Neonatal Apnea M NooriShadkam MDMPH Neonatologist Apneic Spells




- Slides: 37
Neonatal Apnea M. Noori-Shadkam, MD-MPH Neonatologist
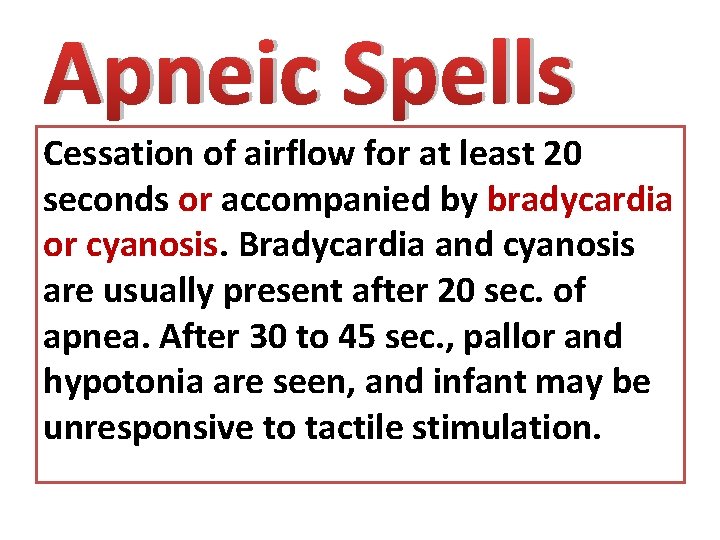
Apneic Spells Cessation of airflow for at least 20 seconds or accompanied by bradycardia or cyanosis. Bradycardia and cyanosis are usually present after 20 sec. of apnea. After 30 to 45 sec. , pallor and hypotonia are seen, and infant may be unresponsive to tactile stimulation.
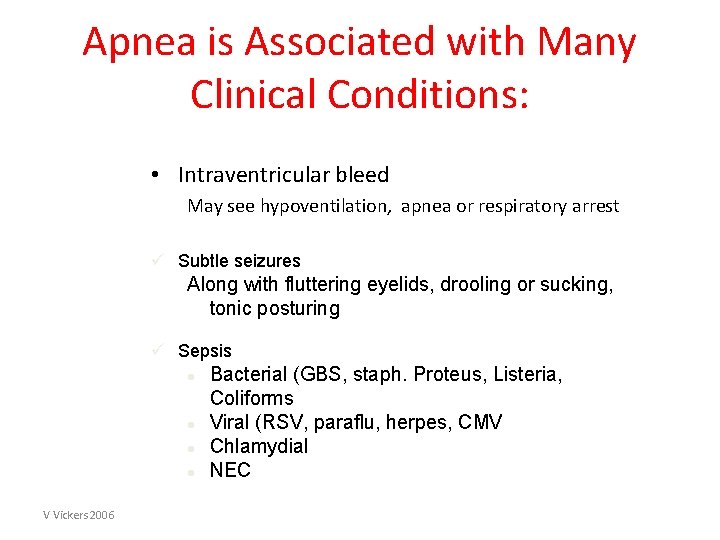
Apnea is Associated with Many Clinical Conditions: • Intraventricular bleed May see hypoventilation, apnea or respiratory arrest ü Subtle seizures Along with fluttering eyelids, drooling or sucking, tonic posturing ü Sepsis l l V Vickers 2006 Bacterial (GBS, staph. Proteus, Listeria, Coliforms Viral (RSV, paraflu, herpes, CMV Chlamydial NEC
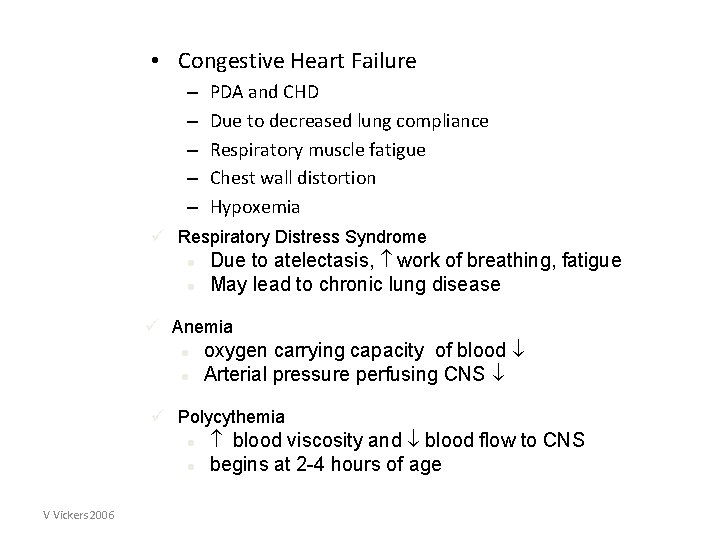
• Congestive Heart Failure – – – PDA and CHD Due to decreased lung compliance Respiratory muscle fatigue Chest wall distortion Hypoxemia ü Respiratory Distress Syndrome l l Due to atelectasis, work of breathing, fatigue May lead to chronic lung disease ü Anemia l l oxygen carrying capacity of blood Arterial pressure perfusing CNS ü Polycythemia l l V Vickers 2006 blood viscosity and blood flow to CNS begins at 2 -4 hours of age
