Periodontal Regeneration From Fundamentals to Potentials 2011 10
- Slides: 39
Periodontal Regeneration From Fundamentals to Potentials 2011년 10월 18일 치주과 R 1 남은희
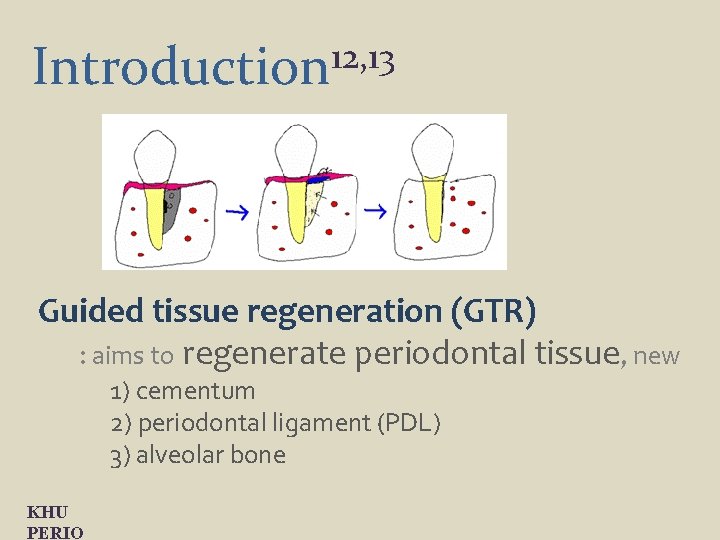
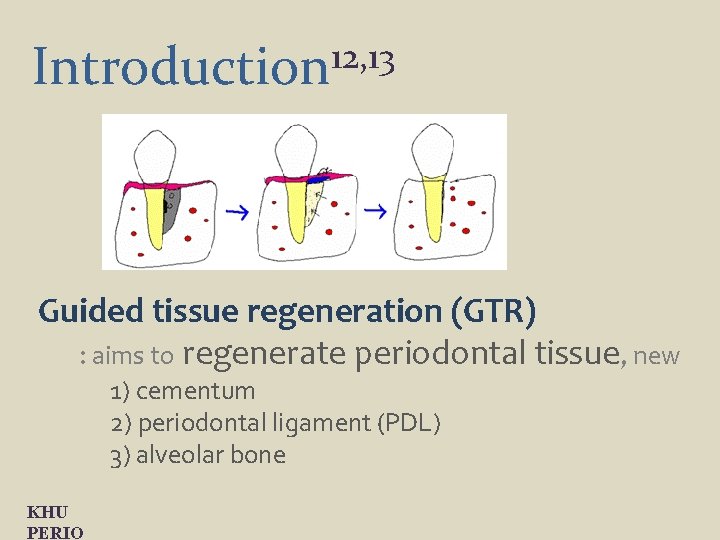
12, 13 Introduction Guided tissue regeneration (GTR) : aims to regenerate periodontal tissue, new 1) cementum 2) periodontal ligament (PDL) 3) alveolar bone KHU PERIO
Long-term stability of clinical attachment following GTR 6, 12, 13 GTR has become a predictable procedure to increase periodontal support by, 1) improved CAL, 2) reduced PD, 3) less gingival recession, 4) hard tissue gain. GTR treated sites have the same susceptibility to periodontal breakdown as root planing treated ones. (cortellini et al. 1996) KHU PERIO
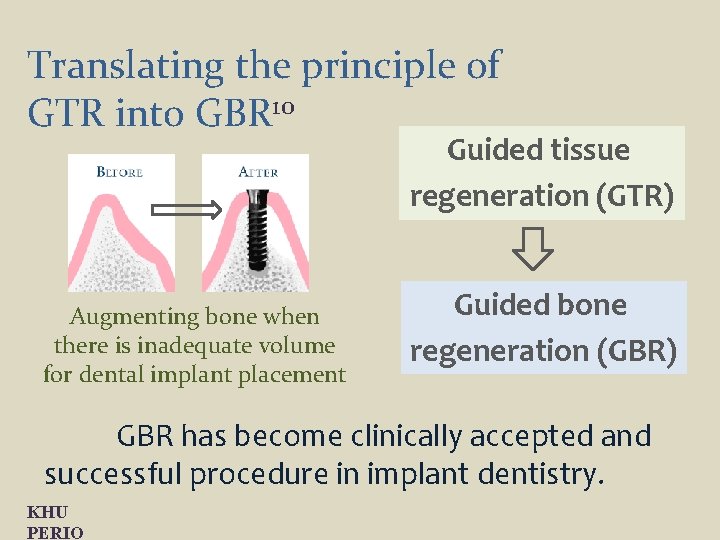
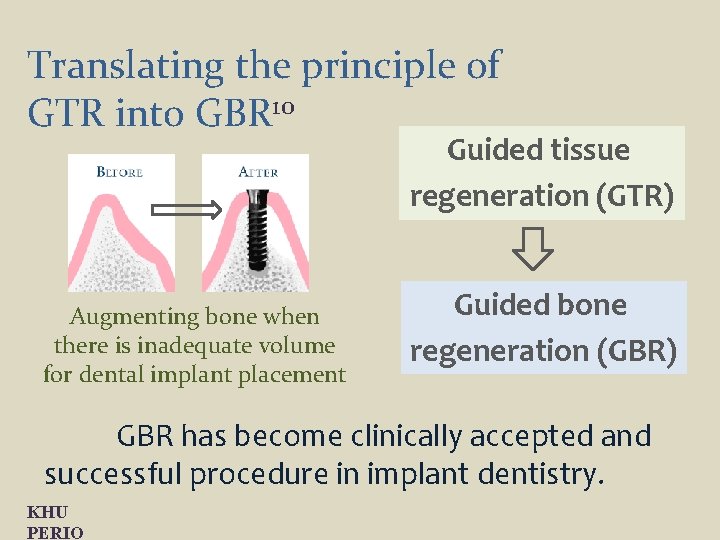
Translating the principle of GTR into GBR 10 Guided tissue regeneration (GTR) Augmenting bone when there is inadequate volume for dental implant placement Guided bone regeneration (GBR) GBR has become clinically accepted and successful procedure in implant dentistry. KHU PERIO
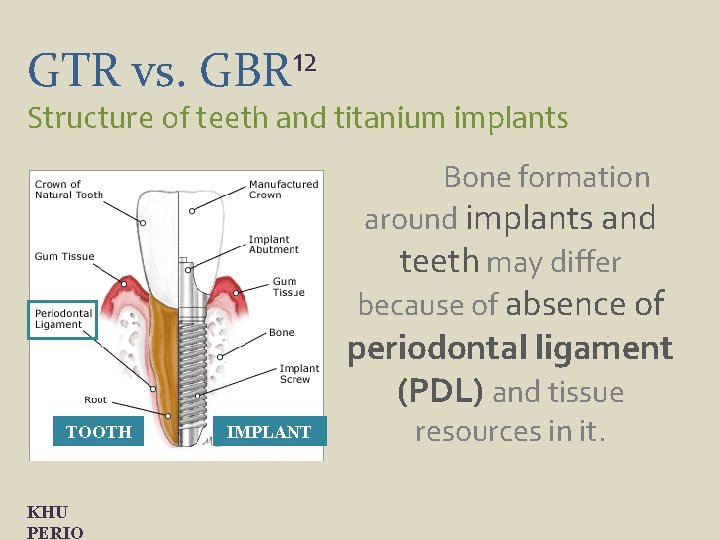
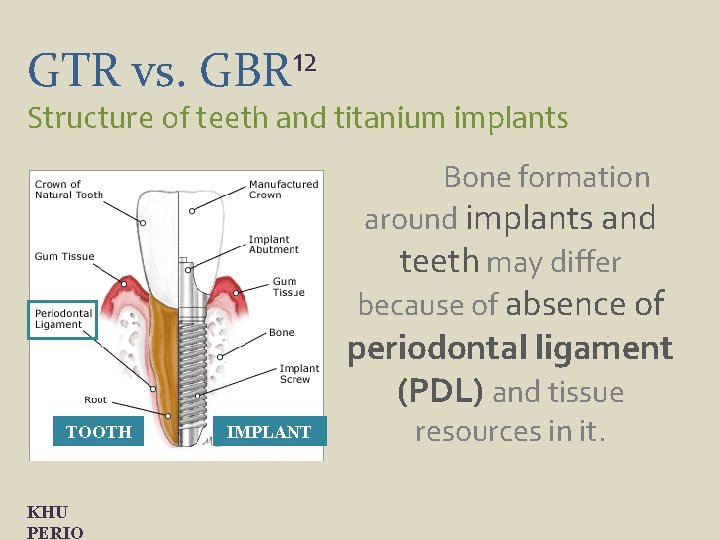
GTR vs. 12 GBR Structure of teeth and titanium implants Bone formation around implants and teeth may differ because of absence of periodontal ligament (PDL) and tissue TOOTH KHU PERIO IMPLANT resources in it.
