INSULIN THERAPY AND NUTRITIONAL MANAGEMENT IN PATIENTS WITH



- Slides: 47
INSULIN THERAPY AND NUTRITIONAL MANAGEMENT IN PATIENTS WITH DIABETES MELLITUS IN THE PERIOPERATIVE PERIOD Josephine Carlos-Raboca MD FPCP Gabriel V. Jasul MD FPCP FPSEM Rosa Allyn G. Sy MD FPCP FPSEM Leilani B. Mercado-Asis, M. D. , Ph. D. FPCP FPSEM
Insulin Therapy and Hyperglycemia in Hospitalized Patients Dr. Josephine Carlos-Raboca Dr. Leilani B. Mercado-Asis
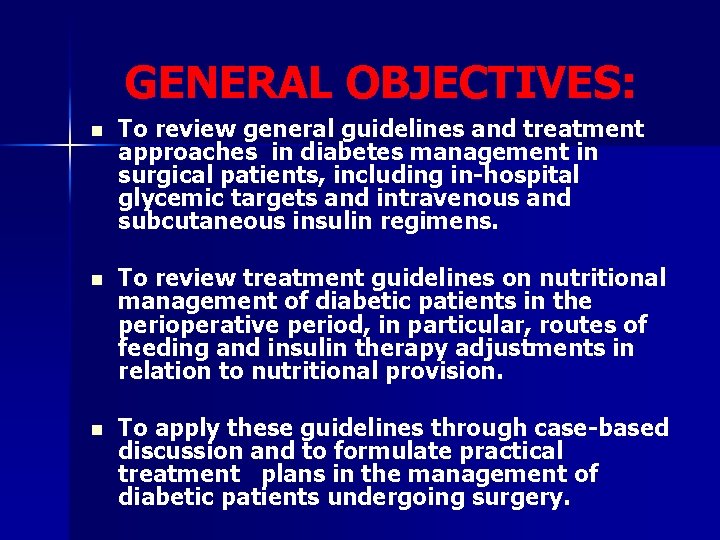
GENERAL OBJECTIVES: n To review general guidelines and treatment approaches in diabetes management in surgical patients, including in-hospital glycemic targets and intravenous and subcutaneous insulin regimens. n To review treatment guidelines on nutritional management of diabetic patients in the perioperative period, in particular, routes of feeding and insulin therapy adjustments in relation to nutritional provision. n To apply these guidelines through case-based discussion and to formulate practical treatment plans in the management of diabetic patients undergoing surgery.
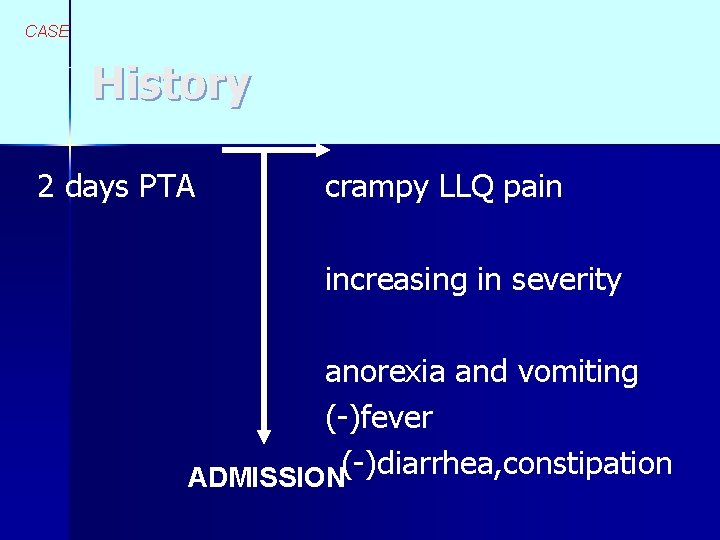
Case VS, 62 M n Type 2 DM X 3 yrs n – Rx: Glibenclamide 5 mg OD Metformin 500 mg BID n admitted due to abdominal pain
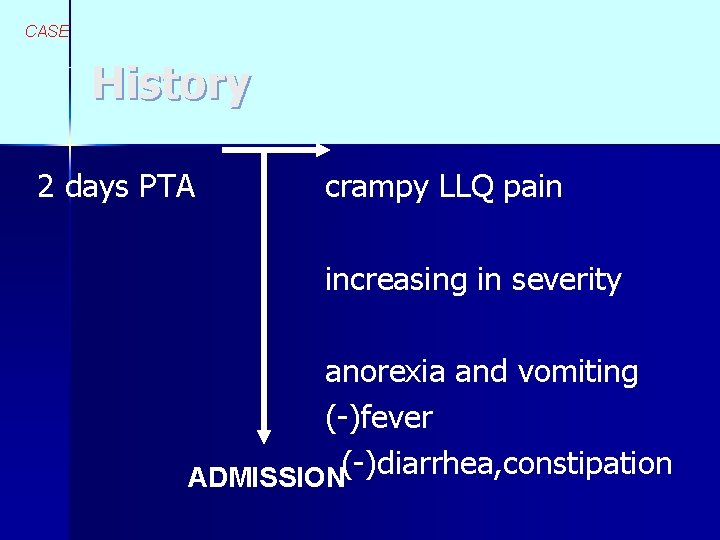
CASE History 2 days PTA crampy LLQ pain increasing in severity anorexia and vomiting (-)fever ADMISSION(-)diarrhea, constipation
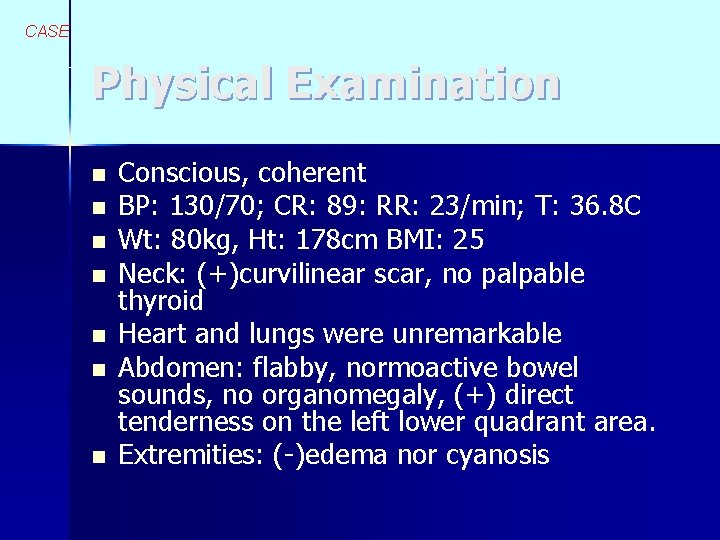
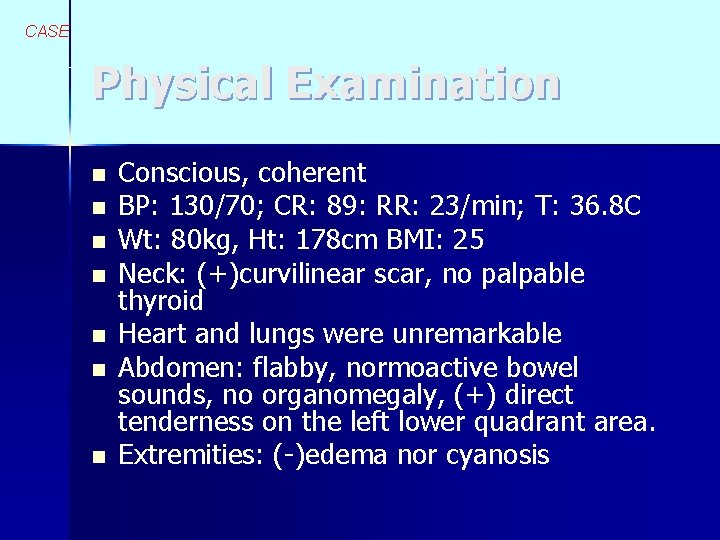
CASE Physical Examination n n n Conscious, coherent BP: 130/70; CR: 89: RR: 23/min; T: 36. 8 C Wt: 80 kg, Ht: 178 cm BMI: 25 Neck: (+)curvilinear scar, no palpable thyroid Heart and lungs were unremarkable Abdomen: flabby, normoactive bowel sounds, no organomegaly, (+) direct tenderness on the left lower quadrant area. Extremities: (-)edema nor cyanosis
