Microcirculation and lymphatic system Microcirculation Most purposeful function
- Slides: 32
Microcirculation and lymphatic system
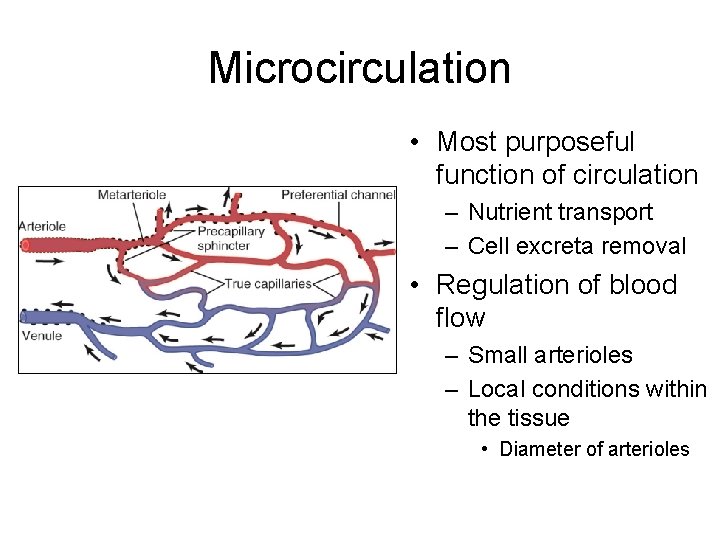
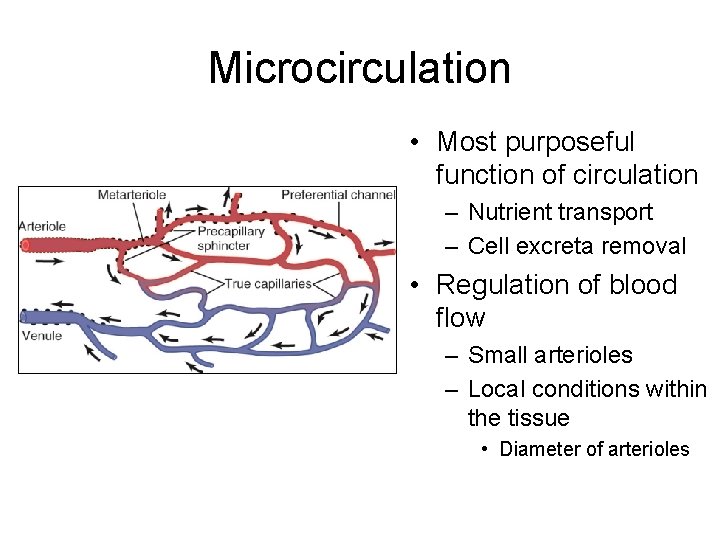
Microcirculation • Most purposeful function of circulation – Nutrient transport – Cell excreta removal • Regulation of blood flow – Small arterioles – Local conditions within the tissue • Diameter of arterioles
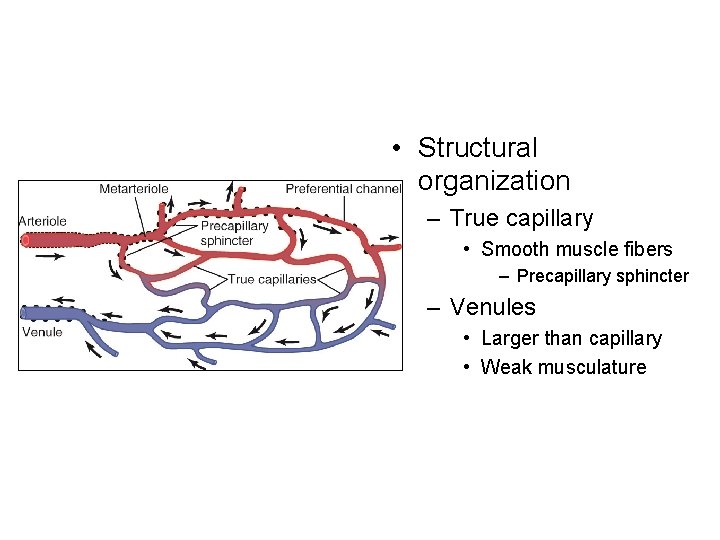
• Structural organization – Organ-specific • Meet its demands – Nutrient artery • Braches 6 to 8 times – Arterioles
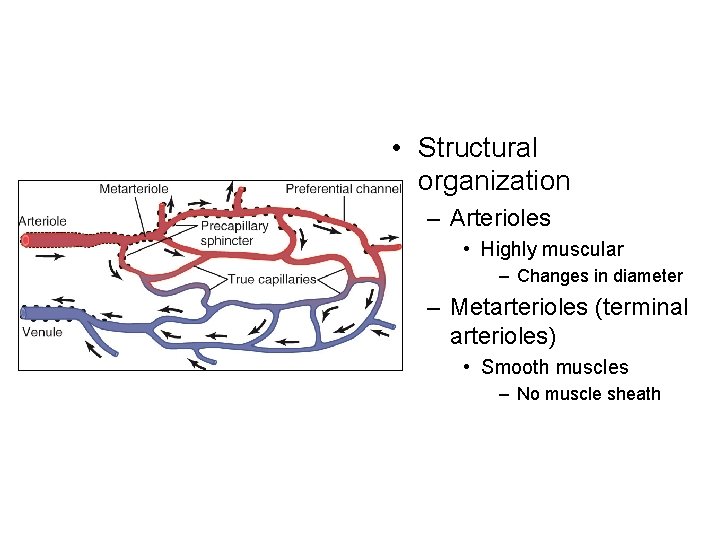
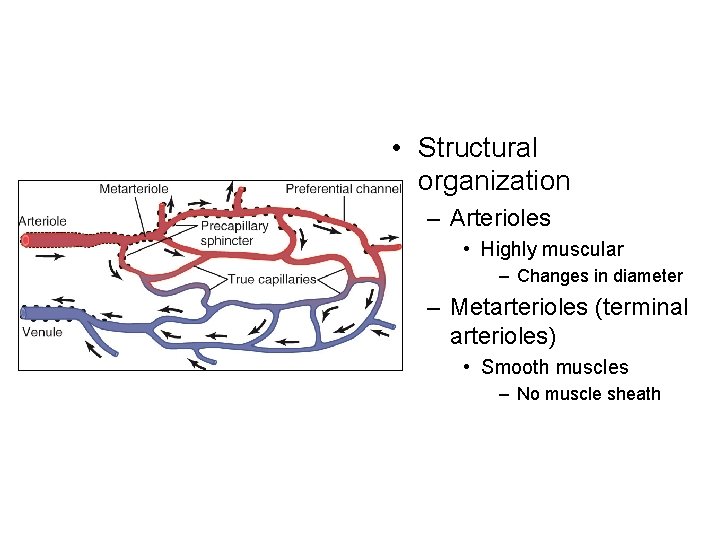
• Structural organization – Arterioles • Highly muscular – Changes in diameter – Metarterioles (terminal arterioles) • Smooth muscles – No muscle sheath
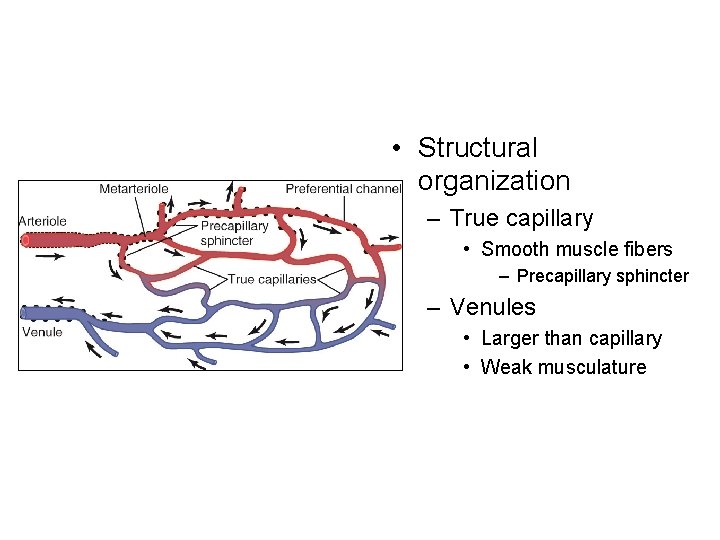
• Structural organization – True capillary • Smooth muscle fibers – Precapillary sphincter – Venules • Larger than capillary • Weak musculature
