Integrated Management of Childhood IllnessIMCI OR Integrated Management





- Slides: 47

Integrated Management of Childhood Illness(IMCI) OR Integrated Management of Neonatal and Childhood illness (IMNCI)
GADCHIROLI MODEL • Home-based neonatal care interventions developed at SEARCH , Society for Education Action and Research in Community Health (SEARCH) , an NGO in Gadchiroli of Maharashtra , founded by Dr Abhay and Dr Rani Bang
GADCHIROLI MODEL • Inspired by the Chinese example of barefoot doctors ; It follows a simple principle that said that healthcare must be available within that distance, which a mother on foot can walk with a sick baby. • In the Bangs’ case, that principle meant providing care to the newborn at home
GADCHIROLI MODEL • Almost all Indian states barring Kerala and Tamil Nadu (which have low IMR) and Chhattisgarh (that already has a similar ‘mitanin’ programme) have initiated the first phase of implementing the Gadchiroli model.
GADCHIROLI MODEL • The National Health System Resource Centre (NHSRC)—a nodal agency for training community health workers or accredited social health activists (ASHA)—is facilitating the training with inputs from SEARCH. • Each ASHA worker will be paid Rs 250 for each infant each tends to, using NRHM funds. 800, 000 village women in India are now being trained by the government under the ASHA programme.
GADCHIROLI MODEL • Six districts in Hyderabad Karnataka (HK) and north Karnataka (NK), and one district in south Karnataka (old Mysore region), that have been identified as High Focus Districts by the Union Government in view of poor health indicators prevailing there, have adopted the new model to address neo-natal and infant deaths. in the districts of Gulbarga, Bidar, Raichur, Koppal, Bijapur, Bagalkot and Chamarajanagar