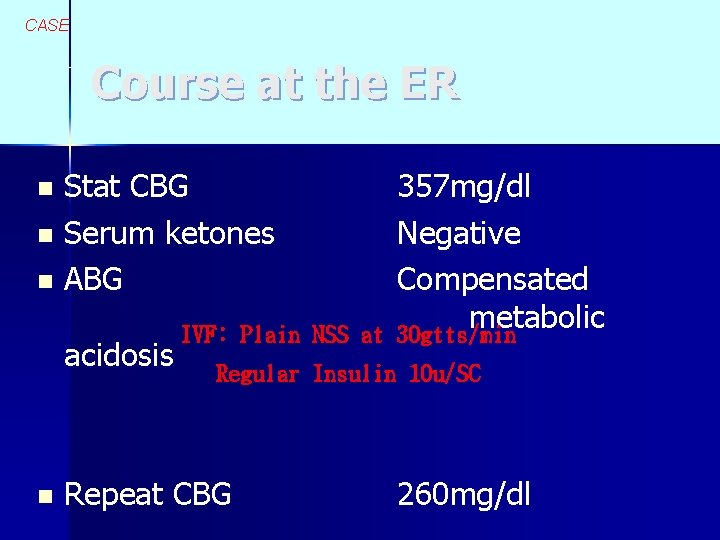
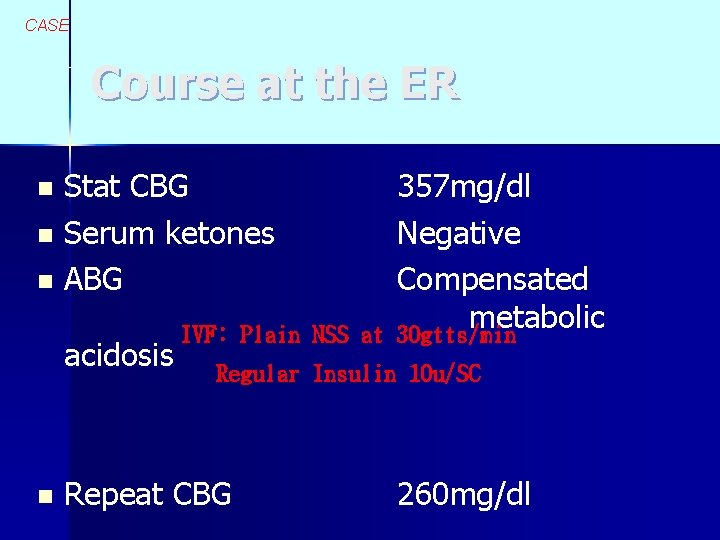
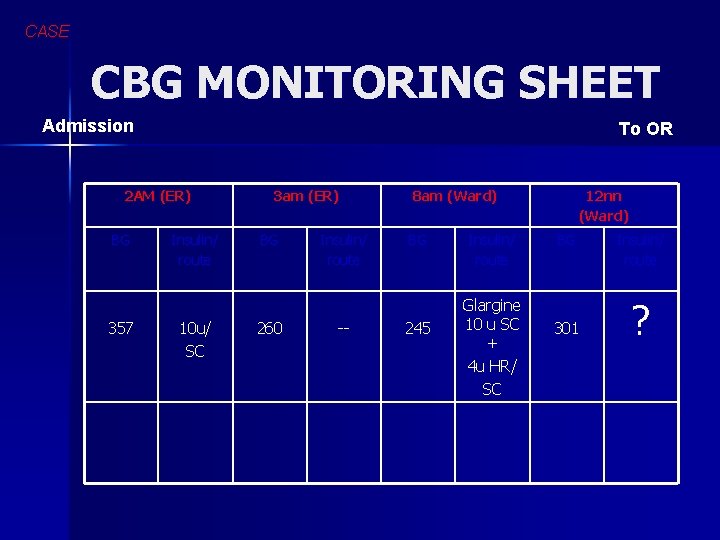
CASE Course at the ER Stat CBG n Serum ketones n ABG n acidosis n IVF: Plain NSS at 357 mg/dl Negative Compensated metabolic 30 gtts/min Regular Insulin 10 u/SC Repeat CBG 260 mg/dl
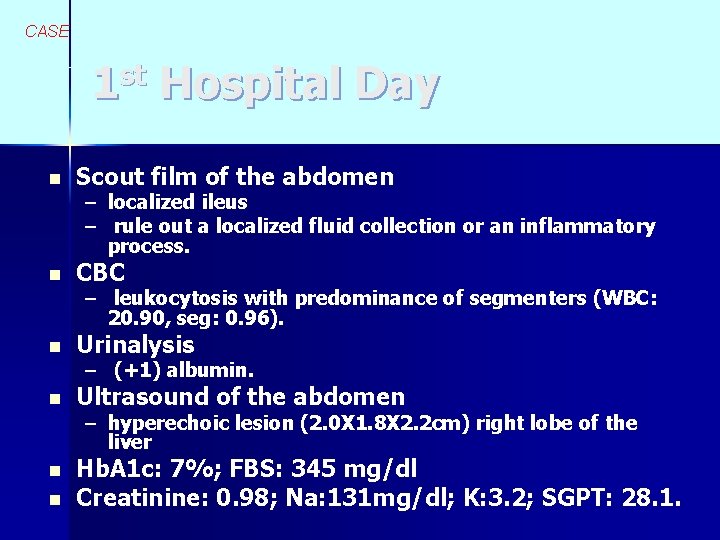
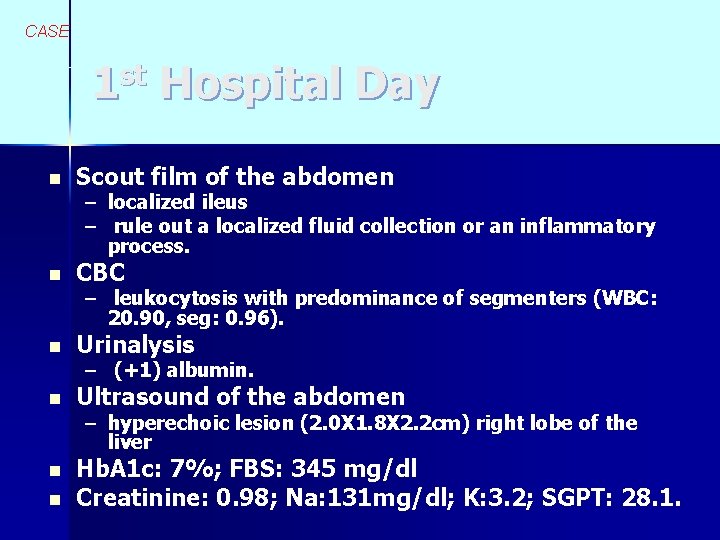
CASE 1 st Hospital Day n Scout film of the abdomen n CBC n Urinalysis n Ultrasound of the abdomen n Hb. A 1 c: 7%; FBS: 345 mg/dl Creatinine: 0. 98; Na: 131 mg/dl; K: 3. 2; SGPT: 28. 1. n – localized ileus – rule out a localized fluid collection or an inflammatory process. – leukocytosis with predominance of segmenters (WBC: 20. 90, seg: 0. 96). – (+1) albumin. – hyperechoic lesion (2. 0 X 1. 8 X 2. 2 cm) right lobe of the liver
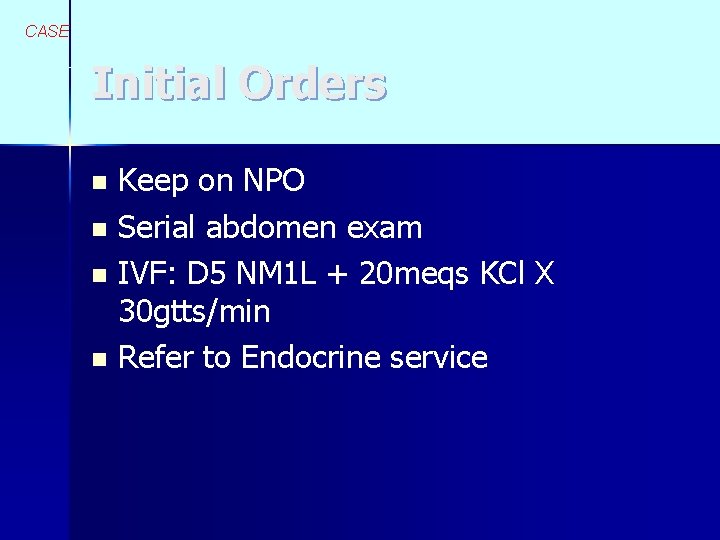
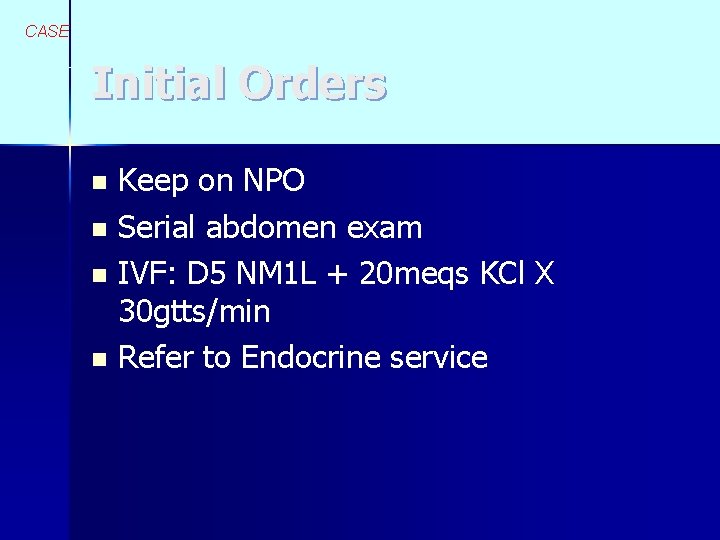
CASE Initial Orders Keep on NPO n Serial abdomen exam n IVF: D 5 NM 1 L + 20 meqs KCl X 30 gtts/min n Refer to Endocrine service n
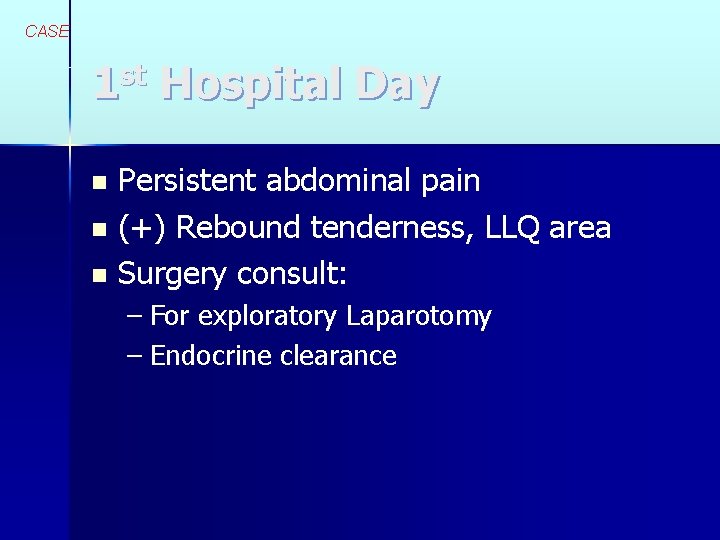
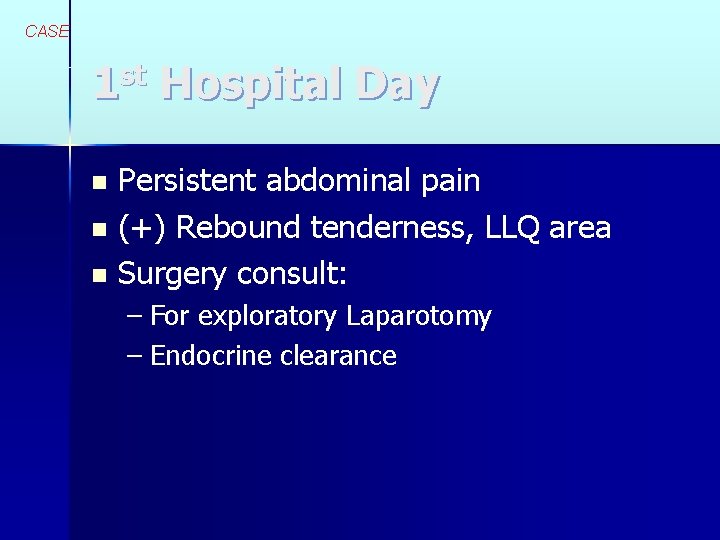
CASE 1 st Hospital Day Persistent abdominal pain n (+) Rebound tenderness, LLQ area n Surgery consult: n – For exploratory Laparotomy – Endocrine clearance
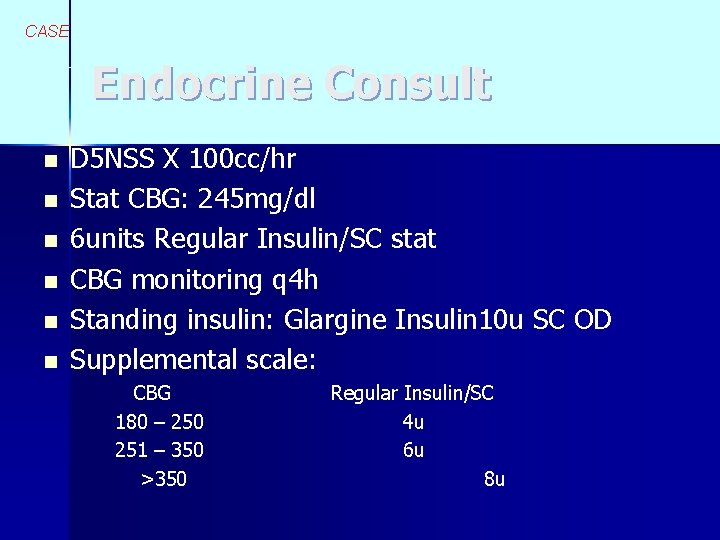
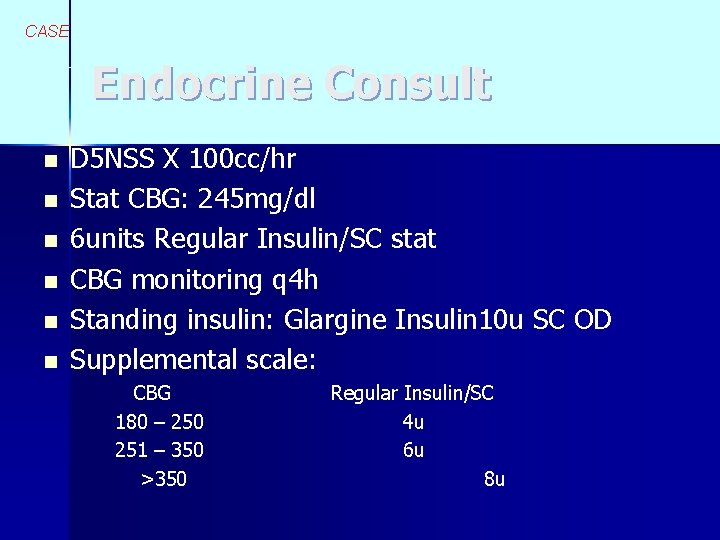
CASE Endocrine Consult n n n D 5 NSS X 100 cc/hr Stat CBG: 245 mg/dl 6 units Regular Insulin/SC stat CBG monitoring q 4 h Standing insulin: Glargine Insulin 10 u SC OD Supplemental scale: CBG 180 – 250 251 – 350 >350 Regular Insulin/SC 4 u 6 u 8 u
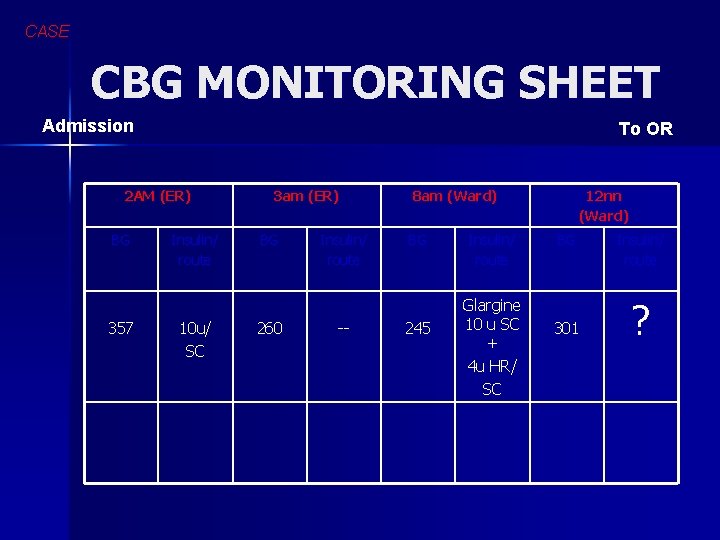
CASE CBG MONITORING SHEET Admission To OR 2 AM (ER) BG 357 Insulin/ route 10 u/ SC 3 am (ER) BG 260 Insulin/ route -- 8 am (Ward) BG 245 Insulin/ route Glargine 10 u SC + 4 u HR/ SC 12 nn (Ward) BG 301 Insulin/ route ?