• Metarterioles and precapillary shincter – Close contact with tissue • Regulation of blood flow – Local condition of tissues
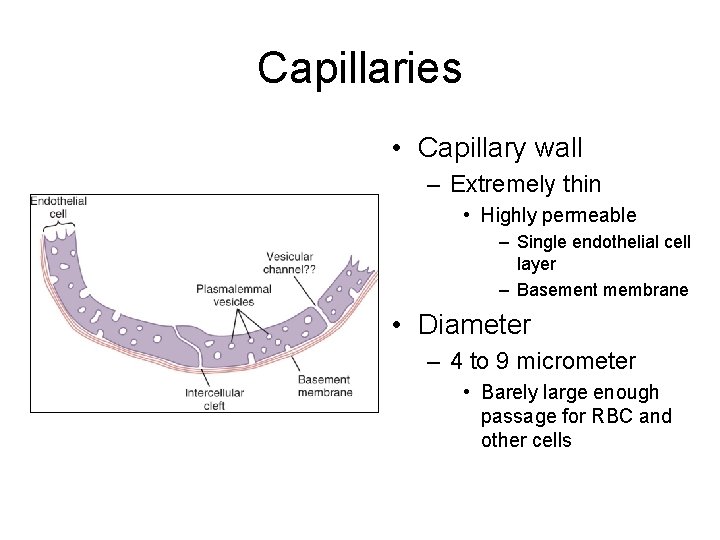
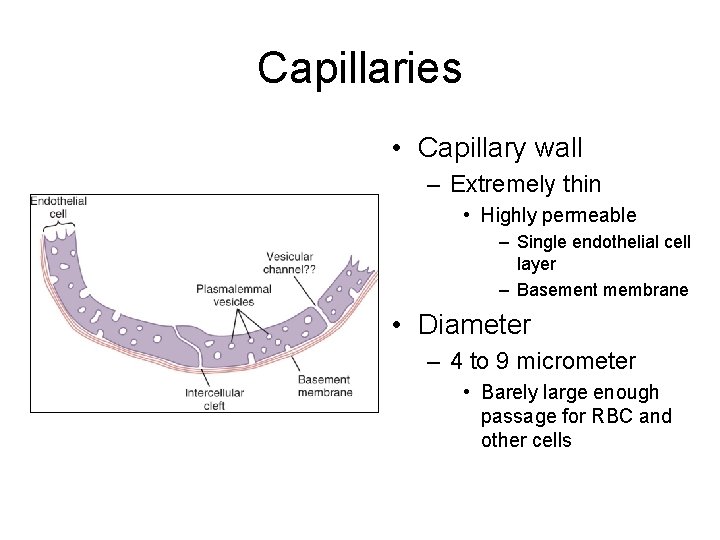
Capillaries • Capillary wall – Extremely thin • Highly permeable – Single endothelial cell layer – Basement membrane • Diameter – 4 to 9 micrometer • Barely large enough passage for RBC and other cells
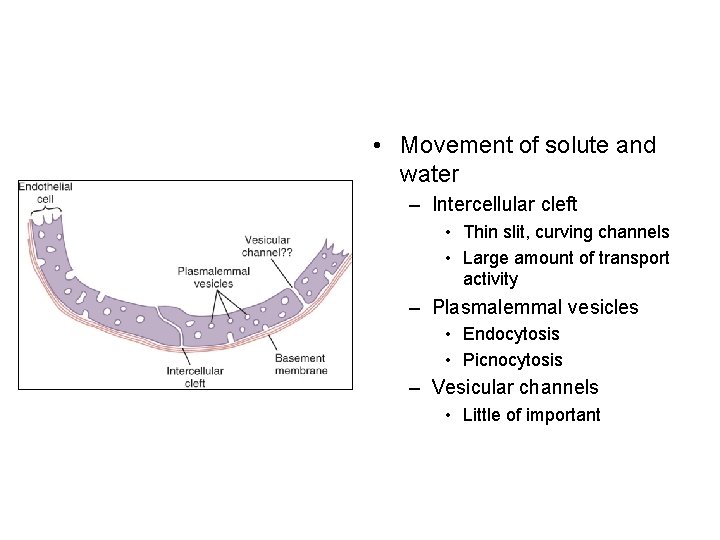
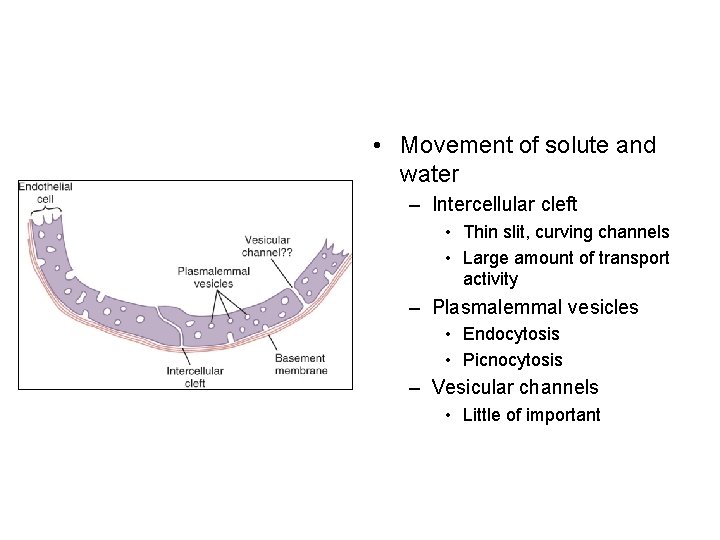
• Movement of solute and water – Intercellular cleft • Thin slit, curving channels • Large amount of transport activity – Plasmalemmal vesicles • Endocytosis • Picnocytosis – Vesicular channels • Little of important
• Specialization – Brain • Blood-brain barrier (tight junctions) – Only small molecules can pass – Liver • Larger pores and slits – GI capillary membrane • Intermediate in size – Glomerular tufts of kidney • Fenestrae (oval window) – Large amount of small molecules and ions
