MAKASSED EXPERIENCE IN MANAGEMENT OF PLACENTA ACCRETA Prepared















- Slides: 39
MAKASSED EXPERIENCE IN MANAGEMENT OF PLACENTA ACCRETA Prepared by : Dr. Amani A. A Rajabi , MD (AL_QUDS UNIV. ) Resident at Makassed Islamic Charitable Hospital Supervised by : Dr. Saadeh S. Jaber MBBS, MRCOG, MRCPI, Head of OBGYN department Al_quds univ. Consultant at Makassed Islamic Charitable Hospital
DEFINITION & PATHOGENESIS Placenta accreta occurs when there is a defect of the decidua basalis , in conjunction with an imperfect development of the Nitabuch membrane , resulting in abnormally invasive implantation of the placenta. Nitabuch membrane is a fibrinoid layer that separates the decidua basalis from the placental villi.
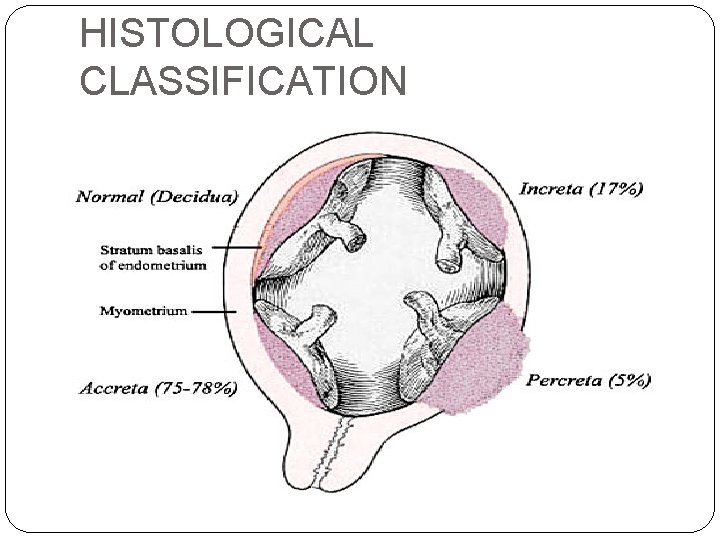
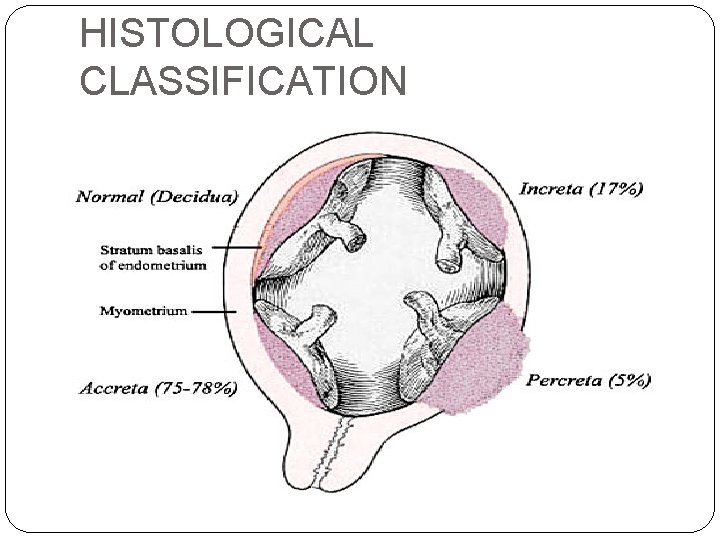
HISTOLOGICAL CLASSIFICATION
INCIDENCE There is marked increase in the incidence of placenta accreta. In 1950 ----- 1 in 30, 000 deliveries. In 1977 -----1 in 7, 000 deliveries. In 1985 -1994 -----1 in 2500 deliveries. In 1982 -2002 -----1 in 533 deliveries. (Am J Obstet Gynecol 1997; 177: 210 -4) (Am J Obstet and Gynecol (2005) 192, 1458– 61)
placenta accreta has been reported to result in a 7% mortality rate. The most common indication for birth related hysterectomy, accounting for 40– 60% of cases. ACOG committee opinion. International Journal of Gynecology & Obstetrics 77 (2002) 77 -78. J. Obstet. Gynaecol. Res. Vol. 33, No. 4: 431– 437, August 2007.
