Wounds ulcers fistulae cysts 1 wounds 2 v





- Slides: 42
Wounds, ulcers, fistulae & cysts 1
wounds 2

v Mechanism of injury § Traumatic wounds ü Sharp, penetrating Blunt Bullet § Surgical wounds ü ü 3
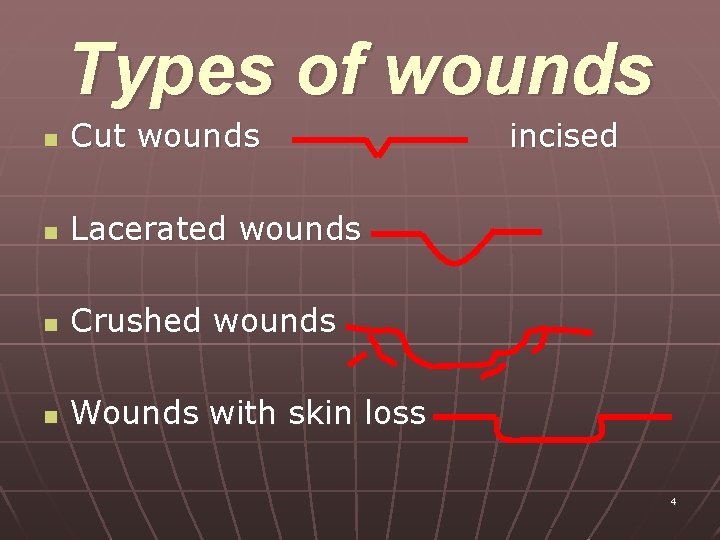
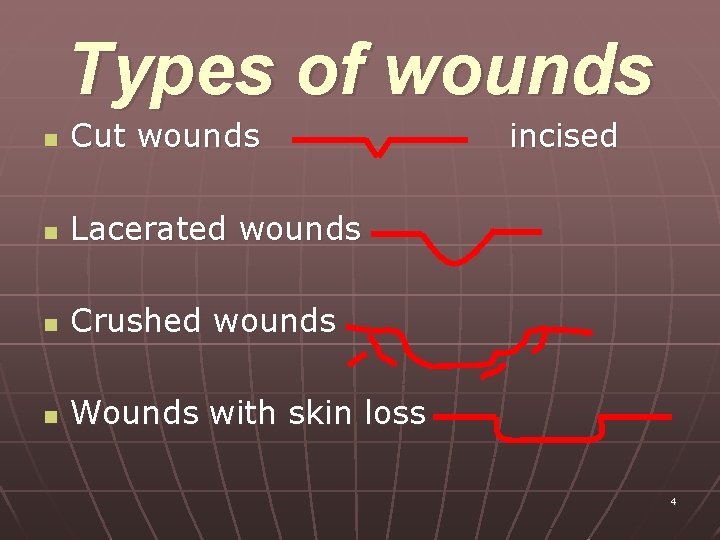
Types of wounds n Cut wounds n Lacerated wounds n Crushed wounds n Wounds with skin loss incised 4
Types of Suturing n n n Primary suturing Excision and primary suturing Delayed primary suturing Secondary suturing Skin grafting 5
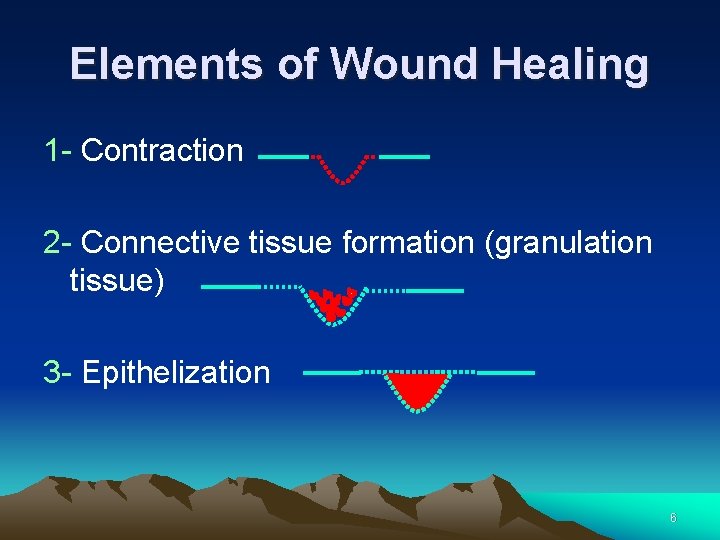
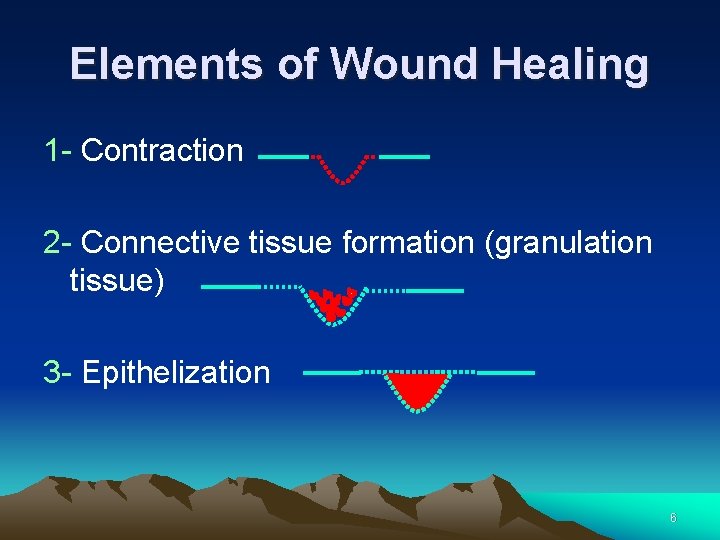
Elements of Wound Healing 1 - Contraction 2 - Connective tissue formation (granulation tissue) 3 - Epithelization 6
Surgical Wounds Clean contaminated Contaminated Dirty 7
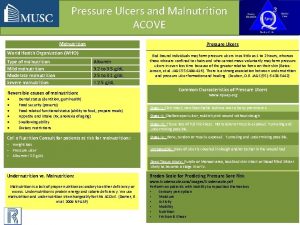
Factors which affect wound healing n General: Malnutrition, ureamia, n Local Factors: malignancy, radiothempy, cytotoxic drugs, duabetes, vitc deficiency. - Blood supply - Tension in wound - presence of necrotic tissue and F. B - presence of haematoma - excessive cauterization, rough manipulation - infection 8
