Poisoning and Overdose Emergencies Topic Overview Emergency Medical

- Slides: 51
Poisoning and Overdose Emergencies
Topic Overview • Emergency Medical Care of Poisoning / Overdose • Relationship to Airway Management
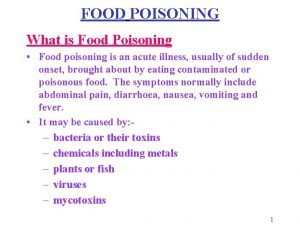
Poisoning and Overdoses Poisonings – There were over 2, 500, 000 reported poisonings reported in 1993 • Poison – Any substance that can harm the body – Can also involve living organisms that produce toxins
Poisoning and Overdoses • Ingested- This can include household and industrial chemicals, medications, improperly prepared foods, plant materials, petroleum products, and agricultural products • NOTE: Extreme care must be taken when ventilating a patient that has ingested any substance. Practice BSI!
Poisoning and Overdoses • Inhaled – Carbon monoxide, ammonia, chlorine, insect sprays, and gases produced by volatile chemicals • Absorbed – Usually through unbroken skin. Many corrosives and irritants can be absorbed after causing the skin to breakdown
Poisoning and Overdoses • Injected- The most common is illicit drugs but can include snakes fangs and insects stingers
Poisoning and Overdoses Patient Assessment-Ingested Poisons – What was the substance? • Get exact name • Bring container – When did the exposure occur? – How much was ingested? • If not known, estimate possible amount
Poisoning / Overdoses – Over how long a period did the ingestion take place? • If not known, estimate shortest and longest possible times – What interventions taken? – What is the patients estimated weight? – Is the patient experiencing any effects from the ingestion?
Poisoning / Overdoses • Ingested Poisons – Signs and Symptoms • • Altered mental status Abdominal pain Chemical burns around mouth Unusual breath odor History of ingestion Nausea / Vomiting Diarrhea
Poisoning and Overdoses Treatment for Ingested Poisons – ABCs- Correct any life-threatening problems – Call Poison Center 1 -800 -POISON 1 – 1 -800 -764 -7661 – Follow directions given by poison control • Activated Charcoal – It is designed to absorb large amounts – Does not work on all poisons
Poisoning / Overdoses • Trade Names: Super. Char, Insta. Char, Liqui. Char
Activated Charcoal • Indications – Poisoning by mouth • Contraindications – Altered mental status – Ingestion of acid or alkali – Patient unable to swallow • Follow directions of Poison Control Center
Poisoning and Overdoses Treatment- (Cont. ) – Check head, neck, chest and abdomen – SAMPLE history – Baseline vital signs – Transport any containers or bottles from the substance – On-going assessment
Poisoning and Overdoses Pediatric Poisonings – Are frequent victims – Very important to have the weight of the patient – Always assume a lethal dose has been ingested
Poisons / Overdoses • Inhaled Poisons – General Signs and Symptoms • • • History of inhalation Difficulty speaking Chest pain Cough Hoarseness Dizziness Headache / Confusion Seizures Altered Mental Status
Poisoning and Overdoses Patient Assessment- Inhaled Poisons – What substance? – When did the exposure occur? – Over how long a period was the exposure? – Any interventions? – What effects have been noted?
Poisoning and Overdoses Treatment - Inhaled Poisons – ABCs- Correct any life-threatening problems – Call Poison Center 1 -800 -POISON 1 – 1 -800 -764 -7661 – Follow directions given by poison control ABCs- Correct any life-threatening
Poisoning and Overdoses • Treatment – Check head, neck, chest and abdomen – SAMPLE history – Baseline vital signs – On-going assessment
Poisoning and Overdoses • Inhaled Poisons – Carbon Monoxide • • Most common inhaled poison Vehicle exhaust and fire suppression Odor-less and color-less Signs & Symptoms – – – Headache Dizziness Dyspnea Cyanosis Altered Mental Status
Poisoning and Overdoses – Smoke Inhalation – S and S • Shortness of Breath – Coughing – Smoky breath odor – Carbon residue around mouth and nose – Black residue in sputum – Nose hairs signed
Poisoning and Overdoses • Absorbed Poisons – Signs and Symptoms • • History of exposure Liquid or powder on skin Burns Itching, irritation, redness
Poisoning and Overdoses Patient Assessment- Absorbed Poisons – What substance? – When did the exposure occur? – Over how long a period of time? – Any interventions? – What effects?
