Cardiac Dysrhythmias NURS 241 Chapter 36 p 818









- Slides: 29
Cardiac Dysrhythmias NURS 241 Chapter 36 (p. 818)
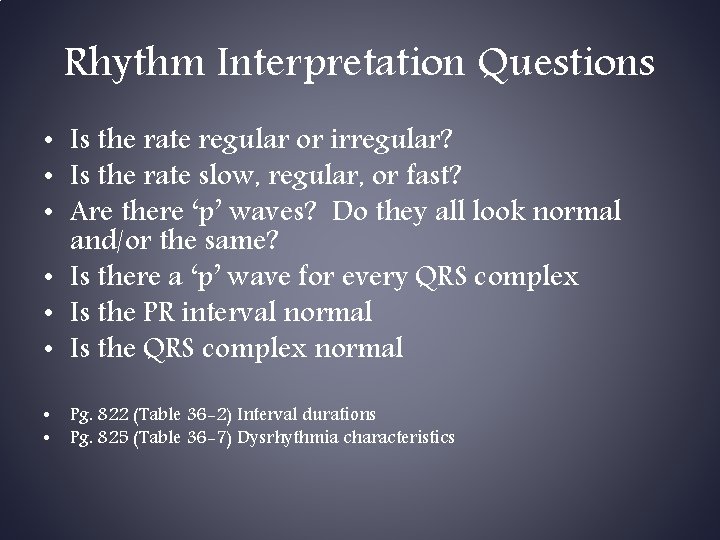
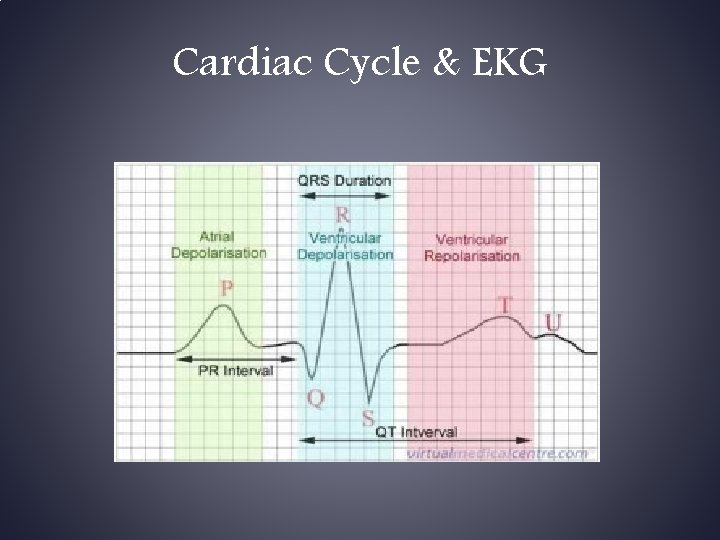
Rhythm Interpretation Questions • Is the rate regular or irregular? • Is the rate slow, regular, or fast? • Are there ‘p’ waves? Do they all look normal and/or the same? • Is there a ‘p’ wave for every QRS complex • Is the PR interval normal • Is the QRS complex normal • • Pg. 822 (Table 36 -2) Interval durations Pg. 825 (Table 36 -7) Dysrhythmia characteristics

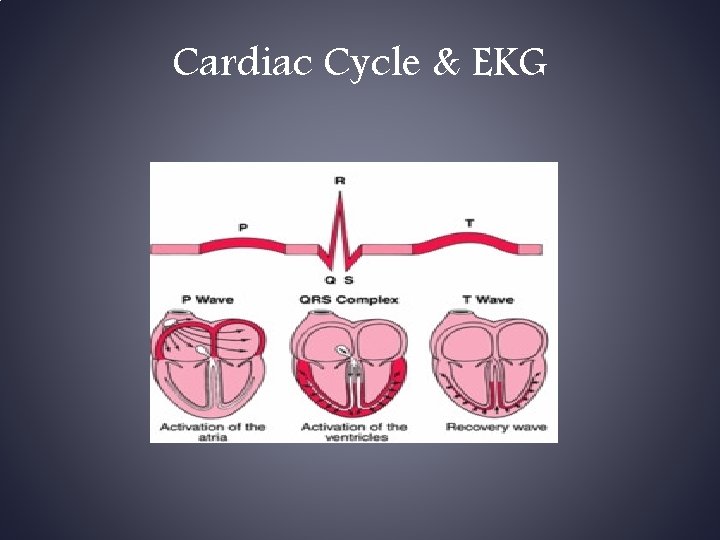
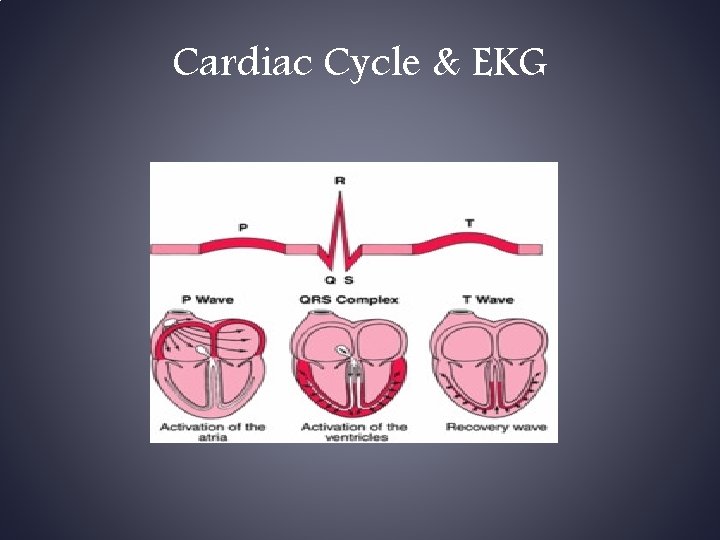
Cardiac Cycle & EKG
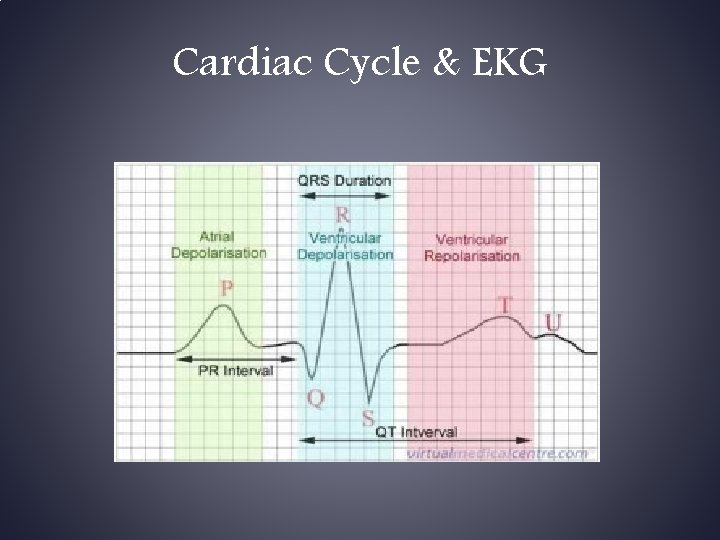
Cardiac Cycle & EKG

Determining Heart Rate • • • 1 mm = 0. 04 sec (or each individual block) 5 mm = 0. 2 sec (or between 2 dark vertical lines) Rate = 300/#5 mm boxes b/w R-to-R Rate = 1500/#1 mm boxes b/w R-to-R If rhythm irregular… count number of R waves in 6 seconds and multiply by 10 for an estimated rate
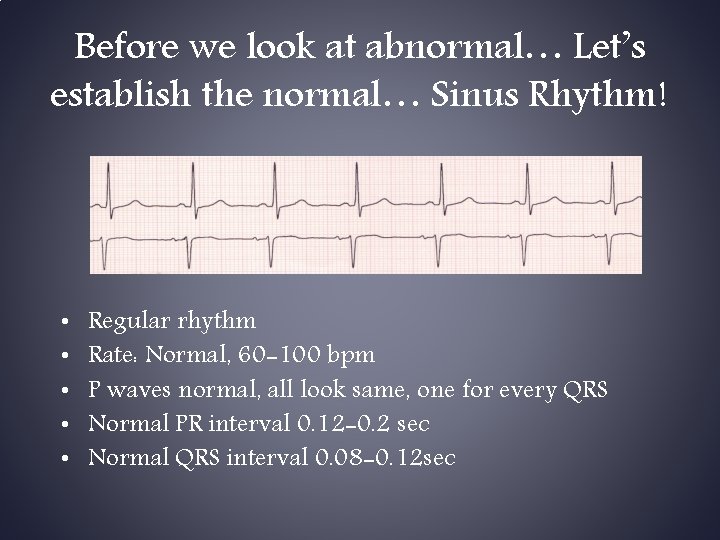
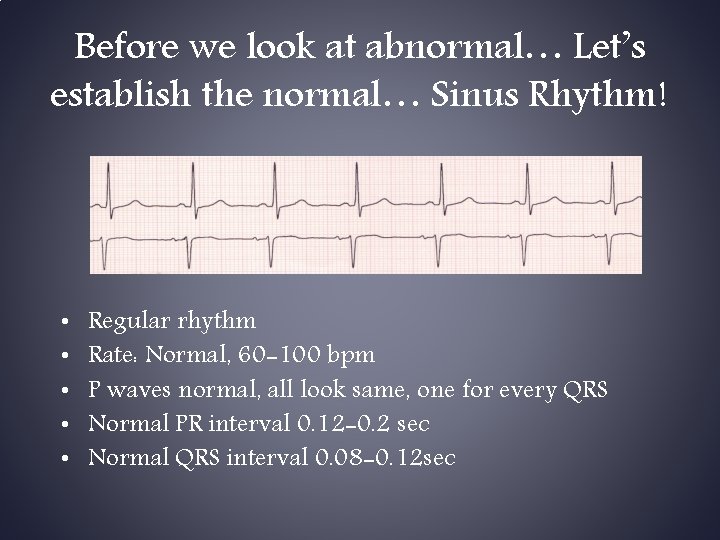
Before we look at abnormal… Let’s establish the normal… Sinus Rhythm! • • • Regular rhythm Rate: Normal, 60 -100 bpm P waves normal, all look same, one for every QRS Normal PR interval 0. 12 -0. 2 sec Normal QRS interval 0. 08 -0. 12 sec

