Odessa National Medical University Department of Normal and








- Slides: 75
Odessa National Medical University Department of Normal and Pathological Clinical Anatomy Lecture on the topic: Adaptation and compensation processes. Regeneration and reparation. Sclerosis.
CELLULAR ADAPTATIONS § Compensatory and adaptive reactions of the complete organism are difficult complexes of physiologic reactions, which change their quantity and quality, take place during any pathological conditions of the organism. There are two main properties for the living system according to CAP (compensation and adaptation processes): Ø constancy for a safety of the shape and the function when conditions are changing (homeostasis) Ø activity and change of the shape and the function during the process of adaptation to environmental conditions
On the molecular level CAP reactions are provided by: Ø obligatory, qualitative stability of the proteineous metabolism; Ø its broad quantitative variations; Ø the availability of the common plastic cellular reserve (the stock of structural-organized proteins, the stock of RNA, the ability to quick decay of RNA, the reproduction of DNA); Ø convertibility of differentiation of structure and function. Regulation mechanism of molecular level of CAP : Ø enzymatic; Ø humoral (a selective action of different metabolites and hormones); Ø nervous.
On cellular level compensation and adaptation reactions are provided by: Ø the common plastic reserve of the cell; Ø the large stock of cells and the ability to alternate work and rest; Ø the ability of cells to reproduce; Ø their ability for metaplasia.
On organic level: Ø the stock of functional units of the organ; Ø difference of their functions; Ø ability to regenerate the functional units On systemic level: Ø Quantitative broad variations of the structure and the function. Morphologic manifestations of compensated and adapted reactions are inflammation, regeneration, immune reactions, etc.
There are three phases of CAP development : 1. Conception of compensation. At this moment all functions strain themselves sharply, the metabolism is excited, it can be a shortage of reserves. Dystrophy and hypoxia develop at the first stages. This stage is sometimes called emergency. 2. The phase of fixing. CAP get complete development. Dystrophic changes are liquidated, the protein begins to be synthesized heavily, organs' mass and weight increase, the function is sometimes increased (by 100150%).
3. The phase of exhaustion (decompensation). Exhaustion always begins after intensified work, because the resynthesis of adenosine triphosphate (ATP) is weakened. The function is completely stops when all ATP is spent.
Adaptation occurs by some different pathological processes : § hypertrophy (hyperplasia) § atrophy § metaplasia § dysplasia § organization (sclerosis)
Hypertrophy and hyperplasia Hypertrophy refers to an increase in the size of parenchymal cells resulting in enlargement of the organ or tissue, without any change in the number of cells. Hyperplasia is an increase in the number of parenchymal cells resulting in enlargement of the organ or tissue. Quite often, both hyperplasia and hypertrophy occur together.
Mechanisms of hypertrophy Ø hypertrophy of tissue arises due to increase of size of functional cells. Thus, the hypertrophied organ has no new cells, just larger cells. Ø hypertrophy of tissue arises due to increase of number of functional cells (hyperplasia of cells). Ø hypertrophy of cells arises due to both increase of size of functional cells and increase of number of ultrastructural elements. Ø { No increased intake of fluid, called cellular swelling or edema, but the synthesis of more structural components}. It is called true hypotrophy.
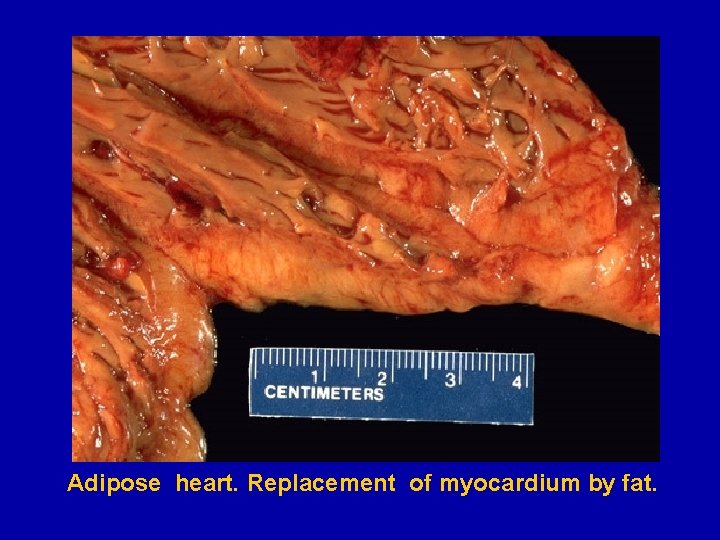
Ø False hypertrophy is the increase of the size of organs due to growth of connective tissue, accumulation of the fluid or fatty tissue. It results in atrophy of organ (hydronephrosis, hydrocephalus, obesity of heart). Ø True hypertrophy (hyperplasia) has adaptative and compensative characteristics and may be physiologic and pathologic:
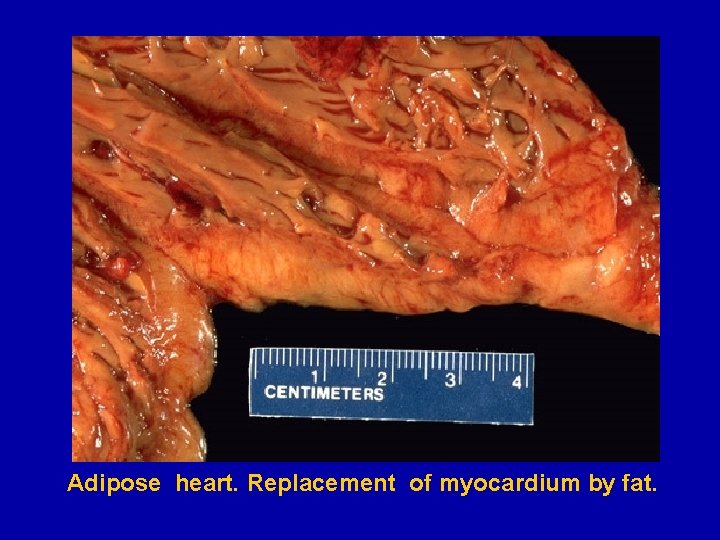
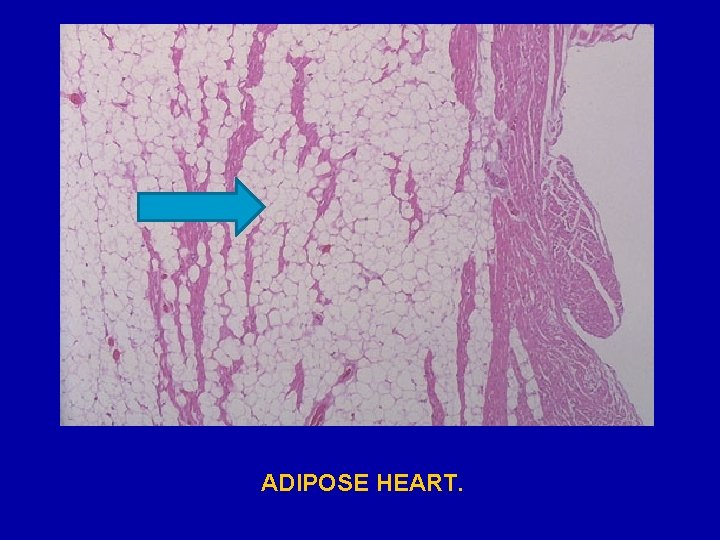
Adipose heart. Replacement of myocardium by fat.
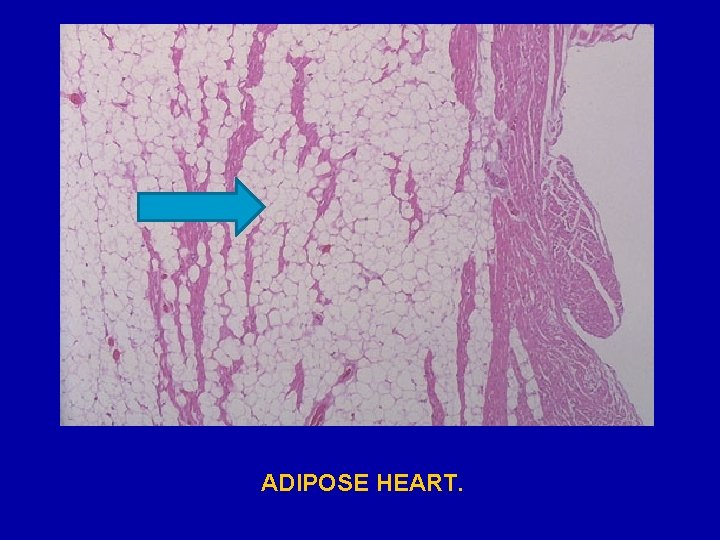
ADIPOSE HEART.
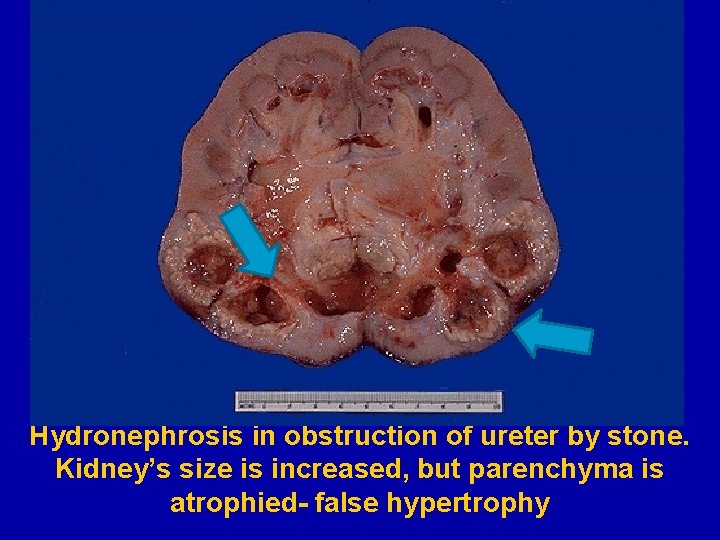
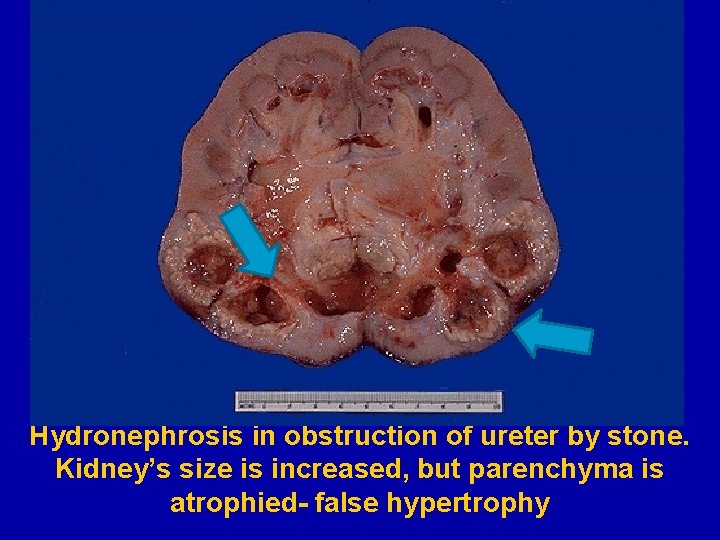
Hydronephrosis in obstruction of ureter by stone. Kidney’s size is increased, but parenchyma is atrophied- false hypertrophy
Hydronephrosis develops in obstruction (stone), compression (tumor, additional renal artery) of ureter or any other difficulty of urine passage (congenital strictures etc. ) § Macroscopically: The kidney is sharply enlarged, cortical and medullary layers are very thin, without clear distinguished border. System pelvis – calyxes is dilated.
