Priorities and challenges of perinatal and neonatal periods






- Slides: 65
Priorities and challenges of perinatal and neonatal periods Prof. Karimjanov I. A.
Lecture • The purpose of the lecture - to acquaint students with intrauterine fetal hypoxia, asphyxia, neonatal encephalopathy • Objectives: - risk factors for fetal and newborn hypoxia - Classification, clinical syndromes of encephalopathy in children - Diagnosis, treatment, prevention - Breastfeeding in children
Maternity and Childhood Protection • The Constitution of the RUz • The state program "For the younger generation, " "Mother and Child“ • Resolution of the Cabinet of Ministers № 242 from 2009 № 1096 " On increasing the medical culture in a family run main lines, women's health, birth and raising a healthy generation "
The main objectives of Pediatrics • Work with healthy children • Creating optimal conditions for their growth and harmonious development • Development of preventive measures that increase the body's resistance to unfavorable influences
Achieving objectives will contribute to: • The study of anatomical and physiological characteristics of the child's body • Timely detection, treatment and prevention of disease • Reducing the mordibity of child • Reduce child mortality
Intrauterine asphixia • Perinatal asphixia of fetus - a pathological condition associated with oxygen deficiency during pregnancy and childbirth. This pathology is one of the most common of perinatal pathology and is one of the most frequent cause of perinatal morbidity (2145%) in the structure of all perinatal pathology
Hypoxic-ishemic encephalopathy pathology is a common complication of pregnancy and childbirth, and diagnosed in newborns up to 5% of cases. Perinatal brain damage is more than 60% of the pathology of the nervous system in childhood, are directly involved in the development of diseases such as: - Cerebral palsy - Epilepsy minimal brain dysfunction
