Agnes Herczegfalvi Seizures convulsions and Neuromuscular diseases Semmelweis

- Slides: 41
Agnes Herczegfalvi Seizures, convulsions and Neuromuscular diseases Semmelweis University II. Pediatric Clinic, Dep. of. Neurology e-mail: herczegfalvi. agnes@med. Semmelweis-univ. hu Budapest, Oct-2017
Agnes Herczegfalvi Seizures, convulsions and Neuromuscular diseases Semmelweis University II. Pediatric Clinic, Dep. of. Neurology e-mail: herczegfalvi. agnes@med. Semmelweis-univ. hu Budapest, Oct-2017
Topic • Seizures • Convulsions • Nonepileptic paroxysmal events (NEPE) • Neuromuscular diseases
Seizure • is defined as an abnormal, disorderly discharging of the brain's nerve cells, resulting in a temporary disturbance of motor sensory, or mental function
Types of seizures • Febrile seizures are the most common type of seizure seen in children • 2 -5% of children have a febrile seizure during their childhood • The cause occurs when a child have infection accompanied by fever. • 1/100 children has epilepsy -recurring seizures <15 y
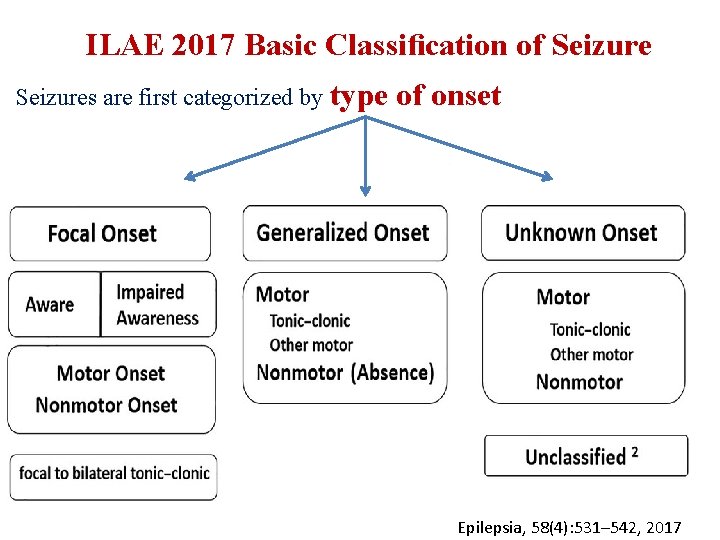
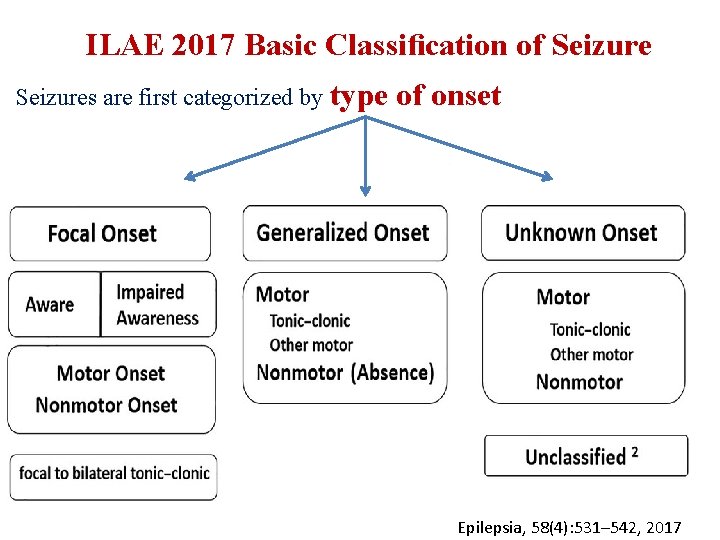
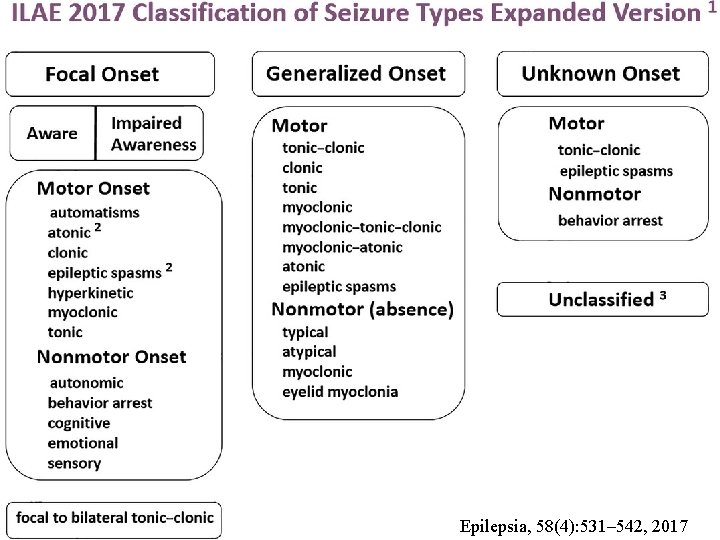
ILAE 2017 Basic Classification of Seizures are first categorized by type of onset Epilepsia, 58(4): 531– 542, 2017
Basic Classification of Seizure by type • Focal-onset seizures are defined as » “originating within networks limited to one hemisphere. » Focal seizures may originate in subcortical structures. ” • Generalized from onset seizures are defined as » “originating at some point within, and rapidly engaging, bilaterally distributed networks. ” • A seizure of unknown onset may still evidence certain defining » motor (e. g. , tonic–clonic) or » nonmotor (e. g. , behavior arrest) characteristics
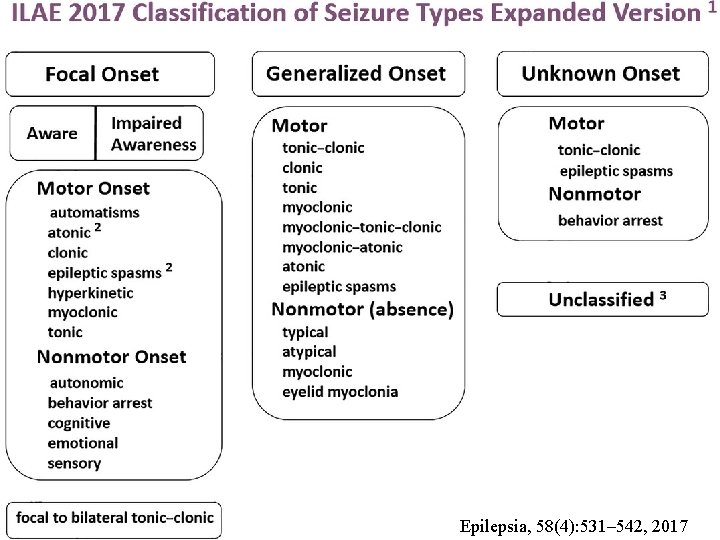
Epilepsia, 58(4): 531– 542, 2017
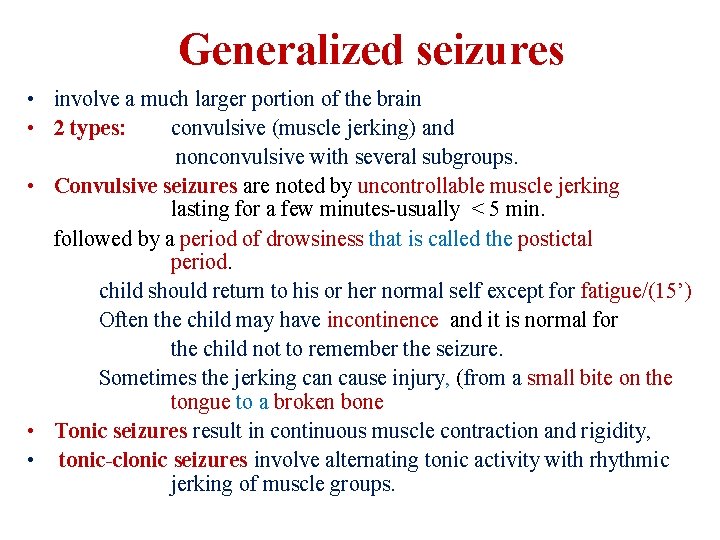
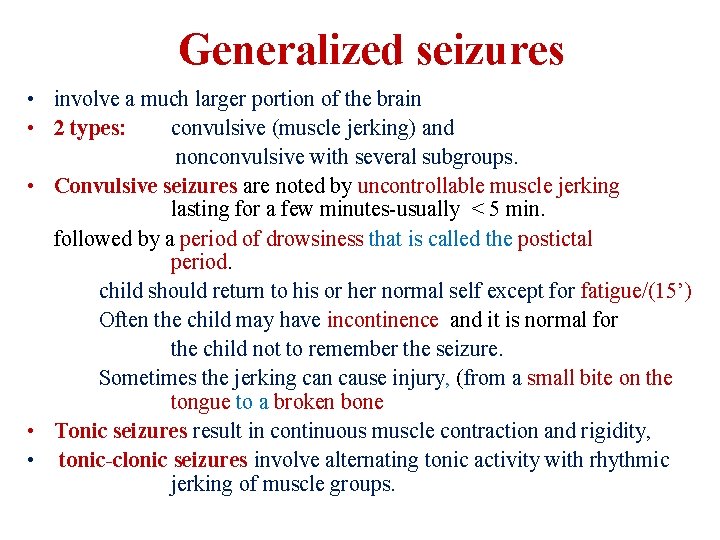
