Integrated Management of Neonatal and Childhood Illness DR












- Slides: 42
Integrated Management of Neonatal and Childhood Illness DR. ARVIND GARG
The Inequities of Child Health • Every year more than 10 million children die in developing countries before they reach their fifth birthday • 7 in 10 deaths are due to acute respiratory infections, diarrhoea, malaria, measles and malnutrition • 3 in 4 episodes of childhood illness are caused by one of these five conditions • The global burden of disease indicate that these conditions will continue to be major contributors to child deaths in the year 2020, unless significantly greater efforts are made to control them
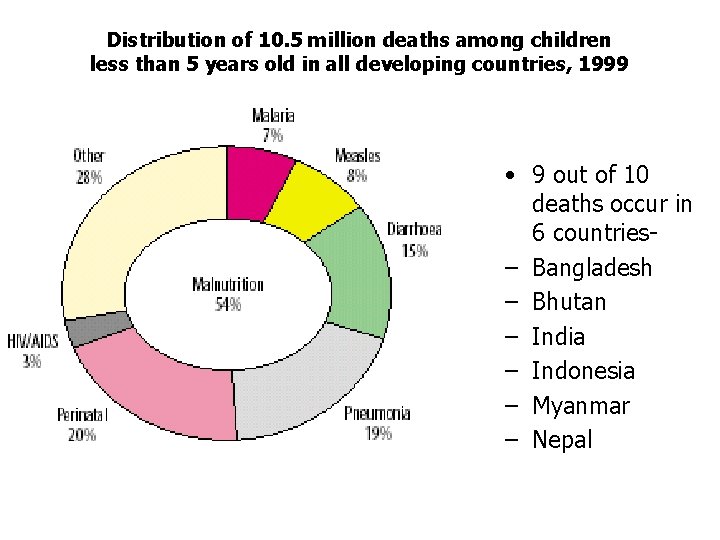
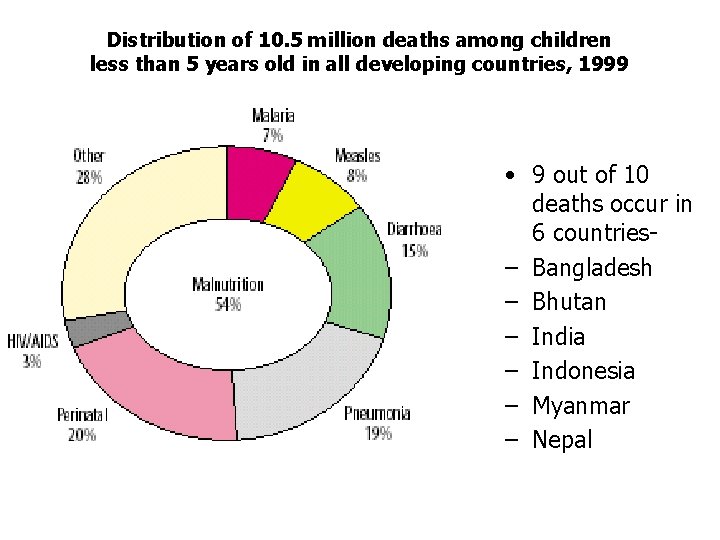
Distribution of 10. 5 million deaths among children less than 5 years old in all developing countries, 1999 • 9 out of 10 deaths occur in 6 countries– Bangladesh – Bhutan – India – Indonesia – Myanmar – Nepal