Sinus Bradycardia Regular rhythm Rate: Slow, less than 60 bpm P waves normal, all look same (kind of), one for every QRS PR & QRS intervals normal Causes: vagal stimulation, hypothermia, inferior MI, increased ICP, hypothyroid, cardiac meds (beta blockers) • Tx w/ atropine ONLY if pt. symptomatic • • •
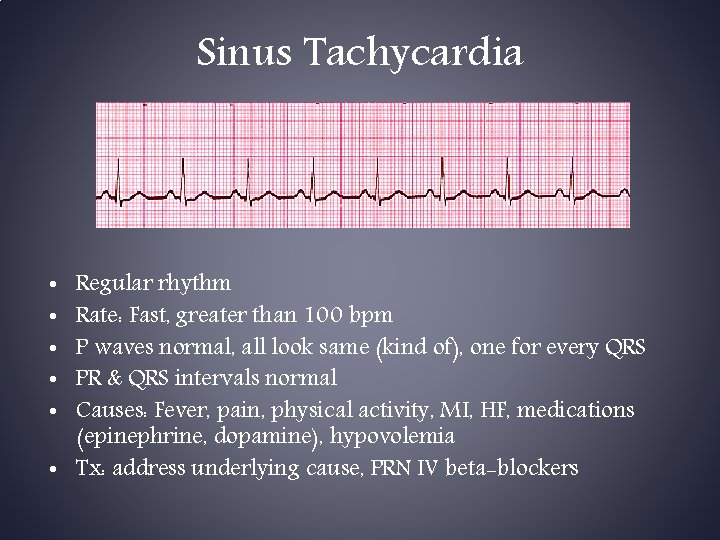
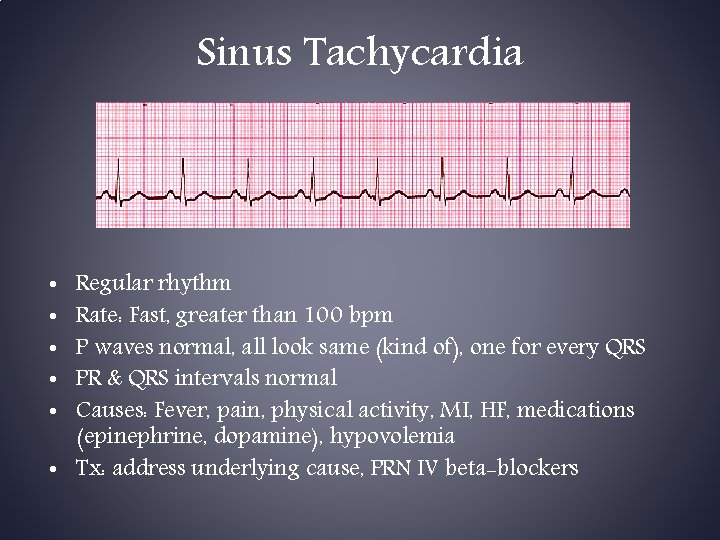
Sinus Tachycardia Regular rhythm Rate: Fast, greater than 100 bpm P waves normal, all look same (kind of), one for every QRS PR & QRS intervals normal Causes: Fever, pain, physical activity, MI, HF, medications (epinephrine, dopamine), hypovolemia • Tx: address underlying cause, PRN IV beta-blockers • • •
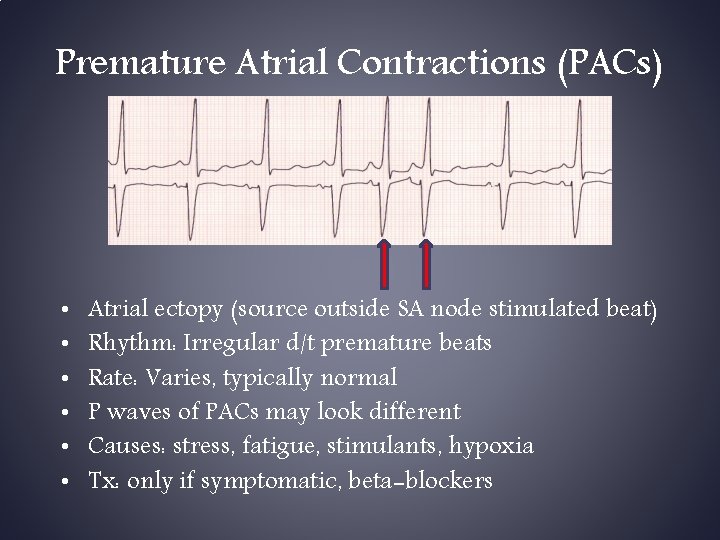
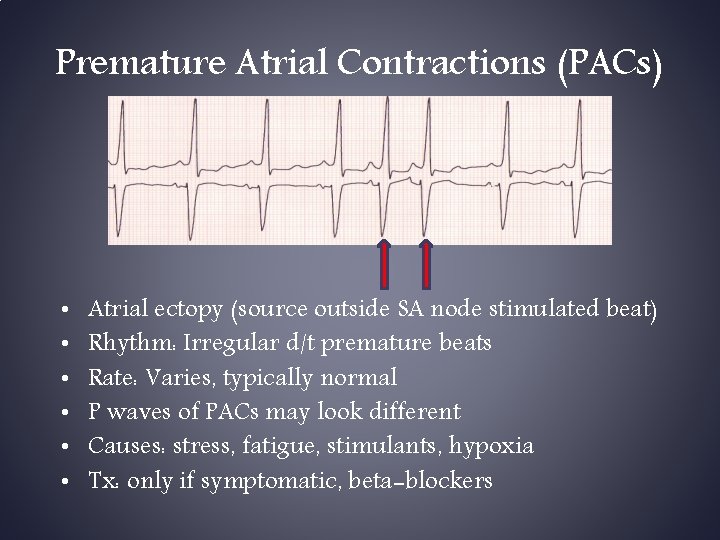
Premature Atrial Contractions (PACs) • • • Atrial ectopy (source outside SA node stimulated beat) Rhythm: Irregular d/t premature beats Rate: Varies, typically normal P waves of PACs may look different Causes: stress, fatigue, stimulants, hypoxia Tx: only if symptomatic, beta-blockers
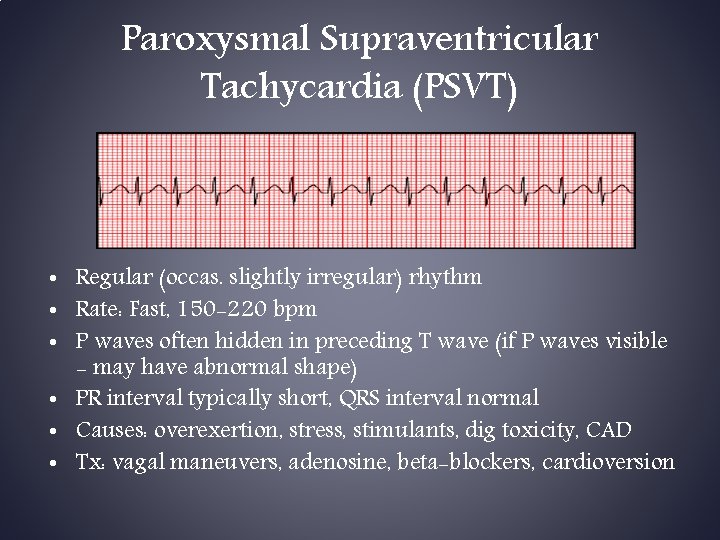
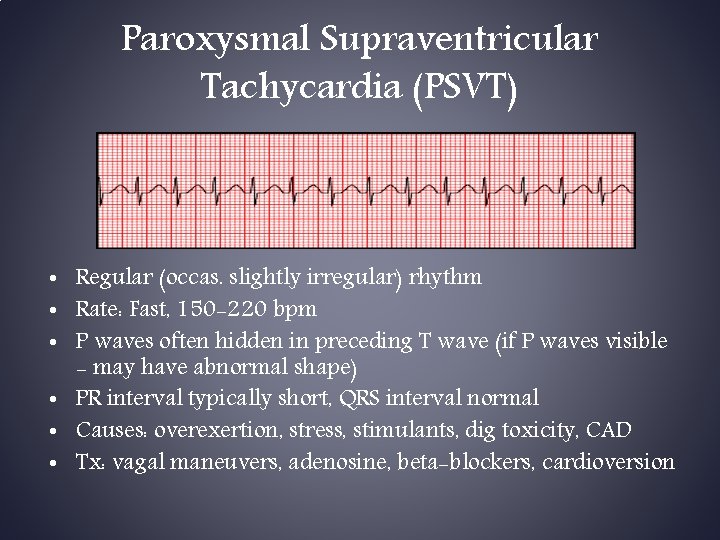