REVIEW GENERAL PRINCIPLES OF PERIOPERATIVE MANAGEMENT OF DIABETES MELLITUS, INCLUDING NUTRITION SUPPORT, CHOICE OF TYPE AND ROUTE OF INSULIN ADMINISTRATION, FREQUENCY OF MONITORING AND FLUID MANAGEMENT
Objective # 3 REVIEW GENERAL PRINCIPLES OF PERIOPERATIVE MANAGEMENT OF DIABETES MELLITUS, INCLUDING CHOICE OF, TYPE AND ROUTE OF INSULIN ADMINISTRATION, FREQUENCY OF MONITORING AND FLUID MANAGEMENT
GENERAL PRINCIPLES OF PERIOPERATIVE MANAGEMENT OF DIABETES MELLITUS n n n Oral agents may be contraindicated Dose adjustment of oral agents may require time and may be ineffective Stress, intravenous dextrose, and enteral feedings, may increase dose requirements for exogenous insulin Pattern of carbohydrate exposure may change, necessitating pattern adjustment of insulin therapy Nutritional assessment is important
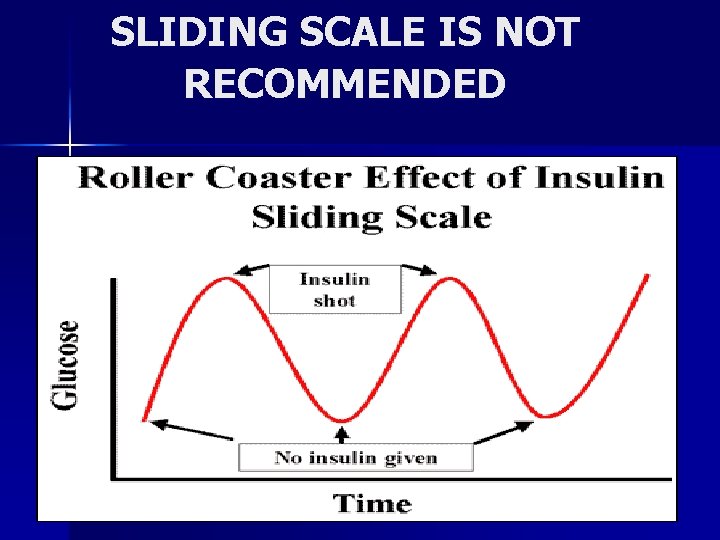
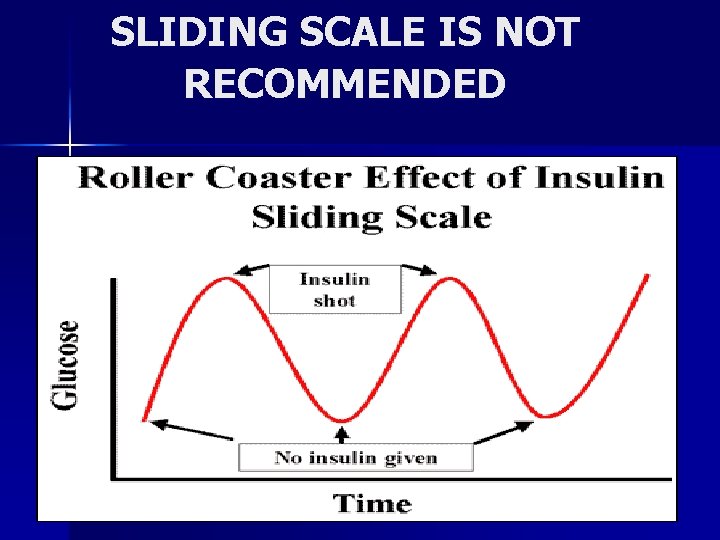
SLIDING SCALE IS NOT RECOMMENDED
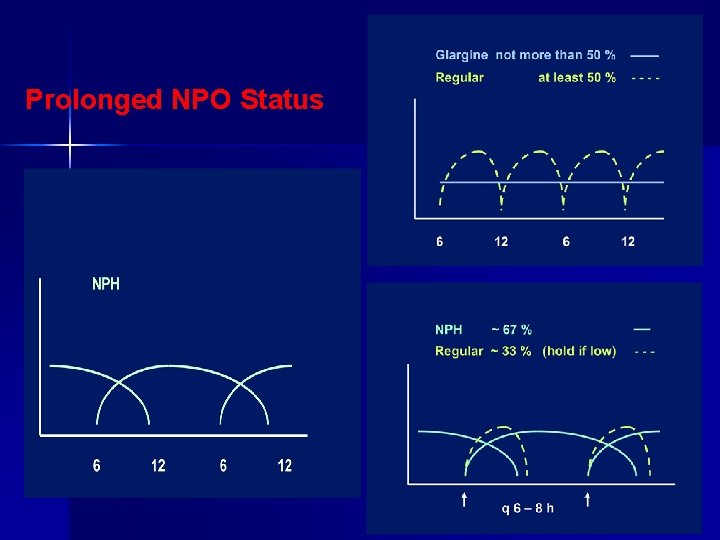
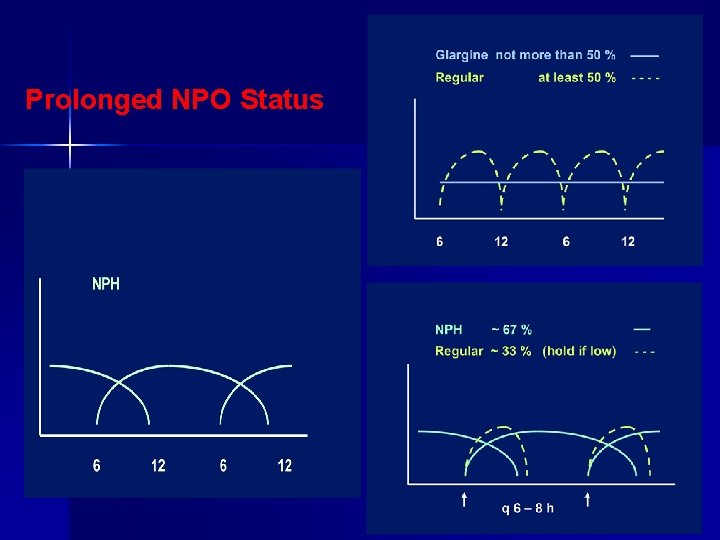
Prolonged NPO Status.