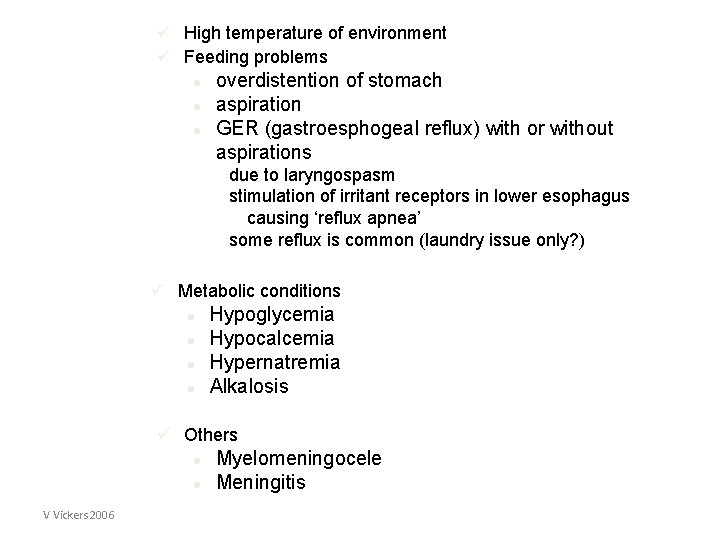
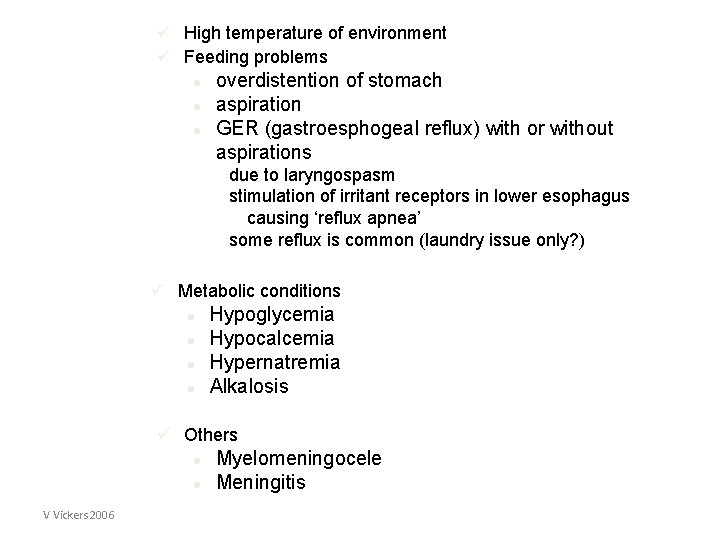
ü High temperature of environment ü Feeding problems l l l overdistention of stomach aspiration GER (gastroesphogeal reflux) with or without aspirations due to laryngospasm stimulation of irritant receptors in lower esophagus causing ‘reflux apnea’ some reflux is common (laundry issue only? ) ü Metabolic conditions l l Hypoglycemia Hypocalcemia Hypernatremia Alkalosis ü Others l l V Vickers 2006 Myelomeningocele Meningitis
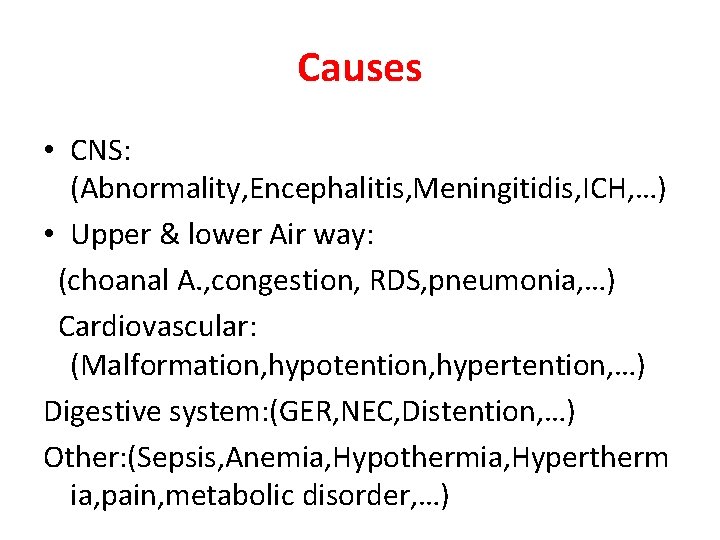
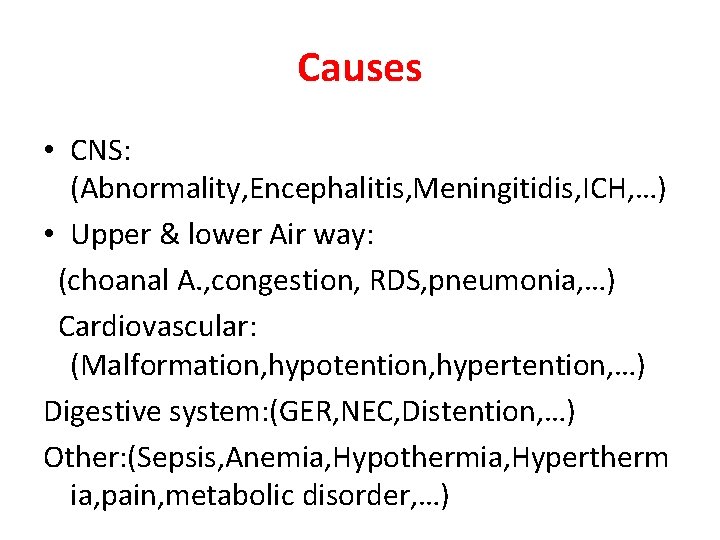
Causes • CNS: (Abnormality, Encephalitis, Meningitidis, ICH, …) • Upper & lower Air way: (choanal A. , congestion, RDS, pneumonia, …) Cardiovascular: (Malformation, hypotention, hypertention, …) Digestive system: (GER, NEC, Distention, …) Other: (Sepsis, Anemia, Hypothermia, Hypertherm ia, pain, metabolic disorder, …)
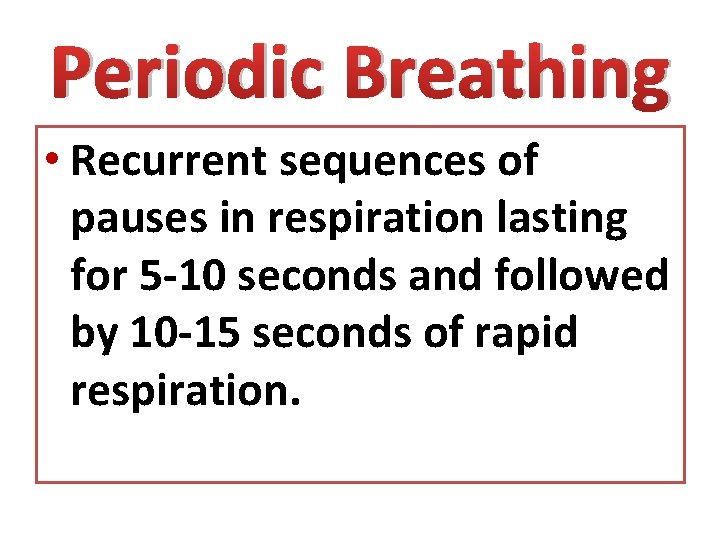
Periodic Breathing • Recurrent sequences of pauses in respiration lasting for 5 -10 seconds and followed by 10 -15 seconds of rapid respiration.
