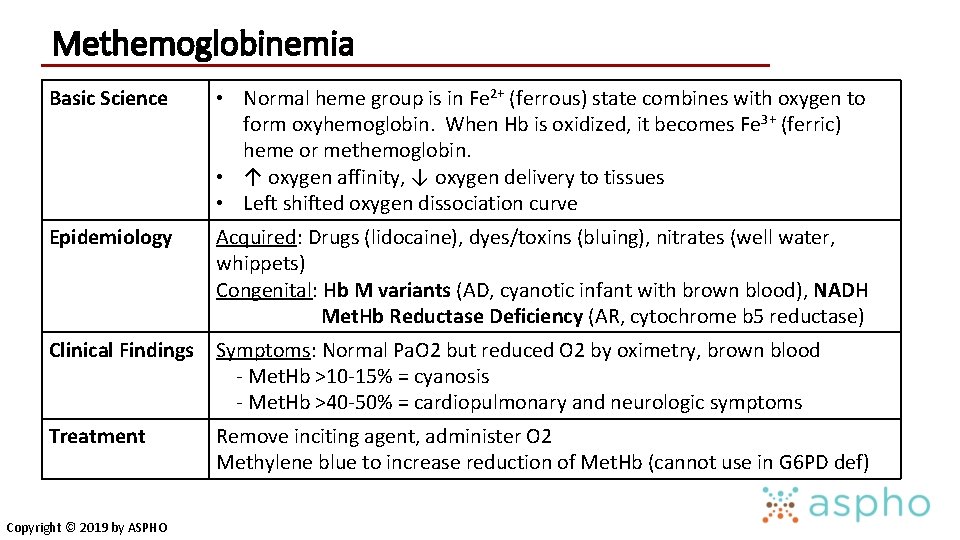
Methemoglobinemia Basic Science • Normal heme group is in Fe 2+ (ferrous) state combines with oxygen to form oxyhemoglobin. When Hb is oxidized, it becomes Fe 3+ (ferric) heme or methemoglobin. • ↑ oxygen affinity, ↓ oxygen delivery to tissues • Left shifted oxygen dissociation curve Epidemiology Acquired: Drugs (lidocaine), dyes/toxins (bluing), nitrates (well water, whippets) Congenital: Hb M variants (AD, cyanotic infant with brown blood), NADH Met. Hb Reductase Deficiency (AR, cytochrome b 5 reductase) Clinical Findings Symptoms: Normal Pa. O 2 but reduced O 2 by oximetry, brown blood - Met. Hb >10 -15% = cyanosis - Met. Hb >40 -50% = cardiopulmonary and neurologic symptoms Treatment Remove inciting agent, administer O 2 Methylene blue to increase reduction of Met. Hb (cannot use in G 6 PD def) Copyright © 2019 by ASPHO
Immune Mediated Hemolysis Copyright © 2019 by ASPHO
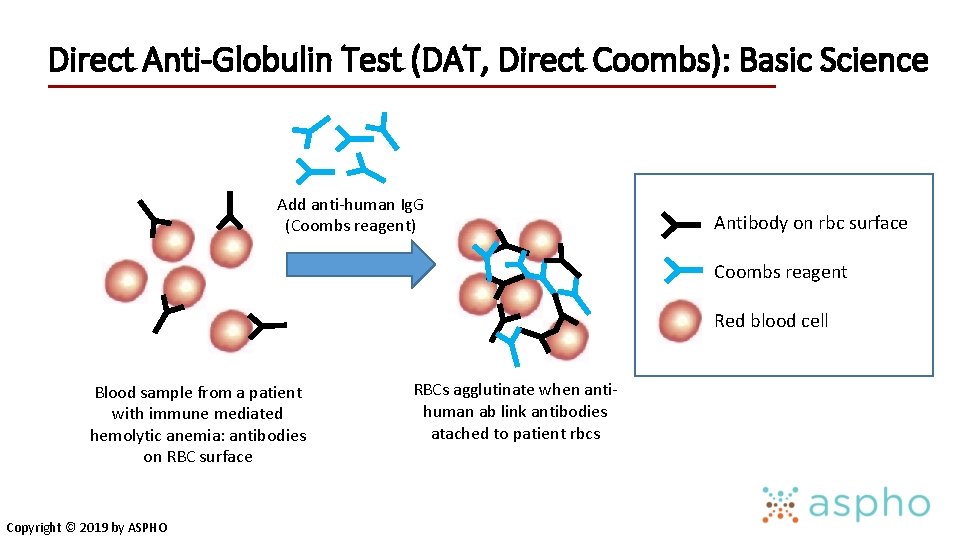
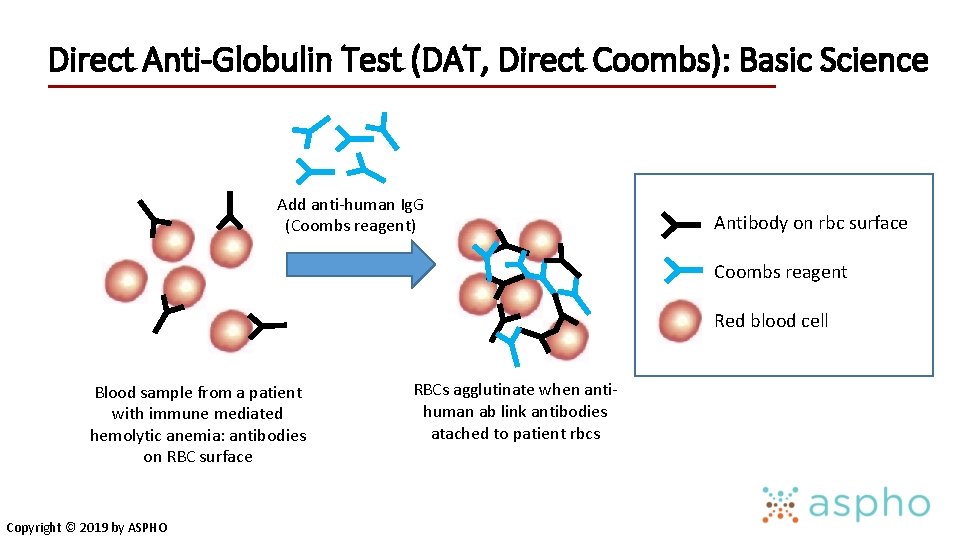
Direct Anti-Globulin Test (DAT, Direct Coombs): Basic Science Add anti-human Ig. G (Coombs reagent) Antibody on rbc surface Coombs reagent Red blood cell Blood sample from a patient with immune mediated hemolytic anemia: antibodies on RBC surface Copyright © 2019 by ASPHO RBCs agglutinate when antihuman ab link antibodies atached to patient rbcs
