Insulin Initiation and Titration Insulin topics we will


- Slides: 52
Insulin Initiation and Titration
Insulin topics we will not cover today �Inhaled Insulin �Insulin Pump �Insulin management of the surgical and ICU patient �Insulin Requirements in Pregnancy
Goals for this session: �Know the indications for starting insulin �Know typical starting dose of Daily intermediate or long-acting insulin �Titrate the intermediate or long-acting insulin based on glucose readings �Be able to calculate starting doses based on weight for 70/30 insulin BID dosing �Titrate the 70/30 insulin based on glucose readings �Identify causes of hypoglycemia and hyperglycemia �Manage hypoglycemia and hyperglycemia
Complete 3 activities after this lecture �Calculating Insulin Starting Doses and Titration Case Studies �How to draw up and inject insulin �Hypoglycemia & Hyperglycemia identification & treatment. Glucose monitoring and the importance of the glucose logbook in titrating insulin doses.
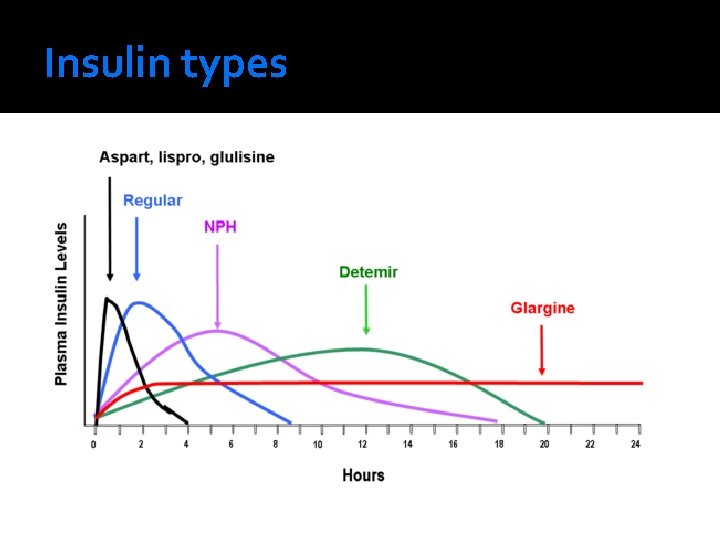
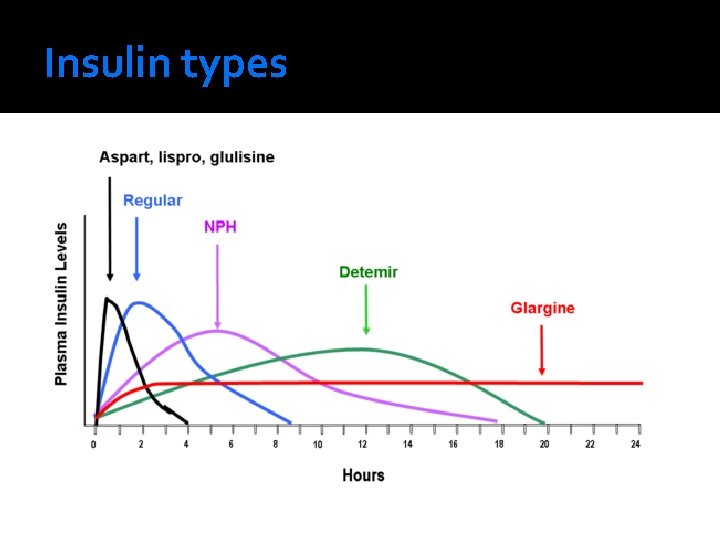
Insulin types
Insulin Terms �Basal Insulin Replacement That insulin required to suppress hepatic glucose production overnight and between meals
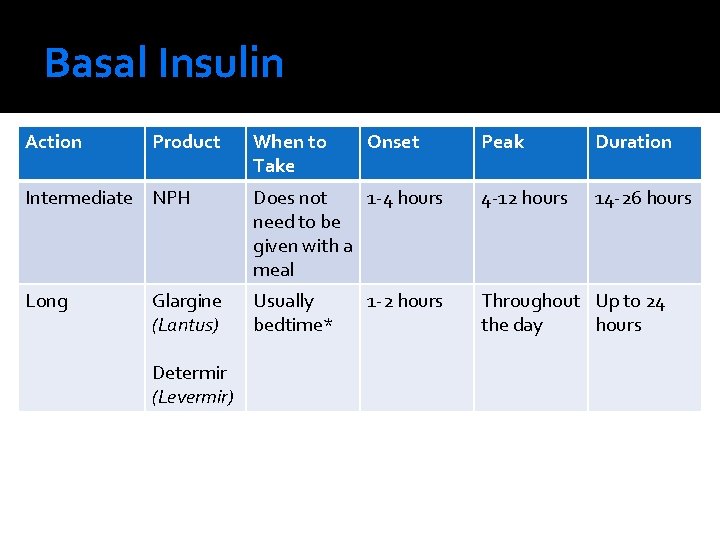
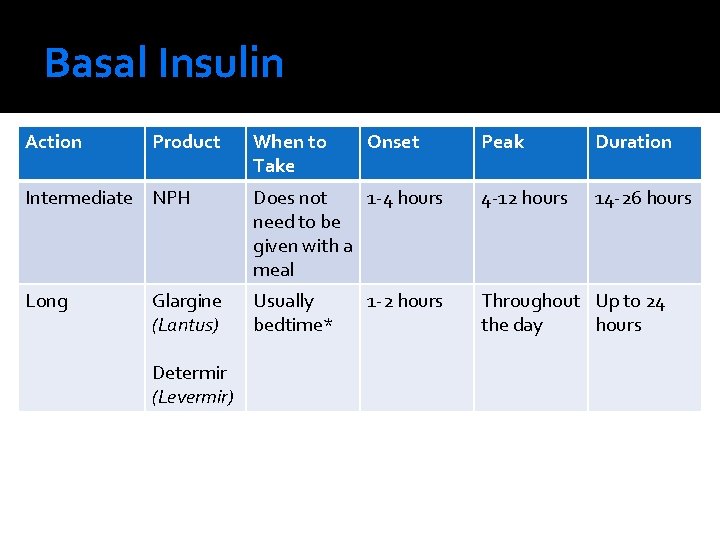
Basal Insulin Action Product When to Take Onset Peak Duration 14 -26 hours Intermediate NPH Does not 1 -4 hours need to be given with a meal 4 -12 hours Long Usually bedtime* Throughout Up to 24 the day hours Glargine (Lantus) Determir (Levermir) 1 -2 hours
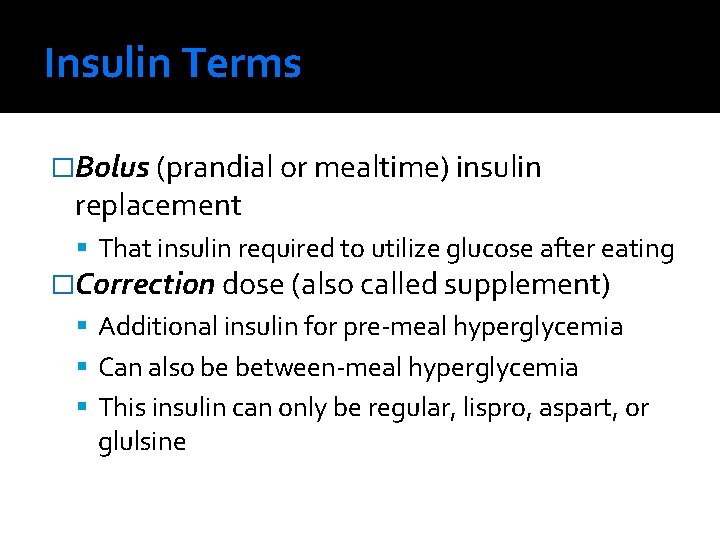
