Neonatal Sepsis Definition n Clinical syndrome of systemic




- Slides: 30
Neonatal Sepsis
Definition n Clinical syndrome of systemic illness accompanied by bacteremia occurring in the first month of life n Mortality rate is high – Higher rates in premature infants – Neonatal sepsis is a common cause of morbidity and mortality
Types • Early Onset Sepsis (EOS): – Culture proven infection within the first 3 -7 days of life • Late Onset Sepsis (LOS): – Culture proven infection after 7 days of life – UTI, pneumonia, meningitis, osteomyelitis, NEC
Early Onset n First 3 -7 days of life n Usually multisystem fulminant illness with prominent respiratory symptoms (probably due to aspiration of infected amniotic fluid) n High mortality rate n Typically acquired during intrapartum period from maternal genital tract – Associated with maternal chorioamnionitis
Late Onset n occur after the first week of life n Usually have an identifiable focus – Most often meningitis or sepsis – Nosocomial or focal infection
Etiology: EOS • Early Onset Sepsis (EOS): – Group B Streptococcus (GBS) – E. Coli – Listeria monocytogenes (gram +ve) • Due to maternal or perinatal factors
Etiology: LOS • Late Onset Sepsis (LOS): – Staphylococcus aureus – Gram negative bacilli ie. Klebsiella – pseudomonas • Nosocomial or focal infection
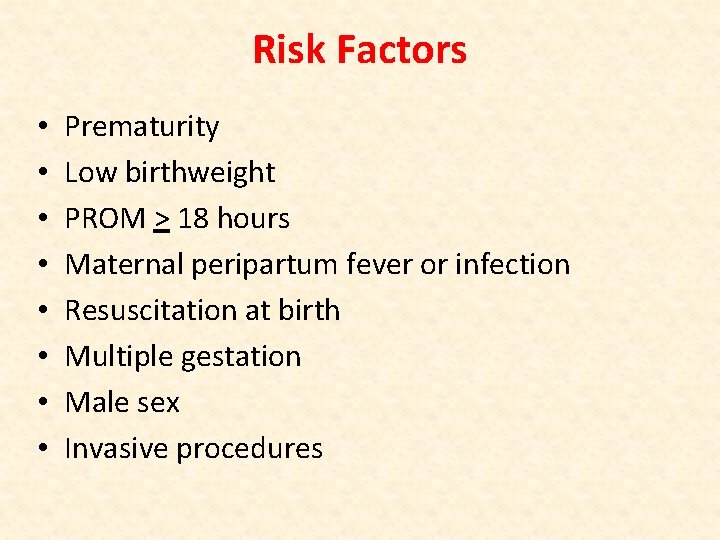
Risk Factors • • Prematurity Low birthweight PROM > 18 hours Maternal peripartum fever or infection Resuscitation at birth Multiple gestation Male sex Invasive procedures
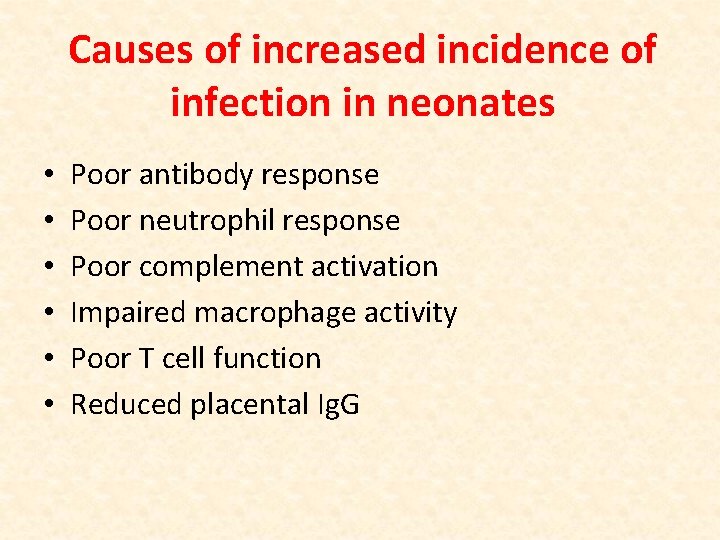
Causes of increased incidence of infection in neonates • • • Poor antibody response Poor neutrophil response Poor complement activation Impaired macrophage activity Poor T cell function Reduced placental Ig. G
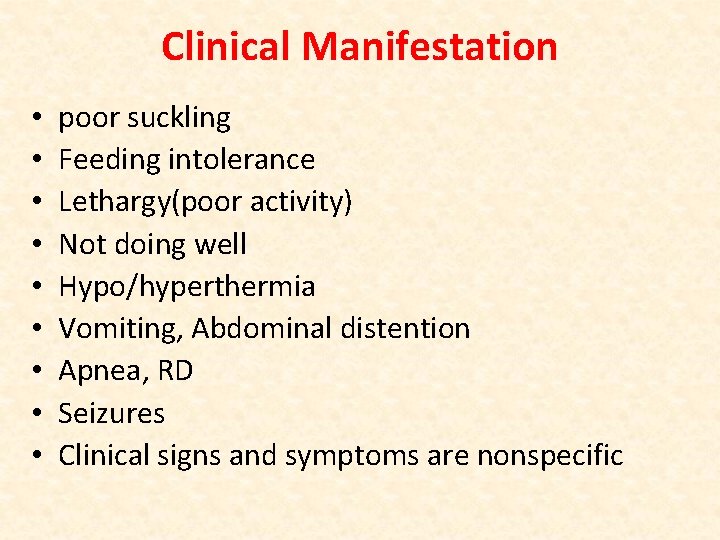
Clinical Manifestation • • • poor suckling Feeding intolerance Lethargy(poor activity) Not doing well Hypo/hyperthermia Vomiting, Abdominal distention Apnea, RD Seizures Clinical signs and symptoms are nonspecific
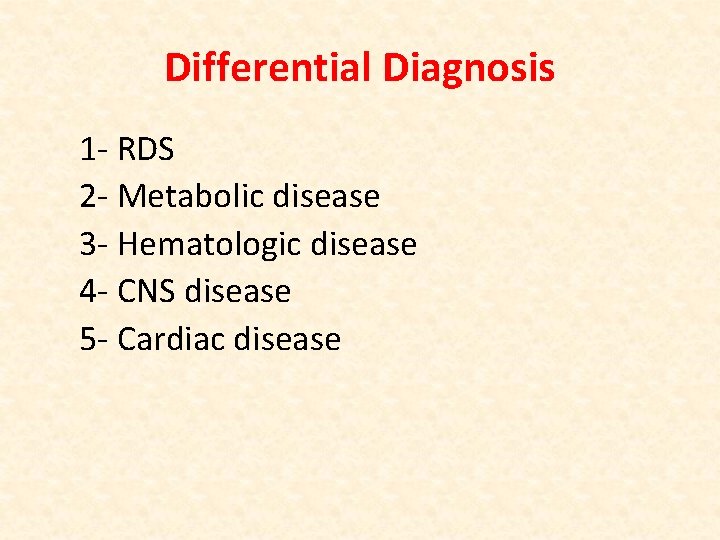
Differential Diagnosis 1 - RDS 2 - Metabolic disease 3 - Hematologic disease 4 - CNS disease 5 - Cardiac disease
