PreICU training CV CR AMI EKG cardiac enzyme



- Slides: 55
Pre-ICU training CV CR 蕭智忠
AMI • EKG, cardiac enzyme serially check , CXR • Aspirin, Plavix, Enoxaparin , IIB -IIIa , statin , • Nitrite , ACEI , B-blocker and diuretic 視情形 給與 • Heart echo – 值班時注意AMI的多種complication 如 VSD , acute MR , cardiac rupture, cardiac tamponade, 如有懷疑應call CR 施行緊急心臟超音波或pericardiocentesis with drainage • Intervention的時機 – AMI病人如有unstable hemodynamic status , on going chest pain , new EKG change 應call duty CV CR 評估是否 放置IABP or 施行緊急心導管
CHF with pulmonary edema • • • Nitrate + Diuretics and keep I/O negative ACEI O 2 Correct hypoalbuminemia Swan-ganz monitor
TPM or PPM
Indication • Bradycardia with symptom and refractory to medication – 病人如有bradycardia , high degree AV block with unstable BP 應放置TCP 並call duty CR 評估是否放置TPM – 病人放置PPM或曾施行CVP puncture , 如 Ablation 應f/u CXR 注意有無 pneumothorax, 位置是否正確, 有無移位並f/u EKG注意是否有相應的變化
Swan-ganz
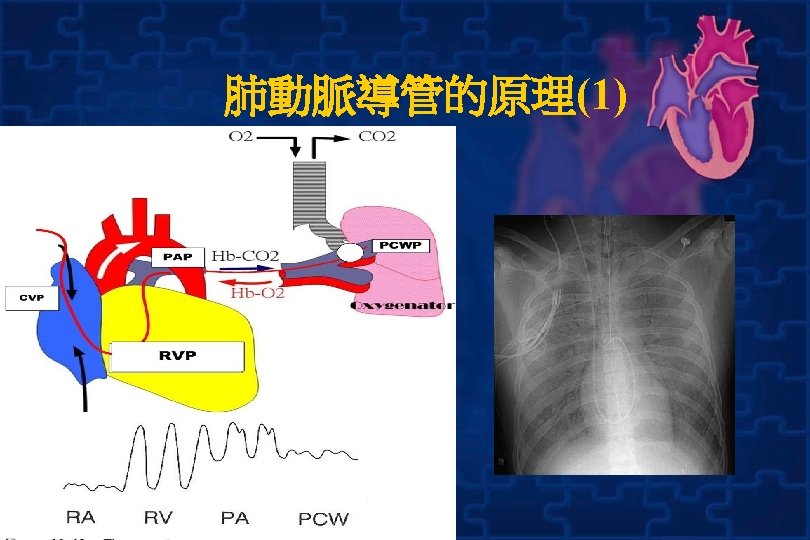
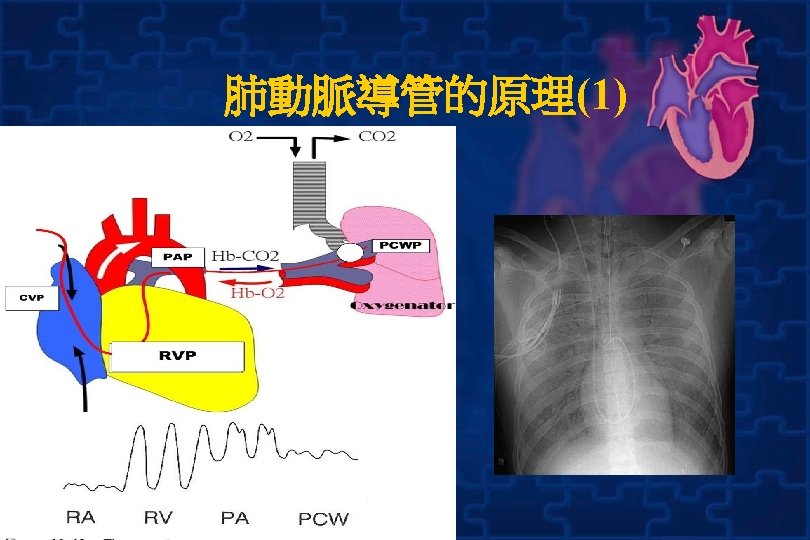
