Perinatal Periods of Risk Introduction Overview 2012 Carol





- Slides: 66
Perinatal Periods of Risk: Introduction & Overview 2012 Carol Gilbert, BS, MS, Data Analyst, City. Mat. CH 1
• City. Mat. CH Mission: Improving the health and well-being of urban women, children and families by strengthening the public health organizations and leaders in their communities • PPOR is an approach for investigating high infant mortality rates in cities. • Thanks to Dr. Magda Peck, Dr. William Sappenfield, Dr. Brian Mc. Carthy, Patrick Simpson, Jennifer Skala, Dr. Laurin Kasehagen, and City. Mat. CH Member Health Departments across the USA 2
Not every city can do PPOR. You need: 1. At least 60 deaths in at most a 5 -year period 2. Three vital records data files (deaths, births, fetal deaths) 3. You need someone who knows what to do with the data files 3
Why do we need PPOR? Infant mortality is complex Important time periods • Preconception health • Prenatal • Neonatal • Post-neonatal • Life course • Intergenerational Goes beyond medical • Chronic disease prevention • Behavioral health • Social determinants • Health care system • Environment • Built Environment • Education system • Justice system … 4
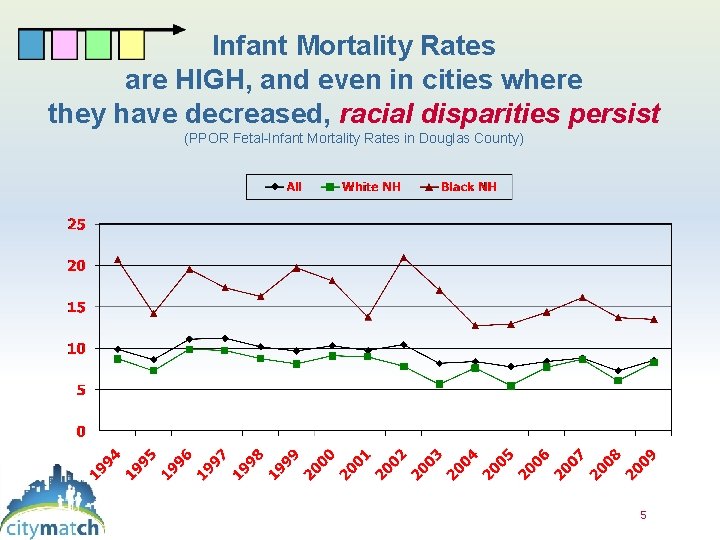
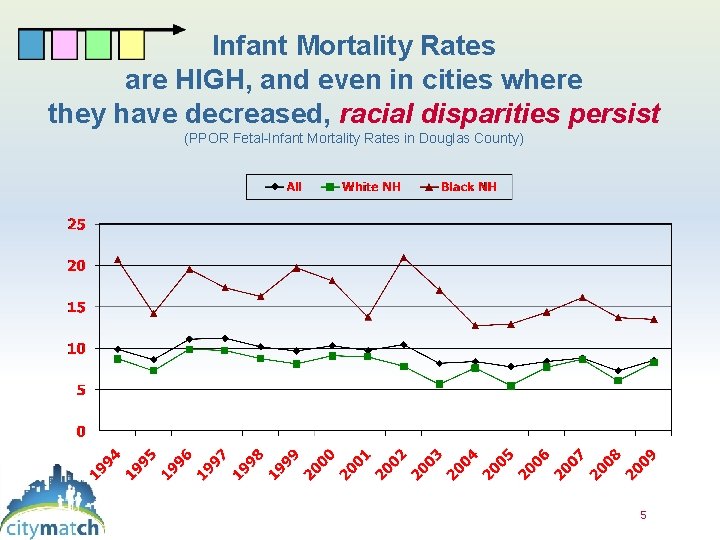
Infant Mortality Rates are HIGH, and even in cities where they have decreased, racial disparities persist (PPOR Fetal-Infant Mortality Rates in Douglas County) 5
Communities needed help! 6

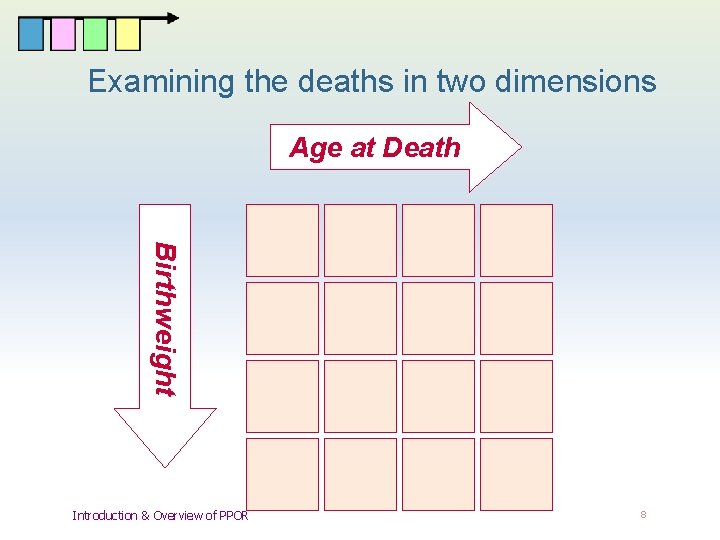
Causes of infant and fetal death are closely related to both age at death and birth weight. Why not use both pieces of information simultaneously, to learn more about why babies are dying ? The PPOR approach examines fetal and infant mortality in two dimensions 7
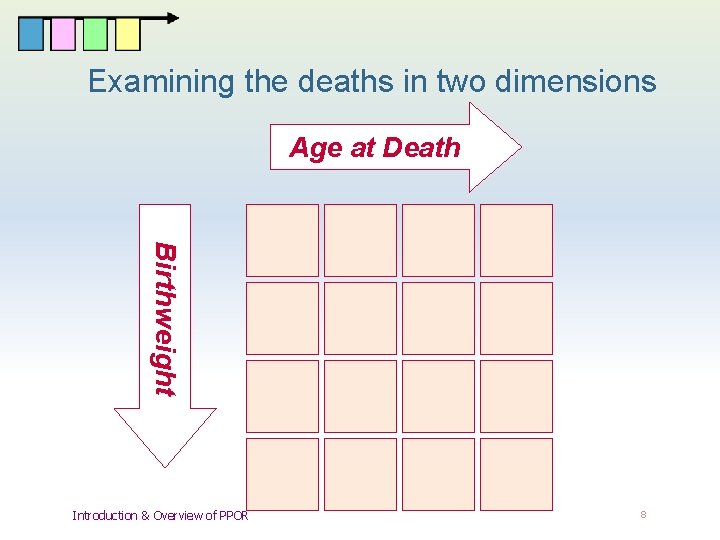
Examining the deaths in two dimensions Age at Death Birthweight Introduction & Overview of PPOR 10 11 12 14 15 16 8
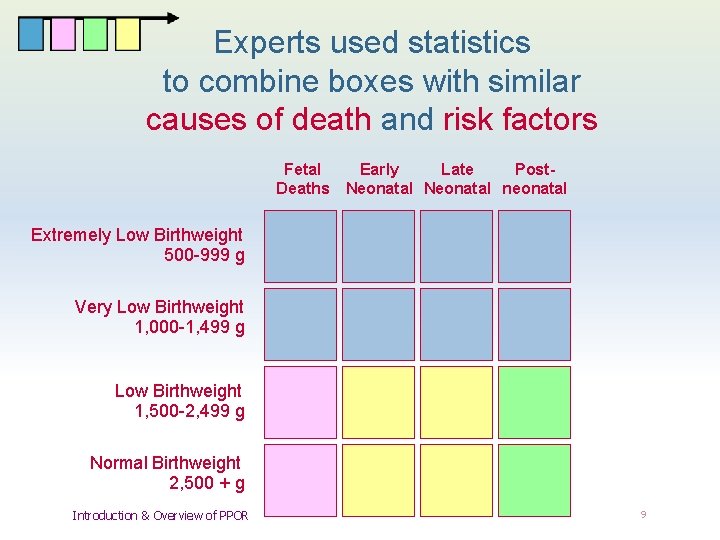
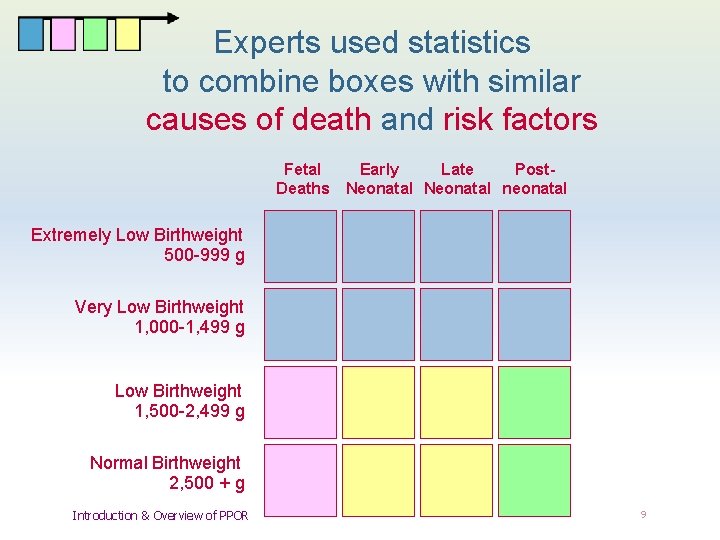
Experts used statistics to combine boxes with similar causes of death and risk factors Fetal Early Late Post- Deaths Neonatal neonatal Extremely Low Birthweight 500 -999 g Very Low Birthweight 1, 000 -1, 499 g Low Birthweight 1, 500 -2, 499 g 9 10 11 12 Normal Birthweight 2, 500 + g 13 14 15 16 Introduction & Overview of PPOR 9