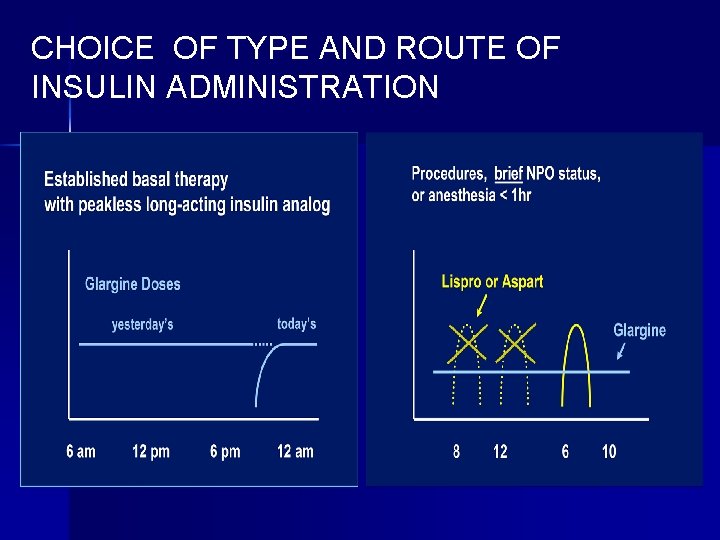
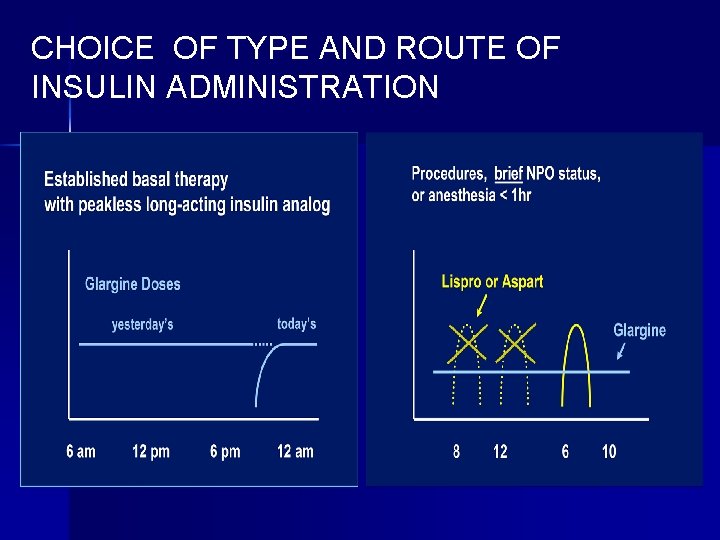
CHOICE OF TYPE AND ROUTE OF INSULIN ADMINISTRATION
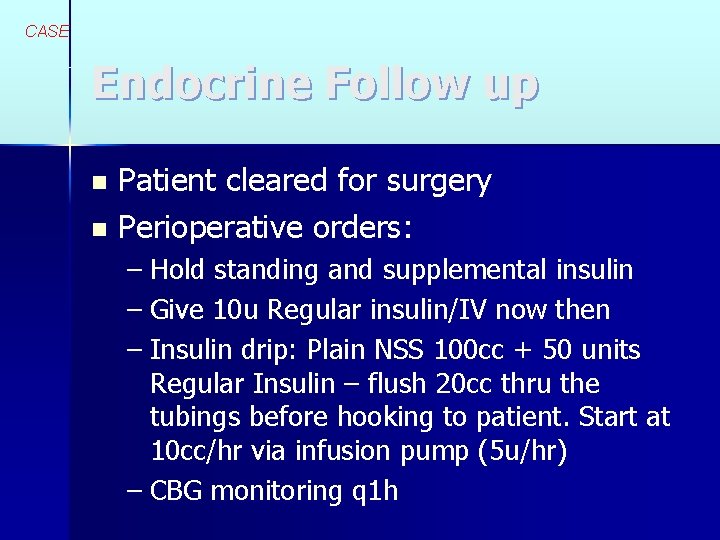
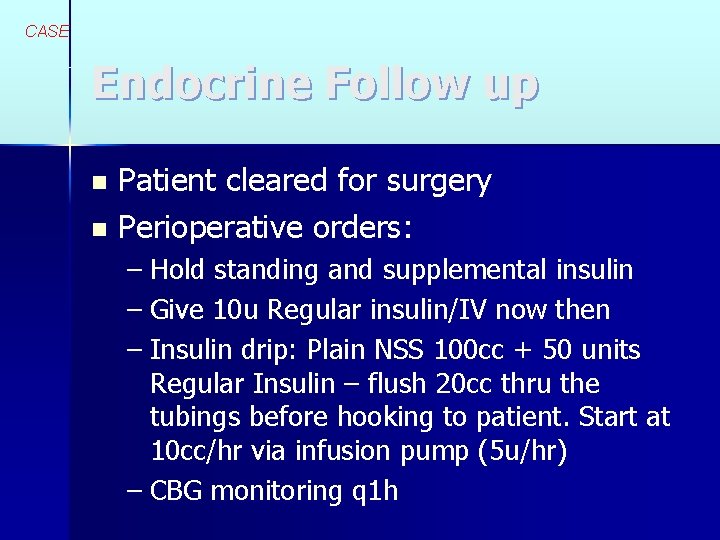
CASE Endocrine Follow up Patient cleared for surgery n Perioperative orders: n – Hold standing and supplemental insulin – Give 10 u Regular insulin/IV now then – Insulin drip: Plain NSS 100 cc + 50 units Regular Insulin – flush 20 cc thru the tubings before hooking to patient. Start at 10 cc/hr via infusion pump (5 u/hr) – CBG monitoring q 1 h
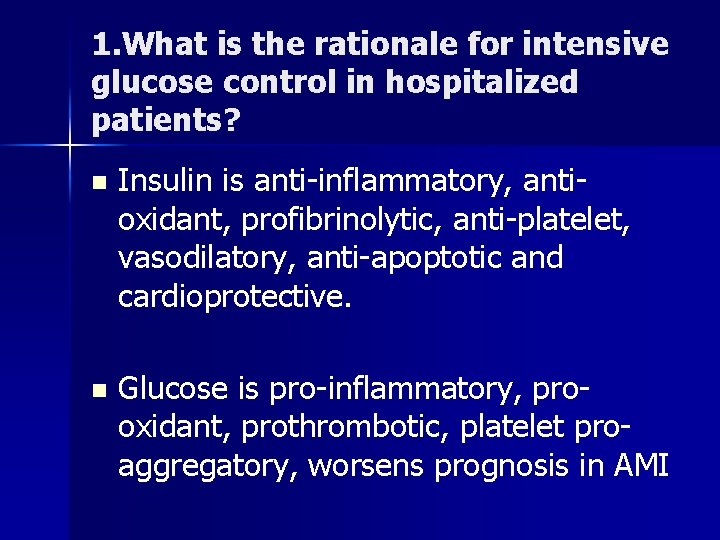
Objective # 1 Review rationale for intensive glucose control in hospitalized patients and in particular, in surgical patients
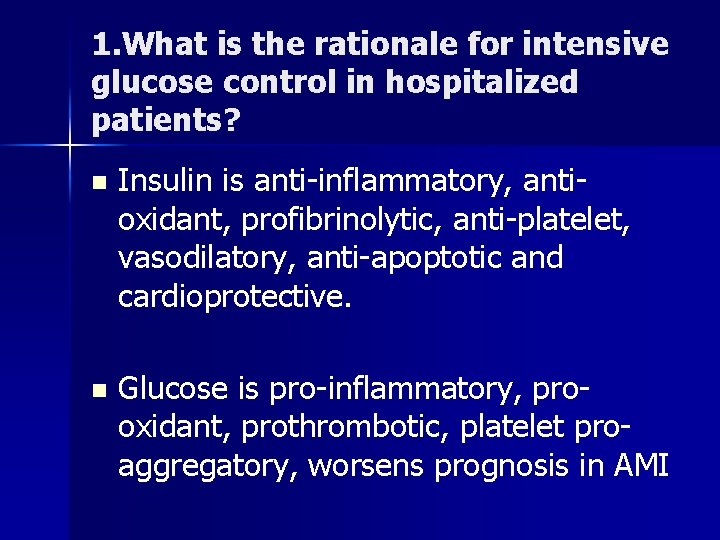
1. What is the rationale for intensive glucose control in hospitalized patients? n Insulin is anti-inflammatory, antioxidant, profibrinolytic, anti-platelet, vasodilatory, anti-apoptotic and cardioprotective. n Glucose is pro-inflammatory, prooxidant, prothrombotic, platelet proaggregatory, worsens prognosis in AMI
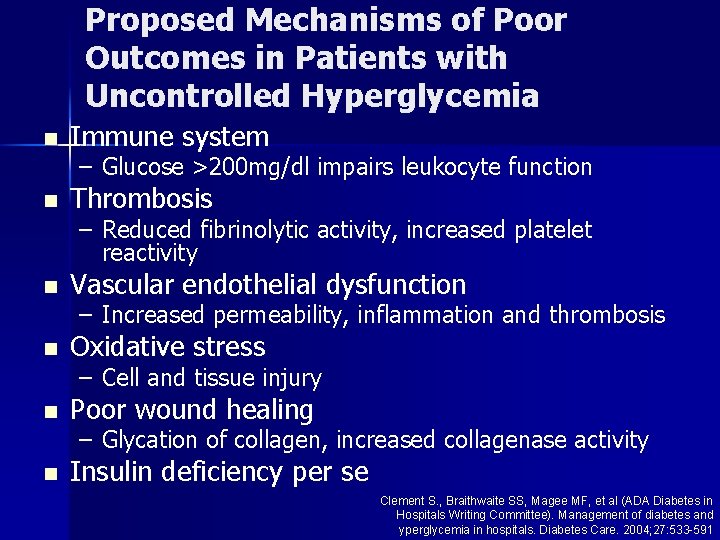
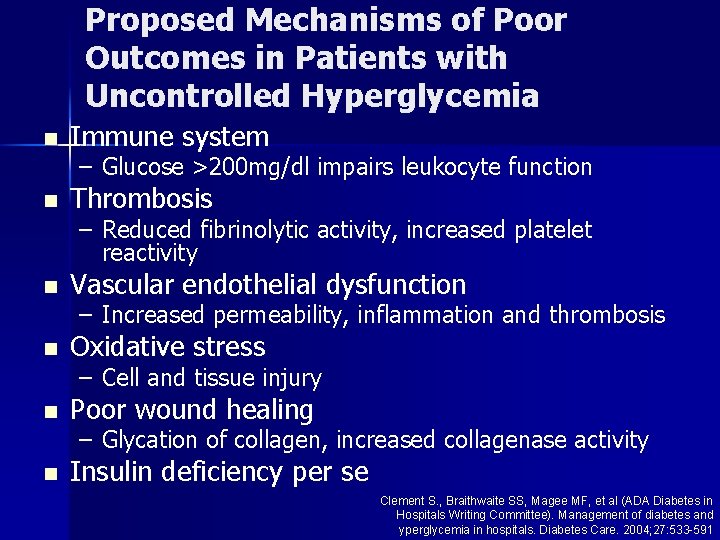
Proposed Mechanisms of Poor Outcomes in Patients with Uncontrolled Hyperglycemia n Immune system n Thrombosis n Vascular endothelial dysfunction n Oxidative stress n Poor wound healing n Insulin deficiency per se – Glucose >200 mg/dl impairs leukocyte function – Reduced fibrinolytic activity, increased platelet reactivity – Increased permeability, inflammation and thrombosis – Cell and tissue injury – Glycation of collagen, increased collagenase activity Clement S. , Braithwaite SS, Magee MF, et al (ADA Diabetes in Hospitals Writing Committee). Management of diabetes and yperglycemia in hospitals. Diabetes Care. 2004; 27: 533 -591
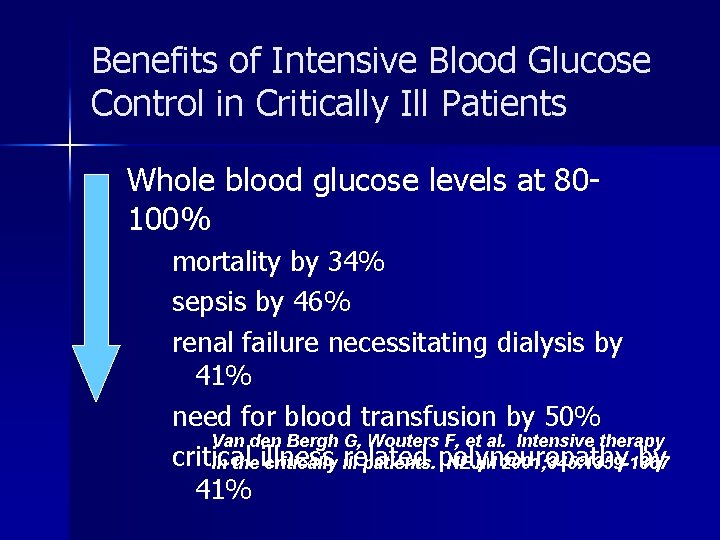
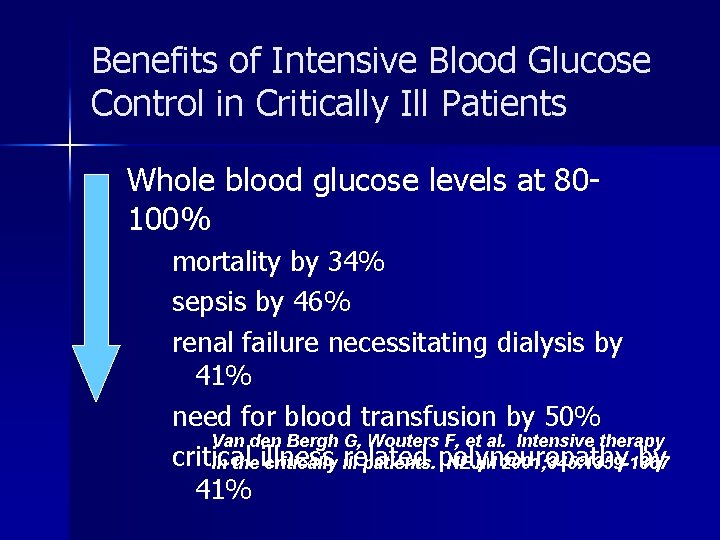
