Neonatal mortality and encephalopathy JEANIE CHEONG NEONATOLOGIST ROYAL


- Slides: 32

Neonatal mortality and encephalopathy JEANIE CHEONG NEONATOLOGIST ROYAL WOMEN’S HOSPITAL, MELBOURNE, AUSTRALIA
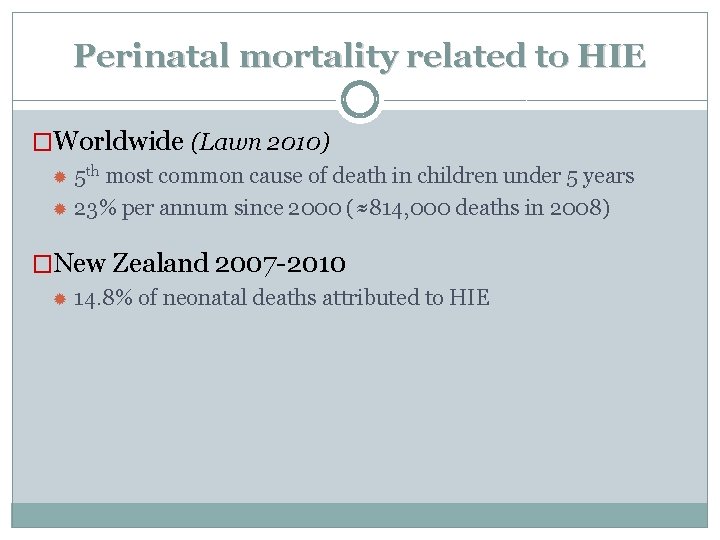
Perinatal mortality related to HIE �Worldwide (Lawn 2010) 5 th most common cause of death in children under 5 years 23% per annum since 2000 (≈814, 000 deaths in 2008) �New Zealand 2007 -2010 14. 8% of neonatal deaths attributed to HIE
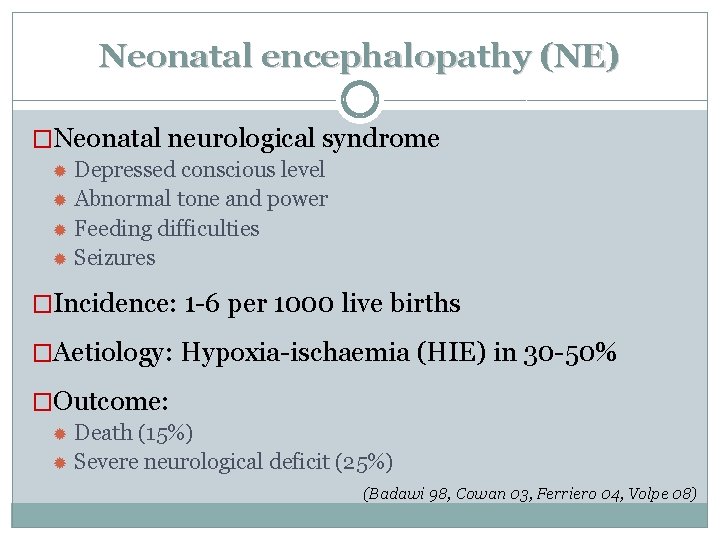
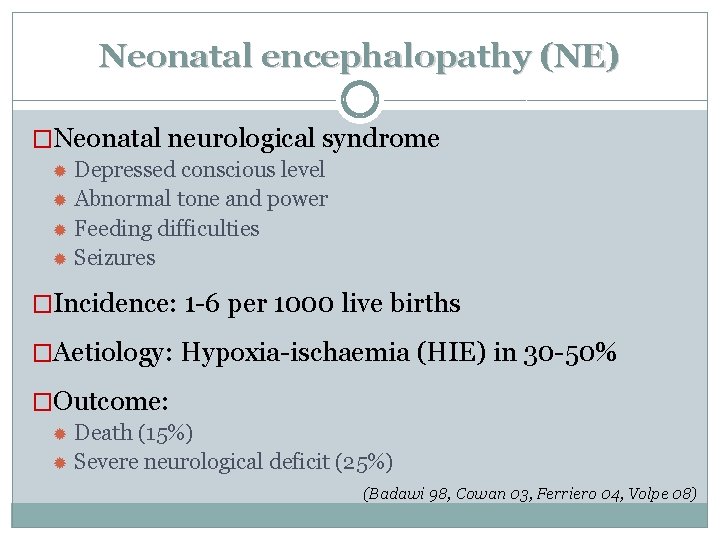
Neonatal encephalopathy (NE) �Neonatal neurological syndrome Depressed conscious level Abnormal tone and power Feeding difficulties Seizures �Incidence: 1 -6 per 1000 live births �Aetiology: Hypoxia-ischaemia (HIE) in 30 -50% �Outcome: Death (15%) Severe neurological deficit (25%) (Badawi 98, Cowan 03, Ferriero 04, Volpe 08)
Diagnostic & Prognostic tools in HIE �Clinical evaluation �Biochemistry �Electrophysiology �Neuroimaging
Clinical evaluation
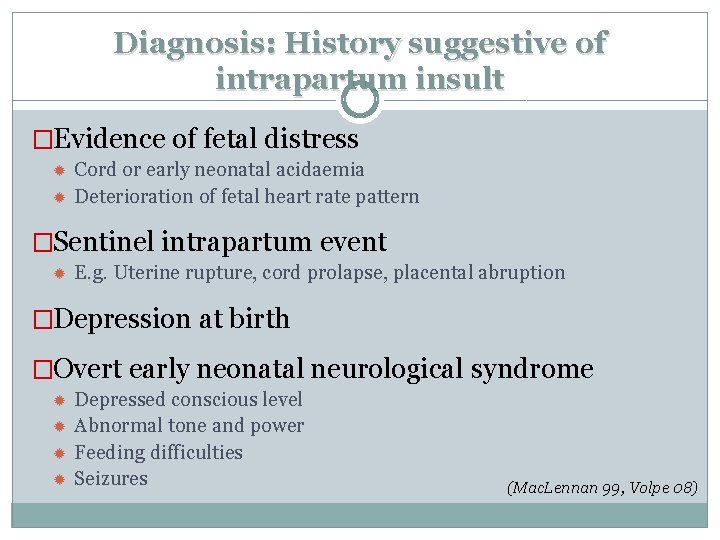
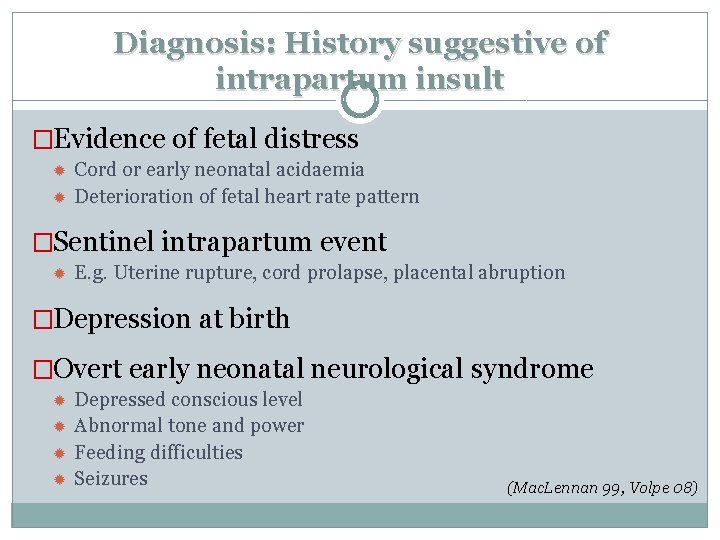
Diagnosis: History suggestive of intrapartum insult �Evidence of fetal distress Cord or early neonatal acidaemia Deterioration of fetal heart rate pattern �Sentinel intrapartum event E. g. Uterine rupture, cord prolapse, placental abruption �Depression at birth �Overt early neonatal neurological syndrome Depressed conscious level Abnormal tone and power Feeding difficulties Seizures (Mac. Lennan 99, Volpe 08)
