Is Restless Legs Syndrome an Inflammatory Disease Leonard

- Slides: 52
Is Restless Legs Syndrome an Inflammatory Disease? Leonard Weinstock, MD Associate Professor of Clinical Medicine Washington University School of Medicine President, Specialists in Gastroenterology
Disclosures w Speakers Bureau § Salix, Entera Health, Actavis, Romark w Consultant § Actavis w Off label use of medicine – educational information, not promotional
RLS clinical importance Pathophysiology Role of SIBO Rifaximin studies Inflammation & endorphin def Sequential rifaximin & LDN study
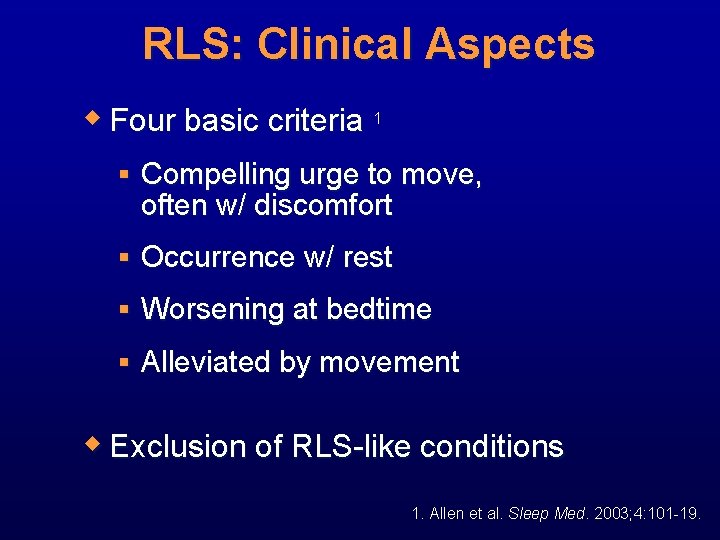
RLS: Clinical Aspects w Four basic criteria 1 § Compelling urge to move, often w/ discomfort § Occurrence w/ rest § Worsening at bedtime § Alleviated by movement w Exclusion of RLS-like conditions 1. Allen et al. Sleep Med. 2003; 4: 101 -19.
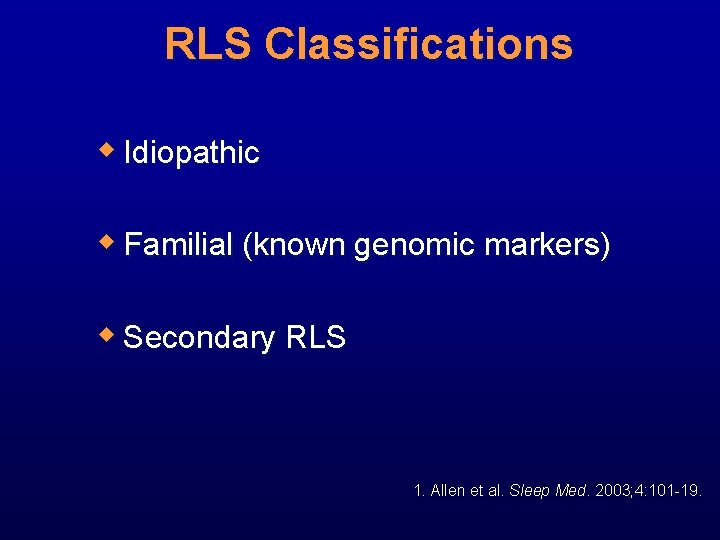
RLS Classifications w Idiopathic w Familial (known genomic markers) w Secondary RLS 1. Allen et al. Sleep Med. 2003; 4: 101 -19.
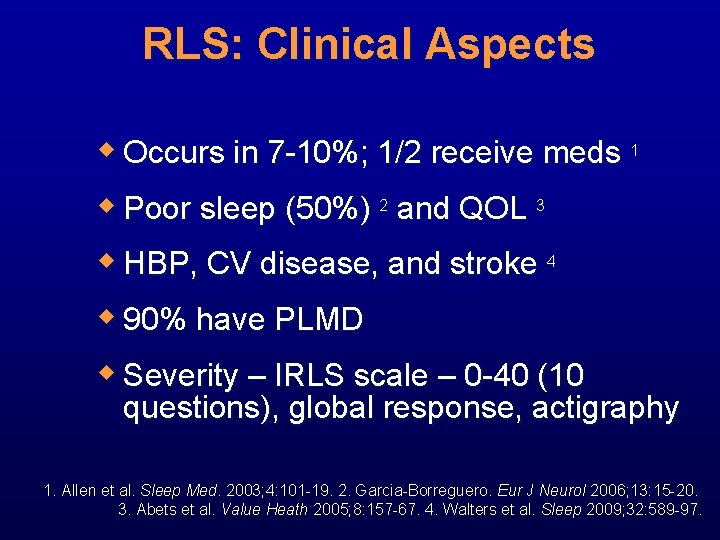
RLS: Clinical Aspects w Occurs in 7 -10%; 1/2 receive meds 1 w Poor sleep (50%) 2 and QOL 3 w HBP, CV disease, and stroke 4 w 90% have PLMD w Severity – IRLS scale – 0 -40 (10 questions), global response, actigraphy 1. Allen et al. Sleep Med. 2003; 4: 101 -19. 2. Garcia-Borreguero. Eur J Neurol 2006; 13: 15 -20. 3. Abets et al. Value Heath 2005; 8: 157 -67. 4. Walters et al. Sleep 2009; 32: 589 -97.
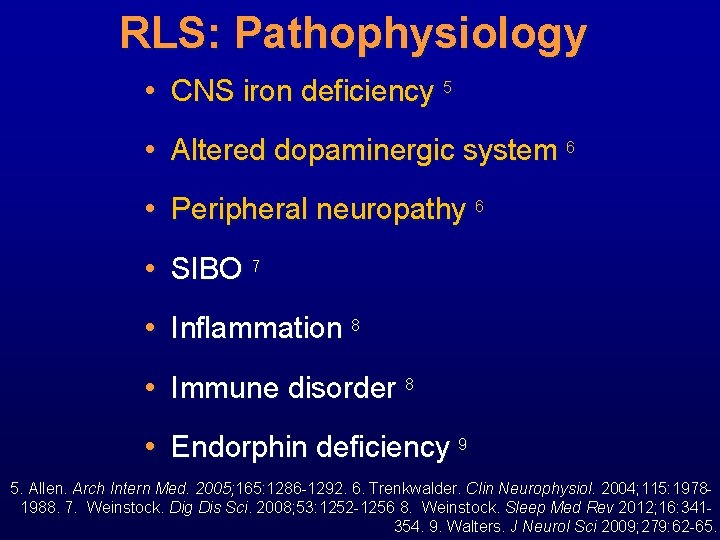
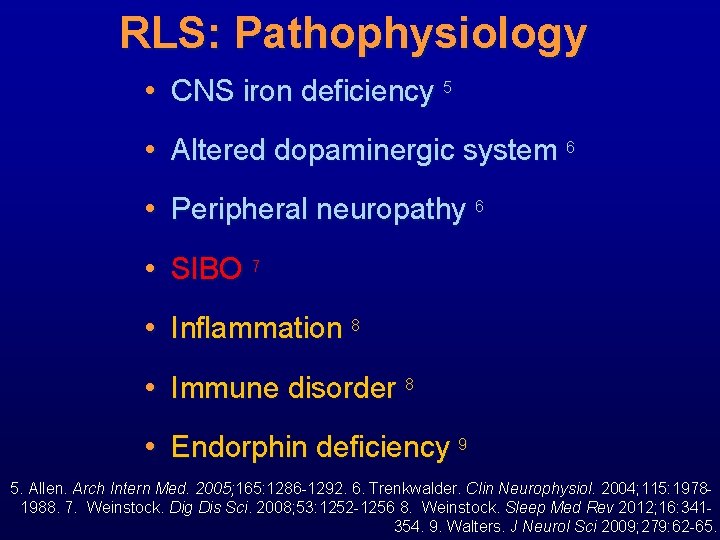
RLS: Pathophysiology • CNS iron deficiency 5 • Altered dopaminergic system 6 • Peripheral neuropathy 6 • SIBO 7 • Inflammation 8 • Immune disorder 8 • Endorphin deficiency 9 5. Allen. Arch Intern Med. 2005; 165: 1286 -1292. 6. Trenkwalder. Clin Neurophysiol. 2004; 115: 19781988. 7. Weinstock. Dig Dis Sci. 2008; 53: 1252 -1256 8. Weinstock. Sleep Med Rev 2012; 16: 341354. 9. Walters. J Neurol Sci 2009; 279: 62 -65.
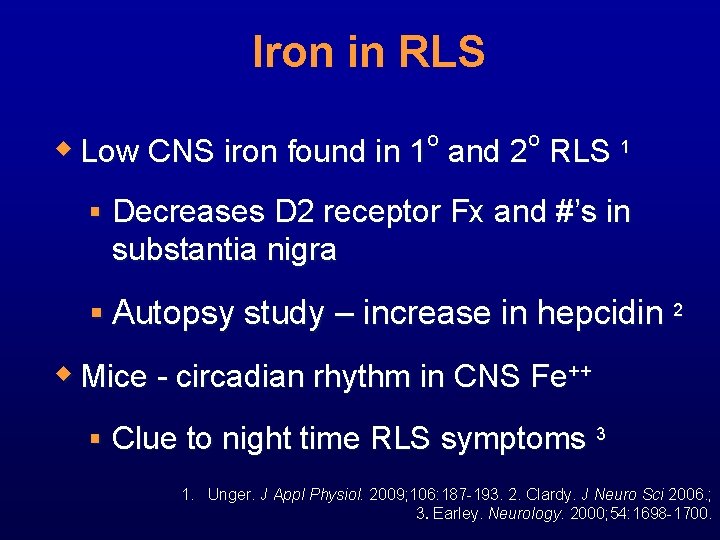
Iron in RLS o o w Low CNS iron found in 1 and 2 RLS 1 § Decreases D 2 receptor Fx and #’s in substantia nigra § Autopsy study – increase in hepcidin 2 w Mice - circadian rhythm in CNS Fe++ § Clue to night time RLS symptoms 3 1. Unger. J Appl Physiol. 2009; 106: 187 -193. 2. Clardy. J Neuro Sci 2006. ; 3. Earley. Neurology. 2000; 54: 1698 -1700.
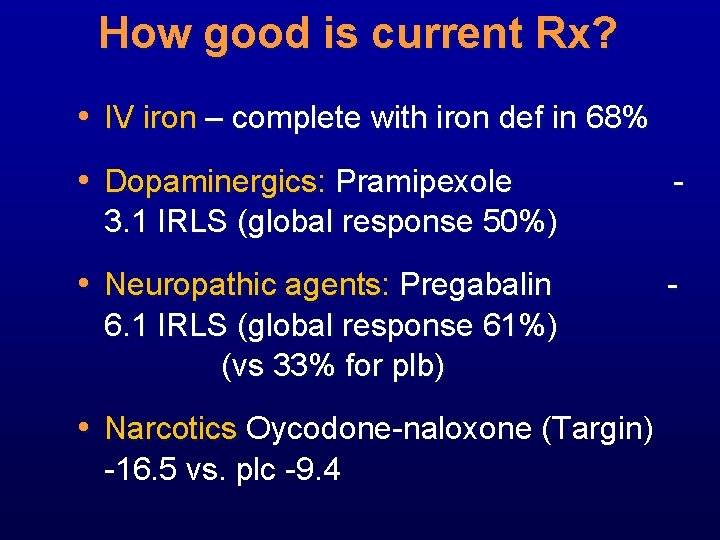
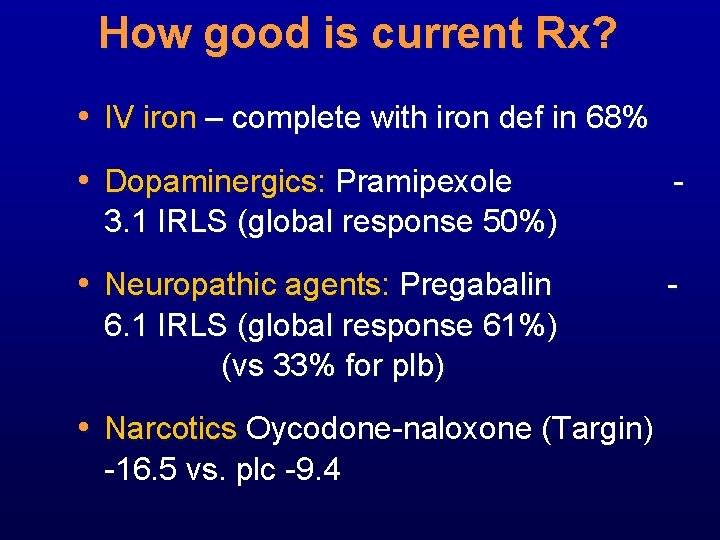