Generalized seizures • involve a much larger portion of the brain • 2 types: convulsive (muscle jerking) and nonconvulsive with several subgroups. • Convulsive seizures are noted by uncontrollable muscle jerking lasting for a few minutes-usually < 5 min. followed by a period of drowsiness that is called the postictal period. child should return to his or her normal self except for fatigue/(15’) Often the child may have incontinence and it is normal for the child not to remember the seizure. Sometimes the jerking can cause injury, (from a small bite on the tongue to a broken bone • Tonic seizures result in continuous muscle contraction and rigidity, • tonic-clonic seizures involve alternating tonic activity with rhythmic jerking of muscle groups.
Generalized seizures tonic-clonic seizures
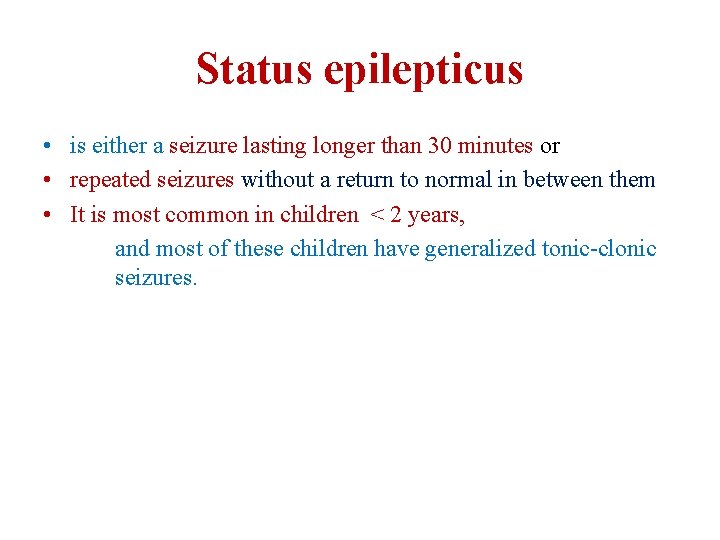
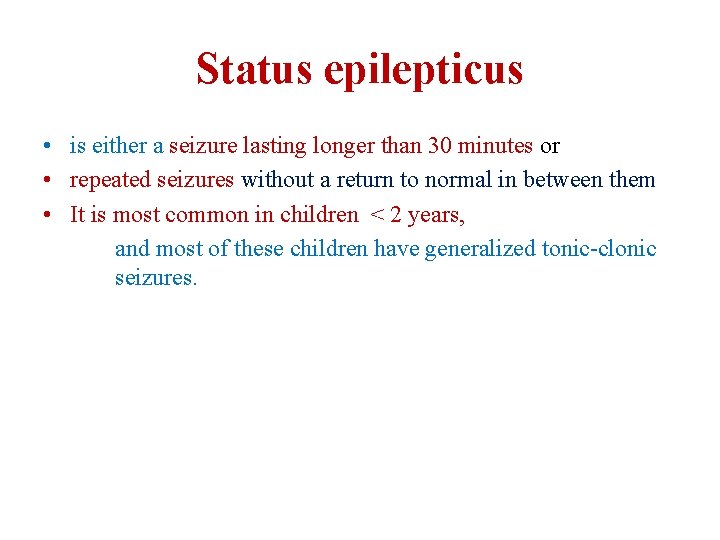
Status epilepticus • is either a seizure lasting longer than 30 minutes or • repeated seizures without a return to normal in between them • It is most common in children < 2 years, and most of these children have generalized tonic-clonic seizures.
Status epilepticus
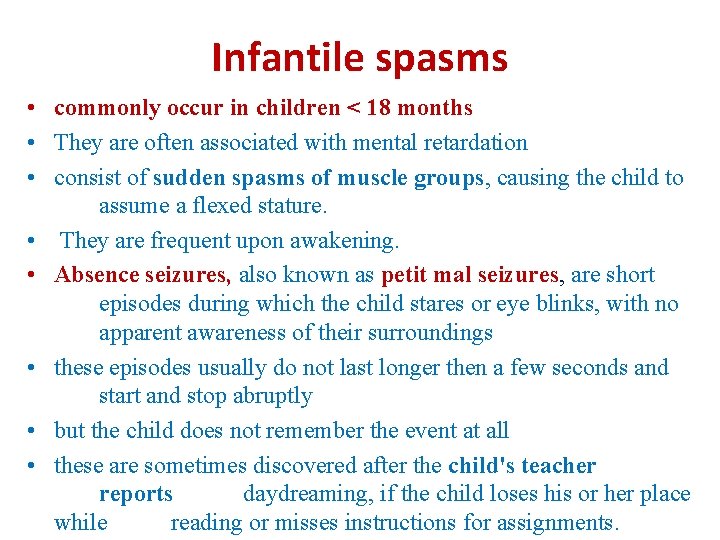
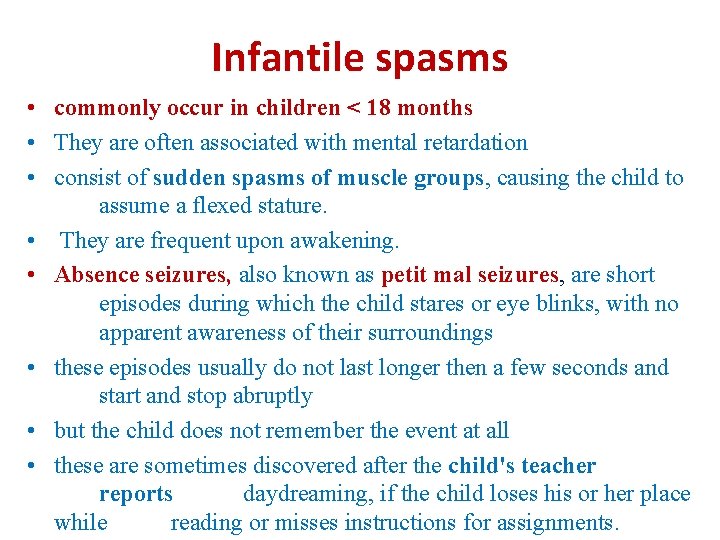
Infantile spasms • commonly occur in children < 18 months • They are often associated with mental retardation • consist of sudden spasms of muscle groups, causing the child to assume a flexed stature. • They are frequent upon awakening. • Absence seizures, also known as petit mal seizures, are short episodes during which the child stares or eye blinks, with no apparent awareness of their surroundings • these episodes usually do not last longer then a few seconds and start and stop abruptly • but the child does not remember the event at all • these are sometimes discovered after the child's teacher reports daydreaming, if the child loses his or her place while reading or misses instructions for assignments.
