Wound Closure Sutures staples and adhesives Some material







- Slides: 26
Wound Closure Sutures, staples, and adhesives Some material taken from http: //www. vetmed. auburn. edu/~hendera/guide 1. htm#outline
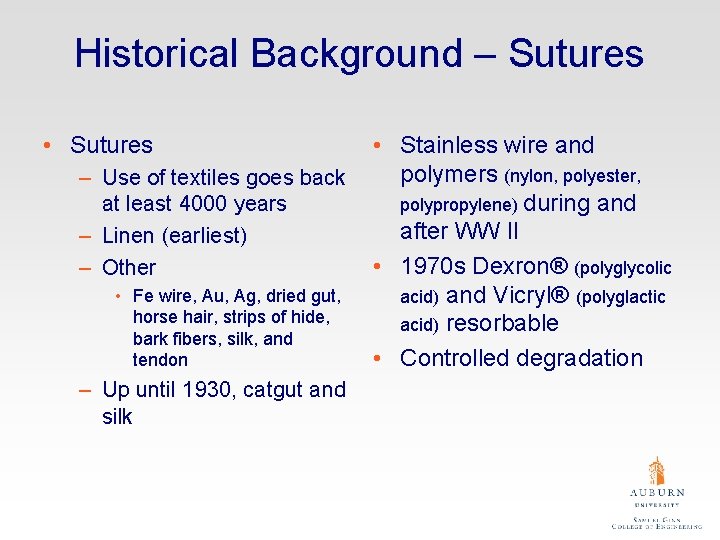
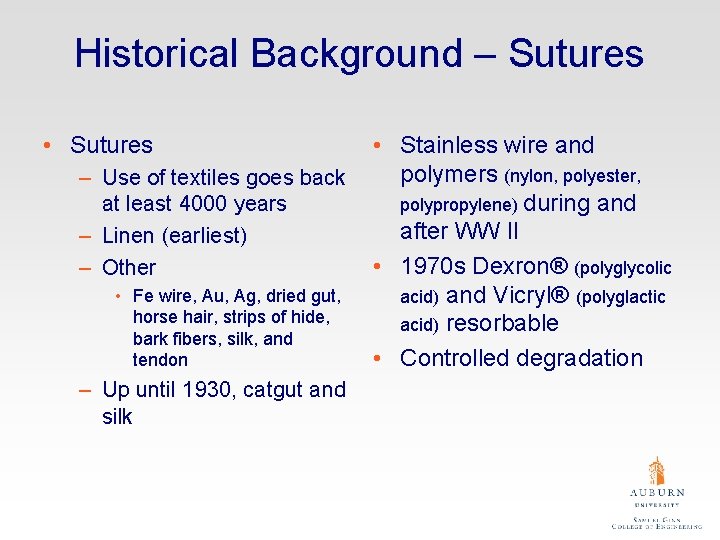
Historical Background – Sutures • Sutures – Use of textiles goes back at least 4000 years – Linen (earliest) – Other • Fe wire, Au, Ag, dried gut, horse hair, strips of hide, bark fibers, silk, and tendon – Up until 1930, catgut and silk • Stainless wire and polymers (nylon, polyester, polypropylene) during and after WW II • 1970 s Dexron® (polyglycolic acid) and Vicryl® (polyglactic acid) resorbable • Controlled degradation
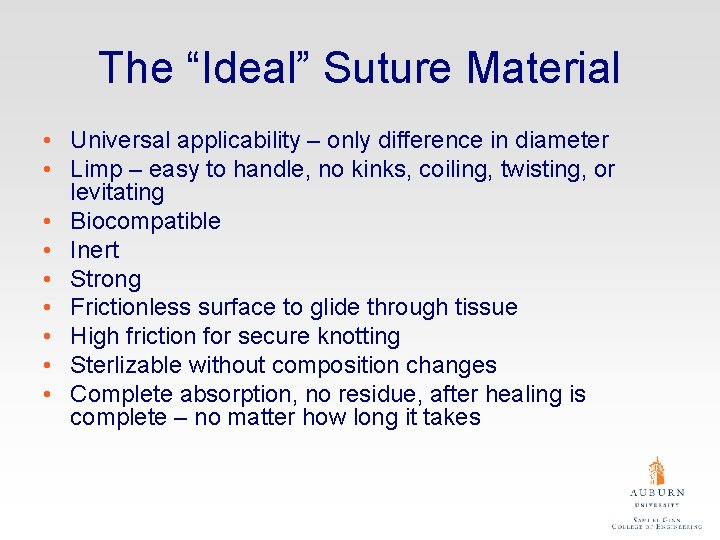
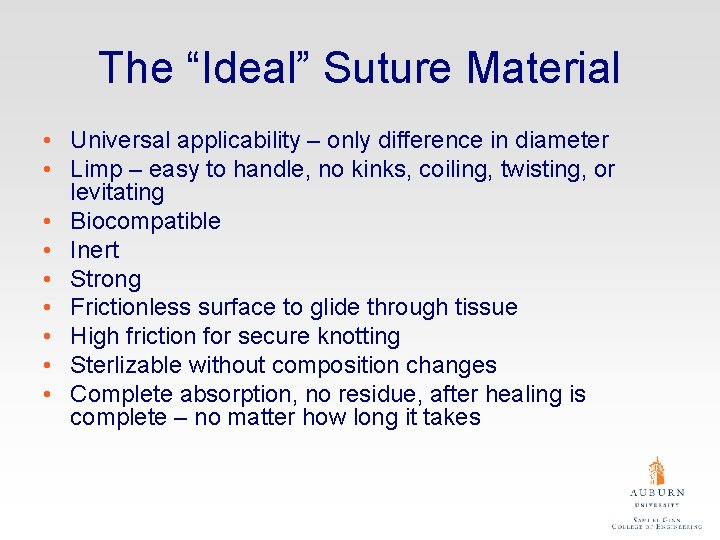
The “Ideal” Suture Material • Universal applicability – only difference in diameter • Limp – easy to handle, no kinks, coiling, twisting, or levitating • Biocompatible • Inert • Strong • Frictionless surface to glide through tissue • High friction for secure knotting • Sterlizable without composition changes • Complete absorption, no residue, after healing is complete – no matter how long it takes

