pericardial diseases Dr SHEHZAD ASLAM Head of Department

- Slides: 43
pericardial diseases Dr SHEHZAD ASLAM Head of Department Cardiology
Anatomy and Physiology of the Pericardium n 1. 2. The pericardium is composed of two layers, The visceral pericardium, a monolayer membrane of mesothelial cells and associated collagen and elastin fibers that is adherent to the epicardial surface of the heart, and The fibrous parietal layer, which is about 2 mm thick in normal humans and surrounds most of the heart
n n The pericardial space or sac is contained within these two layers and normally contains up to 50 m. L of serous fluid. The best-characterized mechanical function of the pericardium is its restraining effect on cardiac volume. The parietal pericardium has a tensile strength similar to that of rubber. At low applied stresses similar to those at physiologic or subphysiologic cardiac volumes, it is very elastic. As stretch increases, the tissue fairly abruptly becomes stiff and resistant to further stretch.
Acute pericarditis n Acute pericarditis, defined as symptoms or signs resulting from pericardial inflammation of no more than 1 to 2 weeks in duration
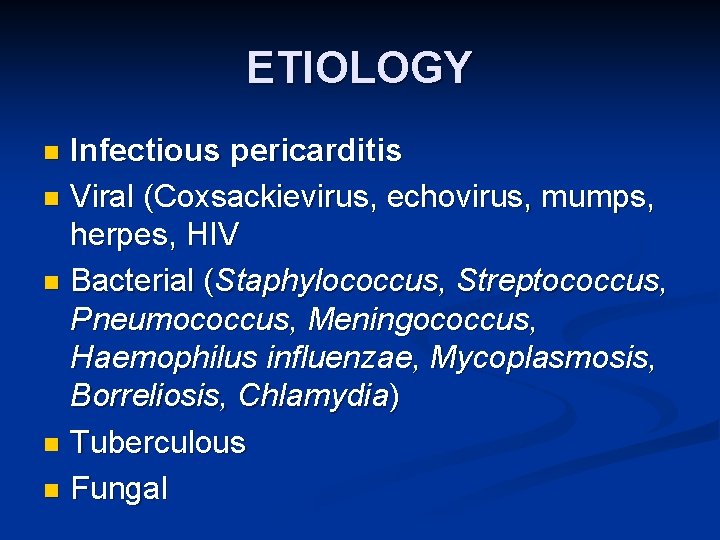
ETIOLOGY Infectious pericarditis n Viral (Coxsackievirus, echovirus, mumps, herpes, HIV n Bacterial (Staphylococcus, Streptococcus, Pneumococcus, Meningococcus, Haemophilus influenzae, Mycoplasmosis, Borreliosis, Chlamydia) n Tuberculous n Fungal n
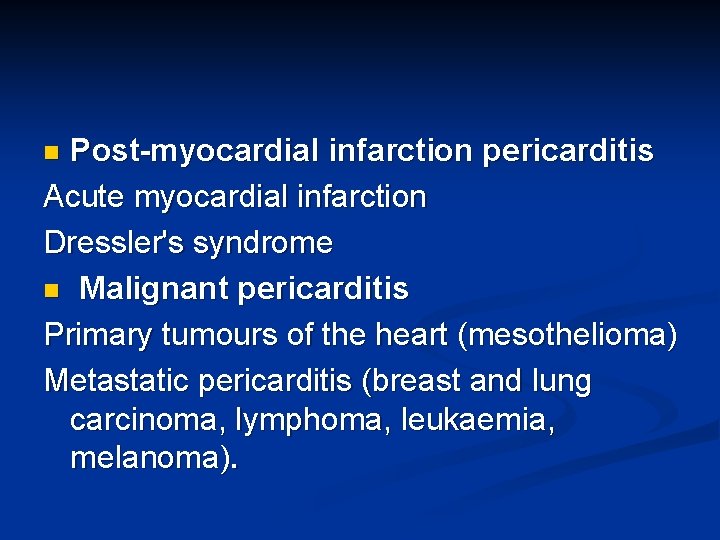
Post-myocardial infarction pericarditis Acute myocardial infarction Dressler's syndrome n Malignant pericarditis Primary tumours of the heart (mesothelioma) Metastatic pericarditis (breast and lung carcinoma, lymphoma, leukaemia, melanoma). n
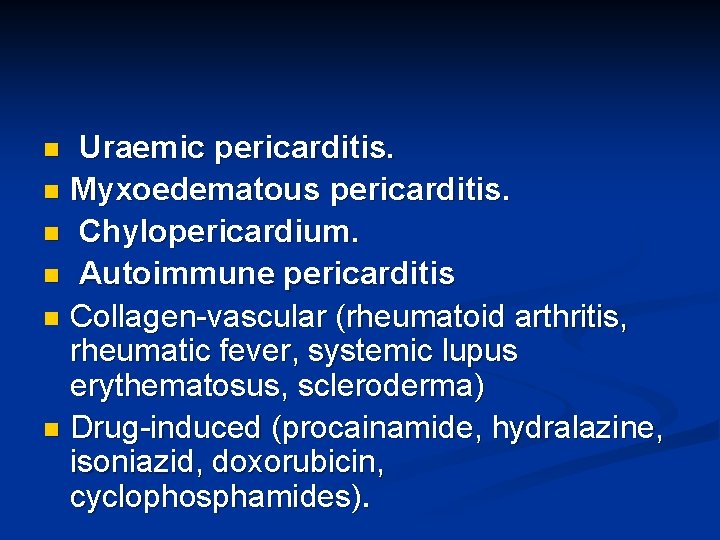
Uraemic pericarditis. n Myxoedematous pericarditis. n Chylopericardium. n Autoimmune pericarditis n Collagen-vascular (rheumatoid arthritis, rheumatic fever, systemic lupus erythematosus, scleroderma) n Drug-induced (procainamide, hydralazine, isoniazid, doxorubicin, cyclophosphamides). n
Post-radiation pericarditis. n Post-surgical pericarditis n Post-traumatic pericarditis. n Familial and idiopathic pericarditis n
Viral pericarditis. The most common viral causes are Coxsackie B virus and echovirus. n Viral pericarditis is usually painful but has a short time course and rarely long-term effects. Increasingly, HIV is implicated in the aetiology of pericarditis, both directly and via immunosuppression, which predisposes the subject to infective causes. n