How good is current Rx? • IV iron – complete with iron def in 68% • Dopaminergics: Pramipexole - 3. 1 IRLS (global response 50%) • Neuropathic agents: Pregabalin 6. 1 IRLS (global response 61%) (vs 33% for plb) • Narcotics Oycodone-naloxone (Targin) -16. 5 vs. plc -9. 4 -
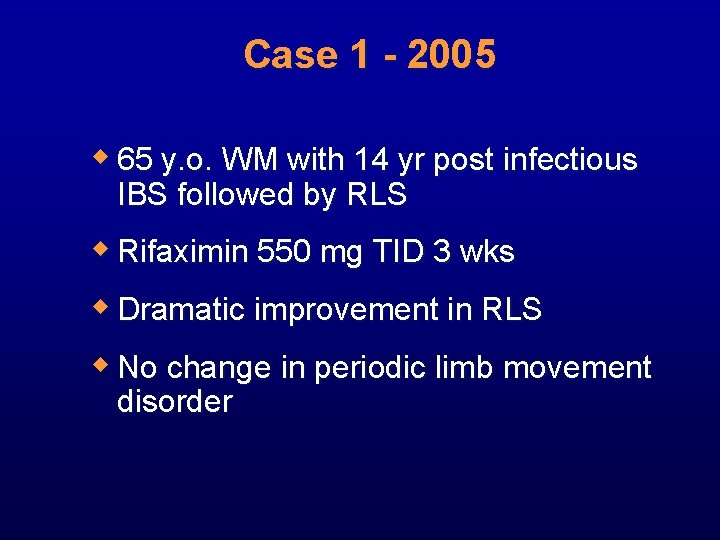
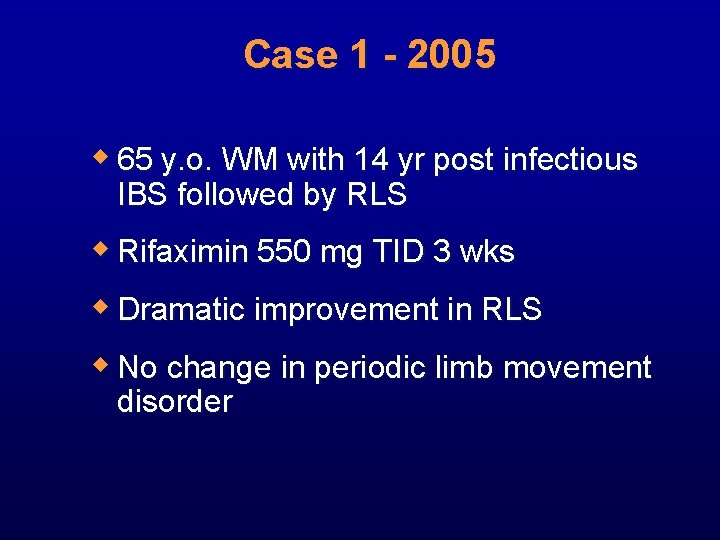
Case 1 - 2005 w 65 y. o. WM with 14 yr post infectious IBS followed by RLS w Rifaximin 550 mg TID 3 wks w Dramatic improvement in RLS w No change in periodic limb movement disorder
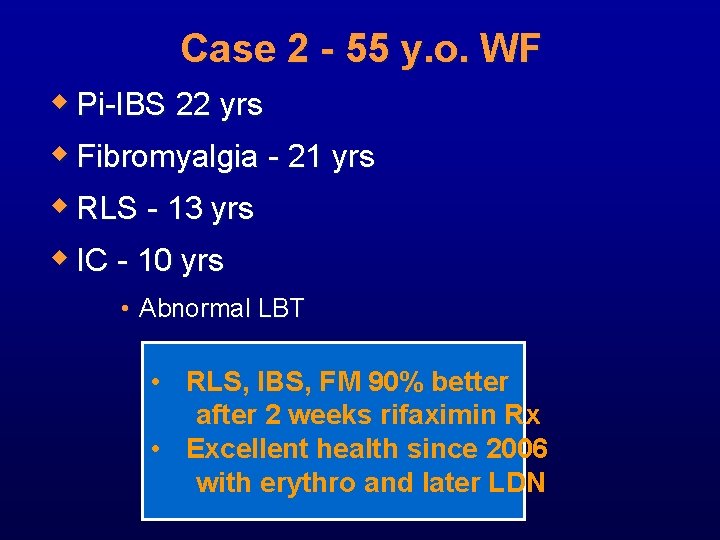
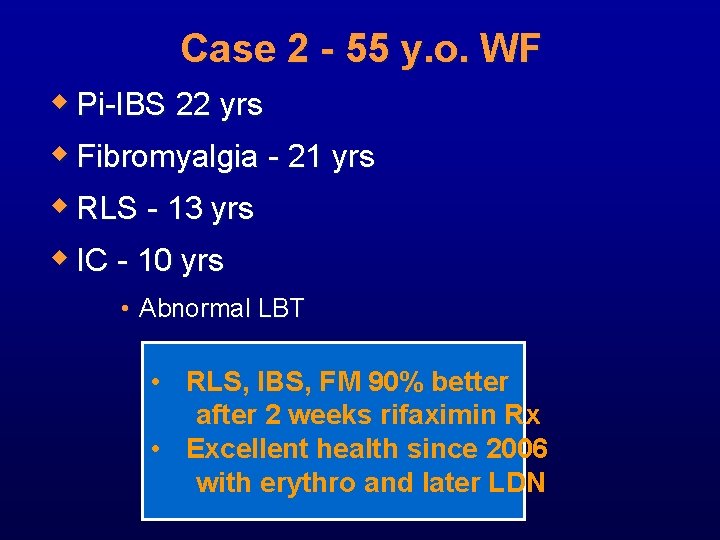
Case 2 - 55 y. o. WF w Pi-IBS 22 yrs w Fibromyalgia - 21 yrs w RLS - 13 yrs w IC - 10 yrs • Abnormal LBT • RLS, IBS, FM 90% better after 2 weeks rifaximin Rx • Excellent health since 2006 with erythro and later LDN
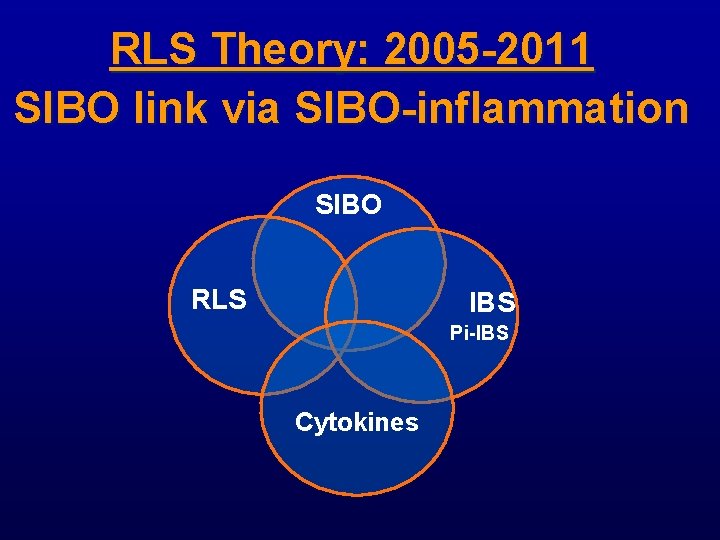
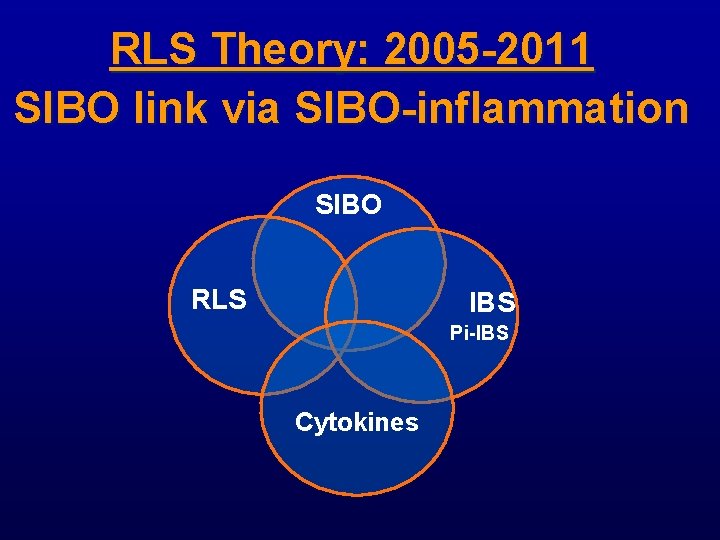
RLS Theory: 2005 -2011 SIBO link via SIBO-inflammation SIBO RLS IBS Pi-IBS Cytokines
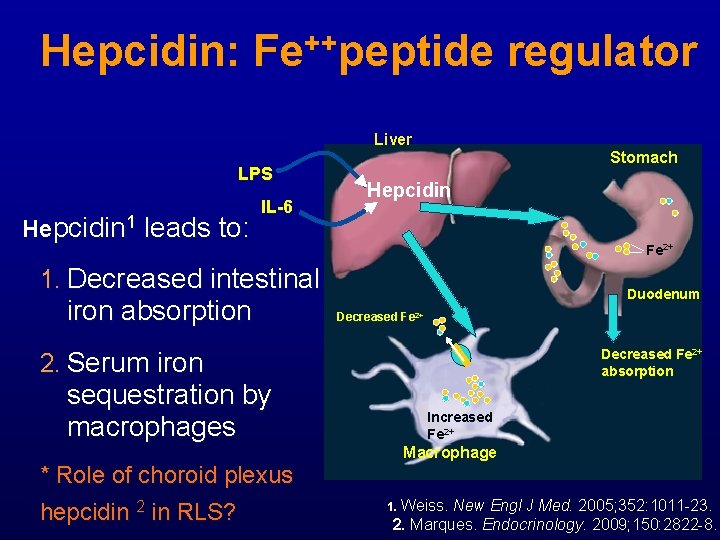
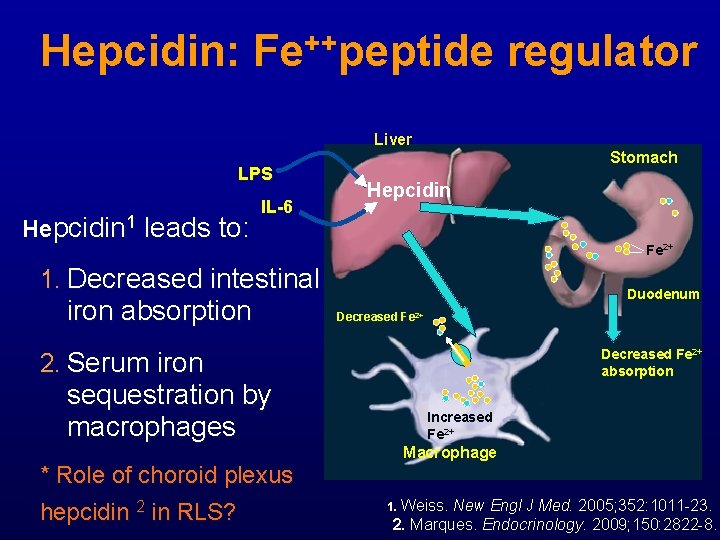
Hepcidin: Fe++peptide regulator Liver LPS Hepcidin 1 leads to: IL-6 Stomach Hepcidin Fe 2+ 1. Decreased intestinal iron absorption Duodenum Decreased Fe 2+ 2. Serum iron sequestration by macrophages Decreased Fe 2+ absorption Increased Fe 2+ Macrophage * Role of choroid plexus hepcidin 2 in RLS? 1. Weiss. New Engl J Med. 2005; 352: 1011 -23. 2. Marques. Endocrinology. 2009; 150: 2822 -8.
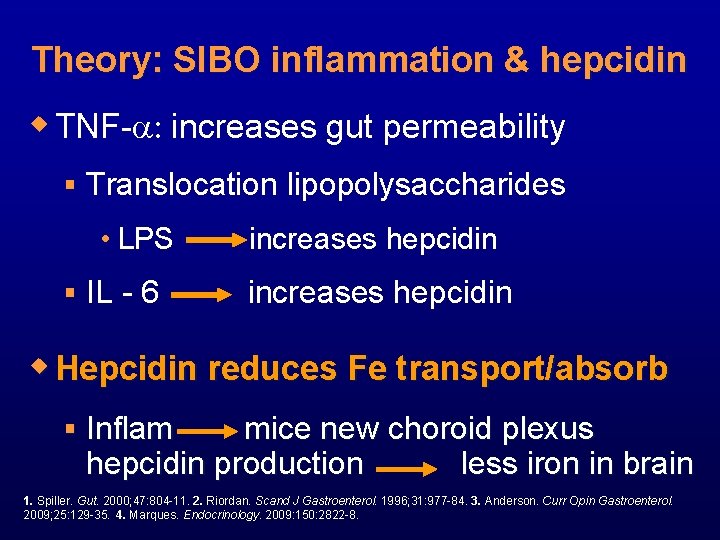
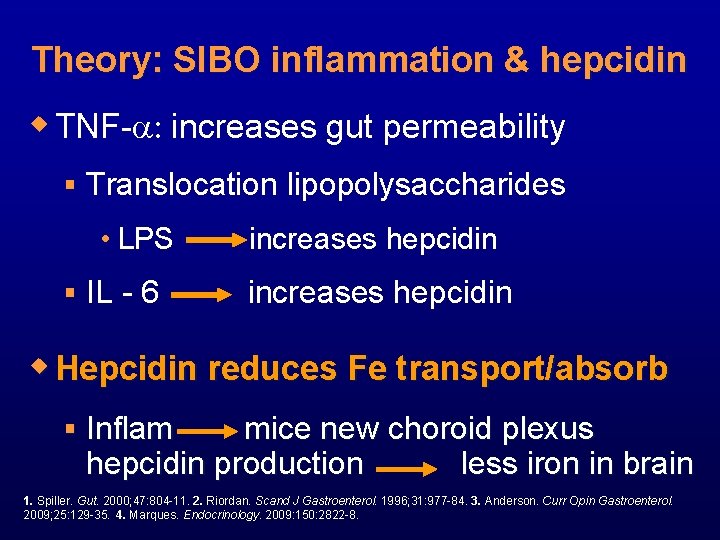
Theory: SIBO inflammation & hepcidin w TNF-a: increases gut permeability § Translocation lipopolysaccharides • LPS § IL - 6 increases hepcidin w Hepcidin reduces Fe transport/absorb § Inflam mice new choroid plexus hepcidin production less iron in brain 1. Spiller. Gut. 2000; 47: 804 -11. 2. Riordan. Scand J Gastroenterol. 1996; 31: 977 -84. 3. Anderson. Curr Opin Gastroenterol. 2009; 25: 129 -35. 4. Marques. Endocrinology. 2009: 150: 2822 -8.
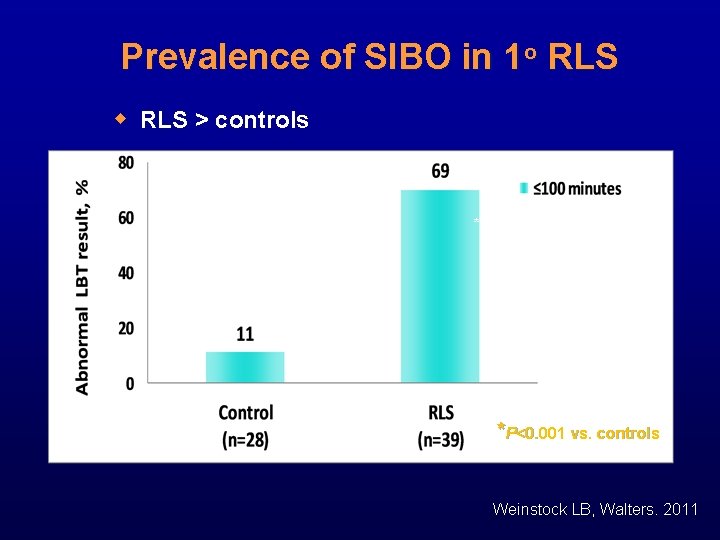
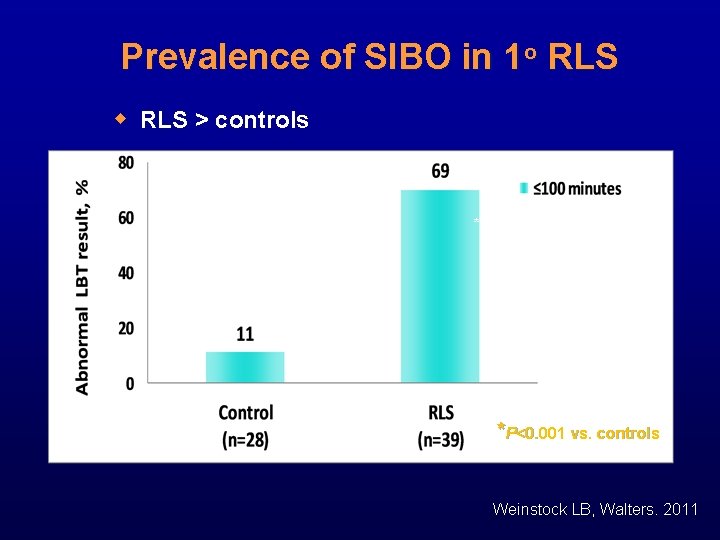
Prevalence of SIBO in 1 o RLS w RLS > controls * *P<0. 001 vs. controls Weinstock LB, Walters. 2011
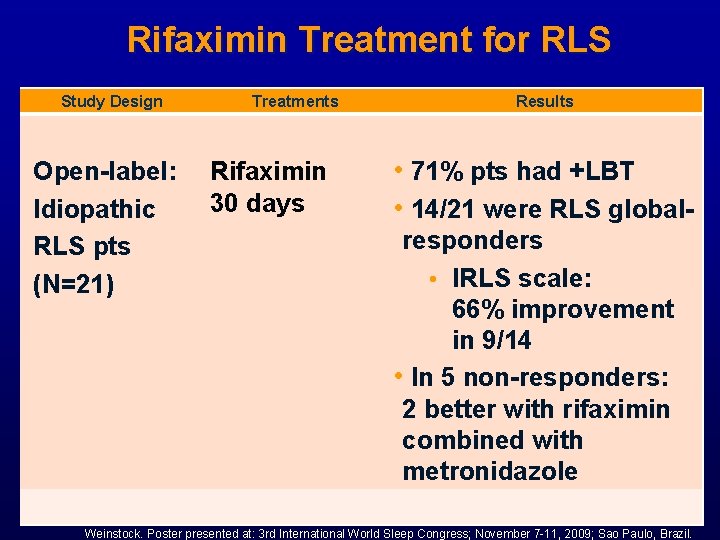
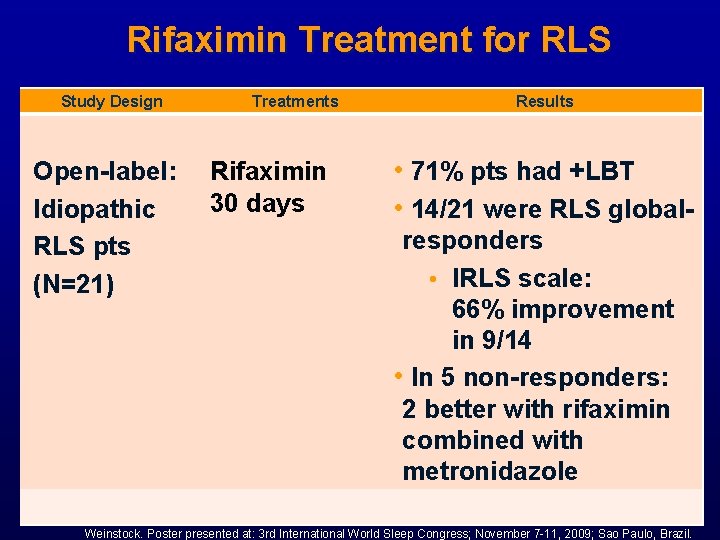
Rifaximin Treatment for RLS Study Design Open-label: Idiopathic RLS pts (N=21) Treatments Results Rifaximin • 71% pts had +LBT 30 days • 14/21 were RLS globalresponders • IRLS scale: 66% improvement in 9/14 • In 5 non-responders: 2 better with rifaximin combined with metronidazole Weinstock. Poster presented at: 3 rd International World Sleep Congress; November 7 -11, 2009; Sao Paulo, Brazil.
