Approach To Management of poisoning Poisoning and Overdose
- Slides: 44
Approach To Management of poisoning
Poisoning and Overdose • Poisoning represents the harmful effects of accidental or intentional exposure to toxic amounts of any substance • Although most poisons have predictable doserelated effects, individual variability in the response to a given dose may occur because of genetic polymorphism, enzymatic induction or inhibition in the presence of other xenobiotics, or acquired tolerance
Depending on • the route of exposure, • the chemical and physical properties of poisons • its mechanism of action Poisoning may be a. Local (e. g. , skin, eyes, lungs) or b. Systemic Ø The severity and reversibility of poisoning also depend on the functional reserve of the individual or target organ
Epidemiology • > 2 million human poisoning exposures reported annually • > 50% occur in children < 6 year old • > 90% of exposures in children occur in the home • Most are acute, accidental, involve a single agent, occur in the home, result in minor or no toxicity • Pharmaceuticals involved in 47% of exposures and 84% of serious or fatal poisonings
Unintentional exposures can result from ü Improper use of chemicals at work or play ü Label misreading; ü Product mislabeling; ü Mistaken identification of unlabeled chemicals; ü Uninformed self-medication ü Dosing errors by nurses, pharmacists, physicians, parents and the elderly
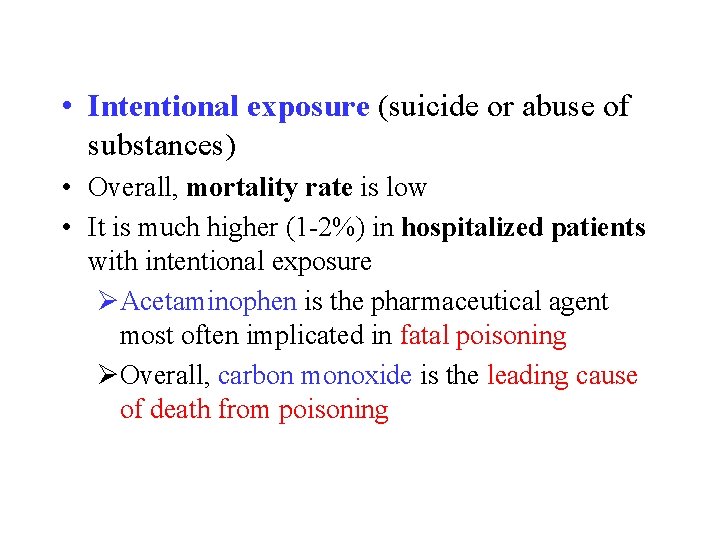
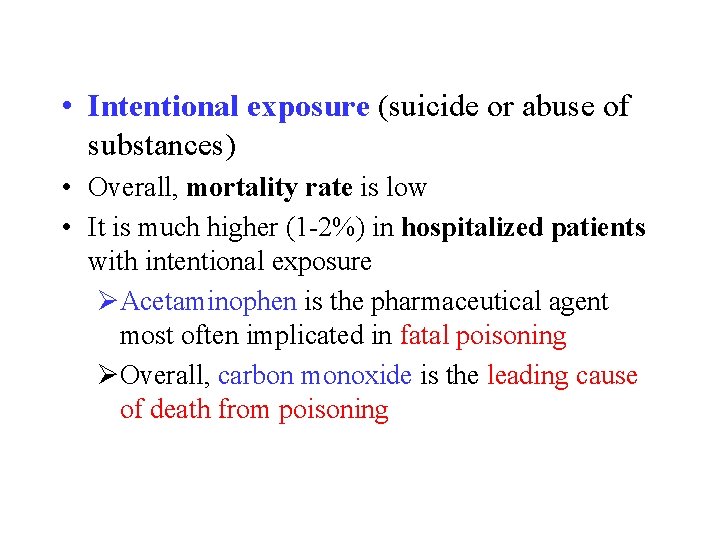
• Intentional exposure (suicide or abuse of substances) • Overall, mortality rate is low • It is much higher (1 -2%) in hospitalized patients with intentional exposure ØAcetaminophen is the pharmaceutical agent most often implicated in fatal poisoning ØOverall, carbon monoxide is the leading cause of death from poisoning
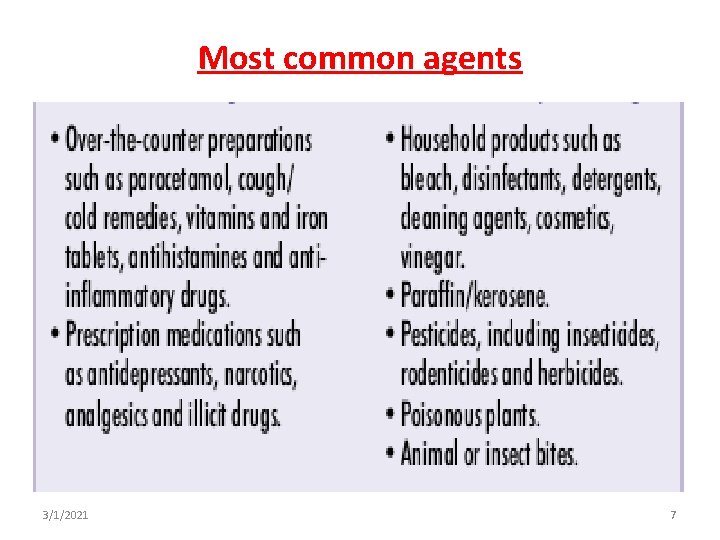
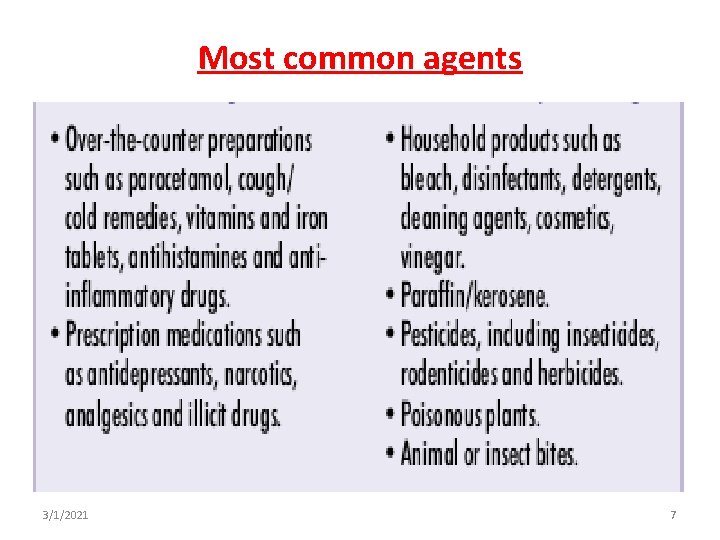
Most common agents 3/1/2021 7
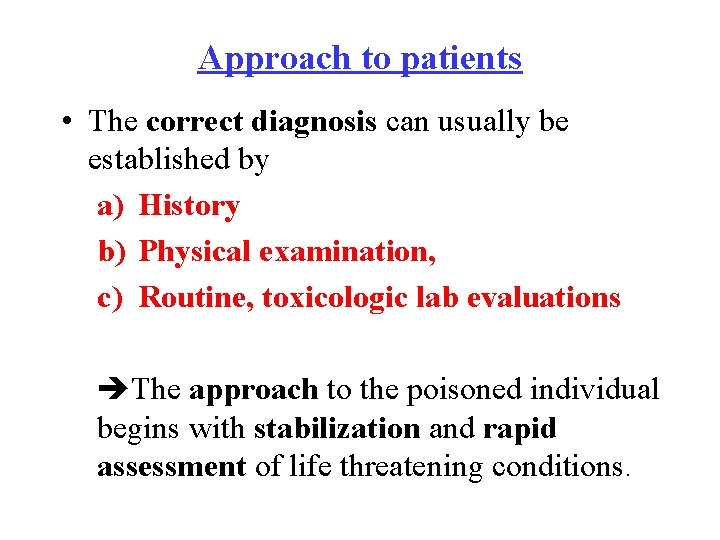
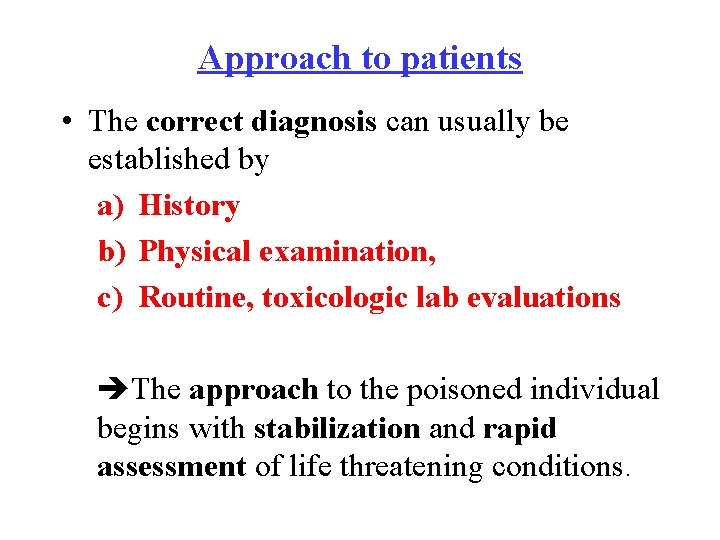
Approach to patients • The correct diagnosis can usually be established by a) History b) Physical examination, c) Routine, toxicologic lab evaluations The approach to the poisoned individual begins with stabilization and rapid assessment of life threatening conditions.
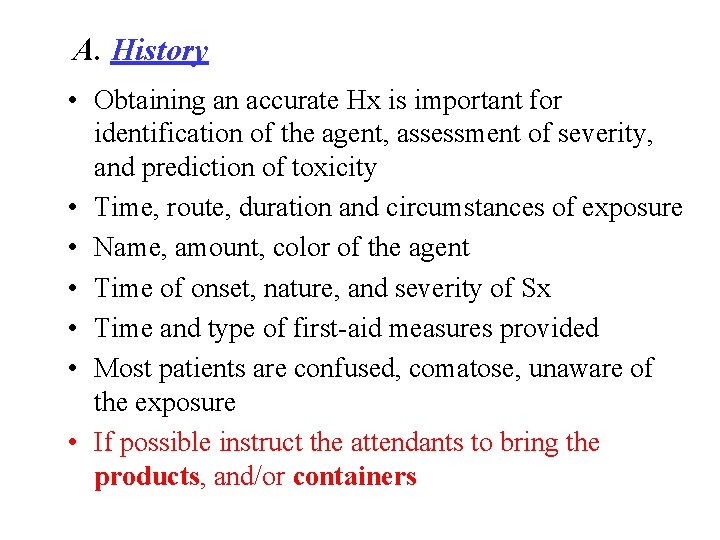
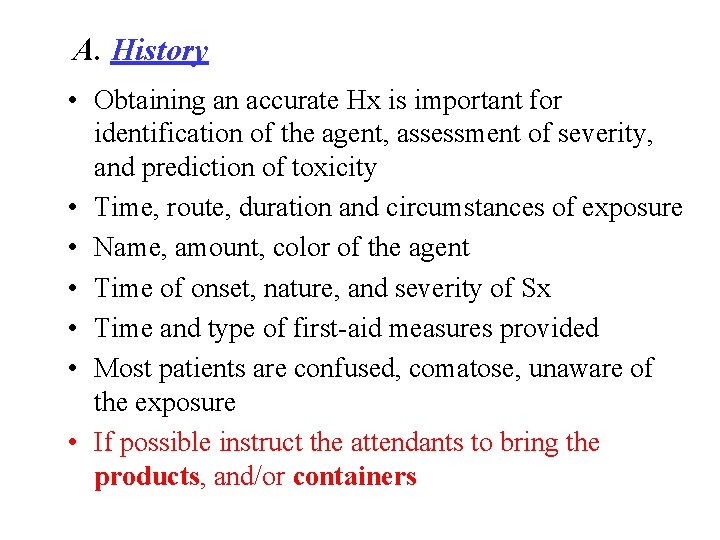