Post-myocardial infarction pericarditis n n n It occurs in about 20% of patients in the first few days following MI. It occurs more commonly with anterior MI and ST elevation MI with high serum cardiac enzymes, Pericarditis may also occur later on in the recovery phase after infarction. This usually occurs as a feature of Dressler's syndrome, an autoimmune response to cardiac damage occurring 2 -10 weeks post-
Uraemic pericarditis is due to irritation of the pericardium by accumulating toxins. n It can occur in 6 -10% of patients with advanced renal failure if dialysis is delayed. n It is an indication for urgent dialysis as it continues to be associated with significant morbidity and mortality n
CLINICAL FEATURES chest pain. n n n The pain of pericarditis can be quite severe. It is variable in quality but almost always pleuritic. Pericardial pain typically has a relatively rapid onset and sometimes begins remarkably abruptly. It is most commonly substernal but can be centered in the left anterior chest or epigastrium. Left arm radiation is not unusual. The most characteristic radiation is to the trapezius ridge, which is highly specific for pericarditis.
Pericardial pain is almost always relieved by sitting forward and worsened by lying down. n Associated symptoms can include dyspnoea, cough, and occasionally hiccoughs. n An antecedent history of symptoms suggesting a viral syndrome is common. n It is important to review the past medical history for clues to specific etiologic n
Physical Examination Patients with uncomplicated acute pericarditis often appear uncomfortable and anxious n and may have low-grade fever and sinus tachycardia. n It is important to perform a careful, complete physical examination in a patient with acute pericarditis and to look for clues to specific etiologic diagnoses. n
PERICARDIAL RUB n n n caused by contact between visceral and parietal pericardium. It consists of three components corresponding to ventricular systole, early diastolic filling, and atrial contraction and is similar to the sound made when walking on crunchy snow. The rub is usually loudest at the lower left sternal border and is best heard with the patient leaning forward. It is often dynamic, disappearing and returning during short periods.
n Sometimes what is considered a pericardial rub has only two components or even one component. Such findings should be labeled rubs with caution because the sound may actually represent a murmur.