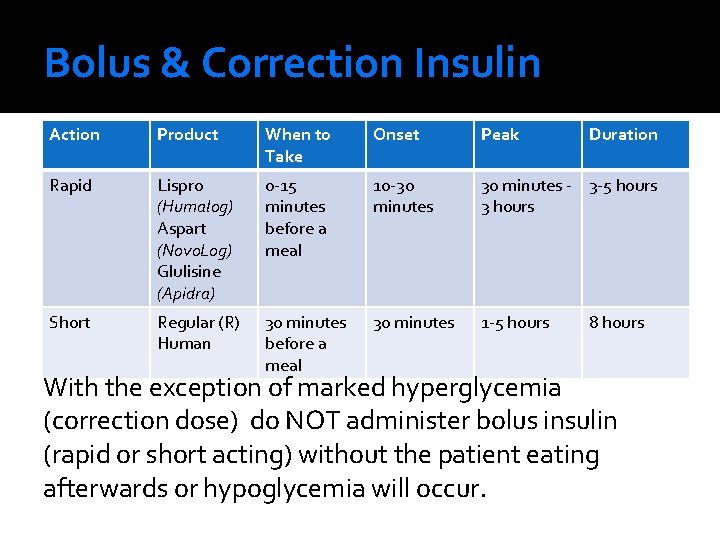
Insulin Terms �Bolus (prandial or mealtime) insulin replacement That insulin required to utilize glucose after eating �Correction dose (also called supplement) Additional insulin for pre-meal hyperglycemia Can also be between-meal hyperglycemia This insulin can only be regular, lispro, aspart, or glulsine
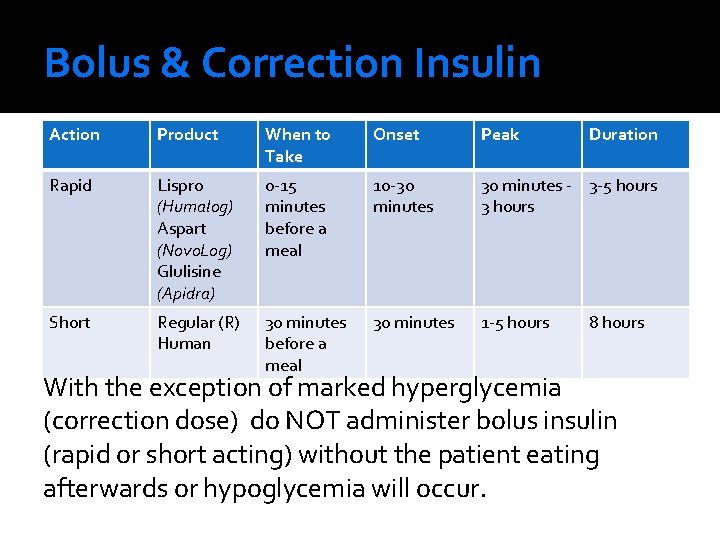
Bolus & Correction Insulin Action Product When to Take Onset Peak Duration Rapid Lispro (Humalog) Aspart (Novo. Log) Glulisine (Apidra) 0 -15 minutes before a meal 10 -30 minutes - 3 -5 hours 3 hours Short Regular (R) Human 30 minutes before a meal 30 minutes 1 -5 hours 8 hours With the exception of marked hyperglycemia (correction dose) do NOT administer bolus insulin (rapid or short acting) without the patient eating afterwards or hypoglycemia will occur.
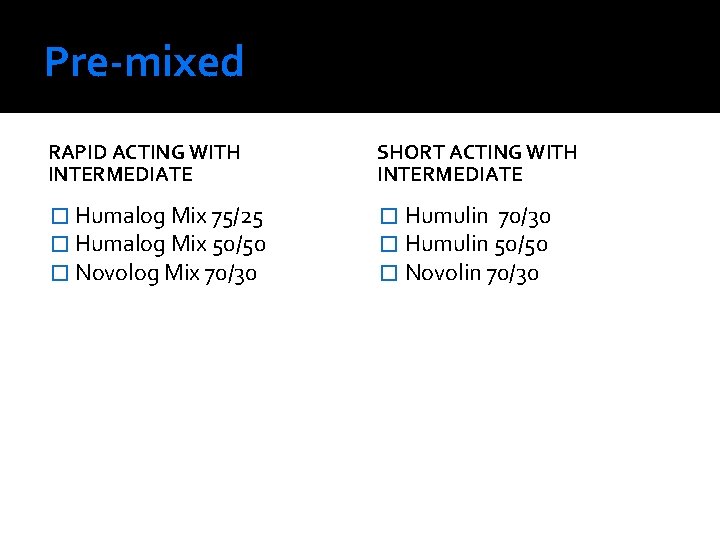
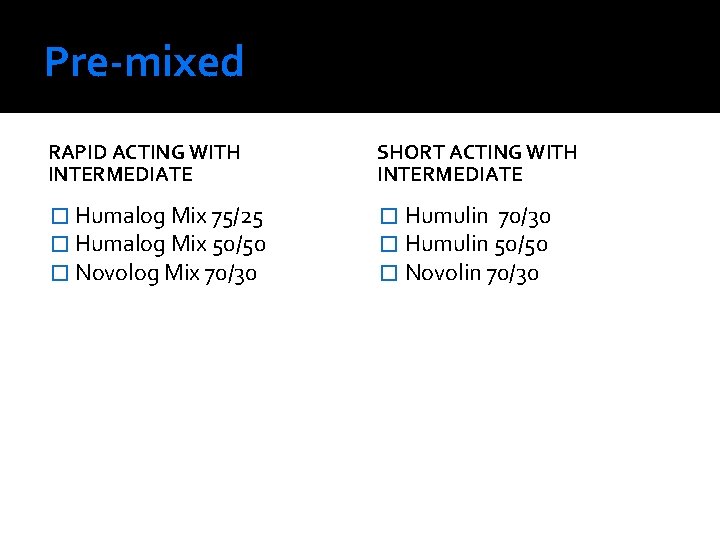
Pre-mixed RAPID ACTING WITH INTERMEDIATE SHORT ACTING WITH INTERMEDIATE � Humalog Mix 75/25 � Humalog Mix 50/50 � Novolog Mix 70/30 � Humulin 50/50 � Novolin 70/30
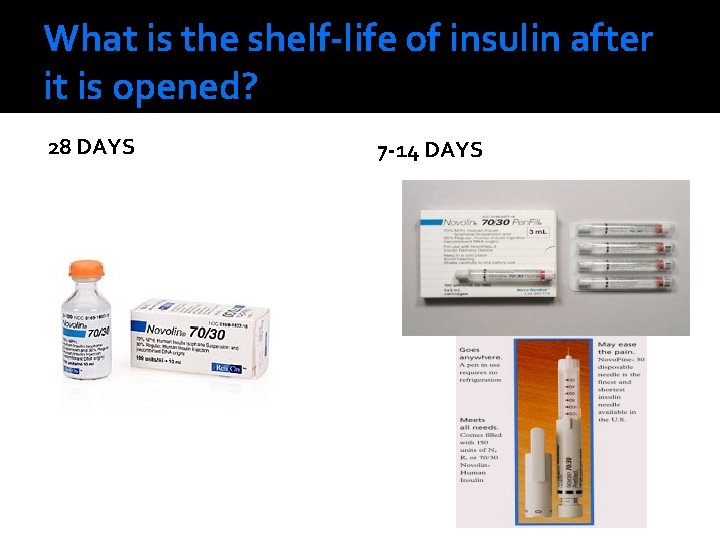
What is the shelf-life of insulin after it is opened? 28 DAYS 7 -14 DAYS
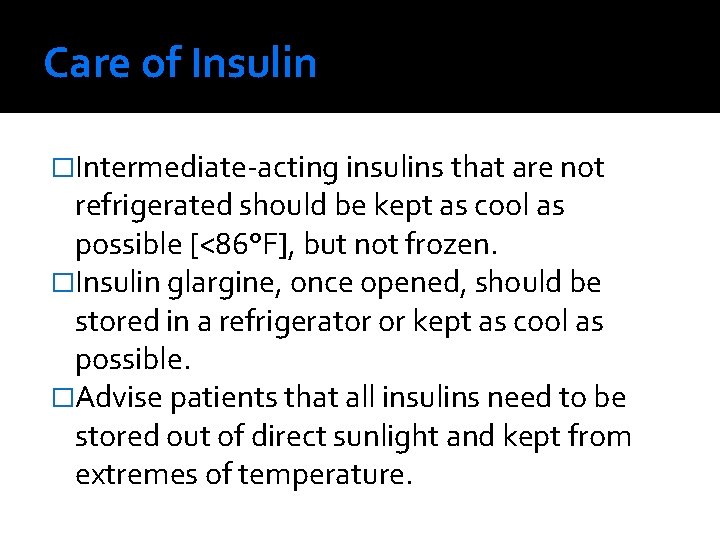
Care of Insulin �Intermediate-acting insulins that are not refrigerated should be kept as cool as possible [<86°F], but not frozen. �Insulin glargine, once opened, should be stored in a refrigerator or kept as cool as possible. �Advise patients that all insulins need to be stored out of direct sunlight and kept from extremes of temperature.
