Open Wounds Understanding SelfInjury nonsuicidal selfinjury NSSI Stefanie





- Slides: 51
Open Wounds Understanding Self-Injury: nonsuicidal self-injury (NSSI) Stefanie Shoults RN MSNclinical perspective Kathie Rodriguez LPN MSfamily perspective
nonsuicidal self-injury (NSSI) Self Injury 1. Who self injures? 2. Why do they do it? 3. What it is and is not. 4. How can we help?
Nonsuicidal Self-Injury (NSSI) is the intentional harm of one’s own body without conscious suicidal intent and for purposes not socially sanctioned. (Aldeman, 1998, Favazza, 1998, van der Kolk, et al. , 1991) Treating Self-Injury: A Practical Guide (International Society for the Study of Self-Injury, 2007).
Alternate terms for NSSI that have been used in both literature and clinical settings are: §Deliberate self-harm § Cutting § Self wounding § Self-Mutilation § Focal suicide § Parasuicide
nonsuicidal self-injury (NSSI) • Although considered to be a recently growing problem in the mental health community, nonsuicidal self-injury (NSSI) has been of clinical interest since the 1930’s. American psychiatrist, Karl Menninger, was one of the first researchers to identify self-injury as a distinct clinical behavior (Conterio & Lader, 1998). Labeling it focal suicide, Menninger (1938) identified individuals who engaged in “localized self-destruction” of body tissue in order to keep negative affective states at a manageable level and prevent painful memories from surfacing. He recognized that self-injurious behaviors exist on a spectrum from normal nail biting to severe flesh digging.
NSSI Behaviors • Cutting • Scratching • Abrading • Burning • Some forms of hair pulling • Biting • Inserting foreign objects into the body • Interference with wound healing • Ingesting toxins
What are we talking about? • Self-injury is an attempt to cope with a problem and not the problem itself. It is often a cry for help (either conscious or unconscious). • Self-injurers may experience themselves as being invisible. Ignoring the behavior only validates this belief, possibly causing them to become even more dangerous to themselves. • The key is to focus on the underlying feelings and issues rather than focusing on the behavior itself.
Typical locations for inflicting NSSI § Hands, arms, legs, and other areas in the front of the body, presumably because these are the easiest areas to self-inflict injury, as well as the easiest areas to conceal visible injuries. § NSSI on body parts other than the forearms is thought to be indicative of more severe psychopathology.
The goal is to respond in a calm, nonjudgmental fashion. • School professionals such as teachers, nurses and counselors are frequently the first adults to know of a student's selfinjurious behavior. • They may notice wounds, or may be notified by another student. • On occasion, a student will decide to disclose to a teacher whom they trust. • When a staff member notices that a student has wounds, suspects that a student is injuring or has the behavior brought to their attention by another student, the situation must be addressed and not ignored. • One of the most important things to remember is that the tone of your response can be equally, or even more important than your actual words.
Don't be afraid • State, "I've noticed injuries that appear to be selfinflicted, I care about why you might be doing that" or "it appears you have hurt yourself, do you want to talk about it? ". • Even if the student denies that the wounds are selfinflicted, the fact that the behavior was attended to and addressed directly is the first step towards healing. • You have made it clear that they are not invisible and that you are available when the student is ready to seek help.
If you believe that a student is self-injuring • Let them know that you want to aid them in getting the help they need. • It is most important to be empathic with the student. • Remember, the self-abuser may be feeling shame and you do not want to further this shame. • Please DO NOT reprimand or send the student to the principal as a behavioral problem. • Instead, your concerns should be brought to the attention of the mental health counselor if one is available to you. • If your school does not have access to a mental health counselor, then another school professional (depending on your school's protocol) will need to assess the student for safety, especially if suicidal thoughts accompany the self-injurious behavior.
Follow your school's protocol • You will also need to follow your school's protocol with regards to letting the parents of the student know what is happening with their child. • It may be best to encourage the student to tell their parent(s) or guardian about their self injury. • Giving the student the option to do so, prior to you telling a parent/guardian, allows the student to have a greater measure of control over the situation. • If the student fails to tell their parent, then it would be up to the individual to follow the protocol set forth by the school.