Indication • Shock D/D – Pulmonary artery catheter 可幫助鑑別 cardiogenic or no-cardogenic shock , 區 別pulmonary edema or ARDS, 病人如有上述 情形應考慮置放Pulmonary artery catheter 以為鑑別, 亦可當作治療指標 • Monitor fluid and C/O and adjust medication • Swan-Gan會開立固定測量時間(q 6 h, q 8 h), 但如果病情有需要即應及時測量

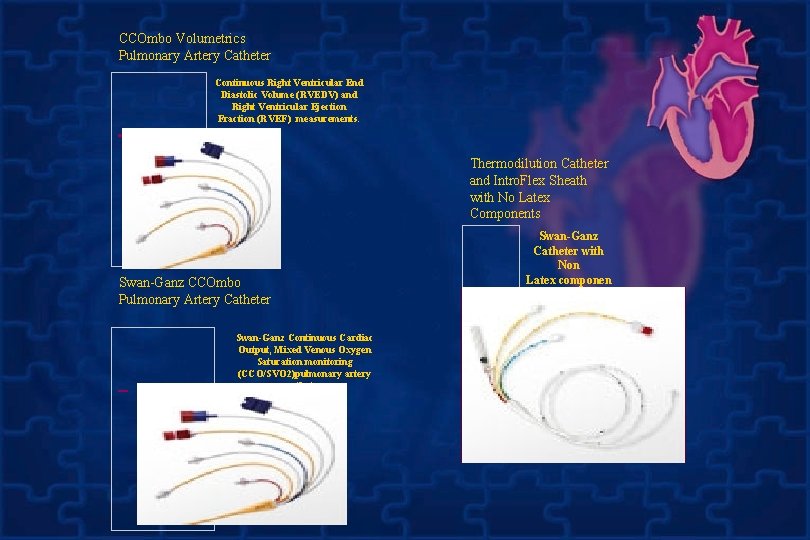
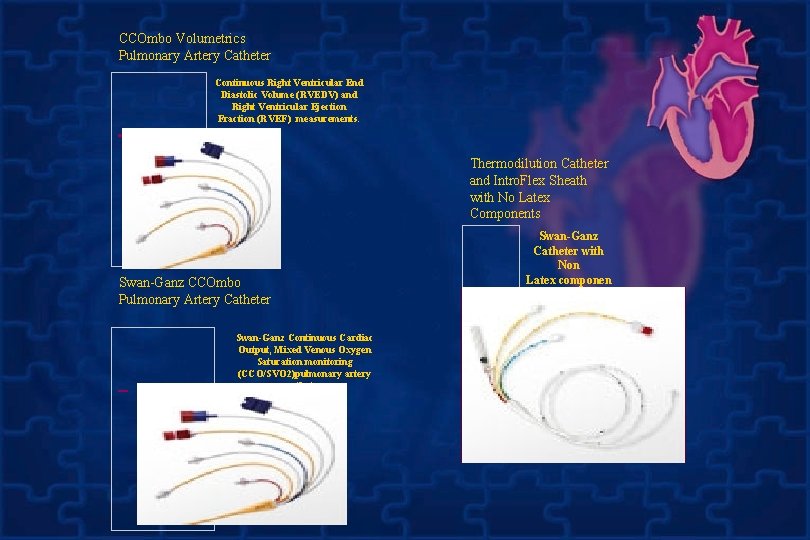
CCOmbo Volumetrics Pulmonary Artery Catheter Continuous Right Ventricular End Diastolic Volume (RVEDV) and Right Ventricular Ejection Fraction (RVEF) measurements. Thermodilution Catheter and Intro. Flex Sheath with No Latex Components Swan-Ganz CCOmbo Pulmonary Artery Catheter Swan-Ganz Continuous Cardiac Output, Mixed Venous Oxygen Saturation monitoring (CCO/SVO 2)pulmonary artery catheter Swan-Ganz Catheter with Non Latex componen ts for assessment of right heart pressures, cardiac output
Indications • Diagnostic – – – – – Diagnosis of shock states Differentiation of high- versus low-pressure pulmonary edema Diagnosis of primary pulmonary hypertension (PPH) Diagnosis