MANAGEMENT OF HIV POSITIVE HEALTH PROFESSIONALS IN THE

- Slides: 44

MANAGEMENT OF HIV POSITIVE HEALTH PROFESSIONALS IN THE UK THE TRIPARTITE WORKING GROUP AND BEYOND
OUTLINE 1. The background to exclusion of HCW who are HIV positive from undertaking exposure prone procedures. 2. The Tripartite Working Group recommendations, the Consultation document and Department of Health’s response. 3. Implementation of the new policy in 2014 4. The challenges which remain and the Desmond De Mello case.
BACKGROUND GMC STATEMENT ON DUTIES OF DOCTORS WITH HIV OR AIDS 1987 It is imperative, both in the public interest and on ethical grounds, that any doctors who consider that they may have been infected with HIV should seek appropriate diagnostic testing and counselling, and if found to be infected, should have regular medical supervision. They should also seek specialist advice on the extent to which they should limit their professional practice in order to protect their patients. They must act upon that advice, which in some circumstances would include a requirement not to practice or to limit their practice in certain ways. No doctors should continue in clinical practice merely on the basis of their own assessment of risk to patients.
1988 EXPERT ADVISORY GROUP ON HIV AND AIDS HCWs who knew or who suspected that they were infected with HIV and who ordinarily performed or assisted in surgical invasive procedures, where blood-to-tissue contact could occur, must seek expert advice on whethere was a need to limit or alter their working practice. All HCWs who had any reason to believe they might have been exposed to HIV infection, must promptly seek advice on whether they should be tested for HIV.
EXPERT ADVISORY GROUP ON AIDS 1991 “HIV infected healthcare workers should not perform invasive surgical procedures in which injury to the worker could result in blood contaminating a patients open tissues”
EXPERT ADVISORY GROUP ON AIDS POLICY CONCERNING EXPOSURE PRONE PROCEDURES 1993 “those invasive procedures where there is a risk that injury to the worker may result in exposure of the patients open tissues to the blood of the worker. These include procedures where the workers gloved hands may be in contact with sharp instruments, needle tips or sharp tissues ( e. g spicules of bone or teeth inside a patents open body cavity, wound or confidence anatomical space where the hands or fingertips may not be completely visible at all times. ”
NOTIFICATION PROCEDURES 1. Patients operated upon by a HCW who was infected “should be notified of the risk they may have been exposed to, as far as is practicable”. 2. Patients who may have been infected should be detected. This was so that they could be offered necessary care and to prevent onward viral transmission 3. Data was to be collected to assist in refining current understanding on risk estimates.
HIV Infected Health Care Workers: Guidance on Management and Patient Notification 2005 HCW who were HIV could not perform exposure prone procedures Patients only needed to be notified in a situation in which there was a distinct risk of bleed -back from HIV positive health care workers during an exposure prone procedures.
PATIENT NOTIFICATION PROCEDURES A smaller subgroup of patients identified. These were there was deemed to be a higher risk in relation to EPP’s even though this risk was low. Here not only should they be notified but encouraged rather than simply offered a test. also patients should be
DEPARTMENT OF HEALTH 2007: HEALTH CLEARANCE MEASURES FOR NEW HEALTH CARE WORKERS All new HCWs who will perform EPPs have to demonstrate, through appropriate testing, that they are non-infectious for HIV, hepatitis B and hepatitis C. If found to be infectious, the HCW is ineligible for an EPP position
CHANGING PERSPECTIVES: CHANGING POLICY Evidence of Risk Impact of being excluded from practice Also questions of discrimination and equality
MEMBERSHIP OF THE TRIPARTITE GROUP Members drawn from: UK Advisory Panel for Healthcare Workers Infected with Blood-bourne Viruses Advisory Group on Hepatitis Expert Advisory Group on HIV and AIDS.
REMIT OF THE WORKING GROUP To undertake a review of the current policies on the restriction of HCWs infected with BBVs whose clinical duties rely on performing exposure prone procedures (EPPs). To make recommendations for changes to the guidance, if appropriate, for approval by AGH and EAGA before submission to the Department of Health and the Devolved Administrations. To consider whether the following principles should continue to underlie the guidance: Policy should continue to be based on an assumption of high rather than substandard clinical and infection control practice. Infected HCWs in different specialties should be managed consistently, including groups such as dentists and paramedics who face greater practical and financial difficulties when restricted either permanently or temporarily… L
REMIT OF THE WORKING GROUP The concept of ‘exposure prone procedure’ as an objective method of classifying and comparing the risk of bleed-back 4 in a wide range of procedures across different healthcare specialties To consider the following specific issues in relation to the guidance: Whether to emphasise the duty of HCWs to seek occupational health advice when they are at risk of blood-borne virus infection, perhaps by incorporating this requirement into a single, consolidated generic guidance document on the management of HCWs infected with BBVs. Whether variations in policy are required in relation to HCWs with BBV co-infection, in terms of the risk of transmission of the viruses to patients, patient notification exercises and the management of the infected HCWs.