Integrated Management of Childhood Illness(IMCI) OR Integrated Management of Neonatal and Childhood illness (IMNCI)
Basis for introducing IMCI 1) Integration is supposed to tackle: • Complexity of different independent services and administrative structures in achieving common goals 2) Improvements in child health are not necessarily dependent on the use of sophisticated and expensive technologies

Meaning of integration At patient level • Means case management irrespective of the speciality At point of delivery • Multiple interventions are provided through one delivery channel. • Eg. : Vaccination is combined with Vit A At system level • Bringing together management and support function of different subprograms and ensuring inter-sectoral co-ordination
Rationale • Signs and symptoms of more than one illness in most sick children • Need to combine treatment for several conditions • IMCI strategy combines - Improved management of childhood illness - With aspects of nutrition, immunization, and other important disease prevention and health promotion

Main Components 1) Improvement in case management skills of health staff through the provision of locally adapted guidelines 2) Improvement of infrastructure in health system required for effective management of childhood illness 3) Improvement in family and community practice
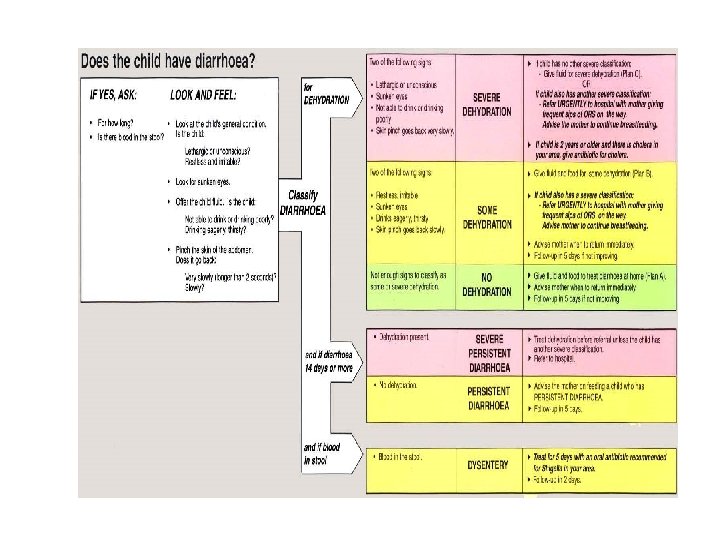
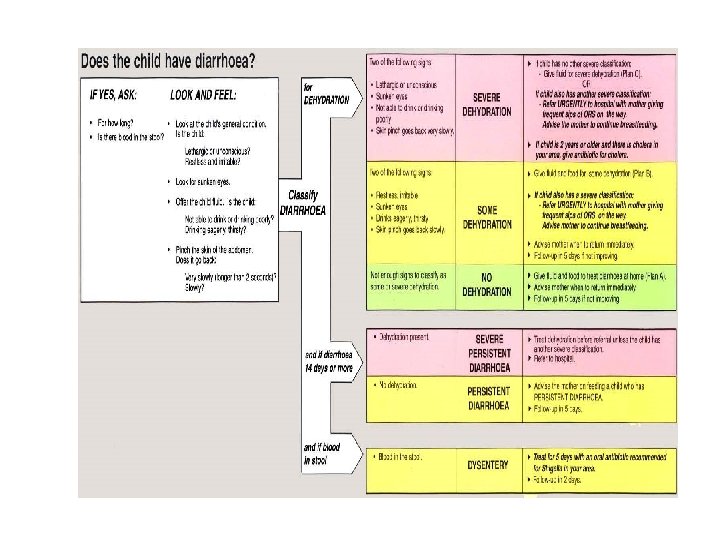
Focus of IMCI • Diarrhea • ARI • Malaria • Measles • Malnutrition Ø Improve parental understanding of childcare
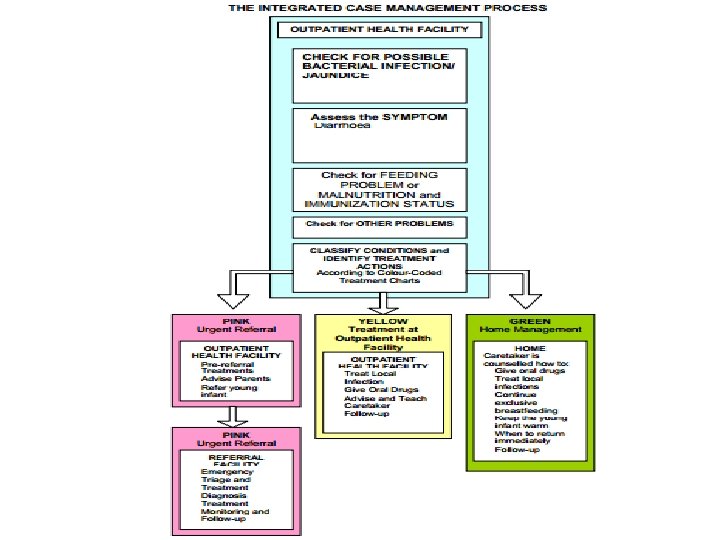
Elements of Management process • • • Assess Classify Identify Treatment Counsel Follow-up care
Assessment • Checking first for danger signs • Asking questions regarding common conditions • Examination • Checking nutrition and immunization status • Checking for other health problems