Focus on the events and feelings • If the student has fresh wounds, they will need to be assessed by the school nurse and/or emergency room to determine severity and to make sure that the wound is properly treated. • Our practice is to not focus on the injury, but rather on the events, feelings and thoughts preceding and following injuring.
Severity and duration of practice • If the student has been injuring a long time, or is injuring severely, it may be time to consider some intensive treatment. • Family therapy is considered an integral part in the healing process for the self-injuring child. • If self injury is having a negative impact on the student's life and therapy does not seem to be working, there is more intensive help available. • There are residential treatment programs specifically for the intensive treatment of the many forms of self injury. (depends on where you are located and proximity to facility. )
Warning signs • Unexplained frequent cuts or burns • Wearing long sleeves or pants in warm weather • Avoiding swimming pools or changing clothing for PE. • Wearing thick bracelets to cover wrists • Having sharp objects in purse or back pack. • Difficulty expressing feelings • Withdrawal from close relationships
Interventions - handout • Intervention Tips: Unstable, unpredictable or invalidating environments contribute to adolescent anxiety and frustration, which, in turn, can contribute to an increase in self-injurious impulses and injury. Therefore, stability and empathy are among the most important ingredients for success in working with self-injurers. Everyone in the system is responsible for providing a caring environment. Some descriptors of a caring environment are: • Neutral (i. e. , non-judgmental and non-punitive). • Accepting. Staff can validate self-injurers' emotions. (A common theme among self-injurers is that their emotions were not validated during early family life). • Amenable to staff contact. Since we want to encourage students to talk to staff about self-injurious impulses, staff can demonstrate openness to listening to them. • Calm. Staff serves as models for emotional control, conflict-resolution and problemsolving skills. • Dependable, structured and predictable (schedules, individual sessions, group time, consequences and/or expectations). • Consistent (staff remains neutral: rules, rewards and consequences are the same each day). Further, staff members display a consistent "personality" each day. • Confidential and private. Staff refrains from discussing students when others are around and refrains from discussing sensitive issues with students (i. e. , diagnosis, family conflict, etc. ) in public (i. e. , hallways, classrooms). • For more specific direction on how to intervene with students who injure and helping them disclose to parent(s)/guardian(s), please see "Self-Injury: A Manual for School Professionals".
Is it related to Borderline • NSSI was once thought to occur exclusively in females with Borderline Personality Disorder (Muehlenkamp, 2005). Current research supports that NSSI is no longer synonymous with a diagnosis of Borderline Personality Disorder, and is also quite frequently performed by males. A substantial amount of research actually supports equivalent ratios of NSSI among males and females.
Statistics • Males and females • All races and socio-economic levels • Ages 15 -50’s • Not easily identifiable • Roughly 2% (1 -4%) of the population. In some studies reported as high as 8 million Americans self-mutilate. • 30 times the rate of suicide attempts • 140 times the rate of completed suicides • May also suffer from eating disorders • 90% who cut began as teenagers
Characteristics • are often depressed, feel powerless or anxious • have difficulty expressing their emotions verbally • experience difficulty with relationships • aim for perfection • often have negative body image • lack impulse control/suppressed anger • do not have a repertoire of coping skills • may have serotonin dysfunction • possible trauma
Adolescents report two main reasons for NSSI: social and emotional • Self-injurers report engaging in NSSI to relieve unpleasant emotions, including anxiety, guilt, anger, loneliness, and self-hatred • The most commonly reported reason for NSSI (41%) was to feel anything at all, even pain. • At or above 33% were “to stop bad feelings, ” “to get control of the situation, ” “to give yourself something to do when alone, ” and “to relieve feeling numb or empty, ”
Abuse • No evidence that all NSSI is precipitated by childhood physical or sexual abuse. Everyone who self injures has a pain narrative, not necessarily an abuse narrative. It may be about half. • While research has not conclusively shown a cause and effect relationship between NSSI and traumatic events, Many who self-injure did not suffer childhood abuse 50 -60% suffered childhood abuse or trauma while 40 -50% did not.