Paroxysmal Supraventricular Tachycardia (PSVT) • Regular (occas. slightly irregular) rhythm • Rate: Fast, 150 -220 bpm • P waves often hidden in preceding T wave (if P waves visible - may have abnormal shape) • PR interval typically short, QRS interval normal • Causes: overexertion, stress, stimulants, dig toxicity, CAD • Tx: vagal maneuvers, adenosine, beta-blockers, cardioversion

Atrial Flutter • • • Regular rhythm typically Rate: atrial 200 -350 bpm, ventricular varies No P waves, only flutter waves, sawtooth appearance Causes: CAD, HTN, MV disease, chronic lung disease Tx: beta-blockers, Ca channel blockers, cardioversion, antidysrhythmic Rx, cardiac ablation
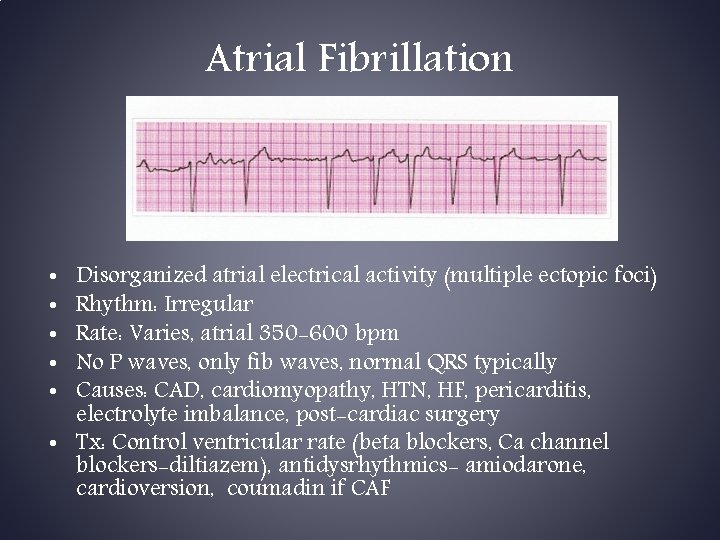
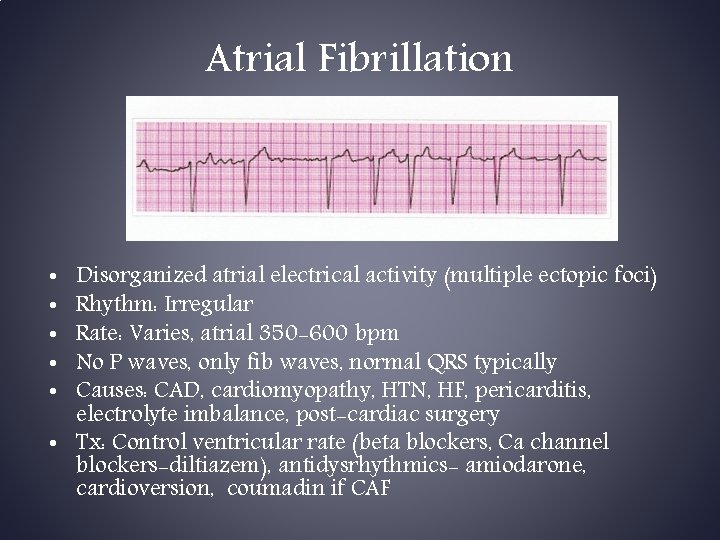
Atrial Fibrillation Disorganized atrial electrical activity (multiple ectopic foci) Rhythm: Irregular Rate: Varies, atrial 350 -600 bpm No P waves, only fib waves, normal QRS typically Causes: CAD, cardiomyopathy, HTN, HF, pericarditis, electrolyte imbalance, post-cardiac surgery • Tx: Control ventricular rate (beta blockers, Ca channel blockers-diltiazem), antidysrhythmics- amiodarone, cardioversion, coumadin if CAF • • •
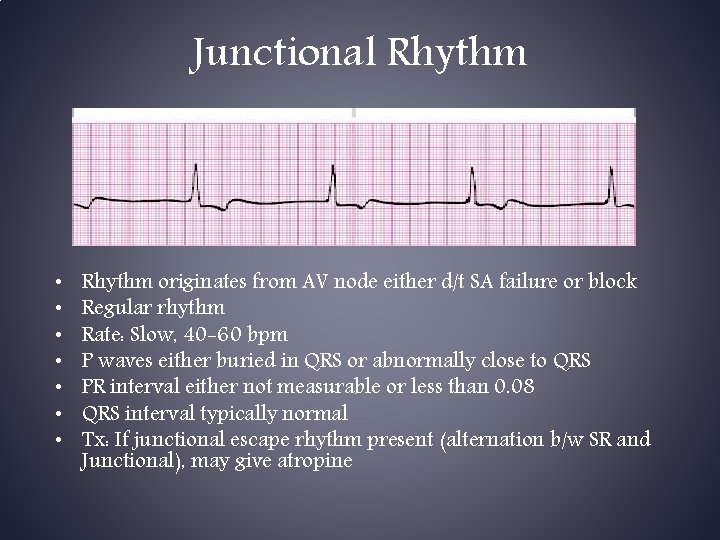
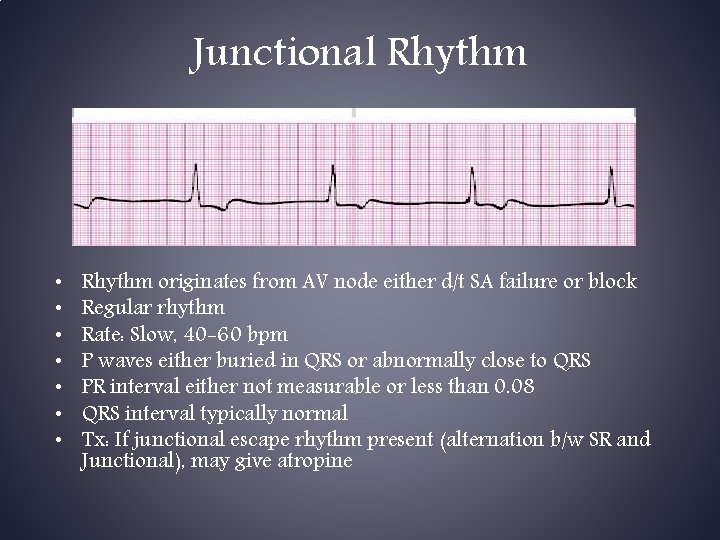