Risk Factors • • • • Mother's age (younger than 20 and older than 35 years) Premature placental abruption Placenta previa Preeclampsia Premature or late birth Coloration of amniotic fluid with meconium Prolonged dry period Diabetes mothers Any diseases of mother during pregnancy Fetus potentially dangerous drugs Ceser section (planned or emergency) The use of forceps (акушерские щипцы) Smoking or other drug addiction during pregnant
Newborn asphyxia - syndrome, characterized by the absence of breathing and the individual not regular, not effective in the presence of cardiac activity
Diagnostics • Assessment of the newborn in a number of parameters: Apgar score (1910) • Signs on the 0 -1 -2 system: state of the heart, respiratory, skin, muscle tone, reflex irritability • A perfect score 10, the rate of 8 -10. distinguish between middle (6 -5 points) and heavy(41 points) the degree of asphyxia. 0 points a dead birth • The visual characteristics of neonatal asphyxia: blue asphyxia (6 -5 p) white asphyxia(4 -1 p)
The sequence of reanimation activities in asphyxia moderate: • Release of the respiratory tract (suction, pear). • Warming the child, MV(ИВЛ) • To the vessels in the umbilical cord is introduced: glucose 10%-5 ml per 1 kg of weight, sodium bicarbonate 2 -4 ml / kg of calcium gluconate 1 ml/kg
The sequence of resustitation activities in asphyxia moderate: • • restore patency of the upper respiratory tract warming of the child intubation, АV I/V(ВВ) products listed higher than 5 mg/kg + hydrocortisone or prednisolone 1 mg / kg • if needed external cardiac massage • Reanimation of the newborn is terminated: 1. If the cardiac activity is not restored within 8 -10 min. 2. If the heart efficiently, but breathing is not restored within 15 -20 minutes. On mechanical ventilation.
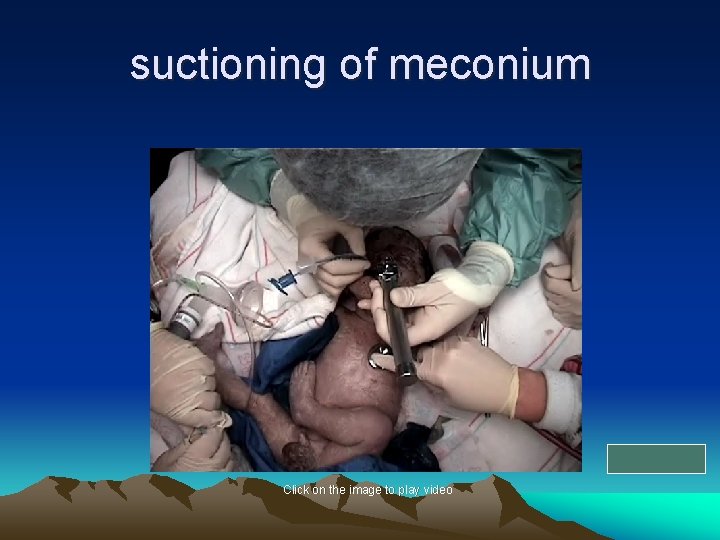
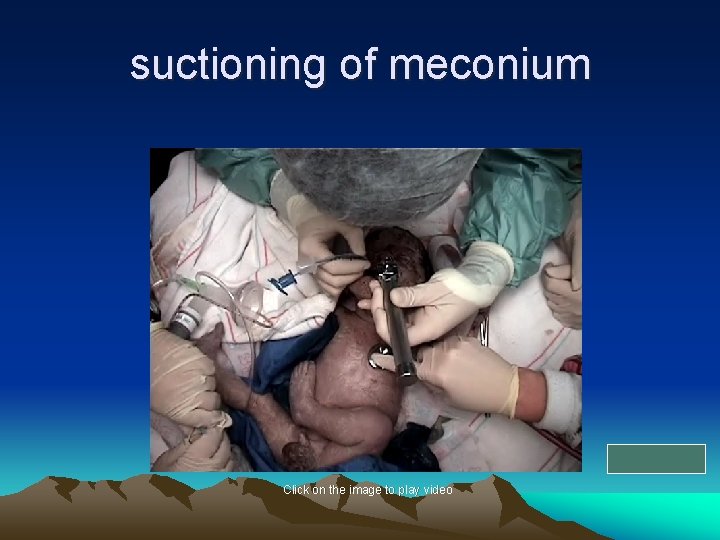
suctioning of meconium Click on the image to play video
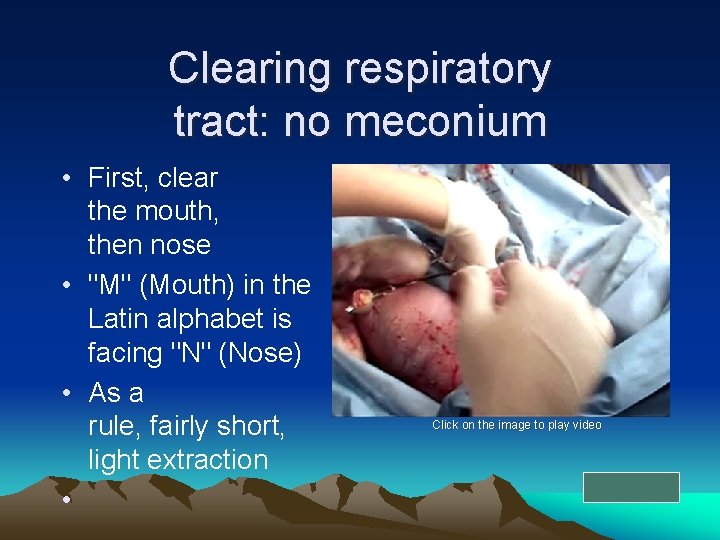
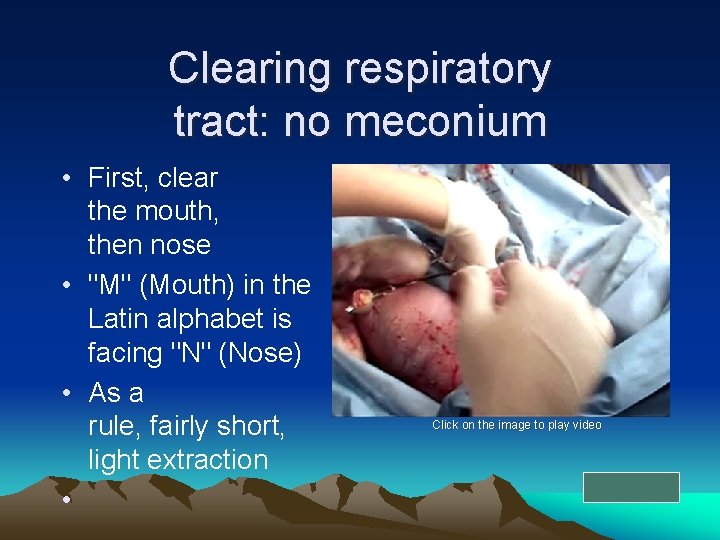
Clearing respiratory tract: no meconium • First, clear the mouth, then nose • "M" (Mouth) in the Latin alphabet is facing "N" (Nose) • As a rule, fairly short, light extraction • Click on the image to play video
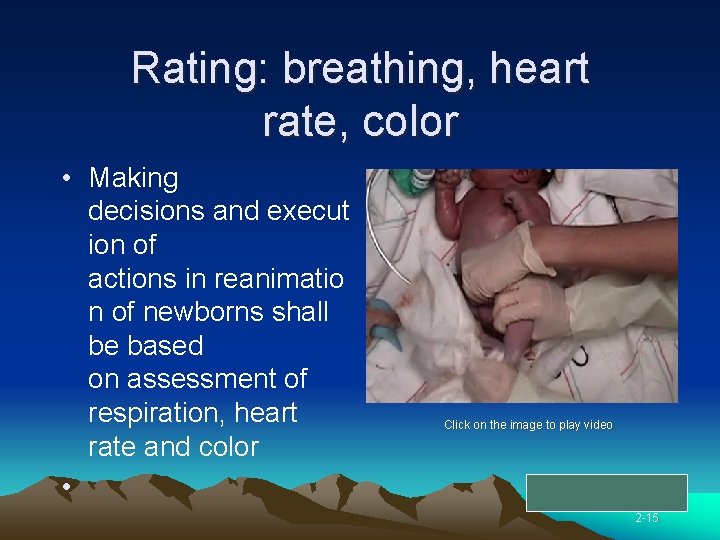