Infantile spasms
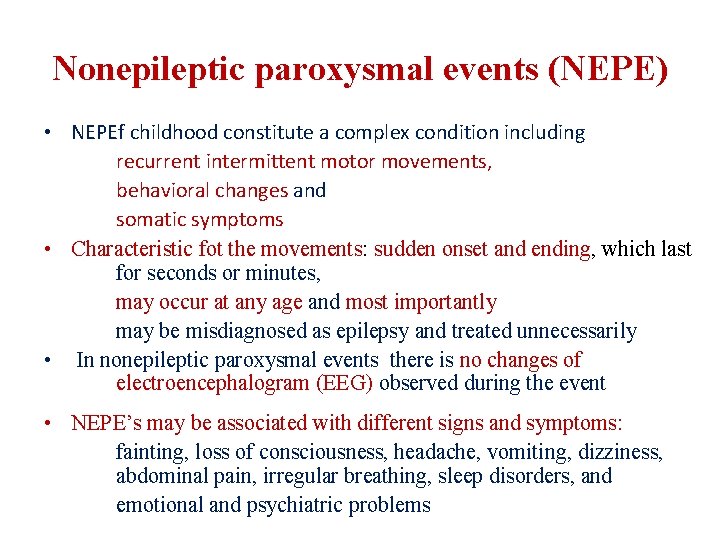
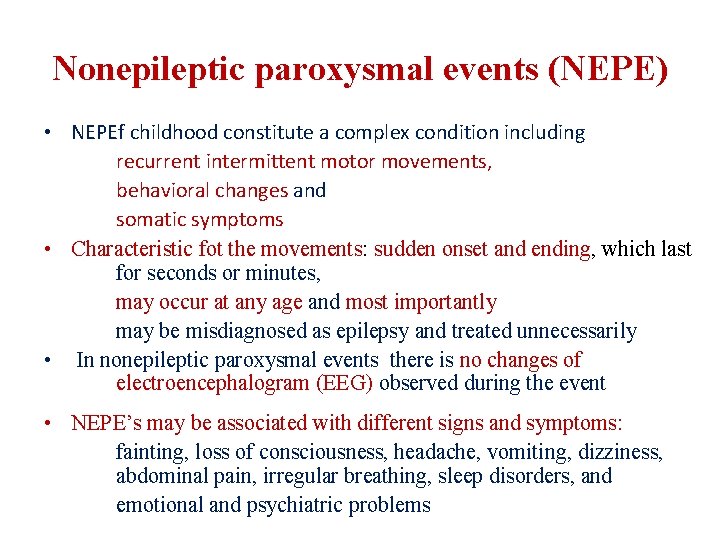
Nonepileptic paroxysmal events (NEPE) • NEPEf childhood constitute a complex condition including recurrent intermittent motor movements, behavioral changes and somatic symptoms • Characteristic fot the movements: sudden onset and ending, which last for seconds or minutes, may occur at any age and most importantly may be misdiagnosed as epilepsy and treated unnecessarily • In nonepileptic paroxysmal events there is no changes of electroencephalogram (EEG) observed during the event • NEPE’s may be associated with different signs and symptoms: fainting, loss of consciousness, headache, vomiting, dizziness, abdominal pain, irregular breathing, sleep disorders, and emotional and psychiatric problems
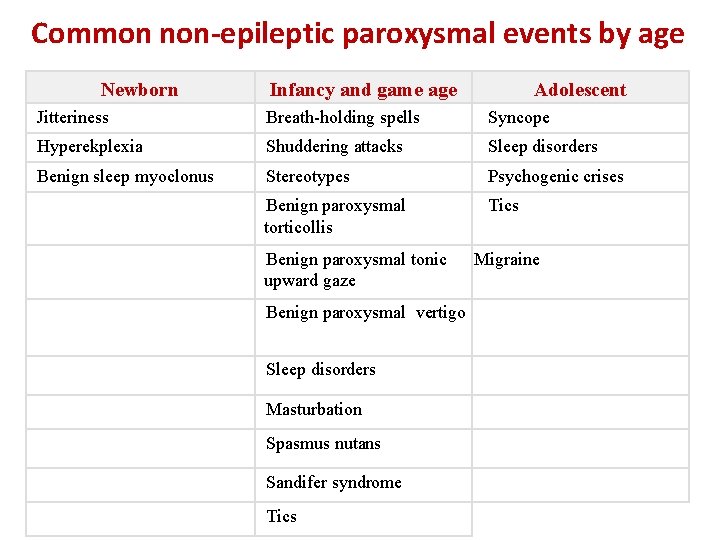
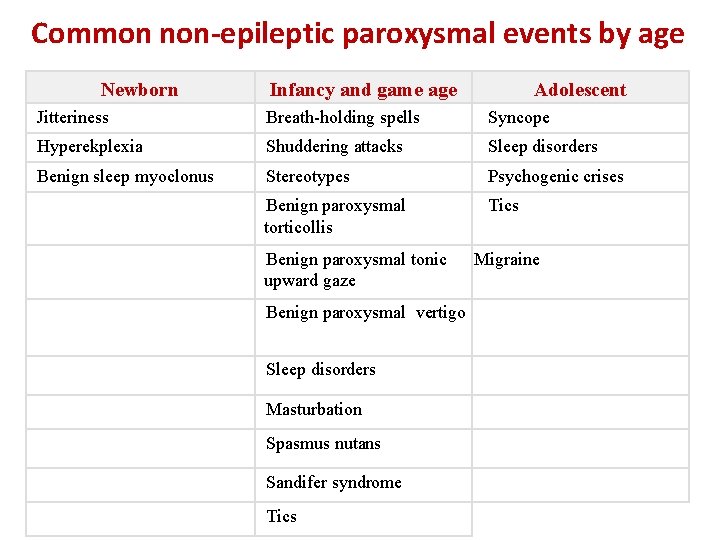
Common non-epileptic paroxysmal events by age Newborn Infancy and game age Adolescent Jitteriness Breath-holding spells Syncope Hyperekplexia Shuddering attacks Sleep disorders Benign sleep myoclonus Stereotypes Psychogenic crises Benign paroxysmal torticollis Tics Benign paroxysmal tonic upward gaze Benign paroxysmal vertigo Sleep disorders Masturbation Spasmus nutans Sandifer syndrome Tics Migraine
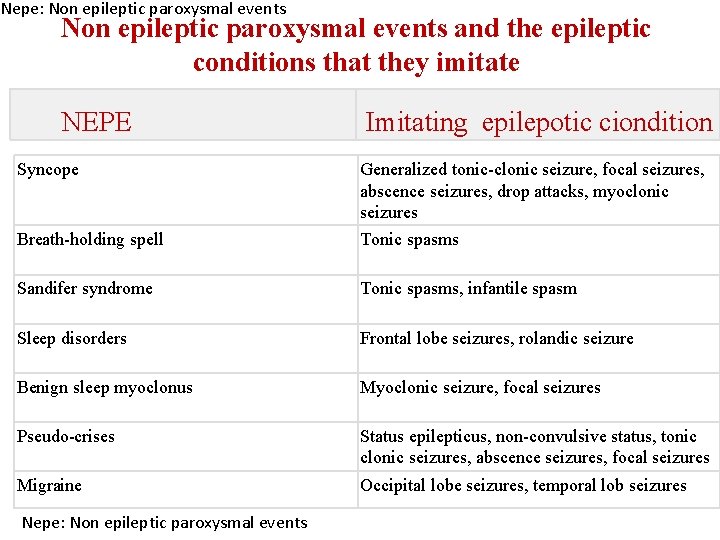
