Neurological Emergencies Coma Seizures Syncope Stroke Coma H

- Slides: 49
Neurological Emergencies Coma, Seizures, Syncope, Stroke
Coma H State of unconsciousness from which patient cannot be aroused
Coma H Unconsciousness = Immediate Life Threat H Loss of airway H Aspiration
Coma H Management of ABC’s must come before investigation of cause
Airway H H Open, clear, maintain If trauma present or no history available, immediately control C -spine
Breathing H H H Assess presence, adequacy High concentration O 2 immediately on all patients with decreased LOC Assist if respiratory rate, tidal volume inadequate
Circulation Pulses? Perfusion?
After ABC’s stabilized. . . H H Quickly investigate cause DERM
D = Depth of coma H H What does patient respond to? How does he respond?
E = Eyes H H H Pupils equal, dilated, constricted, Responsive to light? How?
R = Respiratory pattern H H H Rate? Unusually deep or shallow? Altered pattern?
M = Motor Function H H H Evidence of paralysis? Movement on stimulation? How?
Vital Signs H H H Shock? Increased ICP? Arrhythmias?
Head to Toe Survey H H H Injuries causing coma? Injuries caused by fall? What do the scene, bystanders tell you?
Possible Causes H H Not enough oxygen Not enough sugar Not enough blood flow to deliver O 2, sugar Direct brain injury H Structural (trauma) H Metabolic (toxins, infections, temperature)
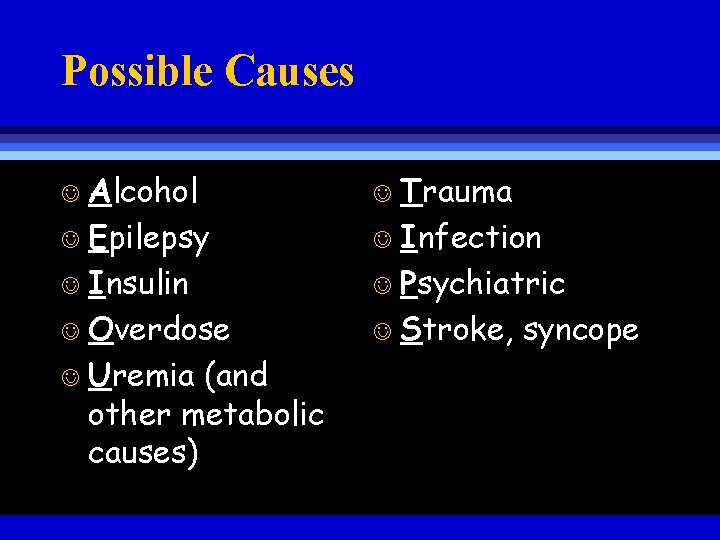
Possible Causes Alcohol J Epilepsy J Insulin J Overdose J Uremia (and other metabolic causes) J Trauma J Infection J Psychiatric J Stroke, syncope J
Management H H Secure airway Protective reflexes may be lost Immobilize spine unless absolutely certain injury not present Spinal injury not suspected - patient on left side
Management H High concentration O 2 Assist ventilation as needed Monitor neurological/vital signs every 5 minutes
Management H H H Protect patient’s eyes on long transports (tape shut, moist pads) Patient may hear, understand even though unable to respond Treat, reassure accordingly
Seizures H H Episodes of uncoordinated electrical activity in brain Signs/symptoms depend on area involved

Epilepsy H Tendency to have repeated episodes of seizure activity
Seizure Types H H Grand mal (major motor) Petit mal (absence) Focal motor (simple partial) Psychomotor (complex partial)
Grand Mal Seizure H Aura H Sensation coming before convulsion H Patient may recognize as sign of impending seizure H May help locate origin of seizure in brain
Grand Mal Seizure H Convulsion H Loss of consciousness H Tonic phase - rigidity H Clonic phase - rhythmic jerking, incontinence, ineffective breathing
Grand Mal Seizure H Post-ictal Phase H H Exhaustion Drowsiness Headache Possible hemiparesis (Todd’s paralysis)
Petit Mal Seizure H H H Loss of consciousness No loss of postural tone More common in children
Focal Motor Seizure H H Rhythmic jerking of limb, one side of body No loss of consciousness
Psychomotor Seizure H H Loss of consciousness Sterotyped movements (automatisms) H May look purposeful, but aren’t H Lip smacking, movements of hands H May be called in as “drunk”, “O. D. ”, “psych patient”
