MEDICAL GRANDROUNDS Kathryn Hazel C Trinidad M D




- Slides: 76
MEDICAL GRANDROUNDS Kathryn Hazel C. Trinidad M. D. First Year Medical Resident
OBJECTIVES To be able to present a known case of SLE who developed seizure during the course of illness To be able to know the diagnosis, treatment, and prognosis of NPSLE To be able to know the latest updates with regards to NPSLE
THE CASE H. M 35 year old G 3 P 2 (1112) female right-handed known case of SLE maintained on Prednisone 20 mg 2 x/day known case of APAS, maintained on ASA 80 mg OD housewife
Seizure CHIEF COMPLAINT
INTERVAL HISTORY May 2002 experienced on-off fever (Tmax 40 C), malar rash, joint pains, vomiting, photosensitivity, and oral ulcers. diagnosed with SLE; started on Prednisone 5 mg OD; regular OPD follow-up Nov 2007 (+) miscarriage; OPD follow-up for clearance prior to dilatation and curettage
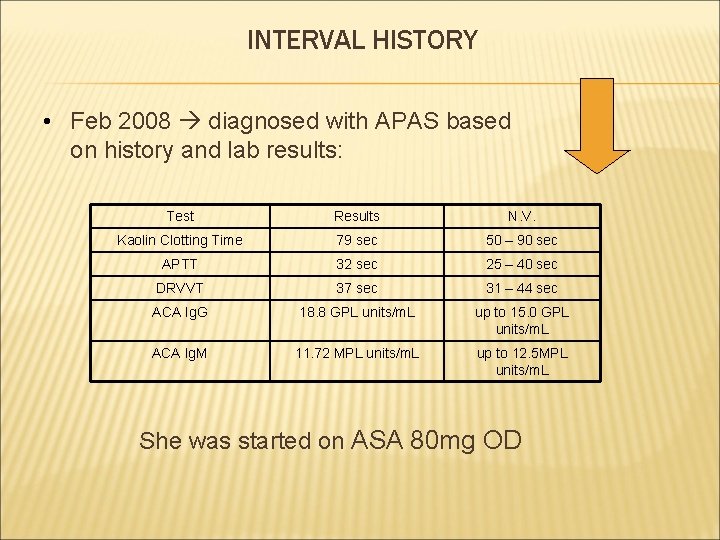
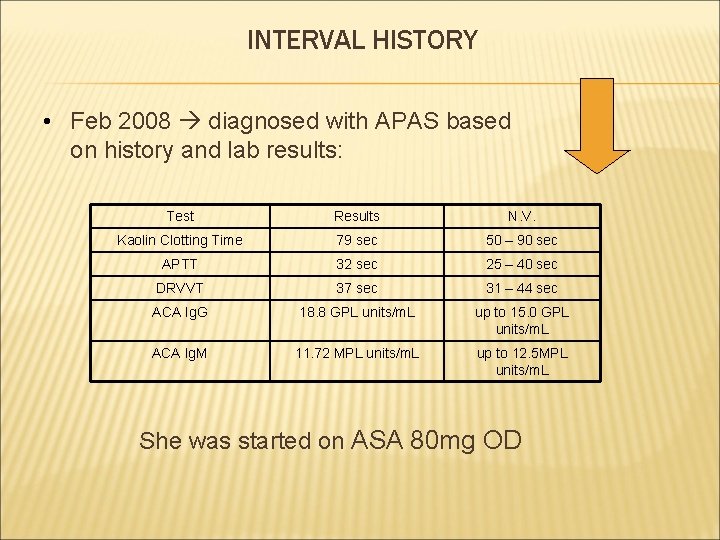
INTERVAL HISTORY • Feb 2008 diagnosed with APAS based on history and lab results: Test Results N. V. Kaolin Clotting Time 79 sec 50 – 90 sec APTT 32 sec 25 – 40 sec DRVVT 37 sec 31 – 44 sec ACA Ig. G 18. 8 GPL units/m. L up to 15. 0 GPL units/m. L ACA Ig. M 11. 72 MPL units/m. L up to 12. 5 MPL units/m. L She was started on ASA 80 mg OD
INTERVAL HISTORY 9 months PTA(July 2008) 1 st prenatal check-up at 7 wks AOG. No rashes, joint pains, and oral ulcers; Started on Heparin 5, 000 IU SQ OD Prednisone 5 mg OD and ASA 80 mg OD continued. Monthly prenatal check-up with both Rheumatology and OB-GYN services
INTERVAL HISTORY 2 months PTA(March 2009) gave birth to a live preterm male via LTCS; Discharged with ASA 80 mg OD and Heparin 5, 000 IU/m. L; Prednisone was not resumed
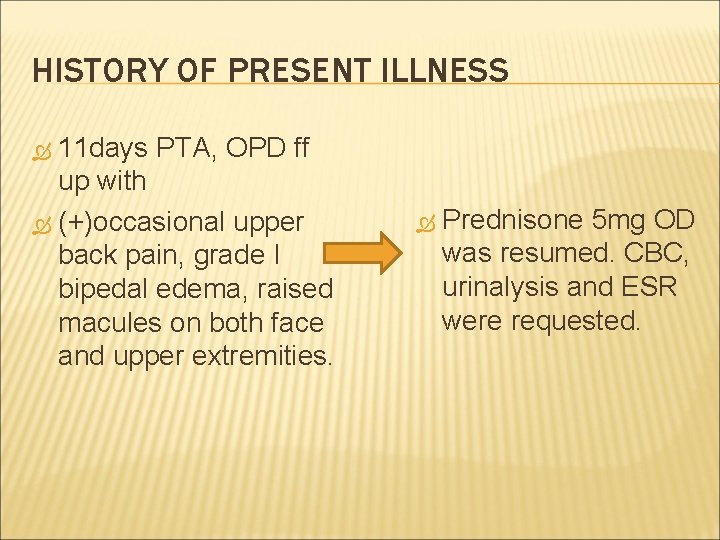
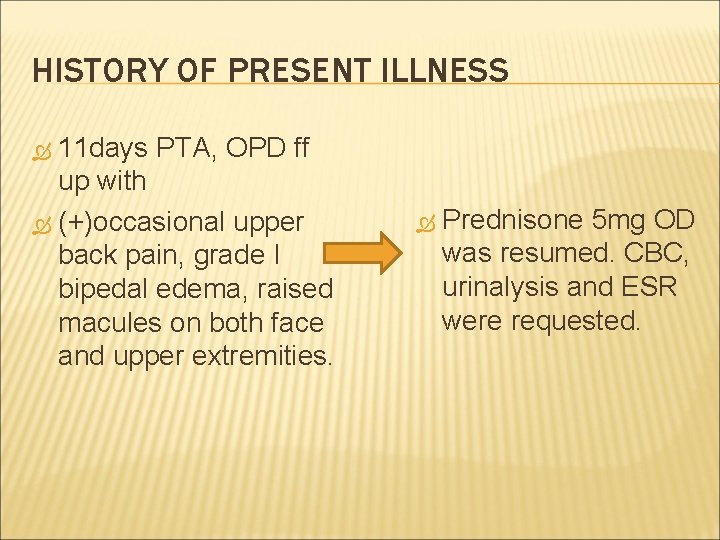
HISTORY OF PRESENT ILLNESS 11 days PTA, OPD ff up with (+)occasional upper back pain, grade I bipedal edema, raised macules on both face and upper extremities. Prednisone 5 mg OD was resumed. CBC, urinalysis and ESR were requested.
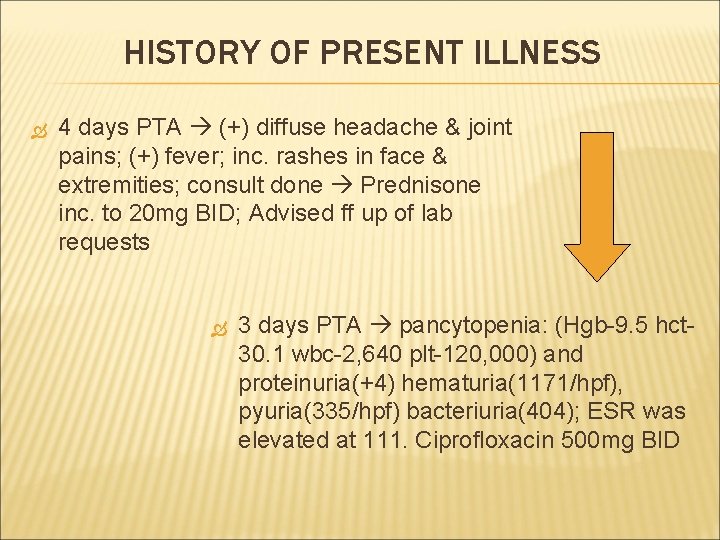
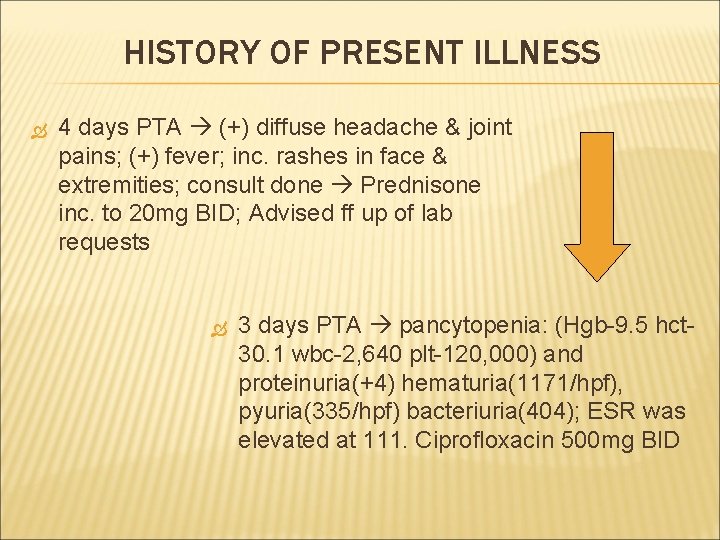
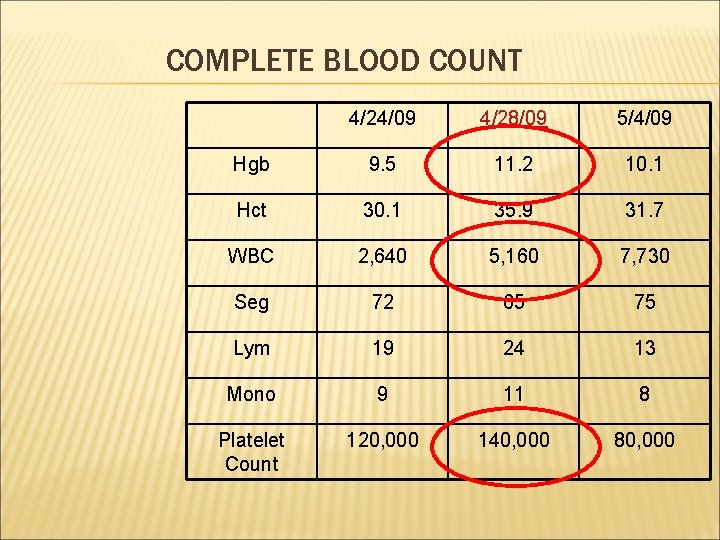
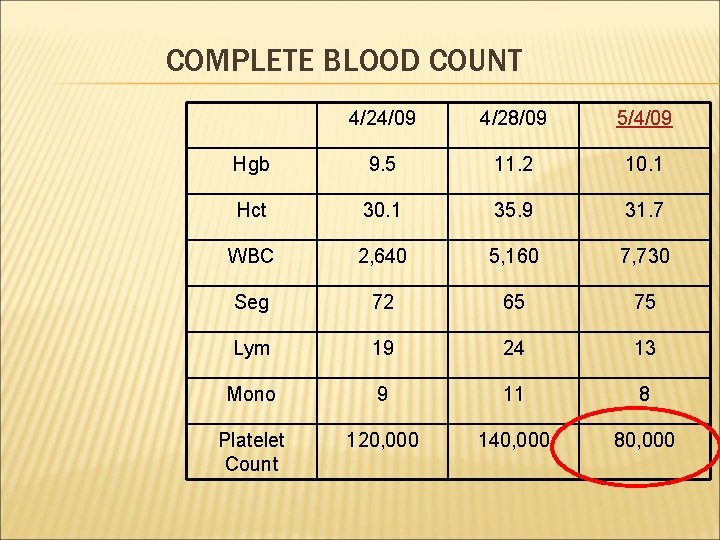
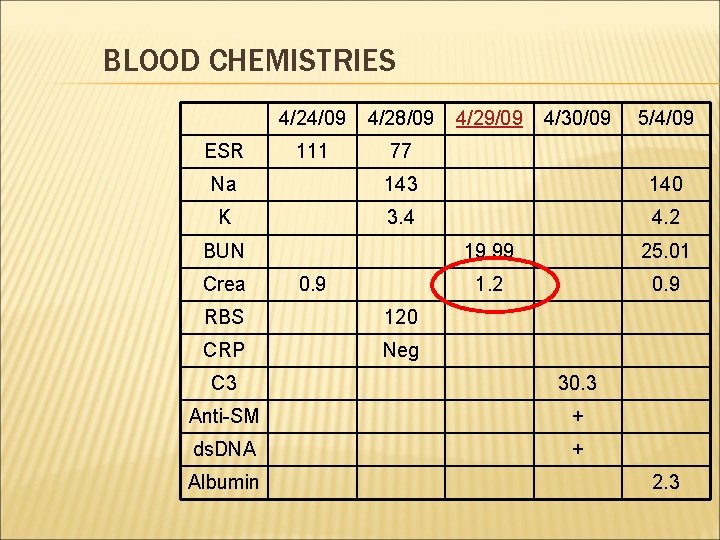
HISTORY OF PRESENT ILLNESS 4 days PTA (+) diffuse headache & joint pains; (+) fever; inc. rashes in face & extremities; consult done Prednisone inc. to 20 mg BID; Advised ff up of lab requests 3 days PTA pancytopenia: (Hgb-9. 5 hct 30. 1 wbc-2, 640 plt-120, 000) and proteinuria(+4) hematuria(1171/hpf), pyuria(335/hpf) bacteriuria(404); ESR was elevated at 111. Ciprofloxacin 500 mg BID
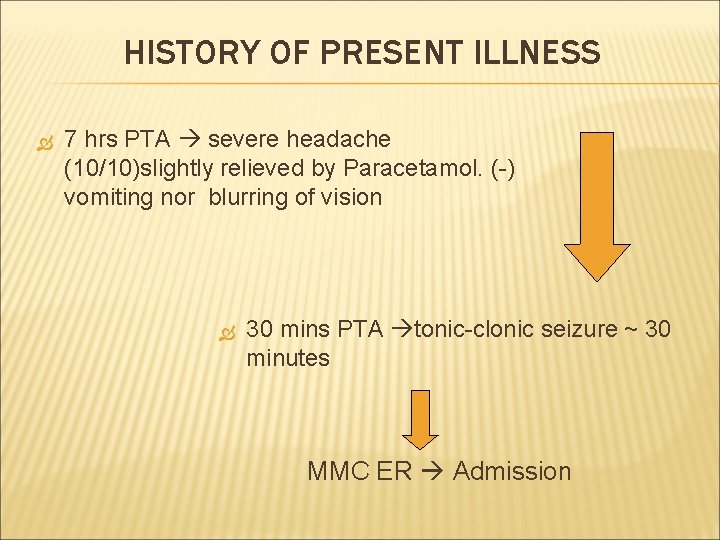
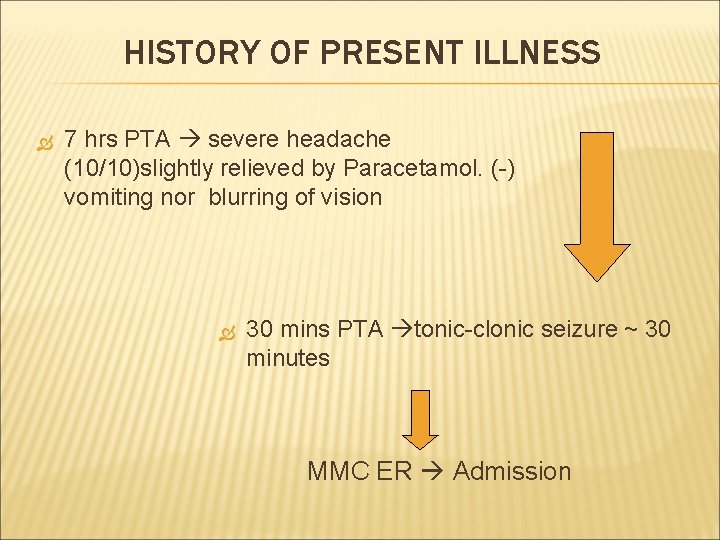
HISTORY OF PRESENT ILLNESS 7 hrs PTA severe headache (10/10)slightly relieved by Paracetamol. (-) vomiting nor blurring of vision 30 mins PTA tonic-clonic seizure ~ 30 minutes MMC ER Admission
