Insulin Initiation and Intensification Insulin Therapy at the

- Slides: 35

+ Insulin Initiation and Intensification
+ Insulin Therapy at the diagnosis of T 2 DM Dr. Ravi Kant M. B. B. S, M. D (Medicine), P. Gd(Preventive cardiology), Master (European and American Heart Association), P. Gd. Diabetology (Boston University) Associate Professor Department of Internal Medicine All India Institute of Medical Sciences Rishikesh, Uttarakhand
+ Overview n Why Insulin: n Advantages vs disadvantages n When to initiate insulin n Early vs late (OAD failure) n Which insulin to initiate n Basal, prandial, premix, basal-bolus n What to do for follow-up n Titration, hypoglycemia, achieving targets
+ Overview n Why Insulin: n Advantages vs disadvantages
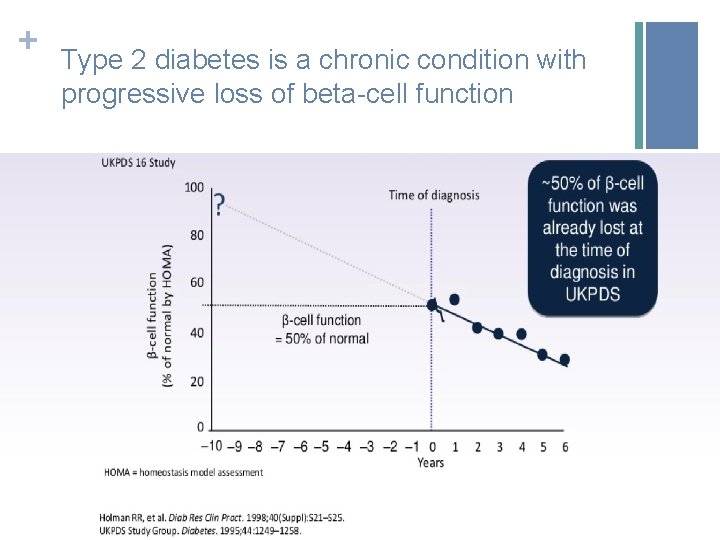
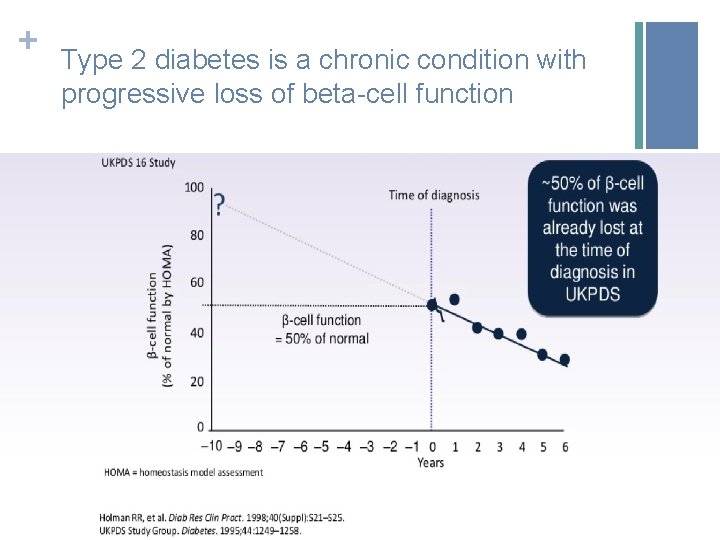
+ Type 2 diabetes is a chronic condition with progressive loss of beta-cell function
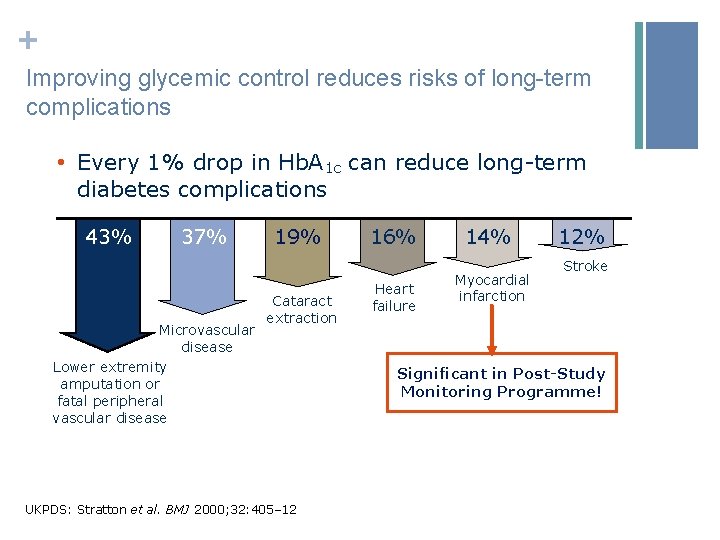
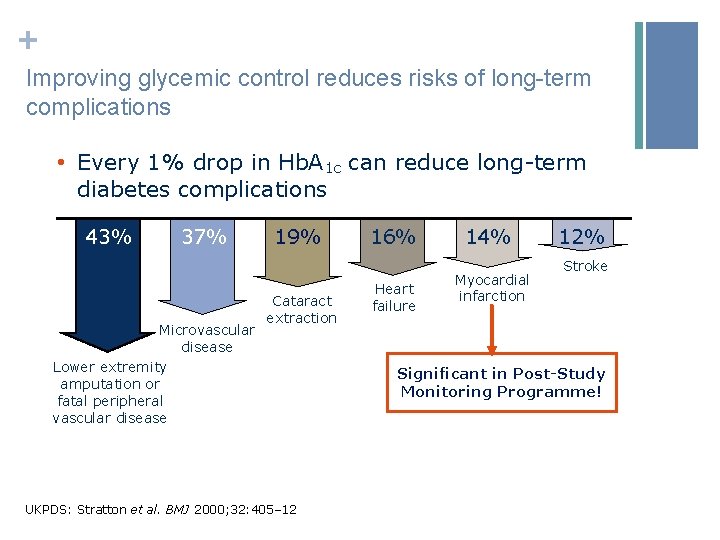
+ Improving glycemic control reduces risks of long-term complications • Every 1% drop in Hb. A 1 c can reduce long-term diabetes complications 43% 37% Microvascular disease Lower extremity amputation or fatal peripheral vascular disease 19% Cataract extraction UKPDS: Stratton et al. BMJ 2000; 32: 405– 12 16% Heart failure 14% Myocardial infarction 12% Stroke Significant in Post-Study Monitoring Programme!