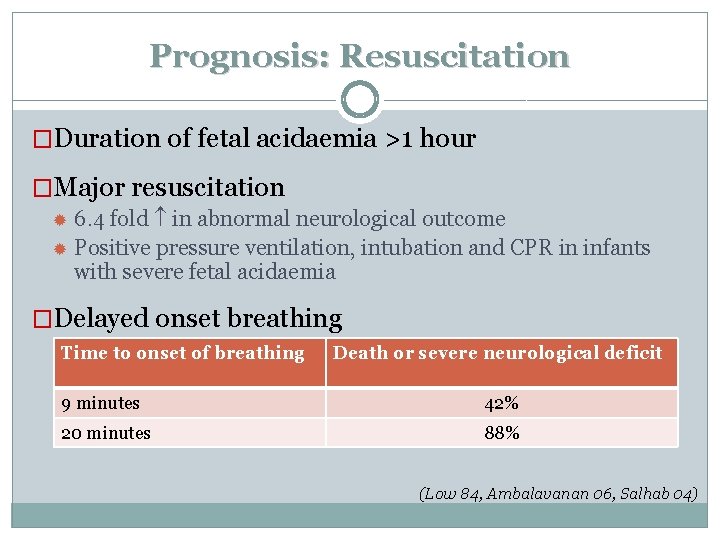
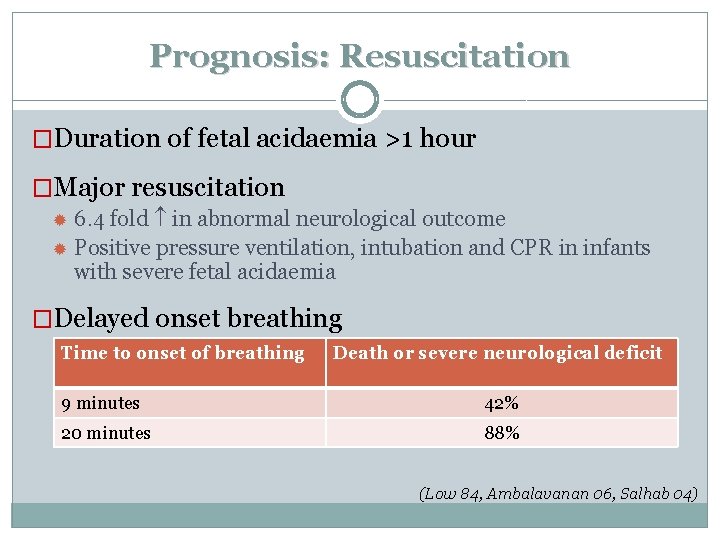
Prognosis: Resuscitation �Duration of fetal acidaemia >1 hour �Major resuscitation 6. 4 fold in abnormal neurological outcome Positive pressure ventilation, intubation and CPR in infants with severe fetal acidaemia �Delayed onset breathing Time to onset of breathing Death or severe neurological deficit 9 minutes 42% 20 minutes 88% (Low 84, Ambalavanan 06, Salhab 04)
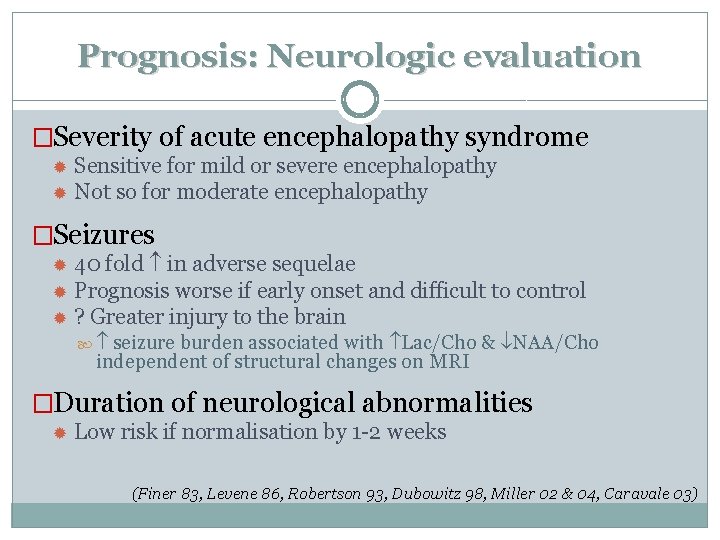
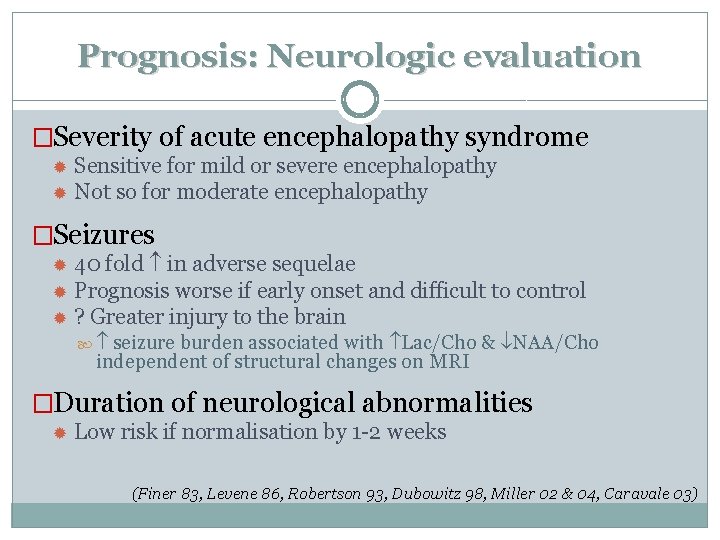
Prognosis: Neurologic evaluation �Severity of acute encephalopathy syndrome Sensitive for mild or severe encephalopathy Not so for moderate encephalopathy �Seizures 40 fold in adverse sequelae Prognosis worse if early onset and difficult to control ? Greater injury to the brain seizure burden associated with Lac/Cho & NAA/Cho independent of structural changes on MRI �Duration of neurological abnormalities Low risk if normalisation by 1 -2 weeks (Finer 83, Levene 86, Robertson 93, Dubowitz 98, Miller 02 & 04, Caravale 03)
Prognosis: Other clinical aspects �“Traditional signs of recovery” Apgar scores Signs of recovery e. g. Early establishment of suck feeds Visual responsiveness Head growth have low sensitivity/specificity for predicting neurodisability (Nelson 81, Mercuri 97, 99 & 00, Stark 06)