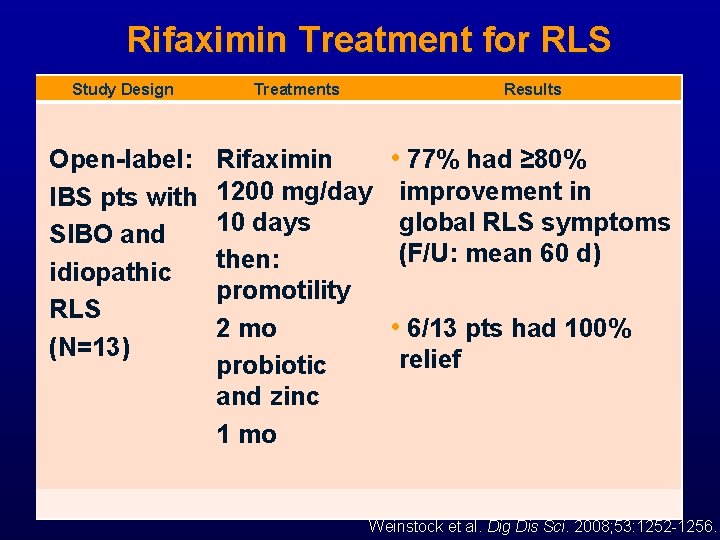
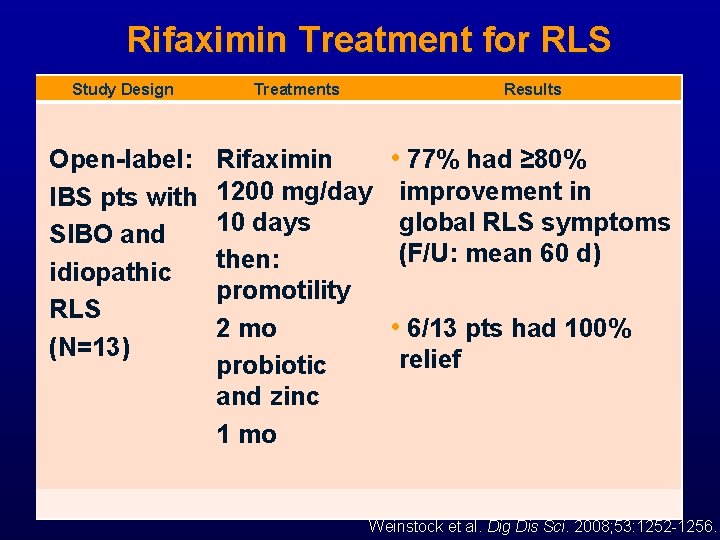
Rifaximin Treatment for RLS Study Design Treatments Results Open-label: Rifaximin • 77% had ≥ 80% IBS pts with 1200 mg/day improvement in 10 days global RLS symptoms SIBO and (F/U: mean 60 d) then: idiopathic promotility RLS 2 mo • 6/13 pts had 100% (N=13) probiotic relief and zinc 1 mo Weinstock et al. Dig Dis Sci. 2008; 53: 1252 -1256.
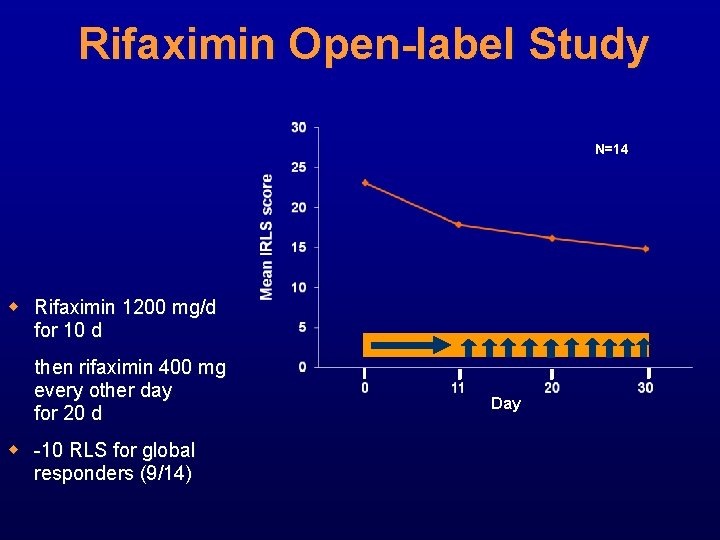
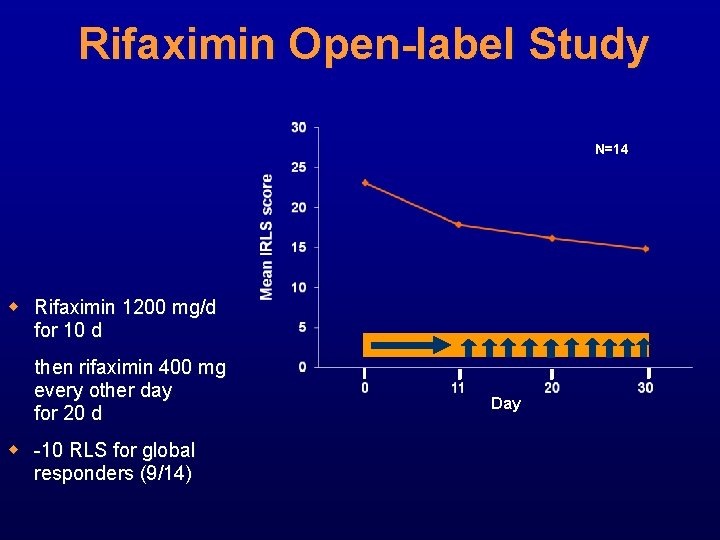
Rifaximin Open-label Study N=14 w Rifaximin 1200 mg/d for 10 d then rifaximin 400 mg every other day for 20 d w -10 RLS for global responders (9/14) Day
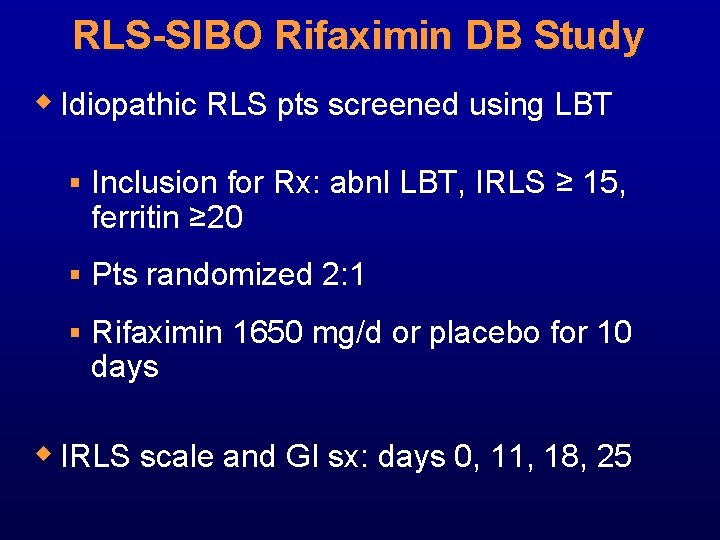
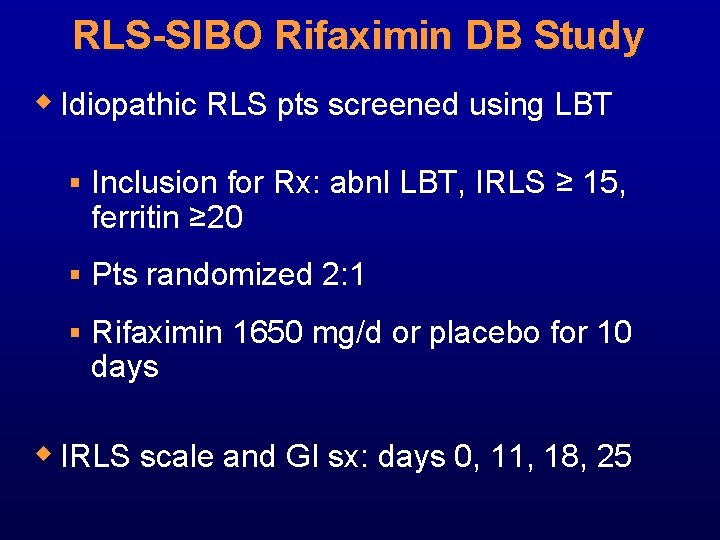
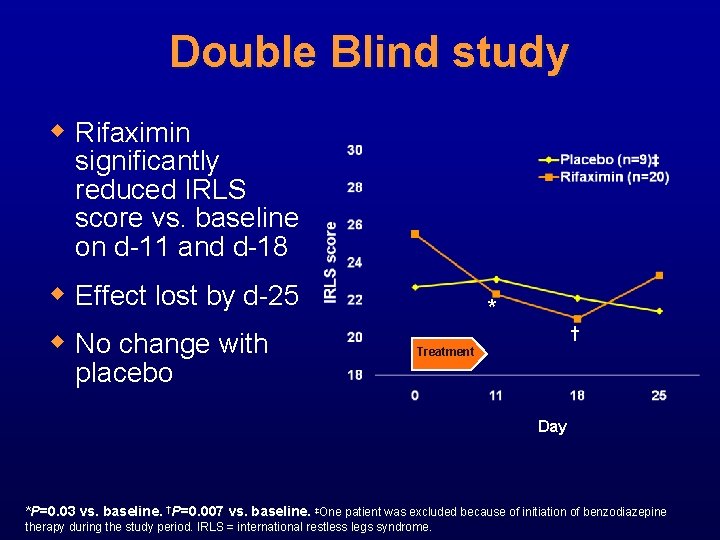
RLS-SIBO Rifaximin DB Study w Idiopathic RLS pts screened using LBT § Inclusion for Rx: abnl LBT, IRLS ≥ 15, ferritin ≥ 20 § Pts randomized 2: 1 § Rifaximin 1650 mg/d or placebo for 10 days w IRLS scale and GI sx: days 0, 11, 18, 25
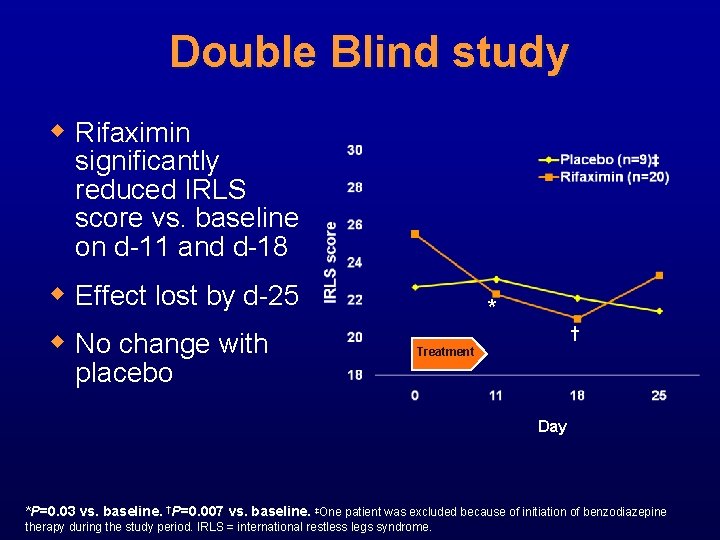
Double Blind study w Rifaximin significantly reduced IRLS score vs. baseline on d-11 and d-18 w Effect lost by d-25 w No change with placebo * † Treatment Day *P=0. 03 vs. baseline. †P=0. 007 vs. baseline. ‡One patient was excluded because of initiation of benzodiazepine therapy during the study period. IRLS = international restless legs syndrome.
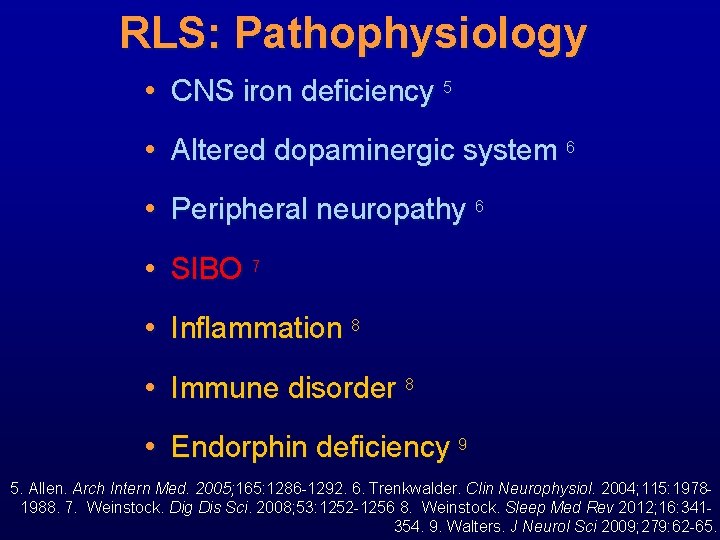
RLS: Pathophysiology • CNS iron deficiency 5 • Altered dopaminergic system 6 • Peripheral neuropathy 6 • SIBO 7 • Inflammation 8 • Immune disorder 8 • Endorphin deficiency 9 5. Allen. Arch Intern Med. 2005; 165: 1286 -1292. 6. Trenkwalder. Clin Neurophysiol. 2004; 115: 19781988. 7. Weinstock. Dig Dis Sci. 2008; 53: 1252 -1256 8. Weinstock. Sleep Med Rev 2012; 16: 341354. 9. Walters. J Neurol Sci 2009; 279: 62 -65.