Junctional Rhythm • • Rhythm originates from AV node either d/t SA failure or block Regular rhythm Rate: Slow, 40 -60 bpm P waves either buried in QRS or abnormally close to QRS PR interval either not measurable or less than 0. 08 QRS interval typically normal Tx: If junctional escape rhythm present (alternation b/w SR and Junctional), may give atropine

Accelerated Junctional • Regular rhythm • Rate: Normal, 61 -100 bpm • P waves either buried in QRS or abnormally close to QRS • PR interval either not measurable or less than 0. 08 • QRS interval typically normal
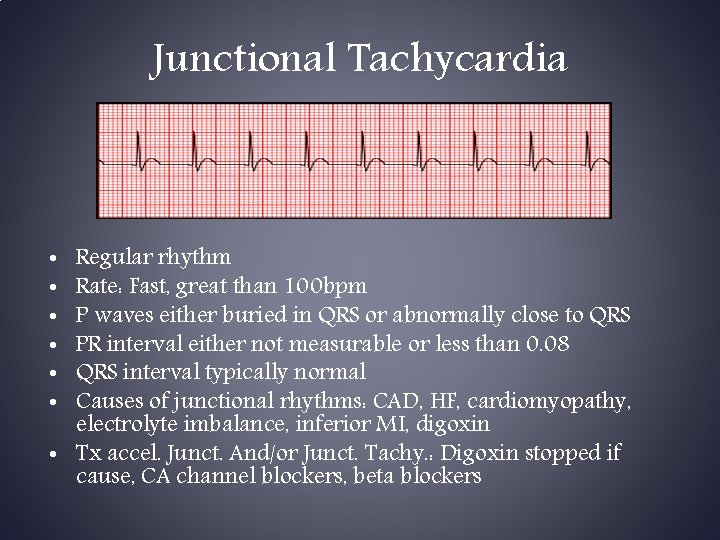
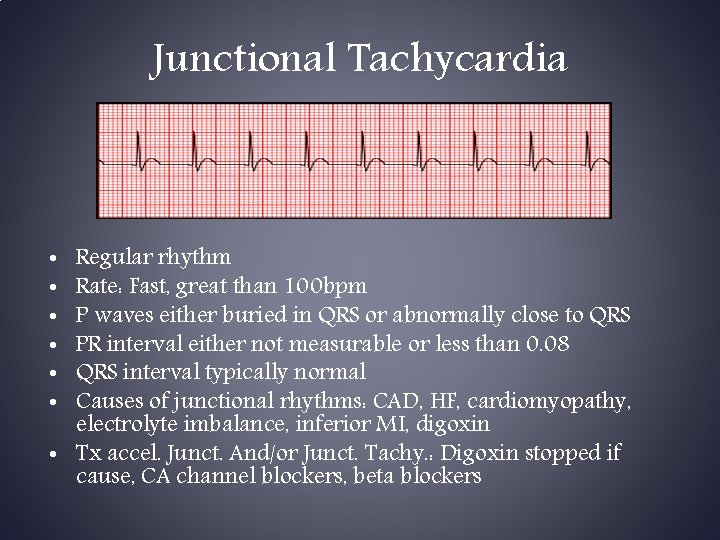
Junctional Tachycardia Regular rhythm Rate: Fast, great than 100 bpm P waves either buried in QRS or abnormally close to QRS PR interval either not measurable or less than 0. 08 QRS interval typically normal Causes of junctional rhythms: CAD, HF, cardiomyopathy, electrolyte imbalance, inferior MI, digoxin • Tx accel. Junct. And/or Junct. Tachy. : Digoxin stopped if cause, CA channel blockers, beta blockers • • •

First Degree AV Block Regular Rhythm Rate: typically normal but can be faster/slower P waves for every QRS, normal in appearance, but… PR interval is prolonged, greater than 0. 2 sec QRS normal Causes: MI, CAD, hyperthyroid, digoxin, beta blockers, Ca channel blockers • Tx: removal of causal drug if applicable, monitor for worsening block • • •
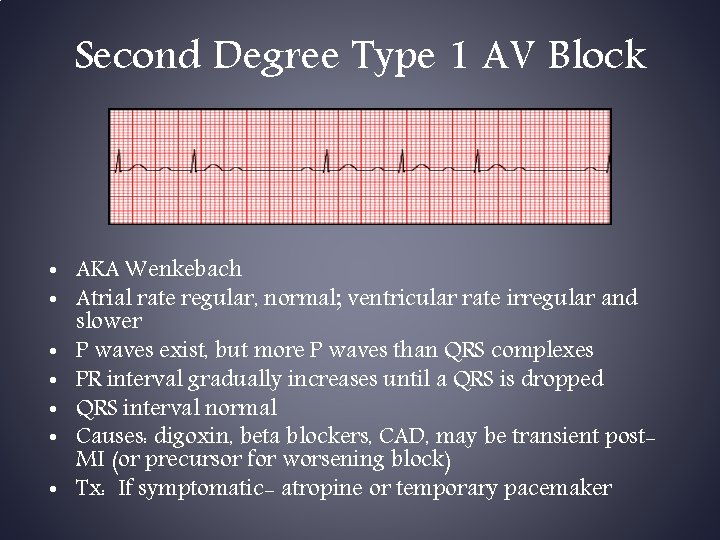