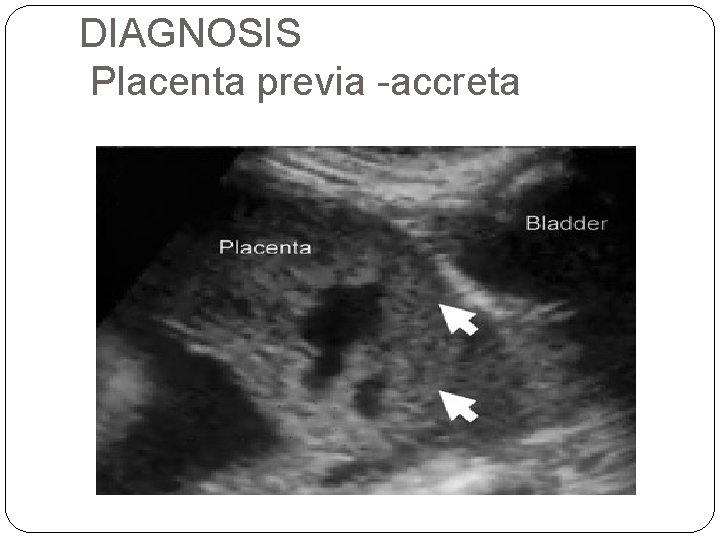
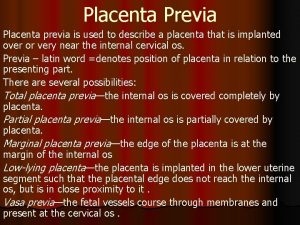
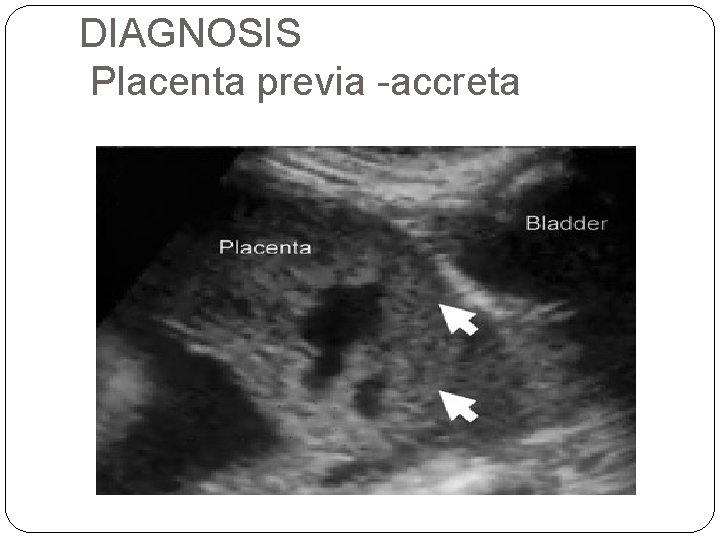
DIAGNOSIS Placenta previa -accreta
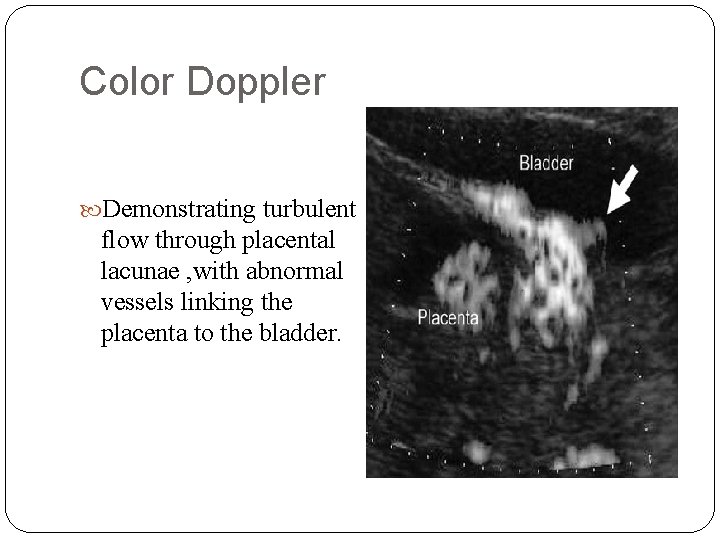
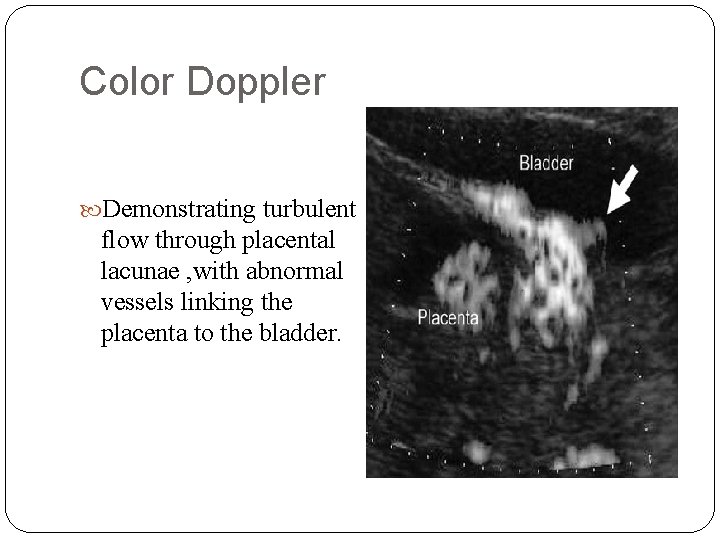
Color Doppler Demonstrating turbulent flow through placental lacunae , with abnormal vessels linking the placenta to the bladder.
Magnetic resonance imaging The role of MRI is to complement, rather than replace, information obtained via standard sonographic imaging. The main advantage offered by this type of imaging is : Ø The ability to diagnose posterior placenta accreta more confidently. Ø The assessment of bladder invasion in cases of placenta percreta.
