Liver Failure NURS 241 Chapter 44 p 1058
- Slides: 45
Liver Failure NURS 241 Chapter 44 (p. 1058)
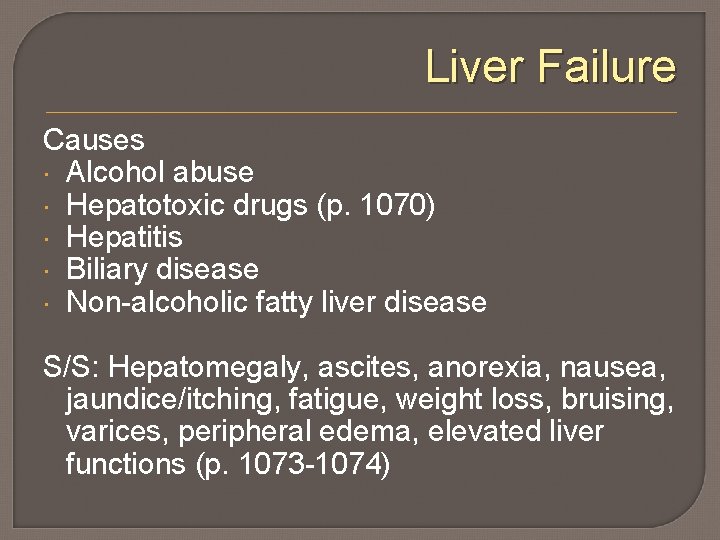
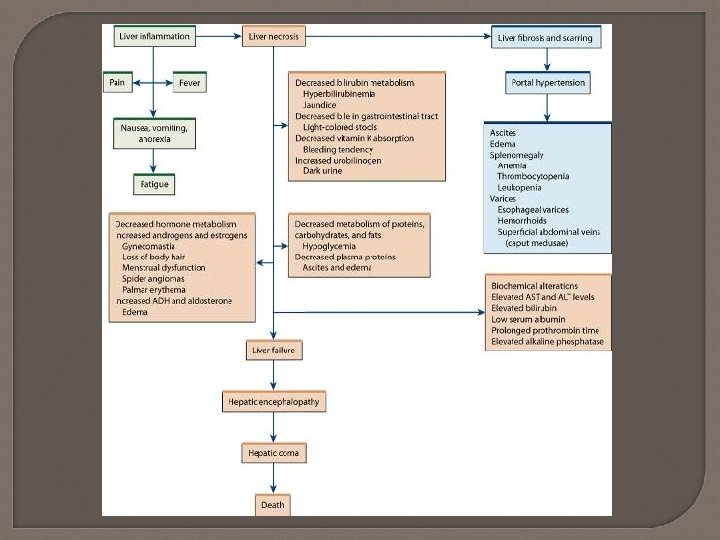
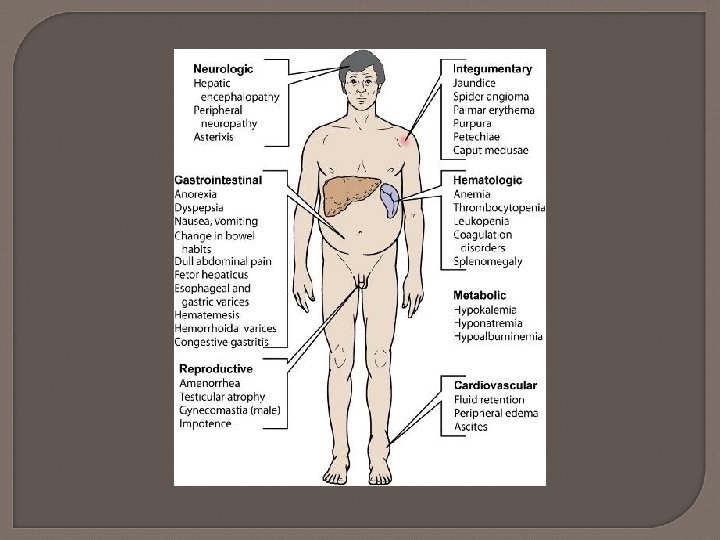
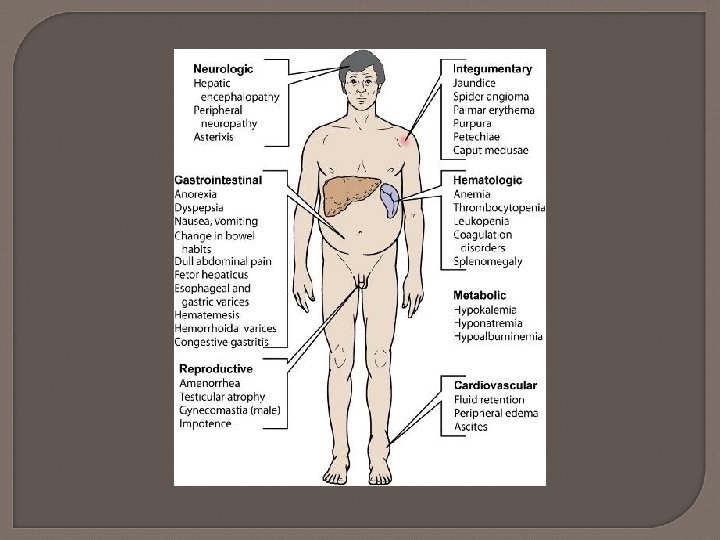
Liver Failure Causes Alcohol abuse Hepatotoxic drugs (p. 1070) Hepatitis Biliary disease Non-alcoholic fatty liver disease S/S: Hepatomegaly, ascites, anorexia, nausea, jaundice/itching, fatigue, weight loss, bruising, varices, peripheral edema, elevated liver functions (p. 1073 -1074)