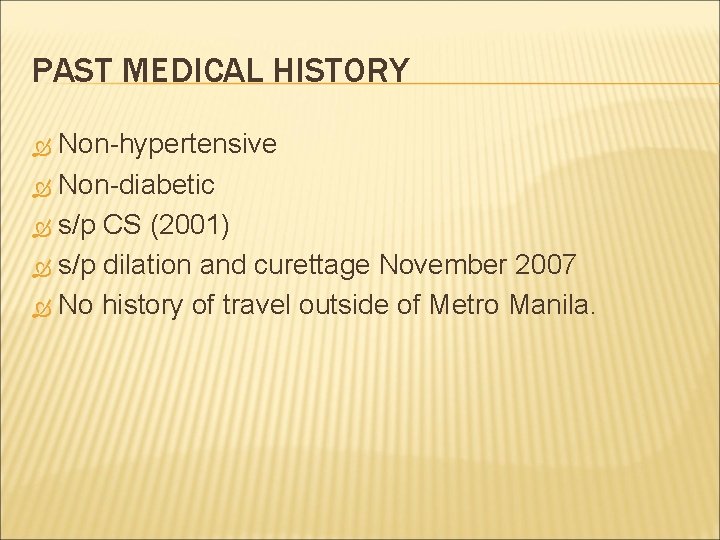
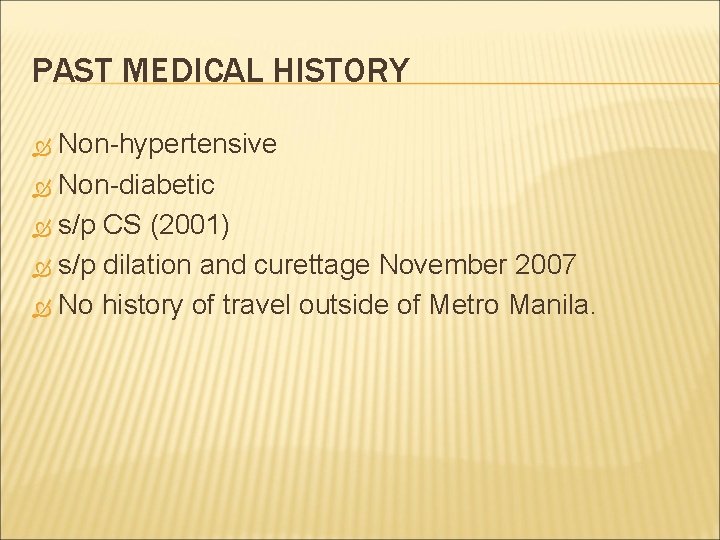
PAST MEDICAL HISTORY Non-hypertensive Non-diabetic s/p CS (2001) s/p dilation and curettage November 2007 No history of travel outside of Metro Manila.
Family History: No hypertension No diabetes No connective tissue disease. Personal and Social History: Non-smoker Non-alcoholic beverage drinker Worked as a bank teller prior to being diagnosed with SLE Currently stays at home and takes care of her children; can do light household chores
PHYSICAL EXAM Gen. Survey: Drowsy, not in cardio-respiratory distress Vital signs: BP = 200/100 170/100 HR 81 RR 20 Temp 36. 7 C Skin: raised macules on the face and both upper extremities • HEENT: Anicteric sclerae, pink palpebral conjunctivae, (+) subconjunctival effusion, no tonsillopharyngeal discharge, no cervical lymphadenopathy • Chest: Symmetrical chest expansion, no retractions, clear breath sounds
PHYSICAL EXAMINATION Heart: Adynamic precordium, distinct S 1 and S 2, normal rate and rhythm, no murmurs Abdomen: Flabby abdomen, soft, non-tender, normoactive bowel sounds Extremities: Full and equal pulses, no cyanosis and no edema
NEUROLOGICAL EXAM MSE: Drowsy, opens eyes to verbal stimulation but non-sustained, does not follow commands Cranial Nerves: Pupils 3 mm EBRTL; Full EOMS; (+) visual threat on all planes; (-) facial asymmetry; (+) gag Sensory: Withdraws to pain in all extremities MMT: Moves all extremities non-purposely Reflexes: +2 in all reflexes Pathologic Reflexes: No Babinski Meninges: Supple neck
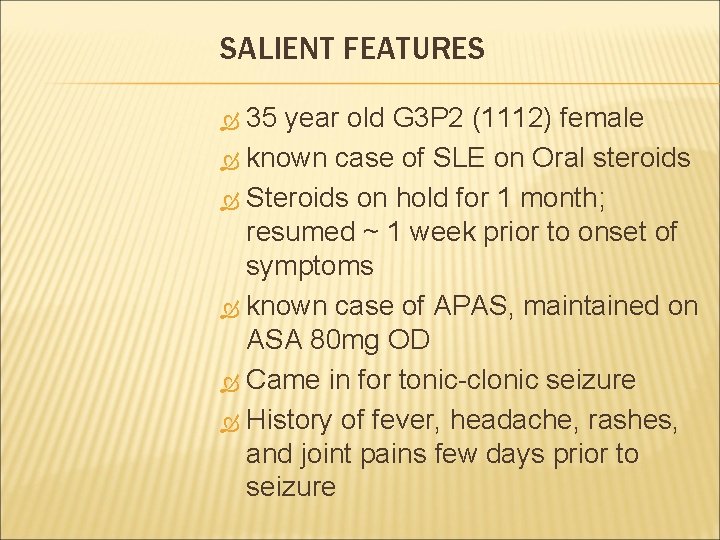
SALIENT FEATURES 35 year old G 3 P 2 (1112) female known case of SLE on Oral steroids Steroids on hold for 1 month; resumed ~ 1 week prior to onset of symptoms known case of APAS, maintained on ASA 80 mg OD Came in for tonic-clonic seizure History of fever, headache, rashes, and joint pains few days prior to seizure
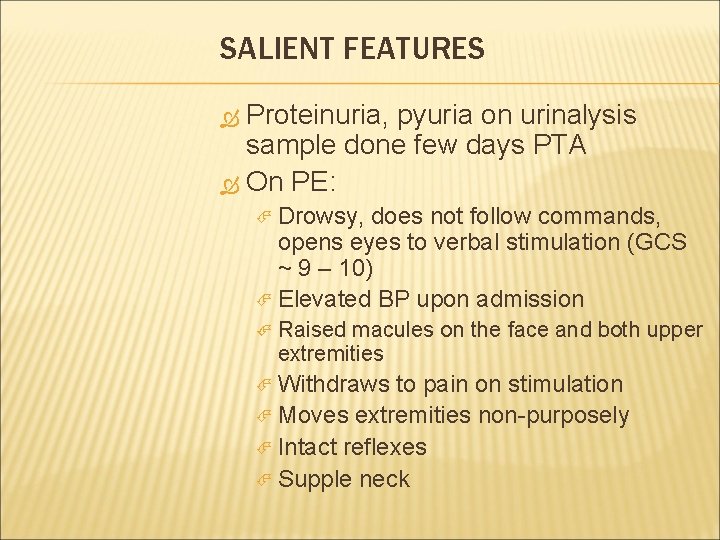
SALIENT FEATURES Proteinuria, pyuria on urinalysis sample done few days PTA On PE: Drowsy, does not follow commands, opens eyes to verbal stimulation (GCS ~ 9 – 10) Elevated BP upon admission Raised macules on the face and both upper extremities Withdraws to pain on stimulation Moves extremities non-purposely Intact reflexes Supple neck
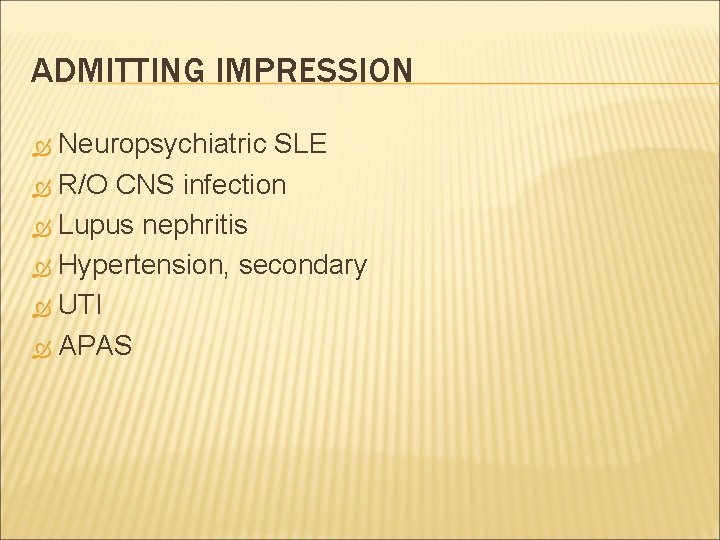
ADMITTING IMPRESSION Neuropsychiatric SLE R/O CNS infection Lupus nephritis Hypertension, secondary UTI APAS
COURSE IN THE WARD
UPON ADMISSION CBC, Urinalysis, C 3, 24 hour urine, ESR, anti. Smith, antids. DNA Complete Blood Count revealed improvement in pancytopenia Hydrocortisone 100 mg IV q 8 Referral to neurology service NGT feeding started
UPON ADMISSION…. 3 episodes of seizures at ER – Midazolam 5 mg IV Loading dose Phenytoin 300 mg IV x 2 doses 1 hour apart Phenytoin 100 mg IV q 8 Citicholine 1 g IV q 12 Mannitol 20% 75 ml IV q 6