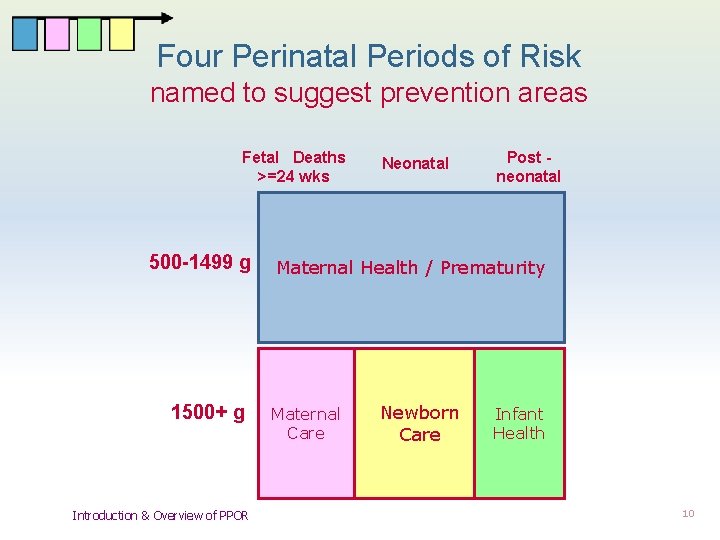
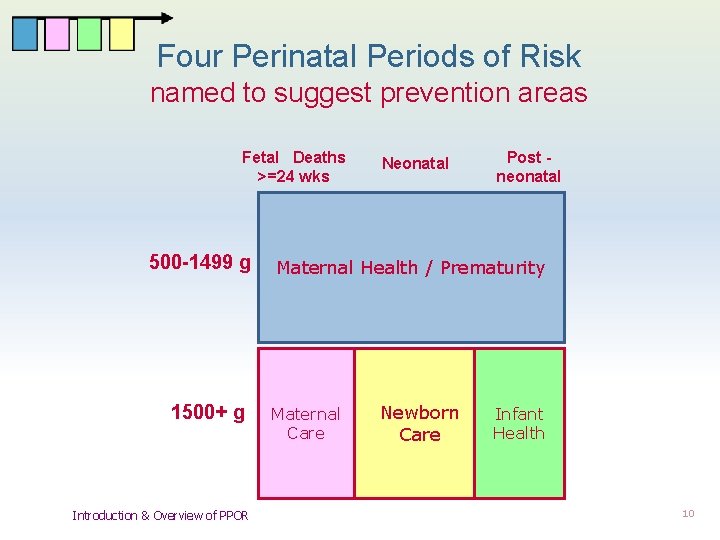
Four Perinatal Periods of Risk named to suggest prevention areas Fetal Deaths >=24 wks 500 -1499 g 1500+ g Introduction & Overview of PPOR Neonatal Post neonatal Maternal Health / Prematurity 9 10 11 13 14 15 Maternal Care Newborn Care 12 Infant Health 16 10
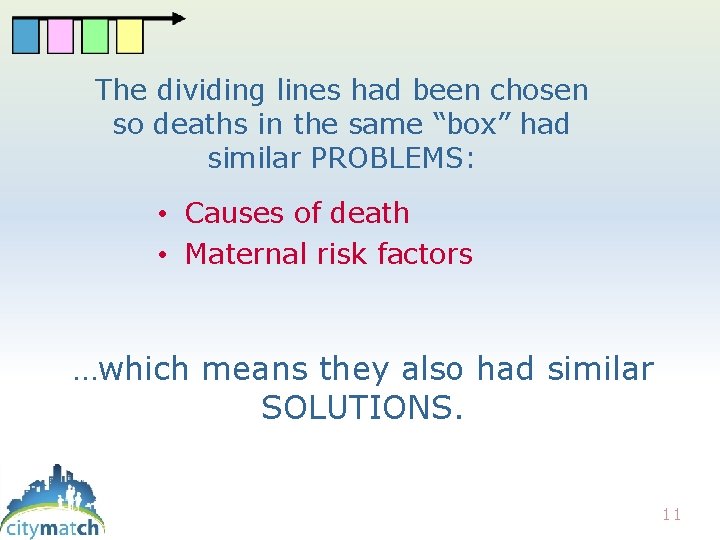
The dividing lines had been chosen so deaths in the same “box” had similar PROBLEMS: • Causes of death • Maternal risk factors …which means they also had similar SOLUTIONS. 11
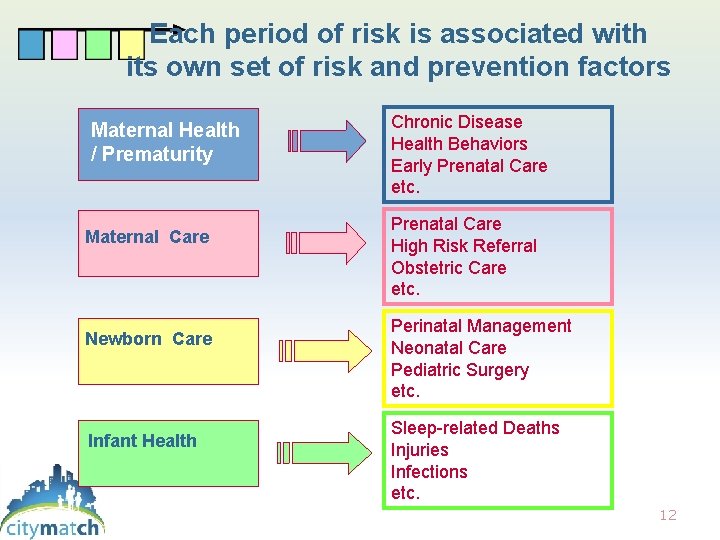
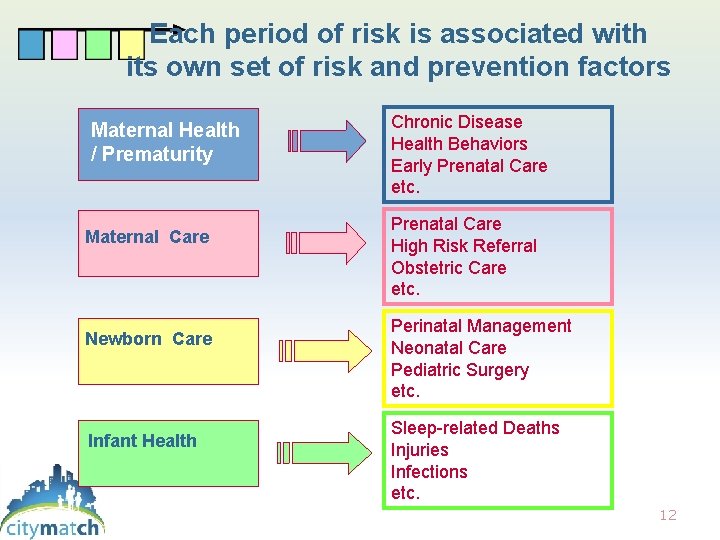
Each period of risk is associated with its own set of risk and prevention factors Maternal Health / Prematurity Maternal Care Newborn Care Infant Health Chronic Disease Health Behaviors Early Prenatal Care etc. Prenatal Care High Risk Referral Obstetric Care etc. Perinatal Management Neonatal Care Pediatric Surgery etc. Sleep-related Deaths Injuries Infections etc. 12
The four periods provide a framework that helps communities Move from having data to using data u Prioritize limited resources u Use evidence to maximize impact u 13
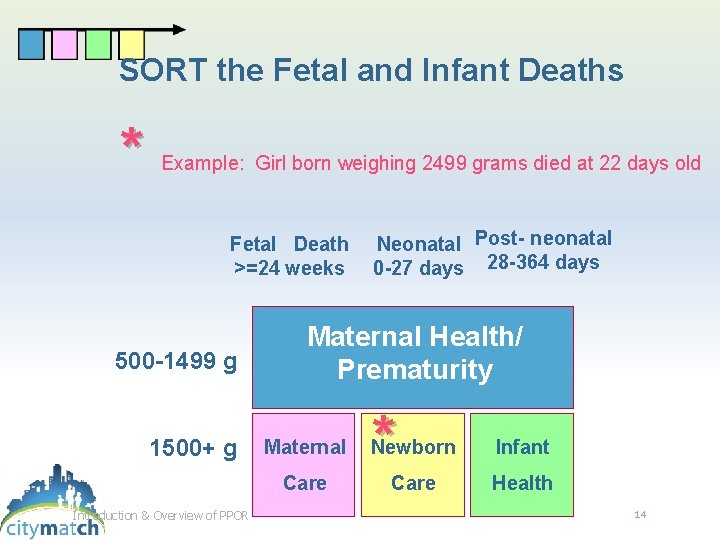
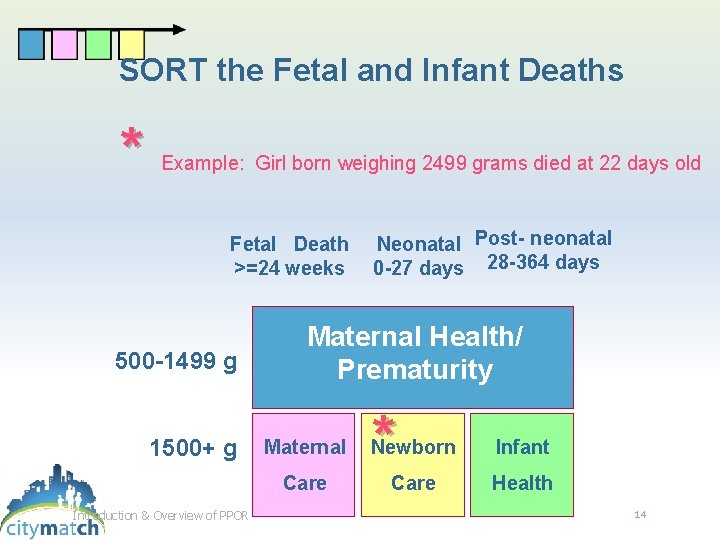
SORT the Fetal and Infant Deaths * Example: Girl born weighing 2499 grams died at 22 days old Fetal Death Neonatal Post- neonatal >=24 weeks 0 -27 days 28 -364 days 500 -1499 g 1500+ g Maternal Health/ Prematurity Care Introduction & Overview of PPOR * Maternal Newborn Care Infant Health 14
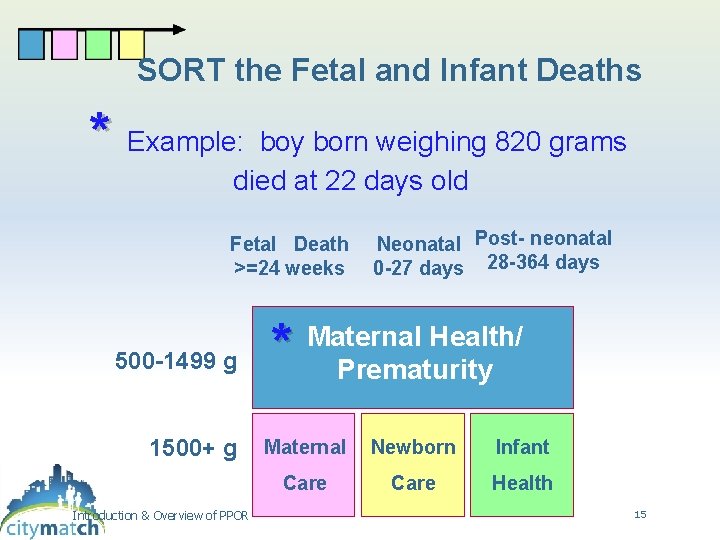
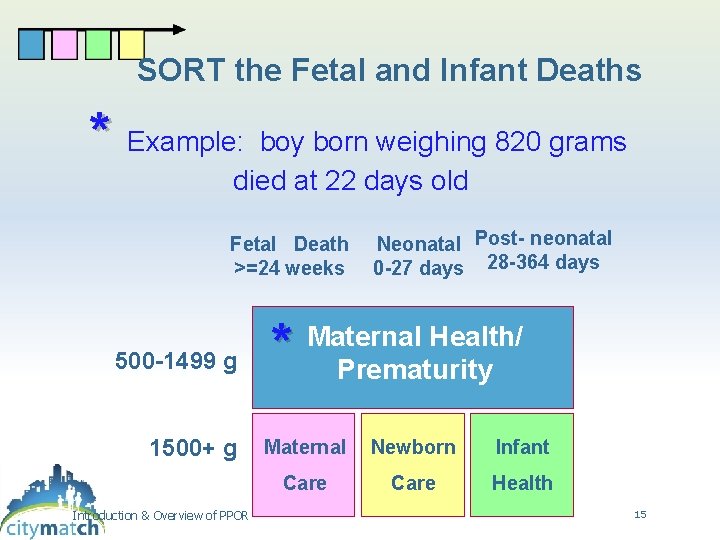
SORT the Fetal and Infant Deaths * Example: boy born weighing 820 grams died at 22 days old Fetal Death Neonatal Post- neonatal >=24 weeks 0 -27 days 28 -364 days 500 -1499 g 1500+ g * Maternal Health/ Prematurity Maternal Newborn Care Introduction & Overview of PPOR Care Infant Health 15
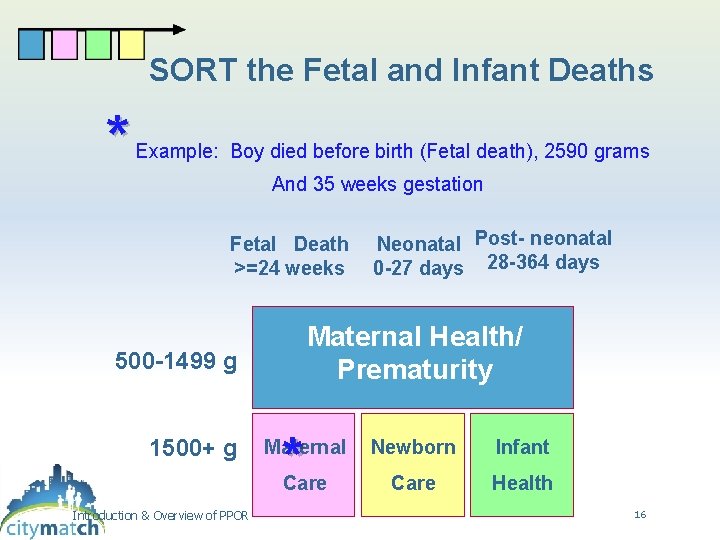
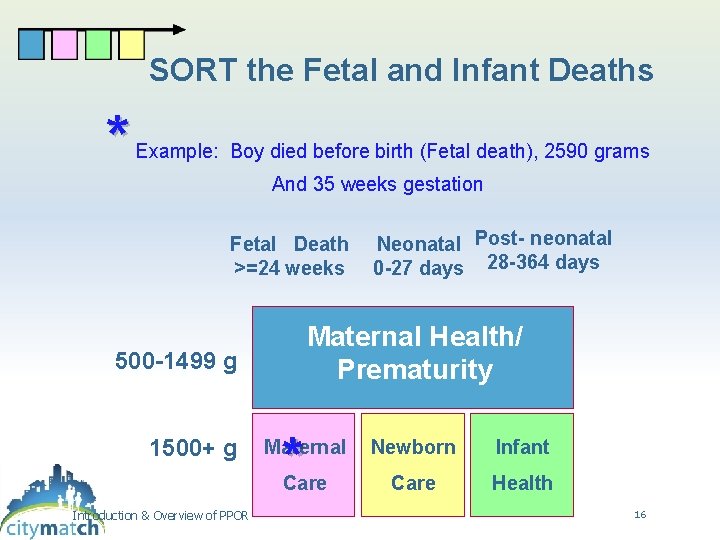
SORT the Fetal and Infant Deaths * Example: Boy died before birth (Fetal death), 2590 grams And 35 weeks gestation Fetal Death Neonatal Post- neonatal >=24 weeks 0 -27 days 28 -364 days Maternal Health/ Prematurity 500 -1499 g 1500+ g * Maternal Newborn Care Introduction & Overview of PPOR Care Infant Health 16