Investigation 1 - blood culture 2 - CBC with differential White blood cell count and differential – Neutropenia can be an ominous sign Platelet count – Late sign Acute phase reactants – CRP rises early, monitor serial values Other tests: bilirubin, glucose, sodium
3 - Urine cultures 4 - Lumbar puncture 5 - Tracheal aspirates
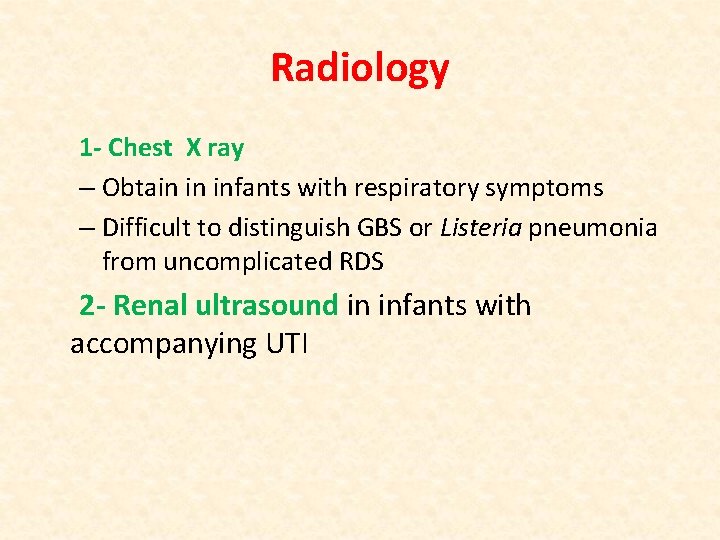
Radiology 1 - Chest X ray – Obtain in infants with respiratory symptoms – Difficult to distinguish GBS or Listeria pneumonia from uncomplicated RDS 2 - Renal ultrasound in infants with accompanying UTI

Treatment Empiric Antibiotic Therapy • EOS – Ampicillin and Gentamicin • LOS – Vancomycin and Gentamicin • Duration Uncomplicated sepsis Meningitis 10 -14 days 21 days
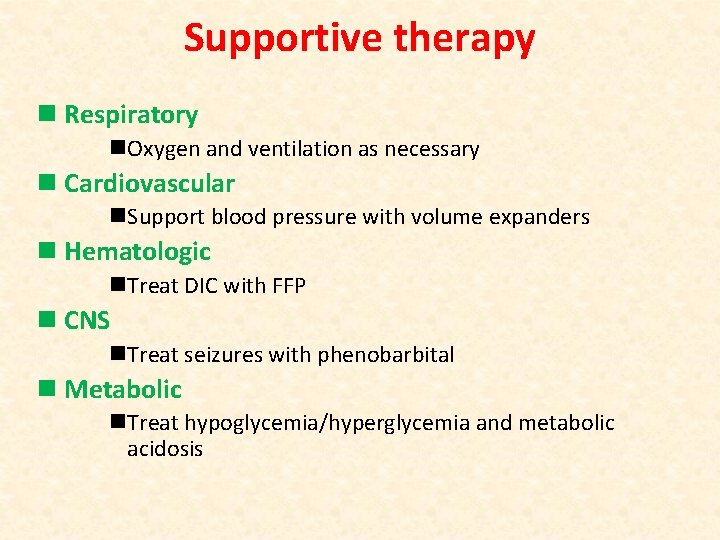
Supportive therapy n Respiratory n. Oxygen and ventilation as necessary n Cardiovascular n. Support blood pressure with volume expanders n Hematologic n. Treat DIC with FFP n CNS n. Treat seizures with phenobarbital n Metabolic n. Treat hypoglycemia/hyperglycemia and metabolic acidosis
Congenital Infections
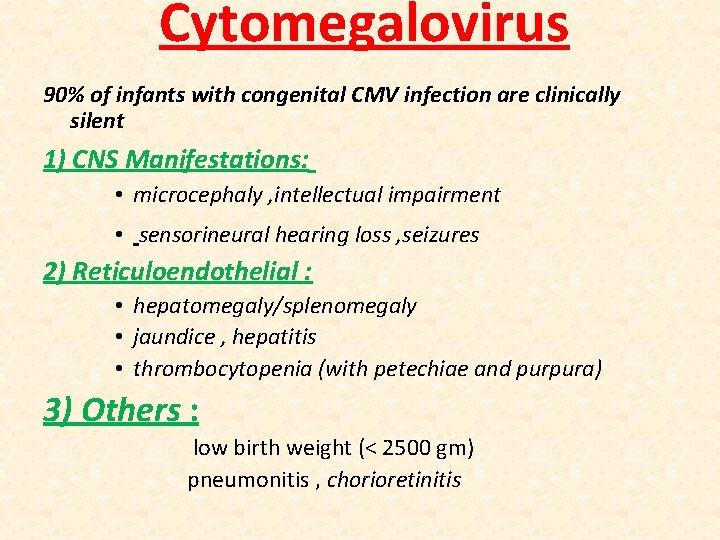