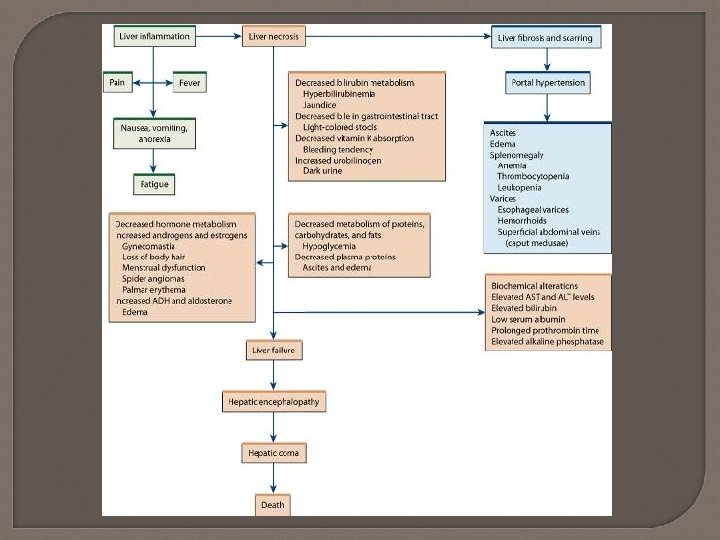
Cirrhosis Etiology and pathophysiology • Chronic, progressive degeneration of liver parenchymal Alcohol abuse is most common cause Hepatitis, primary biliary cirrhosis, primary sclerosing cholangitis, long standing R sided heart failure (aka cardiac cirrhosis)
Cirrhosis Cells try to regenerate but process is disorganized and blood vessel and bile duct flow become impeded Eventually hypoxia causes scarring and decreased liver functioning Controversial- but possibly alcoholic malnutrition exacerbates cirrhotic process