Rationale for an Integrated Evidence. Based Syndromic Approach to Case. Management • Overlapping signs and symptoms • Single diagnosis is not possible or appropriate • Improvements in child health are not necessarily dependent on the use of sophisticated and expensive technologies • Careful and systemic assessment of common symptoms and well-selected specific clinical signs provide sufficient information to guide rational and effective actions

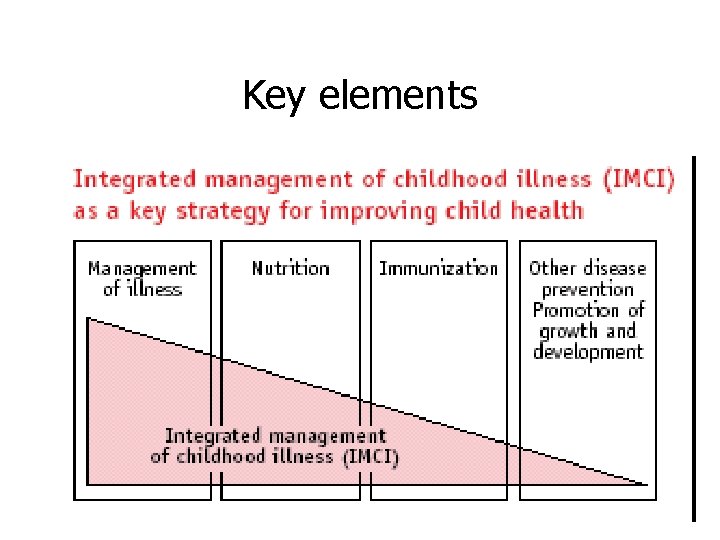
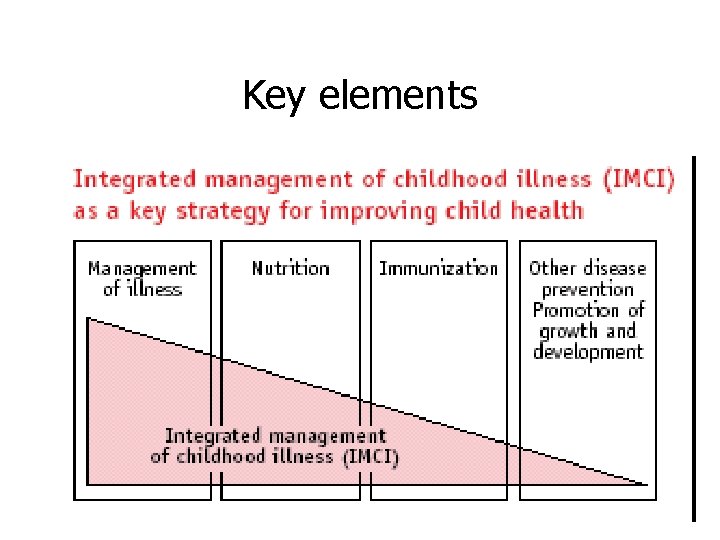
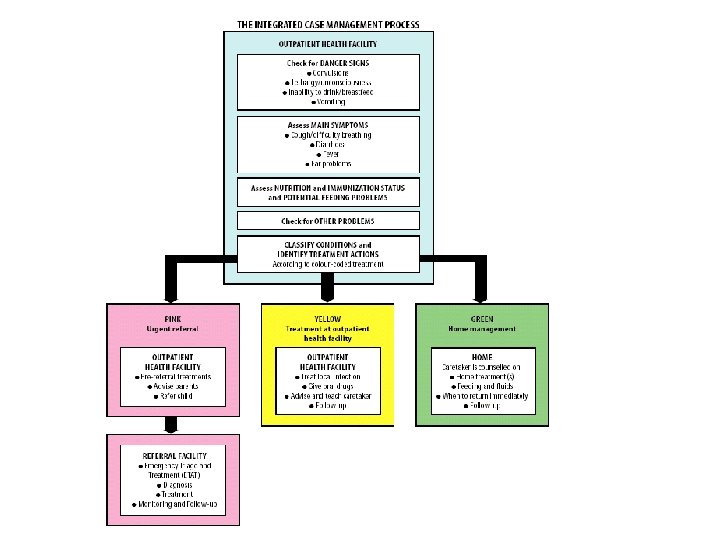
Key elements

Components of Integrated approach • Improvement in case management skills of health staff through locally-adapted guidelines • Improvements in overall health system • Improvements in family and community health care practices

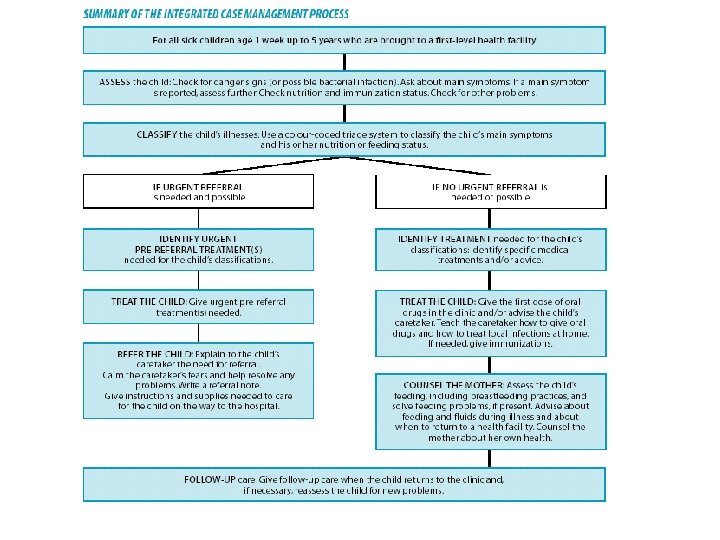
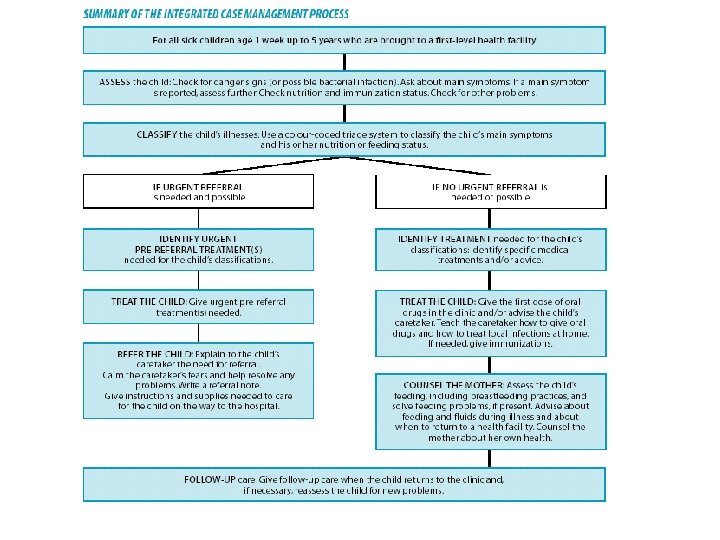
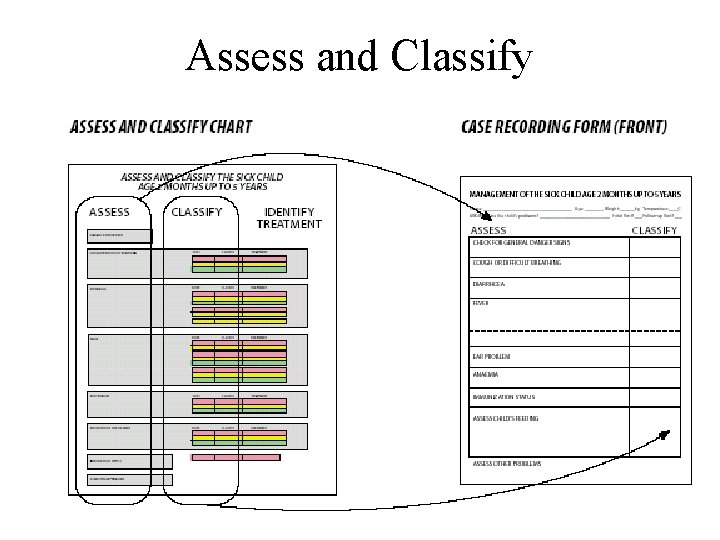
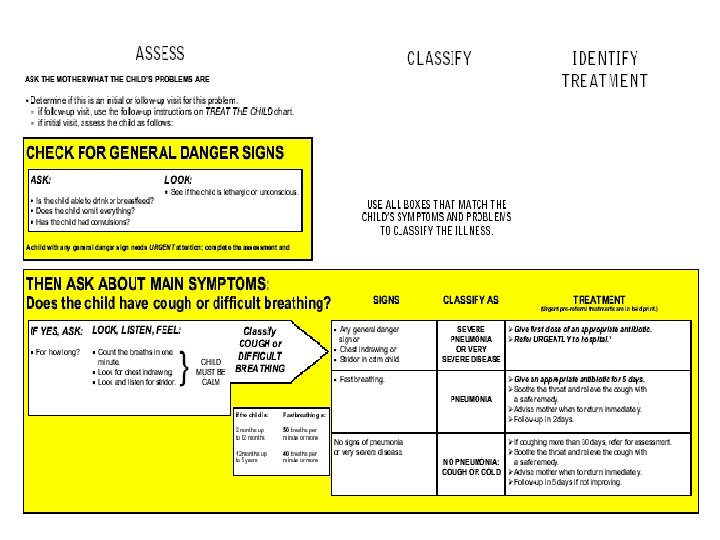
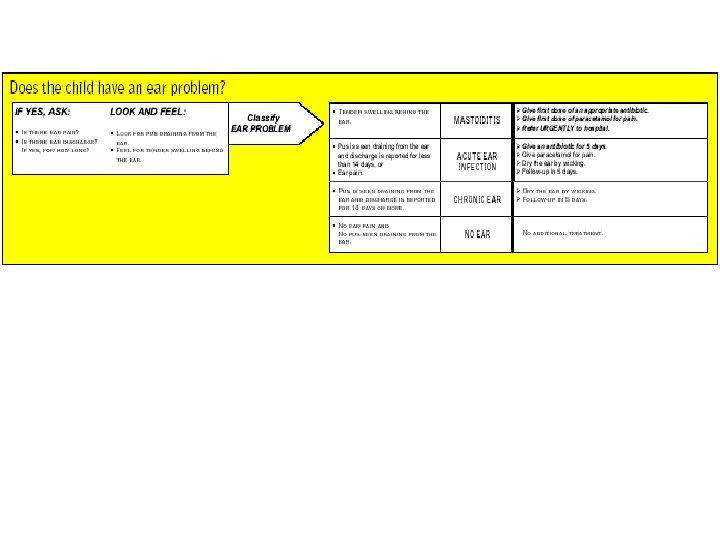
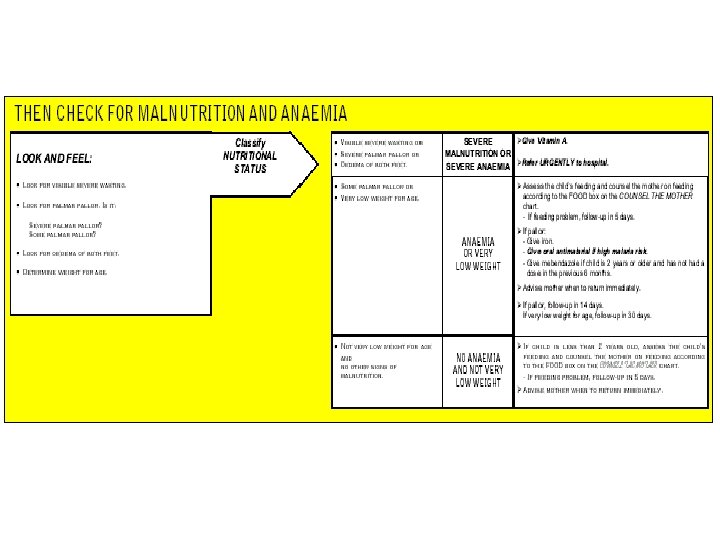
Assess and Classify
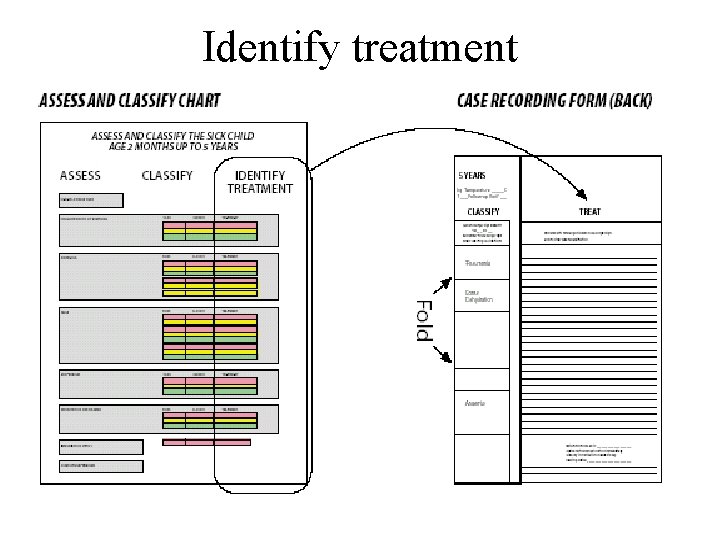
Identify treatment
Treat the child
Counsel the mother
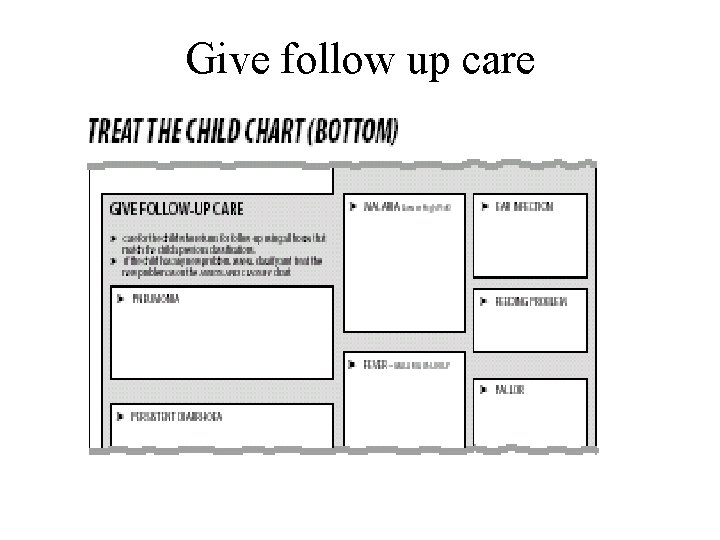
Give follow up care