When should you start insulin? �Type I Diabetes Always
When should you start insulin in Type II Diabetes? Glucose levels are so acutely elevated that immediate safety is a concern ▪ Marked hyperglycemia OR Significant weight loss OR Severe/significant symptoms OR 2+ or greater ketonuria OR DKA/ hyperosmolar state OR Severe intercurrent illness or surgery Chronic suboptimal control of glucose despite oral hypoglycemic medications/GLP-1 agonists/ ▪ Fasting Plasma Glucose > 140 OR 2 Hr Postprandial Plasma Glucose > 180 OR A 1 C > 7. 0%
What fears do patients have about starting insulin?
Insulin Initiation Options for Type II Patients
Insulin options for patients with Type II DM 1) Continue PO medications & add nighttime basal insulin 2) Pre-mixed Insulin Program 3) Basal insulin + mealtime (bolus) insulin We will not cover this today
Option #1: Continue PO medications & add nighttime basal insulin NOTE: This is NOT an option for patients with Type II DM who have an A 1 c >8. 5% on max oral hypoglycemics (they will never get to goal). 2) This is NOT an option for Type I diabetics 1)
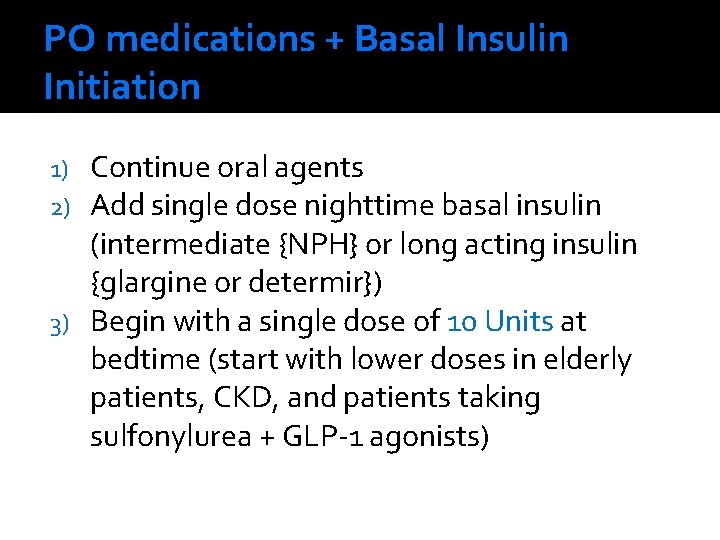
PO medications + Basal Insulin Initiation Continue oral agents Add single dose nighttime basal insulin (intermediate {NPH} or long acting insulin {glargine or determir}) 3) Begin with a single dose of 10 Units at bedtime (start with lower doses in elderly patients, CKD, and patients taking sulfonylurea + GLP-1 agonists) 1) 2)
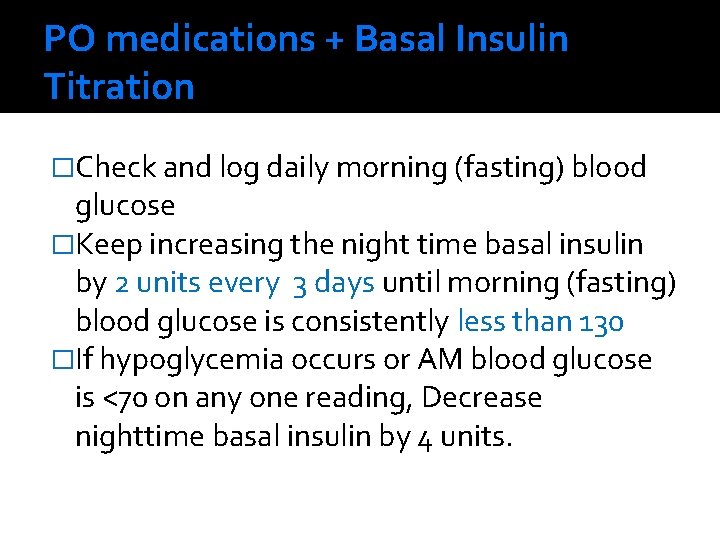
PO medications + Basal Insulin Titration �Check and log daily morning (fasting) blood glucose �Keep increasing the night time basal insulin by 2 units every 3 days until morning (fasting) blood glucose is consistently less than 130 �If hypoglycemia occurs or AM blood glucose is <70 on any one reading, Decrease nighttime basal insulin by 4 units.