Rating: breathing, heart rate, color • Making decisions and execut ion of actions in reanimatio n of newborns shall be based on assessment of respiration, heart rate and color • Click on the image to play video 2 -15
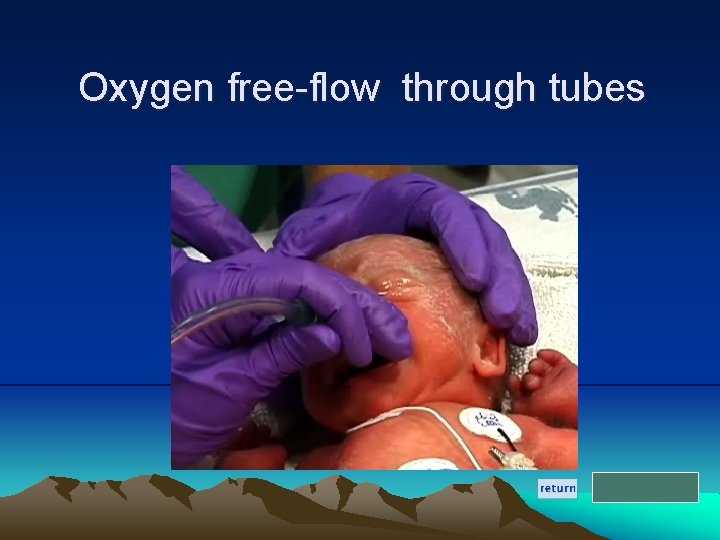
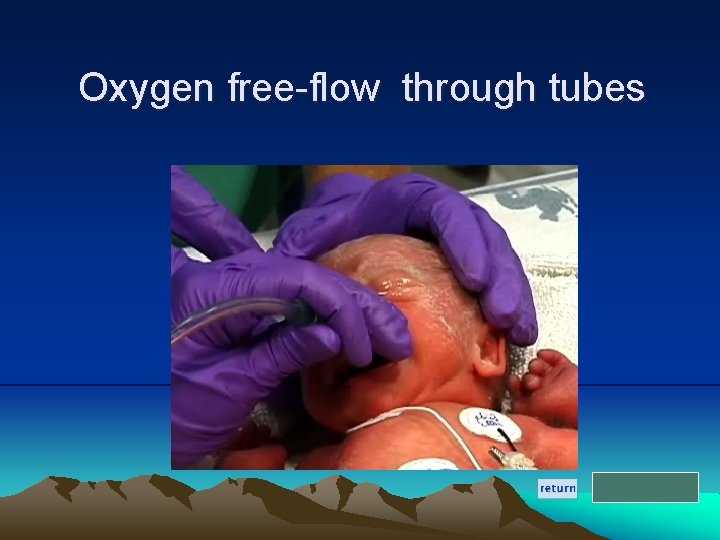
Oxygen free-flow through tubes
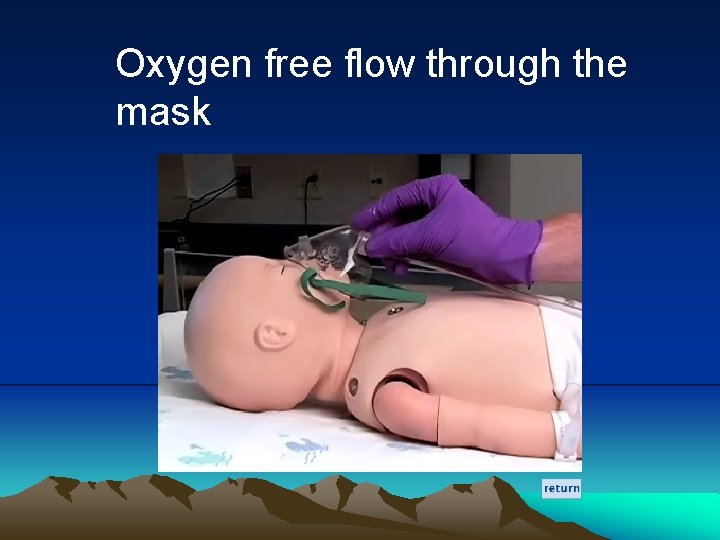
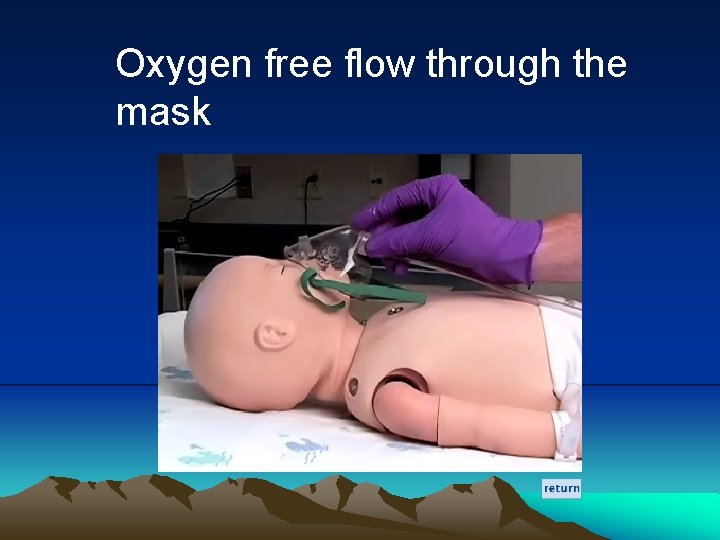
Oxygen free flow through the mask
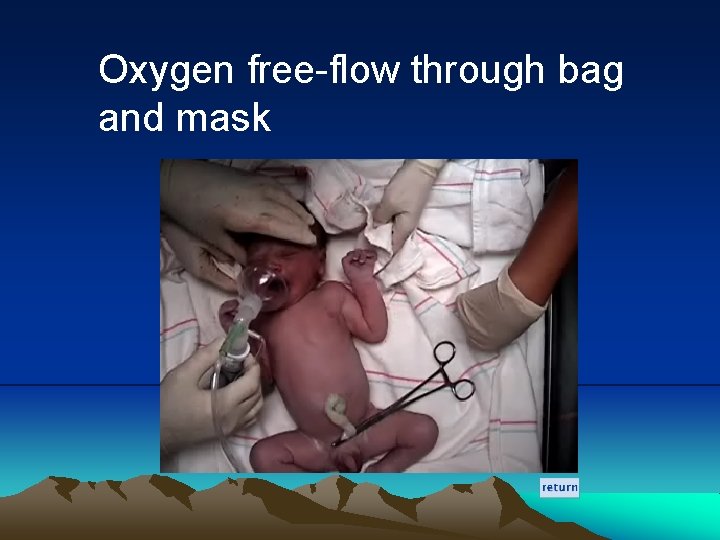
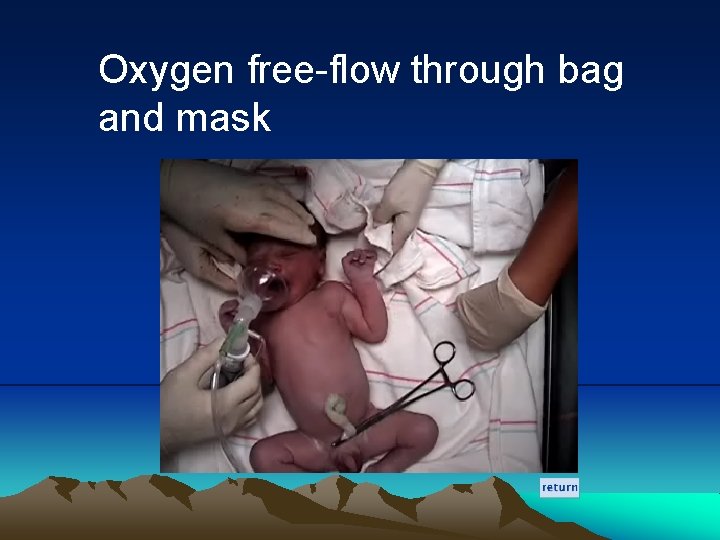
Oxygen free-flow through bag and mask
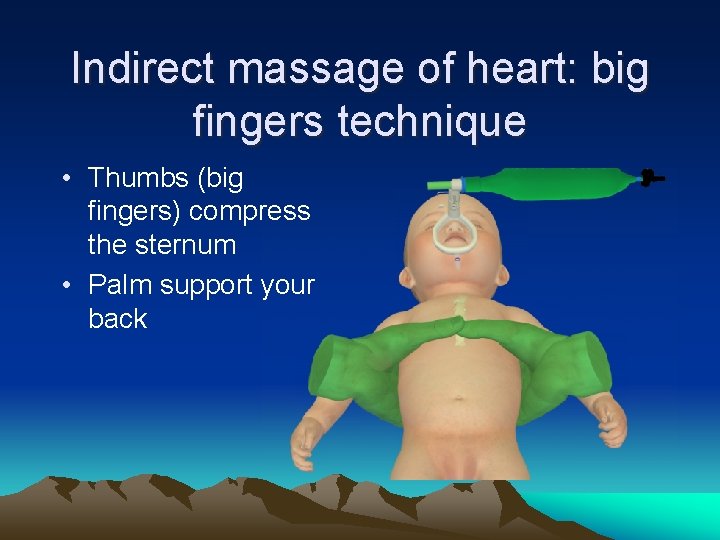
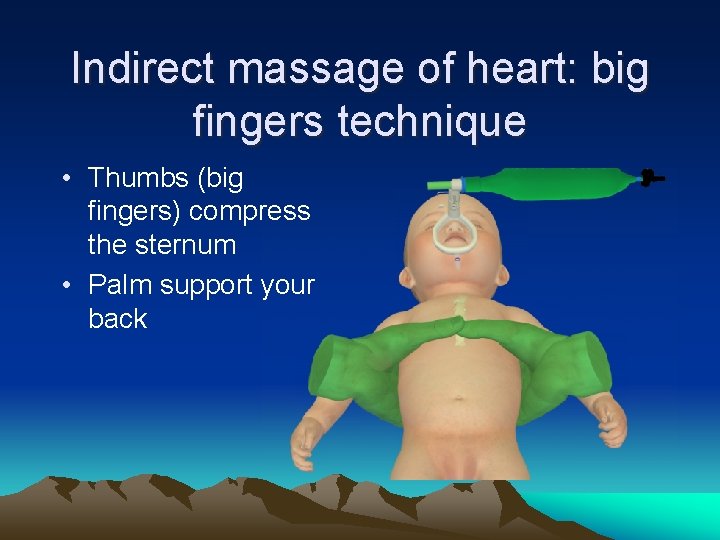
Indirect massage of heart: big fingers technique • Thumbs (big fingers) compress the sternum • Palm support your back
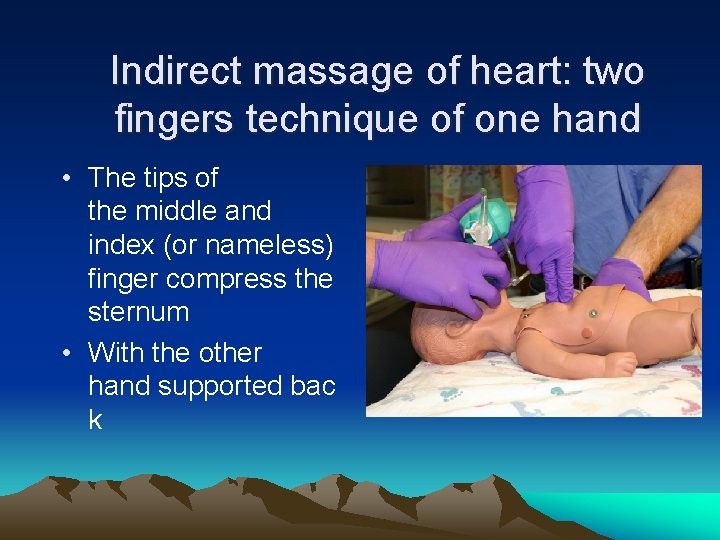
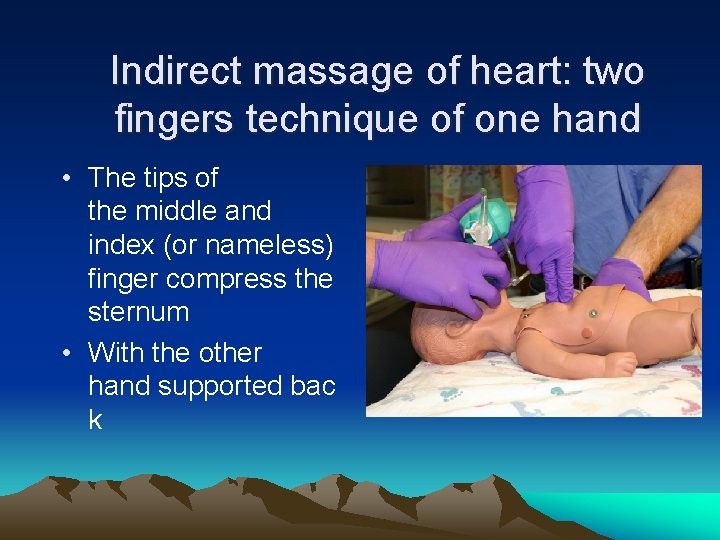
Indirect massage of heart: two fingers technique of one hand • The tips of the middle and index (or nameless) finger compress the sternum • With the other hand supported bac k
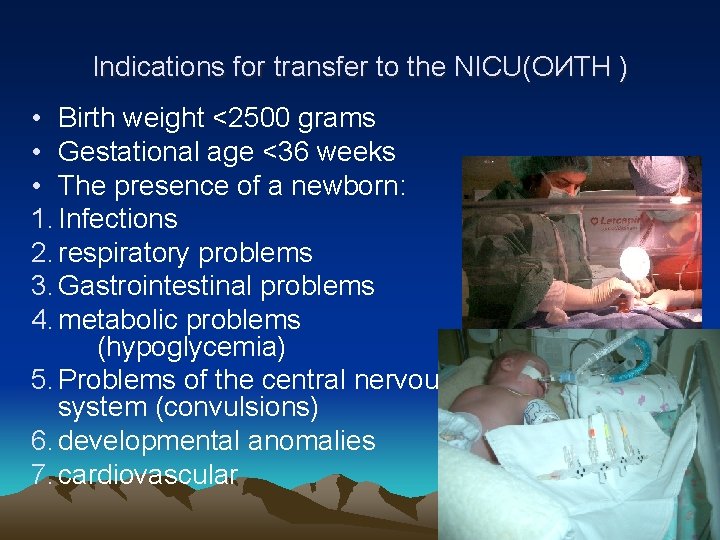
Indications for transfer to the NICU(ОИТН ) • Birth weight <2500 grams • Gestational age <36 weeks • The presence of a newborn: 1. Infections 2. respiratory problems 3. Gastrointestinal problems 4. metabolic problems (hypoglycemia) 5. Problems of the central nervous system (convulsions) 6. developmental anomalies 7. cardiovascular
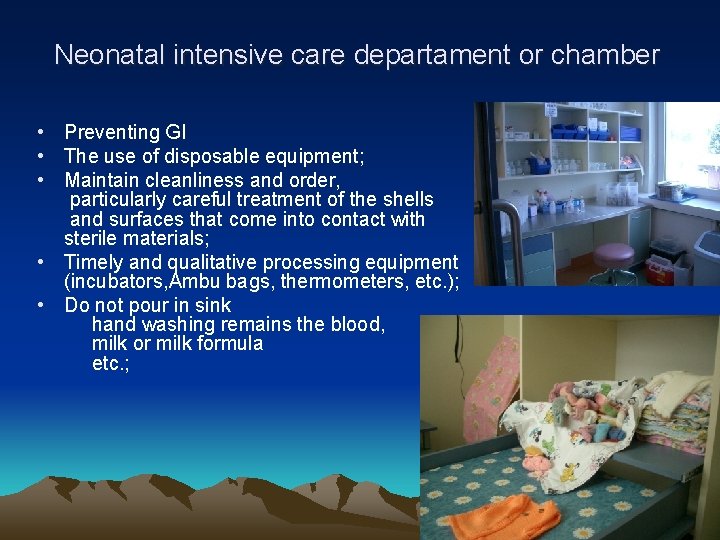
Neonatal intensive care departament or chamber • Preventing GI • The use of disposable equipment; • Maintain cleanliness and order, particularly careful treatment of the shells and surfaces that come into contact with sterile materials; • Timely and qualitative processing equipment (incubators, Ambu bags, thermometers, etc. ); • Do not pour in sink hand washing remains the blood, milk or milk formula etc. ;

Risk Factors • High-risk factor is the neonatal period, the period of adaptation to extrauterine conditions • Processes of respiration, circulation, selection performed with maximum intensity, rapidly growing body weight, renal failure and neuroendocrine regulation of metabolism of water causes dehydration • Transient deficiency of coagulation factors and increased vascular permeability leads to increased bleeding, acidosis