Biochemistry
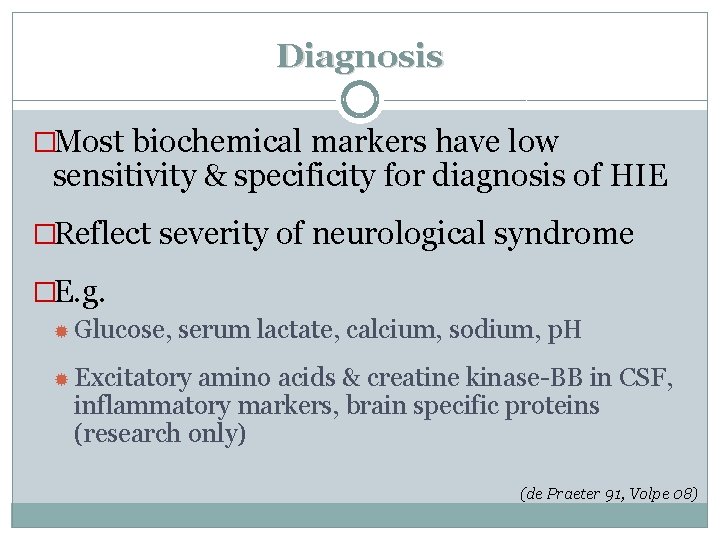
Diagnosis �Most biochemical markers have low sensitivity & specificity for diagnosis of HIE �Reflect severity of neurological syndrome �E. g. Glucose, serum lactate, calcium, sodium, p. H Excitatory amino acids & creatine kinase-BB in CSF, inflammatory markers, brain specific proteins (research only) (de Praeter 91, Volpe 08)
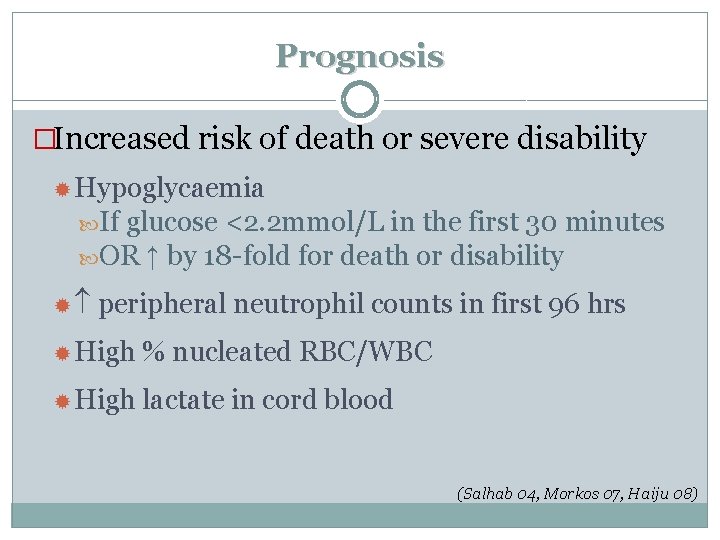
Prognosis �Increased risk of death or severe disability Hypoglycaemia If glucose <2. 2 mmol/L in the first 30 minutes OR ↑ by 18 -fold for death or disability peripheral neutrophil counts in first 96 hrs High % nucleated RBC/WBC High lactate in cord blood (Salhab 04, Morkos 07, Haiju 08)
Electrophysiology
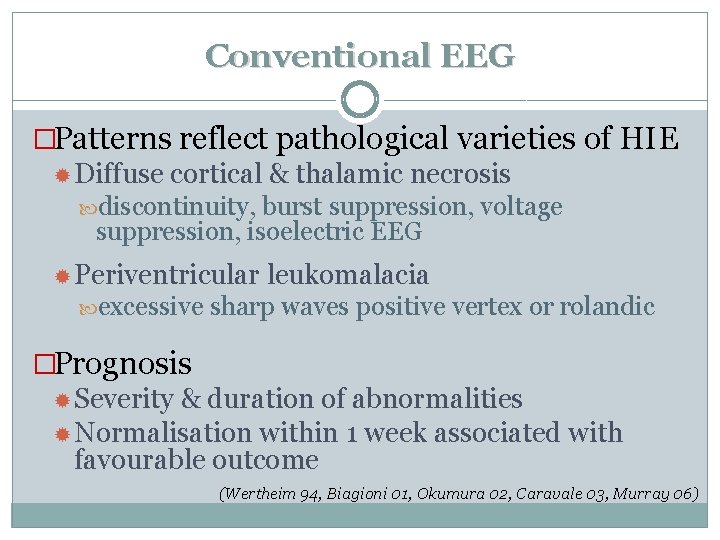
Conventional EEG �Patterns reflect pathological varieties of HIE Diffuse cortical & thalamic necrosis discontinuity, burst suppression, voltage suppression, isoelectric EEG Periventricular excessive leukomalacia sharp waves positive vertex or rolandic �Prognosis Severity & duration of abnormalities Normalisation within 1 week associated with favourable outcome (Wertheim 94, Biagioni 01, Okumura 02, Caravale 03, Murray 06)