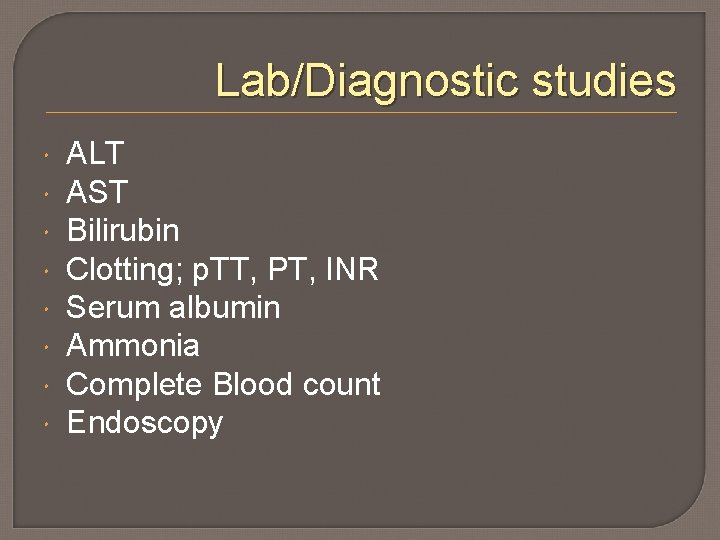
Lab/Diagnostic studies ALT AST Bilirubin Clotting; p. TT, PT, INR Serum albumin Ammonia Complete Blood count Endoscopy
Complications of Cirrhosis * Portal hypertension * Esophageal and gastric varices * Peripheral edema and ascites * Hepatic encephalopathy * Hepatorenal syndrome
Portal Hypertension Increased venous pressure caused by obstruction to the normal flow of blood through the portal system Esophageal varices develop; tortured, fragile