Disease of neuromuscular junction The Neuromuscular Junction is


- Slides: 26
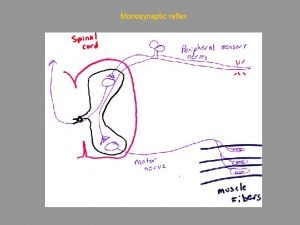
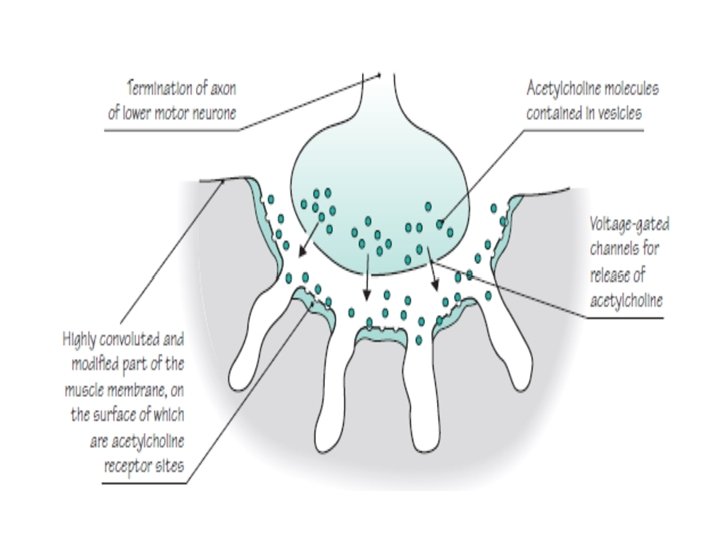
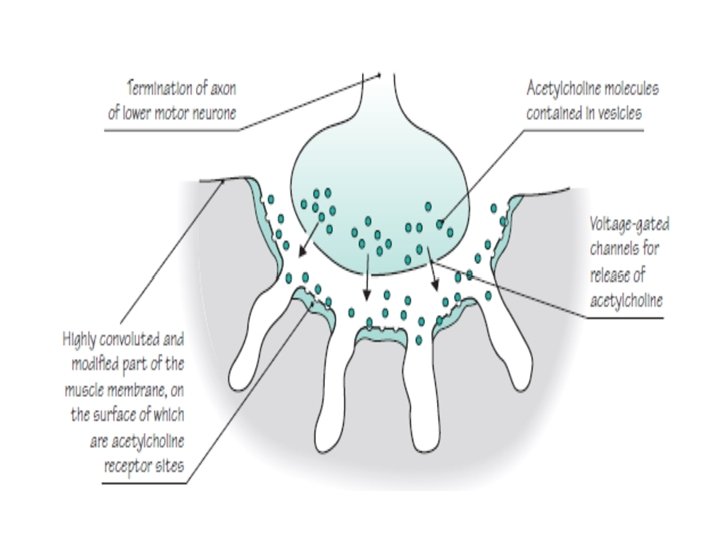
Disease of neuromuscular junction The Neuromuscular Junction is composed of : Presynaptic membrane Postsynaptic membrane Synaptic cleft Presynaptic membrane contains vesicles with Acetylcholine (ACh) which are released into synaptic cleft in a calcium dependent manner ACh attached to ACh receptors (ACh. R) on postsynaptic membrane The Acetylcholine receptor (Ach R) is a sodium channel that opens when bound by Ach : There is a partial depolarization of the postsynaptic membrane and this causes an excitatory postsynaptic potential (EPSP) If enough sodium channels open and a threshold potential is reached" a muscle action potential is generated in the postsynaptic membrane
• Myasthenia gravis • It is an acquired autoimmune disorder, clinically characterized by weakness of skeletal muscles and fatigability on exertion. • pathophysiology • In MG, antibodies(lg. G) are directed toward the acetylcholine Nicotinic receptors at the neuromuscular junction of skeletal muscles resulting in; • Decreased number of receptors at the motor end-plate • Reduced postsynaptic membrane folds • Widened synaptic cleft

• Role of thymus • 75 % of cases of MG the thymus was abnormal • 65% had thymus hyperplasia • 10 % had thymoma (rarely in children) • epidemiology • MG has two peak onset; • first at 20 -30 years of age, mostly affect Females • The second at 40 -60 years of age, mostly affect males • (Overall, female are more frequently affected than male in a ratio of approximately 3 -2 • familial cases are rare.