A. History • Obtaining an accurate Hx is important for identification of the agent, assessment of severity, and prediction of toxicity • Time, route, duration and circumstances of exposure • Name, amount, color of the agent • Time of onset, nature, and severity of Sx • Time and type of first-aid measures provided • Most patients are confused, comatose, unaware of the exposure • If possible instruct the attendants to bring the products, and/or containers
Suspicious circumstances include • unexplained sudden illness in a previously healthy person / in a group • Hx of psychiatric problems (particularly depression); • Recent changes in health, economic status, or social relationships; • Onset of illness while working with chemicals or after ingesting food, drink or medications
Symptoms • Sx experienced after ingestion, • Ocular: Discharge, burning • Cutaneous: Diaphoresis, dryness • Oral: Salivation, Oral burns • GI: Diarrhea , Hematemesis , bowel change • CVS: SOB, palpitation • Resp: cough • CNS: altered mental status
B. Physical examination • • Vital signs and reassessing them frequently Cardiopulmonary system Neurologic status Characterize the overall physiologic state as stimulated, depressed or normal • Focal neurologic findings are uncommon
• Examination of the eyes, abdomen, skin • All orifices should be examined • The odor of breath or vomitus and the color of nails, skin or urine • Patients should also be examined for evidence of trauma and underlying illnesses
C. Laboratory assessment Investigations - RBS - CBC, LP - RFT - Electrolytes - LFT - CXR, for possible aspiration pneumonia - ECG - CT
• Toxicologic analysis of urine and blood (and occasionally of gastric contents and chemical samples) • The response to antidotes is sometimes useful for diagnostic purposes IV administration of: ü Naloxone ü Flumazenil - the response is within minutes
Management General Principle Objectives ü Maintain airway, breathing and circulation ü Reduce absorption and enhance elimination ü Antagonize or neutralize the effects ü Relieve symptoms ü Prevent organ damage or impairment
Supportive Care § Airway protection § Treatment of hypoxia § Correct hypotension/arrhythmia § Treatment of seizures § Correction of temperature abnormalities § Correction of metabolic derangements
Prevention of Further Poison Absorption Ø Gastric lavage Ø Activated charcoal administration Ø Decontamination of eye, skin Enhancement of elimination § § Multiple-dose activated charcoal Urinary p. H alkalization Hemodialysis Oxygenation Administration of Anti-dotes § Neutralization § Metabolic or Physiologic antagonism