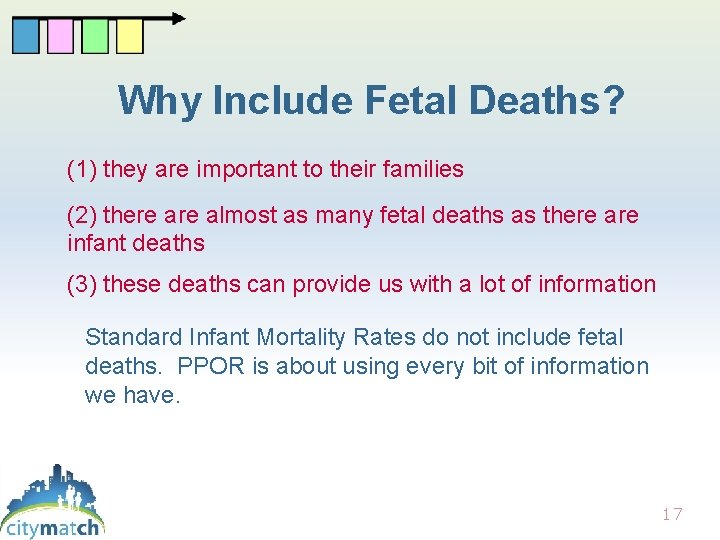
Why Include Fetal Deaths? (1) they are important to their families (2) there almost as many fetal deaths as there are infant deaths (3) these deaths can provide us with a lot of information Standard Infant Mortality Rates do not include fetal deaths. PPOR is about using every bit of information we have. 17
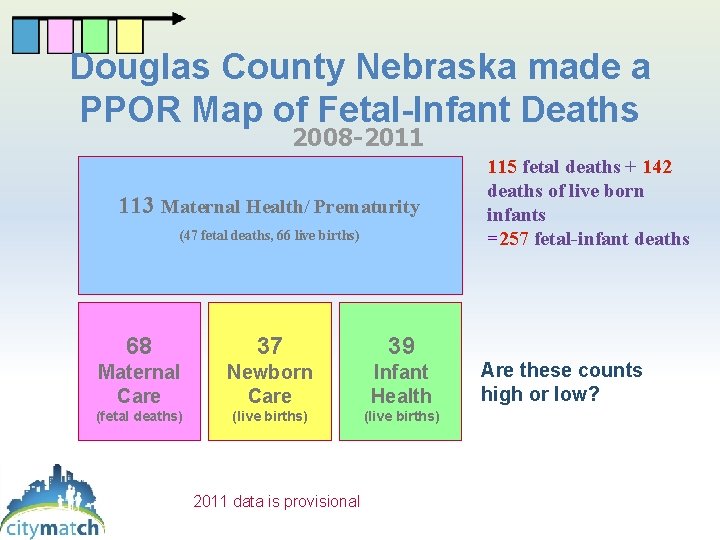
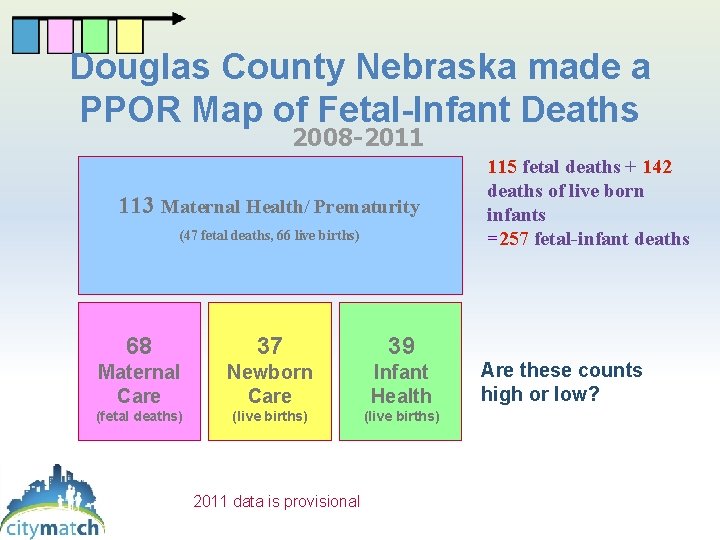
Douglas County Nebraska made a PPOR Map of Fetal-Infant Deaths 2008 -2011 113 Maternal Health/ Prematurity (47 fetal deaths, 66 live births) 68 37 39 Maternal Care Newborn Care Infant Health (fetal deaths) (live births) 2011 data is provisional (live births) 115 fetal deaths + 142 deaths of live born infants =257 fetal-infant deaths Are these counts high or low?
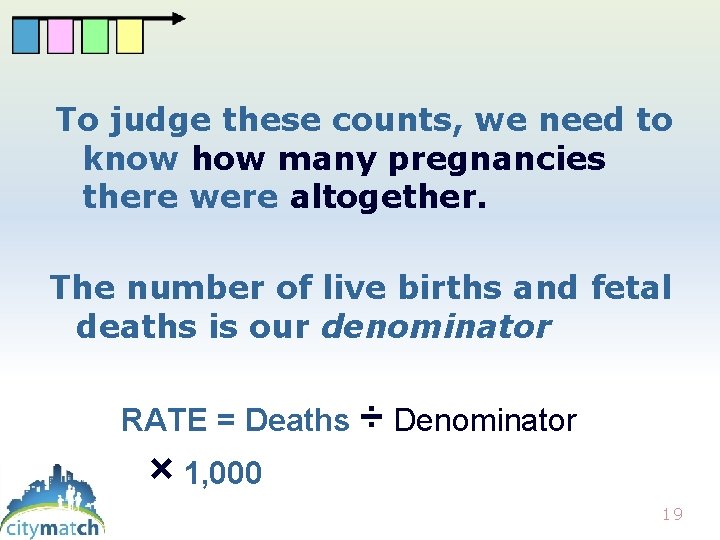
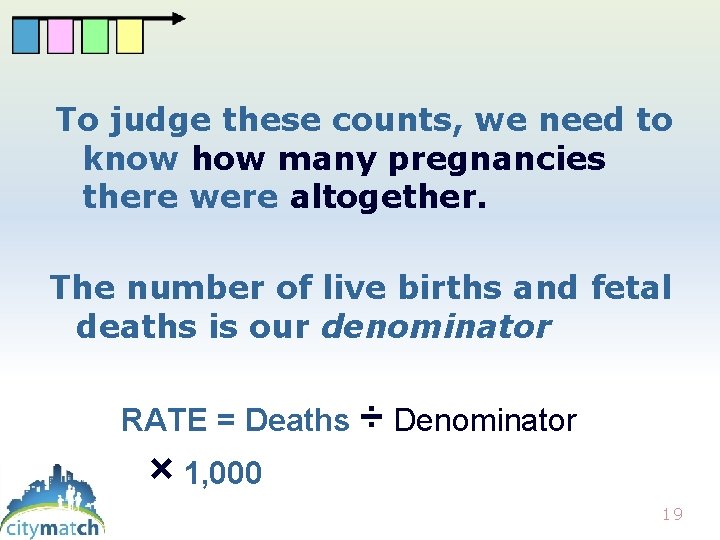
To judge these counts, we need to know how many pregnancies there were altogether. The number of live births and fetal deaths is our denominator RATE = Deaths ÷ Denominator × 1, 000 19
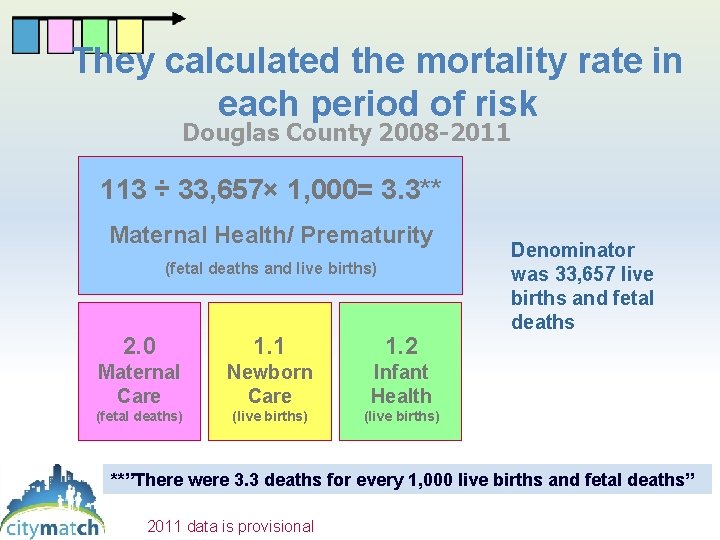
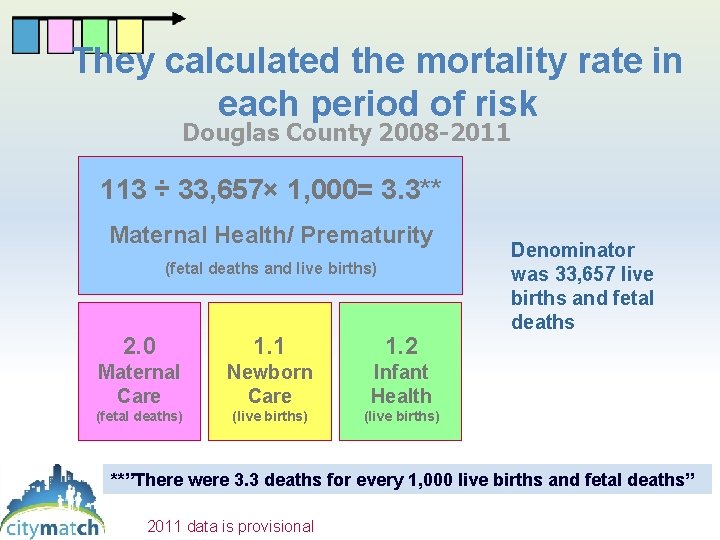
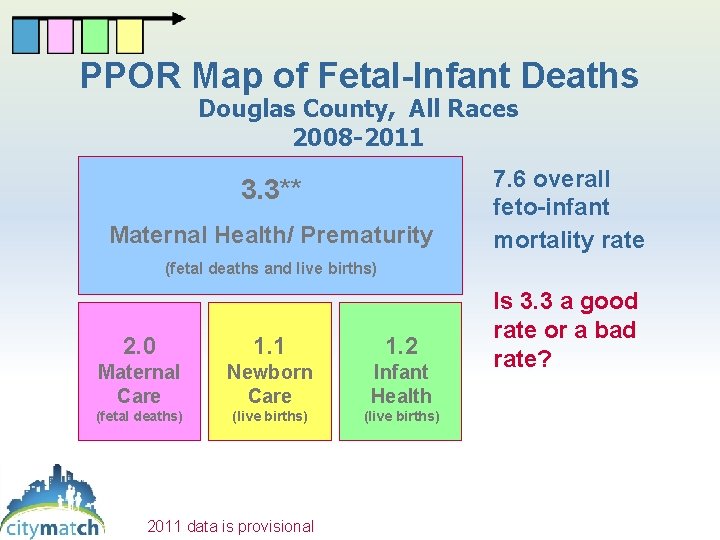
They calculated the mortality rate in each period of risk Douglas County 2008 -2011 113 ÷ 33, 657× 1, 000= 3. 3** Maternal Health/ Prematurity (fetal deaths and live births) 2. 0 1. 1 1. 2 Maternal Care Newborn Care Infant Health (fetal deaths) (live births) Denominator was 33, 657 live births and fetal deaths (live births) **”There were 3. 3 deaths for every 1, 000 live births and fetal deaths” 2011 data is provisional
Quick side trip #1: How do we find out about the deaths to count them? 21
The US Vital Records System • A certificate of death is required by state law for every death in the United States. • Fetal deaths are also recorded, though state laws and practices vary. • All these are entered into computer data files as are live births records. 22
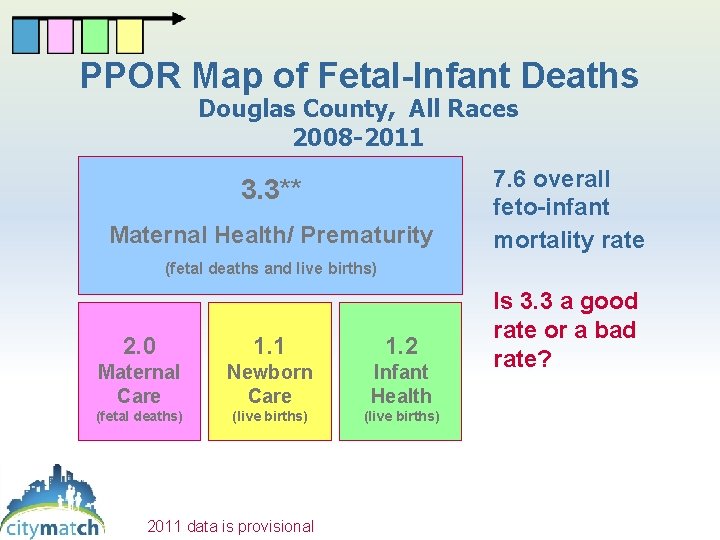
PPOR Map of Fetal-Infant Deaths Douglas County, All Races 2008 -2011 3. 3** Maternal Health/ Prematurity 7. 6 overall feto-infant mortality rate (fetal deaths and live births) 2. 0 1. 1 1. 2 Maternal Care Newborn Care Infant Health (fetal deaths) (live births) 2011 data is provisional (live births) Is 3. 3 a good rate or a bad rate?