Suture Classification Physical/Mechanical Size (diameter) Number of Filaments Tensile strength and elongation Elastic modulus Bending stiffness Stress relaxation and creep Capillarity Swelling Coefficient of friction Handling Biocompatibility Pliability Inflammatory reaction Packaging memory Propensity toward Knot tie-down wound Knot slippage infection, Tissue drag thrombi formation, carcinogenicity, and allergy Biodegradation Tensile breaking strength and mass loss Biocompatibility of degradation properties

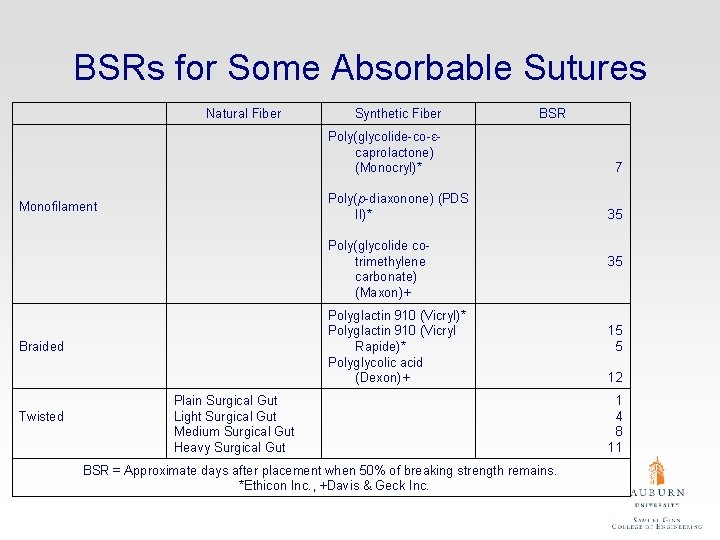
Absorbability • Lose 50% of breaking strength within 60 days of implanting • Monofilament, braided, or twisted • Natural or synthetic – Natural – enzymatic attack – Synthetic – hydrolysis • More stable mechanism • Rapidity commonly rated as percentage of breaking strength – breaking strength rate (BSR) – Can be modified in synthetic sutures
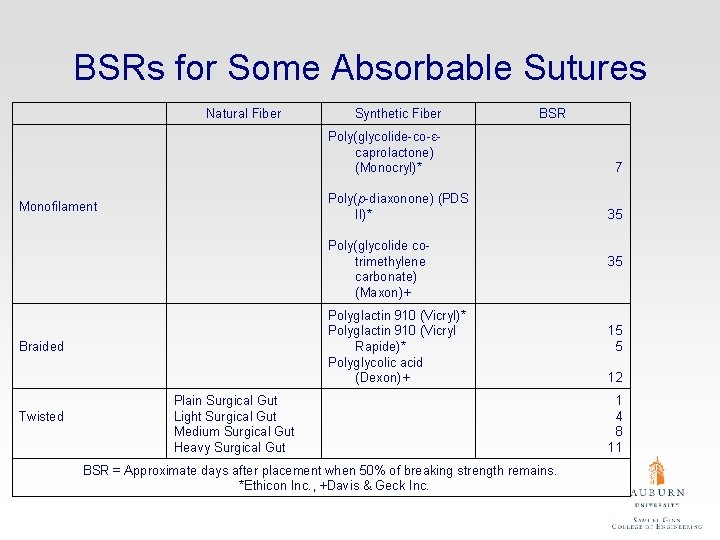