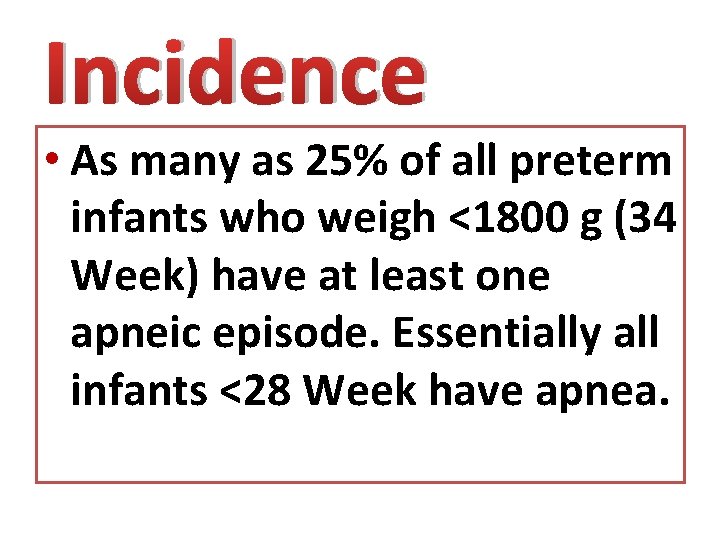
Incidence • As many as 25% of all preterm infants who weigh <1800 g (34 Week) have at least one apneic episode. Essentially all infants <28 Week have apnea.
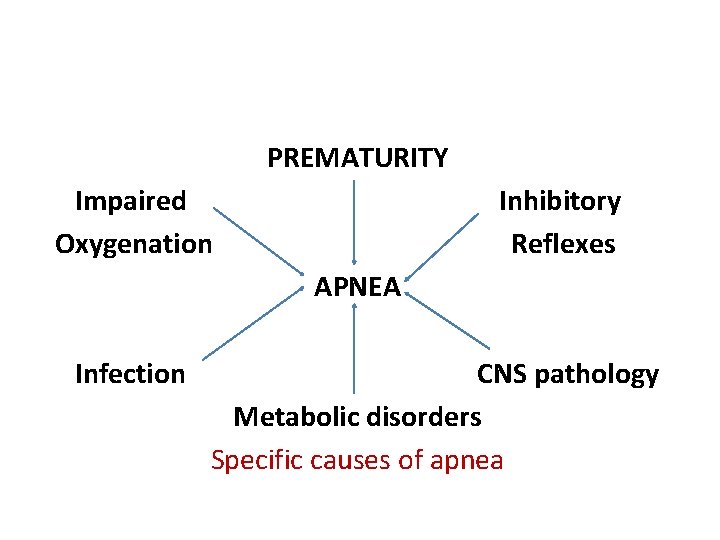
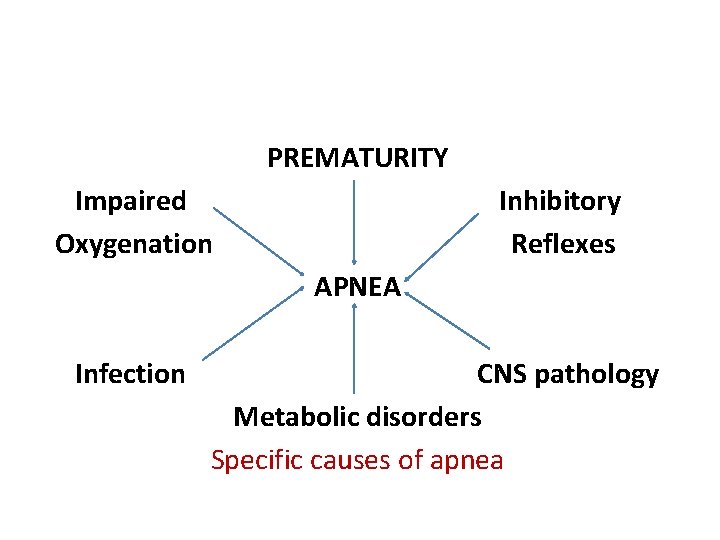
PREMATURITY Impaired Oxygenation Inhibitory Reflexes APNEA Infection CNS pathology Metabolic disorders Specific causes of apnea


Neonatal Apnea Preterm infants respond to a fall in inspired oxygen with a transient hyperventilation followed by hypoventilation and sometimes apnea.