q Activated charcoal may reduce systemic absorption of a variety of substances • The greatest benefit is achieved if activated charcoal is given within one hour after ingestion q Alkalization of urine • Attempt to achieve urine p. H of 7. 5 • Sodium bicarbonate, IV, 50 – 100 m. Eq in 1 L sodium chloride 0. 45%. Administer 250 – 500 m. L over 1– 2 hours.
Prevention of Re-exposure § Child-proofing § Psychiatric referral NB: induction of vomiting is contraindicated in patients who ingested caustic or corrosive substances and hydrocarbons, comatose patients and those with seizures
Pharmacologic treatment Initial Management 1. Hypoglycemia 40% Dextrose, IV, 40 -60 ml over 1 -3 min 2. Hypotension Normal saline, IV, 1000 ml fast then according to the response
Organophosphate and carbamate poisoning § Are potent cholinesterase inhibitors capable of causing severe cholinergic toxicity following cutaneous exposure, inhalation, or ingestion § Organophosphate and carbamate manifest similar clinical manifestations with toxicity and the management is also similar
EPIDEMIOLOGY and SOURCE OF EXPOSURE • Worldwide, an estimated 3 million people are exposed to organophosphate or carbamate agents each year, with ≈ 300, 000 fatalities • Toxicity generally results from accidental or intentional exposure to agricultural pesticides • Specific agents linked to poisoning include both carbamate and organophosphate insecticides (parathion, malathion, diazinon)
Mechanism of action • Organophosphorous compounds contain carbon and phosphorous acid derivatives • These agents are well absorbed through the skin, lungs, and GIT • They bind to acetylcholinesterase (ACh. E), and render this enzyme non-functional • the enzyme is responsible for hydrolysis of Ach to choline + acetic acid, and inhibition leads to an over abundance of Ach at the neuronal synapses and the NMJ
• Carbamates are rapidly absorbed via all routes of exposure • Unlike organophosphates, they are transient cholinesterase inhibitors, which spontaneously hydrolyze from the cholinesterase site within 48 hours • Carbamate toxicity tends to be of shorter duration that caused by organophosphates, although the mortality rates are similar
CLINICAL FEATURES • Onset and duration of ACh. E inhibition varies depending on: Øthe organophosphorous agent's Ørate of ACh. E inhibition, Øroute of absorption, Øenzymatic conversion to active metabolites Ølipophilicity of organophosphorous agent