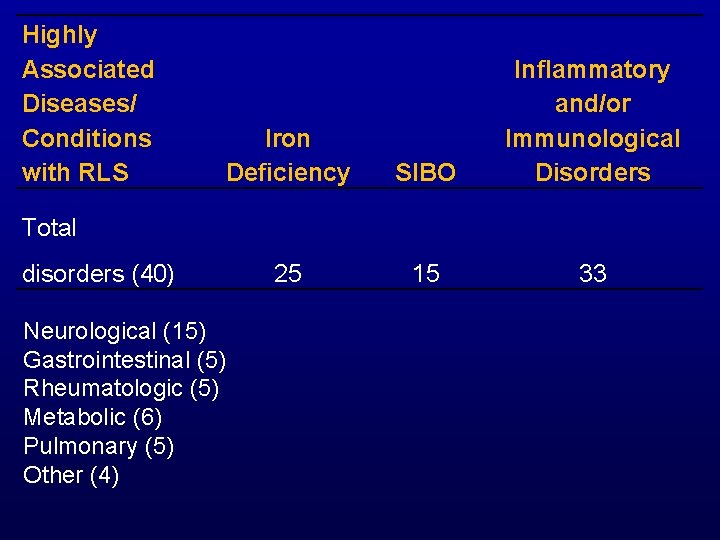
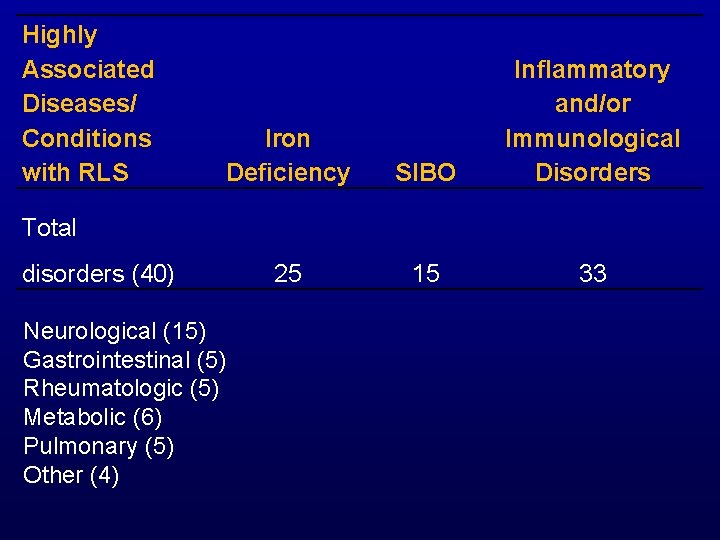
Highly Associated Diseases/ Conditions with RLS Iron Deficiency SIBO Inflammatory and/or Immunological Disorders 25 15 33 Total disorders (40) Neurological (15) Gastrointestinal (5) Rheumatologic (5) Metabolic (6) Pulmonary (5) Other (4)
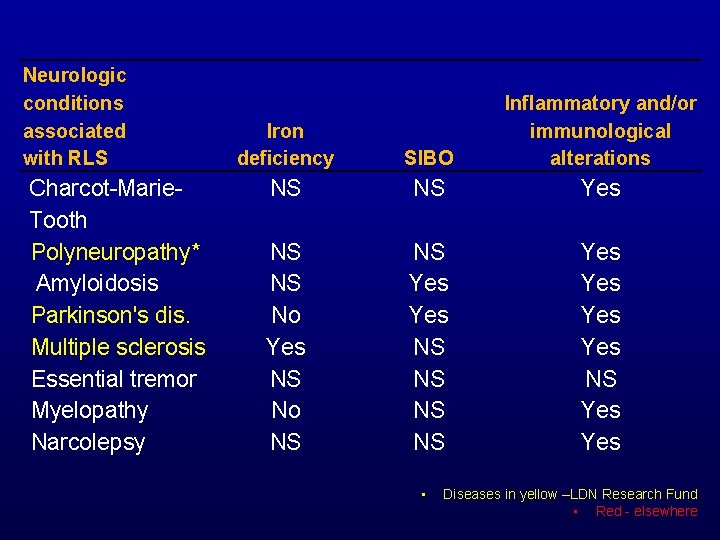
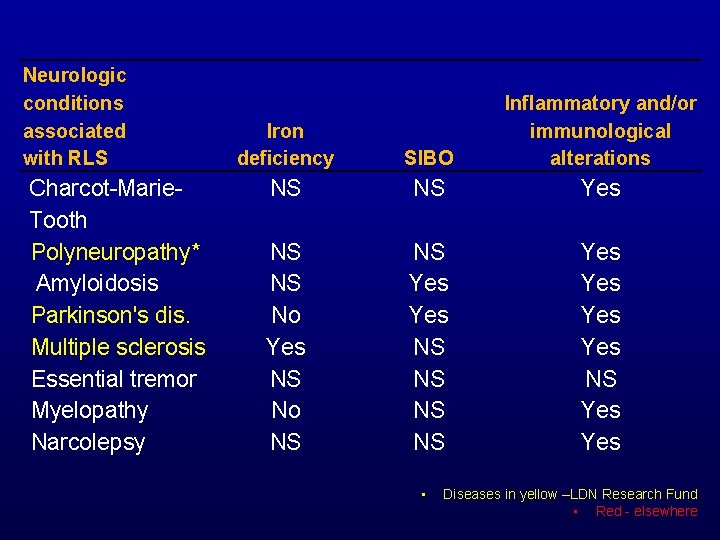
Neurologic conditions associated with RLS Charcot-Marie. Tooth Polyneuropathy* Amyloidosis Parkinson's dis. Multiple sclerosis Essential tremor Myelopathy Narcolepsy Iron deficiency SIBO Inflammatory and/or immunological alterations NS NS Yes NS NS No Yes NS No NS NS Yes Yes NS Yes • Diseases in yellow –LDN Research Fund • Red - elsewhere
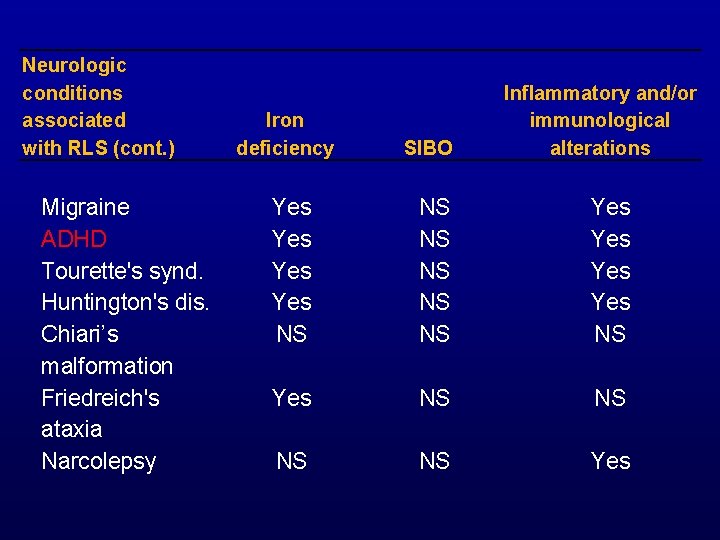
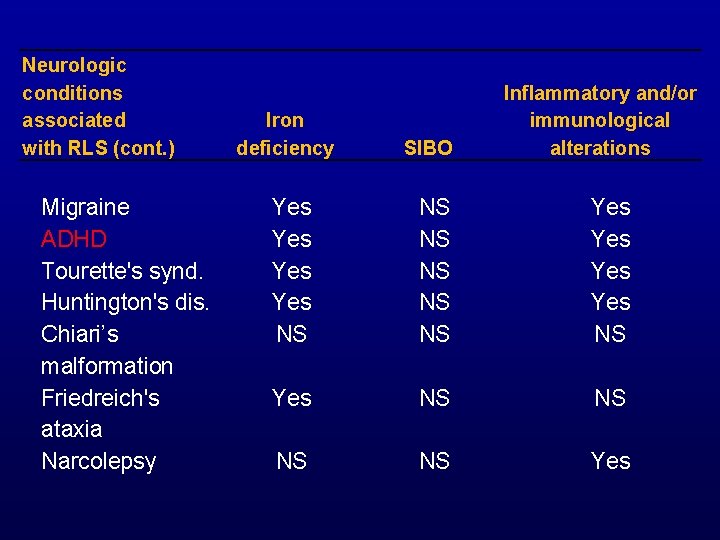
Neurologic conditions associated with RLS (cont. ) Migraine ADHD Tourette's synd. Huntington's dis. Chiari’s malformation Friedreich's ataxia Narcolepsy Iron deficiency SIBO Inflammatory and/or immunological alterations Yes Yes NS NS NS Yes Yes NS NS Yes
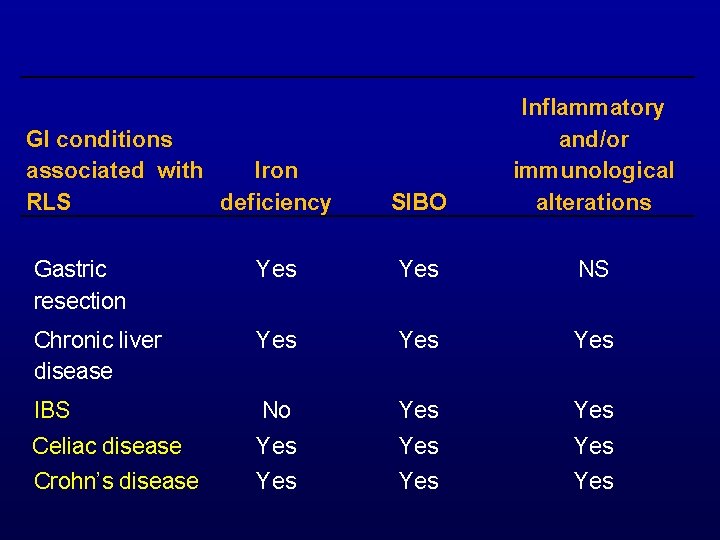
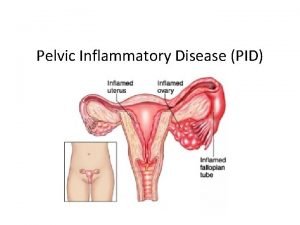
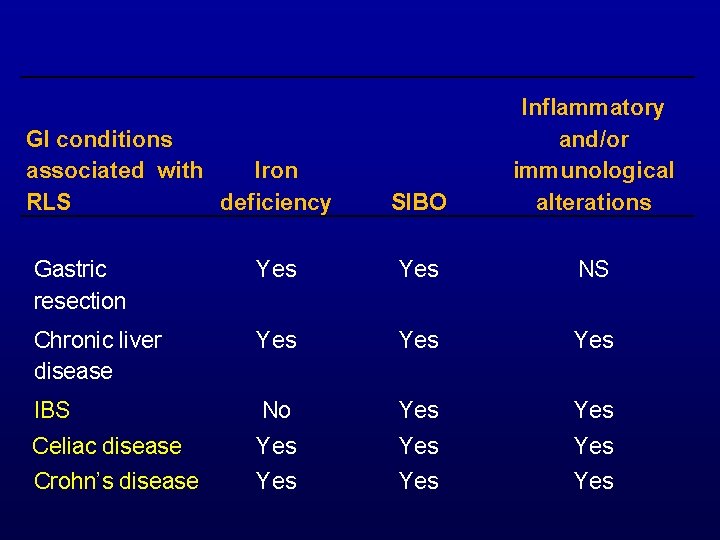
GI conditions associated with Iron RLS deficiency SIBO Inflammatory and/or immunological alterations Gastric resection Yes NS Chronic liver disease Yes Yes IBS No Yes Celiac disease Yes Yes Crohn’s disease Yes Yes
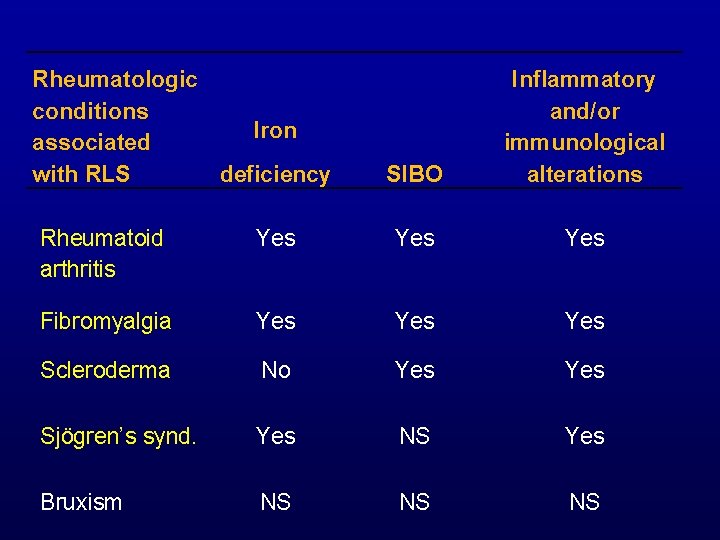
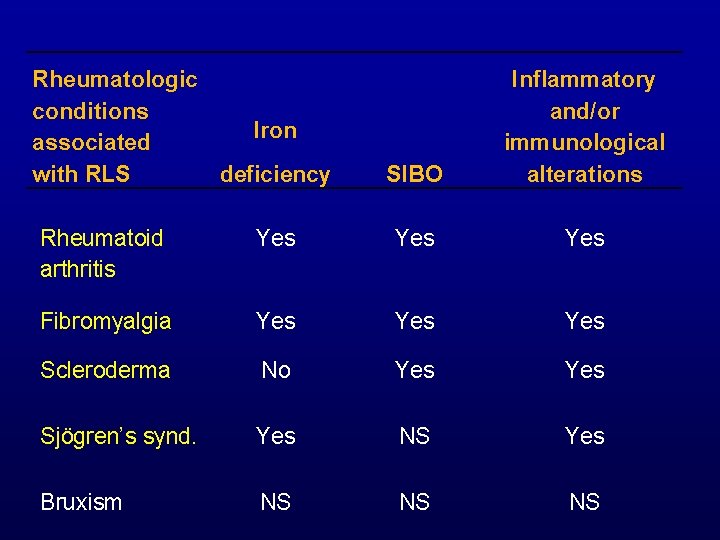
Rheumatologic conditions Iron associated with RLS deficiency Rheumatoid Yes arthritis SIBO Inflammatory and/or immunological alterations Yes Fibromyalgia Yes Yes Scleroderma No Yes Sjögren’s synd. Yes NS Yes Bruxism NS NS NS
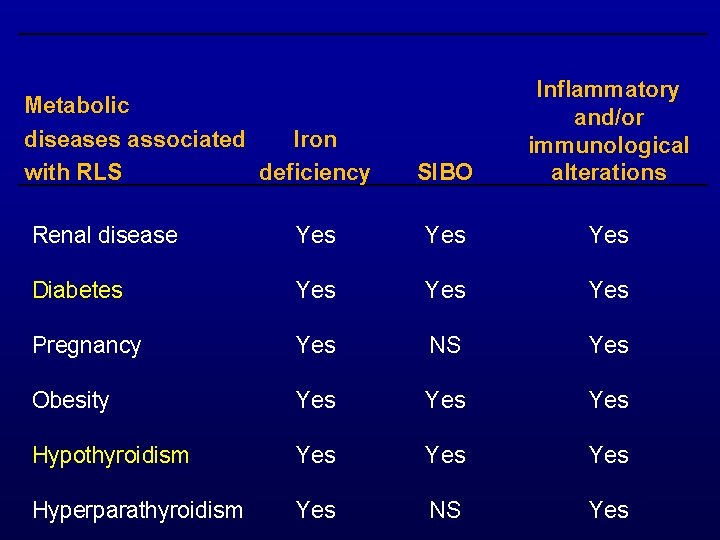
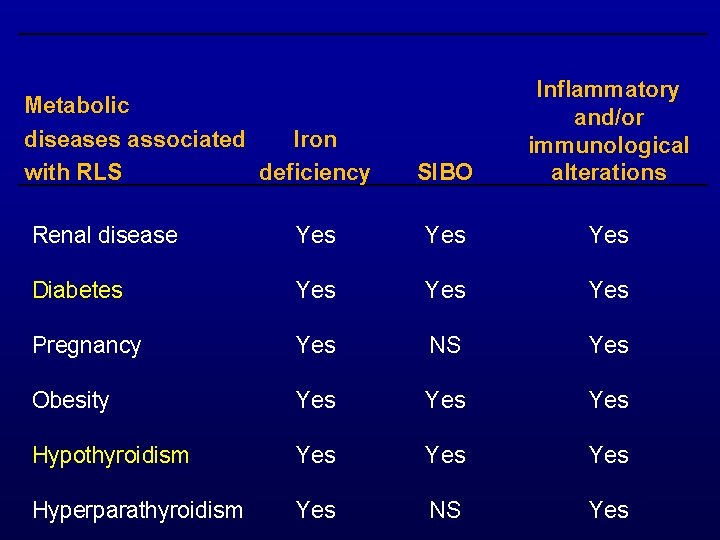
Metabolic diseases associated Iron with RLS deficiency SIBO Inflammatory and/or immunological alterations Renal disease Yes Yes Diabetes Yes Yes Pregnancy Yes NS Yes Obesity Yes Yes Hypothyroidism Yes Yes Hyperparathyroidism Yes NS Yes
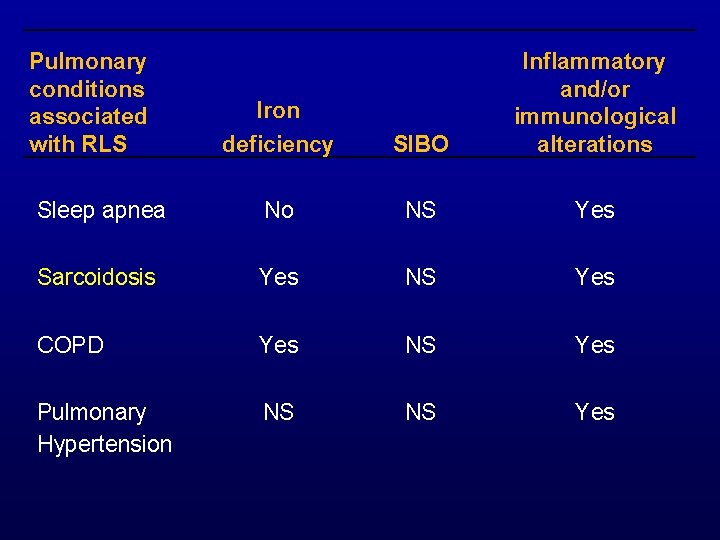
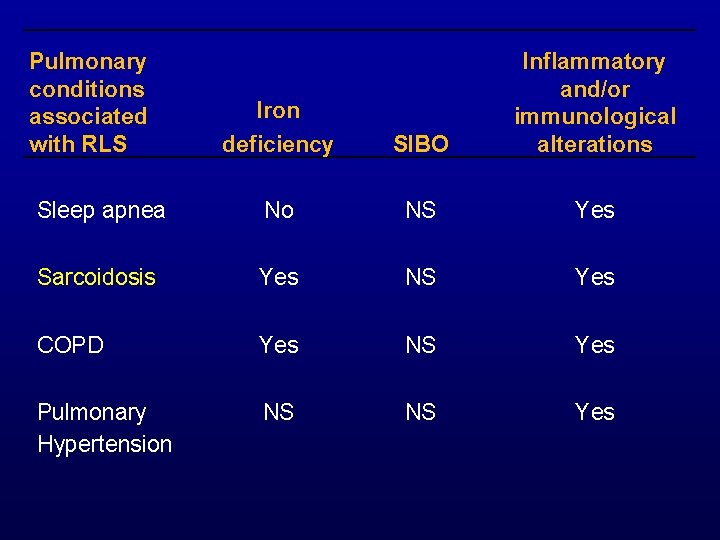
Pulmonary conditions associated with RLS Iron deficiency SIBO Inflammatory and/or immunological alterations Sleep apnea No NS Yes Sarcoidosis Yes NS Yes COPD Yes NS Yes Pulmonary Hypertension NS NS Yes