Amplitude integrated EEG (a. EEG) �a. EEG background pattern: Reflect severity of HI insult Prognostic in the first 6 hours Normalisation within 24 hours in 10 -50% of abnormal a. EEG Rapid recovery - good outcome PPV if combined with clinical evaluation or MRI Quantitative a. EEG-based index (Cerebral health index/b) Research tool (Eken 95, Hellstrom-Westas 95, Toet 99, van Rooij 05, de Vries 05, Shalak 03, Leijser 07, Hathi 09)
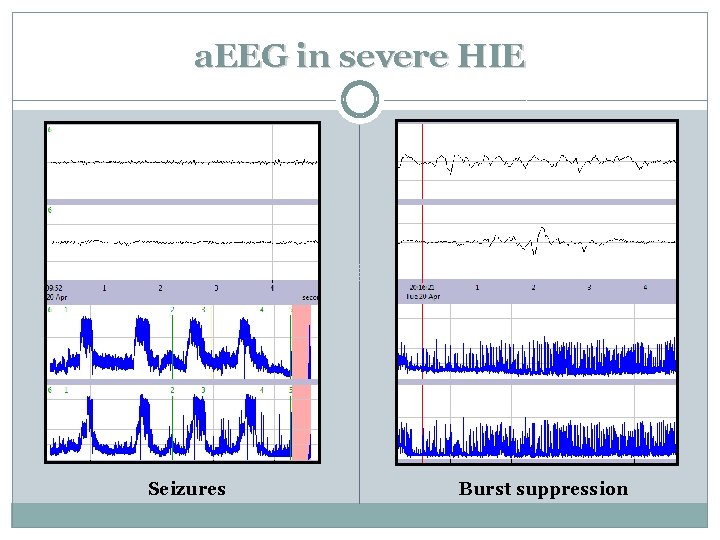
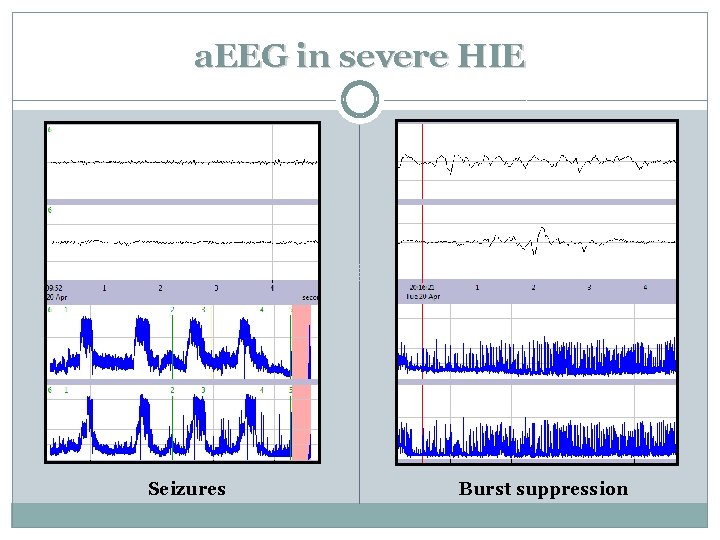
a. EEG in severe HIE Seizures Burst suppression
Evoked potentials & NIRS �Visual evoked potentials (VEP) & somatosensory evoked potentials (SSEP) Predictive if done within 6 hours �Near infrared spectroscopy (NIRS) Direct measure of cerebral blood flow Predictive if done in the first few days Research tool only (de Vries 91, Taylor 92, Eken 95, Meek 99)
Neuroimaging
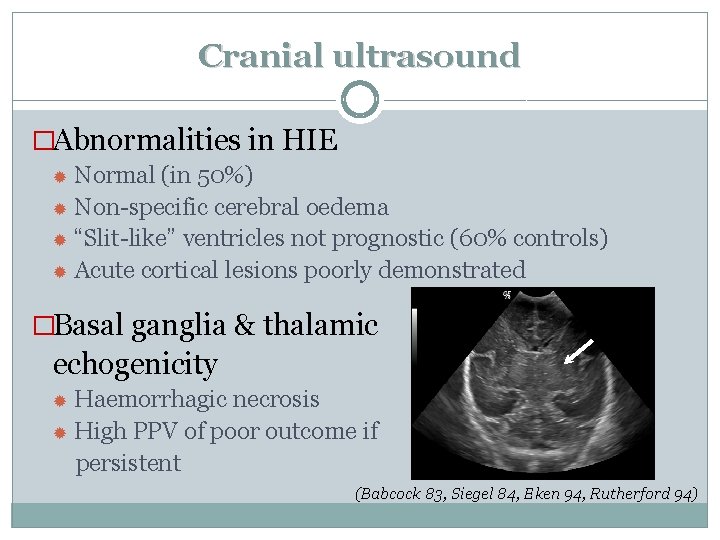
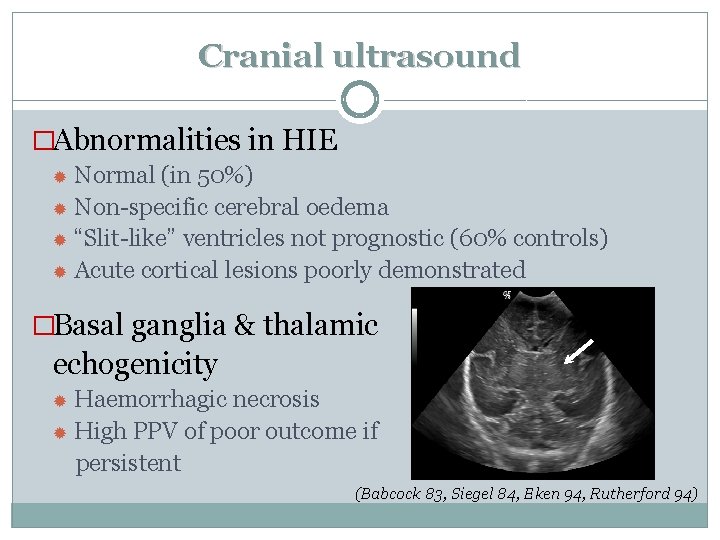
Cranial ultrasound �Abnormalities in HIE Normal (in 50%) Non-specific cerebral oedema “Slit-like” ventricles not prognostic (60% controls) Acute cortical lesions poorly demonstrated �Basal ganglia & thalamic echogenicity Haemorrhagic necrosis High PPV of poor outcome if persistent (Babcock 83, Siegel 84, Eken 94, Rutherford 94)
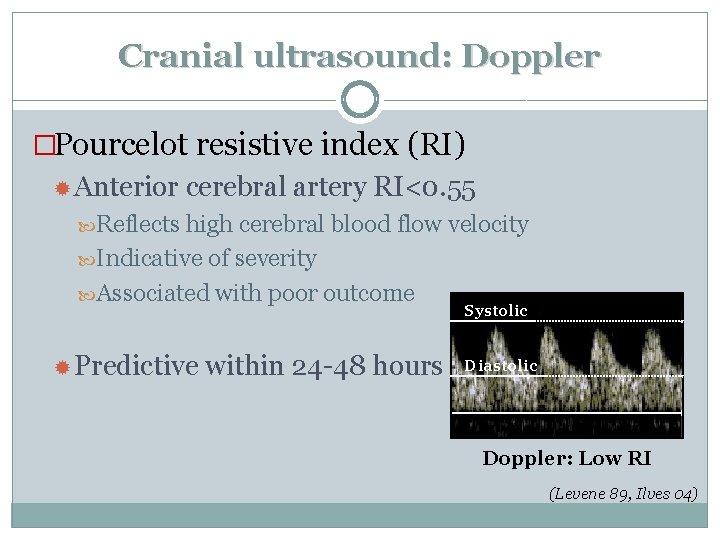
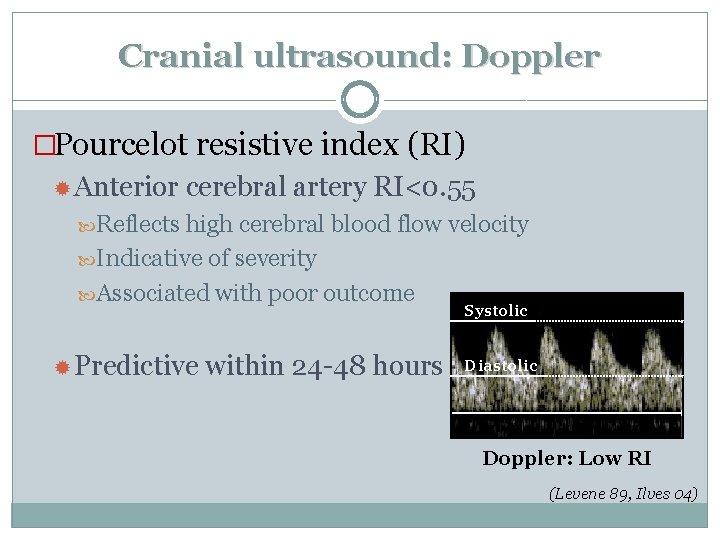
Cranial ultrasound: Doppler �Pourcelot resistive index (RI) Anterior cerebral artery RI<0. 55 Reflects high cerebral blood flow velocity Indicative of severity Associated with poor outcome Systolic Predictive within 24 -48 hours Diastolic Doppler: Low RI (Levene 89, Ilves 04)