of valvular disease, intracardiac shunts, cardiac tamponade, and pulmonary embolus (PE) Monitoring and management of complicated AMI Assessing hemodynamic response to therapies Management of multiorgan system failure and/or severe burns Management of hemodynamic instability after cardiac surgery Assessment of response to treatment in patients with PPH • Therapeutic - Aspiration of air emboli
Contraindications • Tricuspid or pulmonary valve mechanical prosthesis • Right heart mass (thrombus and/or tumor) • Tricuspid or pulmonary valve endocarditis
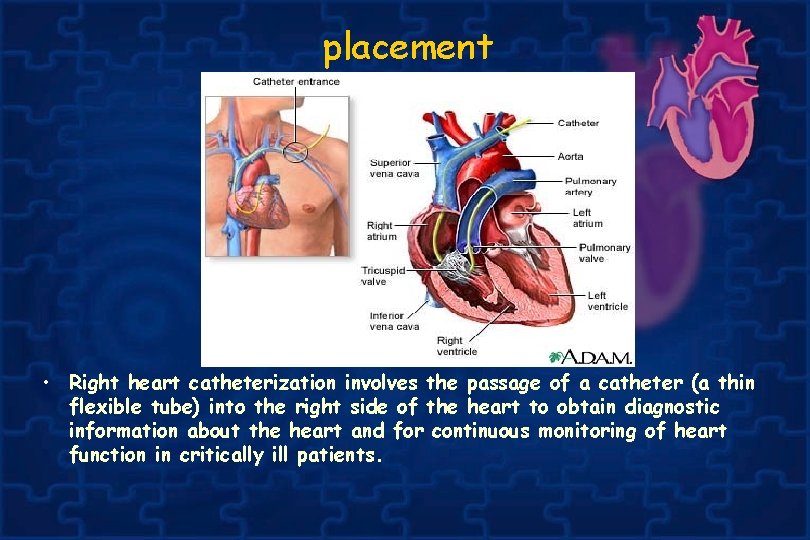
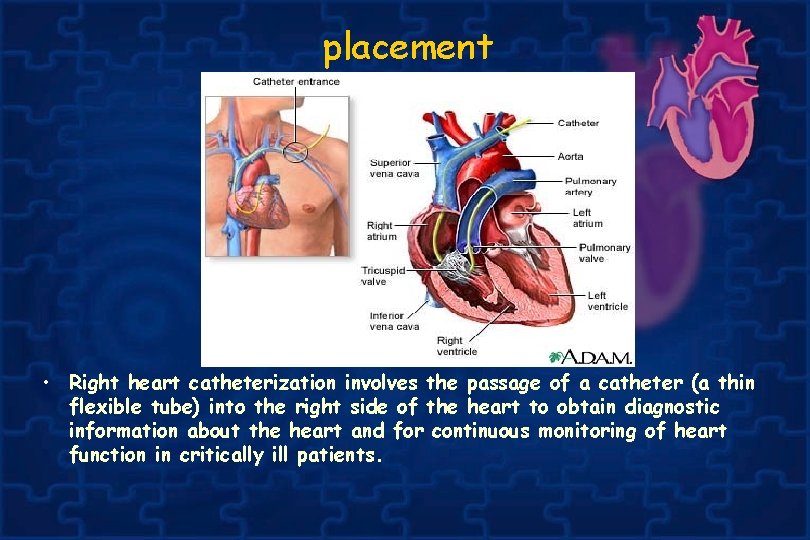
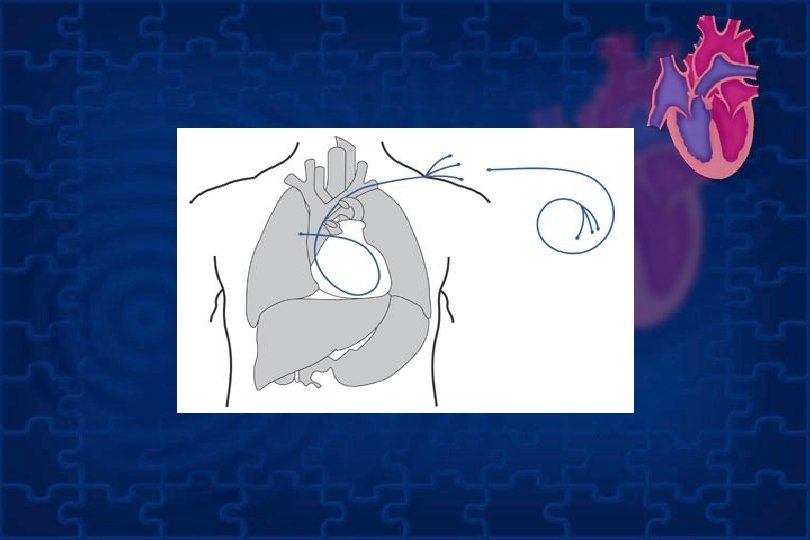
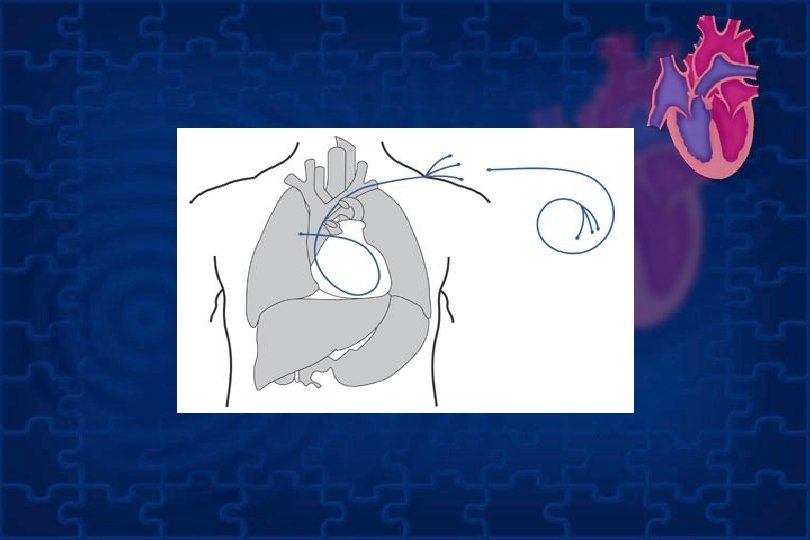
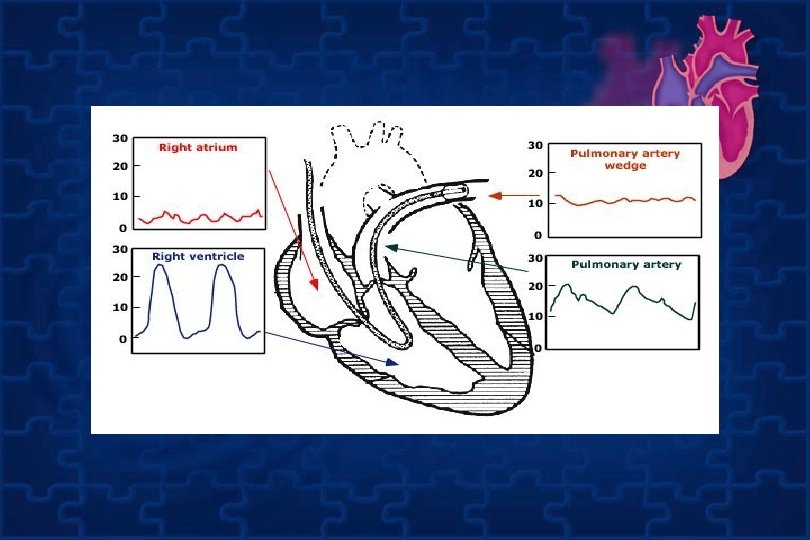
placement • Right heart catheterization involves the passage of a catheter (a thin flexible tube) into the right side of the heart to obtain diagnostic information about the heart and for continuous monitoring of heart function in critically ill patients.