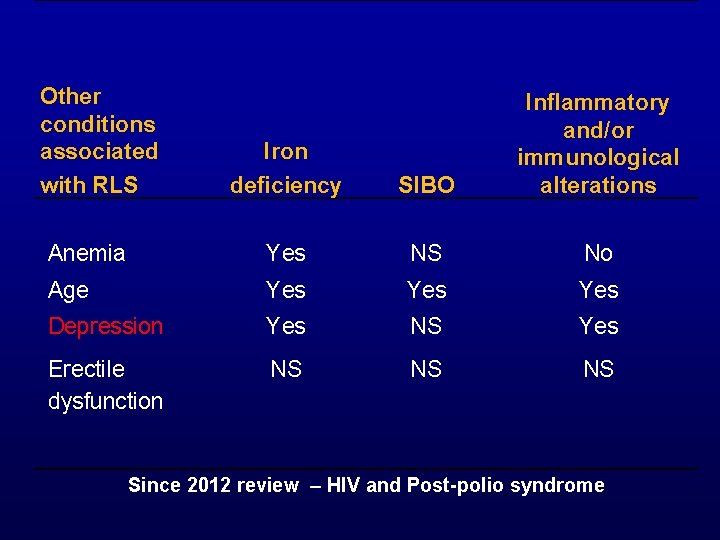
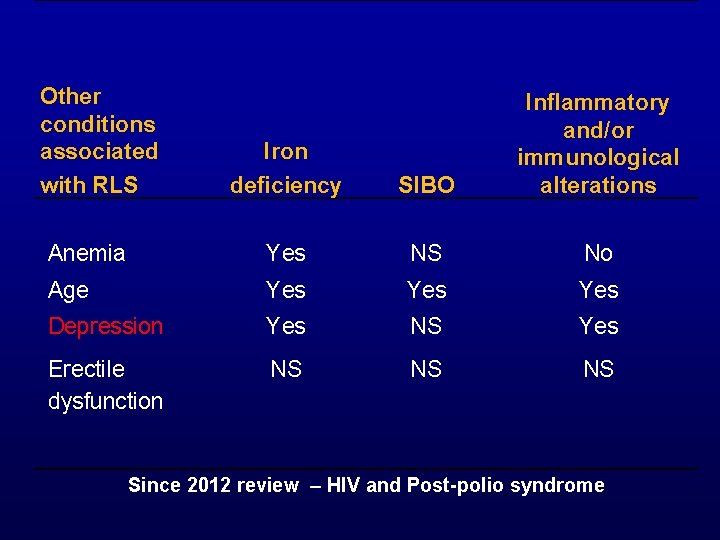
Other conditions associated with RLS Iron deficiency SIBO Inflammatory and/or immunological alterations Anemia Yes NS No Age Yes Yes Depression Yes NS Yes Erectile dysfunction NS NS NS Since 2012 review – HIV and Post-polio syndrome
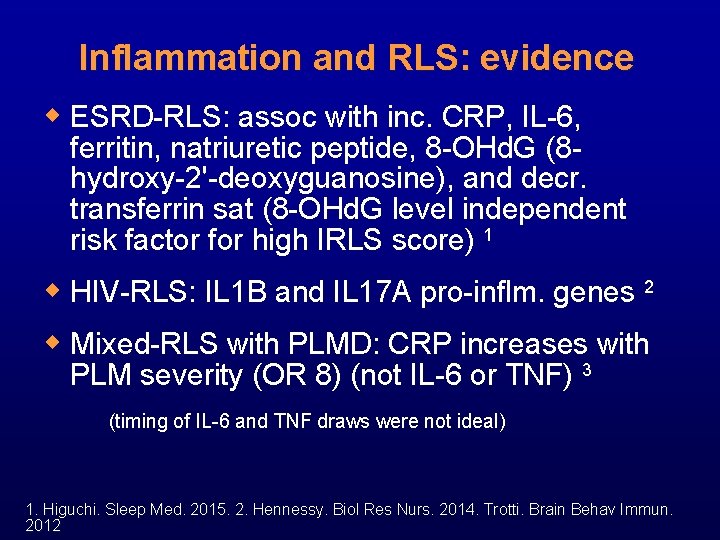
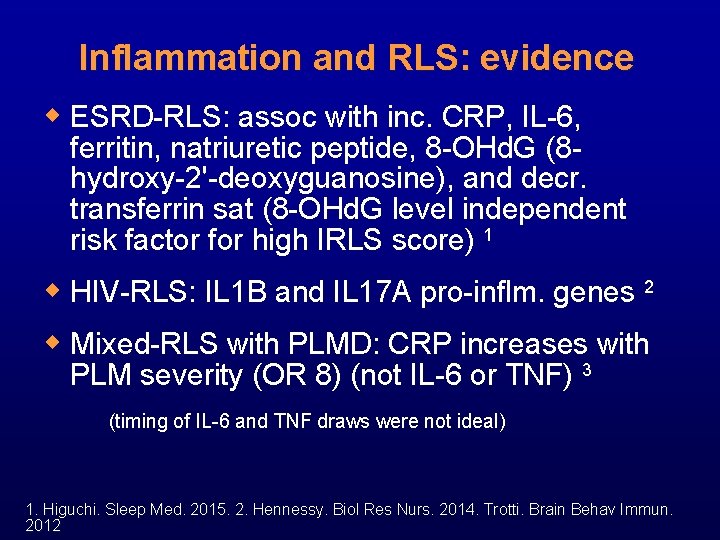
Inflammation and RLS: evidence w ESRD-RLS: assoc with inc. CRP, IL-6, ferritin, natriuretic peptide, 8 -OHd. G (8 hydroxy-2'-deoxyguanosine), and decr. transferrin sat (8 -OHd. G level independent risk factor for high IRLS score) 1 w HIV-RLS: IL 1 B and IL 17 A pro-inflm. genes 2 w Mixed-RLS with PLMD: CRP increases with PLM severity (OR 8) (not IL-6 or TNF) 3 (timing of IL-6 and TNF draws were not ideal) 1. Higuchi. Sleep Med. 2015. 2. Hennessy. Biol Res Nurs. 2014. Trotti. Brain Behav Immun. 2012
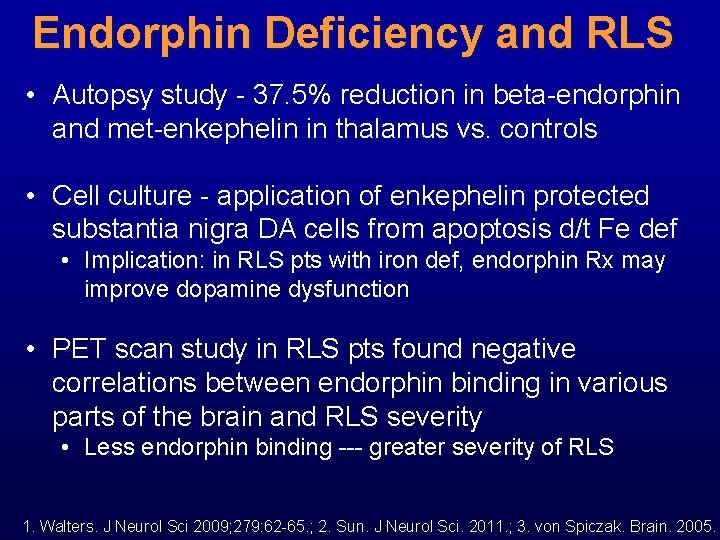
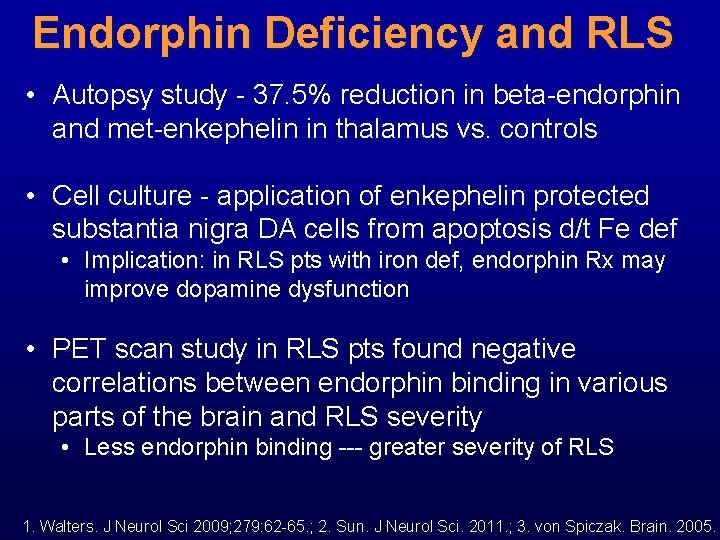
Endorphin Deficiency and RLS • Autopsy study - 37. 5% reduction in beta-endorphin and met-enkephelin in thalamus vs. controls • Cell culture - application of enkephelin protected substantia nigra DA cells from apoptosis d/t Fe def • Implication: in RLS pts with iron def, endorphin Rx may improve dopamine dysfunction • PET scan study in RLS pts found negative correlations between endorphin binding in various parts of the brain and RLS severity • Less endorphin binding --- greater severity of RLS 1. Walters. J Neurol Sci 2009; 279: 62 -65. ; 2. Sun. J Neurol Sci. 2011. ; 3. von Spiczak. Brain. 2005.
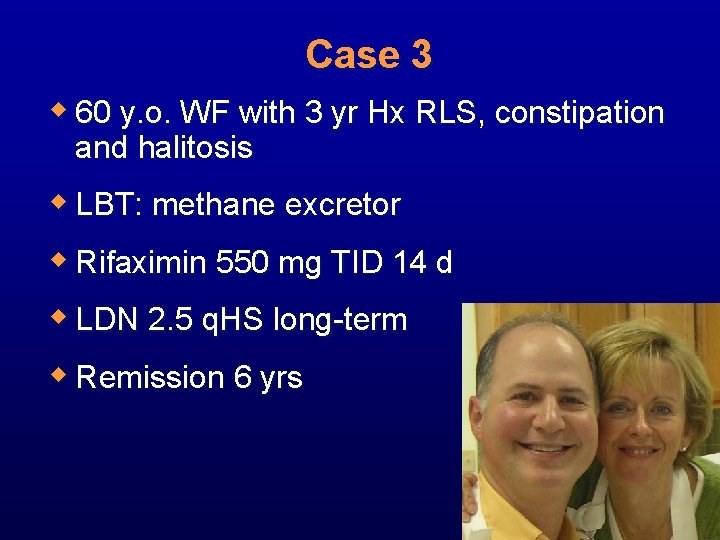
Case 3 w 60 y. o. WF with 3 yr Hx RLS, constipation and halitosis w LBT: methane excretor w Rifaximin 550 mg TID 14 d w LDN 2. 5 q. HS long-term w Remission 6 yrs
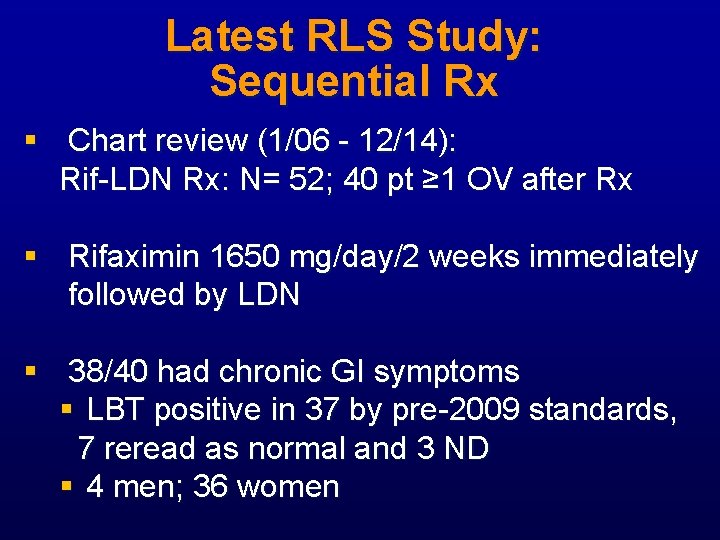
Latest RLS Study: Sequential Rx § Chart review (1/06 - 12/14): Rif-LDN Rx: N= 52; 40 pt ≥ 1 OV after Rx § Rifaximin 1650 mg/day/2 weeks immediately followed by LDN § 38/40 had chronic GI symptoms § LBT positive in 37 by pre-2009 standards, 7 reread as normal and 3 ND § 4 men; 36 women