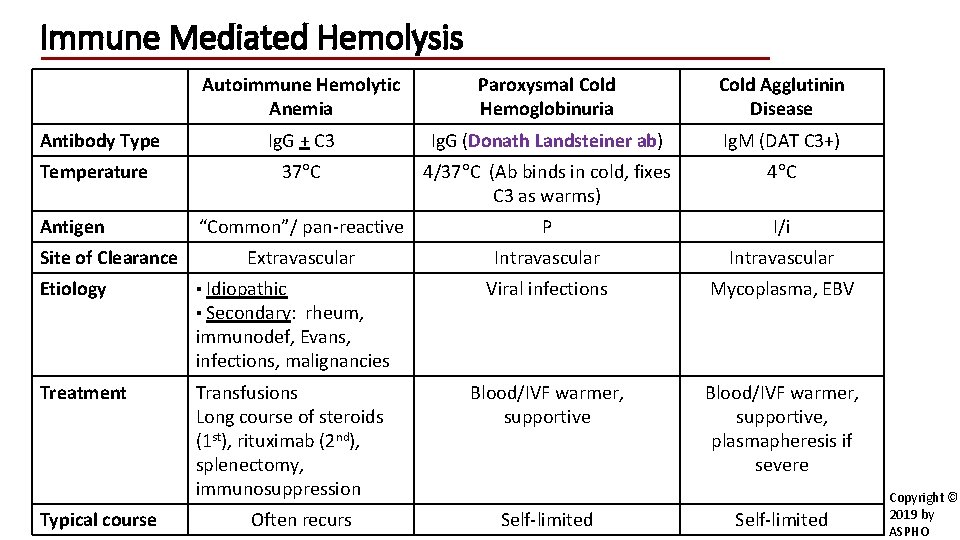
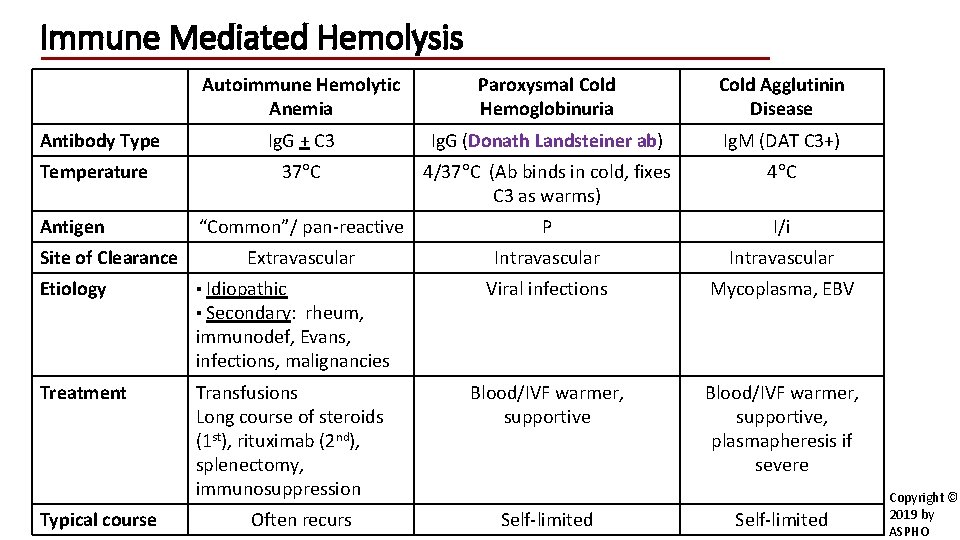
Immune Mediated Hemolysis Antibody Type Temperature Antigen Site of Clearance Etiology Autoimmune Hemolytic Anemia Paroxysmal Cold Hemoglobinuria Cold Agglutinin Disease Ig. G + C 3 Ig. G (Donath Landsteiner ab) Ig. M (DAT C 3+) 37 C 4/37 C (Ab binds in cold, fixes C 3 as warms) 4 C “Common”/ pan-reactive P I/i Extravascular Intravascular Viral infections Mycoplasma, EBV Blood/IVF warmer, supportive, plasmapheresis if severe ▪ Idiopathic ▪ Secondary: rheum, immunodef, Evans, infections, malignancies Treatment Typical course Transfusions Long course of steroids (1 st), rituximab (2 nd), splenectomy, immunosuppression Often recurs Self-limited Copyright © 2019 by ASPHO
Neonatal Alloimmune Hemolytic Anemia (Erythroblastosis Fetalis or HDN) Pathophysiology • Transplacental passage of maternal alloantibody directed against fetal antigens hemolysis of fetal RBCs: • May be due to Rh incompatibility, ABO, or other blood groups (Kell, Duffy, etc) • Feto-maternal hemorrhage leads to maternal immune response • May occur spontaneously or following amniocentesis, trauma, abortions, external