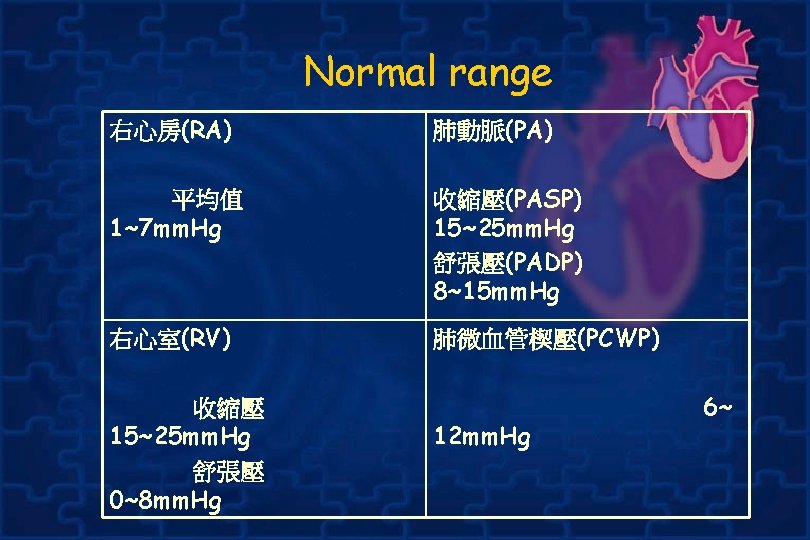
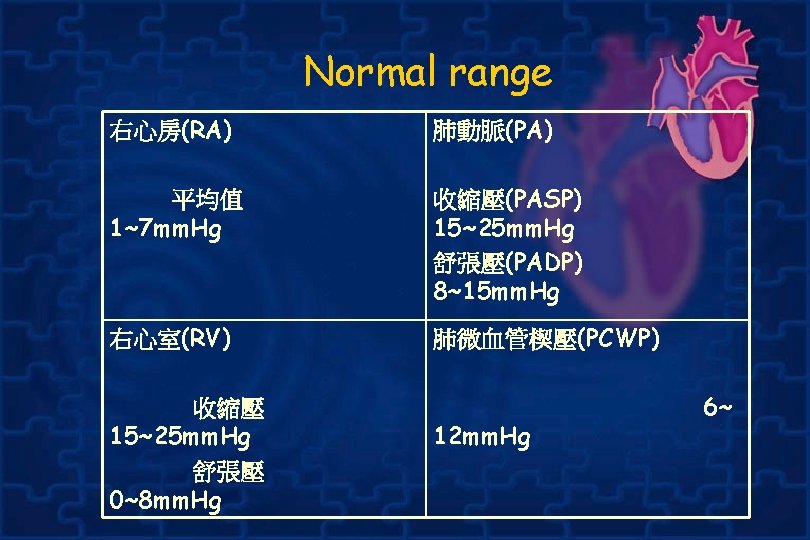
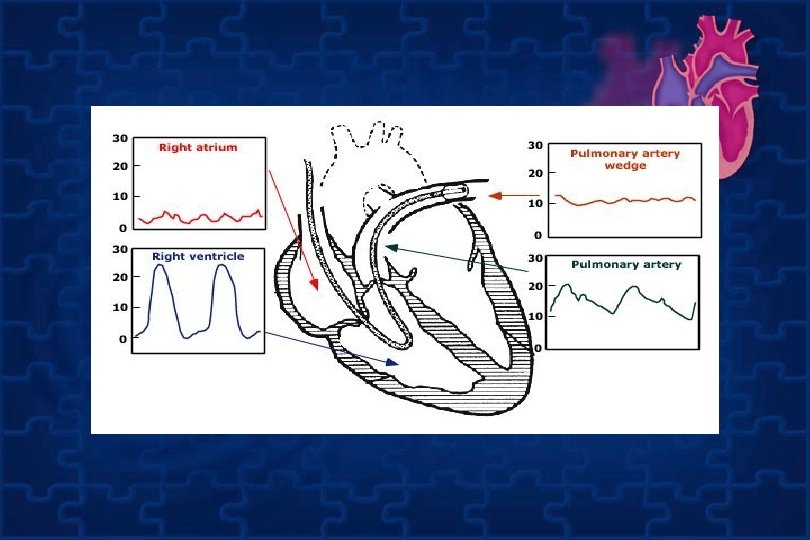
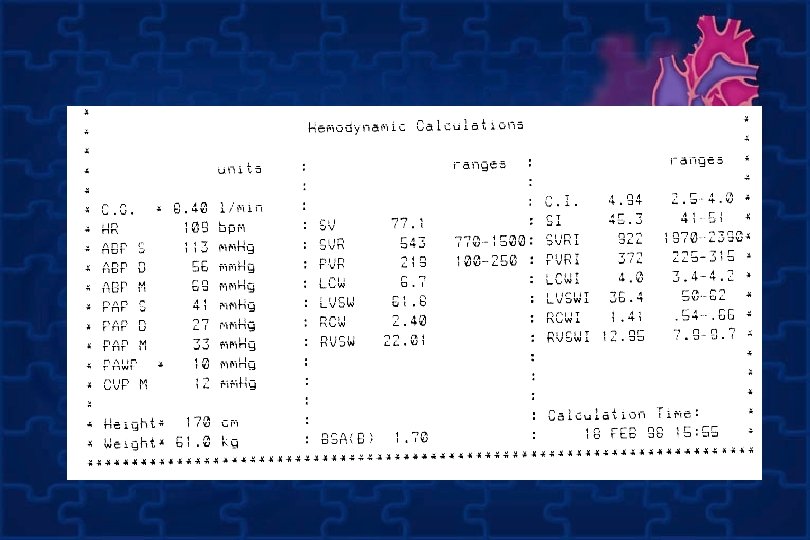
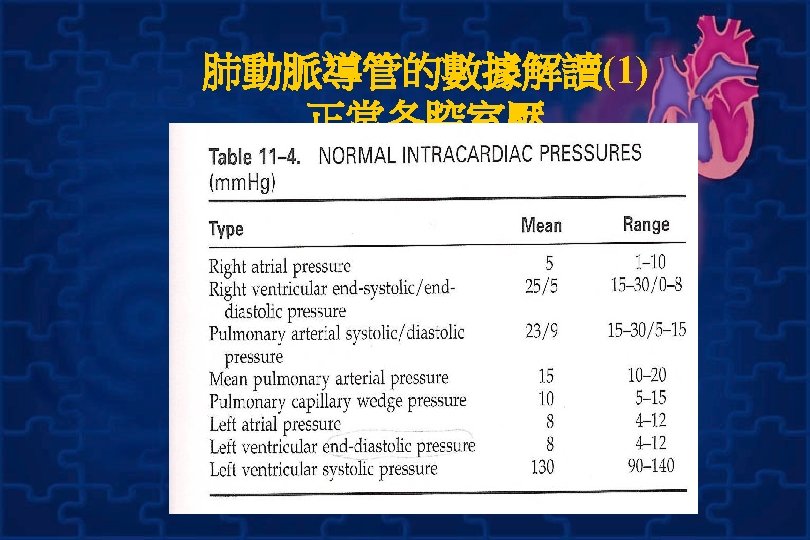
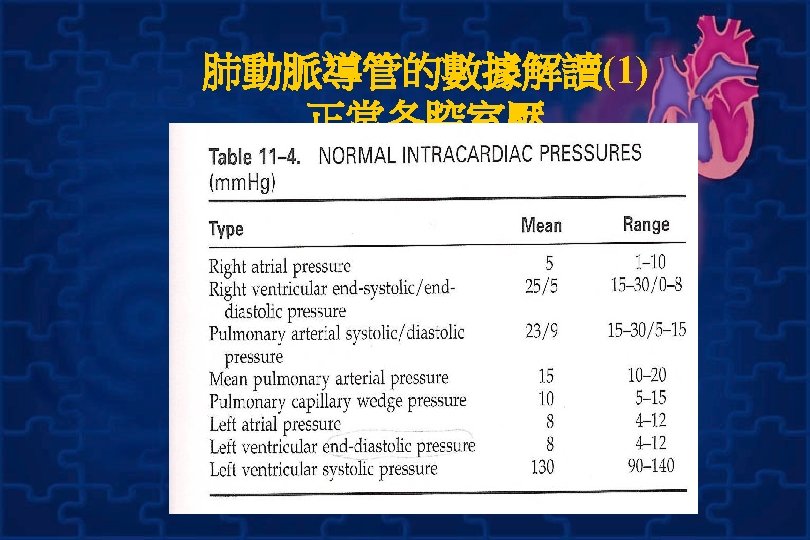
Normal range 右心房(RA) 肺動脈(PA) 平均值 1~7 mm. Hg 收縮壓(PASP) 15~25 mm. Hg 舒張壓(PADP) 8~15 mm. Hg 右心室(RV) 肺微血管楔壓(PCWP) 收縮壓 15~25 mm. Hg 舒張壓 0~8 mm. Hg 12 mm. Hg 6~

Complications from the technique • • • vascular damage hematoma infection pulmonary thrombosis kinking of catheter premature atrial contractions premature ventricular contractions ventricular fibrillation complete heart arrest right bundle branch block 發生於導管頂端通過右心房 時
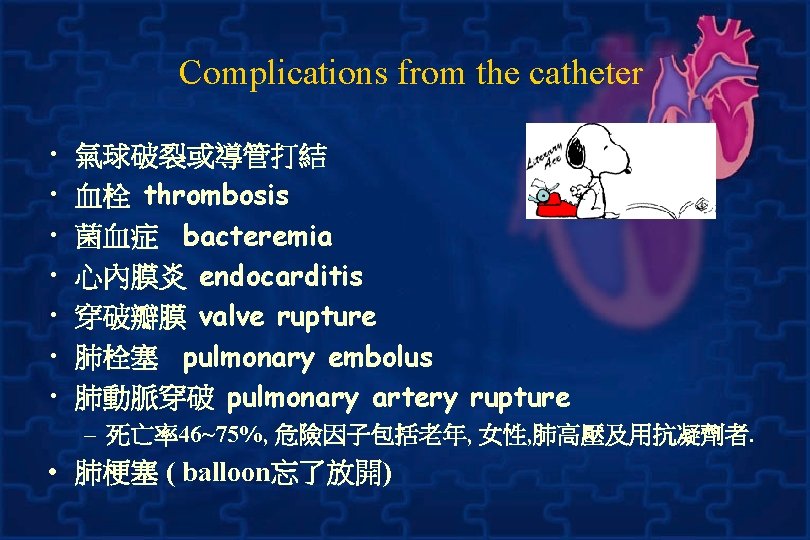
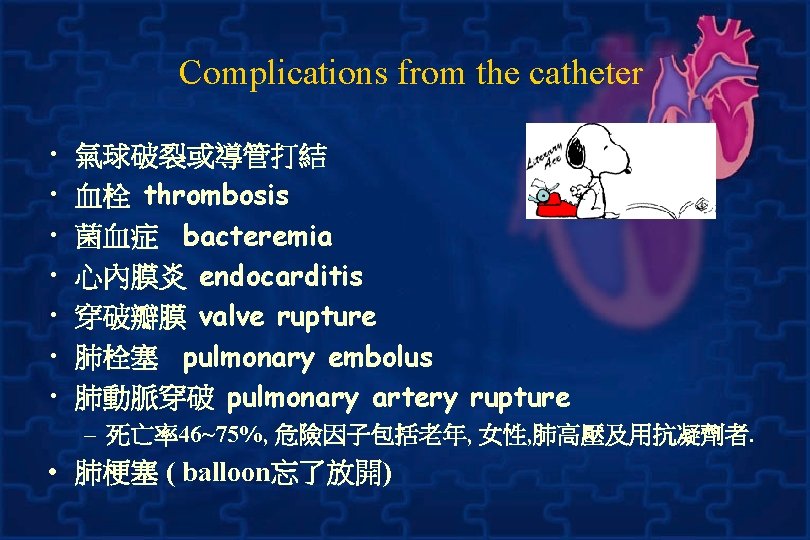
Complications from the catheter • • 氣球破裂或導管打結 血栓 thrombosis 菌血症 bacteremia 心內膜炎 endocarditis 穿破瓣膜 valve rupture 肺栓塞 pulmonary embolus 肺動脈穿破 pulmonary artery rupture – 死亡率46~75%, 危險因子包括老年, 女性, 肺高壓及用抗凝劑者. • 肺梗塞 ( balloon忘了放開)
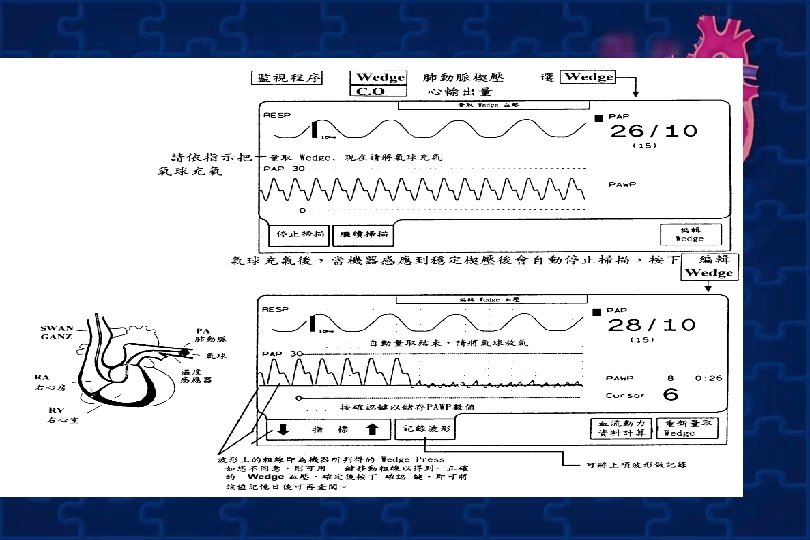