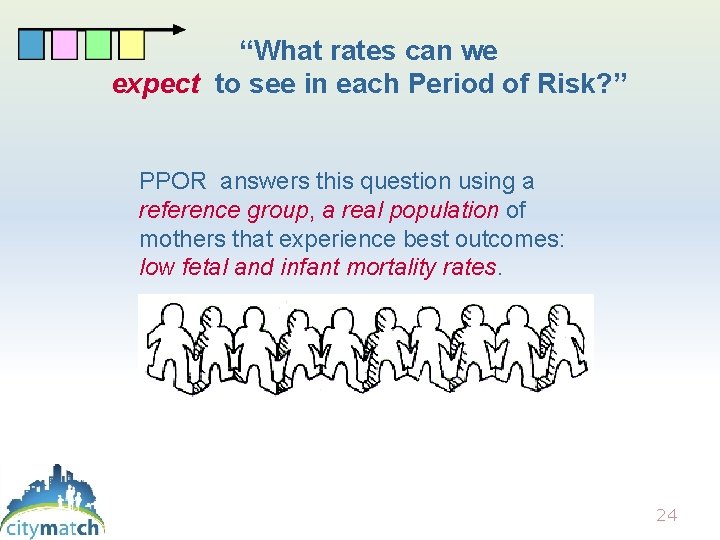
“What rates can we expect to see in each Period of Risk? ” PPOR answers this question using a reference group, a real population of mothers that experience best outcomes: low fetal and infant mortality rates. 24
The Reference Group is about Justice • The underlying assumption is that if the reference group can have low mortality, our study group should be able to reach that goal. Community stakeholders choose the reference group. They agree that it is an appropriate standard or goal for their community. 25
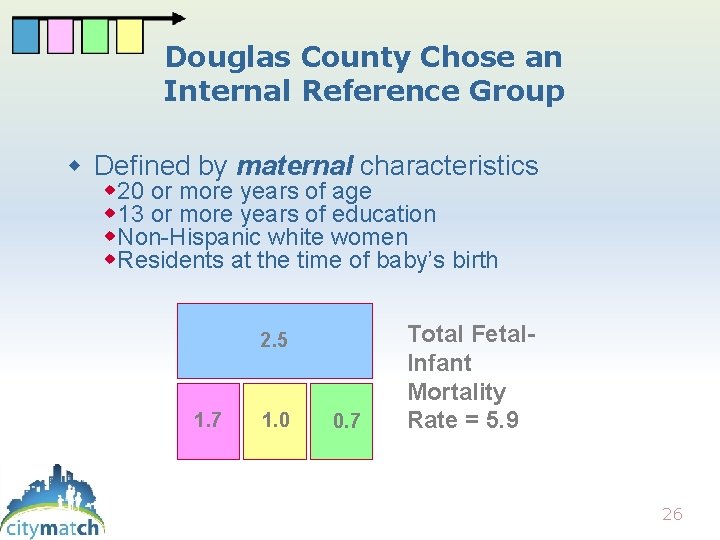
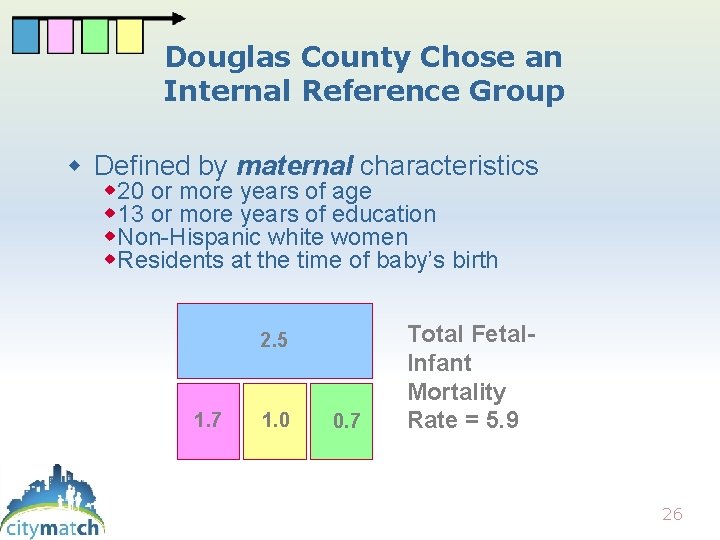
Douglas County Chose an Internal Reference Group Defined by maternal characteristics 20 or more years of age 13 or more years of education Non-Hispanic white women Residents at the time of baby’s birth 2. 5 1. 7 1. 0 0. 7 Total Fetal. Infant Mortality Rate = 5. 9 26
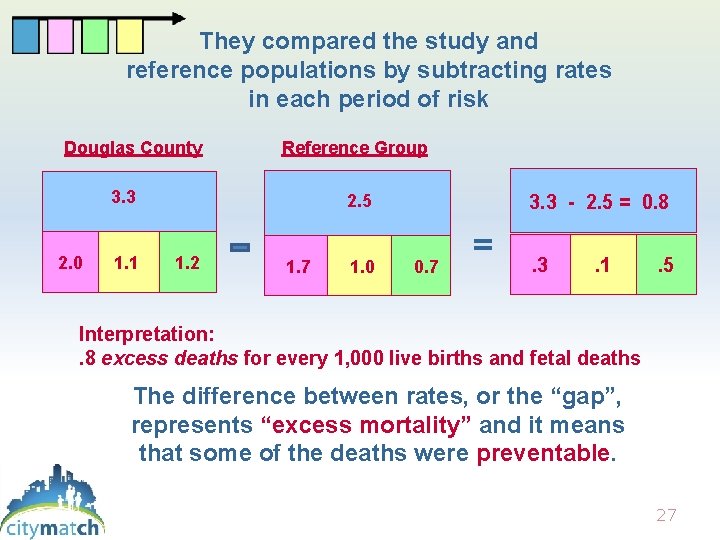
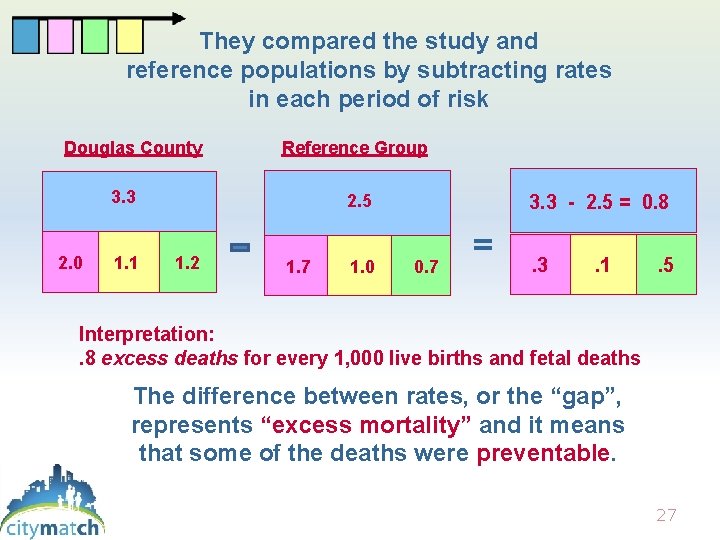
They compared the study and reference populations by subtracting rates in each period of risk Douglas County Reference Group 3. 3 2. 0 1. 1 2. 5 1. 2 1. 7 1. 0 3. 3 - 2. 5 = 0. 8 0. 7 = . 3 . 1 . 5 Interpretation: . 8 excess deaths for every 1, 000 live births and fetal deaths The difference between rates, or the “gap”, represents “excess mortality” and it means that some of the deaths were preventable. 27
Why are babies dying? The reference group allows us to understand from the population perspective …even though we may not be able to determine underlying causes for each individual case. 28
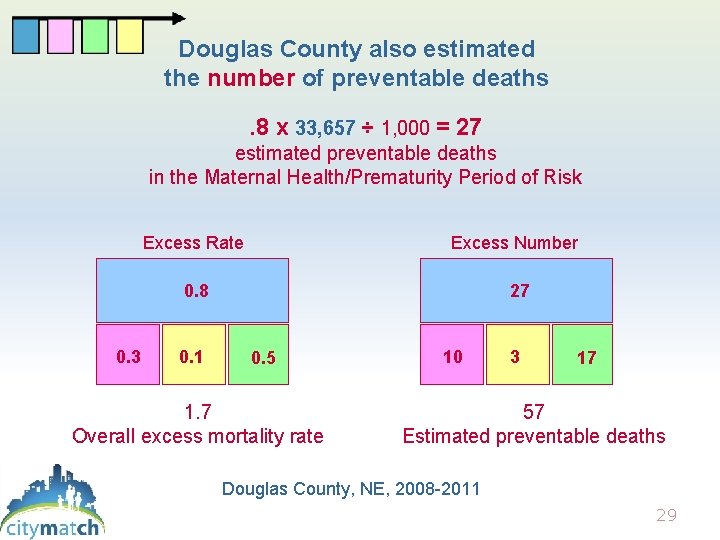
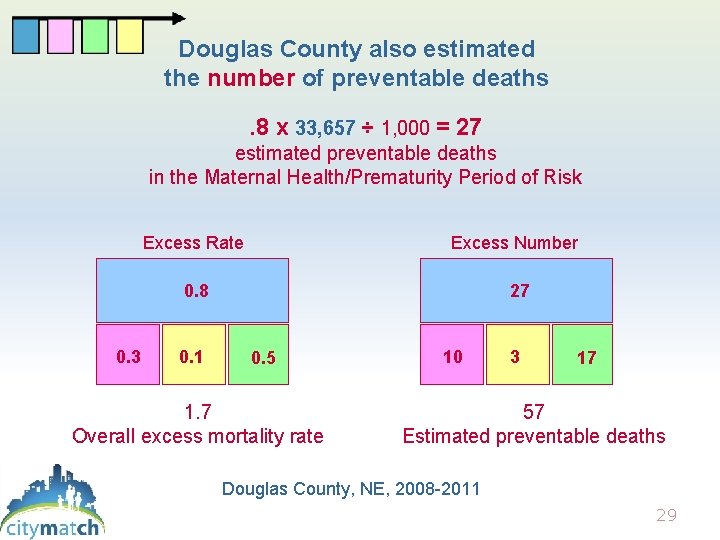
Douglas County also estimated the number of preventable deaths. 8 x 33, 657 ÷ 1, 000 = 27 estimated preventable deaths in the Maternal Health/Prematurity Period of Risk 0. 3 Excess Rate Excess Number 0. 8 27 0. 1 0. 5 1. 7 Overall excess mortality rate 10 3 17 57 Estimated preventable deaths Douglas County, NE, 2008 -2011 29
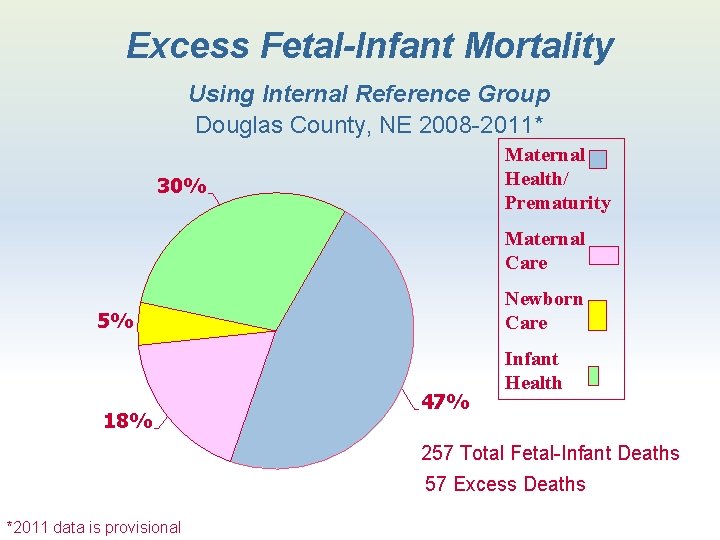
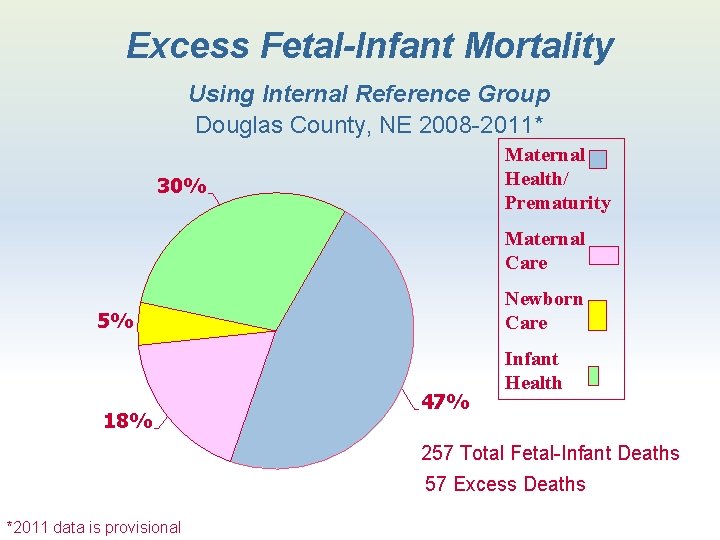
Excess Fetal-Infant Mortality Using Internal Reference Group Douglas County, NE 2008 -2011* Maternal Health/ Prematurity 30% Maternal Care Newborn Care 5% 18% 47% Infant Health 257 Total Fetal-Infant Deaths 57 Excess Deaths *2011 data is provisional
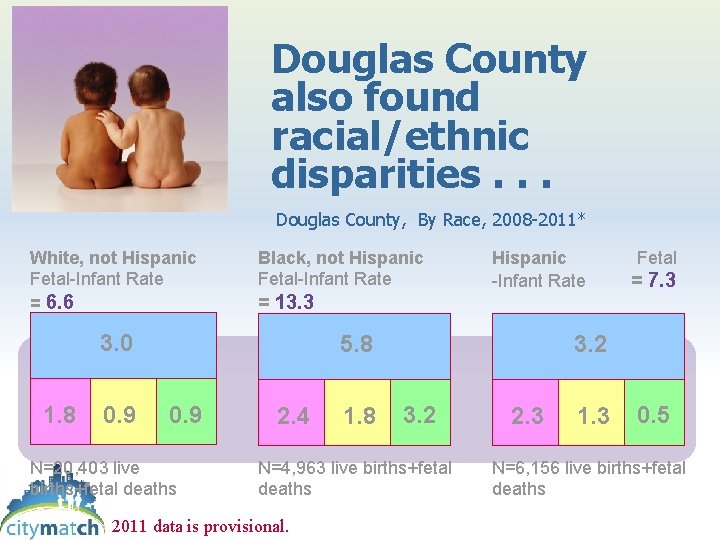
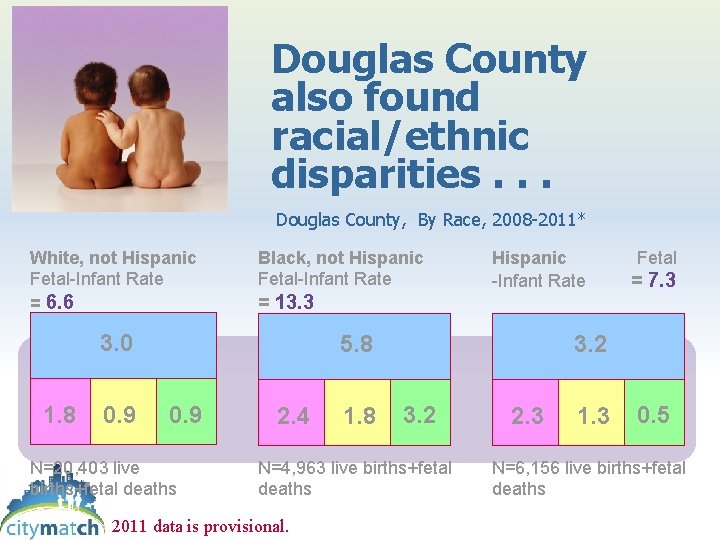
Douglas County also found racial/ethnic disparities. . . Douglas County, By Race, 2008 -2011* White, not Hispanic Fetal-Infant Rate = 6. 6 Black, not Hispanic Fetal-Infant Rate = 13. 3 3. 0 1. 8 0. 9 Hispanic Fetal -Infant Rate = 7. 3 5. 8 0. 9 N=20, 403 live births+fetal deaths 2. 4 1. 8 3. 2 N=4, 963 live births+fetal deaths 2011 data is provisional. 2. 3 1. 3 0. 5 N=6, 156 live births+fetal deaths
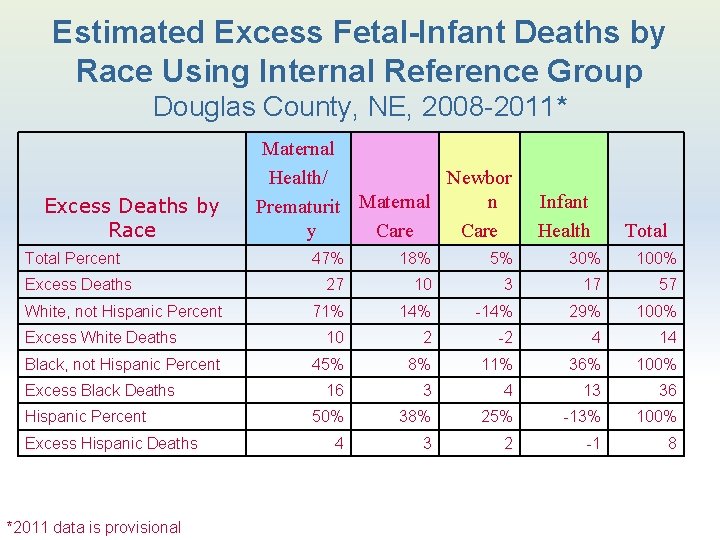
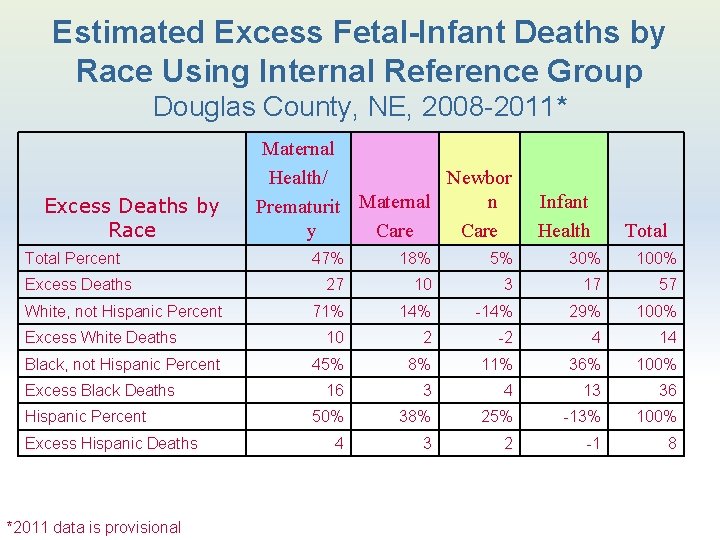