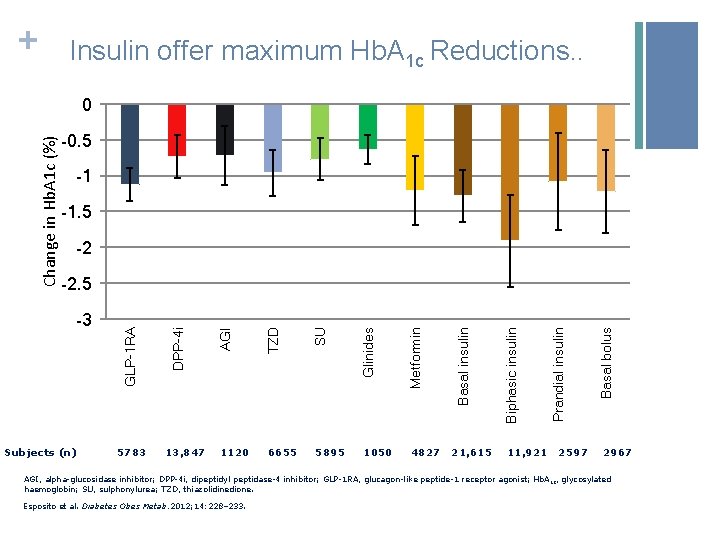
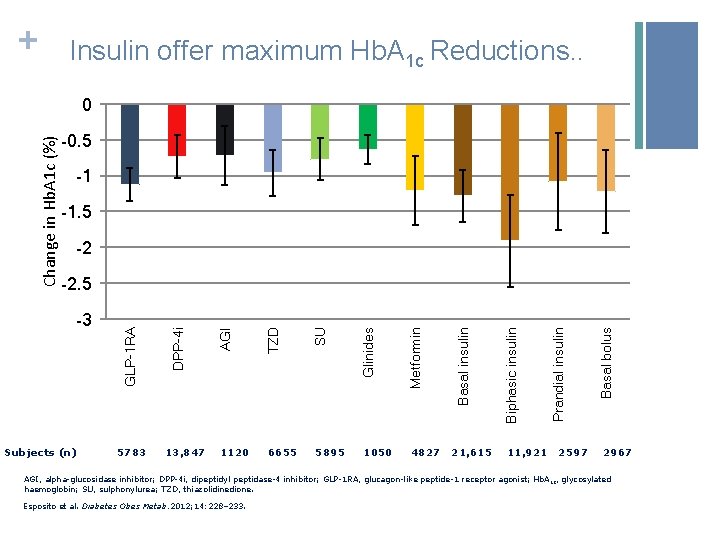
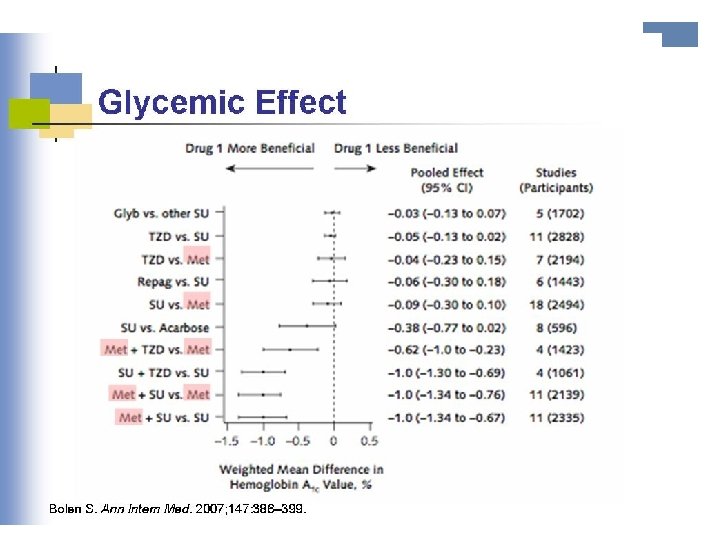
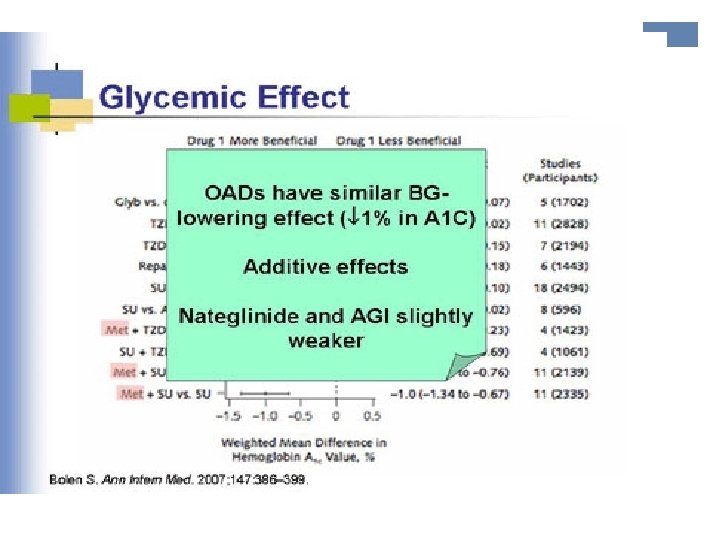
+ Insulin offer maximum Hb. A 1 c Reductions. . -0. 5 -1 -1. 5 -2 13, 847 1050 4827 21, 615 11, 921 2597 Basal bolus Prandial insulin Biphasic insulin 5895 Basal insulin 6655 Metformin 1120 Glinides SU 5783 TZD Subjects (n) AGI -3 DPP-4 i -2. 5 GLP-1 RA Change in Hb. A 1 c (%) 0 2967 AGI, alpha-glucosidase inhibitor; DPP-4 i, dipeptidyl peptidase-4 inhibitor; GLP-1 RA, glucagon-like peptide-1 receptor agonist; Hb. A 1 c, glycosylated haemoglobin; SU, sulphonylurea; TZD, thiazolidinedione. Esposito et al. Diabetes Obes Metab. 2012; 14: 228– 233.
