Non Cardiac Chest pain Prof Dr Yaar Kkardal








- Slides: 42
Non- Cardiac Chest pain Prof. Dr Yaşar Küçükardalı İç Hastalıkları ve Yoğun Bakım Uzmanı
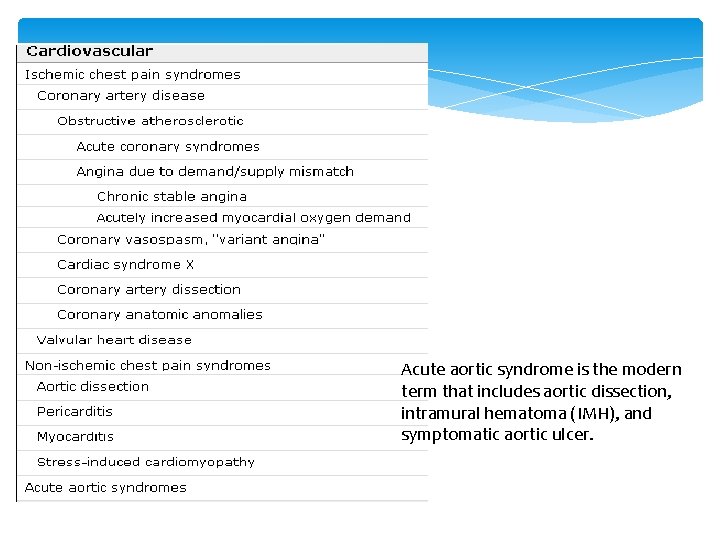
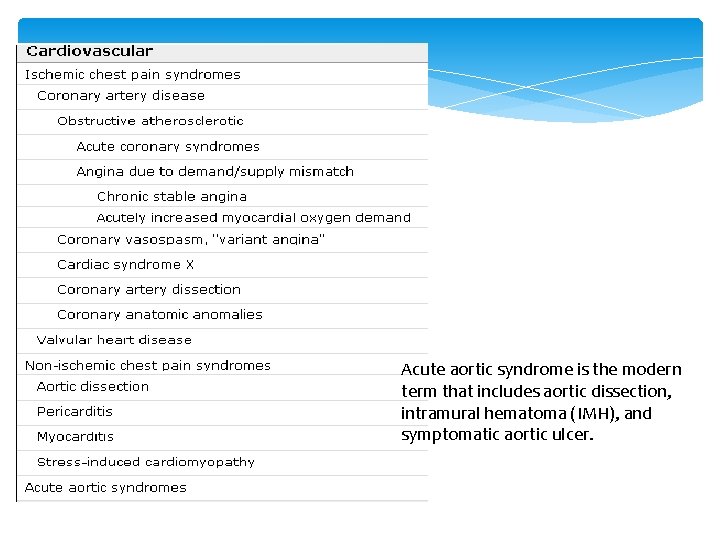
Acute aortic syndrome is the modern term that includes aortic dissection, intramural hematoma (IMH), and symptomatic aortic ulcer.
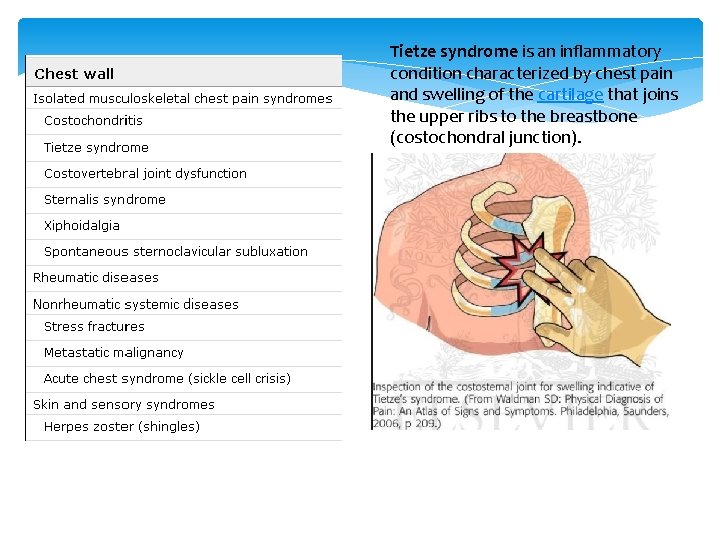
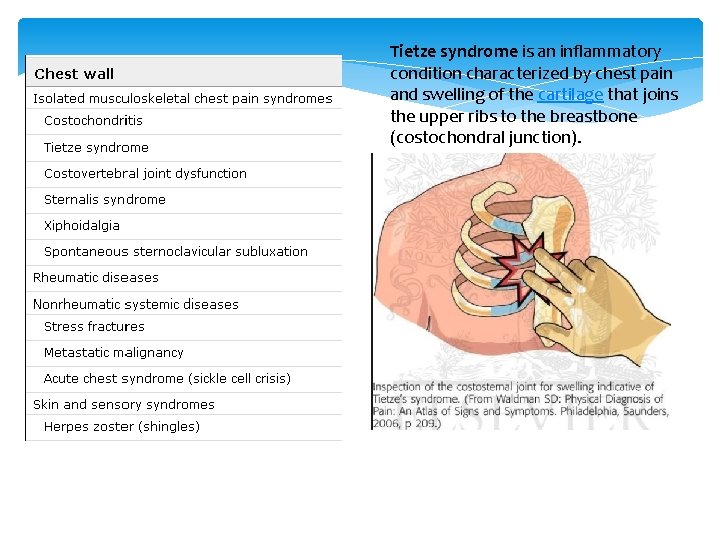
Tietze syndrome is an inflammatory condition characterized by chest pain and swelling of the cartilage that joins the upper ribs to the breastbone (costochondral junction).