Benefits of Intensive Blood Glucose Control in Critically Ill Patients n Whole blood glucose levels at 80100% mortality by 34% sepsis by 46% renal failure necessitating dialysis by 41% need for blood transfusion by 50% Van den Bergh G, Wouters F, et al. Intensive therapy critical related by in the illness critically ill patients. polyneuropathy NEJM 2001; 345: 1359 -1367 41%
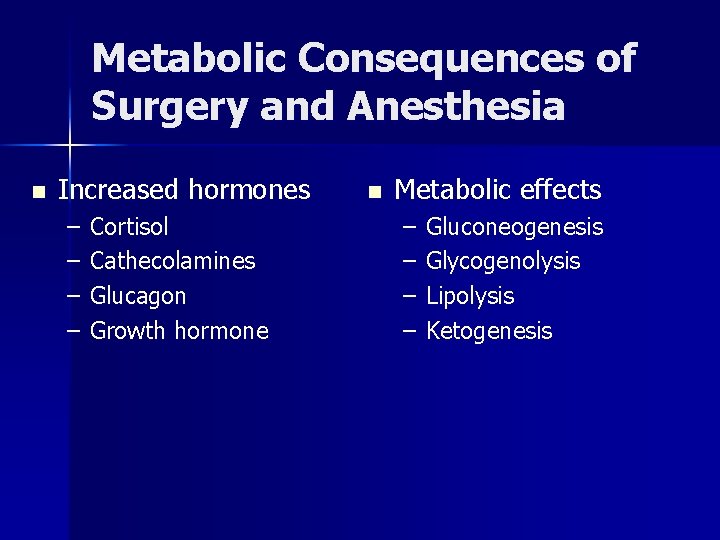
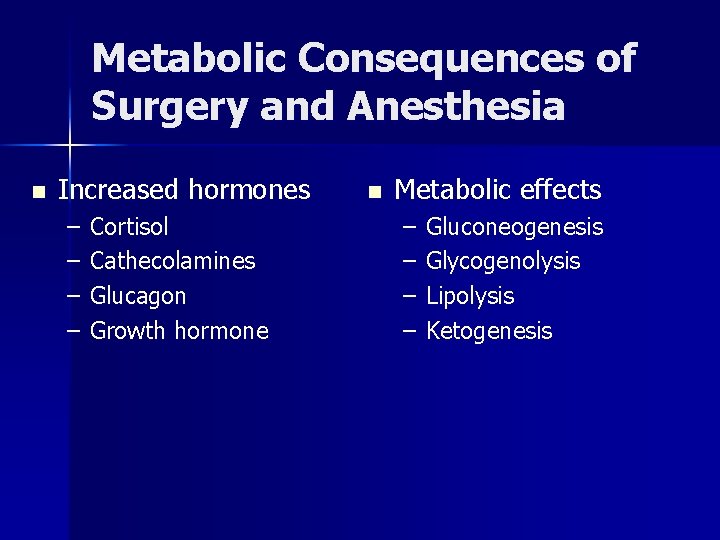
Metabolic Consequences of Surgery and Anesthesia n Increased hormones – – Cortisol Cathecolamines Glucagon Growth hormone n Metabolic effects – – Gluconeogenesis Glycogenolysis Lipolysis Ketogenesis
Objective # 2 DEFINE INTENSIVE GLUCOSE CONTROL IN HOSPITALIZED PATIENTS AND SET GLYCEMIC TARGETS IN THE SURGICAL PATIENTS
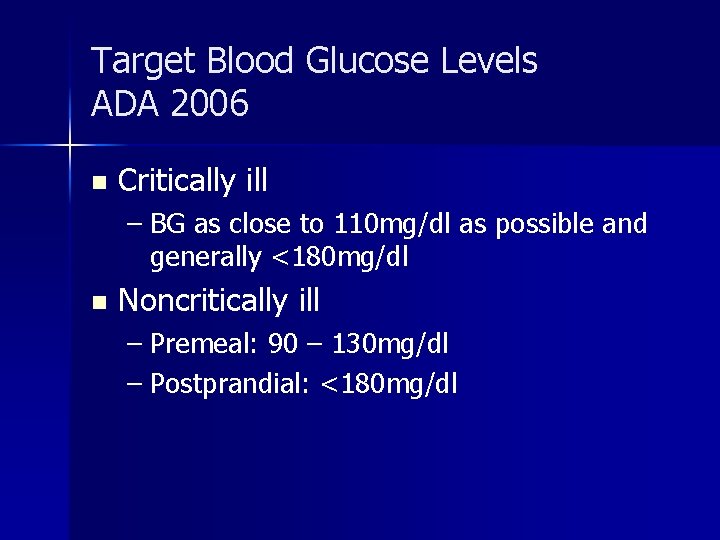
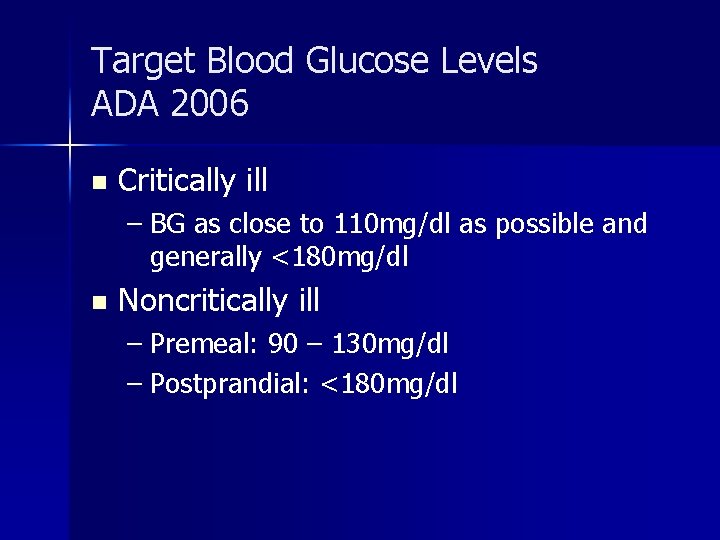
Target Blood Glucose Levels ADA 2006 n Critically ill – BG as close to 110 mg/dl as possible and generally <180 mg/dl n Noncritically ill – Premeal: 90 – 130 mg/dl – Postprandial: <180 mg/dl
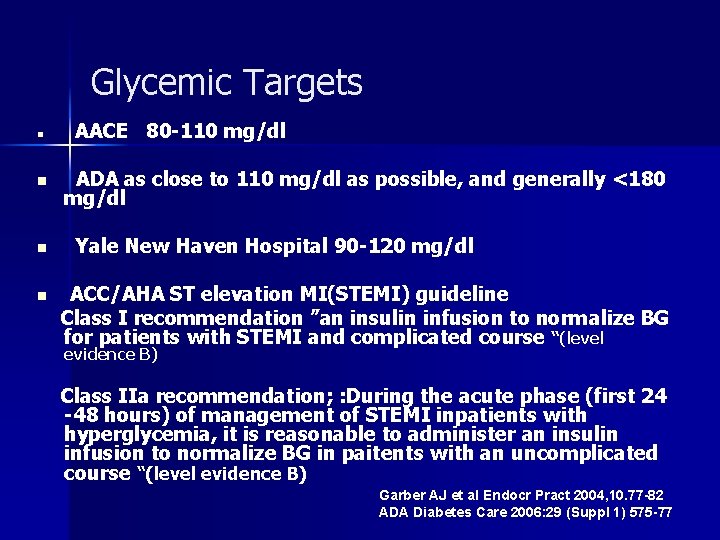
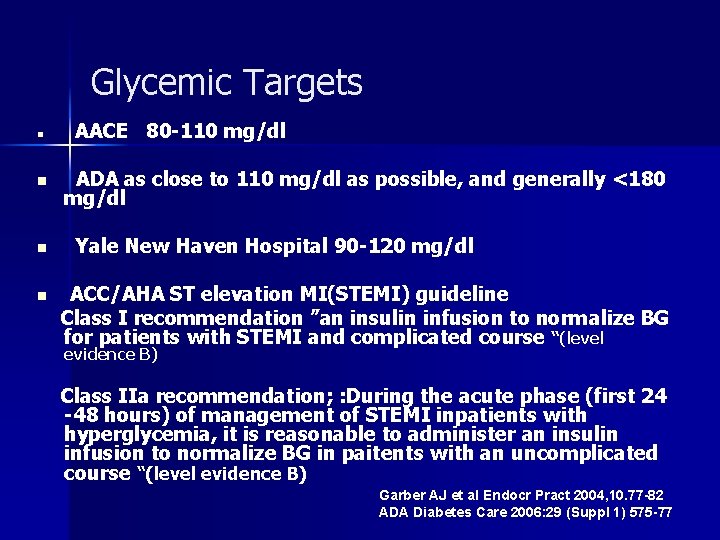
Glycemic Targets n n AACE 80 -110 mg/dl ADA as close to 110 mg/dl as possible, and generally <180 mg/dl Yale New Haven Hospital 90 -120 mg/dl ACC/AHA ST elevation MI(STEMI) guideline Class I recommendation ”an insulin infusion to normalize BG for patients with STEMI and complicated course “(level evidence B) Class IIa recommendation; : During the acute phase (first 24 -48 hours) of management of STEMI inpatients with hyperglycemia, it is reasonable to administer an insulin infusion to normalize BG in paitents with an uncomplicated course “(level evidence B) Garber AJ et al Endocr Pract 2004, 10. 77 -82 ADA Diabetes Care 2006: 29 (Suppl 1) 575 -77
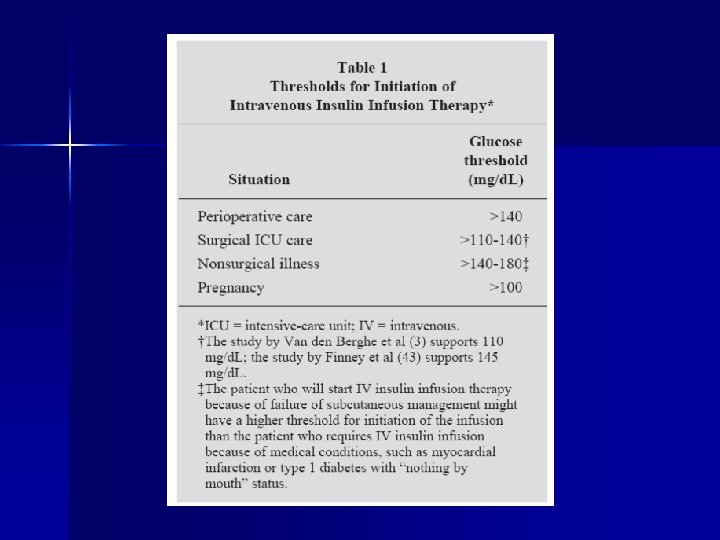
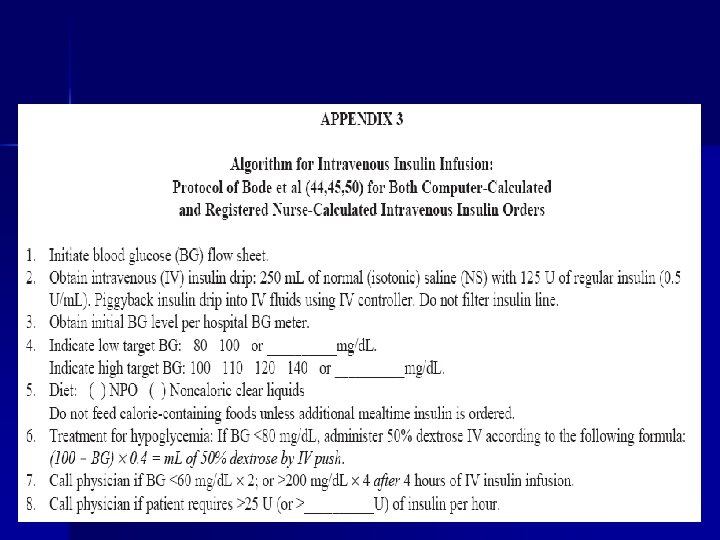
Objective # 4 REVIEW INTRAVENOUS INSULIN PROTOCOLS CURRENTLY IN USE AND DETERMINE THEIR FEASIBILITY FOR USE IN OUR SETTING
Various protocols Atlanta Multiplier method n Van den Berghe (studied in critical care setting) n Portland Protocol (used in surgical setting) n Markovitz (studied in post op heart surgery patients) n Yale protocol (studied in medical intensive care setting) n