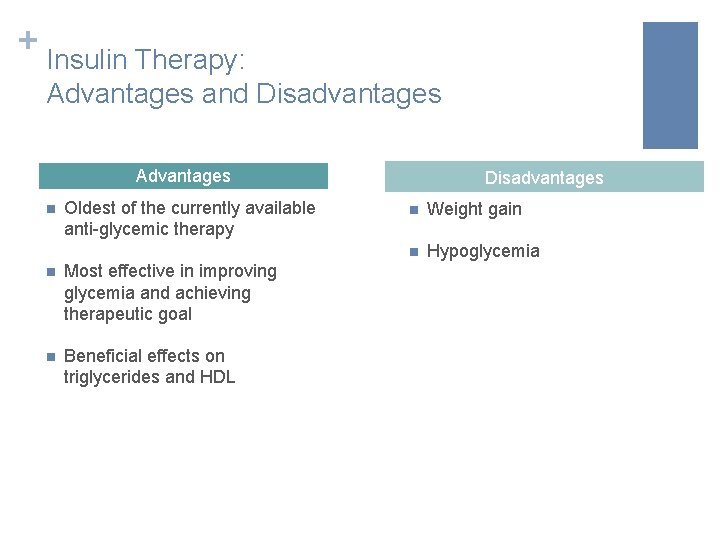
+ Insulin Therapy: Advantages and Disadvantages Advantages n Oldest of the currently available anti-glycemic therapy n Most effective in improving glycemia and achieving therapeutic goal n Beneficial effects on triglycerides and HDL Disadvantages n Weight gain n Hypoglycemia
+ Overview n When to initiate insulin n Early vs late (OAD failure)
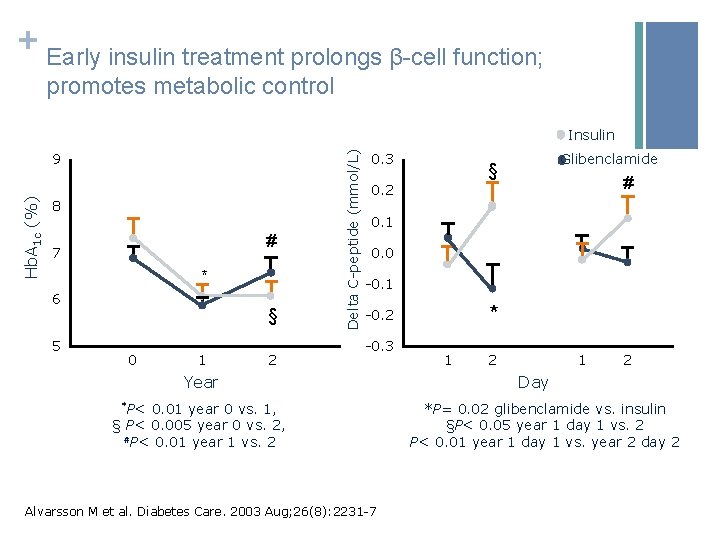
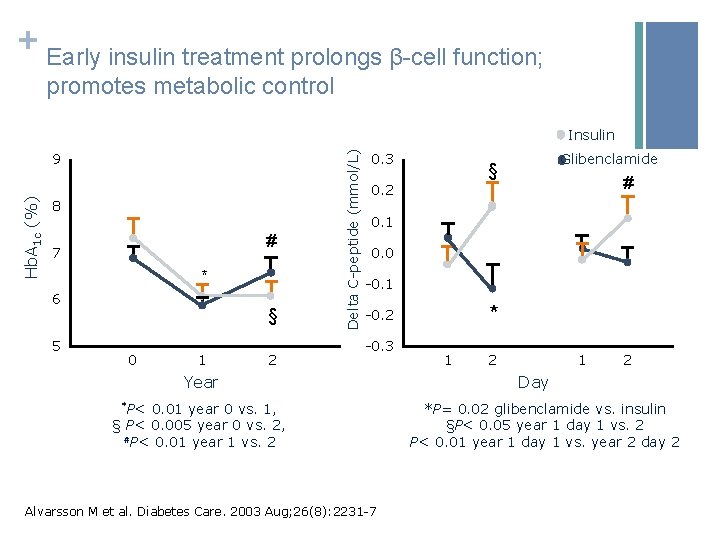
+ Early insulin treatment prolongs β-cell function; promotes metabolic control Hb. A 1 c (%) 9 8 # 7 * 6 5 § 0 1 2 Delta C-peptide (mmol/L) Insulin 0. 3 Glibenclamide § # 0. 2 0. 1 0. 0 -0. 1 * -0. 2 -0. 3 Year *P< 0. 01 year 0 vs. 1, § P< 0. 005 year 0 vs. 2, #P< 0. 01 year 1 vs. 2 Alvarsson M et al. Diabetes Care. 2003 Aug; 26(8): 2231 -7 1 2 Day *P= 0. 02 glibenclamide vs. insulin §P< 0. 05 year 1 day 1 vs. 2 P< 0. 01 year 1 day 1 vs. year 2 day 2