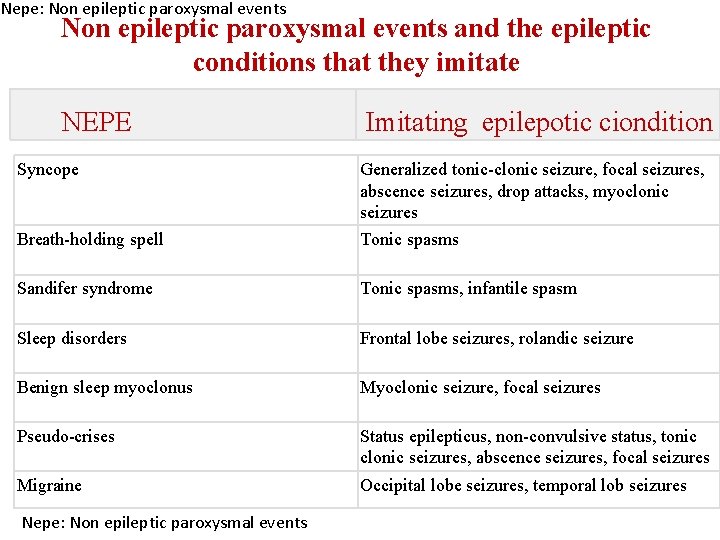
Nepe: Non epileptic paroxysmal events and the epileptic conditions that they imitate NEPE Syncope Imitating epilepotic ciondition Breath-holding spell Generalized tonic-clonic seizure, focal seizures, abscence seizures, drop attacks, myoclonic seizures Tonic spasms Sandifer syndrome Tonic spasms, infantile spasm Sleep disorders Frontal lobe seizures, rolandic seizure Benign sleep myoclonus Myoclonic seizure, focal seizures Pseudo-crises Status epilepticus, non-convulsive status, tonic clonic seizures, abscence seizures, focal seizures Migraine Occipital lobe seizures, temporal lob seizures Nepe: Non epileptic paroxysmal events
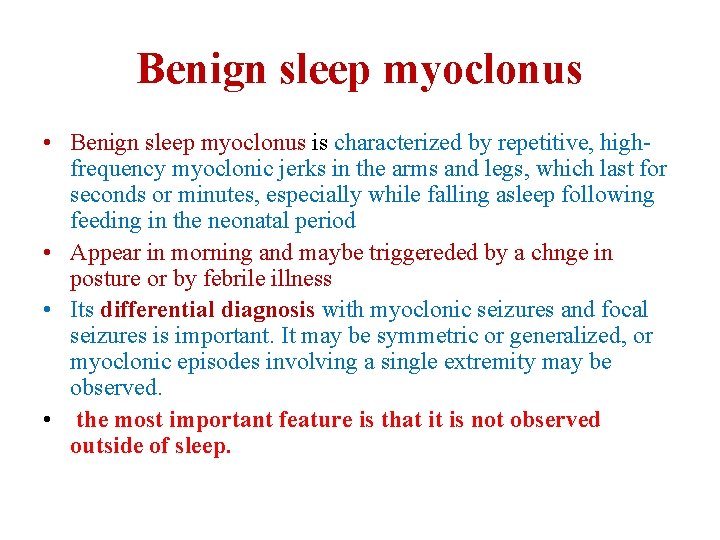
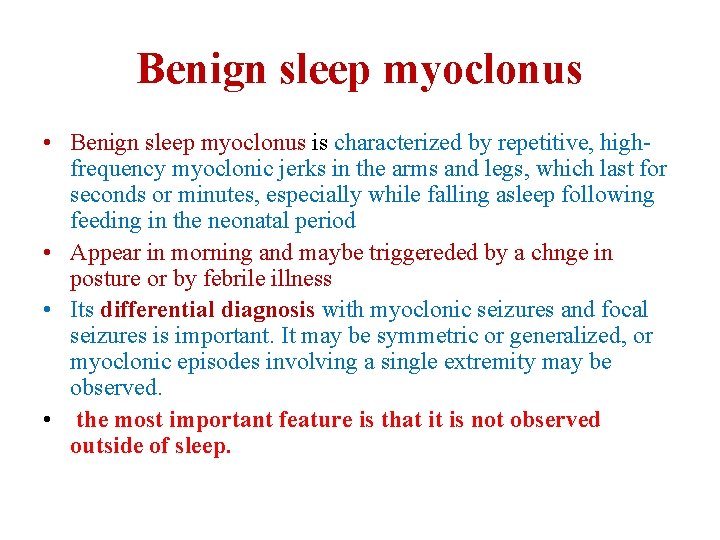
Benign sleep myoclonus • Benign sleep myoclonus is characterized by repetitive, highfrequency myoclonic jerks in the arms and legs, which last for seconds or minutes, especially while falling asleep following feeding in the neonatal period • Appear in morning and maybe triggereded by a chnge in posture or by febrile illness • Its differential diagnosis with myoclonic seizures and focal seizures is important. It may be symmetric or generalized, or myoclonic episodes involving a single extremity may be observed. • the most important feature is that it is not observed outside of sleep.