7. Recorder RAP、RVP、PAP、PCWP 波形及記錄 數值 8. 9. Record PCWP waveform 後,將 balloon off時 即出現PA waveform,當 balloon on 時出現 PAWP waveform sheath與無菌塑膠套前端銜接處轉至mark "O"予lock 10. 消毒傷口,並固定導管位置,照X-ray
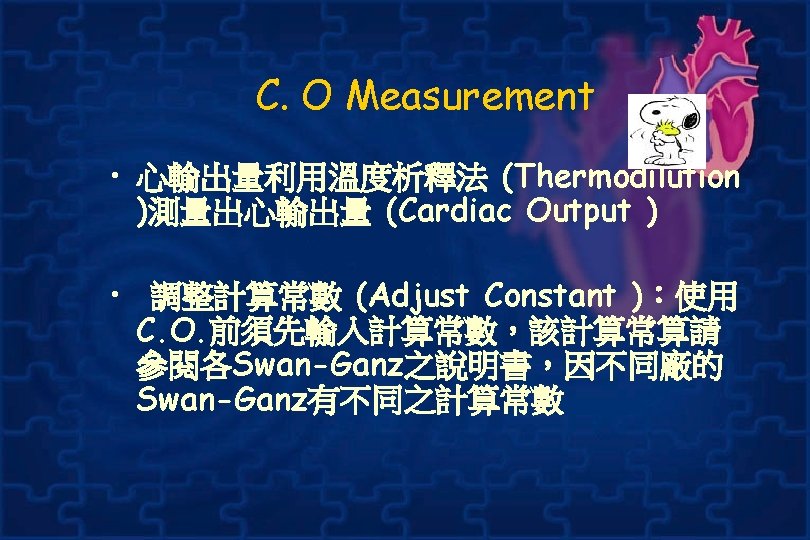
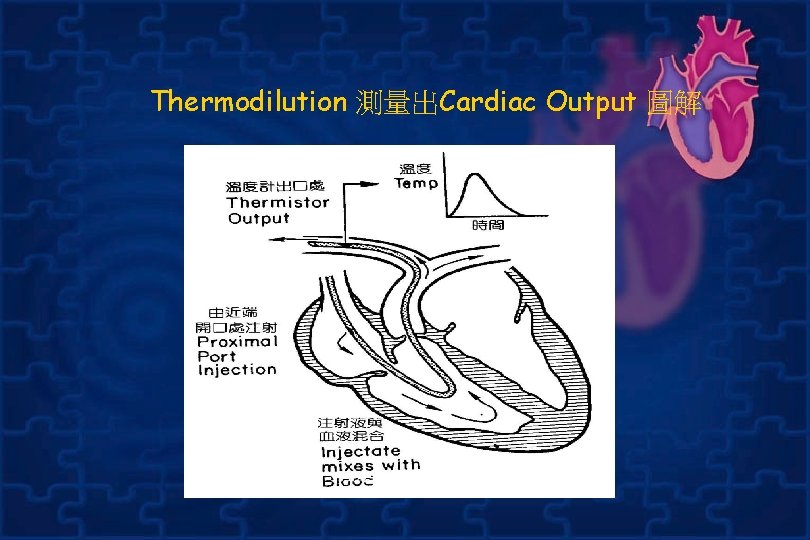
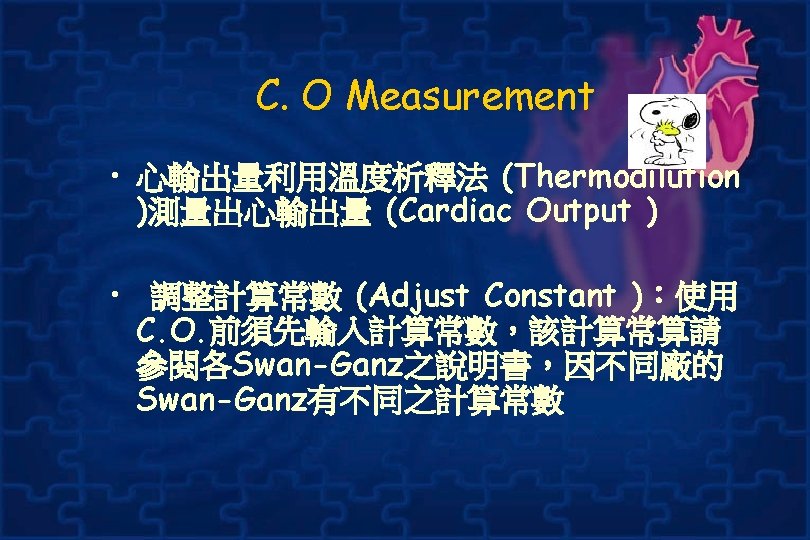
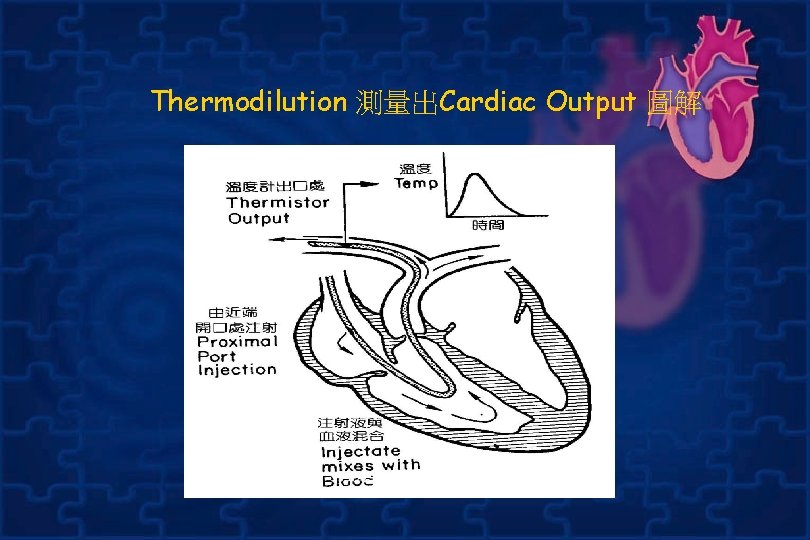
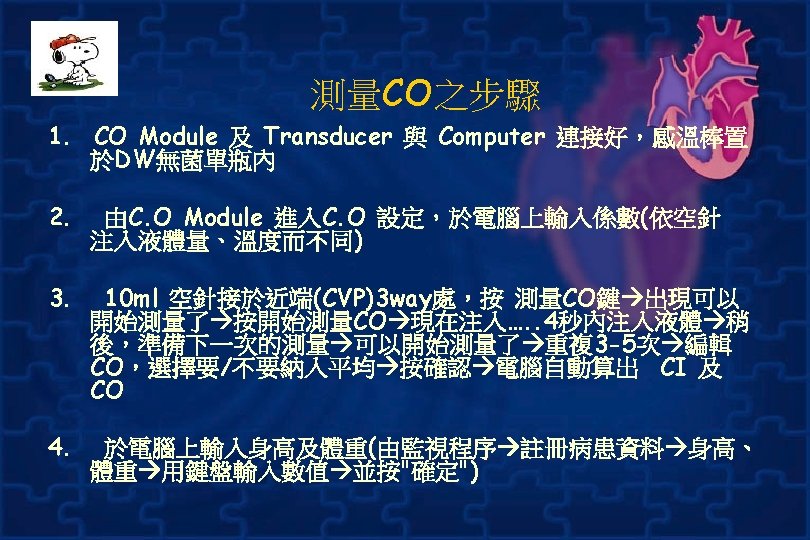
Thermodilution 測量出Cardiac Output 圖解
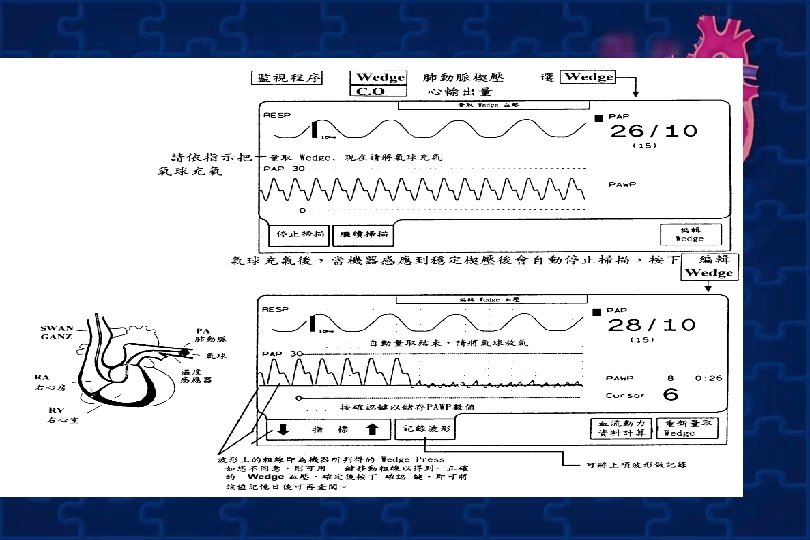
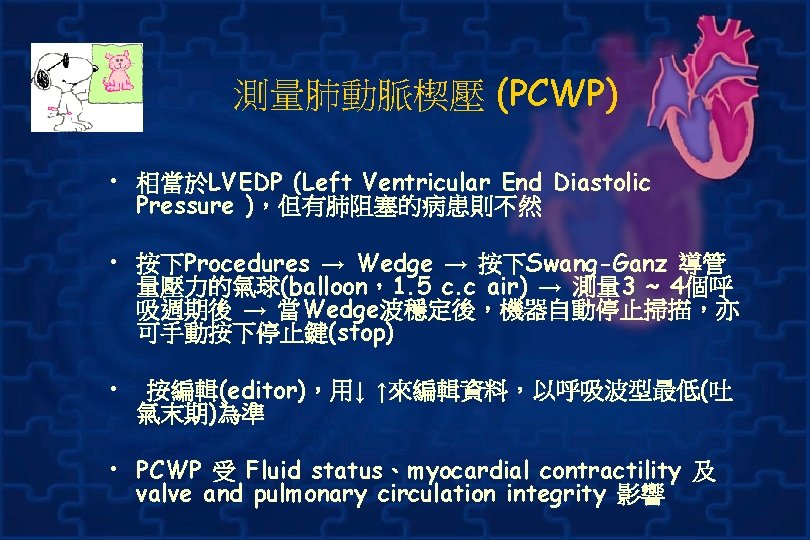
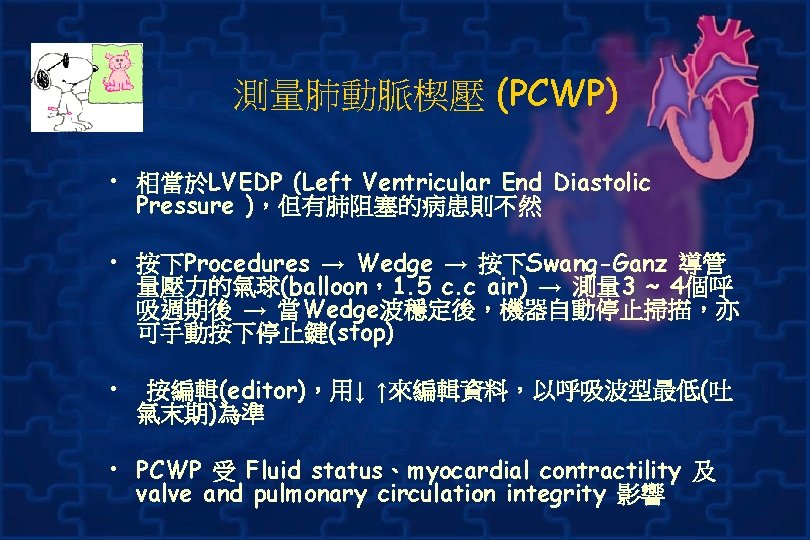
測量肺動脈楔壓 (PCWP) • 相當於LVEDP (Left Ventricular End Diastolic Pressure ),但有肺阻塞的病患則不然 • 按下Procedures → Wedge → 按下Swang-Ganz 導管 量壓力的氣球(balloon,1. 5 c. c air) → 測量 3 ~ 4個呼 吸週期後 → 當Wedge波穩定後,機器自動停止掃描,亦 可手動按下停止鍵(stop) • 按編輯(editor),用↓ ↑來編輯資料,以呼吸波型最低(吐 氣末期)為準 • PCWP 受 Fluid status、myocardial contractility 及 valve and pulmonary circulation integrity 影響
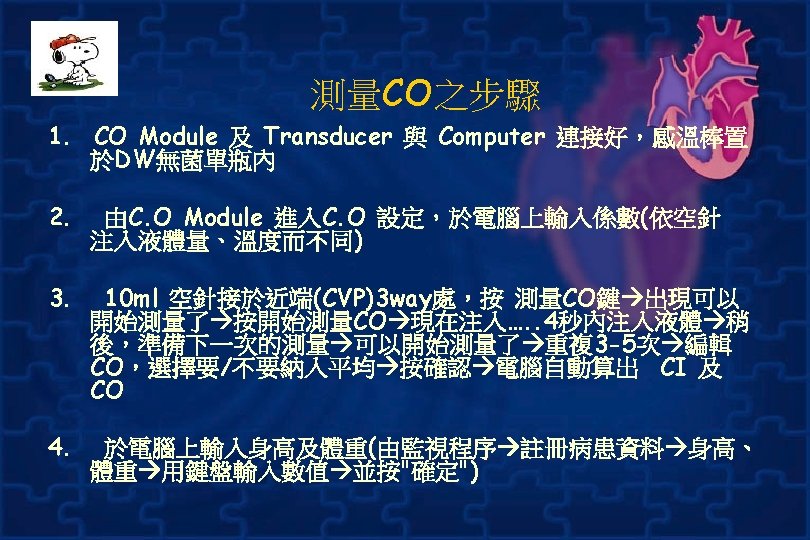
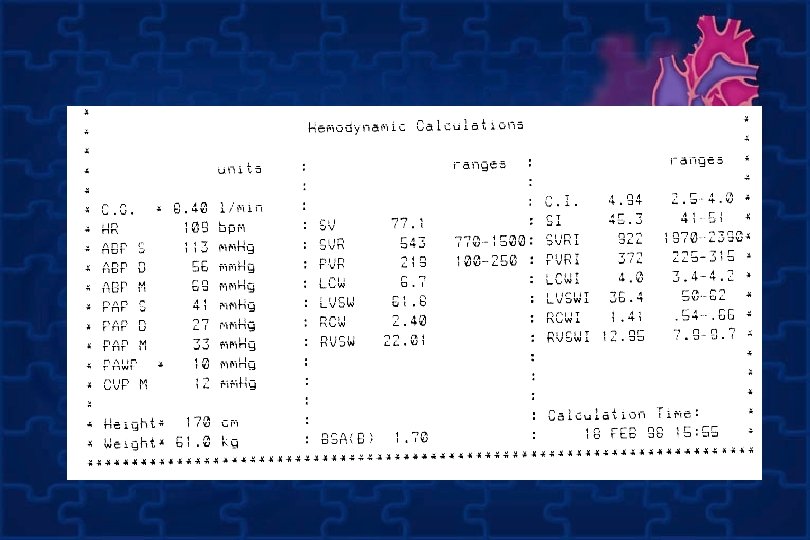
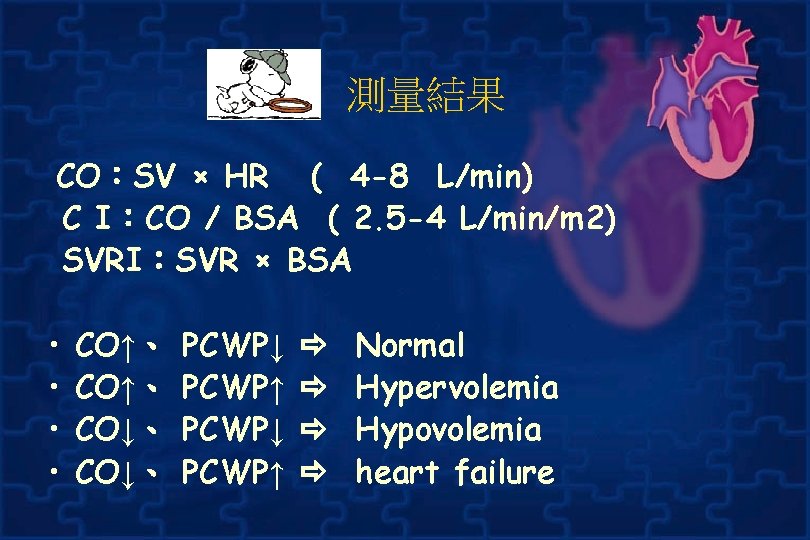