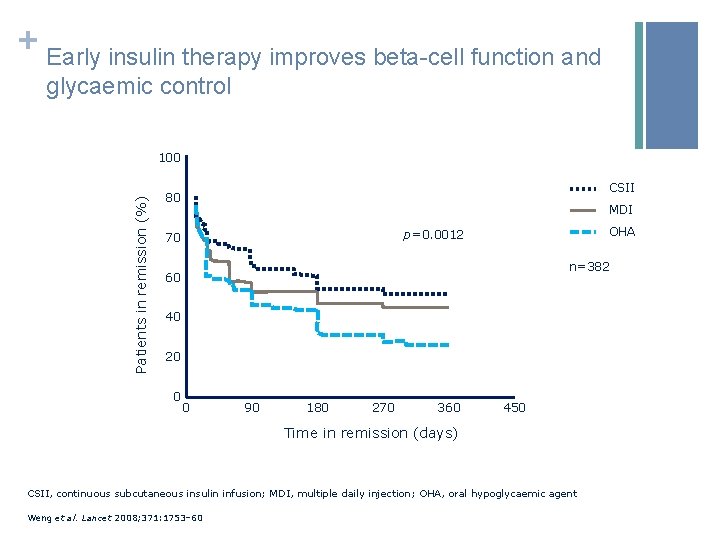
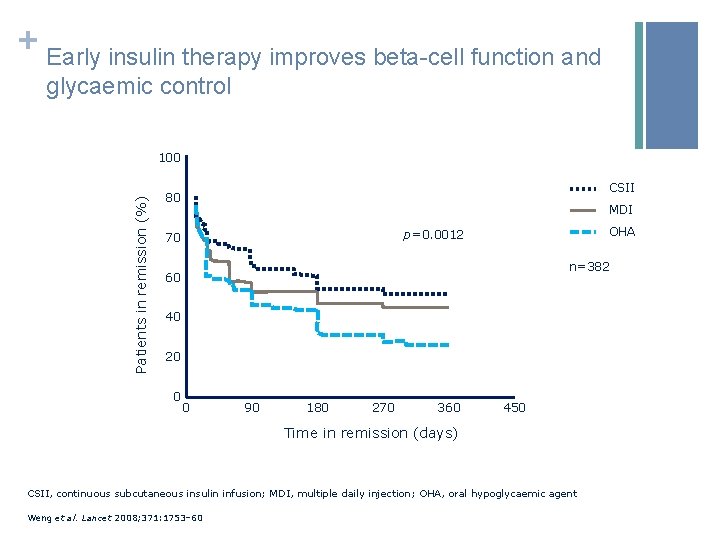
+ Early insulin therapy improves beta-cell function and glycaemic control Patients in remission (%) 100 CSII 80 MDI OHA p=0. 0012 70 n=382 60 40 20 0 0 90 180 270 360 450 Time in remission (days) CSII, continuous subcutaneous insulin infusion; MDI, multiple daily injection; OHA, oral hypoglycaemic agent Weng et al. Lancet 2008; 371: 1753– 60
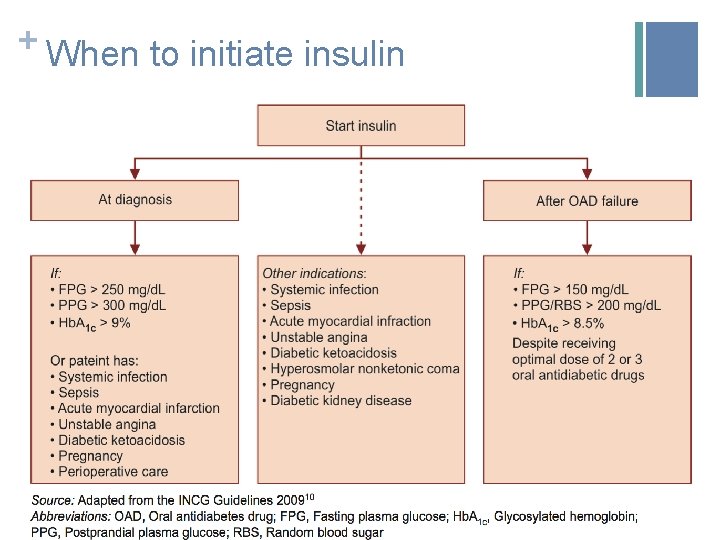
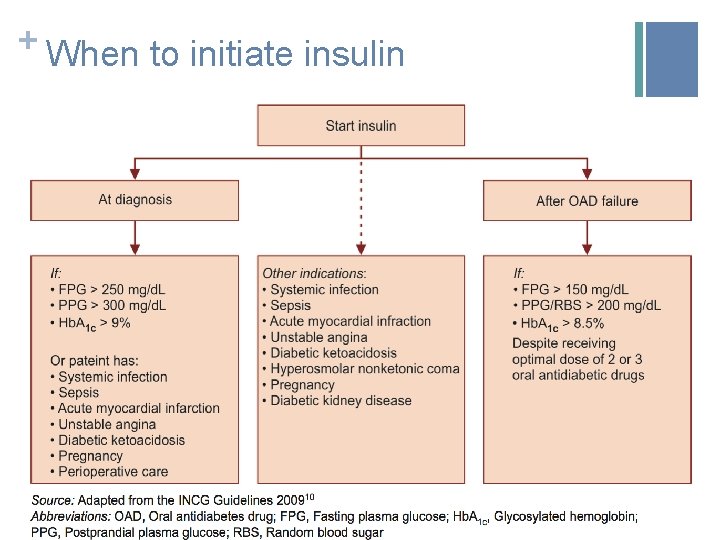
+ When to initiate insulin
+ Ideal candidates for insulin therapy n All diabetes patients! n Type 1 diabetes n Gestational diabetes n Type 2 diabetes on maximal doses of OADs n Acute metabolic decompensation states n Good control but fatigued/losing weight
+ Overview n Which insulin to initiate n Basal, prandial, premix, basal-bolus