Computed tomography (CT) �Patterns of injury in HIE Diffuse cortical neuronal injury: “reversal sign” Basal ganglia & thalamic injury: ↓ attenuation Not sensitive in mild/moderate HI injury “Reversal” sign “Isoattenuation” of deep nuclear grey matter
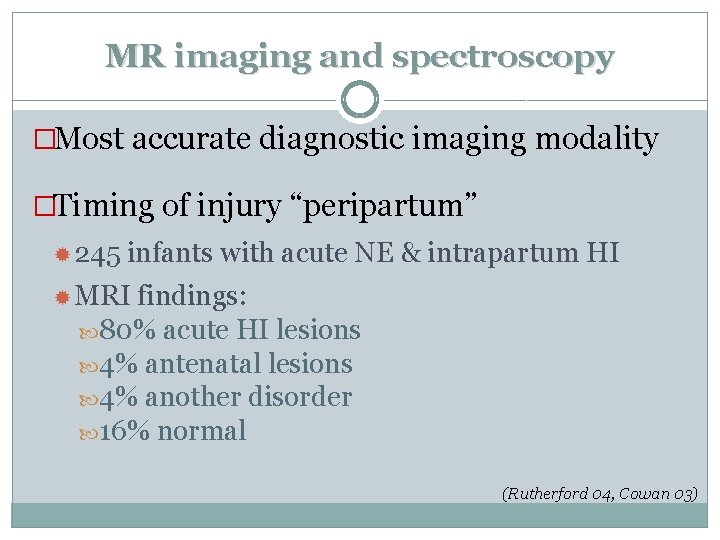
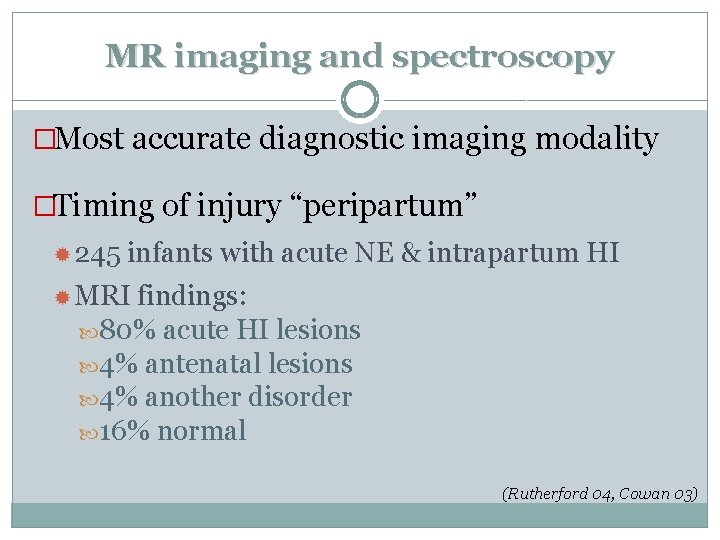
MR imaging and spectroscopy �Most accurate diagnostic imaging modality �Timing of injury “peripartum” 245 infants with acute NE & intrapartum HI MRI findings: 80% acute HI lesions 4% antenatal lesions 4% another disorder 16% normal (Rutherford 04, Cowan 03)
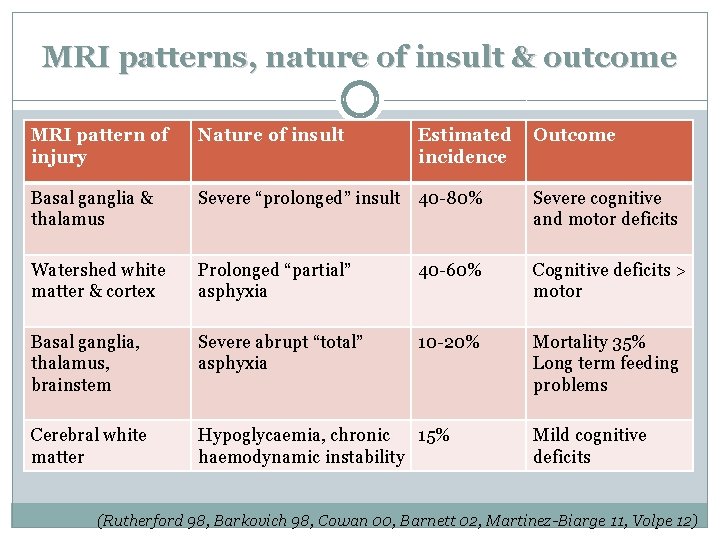
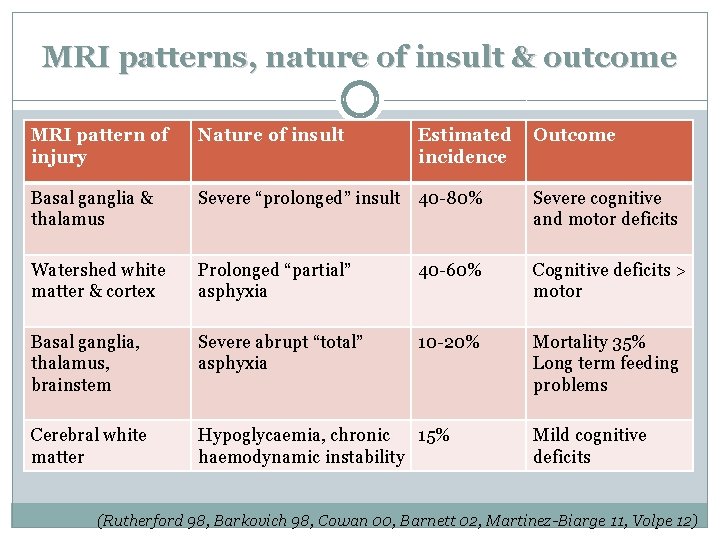
MRI patterns, nature of insult & outcome MRI pattern of injury Nature of insult Estimated incidence Outcome Basal ganglia & thalamus Severe “prolonged” insult 40 -80% Severe cognitive and motor deficits Watershed white matter & cortex Prolonged “partial” asphyxia 40 -60% Cognitive deficits > motor Basal ganglia, thalamus, brainstem Severe abrupt “total” asphyxia 10 -20% Mortality 35% Long term feeding problems Cerebral white matter Hypoglycaemia, chronic 15% haemodynamic instability Mild cognitive deficits (Rutherford 98, Barkovich 98, Cowan 00, Barnett 02, Martinez-Biarge 11, Volpe 12)
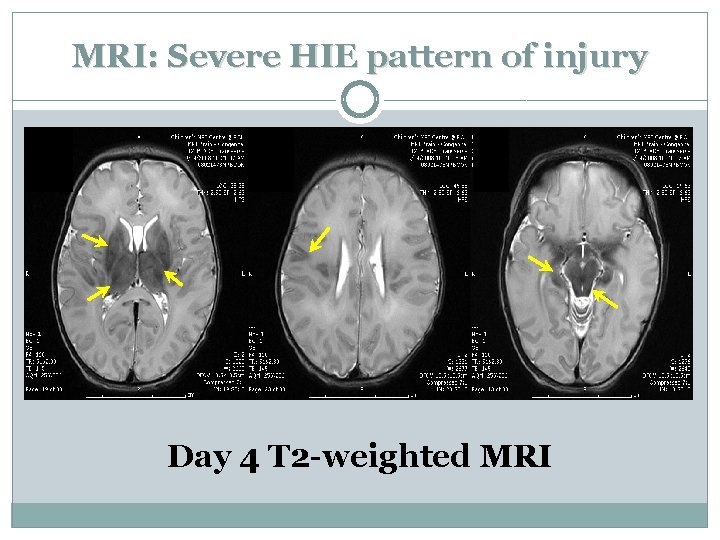
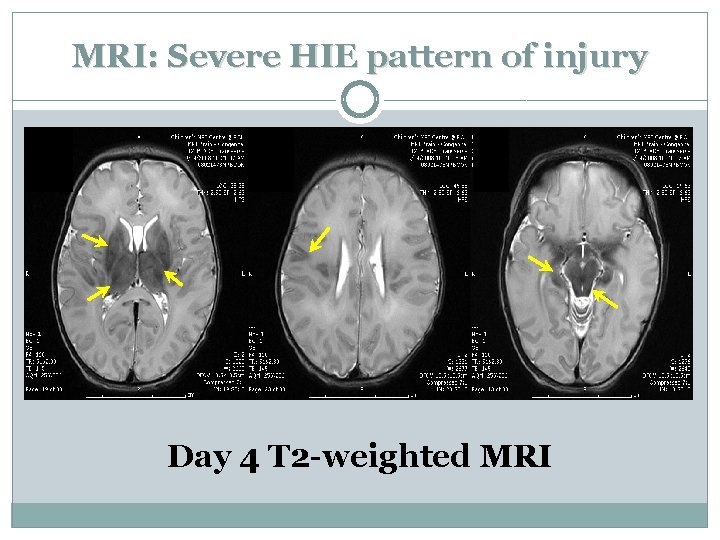