The neonatal period • Border states: physiological jaundice, mastitis, transient fever, the physiological weight loss, albuminuria, sexual crises, urine acid renal infarct • Diseases of the newborn period: viral hepatitis, cytomegaly, malaria, syphilis, toxoplasmosis, CDF(ВПР), birth injuries, cerebral hemocirculation violation, neonatal hemolytic and hemorrhagic disease , septic diseases

Anatomical and physiological features of the nervous system in children • Distinguish the central nervous system (consisting of the brain and spinal cord), peripheral and autonomic nervous system and their activities are coordinated by the cerebral cortex • Brain of newborn is big, functionally immature, and differentiation of its improvementis up to 20 -25 years, the size of 400 g, which is 1 / 8 of the body (adult 1 / 40), doubling the mass is at 9 months, tripling, to 3 years to 20 years increased by 4 -5 times • In the hemispheres of the well-defined grooves and large gyrus, cortical cells, the nervecenters, striate body, the pyramidal paths are not well developed • Gray and white matter little differentiated, neural cortex cells have no processes, no myelinated
Anatomical and physiological features of the nervous system in children • Characterized by weakness and functional, the pulses from Intero and extero receptors cause a passive, long-term deceleration, so the children of the first months of life sleeping most of the time of day. • Basic life functions are regulated by the subcortical centers of the newborn thalamophaliodar system, which explains the unconscious, uncoordinated movements of the newborn •
• Spinal cord at birth 2 -6 g to 5 years tripled, to 20 years and increases by 5 -8 times. It is more perfect than the brain. Myelination antlers of spinal cord occurs in utero, mostly closed arc of innate unconditioned reflexes • The peripheral nervous system of a newborn is presented with rare, not enough myelinated (myelination 2 -4 year) and uneven distribution of nerve fibers • The autonomic nervous system function in the newborn, sympathetic nodes merge into a powerful plexus, sympathicotonia is physiologic, replaced by a 3 -4 year vagotonia •