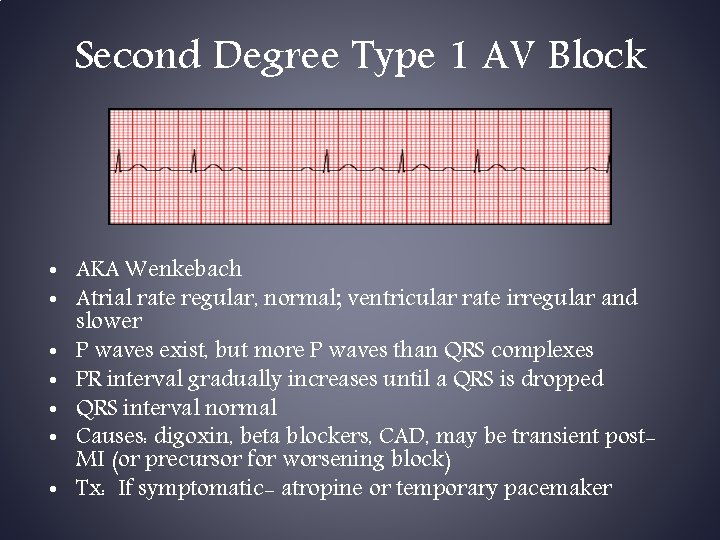
Second Degree Type 1 AV Block • AKA Wenkebach • Atrial rate regular, normal; ventricular rate irregular and slower • P waves exist, but more P waves than QRS complexes • PR interval gradually increases until a QRS is dropped • QRS interval normal • Causes: digoxin, beta blockers, CAD, may be transient post. MI (or precursor for worsening block) • Tx: If symptomatic- atropine or temporary pacemaker
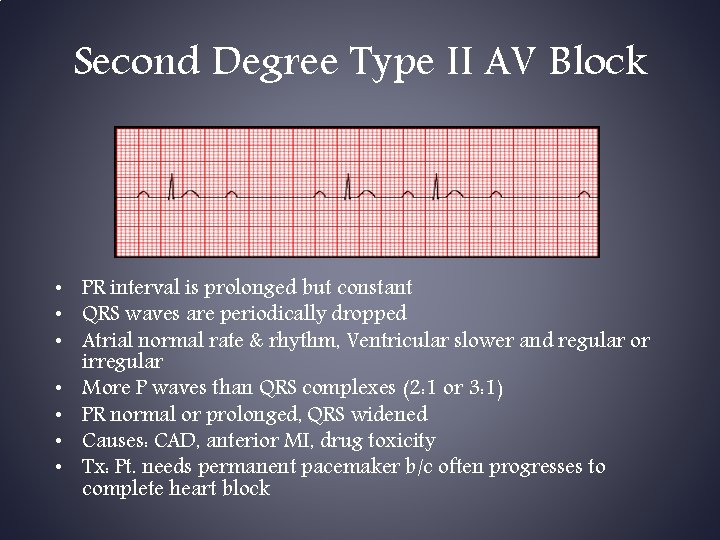
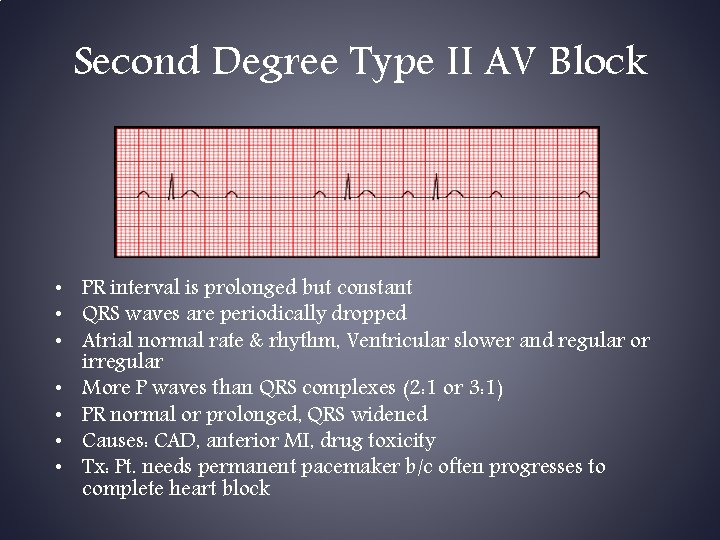
Second Degree Type II AV Block • PR interval is prolonged but constant • QRS waves are periodically dropped • Atrial normal rate & rhythm, Ventricular slower and regular or irregular • More P waves than QRS complexes (2: 1 or 3: 1) • PR normal or prolonged, QRS widened • Causes: CAD, anterior MI, drug toxicity • Tx: Pt. needs permanent pacemaker b/c often progresses to complete heart block
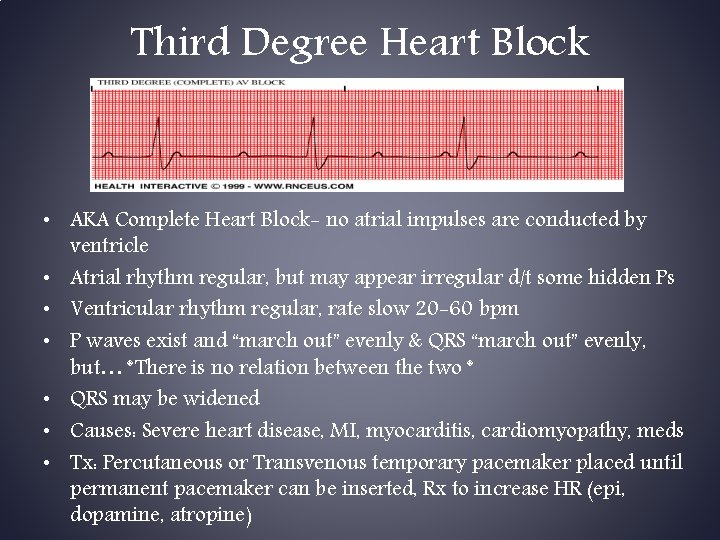
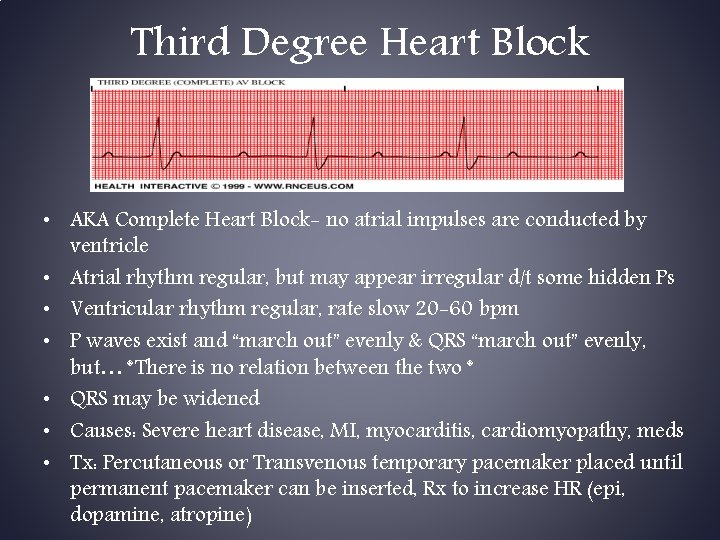
Third Degree Heart Block • AKA Complete Heart Block- no atrial impulses are conducted by ventricle • Atrial rhythm regular, but may appear irregular d/t some hidden Ps • Ventricular rhythm regular, rate slow 20 -60 bpm • P waves exist and “march out” evenly & QRS “march out” evenly, but… *There is no relation between