MRI: Severe HIE pattern of injury Day 4 T 2 -weighted MRI
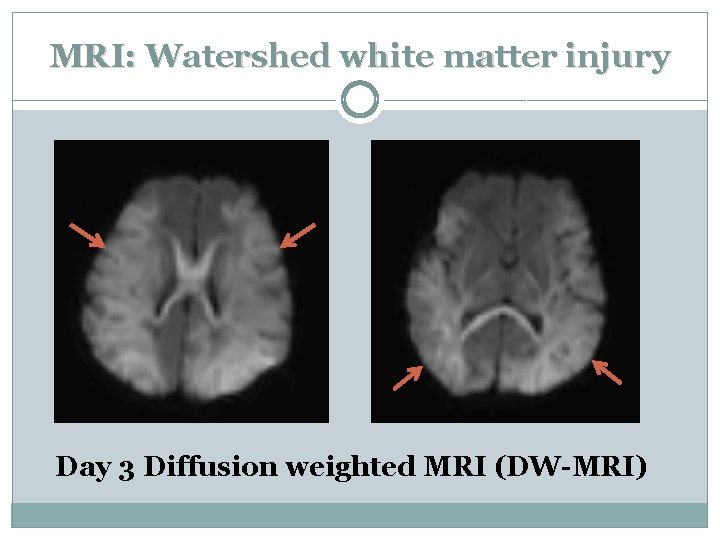
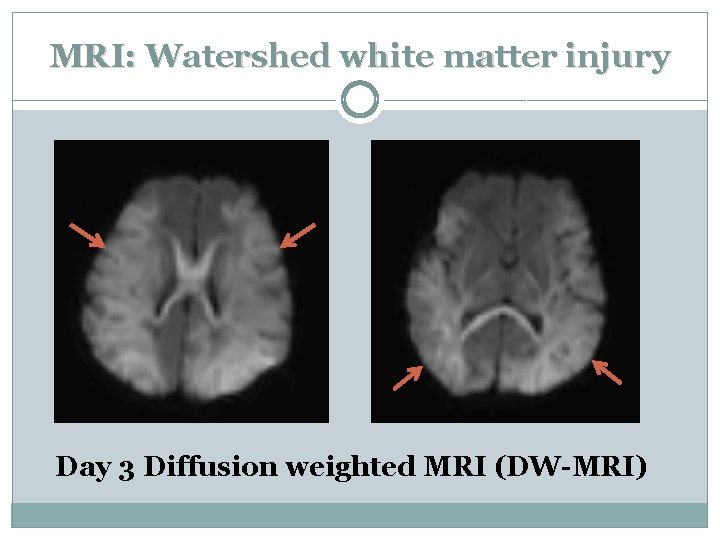
MRI: Watershed white matter injury Day 3 Diffusion weighted MRI (DW-MRI)
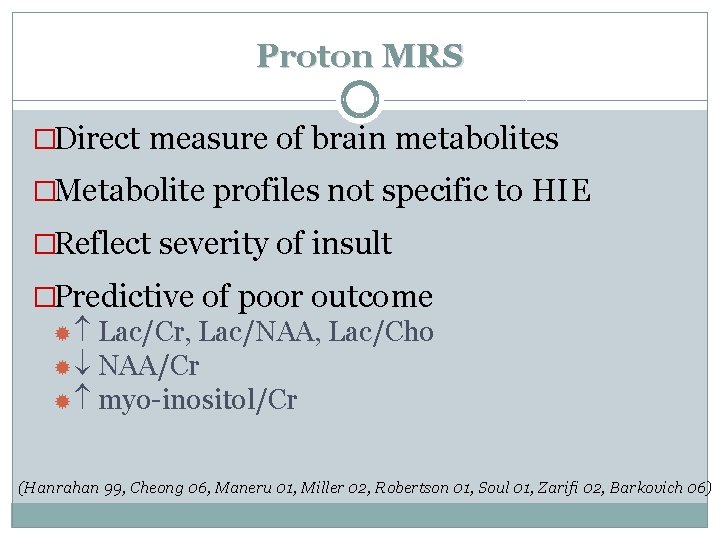
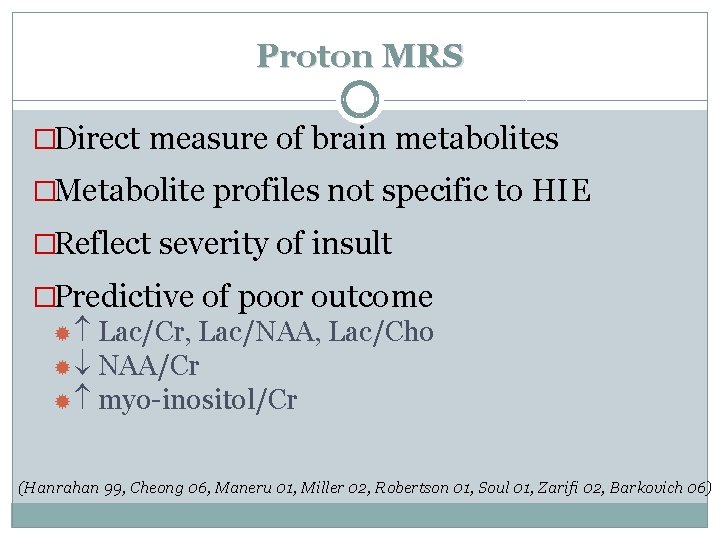
Proton MRS �Direct measure of brain metabolites �Metabolite profiles not specific to HIE �Reflect severity of insult �Predictive of poor outcome Lac/Cr, Lac/NAA, Lac/Cho NAA/Cr myo-inositol/Cr (Hanrahan 99, Cheong 06, Maneru 01, Miller 02, Robertson 01, Soul 01, Zarifi 02, Barkovich 06)
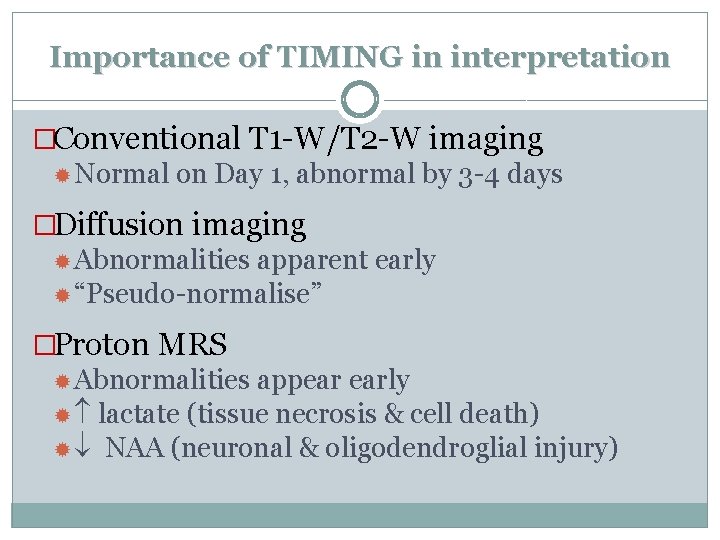
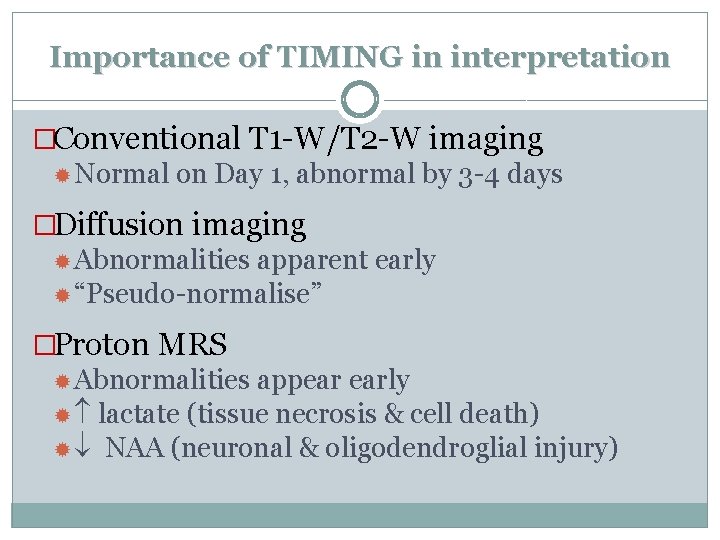
Importance of TIMING in interpretation �Conventional T 1 -W/T 2 -W imaging Normal on Day 1, abnormal by 3 -4 days �Diffusion imaging Abnormalities apparent early “Pseudo-normalise” �Proton MRS Abnormalities appear early lactate (tissue necrosis & cell death) NAA (neuronal & oligodendroglial injury)
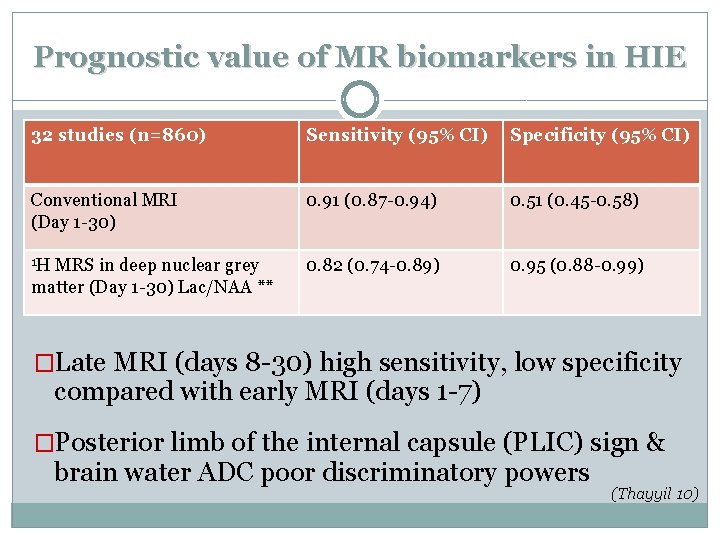
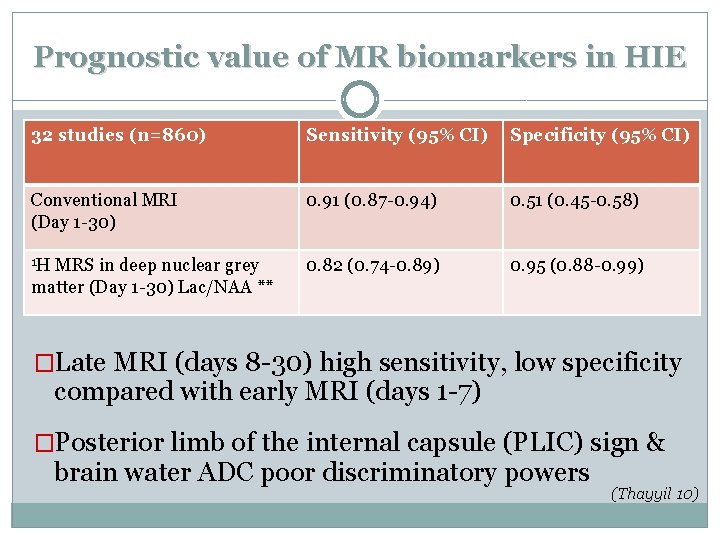
Prognostic value of MR biomarkers in HIE 32 studies (n=860) Sensitivity (95% CI) Specificity (95% CI) Conventional MRI (Day 1 -30) 0. 91 (0. 87 -0. 94) 0. 51 (0. 45 -0. 58) 1 H 0. 82 (0. 74 -0. 89) 0. 95 (0. 88 -0. 99) MRS in deep nuclear grey matter (Day 1 -30) Lac/NAA ** �Late MRI (days 8 -30) high sensitivity, low specificity compared with early MRI (days 1 -7) �Posterior limb of the internal capsule (PLIC) sign & brain water ADC poor discriminatory powers (Thayyil 10)