EXAMPLE �A 84 kg male has consistent elevated glucose readings, and A 1 C of 7. 8 on Metformin 1 g BID, Glyburide 10 mg BID, and Pioglitazone 30 mg daily. The patient has normal estimated Cr. Cl. �Plan: Nighttime basal insulin: glargine or determir or NPH is added to the patient’s medications
EXAMPLE �Q: The patient was started on 10 Units of nighttime glargine in addition to his PO medications: glyburide 5 mg BID, Metformin, 1 g BID, and Pioglitazone 30 mg daily. He checks his fasting glucose every morning and calls you with the following AM results from the past 4 days: 180, 160, 173. What should be done next? �A:
EXAMPLE �Q: The patient calls you in 4 days with the following AM fasting readings: 136, 128, 134, What should you tell the patient? �A:
EXAMPLE �Q: The patient calls you in 4 days with the following AM fasting readings: 102, 98, 88. What should you tell the patient? �A:
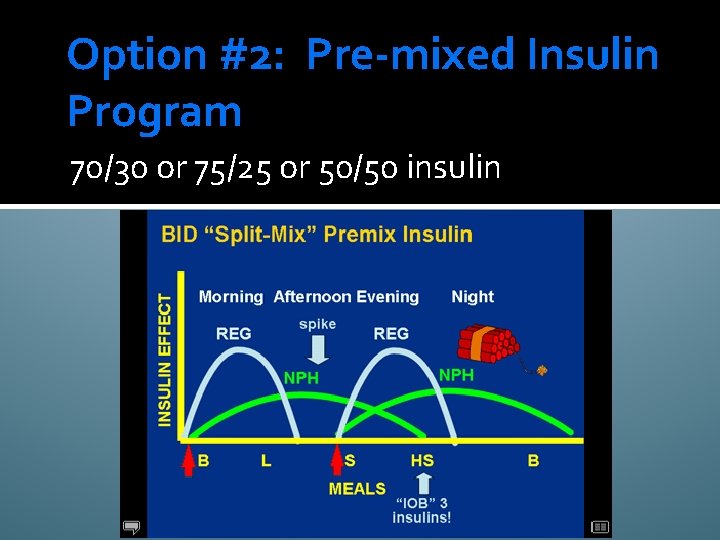
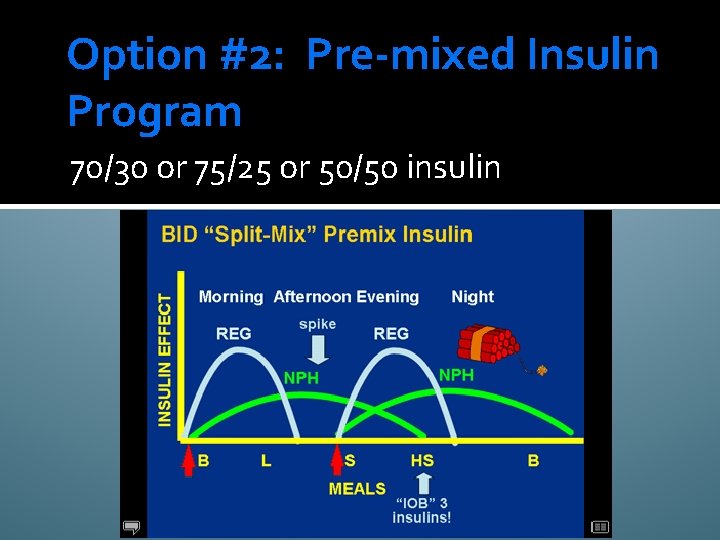
Option #2: Pre-mixed Insulin Program 70/30 or 75/25 or 50/50 insulin
Premixed Insulin Program �Taper and discontinue oral antihyperglycemic medications as insulin is initiated and adjusted, particularly if using short or rapid-acting + basal insulins (exception is METFORMIN - Type 2 diabetics on insulin can improve their glycemic control and lower their insulin dose with metformin. ) �There is an increased risk for edema when insulin and a thiazolidinedione are used together. Rosiglitazone should not be used in combination with insulin.
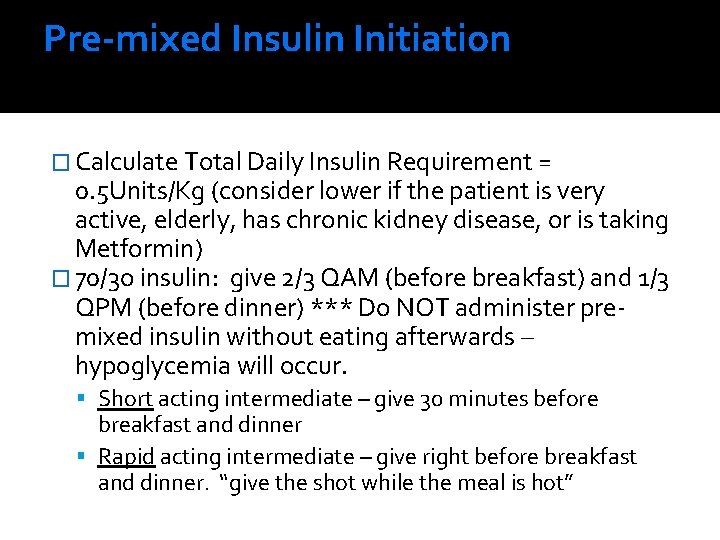
Pre-mixed Insulin Initiation � Calculate Total Daily Insulin Requirement = 0. 5 Units/Kg (consider lower if the patient is very active, elderly, has chronic kidney disease, or is taking Metformin) � 70/3 o insulin: give 2/3 QAM (before breakfast) and 1/3 QPM (before dinner) *** Do NOT administer premixed insulin without eating afterwards – hypoglycemia will occur. Short acting intermediate – give 30 minutes before breakfast and dinner Rapid acting intermediate – give right before breakfast and dinner. “give the shot while the meal is hot”
PRACTICE �Calculate your own total starting dose of 70/30 insulin based on your weight in Kg. Now divide total into 2/3 in the AM (pre-breakfast) and 1/3 in the PM (pre-dinner)
Example �Q: Calculate the insulin for a patient starting 70/30 insulin who is 200 lbs �A:
Example �Q: Calculate the insulin for a patient starting 70/30 insulin who is 140 lbs (64 kg) �A:
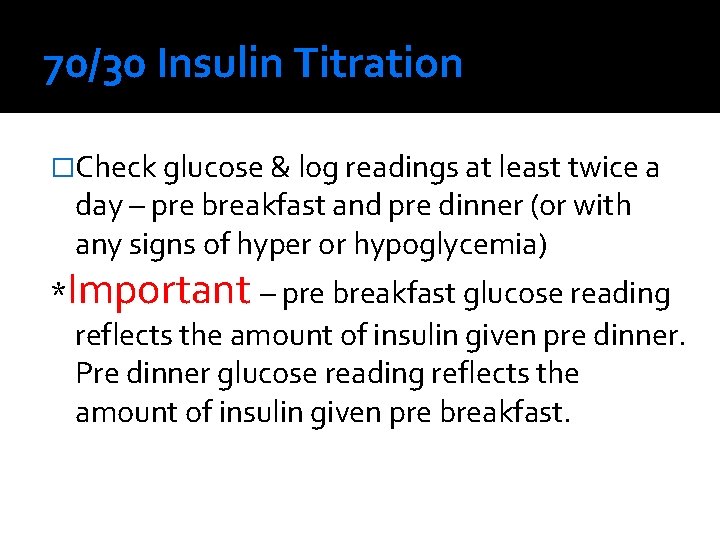
70/30 Insulin Titration �Check glucose & log readings at least twice a day – pre breakfast and pre dinner (or with any signs of hyper or hypoglycemia) *Important – pre breakfast glucose reading reflects the amount of insulin given pre dinner. Pre dinner glucose reading reflects the amount of insulin given pre breakfast.