ØComplications of Wounds: G Wound infection A Wound dehiscence BHyper trophied scar, keloid 9
Principles of wound management Correct all local and systemic factors that might impair wound healing Wound toilet Wound dressing Antibiotics if infected 10
Ulcers 11
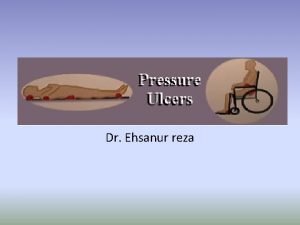
n 1. 2. 3. 4. Ulcers are non-healing wounds that develop on the skin, mucous membranes or eye. Although they have many causes, they are marked by: Loss of integrity of the area Secondary infection of the site by bacteria, fungus or virus Generalized weakness of the patient Delayed healing 12
Location 1. 2. 3. Lower limbs: most ulcers of the foot and leg are caused by underlying vascular insufficiency. The skin breaks down or fails to heal because of repeated insult or trauma. Sacrum and ischium Mouth ulcer 13
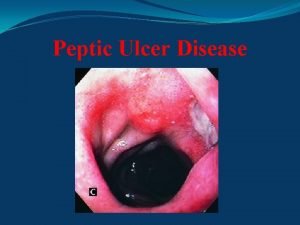
Cont… 4. 5. 6. Peptic ulcer: This includes ulcers of the esophagus, stomach, large and small intestine Genitalia: May be penile, vulvar or labial. Most often are due to sexuallytransmitted disease. Eyes: corneal ulcers are the most common type. Conjunctival ulcers also occur. 14
causes n n n n Bacterial , viral & fungal infection Cancer both primary & secondary Venous stasis Arterial insufficiency Diabetes Rheumatoid arthritis Loss of mobility 15
Description n n n n Site Size Shape Base Edge Tenderness Discharge Surrounding tissue & lymphatics 16
Types n n n Peptic ulcer Mouth ulcer Pressure ulcer (decubitus) Arterial insufficiency ulcer Venous insufficiency ulcer Diabetic foot ulcer 17
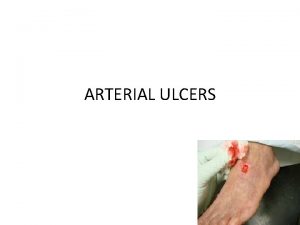
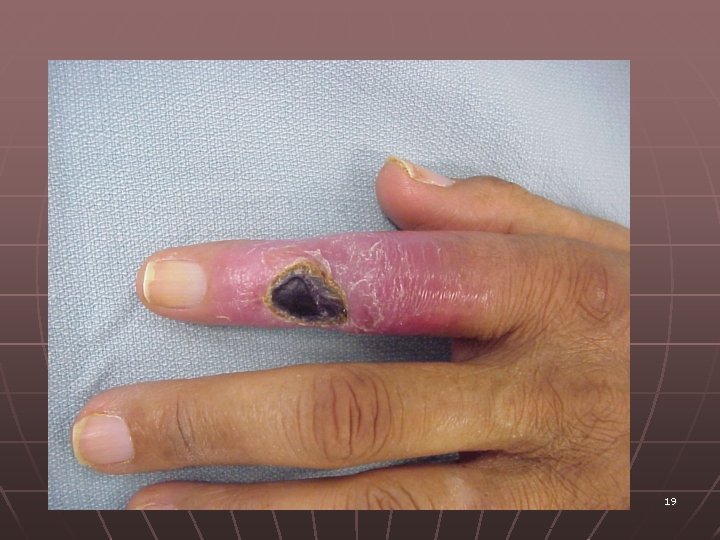
Ischaemic ulceration n n n By definition caused by inadequate blood supply “large small artery obliteration” In elderly , who also have symptoms of coronary vascular disease. Men predominate Risk factor – Smoking, atherosclerosis Very painful, causes rest pain Do not bleed but discharge thin serous exudates which can become purulent Distal pulses are impalpable 18
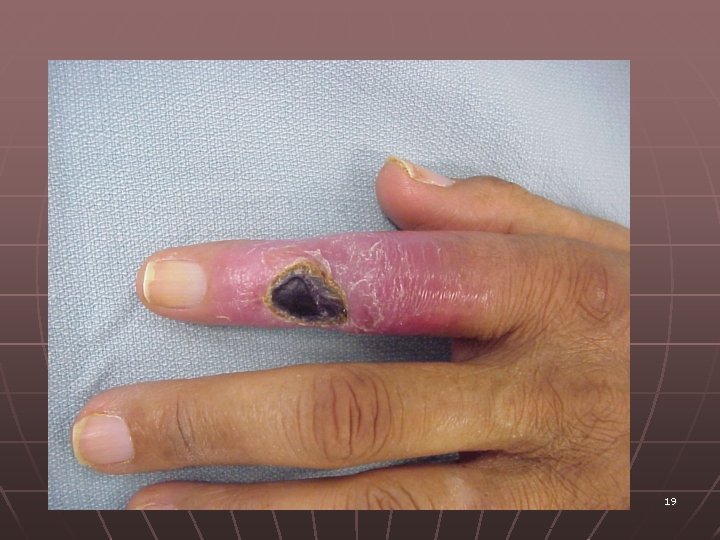
19

20
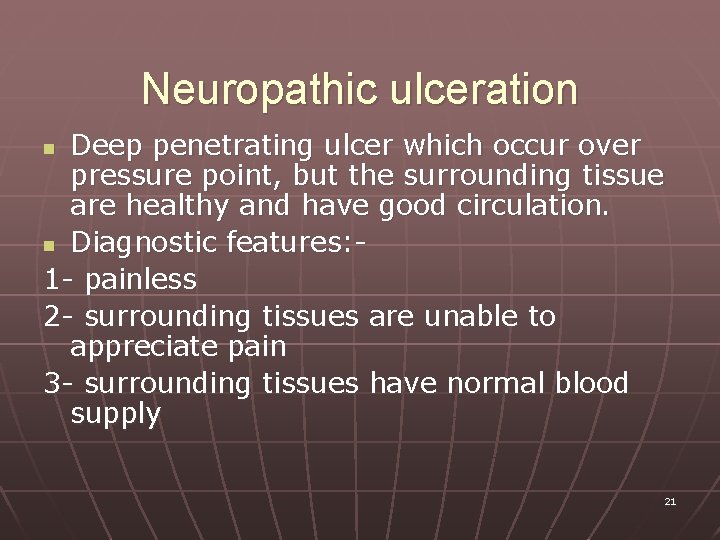
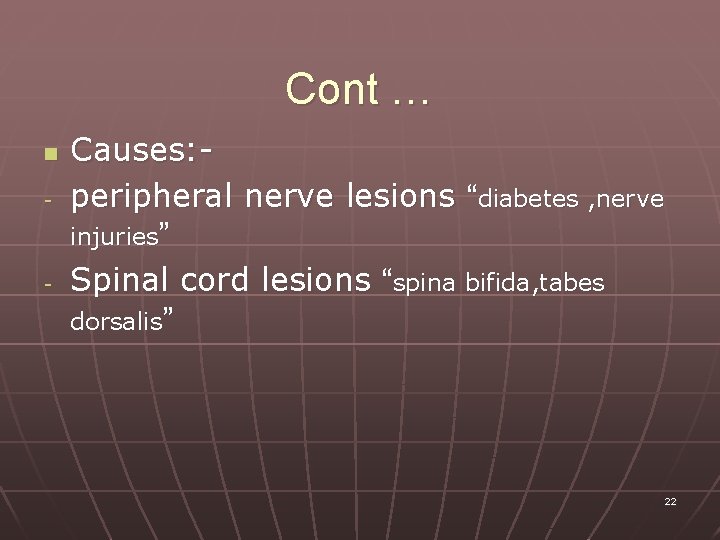
Neuropathic ulceration Deep penetrating ulcer which occur over pressure point, but the surrounding tissue are healthy and have good circulation. n Diagnostic features: 1 - painless 2 - surrounding tissues are unable to appreciate pain 3 - surrounding tissues have normal blood supply n 21
Cont … n - - Causes: peripheral nerve lesions “diabetes , nerve injuries” Spinal cord lesions “spina bifida, tabes dorsalis” 22

23
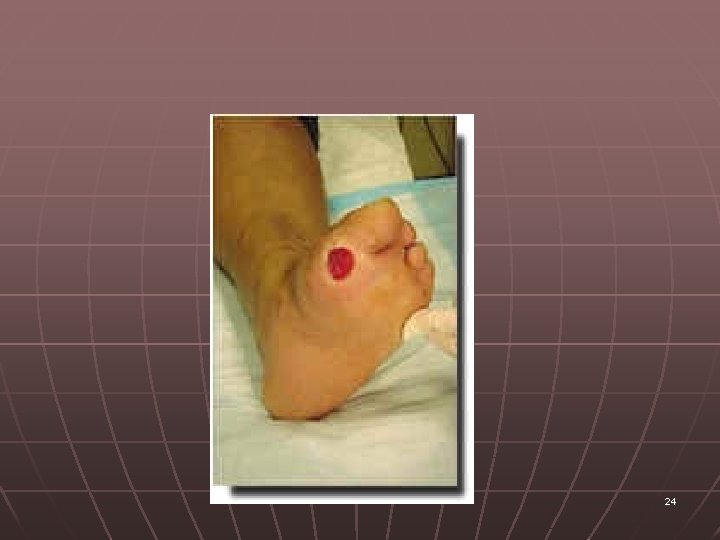
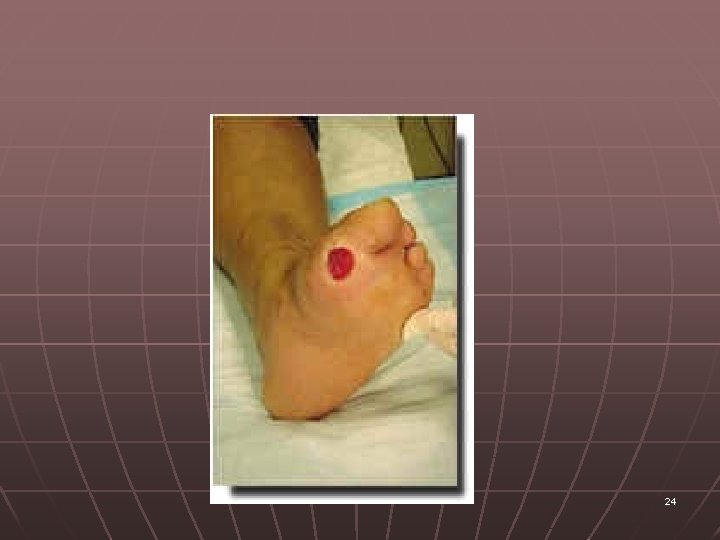
24
Venous ulceration n n Follow many year of venous disease. Commonly occur on the medial side of the leg above the ankle Predominantly in women Risk factor – Varicose veins Pulses are normal 25