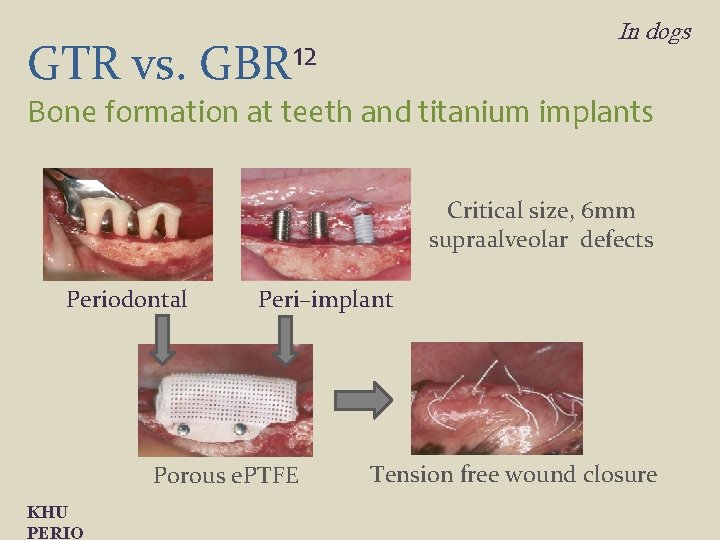
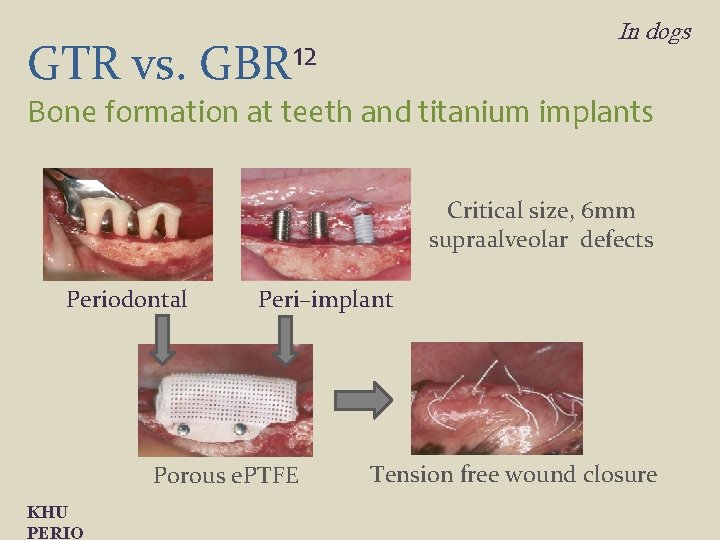
In dogs GTR vs. GBR 12 Bone formation at teeth and titanium implants Critical size, 6 mm supraalveolar defects Periodontal Peri–implant Porous e. PTFE KHU PERIO Tension free wound closure
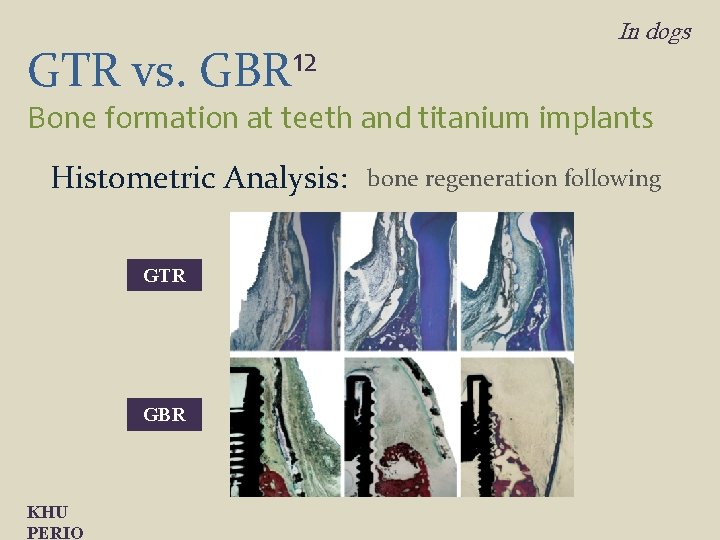
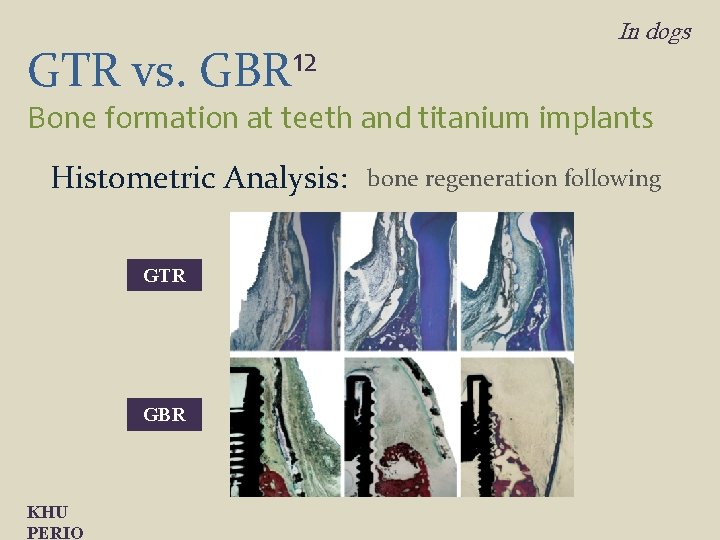
GTR vs. 12 GBR In dogs Bone formation at teeth and titanium implants Histometric Analysis: GTR GBR KHU PERIO bone regeneration following
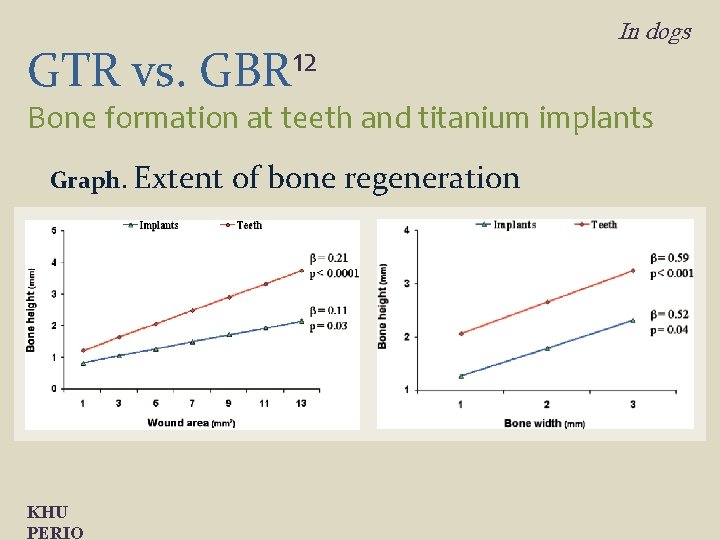
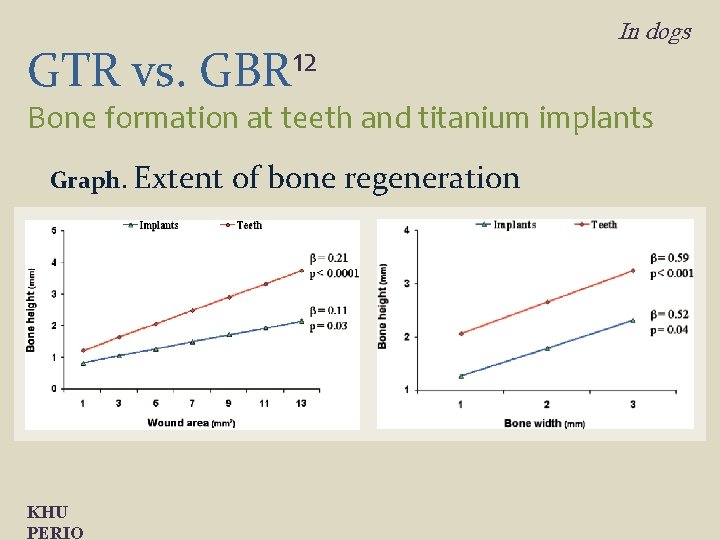
GTR vs. 12 GBR In dogs Bone formation at teeth and titanium implants Graph. Extent KHU PERIO of bone regeneration
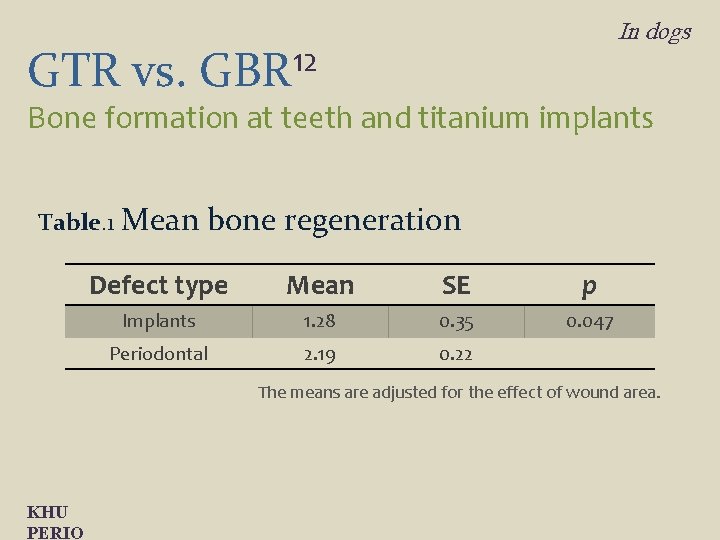
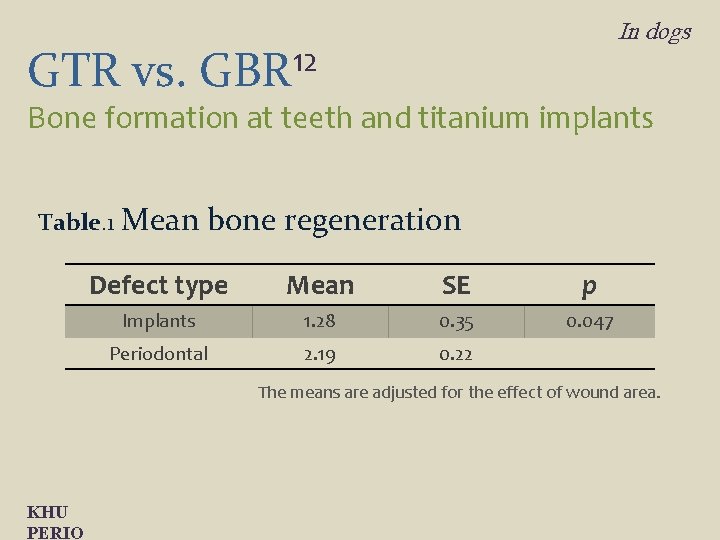
GTR vs. In dogs 12 GBR Bone formation at teeth and titanium implants Table. 1 Mean bone regeneration Defect type Mean SE p Implants 1. 28 0. 35 0. 047 Periodontal 2. 19 0. 22 The means are adjusted for the effect of wound area. KHU PERIO
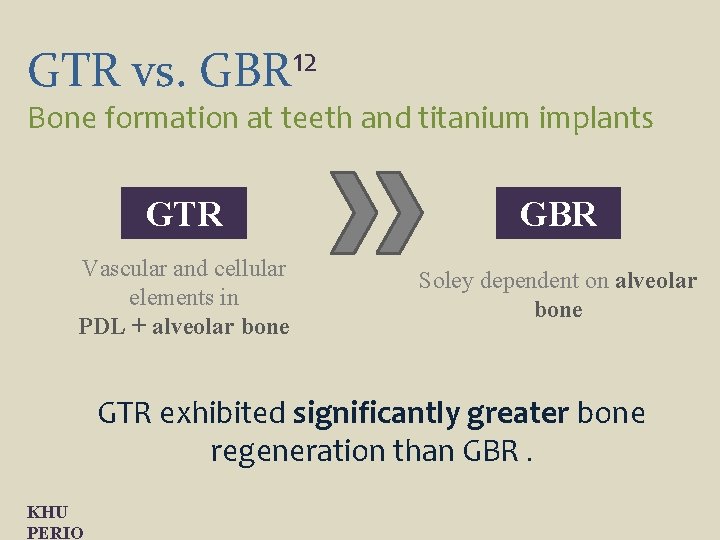
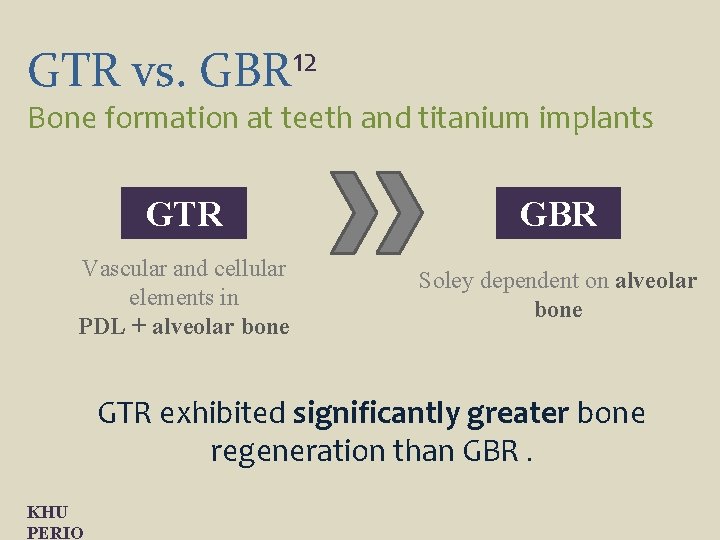
GTR vs. 12 GBR Bone formation at teeth and titanium implants GTR GBR Vascular and cellular elements in PDL + alveolar bone Soley dependent on alveolar bone GTR exhibited significantly greater bone regeneration than GBR. KHU PERIO
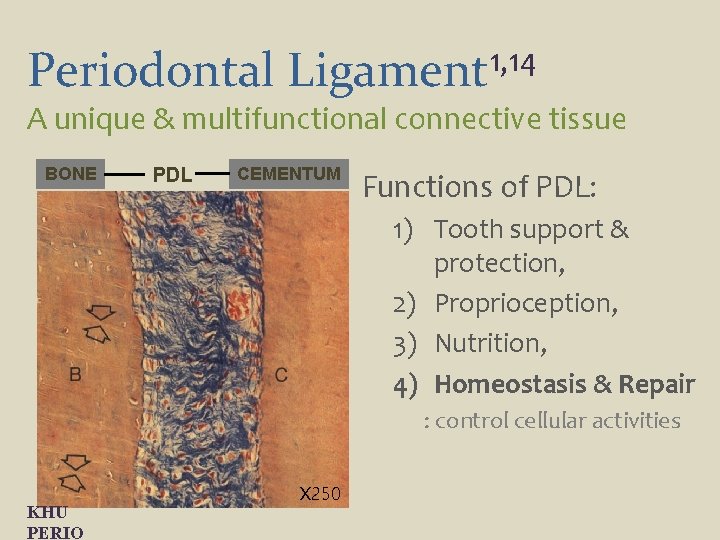
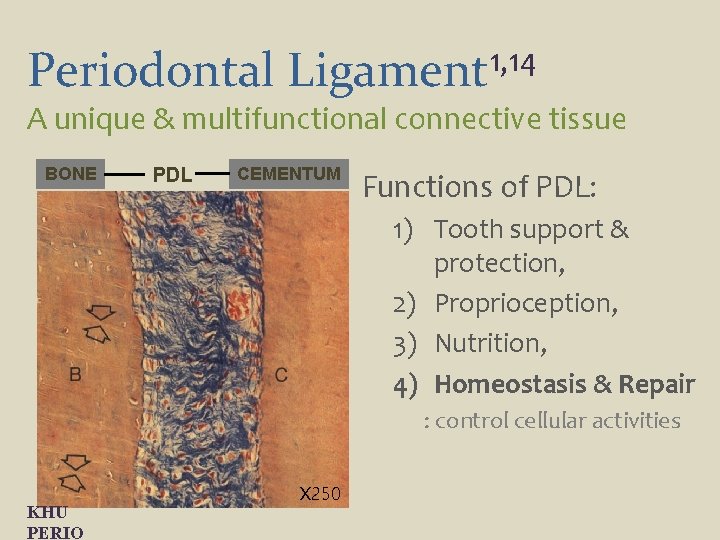
Periodontal 1, 14 Ligament A unique & multifunctional connective tissue BONE PDL CEMENTUM Functions of PDL: 1) Tooth support & protection, 2) Proprioception, 3) Nutrition, 4) Homeostasis & Repair : control cellular activities KHU PERIO X 250
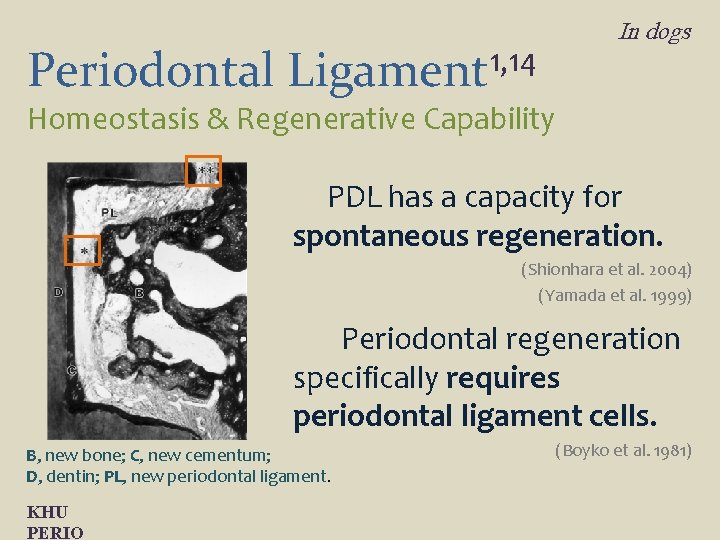
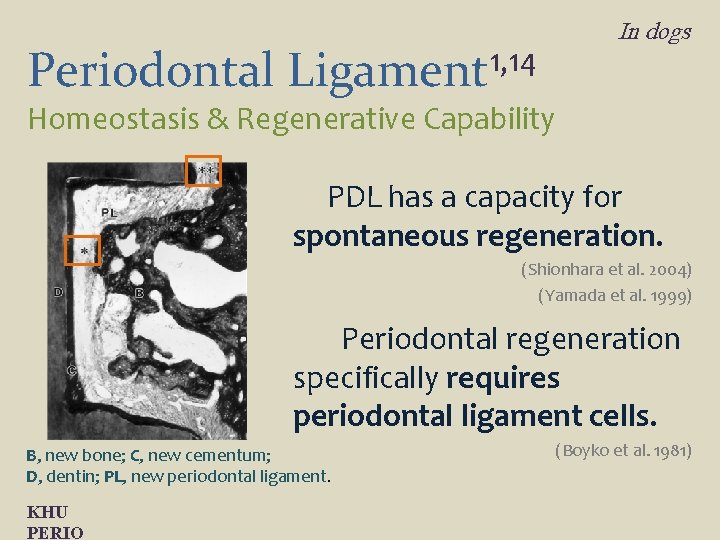
Periodontal 1, 14 Ligament In dogs Homeostasis & Regenerative Capability PDL has a capacity for spontaneous regeneration. (Shionhara et al. 2004) (Yamada et al. 1999) Periodontal regeneration specifically requires periodontal ligament cells. B, new bone; C, new cementum; D, dentin; PL, new periodontal ligament. KHU PERIO (Boyko et al. 1981)