Under the influence • One in five episodes of NSSI are thought to occur while under the influence of alcohol, and one in eight while under the influence of illegal drugs (Madge et al. , 2008). • Children and adolescents who use drugs and alcohol are nearly three times more likely to engage in NSSI than their clean and sober peers.
Four types parenting styles felt to contribute to self-injury: enmeshed, disengaged, chaotic, and rigid. 1. Enmeshed families tend to have extreme forms of in family interactions that result in poorly differentiated boundaries. 2. Disengaged families show characteristics that include strict boundaries where affection and information do not flow easily among family members. 3. Chaotic families are characterized by a lack of structure, rules, and leadership with little order. 4. Rigid family characteristics include resistance to change whereby individual family members who attempt change are often sabotaged to maintain the status quo.
Surprising • A 2014 study found that enmeshed family dysfunction seemed to have little correlation with self-injurious behaviors. This is surprising because previously it as felt this parenting style one of the most predominant causes of NSSI behaviors. • The same study found that rigid family characteristics with a strong resistance to change have a higher self-injury incidence than other parenting styles. • The more chaotic and frequent family conflicts arise feed into both severity and frequency of NSSI. • Disengaged families offer little validation of the child’s feelings or situation let alone assistance in healthier coping mechanisms. NSSI is a way of making these hidden things, visible. • More than parenting styles, research has found that family communication and family satisfaction influence selfdestructive behaviors including NSSI. (Halstead, Pavleov, Hecker and Seliner, 2014)