Benign sleep myoclonus
Jitteriness • is an involuntary movement that is particularly frequent in the newborn • Its hallmark is tremor • The pathogenesis is poorly understood • Jitteriness is often accompanied by other signs of central nervous system excitation, such as hypermotility, hypertonicity, pre-peri-or postnatal events • It must be differentiated from myoclonus and seizure, although they may coexist
Jitteriness
Infancy and school-age period • Breath-holding spells occur between the ages of 6 months and 5 years in children. • Its frequency is 5% • The spells are clinically observed in two forms as cyanotic form and pallid form. • The frequency of the episodes is variable; they may occur a few times a day or every 3– 4 months • Pallid breath-holding spells; the child screams briefly, usually following minor injuries, seeing blood or drawing of blood and painful stimuli (falling, hitting the head) • Afterwards, hypotonia, loss of consciousness, and pale skin occur • The episodes usually last for a period < 60 seconds
Cyanotic breath-holding spells • 65% of breath-holding spells are cyanotic • A stimulant factor (pain, anger or fear) may trigger the episode. • Prolongation of expiration during crying may result in apnea • At the time of breath-holding, the skin color starts to change • This period may result in inspiration or cyanosis may deepen • and secondary hypoxia may be added • Loss of tonus and rarely myoclonic jerks may accompany • A postictal period may be observed depending on the severity of the episode
Breath-holding spells Pallid type cyanotic type
Shuddering attacks • Shuddering attack is an NEPE that initiates with rapid tremor of the head and shapes with continuance of this movement in the shoulder and trunk • The attacks last only for 1– 2 seconds and they are benign movements that recur frequently (sometimes 100 times a day) • Stereotypes • are recurrent, simple movement groups (clapping, shaking arms, and head) that can be stopped voluntarily may be unilateral or bilateral and usually concentrated in the upper extremities and do not occur in the lower extremities these ritual movements including clapping, shaking arms, and shaking the head do not involve complex movement series and complex motor movements • most commonly occur in patients with mental retardation, autism.
Shuddering attacks
Stereotypes