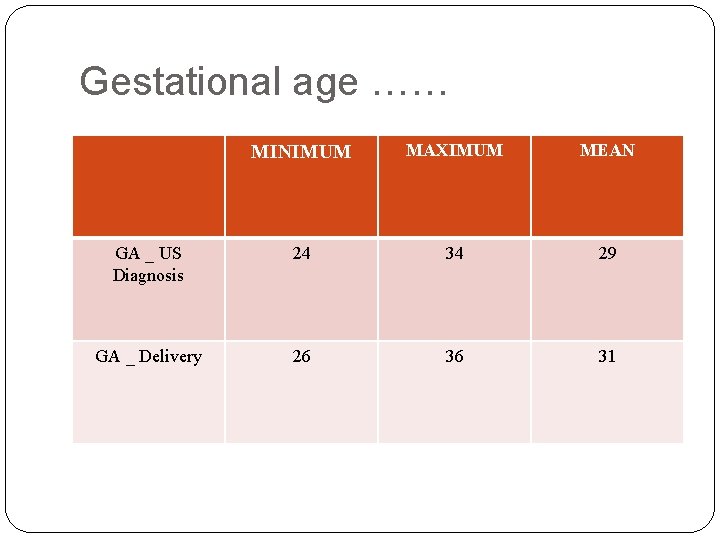
The mean gestational age at diagnosis of placenta accreta by ultrasound is 29 weeks (range: 28– 33 weeks). The mean gestational age at delivery is 36 weeks (range: 32– 38 weeks). J. Obstet. Gynaecol. Res. Vol. 33, No. 4: 431– 437, August 2007.
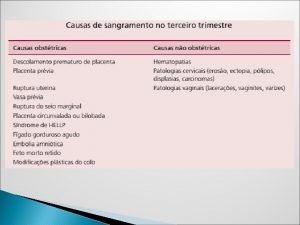
COMPLICATIONS Massive obstetric hemorrhage is the most common complication. Disseminated intravascular coagulopathy. Adult respiratory distress syndrome. Renal failure. Infection Death.
Abstract STUDY DESIGN : Retrospective analysis of medical records & histopathological finding. POPULATION : Women delivered at Makassed Hospital 2007 / 2008 of whom 15 cases of invasive placenta identified. A finding confirmed by histopathology. METHODS : Retrospective analysis complemented with direct communication with patient , using SPSS to analyze data. CONCLISIONS : at the end of presentation.
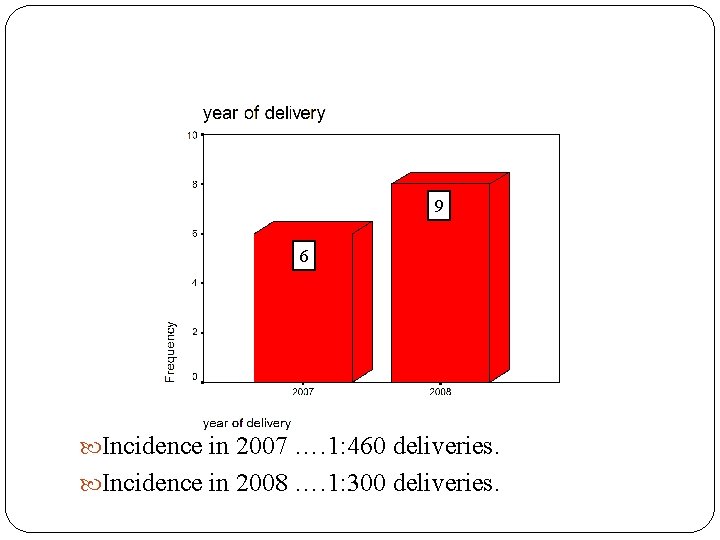
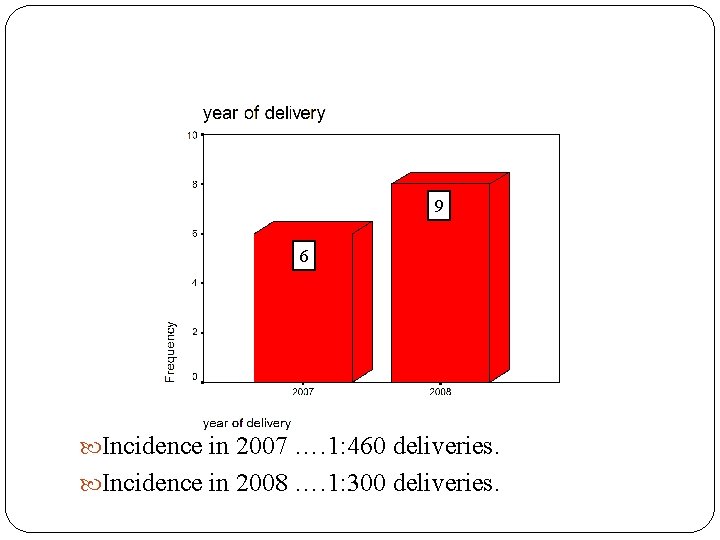
9 6 Incidence in 2007 …. 1: 460 deliveries. Incidence in 2008 …. 1: 300 deliveries.



All of our cases were diagnosed antenatally.
Identified risk factors history of : C S. E &C. IUCD. Other uterine instrumentation.