vessels, bleed easily. Most life threatening complication of cirrhosis!
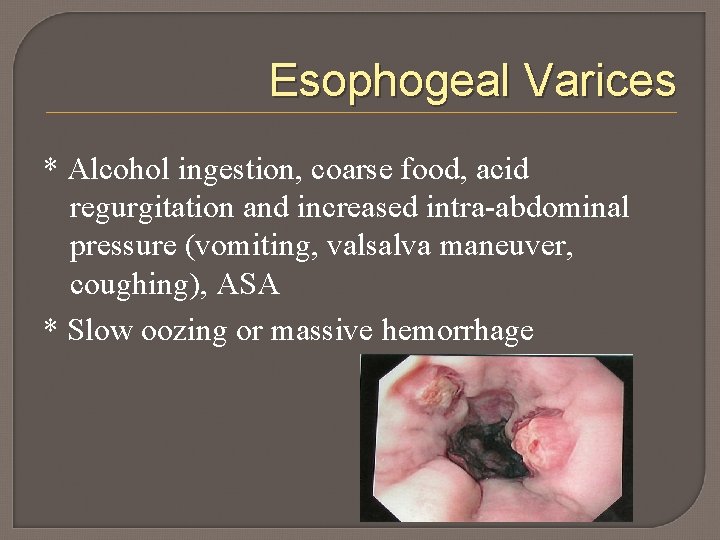
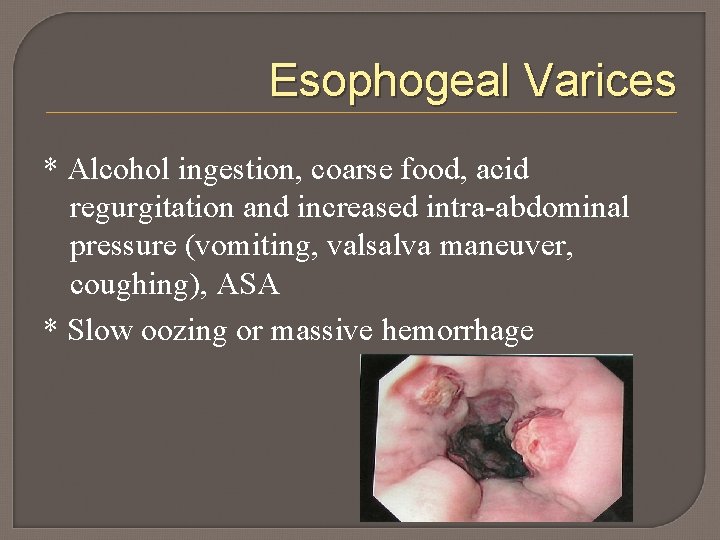
Esophogeal Varices * Alcohol ingestion, coarse food, acid regurgitation and increased intra-abdominal pressure (vomiting, valsalva maneuver, coughing), ASA * Slow oozing or massive hemorrhage
Treatment Beta blockers: prevention of bleeding; lowers portal hypertension Managing bleeding • Endoscopic therapy sclerotherapy, ligation/banding, balloon tamponade • Surgical procedure; shunts • Drugs- sandostatin & vasopressin