TRANSMISSION OF HIV FROM HCW TO PATIENT No reported transmission of HIV from HCW in UK to a patient 4 documented cases of transmission internationally were considered Florida- a HIV positive dentist transferred HIV to 5 of his patients. Diagnosed with HIV in 1986, with AIDS in 1987. Dentist died in 1990 Orthopaedic surgeon in France in 1999. He transmitted HIV during a hip replacement operation. Nurse in France- in 2002 route for transmission of HIV was unclear Gynecologist in Spain in 2003. The procedure was a caesarean section
INTERNATIONAL POSITION Australia/Ireland/Italy and Malta restricts HIV infected HCW’s from invasive EPP’s. Austria/Belgium/Canada/Finland/New Zealand Sweden- this is managed on a case by case basis. US/France and Germany- there was not a national policy.
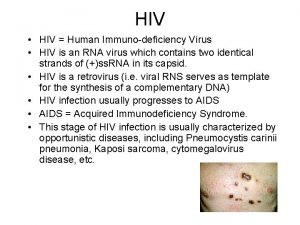
RISK LEVELS RE TRANSMISSION Evidence showed very low/negligible transmission risk Where an infected HCW was on combination antiretroviral therapy then the individuals viral load would be suppressed to what would be an undetectable level In the case of invasive exposure prone procedures such as local anaesthetic or routine tooth extraction in dentistry the risk was seen as negligible. In the case of the most invasive procedures such as caesarean sections or open cardiac surgery was seen as extremely low
RECOMMENDATIONS OF THE WORKING GROUP: RE RISK AND ANTI-RETROVIRAL THERAPY Risk would be further reduced via use if the HCW was on combination anti -retroviral therapy the individuals viral load would be suppressed to an undetectable level. Very statistically small increase in transmission risk. Exception for small category where there is a naturally low viral load which is sustained
ADVANTAGES OF A CHANGE OF POLICY More HCW coming for diagnosis and treatment Reduction in risk to patients with proportion of number of HCW’s who were undiagnosed in treating patients. Possible that “ if there was a large enough increase in the diagnosis of HIV infected healthcare workers this could offset the additional risk partially or completely or the total risk could be reduced compared with the current position. “
CONSULTATION AND DEPARTMENT OF HEALTH RESPONSE “The Department is content with the TWG’s assessment of risk and notes that in the main, respondents agreed, with some considering the estimate to be over-stating the risk. Whilst we acknowledge there are some limitations to the data, there have only been four reported transmissions of HIV from infected and untreated healthcare workers worldwide, and none have been reported in the UK. ”
WOULD MORE HCW’S COME FORWARD FOR TESTING? “The Department acknowledges that it is not possible to say definitively whether implementing the TWG’s recommendations would result in more healthcare workers coming forward for HIV testing. We agree that it is possible that some of the reasons for not coming forward, which are mentioned in the consultation responses, may continue to influence some healthcare workers at risk of HIV infection. However, we believe it is fair to suggest that since the revised policy would no longer automatically signal the end of a chosen career for a healthcare worker who performs EPPs, it would make it more likely that individuals at risk would come forward to protect both their own health and that of their patients. ”
WORKING GROUP: CONDITIONS FOR HCW BEING ALLOWED TO PERFORM EXPOSURE PRONE PROCEDURES If they are on combination retroviral therapy and they have a plasma load which is constantly suppressed to very low or undetectable levels i. e. below 200 copies/ml. Demonstrate a sustained response to combination anti-retroviral therapy before starting or continuing to perform exposure prone procedures. Be subject to viral load testing every three months while they continue to perform these procedures
SHOULD DENTISTS BE TREATED DIFFERENTLY? Some suggestions that dentists should be allowed to practice if not on antiretrovirals. DOH stated that “ Whilst the risk of transmission may be considered ‘negligible’ or ‘very low’, there still remains a risk to patients if HIV positive healthcare workers are permitted to perform any category of EPP and it is imperative that this risk is minimised as much as possible. Whilst the Department is keen to advance the opportunities for healthcare workers with HIV by allowing them, where possible, to perform EPPs, it is of the utmost importance that this is not achieved at the expense of patient safety”
TRIPARTITE GROUP AND THE NEED FOR MONITORING OF HCW’s Effectively HCW practice would be carefully controlled Monitoring every 3 months should be the responsibility of the treating physician and their occupational medicine consultant. If a HIV infected healthcare worker does not comply with monitoring or if their plasma viral load rises significantly above 200 copies/ml i. e. to more than 1000 copies/ml then it should be restricted from performing exposure prone procedures until their viral load returns to being stably below 200 copies
TESTING OF HCW’S : NEW GUIDANCE 2014 All new HCWs employed or starting training (including students) in a clinical care setting, either for the first time or returning to work in the NHS should undergo standard health checks which will include being offered an HIV antibody test. HCWs who will perform EPPs must be tested for HIV antibody HCWs who apply for a post or training which requires the performance of EPPs and who decline to be tested for HIV, Hepatitis B and Hepatitis C should not be cleared for EPP work.