Estimated Excess Fetal-Infant Deaths by Race Using Internal Reference Group Douglas County, NE, 2008 -2011* Excess Deaths by Race Total Percent Excess Deaths White, not Hispanic Percent Excess White Deaths Black, not Hispanic Percent Excess Black Deaths Hispanic Percent Excess Hispanic Deaths *2011 data is provisional Maternal Health/ Newbor n Prematurit Maternal y Care Infant Health Total 47% 18% 5% 30% 100% 27 10 3 17 57 71% 14% -14% 29% 100% 10 2 -2 4 14 45% 8% 11% 36% 100% 16 3 4 13 36 50% 38% 25% -13% 100% 4 3 2 -1 8
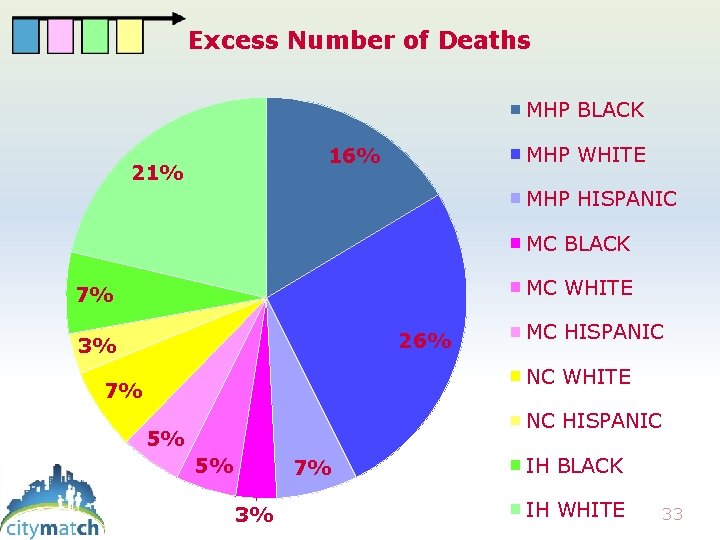
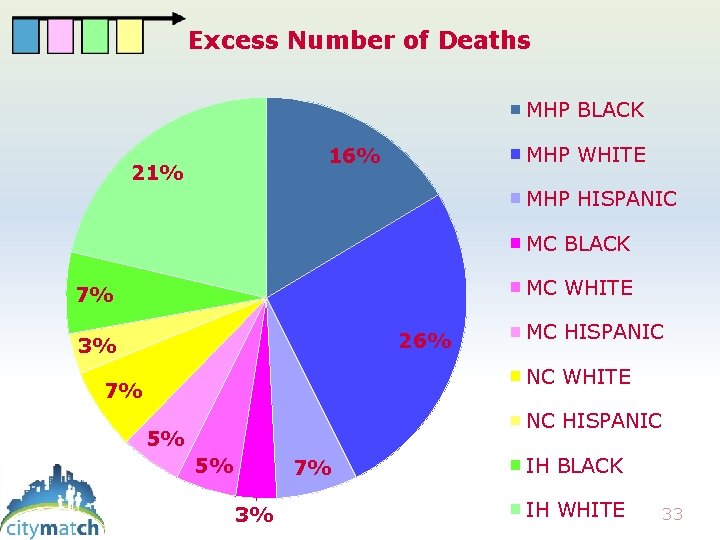
Excess Number of Deaths MHP BLACK MHP WHITE 16% 21% MHP HISPANIC MC BLACK MC WHITE 7% 26% 3% MC HISPANIC NC WHITE 7% NC HISPANIC 5% 5% 7% 3% IH BLACK IH WHITE 33
SUCCESS! Douglas County completed Phase 1 of PPOR analysis Their prize? They had eliminated from consideration many potential causes of infant mortality that were not major contributors in their community. 34
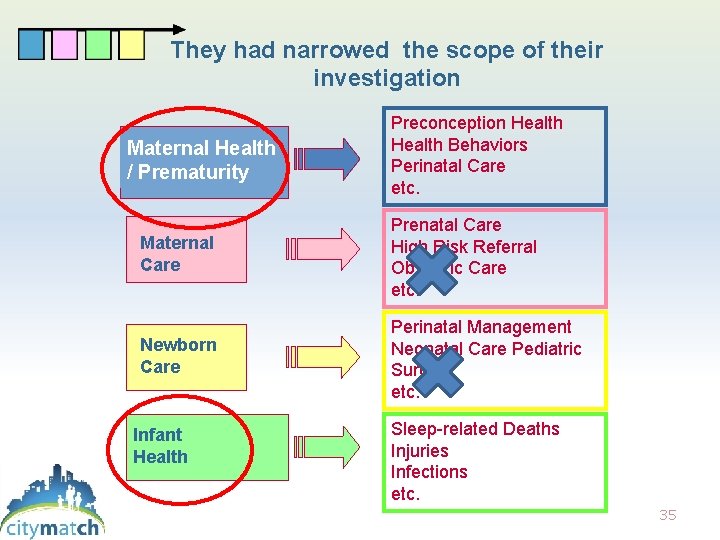
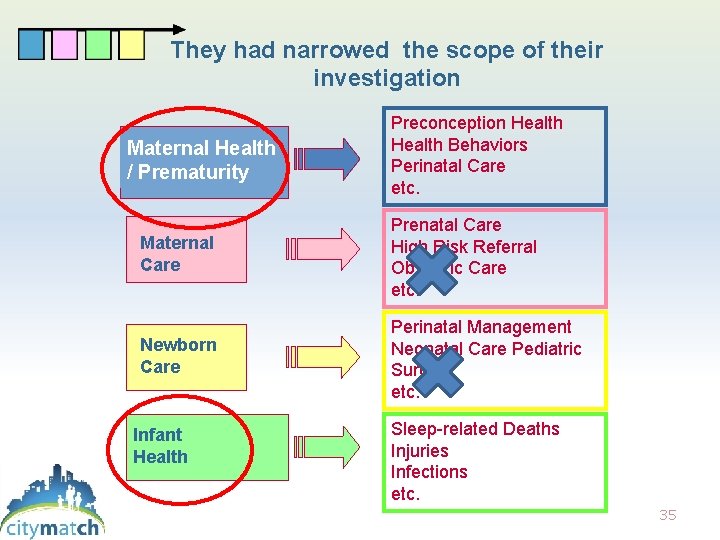
They had narrowed the scope of their investigation Maternal Health / Prematurity Preconception Health Behaviors Perinatal Care etc. Maternal Care Prenatal Care High Risk Referral Obstetric Care etc. Newborn Care Perinatal Management Neonatal Care Pediatric Surgery etc. Infant Health Sleep-related Deaths Injuries Infections etc. 35
Douglas County celebrated these successes, but they didn’t stop there. Phase 2 of PPOR analysis helped them prioritize among the remaining potential causes of excess mortality. 36
“She’s got to be kidding! There’s more? ” Phase 2 analysis explores the reasons for excess mortality, and potential prevention strategies 37
How does Phase 2 work? We’ll show you some of Douglas County’s investigation of its Infant Health Period of Risk. • Other risk periods have different methods • Other cities have different results • The overall strategy is the same 38
There are many common causes of death in the Infant Health Period of Risk SIDS Suffocation in bed Drowning Car accidents Assault Infections Congenital anomalies etc. The first step is to find out which of these are causing excess mortality in our community. 39
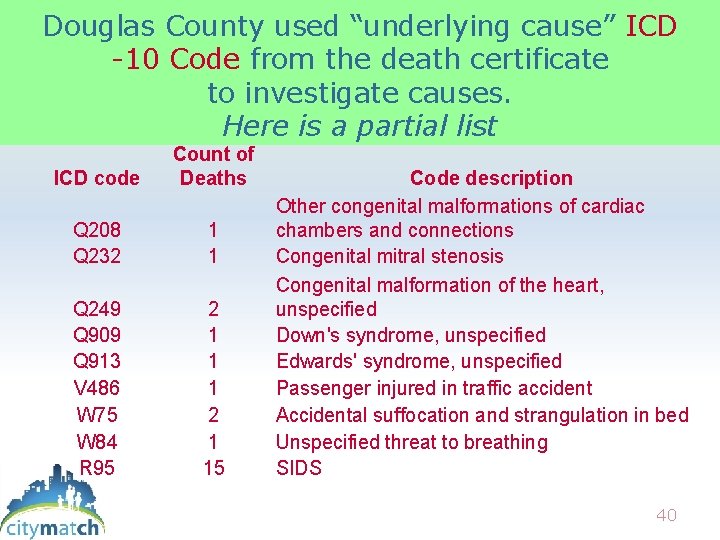
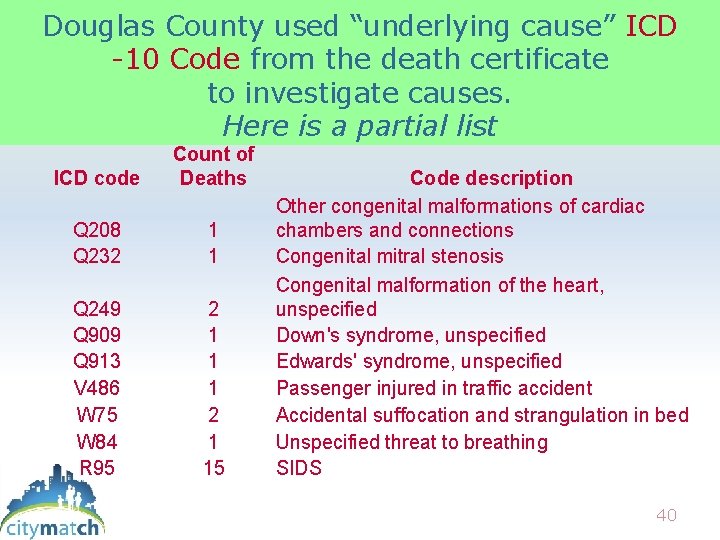
Douglas County used “underlying cause” ICD -10 Code from the death certificate to investigate causes. Here is a partial list ICD code Count of Deaths Q 208 Q 232 1 1 Q 249 Q 909 Q 913 V 486 W 75 W 84 R 95 2 1 1 1 2 1 15 Code description Other congenital malformations of cardiac chambers and connections Congenital mitral stenosis Congenital malformation of the heart, unspecified Down's syndrome, unspecified Edwards' syndrome, unspecified Passenger injured in traffic accident Accidental suffocation and strangulation in bed Unspecified threat to breathing SIDS 40
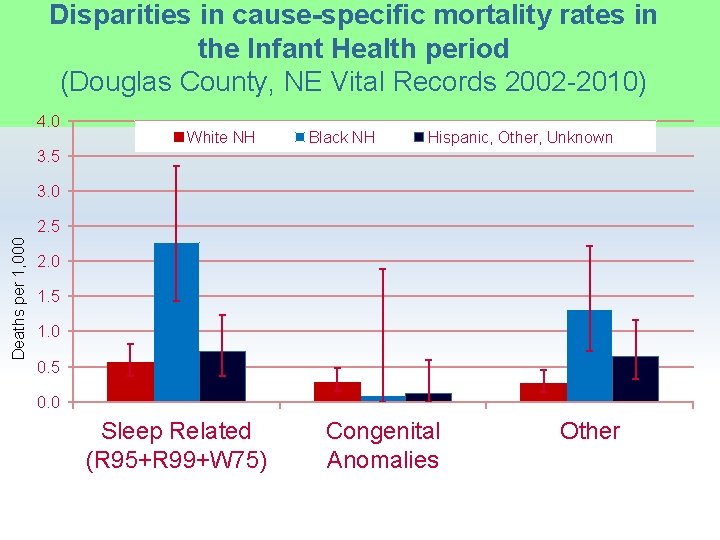
The hundreds of causes were grouped: • SIDS/SUID • Congenital Anomalies • Other causes (include infection, injury, rare causes like cancer) Cause-specific mortality rates were calculated 41
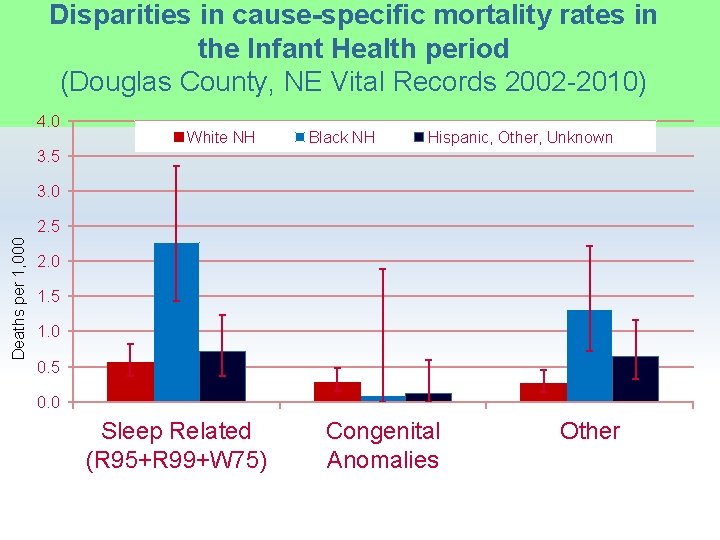
Disparities in cause-specific mortality rates in the Infant Health period (Douglas County, NE Vital Records 2002 -2010) 4. 0 White NH Black NH Hispanic, Other, Unknown 3. 5 3. 0 Deaths per 1, 000 2. 5 2. 0 1. 5 1. 0 0. 5 0. 0 Sleep Related (R 95+R 99+W 75) Congenital Anomalies Other