BSRs for Some Absorbable Sutures Natural Fiber Synthetic Fiber BSR Poly(glycolide-co-εcaprolactone) (Monocryl)* Poly(p-diaxonone) (PDS II)* Monofilament Poly(glycolide cotrimethylene carbonate) (Maxon)+ Polyglactin 910 (Vicryl)* Polyglactin 910 (Vicryl Rapide)* Polyglycolic acid (Dexon)+ Braided Twisted Plain Surgical Gut Light Surgical Gut Medium Surgical Gut Heavy Surgical Gut BSR = Approximate days after placement when 50% of breaking strength remains. *Ethicon Inc. , +Davis & Geck Inc. 7 35 35 15 5 12 1 4 8 11

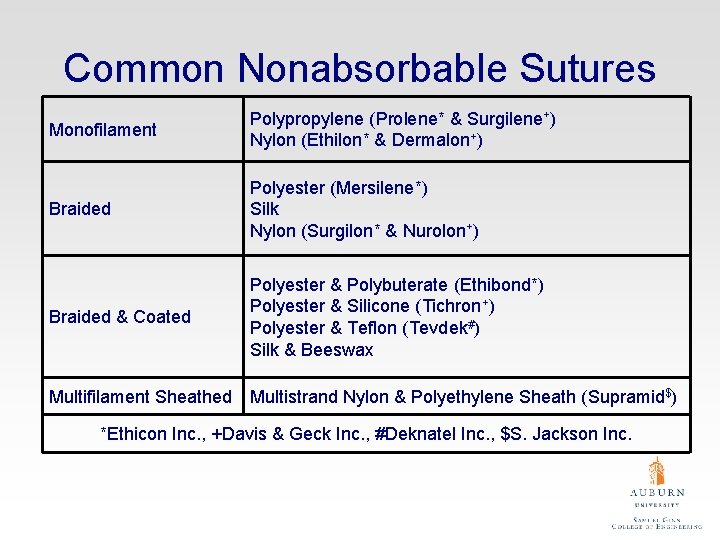
Nonabsorbable • Retain majority of breaking strength for more than 60 days • Three classes – Class I – silk, monofilament, and sheathed – Class II – cotton and linen – Class III – metallics • Classes I and III most common as Class II are prone to contamination and infection
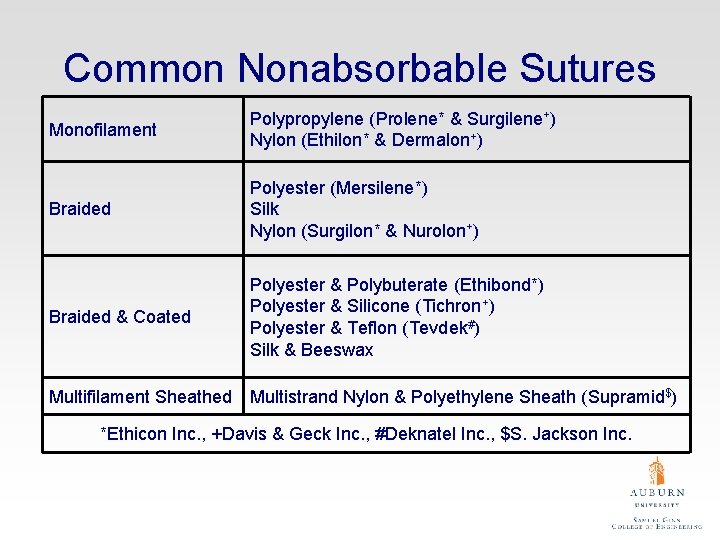
Common Nonabsorbable Sutures Monofilament Polypropylene (Prolene* & Surgilene+) Nylon (Ethilon* & Dermalon+) Braided Polyester (Mersilene*) Silk Nylon (Surgilon* & Nurolon+) Braided & Coated Polyester & Polybuterate (Ethibond*) Polyester & Silicone (Tichron+) Polyester & Teflon (Tevdek#) Silk & Beeswax Multifilament Sheathed Multistrand Nylon & Polyethylene Sheath (Supramid$) *Ethicon Inc. , +Davis & Geck Inc. , #Deknatel Inc. , $S. Jackson Inc.