NEW GUIDANCE 2014: TESTING FOR HCW’S WHO ARE ALREADY PRACTICISING “Practising HCWs who undertake EPPs are under a professional duty to seek medical advice on the need to be tested as soon as they are aware they may have been exposed to HIV infection, occupationally or otherwise (e. g if they meet any of the preceding exposure criteria) and if found to be positive, to obtain and follow appropriate clinical and occupational health advice. “
NEW GUIDANCE 2014 “HIV infected HCWs must meet the following criteria before they can perform EPPs: Either a) be on effective combination antiretroviral therapy (c. ART), and b) have a plasma viral load <200 copies/ml Or c) be an elite controller”
NEW GUIDANCE 2014 “d) be subject to plasma viral load monitoring every three months and e) be under joint supervision of a consultant occupational physician and their treating physician, and f) be registered with the UKAP Occupational Health Monitoring Register (UKAP-OHR)”
NEW GUIDANCE: WHERE HCW REFUSES TO ATTEND OR DOES NOT ATTEND AN APPOINTMENT Where a HCW does not attend for their appointments, or refuses to have their viral load tested, the consultant occupational physician should inform the HCWs manager that they are no longer cleared to perform EPPs, until it has been established that the HCW is continuing with c. ART and their viral load (measured within the past three months) does not exceed 200 copies/ml.
NEW GUIDANCE 2014: ELITE CONTROLLER An elite controller is defined as a person living with HIV who is not receiving antiretroviral therapy and who has maintained their viral load below the limits of assay detection for at least 12 months, based on at least three separate viral load measurements, A HCW who meets the definition of being an elite controller can be cleared for EPP activities without being on treatment. They are to be subject to three-monthly viral load monitoring to ensure they maintain their viral load below 200 copies/ml and to identify any rebound promptly. Any such cases should be referred to UKAP for advice on a case-by-case basis.
IMPLEMENTATION OF TRI-PARTITE GROUP RECOMMENDATIONS Further recommendations were made in relation to implementation by the Expert Advisory Group on AIDS and these were included in the consultation document.
IMPLEMENTATION OF THE PROPOSALS: FRAMEWORK FROM THE EXPERT ADVISORY GROUP ON AIDS NHS to refer of all cases of HIV infected health care workers who wanted to benefit from the policy to UKAP for first 2 years. Public Health England to maintain a database of all the cases.
NOTIFCATION TO UKAP Department of Health agreed : UKAP should be notified of all cases involving healthcare workers with HIV who wish to perform EPPs for two years, to ensure consistent application of the policy. Decisions to clear individual healthcare workers for EPP work will ultimately remain the responsibility of the treating and occupational health physicians. UKAP must be provided with as much information as possible at the time of submitting the request.
DEPARTMENT OF HEALTH RESPONSE ON THE NEED FOR NATIONWIDE MONITORING OF THE NEW POLICY Accepted the need for national/UK wide monitoring. Noted that Public Health England (PHE) have agreed to establish and run a confidential database, to which OH providers can confidentially submit information about individual healthcare workers doing EPPs and their viral load monitoring information. Didn’t see there being a disproportionate workload on OH departments
CONSULTATION AND DEPARTMENT OF HEALTH RESPONSE “The Department accepts the advice of the TWG that viral load testing for HIV positive healthcare workers carrying out EPPs should be at threemonthly intervals to protect patient safety, and that decisions on how effective joint monitoring will work best should be made at a local level”
PATIENT NOTIFICATION EXERCISES A patient notification exercise would only be considered in a situation in which HCW was not on anti-retrivirals or VL was over 1000. Post-exposure testing should be offered to exposed patients.