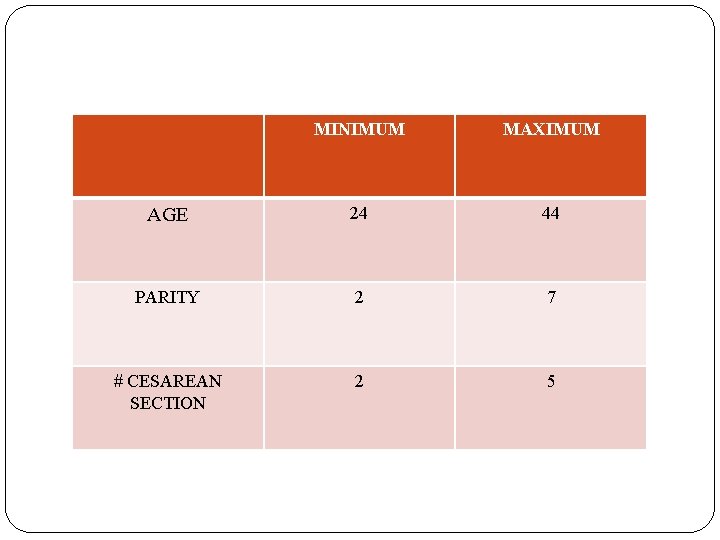
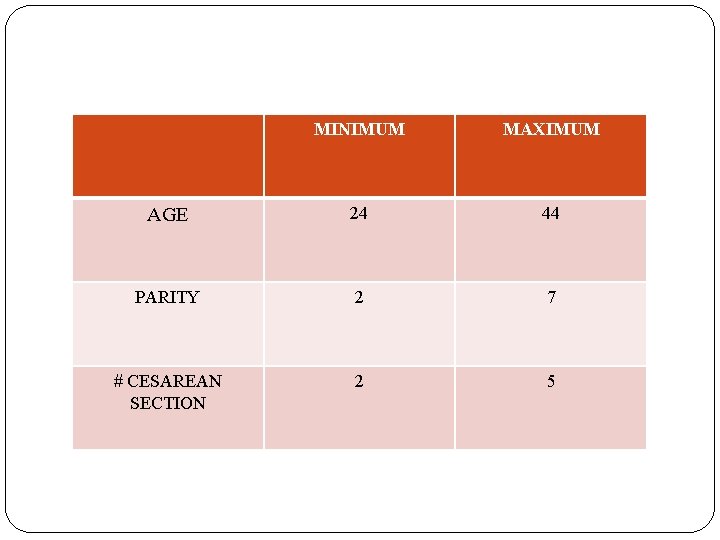
MINIMUM MAXIMUM AGE 24 44 PARITY 2 7 2 5 # CESAREAN SECTION


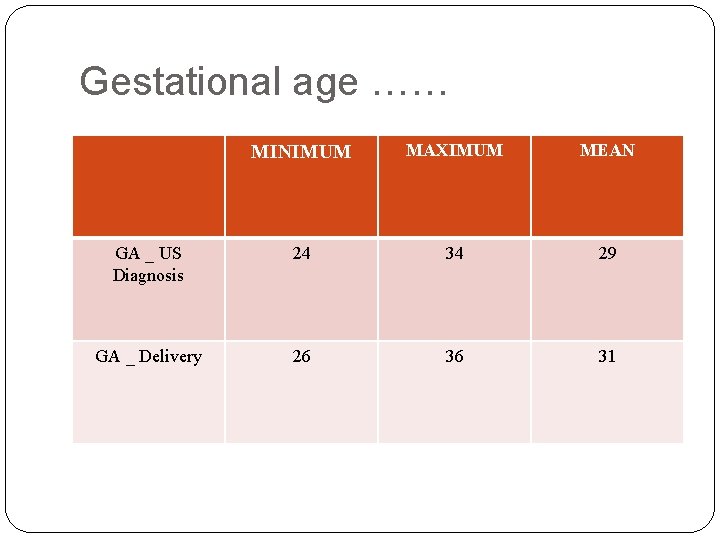
Gestational age …… MINIMUM MAXIMUM MEAN GA _ US Diagnosis 24 34 29 GA _ Delivery 26 36 31

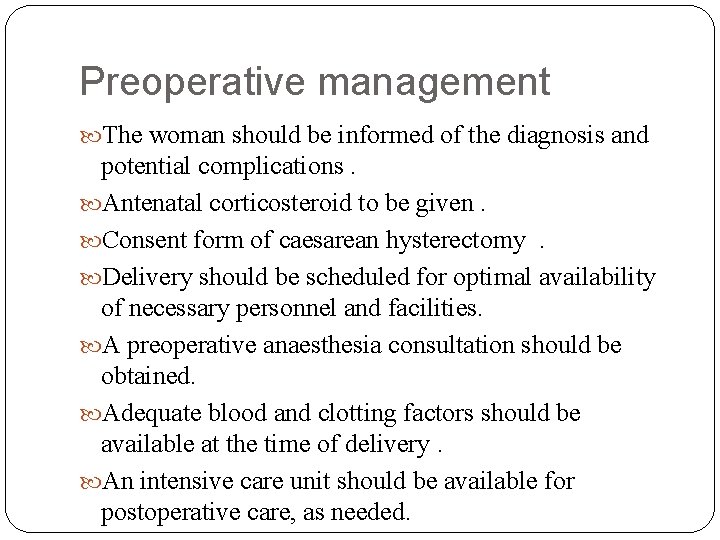
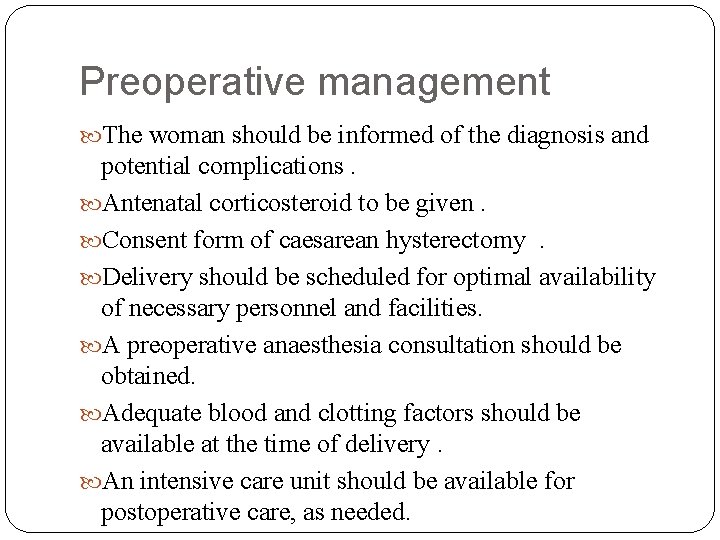
Preoperative management The woman should be informed of the diagnosis and potential complications. Antenatal corticosteroid to be given. Consent form of caesarean hysterectomy . Delivery should be scheduled for optimal availability of necessary personnel and facilities. A preoperative anaesthesia consultation should be obtained. Adequate blood and clotting factors should be available at the time of delivery. An intensive care unit should be available for postoperative care, as needed.