Rifaximin-LDN Sequential Rx Pts (N= 40) Markedly Moderately Slightly better 21 5 Responders = 65% 3 No change 11
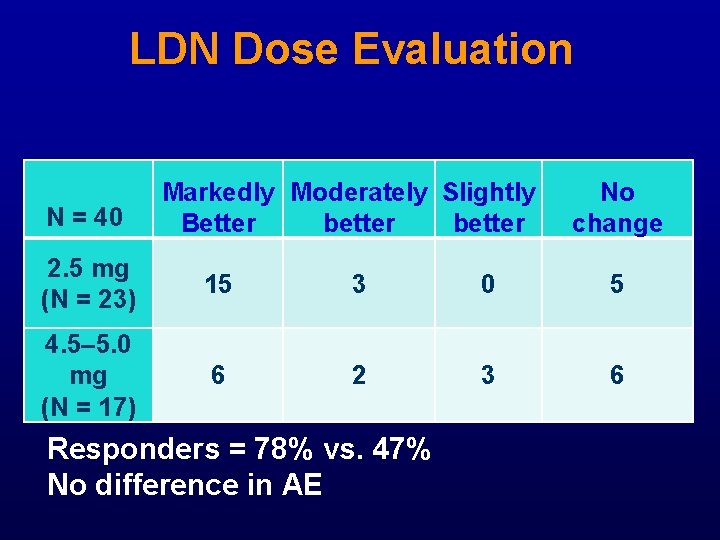
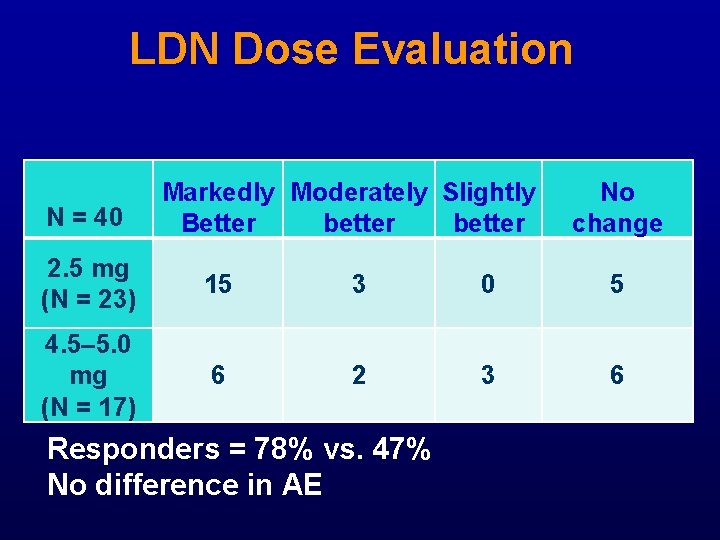
LDN Dose Evaluation N = 40 Markedly Moderately Slightly Better better No change 2. 5 mg (N = 23) 15 3 0 5 4. 5– 5. 0 mg (N = 17) 6 2 3 6 Responders = 78% vs. 47% No difference in AE
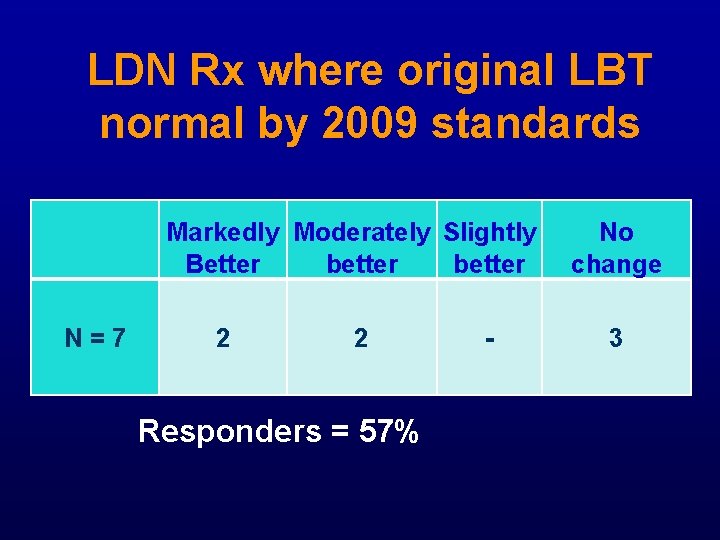
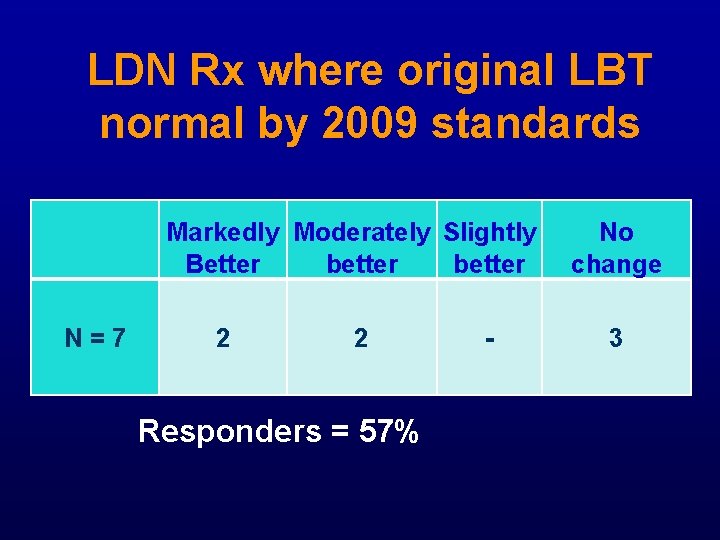
LDN Rx where original LBT normal by 2009 standards N = 7 Markedly Moderately Slightly Better better 2 2 Responders = 57% - No change 3
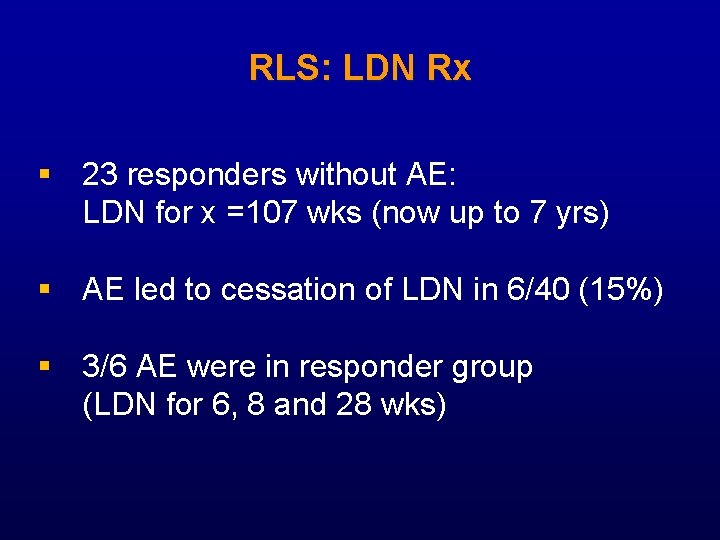
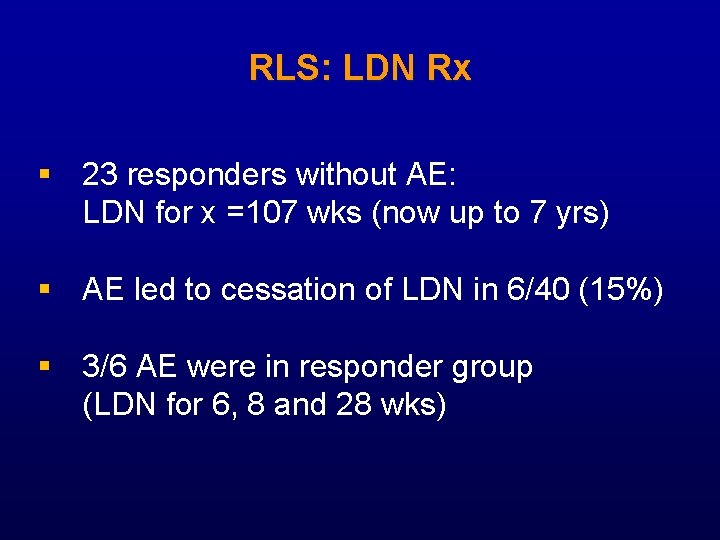
RLS: LDN Rx § 23 responders without AE: LDN for x =107 wks (now up to 7 yrs) § AE led to cessation of LDN in 6/40 (15%) § 3/6 AE were in responder group (LDN for 6, 8 and 28 wks)
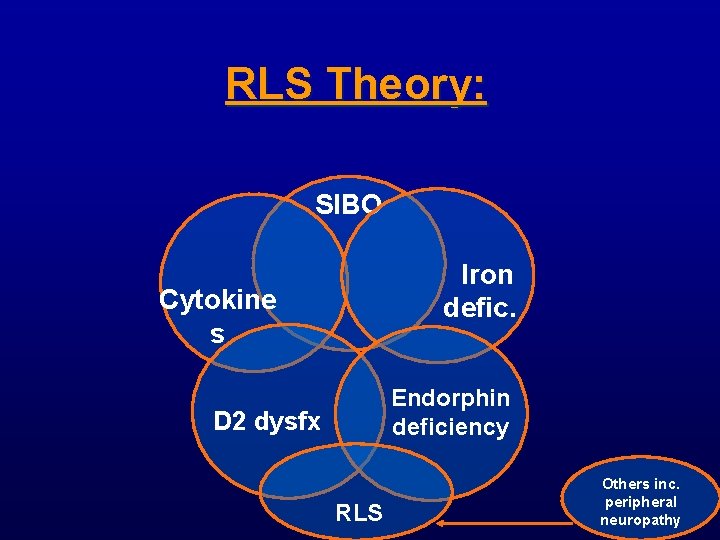
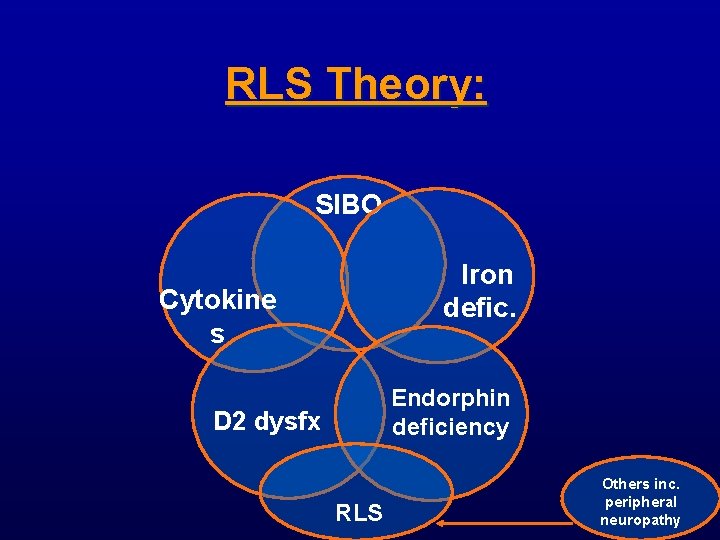
RLS Theory: SIBO Iron defic. Cytokine s Endorphin deficiency D 2 dysfx RLS Others inc. peripheral neuropathy
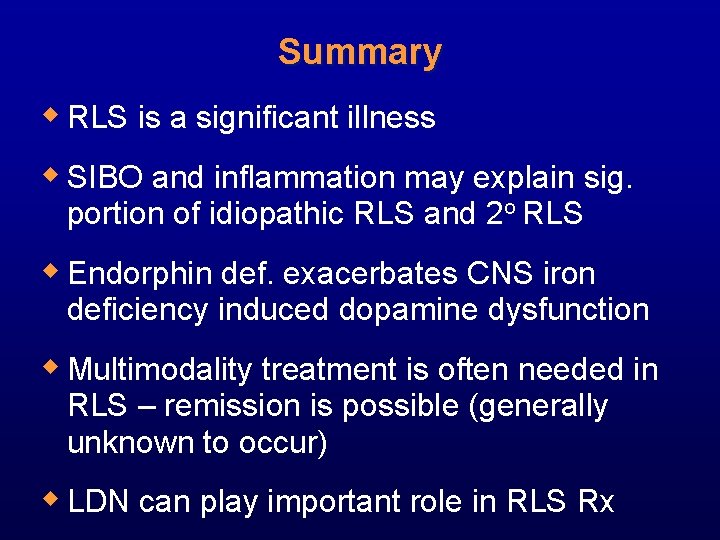
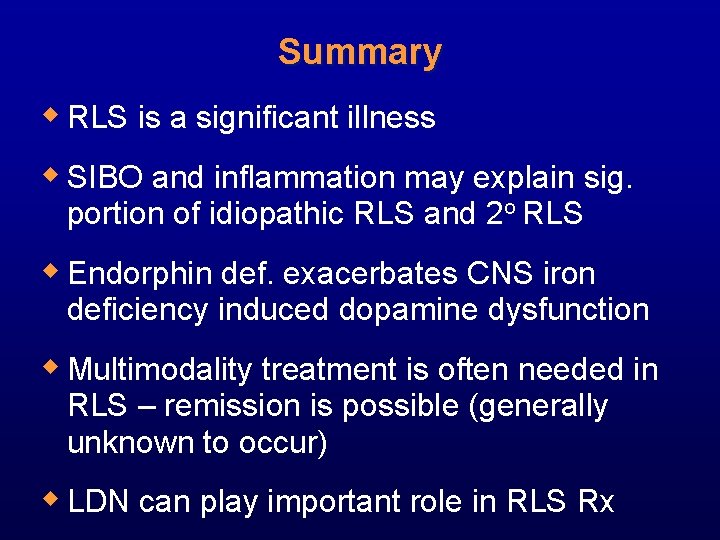
Summary w RLS is a significant illness w SIBO and inflammation may explain sig. portion of idiopathic RLS and 2 o RLS w Endorphin def. exacerbates CNS iron deficiency induced dopamine dysfunction w Multimodality treatment is often needed in RLS – remission is possible (generally unknown to occur) w LDN can play important role in RLS Rx
Back up slides
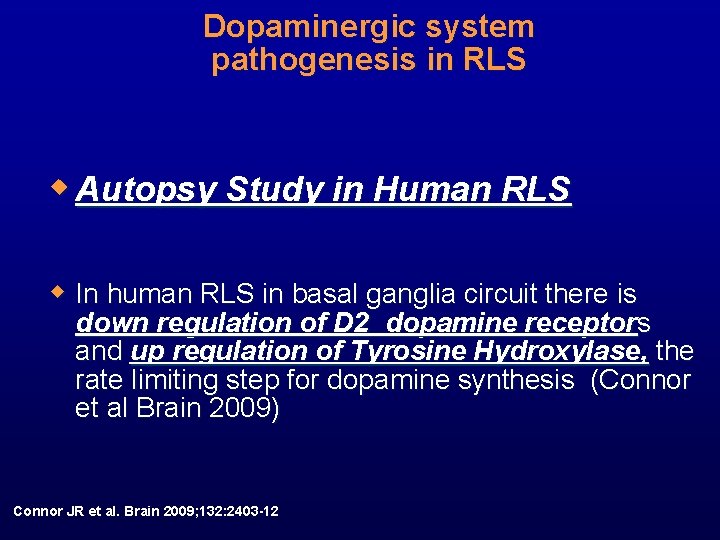
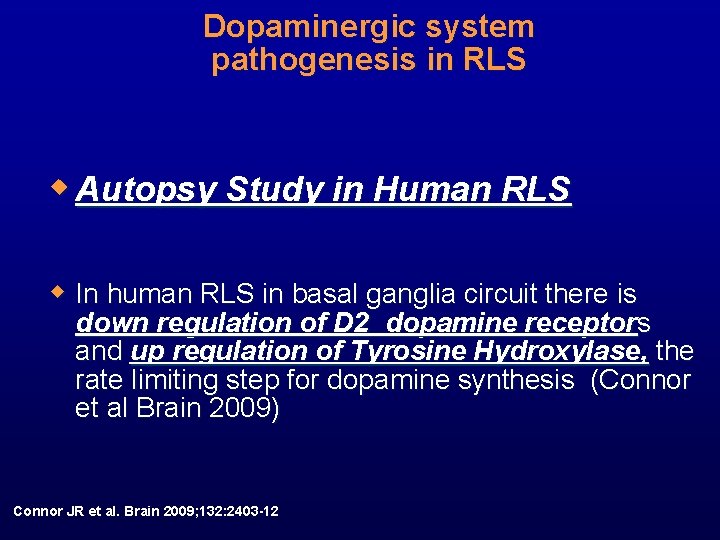
Dopaminergic system pathogenesis in RLS w Autopsy Study in Human RLS w In human RLS in basal ganglia circuit there is down regulation of D 2 dopamine receptors and up regulation of Tyrosine Hydroxylase, the rate limiting step for dopamine synthesis (Connor et al Brain 2009) Connor JR et al. Brain 2009; 132: 2403 -12
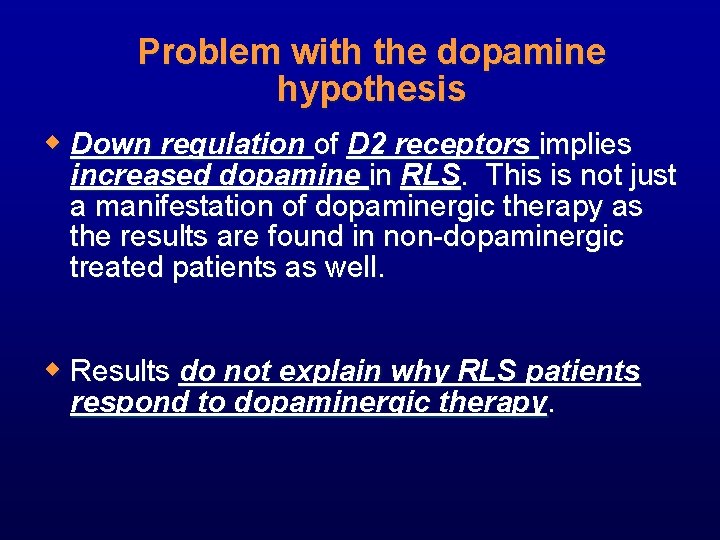
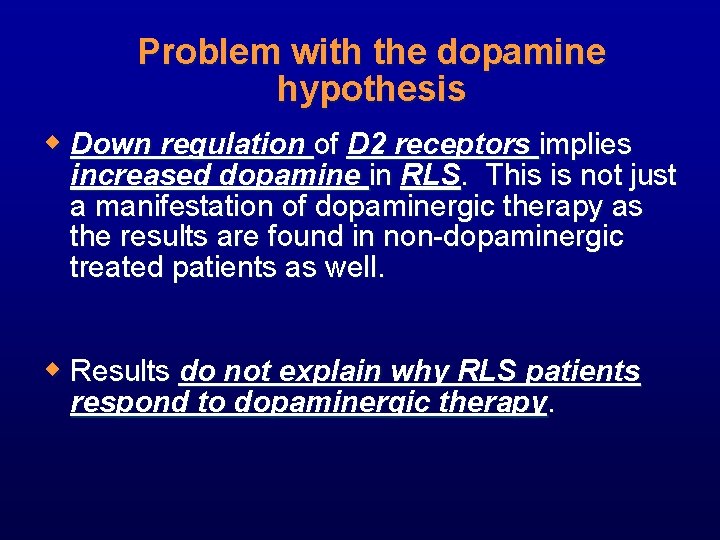
Problem with the dopamine hypothesis w Down regulation of D 2 receptors implies increased dopamine in RLS. This is not just a manifestation of dopaminergic therapy as the results are found in non-dopaminergic treated patients as well. w Results do not explain why RLS patients respond to dopaminergic therapy.