3. Distinguish the following stages of morphological changes in the hypoxic brain: Stage I - edematous-hemorrhagic, Stage II - encefal gliosis, Stage III - leukomalacia (necrosis) Stage IV - leukomalacia with hemorrhage. 4. The clinical picture of hypoxic encephalopathy divided into three periods - Acute (1 st month of life) - Reduction (from 1 month to 1 year, and in immature preterm infants under 2 years) - outcome
According To the stream • Light form • Moderate • Heavy In the acute period allocate 5 clinical syndromes: 1. Increase of neuro-reflex excitability 2. Convulsive 3. Hypertension - hydrocephalic 4. Depression syndrome 5. Comatose •
The syndrome of increased neuroreflex excitability. - Spontaneous motor activity - troubled - superficial sleep - Lengthening the period of active wakefulness - Difficulty falling asleep - Frequent crying unmotivated - Revitalization of unconditioned innate reflexes - Muscle dystonia - Improvement of knee reflexes - Tremor of extremities and chin
Hypertension-hydrocephalic syndrome • - Increasing the size of the head of 1 -2 sm compared with the norm (or the circumference of the chest) - Unlocking the sagittal suture over 0. 5 sm - Increase and a bulging fontanelle large - Graefe symptom - A symptom of "sunset" - Intermittent horizontal nystagmus - Convergent squint •
Depression syndrom • • • Apathy Hypodynamy Reduction of spontaneous activity The general muscle hypotonia Hyporeflexia (decreased reflexes, sucking and swallowing) • Divergent and convergent squint • Nystagmus • Bulbar and pseudobulbar symptoms
• • • • Comatose syndrome reaction to light a small or absent. no response to painful stimuli. "floating" movement of the eyeballs. adynamia, severe lethargy. hypotonia to atony. innate reflexes are not detected. pupils contracted. horizontal and vertical nystagmus. tendon reflexes were depressed. Irregular breathing with frequent apnea bradycardia low blood pressure. Convulsive seizures may occur. does not sulk and swallowing.