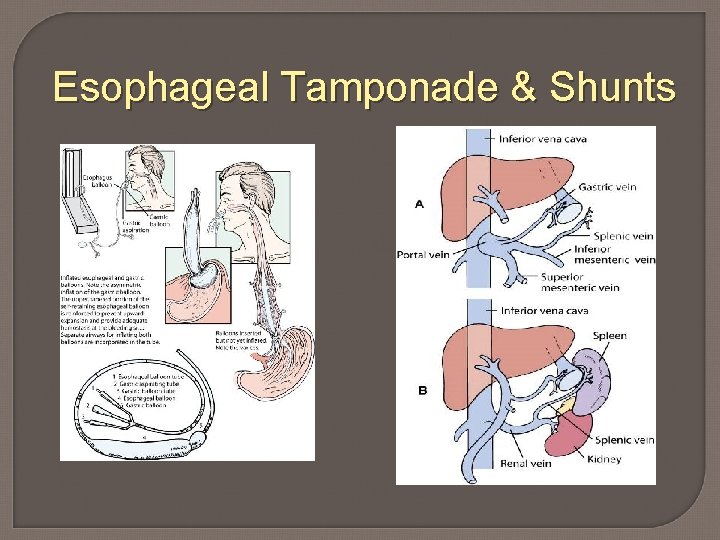
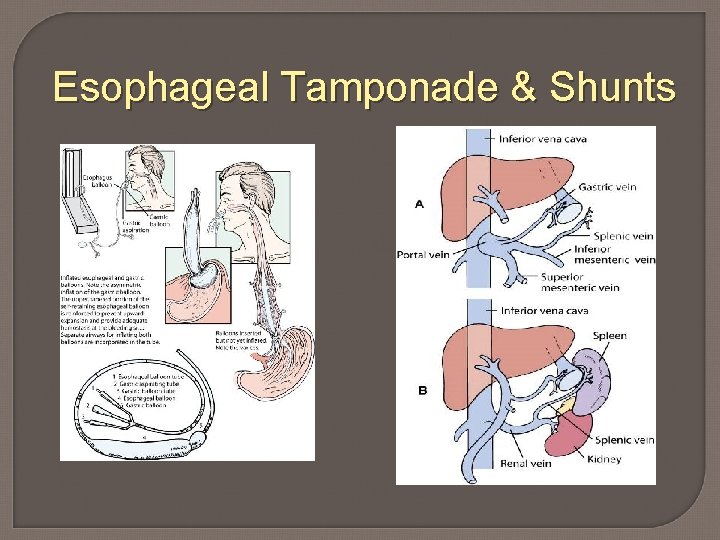
Esophageal Tamponade & Shunts
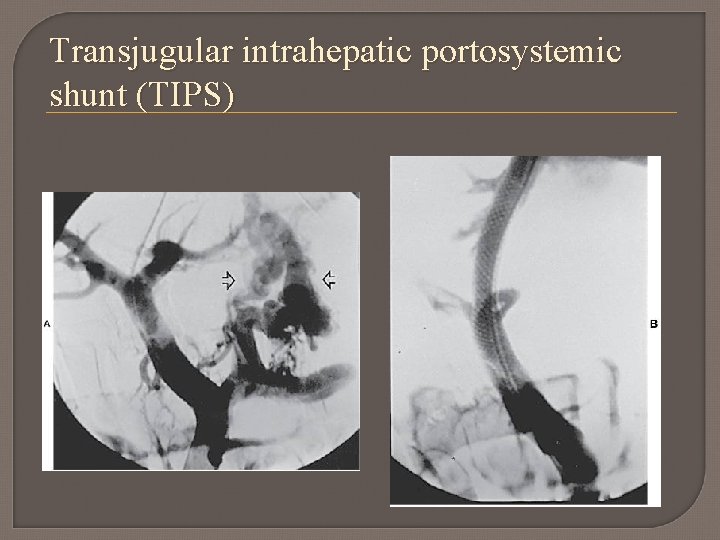
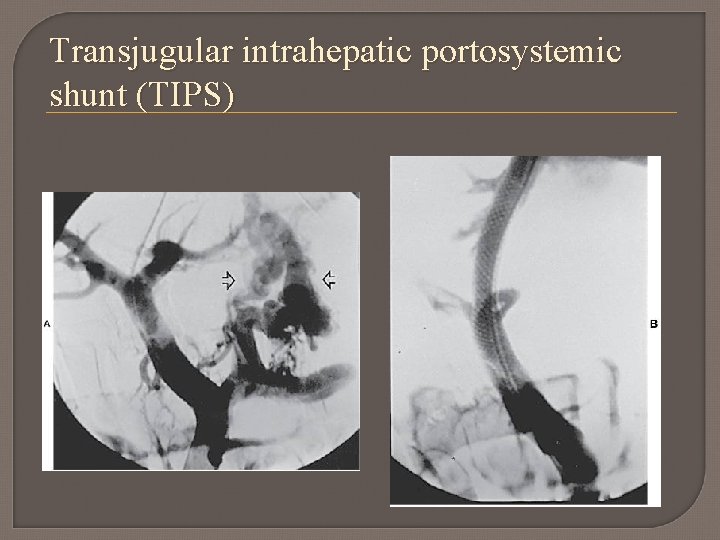
Transjugular intrahepatic portosystemic shunt (TIPS)
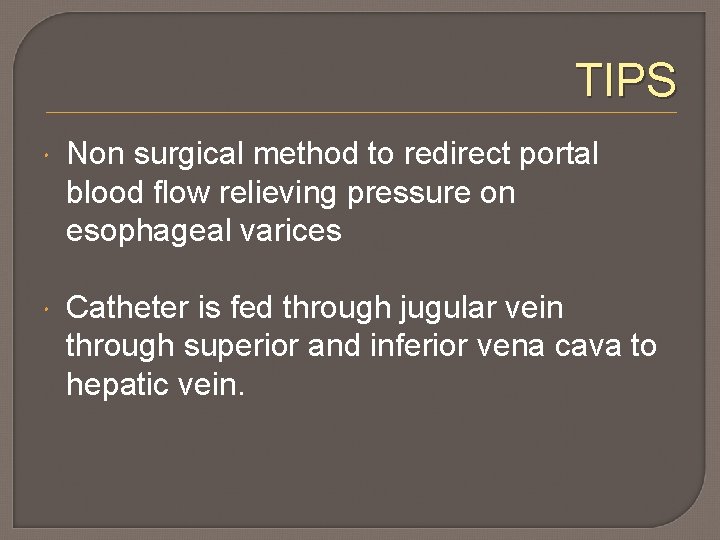
TIPS Non surgical method to redirect portal blood flow relieving pressure on esophageal varices Catheter is fed through jugular vein through superior and inferior vena cava to hepatic vein.