Vasomotion • Capillary flow – Intermittent rather than continuous – Vasomotion • Intermittent contraction of metarterioles and precapillary sphincter • Regulated by oxygen concentrations – Decrease in oxygen concentration (greater tissue demand), increase in vasomotion (increased frequency with longer duration)
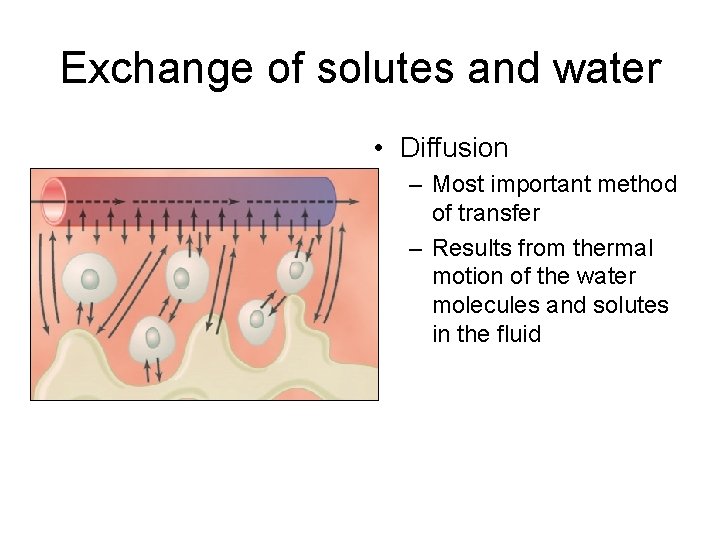
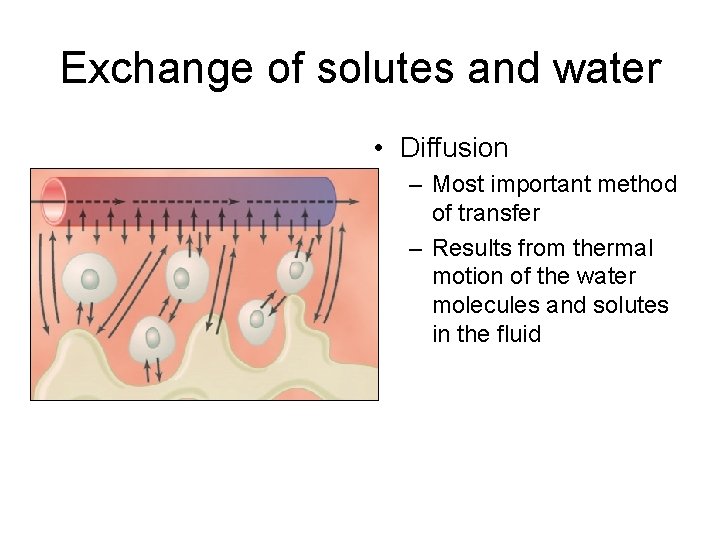
Exchange of solutes and water • Diffusion – Most important method of transfer – Results from thermal motion of the water molecules and solutes in the fluid
• Movement of lipid-soluble substances – Direct diffusion • No pores required – Oxygen – Carbon dioxide – Faster than lipid-insoluble materials • Require facilitation
• Water-soluble materials – Intercellular cleft – Extremely efficient • Cleft occupy 1/1000 of the entire capillary surface area • Diffusion of water is 80 X faster than flow of plasma itself