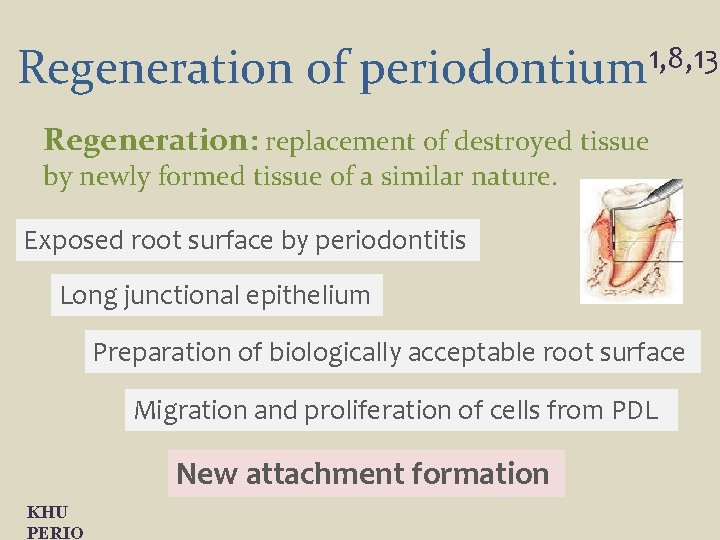
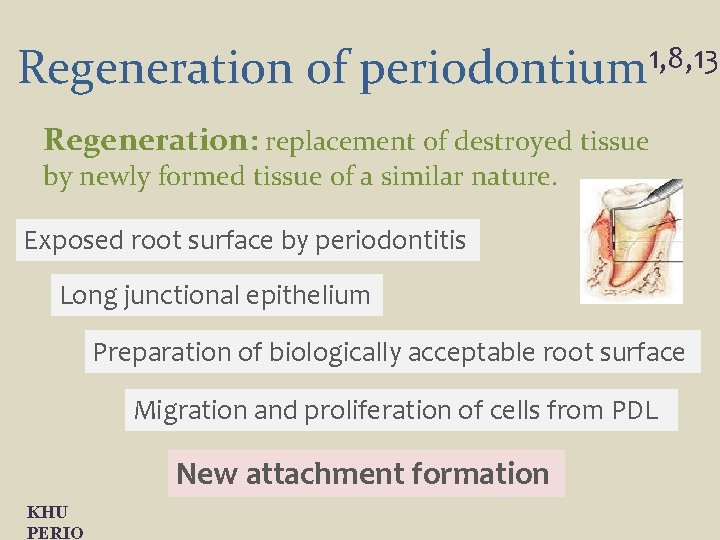
Regeneration of periodontium 1, 8, 13 Regeneration: replacement of destroyed tissue by newly formed tissue of a similar nature. Exposed root surface by periodontitis Long junctional epithelium Preparation of biologically acceptable root surface Migration and proliferation of cells from PDL New attachment formation KHU PERIO
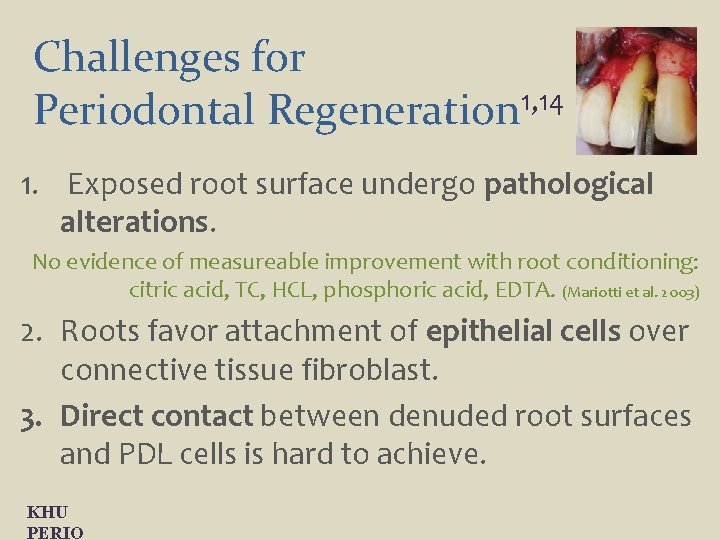
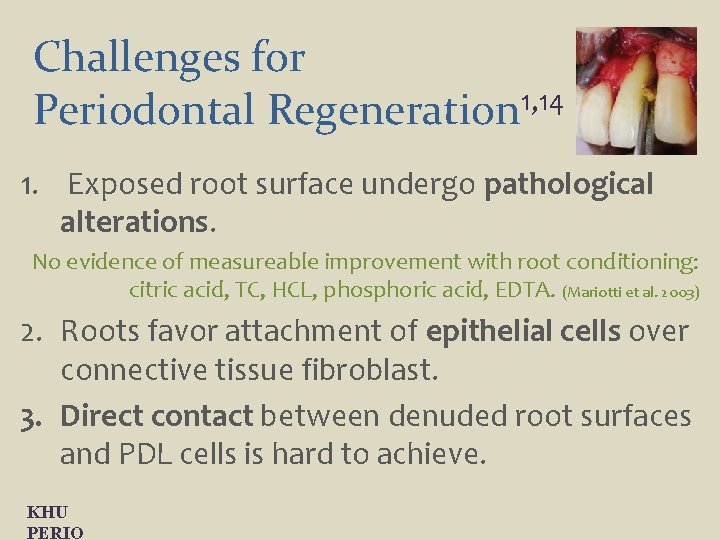
Challenges for Periodontal Regeneration 1, 14 1. Exposed root surface undergo pathological alterations. No evidence of measureable improvement with root conditioning: citric acid, TC, HCL, phosphoric acid, EDTA. (Mariotti et al. 2003) 2. Roots favor attachment of epithelial cells over connective tissue fibroblast. 3. Direct contact between denuded root surfaces and PDL cells is hard to achieve. KHU PERIO
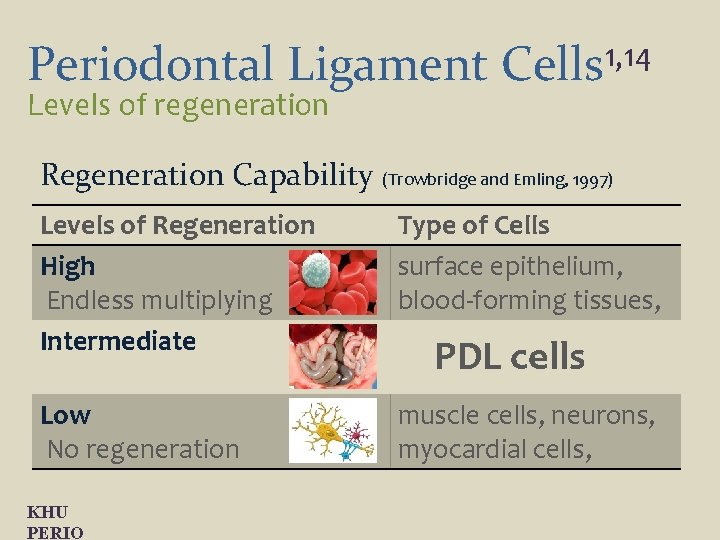
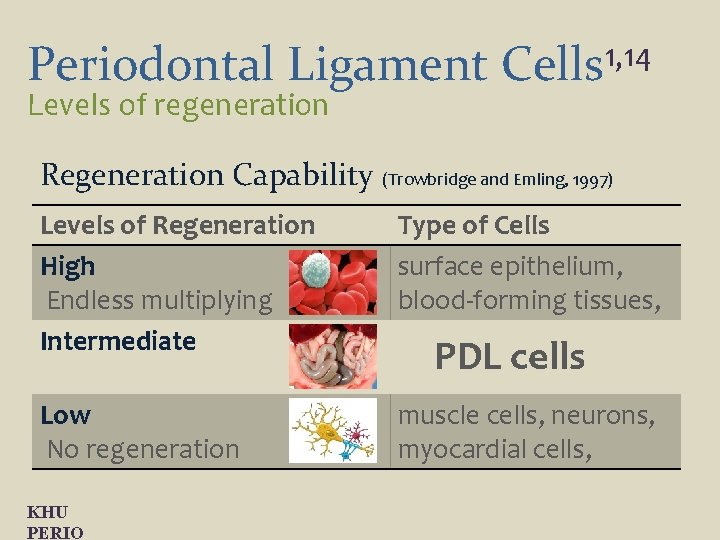
Periodontal Ligament Levels of regeneration 1, 14 Cells Regeneration Capability (Trowbridge and Emling, 1997) Levels of Regeneration High Endless multiplying Intermediate Low No regeneration KHU PERIO Type of Cells surface epithelium, blood-forming tissues, visceral organs, PDL cells mesenchymal cells muscle cells, neurons, myocardial cells,
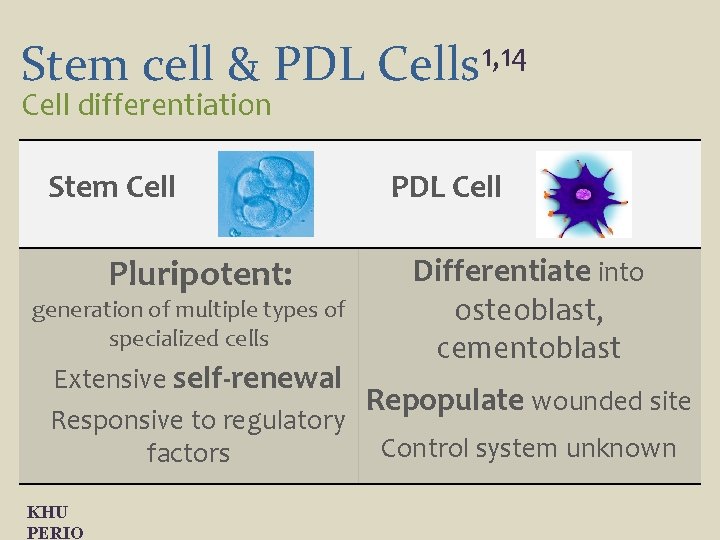
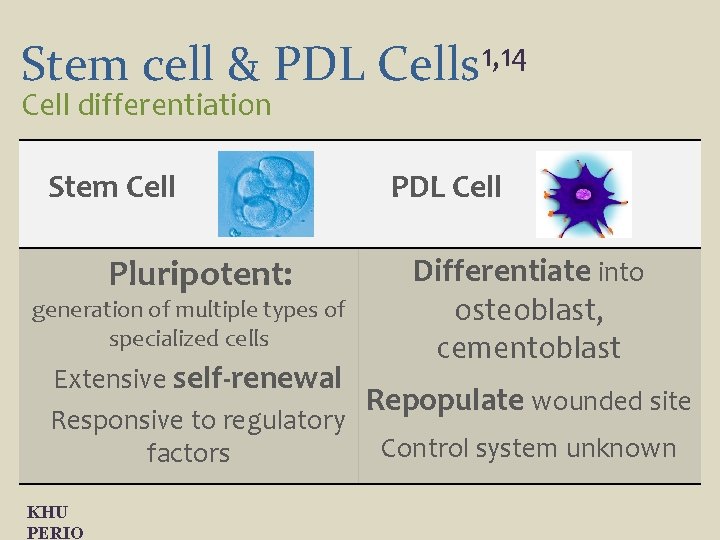
Stem cell & PDL Cell differentiation Stem Cell Pluripotent: generation of multiple types of specialized cells 1, 14 Cells PDL Cell Differentiate into osteoblast, cementoblast Extensive self-renewal Repopulate wounded site Responsive to regulatory Control system unknown factors KHU PERIO
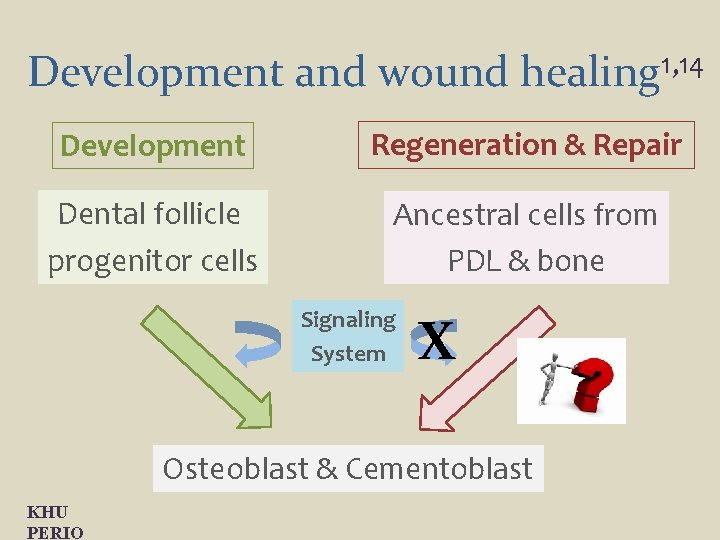
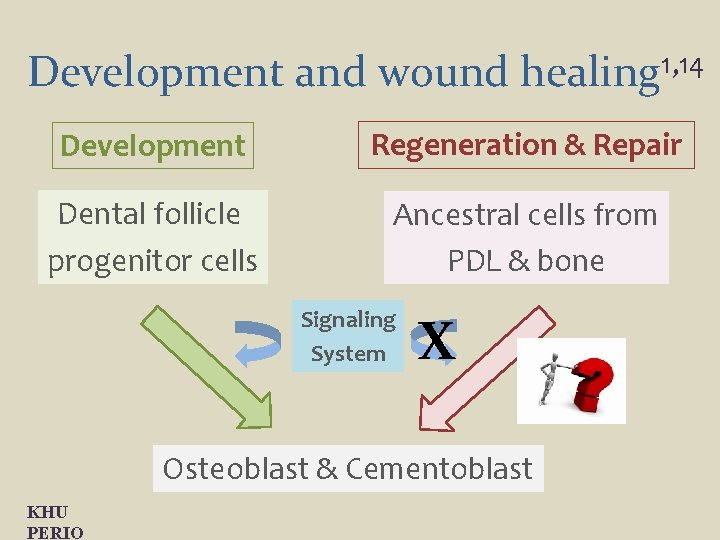
Development and wound healing 1, 14 Development Regeneration & Repair Dental follicle progenitor cells Ancestral cells from PDL & bone Signaling System X Osteoblast & Cementoblast KHU PERIO
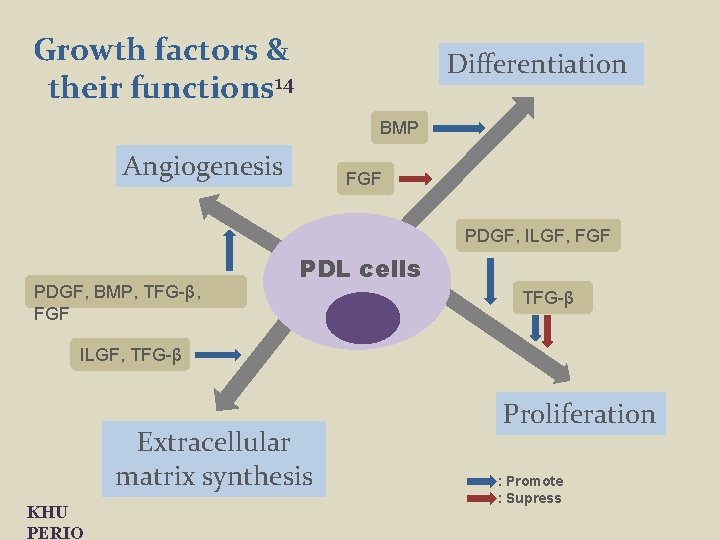
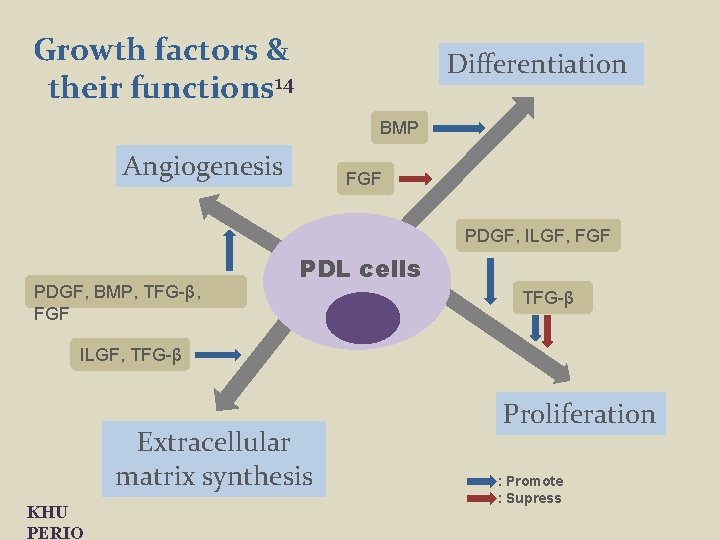