Classify • Color coded triage system: 1) Urgent pre-referral treatment and referral: PINK 2) Specific medical treatment and advice: YELLOW 3) Simple advice on home management: GREEN
Identify • Classify all conditions • Essential treatment before child is transferred • If treatment at home, give first dose in the clinic • Immunization if indicated
Treatment • Practical treatment instructions • Teach the caretaker to give drugs, fluids and feeds • Give clear instructions about when to return • Early visit in case of any danger signs and their identification
Counsel • Counsel regarding feeding practice • Counsel mother regarding her own health Follow-up Care • Re-assess on follow-up and reinforce any practical advice
IMNCI IN Indian • Integrated management of neonatal and childhood illness • Includes children up to one week of age Case management follow 2 sets of chart: 1) Children 2 months to 5 years of age 2) Children less than 2 months of age
Indian Context • NFHS III suggests ARI (17%), diarrhea (13%), fever (27%) and undernutrition (43%) as most common morbidities • Measles coverage is also low • IMNCI provides an integrated strategy to address all these
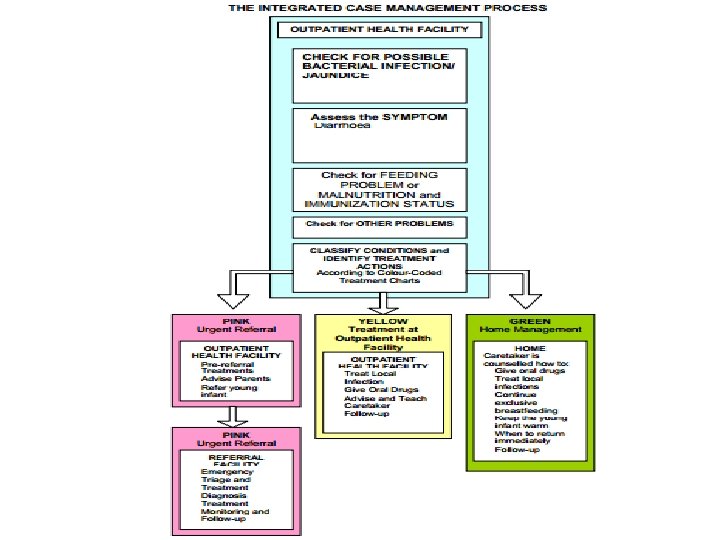
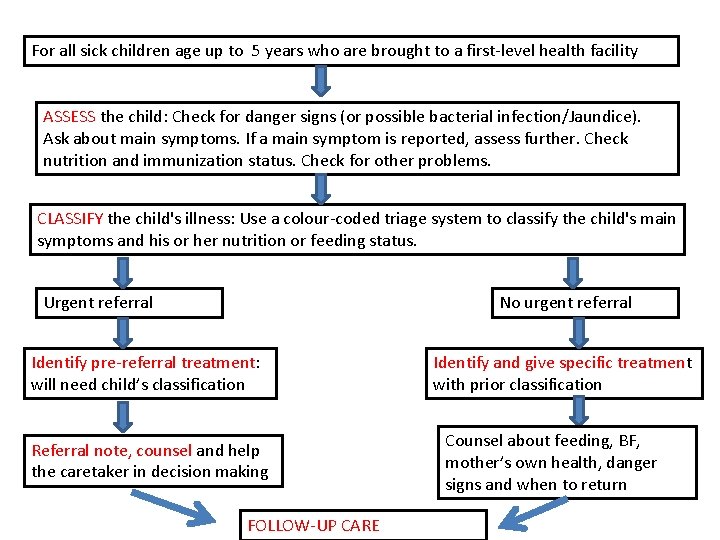
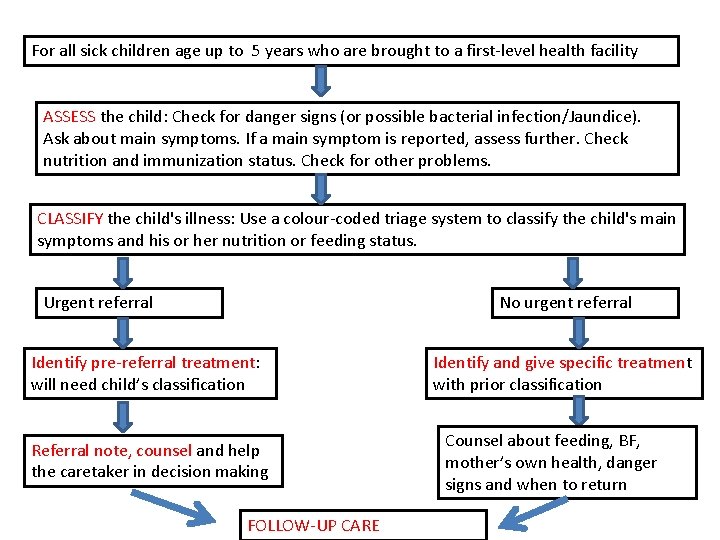
For all sick children age up to 5 years who are brought to a first-level health facility ASSESS the child: Check for danger signs (or possible bacterial infection/Jaundice). Ask about main symptoms. If a main symptom is reported, assess further. Check nutrition and immunization status. Check for other problems. CLASSIFY the child's illness: Use a colour-coded triage system to classify the child's main symptoms and his or her nutrition or feeding status. Urgent referral No urgent referral Identify pre-referral treatment: will need child’s classification Referral note, counsel and help the caretaker in decision making FOLLOW-UP CARE Identify and give specific treatment with prior classification Counsel about feeding, BF, mother’s own health, danger signs and when to return