Benign paroxysmal vertigo • Benign paroxysmal vertigo comprises episodes of dizziness that occur suddenly and last for a few minutes with an onset during infancy • The attacks usually occur at ages of 1– 2 years after the child starts walking, and may last up to the age of 6 years • Nausea, vomiting, and paleness may be prominent. The child is awake, suddenly becomes panicked, as if frightened, and does not want to move until the event ends. • If the child is urged to walk during this period, he/she is unbalanced.
Benign paroxysmal torticollis • is a movement disorder characterized by recurrent episodes with an onset at the age of 2– 8 months in infancy. • Typically, it disappears at the age of 3– 5 years. Episodes may last for 1– 2 hours or for days • The child keeps his/her head turned to one direction; vomiting and paleness may accompany. It is notable that the period and frequency of the episodes decrease as the age gets older.
Adolescence • Syncope • Paroxysmal consciousness disorders with vascular, cardiac or neurologic origin characterized by sudden loss of consciousness, loss of tonus, falling, and spontaneous recovery in a short time are called syncope. • The frequency in the first two decades is about 15% • Vasovagal syncope • is the most common form of syncope in children • It constitutes approximately half of syncope attacks • The mechanism involves sudden loss of vasomotor tonus and as a result, systemic hypotension, bradycardia, and asystole Hypotension and paradoxical bradycardia are present
Neuromuscular disorders
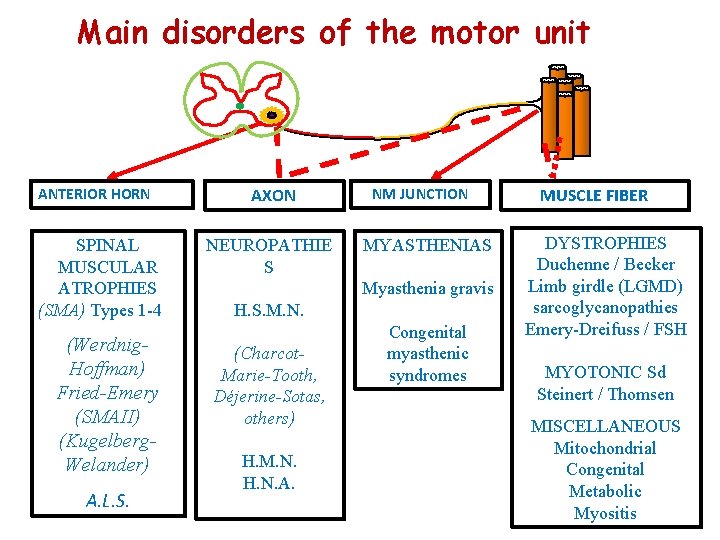
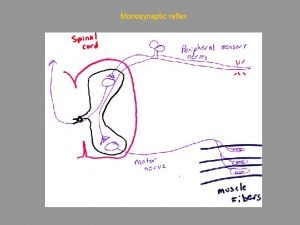
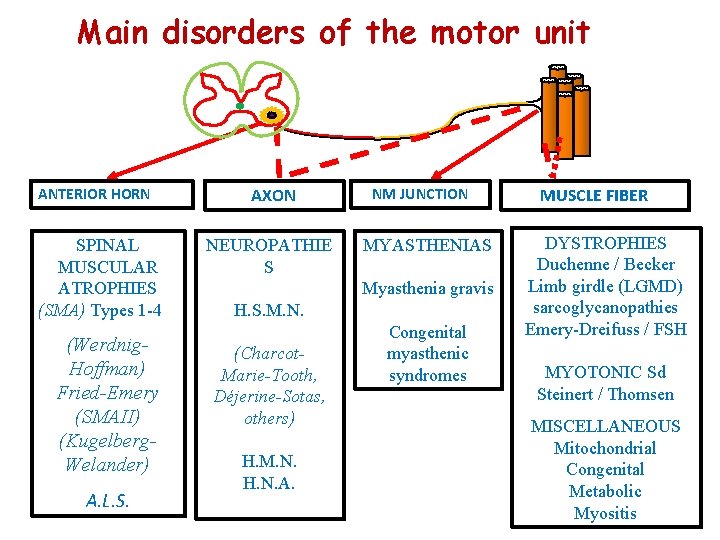
Main disorders of the motor unit ANTERIOR HORN SPINAL MUSCULAR ATROPHIES (SMA) Types 1 -4 (Werdnig. Hoffman) Fried-Emery (SMAII) (Kugelberg. Welander) A. L. S. AXON NEUROPATHIE S NM JUNCTION MYASTHENIAS Myasthenia gravis H. S. M. N. (Charcot. Marie-Tooth, Déjerine-Sotas, others) H. M. N. H. N. A. Congenital myasthenic syndromes MUSCLE FIBER DYSTROPHIES Duchenne / Becker Limb girdle (LGMD) sarcoglycanopathies Emery-Dreifuss / FSH MYOTONIC Sd Steinert / Thomsen MISCELLANEOUS Mitochondrial Congenital Metabolic Myositis
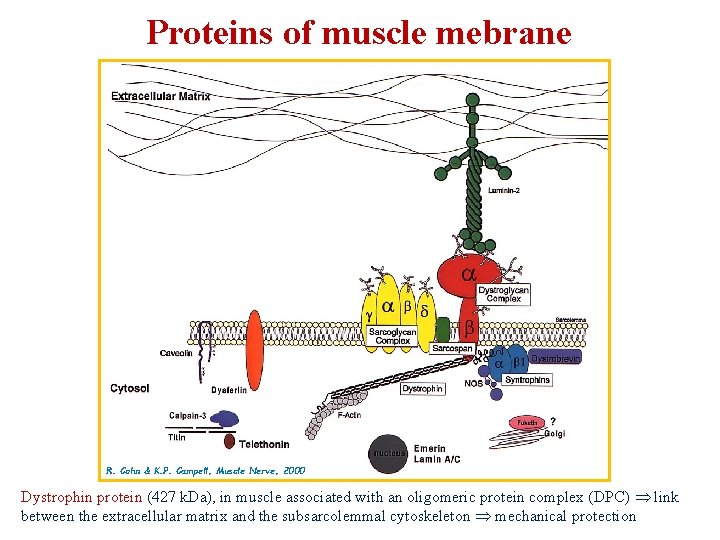
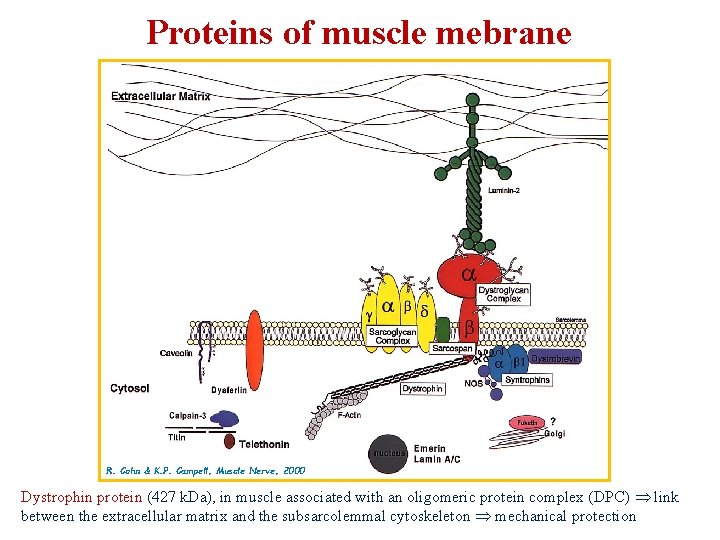
Proteins of muscle mebrane R. Cohn & K. P. Campell, Muscle Nerve, 2000 Dystrophin protein (427 k. Da), in muscle associated with an oligomeric protein complex (DPC) link between the extracellular matrix and the subsarcolemmal cytoskeleton mechanical protection