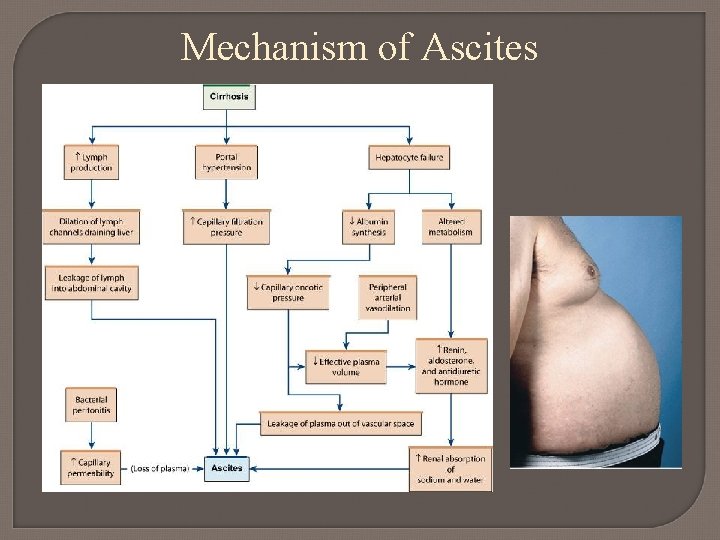
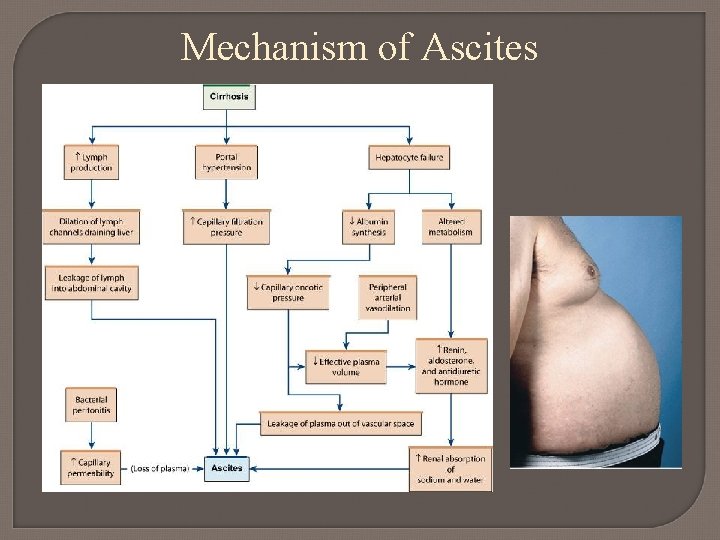
Mechanism of Ascites
Ascites Caused by decrease in collodial oncotic pressure (not enough albumin produced by liver) What commonly occurs to potassium levels? Treatment: Sodium restriction, diuretics and fluid removal (Paracentesis)
Hepatic encephalopathy Neuropsychiatric manifestation of liver damage Terminal complication of liver disease Liver normally detoxifies ammonia and converts to urea, then excreted by kidneys Ammonia crosses blood brain barrier
Signs Early : mood swings, apathy, memory loss, drowsiness, agitation Later ; slow/slurred speech, extreme emotional lability, hicccups, hyperactive reflexes, fetor hepaticus (musty, sweet breath odor) Eventually coma
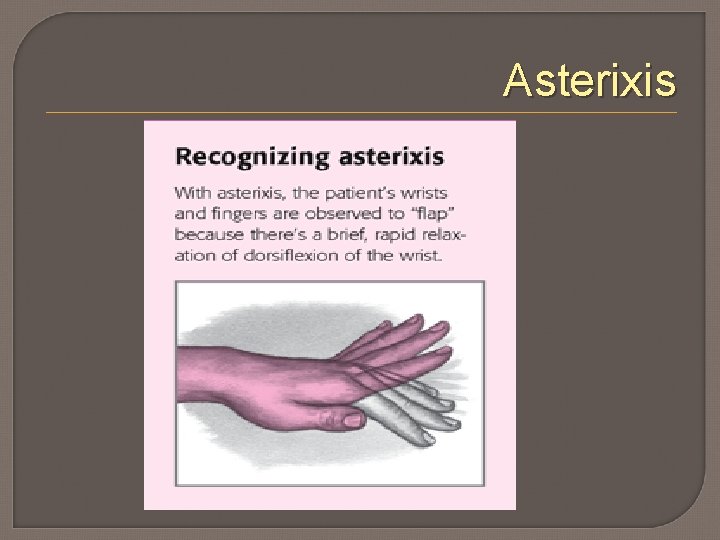
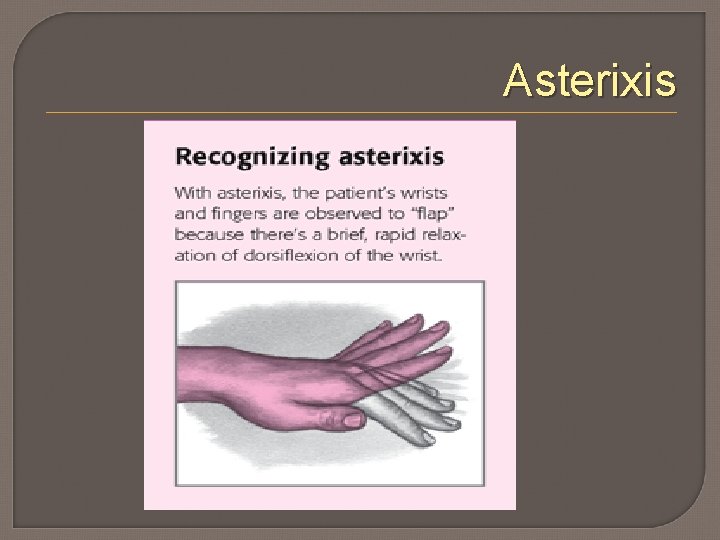
Asterixis
Goals Reduce ammonia formation/level Control GI bleeding to decrease protein in the intestine Lactulose
Hepatorenal syndrome Renal failure, worsening azotemia Portal HTN effects renal blood flow
Nutritional Therapy High calorie, high carbohydrates -3000 kcal/day -At least 1500 -2000 kcal/day to prevent hypoglycemia & catabolism What is recommendation for protein intake? Low sodium… why?
Fulminant Hepatic Failure Acute liver failure- rapid onset in pt. w/o prior hepatic disease Common cause is drugs: ETOH & APAP Hypoperfusion Viral hepatitis AST, ALT, serum bili all elevated. Clotting prolonged
Acetaminophen toxicity 7 -10 grams will do it Administer Mucomyst within 12 hours Limits formation of toxic metabolite Charcoal
Substance Abuse Chapter 12 (pg. 167)
Alcohol dependence *10 % of population *Psychological versus physical dependence (pg. 168)
Alcoholism *Chronic, progressive, potentially fatal disease if untreated
Alcohol is the #1 drug problem in Americans Nearly 1: 4 Americans being admitted to hospitals are undiagnosed alcoholics.