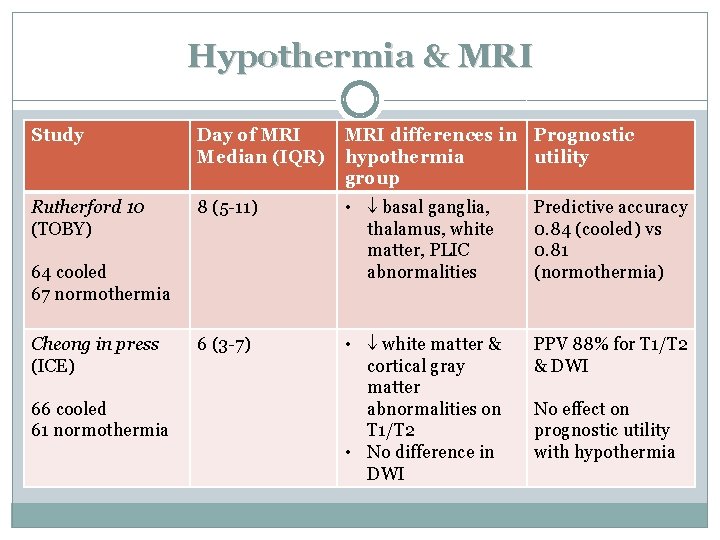
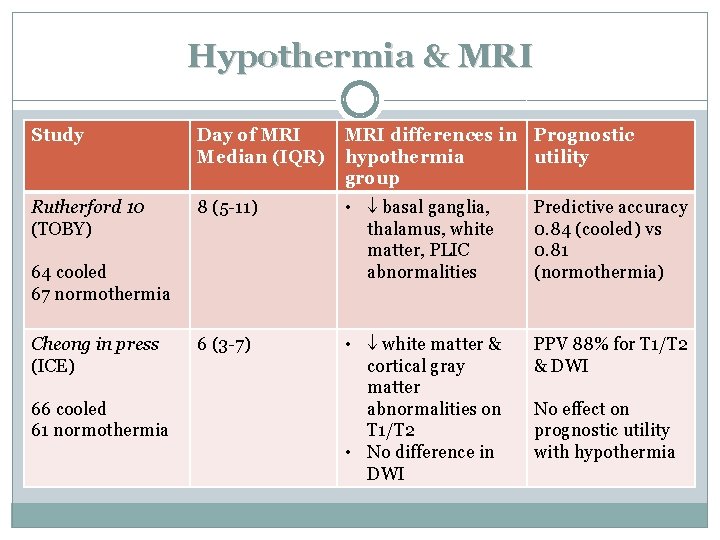
Hypothermia & MRI Study Day of MRI Median (IQR) MRI differences in Prognostic hypothermia utility group Rutherford 10 (TOBY) 8 (5 -11) • basal ganglia, thalamus, white matter, PLIC abnormalities Predictive accuracy 0. 84 (cooled) vs 0. 81 (normothermia) 6 (3 -7) • white matter & cortical gray matter abnormalities on T 1/T 2 • No difference in DWI PPV 88% for T 1/T 2 & DWI 64 cooled 67 normothermia Cheong in press (ICE) 66 cooled 61 normothermia No effect on prognostic utility with hypothermia
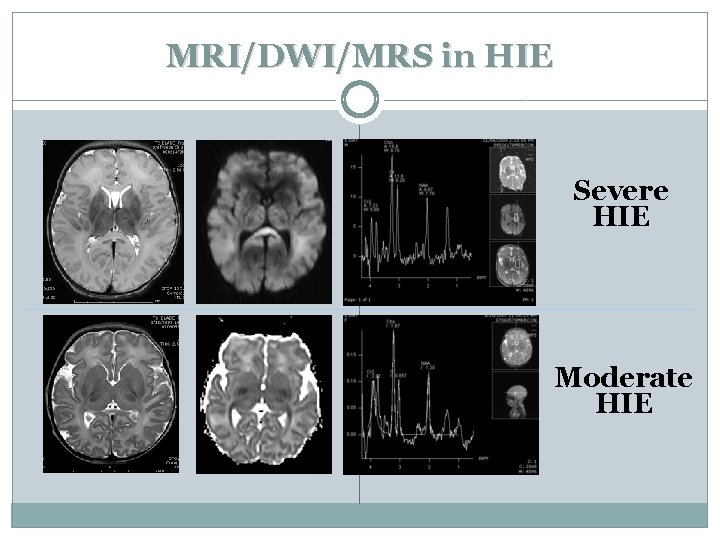
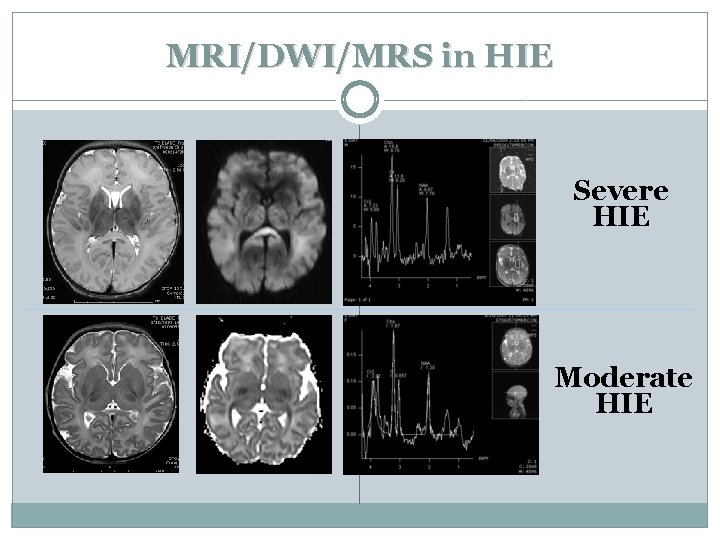
MRI/DWI/MRS in HIE Severe HIE Moderate HIE
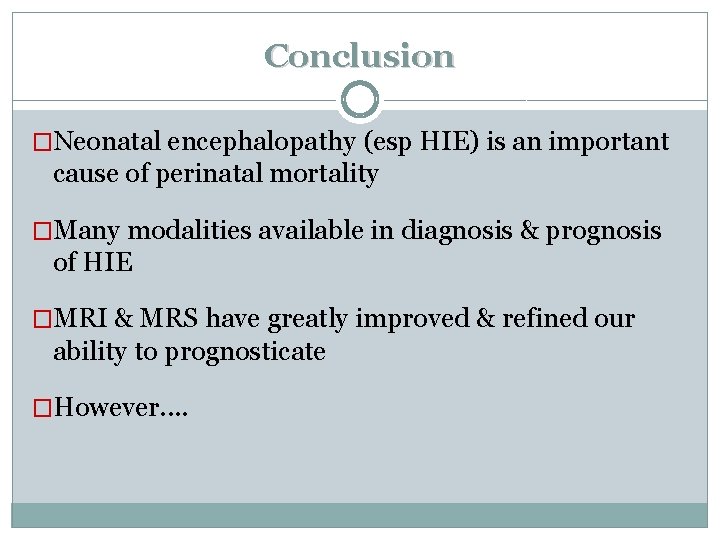
Conclusion �Neonatal encephalopathy (esp HIE) is an important cause of perinatal mortality �Many modalities available in diagnosis & prognosis of HIE �MRI & MRS have greatly improved & refined our ability to prognosticate �However. .
“No neurodiagnostic technique is capable of diminishing the importance of the clinical evaluation of the infant in assessment of outcome in HIE. Clinical and specialised diagnostic approaches are of value only when used in concert” (Volpe 08)
 Jeanie cheong
Jeanie cheong Infant mortality calculation