Cytomegalovirus 90% of infants with congenital CMV infection are clinically silent 1) CNS Manifestations: • microcephaly , intellectual impairment • sensorineural hearing loss , seizures 2) Reticuloendothelial : • hepatomegaly/splenomegaly • jaundice , hepatitis • thrombocytopenia (with petechiae and purpura) 3) Others : low birth weight (< 2500 gm) pneumonitis , chorioretinitis
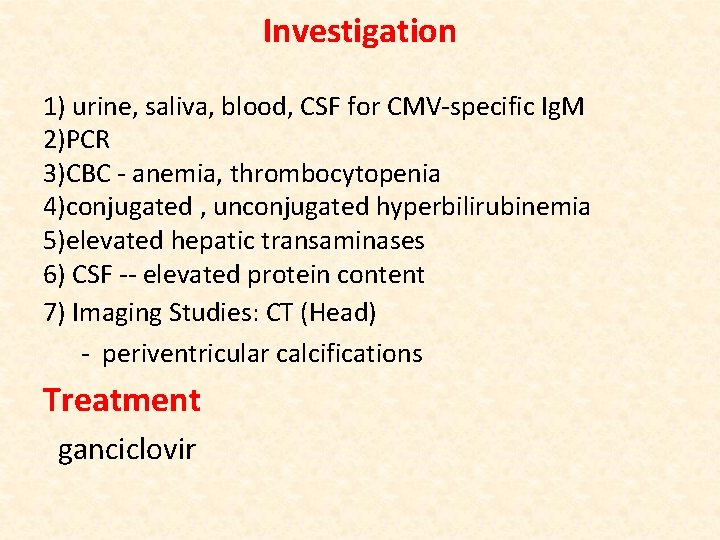
Investigation 1) urine, saliva, blood, CSF for CMV-specific Ig. M 2)PCR 3)CBC - anemia, thrombocytopenia 4)conjugated , unconjugated hyperbilirubinemia 5)elevated hepatic transaminases 6) CSF -- elevated protein content 7) Imaging Studies: CT (Head) - periventricular calcifications Treatment ganciclovir

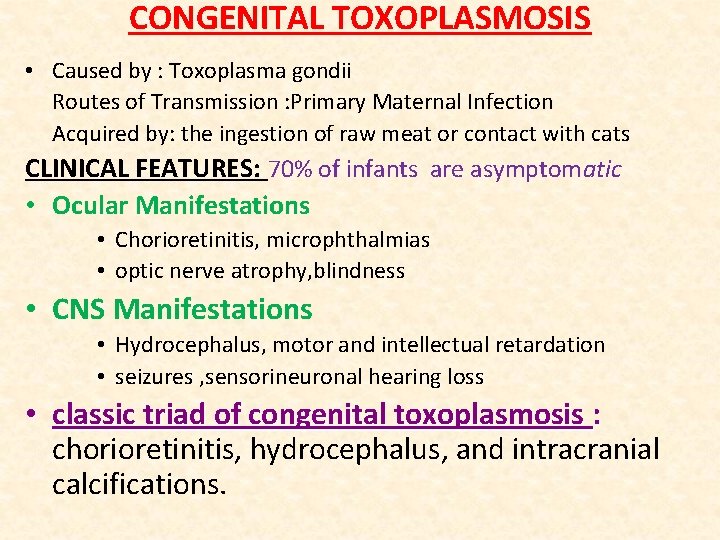
CONGENITAL TOXOPLASMOSIS • Caused by : Toxoplasma gondii Routes of Transmission : Primary Maternal Infection Acquired by: the ingestion of raw meat or contact with cats CLINICAL FEATURES: 70% of infants are asymptomatic • Ocular Manifestations • Chorioretinitis, microphthalmias • optic nerve atrophy, blindness • CNS Manifestations • Hydrocephalus, motor and intellectual retardation • seizures , sensorineuronal hearing loss • classic triad of congenital toxoplasmosis : chorioretinitis, hydrocephalus, and intracranial calcifications.