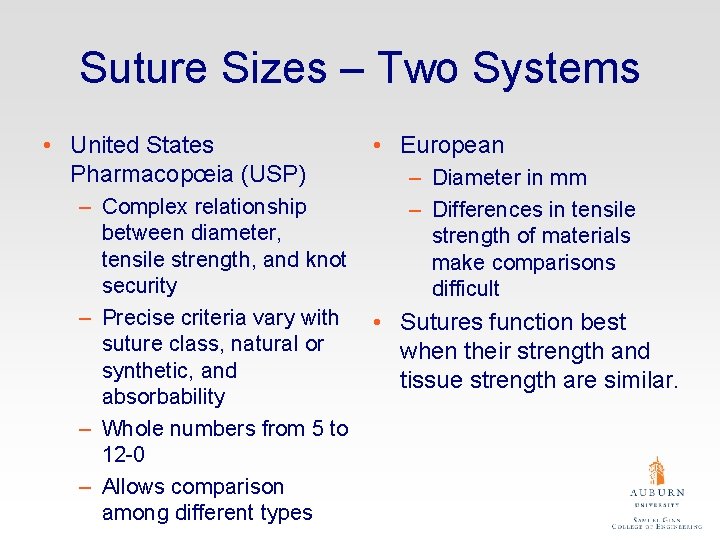
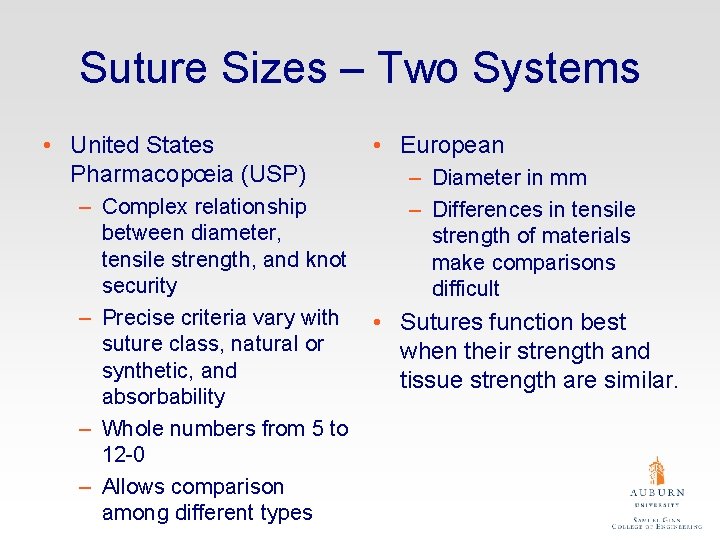
Suture Sizes – Two Systems • United States Pharmacopœia (USP) – Complex relationship between diameter, tensile strength, and knot security – Precise criteria vary with suture class, natural or synthetic, and absorbability – Whole numbers from 5 to 12 -0 – Allows comparison among different types • European – Diameter in mm – Differences in tensile strength of materials make comparisons difficult • Sutures function best when their strength and tissue strength are similar.