Immediate preoperative bilateral uretric stents were inserted in a couple of cases .
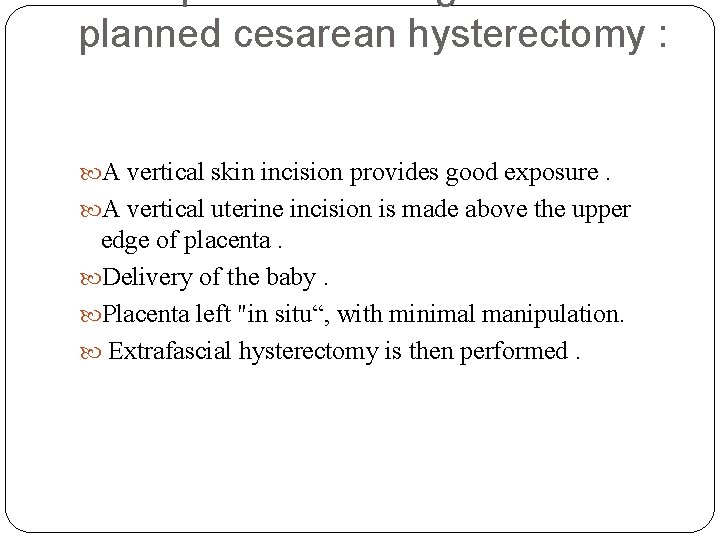
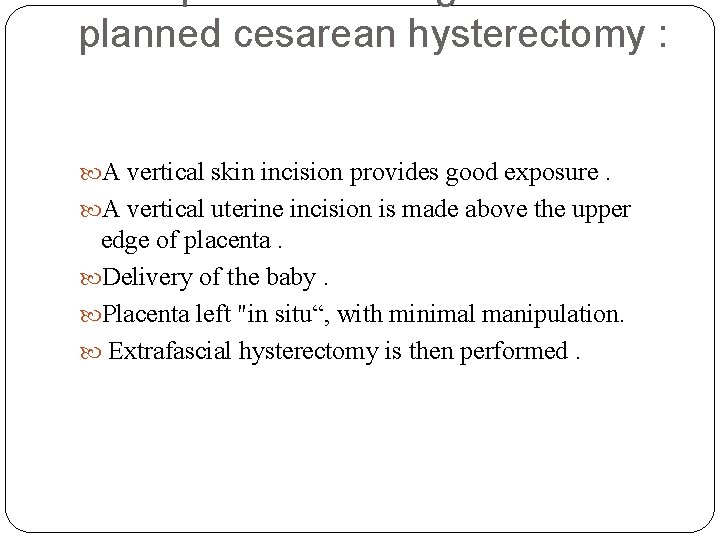
planned cesarean hysterectomy : A vertical skin incision provides good exposure. A vertical uterine incision is made above the upper edge of placenta. Delivery of the baby. Placenta left "in situ“, with minimal manipulation. Extrafascial hysterectomy is then performed.