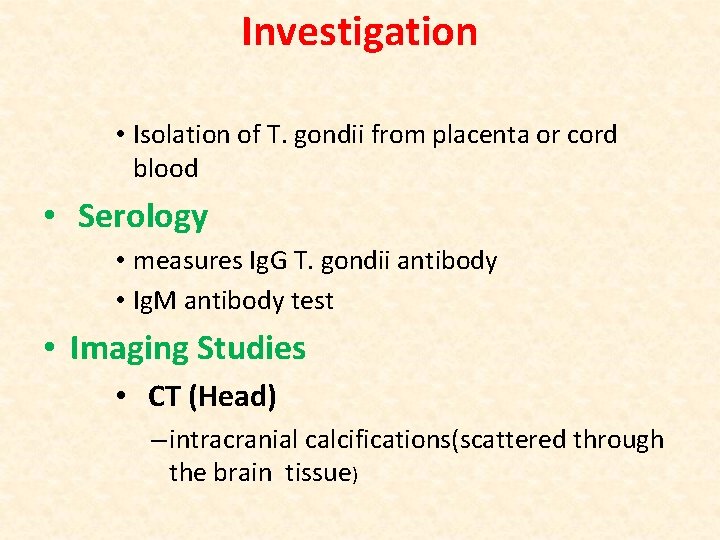
Investigation • Isolation of T. gondii from placenta or cord blood • Serology • measures Ig. G T. gondii antibody • Ig. M antibody test • Imaging Studies • CT (Head) – intracranial calcifications(scattered through the brain tissue)

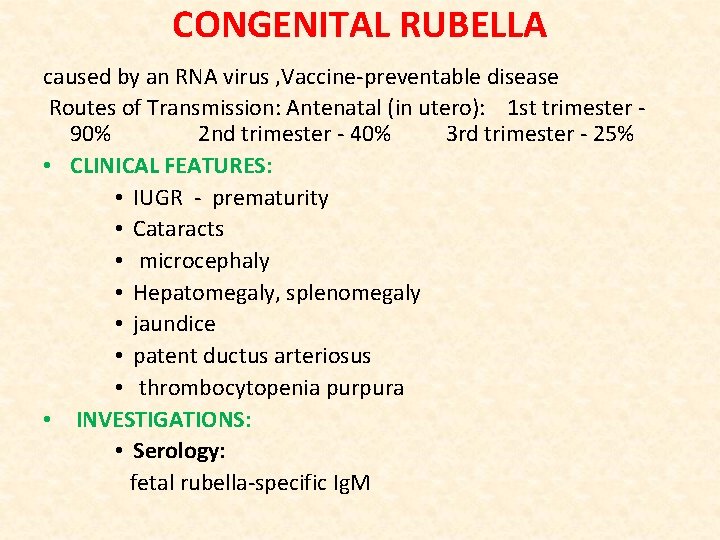
CONGENITAL RUBELLA caused by an RNA virus , Vaccine-preventable disease Routes of Transmission: Antenatal (in utero): 1 st trimester 90% 2 nd trimester - 40% 3 rd trimester - 25% • CLINICAL FEATURES: • IUGR - prematurity • Cataracts • microcephaly • Hepatomegaly, splenomegaly • jaundice • patent ductus arteriosus • thrombocytopenia purpura • INVESTIGATIONS: • Serology: fetal rubella-specific Ig. M

Congenital Rubella: skin Lesions: Blueberry muffin rash but may be present in cytomegalovirus
Neonatal meningitis Clinical Picture: • The clinical presentation of neonatal meningitis often is indistinguishable from that of neonatal sepsis without meningitis. • The commonest C/P are temperature instability , irritability, and poor feeding or vomiting • Respiratory distress (tachypnea, retractions , grunting, apnea) • seizures
• Causitive micro-organism: GBS and Escherichia coli are the two most common organisms • investigation 1 - LP • Isolation of a bacterial pathogen from CSF by culture or visualization by Gram stain • Increased CSF white blood cell (WBC) count (typically >1000 WBC/micro. L, but may be lower, especially with gram-positive organisms), with a predominance of neutrophils
2 - blood culture 3 - Cranial US – Safe, convenient, available at the bedside – Ventricular size, development of hydrocephalus – Not identify infarct, abscess, subdural empyema 4 - CT – Abscess, subdural collections, hydrocephalus