• For most agents, oral or respiratory exposures generally result in Sn or Sx within 3 hrs, while Sx of toxicity from dermal absorption may be delayed up to 12 hrs • Lipophilic agents such as malathion are associated with delayed onset of Sx (up to 5 days) and prolonged illness (> 30 days), which may be related to rapid adipose fat uptake and delayed redistribution from the fat stores
A) Acute toxicity • Presents with manifestations of cholinergic excess • Primary effects involve the ANS, NMJ, CNS
The dominant clinical features of acute cholinergic toxicity include: • The muscarinic signs can be remembered by use of one of the two mnemonics: ü SLUDGE/BBB Salivation, Lacrimation, Urination, Defecation, G astric Emesis, Bronchorrhea, Bronchospasm, Bradycardia ü DUMBELS Defecation, Urination, Miosis, Bronchorrhea/Bro nchospasm/Bradycardia, Emesis, Lacrimation, Salivation
The nicotinic effects include: • Fasciculations, muscle weakness and paralysis via Ach stimulation of receptors at the NMJ • Nicotinic and muscarinic receptors also have been identified in the brain, and may contribute to central respiratory depression, lethargy, excitability, seizures and coma • Cardiac arrhythmias, including heart block
• Fatalities from acute organophosphate poisoning generally result from respiratory failure due to a combination of depression of the CNS respiratory center, neuromuscular weakness, excessive respiratory secretions, and bronchoconstriction • Fatalities also occur due to cardiovascular collapse • Survivors of acute organophosphate poisoning may have neuro behavioral deficits such as decreased memory and Parkinsonism, which may be permanent
B. Intermediate syndrome • 10 to 40% of patients develop a distinct neurologic disorder 24 - 96 hrs after exposure • It consists of characteristic neurological findings including: neck flexion weakness, decreased deep tendon reflexes, cranial nerve abnormalities, proximal muscle weakness, and respiratory insufficiency
• Rarely been described following carbamate poisoning • With adequate supportive care, including prolonged mechanical ventilation, most patients have complete resolution of neurologic dysfunction within 2 to 3 wks
C. Delayed neurotoxicity • Organophosphate agent induced delayed neuropathy typically occurs 1 to 3 weeks after ingestion of some specific organophosphate agents • Affected patients may present with transient, painful "stocking-glove" paresthesias followed by a symmetrical motor polyneuropathy characterized by flaccid weakness of the lower extremities, which ascends to involve the upper extremities