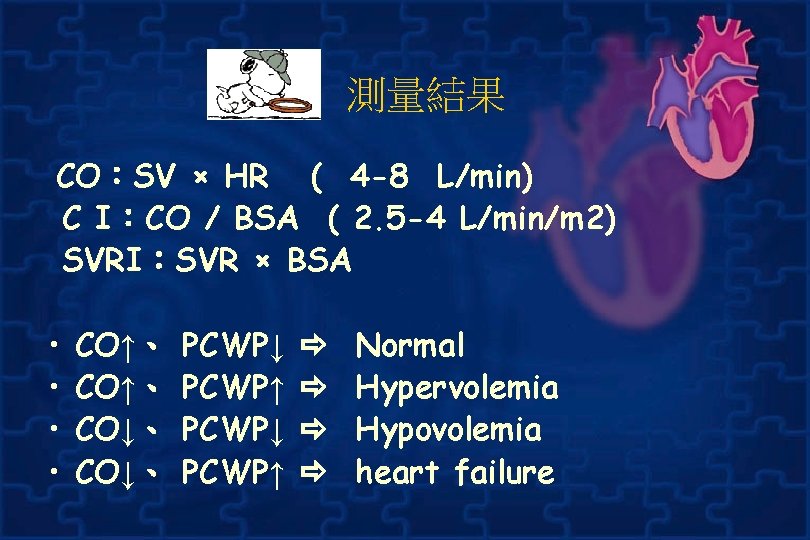
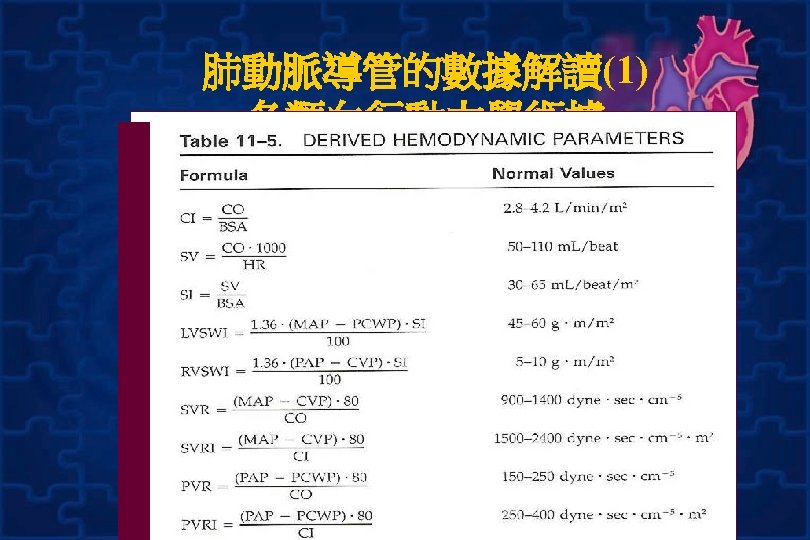
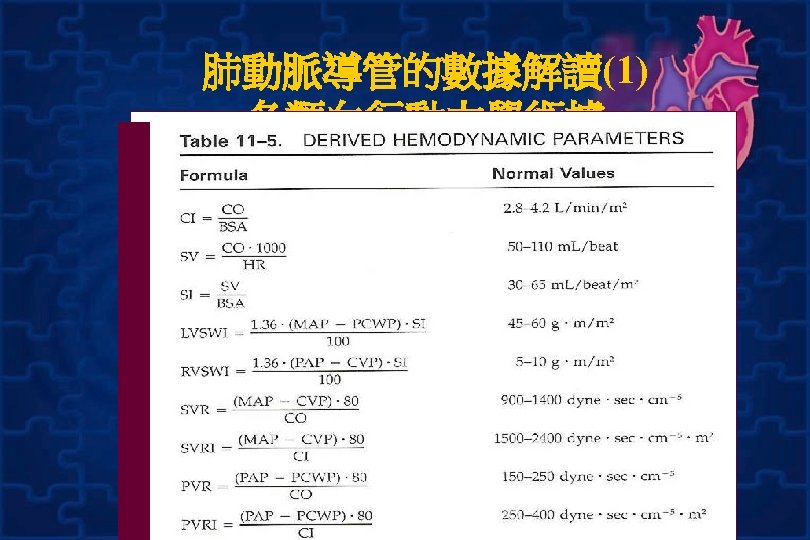
測量結果 CO:SV × HR ( 4 -8 L/min) C I:CO / BSA ( 2. 5 -4 L/min/m 2) SVRI:SVR × BSA • • CO↑、 CO↓、 PCWP↓ PCWP↑ Normal Hypervolemia Hypovolemia heart failure

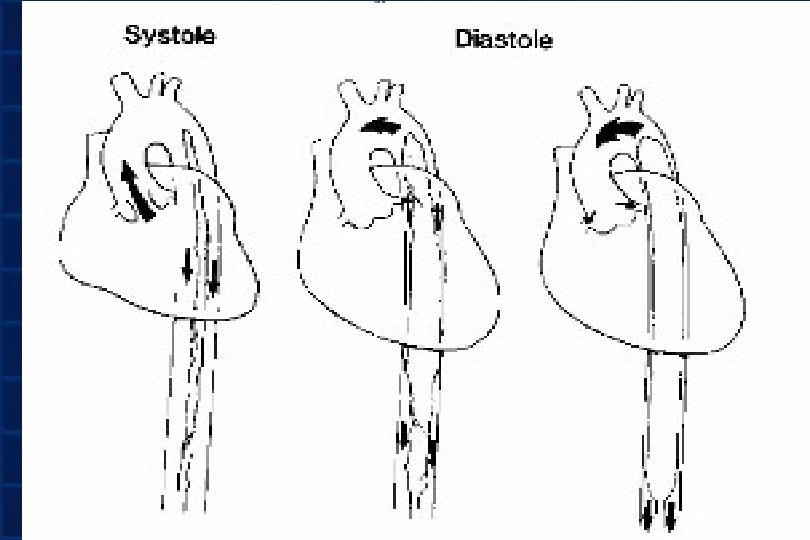
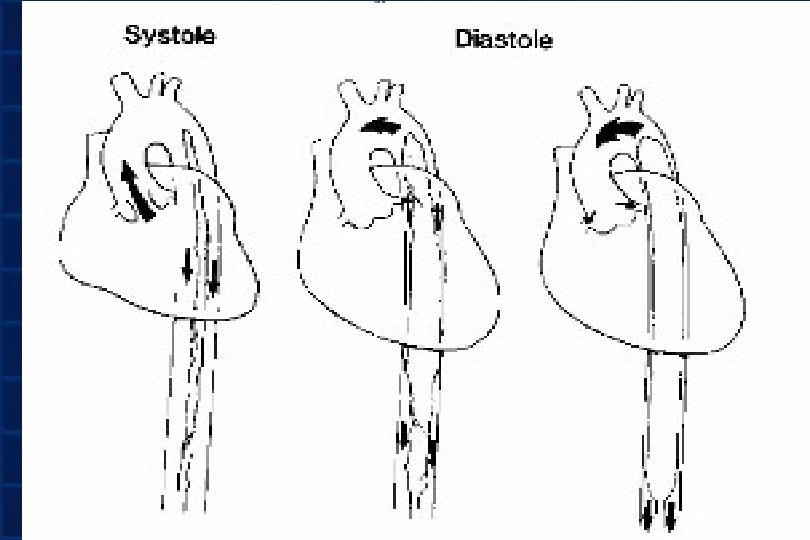
IABP
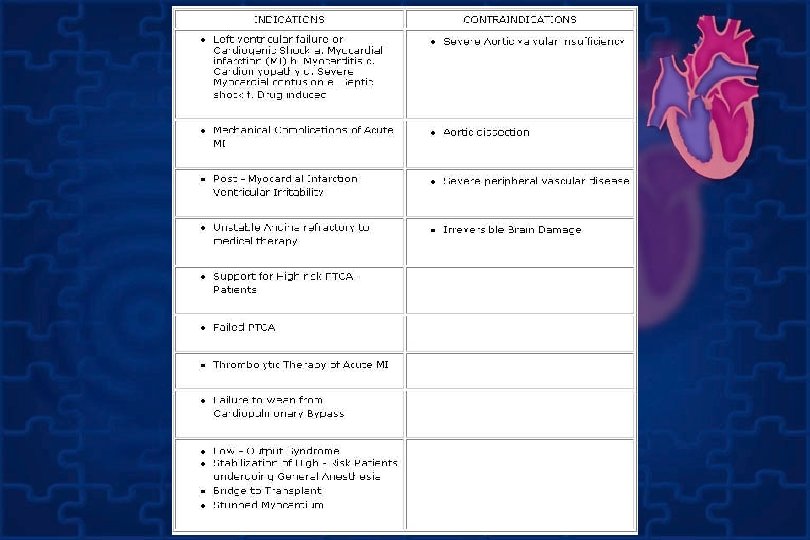
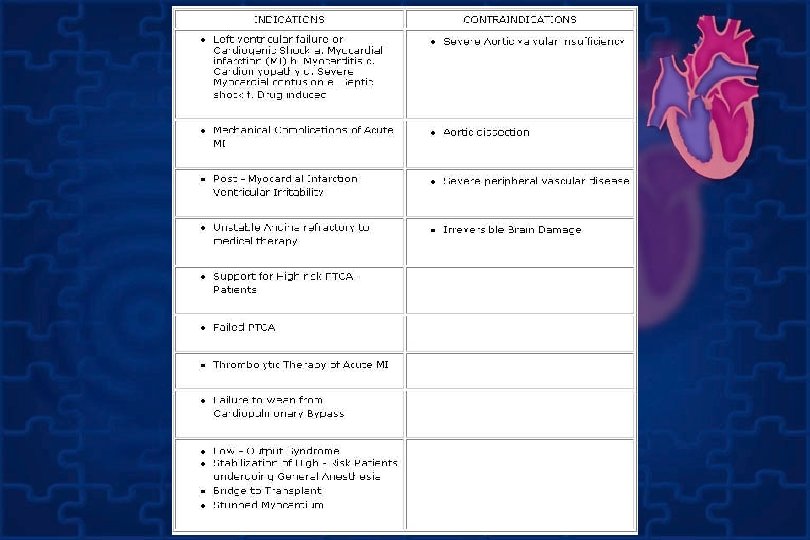
Indication • A. cardiogenic shock – Bridge to revascularization – Bridge to tertiary center • • B. Refractory unstable angina C. Acute MI cathter based perfusion D. High risk percutaneous revascularization E. End stage cardiomyopathy/bridge to heart transplantation
Indication • G. Mechanical complication of acute MI. Acute MR and VSD • H. decompensated aortic stenosis • I. Refractory ventricular arrythmias • J. Weaning from cardiopulmonary bypass /post operative pump failure
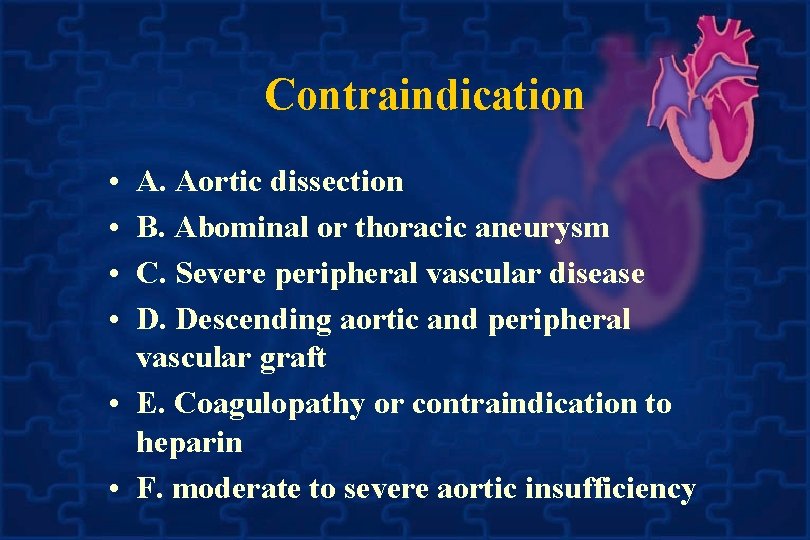
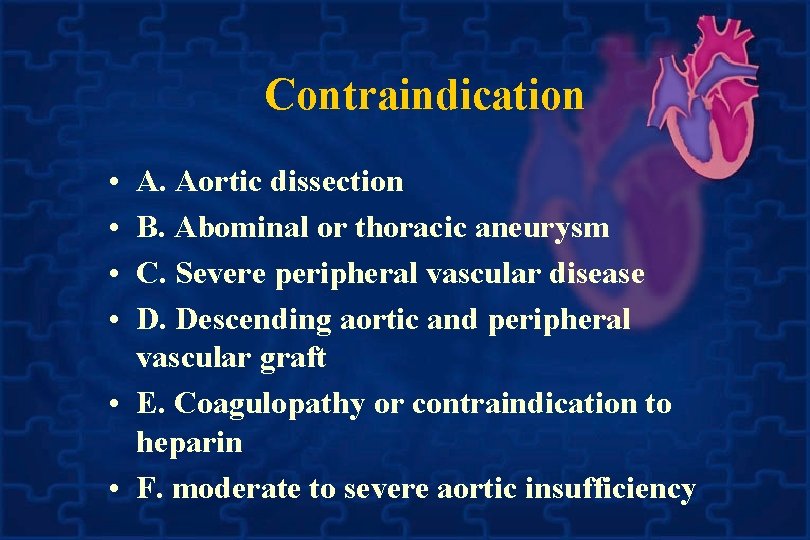