UPON ADMISSION Urinalysis Co- amoxiclav 1. 2 g IV every 8 hours
UPON ADMISSION Lumbar tap done CT Scan revealed normal EEG Methylprednisolone 1 g IV in D 5 W 500 m. L x 4 hours for 3 days
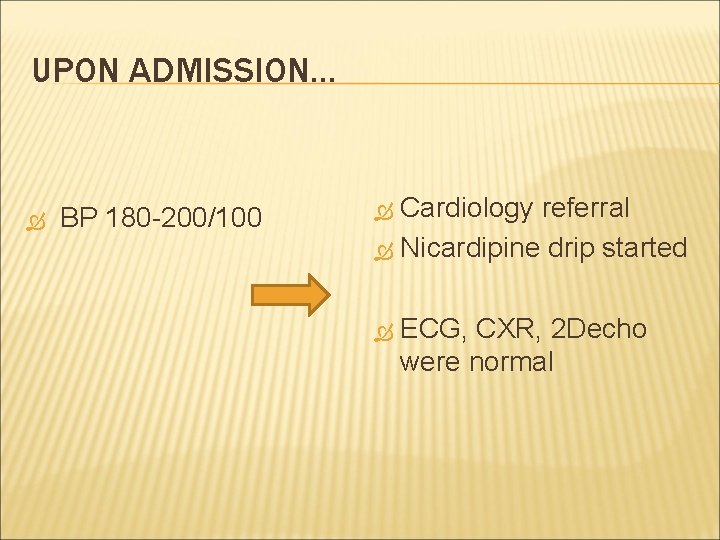
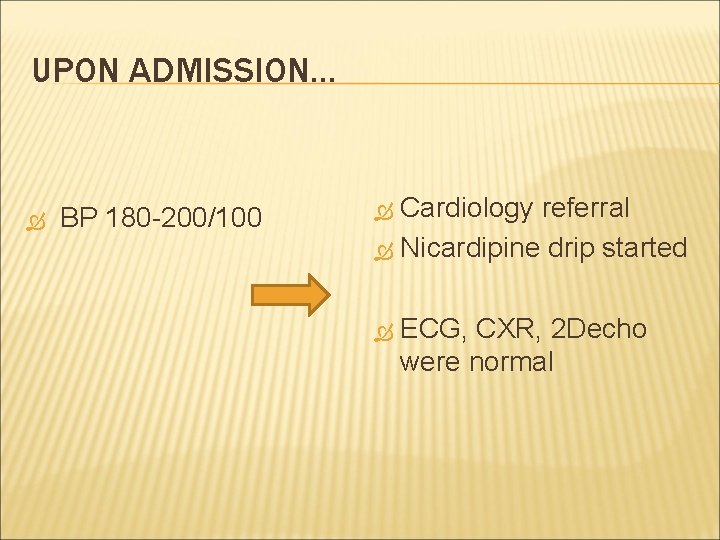
UPON ADMISSION… BP 180 -200/100 Cardiology referral Nicardipine drip started ECG, CXR, 2 Decho were normal
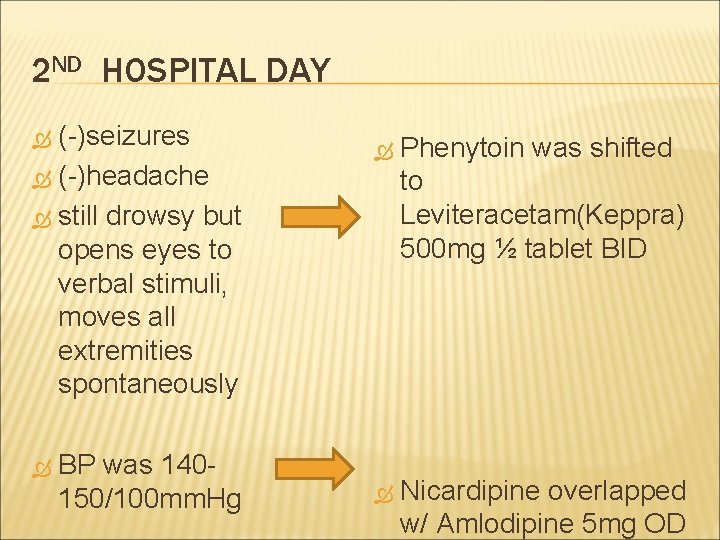
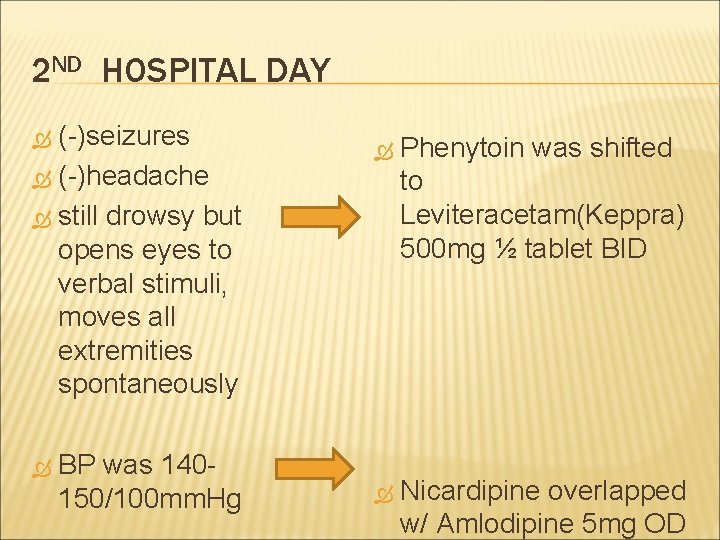
2 ND HOSPITAL DAY (-)seizures (-)headache still drowsy but opens eyes to verbal stimuli, moves all extremities spontaneously BP was 140150/100 mm. Hg Phenytoin was shifted to Leviteracetam(Keppra) 500 mg ½ tablet BID Nicardipine overlapped w/ Amlodipine 5 mg OD
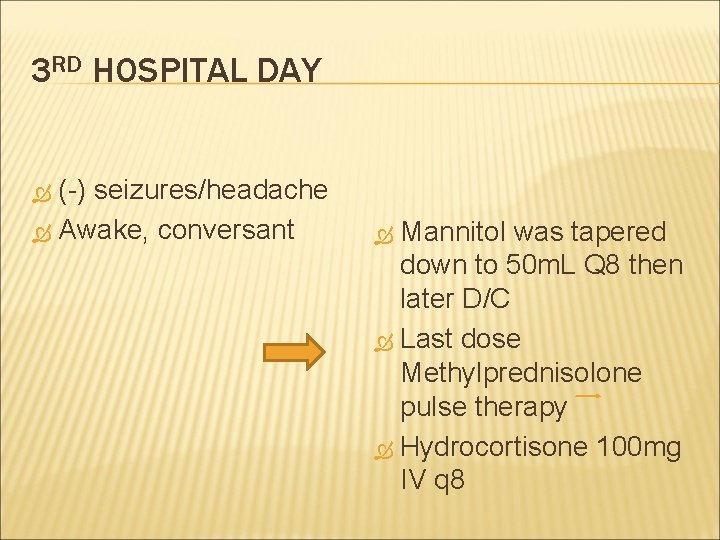
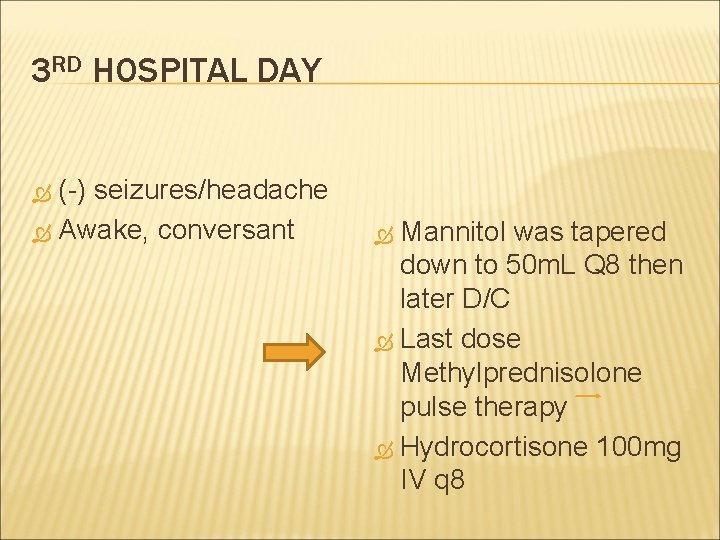
3 RD HOSPITAL DAY (-) seizures/headache Awake, conversant Mannitol was tapered down to 50 m. L Q 8 then later D/C Last dose Methylprednisolone pulse therapy Hydrocortisone 100 mg IV q 8
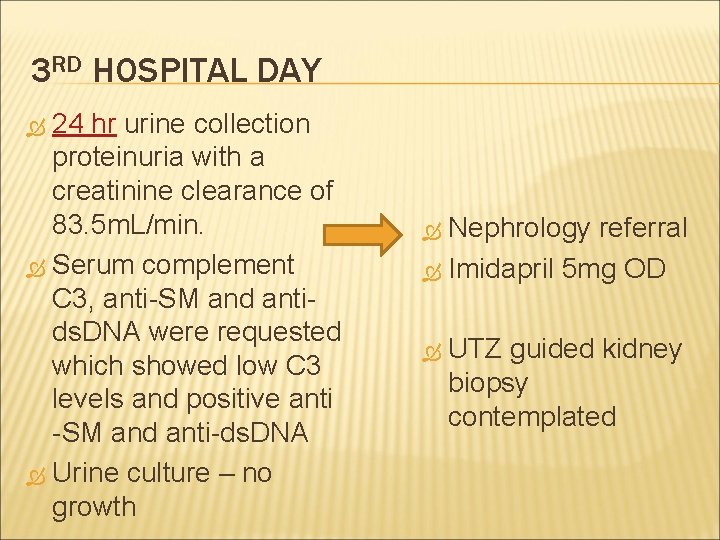
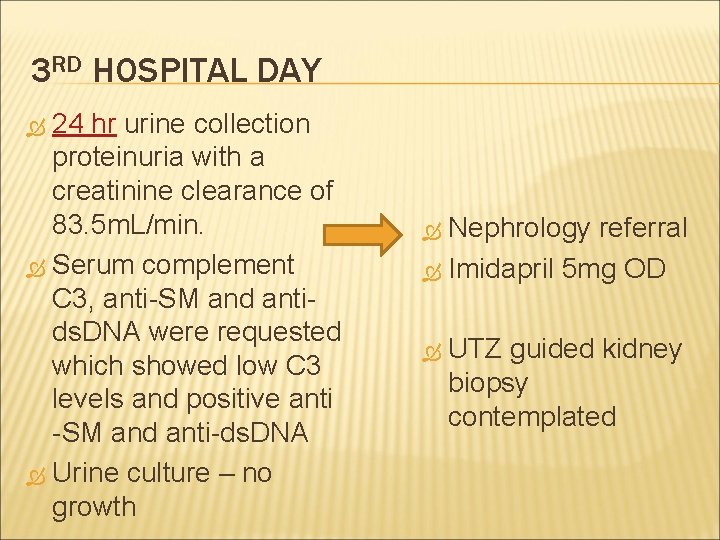
3 RD HOSPITAL DAY 24 hr urine collection proteinuria with a creatinine clearance of 83. 5 m. L/min. Serum complement C 3, anti-SM and antids. DNA were requested which showed low C 3 levels and positive anti -SM and anti-ds. DNA Urine culture – no growth Nephrology referral Imidapril 5 mg OD UTZ guided kidney biopsy contemplated
4 TH HOSPITAL DAY (-) seizures/headache Awake, conscious, coherent Tolerated soft diet, NGT removed Placed on full diet Hydrocortisone shifted to Prednisone 25 mg BID
5 TH HOSPITAL DAY No recurrence of seizures, headache, no fever Co- Amoxiclav IV was shifted to oral Co- Amoxiclav 625 mg BID ASA discontinued anticipating kidney biopsy Leviteracetam continued

6 TH HOSPITAL DAY No recurrence of seizures, headache, no fever Decrease in raised macules on face and UE CBC showed decrease in platelet to 80, 000 Prednisone increased to 30 mg BID Kidney biopsy to be done as outpatient
7 TH HOSPITAL DAY No recurrence of seizures, headache, no fever, significant decrease in malar rash and macules on upper extremities Patient cleared for discharge from all services
8 TH HOSPITAL DAY Patient discharged improved and stable
FINAL DIAGNOSIS NPSLE Lupus Nephritis Hypertension, secondary Urinary Tract Infection, resolved APAS

DISCUSSION
BACKGROUND Systemic lupus erythematosus (SLE) multisystem autoimmune connective tissue disorder with various clinical presentations Affects many organ systems, including the central and peripheral nervous systems and muscles. 90% of patients are women of childbearing age Incidence is 12 -39 cases per 100, 000 people With full access to medical care, overall survival for SLE is 85% at 5 years and 63% at 15 years Harrison’s Principles of Internal Medicine 17 th Ed.