Young Infants age upto 2 months • • Not used for well infant brought for immunization Injury Burn Care of new born at birth • Greet the mother • Ask the mother what the young infant’s problems are • Determine if this is an initial or follow up visit • Use the young infant recording form

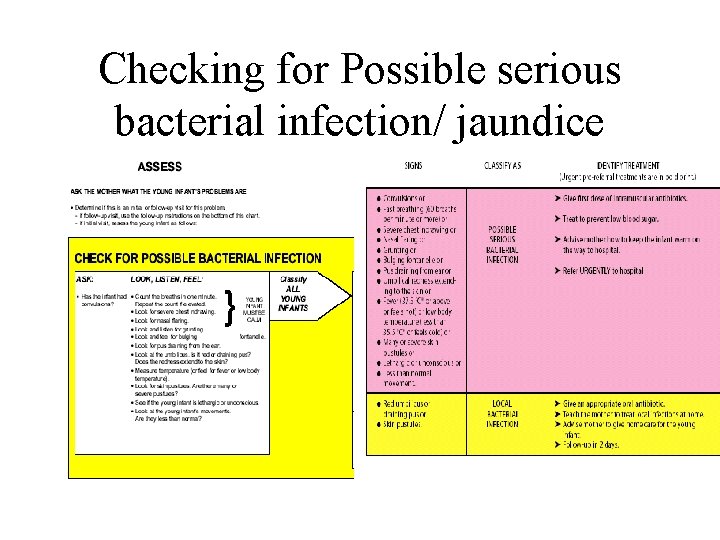
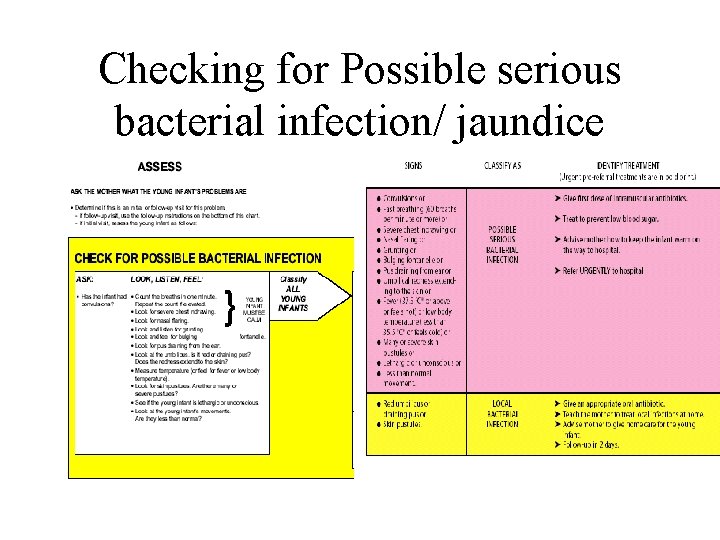
Checking for Possible serious bacterial infection/ jaundice
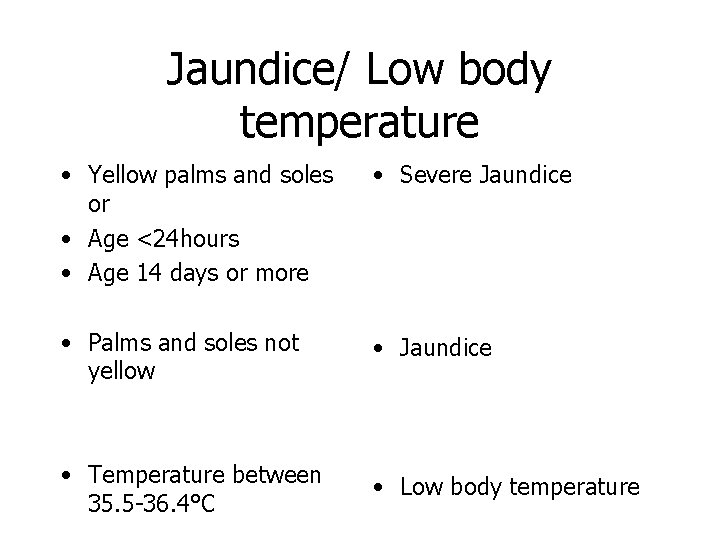
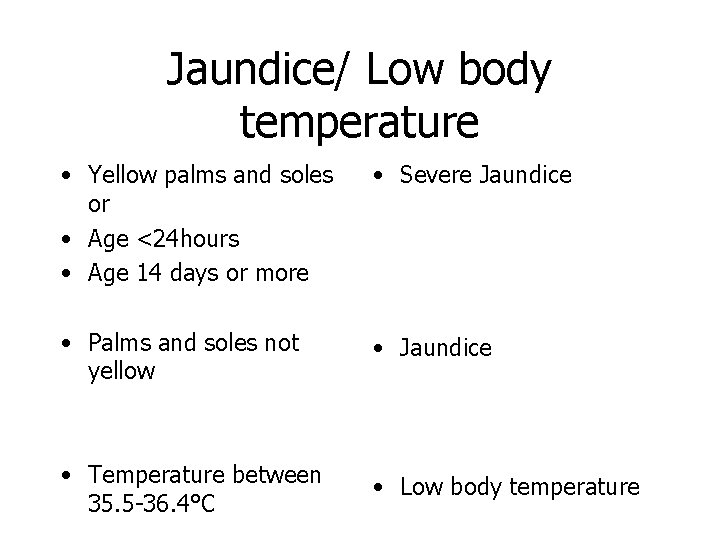
Jaundice/ Low body temperature • Yellow palms and soles or • Age <24 hours • Age 14 days or more • Severe Jaundice • Palms and soles not yellow • Jaundice • Temperature between 35. 5 -36. 4°C • Low body temperature
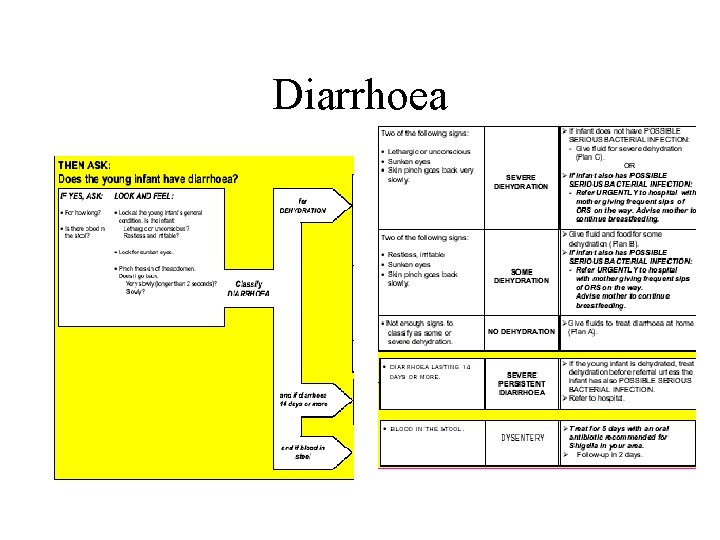
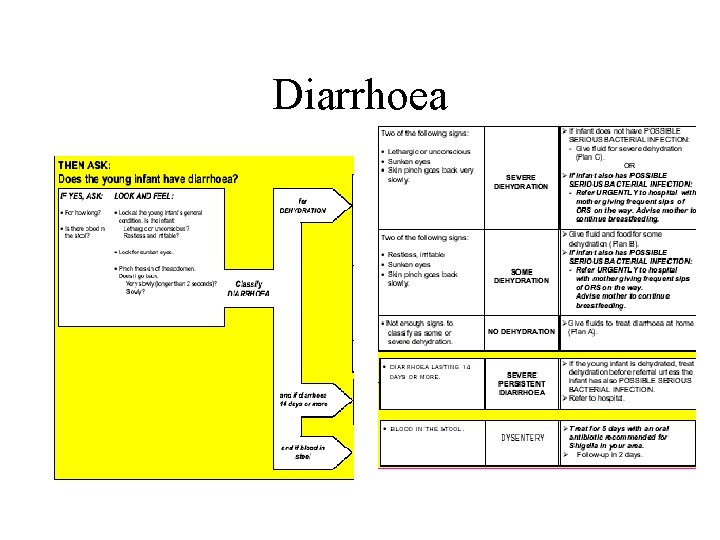
Diarrhoea
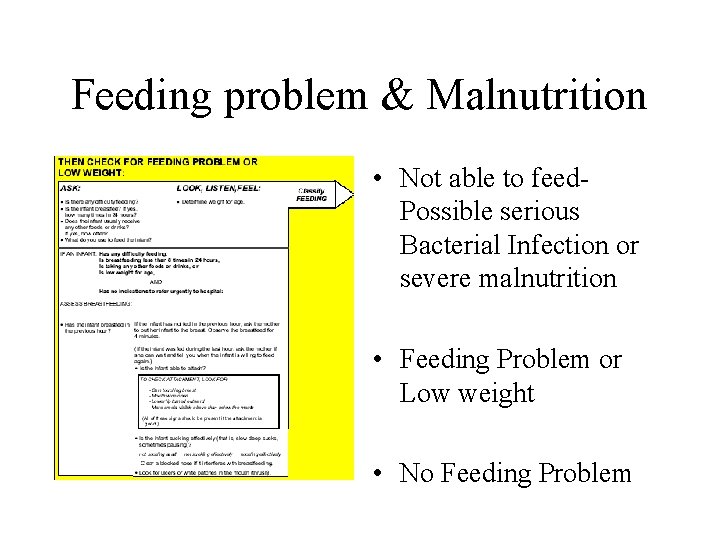
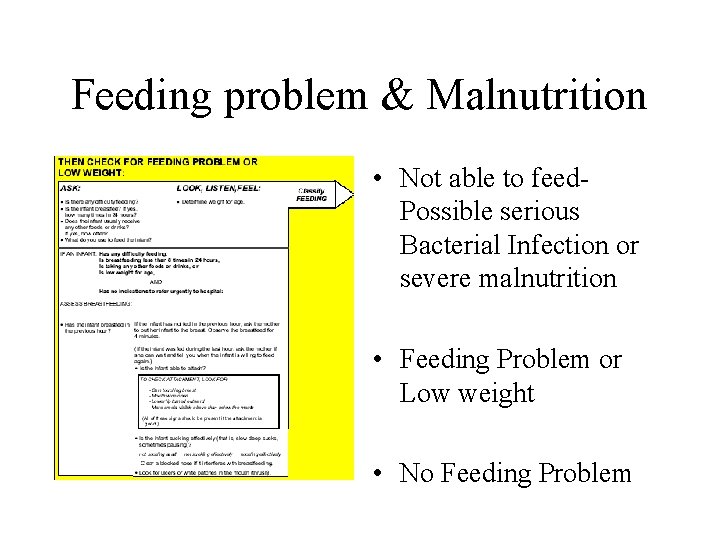
Feeding problem & Malnutrition • Not able to feed. Possible serious Bacterial Infection or severe malnutrition • Feeding Problem or Low weight • No Feeding Problem
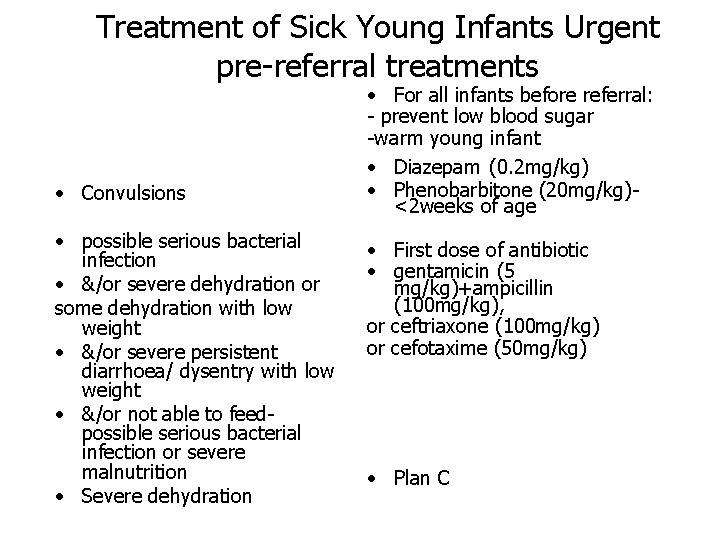