The Respiratory Pump • The neonatal diaphragm • The ribcage and chest wall muscles
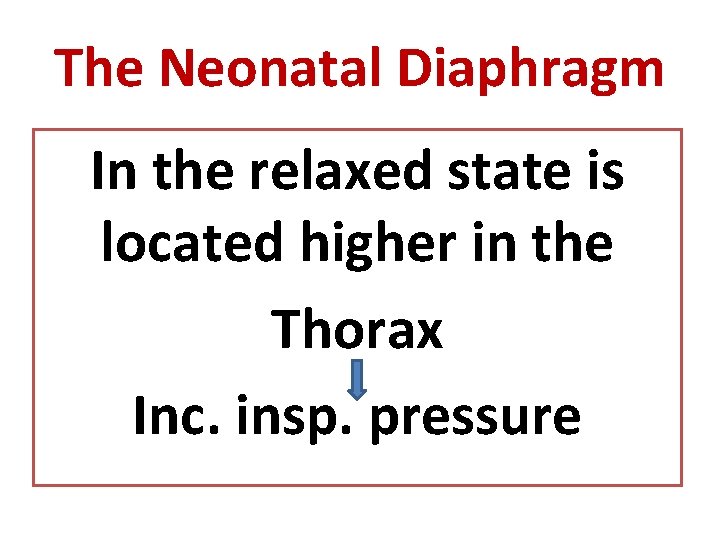
The Neonatal Diaphragm In the relaxed state is located higher in the Thorax Inc. insp. pressure
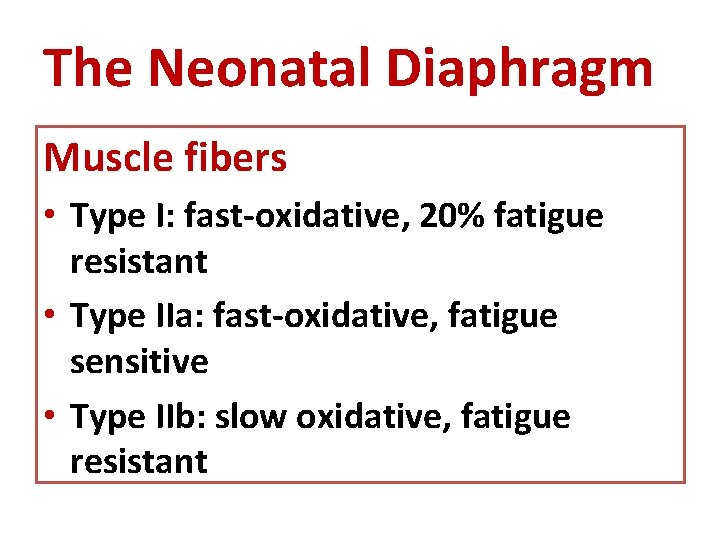
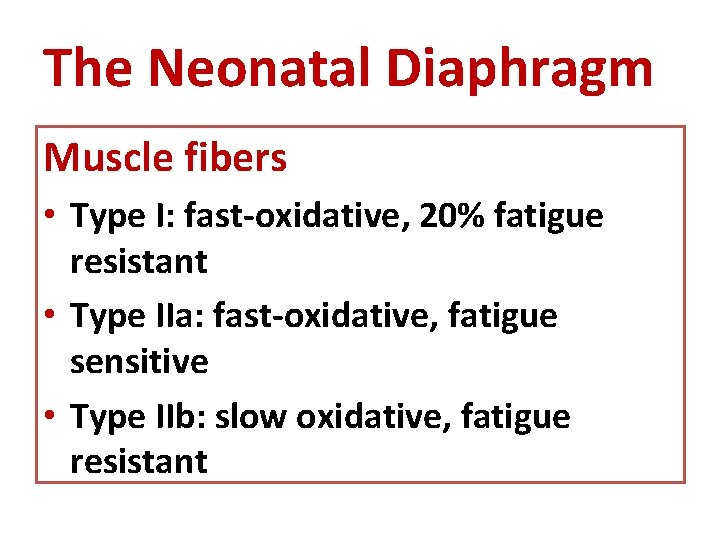
The Neonatal Diaphragm Muscle fibers • Type I: fast-oxidative, 20% fatigue resistant • Type IIa: fast-oxidative, fatigue sensitive • Type IIb: slow oxidative, fatigue resistant
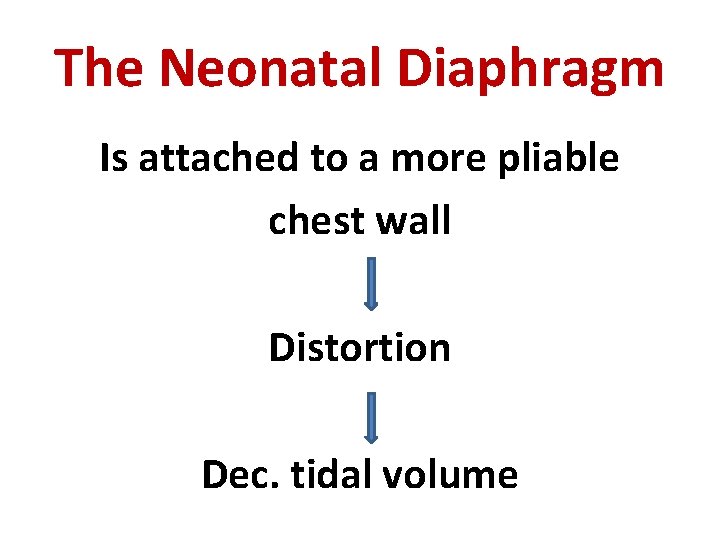
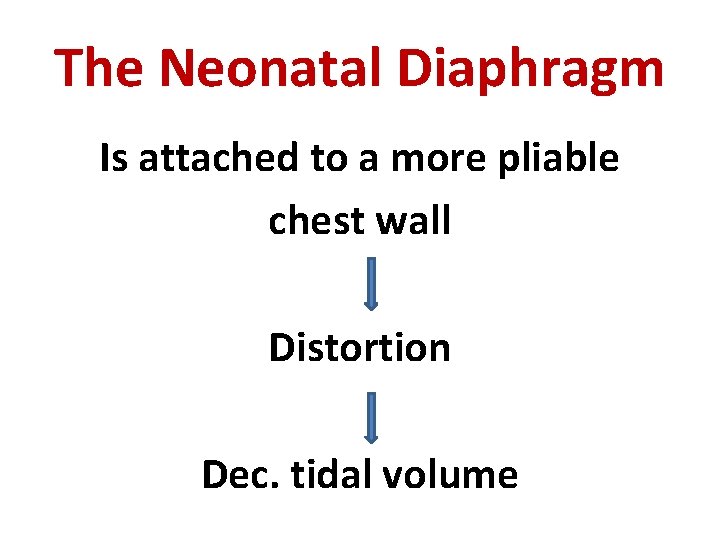
The Neonatal Diaphragm Is attached to a more pliable chest wall Distortion Dec. tidal volume
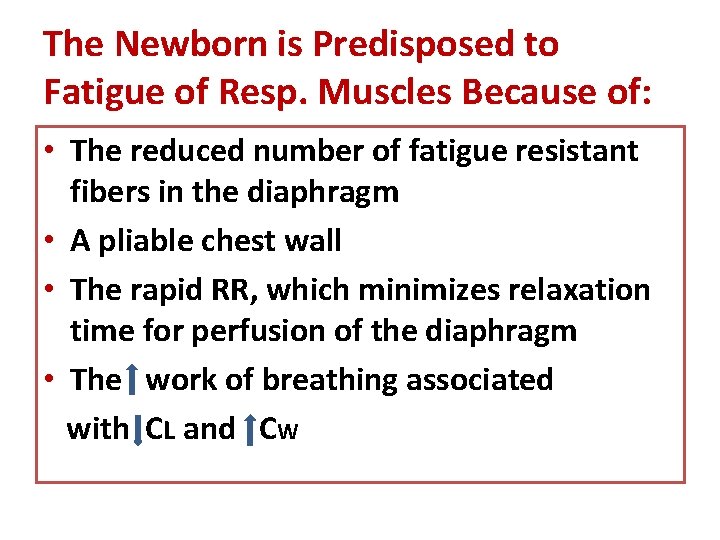
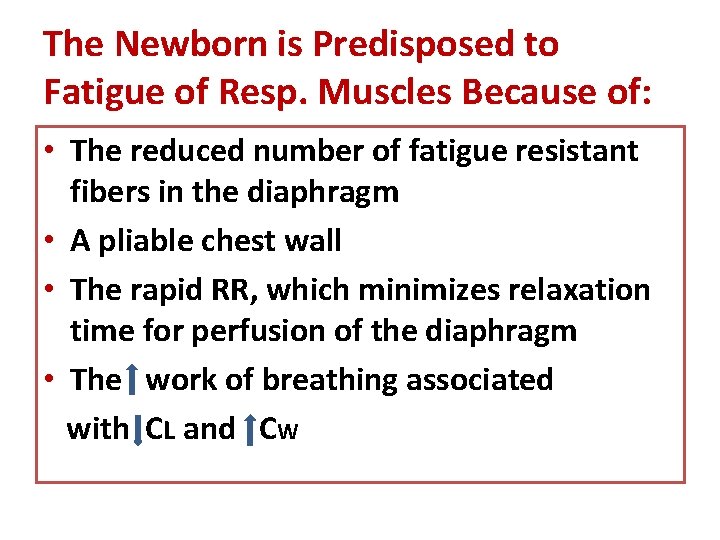
The Newborn is Predisposed to Fatigue of Resp. Muscles Because of: • The reduced number of fatigue resistant fibers in the diaphragm • A pliable chest wall • The rapid RR, which minimizes relaxation time for perfusion of the diaphragm • The work of breathing associated with CL and CW
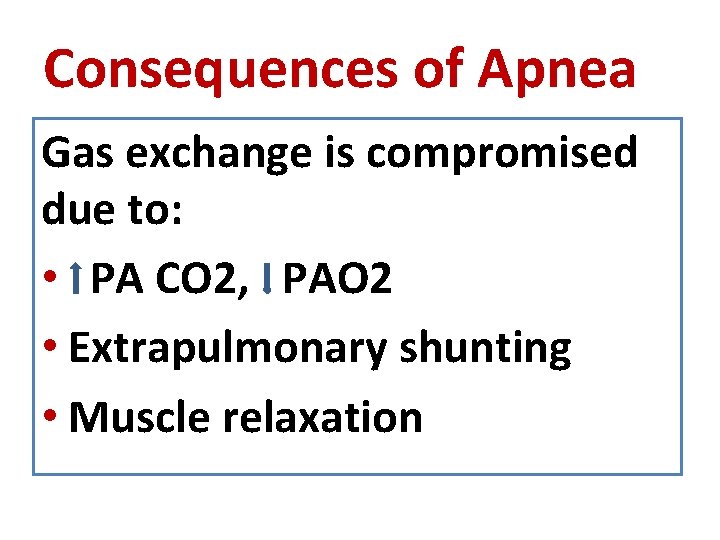
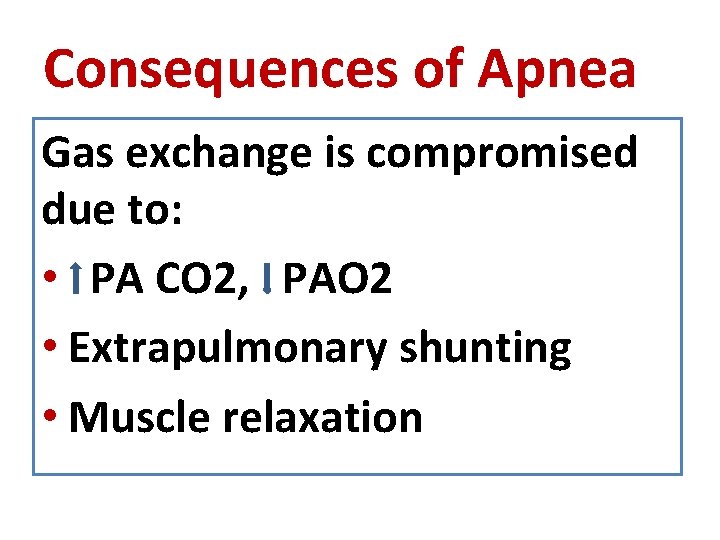
Consequences of Apnea Gas exchange is compromised due to: • PA CO 2, PAO 2 • Extrapulmonary shunting • Muscle relaxation
Types of Neonatal Apnea 1. Central (diaphragmatic) 2. Peripheral (obstructive) 3. Mixed

Monitoring • All preterm infants below 35 WG must be monitored for at least the first week after birth. Monitoring should continue until no significant apneic episode has been detected for at least 5 days.