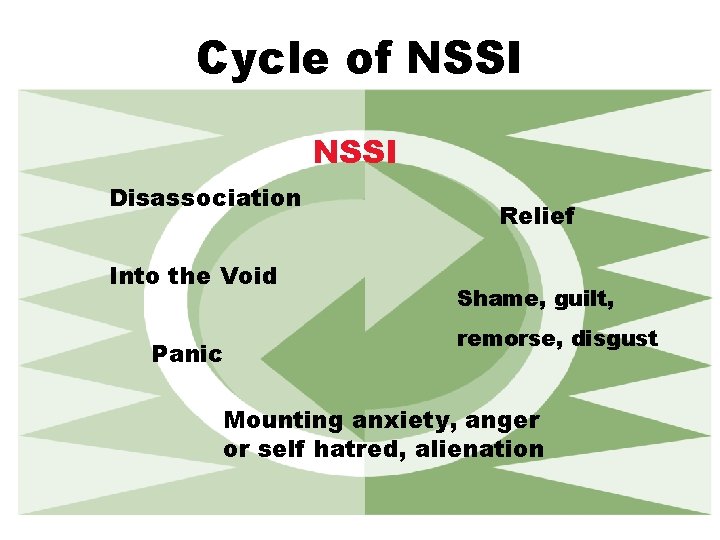
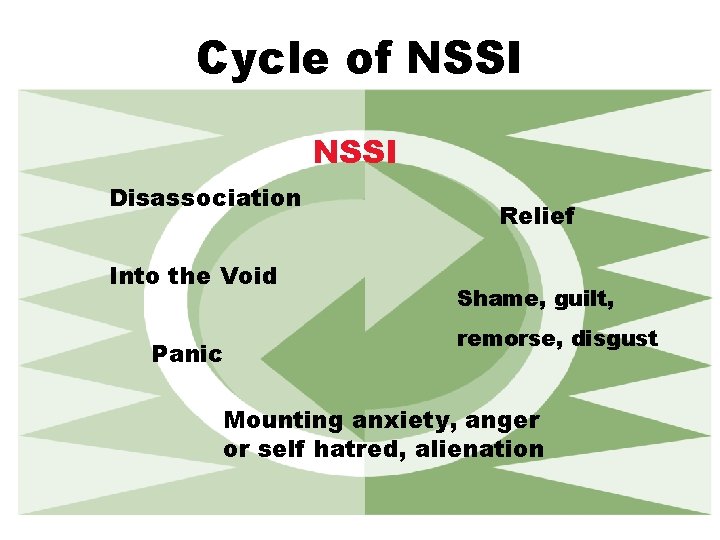
Cycle of NSSI Disassociation Into the Void Panic Relief Shame, guilt, remorse, disgust Mounting anxiety, anger or self hatred, alienation
Interrupting the Cycle • Dispute irrational thoughts, feelings • Triggering event • Unbearable tension, anxiety • Dissociation • Self injury • Relapse

What about the DSM? q Currently listed as a symptom associated with a number of mental health disorders q Nonsuicidal self-injury (NSSI) is included as conditions for further study in the DSM-5. Therefore, it is necessary to investigate the proposed diagnostic criteria and the diagnostic and clinical correlates for the validity of a diagnostic entity. q NSSI is not in the classification system of the International Classification of Diseases, tenth revision (ICD-10)
SI is often associated with: • Borderline Personality Disorder • Obsessive-Compulsive Disorder • Post-Traumatic Stress Disorder • Dissociative Identity Disorder • Eating Disorders • Substance Abuse • Depression
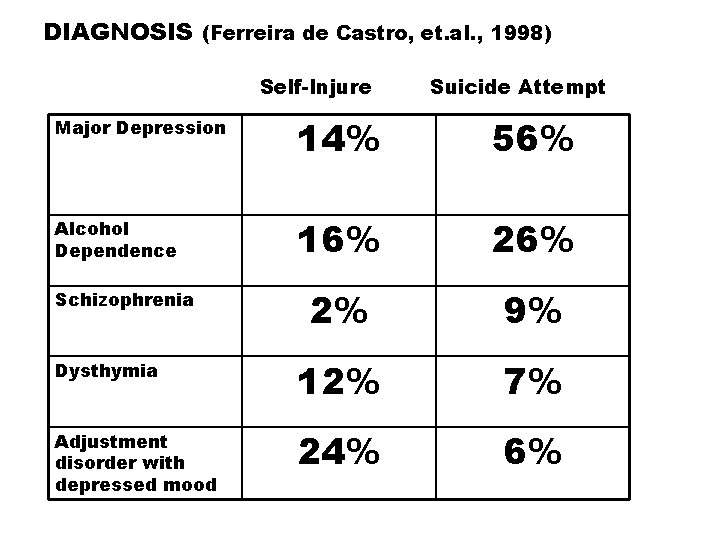
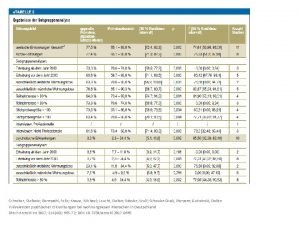
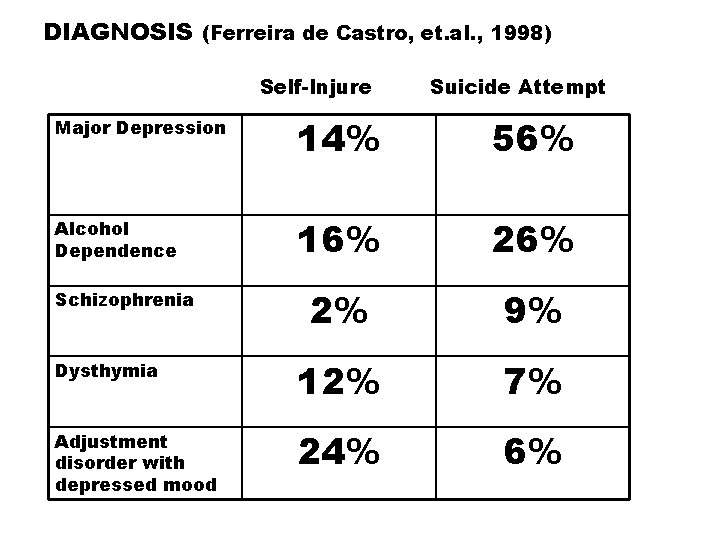
DIAGNOSIS (Ferreira de Castro, et. al. , 1998) Self-Injure Suicide Attempt Major Depression 14% 56% Alcohol Dependence 16% 2% 9% Dysthymia 12% 7% Adjustment disorder with depressed mood 24% 6% Schizophrenia
In their own words. . . • I was hurting myself for 2 years before I ever told anyone. I didn't even know that it was called self-harm. I was scratching and burning myself, then I moved on to NSSI. I was so upset all of the time and the frustrating thing was I didn't even know why.