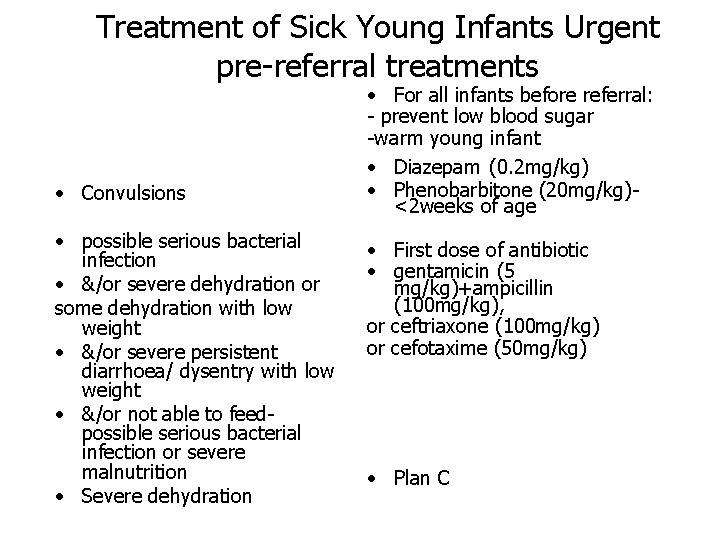
Treatment of Sick Young Infants Urgent pre-referral treatments • Convulsions • possible serious bacterial infection • &/or severe dehydration or some dehydration with low weight • &/or severe persistent diarrhoea/ dysentry with low weight • &/or not able to feedpossible serious bacterial infection or severe malnutrition • Severe dehydration • For all infants before referral: - prevent low blood sugar -warm young infant • Diazepam (0. 2 mg/kg) • Phenobarbitone (20 mg/kg)<2 weeks of age • First dose of antibiotic • gentamicin (5 mg/kg)+ampicillin (100 mg/kg), or ceftriaxone (100 mg/kg) or cefotaxime (50 mg/kg) • Plan C

Treatment in the outpatient clinic for sick young infants age up to 2 months • Local bacterial infection • Some deydration (without low weight) • No dehydration • Feeding problem or low weight • Oral antibiotic • Plan B • Plan. A • Give feeding advice
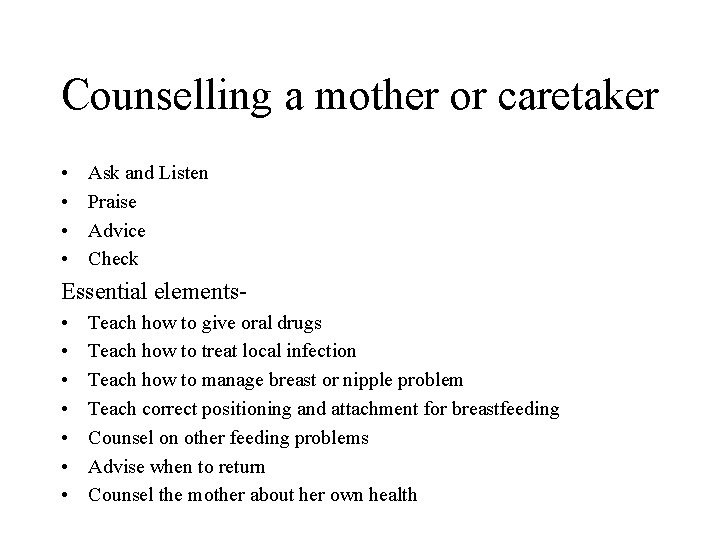