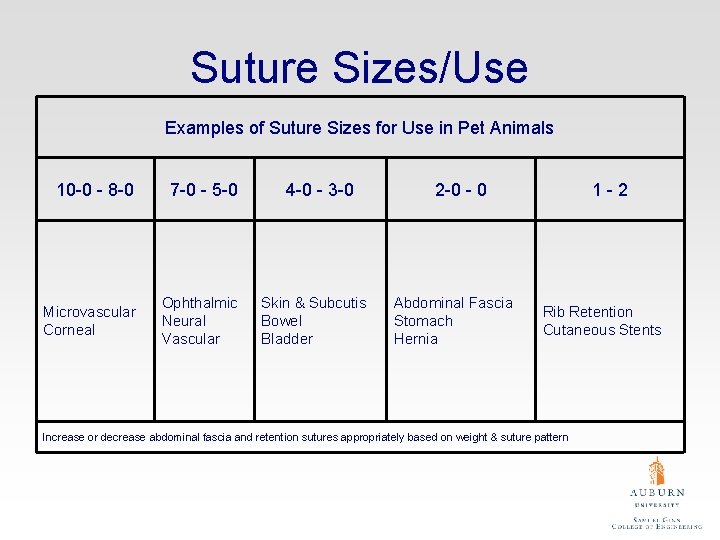
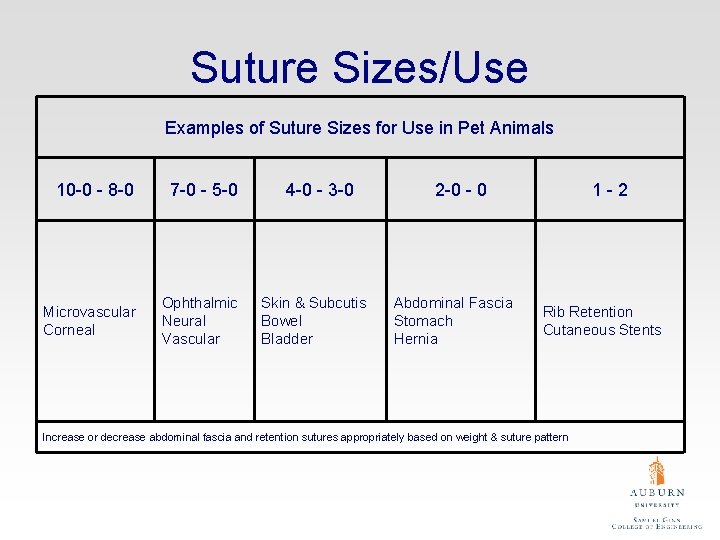
Suture Sizes/Use Examples of Suture Sizes for Use in Pet Animals 10 -0 - 8 -0 7 -0 - 5 -0 Microvascular Corneal Ophthalmic Neural Vascular 4 -0 - 3 -0 Skin & Subcutis Bowel Bladder 2 -0 - 0 Abdominal Fascia Stomach Hernia 1 -2 Rib Retention Cutaneous Stents Increase or decrease abdominal fascia and retention sutures appropriately based on weight & suture pattern
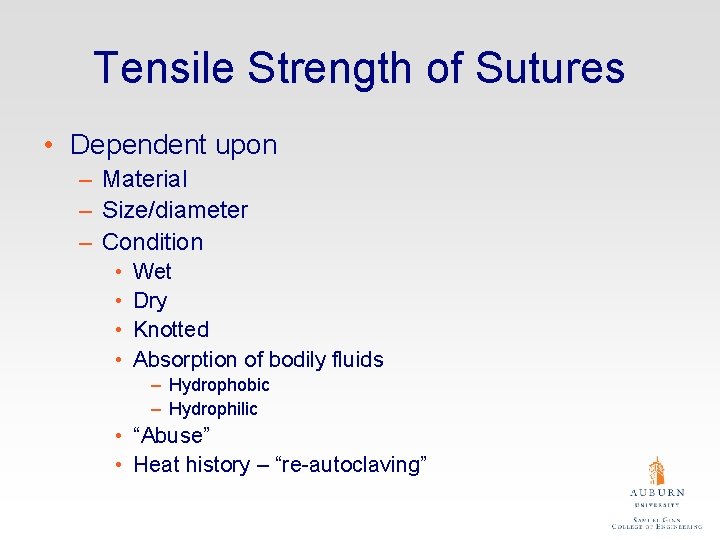
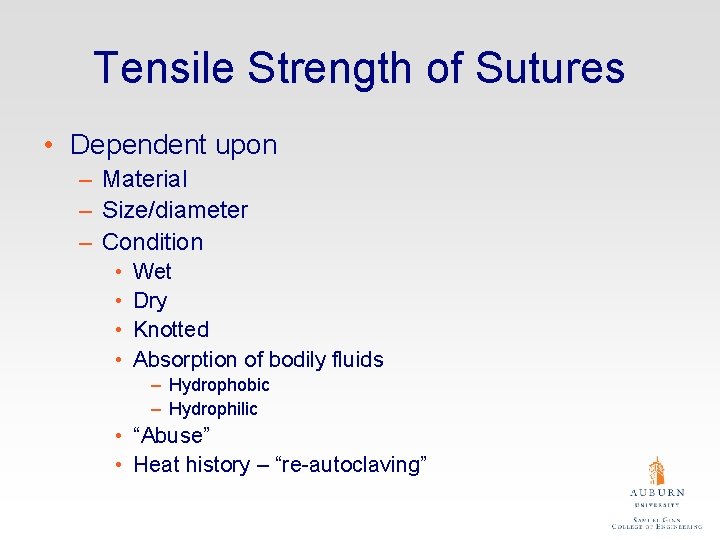
Tensile Strength of Sutures • Dependent upon – Material – Size/diameter – Condition • • Wet Dry Knotted Absorption of bodily fluids – Hydrophobic – Hydrophilic • “Abuse” • Heat history – “re-autoclaving”
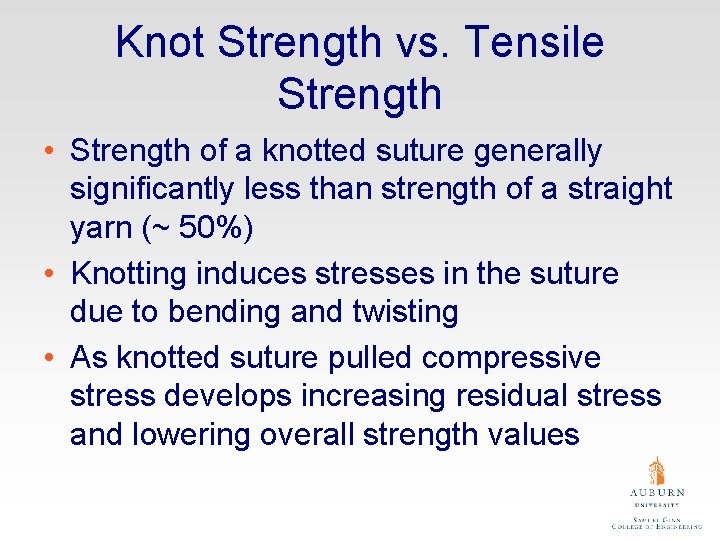
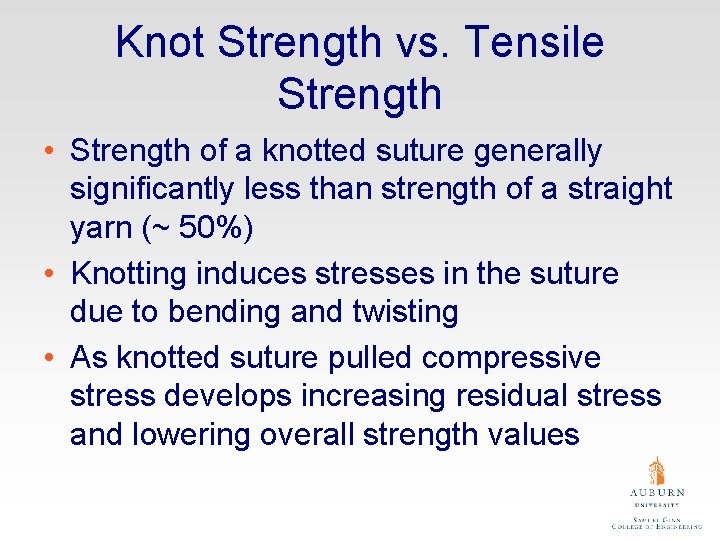
Knot Strength vs. Tensile Strength • Strength of a knotted suture generally significantly less than strength of a straight yarn (~ 50%) • Knotting induces stresses in the suture due to bending and twisting • As knotted suture pulled compressive stress develops increasing residual stress and lowering overall strength values
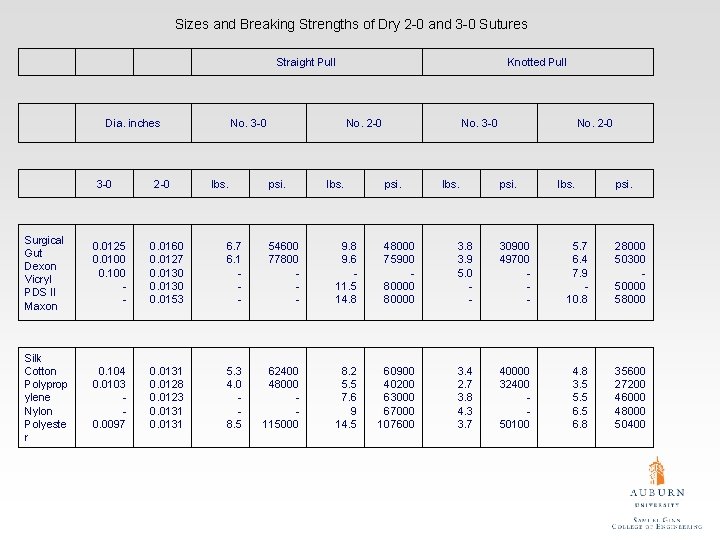
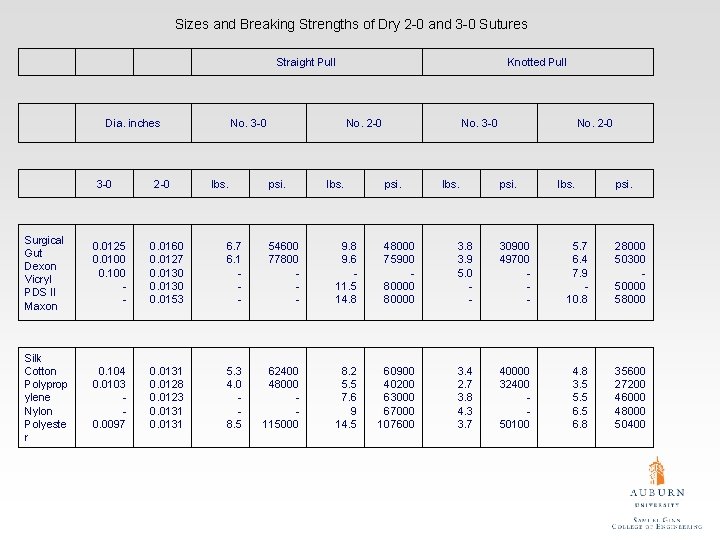
Sizes and Breaking Strengths of Dry 2 -0 and 3 -0 Sutures Straight Pull Dia. inches 3 -0 2 -0 No. 3 -0 lbs. Knotted Pull No. 2 -0 psi. lbs. No. 3 -0 psi. lbs. No. 2 -0 psi. lbs. psi. Surgical Gut Dexon Vicryl PDS II Maxon 0. 0125 0. 0100 0. 100 - 0. 0160 0. 0127 0. 0130 0. 0153 6. 7 6. 1 - 54600 77800 - 9. 8 9. 6 11. 5 14. 8 48000 75900 80000 3. 8 3. 9 5. 0 - 30900 49700 - 5. 7 6. 4 7. 9 10. 8 28000 50300 50000 58000 Silk Cotton Polyprop ylene Nylon Polyeste r 0. 104 0. 0103 0. 0097 0. 0131 0. 0128 0. 0123 0. 0131 5. 3 4. 0 8. 5 62400 48000 115000 8. 2 5. 5 7. 6 9 14. 5 60900 40200 63000 67000 107600 3. 4 2. 7 3. 8 4. 3 3. 7 40000 32400 50100 4. 8 3. 5 5. 5 6. 8 35600 27200 46000 48000 50400