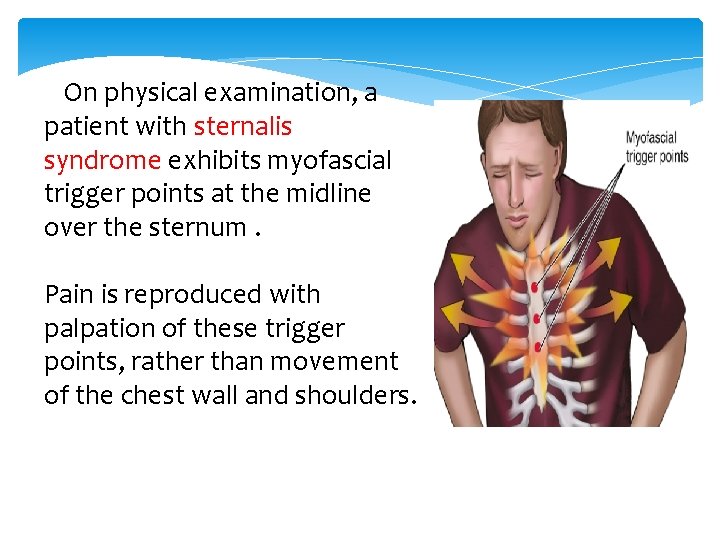
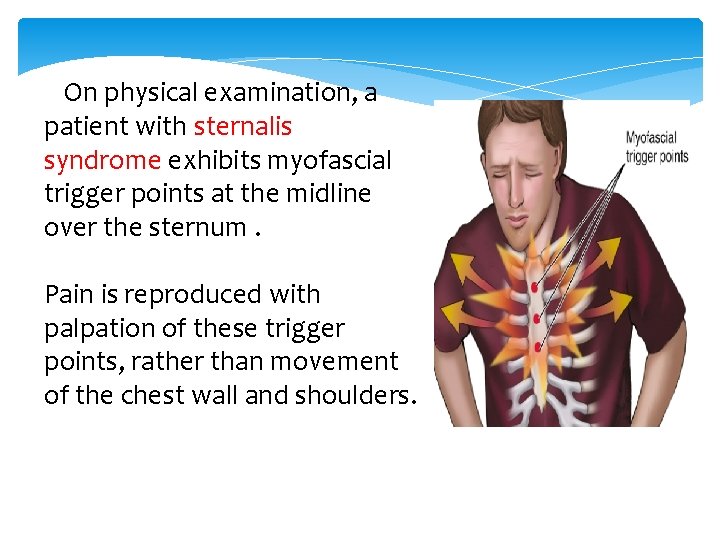
On physical examination, a patient with sternalis syndrome exhibits myofascial trigger points at the midline over the sternum. Pain is reproduced with palpation of these trigger points, rather than movement of the chest wall and shoulders.


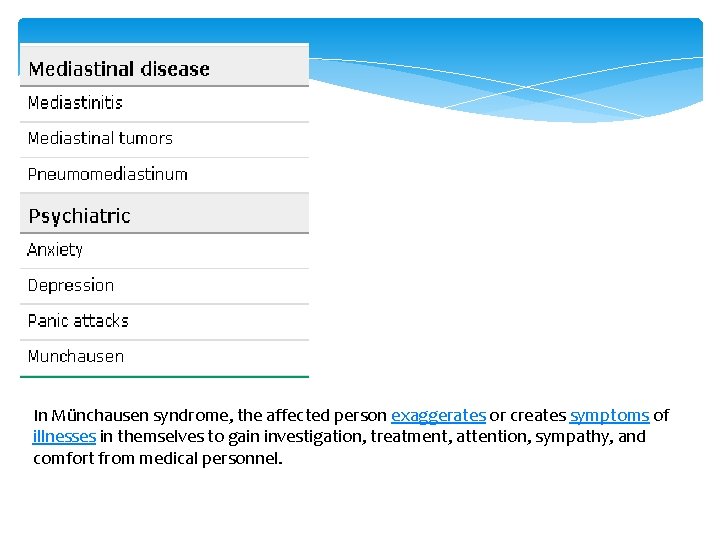
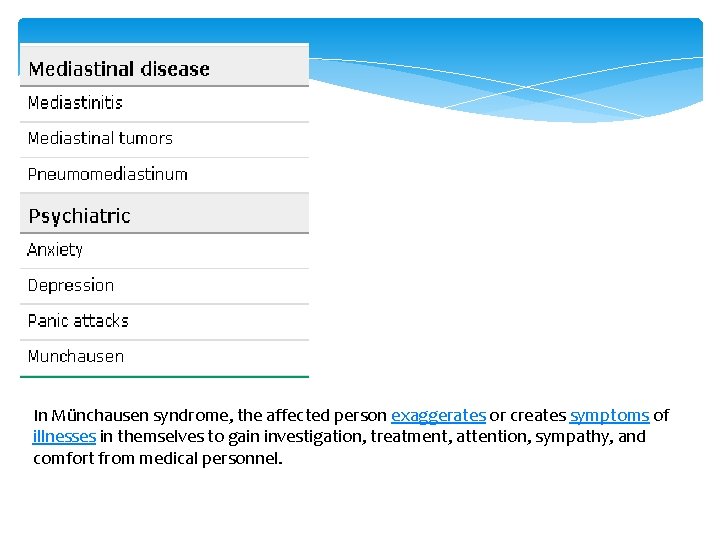
In Münchausen syndrome, the affected person exaggerates or creates symptoms of illnesses in themselves to gain investigation, treatment, attention, sympathy, and comfort from medical personnel.