• Most cases of mild delayed neurotoxicity improve with time; in severe cases, an UMN syndrome with spasticity of the lower extremities usually causes permanent disability
DIAGNOSIS q Taking History q Clinically q Laboratory q Direct measurement of Ach. E activity
MANAGEMENT • ABC of life • Atropine - competes with Ach at muscarinic receptors, preventing cholinergic activation • For moderate to severe cholinergic toxicity, Atropine should be administered beginning at a dose of 2 -5 mg IV for adults and 0. 05 mg/kg, IV for children • If no effect is noted, the dose should be doubled every 3 to 5 minutes until pulmonary muscarinic sign and Sx are alleviated
• dosing should be titrated to therapeutic end point of the clearing of respiratory secretions and the cessation of bronchoconstriction • Tachycardia and mydriasis are NOT appropriate markers for therapeutic improvement, as they may indicate continued hypoxia, hypovolemia, or sympathetic stimulation. • In patients with severe poisoning, large amount of atropine by bolus and continuous infusion may required over the course of several days
• Pralidoxime - since atropine does not bind to nicotinic receptors, it is ineffective in treating neuromuscular dysfunction. • Pralidoxime is a cholinesterase reactivating agent that is effective in treating both muscarinic and nicotinic Sx • It should NOT be administered without concurrent atropine in order to prevent worsening Sx due to transient oxime-induced Ach. E inhibition
• The current WHO recommendation for IV bolus therapy with pralidoxime is at least 30 mg/kg in adults, and 25 to 50 mg/kg for children, based on the severity of Sx • It should be administered slowly over 30 minutes, since rapid administration occasionally been associated with cardiac arrest • After the bolus dose, pralidoxime given as a continuous infusion of at least 8 mg/kg/hr in adults and 10 to 20 mg/kg/hr for children
Benzodiazepines • Organophosphate induced seizures should be treated with a benzodiazepine • Prophylactic diazepam has been shown to decrease neurocognitive dysfunction after organophosphate agent poisoning
Decontamination • In cases of topical exposure with potential dermal absorption, aggressive decontamination with complete removal of the patient's clothes and vigorous irrigation of the affected areas should be performed. • The patient's clothes and belongings should be discarded since they absorb the agent, and re-exposure may occur even after washing.