ELITE CONTROLLERS In relation to elite controllers whether these should be required to take ARV’s was something which should be referred to UKAP on a case by case basis
GUIDANCE 2014: OBLIGATIONS ON HCW Must be under the care of a designated consultant occupational physician Must accept that it is a condition of undertaking EPPs that they consent to ongoing monitoring while they continue to practise exposure-prone procedures, including:
GUIDANCE 2014: OBLIGATION ON THE CONSULTANT OCCUPATIONAL PHYSICIAN “The consultant occupational physician is responsible for the monitoring of the infected HCW including: i. ensuring that the testing protocol and timings are followed ii. reacting promptly to any alerts received via UKAP-OHR iii. taking appropriate action when those who should present for tests do not do so e. g notifying the relevant manager of the HCW’s non-attendance and restriction from EPP practice iv. taking IVS samples, and ensuring samples are sent to laboratories; v. interpreting the viral load results in relation to clearance to perform EPPs vi. ensuring that the UKAP-OHR is updated in a timely manner vii. advising the HCW and the employer, on an ongoing basis, on whether the HCW is fit to perform EPPs viii. timely liaison with treating physicians “
OBLIGATION ON THE TREATING PHYSICIAN The treating physician is responsible for I. clinical management and support of the HCW I I. Advising and maintaining timely communications with the consultant occupational physician responsible for monitoring the infected HCW.
BROADER IMPLICATIONS OF THE POLICY IN RELATION TO EQUALITY AND RIGHTS: DEPARTMENT OF HEALTH’S RESPONSE “The Department is content that the equality assessment that has been published alongside this document reflects the equality issues in this context. It is agreed that the overall impact of the new policy on equality will be beneficial; in particular, that it will advance equality of opportunity for healthcare workers with HIV infection. Further to the comments received, emphasis on the impact on individual healthcare workers in the impact assessment has been strengthened”
CHANGE IN UK POLICY Change of policy announced in August 2013 “It is more likely that somebody will be struck by lightening than be infected by HIV by their doctor or dentist. ” Dame Sally Davies, Chief Medical Officer
WHEN THINGS GO WRONG Dentist Desmond de Mello Poor infection control procedures Notification of patients
REFLECTIONS ON THE TRIPARTITE WORKING GROUP A pragmatic approach to risk assessment A recognition that there may be some therapeutic benefits Not a “hands off” approach- clear lines of responsibility and accountability on OH and on HCW Oversight at national level and development at a database Cautious and measured reform
 Hiv test results example
Hiv test results example Haivn
Haivn Types of health professionals
Types of health professionals Health professionals follow-up study
Health professionals follow-up study List of all allied health professions
List of all allied health professions Allied health professionals
Allied health professionals Solid
Solid Hosa mission statement
Hosa mission statement Focus on pharmacology essentials for health professionals
Focus on pharmacology essentials for health professionals Focus on pharmacology
Focus on pharmacology Agar
Agar Negative numbers rules
Negative numbers rules Positive practice positive outcomes
Positive practice positive outcomes Quang trung
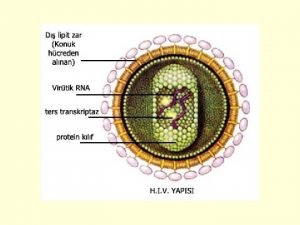
Quang trung Hiv reverse transcription
Hiv reverse transcription Test wiedzy o aids z odpowiedziami
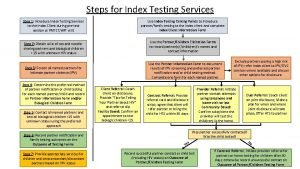
Test wiedzy o aids z odpowiedziami Approche index testing
Approche index testing Program nasional akreditasi
Program nasional akreditasi Phdp in hiv
Phdp in hiv Chii chinonzi hiv
Chii chinonzi hiv Window period hiv
Window period hiv Dot
Dot Iris hiv
Iris hiv Hiv
Hiv Hiv risk factors
Hiv risk factors Asante hiv-1 rapid recency assay
Asante hiv-1 rapid recency assay Fiebig hiv
Fiebig hiv Hiv case-based surveillance in ethiopia
Hiv case-based surveillance in ethiopia Triệu chứng nhiễm hiv
Triệu chứng nhiễm hiv A bacterial std that usually affects mucous membranes
A bacterial std that usually affects mucous membranes Chapter 24 sexually transmitted diseases and hiv/aids
Chapter 24 sexually transmitted diseases and hiv/aids Basic hiv course
Basic hiv course Stakeholders in hiv prevention
Stakeholders in hiv prevention Hiv treatments
Hiv treatments Causative organism of hiv/aids
Causative organism of hiv/aids What does hiv stand
What does hiv stand Aids 101
Aids 101 Hiv test window period
Hiv test window period Hiv stool color
Hiv stool color Procentowe ryzyko zakażenia hiv
Procentowe ryzyko zakażenia hiv Hiv adalah
Hiv adalah Hiv lifecycle
Hiv lifecycle 4.jenerasyon vidas hıv duo ultra testi güvenilir mi
4.jenerasyon vidas hıv duo ultra testi güvenilir mi Hiv lifecycle
Hiv lifecycle Hiv
Hiv