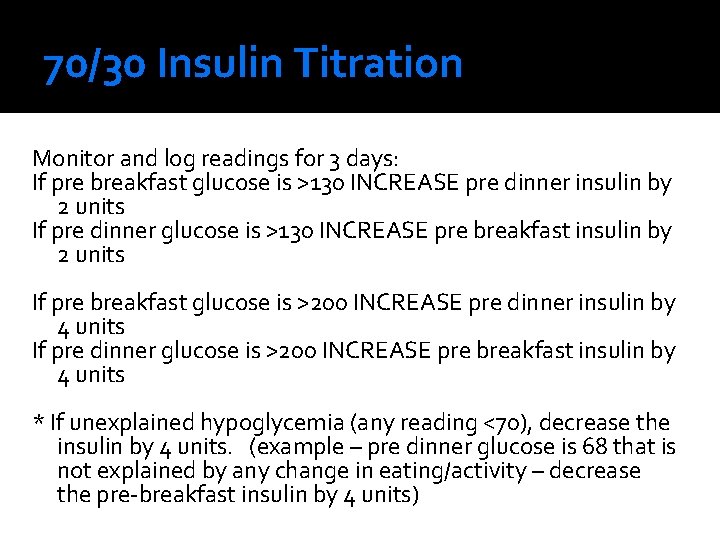
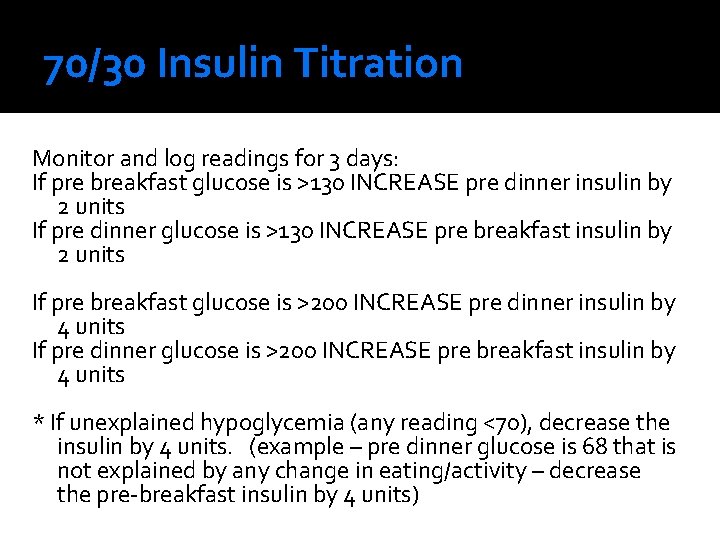
70/30 Insulin Titration Monitor and log readings for 3 days: If pre breakfast glucose is >130 INCREASE pre dinner insulin by 2 units If pre dinner glucose is >130 INCREASE pre breakfast insulin by 2 units If pre breakfast glucose is >200 INCREASE pre dinner insulin by 4 units If pre dinner glucose is >200 INCREASE pre breakfast insulin by 4 units * If unexplained hypoglycemia (any reading <70), decrease the insulin by 4 units. (example – pre dinner glucose is 68 that is not explained by any change in eating/activity – decrease the pre-breakfast insulin by 4 units)
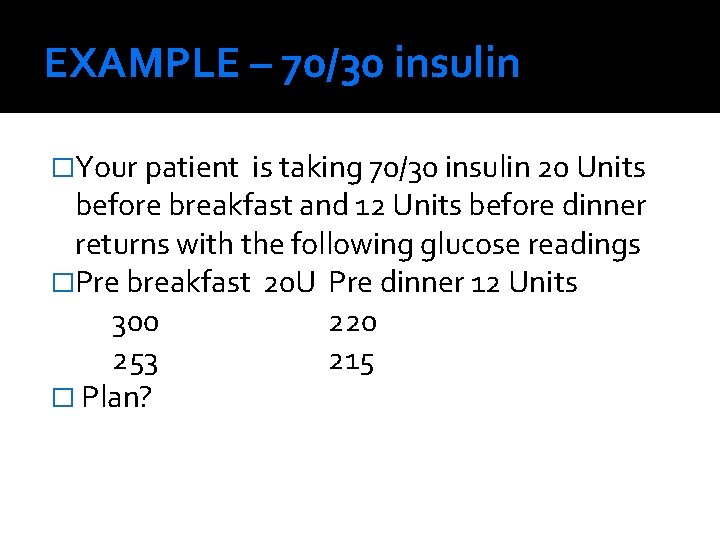
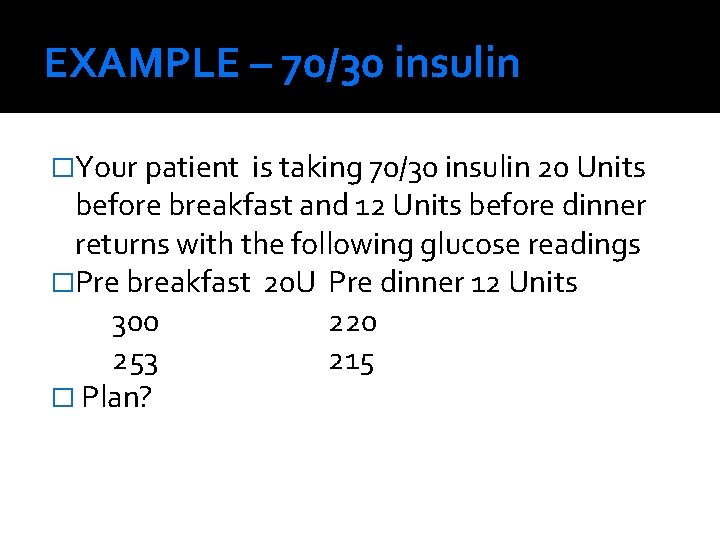
EXAMPLE – 70/30 insulin �Your patient is taking 70/30 insulin 20 Units before breakfast and 12 Units before dinner returns with the following glucose readings �Pre breakfast 20 U Pre dinner 12 Units 300 220 253 215 � Plan?
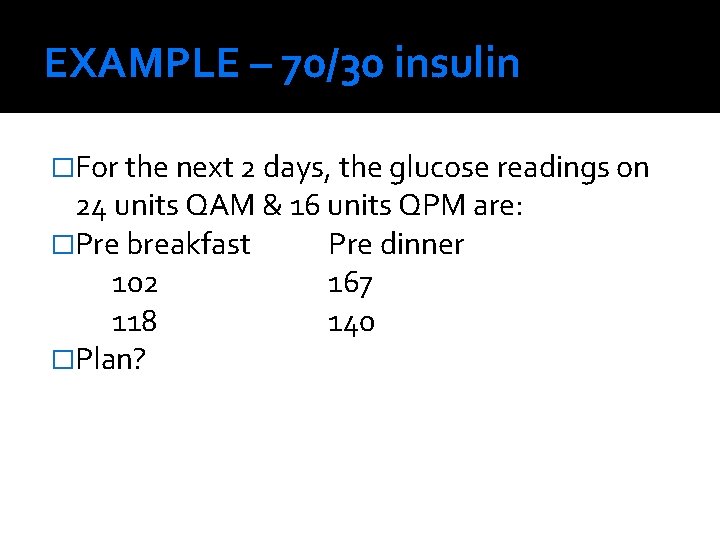
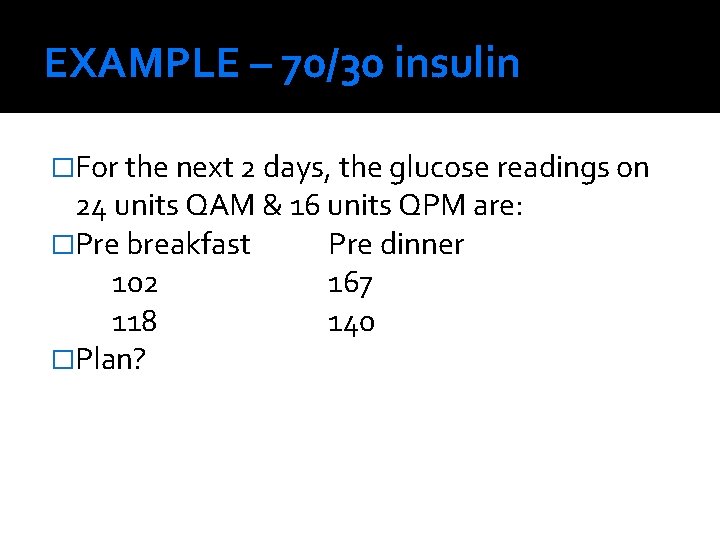
EXAMPLE – 70/30 insulin �For the next 2 days, the glucose readings on 24 units QAM & 16 units QPM are: �Pre breakfast Pre dinner 102 167 118 140 �Plan?