Contraindication • • A. Aortic dissection B. Abominal or thoracic aneurysm C. Severe peripheral vascular disease D. Descending aortic and peripheral vascular graft • E. Coagulopathy or contraindication to heparin • F. moderate to severe aortic insufficiency
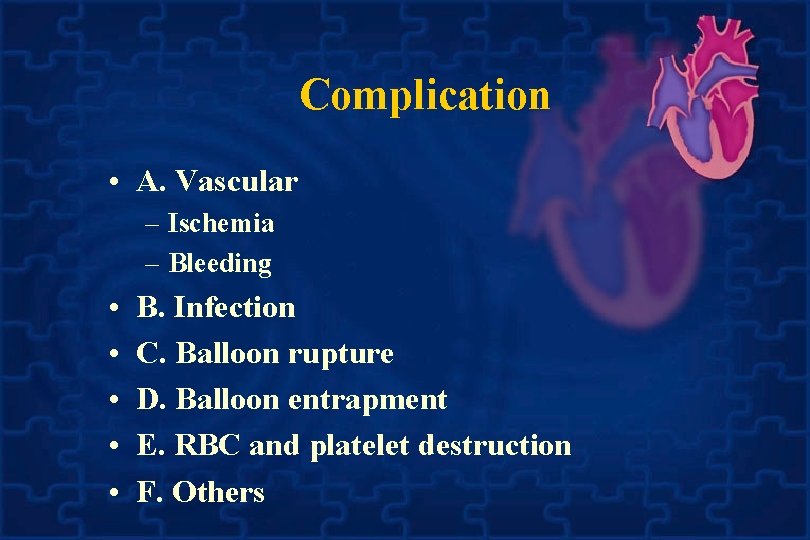
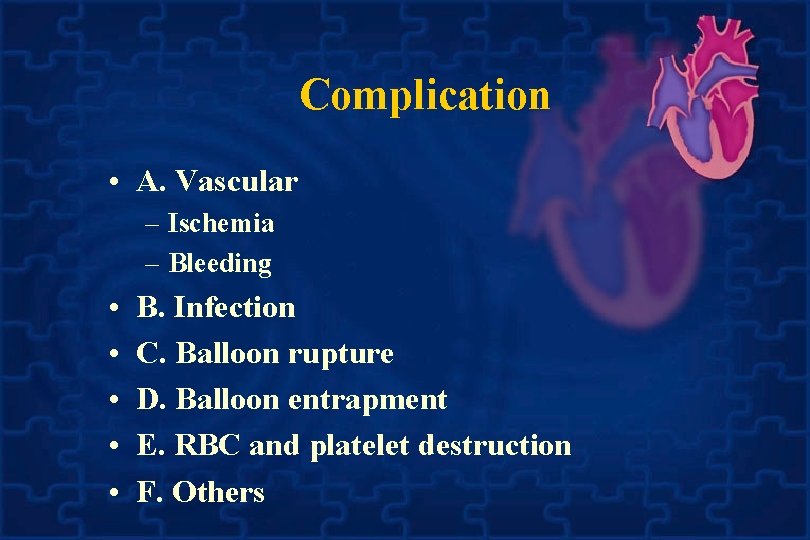
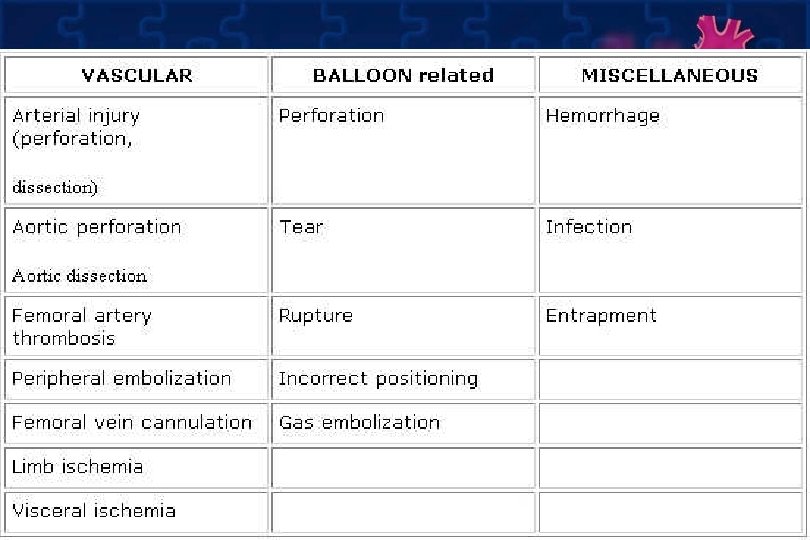
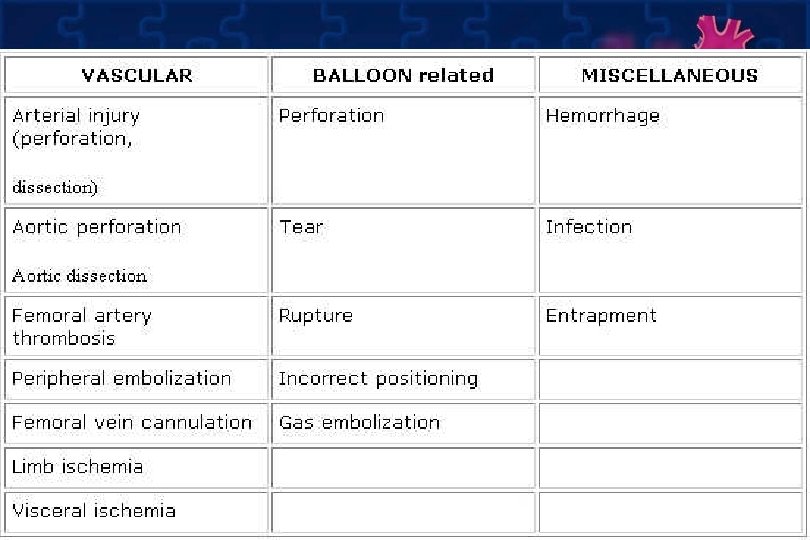
Complication • A. Vascular – Ischemia – Bleeding • • • B. Infection C. Balloon rupture D. Balloon entrapment E. RBC and platelet destruction F. Others
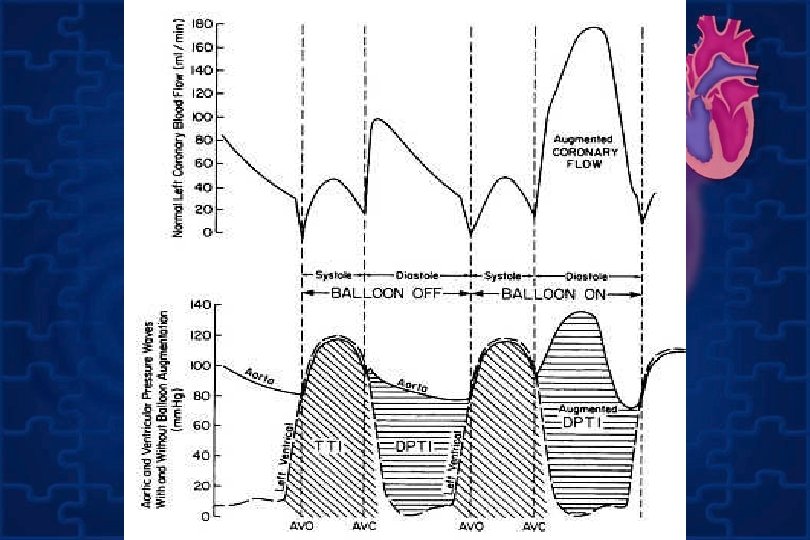
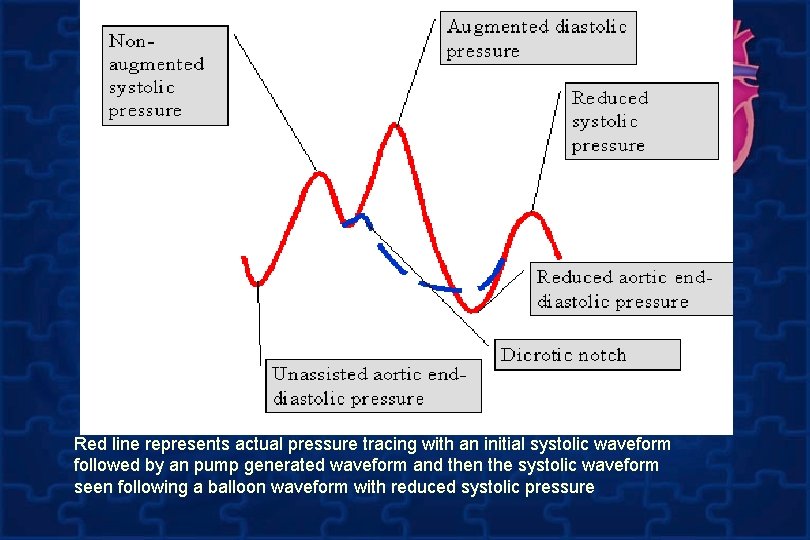
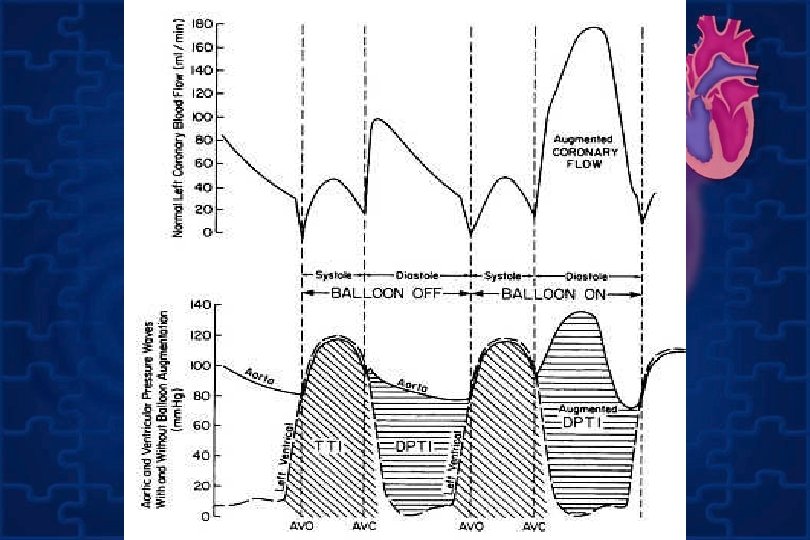
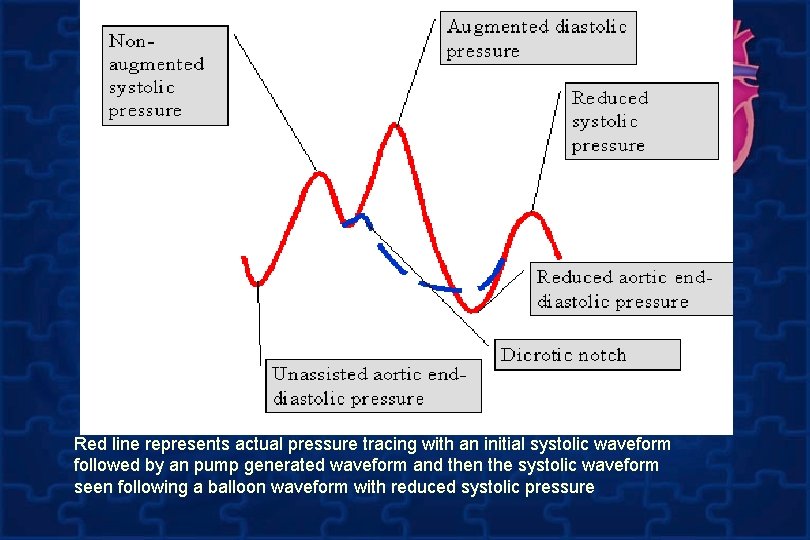
Red line represents actual pressure tracing with an initial systolic waveform followed by an pump generated waveform and then the systolic waveform seen following a balloon waveform with reduced systolic pressure
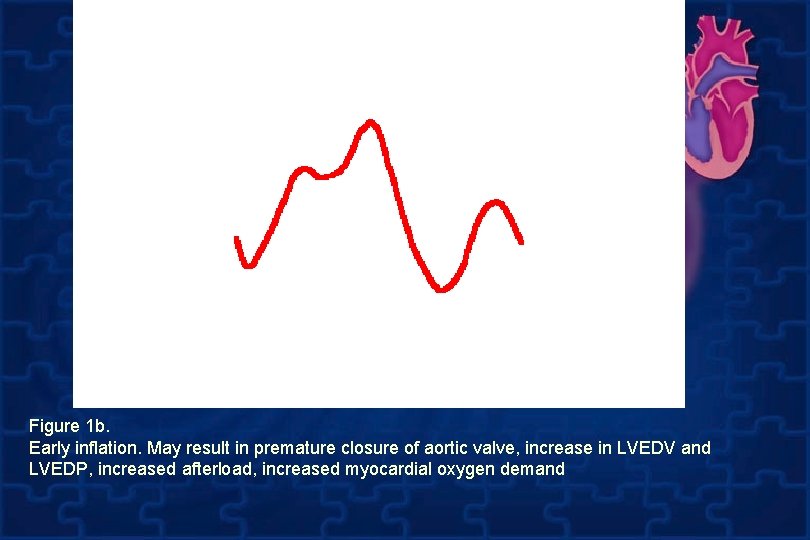
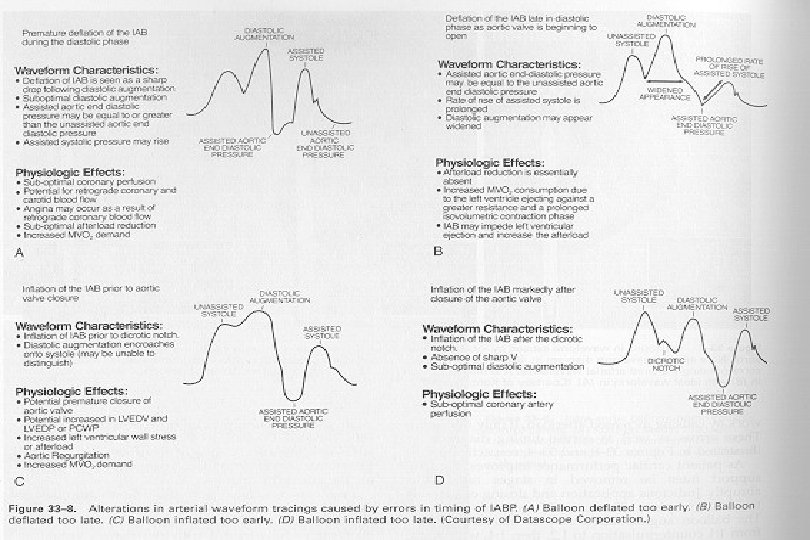