Insulin (units per hour) = multiplier × (BG - 60) With use of this algorithm manually, the initial multiplier is set at 0. 02, and a BG value is determined every hour in conjunction with calculation of the units of IV insulin therapy per hour. The multiplier is adjusted every hour by 0. 01 to obtain the target BG level—if the result is less than the target, decrease by 0. 01; if within target range, no change is needed; if more than the target and the BG level has not decreased by 25%, increase by 0. 01. The BG is always determined hourly until stable results are achieved; then it is measured every 2 hours.



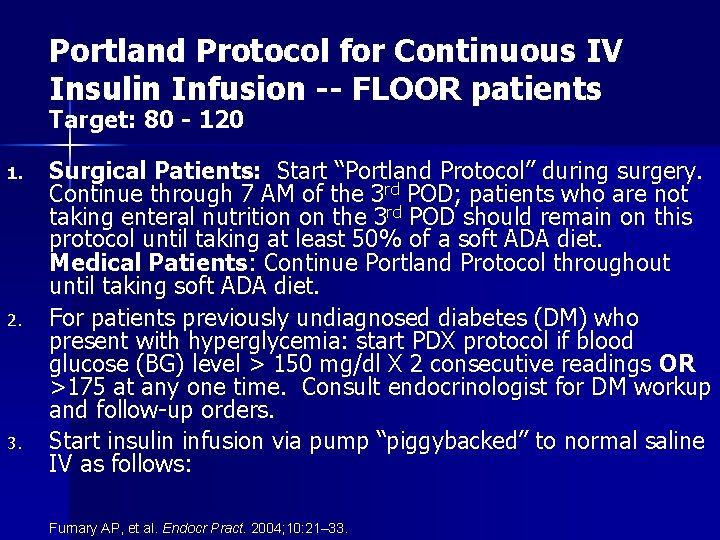
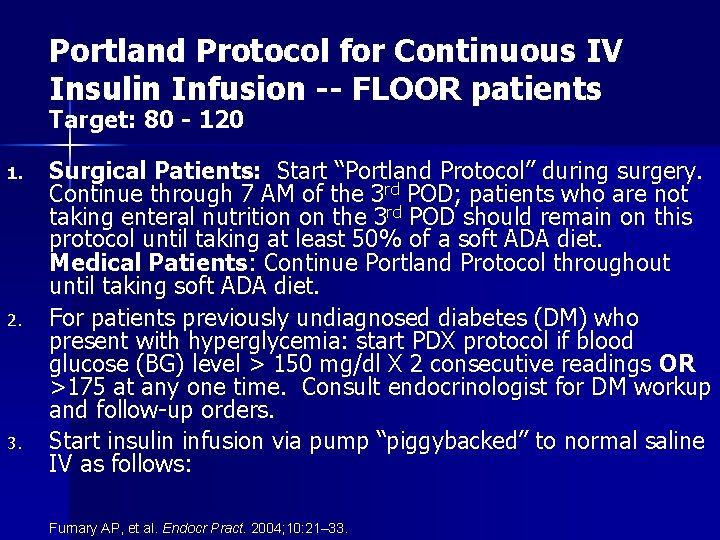
Portland Protocol for Continuous IV Insulin Infusion -- FLOOR patients Target: 80 - 120 1. 2. 3. Surgical Patients: Start “Portland Protocol” during surgery. Continue through 7 AM of the 3 rd POD; patients who are not taking enteral nutrition on the 3 rd POD should remain on this protocol until taking at least 50% of a soft ADA diet. Medical Patients: Continue Portland Protocol throughout until taking soft ADA diet. For patients previously undiagnosed diabetes (DM) who present with hyperglycemia: start PDX protocol if blood glucose (BG) level > 150 mg/dl X 2 consecutive readings OR >175 at any one time. Consult endocrinologist for DM workup and follow-up orders. Start insulin infusion via pump “piggybacked” to normal saline IV as follows: Furnary AP, et al. Endocr Pract. 2004; 10: 21– 33.
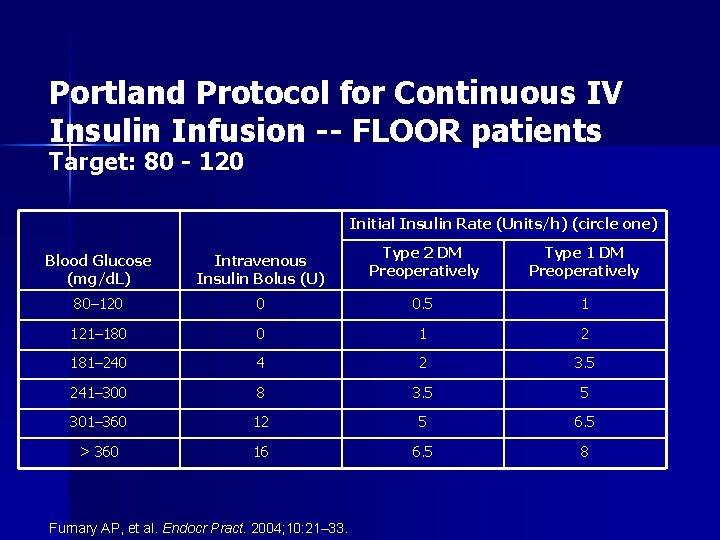
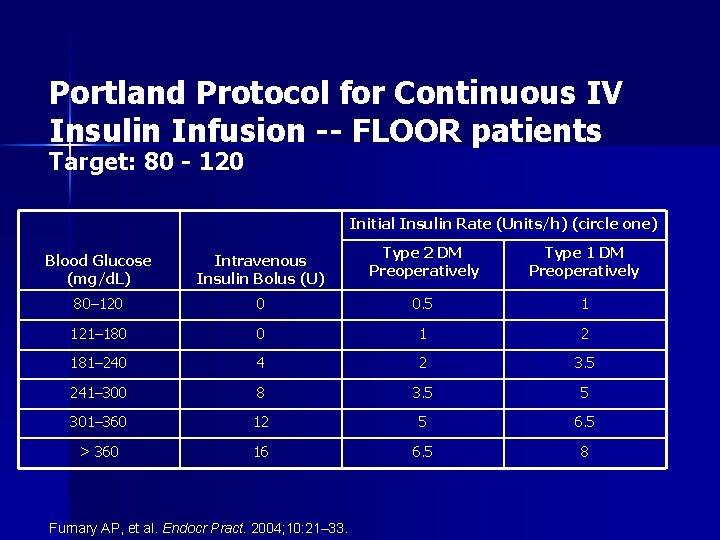
Portland Protocol for Continuous IV Insulin Infusion -- FLOOR patients Target: 80 - 120 Initial Insulin Rate (Units/h) (circle one) Type 2 DM Preoperatively Type 1 DM Preoperatively 0 0. 5 1 121– 180 0 1 2 181– 240 4 2 3. 5 241– 300 8 3. 5 5 301– 360 12 5 6. 5 > 360 16 6. 5 8 Blood Glucose (mg/d. L) Intravenous Insulin Bolus (U) 80– 120 Furnary AP, et al. Endocr Pract. 2004; 10: 21– 33.