SUCCESS! Douglas County Stakeholders had discovered that over half the deaths in the infant health period are caused by “SIDS” or suffocation, and occur during sleep Infant Health Period Sleep related death Accidental injuries Assault Infections Congenital anomalies etc. 43

They had eliminated causes that were not large contributors to their infant mortality disparity and further narrowed the scope of their investigation. But they could do better! 44
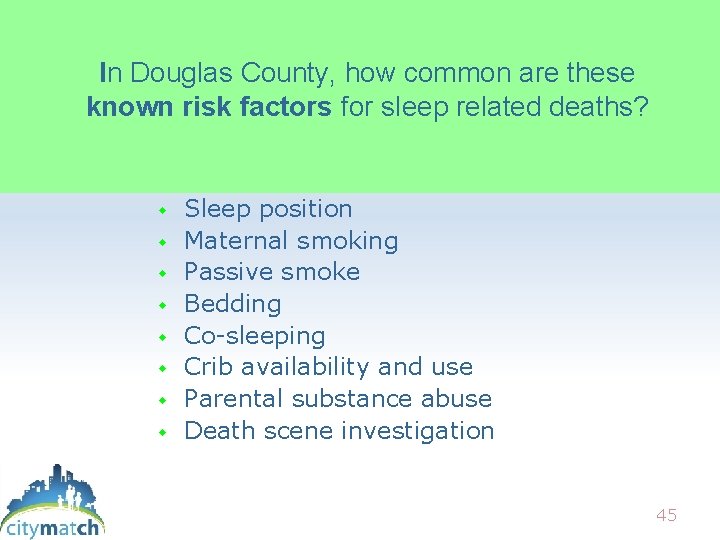
In Douglas County, how common are these known risk factors for sleep related deaths? Sleep position Maternal smoking Passive smoke Bedding Co-sleeping Crib availability and use Parental substance abuse Death scene investigation 45
PRAMS, the Pregnancy Risk Assessment Monitoring System is a CDC survey in which Nebraska has participated since 1999 • New mothers are mailed a booklet with questions on their experiences before, during, and after pregnancy. • Questions cover medical, social, behavioral, and health systems issues. 46
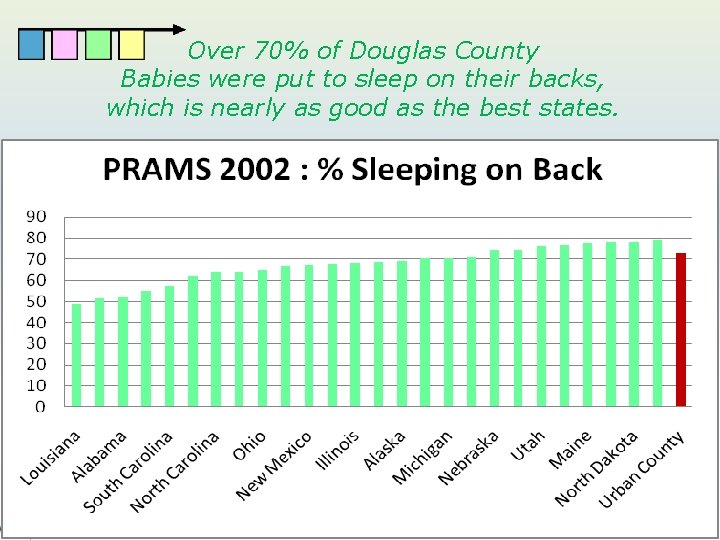
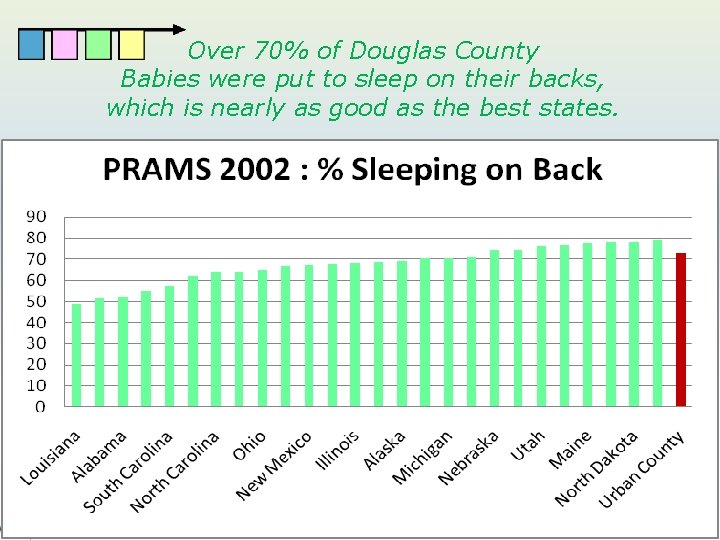
Over 70% of Douglas County Babies were put to sleep on their backs, which is nearly as good as the best states. 47
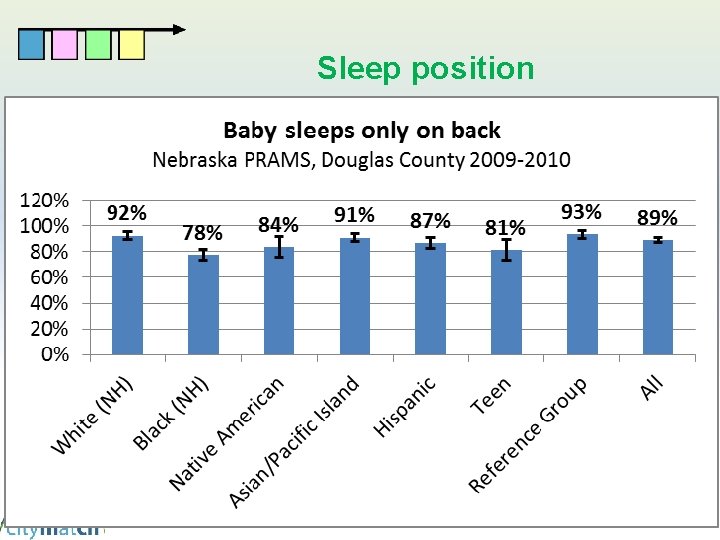
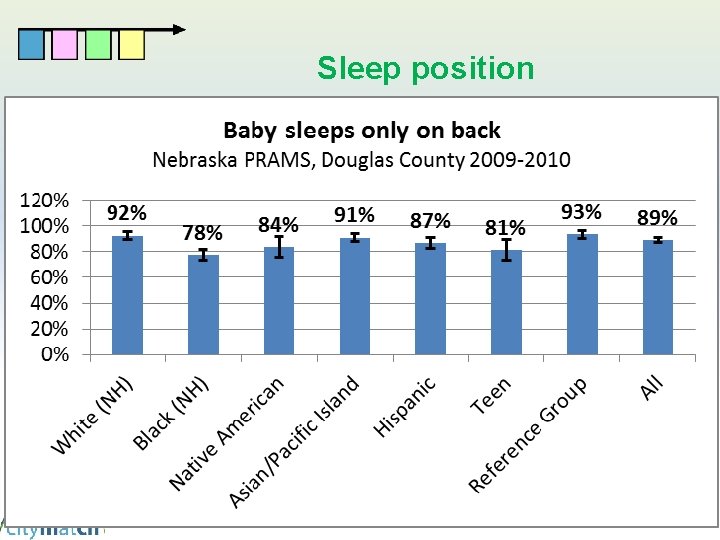
Sleep position
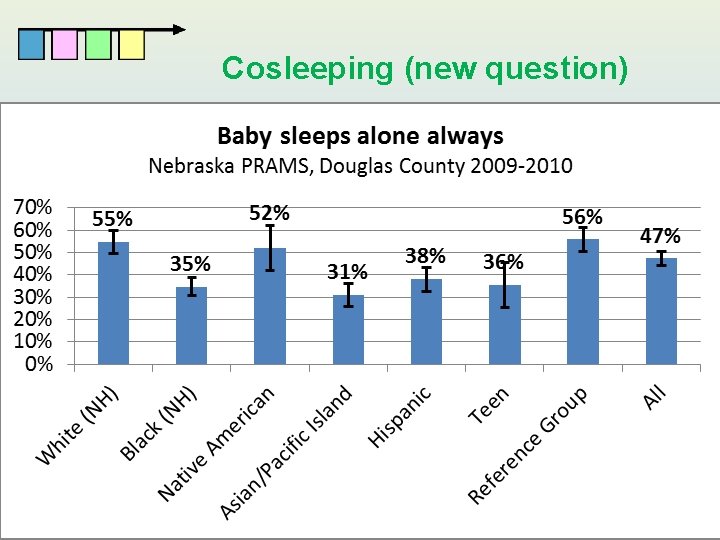
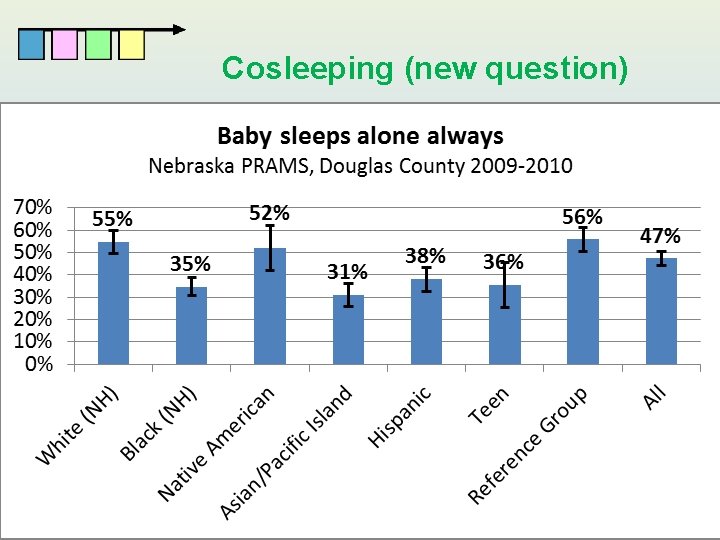
Cosleeping (new question)
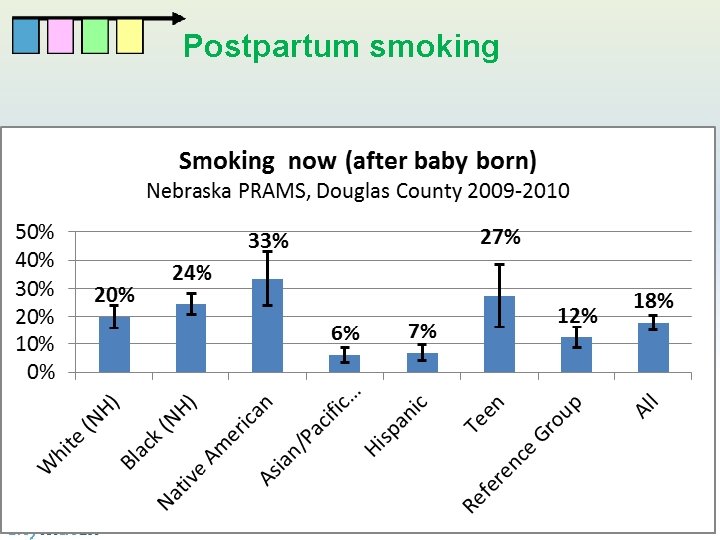
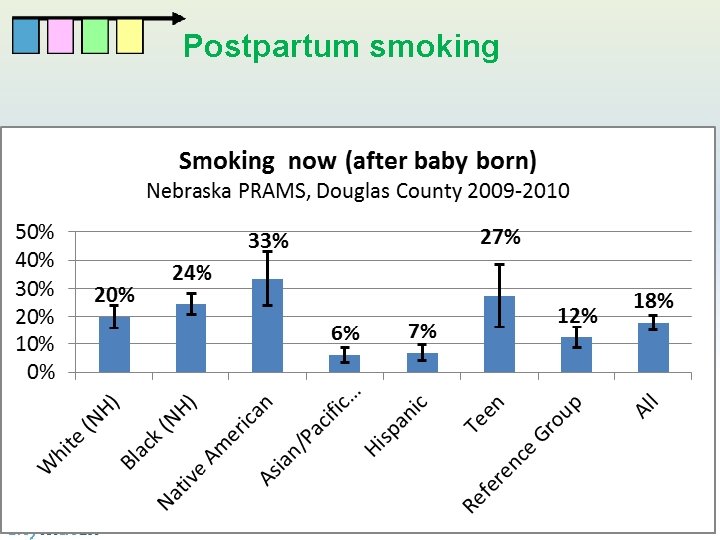
Postpartum smoking
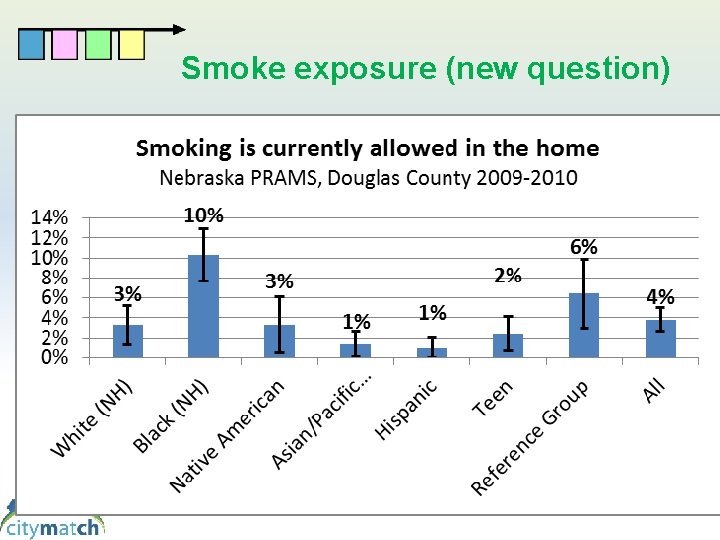
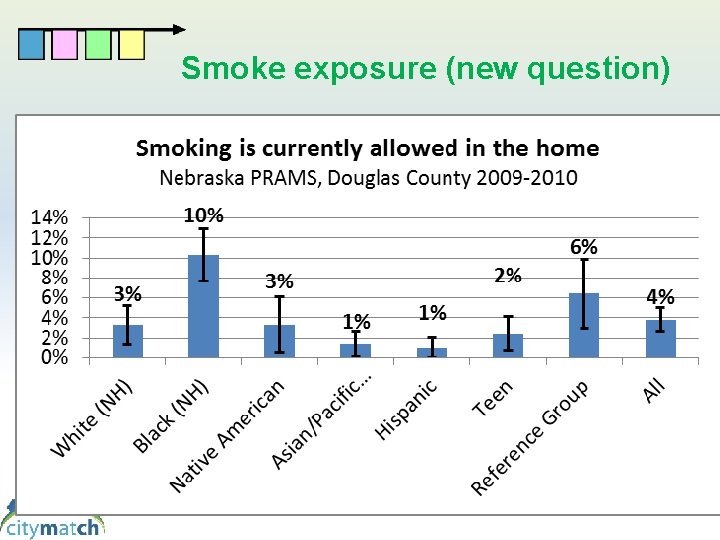
Smoke exposure (new question)
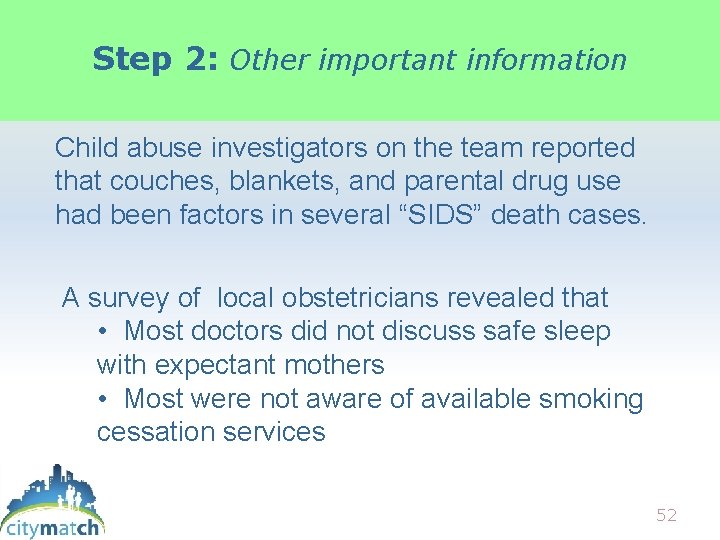
Step 2: Other important information Child abuse investigators on the team reported that couches, blankets, and parental drug use had been factors in several “SIDS” death cases. A survey of local obstetricians revealed that • Most doctors did not discuss safe sleep with expectant mothers • Most were not aware of available smoking cessation services 52
Step 2: Guided by PPOR findings, the Fetal Infant Mortality Review team reviewed ALL Sleep-related deaths. The Fetal Infant Mortality Review Team reported that the physical and mental health of mothers was a factor in many of these deaths, including • chronic stressful conditions • lack of social support 53
What FIMR brings to the table FIMR can give us answers when we don’t even know what the question is yet! FIMR can identify cause and effect relationships. FIMR works in small neighborhoods. FIMR “Paints faces behind the numbers” 54
Step 3: Douglas County estimated the impact of risk factors, and the potential impact of interventions Statistically estimated how many lives could potentially be saved if certain risks were reduced (Population Attributable Risk) • Which factors are modifiable? • Do evidence-based interventions exist? • What are our community assets, capacity, and commitment? 55