+ Which Insulin? Basal Prandial Premix Basal-bolus
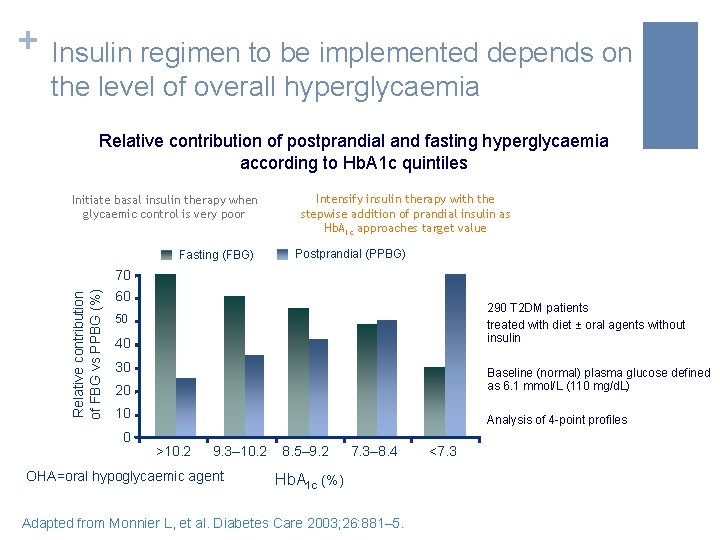
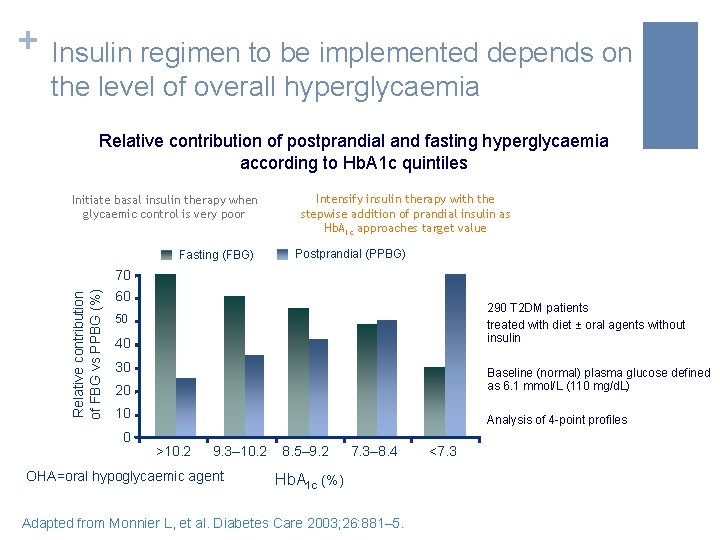
+ Insulin regimen to be implemented depends on the level of overall hyperglycaemia Relative contribution of postprandial and fasting hyperglycaemia according to Hb. A 1 c quintiles Initiate basal insulin therapy when glycaemic control is very poor Fasting (FBG) Intensify insulin therapy with the stepwise addition of prandial insulin as Hb. A 1 c approaches target value Postprandial (PPBG) Relative contribution of FBG vs PPBG (%) 70 60 290 T 2 DM patients treated with diet ± oral agents without insulin 50 40 30 20 Baseline (normal) plasma glucose defined as 6. 1 mmol/L (110 mg/d. L) 10 Analysis of 4 -point profiles 0 >10. 2 9. 3– 10. 2 OHA=oral hypoglycaemic agent 8. 5– 9. 2 7. 3– 8. 4 Hb. A 1 c (%) Adapted from Monnier L, et al. Diabetes Care 2003; 26: 881– 5. <7. 3