Differential Diagnosis n n n n Acute myocardial infarction. Pneumonia or pneumonitis with pleurisy Pulmonary embolus or infarction, Costochondritis , and gastroesophageal reflux disease. Aortic dissection, Pneumothorax , and Herpes zoster pain before skin lesions appear. Finally, acute pericarditis is occasionally the presenting manifestation of a preceding, silent MI.
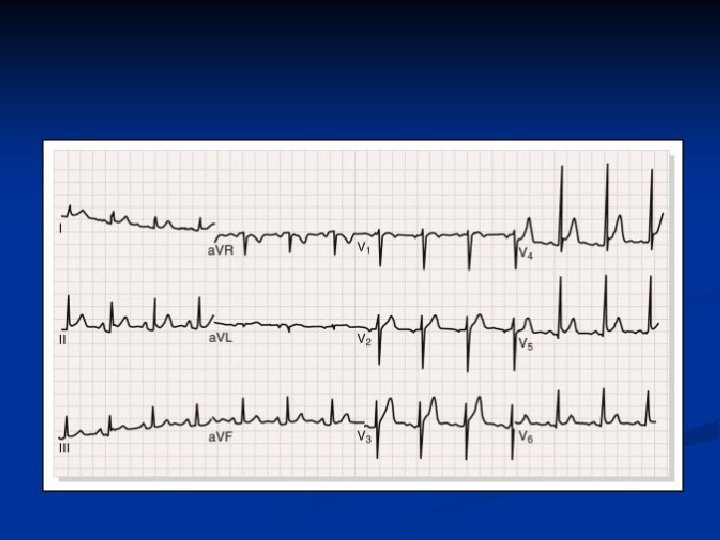
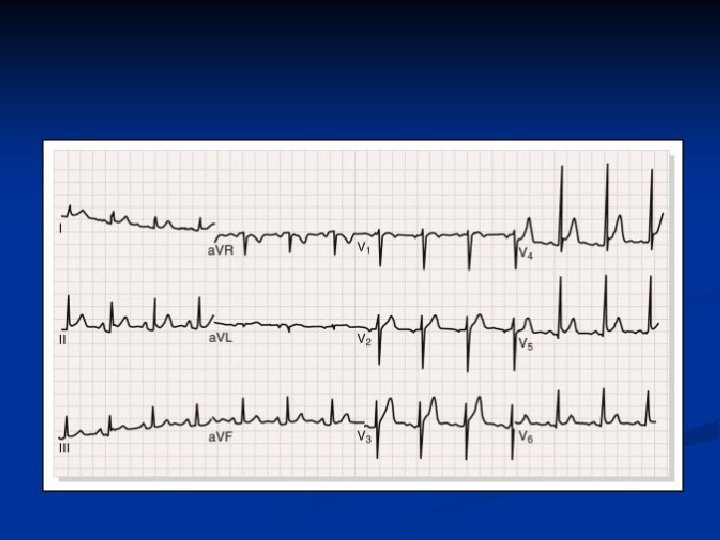
INVESTIGATIONS ECG The classic finding is diffuse ST-segment elevation in all leads except a. VR and often V 1. n The ST segment is usually coved upward n the distinction between acute pericarditis and transmural ischemia is usually not difficult because of more extensive lead involvement in pericarditis and the presence of much more prominent
n n n PR-segment depression is also common PR depression can occur without ST elevation and be the initial or sole electrocardiographic manifestation of acute pericarditis. The ECG reverts to normal during days or weeks. In others, the elevated ST segment passes through the isoelectric point and progresses to ST-segment depression and T wave inversions in leads with upright QRS complexes. Atrioventricular block may indicate Lyme disease, Pathologic Q waves can signify a previous silent MI
n Hemogram Modest elevations of the white blood cell count with mild lymphocytosis are common in acute idiopathic pericarditis. Higher counts are an alert for the presence of other causes, as is anemia. n Cardiac Enzymes and Troponin Measurements A significant fraction of patients have elevated creatine kinase MB fraction or troponin I values. This suggests a significant incidence of concomitant, otherwise silent myocarditis.