Poisoning and Overdoses • Care – Absorbed Poisons – Remove patient from source – Remove clothing or substance from the patient which might be contaminated – Brush powders from patient – Irrigate with water for at least 20 minutes – Initial Assessment – SAMPLE History
Poisoning and Overdoses • Care – Absorbed Poisons – Eye • Irrigate with clean water for at least 20 minutes or until EMS arrives
Poisoning and Overdoses • GENERAL SAFETY For Inhaled and/or Absorbed Poisons – Need to know wind direction and speed – Park Uphill and Upwind of the incident
Poisons / Overdoses • Relationship to Airway Management – When treating a poisoned or overdoses patient whose airway is patent, be prepared for deterioration and need to secure airway
Poisoning and Overdoses Alcohol Abuse (ETOH) – Can be a real problem to assess – May require police assistance – Patient often has multiple problems in addition to the abuse of alcohol
Poisoning and Overdoses Patient Assessment – Odor of alcohol on the patient’s breath – Swaying and unsteady gait – Slurred speech, rambling, incoherent words – Flushed appearance to the face – Poor coordination
Poisoning and Overdoses Patient Assessment – Slowed reaction time – Blurred vision – Confusion – Hallucinations – Blackouts – Altered LOC
Poisoning and Overdoses Signs & Symptoms of ETOH Withdrawal (DTs) – Confusion and restlessness – Unusual behavior – Hallucinations – Gross tremors – Profuse sweating – Seizures – Watch for vital signs changes ETOH abuser often mix with recreational drugs
Poisoning and Overdoses Patient Care for ETOH Abuse – Watch for respiratory problems – Watch for altered LOC – Vital signs – Treat for shock – Protect the patient from self-injury – Watch for seizures – Activate EMS
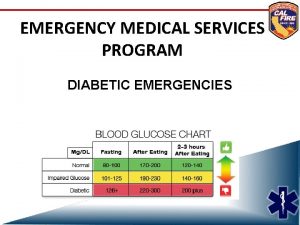
Poisoning and Overdoses • Do Not Assume That All Patients You Suspect Of ETOH Abuse Do Not Have Any Underlying Medical Condition – Many persons are arrested for DWI and later found to be a diabetic with low blood sugar • Do a good patient assessment
Poisoning and Overdoses Substance Abuse – Stimulants • Amphetamines, Uppers, Cocaine, Methamphetamine – Depressants • Barbiturates, Downers, Valium, Heroin, Morphine, Codeine, Inhalants, Alcohol – Psychedelics (Hallucinogens) • LSD, PCP, Mescaline, Cannabis
Poisoning and Overdoses Patient Assessment- Substance Abuse • Stimulants – Excitement, increased alertness, euphoria – Increased pulse and breathing – Restlessness, irritability, Insomnia – Rapid Speech – Dry mouth – Dilated Pupils – Decreased appetite
Poisoning and Overdoses Patient Assessment- Substance Abuse • Depressants – Relaxation, decreased awareness – Drowsiness – Slowing pulse and respirations – Impaired coordination – Slurred speech – Stupor, death
Poisoning and Overdoses Patient Assessment-Substance Abuse • Hallucinogens – Breakdown of Inhibitions – Alteration of perceptions (hallucinations) • Visual and Auditory - Bugs crawling on the wall – Increased appetite – Rapid Pulse, Dilated Pupils, Flushed Face – Tremors, Death
Poisoning and Overdoses Patient Care- Substance Abuse – Initial Assessment – Watch for airway problems – Treat for shock – Try to gain the patient’s confidence – Perform a rapid trauma assessment – Check for track marks
Poisoning and Overdoses Patient Care- Substance Abuse – Protect the patient from self-injury – Transport ASAP and contract medical control – On-going Assessment
Poisoning and Overdoses ALWAYS CLOSELY MOINTER SUBSTANCE ABUSE PATIENTS FOR CHANGES IN CONDITION AND FOR TENDENCY TO BECOME VIOLENT
Bites and Stings • Assessment – Signs and Symptoms – History of spider / snake bite / insect / scorpion / marine animal sting • • • Pain, redness, swelling Dizziness and chills Fever Nausea and vomiting Bite marks or stinger
Bites and Stings • Bites and Stings – Emergency Care • • Wash area gently Remove jewelry distal to affected area Position injection site slightly below heart Observe for allergic reaction
Snakes, Spiders, Scorpions • Review information from Tri 5 Phar/Tox • To review go to Basic Sciences, Pharmacology/Toxicology, Dr. Giggleman’s lecture notes on Spiders and Snakes.