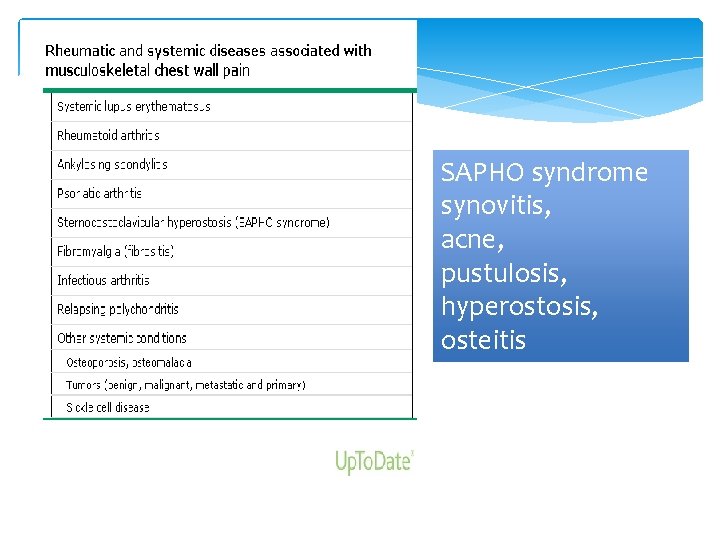
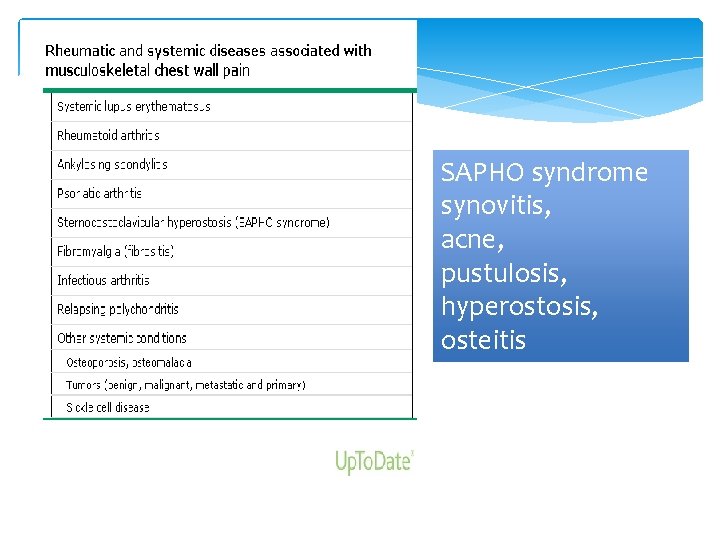
SAPHO syndrome synovitis, acne, pustulosis, hyperostosis, osteitis
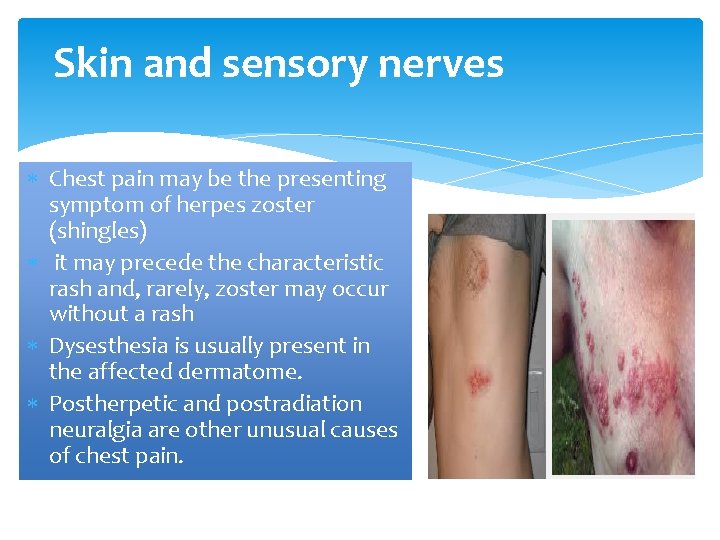
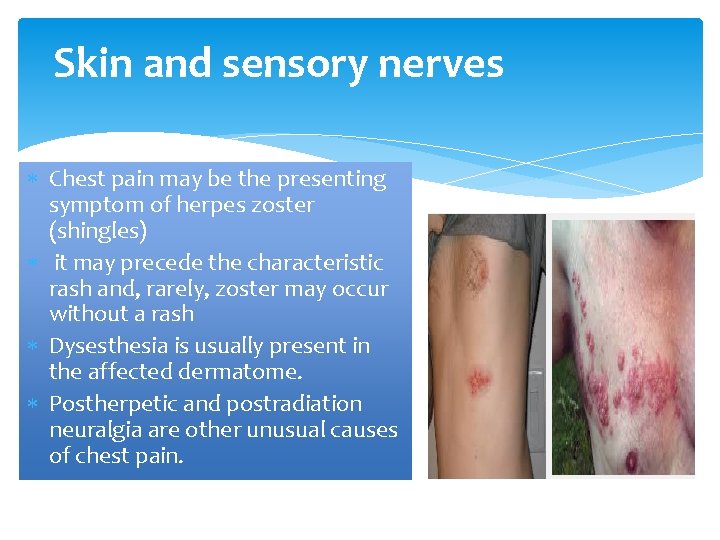
Skin and sensory nerves Chest pain may be the presenting symptom of herpes zoster (shingles) it may precede the characteristic rash and, rarely, zoster may occur without a rash Dysesthesia is usually present in the affected dermatome. Postherpetic and postradiation neuralgia are other unusual causes of chest pain.
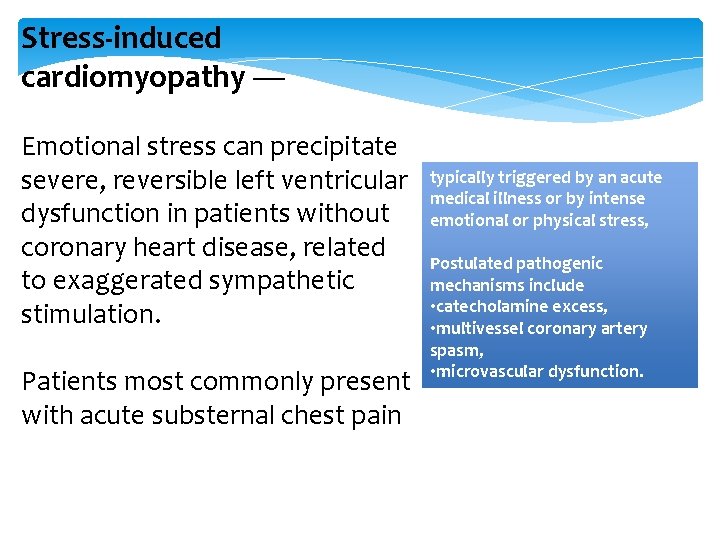
Stress-induced cardiomyopathy — Emotional stress can precipitate severe, reversible left ventricular dysfunction in patients without coronary heart disease, related to exaggerated sympathetic stimulation. Patients most commonly present with acute substernal chest pain typically triggered by an acute medical illness or by intense emotional or physical stress, Postulated pathogenic mechanisms include • catecholamine excess, • multivessel coronary artery spasm, • microvascular dysfunction.