§ Microscopically: cortex and pyramids sharply reduced. Glomeruli undergo atrophy with following replacement by connective tissue. Same changes develop in convoluted tubules with partial cystic transformation, formation of proteineous cylinders (homogenic eosinophilic mass), reduction of epithelium.
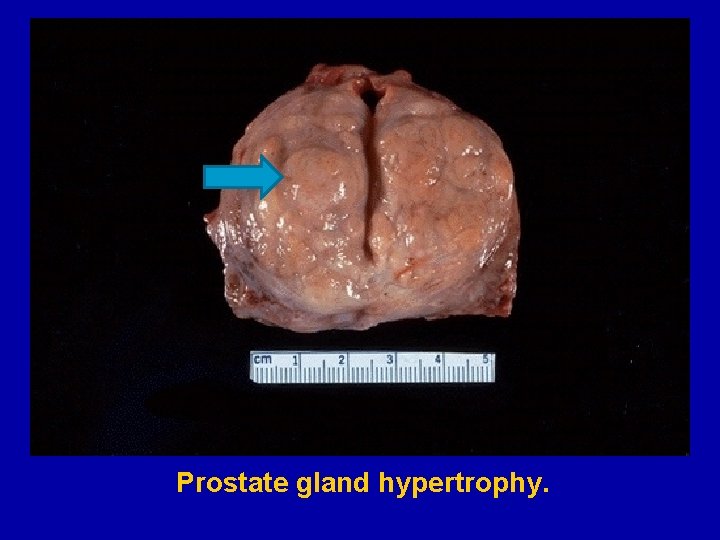
A. Physiologic hypertrophy (hyperplasia). 1. Neurohumoral (hormonal) hypertrophy: hypertrophy of female breast at puberty, during pregnancy and lactation, hypertrophy of pregnant uterus, proliferative activity of normal endometrium after a normal menstrual cycle, prostatic hyperplasia in old age. 2. Working hypertrophy of skeletal muscle: hypertrophied muscles in athletes and manual labour.
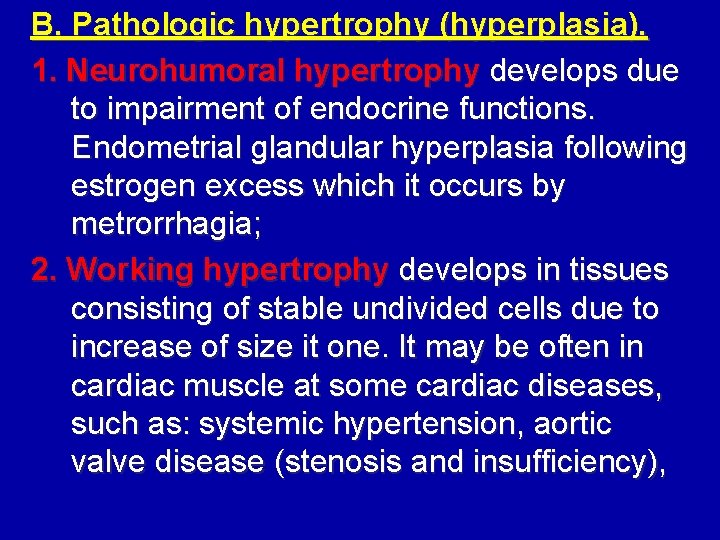
B. Pathologic hypertrophy (hyperplasia). 1. Neurohumoral hypertrophy develops due to impairment of endocrine functions. Endometrial glandular hyperplasia following estrogen excess which it occurs by metrorrhagia; 2. Working hypertrophy develops in tissues consisting of stable undivided cells due to increase of size it one. It may be often in cardiac muscle at some cardiac diseases, such as: systemic hypertension, aortic valve disease (stenosis and insufficiency),
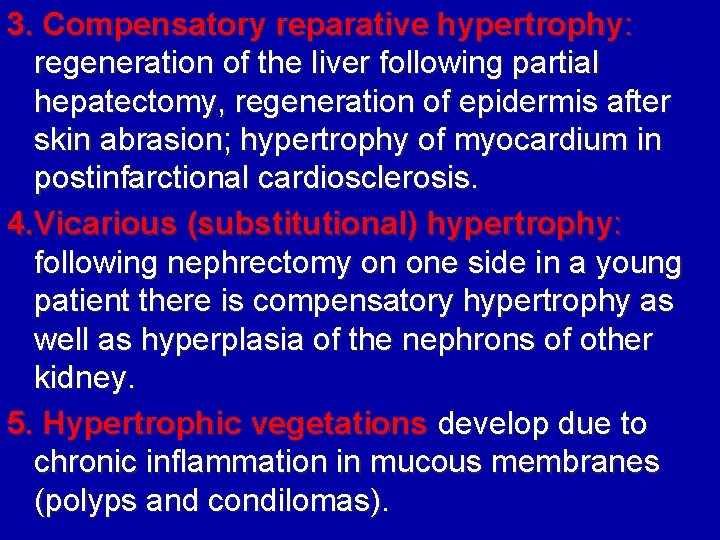
3. Compensatory reparative hypertrophy: regeneration of the liver following partial hepatectomy, regeneration of epidermis after skin abrasion; hypertrophy of myocardium in postinfarctional cardiosclerosis. 4. Vicarious (substitutional) hypertrophy: following nephrectomy on one side in a young patient there is compensatory hypertrophy as well as hyperplasia of the nephrons of other kidney. 5. Hypertrophic vegetations develop due to chronic inflammation in mucous membranes (polyps and condilomas).
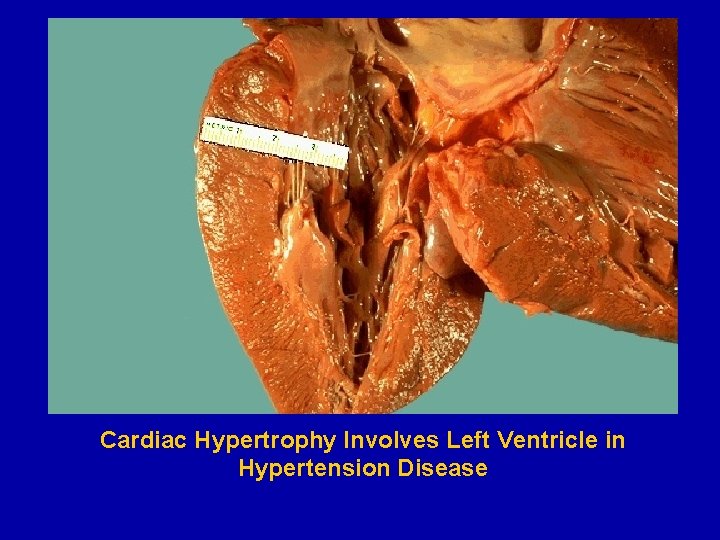
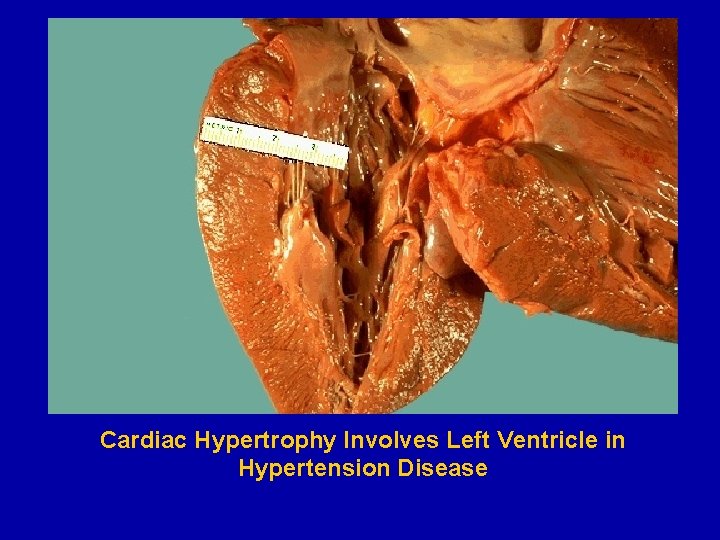
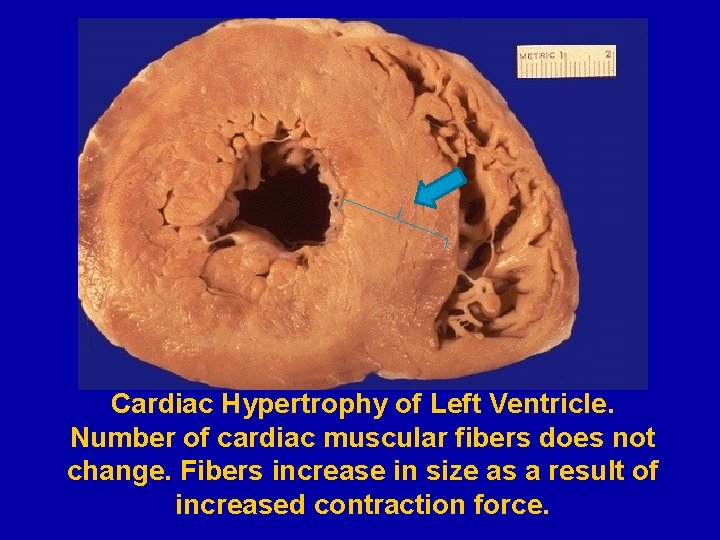
Cardiac Hypertrophy Involves Left Ventricle in Hypertension Disease
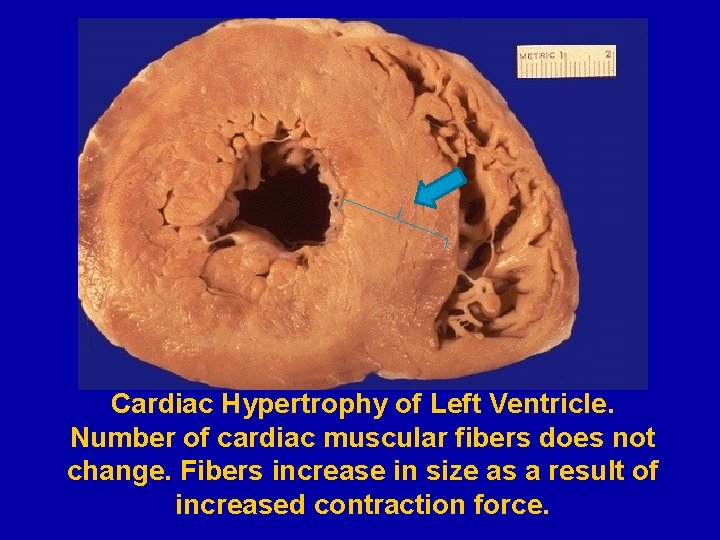
Cardiac Hypertrophy of Left Ventricle. Number of cardiac muscular fibers does not change. Fibers increase in size as a result of increased contraction force.