Chest Radiography n n n The chest radiograph is usually normal in uncomplicated acute idiopathic pericarditis. Tuberculous pericarditis can occur with or without associated pulmonary disease. Mass lesions and enlarged lymph nodes suggestive of neoplastic disease also have great significance. Small to even moderate effusions may not cause an abnormal cardiac silhouette
Echocardiography The echocardiogram is normal in most patients with acute idiopathic pericarditis. n The main reason for its performance is to exclude an otherwise silent effusion. Echocardiography is also useful in delineating whether associated myocarditis is severe enough to alter ventricular function as well as in detection of MI. n
TREETMENT Acute idiopathic pericarditis is a self-limited disease without significant complications or recurrence in 70% to 90% of patients. n Nonsteroidal anti-inflammatory drugs (NSAIDs) should be initiated. n Ibuprofen (600 to 800 mg orally three times daily) with discontinuation if pain is no longer present after 2 weeks n
Patients who respond slowly or inadequately to NSAIDs may require supplementary narcotic analgesics to allow time for a full response or a course of colchicine. n Colchicine is administered as a 2 - to 3 -mg oral loading dose followed by 1 mg daily for 10 to 14 days. n
Recurrent or relapsing pericarditis Treatment of recurrent pain is empiric. For an initial relapse, a second 2 -week course of an NSAID is often effective. n A course of colchicine may be at least as effective. n
Pericardial Effusion and Cardiac Tamponade n A pericardial effusion is a collection of fluid within the potential space of the serous pericardial sac commonly accompanying an episode of acute pericarditis. n Cardiac Tamponade When a large volume collects in this space, ventricular filling is compromised leading to embarrassment of the circulation. This is known as cardiac tamponade.
Clinical features n n Heart sounds are soft and distant. Apex beat is commonly obscured. A friction rub may be evident due to pericarditis in the early stages, but this becomes quieter as fluid accumulates and pushes the layers of the pericardium apart. Rarely, the effusion may compress the base of the left lung, producing an area of dullness to percussion below the angle of the left scapula (Ewart's sign).
Hemodynamic Consequences 1. n n n EQUALIZATION OF FILLING PRESSURES As fluid accumulates, left- and right-sided atrial and ventricular diastolic pressures rise and in severe tamponade equalize at a pressure similar to that in the pericardial sac, typically 15 to 20 mm Hg Equalization is closest during inspiration. Thus, the pericardial pressure dictates the intracavitary pressure, and the transmural filling pressures of the cardiac chambers are very low. Because transmural right-sided heart filling pressure is normally lower than left-sided heart filling pressure (upper limit of right atrial pressure ∼ 7 mm Hg, left atrial pressure ∼ 12 mm Hg), as fluid accumulates, filling pressure increases more rapidly in the right side than in the left side of the heart.
2: LOSS OF Y DECENT IN JVP (FRIEDREICH'S SIGN) The x and y descents of the venous pressure waveform correspond to periods when flow is increasing. Loss of the y descent has been explained on the basis of the concept that total heart volume is fixed in severe tamponade. Thus, blood can enter the heart only when blood is simultaneously leaving. The right atrial y descent begins when the tricuspid valve opens, that is, when blood is not leaving the heart. Thus, no blood can enter, and the y descent is lost.