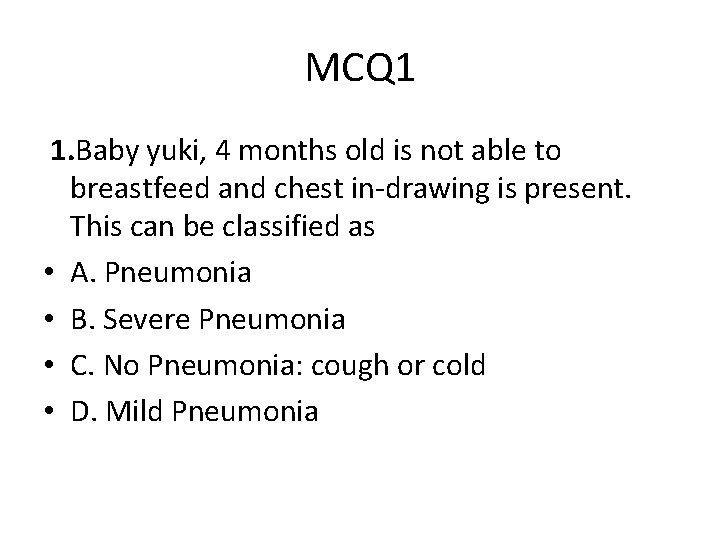
MCQ 1 1. Baby yuki, 4 months old is not able to breastfeed and chest in-drawing is present. This can be classified as • A. Pneumonia • B. Severe Pneumonia • C. No Pneumonia: cough or cold • D. Mild Pneumonia
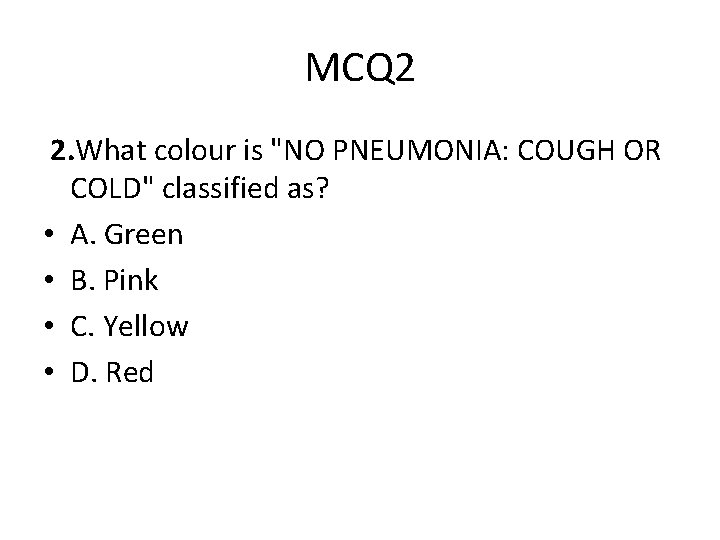
MCQ 2 2. What colour is "NO PNEUMONIA: COUGH OR COLD" classified as? • A. Green • B. Pink • C. Yellow • D. Red
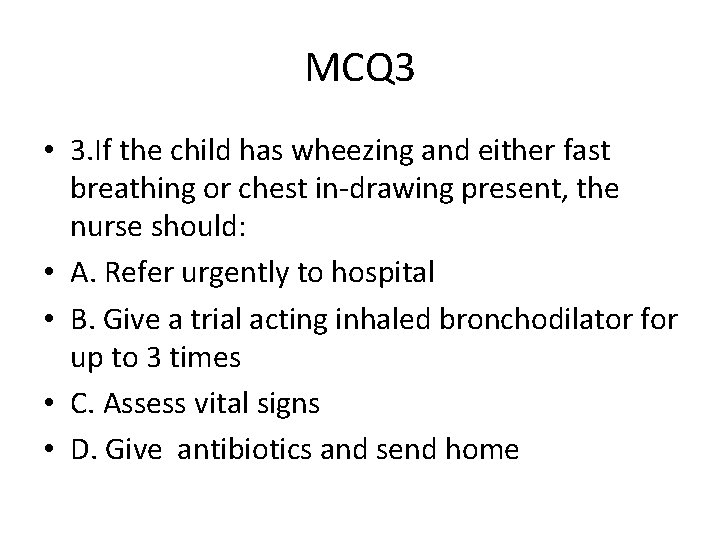
MCQ 3 • 3. If the child has wheezing and either fast breathing or chest in-drawing present, the nurse should: • A. Refer urgently to hospital • B. Give a trial acting inhaled bronchodilator for up to 3 times • C. Assess vital signs • D. Give antibiotics and send home
Rashtriya Bal Swasthya Karyakram Child Health Screening & Early Intervention Services
Introduction • Started under the aegis of NRHM in Feb 2013 • Initiated by MOHFW • To reduce child mortality under NRHM • To improve the overall quality of the life of children • Enable a systematic approach to Child health screening and early intervention • “School Health Programme” expanded to cover children from birth to 18 years
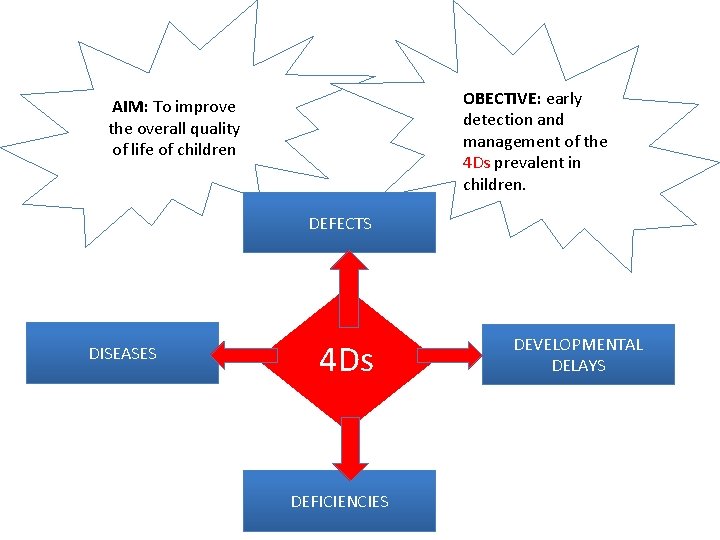
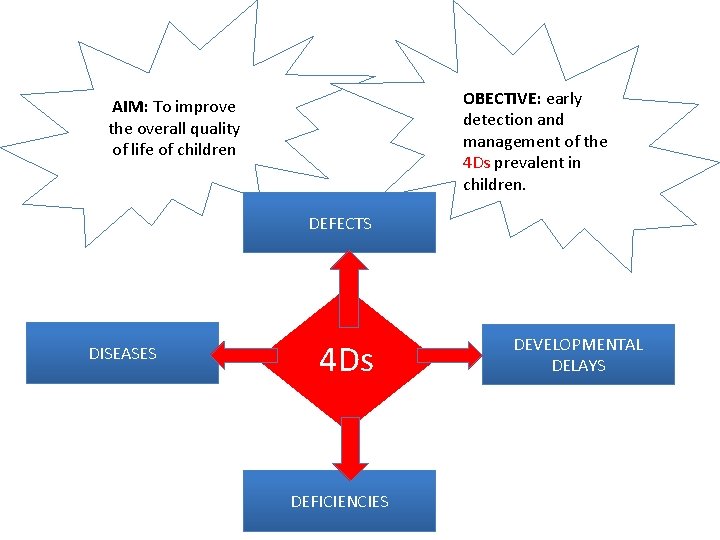
OBECTIVE: early detection and management of the 4 Ds prevalent in children. AIM: To improve the overall quality of life of children DEFECTS DISEASES 4 Ds DEFICIENCIES DEVELOPMENTAL DELAYS
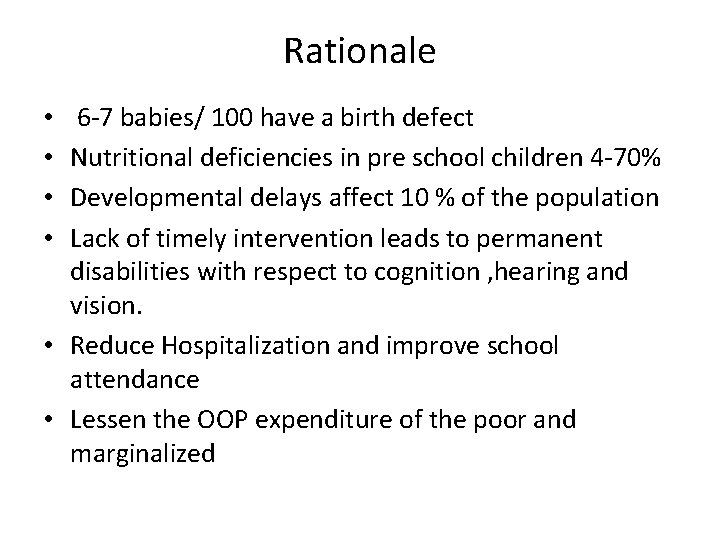