Infant mortality calculation Neonatal mortality rate formula
Neonatal mortality rate formula Jeanie reuter
Jeanie reuter Arion cheong
Arion cheong Arion cheong
Arion cheong Cheon seong gyeong
Cheon seong gyeong Yuet cheong produce
Yuet cheong produce Debin gao
Debin gao Professor cheong hee kiat
Professor cheong hee kiat Ocean amber pte ltd
Ocean amber pte ltd Tyler wozniak
Tyler wozniak Rachel summer cheong
Rachel summer cheong Cheon seong gyeong
Cheon seong gyeong Arion cheong
Arion cheong Mortality vs morbidity
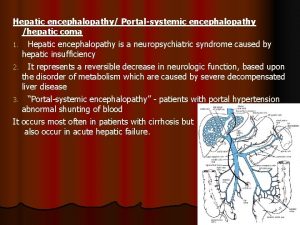
Mortality vs morbidity Hepatic encephalopathy pathophysiology
Hepatic encephalopathy pathophysiology Hepatic encephalopathy diagnosis
Hepatic encephalopathy diagnosis Hypertensive encephalopathy
Hypertensive encephalopathy Encephalopathy stages
Encephalopathy stages Hepatic encephalopathy symptoms
Hepatic encephalopathy symptoms Epiology definition
Epiology definition Diet hepatic encephalopathy
Diet hepatic encephalopathy Liver failure criteria
Liver failure criteria Hepatic encephalopathy stages
Hepatic encephalopathy stages Alain sauvage
Alain sauvage Uremic encephalopathy
Uremic encephalopathy Constructional apraxia
Constructional apraxia Normal bun
Normal bun Posology formula
Posology formula Encephalopathy stages
Encephalopathy stages Bilirubn
Bilirubn Bilateral cataract ketones and raised liver enzymes
Bilateral cataract ketones and raised liver enzymes