the two * • QRS may be widened • Causes: Severe heart disease, MI, myocarditis, cardiomyopathy, meds • Tx: Percutaneous or Transvenous temporary pacemaker placed until permanent pacemaker can be inserted, Rx to increase HR (epi, dopamine, atropine)
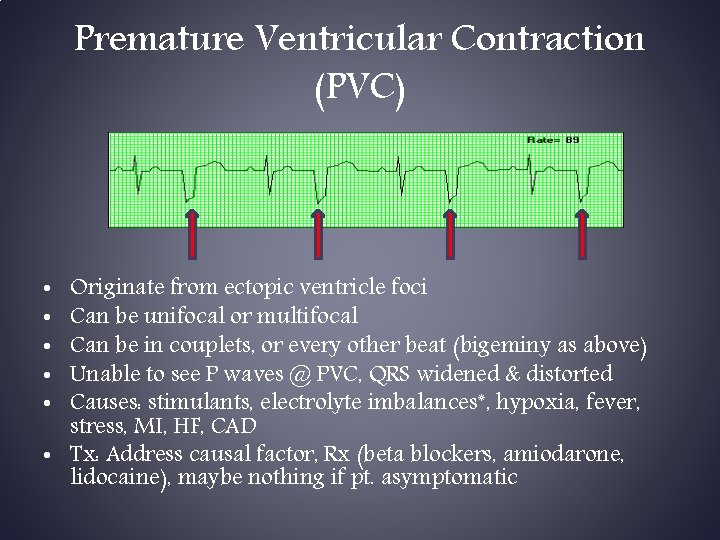
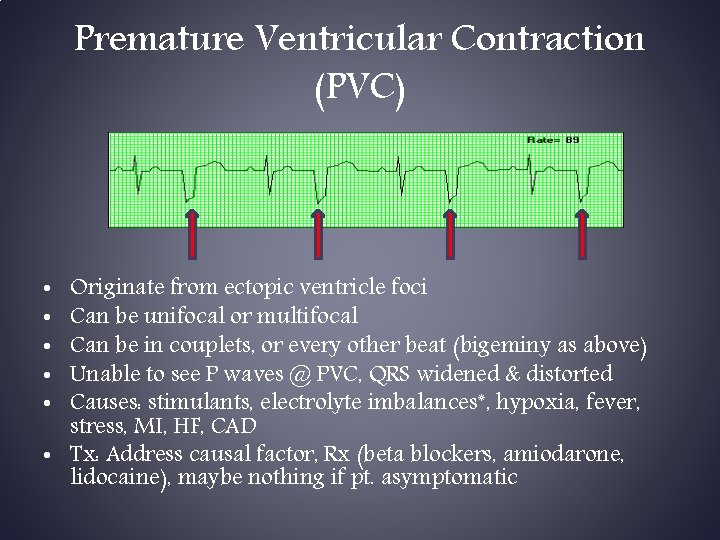
Premature Ventricular Contraction (PVC) Originate from ectopic ventricle foci Can be unifocal or multifocal Can be in couplets, or every other beat (bigeminy as above) Unable to see P waves @ PVC, QRS widened & distorted Causes: stimulants, electrolyte imbalances*, hypoxia, fever, stress, MI, HF, CAD • Tx: Address causal factor, Rx (beta blockers, amiodarone, lidocaine), maybe nothing if pt. asymptomatic • • •
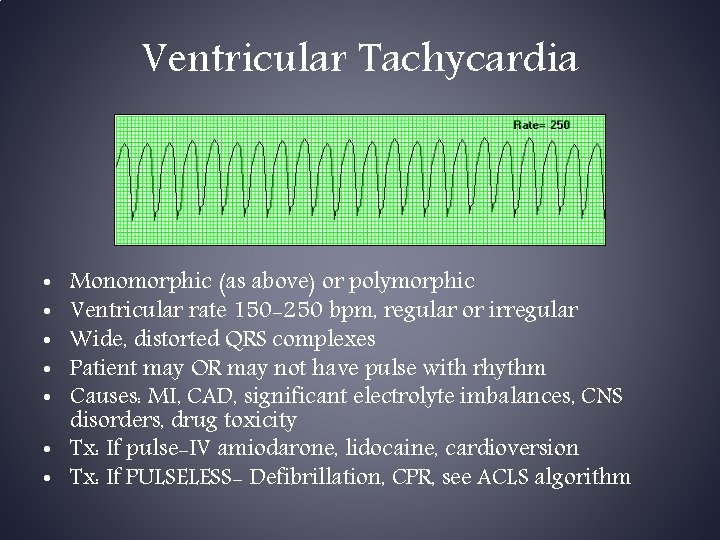
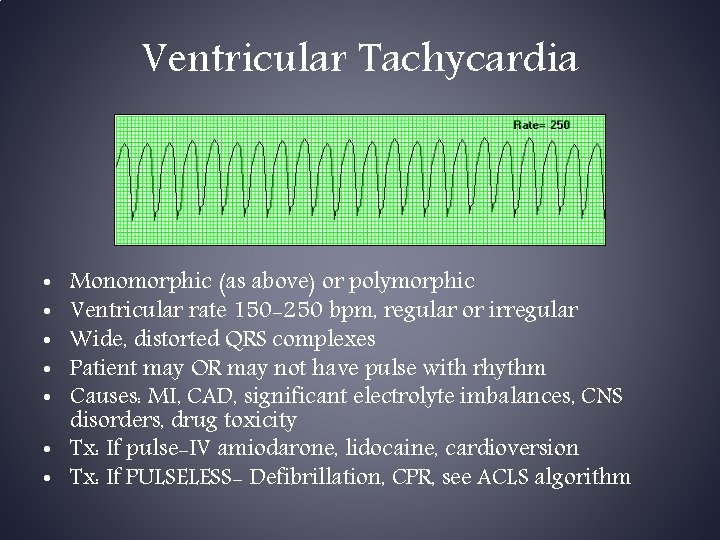
Ventricular Tachycardia Monomorphic (as above) or polymorphic Ventricular rate 150 -250 bpm, regular or irregular Wide, distorted QRS complexes Patient may OR may not have pulse with rhythm Causes: MI, CAD, significant electrolyte imbalances, CNS disorders, drug toxicity • Tx: If pulse-IV amiodarone, lidocaine, cardioversion • Tx: If PULSELESS- Defibrillation, CPR, see ACLS algorithm • • •
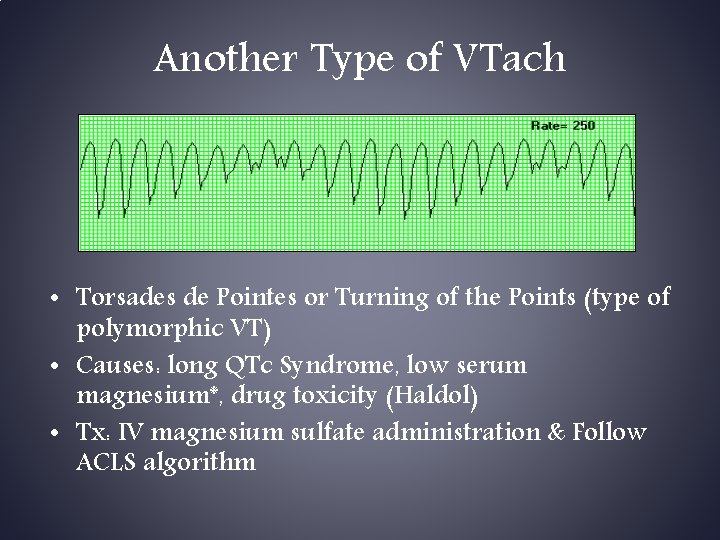
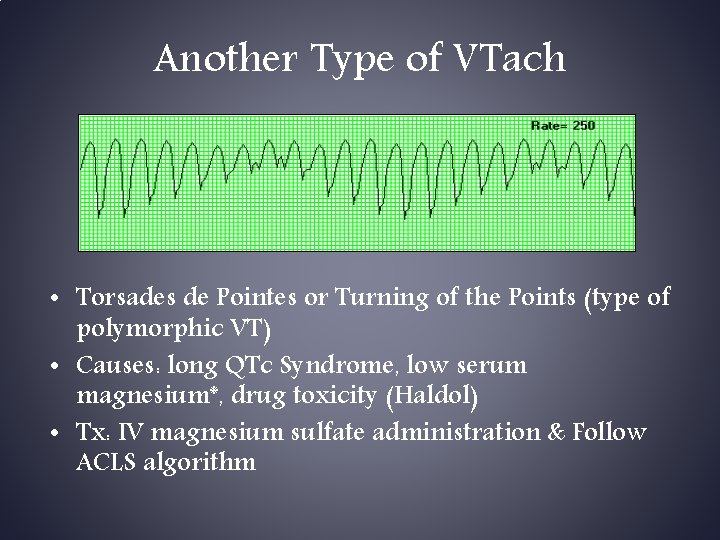