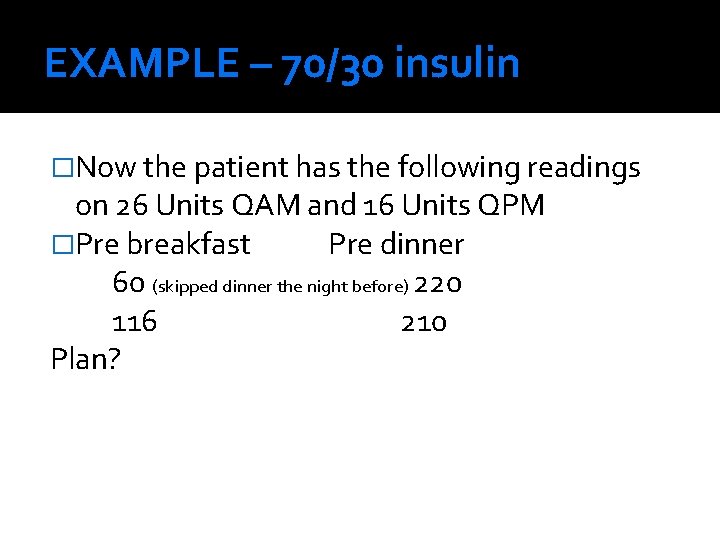
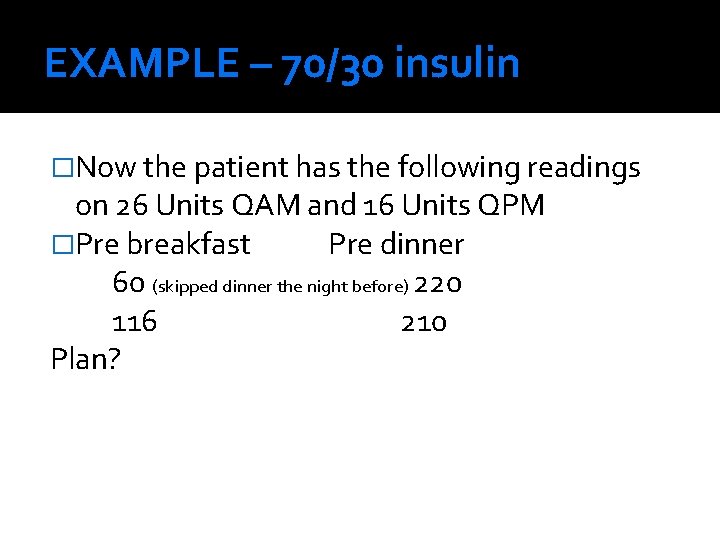
EXAMPLE – 70/30 insulin �Now the patient has the following readings on 26 Units QAM and 16 Units QPM �Pre breakfast Pre dinner 60 (skipped dinner the night before) 220 116 210 Plan?
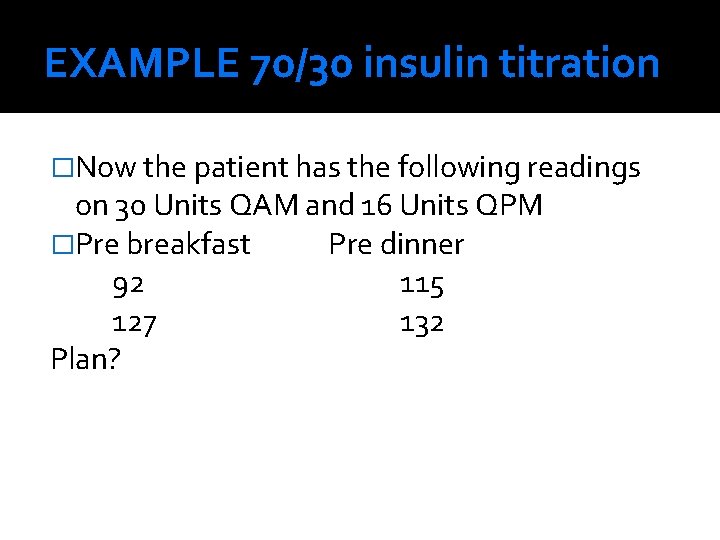
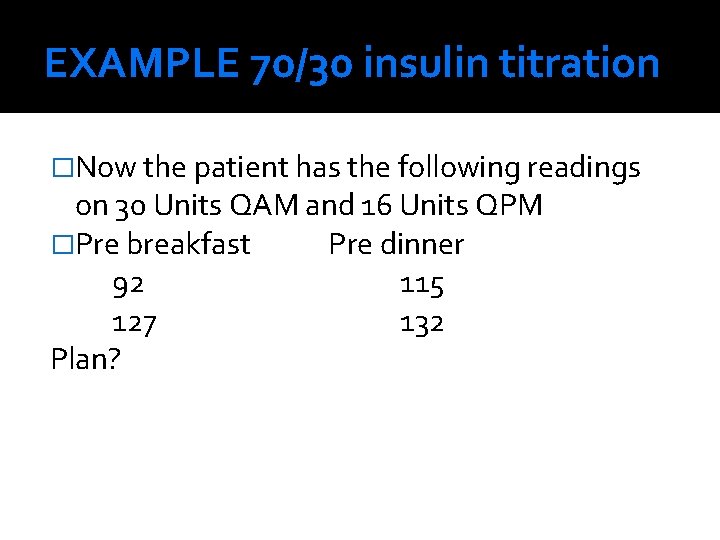
EXAMPLE 70/30 insulin titration �Now the patient has the following readings on 30 Units QAM and 16 Units QPM �Pre breakfast Pre dinner 92 115 127 132 Plan?
Option #3: Basal insulin + mealtime (bolus) insulin For Type II patients who require insulin For Type I patients
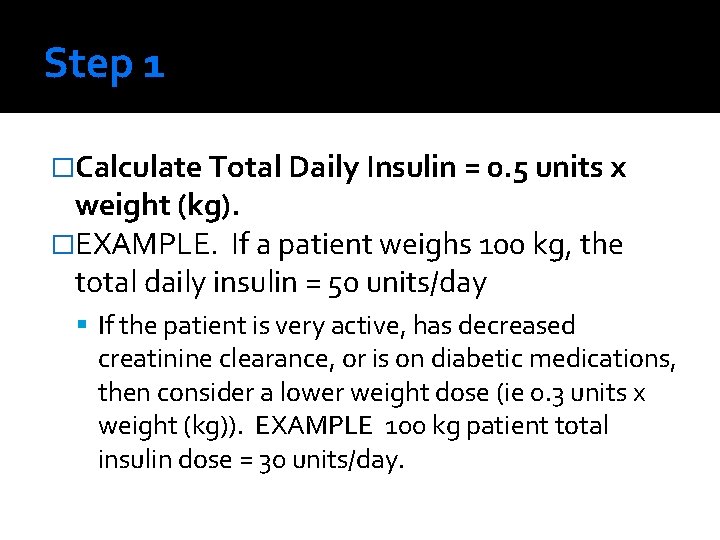
Step 1 �Calculate Total Daily Insulin = 0. 5 units x weight (kg). �EXAMPLE. If a patient weighs 100 kg, the total daily insulin = 50 units/day If the patient is very active, has decreased creatinine clearance, or is on diabetic medications, then consider a lower weight dose (ie 0. 3 units x weight (kg)). EXAMPLE 100 kg patient total insulin dose = 30 units/day.
Step 2 �Split Total Insulin dose 50: 50 basal and bolus insulin 50% of dose is basal 50% of dose is bolus between ▪ Further divide bolus insulin into 1/3 for 3 meal coverage.