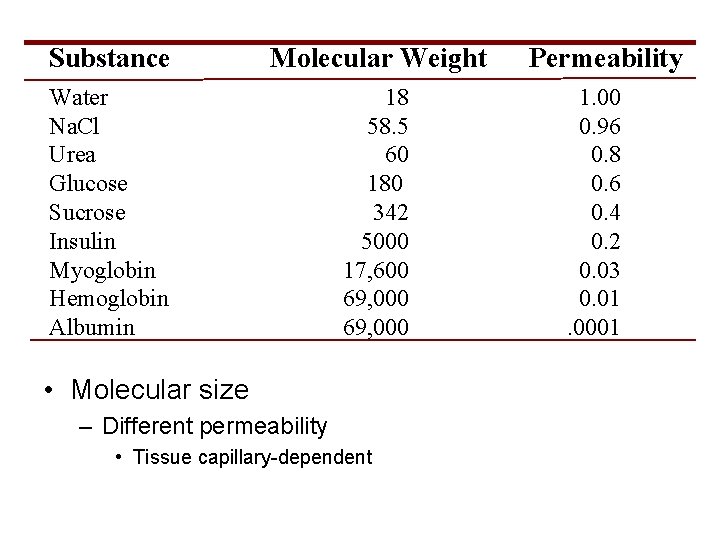
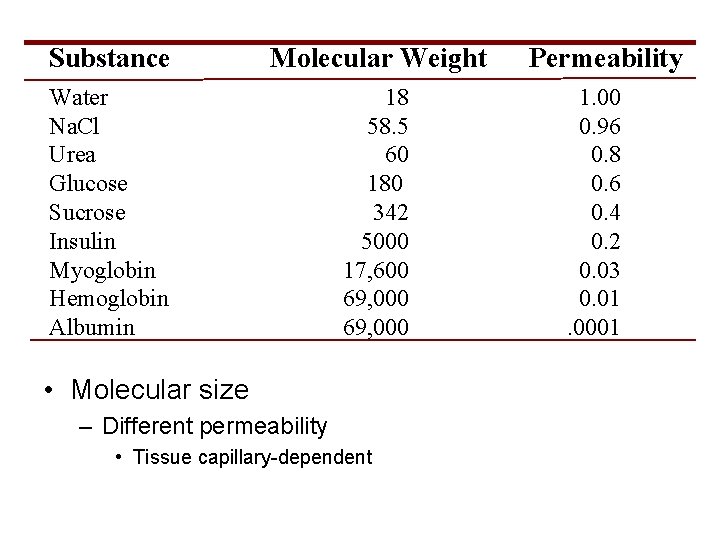
Substance Molecular Weight Water Na. Cl Urea Glucose Sucrose Insulin Myoglobin Hemoglobin Albumin 18 58. 5 60 180 342 5000 17, 600 69, 000 • Molecular size – Different permeability • Tissue capillary-dependent Permeability 1. 00 0. 96 0. 8 0. 6 0. 4 0. 2 0. 03 0. 01. 0001
• Concentration gradient – Greater the difference in concentrations between inside and outside, faster the rate of diffusion – Rates of diffusion of most nutrients • Much greater than other materials • Require small concentration differences
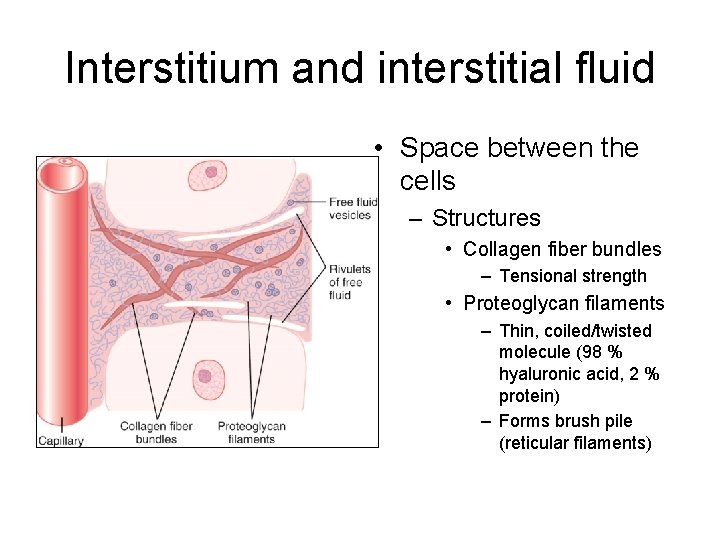
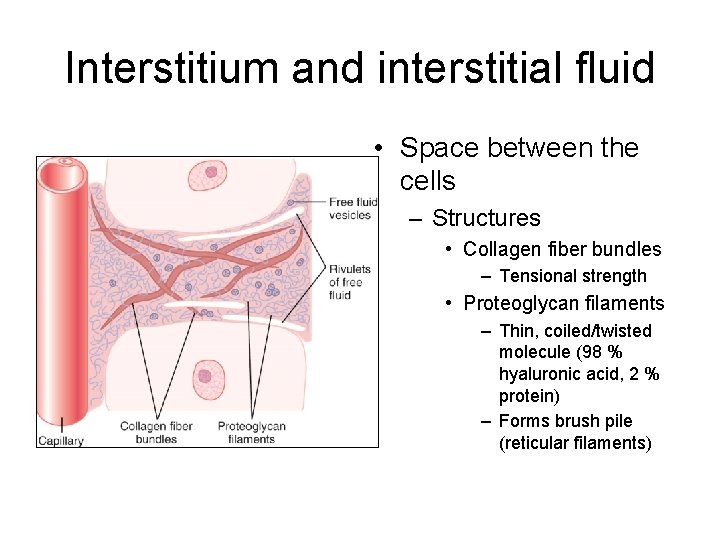
Interstitium and interstitial fluid • Space between the cells – Structures • Collagen fiber bundles – Tensional strength • Proteoglycan filaments – Thin, coiled/twisted molecule (98 % hyaluronic acid, 2 % protein) – Forms brush pile (reticular filaments)