Growth factors & their functions 14 Differentiation BMP Angiogenesis FGF PDGF, ILGF, FGF PDGF, BMP, TFG-β, FGF PDL cells TFG-β ILGF, TFG-β Extracellular matrix synthesis KHU PERIO Proliferation : Promote : Supress
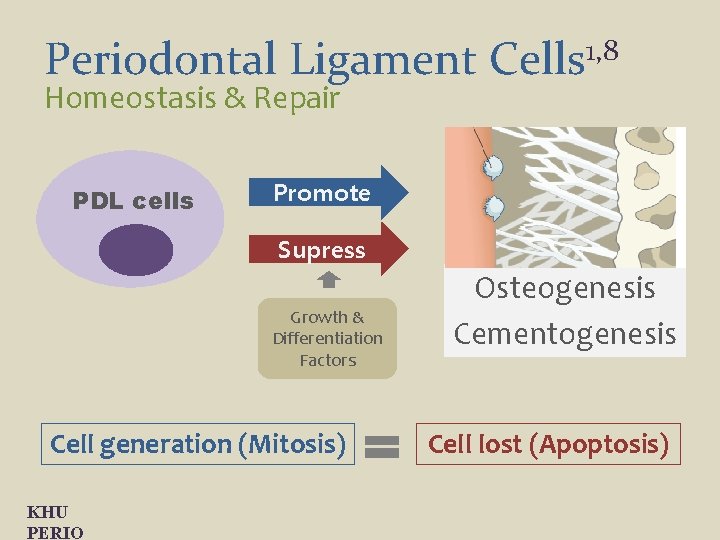
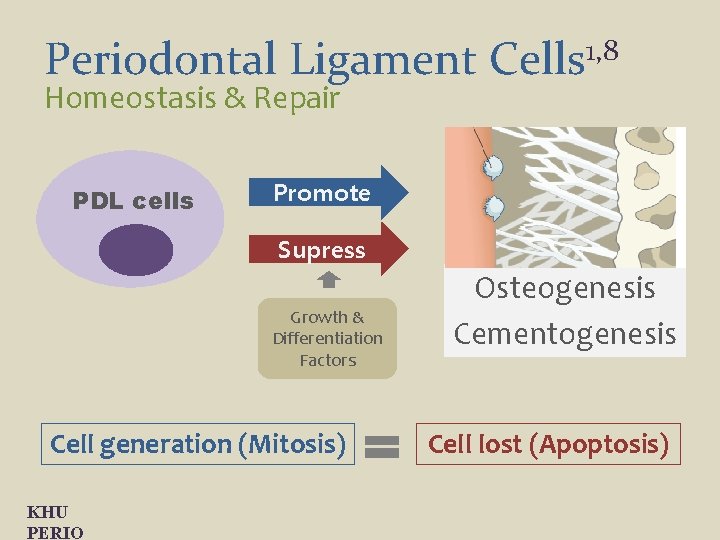
Periodontal Ligament Cells 1, 8 Homeostasis & Repair PDL cells Promote Supress Growth & Differentiation Factors Cell generation (Mitosis) KHU PERIO Osteogenesis Cementogenesis Cell lost (Apoptosis)
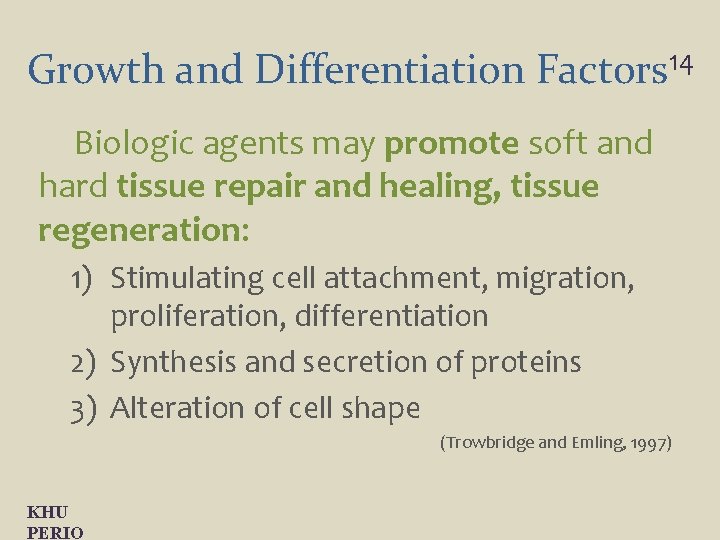
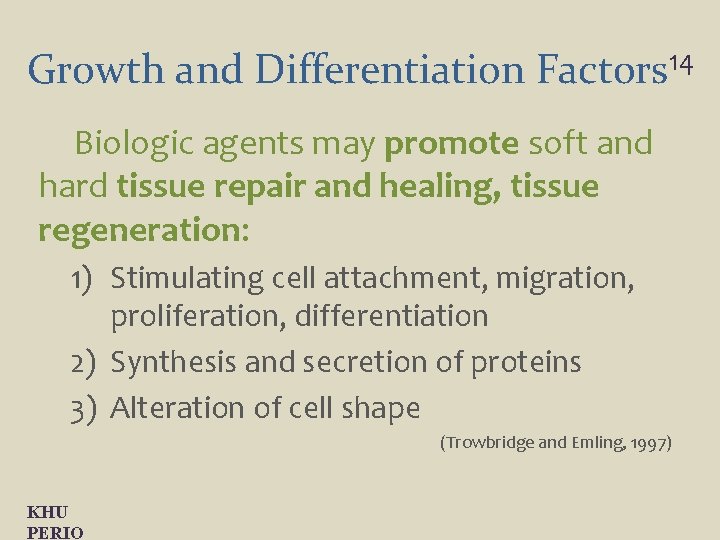
Growth and Differentiation Factors 14 Biologic agents may promote soft and hard tissue repair and healing, tissue regeneration: 1) Stimulating cell attachment, migration, proliferation, differentiation 2) Synthesis and secretion of proteins 3) Alteration of cell shape (Trowbridge and Emling, 1997) KHU PERIO
Growth and Differentiation Factors 14 How effective are they
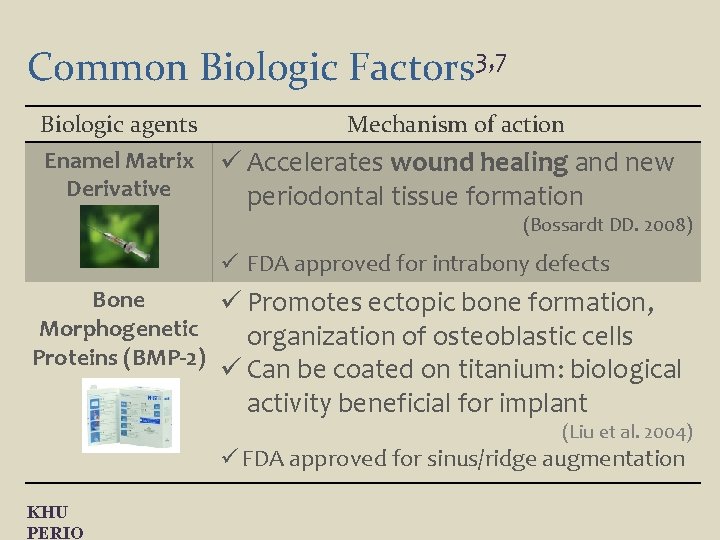
Common Biologic Factors 3, 7 Biologic agents Enamel Matrix Derivative (EMD) Mechanism of action ü Accelerates wound healing and new periodontal tissue formation (Bossardt DD. 2008) ü FDA approved for intrabony defects Bone ü Promotes ectopic bone formation, Morphogenetic organization of osteoblastic cells Proteins (BMP-2) ü Can be coated on titanium: biological activity beneficial for implant (Liu et al. 2004) ü FDA approved for sinus/ridge augmentation KHU PERIO
Common Biologic Factors 3, 7 Biologic agents Platelet-Rich Fibrin (PRF) Mechanism of action üContains high amounts of bioactive growth factors to enhance wound healing: (Cochran & Wozney 1999) Platelet-Derived üStimulates the regenerative potential Growth Factor of periodontal tissues (PDGF) (Dereka et al. 2006) üFDA approved for intrabony defects, furcation, gingival recession KHU PERIO
Common Biologic Factors 3, 7 Biologic agents Mechanism of action Fibroblast ü Stimulates angiogenesis and mitosis of Growth Factor mesenchymal cells (FGF-2) ü Not commercially available ü No FDA approval Parathyroid ü Endogenous hormone: catabolic / anabolic Hormone (PTH) properties in bone ü Promoted periodontal regeneration in infrabony defects (Bashutski et al. 2010) ü FDA approval only for the treatment of osteoporosis KHU PERIO