cephalic version Clinical Findings • Anemia, hyperbilirubinemia, risk of hydrops fetalis, risk of kernicterus • Compounds effect of newborn Hb nadir Treatment • Exchange transfusion/phototherapy, RBC transfusions Copyright © 2019 by ASPHO
HDN: Rh Hemolytic Disease Pathophysiology: • Rh is the most immunogenic of blood groups • Hemolysis does not occur with first pregnancy • Alloimmunization does occur with first pregnancy Laboratory findings: • Infant’s Direct Antiglobulin Test (DAT) will be positive • Maternal antibody screen will be positive for a paternal antigen she lacks • Infant blood smear: NRBCs, polychromasia, not usually spherocytes Prevention: • Rh. Ig. G (Anti-D: Rho. Gam or Win. Rho) is given to Rh- mothers to prevent alloimmunization • Given at 28 weeks, at delivery, and after any invasive procedure (amniocentesis, chorionic villus sampling) Copyright © 2019 by ASPHO
HDN: ABO Incompatibility Pathophysiology: • Isohemagglutinins are naturally occurring antibodies • Typically Ig. M, but only Ig. G can cross placenta • Can occur in the first pregnancy • “ABO Set up” with Group O mom and Group A or B infant (20% of pregnancies, but only 2% affected by HDN) • DAT is usually positive (may be weak) Clinical Findings: • Infant peripheral smear: polychromasia, NRBCs, spherocytes • ABO antigens not expressed in early fetal RBCs, thus ABO HDN is not usually severe Copyright © 2019 by ASPHO