In their own words. . . “It’s like opening up a safety valve or letting steam out of a covered pot. ” “Sometimes I cut just to make myself feel something because I am just totally numb. ” (In Strong, 1998, p. 7)
“I needed to cut the way your lungs scream for air when you swim the length of the pool underwater in one breath. It was a craving so organic it seemed to have risen from my skin itself. ” Caroline Kettlewell Skin Game
Insight. . . "How will you know I am hurting, if you cannot see my pain? To wear it on my body tells what words cannot explain. " ~C. Blount "The lines I wear around my wrist are there to prove that I exist. " ~Anonymous "I can feel the hurt. There's something good about it. Mostly it makes me stop remembering. " ~Albert Borris, Crash Into Me “Better to inflict pain on myself than to let other people do it. ” –Tracy Thompson, The Beast: A Reckoning with Depression “I wrote you a poem on my wrists. I used a razor as a pen and I signed my name in blood. But you wouldn’t read it. ” –written by Molly Ringwald’s character in Surviving
“I felt like I was isolated from the world, dead, with no emotions at all. The blood told me I was alive, that I could feel…Also I couldn’t cry, and bleeding was a different form of crying. ” (Lindsay in Strong, p. 57)
“This is yet another secret I must hold to myself because my therapist has given me an ultimatum, either no more hurting myself or we will have to discontinue our therapy. So a little distance comes between us now, a secret that hold great importance which we could both learn from, if I was able to tell her…JML
Helping: What to Do • Learn about self-injury. • Talk about SI. Ask about it. • Be supportive. Show you care. • Acknowledge the effort to cope with very difficult emotions • Set limits • Be available, but refer when appropriate • Don’t discourage self-injury • Recognize the severity of the distress

Therapeutic Goals • Encourage communication about self-injury and relevant aspects of the child’s life. • Improve the quality of child’s life as it relates to self-injury. • Explore themes of guilt and shame. • Diminish use of self-injury as the coping skill when client desires to make changes. (Conners, Rubin, et, al, 2002). • Improve communication of child and family Correlation between family communication and frequency of self-injury ---family communication has an impact on the development, maintenance, and cessation of self-injury. (Selekman 2002)