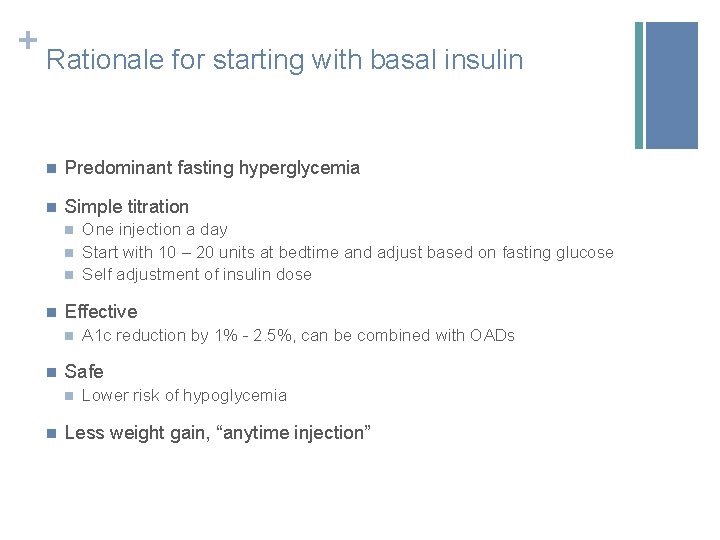
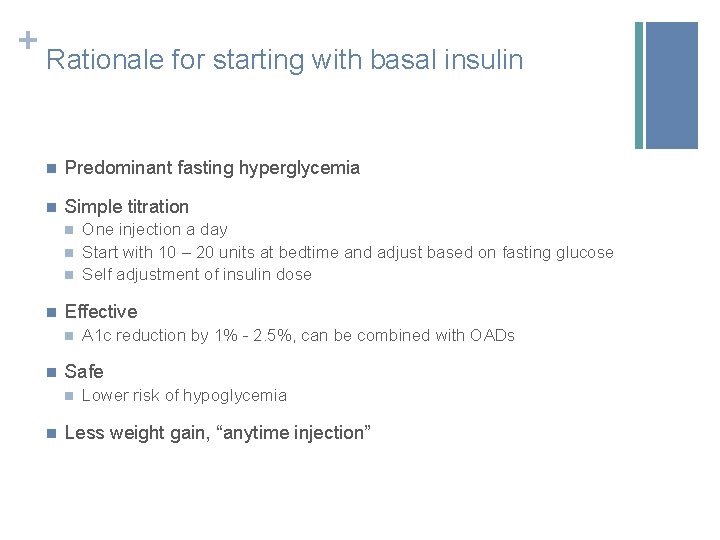
+ Rationale for starting with basal insulin n Predominant fasting hyperglycemia n Simple titration n n Effective n n A 1 c reduction by 1% - 2. 5%, can be combined with OADs Safe n n One injection a day Start with 10 – 20 units at bedtime and adjust based on fasting glucose Self adjustment of insulin dose Lower risk of hypoglycemia Less weight gain, “anytime injection”
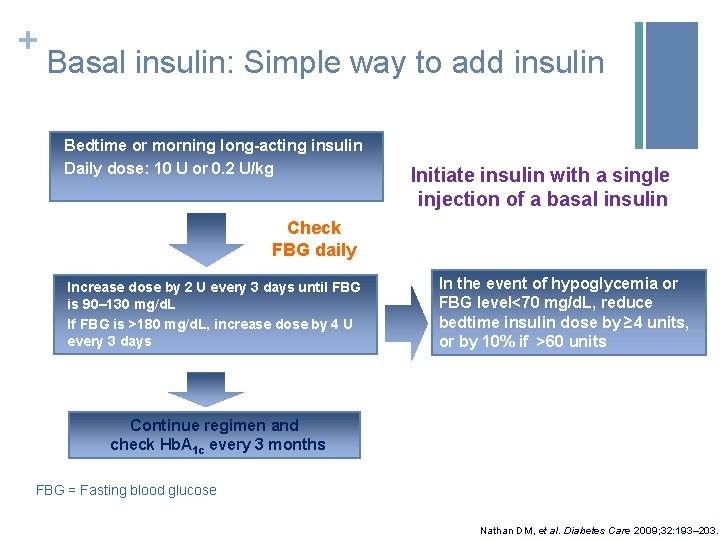
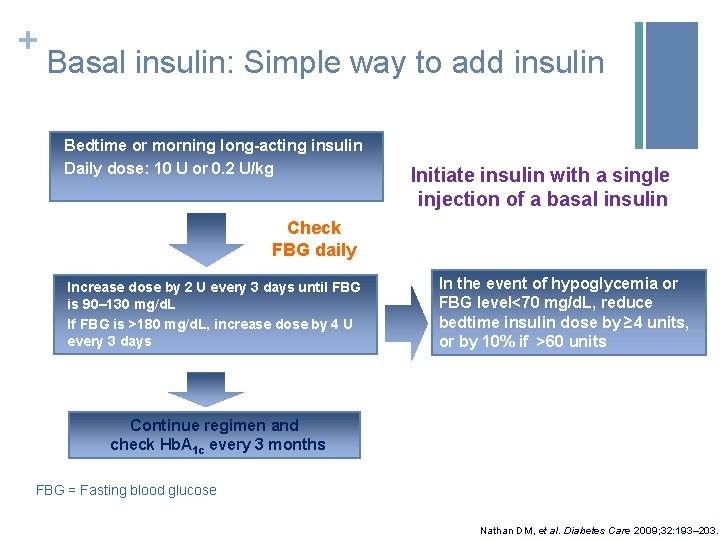
+ Basal insulin: Simple way to add insulin Bedtime or morning long-acting insulin Daily dose: 10 U or 0. 2 U/kg Initiate insulin with a single injection of a basal insulin Check FBG daily Increase dose by 2 U every 3 days until FBG is 90– 130 mg/d. L If FBG is >180 mg/d. L, increase dose by 4 U every 3 days In the event of hypoglycemia or FBG level<70 