• Interstitial fluid – Filtrate and diffusion of plasma components • Same constituents but lower concentrations of proteins – Entrapped in minute space along proteoglycan filaments • Formation of tissue gel • Diffusion of fluid and molecules – Very rapid
• Interstitial fluid – Free fluid • Very small amount (less than 1 %) – Edema • Expansion of fluid stored in the interstitium until 50 % of fluid becomes free of proteoglycan – Rivulets – Pockets
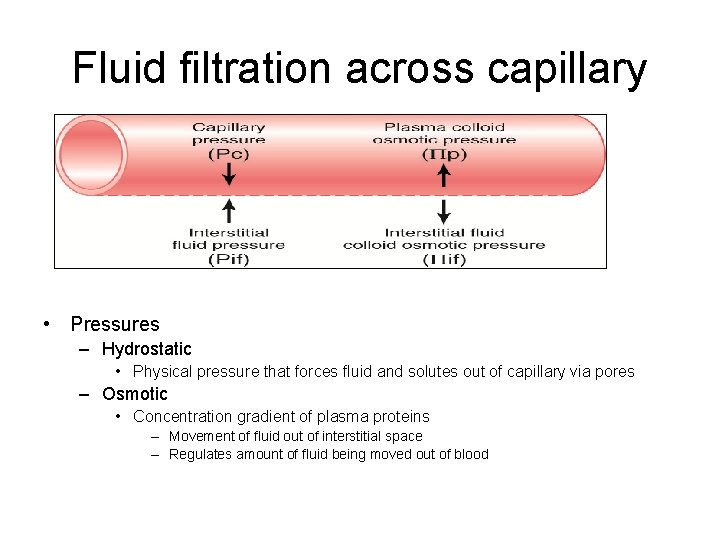
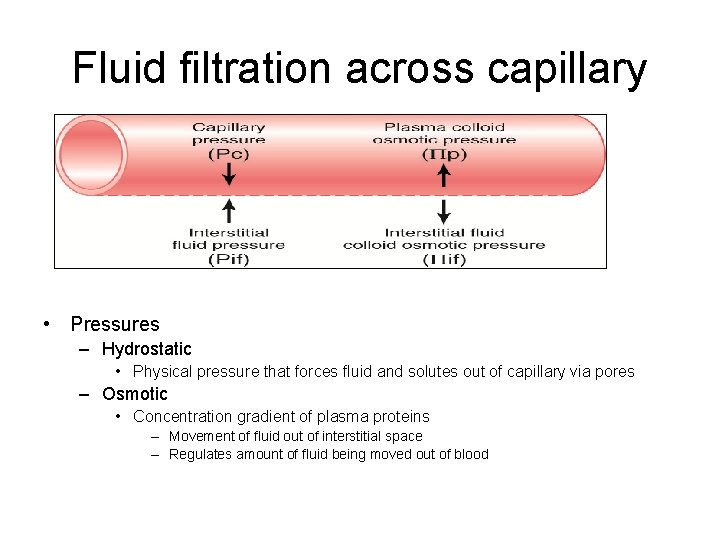
Fluid filtration across capillary • Pressures – Hydrostatic • Physical pressure that forces fluid and solutes out of capillary via pores – Osmotic • Concentration gradient of plasma proteins – Movement of fluid out of interstitial space – Regulates amount of fluid being moved out of blood
• Role of lymphatic system – Return of excess fluid and proteins to blood • Leakage into interstitial space
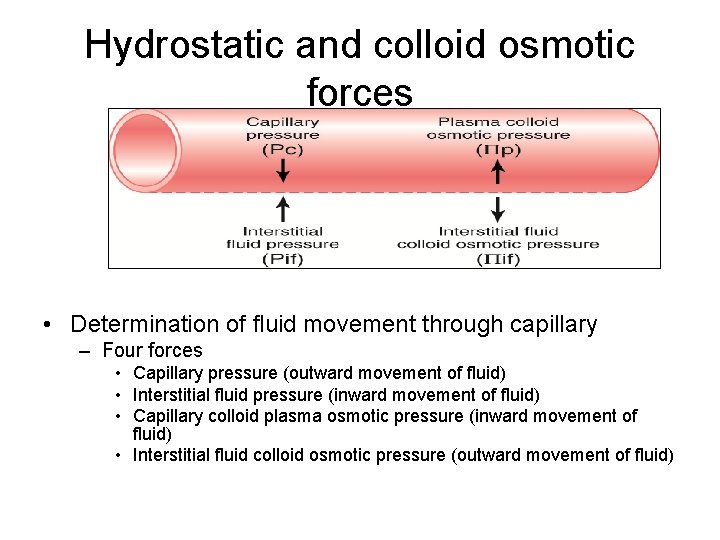
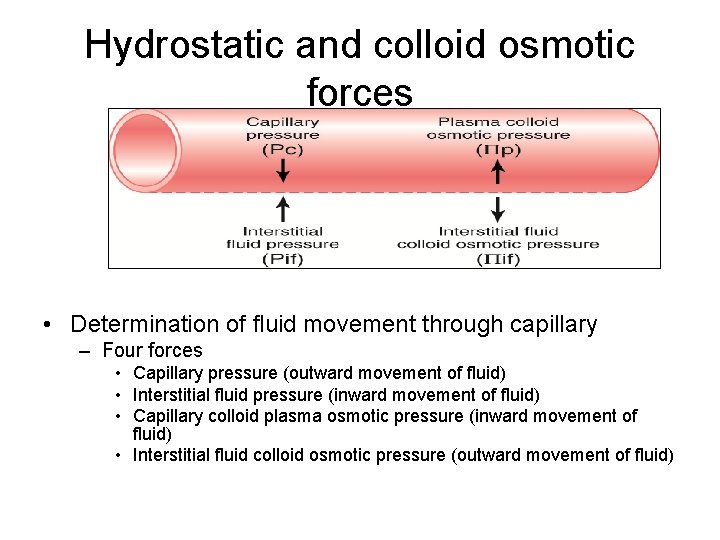