Another Type of VTach • Torsades de Pointes or Turning of the Points (type of polymorphic VT) • Causes: long QTc Syndrome, low serum magnesium*, drug toxicity (Haldol) • Tx: IV magnesium sulfate administration & Follow ACLS algorithm
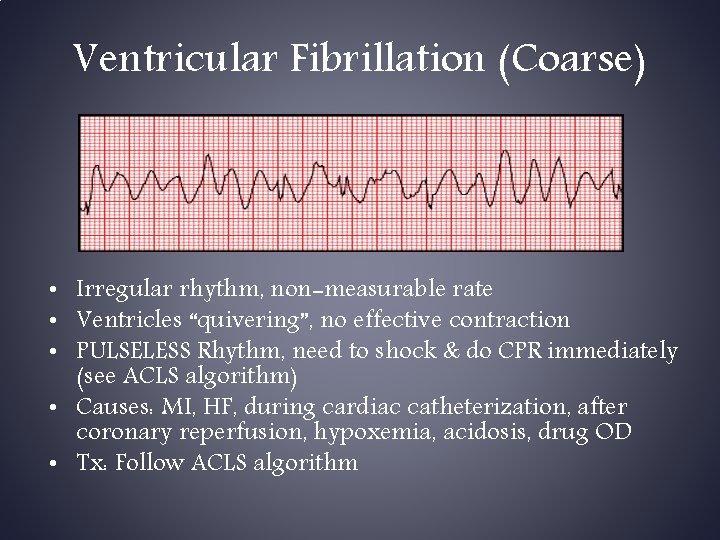
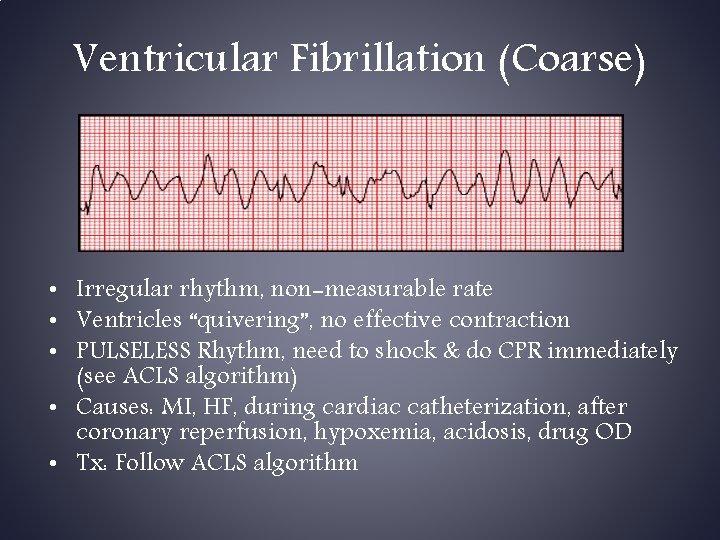
Ventricular Fibrillation (Coarse) • Irregular rhythm, non-measurable rate • Ventricles “quivering”, no effective contraction • PULSELESS Rhythm, need to shock & do CPR immediately (see ACLS algorithm) • Causes: MI, HF, during cardiac catheterization, after coronary reperfusion, hypoxemia, acidosis, drug OD • Tx: Follow ACLS algorithm

Ventricular Fibrillation (Fine) • Same causes & Tx modalities • Same as coarse VF except energy stores running out and essentially indicating worsening of situation • Next progression… asystole

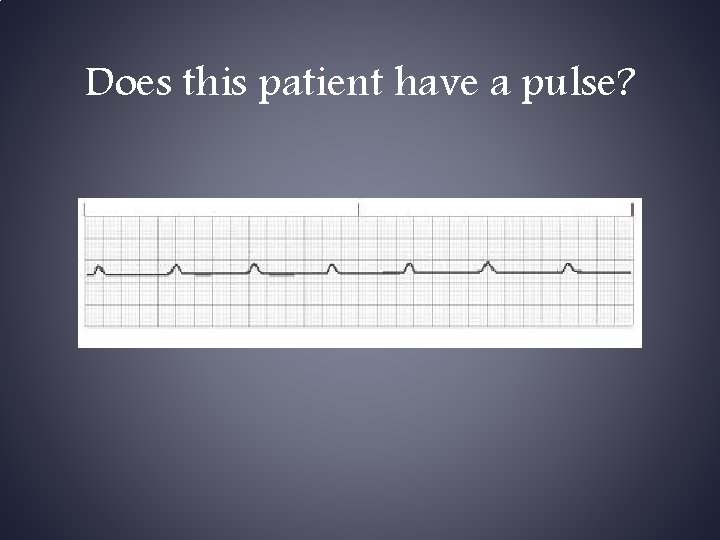
Pulseless Electrical Activity • May see a rhythm on monitor BUT there is NO PULSE • Poor Prognosis unless cause identified & treated • Causes: hypovolemia, hypoxia, metabolic acidosis, hyper or hypokalemia, hypothermia, drug OD, cardiac tamponade, MI, PE, tension pneumothorax • Tx: Follow ACLS algorithm
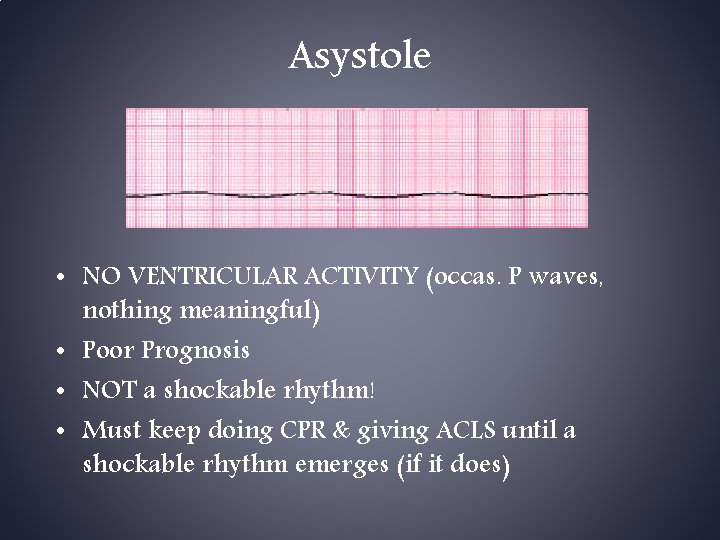
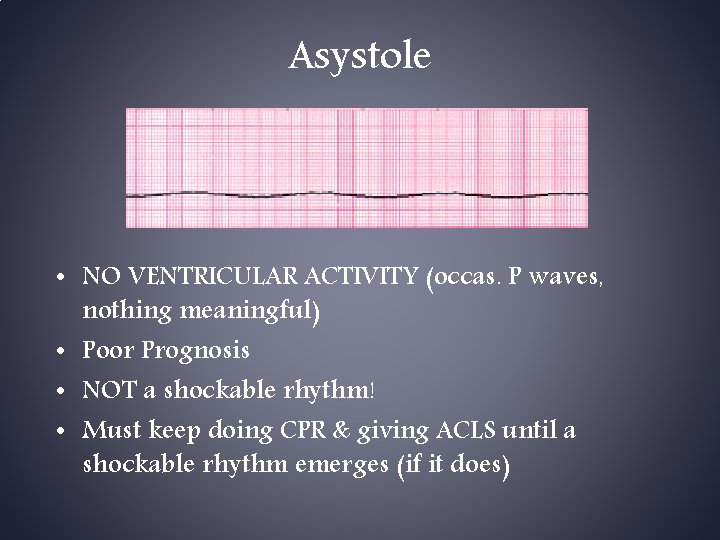