Do not perform gastric lavage • Following initial resuscitation and treatment, we suggest activated charcoal be given to patients presenting within 1 hr of an organophosphate or carbamate ingestion. • The standard dose is 1 gm/kg (with max. dose of 50 gm)
10 Q!!
 Vitamin b6 overdose symptoms
Vitamin b6 overdose symptoms Tricyclic antidepressants overdose
Tricyclic antidepressants overdose Magnesium overdose
Magnesium overdose Dan muse
Dan muse Normal range calcium
Normal range calcium Zoplicone overdose
Zoplicone overdose Acute liver failure
Acute liver failure Opioid overdose
Opioid overdose Opioid overdose
Opioid overdose Opioid overdose
Opioid overdose Glipizide interactions
Glipizide interactions Www dcjs virginia gov
Www dcjs virginia gov Function of vitamin a
Function of vitamin a Too much caffeine symptoms
Too much caffeine symptoms Difference between virtual circuit and datagram networks
Difference between virtual circuit and datagram networks Tony wagner's seven survival skills
Tony wagner's seven survival skills Cognitive approach vs behavioral approach
Cognitive approach vs behavioral approach Waterfall vs shower approach
Waterfall vs shower approach Multiple approach avoidance conflict
Multiple approach avoidance conflict Bandura's reciprocal determinism
Bandura's reciprocal determinism What is research approach
What is research approach Traditional approach of development
Traditional approach of development Tripod position
Tripod position Dioxin poisoning
Dioxin poisoning Ld 50
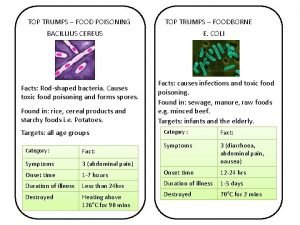
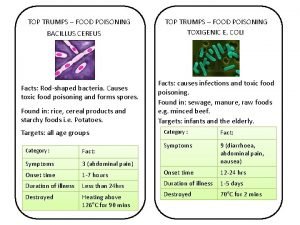
Ld 50 Top trumps food
Top trumps food Bacillus cereus symptoms
Bacillus cereus symptoms Dioxin poisoning
Dioxin poisoning Seo poisoning wikipedia
Seo poisoning wikipedia Satirical argument examples
Satirical argument examples Organophosphate poisoning
Organophosphate poisoning Methanol poisoning
Methanol poisoning Mercury poisoning symptoms
Mercury poisoning symptoms Whats lead poisoning
Whats lead poisoning Intoksikasi makanan icd 10
Intoksikasi makanan icd 10 Oxygen therapy
Oxygen therapy Food poisoning onset
Food poisoning onset Hondala poisoning
Hondala poisoning Prinso poisoning
Prinso poisoning Chapter 17:7 providing first aid for heat exposure
Chapter 17:7 providing first aid for heat exposure Bgp poisoning
Bgp poisoning Neminath hubballi
Neminath hubballi Barbiturate poisoning
Barbiturate poisoning Diya kaduru
Diya kaduru Dose of atropine in op poisoning
Dose of atropine in op poisoning