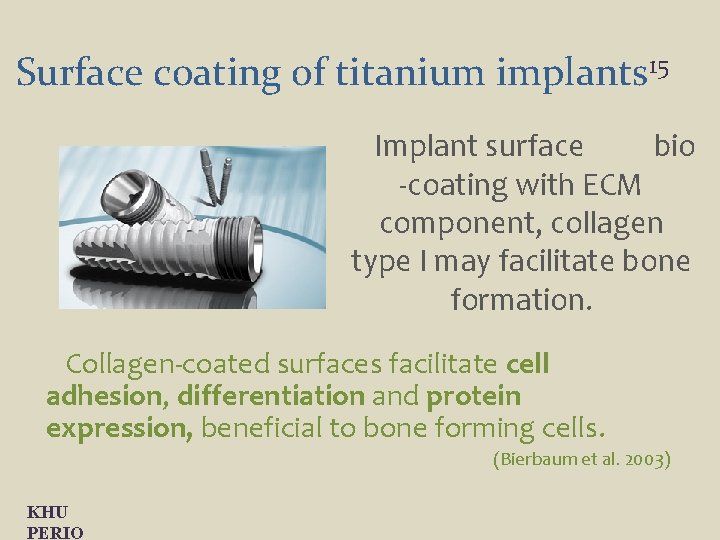
Surface coating of titanium implants 15 Implant surface bio -coating with ECM component, collagen type I may facilitate bone formation. Collagen-coated surfaces facilitate cell adhesion, differentiation and protein expression, beneficial to bone forming cells. (Bierbaum et al. 2003) KHU PERIO
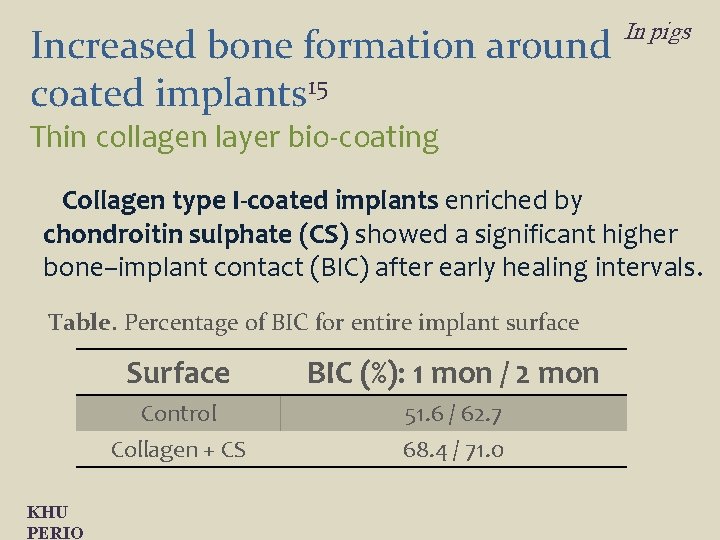
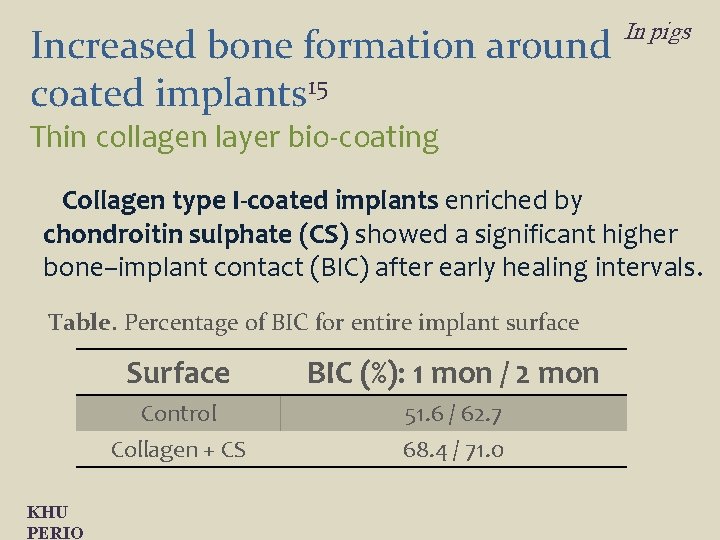
Increased bone formation around coated implants 15 In pigs Thin collagen layer bio-coating Collagen type I-coated implants enriched by chondroitin sulphate (CS) showed a significant higher bone–implant contact (BIC) after early healing intervals. Table. Percentage of BIC for entire implant surface KHU PERIO Surface BIC (%): 1 mon / 2 mon Control Collagen + CS 51. 6 / 62. 7 68. 4 / 71. 0
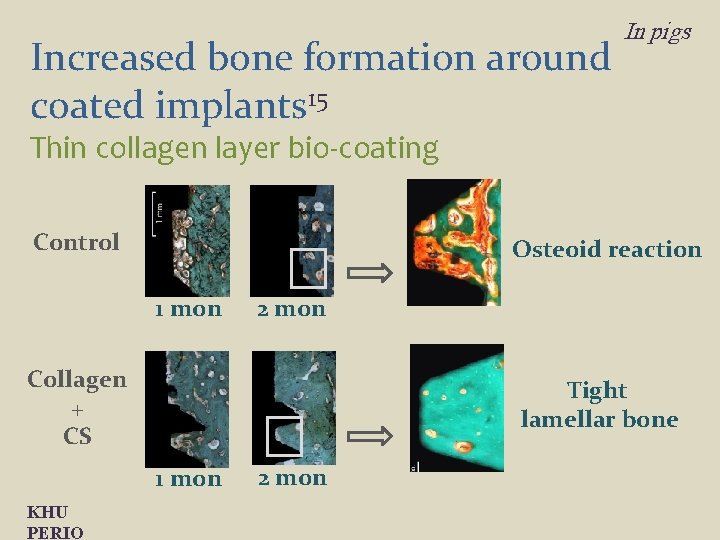
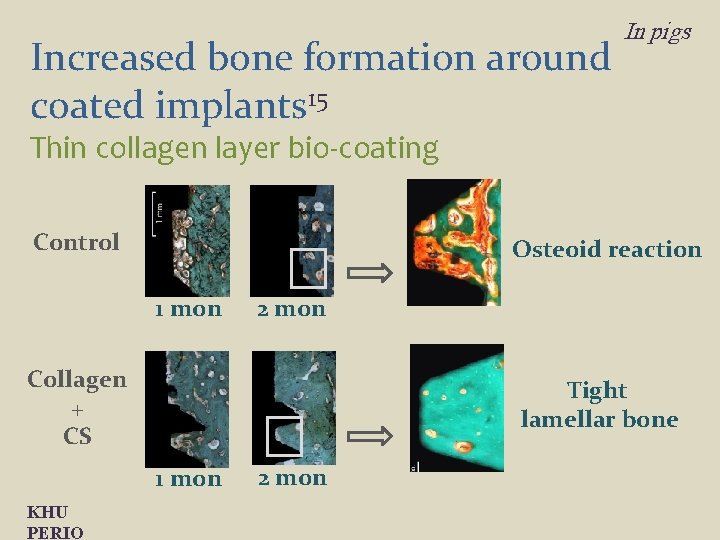
Increased bone formation around coated implants 15 In pigs Thin collagen layer bio-coating Control Osteoid reaction 1 mon 2 mon Collagen + CS Tight lamellar bone 1 mon KHU PERIO 2 mon
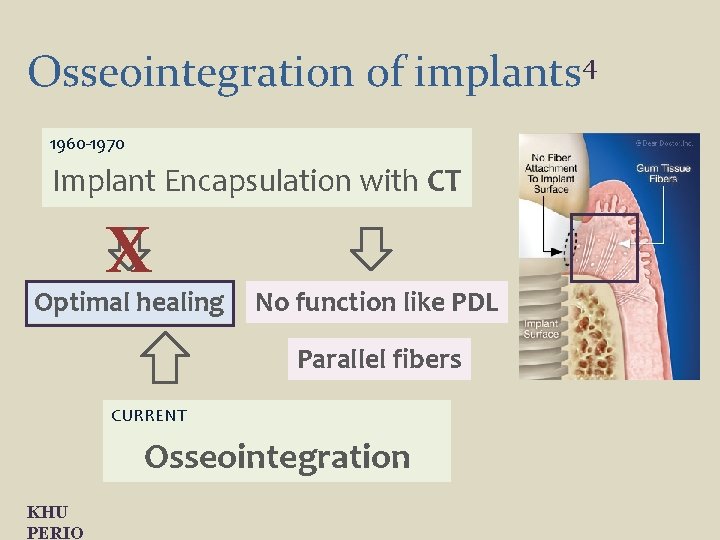
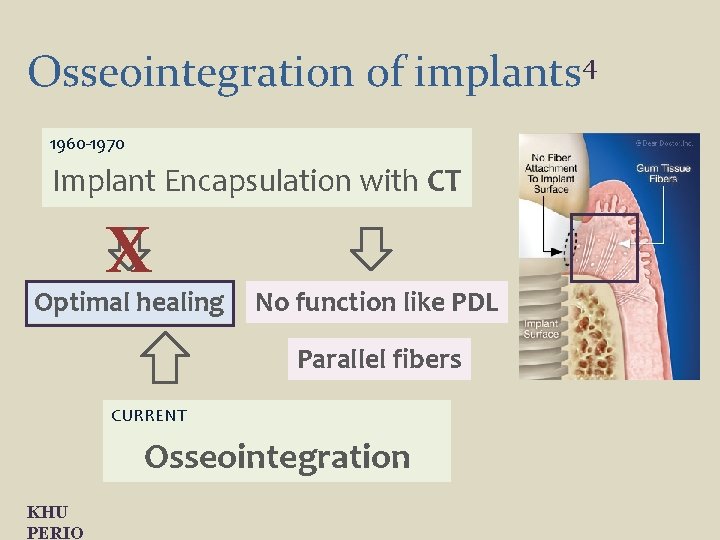
Osseointegration of implants 4 1960 -1970 Implant Encapsulation with CT X Optimal healing No function like PDL Parallel fibers CURRENT Osseointegration KHU PERIO
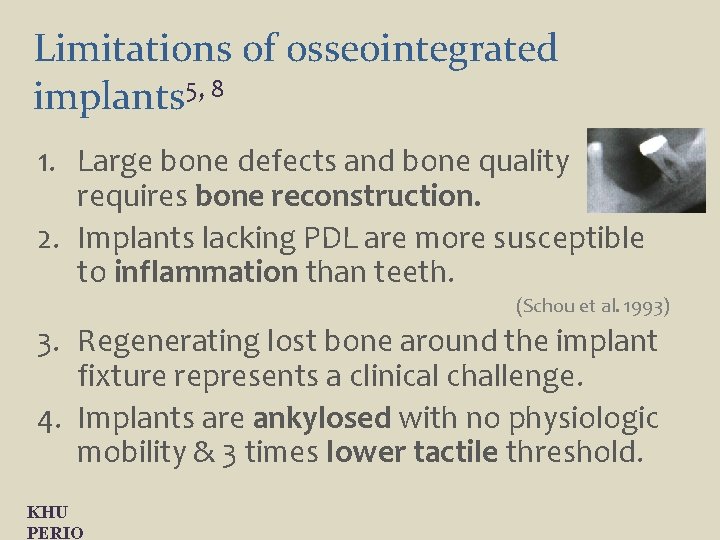
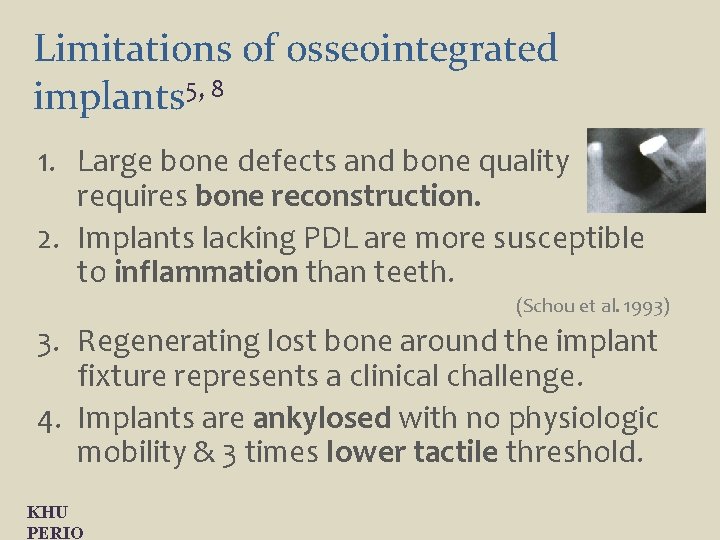
Limitations of osseointegrated implants 5, 8 1. Large bone defects and bone quality requires bone reconstruction. 2. Implants lacking PDL are more susceptible to inflammation than teeth. (Schou et al. 1993) 3. Regenerating lost bone around the implant fixture represents a clinical challenge. 4. Implants are ankylosed with no physiologic mobility & 3 times lower tactile threshold. KHU PERIO
PDL would allow more dynamic role for oral implants. Implant KHU PERIO Periodontal Ligament Cells