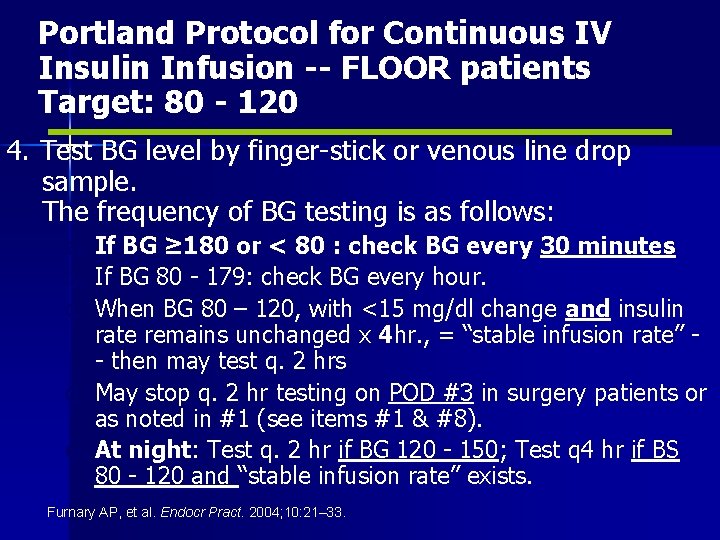
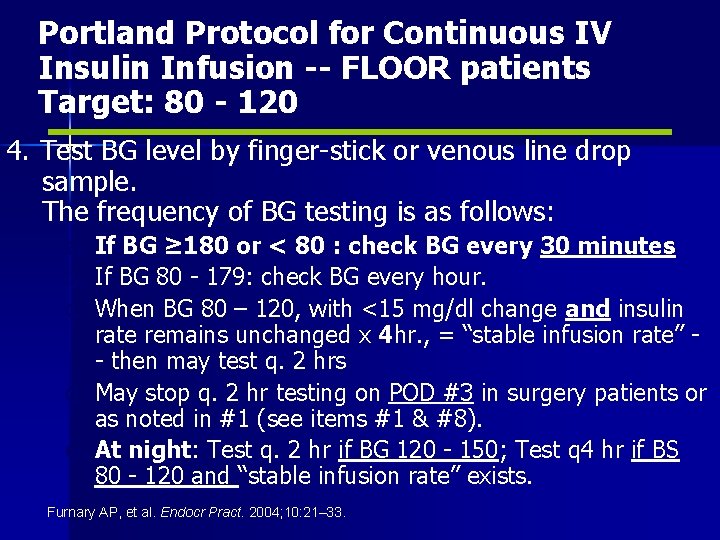
Portland Protocol for Continuous IV Insulin Infusion -- FLOOR patients Target: 80 - 120 4. Test BG level by finger-stick or venous line drop sample. The frequency of BG testing is as follows: a. If BG ≥ 180 or < 80 : check BG every 30 minutes b. If BG 80 - 179: check BG every hour. c. When BG 80 – 120, with <15 mg/dl change and insulin rate remains unchanged x 4 hr. , = “stable infusion rate” - then may test q. 2 hrs d. May stop q. 2 hr testing on POD #3 in surgery patients or as noted in #1 (see items #1 & #8). e. At night: Test q. 2 hr if BG 120 - 150; Test q 4 hr if BS 80 - 120 and “stable infusion rate” exists. Furnary AP, et al. Endocr Pract. 2004; 10: 21– 33.
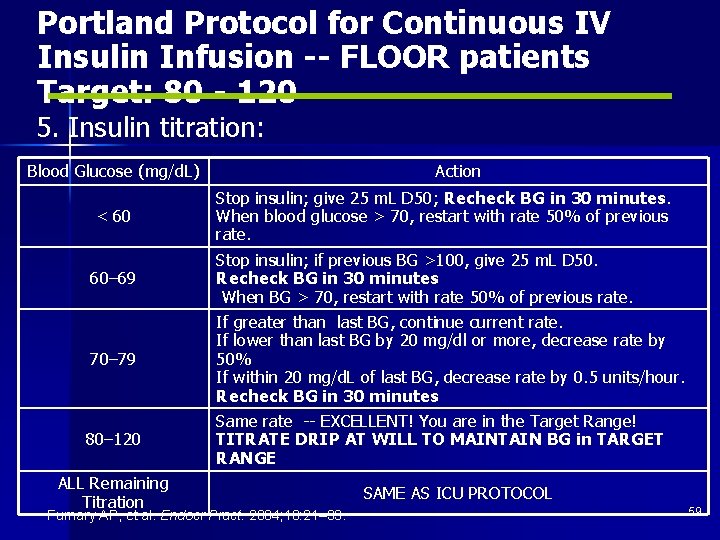
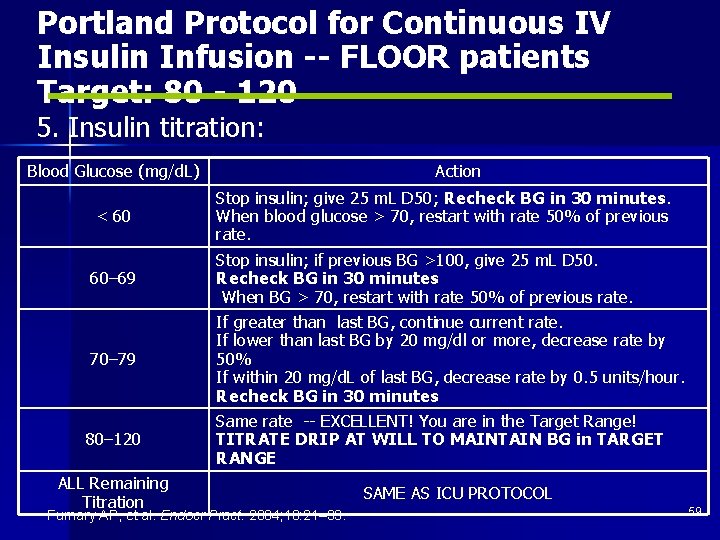
Portland Protocol for Continuous IV Insulin Infusion -- FLOOR patients Target: 80 - 120 5. Insulin titration: Blood Glucose (mg/d. L) < 60 60– 69 70– 79 80– 120 ALL Remaining Titration Action Stop insulin; give 25 m. L D 50; Recheck BG in 30 minutes. When blood glucose > 70, restart with rate 50% of previous rate. Stop insulin; if previous BG >100, give 25 m. L D 50. Recheck BG in 30 minutes When BG > 70, restart with rate 50% of previous rate. If greater than last BG, continue current rate. If lower than last BG by 20 mg/dl or more, decrease rate by 50% If within 20 mg/d. L of last BG, decrease rate by 0. 5 units/hour. Recheck BG in 30 minutes Same rate -- EXCELLENT! You are in the Target Range! TITRATE DRIP AT WILL TO MAINTAIN BG in TARGET RANGE Furnary AP, et al. Endocr Pract. 2004; 10: 21– 33. SAME AS ICU PROTOCOL 59
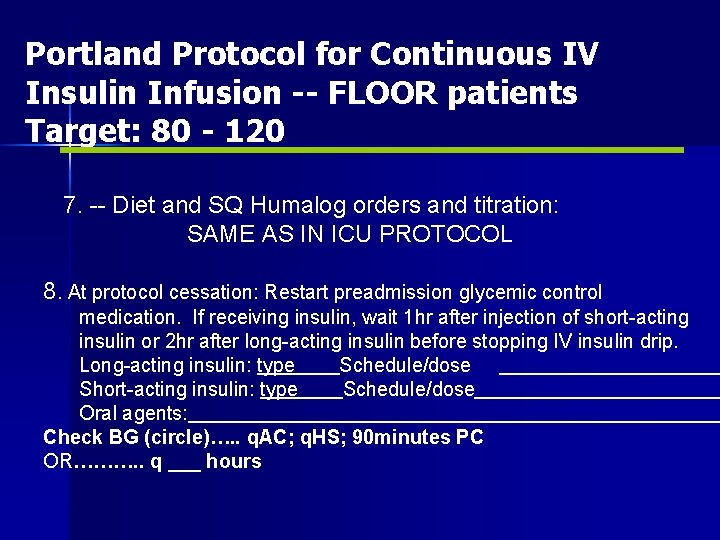
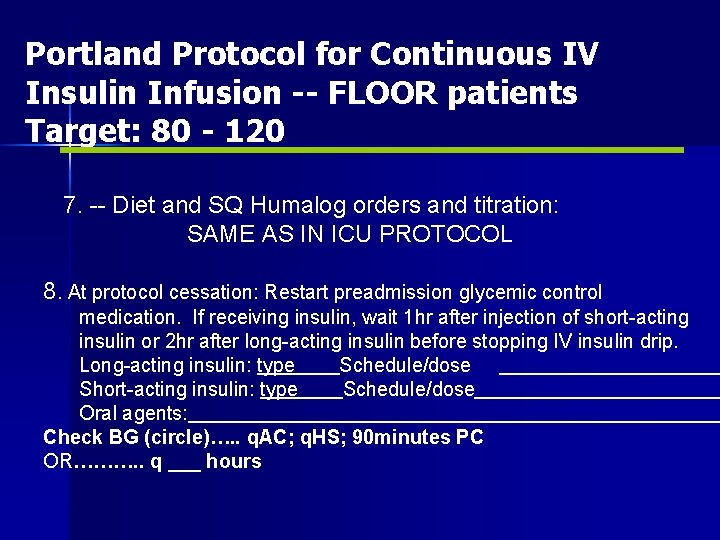
Portland Protocol for Continuous IV Insulin Infusion -- FLOOR patients Target: 80 - 120 6. 7. -- Diet and SQ Humalog orders and titration: SAME AS IN ICU PROTOCOL 8. At protocol cessation: Restart preadmission glycemic control medication. If receiving insulin, wait 1 hr after injection of short-acting insulin or 2 hr after long-acting insulin before stopping IV insulin drip. Long-acting insulin: type Schedule/dose Short-acting insulin: type Schedule/dose Oral agents: Check BG (circle)…. . q. AC; q. HS; 90 minutes PC OR………. . q ___ hours
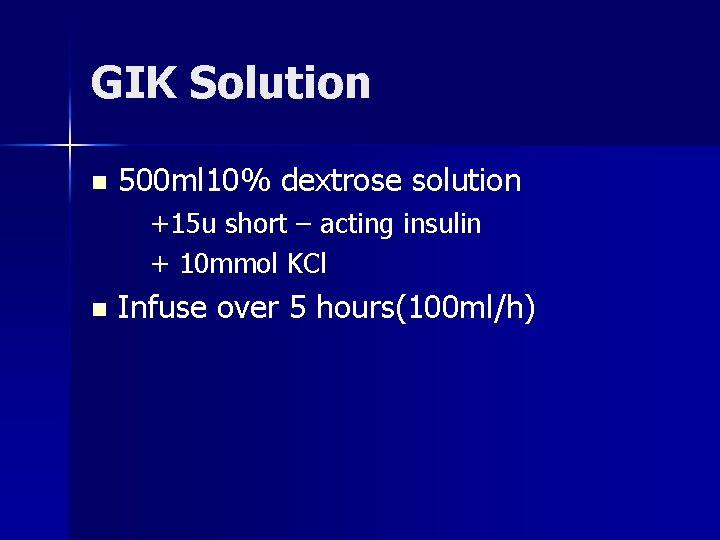
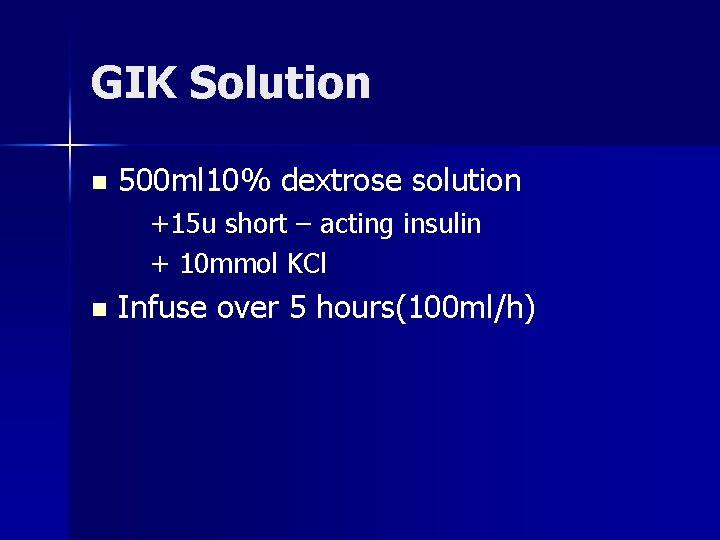
GIK Solution n 500 ml 10% dextrose solution +15 u short – acting insulin + 10 mmol KCl n Infuse over 5 hours(100 ml/h)
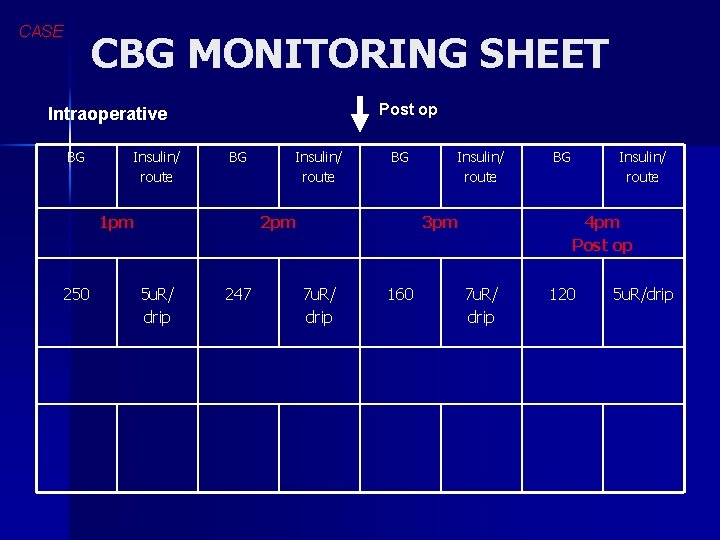
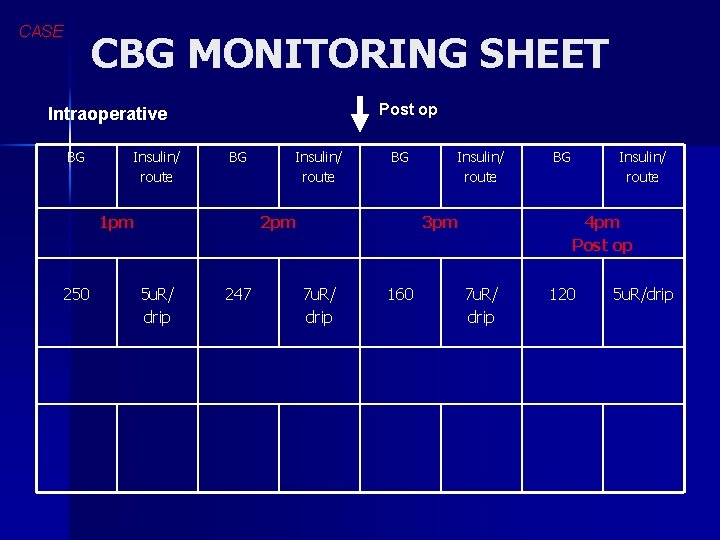
CASE CBG MONITORING SHEET Post op Intraoperative BG Insulin/ route BG 1 pm 250 Insulin/ route BG 2 pm 5 u. R/ drip 247 Insulin/ route 3 pm 7 u. R/ drip 160 BG Insulin/ route 4 pm Post op 7 u. R/ drip 120 5 u. R/drip
WHEN AND HOW DO YOU INITIATE NUTRITIONAL SUPPORT ?
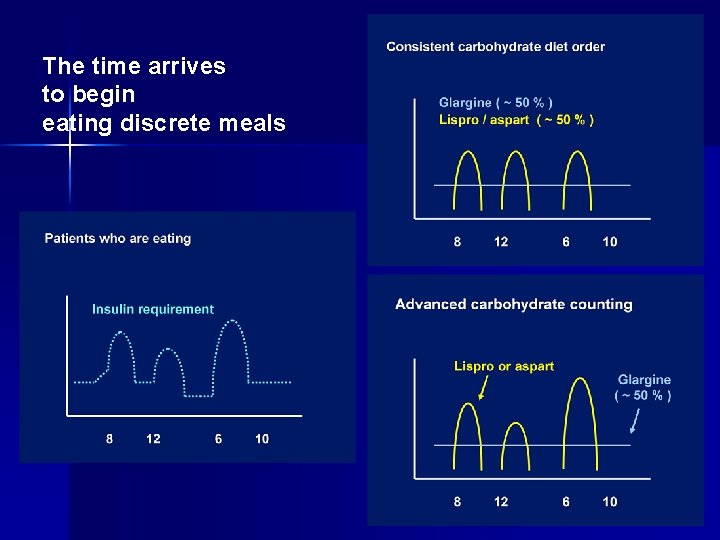
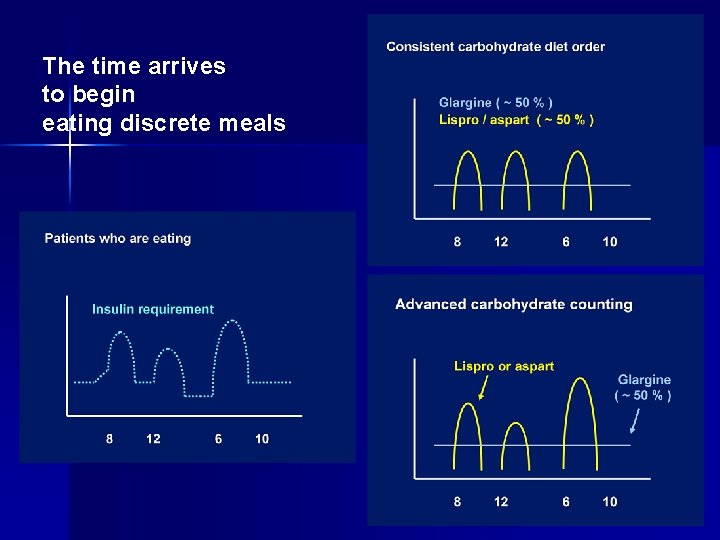
The time arrives to begin eating discrete meals
4. How do you shift from IV to SC insulin? Establish 24 hour insulin requirement n Extrapolated from average over last 4 hours of stable n Give 50% as basal and 50% as total bolus n Correction bolus for BG>140 n
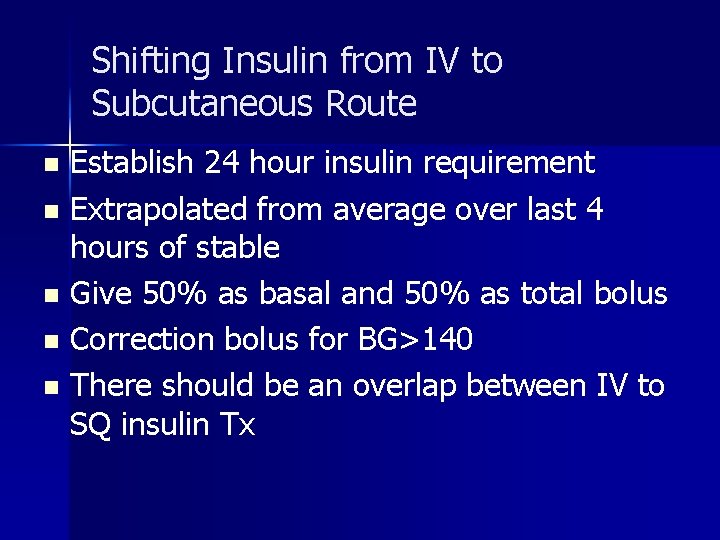
Shifting Insulin from IV to Subcutaneous Route Establish 24 hour insulin requirement n Extrapolated from average over last 4 hours of stable n Give 50% as basal and 50% as total bolus n Correction bolus for BG>140 n There should be an overlap between IV to SQ insulin Tx n