Expressive Arts • Journals • Poetry • Music • Art
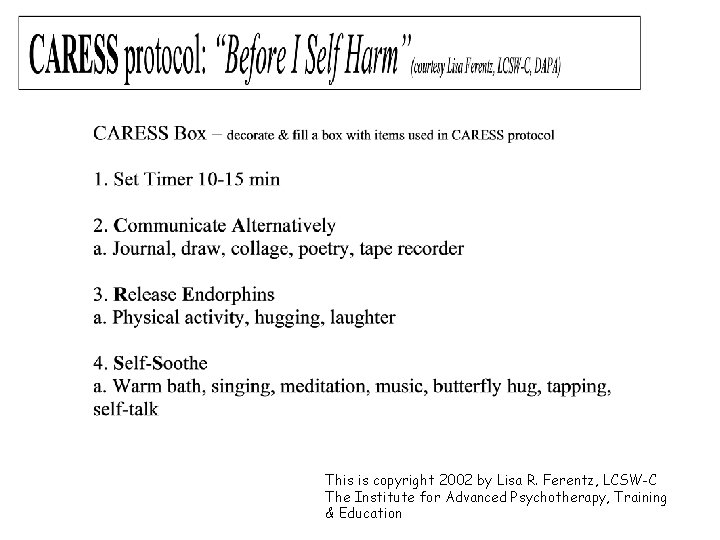
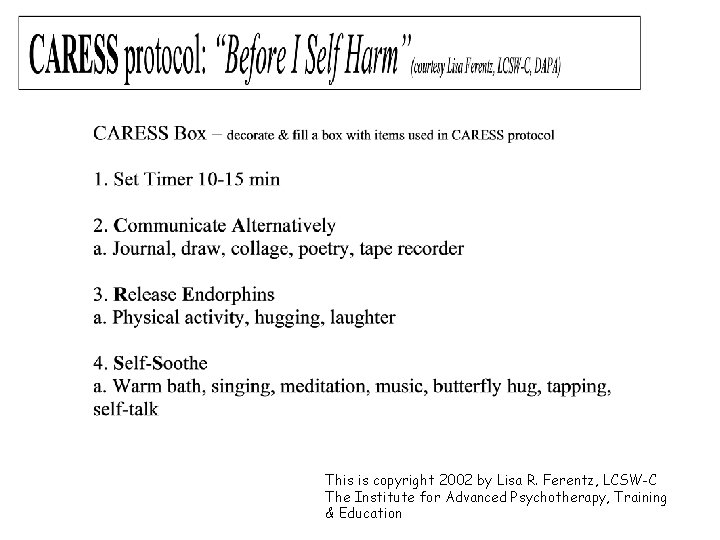
This is copyright 2002 by Lisa R. Ferentz, LCSW-C The Institute for Advanced Psychotherapy, Training & Education

Taking Care of Yourself • Monitor your own horror and confusion • Broaden your perspective past the behavior to the intent behind it • Seek consultation • Get support for yourself
Care and Concern • The capacity to derive comfort from another is the single biggest predictor of whether traumatized patients are able to give up their self-destructive habits. Bessel van der Kolk
Care and Concern • The development of a safe and trusting relationship is vital for the child to learn to sooth and care for him or herself in a healthy manner by internalizing their therapist’s care and concern. (Strong, 1988)
Care and Concern “_____ was the first to acknowledge that maybe I was in pain, as opposed to ‘doing it for attention’. This affirmation of my inner pain was a healing force. “

In Summary – • Synopsis to use with your own team when you return home
What Self Injury is NOT • It is not a suicide attempt (attempting to feel better, not escape all feelings) • It is not usually attention seeking • It is not a danger signal to others
NOT SUICIDAL BEHAVIOR • “…self-mutilation is distinct from suicide…A basic understanding is that a person who truly attempts suicide seeks to end all feelings where as a person who selfmutilates seeks to feel better. ” (Favazza, 1998) • Intention-does not intend to die as a result of his/her acts. Intends to live.
Why do they harm themselves? • To release intense feelings • The physical pain may be easier to deal with than the emotional pain • To feel real, alive • To exert some control • Acting out self punishment
What Not to Do • Be afraid to ask the question, “Do you selfinjure? ” • Make eliminating the behavior the primary goal • Make a safety contract or use contracts as a reward or punishment • Visibly monitor their injuries • Make him or her feel ashamed or guilty about the behavior
QUESTIONS?