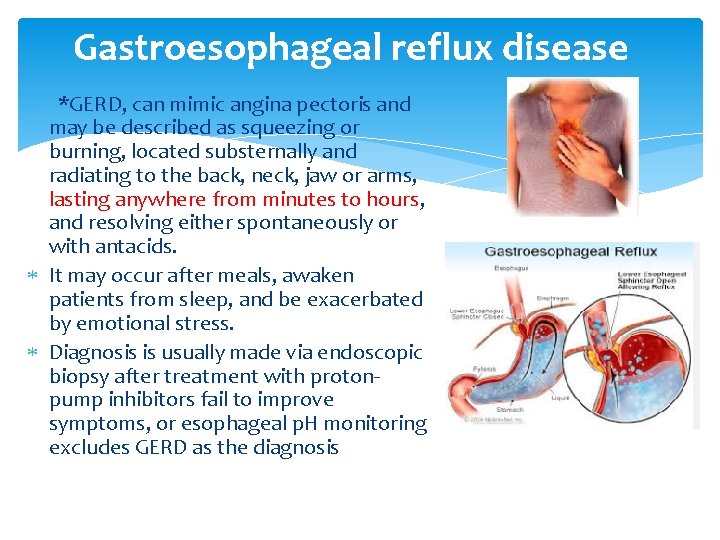
Gastroesophageal reflux disease *GERD, can mimic angina pectoris and may be described as squeezing or burning, located substernally and radiating to the back, neck, jaw or arms, lasting anywhere from minutes to hours, and resolving either spontaneously or with antacids. It may occur after meals, awaken patients from sleep, and be exacerbated by emotional stress. Diagnosis is usually made via endoscopic biopsy after treatment with protonpump inhibitors fail to improve symptoms, or esophageal p. H monitoring excludes GERD as the diagnosis
Esophageal hypersensitivity There are considerable experimental data to indicate that some patients with chest pain have a lower threshold for esophageal pain than normal subjects. Studies utilizing intraesophageal balloon distension have shown that many patients with unexplained chest pain experience their pain at a lower volume of balloon inflation that found in appropriate control subjects
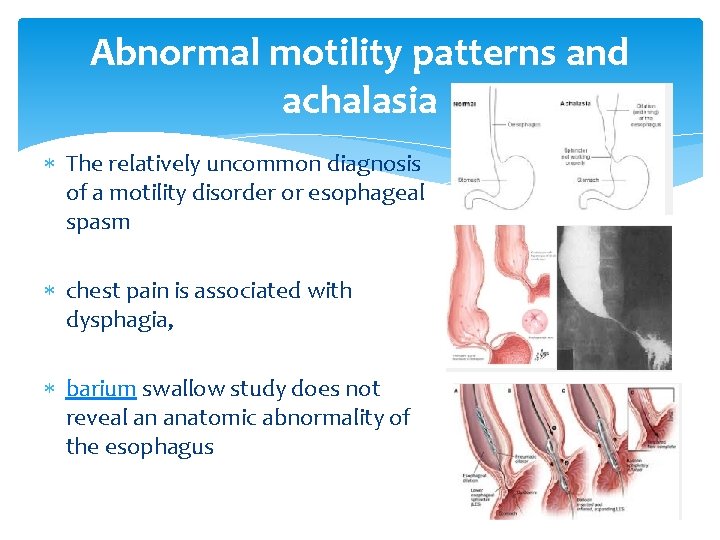
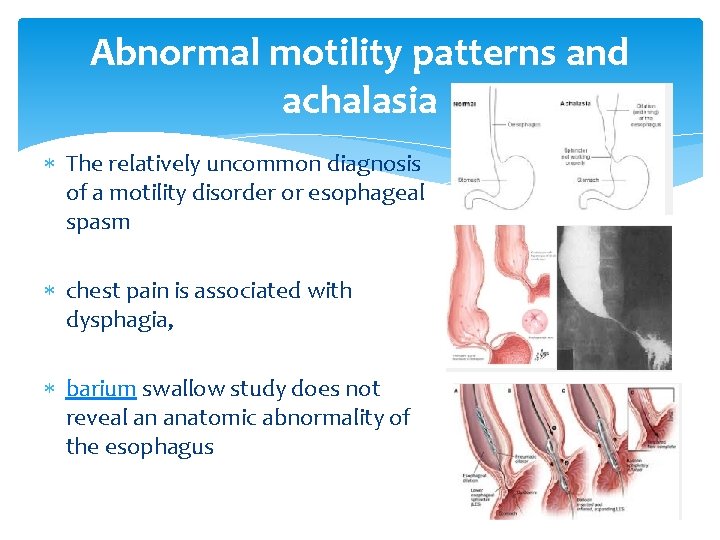
Abnormal motility patterns and achalasia The relatively uncommon diagnosis of a motility disorder or esophageal spasm chest pain is associated with dysphagia, barium swallow study does not reveal an anatomic abnormality of the esophagus
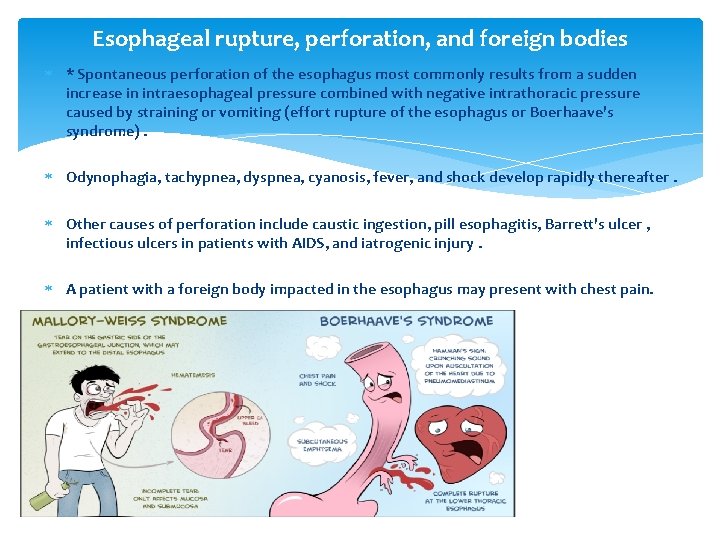
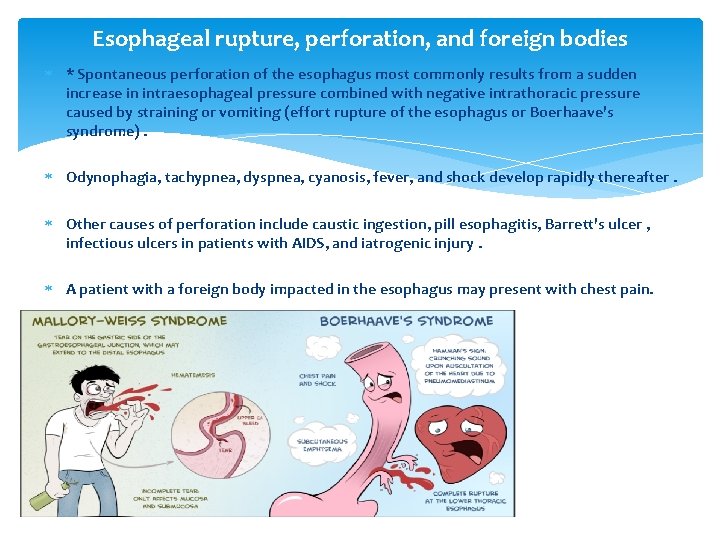
Esophageal rupture, perforation, and foreign bodies * Spontaneous perforation of the esophagus most commonly results from a sudden increase in intraesophageal pressure combined with negative intrathoracic pressure caused by straining or vomiting (effort rupture of the esophagus or Boerhaave's syndrome). Odynophagia, tachypnea, dyspnea, cyanosis, fever, and shock develop rapidly thereafter. Other causes of perforation include caustic ingestion, pill esophagitis, Barrett's ulcer , infectious ulcers in patients with AIDS, and iatrogenic injury. A patient with a foreign body impacted in the esophagus may present with chest pain.