Hydrostatic and colloid osmotic forces • Determination of fluid movement through capillary – Four forces • Capillary pressure (outward movement of fluid) • Interstitial fluid pressure (inward movement of fluid) • Capillary colloid plasma osmotic pressure (inward movement of fluid) • Interstitial fluid colloid osmotic pressure (outward movement of fluid)
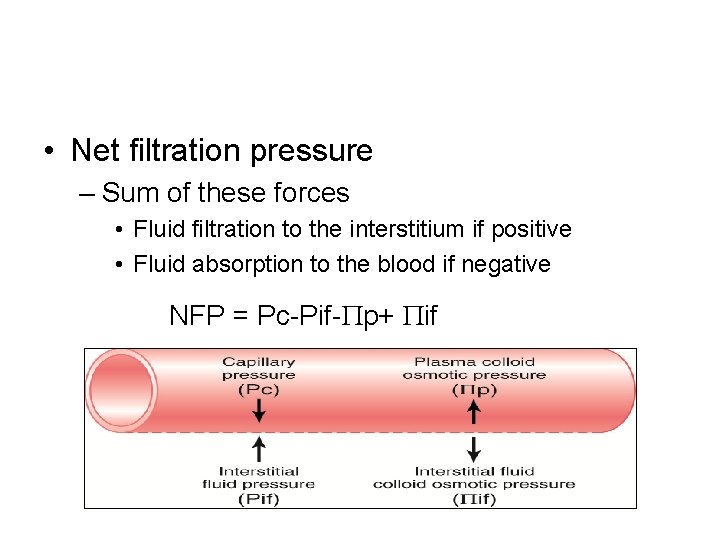
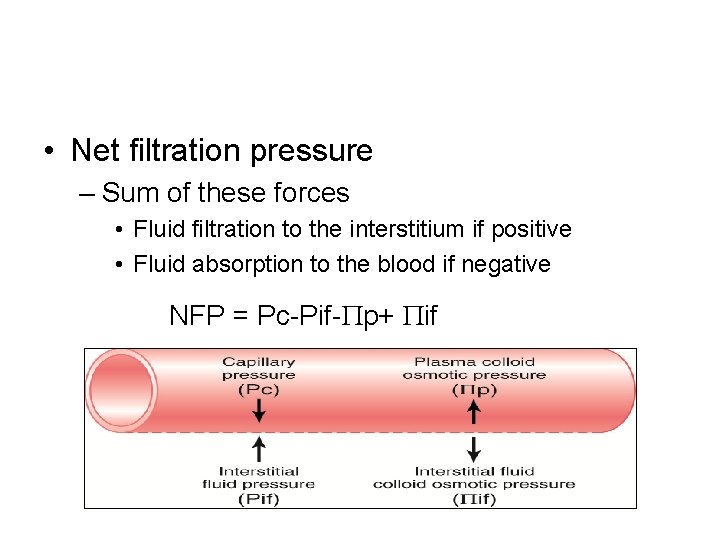
• Net filtration pressure – Sum of these forces • Fluid filtration to the interstitium if positive • Fluid absorption to the blood if negative NFP = Pc-Pif- p+ if
• Other factors – Filtration coefficient (Kf) • Pore size • Pore number • Number of capillaries Filtration = Kf X NFP
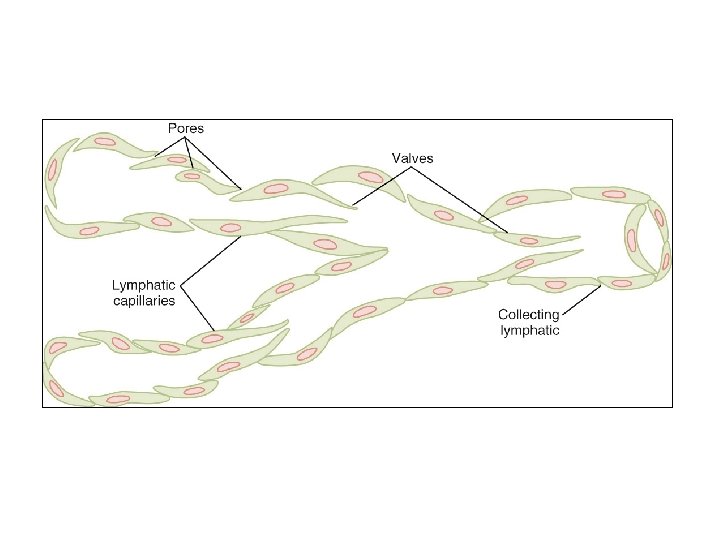
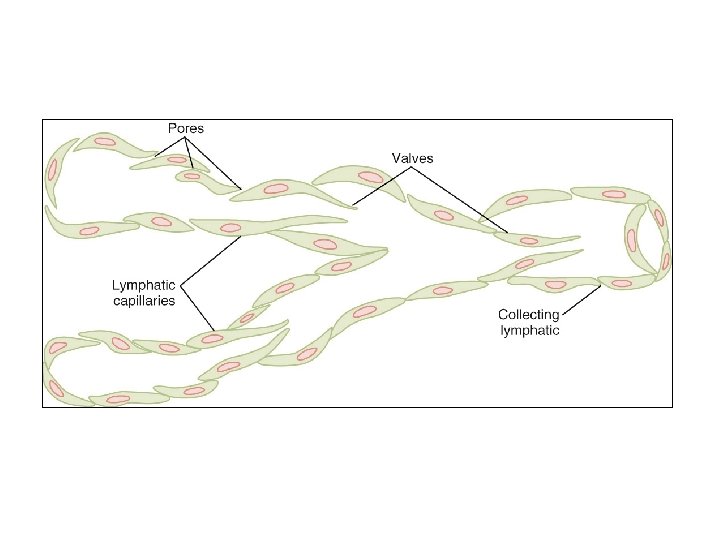
Lymphatic system • Accessory route – Flow of fluid from interstitium to the blood • Movement of proteins and large particles away from tissue to the blood – Extremely critical • Lethal if no movement • Drainage – Channels • Not present on skin, the CNS, endomysium, and bones – Prelymphatics