Blood Alcohol Concentration (BAC) Table 12 -8 (pg. 174) ETOH metabolized by liver and small amount by the stomach What are Potentiation & Crosstolerance?
Alcohol toxicity Acute; CNS depression, respiratory & circulatory failure Chronic; Wernicke’s encephalopathy • Inflammatory, hemorrhagic degenerative condition of the brain • Thiamine deficiency results from poor diet • Untreated can lead to Korsakoffs psychosis (irreversible)
Alcohol Withdrawal Goal: Safe detoxification
Group of symptoms that may occur from suddenly stopping the use of alcohol after chronic or prolonged use Pathophysiology: The brain maintains neurochemical balance through inhibitory and excitatory neurotransmitters (GABA, GABA-A & NMDA). Abrupt cessation of alcohol results in brain hyper excitability because receptors previously inhibited by alcohol are no longer inhibited
ETOH Withdrawal Analogous to having an accelerator without a brake
ETOH Withdrawal *Can occur as soon as 4 -6 hours after the last drink, and may last up to 5 days or more * Seizures are most likely to occur 7 -48 hours post last drink
Minor Withdrawal: • Restlessness, anxiety, sleeping difficulties, agitation, tremors, tachycardia, low-grade fever, diaphoresis & elevated BP Major Withdrawal: • Visual or auditory hallucinations, delirium tremens (DTs), diastolic pressure above 100 mm/Hg, pronounced diaphoresis, & vomiting; minor withdrawal symptoms may still be seen Life-threatening withdrawal: • DT, disorientation times, global confusion & inability to recognize familiar objects or people
ETOH Withdrawal Delirium Also known as Delirium Tremens Severe complication Disorientation and global confusion May occur 30 -120 hrs after last drink The greater the ETOH dependence, the greater the risk of development of SEVERE withdrawal symptoms
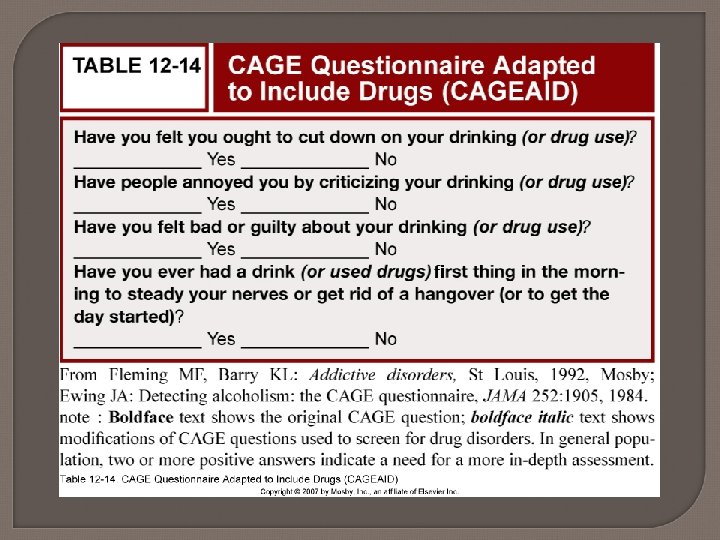