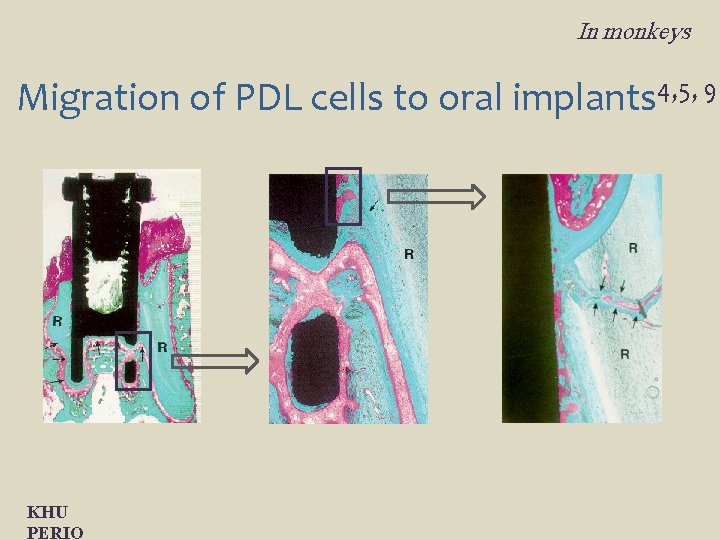
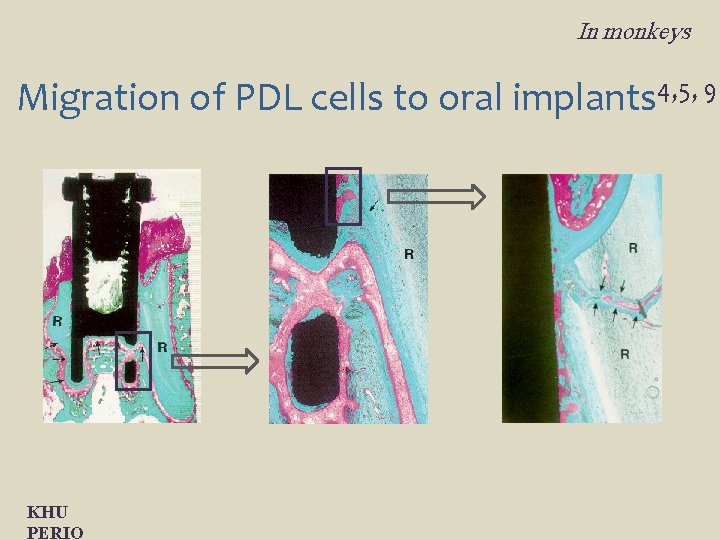
In monkeys Migration of PDL cells to oral implants 4, 5, 9 KHU PERIO
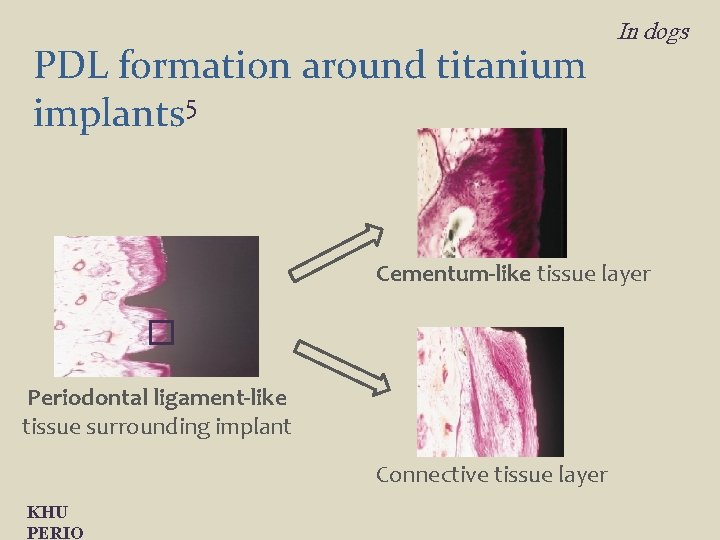
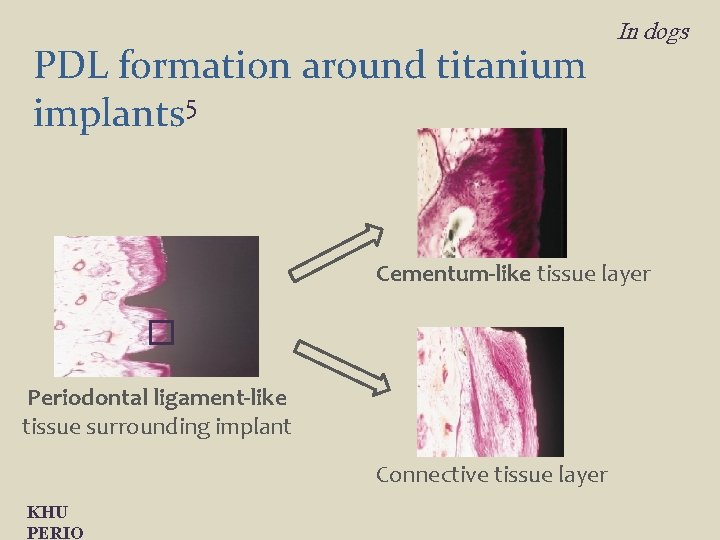
PDL formation around titanium implants 5 In dogs Cementum-like tissue layer Periodontal ligament-like tissue surrounding implant Connective tissue layer KHU PERIO
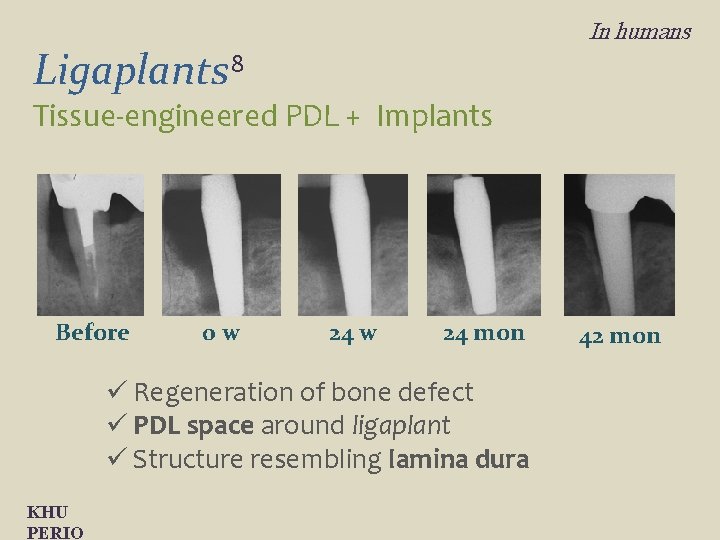
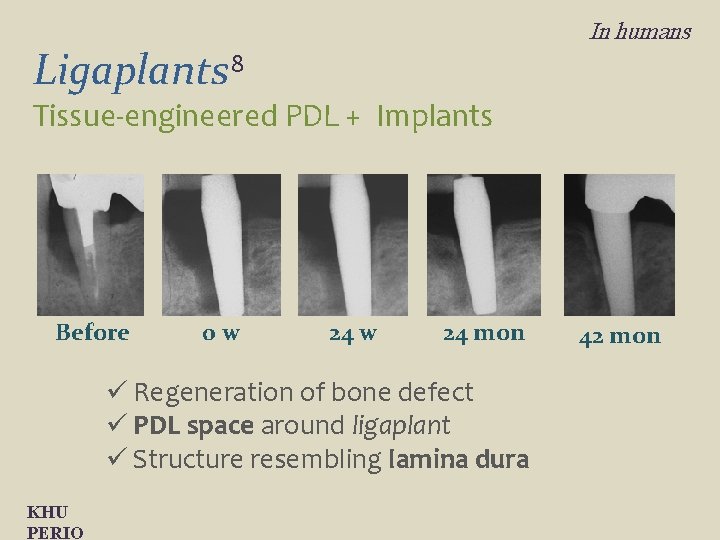
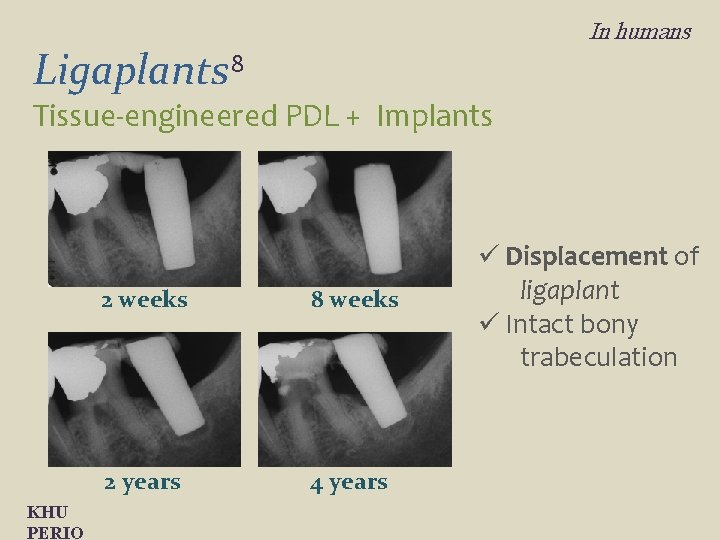
In humans Ligaplants 8 Tissue-engineered PDL + Implants Before 0 w 24 mon ü Regeneration of bone defect ü PDL space around ligaplant ü Structure resembling lamina dura KHU PERIO 42 mon
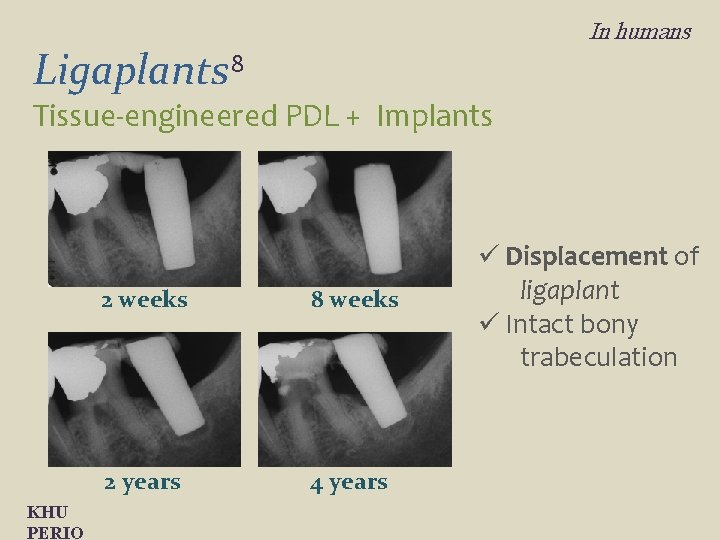
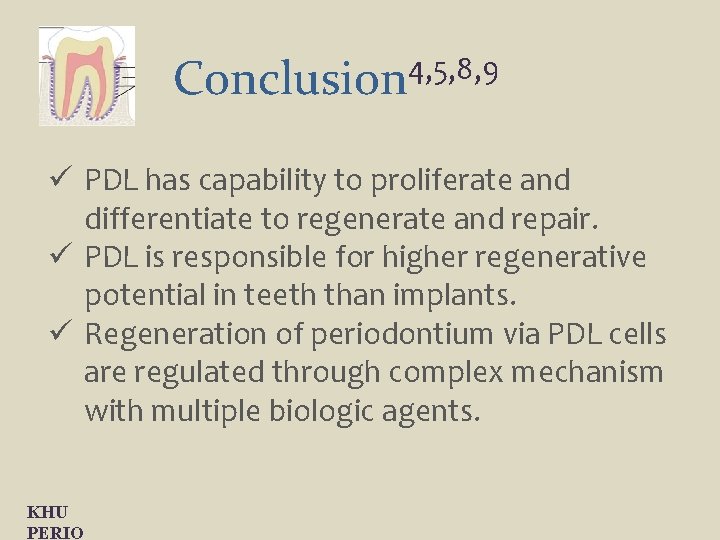
In humans Ligaplants 8 Tissue-engineered PDL + Implants KHU PERIO 2 weeks 8 weeks 2 years 4 years ü Displacement of ligaplant ü Intact bony trabeculation
4, 5, 8, 9 Conclusion ü PDL has capability to proliferate and differentiate to regenerate and repair. ü PDL is responsible for higher regenerative potential in teeth than implants. ü Regeneration of periodontium via PDL cells are regulated through complex mechanism with multiple biologic agents. KHU PERIO
4, 5, 8, 9 Conclusion ü Tissue engineering is currently emerging field in regenerative periodontics. ü Studies on clinical efficacy of various biologic agents and direct application of PDL cells in implant dentistry have shown great potentials. ü Further technical development is required in tissue engineering in before routine clinical use. KHU PERIO
References 1. 2. 3. 4. 5. Beertsen et al. The periodontal ligament: a unique, multifunctional connective tissue. Periodontology 2000 1997; 13; 20 -40. Behring et al. Toward guided tissue and bone regeneration: morphology, attachment, proliferation, and migration of cells cultured on collagen barrier membranes. A systematic review. Odontology 2008; 96; 1 -11. Bashutski & Wang. Biologic agents to promote periodontal regeneration and