Rationale 6 -7 babies/ 100 have a birth defect Nutritional deficiencies in pre school children 4 -70% Developmental delays affect 10 % of the population Lack of timely intervention leads to permanent disabilities with respect to cognition , hearing and vision. • Reduce Hospitalization and improve school attendance • Lessen the OOP expenditure of the poor and marginalized • •
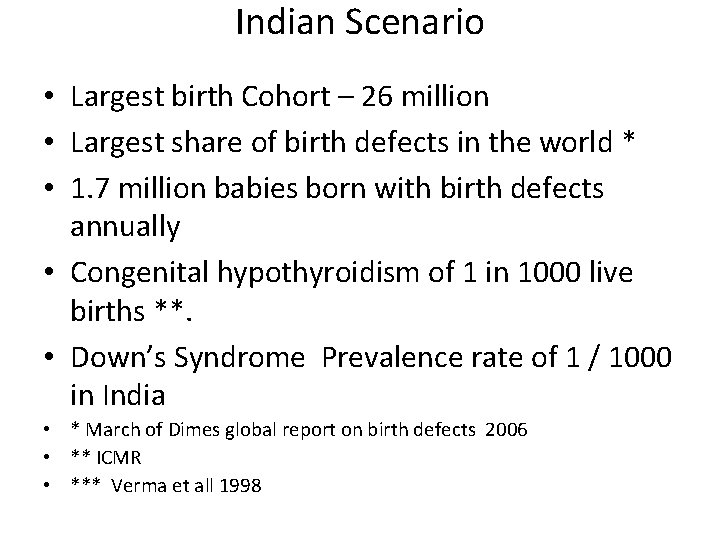
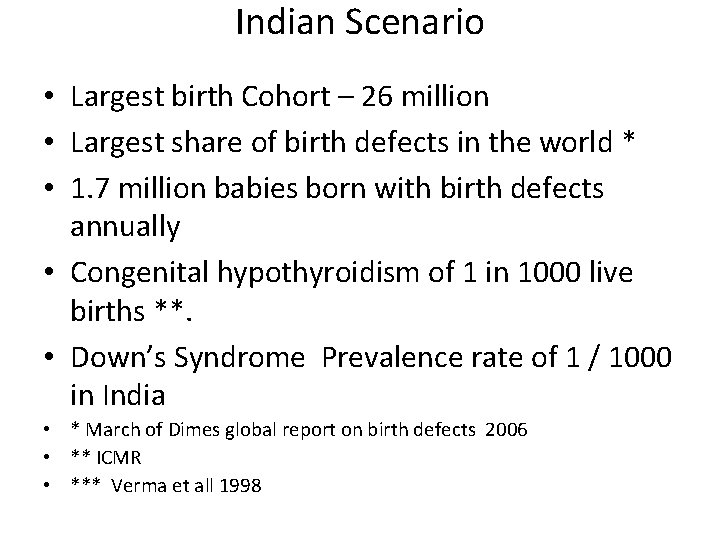
Indian Scenario • Largest birth Cohort – 26 million • Largest share of birth defects in the world * • 1. 7 million babies born with birth defects annually • Congenital hypothyroidism of 1 in 1000 live births **. • Down’s Syndrome Prevalence rate of 1 / 1000 in India • * March of Dimes global report on birth defects 2006 • ** ICMR • *** Verma et all 1998
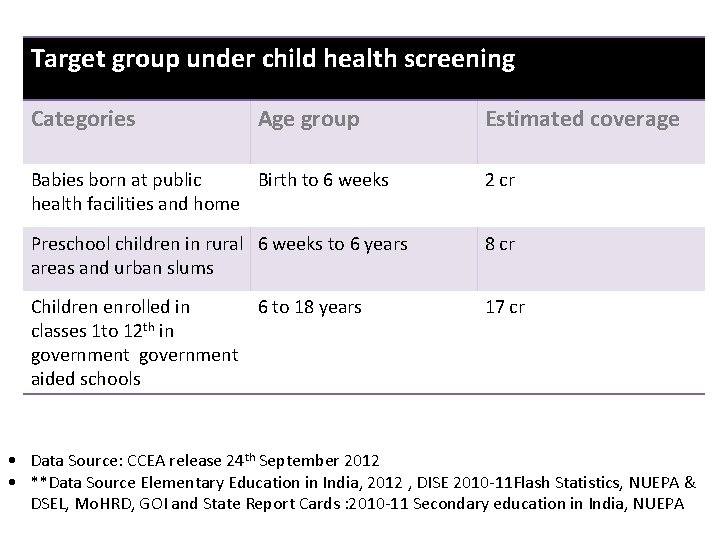
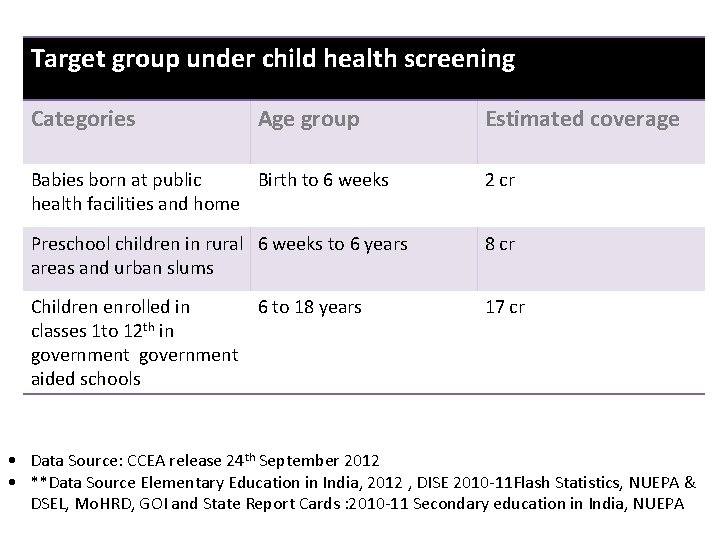
Target group under child health screening Categories Age group Estimated coverage Babies born at public Birth to 6 weeks health facilities and home 2 cr Preschool children in rural 6 weeks to 6 years areas and urban slums 8 cr Children enrolled in 6 to 18 years classes 1 to 12 th in government aided schools 17 cr • Data Source: CCEA release 24 th September 2012 • **Data Source Elementary Education in India, 2012 , DISE 2010 -11 Flash Statistics, NUEPA & DSEL, Mo. HRD, GOI and State Report Cards : 2010 -11 Secondary education in India, NUEPA
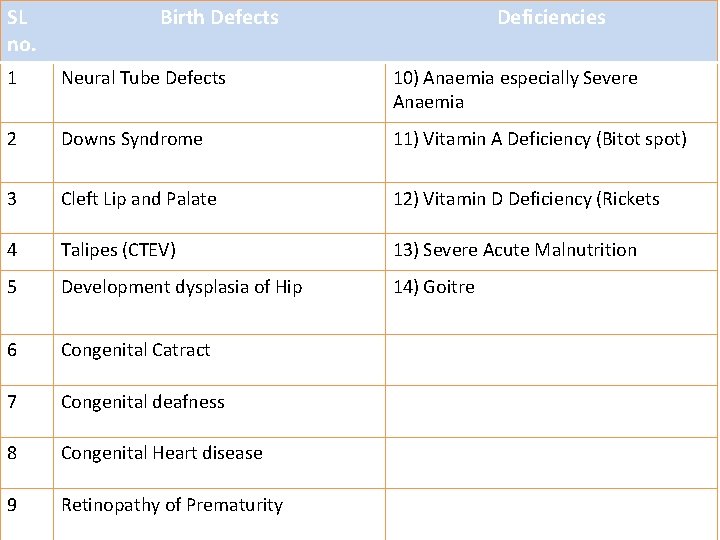
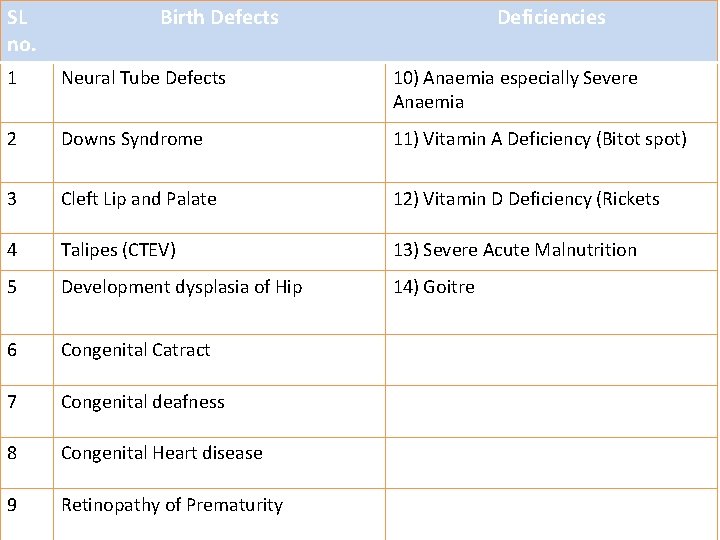
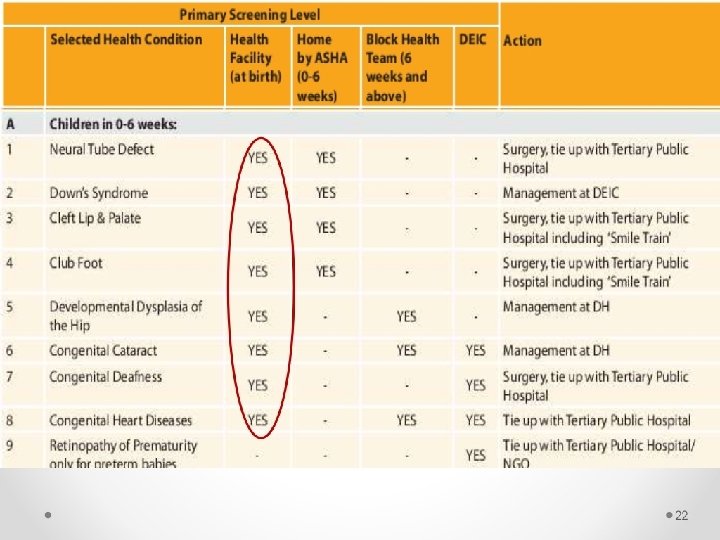
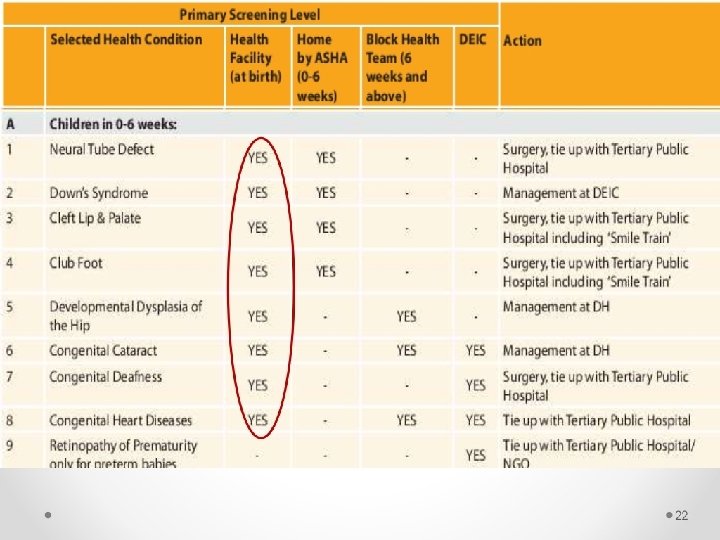
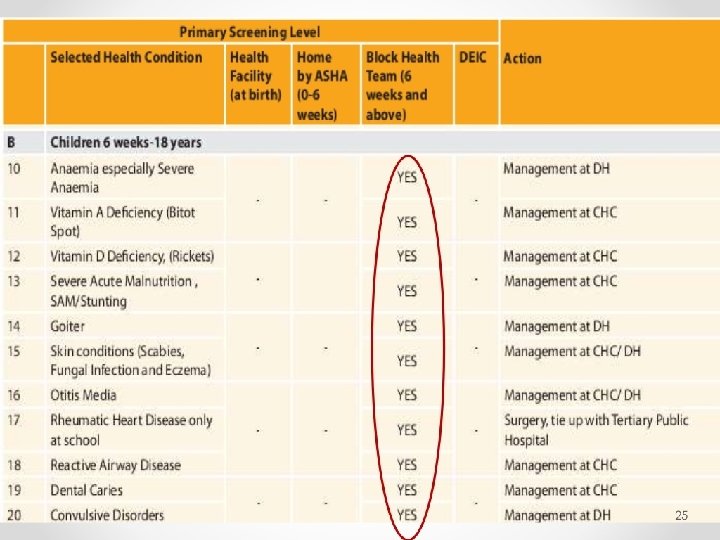
SL no. Birth Defects Deficiencies 1 Neural Tube Defects 10) Anaemia especially Severe Anaemia 2 Downs Syndrome 11) Vitamin A Deficiency (Bitot spot) 3 Cleft Lip and Palate 12) Vitamin D Deficiency (Rickets 4 Talipes (CTEV) 13) Severe Acute Malnutrition 5 Development dysplasia of Hip 14) Goitre 6 Congenital Catract 7 Congenital deafness 8 Congenital Heart disease 9 Retinopathy of Prematurity