PATHOPHYSIOLOGY SLE is caused by interactions between susceptible genes and environmental factor resulting in abnormal immune response 1. Hyper-reactivity and hypersensitivity of T and B lymphocytes 2. Ineffective regulation of antigen availability and ongoing antibody response Harrison’s Principles of Internal Medicine 17 th Ed.
PATHOPHYSIOLOGY End result: sustained production of pathogenic auto -antibodies and formation of immune complexes that bind target tissues, resulting in: 1. Sequestration and destruction of Ig-coated circulating cells 2. Fixation and cleaving of complement proteins 3. Release of chemotaxins, vasoactive peptides, and destructive enzymes into tissues

ARA CRITERIA FOR DIAGNOSIS: Malar rash Discoid rash Photosensitivity Oral ulcers Fixed erythema, flat or raised, over malar eminence Erythematous circular raised patches with adherent keratotic scaling and follicular plugging; atropic scarring may occur Exposure to UV light causes rashes Oral or nasopharyngeal Arthritis Nonerosive, involving 2 or more joints Serositis Pleuritis: + pleuritic pain or rub, OR pleural effusion, OR pericardial effusion Renal disorder Neurologic disorder Persistent proteinuria OR cellular casts Seizures or psychosis Hematologic disorder Hemolytic anemia with reticulocytosis OR Leukopenia < 4000 OR lymphopenia < 1, 500 OR thrombocytopenia < 100, 000 ANA Positive; if negative, check for anti-SSA (Ro) antibodies Anti-ds. DNA or antismith antibody Positive; highly specific for SLE Harrison’s Principles of Internal Medicine 17 th Ed.
NEUROPSYCHIATRIC SLE
HISTORICAL BACKGROUND Hebra and Kaposi (1875) Noted first neurologic involvement in SLE Over the last 3 decades, appreciation of • Baum (1904) Related active delirium, Clinical significance of antineuronal, aphasia and hemiparesis to probable antiribosomal P, and antiphospholipid disseminated LE antibodies as well as advances in brain • Daly (1945) conducted 1 st modern Imaging have again altered our concept of study of NP-SLE • Lewis (1954) 1 st to focus on importance of EEG findings and psychometric testing in patients with NP-SLE Joseph FG, Lammie AG, Scolding NG. CNS lupus: A study of 41 patients. Neurology. 2007
CLASSIFICATION AND CLINICAL PRESENTATION Incidence of neuropsychiatric manifestations in SLE ranges from 14 – 75% • Patients with NP-SLE can present with a myriad of diffuse and/or focal symptoms and signs involving the brain, spinal cord, or peripheral nervous system
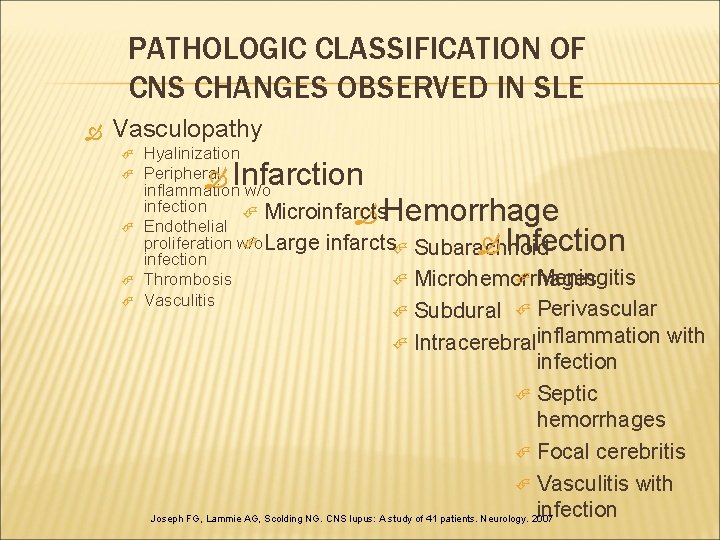
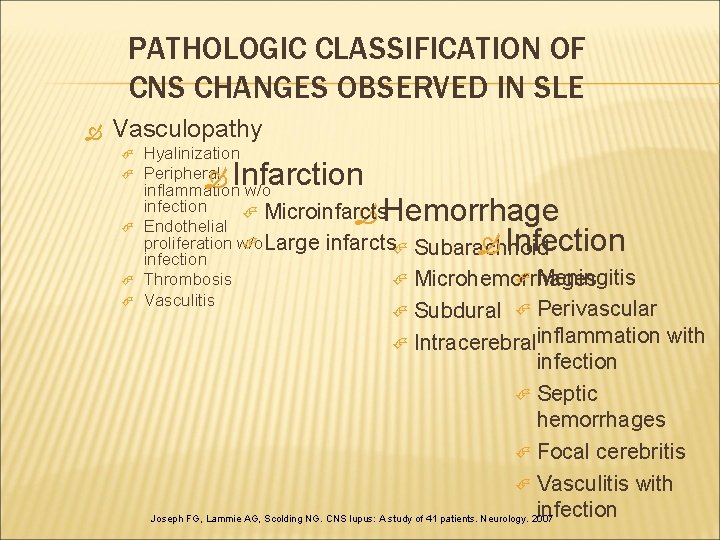
PATHOLOGIC CLASSIFICATION OF CNS CHANGES OBSERVED IN SLE Vasculopathy Hyalinization Peripheral inflammation w/o infection Microinfarcts Endothelial proliferation w/o Large infarcts infection Thrombosis Vasculitis Infarction Hemorrhage Infection Subarachnoid Meningitis Microhemorrhages Subdural Perivascular Intracerebralinflammation with infection Septic hemorrhages Focal cerebritis Vasculitis with infection Joseph FG, Lammie AG, Scolding NG. CNS lupus: A study of 41 patients. Neurology. 2007
PATHOPHYSIOLOGY OF NERVOUS SYSTEM INVOLVEMENT 1. 2. 3. Vasculopathy Auto-antibodies Others Schur PH, Khoshbin S. Neurologic manifestations of systemic lupus erythematosus. www. Uptodate. com
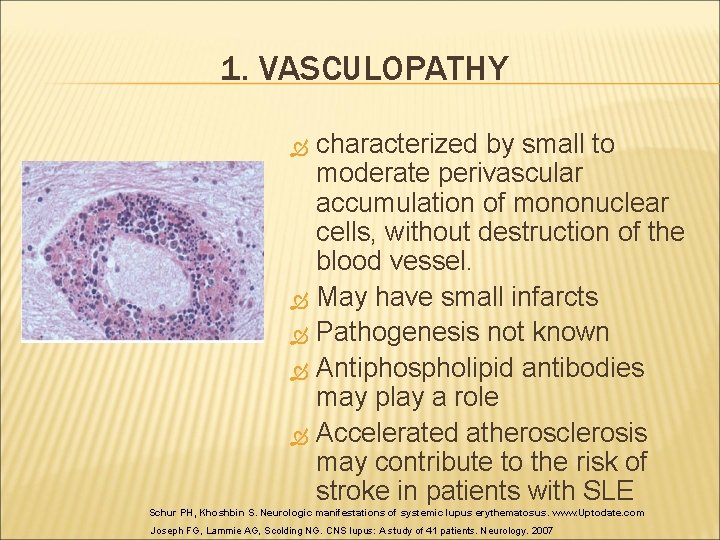
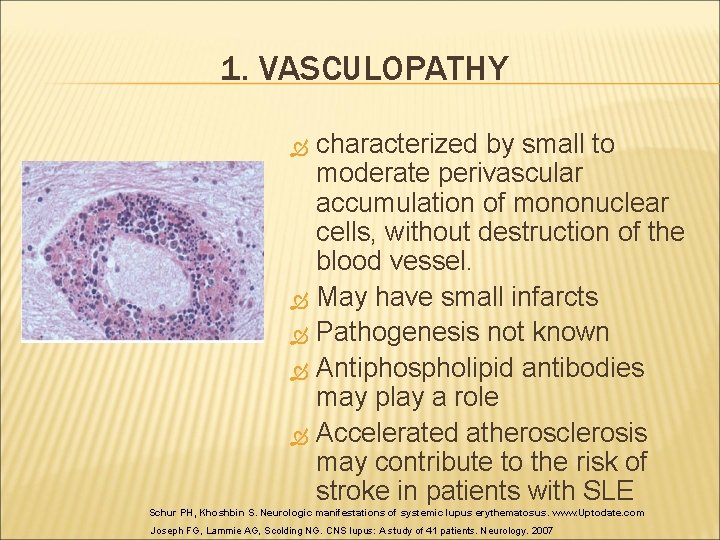
1. VASCULOPATHY characterized by small to moderate perivascular accumulation of mononuclear cells, without destruction of the blood vessel. May have small infarcts Pathogenesis not known Antiphospholipid antibodies may play a role Accelerated atherosclerosis may contribute to the risk of stroke in patients with SLE Schur PH, Khoshbin S. Neurologic manifestations of systemic lupus erythematosus. www. Uptodate. com Joseph FG, Lammie AG, Scolding NG. CNS lupus: A study of 41 patients. Neurology. 2007
2. AUTO-ANTIBODIES (+) Antineuronal antibodies found in one report in 45 percent of patients with CNS lupus Cognitive dysfunction associated with lymphocytotoxic antibodies Antiphospholipid antibodies increase the risk of stroke syndromes, recurrent seizures and abnormal findings on MRI Schur PH, Khoshbin S. Neurologic manifestations of systemic lupus erythematosus. www. Uptodate. com