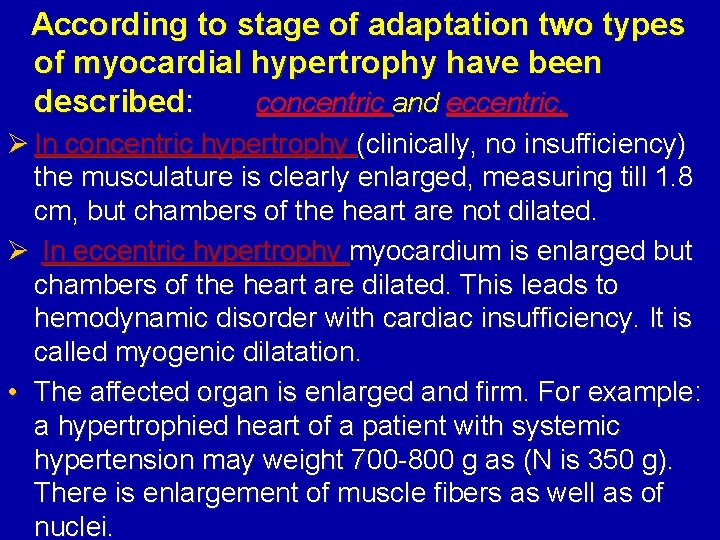
According to stage of adaptation two types of myocardial hypertrophy have been described: concentric and eccentric. Ø In concentric hypertrophy (clinically, no insufficiency) the musculature is clearly enlarged, measuring till 1. 8 cm, but chambers of the heart are not dilated. Ø In eccentric hypertrophy myocardium is enlarged but chambers of the heart are dilated. This leads to hemodynamic disorder with cardiac insufficiency. It is called myogenic dilatation. • The affected organ is enlarged and firm. For example: a hypertrophied heart of a patient with systemic hypertension may weight 700 -800 g as (N is 350 g). There is enlargement of muscle fibers as well as of nuclei.
§ § Mechanisms of working myocardial hypertrophy Hypertrophy of intracellular organelles Hyperplasia of cytoplasmic structures such as EPR, ribosome, myofilaments, mitochondria Polyploidy of cardiac muscle nuclei Number of cardiac muscle cells does not increase
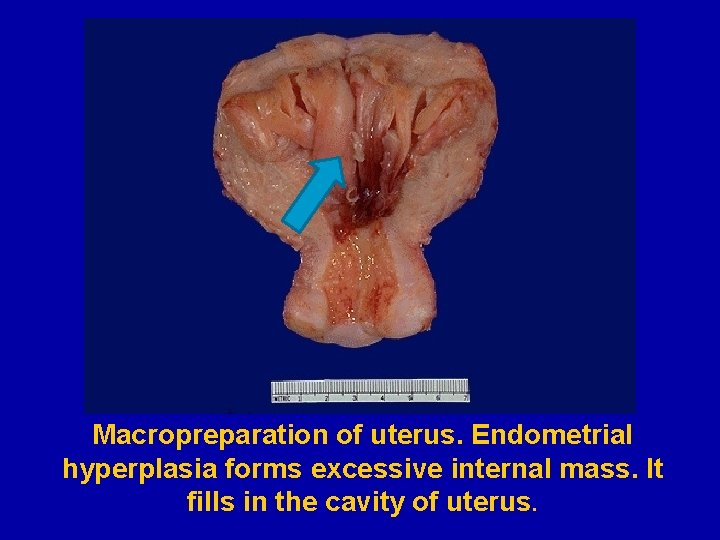
Glandular hyperplasia of endometrium § It is example of neurohumoral (hormonal) hypertrophy. Develops under the action of dysfunctional ovarian hormones production. § Macroscopically: endometrium is markly thick, crumbly, easily detached
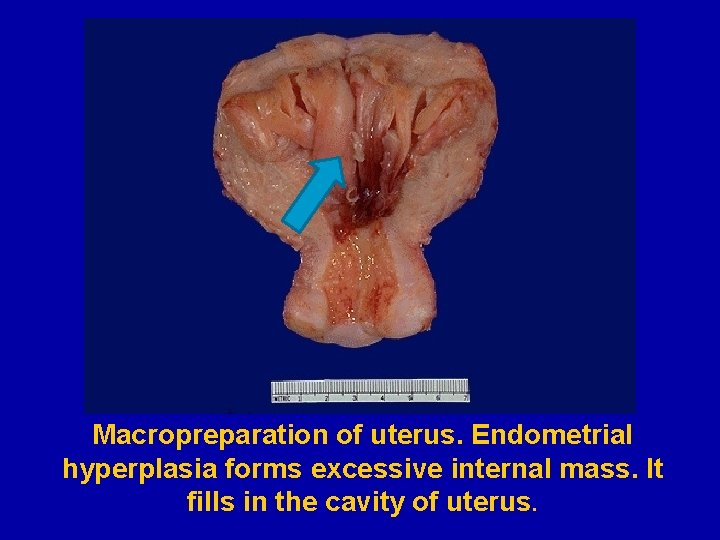
Macropreparation of uterus. Endometrial hyperplasia forms excessive internal mass. It fills in the cavity of uterus.
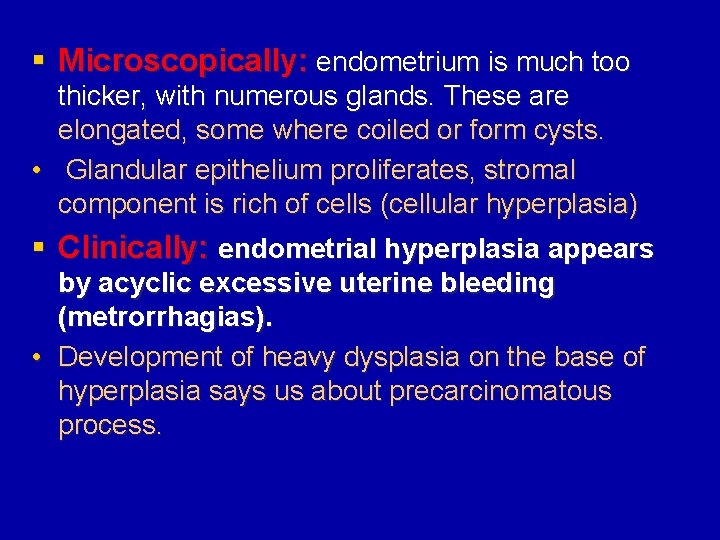
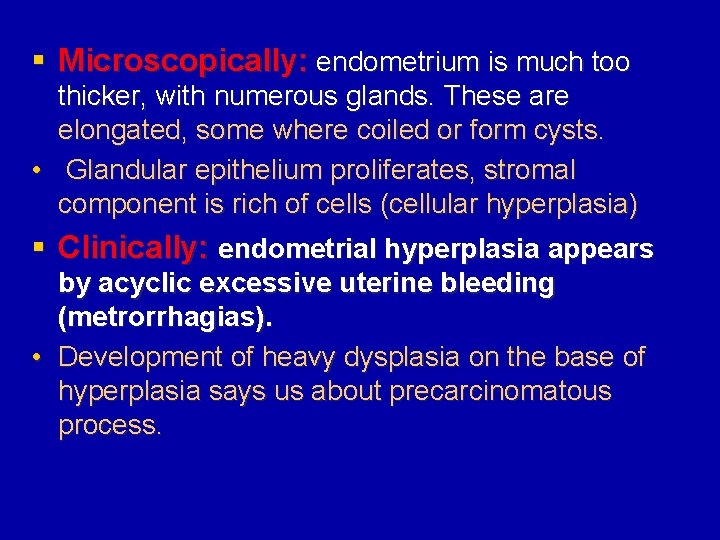
§ Microscopically: endometrium is much too thicker, with numerous glands. These are elongated, some where coiled or form cysts. • Glandular epithelium proliferates, stromal component is rich of cells (cellular hyperplasia) § Clinically: endometrial hyperplasia appears by acyclic excessive uterine bleeding (metrorrhagias). • Development of heavy dysplasia on the base of hyperplasia says us about precarcinomatous process.
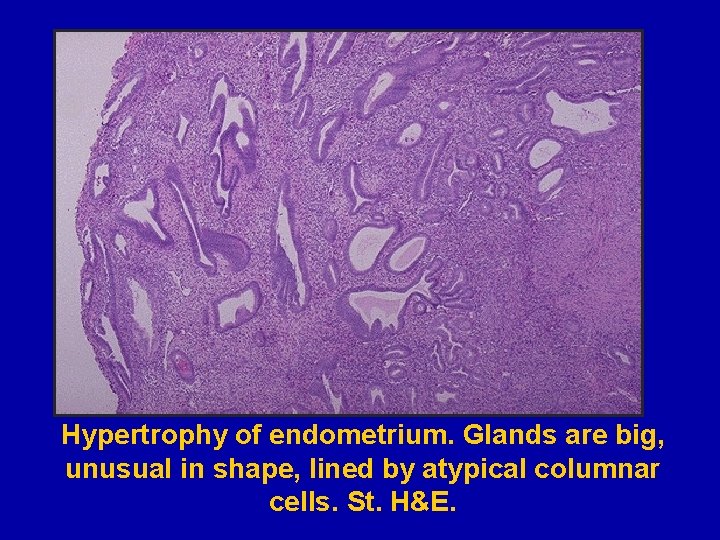
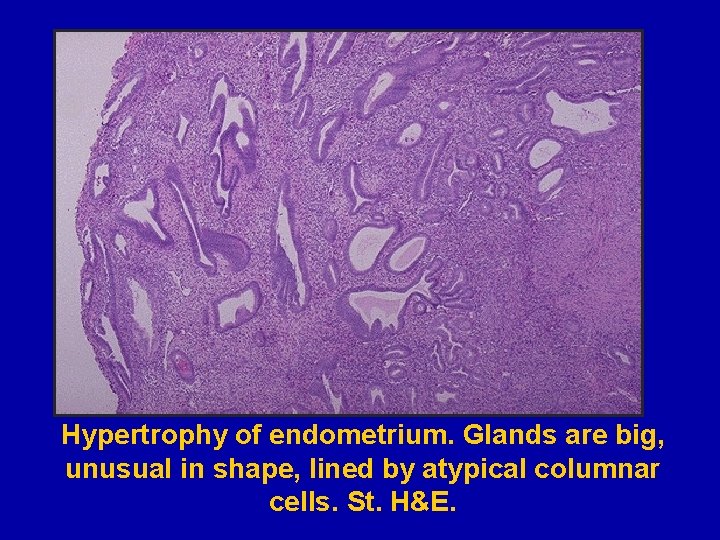
Hypertrophy of endometrium. Glands are big, unusual in shape, lined by atypical columnar cells. St. H&E.