n n PULSUS PARADOXUS. Abnormally large decline in systemic arterial pressure during inspiration (usually defined as a drop of >10 mm Hg in systolic pressure). The interventricular septum shifts to the left in exaggerated fashion on inspiration, encroaching on the left ventricle such that its stroke volume and pressure generation are further reduced
Although the inspiratory increase in right-sided heart volume (preload) causes an increase in right ventricular stroke volume, this requires several cardiac cycles to increase left ventricular filling and stroke volume and to counteract the septal shift. n Increased afterload caused by transmission of negative intrathoracic pressure to the aorta and traction on the pericardium caused by descent of the diaphragm, which increases pericardial pressure
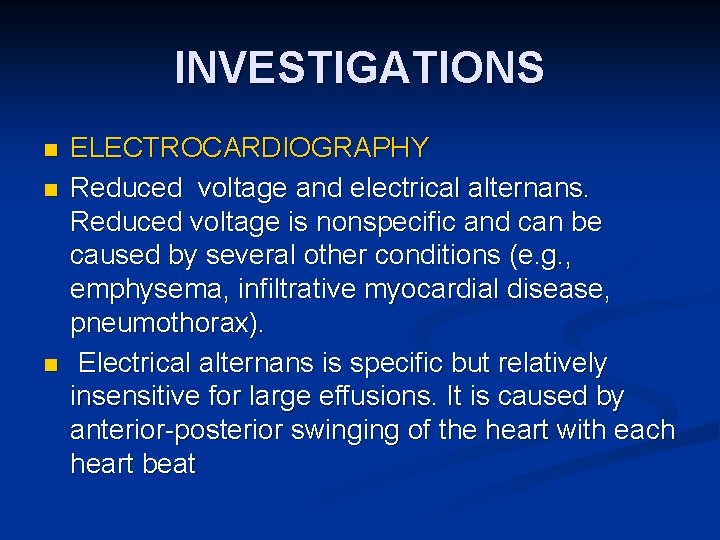
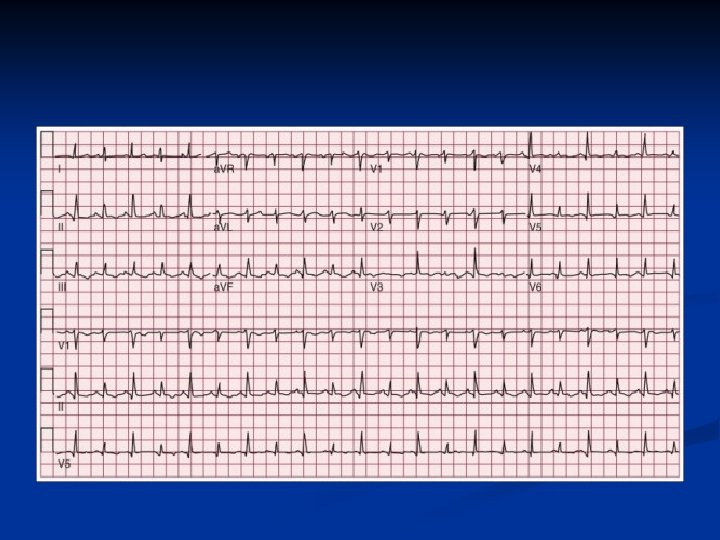
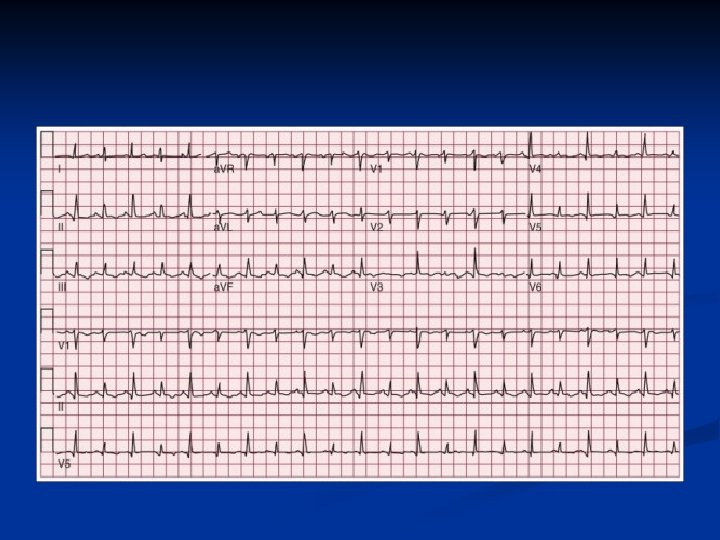