Ticks • Tick Removal – Using forceps grasp tick at apex of thorax (toward the head) and apply gently backward pressure until the tick releases. Remove the tick. – Scrub area vigorously with soap and water – Watch for signs of infection
Marine Life Injuries
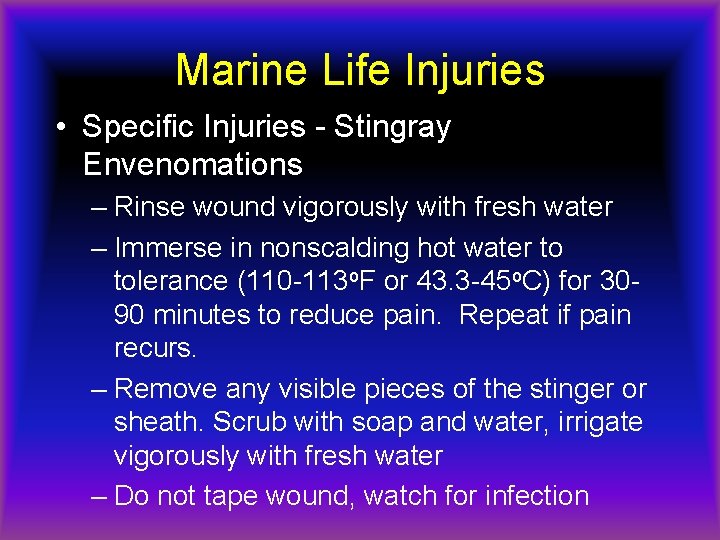
Marine Life Injuries • Specific Injuries - Stingray Envenomations – Rinse wound vigorously with fresh water – Immerse in nonscalding hot water to tolerance (110 -113 o. F or 43. 3 -45 o. C) for 3090 minutes to reduce pain. Repeat if pain recurs. – Remove any visible pieces of the stinger or sheath. Scrub with soap and water, irrigate vigorously with fresh water – Do not tape wound, watch for infection
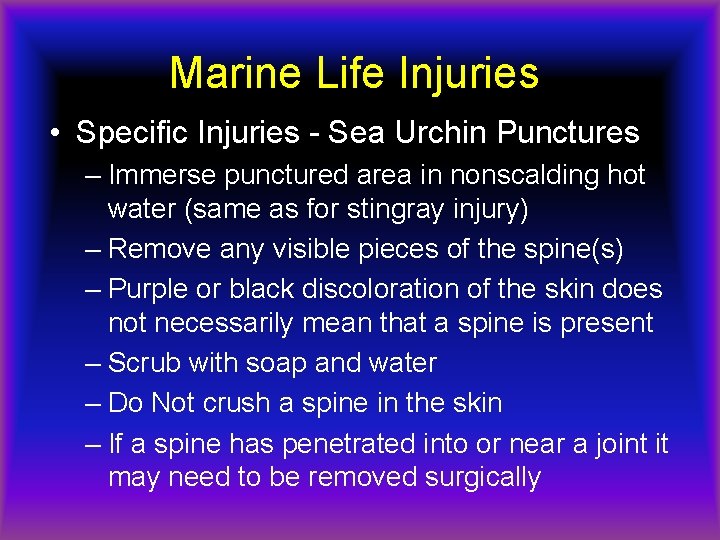
Marine Life Injuries • Specific Injuries - Sea Urchin Punctures – Immerse punctured area in nonscalding hot water (same as for stingray injury) – Remove any visible pieces of the spine(s) – Purple or black discoloration of the skin does not necessarily mean that a spine is present – Scrub with soap and water – Do Not crush a spine in the skin – If a spine has penetrated into or near a joint it may need to be removed surgically
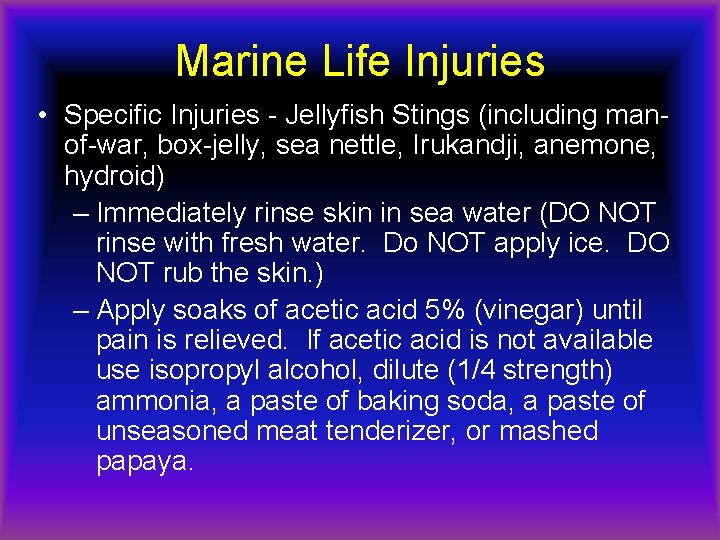
Marine Life Injuries • Specific Injuries - Jellyfish Stings (including manof-war, box-jelly, sea nettle, Irukandji, anemone, hydroid) – Immediately rinse skin in sea water (DO NOT rinse with fresh water. Do NOT apply ice. DO NOT rub the skin. ) – Apply soaks of acetic acid 5% (vinegar) until pain is relieved. If acetic acid is not available use isopropyl alcohol, dilute (1/4 strength) ammonia, a paste of baking soda, a paste of unseasoned meat tenderizer, or mashed papaya.