Counselling a mother or caretaker • • Ask and Listen Praise Advice Check Essential elements • • Teach how to give oral drugs Teach how to treat local infection Teach how to manage breast or nipple problem Teach correct positioning and attachment for breastfeeding Counsel on other feeding problems Advise when to return Counsel the mother about her own health
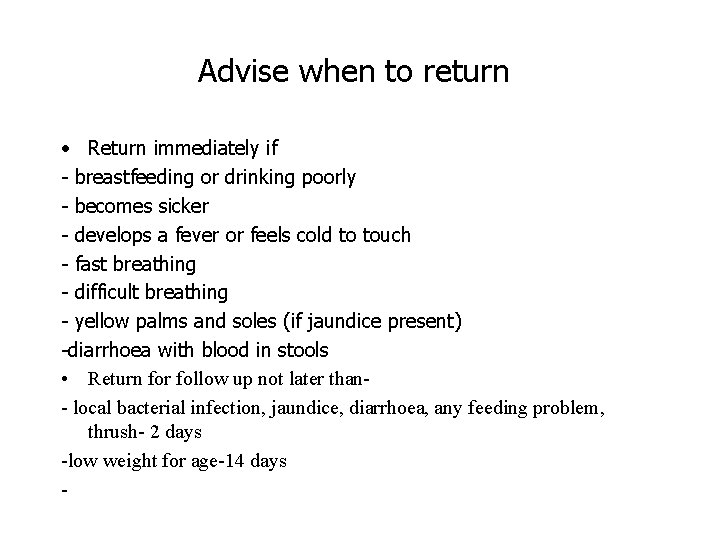
Advise when to return • Return immediately if - breastfeeding or drinking poorly - becomes sicker - develops a fever or feels cold to touch - fast breathing - difficult breathing - yellow palms and soles (if jaundice present) -diarrhoea with blood in stools • Return for follow up not later than- local bacterial infection, jaundice, diarrhoea, any feeding problem, thrush- 2 days -low weight for age-14 days -
Outpatient management of children age 2 months up to 5 years
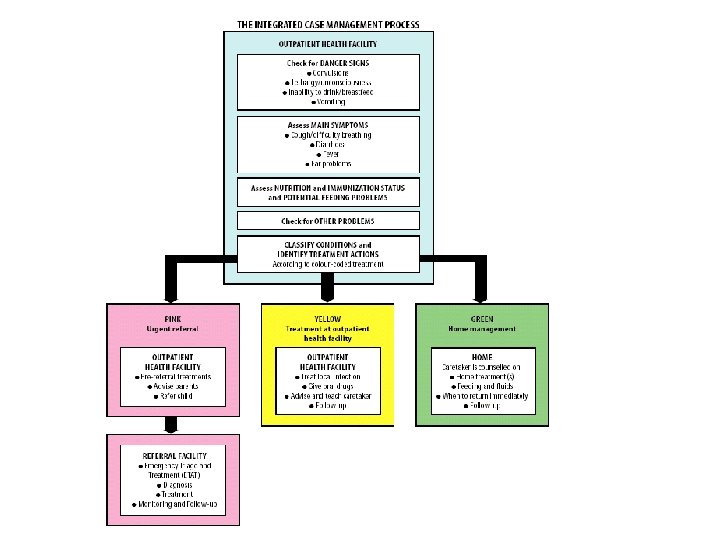
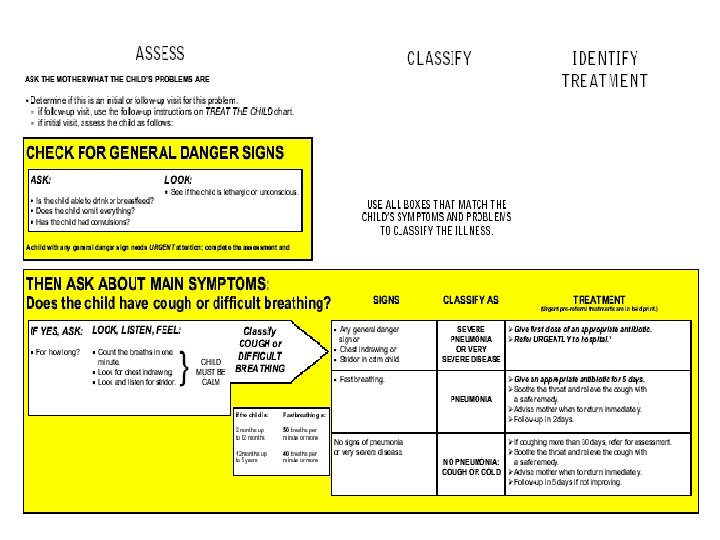


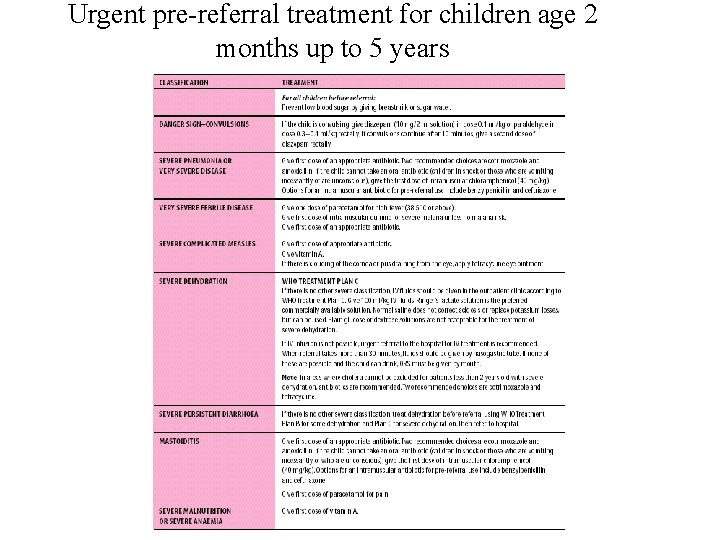
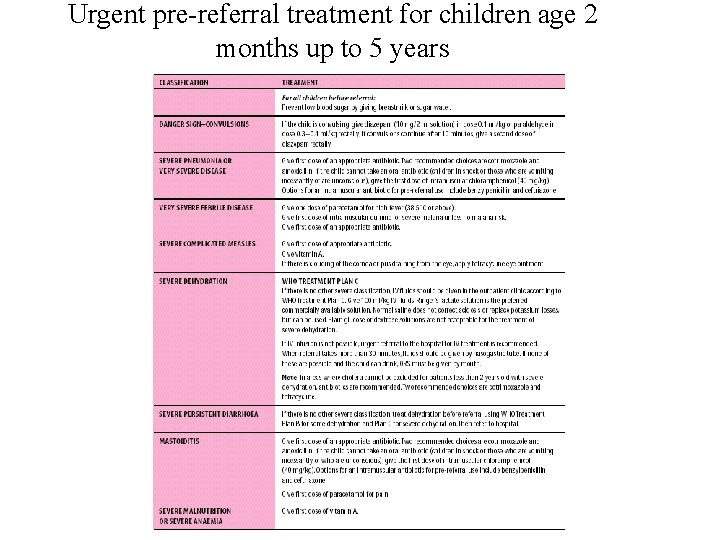
Urgent pre-referral treatment for children age 2 months up to 5 years

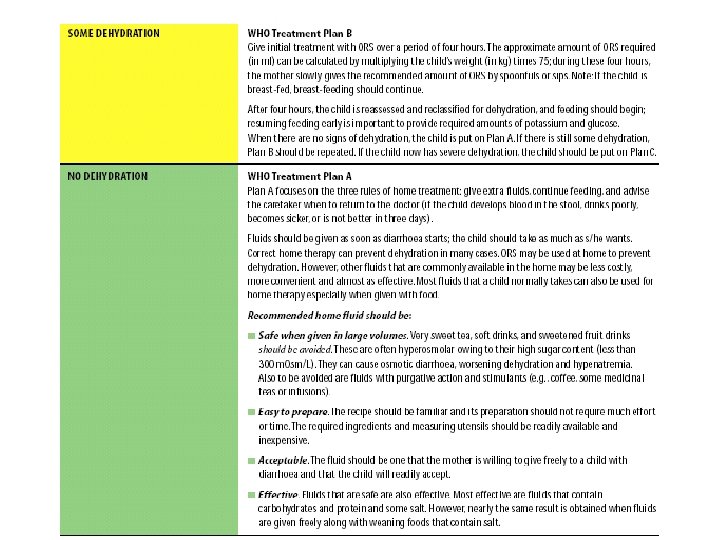
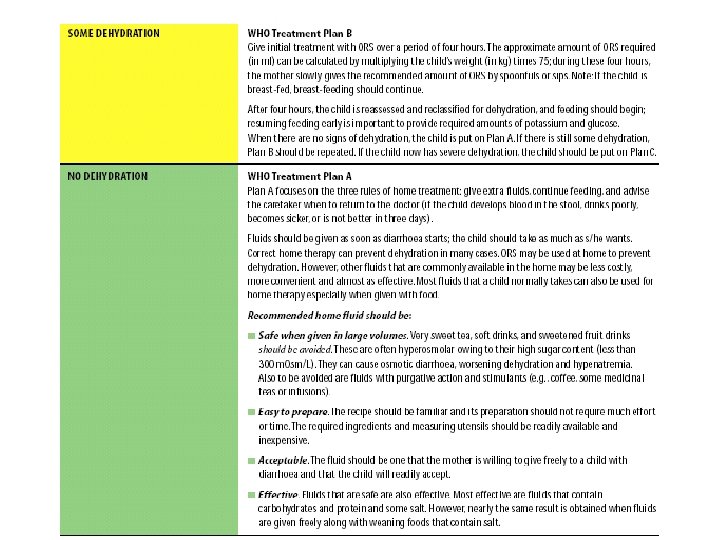
Treatment in outpatient facility



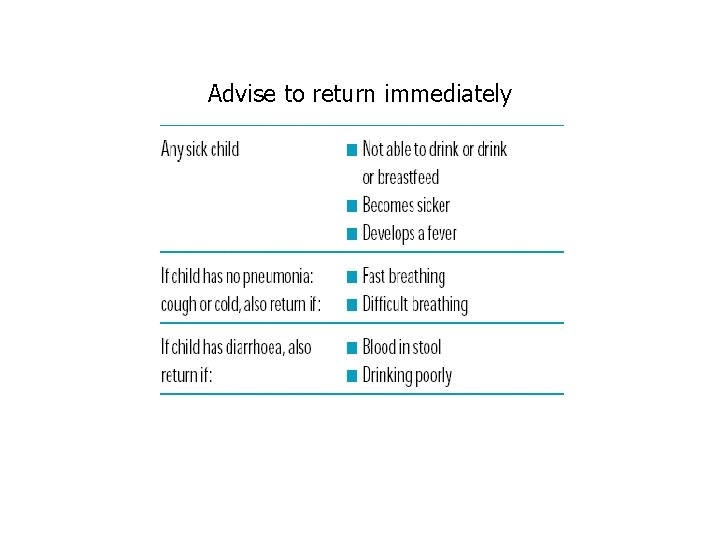