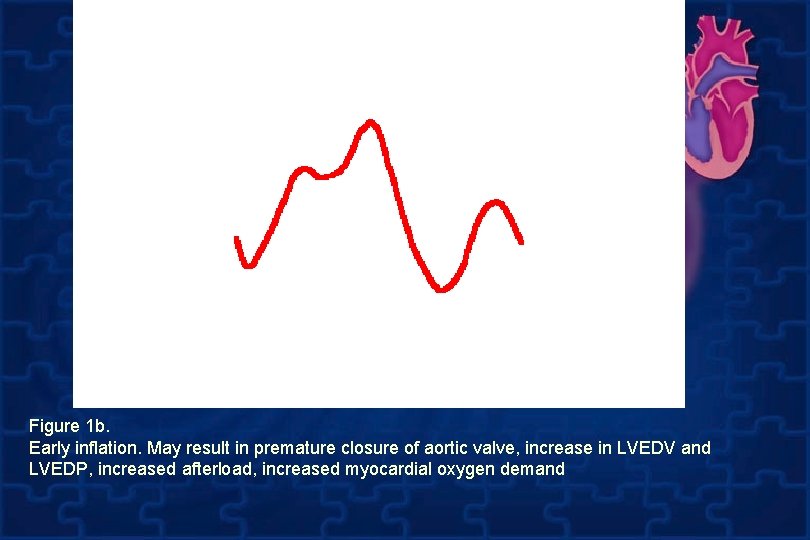
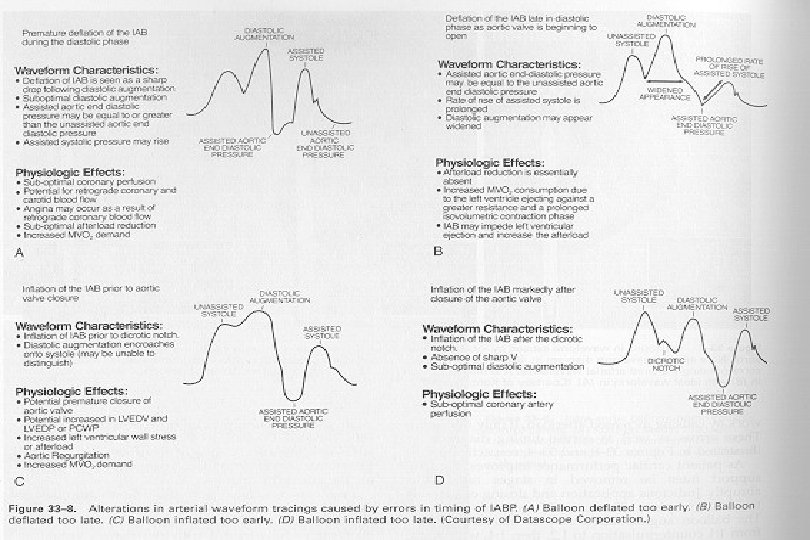
Figure 1 b. Early inflation. May result in premature closure of aortic valve, increase in LVEDV and LVEDP, increased afterload, increased myocardial oxygen demand
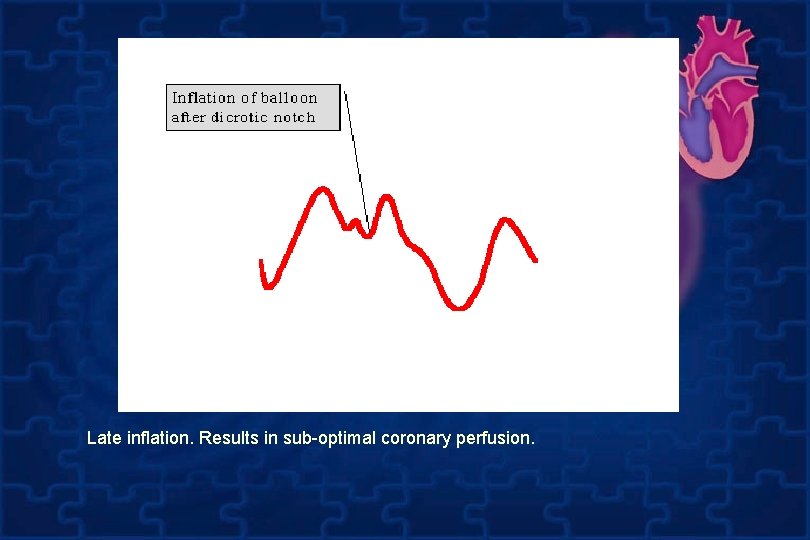
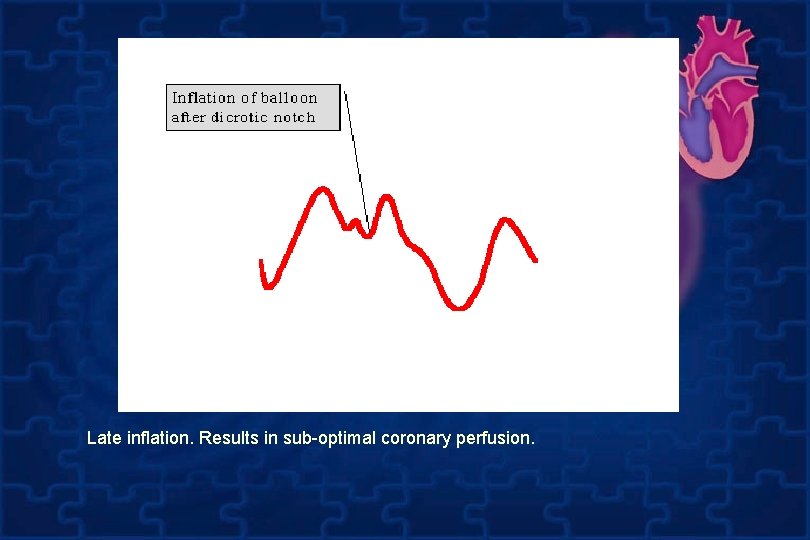
Late inflation. Results in sub-optimal coronary perfusion.
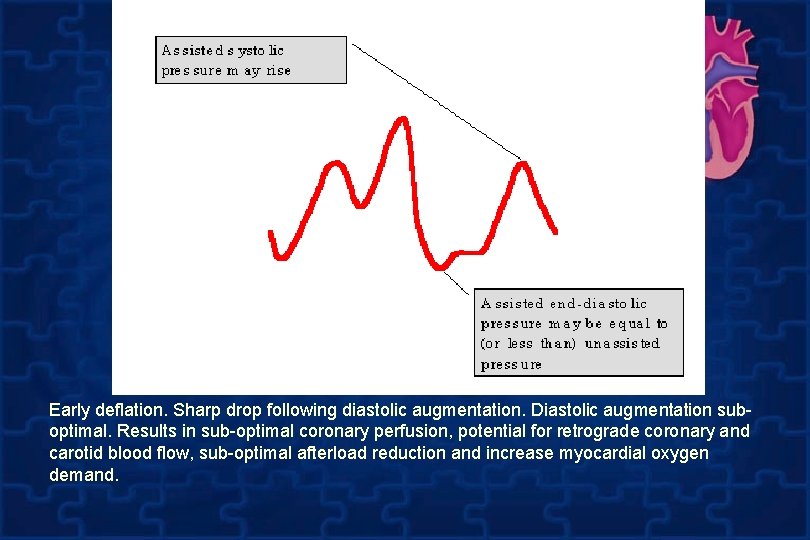
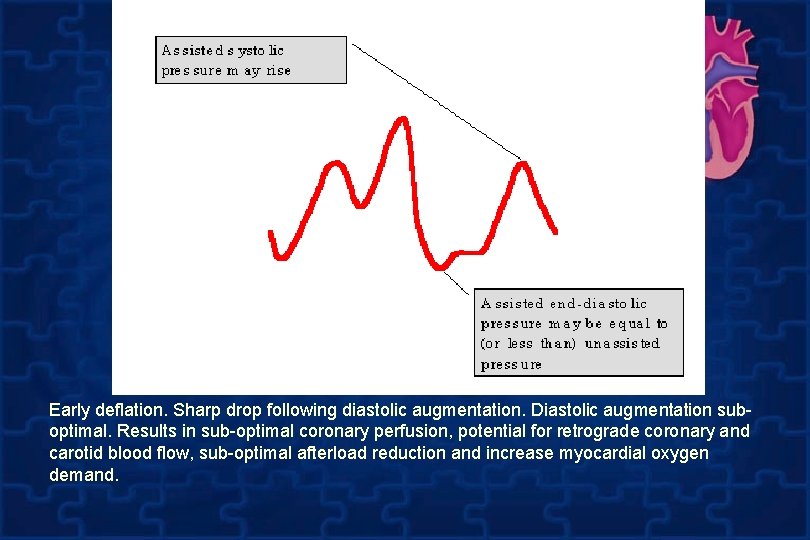
Early deflation. Sharp drop following diastolic augmentation. Diastolic augmentation suboptimal. Results in sub-optimal coronary perfusion, potential for retrograde coronary and carotid blood flow, sub-optimal afterload reduction and increase myocardial oxygen demand.
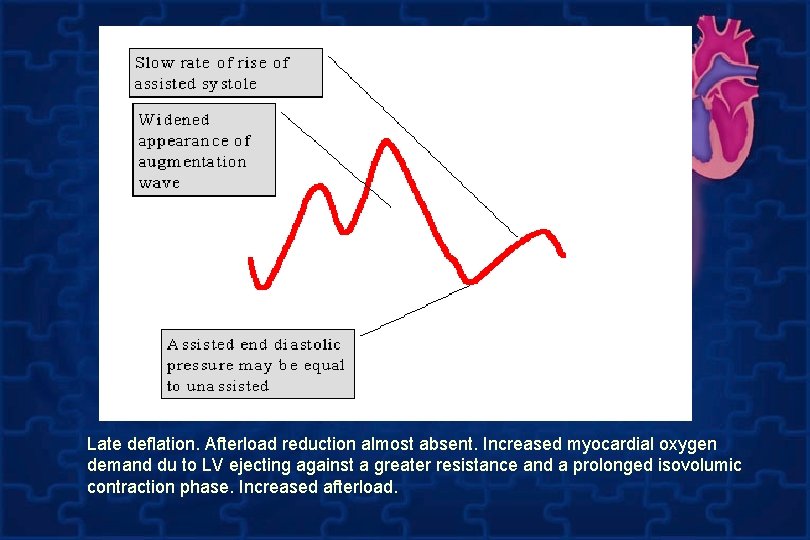
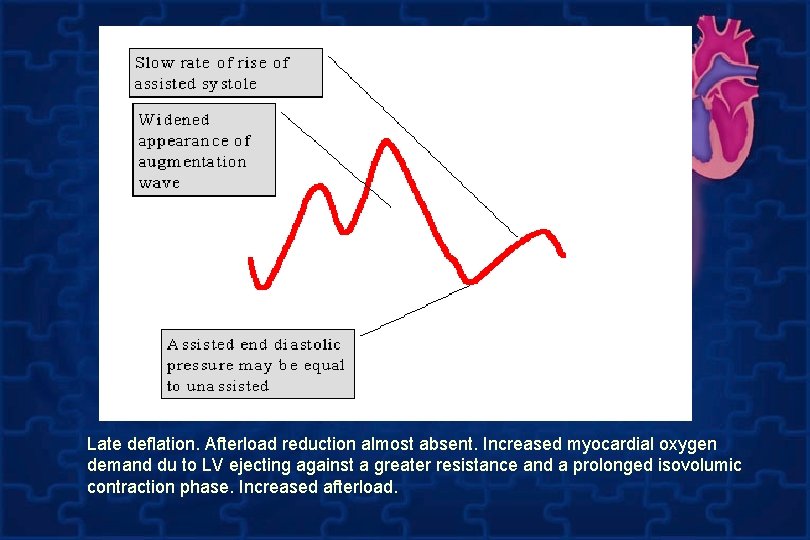
Late deflation. Afterload reduction almost absent. Increased myocardial oxygen demand du to LV ejecting against a greater resistance and a prolonged isovolumic contraction phase. Increased afterload.