Convulsive syndrome • - In the acute stage is usually / combined with the syndrome of depression or comatose - Arises as a result of hypoxic brain edema - - Hypomagnemy or intracranial hemorrhage - Appears in the first days of life tonic-clonic or tonic convulsions - Convulsions in neonates differ brevity of sudden onset - The lack of regularity and repetition of the state of sleep or wakefulness - Convulsions are observed in the small amplitude tremor guide short-term cessation of breathing - Tonic spasm of the eyeballs by the type of paresis of gaze upwards - Simulate the symptoms of "sunset" and nystagmus - Convulsions, by its nature is sometimes reminiscent of spontaneous movements •
The recovery period hypoxic encephalopathy syndromes include the following • improvement of neuro-reflex excitability • hypertension-hydrocephalic • vegetative-visceral dysfunctions • movement disorders • psychomotor retardation
А. Syndrome increase the neuro-reflex excitability During the recovery period has two current version: 1. marked decrease or disappearance of symptoms of increased neuro-reflex excitability in a period of 4 - 6 months to 1 year. 2. In the worst case, especially in premature infants, may develop epileptic syndrome
B. Hypertension-hydrocephalic syndrome Has two current version: 1) hypertension-hydrocephalic syndrome with favorable course, in which the disappearance of hypertensive symptoms, delay in hydrocephalic; 2) The worst case of hypertensionhydrocephalic syndrome occurring in organic symptom complex cerebral syndrome Outcomes of hypertension - hydrocephalic syndrome: 1. Normalization of growth in head circumference at 6 months. 2. Compensated hydrocephalic syndrome in 8 - 12 months. 3. The development of hydrocephalus
C. The syndrome of vegetative- visceral dysfunctions Begins to emerge after 1 -1. 5 months of life on • • background of increased neuro-reflex excitability and hypertension - hydrocephalic syndrome. The clinical picture: persistent regurgitation. persistent hypotrophy. violation of the respiratory rate and apnea. discoloration of the skin, acrocyanosis. paroxysmal tachycardia - and bradipnoe. disorder of thermoregulation. dysfunction of the gastrointestinal tract. temporal alopecia.
D. Epileptic syndrome Observed in generalized convulsive seizures • • • (Tonic-clonic, tonic) abortive Focal Hemi-convulsive polymorphic convulsions simple and complex absences. In terms of frequency, is dominated by polymorphic forms of convulsions. . Premature infants with perinatal encephalopathy and propulsive impulse paroxysms in isolation does not occur, and occur only in the polymorphic convulsions. The greatest difficulty in diagnosis are aborted and nonconvulsive form of paroxysms
E. The syndrome of motor disorders proceeds with muscular hypotonia or hypertonia. • When the syndrome of motor disorders with hypotonia there is a decrease of spontaneous motor activity. • suppression of tendon reflexes and innate unconditioned reflexes of newborns. • The increase in muscle hypertension in term infants, the emergence of multilateralism focal symptoms should alert in terms of development infantile cerebral paralysis. •
F. Psychomotor retardation syndrome Begins to manifest itself with 1 - 2 months • violation of unconditional reduction innate reflexes • retention the formation of rectifying the labyrinth of chain tonic reflexes • to months of age there is not enough stable fixation • short-term follow up with the rapid depletion • unfavorable long-term mental retardation.
G. Psychomotor retardation syndrome • No reaction to his mother's voice, acoustic concentration • By 2 to 3 months of age there is insufficient recovery in communication, low-expressive cry, there is no "hoolin" • For half a year - are not actively interested in the toys and the surrounding objects, there is no active attention. • Age-related motor function are beginning to be compensated after 6 -7 months and usually are restored to 1 - 1. 5 years. Prognostically unfavorable long delay in psychomotor development
Diagnostics • In the study of ocular fundus in the acute period of moderately degree dilatated veins mark, edema, some hemorrhage. In Heavy degree damage on the background of edema, vasodilatation observed stushevan nost border of the optic nerve, hemorrhage.
• Neurosonography - twodimensional ultrasonic research anatomical structures of the brain through a large fontanel - allows setting of periventricular hemorrhage, leukomalacia cent ers, expansion of the ventricular system ventriculomegaly. • Signs of hypoplasia of the brain: an increase in subarachnoid space, the expansion ofthe interhemispheric gap, ventriculomegaly, increased density in the brain parenchymawithout clear differentiation of gyri
• In the cerebrospinal fluid detected changes in the presence of intracranial hemorrhage. In these cases, the cerebrospinal fluid are fresh and leached red blood cells. • After 7 - 10 days of life confirmation the transferred hemorrhage is the presence of macrophages in the cerebrospinal fluid.
• Electroencephalographic (EEG) study reveals centers of slow-wave activity, reduction centers of cortical rhythm, centers of epileptic activity. • EEG is used to allocate risk for convulsions and diagnosis of clinically "silent" attacks. An indirect confirmation of convulsive syndrome, as well as a sign of lowering the threshold of convulsive readiness of patients is the presence of paroxysmal EEG changes. Repeated convulsions can lead to increased expression of paroxysmal activity on EEG.
• From biochemical researches in acute hypoxic disorders the depth indicator is assessment of a mixed acidosis to expressed decompensated, metabolic. • At heavy hypoxia increases the osmotic pressure of blood plasma, increased levels of lactate dehydrogenase.
Treatment of the acute period • 1. Reduction of vascular permeability: 12. 5% etamzilate solution intramuscularly or intravenously, 1% vikasol 0. 1 ml / kg. 2. Metabolic and anti-oxidant therapy: piracetam 50 mg / kg, 10% glucose 10 ml / kg, , Actovegin - intravenously, 5% vitamin E 0. 1 ml per day. 3. Vascular Therapy: Vinpocetine 1 mg/kg intravenously. 4. Dehydration therapy: 3 -10 mg hydrocortisone / kg prednisolone 1 - 2 mg / kg, 25% magnesium sulfate 0. 2 ml / kg. 5. Improvement of cardiac muscle tissue metabolism: cocarboxylase 8 mg / kg, ATP 10 mg / kg. 6. Anticonvulsant therapy: diazepam 1 mg/kg intramuscul arly or intravenously, GHB, 50 mg / kg, barbiturates.