Monitoring • Because impedance apnea monitors may not distinguish respiratory efforts during airway obstruction from normal breaths, heart rate should be monitored in addition to, or instead of, respiration.
Monitoring • BP should be measured frequently and hypotension with oliguria< 2 m. L/kg/h should be treated accordingly • Hct should be> 45% ? ? ?
Care of The Infant 1. Prevent hyperflexion of the neck 2. Nurse the baby in prone position 3. Set thermal environment to obtain a central temperature of 36. 537⁰ C 4. Minimize the duration and rate of pharyngeal suction cont’d
Care of The Infant 5. Place the orogastric tube carefully 6. Avoid sudden gastric distension 7. Continuous gastric feeding if apnea occurs with gavage 8. Warm air and oxygen to incubator temperature
Nursing Management During Apneic Episode 1. Check infant at once 2. Cancel alarm 3. Stimulate if there is no obvious vomit 4. Suction cont’d
Nursing Management During Apneic Episode 5. Give O 2 via face mask in same concentration as infant had been receiving 6. Summon help if infant does not respond 7. Document and report 8. Intubation if indicated
Management of Idiopathic Apnea • When apneic spells are repeated and prolonged, (i. e. , more than 2 to 3 times/h. ) or when they require frequent bag and mask ventilation, treatment should be initiated. cont’d