Mechanical Hemolysis (Fragmentation) Copyright © 2019 by ASPHO
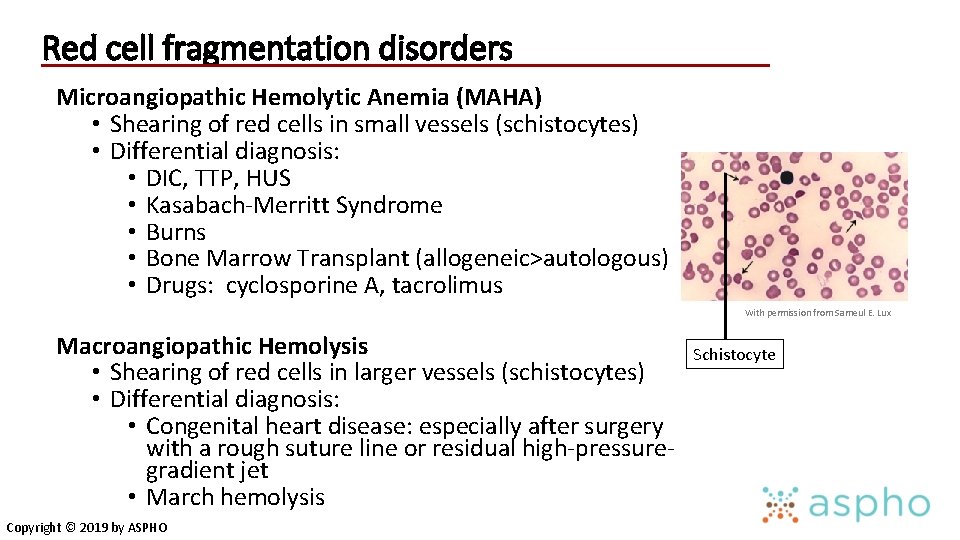
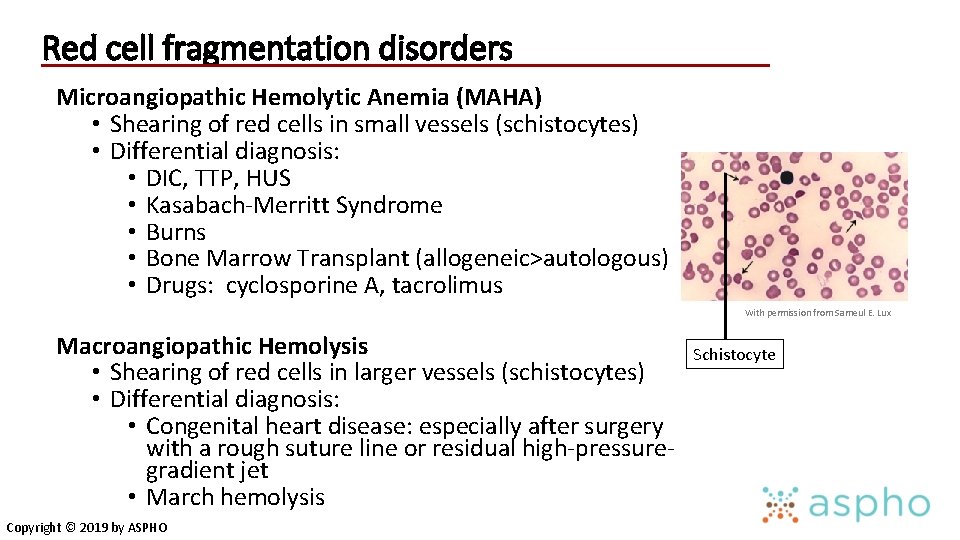
Red cell fragmentation disorders Microangiopathic Hemolytic Anemia (MAHA) • Shearing of red cells in small vessels (schistocytes) • Differential diagnosis: • DIC, TTP, HUS • Kasabach-Merritt Syndrome • Burns • Bone Marrow Transplant (allogeneic>autologous) • Drugs: cyclosporine A, tacrolimus With permission from Sameul E. Lux Macroangiopathic Hemolysis • Shearing of red cells in larger vessels (schistocytes) • Differential diagnosis: • Congenital heart disease: especially after surgery with a rough suture line or residual high-pressuregradient jet • March hemolysis Copyright © 2019 by ASPHO Schistocyte
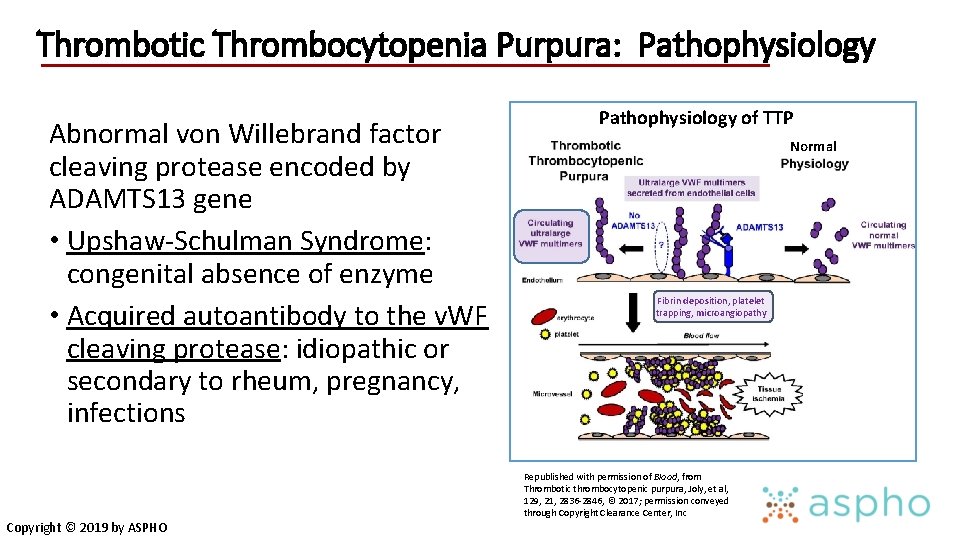
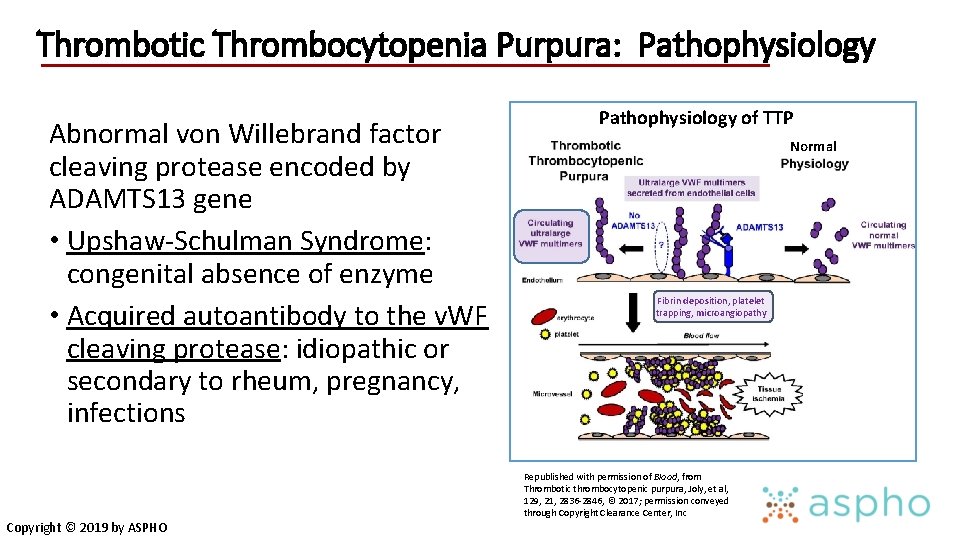
Thrombotic Thrombocytopenia Purpura: Pathophysiology Abnormal von Willebrand factor cleaving protease encoded by ADAMTS 13 gene • Upshaw-Schulman Syndrome: congenital absence of enzyme • Acquired autoantibody to the v. WF cleaving protease: idiopathic or secondary to rheum, pregnancy, infections