Treatment in the recovery period 1. Syndrome of increased excitability of the neuroreflex manifestations of vegetative-visceral dysfunctions are shown sedative: Diazepam 0. 001 g, 2 times a day, with citral mixture of 1 teaspoon 3 times a day. 2. When hypertension-hydrocephalic syndrome advisable to appoint furosemide 0, 002 g / kg per day with panangina, glycerol and 1 teaspoon 3 times a day. When expressed forms of hypertension-hydrocephalic syndrome diakarb is useful 0. 02 g / kg per day once under the scheme: 3 days - reception, a 1 day of break, the course of 3 weeks to 1 - 1. 5 months, with panangina. 3. Syndrome of motor disorders: vitamin B 6 5 mg, Vitamin B 1 2 mg, 0. 5 ml ATP 10 -12 injections, piritinol 10 - 20 drops to 1 kg of body weight 2 times a day in the morning 1 -3 months. Massage. Gymnastics, mothers are trained rehabilitation skills 4. At a syndrome of psychomotor retardation: Piracetam 30 - 50 mg / kg in 3 divided doses.

Safe and proper use of technology

proper technology • The effectiveness and safety (DM) • Effectiveness and stability • Eligibility for both patient and healthcare workers

Being together mother and child, and kangaroo method are the appropriate technologies
Benefits of breastfeeding • Natural feeding - feeding infants breast milk, followed by supplemental feeding with 6 months • Breastfeeding the most physiologic of quantitative and qualitative composition and optimally cover all the needs of the child in proteins, fats, carbohydrates, vitamins, minerals, etc. •
Benefits of breastfeeding • Breastmilk is dominated by fine dispersed proteins (albumins), cow's milk proteinscoarsely dispersed (casein) and protein is smaller than in cow's milk • Breast milk contains several times more polyunsaturated fatty acids and lipolysis in the stomach in children begins under the influence of breast milk lipase • Breast milk contains large amounts of carbohydrates (blactose) in the cow's milk is alactose. Lactose milk stimulates the growth of bifidobacteria.
Benefits of breastfeeding • Breast milk is rich in enzymes: amylase (100 times), trypsin, lipase (15 times). This compensates for the temporary low enzyme activity and provides digestibility • The concentration of microelements, vitamins, enzymes in human breast milk is optimal and corresponds to the needs of the child • Breast milk is rich in immunoglobulins (A, G), contains the factors of specific and nonspecific resistance • Formed a psychological link between baby and mother, developed a sense of parenting
Reasons of hypogalactia • Later breastfeeding, a rare breastfeeding, reglementation of breastfeeding a technical approach to control the process of lactation disorder, hurrying • In case of insufficient lactation recommended frequent (2 -2, 5 hours, without night interval) feeding • The mother produced as much milk as a baby needs to feed to give both breasts to prevent lactostasis and to stimulate lactation • Child with breastfeeding should not drink water, because breast milk to 80% water and therefore quench the thirst
Reasons of hypogalactia • Violation of the regime breastfeeding women (excessive physical and mental stress, lack of sleep disorders to diet, disease, age) reduces the lactation • Less likely to breast feed very young and elderly mother. In elderly is attributable to biological causes, the young - the social and psychological (absence family planning, casual birth, lack of spirit in breastfeeding) Incorrectly feeding techniques
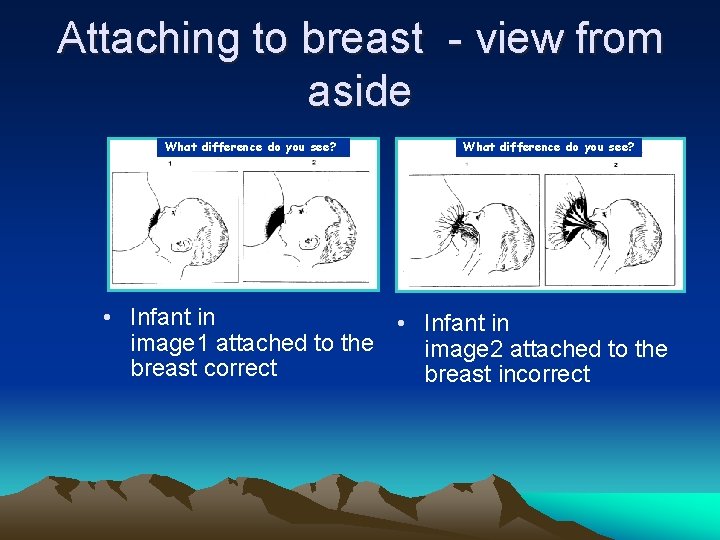
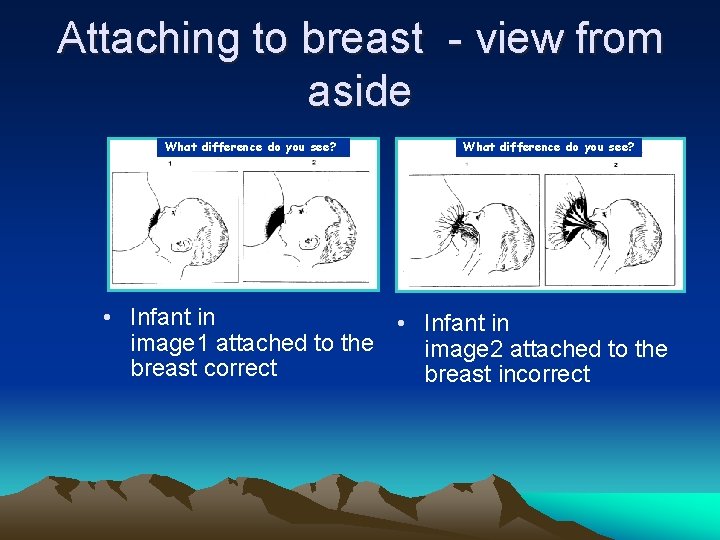
Attaching to breast - view from aside What difference do you see? • Infant in image 1 attached to the image 2 attached to the breast correct breast incorrect
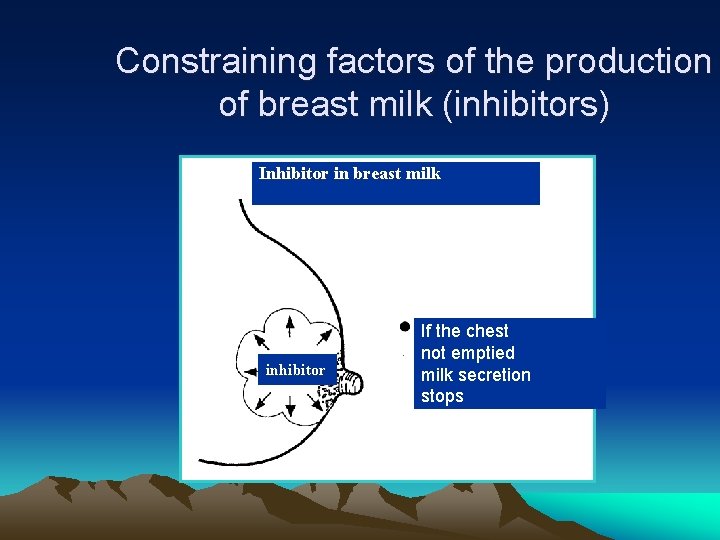
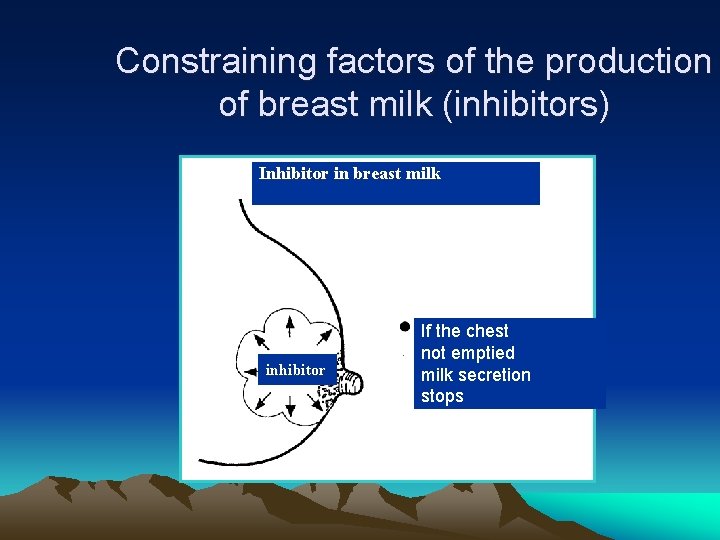
Constraining factors of the production of breast milk (inhibitors) Inhibitor in breast milk inhibitor If the chest not emptied milk secretion stops
Regulation secretion of milk in the mammary gland • Inhibitor of lactation in breastmilk synthesized by stagnation of milk in the ducts • Synthesis and secretion are regulated by extension alveolar cells •