Other causes of esophagitis The types of medication causing direct esophageal injury can be roughly divided into antibiotics (most commonly tetracyclines and clindamycin), antiinflammatory agents (especially aspirin), bisphonates potassium chloride, quinidine preparations, and iron compounds Esophagitis may also be due to infectious causes, including esophageal candidiasis or CMV esophagitis, particularly in immunocompromised hosts due to AIDS or stem-cell transplant patients. Radiation injury may also induce esophagitis.
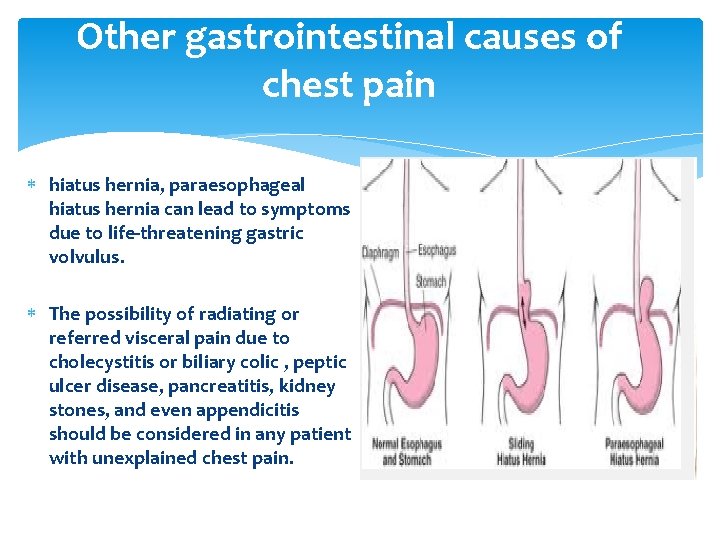
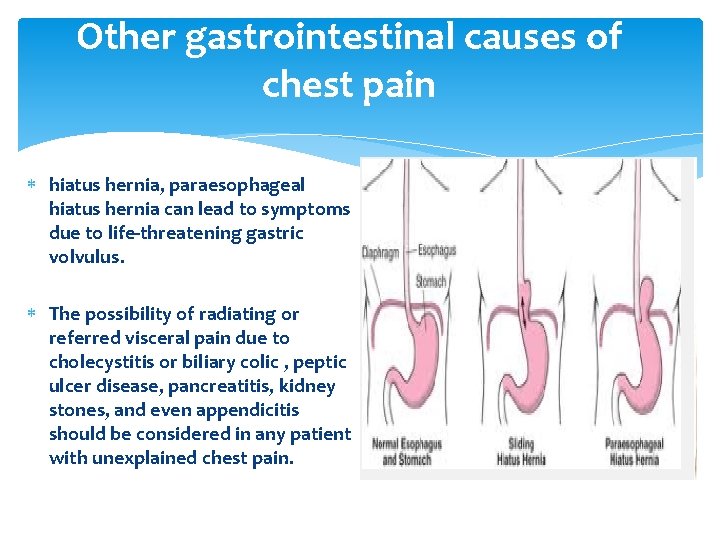
Other gastrointestinal causes of chest pain hiatus hernia, paraesophageal hiatus hernia can lead to symptoms due to life-threatening gastric volvulus. The possibility of radiating or referred visceral pain due to cholecystitis or biliary colic , peptic ulcer disease, pancreatitis, kidney stones, and even appendicitis should be considered in any patient with unexplained chest pain.
Acute pulmonary embolism It should be considered in any patient who presents with chest pain Individual symptoms and signs are not helpful diagnostically The most common symptoms of pulmonary embolism were dyspnea (73 percent), pleuritic chest pain (66 percent), cough (37 percent), and hemoptysis (13 percent). 90 percent had dyspnea, tachypnea, or signs of deep venous thrombosis; 84 percent had a chest x-ray abnormality; 50 percent had nonspecific electrocardiographic abnormalities.

Pulmonary hypertension (PH) and cor pulmonale Patients with secondary PH often have symptoms that reflect the underlying etiology (eg, chronic obstructive pulmonary disease, pulmonary embolic disease, collagen vascular disease). There are, however, symptoms directly attributable to secondary PH including dyspnea on exertion, fatigue, lethargy, chest pain, and syncope with exertion. Idiopathic PH is a rare disease. Most patients present with exertional dyspnea, which is indicative of an inability to increase cardiac output with exercise. Exertional chest pain, syncope, and edema are indications of more severe PH and impaired right heart function
Pneumonia The patient with community acquired pneumonia (CAP) caused by pyogenic organisms classically presents with the sudden onset of rigors followed by fever, pleuritic chest pain, and cough productive of purulent sputum. Chest pain occurs in 30 percent of cases, chills in 40 to 50 percent, and rigors in 15 percent. Because of the rapid onset of symptoms, most individuals seek medical care within six days
Cancer Isolated chest pain is a relatively rare presentation of lung cancer. The chest pain experienced by 25 to 50 percent of lung cancer patients is usually in association with cough, dyspnea, weight loss, or hemoptysis. Some patients have a dull, intermittent pain on the side of the tumor; severe or persistent pain often indicates chest wall or mediastinal invasion.