Copyright © 2019 by ASPHO Pathophysiology of TTP Normal Fibrin deposition, platelet trapping, microangiopathy Republished with permission of Blood, from Thrombotic thrombocytopenic purpura, Joly, et al, 129, 21, 2836 -2846, © 2017; permission conveyed through Copyright Clearance Center, Inc
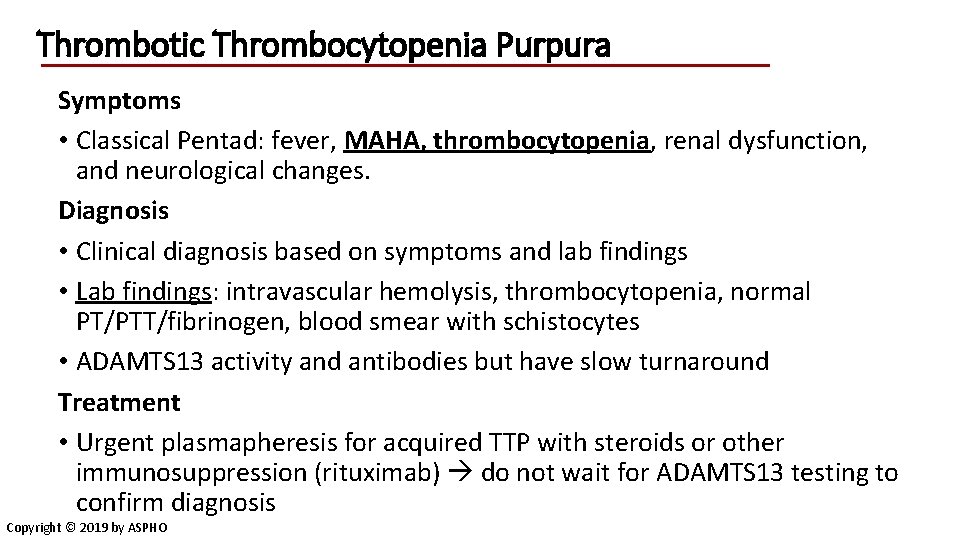
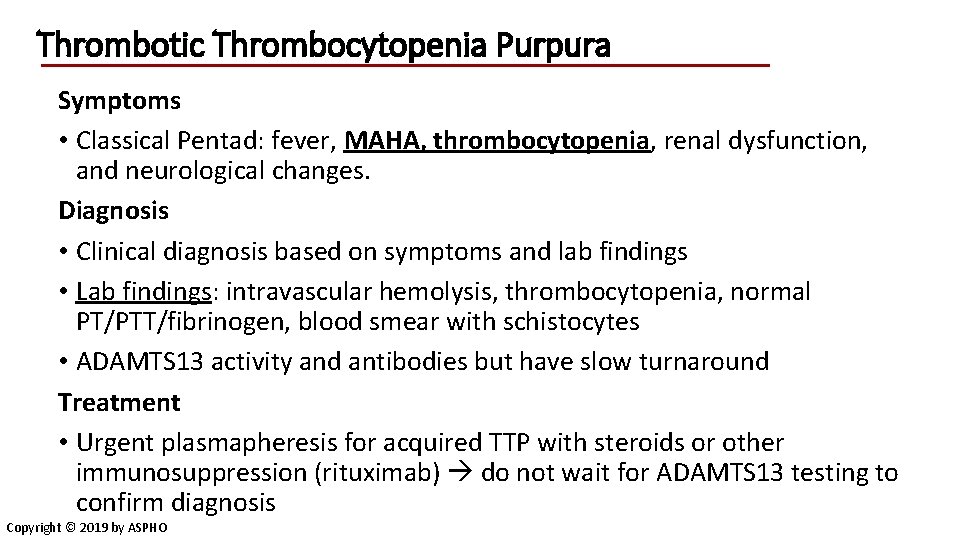
Thrombotic Thrombocytopenia Purpura Symptoms • Classical Pentad: fever, MAHA, thrombocytopenia, renal dysfunction, and neurological changes. Diagnosis • Clinical diagnosis based on symptoms and lab findings • Lab findings: intravascular hemolysis, thrombocytopenia, normal PT/PTT/fibrinogen, blood smear with schistocytes • ADAMTS 13 activity and antibodies but have slow turnaround Treatment • Urgent plasmapheresis for acquired TTP with steroids or other immunosuppression (rituximab) do not wait for ADAMTS 13 testing to confirm diagnosis Copyright © 2019 by ASPHO
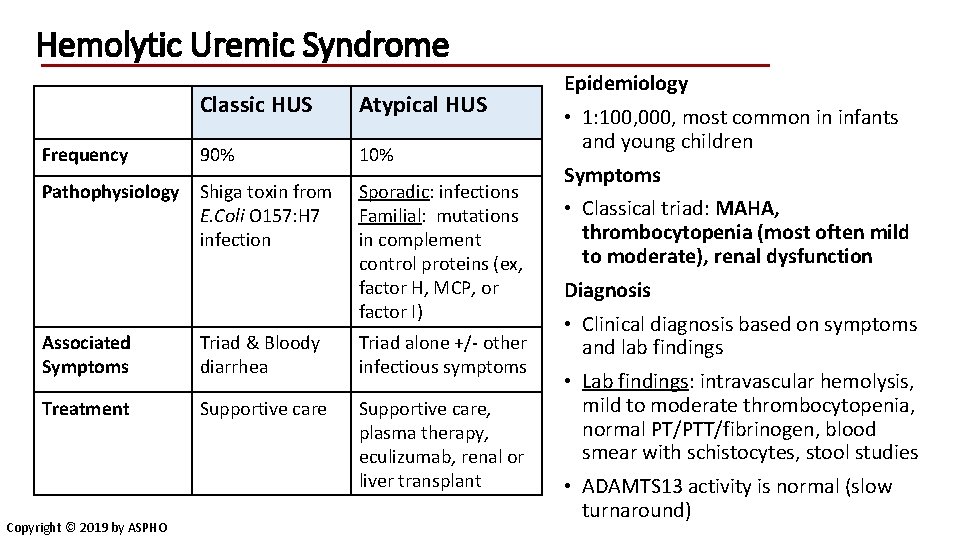
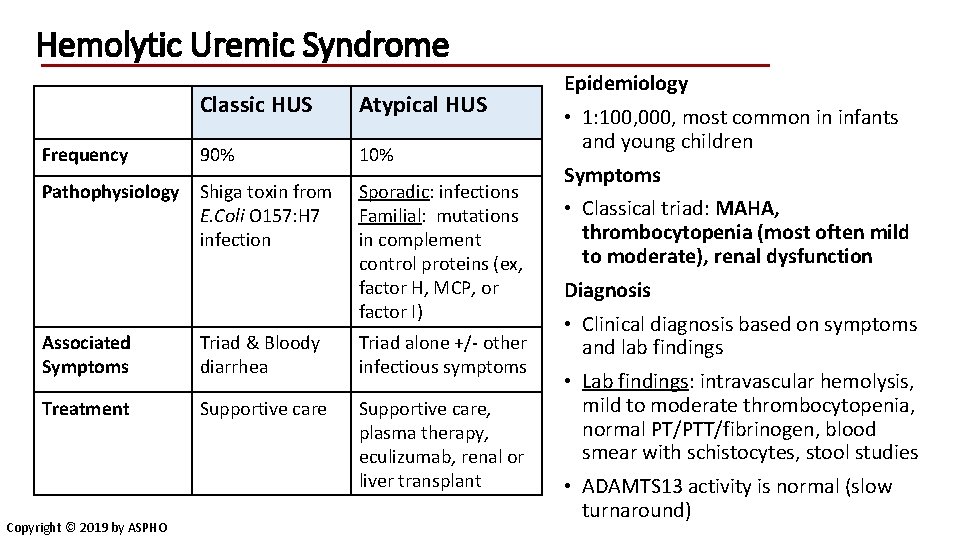
Hemolytic Uremic Syndrome Classic HUS Atypical HUS Frequency 90% 10% Pathophysiology Shiga toxin from E. Coli O 157: H 7 infection Sporadic: infections Familial: mutations in complement control proteins (ex, factor H, MCP, or factor