Asystole • NO VENTRICULAR ACTIVITY (occas. P waves, nothing meaningful) • Poor Prognosis • NOT a shockable rhythm! • Must keep doing CPR & giving ACLS until a shockable rhythm emerges (if it does)
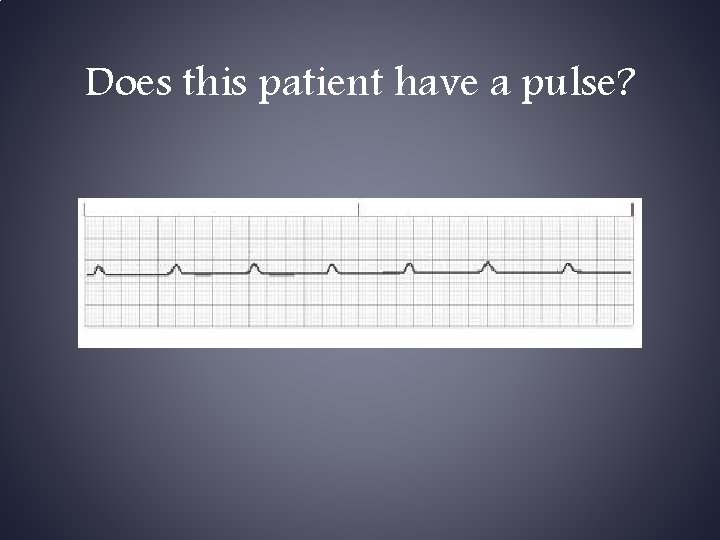
Does this patient have a pulse?

 Wandering pacemaker
Wandering pacemaker Dewey decimal vs library of congress
Dewey decimal vs library of congress Dewey decimal 808
Dewey decimal 808 Sqlcode 922
Sqlcode 922 Nurs 200
Nurs 200 Nurs 425
Nurs 425 Nurs 425
Nurs 425 Nfpa 241 requirements
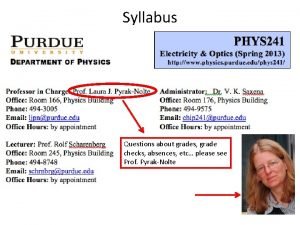
Nfpa 241 requirements Physics 241 purdue
Physics 241 purdue 241 bce
241 bce 341 rounded to the nearest ten
341 rounded to the nearest ten Fon 241
Fon 241 Cob 241
Cob 241 Ceng 241
Ceng 241 Psyco 241
Psyco 241 Cs 241 vector mp
Cs 241 vector mp Ceng 241
Ceng 241 Chm 241
Chm 241 Orthographic drawing
Orthographic drawing Mappa concettuale legge 241/90
Mappa concettuale legge 241/90 Spherical differential
Spherical differential Legge 241/90 slide
Legge 241/90 slide Purdue phys 241
Purdue phys 241 Bio 241
Bio 241 241 in arabic
241 in arabic Homometric regulation of cardiac output
Homometric regulation of cardiac output Cardiac distension
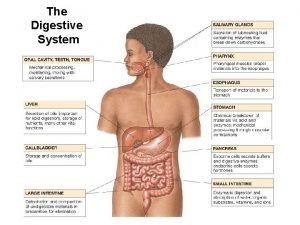
Cardiac distension Peosinogen
Peosinogen Cardiac cycle steps
Cardiac cycle steps Stomach
Stomach