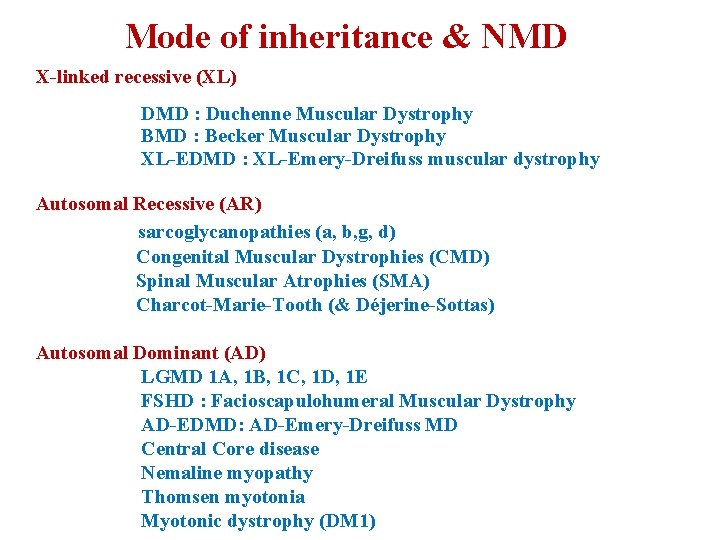
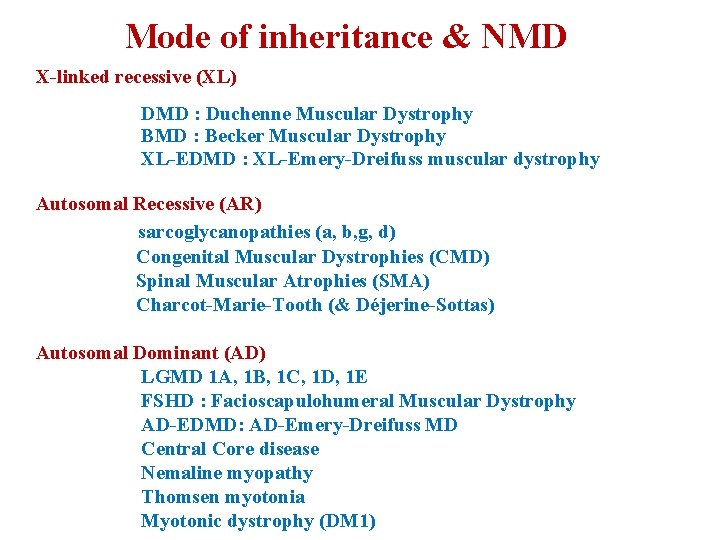
Mode of inheritance & NMD X-linked recessive (XL) DMD : Duchenne Muscular Dystrophy BMD : Becker Muscular Dystrophy XL-EDMD : XL-Emery-Dreifuss muscular dystrophy Autosomal Recessive (AR) sarcoglycanopathies (a, b, g, d) Congenital Muscular Dystrophies (CMD) Spinal Muscular Atrophies (SMA) Charcot-Marie-Tooth (& Déjerine-Sottas) Autosomal Dominant (AD) LGMD 1 A, 1 B, 1 C, 1 D, 1 E FSHD : Facioscapulohumeral Muscular Dystrophy AD-EDMD: AD-Emery-Dreifuss MD Central Core disease Nemaline myopathy Thomsen myotonia Myotonic dystrophy (DM 1)
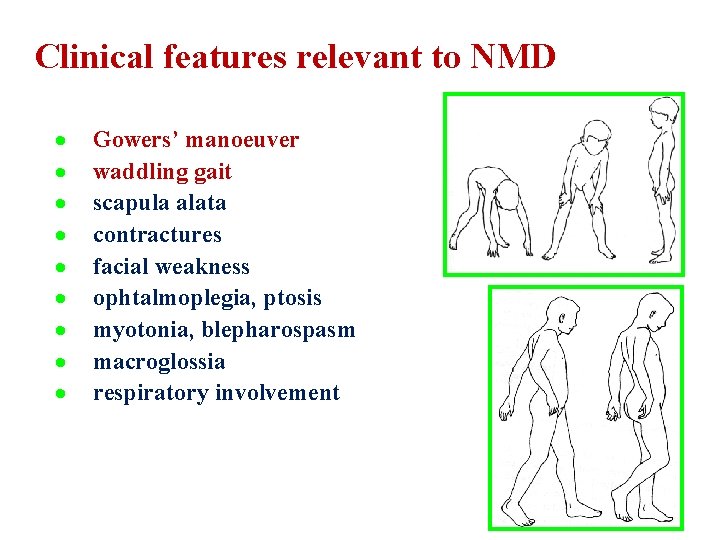
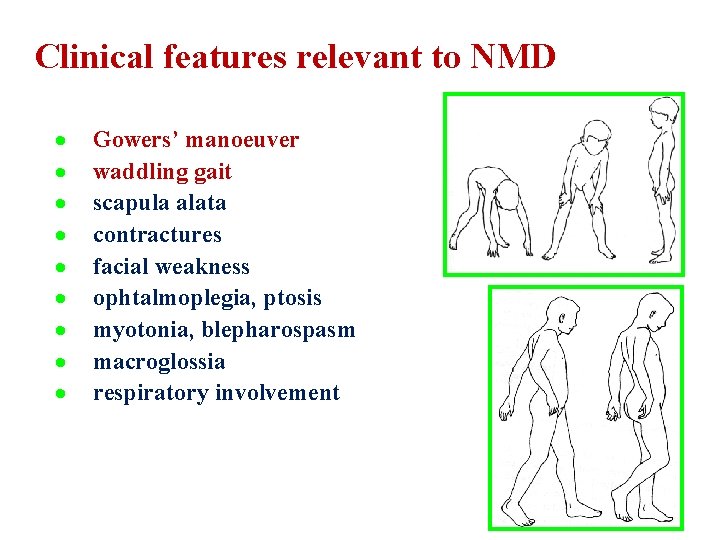
Clinical features relevant to NMD · · · · · Gowers’ manoeuver waddling gait scapula alata contractures facial weakness ophtalmoplegia, ptosis myotonia, blepharospasm macroglossia respiratory involvement
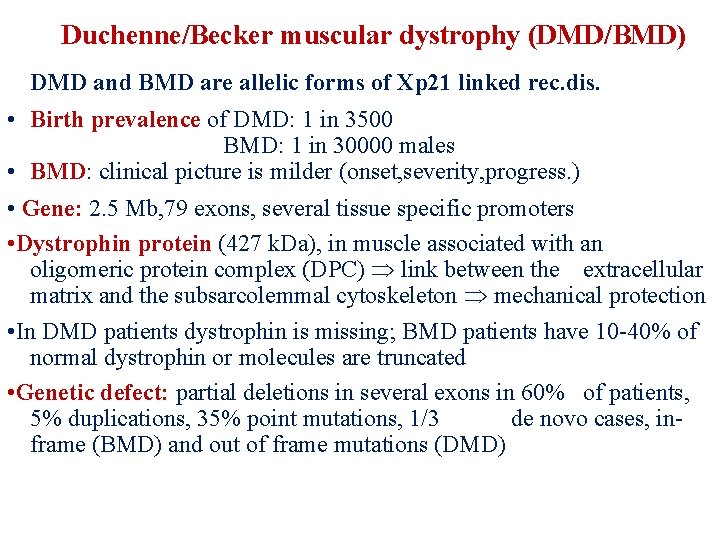
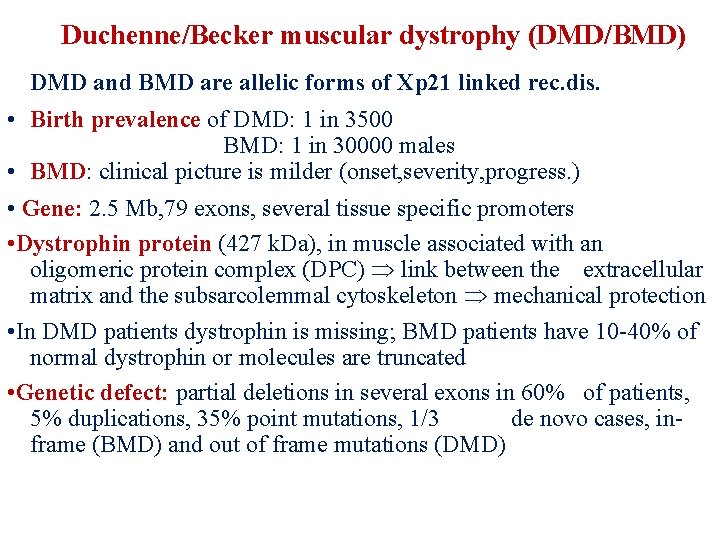
Duchenne/Becker muscular dystrophy (DMD/BMD) • DMD and BMD are allelic forms of Xp 21 linked rec. dis. • Birth prevalence of DMD: 1 in 3500 BMD: 1 in 30000 males • BMD: clinical picture is milder (onset, severity, progress. ) • Gene: 2. 5 Mb, 79 exons, several tissue specific promoters • Dystrophin protein (427 k. Da), in muscle associated with an oligomeric protein complex (DPC) link between the extracellular matrix and the subsarcolemmal cytoskeleton mechanical protection • In DMD patients dystrophin is missing; BMD patients have 10 -40% of normal dystrophin or molecules are truncated • Genetic defect: partial deletions in several exons in 60% of patients, 5% duplications, 35% point mutations, 1/3 de novo cases, inframe (BMD) and out of frame mutations (DMD)
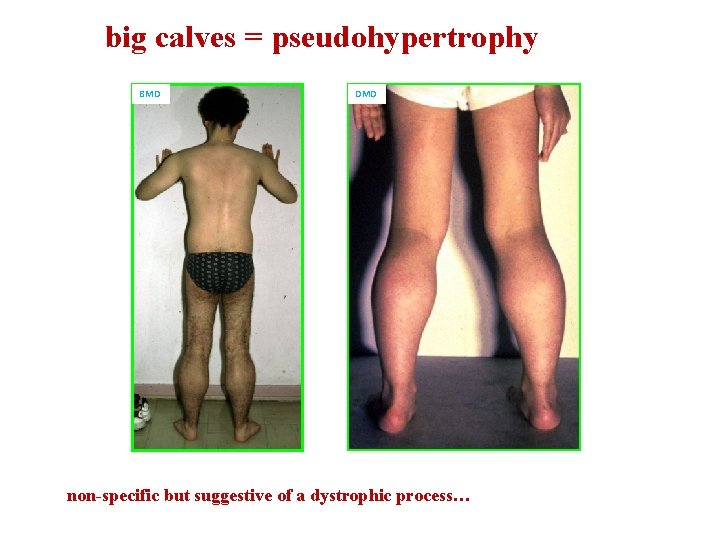
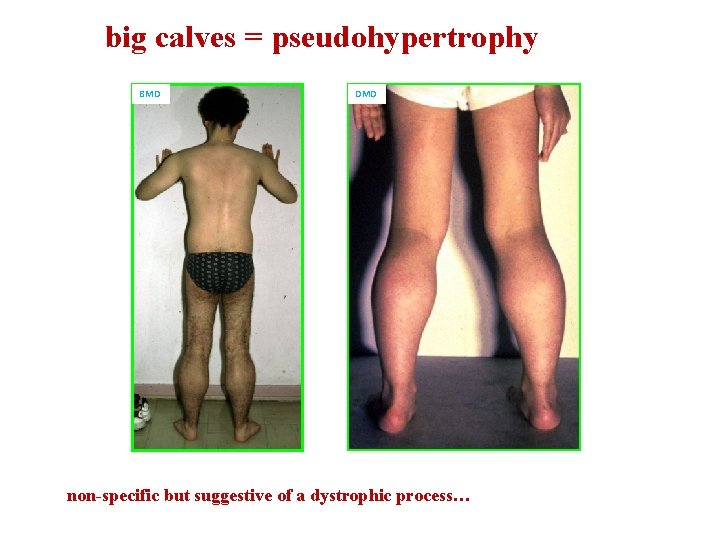
big calves = pseudohypertrophy BMD DMD non-specific but suggestive of a dystrophic process…

Scapula alata – scapular winging suggestive of FSHD when asymmetrical but occurs in LGMD, DMD, others…
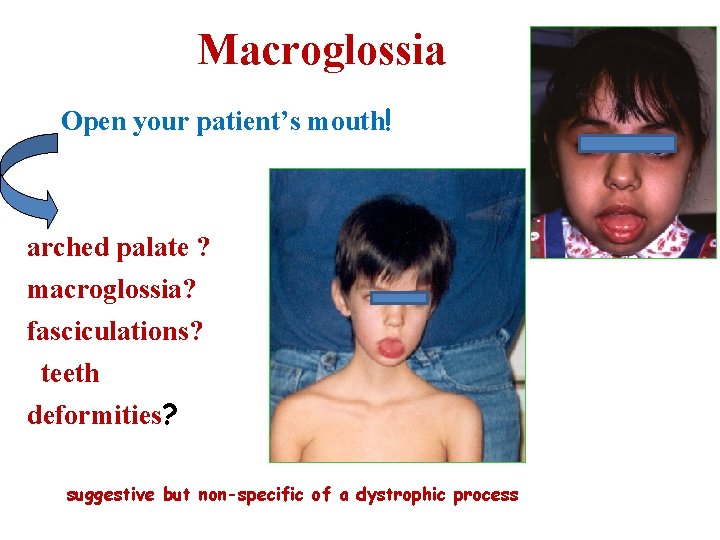
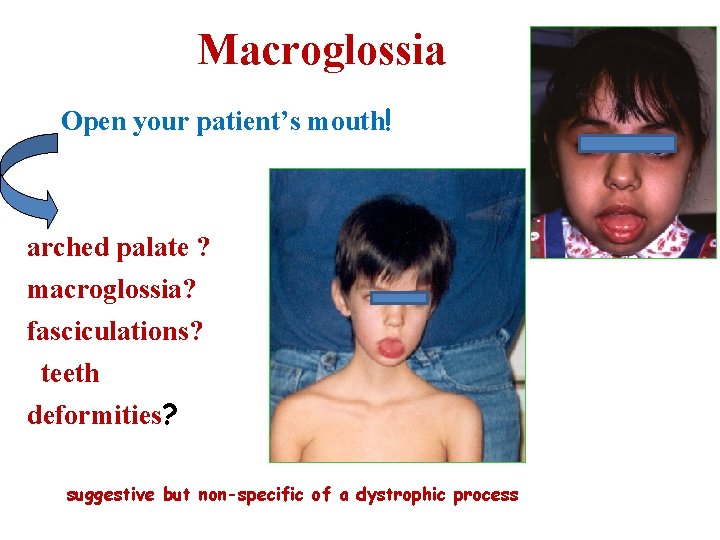
Macroglossia Open your patient’s mouth! arched palate ? macroglossia? fasciculations? teeth deformities? suggestive but non-specific of a dystrophic process