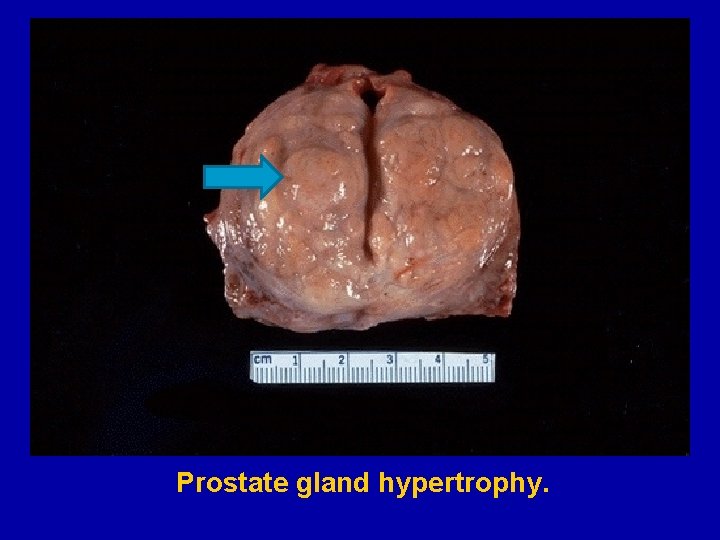
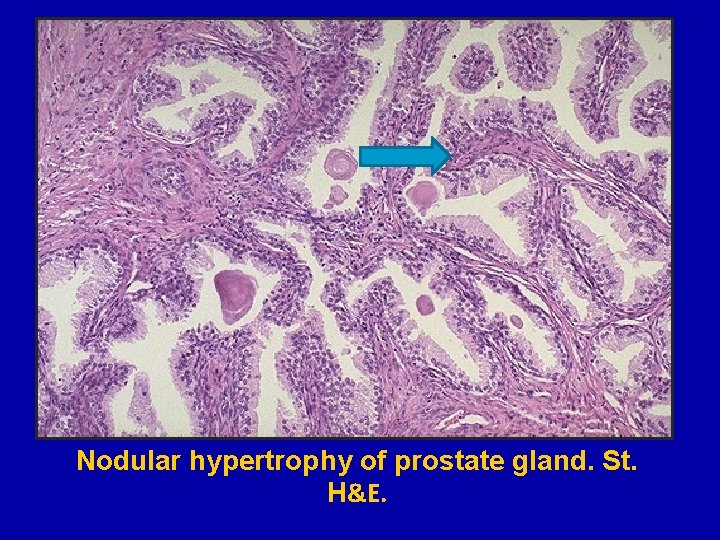
Prostate gland hypertrophy.
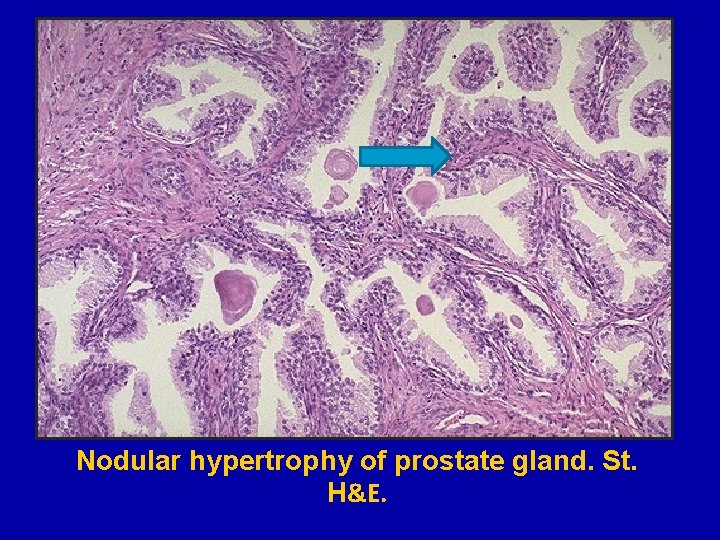
Nodular hypertrophy of prostate gland. St. H&E.
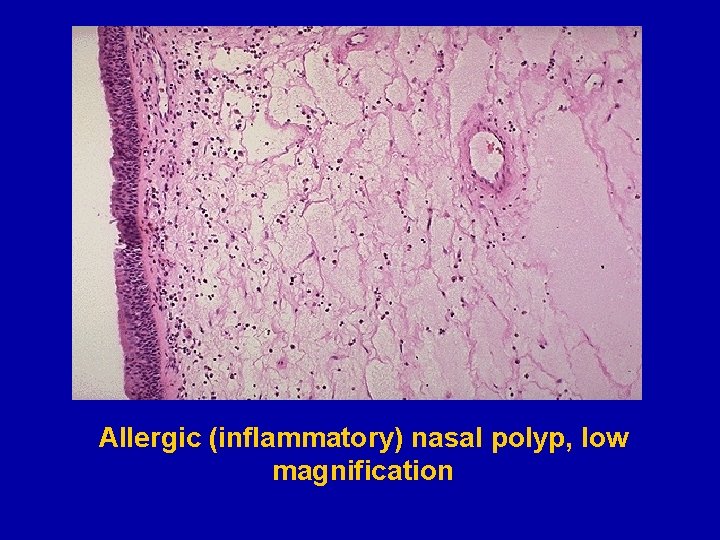
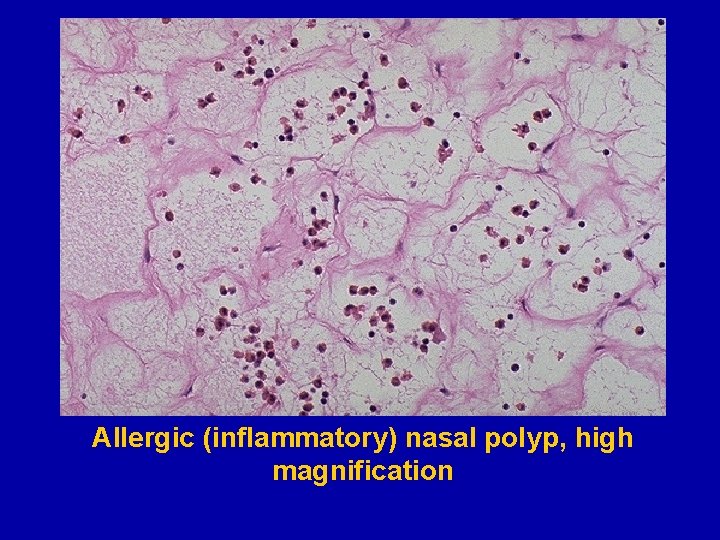
§ Hypertrophic changes lead to enlargement of organs and tissues. § Occurs in inflammation process of mucous membranes with hypertrophic polyps and condylomas formation
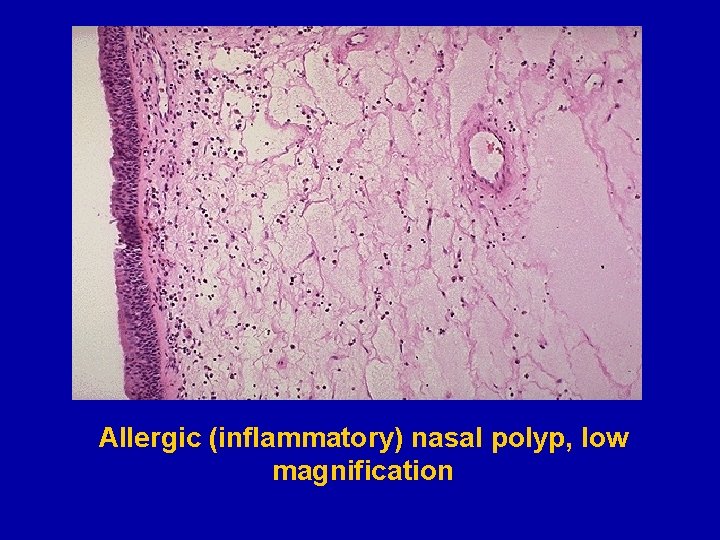
Allergic (inflammatory) nasal polyp, low magnification
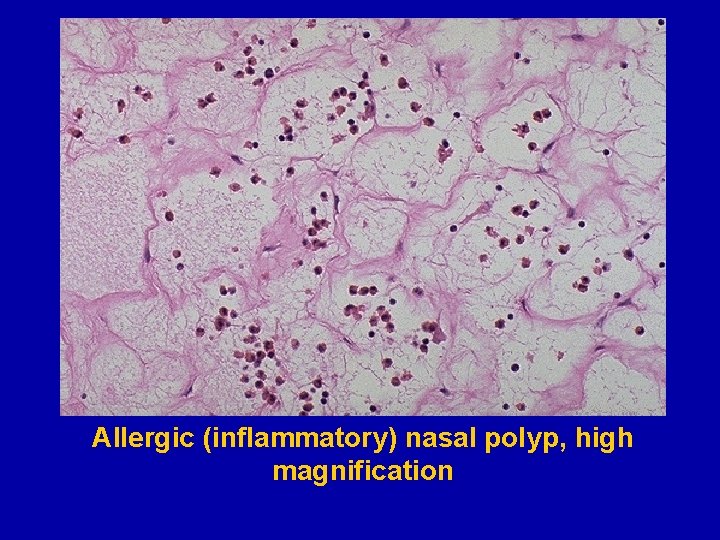
Allergic (inflammatory) nasal polyp, high magnification
Atrophy means reduction of the number and size of cells, tissues and organs in living organism characterized by decrease or stopping their function. § Atrophy may be physiological and pathological. A. Physiological atrophy. It is a normal process of aging in some tissues: Ø Atrophy of lymphoid tissue in lymph nodes, appendix and thymus. Ø Atrophy of gonads after menopause. Ø Atrophy of brain. Ø Atrophy of bones. Ø It may be obliteration of the umbilical arteries and arterial duct (Botallow’s) after birth.
B. Pathological atrophy may be general and local. General atrophy is observed in cachexia due to Ø Oncologic and chronic diseases. Ø Starvation. Ø Injury of hypophysis (endocrine cachexia). Ø Injury of hypothalamus (cerebral cachexia).
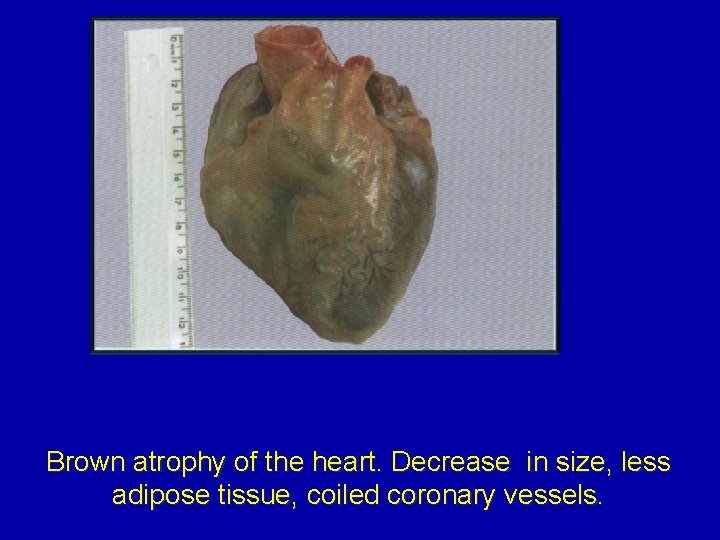
Gross (macroscopical) appearance of patients occurs: • Sharp exhaustion. • Adipose tissue is decreased and it has brown color. • Muscles are atrophied; skin is dry and flabby. • Internal organs are small, brown color and often shrunken (brown atrophy). • Osteoporosis takes place.