I) Associated Symptoms Triad & Bloody diarrhea Triad alone +/- other infectious symptoms Treatment Supportive care, plasma therapy, eculizumab, renal or liver transplant Copyright © 2019 by ASPHO Epidemiology • 1: 100, 000, most common in infants and young children Symptoms • Classical triad: MAHA, thrombocytopenia (most often mild to moderate), renal dysfunction Diagnosis • Clinical diagnosis based on symptoms and lab findings • Lab findings: intravascular hemolysis, mild to moderate thrombocytopenia, normal PT/PTT/fibrinogen, blood smear with schistocytes, stool studies • ADAMTS 13 activity is normal (slow turnaround)
Other hemolytic anemias Copyright © 2019 by ASPHO
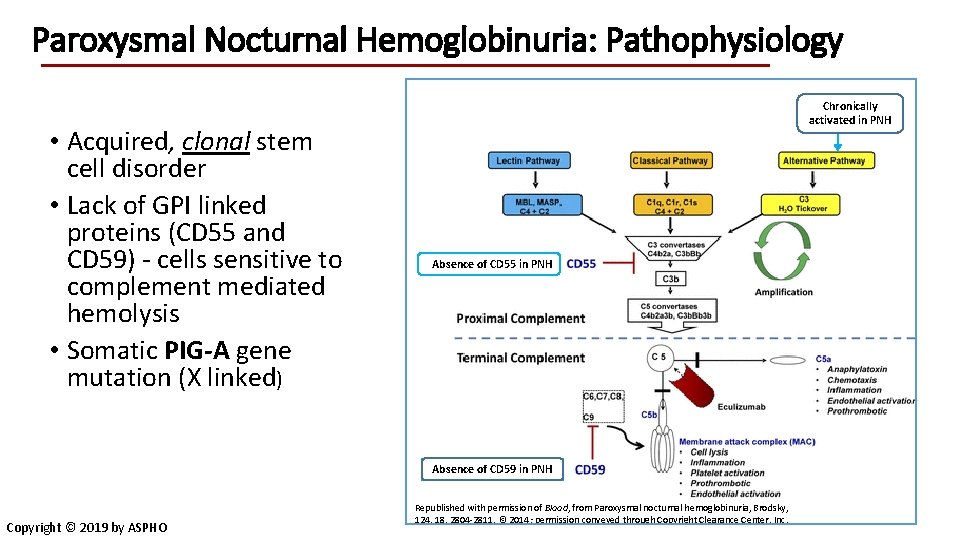
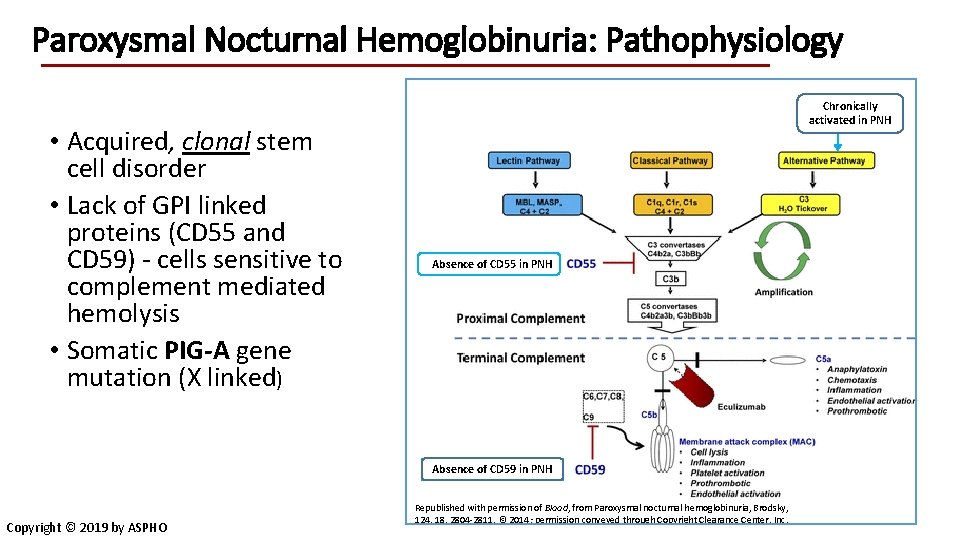
Paroxysmal Nocturnal Hemoglobinuria: Pathophysiology • Acquired, clonal stem cell disorder • Lack of GPI linked proteins (CD 55 and CD 59) - cells sensitive to complement mediated hemolysis • Somatic PIG-A gene mutation (X linked) Chronically activated in PNH Absence of CD 55 in PNH Absence of CD 59 in PNH Copyright © 2019 by ASPHO Republished with permission of Blood, from Paroxysmal nocturnal hemoglobinuria, Brodsky, 124, 18, 2804 -2811, © 2014; permission conveyed through Copyright Clearance Center, Inc.