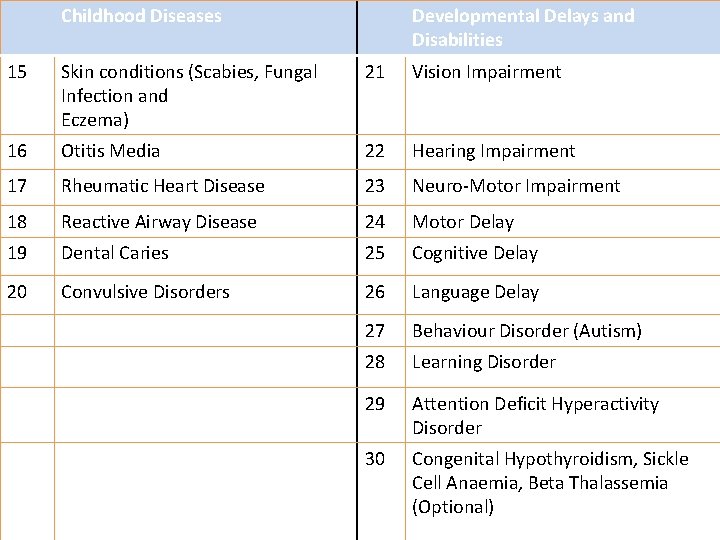
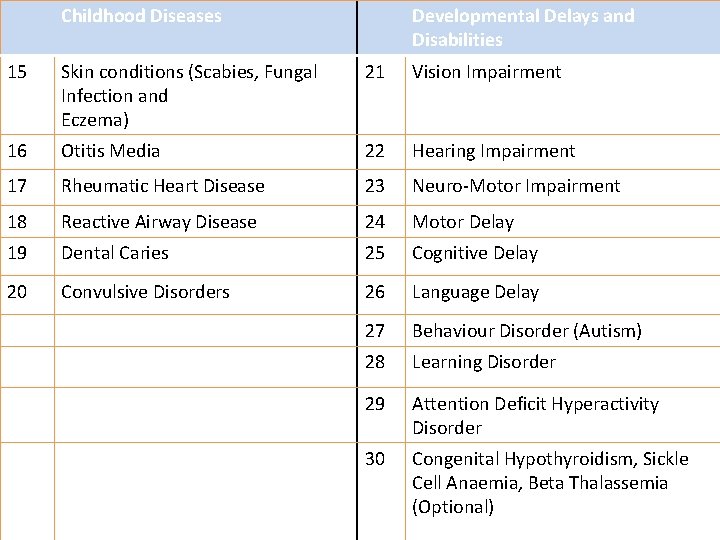
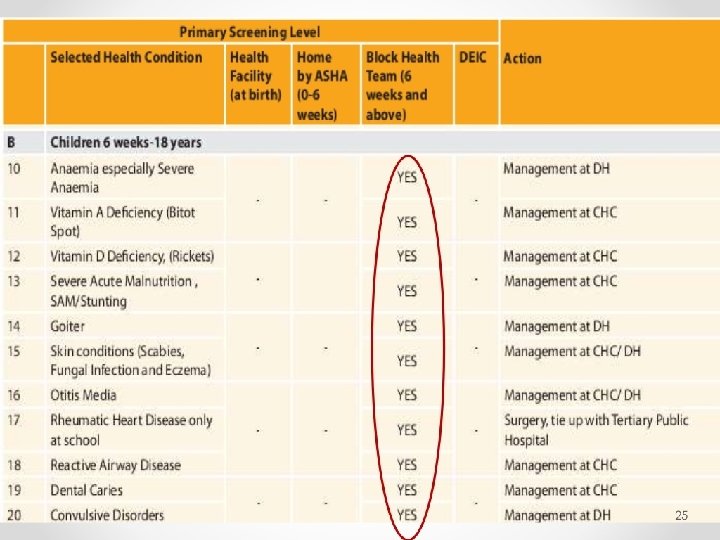
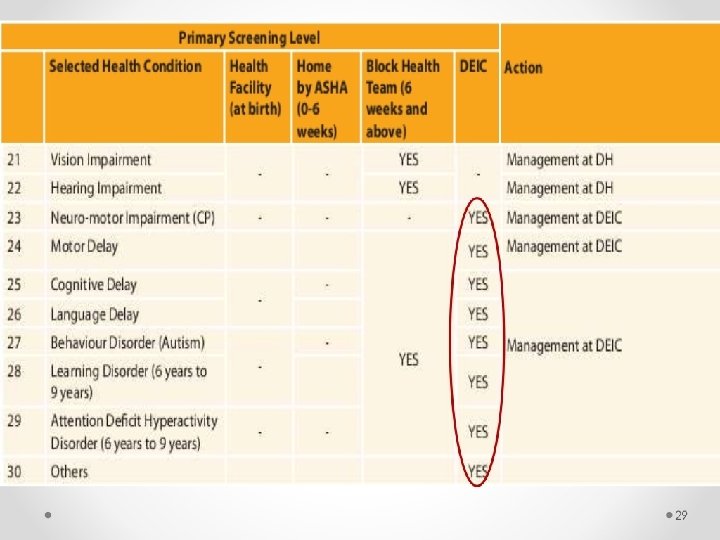
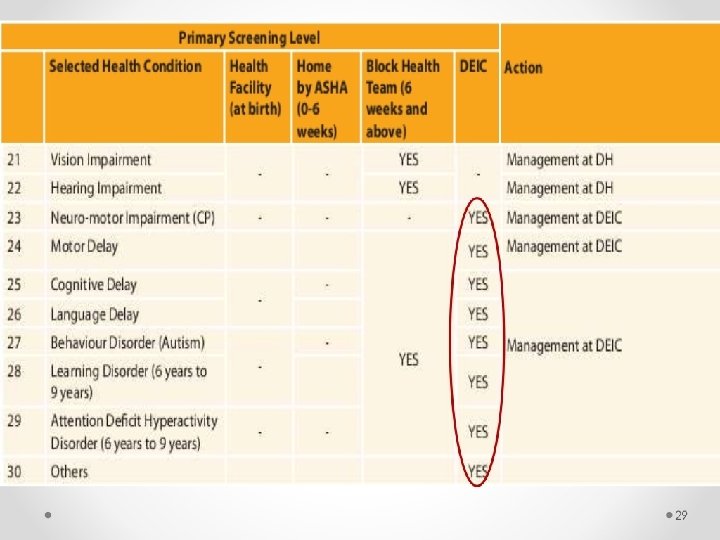
Childhood Diseases Developmental Delays and Disabilities 15 Skin conditions (Scabies, Fungal Infection and Eczema) 21 Vision Impairment 16 Otitis Media 22 Hearing Impairment 17 Rheumatic Heart Disease 23 Neuro-Motor Impairment 18 Reactive Airway Disease 24 Motor Delay 19 Dental Caries 25 Cognitive Delay 20 Convulsive Disorders 26 Language Delay 27 Behaviour Disorder (Autism) 28 Learning Disorder 29 Attention Deficit Hyperactivity Disorder 30 Congenital Hypothyroidism, Sickle Cell Anaemia, Beta Thalassemia (Optional)
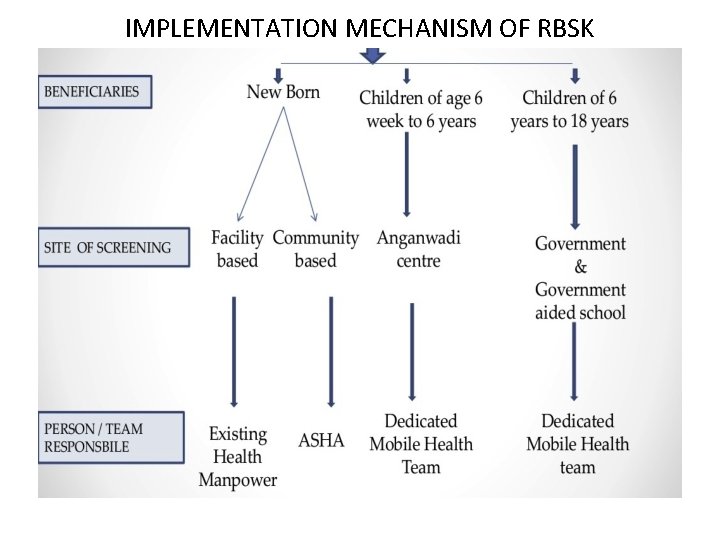
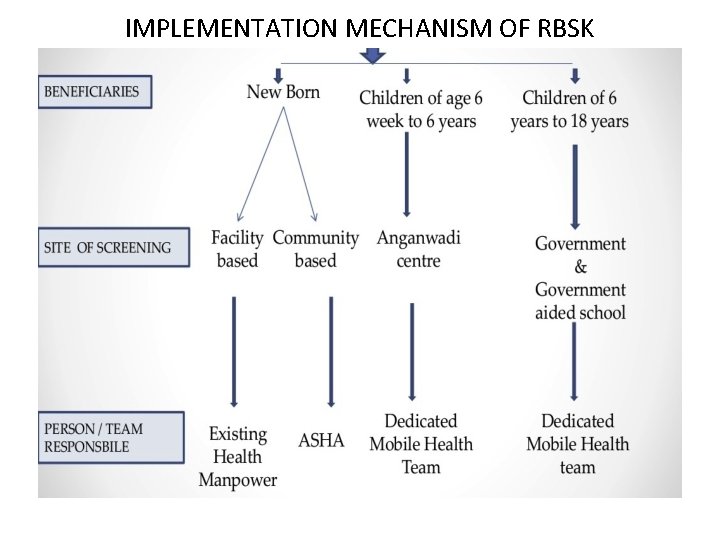
IMPLEMENTATION MECHANISM OF RBSK
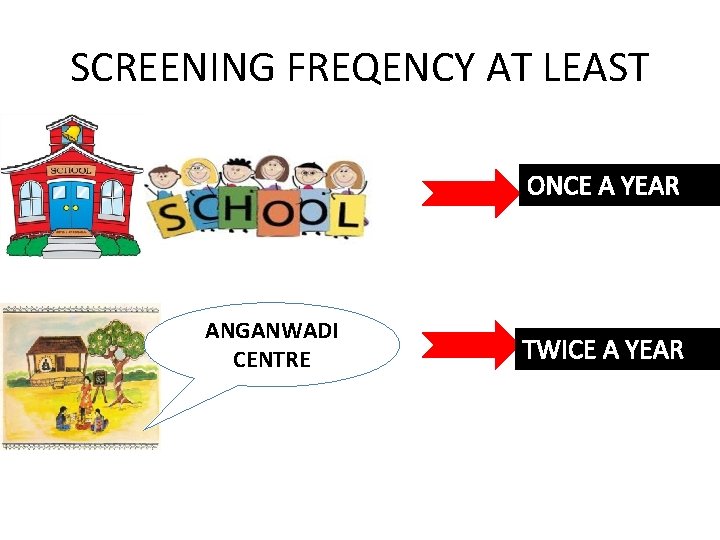
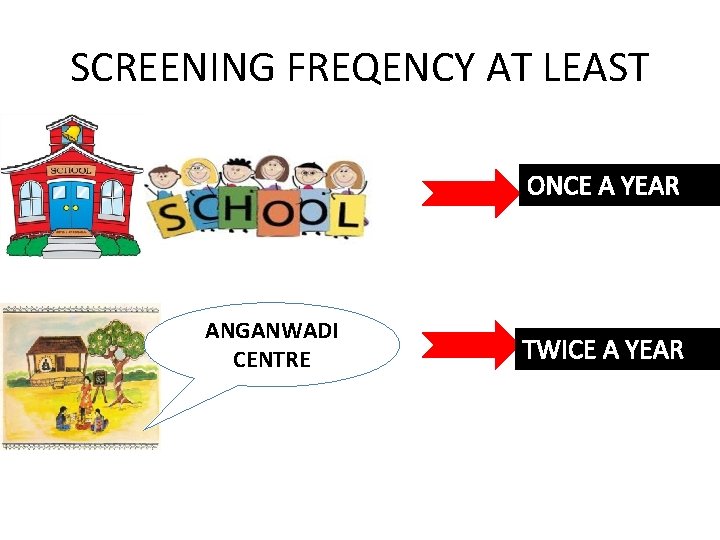
SCREENING FREQENCY AT LEAST ONCE A YEAR ANGANWADI CENTRE TWICE A YEAR
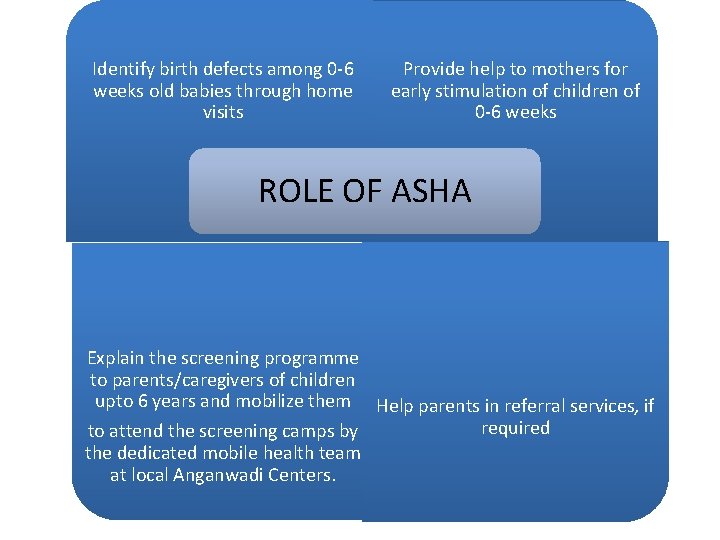
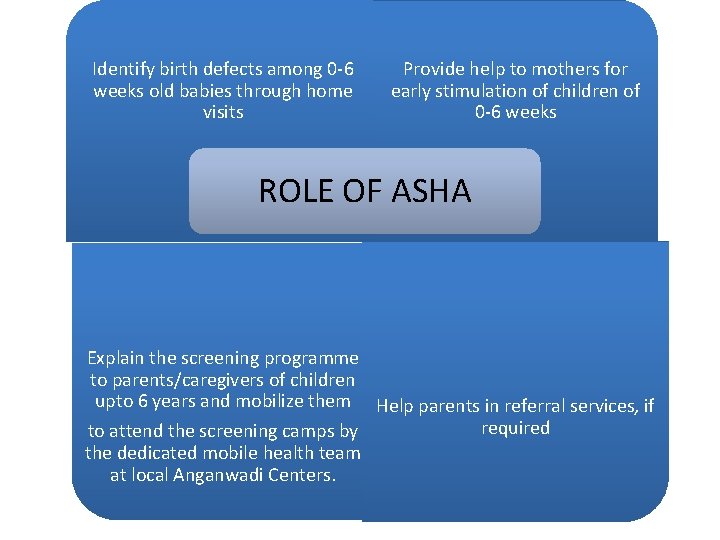
Identify birth defects among 0 -6 weeks old babies through home visits Provide help to mothers for early stimulation of children of 0 -6 weeks ROLE OF ASHA Explain the screening programme to parents/caregivers of children upto 6 years and mobilize them Help parents in referral services, if required to attend the screening camps by the dedicated mobile health team at local Anganwadi Centers.
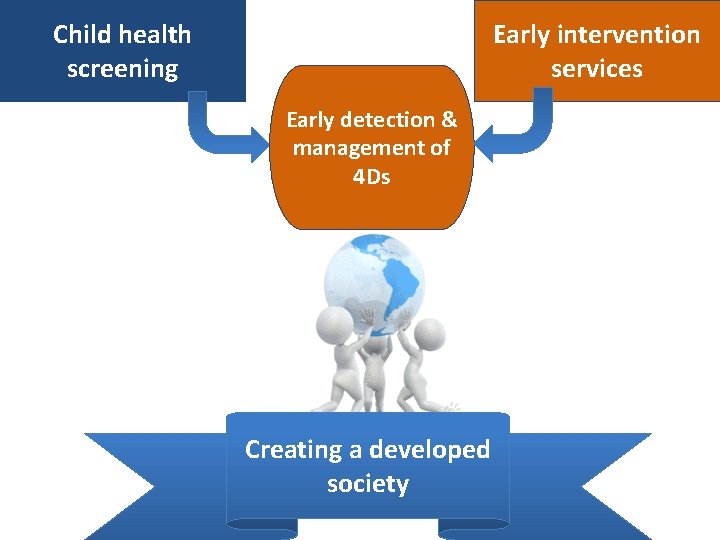
Benefits • Halt the condition from further deterioration • Reduce economic burden • Country wide epidemiological data for planning • Creating a developed society, agile and able to compete with the rest of the world
MCQ 4 • RBSY stands for ? enumerate 4 D