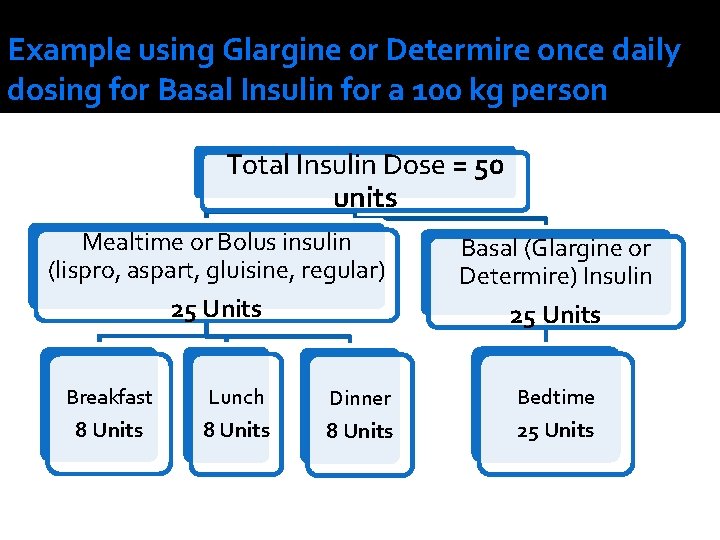
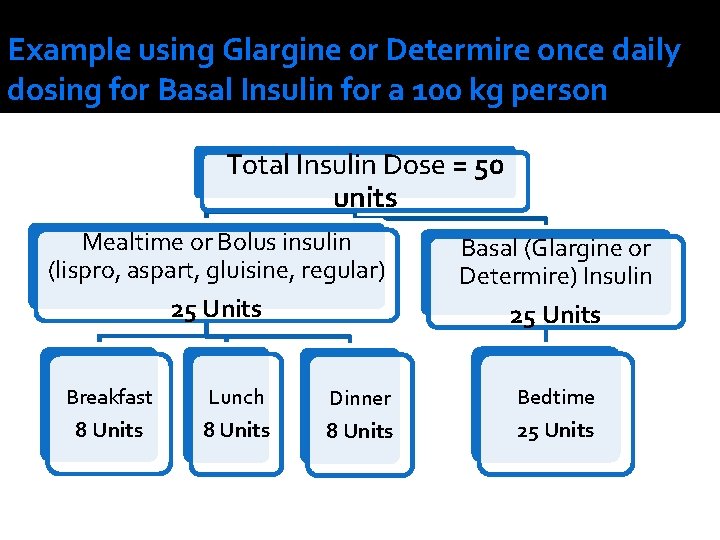
Example using Glargine or Determire once daily dosing for Basal Insulin for a 100 kg person Total Insulin Dose = 50 units Mealtime or Bolus insulin (lispro, aspart, gluisine, regular) 25 Units Breakfast 8 Units Lunch 8 Units Dinner 8 Units Basal (Glargine or Determire) Insulin 25 Units Bedtime 25 Units
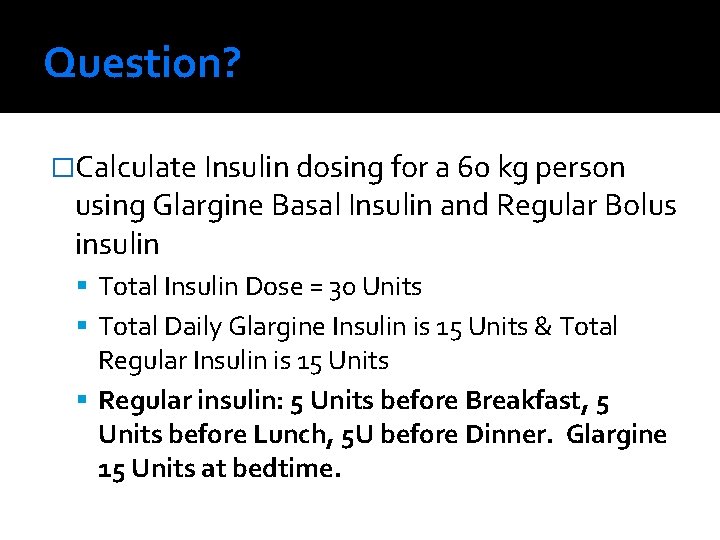
Question? �Calculate Insulin dosing for a 60 kg person using Glargine Basal Insulin and Regular Bolus insulin Total Insulin Dose = 30 Units Total Daily Glargine Insulin is 15 Units & Total Regular Insulin is 15 Units Regular insulin: 5 Units before Breakfast, 5 Units before Lunch, 5 U before Dinner. Glargine 15 Units at bedtime.
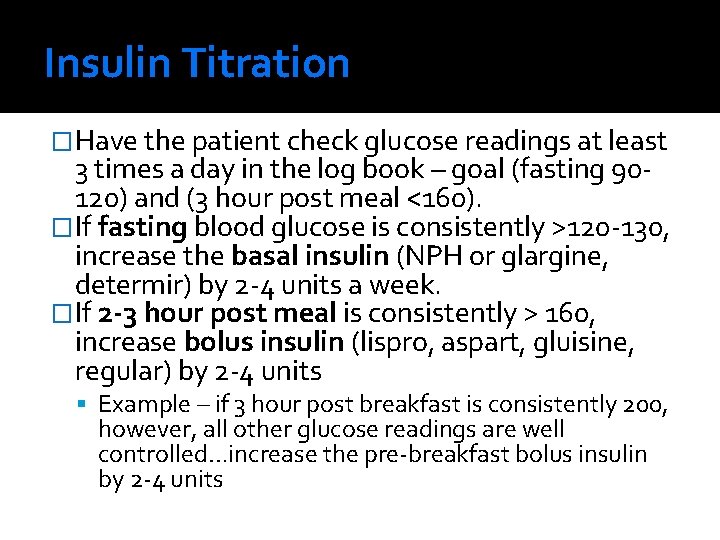
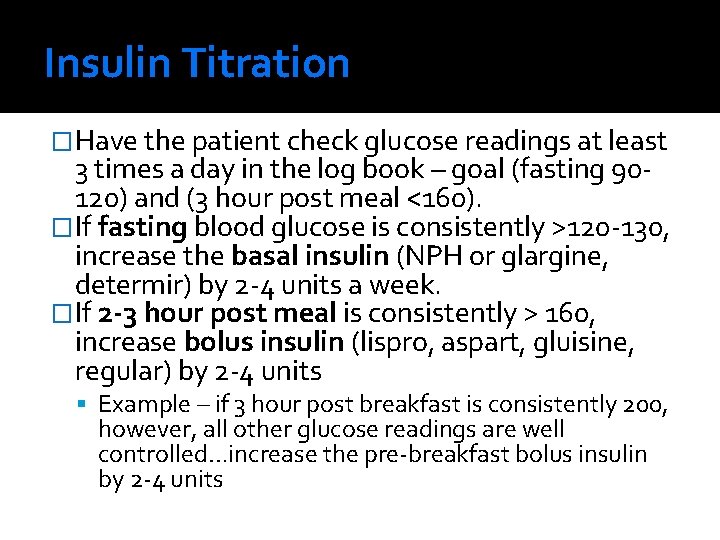
Insulin Titration �Have the patient check glucose readings at least 3 times a day in the log book – goal (fasting 90120) and (3 hour post meal <160). �If fasting blood glucose is consistently >120 -130, increase the basal insulin (NPH or glargine, determir) by 2 -4 units a week. �If 2 -3 hour post meal is consistently > 160, increase bolus insulin (lispro, aspart, gluisine, regular) by 2 -4 units Example – if 3 hour post breakfast is consistently 200, however, all other glucose readings are well controlled…increase the pre-breakfast bolus insulin by 2 -4 units
What about the high readings?