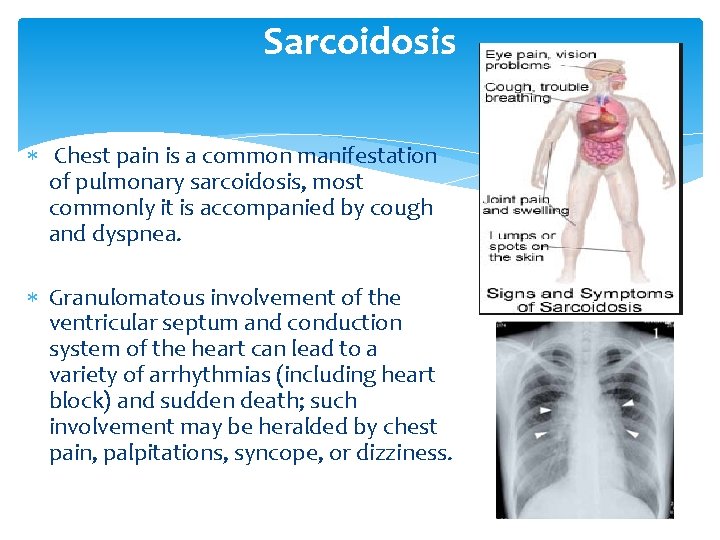
Sarcoidosis Chest pain is a common manifestation of pulmonary sarcoidosis, most commonly it is accompanied by cough and dyspnea. Granulomatous involvement of the ventricular septum and conduction system of the heart can lead to a variety of arrhythmias (including heart block) and sudden death; such involvement may be heralded by chest pain, palpitations, syncope, or dizziness.
Asthma and COPD Diseases of the bronchial airways such as asthma and COPD may present with chest pain. both characterized by airway inflammation and bronchospasm. Chest pain is common in asthma exacerbations, 76 percent asthma and COPD exacerbations often have triggers (such as pneumonia or pulmonary embolism) that may actually be the cause of chest pain.
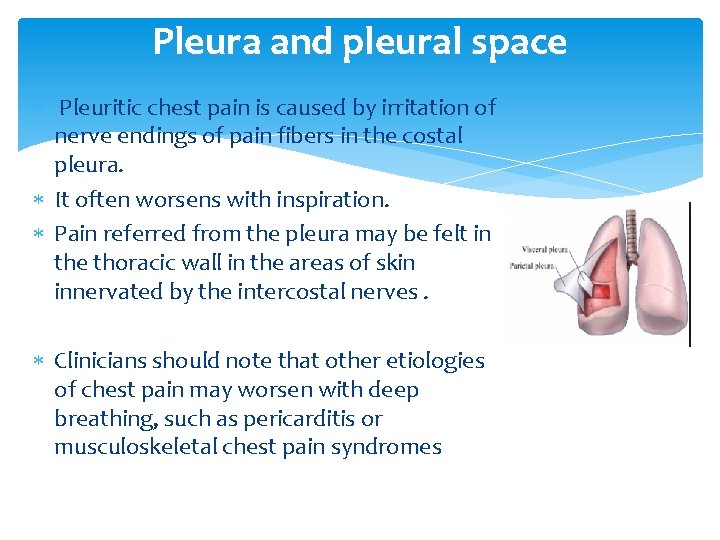
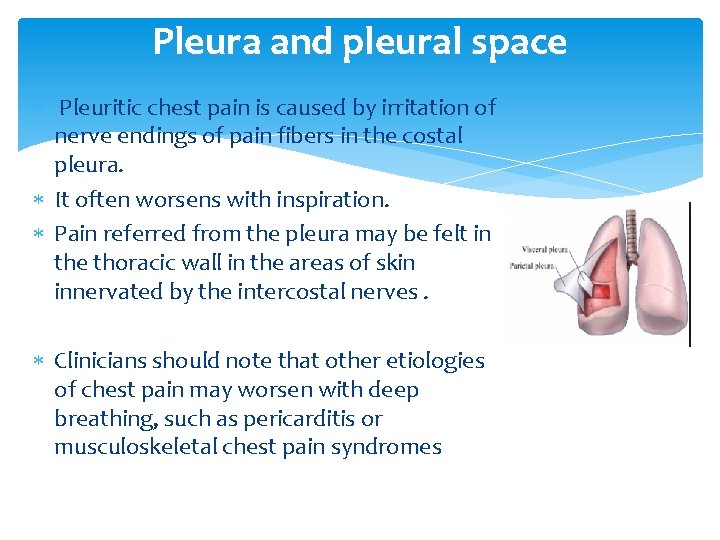
Pleura and pleural space Pleuritic chest pain is caused by irritation of nerve endings of pain fibers in the costal pleura. It often worsens with inspiration. Pain referred from the pleura may be felt in the thoracic wall in the areas of skin innervated by the intercostal nerves. Clinicians should note that other etiologies of chest pain may worsen with deep breathing, such as pericarditis or musculoskeletal chest pain syndromes

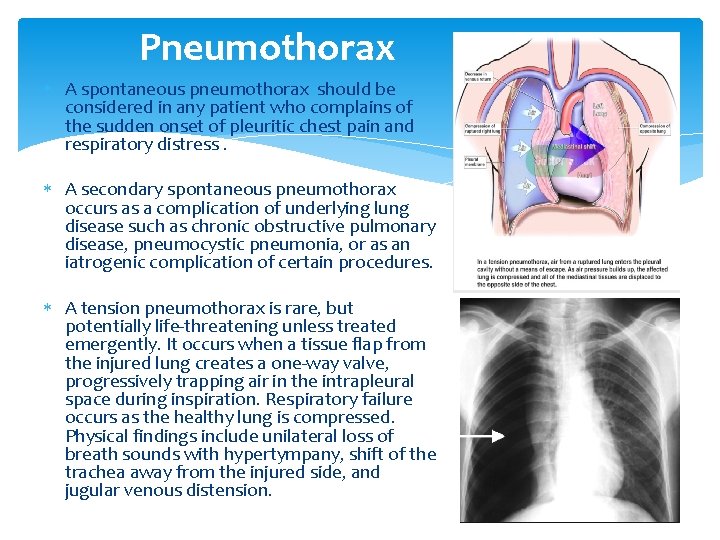
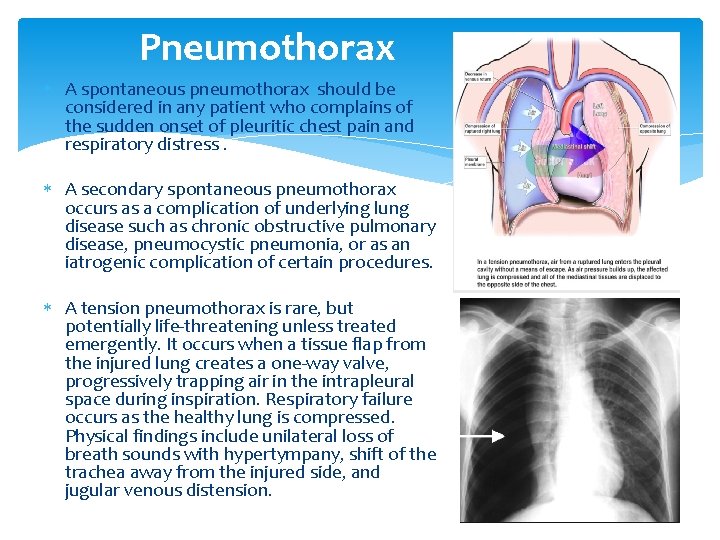
Pneumothorax A spontaneous pneumothorax should be considered in any patient who complains of the sudden onset of pleuritic chest pain and respiratory distress. A secondary spontaneous pneumothorax occurs as a complication of underlying lung disease such as chronic obstructive pulmonary disease, pneumocystic pneumonia, or as an iatrogenic complication of certain procedures. A tension pneumothorax is rare, but potentially life-threatening unless treated emergently. It occurs when a tissue flap from the injured lung creates a one-way