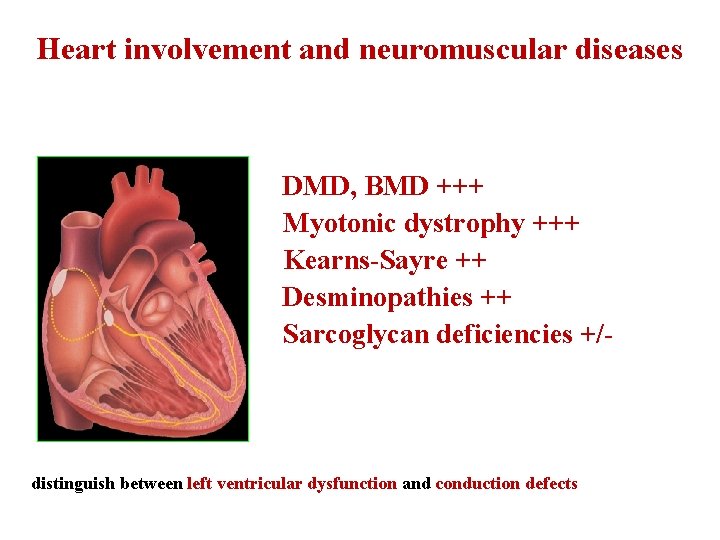
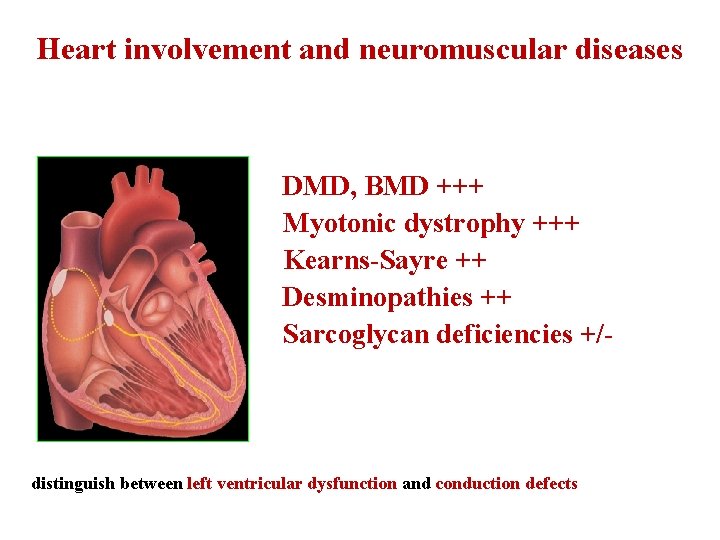
Heart involvement and neuromuscular diseases DMD, BMD +++ Myotonic dystrophy +++ Kearns-Sayre ++ Desminopathies ++ Sarcoglycan deficiencies +/- distinguish between left ventricular dysfunction and conduction defects
Thank you
 Breath holding spells
Breath holding spells Nikki mehta
Nikki mehta Territorial matrix vs interterritorial matrix
Territorial matrix vs interterritorial matrix Classification of anticonvulsant drug
Classification of anticonvulsant drug Basic mechanisms underlying seizures and epilepsy
Basic mechanisms underlying seizures and epilepsy Non epileptic seizures
Non epileptic seizures Pediatric seizures
Pediatric seizures Lorna myers pnes
Lorna myers pnes Psychomotor seizures
Psychomotor seizures Psychomotor seizures
Psychomotor seizures Hemorrhagic irregular tissue fragments
Hemorrhagic irregular tissue fragments Health education for meningitis slideshare
Health education for meningitis slideshare Seizures
Seizures Zomisamide
Zomisamide Tonic vs clonic
Tonic vs clonic Seizure
Seizure Simple partial seizures vs complex
Simple partial seizures vs complex Simple partial seizures vs complex
Simple partial seizures vs complex Acondicionamiento neuromuscular dibujos
Acondicionamiento neuromuscular dibujos Pnf stretching definition
Pnf stretching definition Hypocalcemia neuromuscular excitability
Hypocalcemia neuromuscular excitability Synaptic junction
Synaptic junction Huso neuromuscular
Huso neuromuscular Neurofibrils
Neurofibrils Neuromuscular
Neuromuscular Residual neuromuscular blockade
Residual neuromuscular blockade Focus figure 9.2 excitation-contraction coupling
Focus figure 9.2 excitation-contraction coupling Intubating dose succinylcholine
Intubating dose succinylcholine Neuromuscular junction
Neuromuscular junction Neuromuscular junction
Neuromuscular junction El sistema nervioso
El sistema nervioso Neostigmine atropine reversal
Neostigmine atropine reversal Figure 12
Figure 12 Placas neuromusculares
Placas neuromusculares Solid thyroid nodule
Solid thyroid nodule Sote neptun
Sote neptun Itc semmelweis
Itc semmelweis Retikulinfasern leber
Retikulinfasern leber Semmelweis
Semmelweis Orthodontics semmelweis
Orthodontics semmelweis Semmelweis
Semmelweis Semmelweis egyetem konzerváló fogászati klinika budapest
Semmelweis egyetem konzerváló fogászati klinika budapest