26

27
Fistulas 28
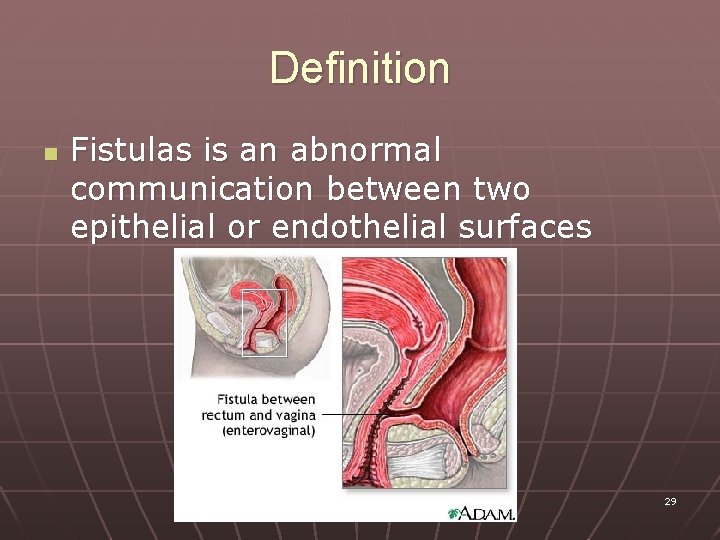
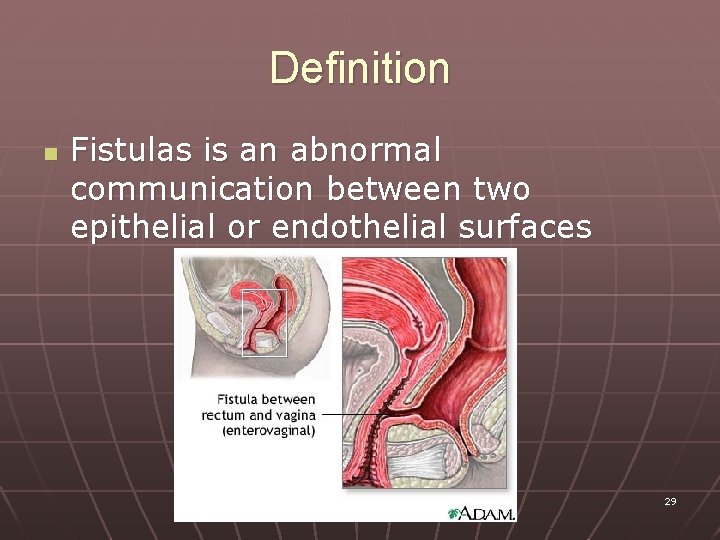
Definition n Fistulas is an abnormal communication between two epithelial or endothelial surfaces 29
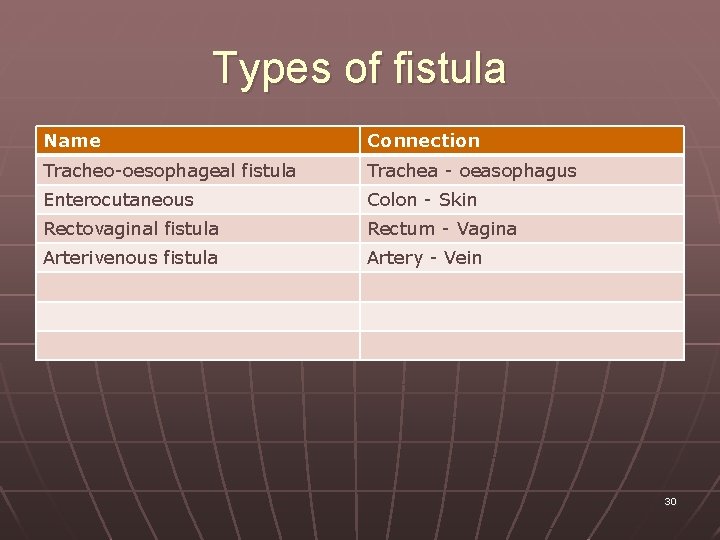
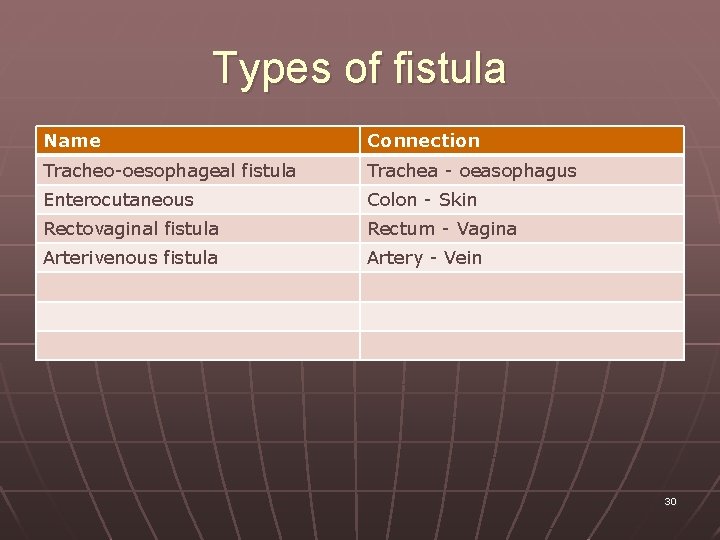
Types of fistula Name Connection Tracheo-oesophageal fistula Trachea - oeasophagus Enterocutaneous Colon - Skin Rectovaginal fistula Rectum - Vagina Arterivenous fistula Artery - Vein 30
Why do they occur? n n Some are congenital e. g. Tracheooesophageal fistula Internal abdominal fistulas : Majority result from an underlying gastrointestinal disease ( e. g. colonic diverticular disease, crohn’s disease, colonic carcinoma, etc ) 31
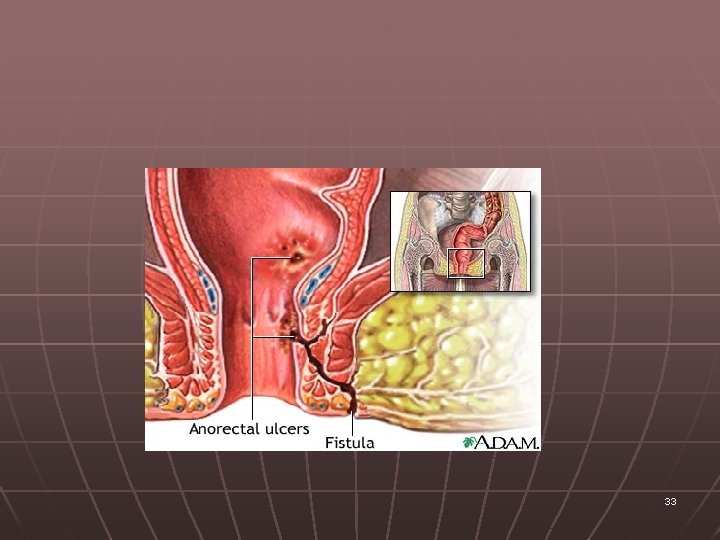
n n External abdominal fistulas arise as a complication of surgery or to the trauma. Other external fistulas are due to primary abscess formation and rupture on to skin. E. g. perianal fistula 32
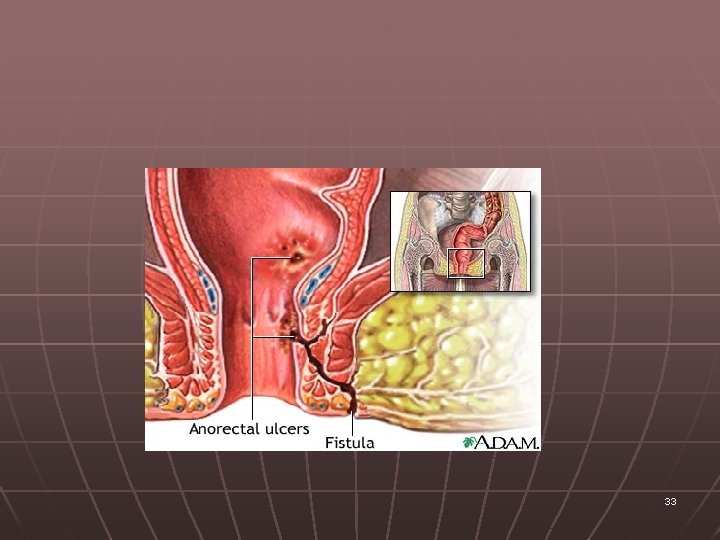