INVESTIGATIONS n n n ELECTROCARDIOGRAPHY Reduced voltage and electrical alternans. Reduced voltage is nonspecific and can be caused by several other conditions (e. g. , emphysema, infiltrative myocardial disease, pneumothorax). Electrical alternans is specific but relatively insensitive for large effusions. It is caused by anterior-posterior swinging of the heart with each heart beat
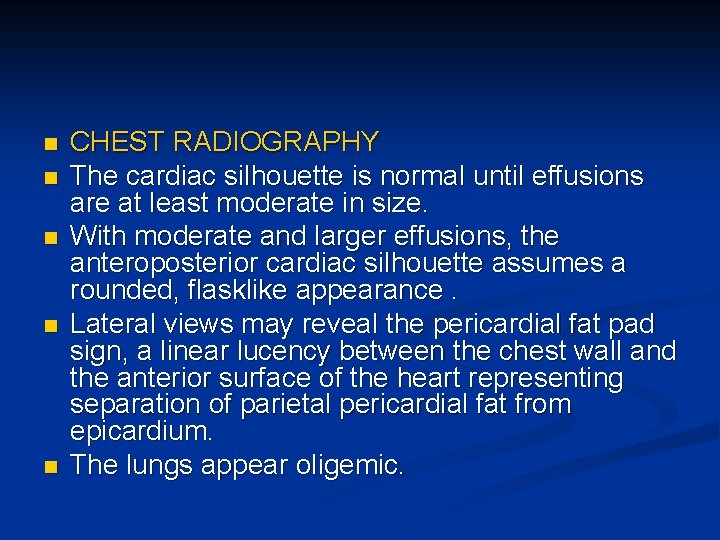
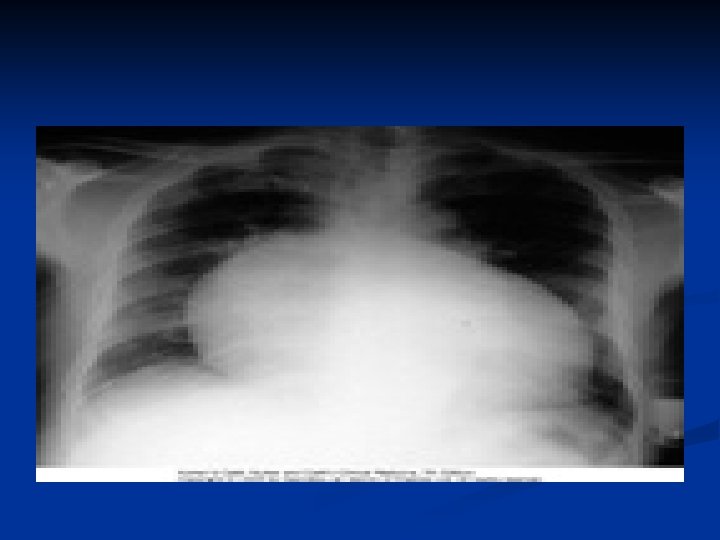
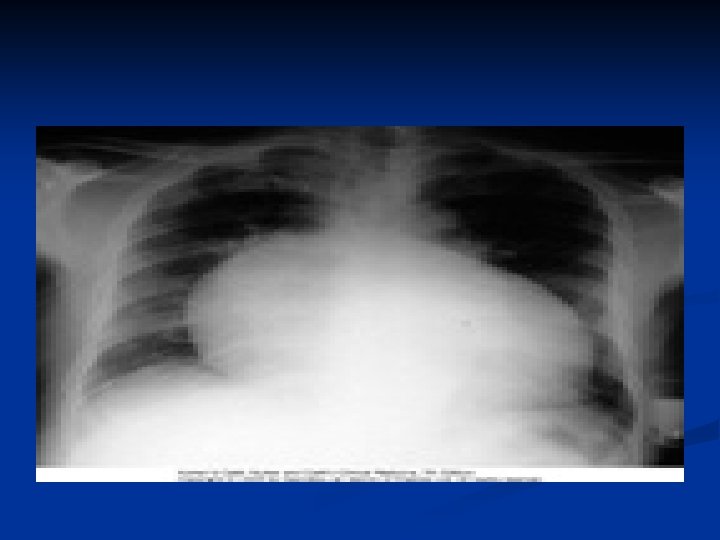
n n n CHEST RADIOGRAPHY The cardiac silhouette is normal until effusions are at least moderate in size. With moderate and larger effusions, the anteroposterior cardiac silhouette assumes a rounded, flasklike appearance. Lateral views may reveal the pericardial fat pad sign, a linear lucency between the chest wall and the anterior surface of the heart representing separation of parietal pericardial fat from epicardium. The lungs appear oligemic.
ECHOCARDIOGRAPHY n SUBCOSTAL VIEW
TREETMENT n Effusions without Actual or Threatened Tamponade cause should be sought and treated if possible. Most pericardial effusions resolve spontaneously.