Generalized Seizure Management H During seizure H Remove from potential harm H Do not forcibly restrain H Roll on side H Avoid putting anything in mouth
Generalized Seizure Management H After seizure ends H Assess ABC’s H Clear airway Most common cause of seizure deaths is post-ictal airway loss
Generalized Seizure Management H High concentration O 2 - immediately!! H Assist breathing if ventilation inadequate
Generalized Seizure Management H Obtain history/physical H Trauma that could have caused, been caused by seizure H Anti-seizure medications H Neuro/vital signs every 5 minutes H If patient ventilating adequately, transport on left side
Seizures H H Anything that injures brain cause seizures (AEIOU/TIPS) Do not assume seizures are due to idiopathic epilepsy until proven otherwise
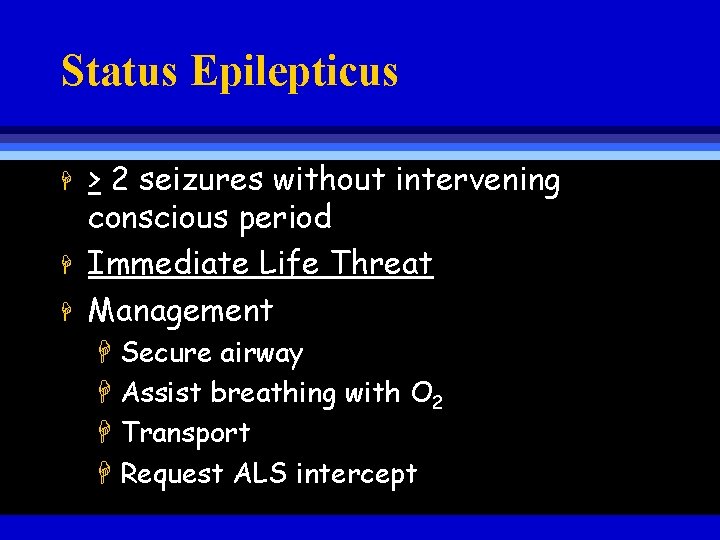
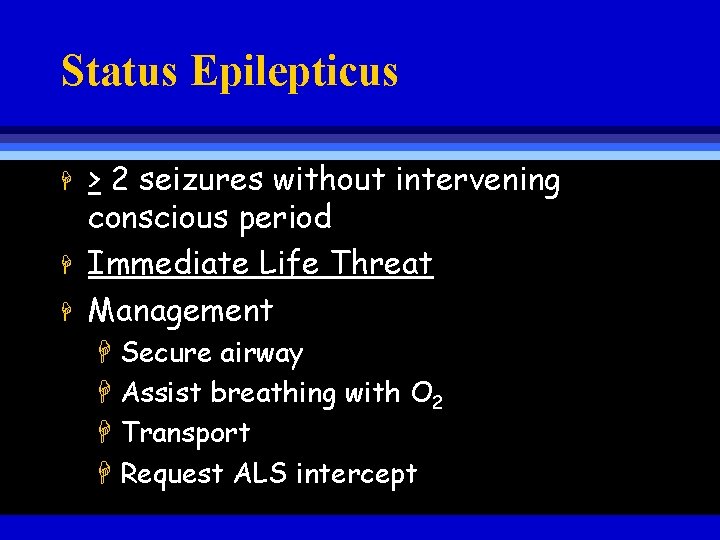
Status Epilepticus H H H > 2 seizures without intervening conscious period Immediate Life Threat Management H Secure airway H Assist breathing with O 2 H Transport H Request ALS intercept
Syncope Fainting J Sudden, temporary loss of consciousness J Caused by lack of blood flow to brain J
Causes J Stress, fright, pain (vasovagal syncope) J Orthostatic hypotension (BP fall on standing) Decreased blood volume J Increased size of vascular space J J Decreased cardiac output J Prolonged forceful coughing
Management J ABCs J Keep patient supine, elevate lower extremities J Oxygen J Assess underlying cause
CVA J Cerebrovascular J Stroke accident
CVA H H Damage of portion of brain due to interruption of blood supply Mechanisms H Thrombosis H Hemorrhage H Embolism
Thrombosis H H Blockage of vessel by thrombus Usually forms at area narrowed by atherosclerosis Typically in older persons Frequently occurs during sleep
Hemorrhage H H H Vessel ruptures Associated with hypertension, aneurysms of cerebral blood vessels Usually characterized by H H Sudden onset Severe signs, symptoms
Embolism H H Blood clots, plaque fragments travel through vessel; lodge, block flow Often associated with: H Atherosclerosis of carotids H Chronic atrial fibrillation
Signs/Symptoms H Alterations in consciousness H Altered affect H Confusion H Dizziness H Coma
Signs/Symptoms H Localizing signs H Paralysis H Loss of sensation H Loss of speech H Unilateral blindness H Loss of vision in half of visual field of both eyes H Unequal pupils
Signs/Symptoms H H H Seizures Headache Stiff neck
Transient Ischemic Attacks H H TIAs “Little strokes” Produce deficits that resolve completely in <24 hours Frequently precede CVA
Management H H H Assess ABC’s Protect airway High concentration O 2 Vital signs every 5 -10 minutes Note increased BP, irregular pulse
Management H H H Nothing by mouth Avoid rough handling Transport paralyzed side down Guard your conversation Patients who cannot speak may still understand!
Management H H CVAs caused by thrombus, embolus may be reversible with thrombolytics (clot busters) Early recognition, rapid transport to appropriate facility is critical