Coating Materials • Facilitate handling – Ease of passing through tissue – Ease in sliding knots down – But can result in poor knot security • Nonabsorbable coatings – – Beeswax Silicone Paraffin wax Poly(tetrafluoroethylene) • Absorbable – Must be absorbable like the suture • Water soluble • Water insoluble – break down by hydrolysis
Problems Associated with Surgical Sutures • Time-consuming nature of secure knot tying • Need for knot security under all conditions with all sutures • Risk of suture breakage during surgery • Loss of control due to needle slippage or rotation within the needle holder • Postsurgical slippage of the knotted suture • Early or pathologically induced degradation of absorbable suture
Ligating Clips • Essentially “clips” to • Requirements replace sutures when – Nontoxic and biocompatible occluding (closing) the – Absence of allergic lumen (central canal) and immunogenic of a vessel or tubular effects organ – Blood vessels – Gynecological & urological (GU) procedures • Metallic or polymeric – Tolerated by wide range of tissue types – High strength and low solubility – Finite longevity – Secure
Metallic Clips • First – Cushing neurosurgery clip, 1910 – Ag wire formed in the shape of a “U” and closed around blood vessel – Tantulum (1940) • Tubule ligation – Others • Co-Cr • Titanium • Stainless Steel • “Memory metal” – Ni-Ti alloy • • Desirable properties in metallic clips – High strength – Malleability & ductility – can make fine wire – Capacity for work-hardening – Corrosion resistance Some problems – Allergic reaction – Radio-opaque – can cause problems with CT, X-ray, and MRI examinations