Effusions with Actual or Threatened Tamponade Hemodynamic monitoring with a pulmonary artery balloon catheter is often useful, especially in those with threatened or mild tamponade in whom a decision is made to defer pericardiocentesis. n For most patients in this category, management should be oriented toward urgent or emergent pericardiocentesis. n
n n Once actual or threatened tamponade is diagnosed, intravenous hydration should be instituted. In a recent report, administration of 500 m. L of normal saline during 10 minutes modestly increased arterial pressure and cardiac output in about 50% of patients with tamponade. Hydration and positive inotropes are temporizing measures and should not be allowed to substitute for or to delay pericardiocentesis.
PROCEDURE n n The most commonly employed approach to closed pericardiocentesis is subxiphoid needle insertion with echocardiographic guidance to minimize the risk of myocardial puncture and to assess completeness of fluid removal. Once the needle has entered the pericardial space, a modest amount of fluid should be immediately removed (perhaps 50 to 150 m. L) in an effort to produce immediate hemodynamic improvement. A guidewire is then inserted, and the needle is replaced with a pigtail catheter
After pericardiocentesis n n repeated echocardiography and in many cases continued hemodynamic monitoring are useful to assess reaccumulation. The duration of monitoring is a matter of judgment, but 24 hours is typically sufficient. A follow-up echocardiogram should be obtained immediately before hemodynamic monitoring is discontinued. We recommend consideration of leaving intrapericardial catheters in place for several days to allow continued fluid removal. This has been shown to minimize recurrencesand facilitates delivery of intrapericardial drugs if indicated.

THANK YOU
 Dr sohail aslam
Dr sohail aslam Neraca lajur perusahaan aslam
Neraca lajur perusahaan aslam Aslam has to study four books
Aslam has to study four books Aslam anis
Aslam anis Vestibule heart
Vestibule heart Fossa ovalis and foramen ovale
Fossa ovalis and foramen ovale Mediastinum contents
Mediastinum contents Pericardial sac
Pericardial sac Anterior mediastinum
Anterior mediastinum What are the 5 heart sounds
What are the 5 heart sounds Pericardial membrane
Pericardial membrane Membrane covering the heart
Membrane covering the heart Atrioventricular orifice
Atrioventricular orifice Pericardial cavity
Pericardial cavity Pericardial sinuses
Pericardial sinuses Kussmal sign
Kussmal sign Hod roles and responsibilities
Hod roles and responsibilities What is tone unit
What is tone unit The attacking firm goes head-to-head with its competitor.
The attacking firm goes head-to-head with its competitor. Pre-head head tonic syllable tail
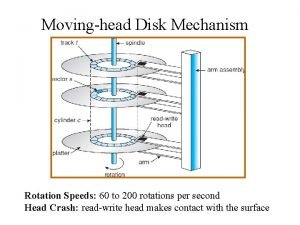
Pre-head head tonic syllable tail The head of moving head disk with 100 tracks
The head of moving head disk with 100 tracks Flooded suction vs suction lift
Flooded suction vs suction lift Moving head disk mechanism in os
Moving head disk mechanism in os Patientsite.com
Patientsite.com 40 to 1 dividing head chart
40 to 1 dividing head chart Body part thigh
Body part thigh Shine skis encapsulated
Shine skis encapsulated Phoenix abscess
Phoenix abscess Lifestyle modern
Lifestyle modern Chapter 8 cardiovascular system
Chapter 8 cardiovascular system Epidemiological triad of malaria
Epidemiological triad of malaria Non communicable diseases
Non communicable diseases What conditions do fungal organisms favor for growth?
What conditions do fungal organisms favor for growth? Immunocompromised diseases list
Immunocompromised diseases list X linked diseases
X linked diseases Chapter 32 childhood communicable diseases bioterrorism
Chapter 32 childhood communicable diseases bioterrorism Chapter 22 genetics and genetically linked diseases
Chapter 22 genetics and genetically linked diseases Venn diagram of communicable and non-communicable diseases
Venn diagram of communicable and non-communicable diseases Human diseases a systemic approach
Human diseases a systemic approach Diseases of the musculoskeletal system
Diseases of the musculoskeletal system Milady chapter 8 skin disorders and diseases
Milady chapter 8 skin disorders and diseases Protein deficiency diseases
Protein deficiency diseases Certain infectious and parasitic diseases
Certain infectious and parasitic diseases