valve, progressively trapping air in the intrapleural space during inspiration. Respiratory failure occurs as the healthy lung is compressed. Physical findings include unilateral loss of breath sounds with hypertympany, shift of the trachea away from the injured side, and jugular venous distension.
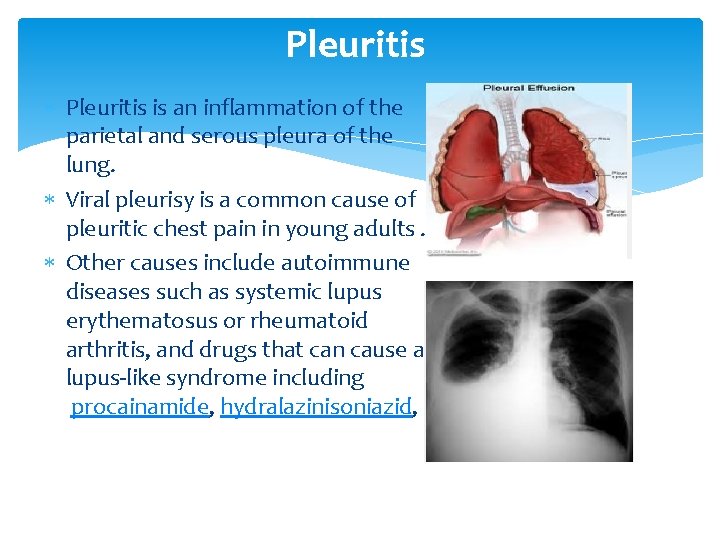
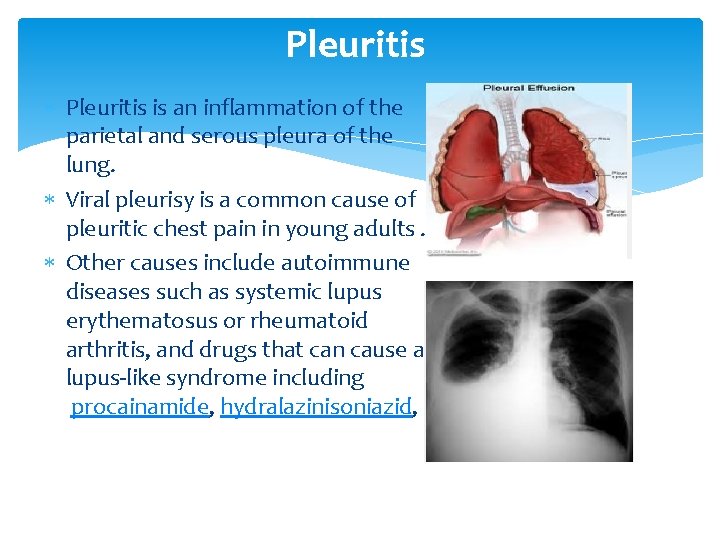
Pleuritis is an inflammation of the parietal and serous pleura of the lung. Viral pleurisy is a common cause of pleuritic chest pain in young adults. Other causes include autoimmune diseases such as systemic lupus erythematosus or rheumatoid arthritis, and drugs that can cause a lupus-like syndrome including procainamide, hydralazinisoniazid,
MEDIASTINAL CAUSES OF CHEST PAIN Disease originating in the mediastinum is a rare cause of chest pain in primary care practice, but may be seen in other settings. Mediastinitis may result from esophageal rupture such as in effort rupture of the esophagus or postoperatively as a complication of cardiac surgery. Spontaneous pneumomediastinum is a rare entity that commonly presents with chest pain
PSYCHOGENIC/PSYCHOSOMATIC CAUSES OF CHEST PAIN Chest pain may be a presenting symptom of panic disorder, depression, and hypochondriasis, as well as cardiac, cancer, or other phobias Reviews of the literature have estimated that approximately one-third of patients presenting to the emergency department for chest pain have a psychiatric disorder, while approximately one-half of patients with noncardiac chest pain have various psychiatric diagnoses. Among patients with chest pain due to coronary artery disease (CAD), 20 to 30 percent also have a coexisting psychiatric disorder. Hyperventilation, which is associated with panic attacks, can also result in nonanginal chest pain and occasionally electrocardiographic changes, particularly nonspecific ST and T wave abnormalities.