Antiribosomal P protein antibodies associated with lupus psychosis and depression but not with cognitive dysfunction or psychologic distress High levels of autoantibodies to a 50 k. Da antigen located in the plasma membrane of brain synaptic terminals in 19 of 20 patients with SLE who had CNS involvement • Antiribosomal-P autoantibodies from psychiatric lupus target a novel neuronal surface protein causing calcium influx and apoptosis Soledad Matus, 1, 2, 4 Patricia V. Burgos, 1, 2, 4 Marcela Bravo-Zehnder, 1, 2, 4 Regine Kraft, 6 Omar H. Porras, 5
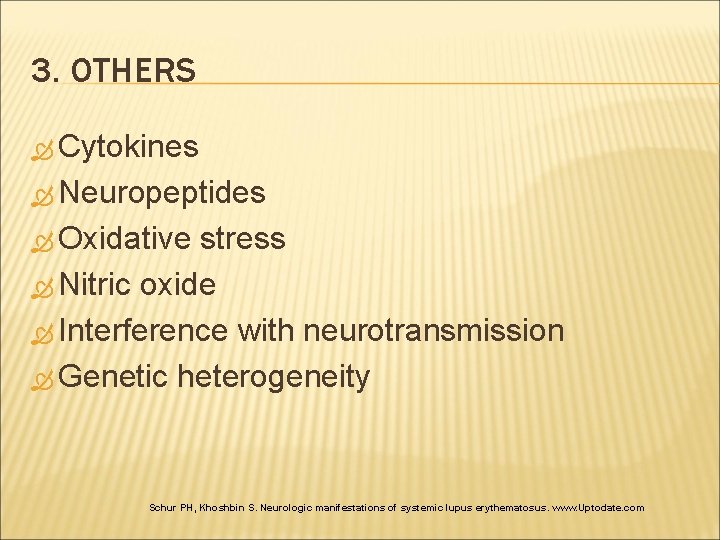
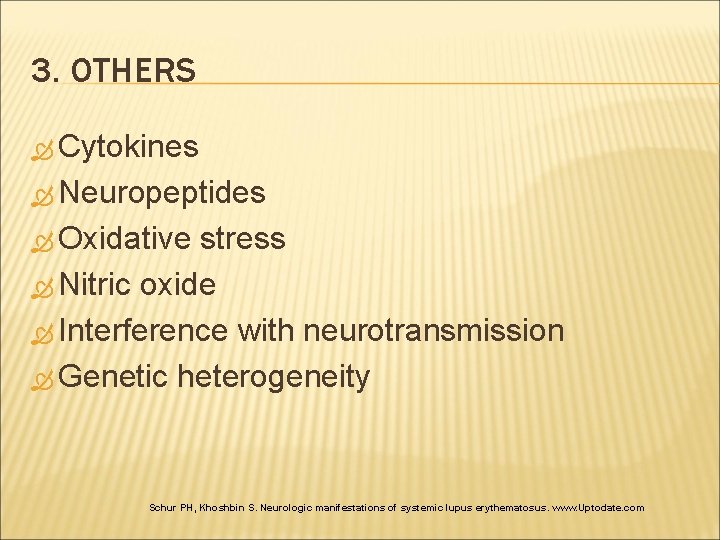
3. OTHERS Cytokines Neuropeptides Oxidative stress Nitric oxide Interference with neurotransmission Genetic heterogeneity Schur PH, Khoshbin S. Neurologic manifestations of systemic lupus erythematosus. www. Uptodate. com
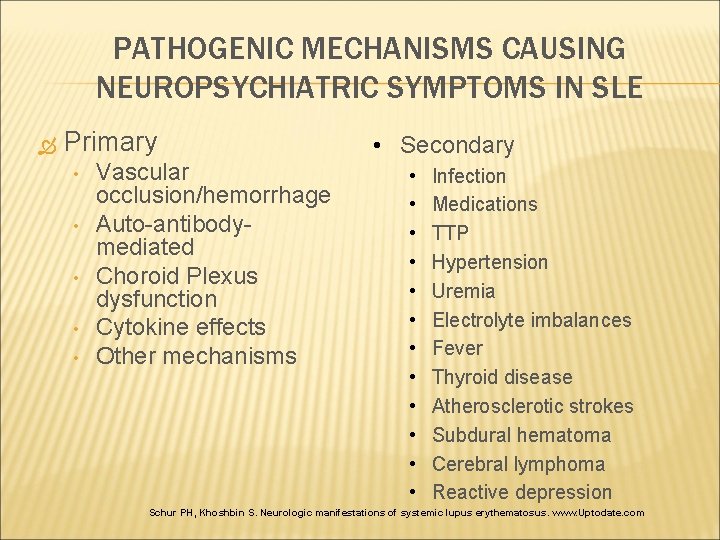
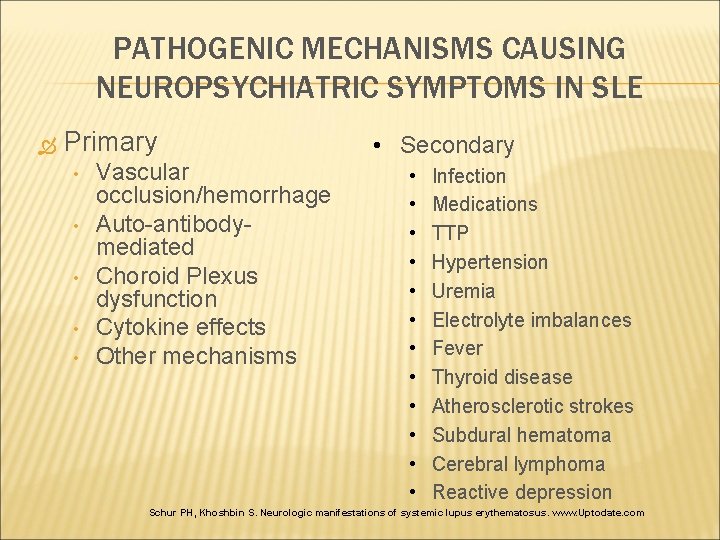
PATHOGENIC MECHANISMS CAUSING NEUROPSYCHIATRIC SYMPTOMS IN SLE Primary • • • Vascular occlusion/hemorrhage Auto-antibodymediated Choroid Plexus dysfunction Cytokine effects Other mechanisms • Secondary • • • Infection Medications TTP Hypertension Uremia Electrolyte imbalances Fever Thyroid disease Atherosclerotic strokes Subdural hematoma Cerebral lymphoma Reactive depression Schur PH, Khoshbin S. Neurologic manifestations of systemic lupus erythematosus. www. Uptodate. com
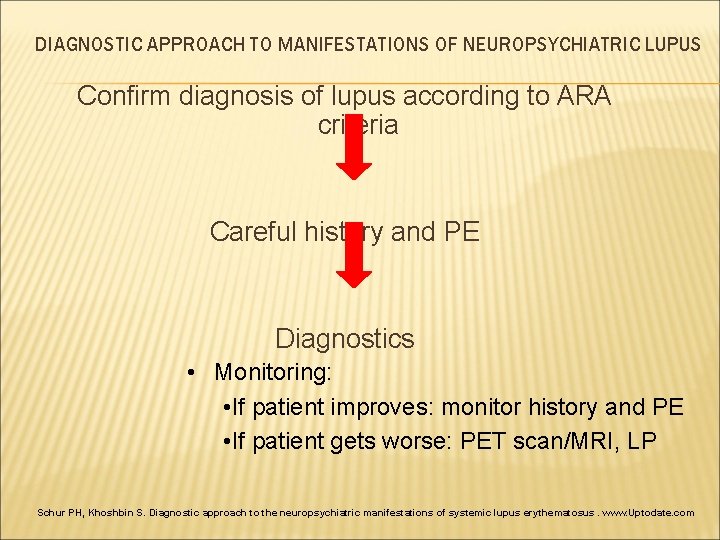
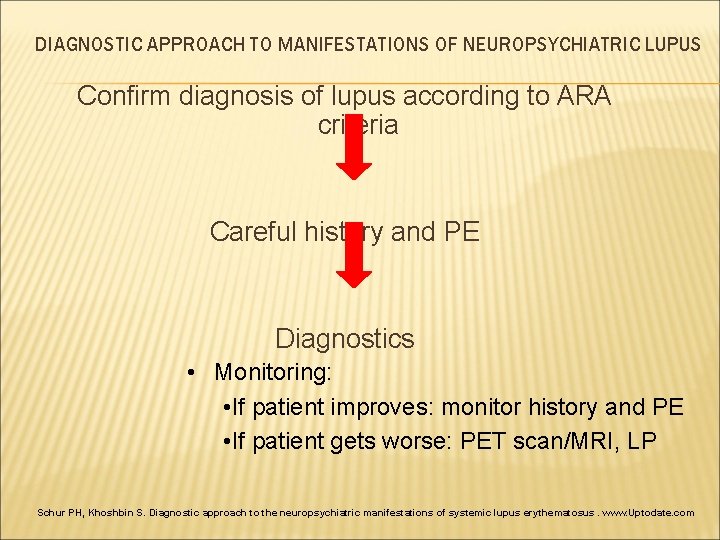
DIAGNOSTIC APPROACH TO MANIFESTATIONS OF NEUROPSYCHIATRIC LUPUS Confirm diagnosis of lupus according to ARA criteria Careful history and PE Diagnostics • Monitoring: • If patient improves: monitor history and PE • If patient gets worse: PET scan/MRI, LP Schur PH, Khoshbin S. Diagnostic approach to the neuropsychiatric manifestations of systemic lupus erythematosus. www. Uptodate. com
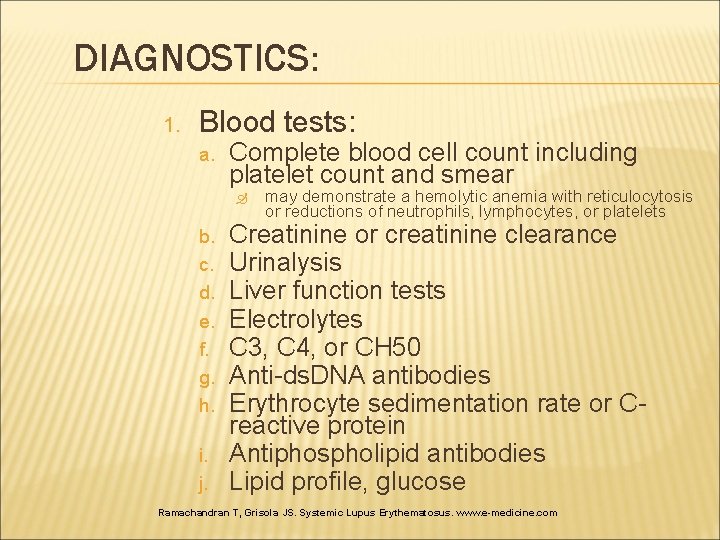
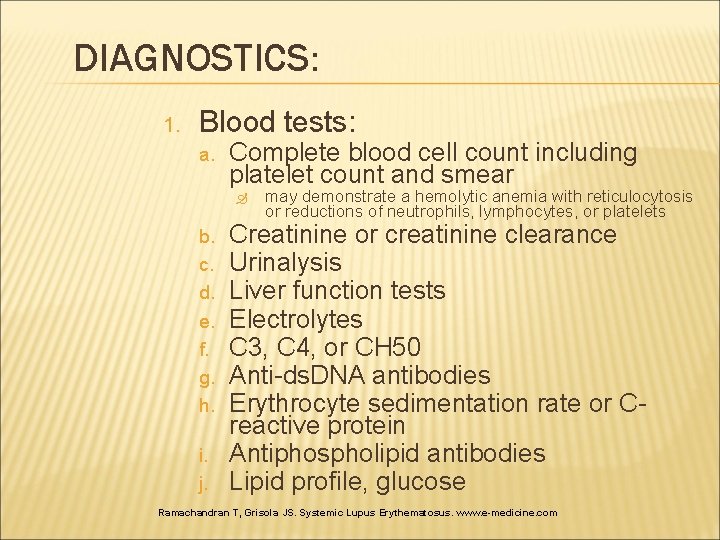
DIAGNOSTICS: 1. Blood tests: a. Complete blood cell count including platelet count and smear b. c. d. e. f. g. h. i. j. may demonstrate a hemolytic anemia with reticulocytosis or reductions of neutrophils, lymphocytes, or platelets Creatinine or creatinine clearance Urinalysis Liver function tests Electrolytes C 3, C 4, or CH 50 Anti-ds. DNA antibodies Erythrocyte sedimentation rate or Creactive protein Antiphospholipid antibodies Lipid profile, glucose Ramachandran T, Grisola JS. Systemic Lupus Erythematosus. www. e-medicine. com
DIAGNOSTICS: 2. CSF Studies: a. b. c. d. e. f. g. h. Cell count Protein Glucose Cultures Gram stain and other special stains VDRL Ig. G index Oligoclonal bands Ramachandran T, Grisola JS. Systemic Lupus Erythematosus. www. e-medicine. com
DIAGNOSTICS: 3. Imaging: a. b. CT Scan indicated for suspected acute hemorrhage and in patients with contraindications to MRI (intracranial metal, pacemakers, etc. ) MRI more sensitive and used to define site and extent of lesions. A negative MRI result does not rule out CNS lupus, and MRI abnormalities may not be diagnostic of NPSLE. Follow-up MRIs may be indicated to document progression, improvement, or significance of lesions Ramachandran T, Grisola JS. Systemic Lupus Erythematosus. www. e-medicine. com
DIAGNOSTICS Positron emission tomography (PET) and single photon emission computed tomography (SPECT) have also been explored as functional imaging tools in lupus and both appear to be more sensitive in detecting subtle brain changes in NPSLE
DIAGNOSTICS: 4. EEG Standard EEG indicated in seizures and encephalopathies. Evoked potentials are performed for suspected demyelinating disease. 5. Psychologic Testing 6. Others: 2 D echo Ramachandran T, Grisola JS. Systemic Lupus Erythematosus. www. e-medicine. com
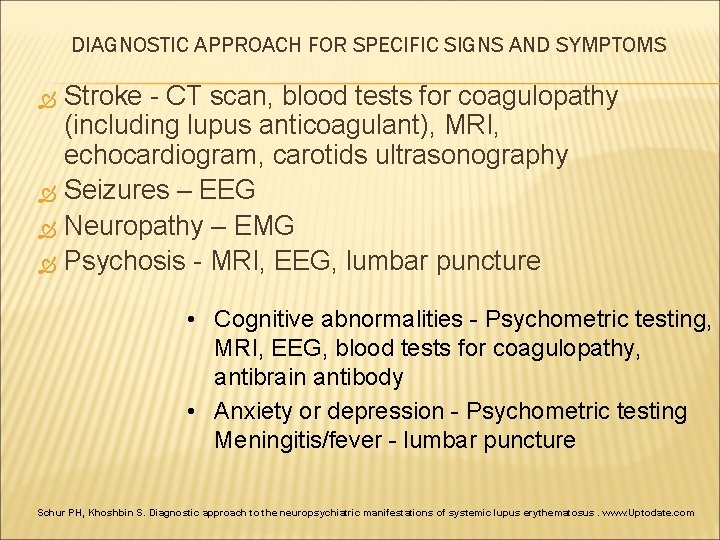
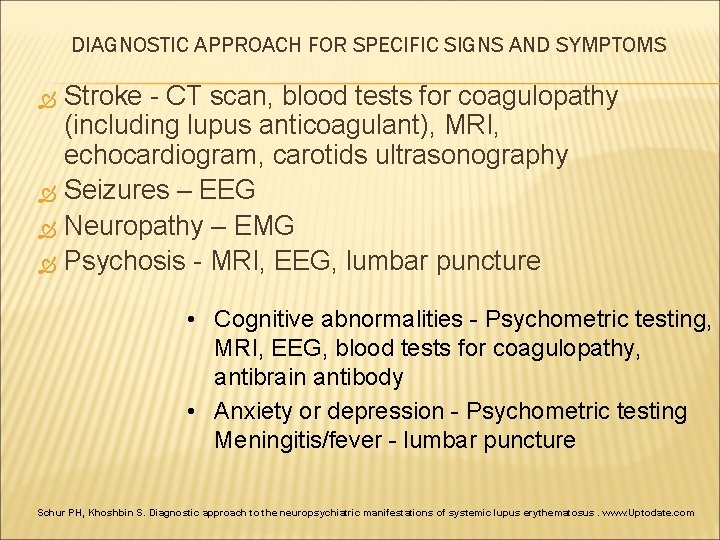