bone augmentation. Clin Adv Periodontics 2011; 1; 80 -87. Buser et al. Titanium implants with a true periodontal ligament: An Alternative to Osseointegrated Implants? Int J Oral Maxillofac Implants 1990; 5; 113 -116. Choi BH. Periodontal ligament formation around titanium implants using cultured periodontal ligament cells: A pilot study. Int J Oral Maxillofac Implants 2000; 15; 193 -196. KHU PERIO
References 6. Cortellini et al. Long-term stability of clinical attachemt following guided tissue regeneration and conventional therapy. J Clin Periodontol 1996; 23; 106 -111. 7. Ellingsen et al. Advances in dental implant materials and tissue regeneration. Periodontology 2000 2006; 41; 136 -156. 8. Gualt et al. Tissue-engineered ligament: implant constructs for tooth replacement. J Clin Periodontol 2010; 37; 750 -758. 9. Giannobile et al. Getting to the Root of dental implant tissue engineering. J Clin Periodontol 2010; 37; 747 -749. 10. Hämmerle & Karring. Guided bone regeneration at oral implant sites. Periodontology 2000 1998; 17; 151 -175. 11. Nidleman et al. Guided tissue regeneration for periodontal infrabony defects. Cochrane Database of Systematic Reviews 2006, Issue 2. [Art. No. : CD 001724. ] KHU PERIO
References 12. Polimeni et al. Prognostic factors for alveolar regeneration: bone formation at teeth and titanium implants. J Clin Periodontol 2004; 31; 927 -932. 13. Polimeni et al. Biology and principles of periodontal wound healing/regeneration. Periodontology 2000 2006; 41; 30 -47. 14. Shimono et al. Regulatory mechanisms of periodontal regeneration. Microsc Res Tech 2003; 60; 491 -502. 15. Stadlinger et al. Increased bone formation around coated implants. J Clin Periodontol 2009; 36; 698 -704. 16. van Steenberghe D. From osseointegration to osseoperception. J Dent Res 2000; 79; 1833 -1837. KHU PERIO
 Heredity
Heredity Nottingham redevelopment
Nottingham redevelopment T-s diagram brayton cycle
T-s diagram brayton cycle Regeneration in gas turbine
Regeneration in gas turbine Gas turbine with regeneration