Factors that increase formation and excretion the mother's milk • Convince the mother to the ability of breast -feeding her baby • Eliminate the disturbing state of the mother • The mother should sit down and try to express her milk • Before pumping it is desirable to lay the child on the mother's abdomen
Factors that increase formation and excretion the mother's milk • It is recommended to drink hot milk and tea to keep warm in the chest, pinch the tips of the breast • You can do a back massage along the spine • Massage the breast before feeding (longitudinal movement from the base of glands to the nipple) • Nicotinic acid, vitamin E, UFL, UHF, ultrasound, herbal medicine

 Clear perinatal quality
Clear perinatal quality Perinatal matrices
Perinatal matrices Fatin organ
Fatin organ Perinatal asphyxia
Perinatal asphyxia Neonatarum
Neonatarum Perinatal audit
Perinatal audit Uyarıcı zenginliği ve yoksunluğu nedir
Uyarıcı zenginliği ve yoksunluğu nedir Indiana perinatal quality improvement collaborative
Indiana perinatal quality improvement collaborative Certain conditions originating in the perinatal period
Certain conditions originating in the perinatal period Ccqi perinatal standards
Ccqi perinatal standards South dakota perinatal association
South dakota perinatal association Standing around crying
Standing around crying Perinatal period
Perinatal period Ruta materno perinatal
Ruta materno perinatal Waiter's tip deformity
Waiter's tip deformity Hie grading
Hie grading Defense priority allocation system
Defense priority allocation system Goals and priorities
Goals and priorities Goals and priorities
Goals and priorities Goals and priorities
Goals and priorities Goals and priorities
Goals and priorities Yorkshire and humber neonatal network
Yorkshire and humber neonatal network Volkswagen of america: managing it priorities
Volkswagen of america: managing it priorities 6 national core standards
6 national core standards Priorities of work patrol base
Priorities of work patrol base Bsa wilderness survival kit
Bsa wilderness survival kit Ggt 2030 application form
Ggt 2030 application form A link between relationships chapter 14
A link between relationships chapter 14 Core priorities
Core priorities Wood badge vision statement examples
Wood badge vision statement examples 6 quality priorities
6 quality priorities Core priorities
Core priorities Ampdu priorities
Ampdu priorities Cross curricular priorities
Cross curricular priorities Preferred priorities for care
Preferred priorities for care Priorities
Priorities Supplier and distributor benchmarking
Supplier and distributor benchmarking Cs 6340
Cs 6340 Mixed priorities
Mixed priorities Xkcd priorities
Xkcd priorities Cerebral
Cerebral Circulação neonatal
Circulação neonatal Triade neonatal
Triade neonatal Tamiz neonatal
Tamiz neonatal Esfuerzo respiratorio neonatal
Esfuerzo respiratorio neonatal Hastalık düzeyini belirleyen ölçütler
Hastalık düzeyini belirleyen ölçütler Neonatal sepsis pathophysiology diagram
Neonatal sepsis pathophysiology diagram Sepsis neonatal temprana y tardía
Sepsis neonatal temprana y tardía Clasificacion de kramer ictericia
Clasificacion de kramer ictericia Infant mortality rate formula
Infant mortality rate formula Poliglobulia
Poliglobulia Exaguinotransfusion
Exaguinotransfusion Phototherapy machine diagram
Phototherapy machine diagram Parâmetros iniciais ventilação mecânica neonatal
Parâmetros iniciais ventilação mecânica neonatal Pain scale with words
Pain scale with words Halo oxigeno
Halo oxigeno As evidenced by nursing
As evidenced by nursing Suprasternal retraction
Suprasternal retraction Neonatal sepsis
Neonatal sepsis L
L Dope neonatal resuscitation
Dope neonatal resuscitation Pathologic jaundice newborn
Pathologic jaundice newborn Iap slides
Iap slides Neonate apgar score
Neonate apgar score Zonas de kramer ictericia neonatal
Zonas de kramer ictericia neonatal Bilirrubina valores normales
Bilirrubina valores normales