Paroxysmal Nocturnal Hemoglobinuria Clinical Symptoms • Hemoglobinuria due to intravascular hemolysis nitric oxide clearance • Other symptoms include abdominal pain, dysphagia, erectile dysfunction • Thrombosis, particularly in intra-abdominal and cerebral veins • Bone marrow failure/PNH clones • Increased risk of developing leukemia Lab Findings • Flow cytometry for CD 55 and/or CD 59 and leukocyte PI-linked proteins Treatment • Eculizumab to block complement-mediated lysis Copyright © 2019 by ASPHO
Drug-induced hemolytic anemia • Often immunological • Haptenized red cell proteins (penicillins) • Bystander immunological -antibodies to drugs adsorbed to RBC • Often drug metabolites, not parent drug • Generally detected as drug-dependent DAT • Distinguish from immunomodulatory drugs which cause AIHA and are independent of antibody (tacrolimus, fludarabine) • Distinguish from non-specific + DAT after IVIG • Much less common than drug related ITP or neutropenia Copyright © 2019 by ASPHO
Toxin Associated hemolysis Clostridium sepsis – Phospholipases result in red cell membrane loss and spherocytes – Occurs in ill patients – smear or automated cell count findings consistent with spherocytes may be the first clue for an ICU patient with ischemic injuries to bowel or extremities Brown recluse spider bite - Some snake and other venoms due to phospholipases Wilson’s disease – Impairment of cellular copper transport resulting in copper toxicity – Findings: unexplained liver disease and new hemolysis – Diagnosis: Serum copper and ceruloplasmin levels Burns – may have acquired spherocytic or HPP-like anemia Copyright © 2019 by ASPHO With permission from Dr. Samuel E. Lux
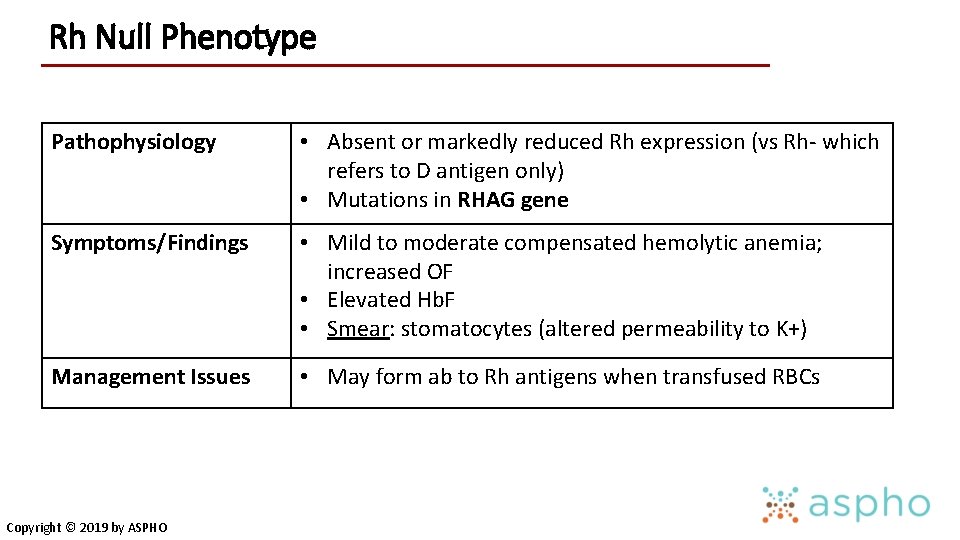
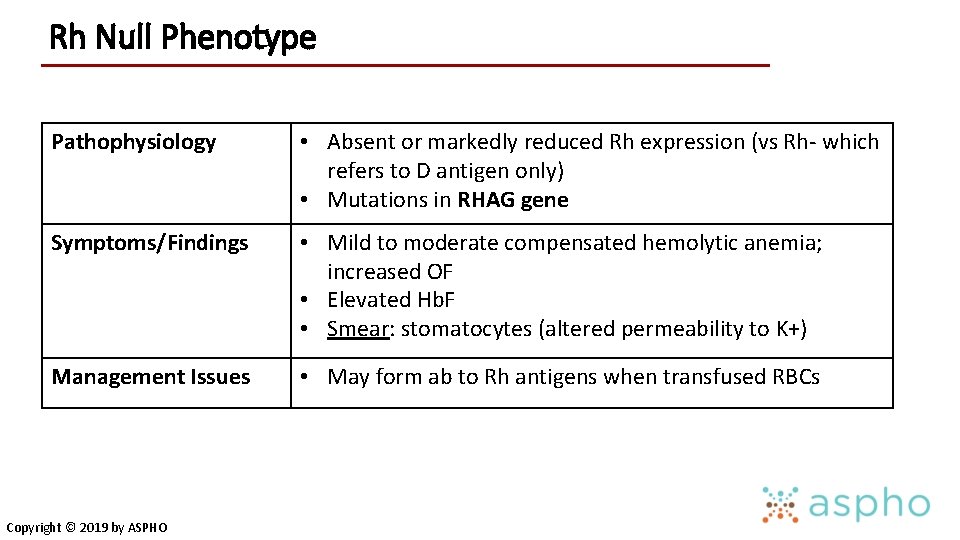
Rh Null Phenotype Pathophysiology • Absent or markedly reduced Rh expression (vs Rh- which refers to D antigen only) • Mutations in RHAG gene Symptoms/Findings • Mild to moderate compensated hemolytic anemia; increased OF • Elevated Hb. F • Smear: stomatocytes (altered permeability to K+) Management Issues • May form ab to Rh antigens when transfused RBCs Copyright © 2019 by ASPHO
Summary - Hemolytic Anemia • Hemolytic anemias share many general features including clinical symptoms, lab findings, and complications • Correct diagnosis is critical for monitoring and treatment • Red cell morphology is key to the diagnostic approach • Genetic testing has an increasing role in congenital RBC disorders but often needs to be combined with functional testing • Many of the acquired hemolytic anemias can be life-threatening and have better outcomes with early recognition and treatment Questions? Rachael. Grace@childrens. harvard. edu Copyright © 2019 by ASPHO
 Causes of hemolysis
Causes of hemolysis Hemolytic anemia signs and symptoms