DIAGNOSTIC APPROACH FOR SPECIFIC SIGNS AND SYMPTOMS Stroke - CT scan, blood tests for coagulopathy (including lupus anticoagulant), MRI, echocardiogram, carotids ultrasonography Seizures – EEG Neuropathy – EMG Psychosis - MRI, EEG, lumbar puncture • Cognitive abnormalities - Psychometric testing, MRI, EEG, blood tests for coagulopathy, antibrain antibody • Anxiety or depression - Psychometric testing Meningitis/fever - lumbar puncture Schur PH, Khoshbin S. Diagnostic approach to the neuropsychiatric manifestations of systemic lupus erythematosus. www. Uptodate. com
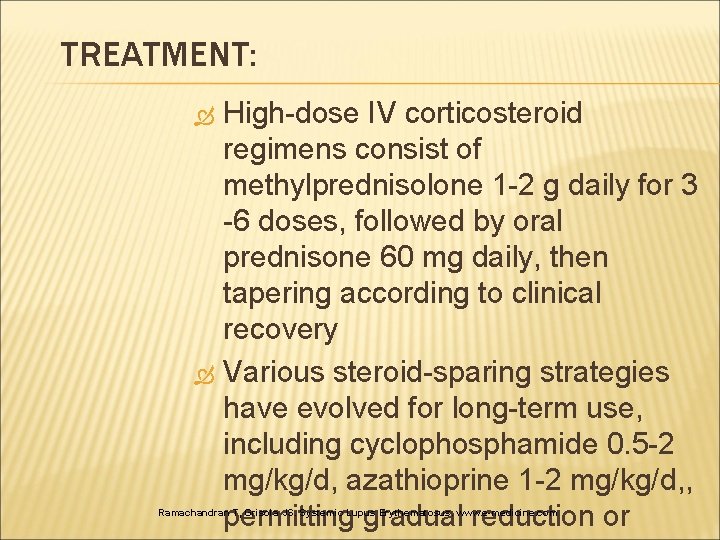
TREATMENT: High-dose IV corticosteroid regimens consist of methylprednisolone 1 -2 g daily for 3 -6 doses, followed by oral prednisone 60 mg daily, then tapering according to clinical recovery Various steroid-sparing strategies have evolved for long-term use, including cyclophosphamide 0. 5 -2 mg/kg/d, azathioprine 1 -2 mg/kg/d, , permitting gradual reduction or Ramachandran T, Grisola JS. Systemic Lupus Erythematosus. www. e-medicine. com
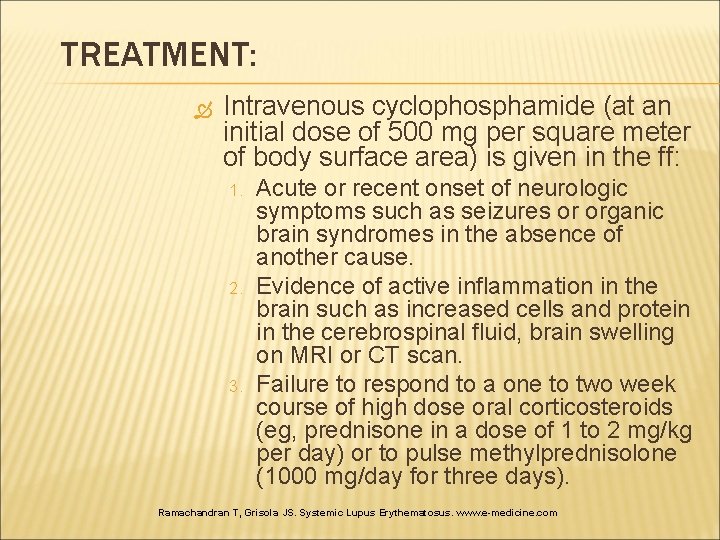
TREATMENT: Intravenous cyclophosphamide (at an initial dose of 500 mg per square meter of body surface area) is given in the ff: 1. 2. 3. Acute or recent onset of neurologic symptoms such as seizures or organic brain syndromes in the absence of another cause. Evidence of active inflammation in the brain such as increased cells and protein in the cerebrospinal fluid, brain swelling on MRI or CT scan. Failure to respond to a one to two week course of high dose oral corticosteroids (eg, prednisone in a dose of 1 to 2 mg/kg per day) or to pulse methylprednisolone (1000 mg/day for three days). Ramachandran T, Grisola JS. Systemic Lupus Erythematosus. www. e-medicine. com
CLINICAL UPDATES
IV CYCLOPHOSPHAMIDE VS METHYLPREDNISOLONE Patients and methods: RCT at two tertiary care centres of patients with SLE with severe NP manifestations such as seizures, optic neuritis, peripheral or cranial neuropathy, coma, brainstem disease, or transverse myelitis. Induction treatment with 3 g of IV methylprednisolone (MP) followed by either IV monthly cyclophosphamide (Cy) versus IV MP bimonthly every 4 months for 1 year and then IV Cy or IV MP every 3 months for another year. The primary end point was response to treatment: at least 20% improvement from basal conditions on clinical, laboratory, or specific neurological testing variables.
RESULTS Of the 32 patients studied, 18/19 receiving Cy and 7/13 receiving MP responded to treatment (p, 0. 03) CONCLUSIONS Cy was significantly more effective than MP. Cy was clearly better in patients with seizures, peripheral neuropathy, optic neuritis, and brainstem disease, while differences were not clear in coma and transverse myelitis
CLINICAL UPDATES
EFFICACY OF RITUXIMAB (ANTI-CD 20) FOR REFRACTORY SLE INVOLVING CNS Study describes the results of treatment of patients with NPSLE who had previously failed to respond to various immunosuppressants. Rituximab anti-CD 20 antibody a chimeric antibody that directly targets B cells a biological preparation that eliminates B cells through a variety of mechanisms such as antibody-dependent cellular cytotoxicity, complement-dependent cytotoxicity and apoptosis. has recently been used for the treatment of a variety of SLE disease conditions and good therapeutic response has been reported
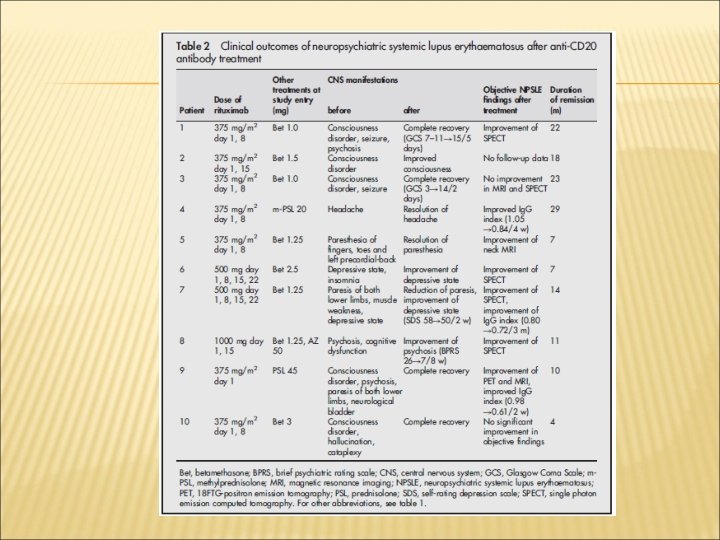
EFFICACY OF RITUXIMAB (ANTI-CD 20) FOR REFRACTORY SLE INVOLVING CNS Inclusion Criteria: 1. 2. Presence of a highly active disease CNS lesions resistant to conventional treatment. such as intravenous cyclophosphamide pulse treatment (IV-CY), cyclosporine A (Cs. A), PE and immunoadsorption therapy Treatment Protocol: • • Patients 1– 5 and 10 treated with 375 mg/m 2 rituximab once a week for 2 weeks Patient 9 treated with single dose of 375 mg/m 2 rituximab Patients 6 and 7 treated with 500 mg rituximab once a week for 4 weeks Patient 8 treated with 1000 mg once biweekly for 4 weeks.