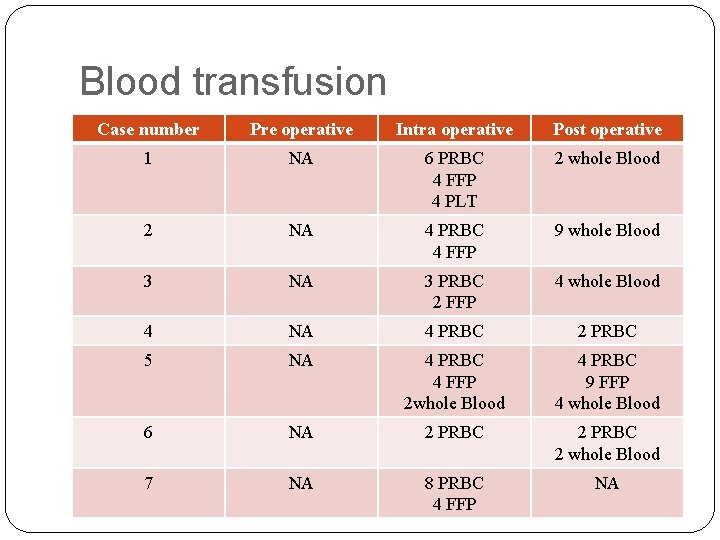
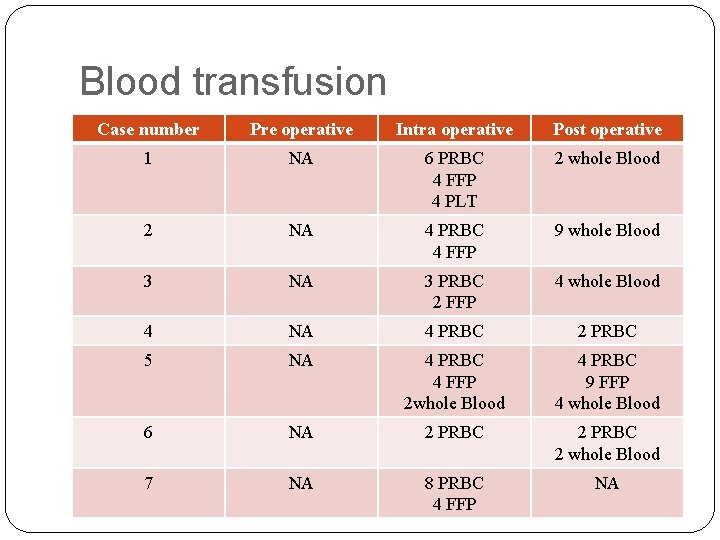
Blood transfusion Case number Pre operative Intra operative Post operative 1 NA 6 PRBC 4 FFP 4 PLT 2 whole Blood 2 NA 4 PRBC 4 FFP 9 whole Blood 3 NA 3 PRBC 2 FFP 4 whole Blood 4 NA 4 PRBC 2 PRBC 5 NA 4 PRBC 4 FFP 2 whole Blood 4 PRBC 9 FFP 4 whole Blood 6 NA 2 PRBC 2 whole Blood 7 NA 8 PRBC 4 FFP NA

Continued Case number Pre operative Intra operative Post operative 8 NA 3 PRBC 1 PRBC 4 FFP 9 NA 4 PRBC 2 whole Blood 2 FFP 10 NA 2 PRBC 11 2 PRBC 2 FFP 12 NA 2 PRBC NA 13 NA 2 PRBC 2 FFP 14 NA NA NA 15 NA 2 PRBC 4 whole Blood 2 FFP 2 whole Blood



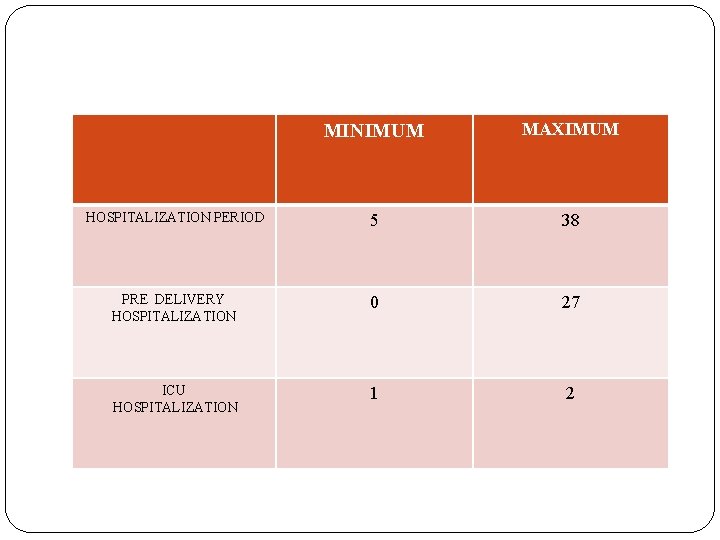