• Clinical Presentation (fatigable) Fluctuating weakness increased by exertion Ø Weakness increases during the day and improves with rest Extraocular muscle weakness Ø Ptosis is present initially in 50% of patients. Ø during the active course of disease in 90% of patients Head extension and flexion weakness Ø Weakness may be worse in proximal muscles
Ocular muscle weakness Ø Asymmetric, usually affects more than one extraocular muscle and is not limited to muscles Innervated by one cranial nerve Ø Ptosis caused by eyelid weakness Ø Diplopia is Very common

Bulbar muscle weakness Palatal muscles Ø Nasal voice, nasal regurgitation Ø Chewing may become difficult Ø Severe jaw weakness may cause jaw to hang open Ø Swallowing may be difficult and aspiration may occur with fluids--coughing and choking while drinking
• Progression of disease q Usually spreads from ocular to facial to bulbar to truncal and limb muscles. q Often, symptoms may remain limited to EOM and eyelid muscles for years q The disease remains ocular in 16% of patients. • Remissions q Spontaneous remission rare q Most remissions with treatment occur within the first three years
• Respiratory muscle weakness of the intercostal muscles and the diaghram may result in C 02 retention due to hypoventilation , and may cause a neuromuscular emergency Weakness of pharyngeal muscles may collapse the upper airway So Monitor vital capacity is important
• Co-existing autoimmune disease Hyperthyroidism: - Occurs in 10 -15% MG patients, exophthalmos and tachycardia point to hyperthyroidism , weakness may not improve with treatment of MG alone in patients with co-existing hyperthyroidism Rheumatoid arthritis Scleroderma Lupus Note: in MG patients. neurological examination is normal with only PROXIMALWEAKNESS
• Differential diagnosis • Amyotrophic Lateral Sclerosis • Brain stem gliomas • Lambert-Eaton"Myasthenic Syndrome • Thyroid disease • Botulism
• Investigation • Laboratory study Anti-acetylcholine receptor antibody Positive in 74% 80% in generalized myasthenia gravis. 50% of patients with pure ocular myasthenia Antistriated muscle AB Present in 84% of patients with thymoma who are younger than 40 years
• Imaging studies Chest x-ray • Plain anteroposterior and lateral views may identify a thymoma as an anterior mediastinal mass. Chest CT scan is mandatory to identify thymoma MRI of the brain and orbits may help to rule out other causes of cranial nerve deficits but should not be used routinely
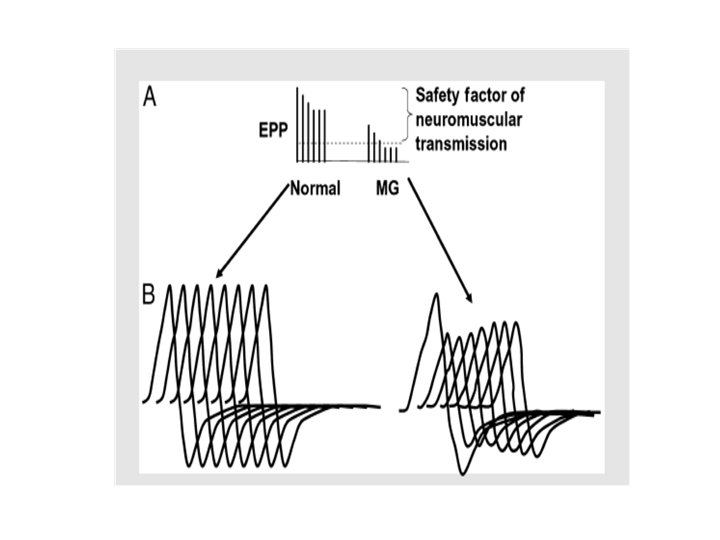
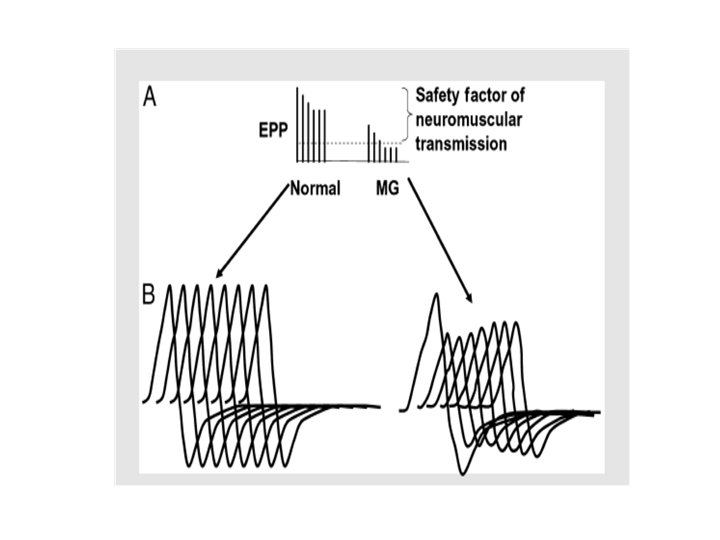
• Electrodiagnostic studies I. Repetitive nerve stimulation RNS 2. Single fiber electromyography (SFEMG) SFEMG is more sensitive than RNS in MG (but it needs much time) Any decrement over 10% is considered abnormal Should not test clinically normal muscle Proximal muscles are better tested • Most common employed stimulation rate is 3 Hz, several factors can affect RNS results e. g. lower temperature increases the amplitude of the compound muscle action potential, and many patients report clinically significant improvement in cold temperatures
• Pharmacological testing • Edrophonium(Tensolon test) Patients with MG have low numbers of ACh. R at the NMJ Ach released from the motor nerve terminal is metabolized by Acetylcholine esterase Edrophonium is a short acting Acetylcholine Esterase Inhibitor that improves muscle weakness Evaluate weakness (i. e. ptosis and ophthalmoplegia) before and after administration
• Treatment of MG • Main line of Rx are: ACh. E inhibitors Immunomodulating therapies Plasmapharesis Thymectomy (Important in treatment, especially if thymoma is present)
• ACh. E inhibitors • Pyridostigmine bromide (Mestinon) • Starts working in 30 -60 minutes and lasts 3 -6 hours • Adult dose: • 60 -360 mg/d PO • 2 mg IV IM q 2 - 3 h • Caution Check for cholinergic crisis due to depolarisation block of motor end plates, with muscle fasciculation, paralysis, pallor, sweating, excessive salivation and small pupils • myasthenic crisis severe weakness due to exacerbation of myasthenia • This may be distinguished by the clinical features and, if necessary, by the injection of a small dose of Edrophonium.