Douglas County’s Community Stakeholders decided on these initial action steps: • Message changed from “sleep on back” to a broader “safe sleep” message • Physician education about smoking cessation services for pregnant women • Partnered with a group that was already working on maternal mental health issues 56
SUCCESS! Douglas County Had won still more valuable prizes. . . • Their time investment was focused • They found some answers • Action steps were more appropriate than initially envisioned (“back to sleep”) 57
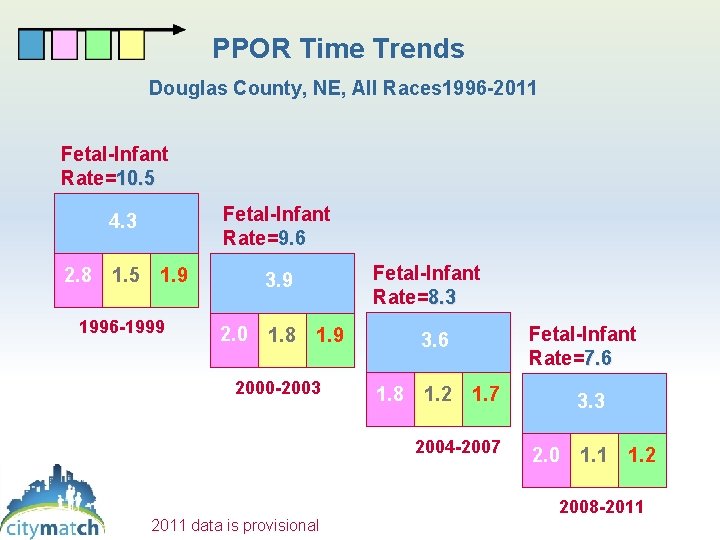
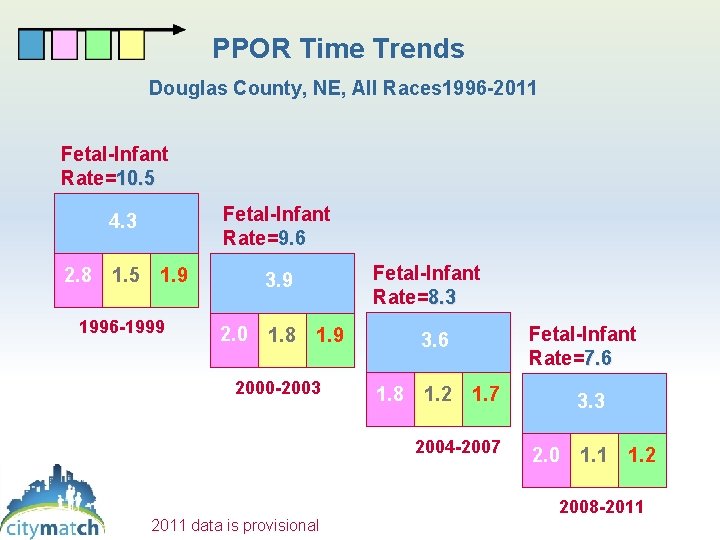
PPOR Time Trends Douglas County, NE, All Races 1996 -2011 Fetal-Infant Rate=10. 5 Fetal-Infant Rate=9. 6 4. 3 2. 8 1. 5 1. 9 1996 -1999 Fetal-Infant Rate=8. 3 3. 9 2. 0 1. 8 1. 9 2000 -2003 Fetal-Infant Rate=7. 6 3. 6 1. 8 1. 2 1. 7 2004 -2007 2011 data is provisional 3. 3 2. 0 1. 1 1. 2 2008 -2011
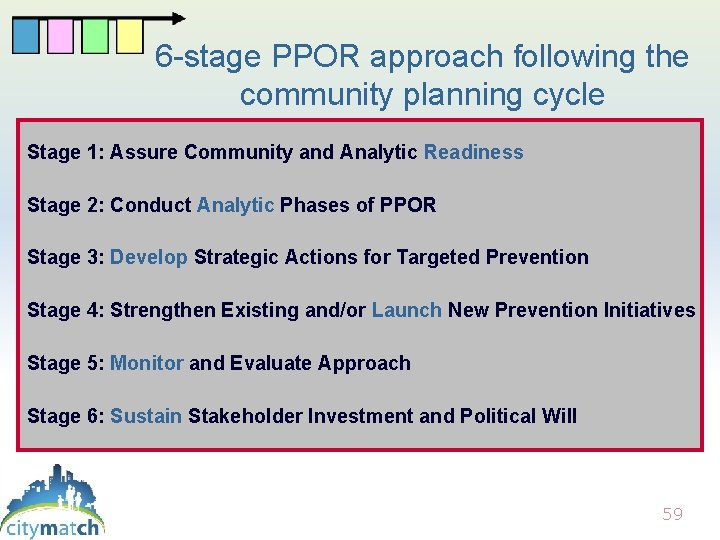
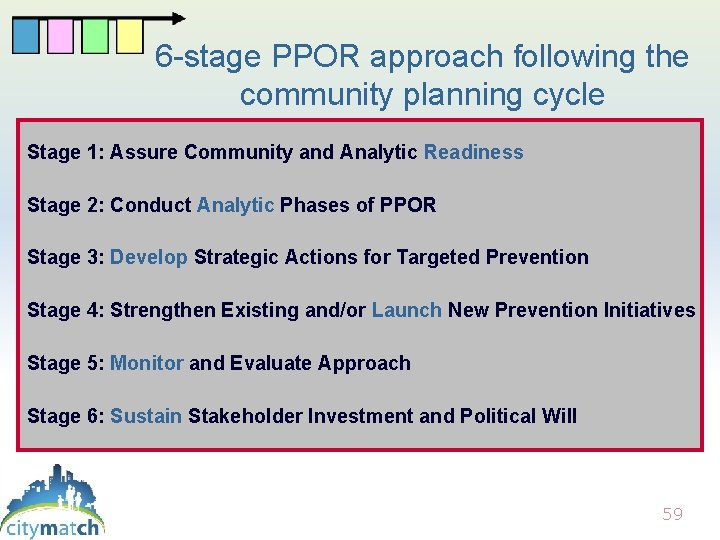
6 -stage PPOR approach following the community planning cycle Stage 1: Assure Community and Analytic Readiness Stage 2: Conduct Analytic Phases of PPOR Stage 3: Develop Strategic Actions for Targeted Prevention Stage 4: Strengthen Existing and/or Launch New Prevention Initiatives Stage 5: Monitor and Evaluate Approach Stage 6: Sustain Stakeholder Investment and Political Will 59

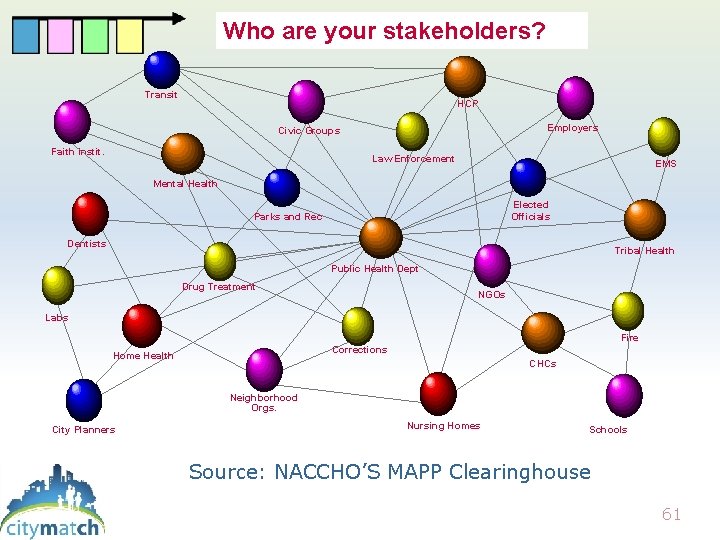
You need community involvement “Data analysis alone does not produce community change. ” • Because infant mortality has many social and medical causes, many stakeholders are needed • Everyone has a different piece of the puzzle 60 60
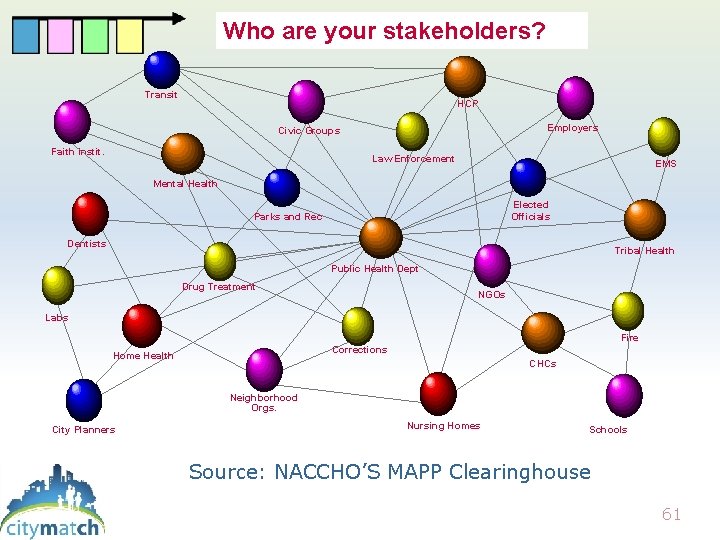
Public Health System Who are your stakeholders? Transit HCP Employers Civic Groups Faith Instit. Law Enforcement EMS Mental Health Elected Officials Parks and Rec Dentists Tribal Health Public Health Dept Drug Treatment NGOs Labs Fire Corrections Home Health CHCs Neighborhood Orgs. City Planners Nursing Homes Schools Source: NACCHO’S MAPP Clearinghouse 61
Collective Impact • Common agenda, shared understanding of where we are and how we want to change • Shared measurement systems, surveillance • Mutually reinforcing activities • Continuous communication • Backbone support organization 62
Why use PPOR? www. citymatch. org 63
64

Baltimore City Lane County, Oregon Chattanooga, TN Bay Area Data Collaborative Maricopa County Public Health Your name here ! 65

Visit us at www. citymatch. org 402 -561 -7500 Carol Gilbert cgilbert@unmc. edu Laurin Kasehagen lkasehagen@unmc. edu 66
 Perinatal risk factors
Perinatal risk factors Market risk credit risk operational risk
Market risk credit risk operational risk Clear perinatal quality
Clear perinatal quality Basic perinatal matrices
Basic perinatal matrices Perinatal mortality rate
Perinatal mortality rate Perinatal asphyxia
Perinatal asphyxia Perinatal asphyxia
Perinatal asphyxia Perinatal audit
Perinatal audit Cem samut
Cem samut Indiana perinatal quality improvement collaborative
Indiana perinatal quality improvement collaborative Certain conditions originating in the perinatal period
Certain conditions originating in the perinatal period Ccqi perinatal standards