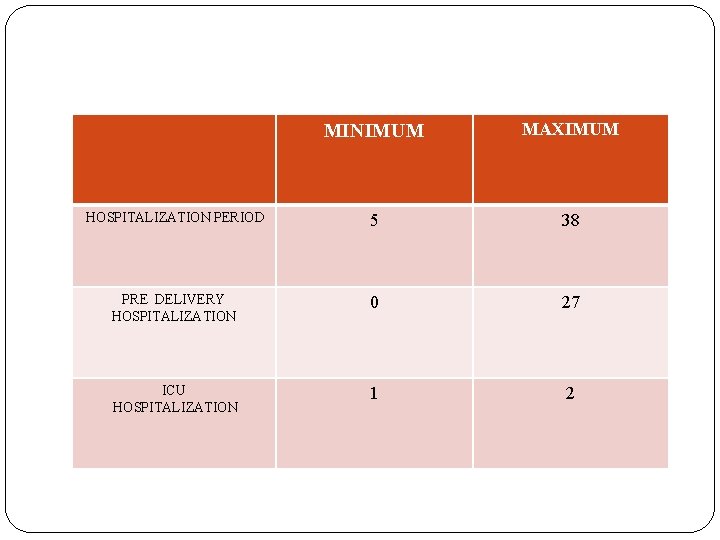
MINIMUM MAXIMUM HOSPITALIZATION PERIOD 5 38 PRE DELIVERY HOSPITALIZATION 0 27 ICU HOSPITALIZATION 1 2
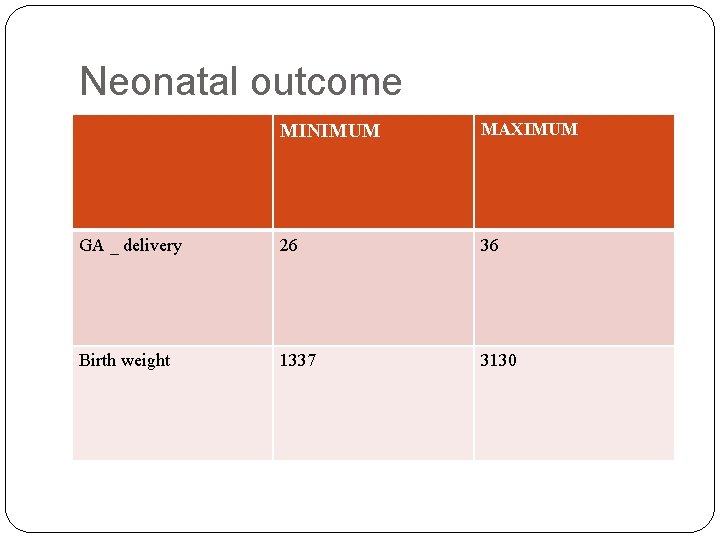
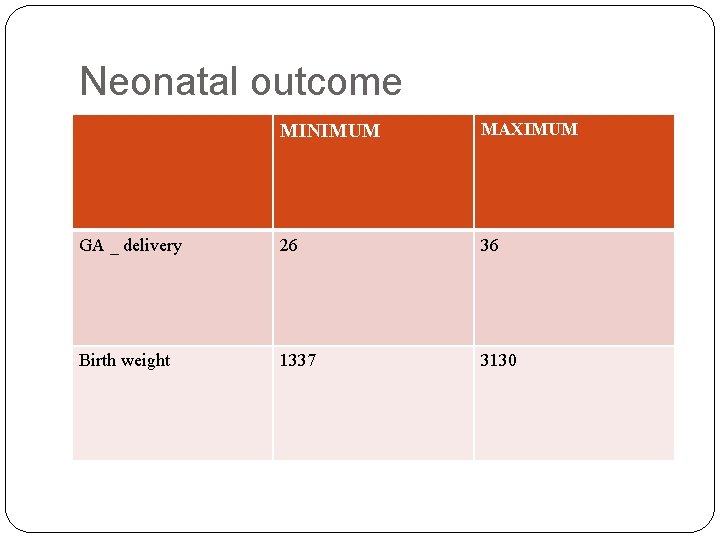
Neonatal outcome MINIMUM MAXIMUM GA _ delivery 26 36 Birth weight 1337 3130

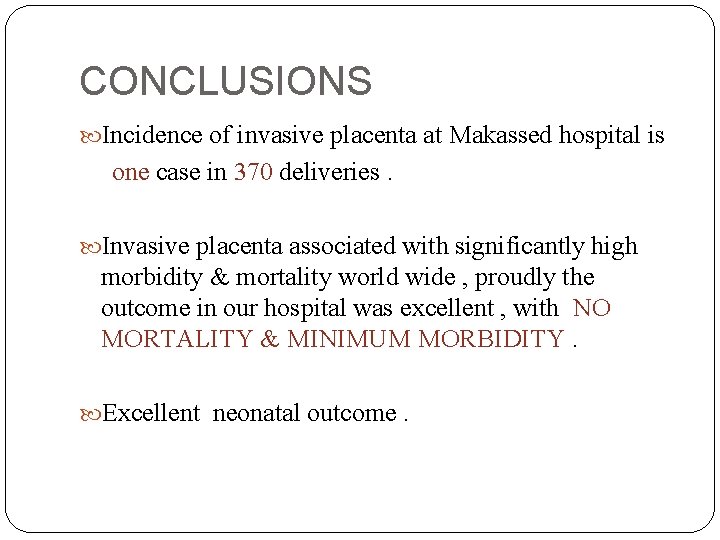
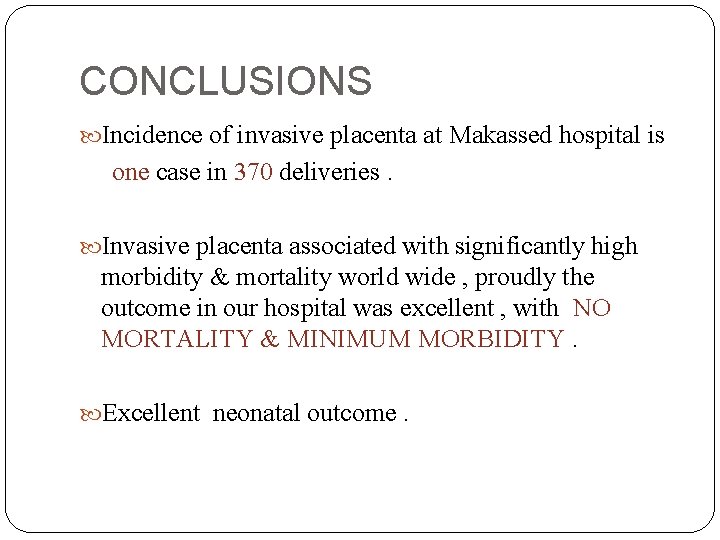
CONCLUSIONS Incidence of invasive placenta at Makassed hospital is one case in 370 deliveries. Invasive placenta associated with significantly high morbidity & mortality world wide , proudly the outcome in our hospital was excellent , with NO MORTALITY & MINIMUM MORBIDITY. Excellent neonatal outcome.