RESULTS Treatment with rituximab resulted in rapid improvement of central nervous systemrelated manifestations, particularly acute confusional state. Rituximab also improved cognitive dysfunction, psychosis and seizure, and reduced the SLE Disease Activity Index Score at day 28 in all 10 patients. These effects lasted for >1 year in five patients. Flow cytometric analysis showed that rituximab down regulated CD 40 and CD 80 on B cells and CD 40 L, CD 69 and inducible costimulator on CD 4+ T cells.
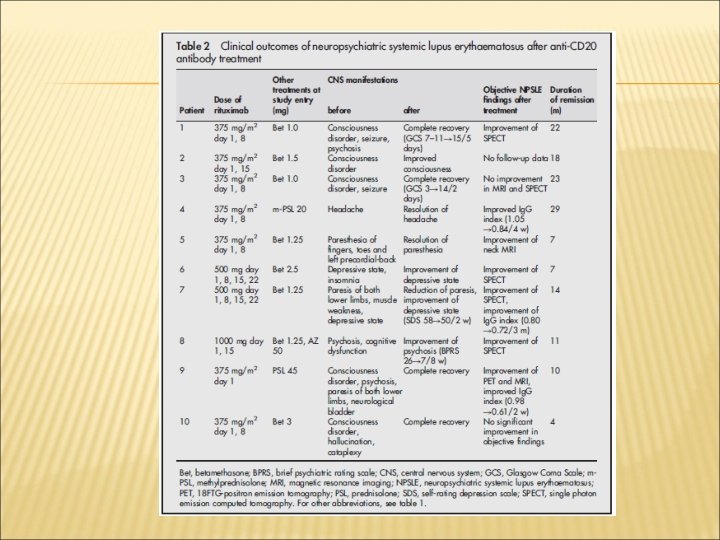
CONCLUSION Rituximab rapidly improved refractory NPSLE, as evident by resolution of various clinical signs and symptoms and improvement of radiographic findings. The down regulation of functional molecules on B and T cells suggests that rituximab modulates the interaction of activated B and T cells through costimulatory molecules. These results warrant further analysis of rituximab as treatment for NPSLE
THANK YOU
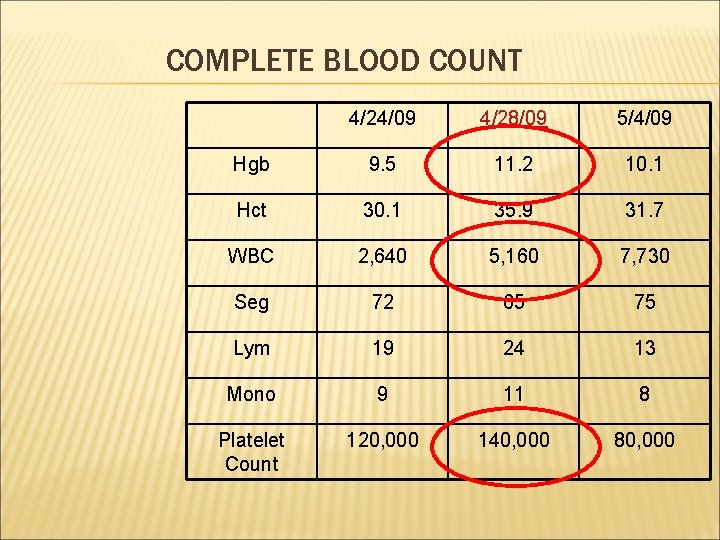
COMPLETE BLOOD COUNT 4/24/09 4/28/09 5/4/09 Hgb 9. 5 11. 2 10. 1 Hct 30. 1 35. 9 31. 7 WBC 2, 640 5, 160 7, 730 Seg 72 65 75 Lym 19 24 13 Mono 9 11 8 Platelet Count 120, 000 140, 000 80, 000
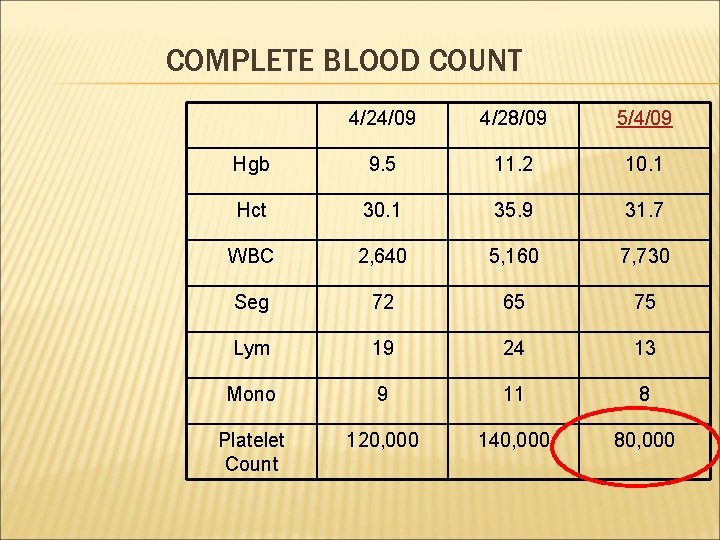
COMPLETE BLOOD COUNT 4/24/09 4/28/09 5/4/09 Hgb 9. 5 11. 2 10. 1 Hct 30. 1 35. 9 31. 7 WBC 2, 640 5, 160 7, 730 Seg 72 65 75 Lym 19 24 13 Mono 9 11 8 Platelet Count 120, 000 140, 000 80, 000
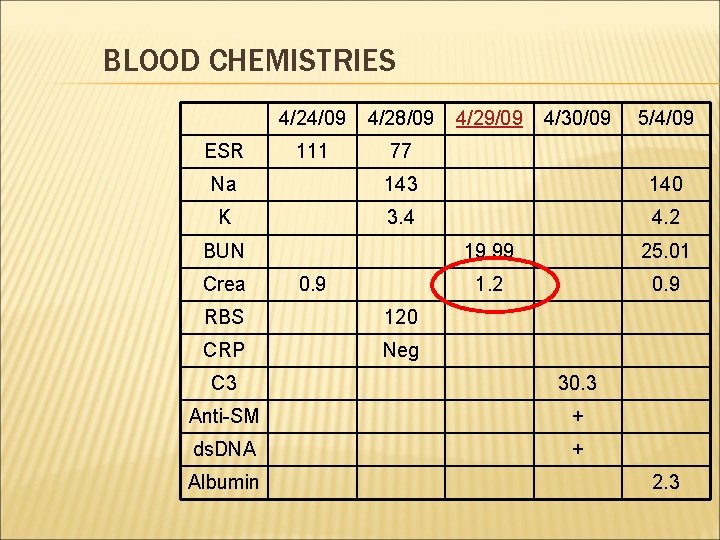
BLOOD CHEMISTRIES ESR 4/24/09 4/28/09 111 77 4/29/09 4/30/09 5/4/09 Na 143 140 K 3. 4 4. 2 BUN Crea 0. 9 RBS 120 CRP Neg 19. 99 25. 01 1. 2 0. 9 C 3 30. 3 Anti-SM + ds. DNA + Albumin 2. 3
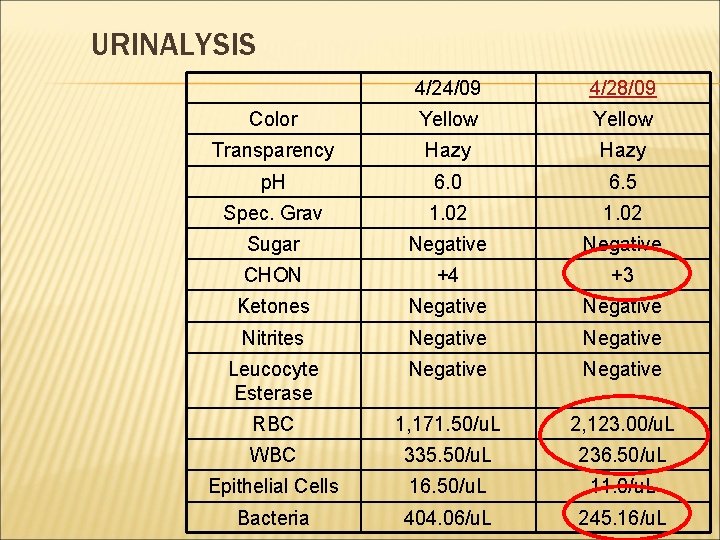
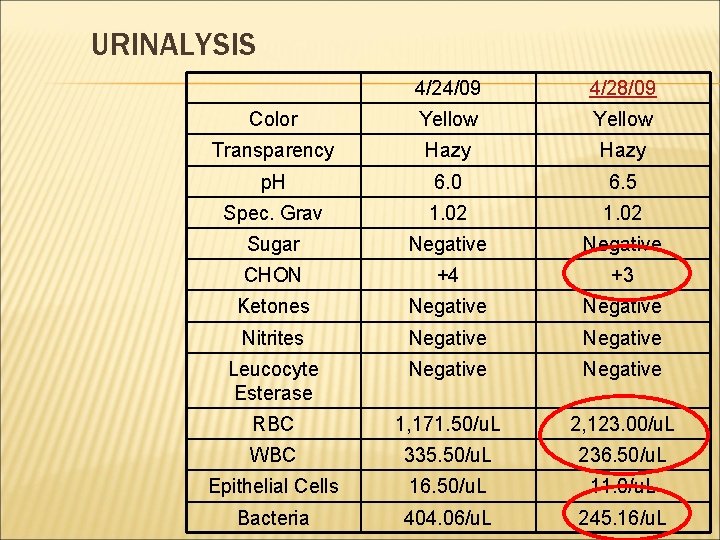
URINALYSIS 4/24/09 4/28/09 Color Yellow Transparency Hazy p. H 6. 0 6. 5 Spec. Grav 1. 02 Sugar Negative CHON +4 +3 Ketones Negative Nitrites Negative Leucocyte Esterase Negative RBC 1, 171. 50/u. L 2, 123. 00/u. L WBC 335. 50/u. L 236. 50/u. L Epithelial Cells 16. 50/u. L 11. 0/u. L Bacteria 404. 06/u. L 245. 16/u. L
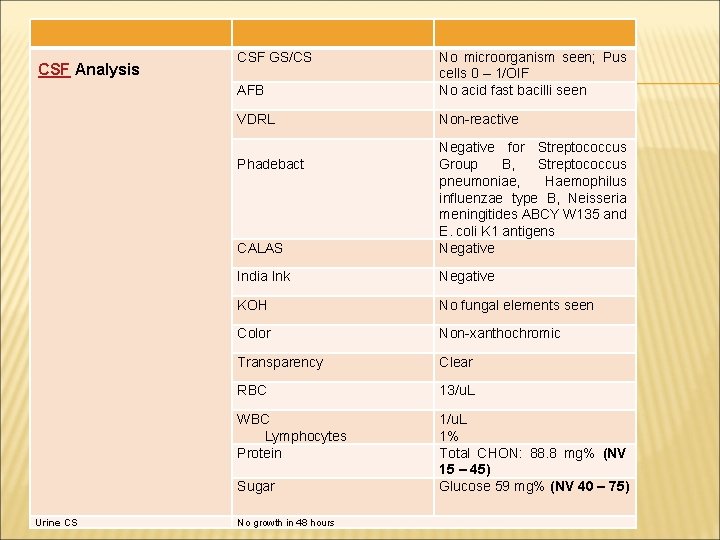
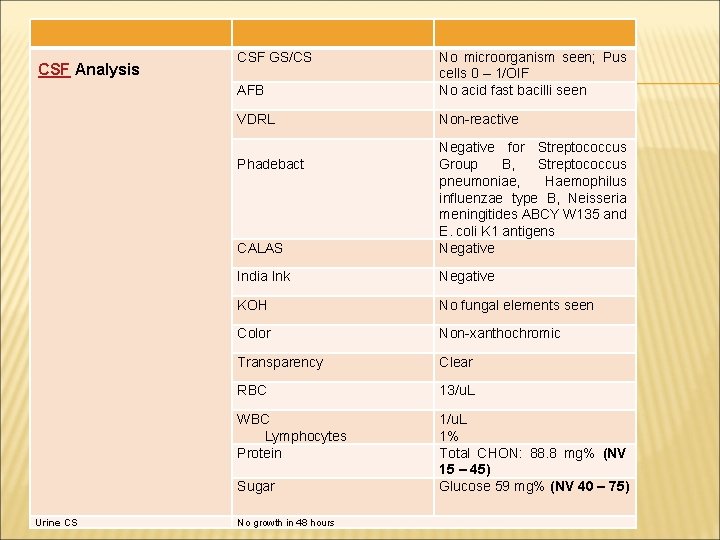
CSF Analysis CSF GS/CS AFB No microorganism seen; Pus cells 0 – 1/OIF No acid fast bacilli seen VDRL Non-reactive CALAS Negative for Streptococcus Group B, Streptococcus pneumoniae, Haemophilus influenzae type B, Neisseria meningitides ABCY W 135 and E. coli K 1 antigens Negative India Ink Negative KOH No fungal elements seen Color Non-xanthochromic Transparency Clear RBC 13/u. L WBC Lymphocytes Protein 1/u. L 1% Total CHON: 88. 8 mg% (NV 15 – 45) Glucose 59 mg% (NV 40 – 75) Phadebact Sugar Urine CS No growth in 48 hours
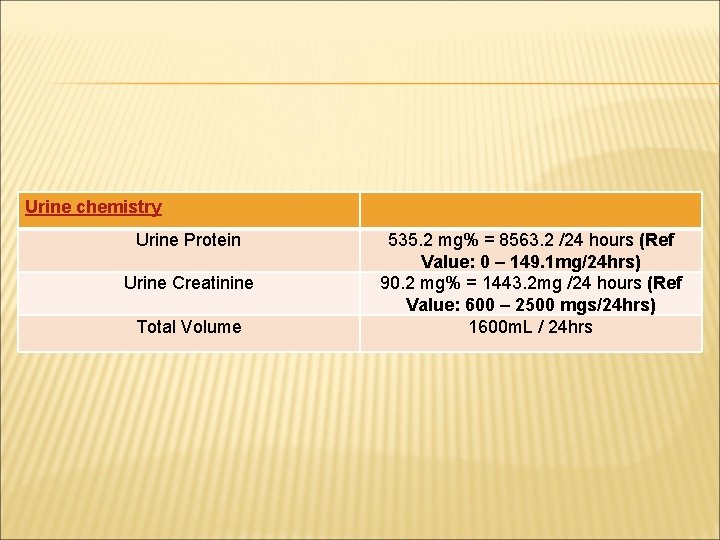
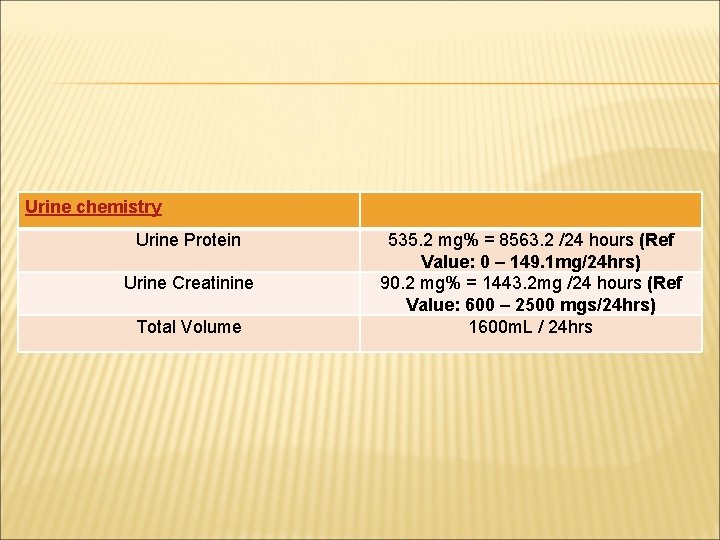
Urine chemistry Urine Protein Urine Creatinine Total Volume 535. 2 mg% = 8563. 2 /24 hours (Ref Value: 0 – 149. 1 mg/24 hrs) 90. 2 mg% = 1443. 2 mg /24 hours (Ref Value: 600 – 2500 mgs/24 hrs) 1600 m. L / 24 hrs
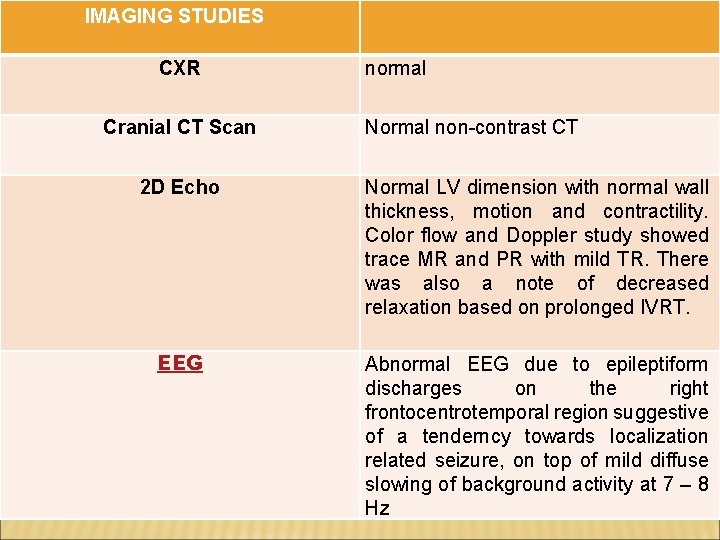
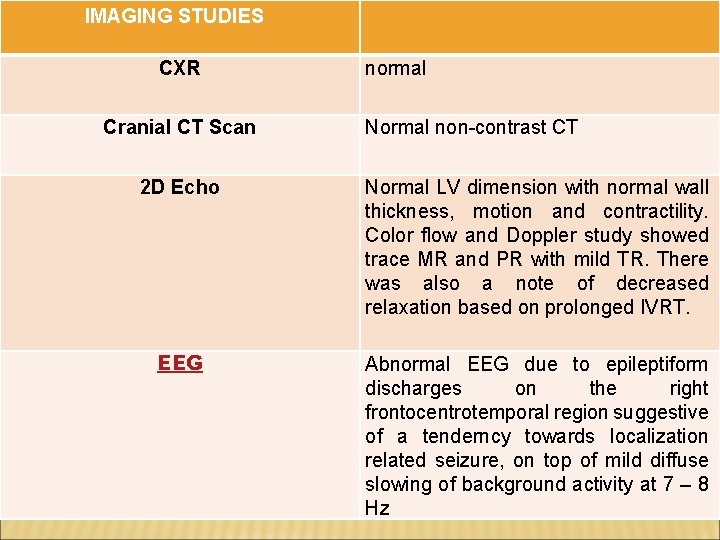
IMAGING STUDIES CXR Cranial CT Scan normal Normal non-contrast CT 2 D Echo Normal LV dimension with normal wall thickness, motion and contractility. Color flow and Doppler study showed trace MR and PR with mild TR. There was also a note of decreased relaxation based on prolonged IVRT. EEG Abnormal EEG due to epileptiform discharges on the right frontocentrotemporal region suggestive of a tenderncy towards localization related seizure, on top of mild diffuse slowing of background activity at 7 – 8 Hz