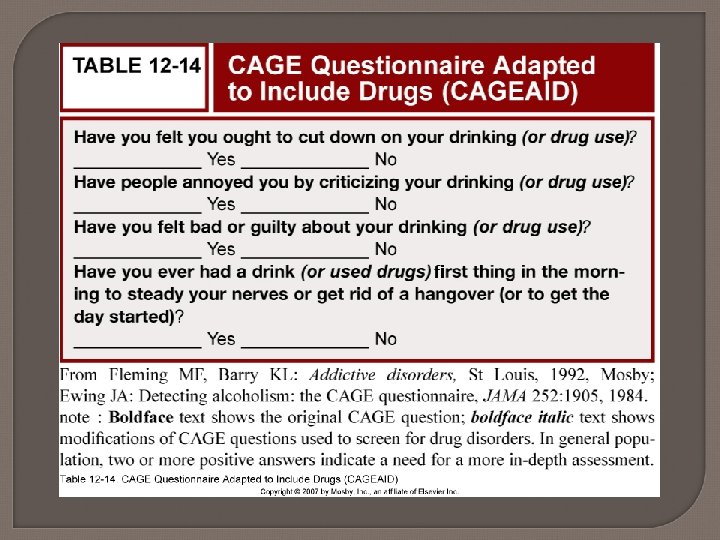
LABS & DIAGNOSTICS Significant thiamine deficiency Diagnosis is made primarily utilizing DSM-IV criteria & with the support of other tools such as CAGE Note: not every person who discontinues drinking experiences withdrawal symptoms, but most people who drink for long periods, or heavily, do experience some form of symptoms if they stop drinking suddenly
PRIORITY Nursing Diagnoses Risk for injury & falls Risk for self & other directed violence Fluid/electrolytes imbalance Anxiety
INTERVENTIONS Implement CIWA protocol Seek individualized orders/plan for treatment from the physician • Symptom triggered therapy Explain alcohol abstinence symptoms to the client Provide a safe, comfortable environment Assessment Seizure precautions
Symptom Triggered Therapy CIWA score…Lorazepam and/or Haldol dose Benzos drug of choice for treatment of alcohol withdrawal • Stimulate GABA (“calming” Neurotransmiter) receptors hence decreasing S/S. • Ativan; short acting, valium; long acting
Collaborative care Supportive measures No antidote for ETOH Thiamine before glucose…why? What is in the usual premixed IV solution administered for alcohol intoxication • “banana” bag
DISCHARGE OUTCOMES Physical Considerations: Pt. will have stable V/S Pt. will have stable function of all body systems Pt. will remain free of other injury Pt. & family will be able to verbalize symptoms of alcohol withdrawal Pt. will be safe, comfortable, & able to control own activities without creating harm to self or others
DISCHARGE PLANNING Arrange clinic, telephone & home contacts Arrange methods of contacting healthcare providers (e. g. phone numbers) to assist with crisis events Consider transfer to inpatient facility when withdrawal is severe Provide support group contact information
Promoting Sustained Abstinence Naltrexone Antabuse Campral