Management of Idiopathic Apnea Diagnosis and treatment of specific causes Nursing care Nasal CPAP (4 -6 cm H 2 O) Methylxanthine therapy Increased environmental O 2 only as necessary to maintain adequate baseline O 2 saturation. Often associated with treatment of anemia • Assisted ventilation if all else fails • • •
Management of Idiopathic Apnea A. General measures 1. Diagnosis and treatment of specific causes 2. SO 2 : 85 -95% 3. Avoid reflexes that may trigger apnea. Suctioning of the pharynx should be done carefully, and oral feeding should be avoided. cont’d
Management of Idiopathic Apnea 4. Position of extreme flexion or extension of the neck should be avoided, to reduce the likelihood of airway obstruction. 5. Avoid swings in environmental temperature. cont’d
Management of Idiopathic Apnea 6. Consider a transfusions of PRBCs if the Hct is <25% and the infant has episodes of apnea and bradycardia that are frequent or severe while methylxanthine levels are therapeutic. cont’d
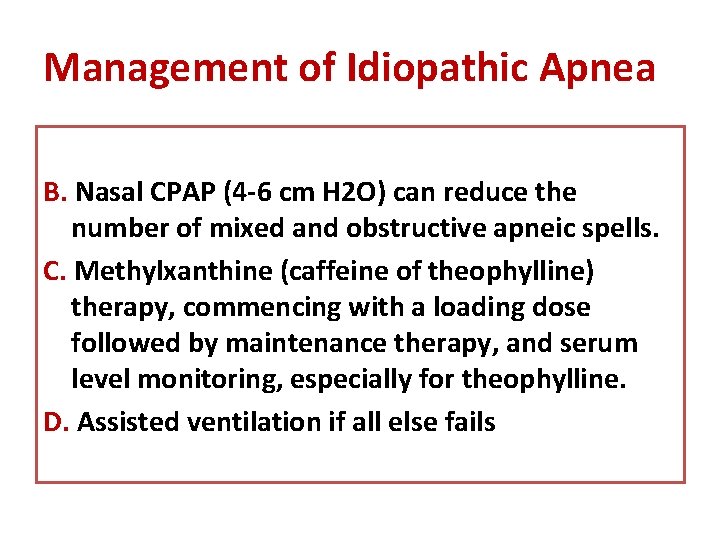
Management of Idiopathic Apnea B. Nasal CPAP (4 -6 cm H 2 O) can reduce the number of mixed and obstructive apneic spells. C. Methylxanthine (caffeine of theophylline) therapy, commencing with a loading dose followed by maintenance therapy, and serum level monitoring, especially for theophylline. D. Assisted ventilation if all else fails
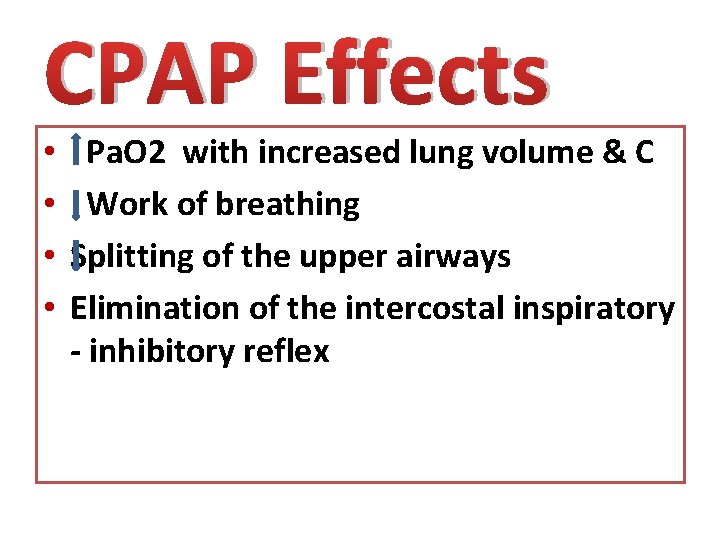
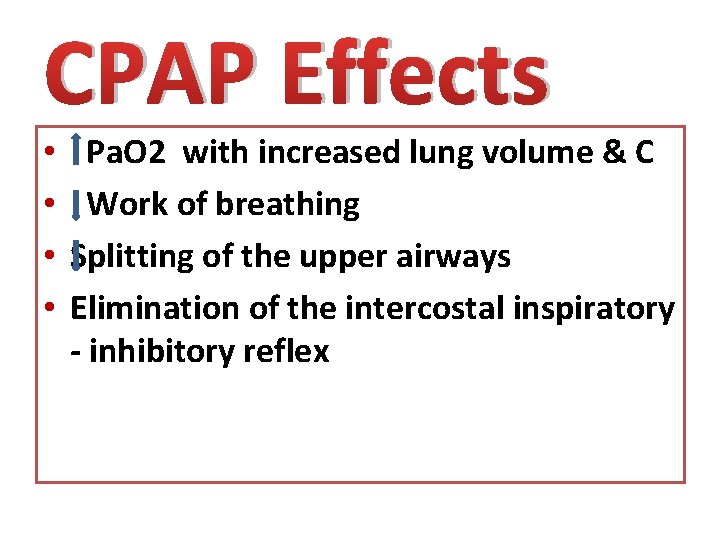