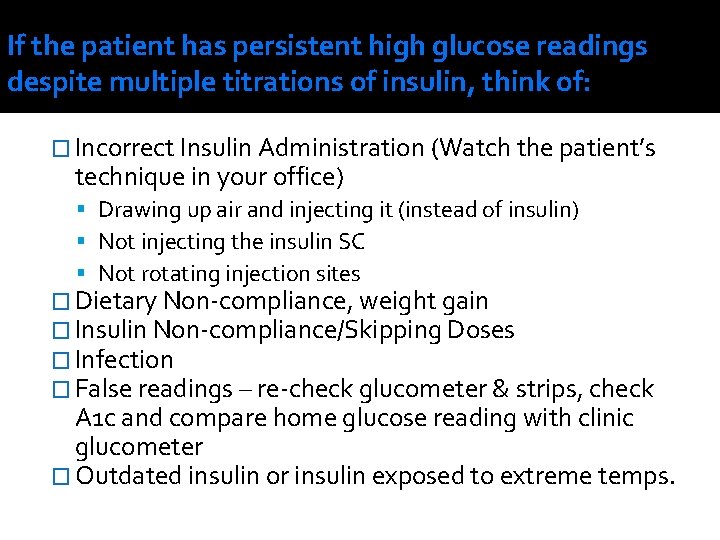
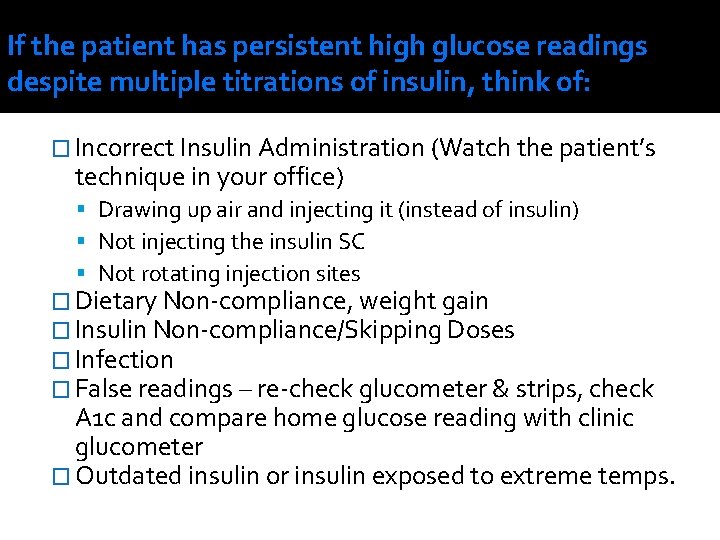
If the patient has persistent high glucose readings despite multiple titrations of insulin, think of: � Incorrect Insulin Administration (Watch the patient’s technique in your office) Drawing up air and injecting it (instead of insulin) Not injecting the insulin SC Not rotating injection sites � Dietary Non-compliance, weight gain � Insulin Non-compliance/Skipping Doses � Infection � False readings – re-check glucometer & strips, check A 1 c and compare home glucose reading with clinic glucometer � Outdated insulin or insulin exposed to extreme temps.
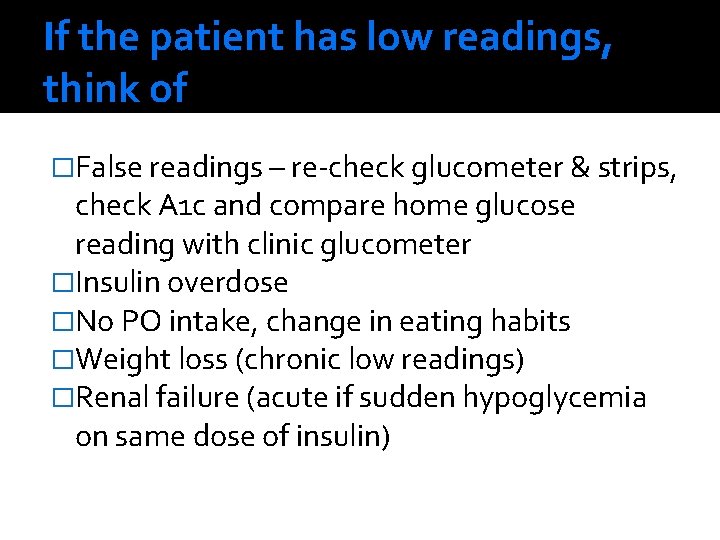
And the low readings?
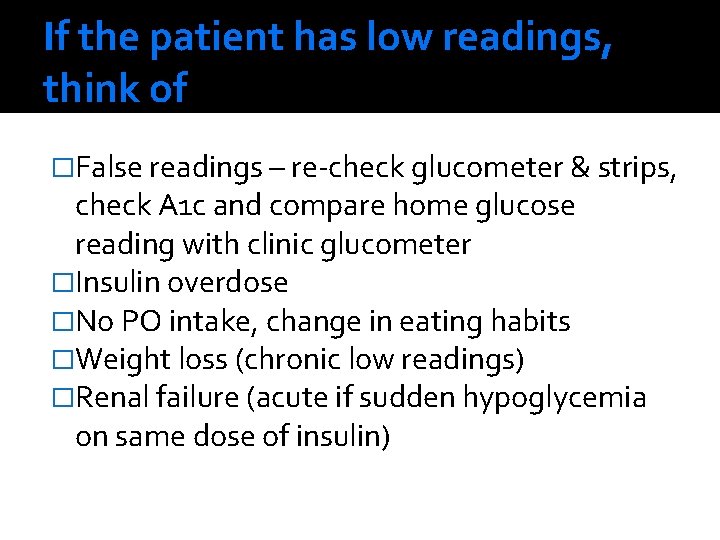
If the patient has low readings, think of �False readings – re-check glucometer & strips, check A 1 c and compare home glucose reading with clinic glucometer �Insulin overdose �No PO intake, change in eating habits �Weight loss (chronic low readings) �Renal failure (acute if sudden hypoglycemia on same dose of insulin)
Summary
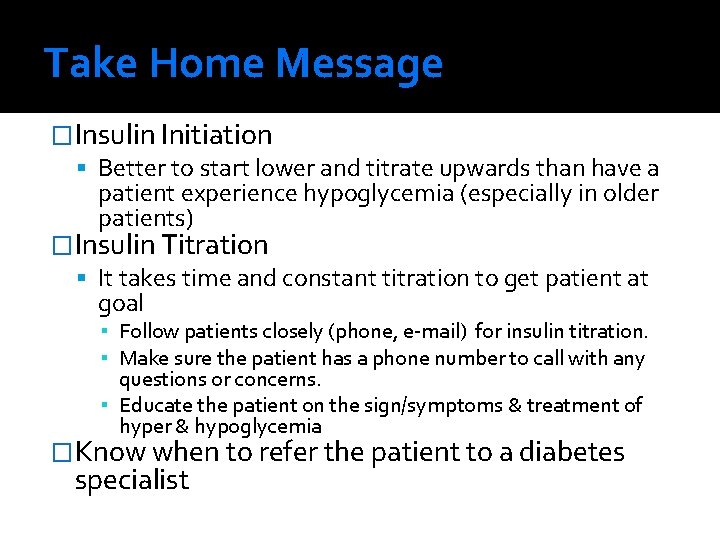
Take Home Message �Insulin Initiation Better to start lower and titrate upwards than have a patient experience hypoglycemia (especially in older patients) �Insulin Titration It takes time and constant titration to get patient at goal ▪ Follow patients closely (phone, e-mail) for insulin titration. ▪ Make sure the patient has a phone number to call with any questions or concerns. ▪ Educate the patient on the sign/symptoms & treatment of hyper & hypoglycemia �Know when to refer the patient to a diabetes specialist
References Joslin Diabetes Center & Joslin Clinical Guideline for Pharmacological Management of Type 2 Diabetes 1/09/2009 www. professionaled. joslin. org 2) Joslin E-Z start Resource Manual for Primary Care Practices 3) Uptodate. com 1)
Learning Outcomes for PD Lab Stations �Effectively dose and titrate insulin for the cases given �Demonstrate correct drawing up insulin and injection of insulin Be able to instruct patients on this technique �Demonstrate correct technique of checking a capillary blood glucose Be able to instruct patients on this technique �Identify the signs and symptoms of hyperglycemia and hypoglycemia