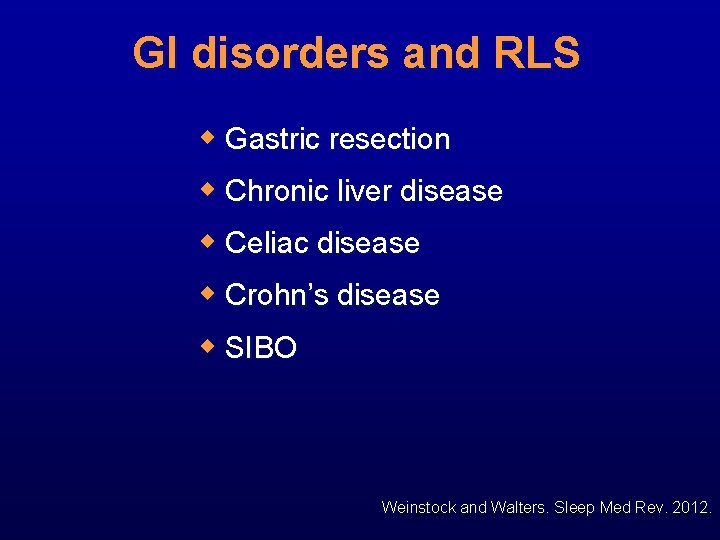
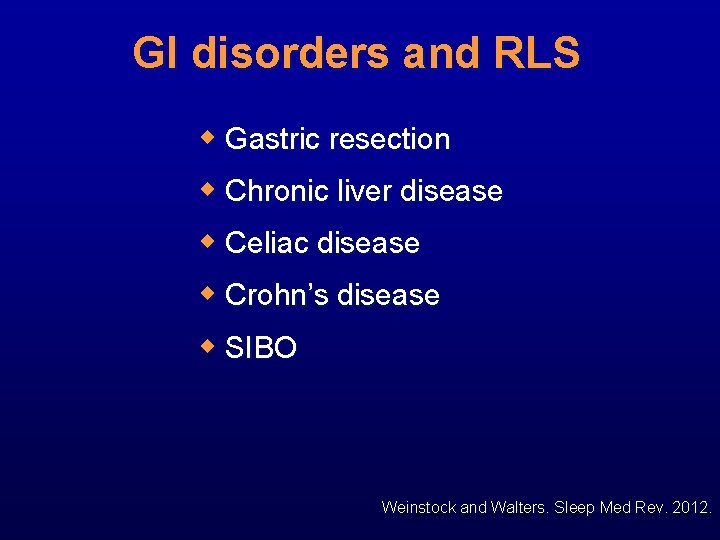
GI disorders and RLS w Gastric resection w Chronic liver disease w Celiac disease w Crohn’s disease w SIBO Weinstock and Walters. Sleep Med Rev. 2012.
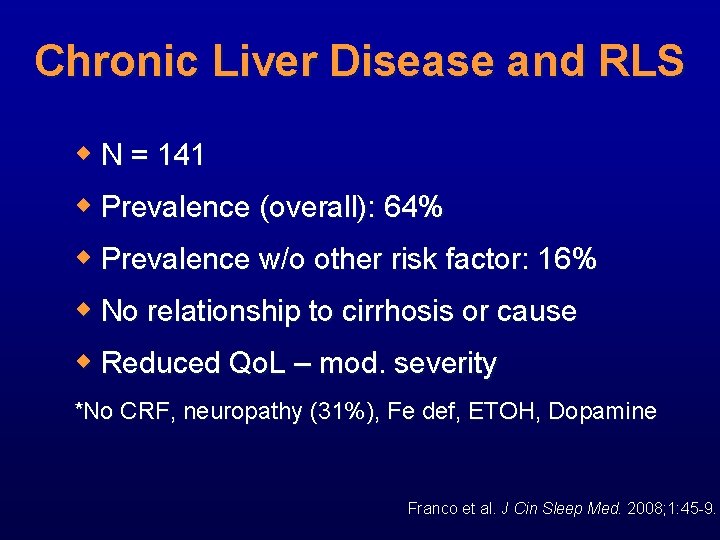
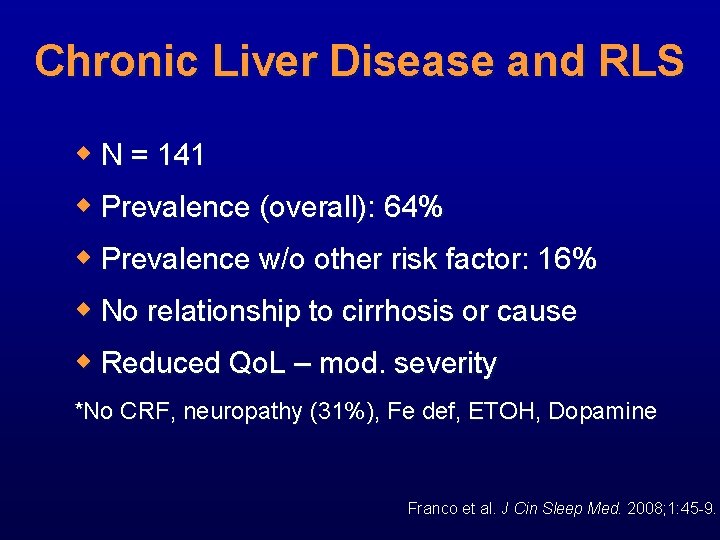
Chronic Liver Disease and RLS w N = 141 w Prevalence (overall): 64% w Prevalence w/o other risk factor: 16% w No relationship to cirrhosis or cause w Reduced Qo. L – mod. severity *No CRF, neuropathy (31%), Fe def, ETOH, Dopamine Franco et al. J Cin Sleep Med. 2008; 1: 45 -9.
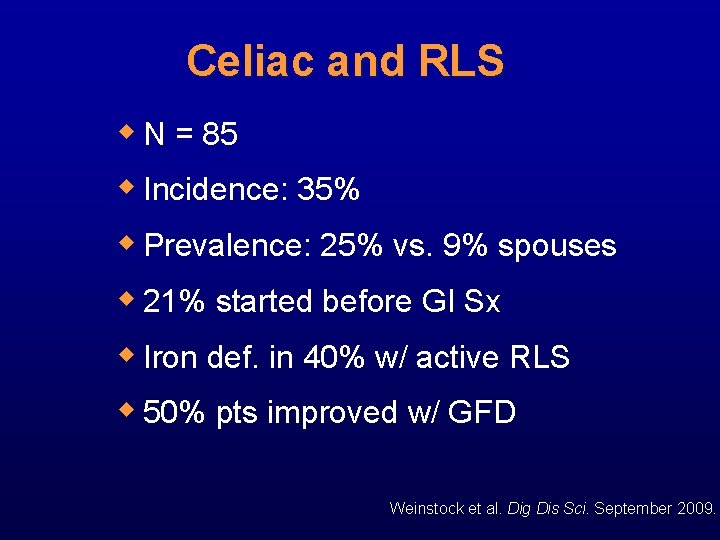
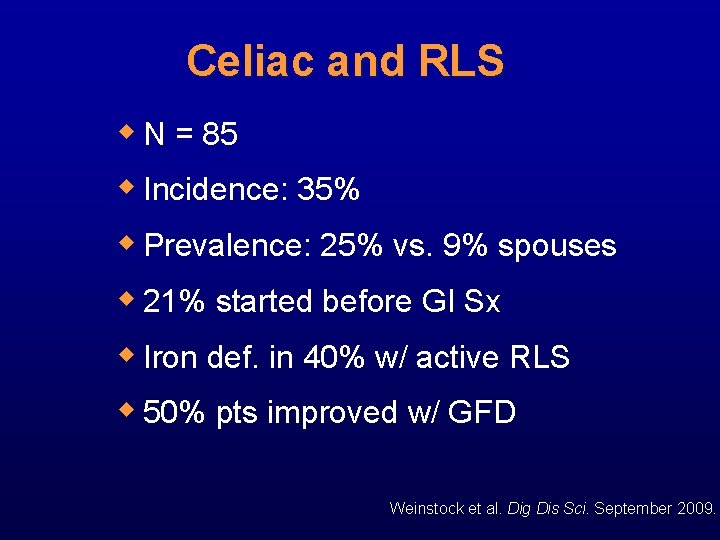
Celiac and RLS w N = 85 w Incidence: 35% w Prevalence: 25% vs. 9% spouses w 21% started before GI Sx w Iron def. in 40% w/ active RLS w 50% pts improved w/ GFD Weinstock et al. Dig Dis Sci. September 2009.
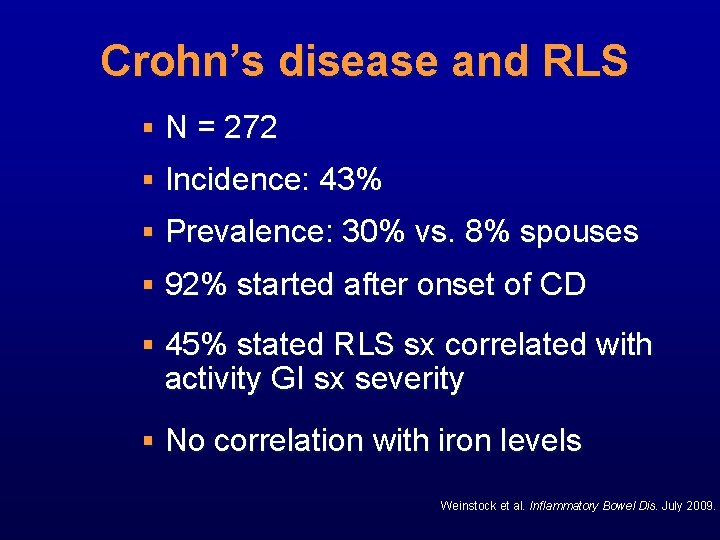
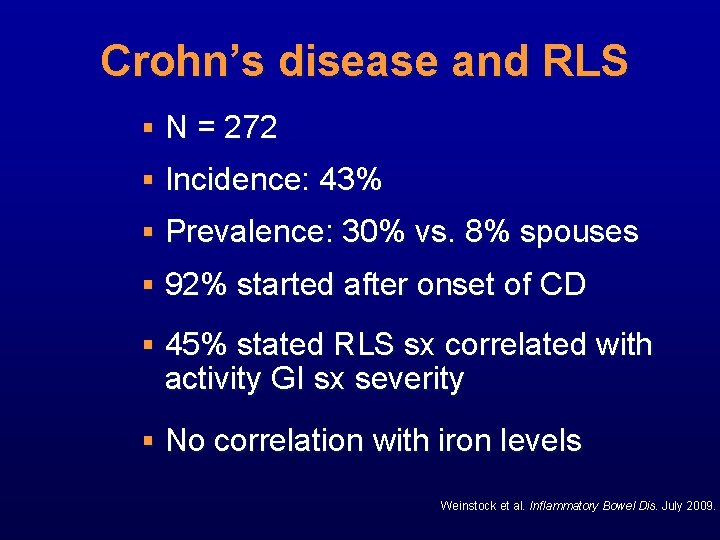
Crohn’s disease and RLS § N = 272 § Incidence: 43% § Prevalence: 30% vs. 8% spouses § 92% started after onset of CD § 45% stated RLS sx correlated with activity GI sx severity § No correlation with iron levels Weinstock et al. Inflammatory Bowel Dis. July 2009.
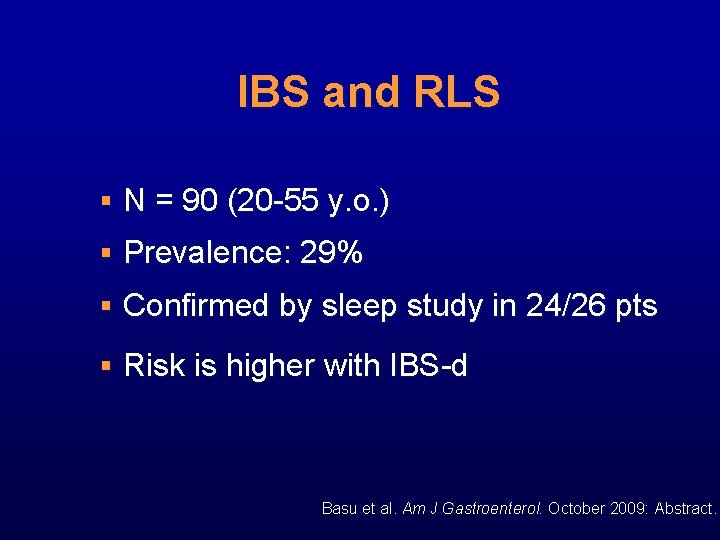
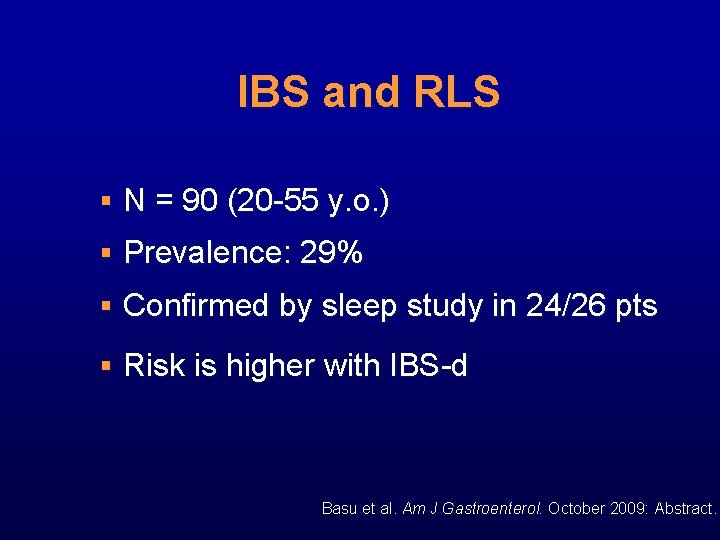
IBS and RLS § N = 90 (20 -55 y. o. ) § Prevalence: 29% § Confirmed by sleep study in 24/26 pts § Risk is higher with IBS-d Basu et al. Am J Gastroenterol. October 2009: Abstract.