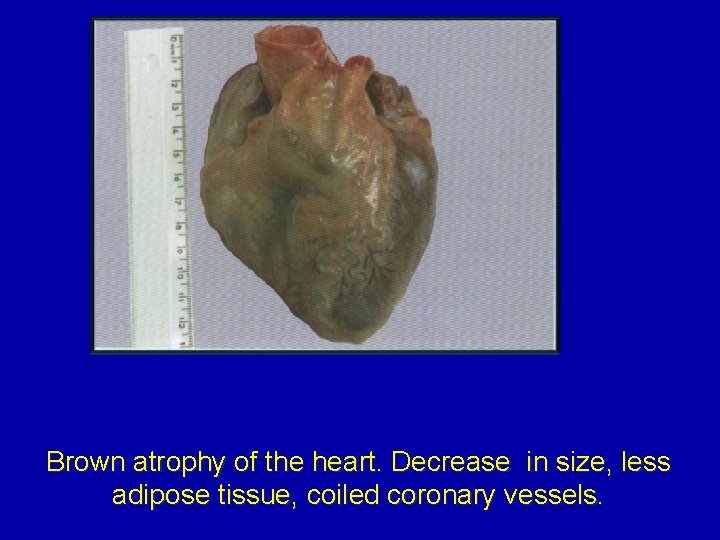
Brown atrophy of the heart. Decrease in size, less adipose tissue, coiled coronary vessels.
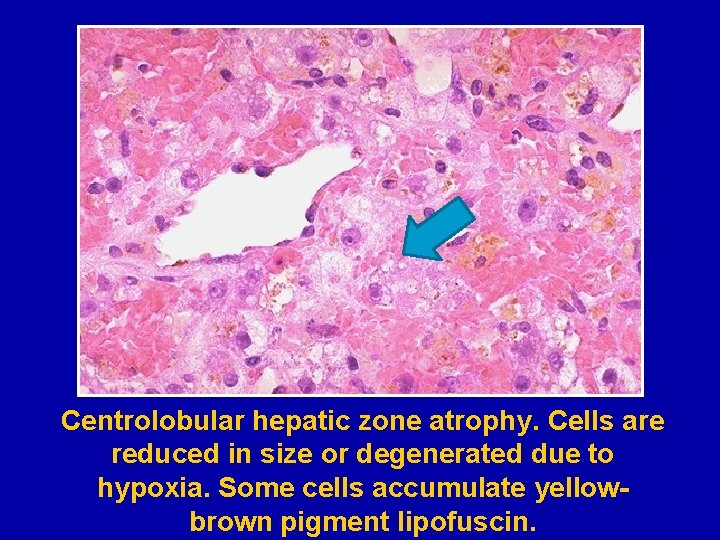
Histologically (microscopical appirience): • Cells become smaller in size but are not dead cells. • Shrinkage in cell size is due to reduction in cell organelles. • Accumulation of lipofuscin around nucleus takes place. Lipofuscin (“wear and tear” pigment) is a golden yellow pigment representing undigested lipid material derived from cellular metabolism.
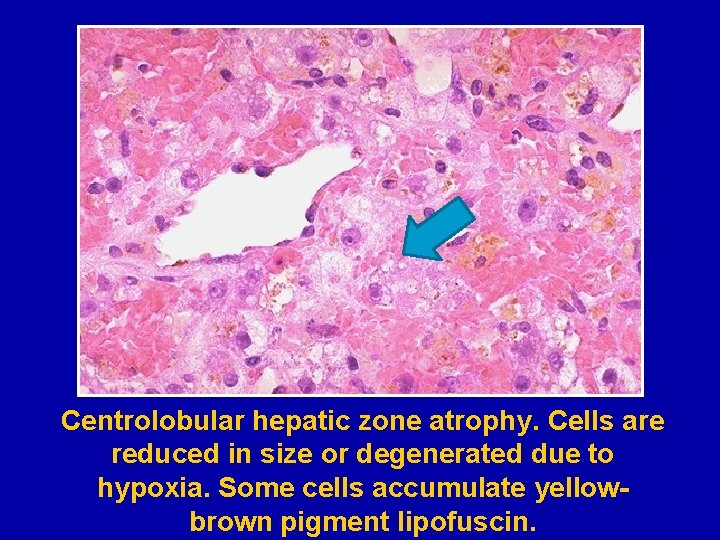
Centrolobular hepatic zone atrophy. Cells are reduced in size or degenerated due to hypoxia. Some cells accumulate yellowbrown pigment lipofuscin.
Local atrophy has several types: 1. Ischemic atrophy develops due to insufficiency of the blood supply. Hypoxia stimulates fibroblasts proliferation and forms sclerosis. For example: small atrophic kidney in atherosclerosis of renal artery, atrophy of brain in cerebral atherosclerosis. 2. Disuse atrophy (dysfunctional) develops due to reduction of the function of organ: atrophy of muscles due to immobility, atrophy of the pancreas in obstruction of pancreatic duct. 3. Neuropathic atrophy due to interrupted nerve supply: poliomyelitis, motor neuron disease, nerve section, and inflammation of facial nerve.
4. Endocrine atrophy: hypopituitarism may lead to atrophy of thyroid, adrenal and gonads; hypothyroidism may cause atrophy of the skin and its adnexal structures. 5. Pressure atrophy: compression of spine by tumor in nerve root, compression of skull by meningioma arising from pia-arachnoid, compression of sternum by aneurysm of arch of aorta, compression of renal tissue by dilated renal pelvic in hydronephrosis, compression of brain tissue by dilated ventricles in hydrocephalus.
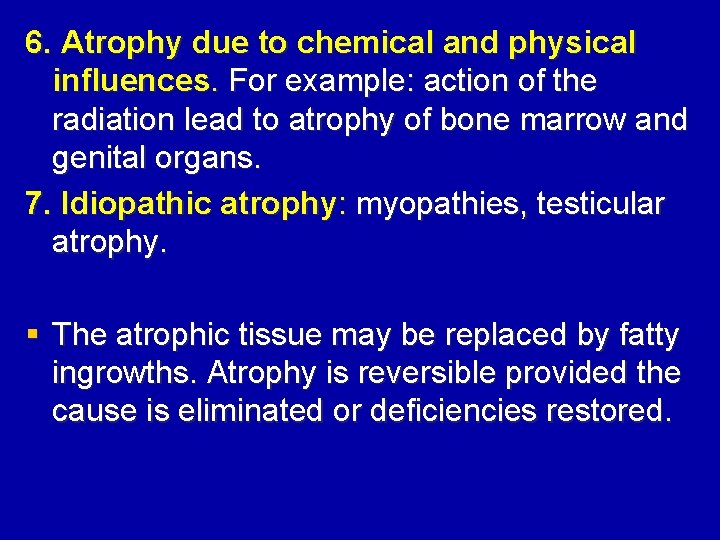
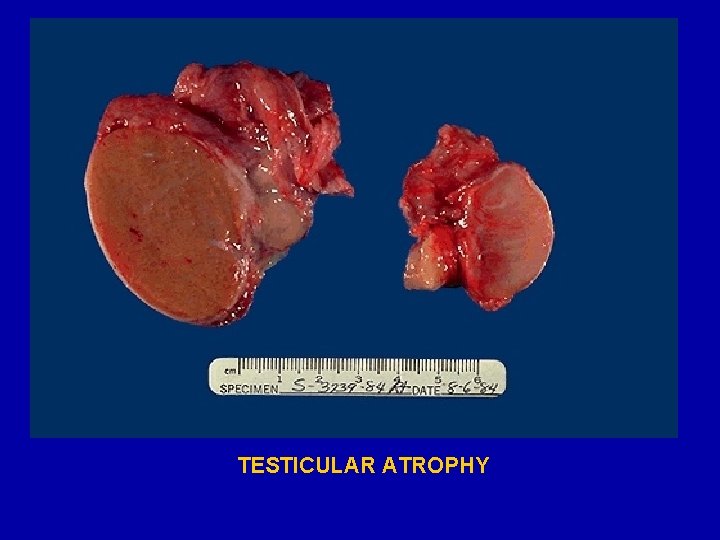