• Others: Neostigmine Bromide • Propantheline( 15 mg tablets) • Given if patient develops abdominal pain/diarrhea, l 5 mg tds or 15 mg taken 30 minutes before each dose of Pyridostigmine • Immunomodulating therapies • prednisolone Most commonly used corticosteroid in MG Significant improvement is often seen after a decreased antibody titer which is usually 1 -4 months No single dose regimen is accepted
• Azathioprine Start on 25 mg bid Increase by 25 mg/day until patient is on a dose of 2. 5 mg/kg BW per day Assess full blood count and LFTs before starting treatment and after a few days of initiation, then weekly for 8 weeks. • cyclosporine • Methotrexate (in adults) 7. 5 -20 mg once weekly • mycophenolate mofetil
• Thymectomy Done when indications for thymectomy present Patient with thymoma - the thymectomy is indicated all . If no thymoma - the patient age, symptoms, duration, severity, response to medication. Thymectomy is not recommended for the neonatal type of myasthenia gravis. In juvenile form - thymectomy for patient with more severe symptoms and lack of response to medical therapy.
• plasma exchange and IVIG this is given in : acute fulminant MG Preoperative (sometime) myasthenic crises • As Five exchanges (3 -4 L/exchange) • IV immunoglobulin- 400 mgl. Kg per day for 5 clays
• prognosis Untreated MG carries a mortality rate of 25 -30 % Treated MG has a 4% mortality rate 40% have ONLY ocular symptoms • Complications of MG Respiratory failure Dysphagia Complications secondary to drug treatment e. g. Long term steroid use like Osteoporosis, cataracts, hyperglycemia, HTN , gastritis, peptic ulcer disease
• Lambert Eaton myasthenic syndrome It is a Presynaptic disorder of the NMJ Voltage gates calcium channel antibodies impede release of acetylcholine • Presented as Weakness more of Lower extremities than Upper Extremities bulbar and ocular muscles less often involved decreased reflexes - post tetanic potentiation Autonomic Nervous System involvement Associated with a cancer in the majority of patients( paraneoplastic) Underlying cancer may be previously unrecognized, Small cell lung cancer is the most common
• Treatment: Underlying cancer Guanidine 3, 4 diamino pyridine
 Neuromuscular junction
Neuromuscular junction Synaptic junction
Synaptic junction Neuromuscular junction
Neuromuscular junction T tubule
T tubule Muscular contraction
Muscular contraction End-plate potential vs action potential
End-plate potential vs action potential Conjunction function
Conjunction function Communicable disease and non communicable disease
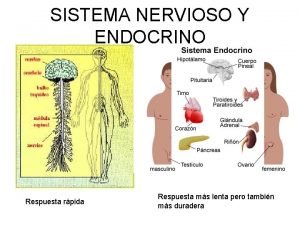
Communicable disease and non communicable disease Hypocalcemia neuromuscular excitability
Hypocalcemia neuromuscular excitability Tono muscular
Tono muscular Definition of anesthesia
Definition of anesthesia Huso neuromuscular
Huso neuromuscular Neuromuscular blocking agents
Neuromuscular blocking agents Acondicionamiento neuromuscular dibujos
Acondicionamiento neuromuscular dibujos Neurofibrils
Neurofibrils Estructura de la placa neuromuscular
Estructura de la placa neuromuscular Proprioceptive neuromuscular facilitation
Proprioceptive neuromuscular facilitation Neuromuscular
Neuromuscular Dạng đột biến một nhiễm là
Dạng đột biến một nhiễm là Biện pháp chống mỏi cơ
Biện pháp chống mỏi cơ Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ độ dài liên kết
độ dài liên kết Chó sói
Chó sói Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan điện thế nghỉ
điện thế nghỉ Phối cảnh
Phối cảnh Một số thể thơ truyền thống
Một số thể thơ truyền thống