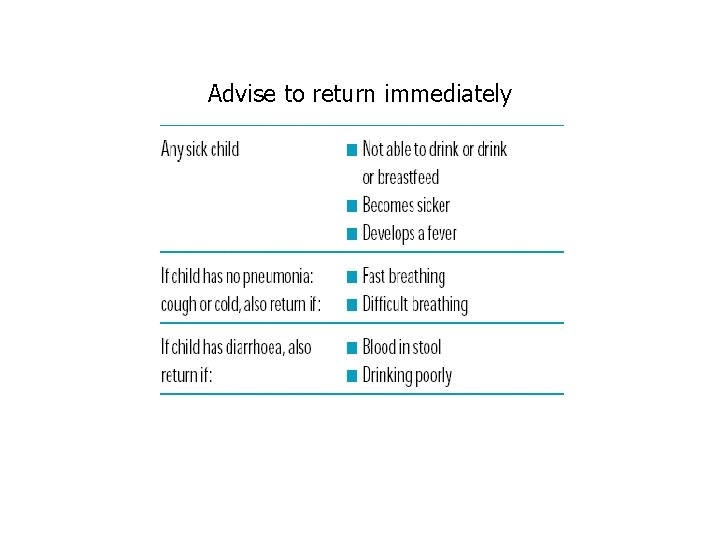
Advise to return immediately
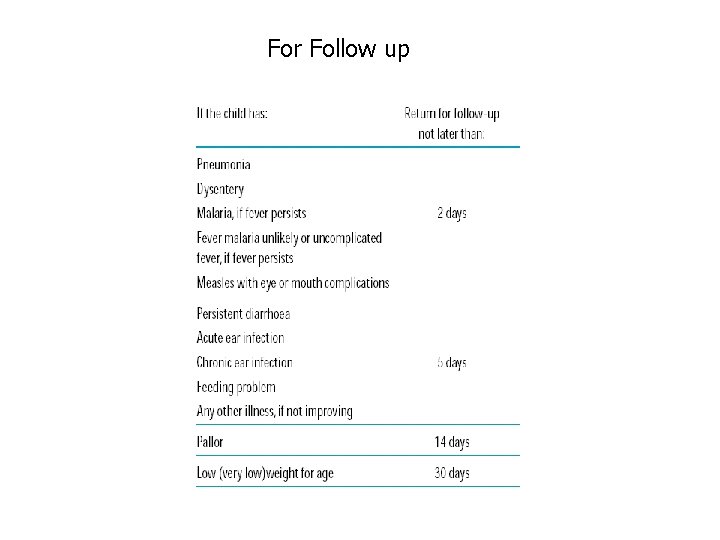
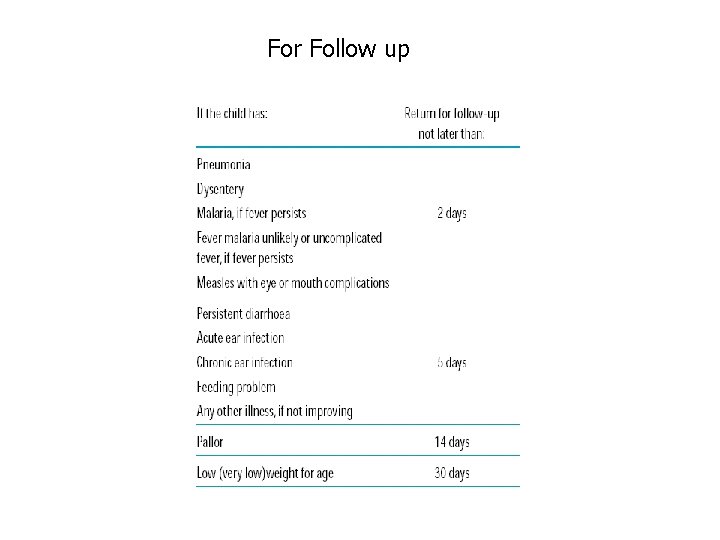
For Follow up

Comments • promotes accurate identification of childhood illnesses in outpatient settings • ensures appropriate combined treatment of all major illnesses • strengthens the counselling of caretakers and the provision of preventive services • speeds up the referral of severely ill children • improve the quality of care of sick children at the referral level • In the home setting, it promotes appropriate careseeking behaviours, improved nutrition and preventive care, and the correct implementation of prescribed care. • cost-effective • Improves equity • has the potential to make a major contribution to health system
 Early childhood and middle childhood
Early childhood and middle childhood Illness management and recovery worksheet
Illness management and recovery worksheet Bilirubin chart
Bilirubin chart Tetanus pathogenesis
Tetanus pathogenesis Yorkshire neonatal network
Yorkshire neonatal network Chapter 20 mental health and mental illness