References: • Alderman, T. (1997). The scarred soul: Understanding & ending self-inflicted violence. Oakland, CA: New Harbinger. • Aldeman, 1998, Favazza, 1998, van der Kolk, et al. , 1991) Treating Self-Injury: A Practical Guide • Boesky, Lisa; 1 edition (July 18, 2007) When to Worry: How to Tell If Your Teen Needs Help & And What to Do About It • Conterio, K. , & Lader, W. (1998). Bodily harm. New York: Hyperion. • Fishman, C. H. (1993). Intensive structural therapy: Treating families in their social context. New York: Basic Books • Ferentz, Lisa R. LCSW-C The Institute for Advanced Psychotherapy, Training & Education. 2002 • Halstead, R. O. , Pavelov, T. W. , Hecker, L. L. , Seliner, M. M. (04/2014). Family dynamics and self-injury behaviors: A correlation. Journal of Marital and Family Therapy, 246 -59. • Jella, S. H. (2007). The family environments of self-injuring female adolescents. (Dissertation, Alliant International University). Received as an email attachment from S. Jella, February, 2009. • Kettlewell, Caroline; Skin Game: A Memoir. St. Martin's Press; 1 st edition (June 4, 2013). • Levenkron, S. (1998). NSSI: Understanding and overcoming self-mutilation. New York: W. W. Norton & Norton. • Levitt, J. L. , Sansone, R. A. , & Cohn, L. (Eds. ) (2004). Self-harm behavior and eating disorders. New York: Bruner- Rutledge. • Selekman, M. D. (2002). Living on the Razor's Edge. New York: W. W. Norton & Company • Strong, Marilee. A Bright Red Scream: Self-Mutilation and the Language of Pain. (October 1, 1999) Penguin Books • Walsh, B. (2006). Treating self-injury: A practical guide. New York: Guildford Press. • Wedig, M. M. , & Nock, M. K. (2007). Parental expressed emotion and adolescent self-injury. Journal of Academy of Child and Adolescent Psychiatry, 46, 1171 -1178.
 The sad persons scale
The sad persons scale Open innovation open science open to the world
Open innovation open science open to the world Define wound healing
Define wound healing Cavitation bullet wounds
Cavitation bullet wounds Jackson's theory of thermal burns
Jackson's theory of thermal burns Innate wisdom vs. educated stupidity
Innate wisdom vs. educated stupidity Kinds of wounds with pictures
Kinds of wounds with pictures Dcapbtls
Dcapbtls Jackson's theory of thermal wounds
Jackson's theory of thermal wounds Unit 15:3 providing first aid for bleeding and wounds
Unit 15:3 providing first aid for bleeding and wounds Staple gun for wounds
Staple gun for wounds Unit 15:8 providing first aid for cold exposure
Unit 15:8 providing first aid for cold exposure 17:7 providing first aid for heat exposure
17:7 providing first aid for heat exposure Veterolegal
Veterolegal The 5 wounds
The 5 wounds Wound description with pictures
Wound description with pictures Concealed puncture wounds
Concealed puncture wounds Spi erzieherausbildung
Spi erzieherausbildung Interlingual translation examples
Interlingual translation examples Stefanie bollinger
Stefanie bollinger Ciekawostki o kardynale stefanie wyszyńskim
Ciekawostki o kardynale stefanie wyszyńskim Stefanie grunow
Stefanie grunow Stefanie heyne
Stefanie heyne Stefanie panke
Stefanie panke Stefanie keller
Stefanie keller Michael leucht
Michael leucht Dr stefanie lord
Dr stefanie lord Stephanie fishel
Stephanie fishel Stefanie gehrke
Stefanie gehrke Stephanie tompkins
Stephanie tompkins Stefanie asendorf
Stefanie asendorf Ssswm
Ssswm Stefanie kosik
Stefanie kosik Stefanie ritz-timme
Stefanie ritz-timme Stefanie scherzinger
Stefanie scherzinger Poems for two voices
Poems for two voices Stefanie reith
Stefanie reith Stefanie hoffer
Stefanie hoffer Open hearts open hands
Open hearts open hands Plc timer symbol
Plc timer symbol Air permits 101
Air permits 101 Basic guidelines for value education
Basic guidelines for value education Business essentials 12th edition free
Business essentials 12th edition free Sqa art expressive evaluation template
Sqa art expressive evaluation template Understanding stem anatomy
Understanding stem anatomy Understanding canadian law (clu3m)
Understanding canadian law (clu3m) Teams typically outperform individuals
Teams typically outperform individuals Sqa higher english understanding standards
Sqa higher english understanding standards The great understanding
The great understanding The understanding group
The understanding group Understanding points lines and planes answer key
Understanding points lines and planes answer key Deepening understanding year 5
Deepening understanding year 5