6. Atrophy due to chemical and physical influences. For example: action of the radiation lead to atrophy of bone marrow and genital organs. 7. Idiopathic atrophy: myopathies, testicular atrophy. § The atrophic tissue may be replaced by fatty ingrowths. Atrophy is reversible provided the cause is eliminated or deficiencies restored.
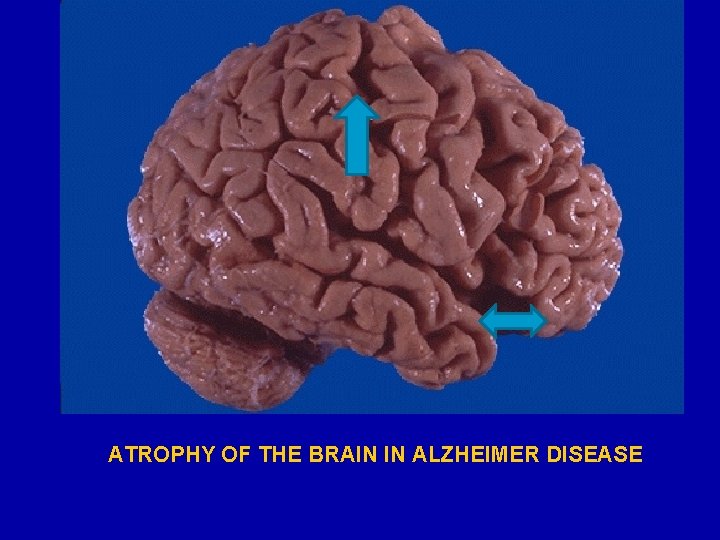
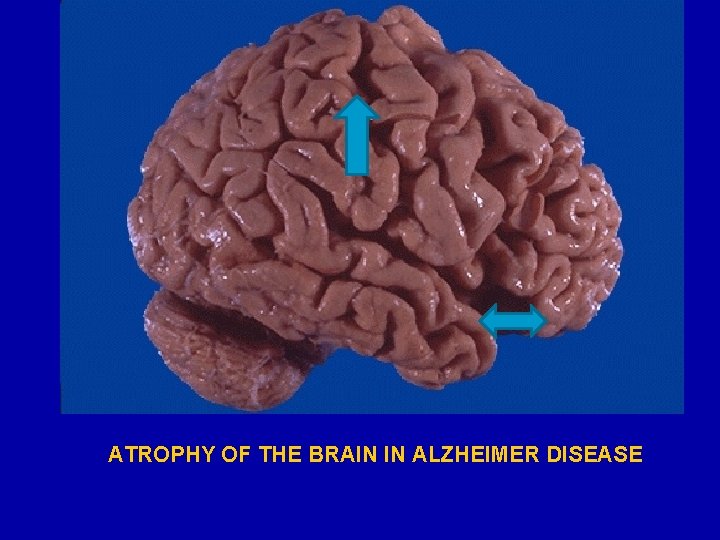
ATROPHY OF THE BRAIN IN ALZHEIMER DISEASE
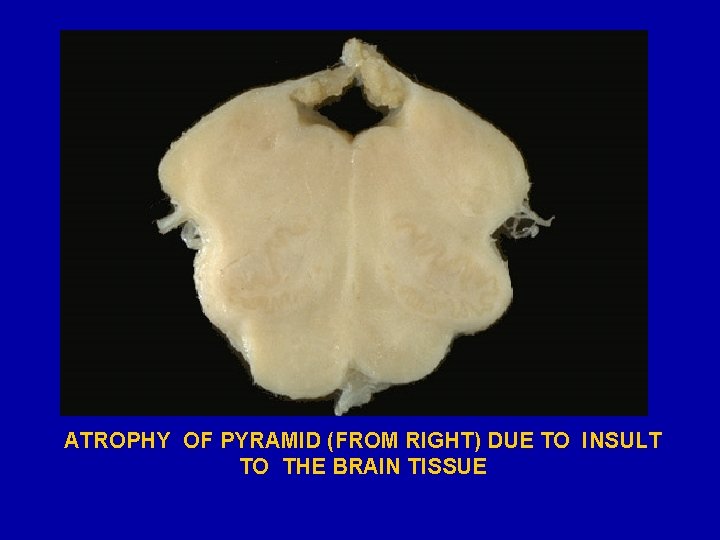
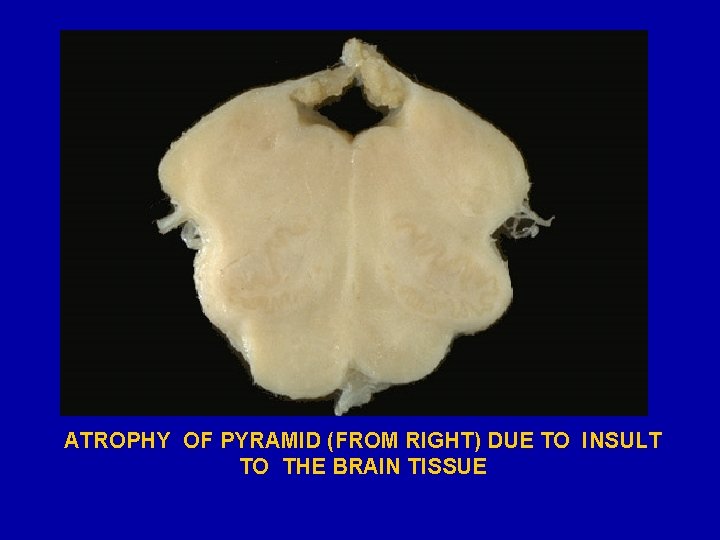
ATROPHY OF PYRAMID (FROM RIGHT) DUE TO INSULT TO THE BRAIN TISSUE
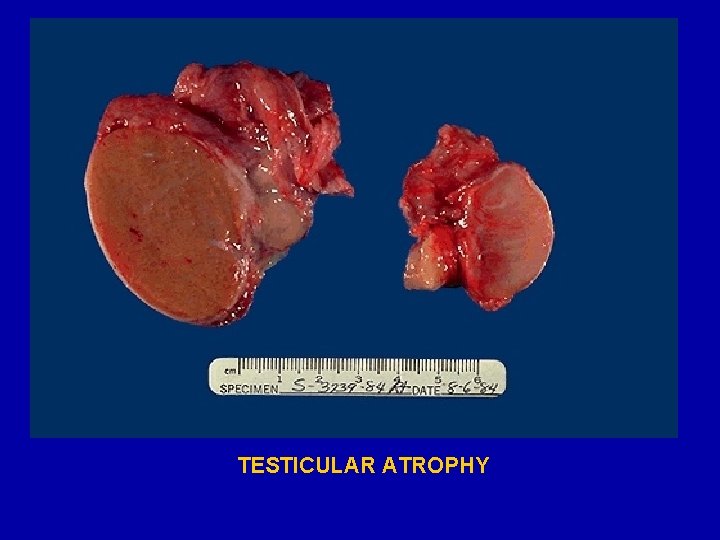
TESTICULAR ATROPHY

SKELETAL MUSCULAR FIBERS ATROPHY, (Threechrom staining)
Metaplasia § Metaplasia is defined as a reversible change of one type to another type of adult epithelial or mesenchymal cells, usually in response to abnormal stimuli (including inflammatory), and often reverts back to normal on removal of stimulus. Metaplasia is broadly divided into 2 types: A. Epithelial metaplasia. B. Mezenhymal metaplasia.
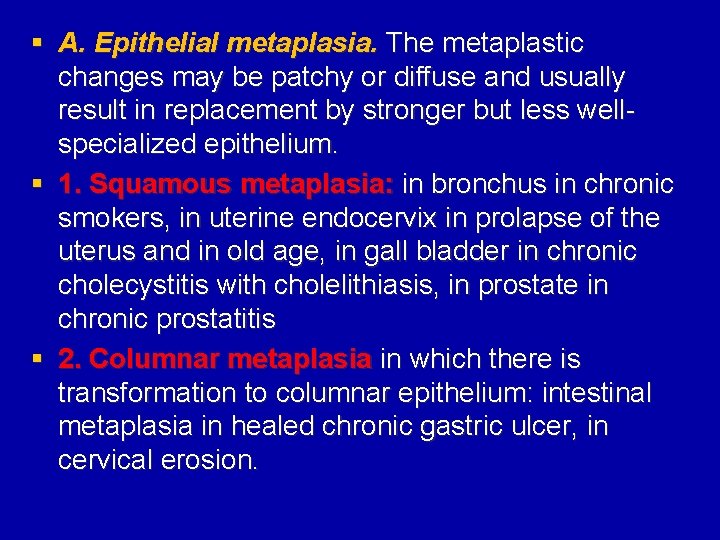
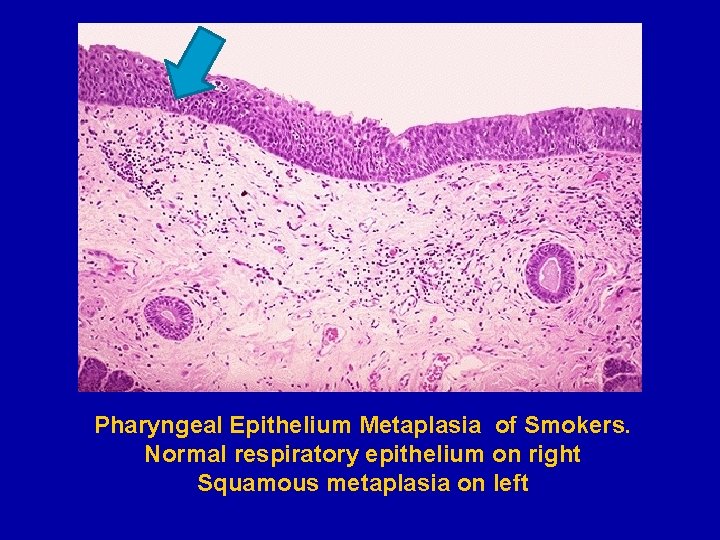
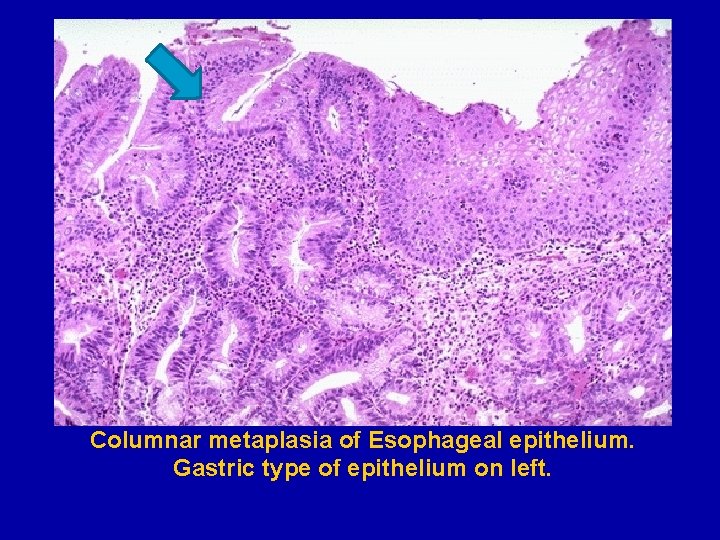
§ A. Epithelial metaplasia. The metaplastic changes may be patchy or diffuse and usually result in replacement by stronger but less wellspecialized epithelium. § 1. Squamous metaplasia: in bronchus in chronic smokers, in uterine endocervix in prolapse of the uterus and in old age, in gall bladder in chronic cholecystitis with cholelithiasis, in prostate in chronic prostatitis § 2. Columnar metaplasia in which there is transformation to columnar epithelium: intestinal metaplasia in healed chronic gastric ulcer, in cervical erosion.

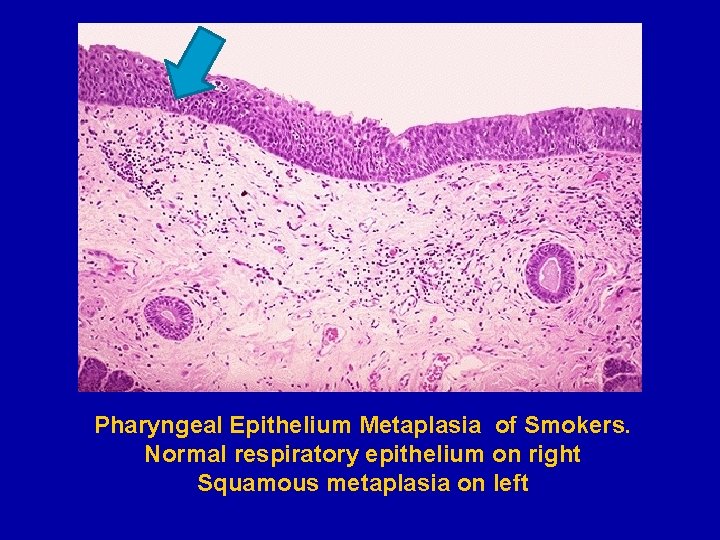
Pharyngeal Epithelium Metaplasia of Smokers. Normal respiratory epithelium on right Squamous metaplasia on left
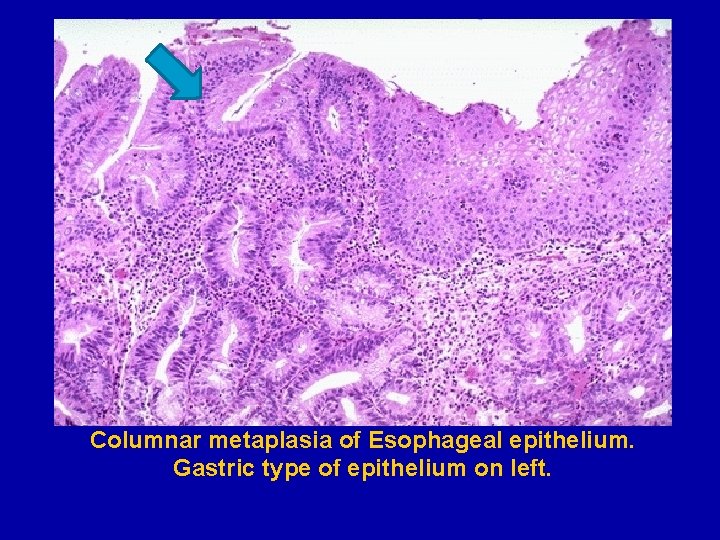
Columnar metaplasia of Esophageal epithelium. Gastric type of epithelium on left.