Chapter 20 mental health and mental illness What is a common signal of sudden illness
What is a common signal of sudden illness Health illness continuum model
Health illness continuum model Illness and wellness continuum
Illness and wellness continuum Eudemonistic model
Eudemonistic model Advantages and disadvantages of integrated weed management
Advantages and disadvantages of integrated weed management Vasculopatía lenticuloestriada definicion
Vasculopatía lenticuloestriada definicion Circulação fetal
Circulação fetal Triade neonatal
Triade neonatal Tamiz neonatal
Tamiz neonatal Ambiente termico neutro
Ambiente termico neutro Hastalık düzeyini belirleyen ölçütler
Hastalık düzeyini belirleyen ölçütler Neonatal sepsis pathophysiology diagram
Neonatal sepsis pathophysiology diagram Sepsis temprana
Sepsis temprana Clasificacion de kramer ictericia
Clasificacion de kramer ictericia Underfive
Underfive Poliglobulia neonatal
Poliglobulia neonatal Poliglobulia neonatal
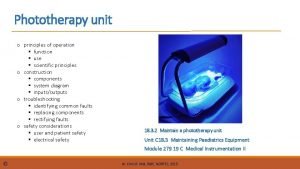
Poliglobulia neonatal Phototherapy principles
Phototherapy principles Parâmetros iniciais ventilação mecânica neonatal
Parâmetros iniciais ventilação mecânica neonatal Pain assessment
Pain assessment Oxigeno por halo
Oxigeno por halo Nursing diagnosis three parts
Nursing diagnosis three parts Neonatal period is defined as
Neonatal period is defined as Neonatarum
Neonatarum Prevention of puerperal sepsis
Prevention of puerperal sepsis Site:slidetodoc.com
Site:slidetodoc.com Iap slides
Iap slides Baby apgar score
Baby apgar score Zonas de kramer ictericia neonatal
Zonas de kramer ictericia neonatal Bilirrubina valores normales pediatria
Bilirrubina valores normales pediatria Hemoglucotest en neonatos
Hemoglucotest en neonatos Escala de kramer modificada
Escala de kramer modificada Diagnostico de hiperbilirrubinemia neonatal
Diagnostico de hiperbilirrubinemia neonatal A.1500g7 desnuda
A.1500g7 desnuda Portal hypertension definition
Portal hypertension definition Bilirrubina recém-nascido valores normais
Bilirrubina recém-nascido valores normais Cuidados de enfermería en oxigenoterapia neonatal
Cuidados de enfermería en oxigenoterapia neonatal