Ccqi perinatal standards South dakota perinatal association
South dakota perinatal association Perinatal
Perinatal Ruta materno perinatal
Ruta materno perinatal Waiter's tip deformity
Waiter's tip deformity Levene staging
Levene staging Multicullar
Multicullar Papercut job tickerting print software
Papercut job tickerting print software Introduction product overview
Introduction product overview Introduction product overview
Introduction product overview Introduction product overview
Introduction product overview A christmas carol introduction lesson
A christmas carol introduction lesson Draw rmmm plan
Draw rmmm plan Risk mitigation avoidance
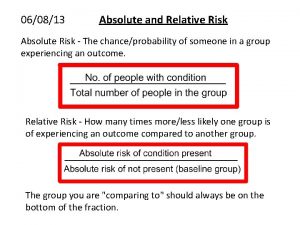
Risk mitigation avoidance Absolute risk vs relative risk
Absolute risk vs relative risk Residual risk and secondary risk pmp
Residual risk and secondary risk pmp Inherent risk vs control risk
Inherent risk vs control risk Absolute risk vs relative risk
Absolute risk vs relative risk Activity sheet 1 about p/e ratios answer key
Activity sheet 1 about p/e ratios answer key Short term risk
Short term risk Risk financing transfer dan risk retention
Risk financing transfer dan risk retention The biggest risk is not taking any risk
The biggest risk is not taking any risk Key risk indicators financial risk management
Key risk indicators financial risk management Ar = ir x cr x dr
Ar = ir x cr x dr Business risk and financial risk leverage
Business risk and financial risk leverage Relative risk calculation
Relative risk calculation Risk map
Risk map Measure of association formula
Measure of association formula Most common pay periods
Most common pay periods Moseley periodic table
Moseley periodic table Topic 15 periods authors and genres
Topic 15 periods authors and genres Periods in roman history
Periods in roman history Periods of music
Periods of music 6-2 pay periods and hourly rates
6-2 pay periods and hourly rates Realism literature period
Realism literature period Periods of prenatal development
Periods of prenatal development Germinal stage
Germinal stage What are the approximate dates of the baroque period
What are the approximate dates of the baroque period Group 18 name
Group 18 name Groups vs periods
Groups vs periods Where to do a heel stick on newborn
Where to do a heel stick on newborn British literary eras
British literary eras American literary period
American literary period Timeline of literary periods in british literature
Timeline of literary periods in british literature Classical music era timeline
Classical music era timeline Stages of infection
Stages of infection Groups vs periods
Groups vs periods Periods of reactivity newborn
Periods of reactivity newborn Place value periods
Place value periods Period in computer
Period in computer Native american writing
Native american writing Fertility blend for women reviews
Fertility blend for women reviews Periods of american literature
Periods of american literature Periods of reactivity newborn
Periods of reactivity newborn The old english period 450 to 1066
The old english period 450 to 1066 6-2 pay periods and hourly rates
6-2 pay periods and hourly rates