Gas turbine with regeneration Fiat doblo dpf regeneration procedure
Fiat doblo dpf regeneration procedure Cellules ciliées régénération
Cellules ciliées régénération London docklands regeneration
London docklands regeneration Planarian regeneration
Planarian regeneration Guided tissue regenration
Guided tissue regenration Objectives of artificial regeneration
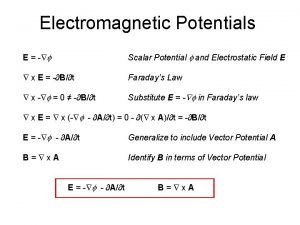
Objectives of artificial regeneration Maxwell relation
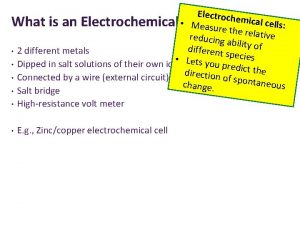
Maxwell relation Table of standard reduction potentials
Table of standard reduction potentials Types of graded potentials
Types of graded potentials Two protons one after the other are launched
Two protons one after the other are launched Use the tabulated half-cell potentials to calculate
Use the tabulated half-cell potentials to calculate Thermodynamic potentials
Thermodynamic potentials Lienard-wiechert potentials
Lienard-wiechert potentials Describe characteristics
Describe characteristics What are electrical synapses
What are electrical synapses Function of synapse
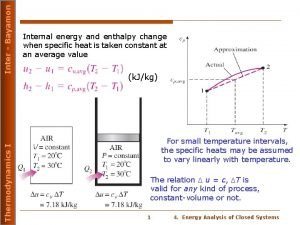
Function of synapse Cp in thermodynamics
Cp in thermodynamics Cathode anode standard reduction potential
Cathode anode standard reduction potential Thermodynamic potentials
Thermodynamic potentials Source of bioelectric potential
Source of bioelectric potential Postsynaptic potentials
Postsynaptic potentials Scalar magnetic potential
Scalar magnetic potential Task 8 electrode potentials answers
Task 8 electrode potentials answers Periodontal cep
Periodontal cep Kista primordial adalah
Kista primordial adalah Histodiferansiyon
Histodiferansiyon Biopulpectomía y necropulpectomía
Biopulpectomía y necropulpectomía Indikasi gingivektomi
Indikasi gingivektomi Maintenance phase of periodontal therapy
Maintenance phase of periodontal therapy Politür patı
Politür patı Seccin 7
Seccin 7 Plicae digestive system
Plicae digestive system Periodontal abscess
Periodontal abscess Glickman's concept
Glickman's concept Russell periodontal index
Russell periodontal index