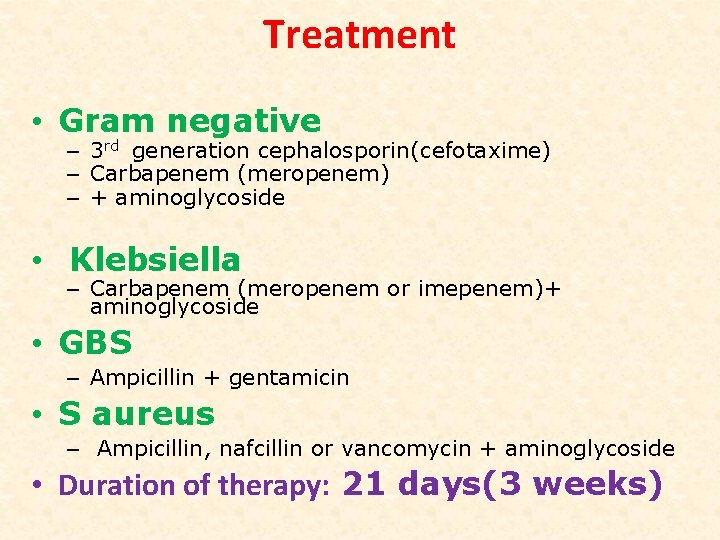
Treatment • Gram negative – 3 rd generation cephalosporin(cefotaxime) – Carbapenem (meropenem) – + aminoglycoside • Klebsiella – Carbapenem (meropenem or imepenem)+ aminoglycoside • GBS – Ampicillin + gentamicin • S aureus – Ampicillin, nafcillin or vancomycin + aminoglycoside • Duration of therapy: 21 days(3 weeks)
Thank you
 Q sofa
Q sofa Neonatal sepsis pathophysiology diagram
Neonatal sepsis pathophysiology diagram Sepsis neonatal temprana y tardía
Sepsis neonatal temprana y tardía Neonatal sepsis
Neonatal sepsis Prevention of puerperal sepsis
Prevention of puerperal sepsis Neonatal sepsis
Neonatal sepsis Nec diagnosis
Nec diagnosis Hoja de balance hidrico en enfermeria
Hoja de balance hidrico en enfermeria Nursing diagnosis three parts
Nursing diagnosis three parts Surviving sepsis definition
Surviving sepsis definition Sepsis definition
Sepsis definition Puerperal sepsis meaning
Puerperal sepsis meaning Neonatal cholestasis definition
Neonatal cholestasis definition Dr sneha sood
Dr sneha sood Immediate newborn care steps
Immediate newborn care steps Sepsis care near palo alto
Sepsis care near palo alto Sepsis
Sepsis La hora dorada medicina
La hora dorada medicina Gdp sepsis decision support tool
Gdp sepsis decision support tool Guido ruiz
Guido ruiz Sepsis 6 bundle
Sepsis 6 bundle Sepsis bundle
Sepsis bundle Driver diagram instructions
Driver diagram instructions Sepsis hour 1 bundle
Sepsis hour 1 bundle Dr alex sepsis
Dr alex sepsis Antonio cuñarro alonso
Antonio cuñarro alonso Sepsis dietary management
Sepsis dietary management Sepsis hour 1 bundle
Sepsis hour 1 bundle Give 3 take 3 sepsis
Give 3 take 3 sepsis What is hypotensis
What is hypotensis Quick sofa
Quick sofa