CPAP Effects • • Pa. O 2 with increased lung volume & C Work of breathing Splitting of the upper airways Elimination of the intercostal inspiratory - inhibitory reflex
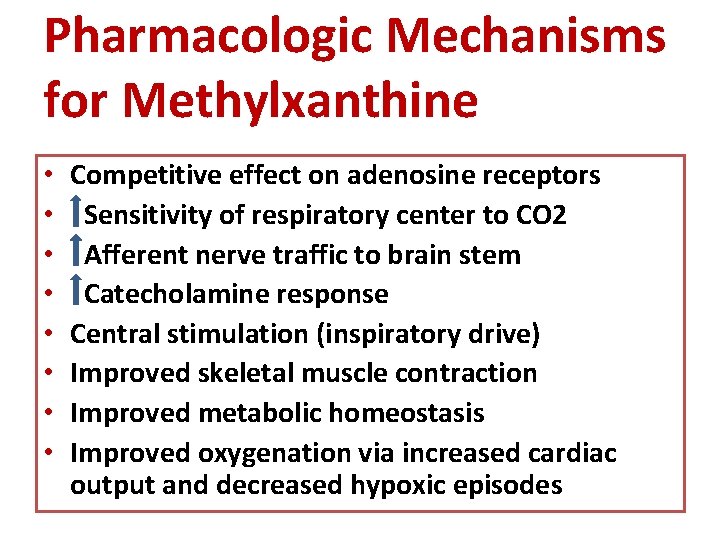
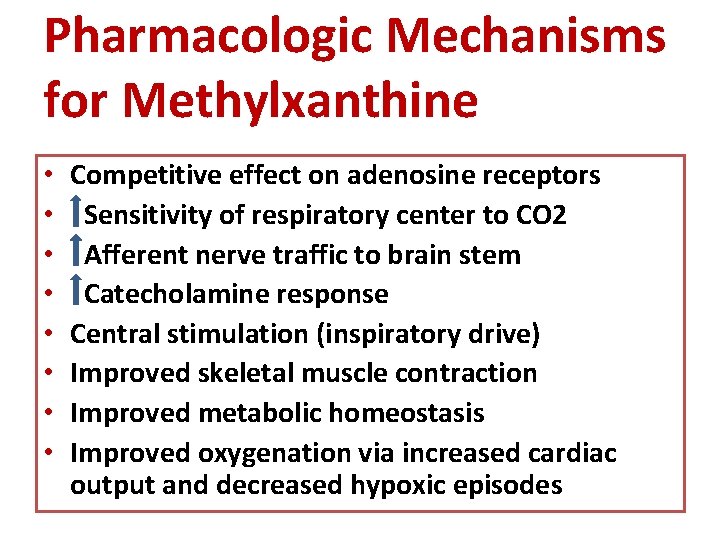
Pharmacologic Mechanisms for Methylxanthine • • Competitive effect on adenosine receptors Sensitivity of respiratory center to CO 2 Afferent nerve traffic to brain stem Catecholamine response Central stimulation (inspiratory drive) Improved skeletal muscle contraction Improved metabolic homeostasis Improved oxygenation via increased cardiac output and decreased hypoxic episodes
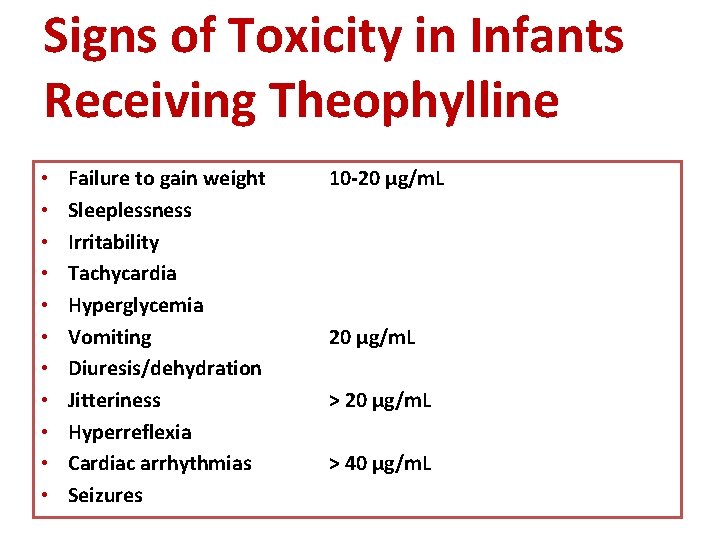
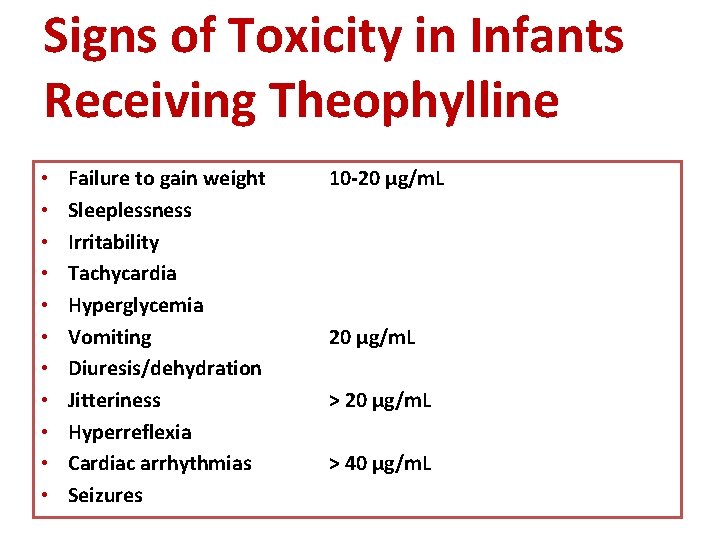
Signs of Toxicity in Infants Receiving Theophylline • • • Failure to gain weight Sleeplessness Irritability Tachycardia Hyperglycemia Vomiting Diuresis/dehydration Jitteriness Hyperreflexia Cardiac arrhythmias Seizures 10 -20 µg/m. L > 40 µg/m. L
 Apneic
Apneic Popular sovereignty
Popular sovereignty A measurable savings goal spells out ________.
A measurable savings goal spells out ________. Laser-assisted uvulopalatoplasty
Laser-assisted uvulopalatoplasty Tet spells
Tet spells Spells for motivation
Spells for motivation Cyanotic spells
Cyanotic spells Santa cruz sleep apnea devices
Santa cruz sleep apnea devices Cyanotic spells
Cyanotic spells Apnea educacion fisica
Apnea educacion fisica Sleep apnea symptoms
Sleep apnea symptoms Breath holding spells