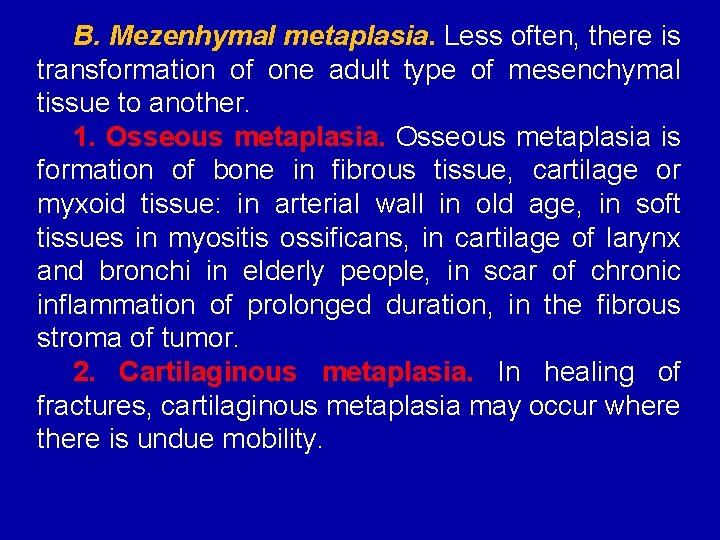
B. Mezenhymal metaplasia. Less often, there is transformation of one adult type of mesenchymal tissue to another. 1. Osseous metaplasia is formation of bone in fibrous tissue, cartilage or myxoid tissue: in arterial wall in old age, in soft tissues in myositis ossificans, in cartilage of larynx and bronchi in elderly people, in scar of chronic inflammation of prolonged duration, in the fibrous stroma of tumor. 2. Cartilaginous metaplasia. In healing of fractures, cartilaginous metaplasia may occur where there is undue mobility.

Dysplasia means “disordered cellular development”, often accompanied with metaplasia and hyperplasia, it is therefore also referred to as atypical hyperplasia. Epithelial dysplasia is characterized by atypical cellular proliferation and differentiation, accompanied by cytological changes, which are: ü Hyperplasia of epithelial layers. ü Disorderly arranged cells from basal layer to the surface layer (tissue atypia).
ü ü ü Cellular and nuclear pleomorphism. Increased nucleocytoplasmic ratios. Nuclear hyperchromatism. Increased mitotic activity. The two most common examples of dysplastic changes are the uterine cervix and respiratory tract.
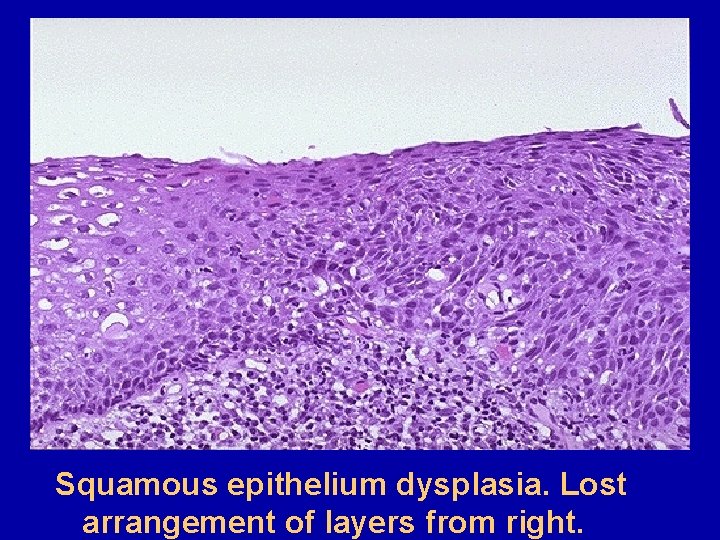
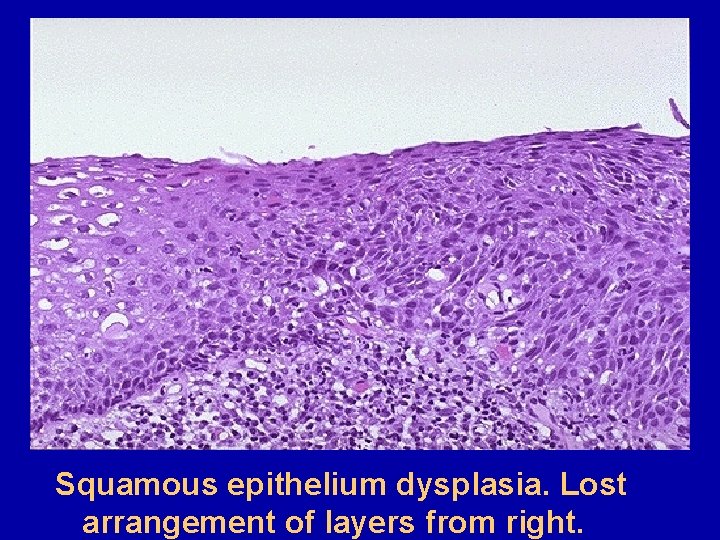
Squamous epithelium dysplasia. Lost arrangement of layers from right.
Healing It is the body response to injury in an attempt to restore normal structure and function. § Complete regeneration (restitution), denoting the replacement of injured cells by cells of the same type, sometimes leaving no residual trace of the previous injury, and § Incomplete regeneration (substitution) or replacement by connective tissue (fibroplasia), which leaves a permanent scar. In most instances, both processes contribute to repair. They are determined by mechanisms involving cell migration, proliferation, and differentiations, as well as cell-matrix interactions.
Depending upon their capacity to divide, the cells of the body can be divided into 3 groups: § Labile cells. These cells continue to multiply throughout life under normal physiologic conditions. (epidermis, alimentary tract, respiratory tract, hematopoietic cells of bone marrow, lymph nodes). § Stable cells. These cells decrease or lose their ability to proliferate after adolescence but retain the capacity to multiply in response to stimuli throughout adult life. (liver, pancreas, kidneys, smooth muscle cells, fibroblasts, endothelium, bone, cartilage cells. § Permanent cells. These cells lose their ability to proliferate around the time of birth. (Neurons of nervous system, skeletal muscle and cardiac muscle cells)
Forms: Ø Cellular: bones, epidermis, mucous membrane, connective tissue, endothelium, hemopoetic system, and limfoid tissue. Ø Intracellular: myocardium, skeletal muscles, ganglial cells and central nervous system (CNS). Ø Mixed: liver, kidneys, lungs, pancreas, endocrine organs, smooth muscles, vegetative nervous system (VNS).
Types: Ø Physiological regeneration is the process of replacement that occurs due to physiologic necrosis (erythrocytes, mucosa). Ø Reparative regeneration (complete, incomplete with regenerative hypertrophy) is the regeneration after some pathologic necrosis. Ø Pathologic regeneration is the slow (hyporegeneration) or pathologically absence one, hyperregeneration or metaplasia (change in cell type).
Repair is the replacement of injured tissue by fibrous tissue. Two processes are involved in repair: Ø 1. Granulation tissue formation. Ø 2. Contraction of wounds. • Repair response takes place by participation of mesenchymal cells (consisting of connective tissue stem cells, fibrocytes and histiocytes), endothelial cells, macrophages, platelets, and the parenchymal cells of the injured organ.
Granulation tissue formation 3 phases are observed in the formation of gr. t. Ø Phase of inflammation. There is acute inflammatory response with exudation of plasma, neutrophils and some monocytes within 24 hours. Ø Phase of clearance. Combination of proteolytic enzymes liberated from neutrophils, autolytic enzymes from dead tissues cells, and phagocytic activity of macrophages clear of the necrotic tissue, debris and red blood cells. Ø Phase of ingrowth of granulation tissue. This phase consists of 2 main processes: angiogenesis or neovascularisation and formation of fibrous tissue.
Angiogenesis (neovascularisation). § Formation of new blood vessels at the site of injury takes place by proliferation of endothelial cells from the margins of severed blood vessels. The process of angiogenesis takes place under the influence of the following: § Endothelial cell growth factors. § Some components of matrix like type IV collagen.
Fibrous tissue formation. § The new fibrocytes originate from fibroblasts as well as by mitotic division of fibroblasts. Some of these fibroblasts have morphologic and functional characteristics of smooth muscle cells (myofibroblasts). Collagen fibrils begin to appear by about 6 th day. As maturation proceeds, more and more of collagen is formed while the number of active fibroblasts and new blood vessels decreases. This results in formation of inactive looking scar known as cicatrisation.
Contraction of wounds The wound starts contracting after 2 -3 days and the process is completed by the 14 th day. In order to explain the mechanism of wound contraction, a number of factors have been proposed: Ø Dehydration as a result of removal of fluid. Ø Contraction of collagen. Ø Discovery of myofibroblasts.
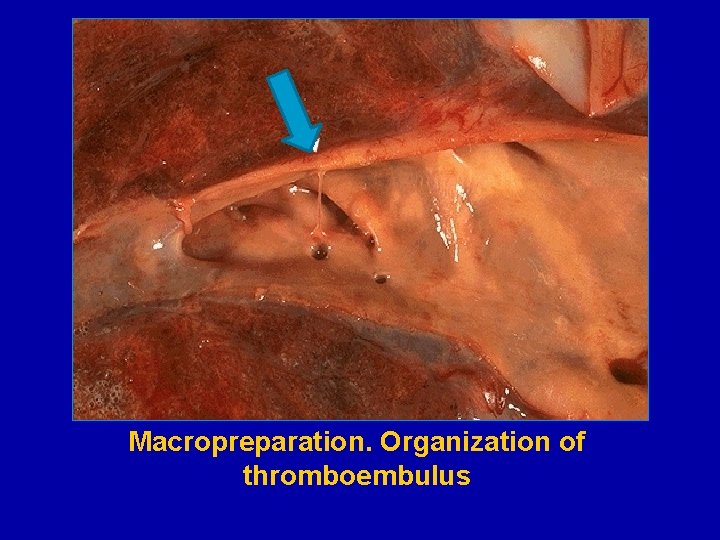
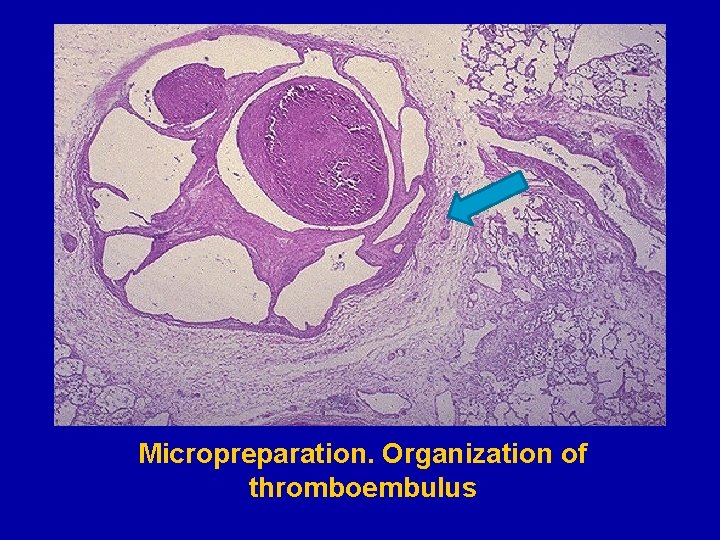
Organization Ø Organization is replacement of necrotic areas, thrombi et. c. by connective tissue or encapsulation. Ø Organization is bound with inflammation and regeneration.