MCQ 5 • • • Which among these is not a birth defect? A. Talipes (CTEV) B. Retinopathy of Prematurity C. Attention Deficit Hyperactivity Disorder D. Downs Syndrome
Child health screening Early intervention services Early detection & management of 4 Ds Creating a developed society
Thank you
 Middle childhood
Middle childhood Performance cycle uncertainty
Performance cycle uncertainty Tyler godoff
Tyler godoff Risk management framework hse
Risk management framework hse Integrated watershed management
Integrated watershed management Integrated university management system
Integrated university management system Integrated talent management scorecards
Integrated talent management scorecards Ism integrated service management
Ism integrated service management Ipm integrated project management
Ipm integrated project management Pas 99 adalah
Pas 99 adalah Enterprise wide quality integrated management system
Enterprise wide quality integrated management system Integrated pest management objectives
Integrated pest management objectives Integrated educational information management system
Integrated educational information management system Power management integrated circuits
Power management integrated circuits Integrated management information system imis
Integrated management information system imis Integrated clinical services management
Integrated clinical services management Integrated brand promotion (ibp) is
Integrated brand promotion (ibp) is Integrated engineering management system
Integrated engineering management system Avaya integrated management site administration
Avaya integrated management site administration Integrated project portfolio management
Integrated project portfolio management What is integrated safety management system
What is integrated safety management system Summary sheet of iqms scores