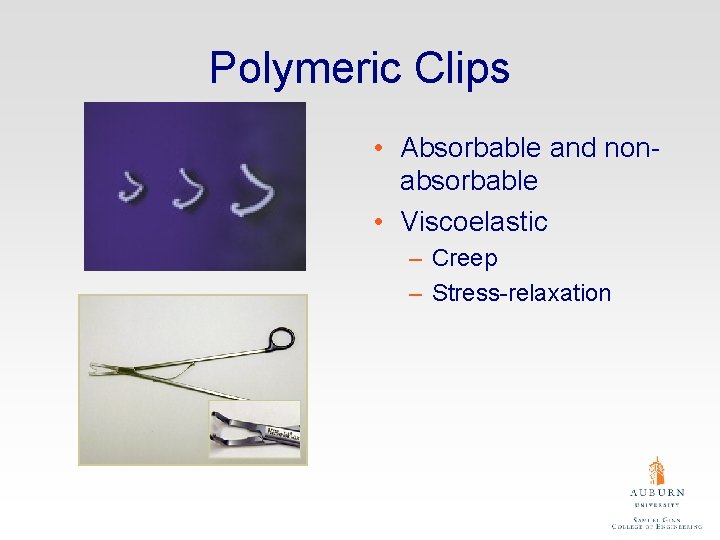
Polymeric Clips • Absorbable and nonabsorbable • Viscoelastic – Creep – Stress-relaxation
Surgical Stapling • Introduced in the late 1970 s • Used widely in human and veterinary medicine – – – Gynecological Cardiovascular Gastrointestinal Esophageal Pulmonary • Staples originally stainless but now Ti and polymeric used – Polymeric – 2 parts • “U”-shaped fastener • Figure “ 8” retainer

Surgical Staples Staple Gun Staple Remover

Staples & Clips vs. Sutures • • • Speed Convenience Reduced infection rate Lower cost If done properly, no cosmetic difference
Tissue Adhesives Before Curing After Curing • Sterilizable • Easy in preparation • Viscous liquid or liquid possible for spray • Nontoxic • Rapidly curable under wet physiological conditions (p. H 7. 3, 37°C, 1 atm) • Reasonable cost • Strongly bondable to tissues • Biostable union until wound healing • Tough and pliable • Resorbable after wound healing • Nontoxic • Nonobstructive to wound healing or promoting wound healing
Natural Tissue – Fibrin Glue • First reported in 1940 • Mimics blood clot – major component fibrin network • Excellent tissue adhesive but insufficient in amount for larger wounds • Nontoxic if human protein sources are used to obtain fibrin
Synthetic Systems: Poly-Alkyl-2 -Cyanoacrylates • Discovered in 1951 • “Crazy Glue” • H 2 C=C―CO 2―R CN • R = alkyl group – CH 3 (methyl) – H 3 CCH 2 (ethyl) • Release small amount of formaldehyde when curing – amount lessens with length of alkyl chain

Characteristics of Currently Available Adhesive Systems Fibrin Glue Cyanoacrylate Handling Excellent Poor Set time Medium Short Poor Good Pliability Excellent Poor Toxicity Low Medium Resorbability Good Poor Cell infiltration Excellent Poor Tissue bonding