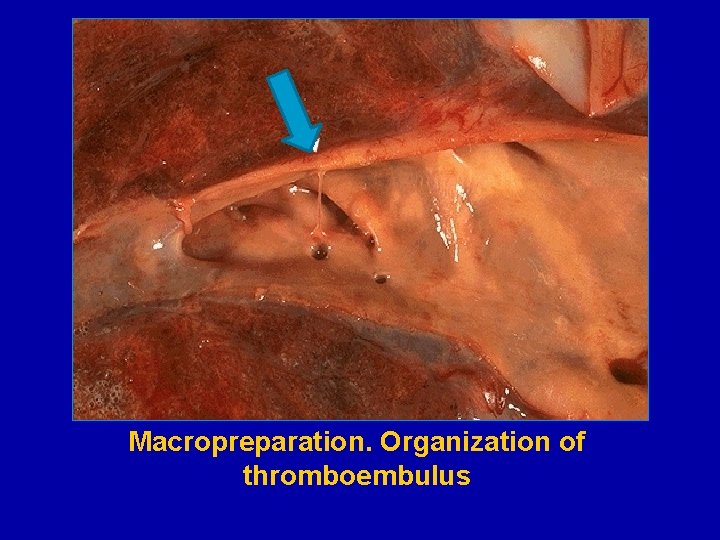
Macropreparation. Organization of thromboembulus
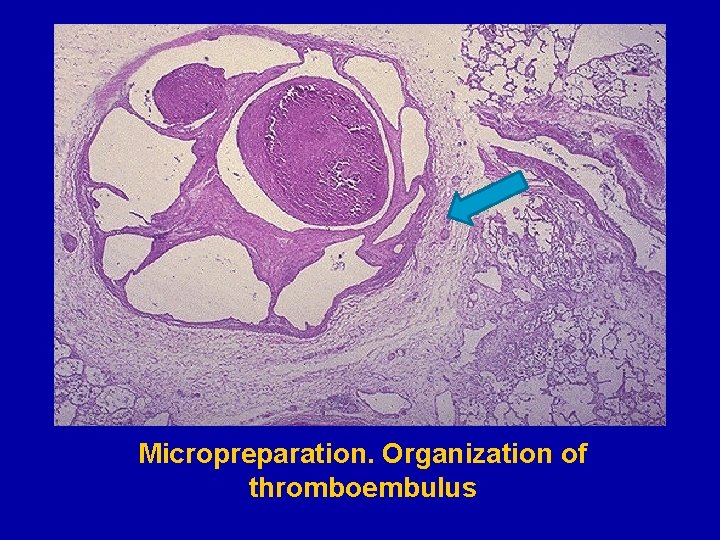
Micropreparation. Organization of thromboembulus
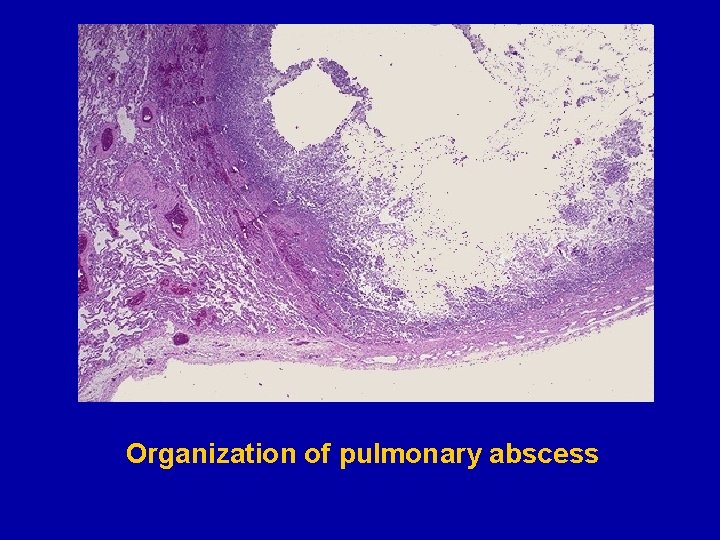
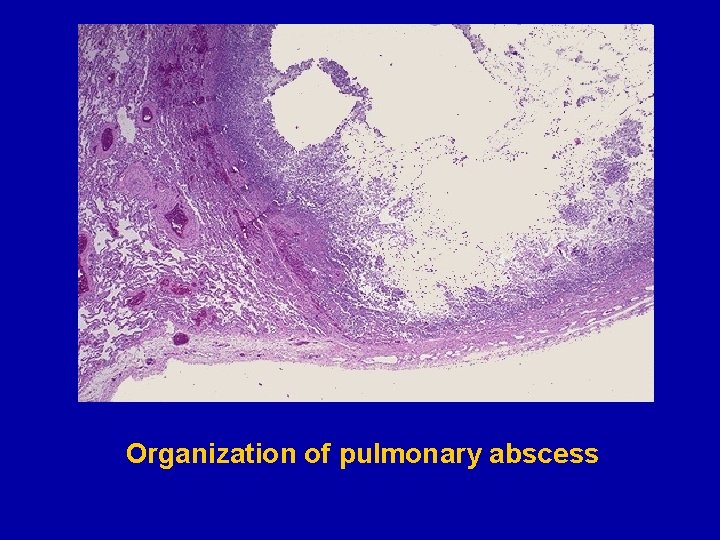
Organization of pulmonary abscess
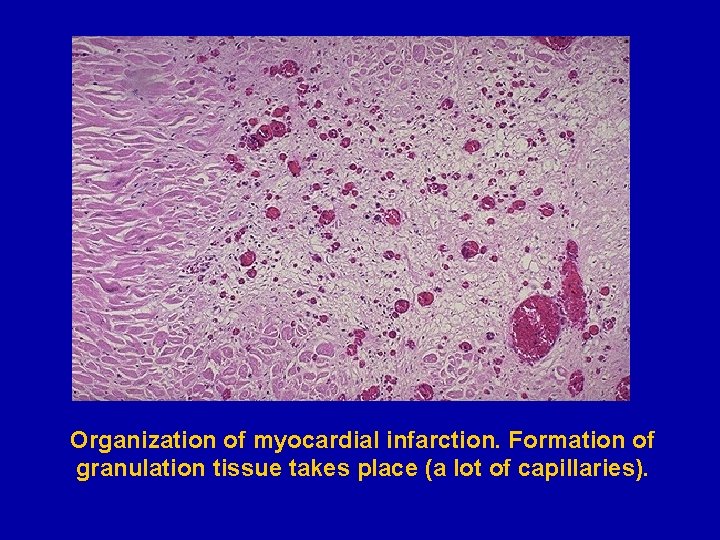
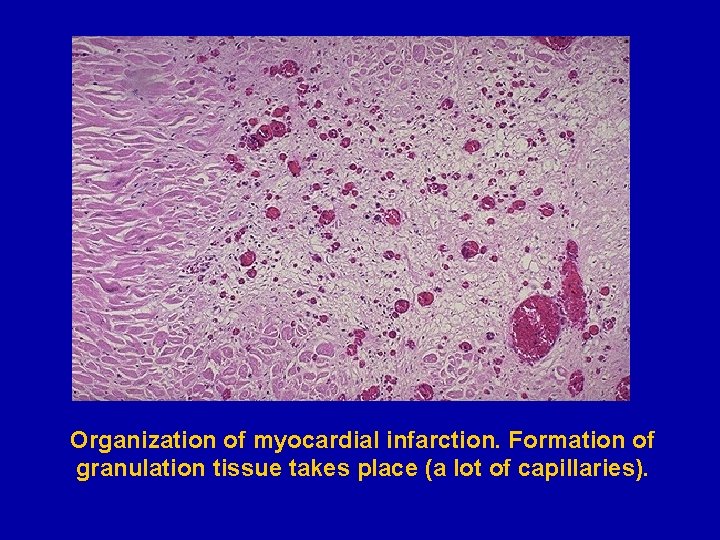
Organization of myocardial infarction. Formation of granulation tissue takes place (a lot of capillaries).

Complications of Wound Healing § Infection. § Implantation (epidermal) cyst. § Pigmentation. § Deficient scar formation. § Incisional hernia. § Hypertrophied scars and keloid formation. § Excessive contraction. § Neoplasia. § Hematological abnormalities.

Thanks for your attention TAKE CARE
 Odessa state environmental university
Odessa state environmental university Odessa state environmental university
Odessa state environmental university Coastal plains of texas major cities
Coastal plains of texas major cities Oc techs
Oc techs Coding bootcamps odessa
Coding bootcamps odessa Kiev odessa
Kiev odessa Brenntag lachine
Brenntag lachine Jobsindice.com odessa tx
Jobsindice.com odessa tx Odessa commercial sea port
Odessa commercial sea port M.gorky donetsk national medical university
M.gorky donetsk national medical university Seoul national university college of medicine
Seoul national university college of medicine Mongolian national university of medical sciences
Mongolian national university of medical sciences Medical education and drugs department
Medical education and drugs department What is a national risk ambulance
What is a national risk ambulance Difference between medical report and medical certificate
Difference between medical report and medical certificate Importance of medical records
Importance of medical records Hymen
Hymen Six quality priorities in health
Six quality priorities in health National audit department
National audit department Ibn sina university of medical and pharmaceutical sciences
Ibn sina university of medical and pharmaceutical sciences National unification and the national state
National unification and the national state Department of law university of jammu
Department of law university of jammu Department of geology university of dhaka
Department of geology university of dhaka University of padova psychology department
University of padova psychology department University of bridgeport it department
University of bridgeport it department University of iowa math
University of iowa math Sputonik v
Sputonik v Texas state psychology program
Texas state psychology program Department of information engineering university of padova
Department of information engineering university of padova Information engineering padova
Information engineering padova Manipal university chemistry department
Manipal university chemistry department Syracuse university psychology department
Syracuse university psychology department Jackson state university finance department
Jackson state university finance department Computer science department columbia
Computer science department columbia Michigan state physics
Michigan state physics Columbia university cs department
Columbia university cs department University of sargodha engineering department
University of sargodha engineering department Claudia arrighi
Claudia arrighi Prerequisites of gait
Prerequisites of gait Prerequisites of gait
Prerequisites of gait Erect position in medicine
Erect position in medicine Kyiv national university of culture and arts
Kyiv national university of culture and arts National and kapodistrian university of athens events
National and kapodistrian university of athens events National yunlin university of science and technology
National yunlin university of science and technology California medical license application
California medical license application Greater baltimore medical center medical records
Greater baltimore medical center medical records Torrance memorial hospital medical records
Torrance memorial hospital medical records Cartersville medical center medical records
Cartersville medical center medical records National board of medical interpreters
National board of medical interpreters National ambulatory medical care survey
National ambulatory medical care survey Abu ali sina university peshawar
Abu ali sina university peshawar Ivf maribor
Ivf maribor Liaoning medical university
Liaoning medical university Vietnam military medical university
Vietnam military medical university Ascaris lumbricoides ova
Ascaris lumbricoides ova Kirovohrad medical university
Kirovohrad medical university University of maryland capital region health
University of maryland capital region health Stavropol state medical university
Stavropol state medical university Empp university medical center
Empp university medical center David tvildiani medical university
David tvildiani medical university Maribor gluten free
Maribor gluten free Columbia university medical center
Columbia university medical center Columbia university medical center
Columbia university medical center Padua university medical school
Padua university medical school Kaohsiung medical university hospital
Kaohsiung medical university hospital Medical university of lublin
Medical university of lublin Osh state medical university logo
Osh state medical university logo Hawler medical university college of nursing
Hawler medical university college of nursing Hawler medical university college of nursing
Hawler medical university college of nursing Marija molan
Marija molan Uq som
Uq som Palm harbor university high school medical program
Palm harbor university high school medical program Chronic meningitis
Chronic meningitis Chernivtsi national university
Chernivtsi national university National university of tainan
National university of tainan Lvivtech city
Lvivtech city