Marine Life Injuries • Specific Injuries - Jellyfish Stings • Do Not apply aftershave, liquor, or organic solvents such as kerosene, turpentine or gas – Remove large tentacle fragments using forceps – Reapply vinegar – Soap affected area in nonscalding hot water (same as for stingray sting)
Marine Life Injuries • Coral Cuts – Irrigate with cleanest water available – Scrub vigorously with soap and water – Flush wound with 1/2 strength solution of hydrogen peroxide in water – Use topical antibiotic if infection develops – Use anti-itch cream if itching develops
Marine Life Injuries • Scorpion Fish, Stone Fish, Lion Fish – Envenomations – Immerse in non-scalding hot water to tolerance (110 -113 o. F or 43. 3 -45 o. C) for 3090 minutes to reduce pain. Repeat if pain recurs. – Keep extremity lower than heart level – Avoid excessive movement – Seek medical attention
Marine Life Injuries • Bites – Control bleeding and attend to other lifethreatening problems – Treat as you would any open soft tissue injury. – Seek medical attention as indicated.
 Vitamin b6 overdose symptoms
Vitamin b6 overdose symptoms Tricyclic antidepressants overdose
Tricyclic antidepressants overdose Magnesium overdose
Magnesium overdose Beta-blocker overdose treatment glucagon
Beta-blocker overdose treatment glucagon Normal range calcium
Normal range calcium Zoplicone overdose
Zoplicone overdose Hepatic encephalopathy stages
Hepatic encephalopathy stages Opioid overdose
Opioid overdose Opioid overdose
Opioid overdose Opioid overdose
Opioid overdose Metformin overdose
Metformin overdose Nys dcjs forms
Nys dcjs forms Function of vitamin a
Function of vitamin a Caffeine uses
Caffeine uses General topic example
General topic example Narrow down the topic
Narrow down the topic Lesson 6: cardiac emergencies and using an aed
Lesson 6: cardiac emergencies and using an aed Endocrine and hematologic emergencies
Endocrine and hematologic emergencies Emt chapter 18 gastrointestinal and urologic emergencies
Emt chapter 18 gastrointestinal and urologic emergencies Chapter 28 lesson 1
Chapter 28 lesson 1 Chapter 14 medical overview
Chapter 14 medical overview Emergency medical responder: first on scene
Emergency medical responder: first on scene Red cross first responder
Red cross first responder Introduction to emergency medical care
Introduction to emergency medical care Chapter 31 assisting in a medical emergency
Chapter 31 assisting in a medical emergency Define medical emergency chapter 31
Define medical emergency chapter 31 Medical emergency student lectures
Medical emergency student lectures Emergency medical dispatch guidecards
Emergency medical dispatch guidecards Texas medicaid transportation
Texas medicaid transportation Tdh ems
Tdh ems Medical
Medical Emergency medical responder first on scene 10th edition
Emergency medical responder first on scene 10th edition Ac veins
Ac veins Emergency medical responder first on scene 11th edition
Emergency medical responder first on scene 11th edition Introduction to emergency medical care
Introduction to emergency medical care Local area orientation dive
Local area orientation dive Chapter 16 respiratory emergencies
Chapter 16 respiratory emergencies Major nutritional deficiency diseases in emergencies
Major nutritional deficiency diseases in emergencies Chapter 32 environmental emergencies
Chapter 32 environmental emergencies Chapter 23 gynecologic emergencies
Chapter 23 gynecologic emergencies The term behavioral crisis is most accurately defined as
The term behavioral crisis is most accurately defined as Chapter 18 neurologic emergencies
Chapter 18 neurologic emergencies Chapter 16 respiratory emergencies
Chapter 16 respiratory emergencies Lsu hematology oncology fellowship
Lsu hematology oncology fellowship Gems diamond geriatric
Gems diamond geriatric Chapter 13 handling emergencies
Chapter 13 handling emergencies Chapter 12 behavioral emergencies
Chapter 12 behavioral emergencies Chapter 32 environmental emergencies
Chapter 32 environmental emergencies Chapter 17 cardiovascular emergencies
Chapter 17 cardiovascular emergencies Psychiatric emergencies
Psychiatric emergencies Qut security emergency extension number
Qut security emergency extension number Immunologic emergencies
Immunologic emergencies