33
Management Difficult to treat Is complex and usually surgical Depend on the site of the fistula 34
Treatment n Conservative : The mainstays of medical management are: - nutritional support - meticulous collection of fistulous discharge - skin-stoma care - control of sepsis 35
n Surgical : The absolute indications for operative intervention are : - intestinal distal obstruction - peritonitis - abscess formation - bowel discontinuity - presence of malignant disease - persistent inflammatory bowel disease 36
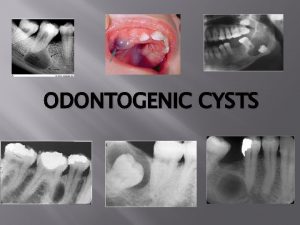
Cysts 37
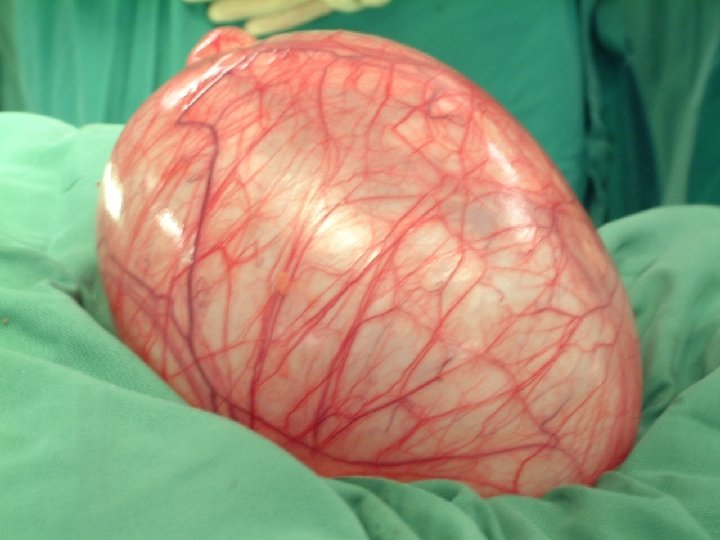
What is a cyst? a cyst is : any closed epithelium-lined cavity or sac, normal or abnormal, usually containing liquid or semisolid material" (Dorland's, 1995, pp. 209). n It is common can occur anywhere any age. n Cysts vary in size n Its wall called the cyst capsule 38
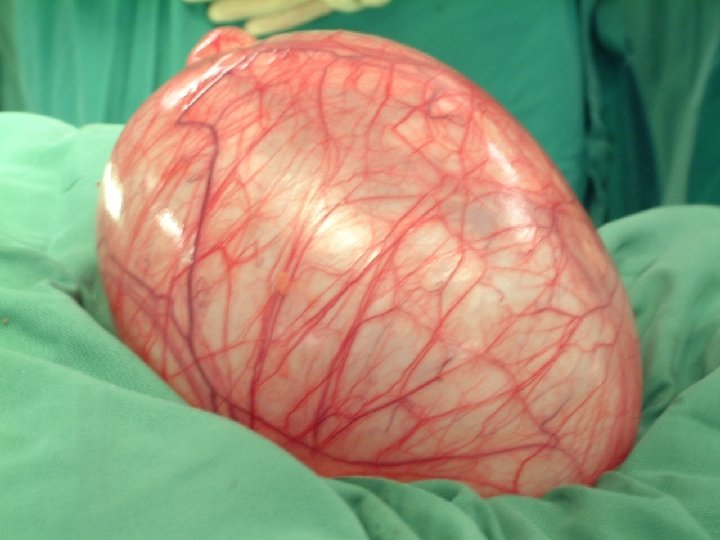
39