 Punnett square blue eyes
Punnett square blue eyes Gabby hill
Gabby hill Green eyed mom and brown eyed dad
Green eyed mom and brown eyed dad Hopi yellow watermelon
Hopi yellow watermelon Hazel bryan
Hazel bryan Behind these hazel eyes guitar chords
Behind these hazel eyes guitar chords Peter van houten
Peter van houten Hurricane morgan 1954
Hurricane morgan 1954 Gretchen raymond
Gretchen raymond Hazel farm guildford
Hazel farm guildford Green vs hazel eye color
Green vs hazel eye color Philip hazel
Philip hazel Felya büdü rabbe hazel beyt
Felya büdü rabbe hazel beyt Monoprotic
Monoprotic Tríptico de san juvenal
Tríptico de san juvenal Subordinacionismo
Subordinacionismo Law association of trinidad and tobago
Law association of trinidad and tobago Lieselle trinidad
Lieselle trinidad Judicial education institute of trinidad and tobago
Judicial education institute of trinidad and tobago Public companies in trinidad and tobago
Public companies in trinidad and tobago Cyber crime unit trinidad
Cyber crime unit trinidad Chemineer mixers tobago
Chemineer mixers tobago Vdocentes
Vdocentes Diabetes in trinidad and tobago
Diabetes in trinidad and tobago Masaccio pinturas
Masaccio pinturas Ito ay masusing pag-aaral ng anyo o hugis ng isang bansa
Ito ay masusing pag-aaral ng anyo o hugis ng isang bansa Assessment in trinidad and tobago
Assessment in trinidad and tobago Homilia santisima trinidad ciclo b
Homilia santisima trinidad ciclo b Trinidad (andréi rubliov)
Trinidad (andréi rubliov) Hfle curriculum trinidad
Hfle curriculum trinidad María del rocío trinidad mohedano jurado
María del rocío trinidad mohedano jurado Trinidad. maldonadd
Trinidad. maldonadd Central statistical office trinidad
Central statistical office trinidad Santisima trinidad para niños
Santisima trinidad para niños Trinidad geography
Trinidad geography Security fence trinidad
Security fence trinidad Police introduction
Police introduction Daniela trinidad
Daniela trinidad Trinidad de dios
Trinidad de dios Denovo trinidad
Denovo trinidad Kathryn singleton
Kathryn singleton Inr levels
Inr levels Erin kathryn 2016
Erin kathryn 2016 Capacoo
Capacoo Kathryn barnard child interaction theory
Kathryn barnard child interaction theory Kathryn coombes md
Kathryn coombes md Kathryn denning
Kathryn denning Nursing division 1
Nursing division 1 Dr catherine dao
Dr catherine dao Paul cairney
Paul cairney Kathryn dapre
Kathryn dapre Kathryn gutteridge
Kathryn gutteridge Kathryn tucker windham museum
Kathryn tucker windham museum Erin kathryn 2014
Erin kathryn 2014 The hurt locker 2008
The hurt locker 2008 Kaimar juss
Kaimar juss Kathryn cave
Kathryn cave Maha diagnosis
Maha diagnosis Erin kathryn
Erin kathryn Kathryn graham alberta innovates
Kathryn graham alberta innovates Water quality act of 1965
Water quality act of 1965 Kathryn elliott
Kathryn elliott Barnard's parent child interaction model
Barnard's parent child interaction model Dr kathryn schmidt
Dr kathryn schmidt Kathryn harris nih
Kathryn harris nih Revenge of the geeks
Revenge of the geeks Kathryn gingras
Kathryn gingras Kathryn coleman cms
Kathryn coleman cms Kathryn waddington
Kathryn waddington Beef recall
Beef recall Kathryn martin
Kathryn martin Kathryn spilios
Kathryn spilios Erin kathryn 2017
Erin kathryn 2017 Kathryn mayne
Kathryn mayne Cartersville medical center medical records
Cartersville medical center medical records Gbmc medical records
Gbmc medical records Hepburn osteometric board
Hepburn osteometric board