Summary sheet of iqms scores Advantages of integrated weed management
Advantages of integrated weed management Ibm thin client
Ibm thin client Integrated health information system
Integrated health information system Gifmis modules
Gifmis modules Integrated financial management system
Integrated financial management system Integrated risk management consulting
Integrated risk management consulting Integrated plant nutrient system
Integrated plant nutrient system Integrated pest management
Integrated pest management Civil integrated management
Civil integrated management Integrated pest management
Integrated pest management Integrated pest management ____ than pesticides
Integrated pest management ____ than pesticides Iaea gsr part 2
Iaea gsr part 2 What is the third step in integrated pest management?
What is the third step in integrated pest management? Integrated logistics management
Integrated logistics management Integrated information management
Integrated information management Ifms integrated financial management system
Ifms integrated financial management system Building integrated management
Building integrated management Enterprise risk management integrated framework
Enterprise risk management integrated framework Integrated service management
Integrated service management William shakespeare childhood
William shakespeare childhood Social construction of childhood
Social construction of childhood Carol ann duffy we remember your childhood well
Carol ann duffy we remember your childhood well Walt disneys childhood
Walt disneys childhood Social development in infancy and childhood
Social development in infancy and childhood Types of early childhood programs
Types of early childhood programs Chapter 2 types of early childhood programs
Chapter 2 types of early childhood programs