What are the causes of a cyst? n 1. 2. 3. 4. 5. Cysts are usually formed through one of these mechanisms: Obstructions to the flow of fluid Infections and chronic inflammations Tumors Genetic (inherited) conditions Defects in developing organs in the embryo 40
Examples of cysts n n n Thyroglossal cyst Ovarian cyst Sebaceous cyst 41
Treatment Usually surgical - Cystectomy 42
 Sru consensus ovarian cysts
Sru consensus ovarian cysts True cysts
True cysts What is a choroidal fissure cyst
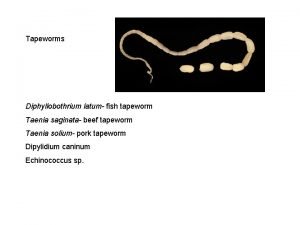
What is a choroidal fissure cyst Diphyllobothrium latum
Diphyllobothrium latum Ova cysts and parasites
Ova cysts and parasites Acute gastritis
Acute gastritis Gastric ulcer definition
Gastric ulcer definition Talipes equinovarus in varicose veins
Talipes equinovarus in varicose veins Intestine
Intestine What causes ulcers
What causes ulcers Gastric ulcer vs duodenal ulcer
Gastric ulcer vs duodenal ulcer Ulcer edge
Ulcer edge Continuous bedside pressure mapping
Continuous bedside pressure mapping Anorexia and stomach ulcers
Anorexia and stomach ulcers Staple gun for wounds
Staple gun for wounds Unit 15:1 providing first aid
Unit 15:1 providing first aid Dcap btls
Dcap btls Veterolegal wounds
Veterolegal wounds The 5 wounds
The 5 wounds Wound description with pictures
Wound description with pictures Rank and wakefield classification of wounds
Rank and wakefield classification of wounds Chapter 17.11 providing first aid for sudden illness
Chapter 17.11 providing first aid for sudden illness Concealed puncture wound
Concealed puncture wound Cavitation bullet wounds
Cavitation bullet wounds Jackson's theory of thermal wounds
Jackson's theory of thermal wounds Hunting group of companions archetype
Hunting group of companions archetype Kinds of wounds with pictures
Kinds of wounds with pictures Jackson's theory of thermal wounds
Jackson's theory of thermal wounds Chapter 16:3 providing first aid for bleeding and wounds
Chapter 16:3 providing first aid for bleeding and wounds