Hemolytic anemia signs and symptoms Acquired hemolytic anemia
Acquired hemolytic anemia Sanctifying grace
Sanctifying grace Grace grace to the mountain
Grace grace to the mountain Once in grace always in grace
Once in grace always in grace Clasificacion morfologica de la anemia
Clasificacion morfologica de la anemia Megaloblastic anemia laboratory findings
Megaloblastic anemia laboratory findings Sideremia baja
Sideremia baja Clasificación morfológica de las anemias
Clasificación morfológica de las anemias Classificacao das anemias
Classificacao das anemias Ciclo da bilirrubina direta e indireta
Ciclo da bilirrubina direta e indireta Anemia clasificación
Anemia clasificación Anemias hemolíticas
Anemias hemolíticas Anemias premedulares
Anemias premedulares Citocromos
Citocromos Lft normal range
Lft normal range Rachael blansett
Rachael blansett Rachael huntley
Rachael huntley Rachael blansett
Rachael blansett Rachael kessler
Rachael kessler Rachael edgerly
Rachael edgerly Rachael hale
Rachael hale Oh quel beau jour devant ta face
Oh quel beau jour devant ta face Rachael trotman
Rachael trotman Nombre comme le sable des plages
Nombre comme le sable des plages Rachael
Rachael Tom hurndall
Tom hurndall Rachael drazan
Rachael drazan Rachael scherer
Rachael scherer Hemolytic transfusion reaction
Hemolytic transfusion reaction Treatment for hemolytic anemia
Treatment for hemolytic anemia Intravascular hemolytic anemia
Intravascular hemolytic anemia Hemolysis symptoms
Hemolysis symptoms Types of hemolytic anemia
Types of hemolytic anemia Why splenomegaly in hemolytic anemia
Why splenomegaly in hemolytic anemia Obstructive jaundice vs hemolytic jaundice
Obstructive jaundice vs hemolytic jaundice Extrinsic hemolytic anemia
Extrinsic hemolytic anemia Why splenomegaly in hemolytic anemia
Why splenomegaly in hemolytic anemia Hemolytic disease of the newborn
Hemolytic disease of the newborn Complication of blood transfusion
Complication of blood transfusion Direct hyperbilirubinemia causes
Direct hyperbilirubinemia causes Hemolytic anemia labs
Hemolytic anemia labs Robert koch institute
Robert koch institute Fresh frozen plasma contents
Fresh frozen plasma contents Febrile nonhemolytic transfusion reaction
Febrile nonhemolytic transfusion reaction Hemolytic facies
Hemolytic facies Pathophysiology of anemia
Pathophysiology of anemia Rbc anomalies
Rbc anomalies Ttn vs rds cxr
Ttn vs rds cxr Congenital pneumonia
Congenital pneumonia Picior equin definitie
Picior equin definitie Trabeculodysgenesis meaning
Trabeculodysgenesis meaning Differential cyanosis
Differential cyanosis Congenital rubella syndrome
Congenital rubella syndrome Congenital malformations
Congenital malformations Congenital voice disorders
Congenital voice disorders