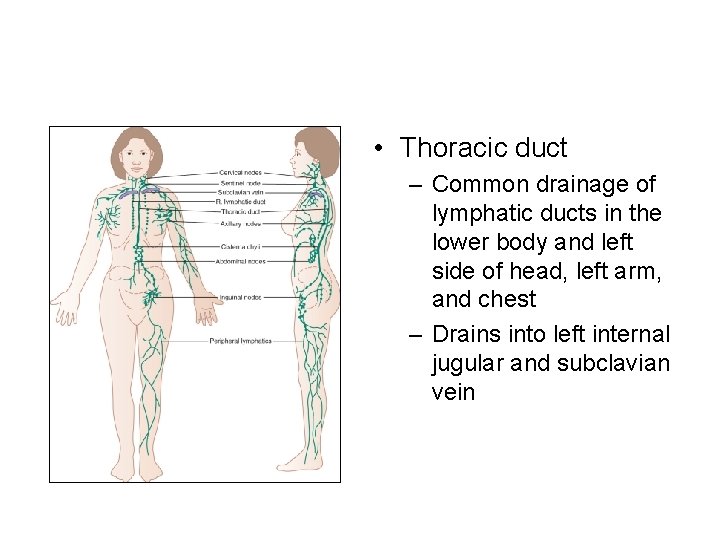
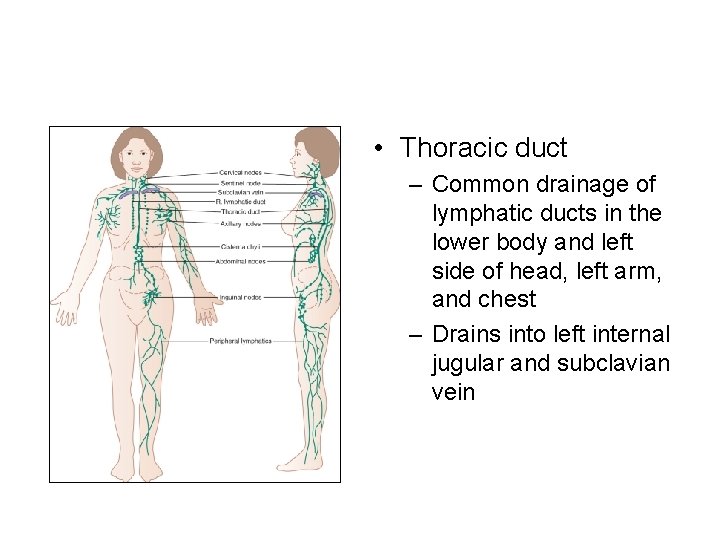
• Thoracic duct – Common drainage of lymphatic ducts in the lower body and left side of head, left arm, and chest – Drains into left internal jugular and subclavian vein
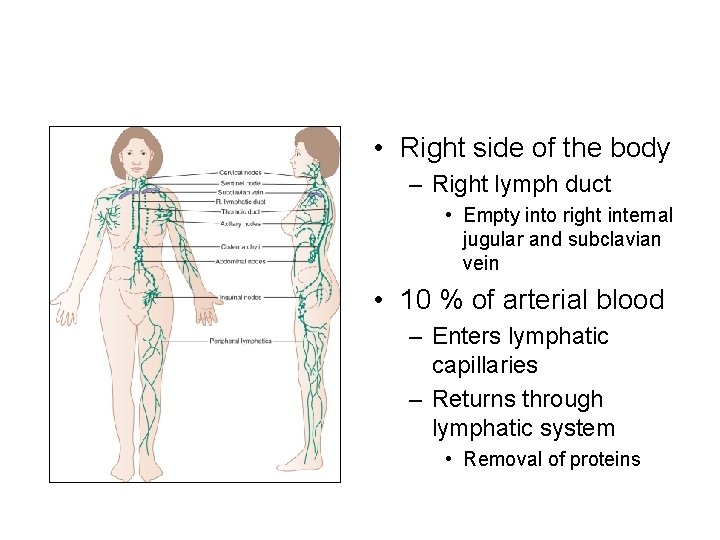
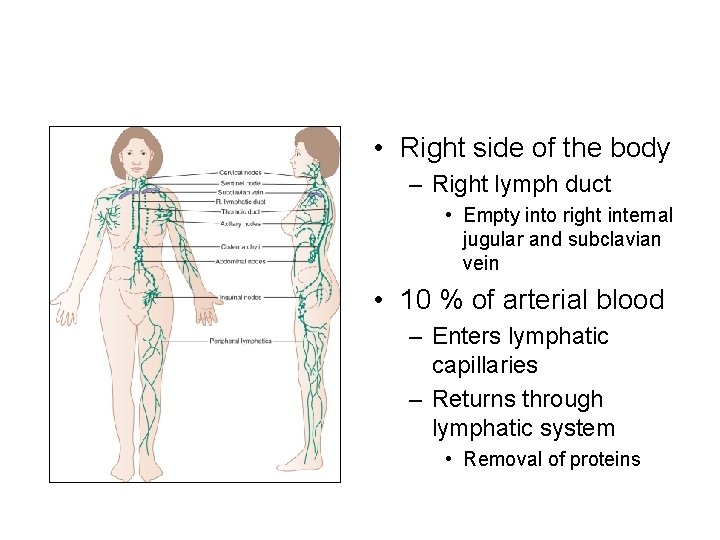
• Right side of the body – Right lymph duct • Empty into right internal jugular and subclavian vein • 10 % of arterial blood – Enters lymphatic capillaries – Returns through lymphatic system • Removal of proteins
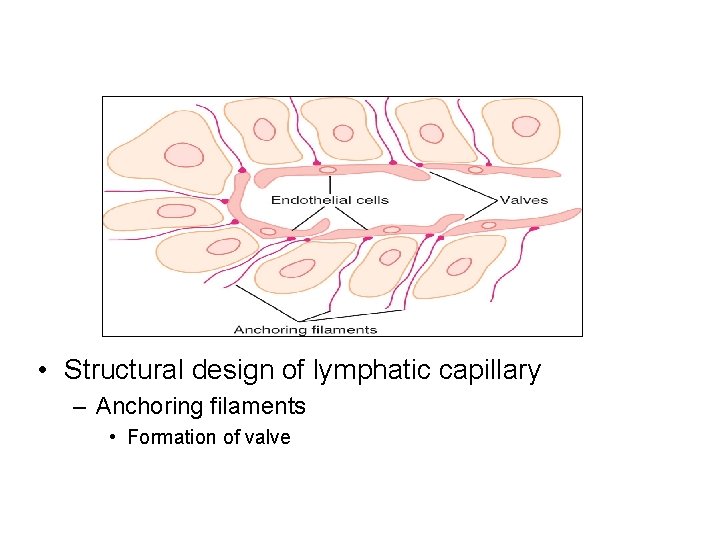
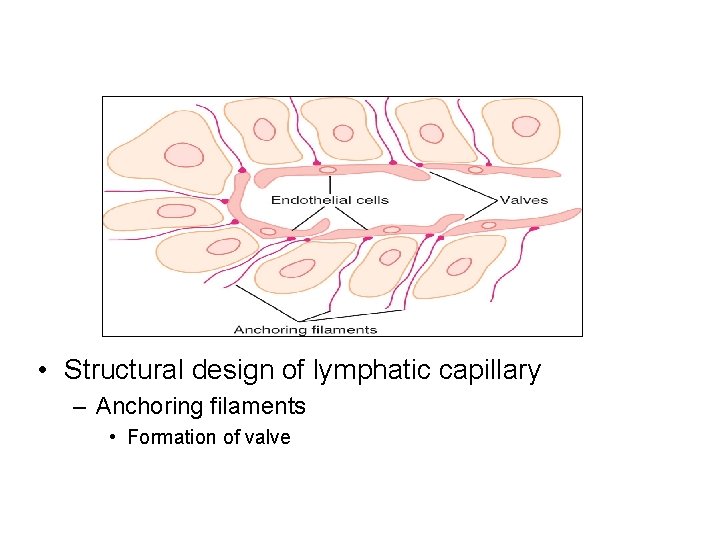
• Structural design of lymphatic capillary – Anchoring filaments • Formation of valve
Lymph formation • Derived from interstitial fluid – Same composition – Differences in protein concentrations • Average 2 g/dl (most tissues) • As high as 6 g/dl in lymphs from the liver • 3 -4 g/dl in lymphs from the intestine – Used for nutrient absorption • Lipids – Infectious agents • Destroyed
Rate of lymph flow • 100 ml per hour through thoracic duct • 20 ml per hour through other channels – 120 ml per hour – 2 -3 L per day • Increased interstitial fluid pressure, increased lymph flow – Changes in balance of fluid exchange
• Lymphatic pumps – Contraction of smooth muscles surrounding lymphatic and large lymph ducts – Compression of lymphatics • Rate of lymph flow – Interstitial fluid pressure X activity of lymphatic pumps
Regulation of interstitial fluid • Protein level – Accumulation of plasma proteins in the interstitium • Small but continuous leakage from the capillary – Alters colloid osmotic pressure – Alters fluid filtration rate and cause fluid accumulation – Alters interstitial fluid pressure and volume – Increased flow of lymph • Removal of proteins