Breath holding spells Scivolo prono in apnea
Scivolo prono in apnea Kaiser sleep apnea clinic
Kaiser sleep apnea clinic Neonatal alloimmün trombositopeni
Neonatal alloimmün trombositopeni Vasculopatía lenticuloestriada definicion
Vasculopatía lenticuloestriada definicion Hipocalcemia neonatal
Hipocalcemia neonatal Icterícia neonatal valores de referência
Icterícia neonatal valores de referência Icterícia neonatal valores de referência
Icterícia neonatal valores de referência Neonatal kolestaz
Neonatal kolestaz Rishika pandey
Rishika pandey Bilirubin levels in premature newborns chart
Bilirubin levels in premature newborns chart Salinoferesis
Salinoferesis Neonatal jaundice
Neonatal jaundice Neonatal progeria
Neonatal progeria Ambiente termico neutro
Ambiente termico neutro Hepatocytolyse
Hepatocytolyse Hipernatremia neonatal
Hipernatremia neonatal Valores de bilirrubina indirecta
Valores de bilirrubina indirecta Hypoglicaemia
Hypoglicaemia Neonatal resuscitation definition
Neonatal resuscitation definition Storch infection
Storch infection Fisiopatologia de ictericia neonatal
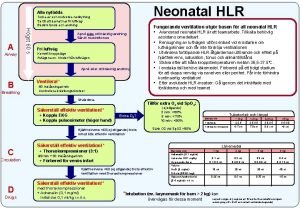
Fisiopatologia de ictericia neonatal Neonatal hlr
Neonatal hlr Circulação fetal
Circulação fetal Neonatal sepsis
Neonatal sepsis Diagnóstico de enfermería para ictericia adulto
Diagnóstico de enfermería para ictericia adulto Cuidados de enfermería en oxigenoterapia neonatal
Cuidados de enfermería en oxigenoterapia neonatal