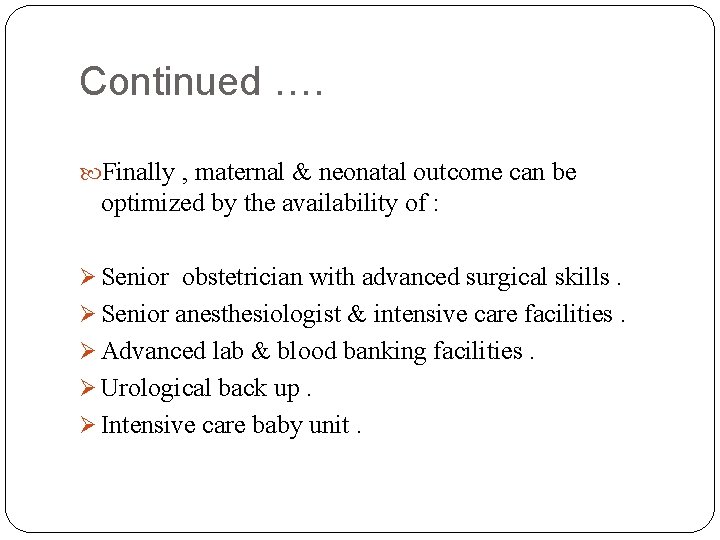
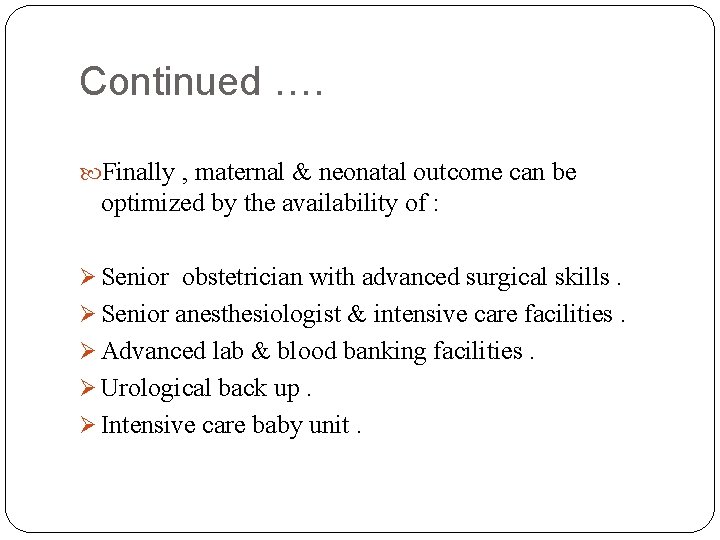
Continued …. Finally , maternal & neonatal outcome can be optimized by the availability of : Ø Senior obstetrician with advanced surgical skills. Ø Senior anesthesiologist & intensive care facilities. Ø Advanced lab & blood banking facilities. Ø Urological back up. Ø Intensive care baby unit.

 Afe pregnancy
Afe pregnancy Imprinting meaning psychology
Imprinting meaning psychology Early experience vs later experience
Early experience vs later experience Direct experience and indirect experience
Direct experience and indirect experience The business plan should be prepared by
The business plan should be prepared by After a node has prepared an lsp it must be disseminated to
After a node has prepared an lsp it must be disseminated to Romeo and juliet act 4 questions
Romeo and juliet act 4 questions Haya shulman
Haya shulman Predisposition test milady
Predisposition test milady Characteristics of a well-prepared upland field
Characteristics of a well-prepared upland field Department accounts are prepared to ascertain
Department accounts are prepared to ascertain The world of food and beverages chapter 4
The world of food and beverages chapter 4 Backhand writing
Backhand writing Gayne corporation's contribution margin ratio
Gayne corporation's contribution margin ratio Are you prepared for the zombie apocalypse
Are you prepared for the zombie apocalypse Exploding comfortably down on the cliffs
Exploding comfortably down on the cliffs Monophasic liquid can be given for
Monophasic liquid can be given for Preparatory arranging
Preparatory arranging Be prepared to give an answer
Be prepared to give an answer Be prepared to give an answer
Be prepared to give an answer Guiding planes on abutment teeth
Guiding planes on abutment teeth Benefits of bsn-prepared nurses
Benefits of bsn-prepared nurses Past form of prepared
Past form of prepared Effervescent granules in pharmacy
Effervescent granules in pharmacy How to prepare to preach the word of god
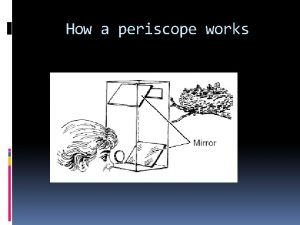
How to prepare to preach the word of god How a periscope works
How a periscope works In williamson’s synthesis, ethoxyethane is prepared by-
In williamson’s synthesis, ethoxyethane is prepared by- Cash distribution plan
Cash distribution plan Be prepared to share the hope
Be prepared to share the hope How standard costs are prepared
How standard costs are prepared Let's get prepared
Let's get prepared Project client name
Project client name Award prepared
Award prepared Trading account is prepared to find out? *
Trading account is prepared to find out? * Institutional catering definition
Institutional catering definition Galenicals examples
Galenicals examples Ezra the scribe
Ezra the scribe Purpose of control accounts
Purpose of control accounts Wake county prepared food tax
Wake county prepared food tax Prepared exclusively for
Prepared exclusively for