 Mechanism of action of insulin
Mechanism of action of insulin Insulin and insulin receptor
Insulin and insulin receptor Chapter 27 nutritional therapy and assisted feeding
Chapter 27 nutritional therapy and assisted feeding Chapter 28 nutritional support and iv therapy
Chapter 28 nutritional support and iv therapy Chapter 28 nutritional support and iv therapy
Chapter 28 nutritional support and iv therapy Chapter 28 nutritional support and iv therapy
Chapter 28 nutritional support and iv therapy Perimylolysis
Perimylolysis Rocking chair therapy for dementia patients
Rocking chair therapy for dementia patients Insulin coma therapy
Insulin coma therapy Nutritional management of diabetes mellitus
Nutritional management of diabetes mellitus Psychoanalytic vs humanistic
Psychoanalytic vs humanistic Bioness integrated therapy system price
Bioness integrated therapy system price What are the major humanistic therapies
What are the major humanistic therapies Management of patients with neurologic trauma
Management of patients with neurologic trauma Management of patients with neurologic trauma
Management of patients with neurologic trauma Cva
Cva Chapter 24 nutritional care and support
Chapter 24 nutritional care and support Nutritional epidemiology definition
Nutritional epidemiology definition Cum se determină valoarea nutritivă a alimentelor
Cum se determină valoarea nutritivă a alimentelor Nutritional habits for hypnum sp
Nutritional habits for hypnum sp As nutritional energy passes through the food chain energy
As nutritional energy passes through the food chain energy Heather rawls
Heather rawls Nutritional status assessment
Nutritional status assessment Optimal nutritional status
Optimal nutritional status Types of nutritional survey
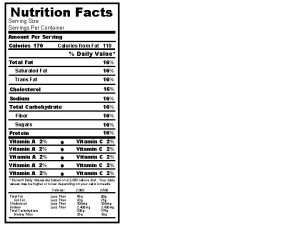
Types of nutritional survey How many servings are in 1 container
How many servings are in 1 container Abcd of nutritional assessment
Abcd of nutritional assessment Major nutritional deficiency diseases in emergencies
Major nutritional deficiency diseases in emergencies Abcd of nutritional assessment
Abcd of nutritional assessment Jennifer colombo
Jennifer colombo Common nutritional problems in bangladesh
Common nutritional problems in bangladesh Abcd of nutritional assessment
Abcd of nutritional assessment Chapter 2 nutritional needs
Chapter 2 nutritional needs Nutritional intervention
Nutritional intervention Nutritional recovery syndrome
Nutritional recovery syndrome Abcd in nutrition assessment
Abcd in nutrition assessment Continuous feeding vs bolus feeding
Continuous feeding vs bolus feeding Nutritional requirements for ruminant animals
Nutritional requirements for ruminant animals Nutritional diseases
Nutritional diseases Nutritional diseases
Nutritional diseases Nutritional diseases
Nutritional diseases What is nutrition quackery
What is nutrition quackery How can we crack nature’s secret nutritional code
How can we crack nature’s secret nutritional code Nutritional requirements of plants
Nutritional requirements of plants Concept of nutritional standard
Concept of nutritional standard Characteristics of a high quality muffin
Characteristics of a high quality muffin Purpose of malnutrition
Purpose of malnutrition Subjective global assessment scoring sheet
Subjective global assessment scoring sheet