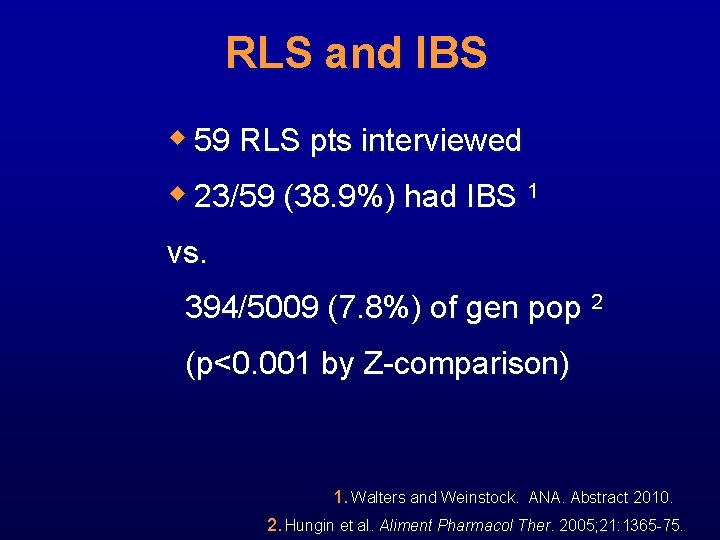
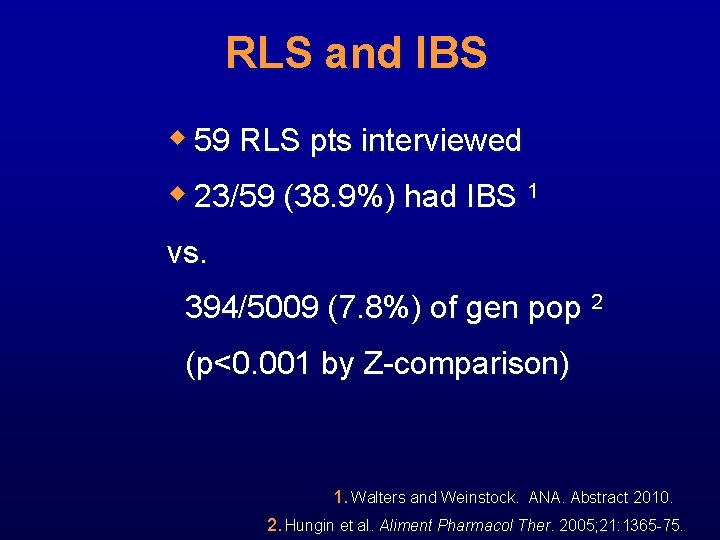
RLS and IBS w 59 RLS pts interviewed w 23/59 (38. 9%) had IBS 1 vs. 394/5009 (7. 8%) of gen pop 2 (p<0. 001 by Z-comparison) 1. Walters and Weinstock. ANA. Abstract 2010. 2. Hungin et al. Aliment Pharmacol Ther. 2005; 21: 1365 -75.
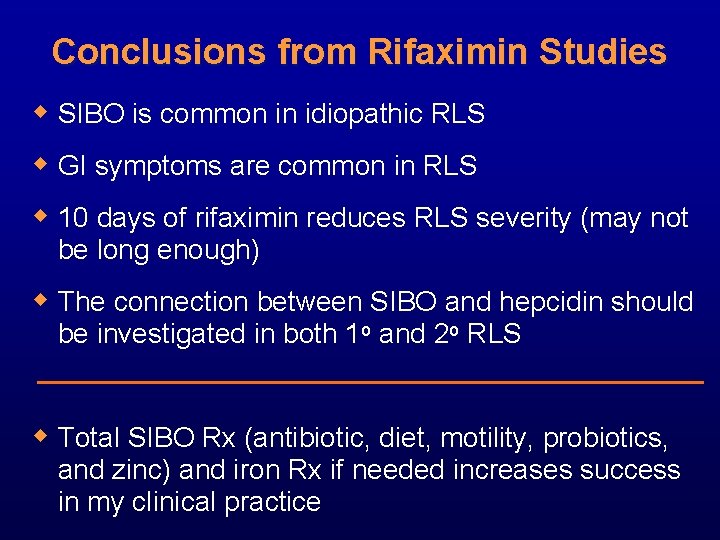
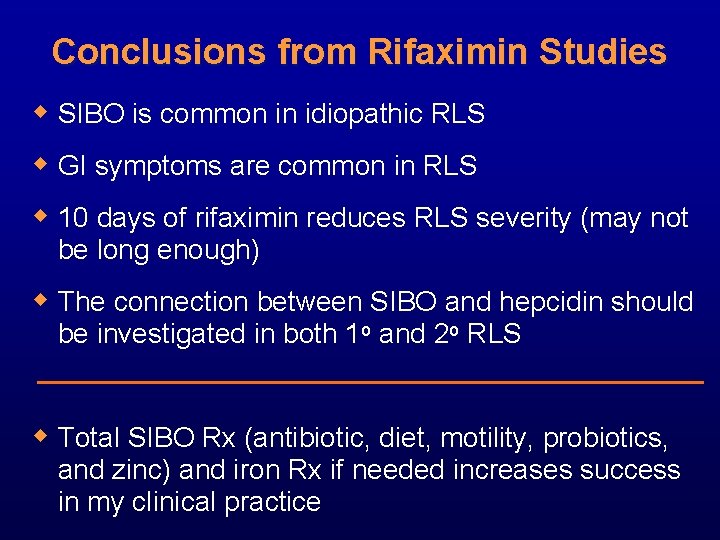
Conclusions from Rifaximin Studies w SIBO is common in idiopathic RLS w GI symptoms are common in RLS w 10 days of rifaximin reduces RLS severity (may not be long enough) w The connection between SIBO and hepcidin should be investigated in both 1 o and 2 o RLS w Total SIBO Rx (antibiotic, diet, motility, probiotics, and zinc) and iron Rx if needed increases success in my clinical practice
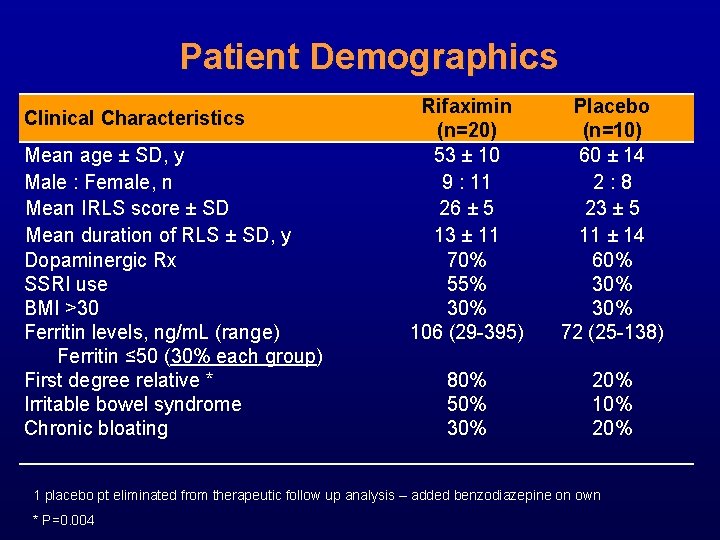
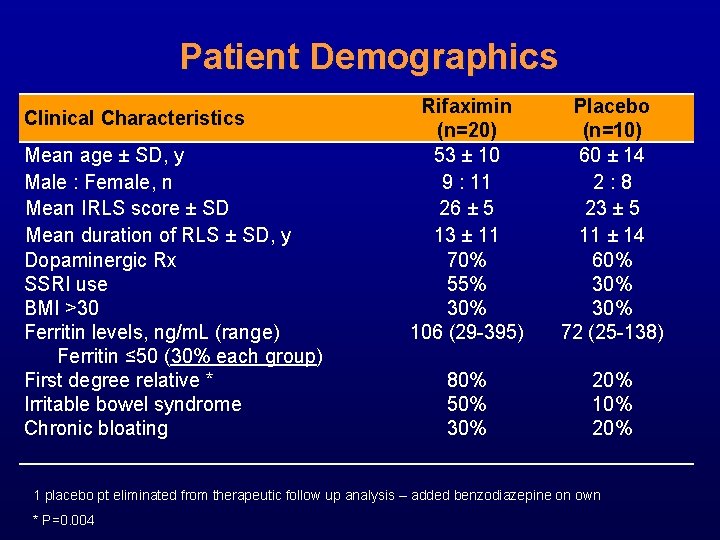
Patient Demographics Clinical Characteristics Mean age ± SD, y Male : Female, n Mean IRLS score ± SD Mean duration of RLS ± SD, y Dopaminergic Rx SSRI use BMI >30 Ferritin levels, ng/m. L (range) Ferritin ≤ 50 (30% each group) First degree relative * Irritable bowel syndrome Chronic bloating Rifaximin (n=20) 53 ± 10 9 : 11 26 ± 5 13 ± 11 70% 55% 30% 106 (29 -395) Placebo (n=10) 60 ± 14 2: 8 23 ± 5 11 ± 14 60% 30% 72 (25 -138) 80% 50% 30% 20% 1 placebo pt eliminated from therapeutic follow up analysis – added benzodiazepine on own * P=0. 004
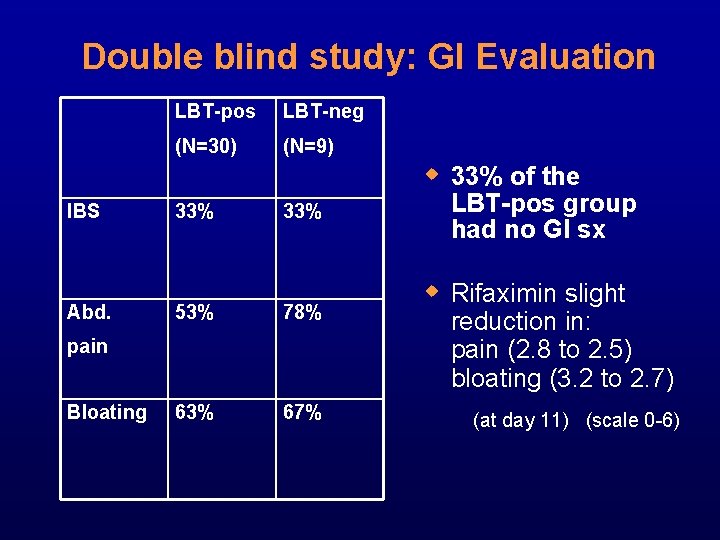
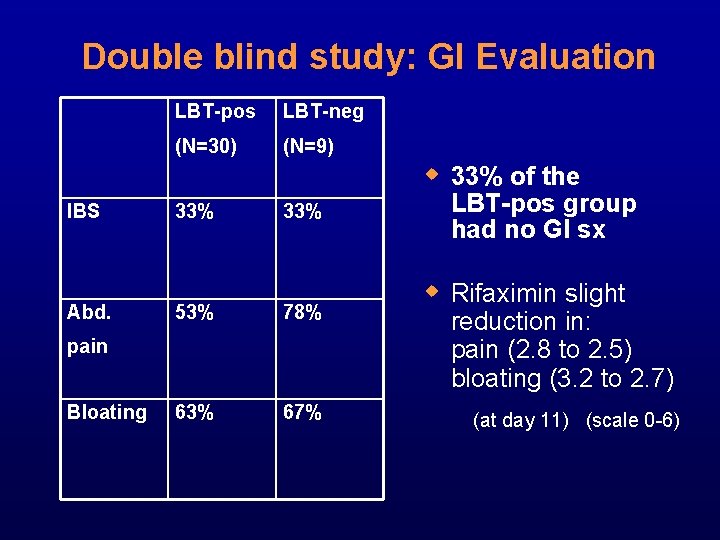
Double blind study: GI Evaluation LBT-pos LBT-neg (N=30) (N=9) w 33% of the IBS Abd. 33% 53% 78% 63% 67% pain Bloating LBT-pos group had no GI sx w Rifaximin slight reduction in: pain (2. 8 to 2. 5) bloating (3. 2 to 2. 7) (at day 11) (scale 0 -6)
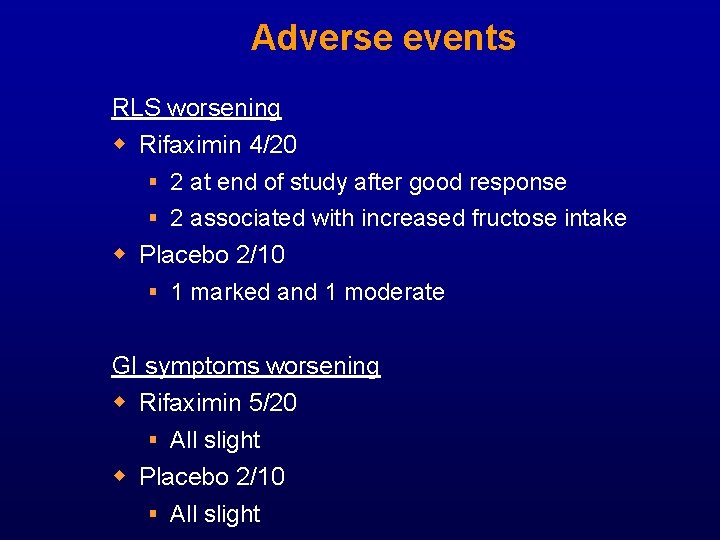
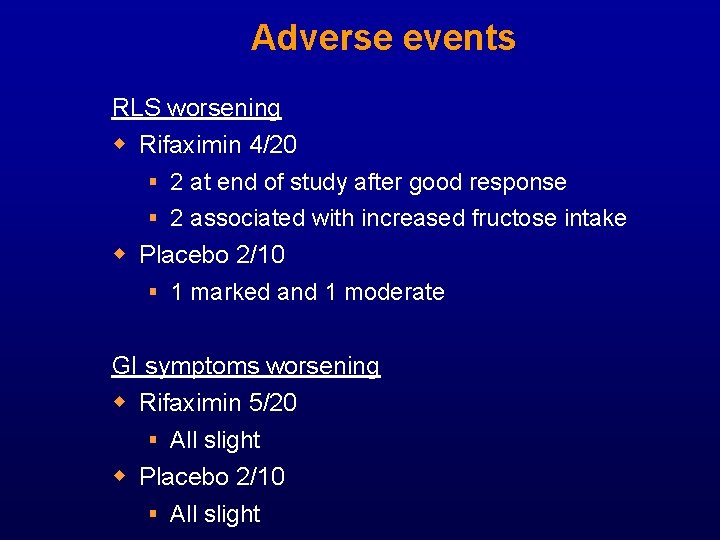
Adverse events RLS worsening w Rifaximin 4/20 § 2 at end of study after good response § 2 associated with increased fructose intake w Placebo 2/10 § 1 marked and 1 moderate GI symptoms worsening w Rifaximin 5/20 § All slight w Placebo 2/10 § All slight
 Restless leg syndrome nz
Restless leg syndrome nz Pelvic inflammatory disease men
Pelvic inflammatory disease men Pelvic girdle pain
Pelvic girdle pain Iliocolitis
Iliocolitis Immune reconstitution inflammatory syndrome
Immune reconstitution inflammatory syndrome Predeksihkhariini
Predeksihkhariini Chapter 7 section 2 restless continents answer key
Chapter 7 section 2 restless continents answer key The crust of the earth is unstable and restless
The crust of the earth is unstable and restless Restless leg synd
Restless leg synd Restful vs restless
Restful vs restless Nicole rime
Nicole rime Inflammatory breast cancer pictures
Inflammatory breast cancer pictures Sick
Sick Mucorrhea causes
Mucorrhea causes Post inflammatory erythema
Post inflammatory erythema Modified schober's test
Modified schober's test Pro and anti inflammatory
Pro and anti inflammatory Tromboflibitis
Tromboflibitis Inflammatory cells
Inflammatory cells Treatment of inflammatory breast cancer
Treatment of inflammatory breast cancer Bharathi viswanathan
Bharathi viswanathan Nursing management of adrenal tumor
Nursing management of adrenal tumor Leonard sacks fda
Leonard sacks fda Leonard kleinrock
Leonard kleinrock Tritone west side story
Tritone west side story Leonard kukic
Leonard kukic Bill leonard
Bill leonard Leonard calabrese
Leonard calabrese Leonard hakizimana
Leonard hakizimana Leonard norman
Leonard norman Anna garcia timeline
Anna garcia timeline Leonard goodstein
Leonard goodstein Horizontal scrub brushing technique
Horizontal scrub brushing technique Komeetta leonard
Komeetta leonard Leonard salmen
Leonard salmen Dr. leonard weinstock
Dr. leonard weinstock Pink gorilla west seattle
Pink gorilla west seattle Leonard de vinci
Leonard de vinci Inflectional or derivational
Inflectional or derivational Autoportrait leonard de vinci
Autoportrait leonard de vinci Leonard ortmann
Leonard ortmann Herman middle school san jose
Herman middle school san jose Contextualized and decontextualized assessment examples
Contextualized and decontextualized assessment examples What does mr. leonard mead most love to do? *
What does mr. leonard mead most love to do? * Leonard pearlin’s theory of psychological distress
Leonard pearlin’s theory of psychological distress Leonard mead character traits
Leonard mead character traits Leonard coatsworth
Leonard coatsworth Dr. leonard weinstock
Dr. leonard weinstock Stees v. leonard
Stees v. leonard Lycée léonard de vinci
Lycée léonard de vinci Pearlin theory
Pearlin theory Leonard de vinci
Leonard de vinci Connie leonard cms
Connie leonard cms