Panic disorder is a particularly common cause of chest pain found that 20 percent had panic disorder as the etiology. Vigilance is necessary since patients with psychiatric disorders may develop organic disease In addition, ischemia may occur during a panic attack in a patient with CAD. Thus organic disease must be reasonably excluded before ascribing chest pain to a nonorganic origin.
Munchausen syndrome In one literature review, 58 patients with cardiac Munchausen syndrome were identified. Of these, 54 (95 percent) were male; the mean age was 44 years (range, 23 to 71). The most common presenting symptom was retrosternal chest pain (50 patients); other presenting complaints were syncope, dyspnea, and back pain. Patients typically gave a history of prior cardiac disease and often reported having "white collar" jobs; Acute myocardial infarction was the most common admitting diagnosis. All subjects had numerous admissions and extensive cardiac testing, which were negative for cardiac disease but which the patients reported were positive. When confronted, most patients changed their history, became uncooperative, and refused psychiatric examination.
PAIN REFERRED TO THE CHEST Referred pain may occur when the same spinal cord segments supplying dermatomal areas of the chest wall also innervate the very sensitive parietal pleura or peritoneum. As an example, irritation of the mediastinal pleura or of the central diaphragm due to gallbladder or liver disease may result in neck and shoulder pain, while more peripheral diaphragmatic irritation may result in inferior chest pain. A herniated thoracic disc may cause "band-like" anterior chest pain
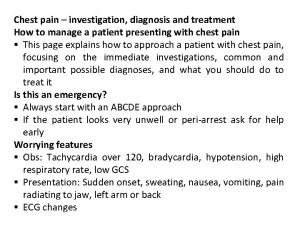
Diagnostic algorithm Step 1 The initial step : a focused history and physical examination, and consider performing an ECG and/or chest x-ray. Once a lifethreatening etiology has been excluded, attempts should be made to identify the specific cause of symptoms and begin treatment. (Evaluate need for emergent care) — Consider potentially lifethreatening causes of chest pain. Patients in whom an acute coronary syndrome (acute myocardial infarction or unstable angina) is suspected should receive emergent care (this generally includes chewing an aspirin while awaiting transport to an emergency department, ideally via an ambulance equipped with a defibrillator). Emergent care should also be provided to patients who appear to be seriously ill and to patients in whom there is a suspicion of a critical noncoronary diagnosis such as pulmonary embolus, pneumothorax, aortic dissection, esophageal rupture, or acute abdomen.
Step 2 Evaluate the patient for gastrointestinal disease. This evaluation may initially involve a trial of acid suppression.

Step 3 (Symptoms not suggestive of angina) Step 3 a— For patients who are felt not to have an ischemic etiology for chest pain but who have significant risk factors for CHD, consider arranging for an evaluation for CHD Step 3 b— If symptoms suggest a musculoskeletal etiology, a trial of an NSAID is appropriate; If pain persists, consider rib films, a bone scan, and plain or CT chest radiography.
Step 3 c— If symptoms suggest a gastrointestinal etiology, evaluate the patient for gastrointestinal disease; otherwise, proceed to step 3 d. This evaluation may initially involve a trial of acid suppression. Step 3 d— If symptoms suggest a psychogenic etiology, evaluate the patient for a psychosocial source of chest pain
Step 3 e— Consider chest anatomy as a guide to other less common causes of non-life-threatening chest pain including: chest wall pain (eg, zoster, breast disease); other cardiac pain such as pericarditis; pathology of the lung parenchyma, vasculature, or pleura; and pain referred to the chest from the gallbladder, diaphragm, or from a disc herniation.
Step 4 (Persistent chest pain) — If chest pain persists and evaluations for CHD , musculoskeletal pain, gastrointestinal pain , psychogenic pain, and other causes have not all been performed, those evaluations should now be undertaken.
Step 5 (Diagnostic evaluations negative) — Patient likely has chronic idiopathic chest pain. Since this is known to cause significant disability, consider referral to a pain management center or medical symptom reduction program. No further evaluation is required unless the patient has a change in symptoms or the symptoms are disabling.
 Yaar uygulaması nedir
Yaar uygulaması nedir Stabbing pain in chest
Stabbing pain in chest Typical vs atypical chest pain
Typical vs atypical chest pain Typical chest pain
Typical chest pain Chest pain in pediatrics
Chest pain in pediatrics Ctas triage
Ctas triage Afebrile vss
Afebrile vss Dmagid
Dmagid Retrosternal chest pain
Retrosternal chest pain Nursing care plan on angina pectoris
Nursing care plan on angina pectoris Causes chest pain
Causes chest pain ömpsq
ömpsq Sympathetic trunk
Sympathetic trunk David lewis mad pain and martian pain
David lewis mad pain and martian pain Sore breasts before period
Sore breasts before period Pms vs pregnancy symptoms
Pms vs pregnancy symptoms Non non non ne failliront jamais lyrics
Non non non ne failliront jamais lyrics Flacc scale
Flacc scale Cps-naid
Cps-naid Michael r. jackson
Michael r. jackson Mitral stenosis chest x ray
Mitral stenosis chest x ray Tactile fremitus
Tactile fremitus Tactile.fremitus
Tactile.fremitus Thoracic cavity
Thoracic cavity How does the heart pump work
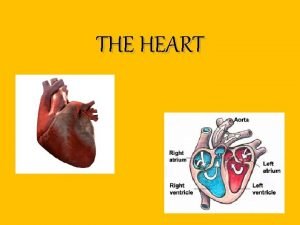
How does the heart pump work Olympic vac-pac
Olympic vac-pac Agnosist
Agnosist Latent tb chest x ray
Latent tb chest x ray Chest area name
Chest area name Symtoms of bronchitis
Symtoms of bronchitis Bronchopneumonia
Bronchopneumonia Mitral stenosis chest x ray
Mitral stenosis chest x ray Cvs xray
Cvs xray Ectomorphic
Ectomorphic Nursing positioning patients in bed
Nursing positioning patients in bed Left lateral recumbent position
Left lateral recumbent position Transudate
Transudate Sitting duck heart persistent truncus arteriosus
Sitting duck heart persistent truncus arteriosus Infant compression to ventilation ratio
Infant compression to ventilation ratio Chest rolls for prone position
Chest rolls for prone position Iss score
Iss score Bilateral chest tubes
Bilateral chest tubes Chest left oblique view
Chest left oblique view