Other Experimental Systems • Gelatin-based adhesives – Mimic coagulation but without fibrin • Polyurethane (-HNOCO-) based adhesives – Capped with isocyanate to rapidly gel upon exposure to water – More flexible than current cyanoacrylate adhesives • Collagen-based adhesives
 Prep and drape
Prep and drape Amulet of wound closure
Amulet of wound closure Watchman flx sizing chart
Watchman flx sizing chart Watchman flx dfu
Watchman flx dfu Chapter 9 adhesives gluing and clamping answer key
Chapter 9 adhesives gluing and clamping answer key Chapter 9 adhesives gluing and clamping
Chapter 9 adhesives gluing and clamping Building materials, fasteners, and adhesives
Building materials, fasteners, and adhesives D aircraft adhesives
D aircraft adhesives Hernia en glissade
Hernia en glissade Gomco clamp
Gomco clamp Vicryl pop offs
Vicryl pop offs Vetafil
Vetafil Sutura continua a sopraggitto
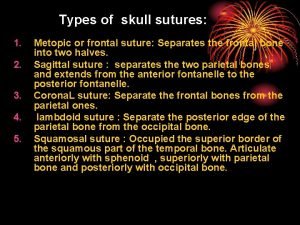
Sutura continua a sopraggitto Skull sutures
Skull sutures Suture colour coding
Suture colour coding Body sutures
Body sutures Appendicular skeleton figure 5-8
Appendicular skeleton figure 5-8 Equicel
Equicel Uterine compression sutures
Uterine compression sutures Uterine compression sutures
Uterine compression sutures Grasping instrument used with sutures
Grasping instrument used with sutures Surgical staples
Surgical staples Uterine compression sutures
Uterine compression sutures Pulley sutures
Pulley sutures Staples copy machine
Staples copy machine Staples protractor and compass
Staples protractor and compass Contact and non contact forces
Contact and non contact forces