mg/d. L, reduce bedtime insulin dose by ≥ 4 units, or by 10% if >60 units Continue regimen and check Hb. A 1 c every 3 months FBG = Fasting blood glucose Nathan DM, et al. Diabetes Care 2009; 32: 193– 203.
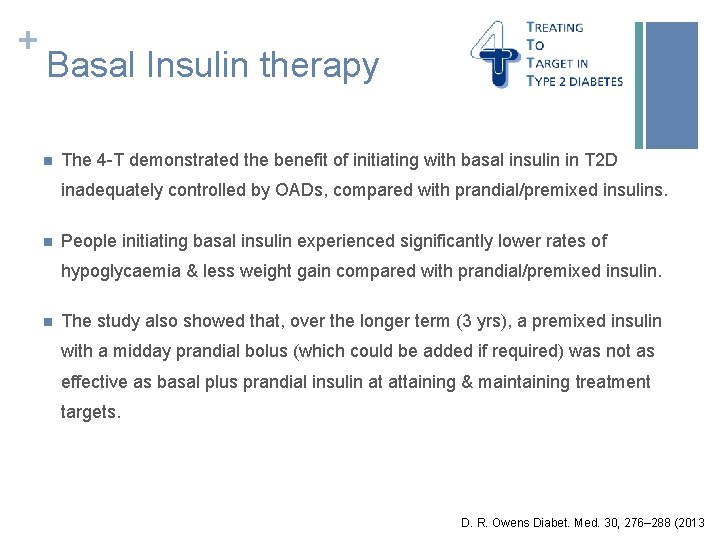
+ Basal Insulin therapy n The 4 -T demonstrated the benefit of initiating with basal insulin in T 2 D inadequately controlled by OADs, compared with prandial/premixed insulins. n People initiating basal insulin experienced significantly lower rates of hypoglycaemia & less weight gain compared with prandial/premixed insulin. n The study also showed that, over the longer term (3 yrs), a premixed insulin with a midday prandial bolus (which could be added if required) was not as effective as basal plus prandial insulin at attaining & maintaining treatment targets. D. R. Owens Diabet. Med. 30, 276– 288 (2013
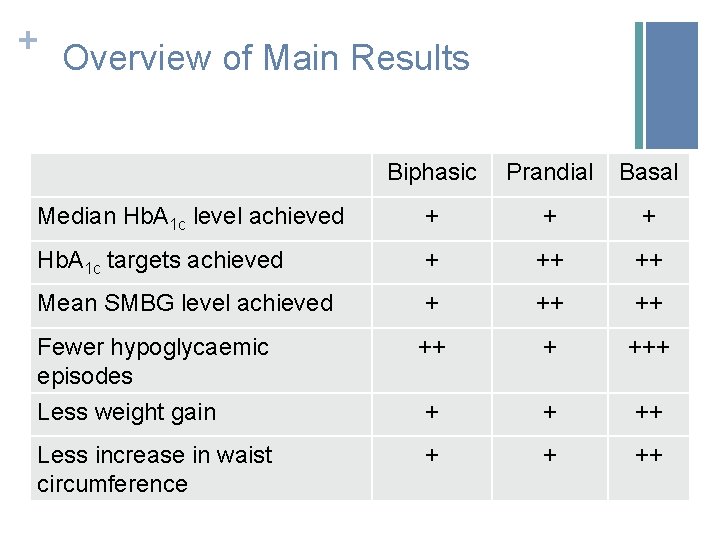
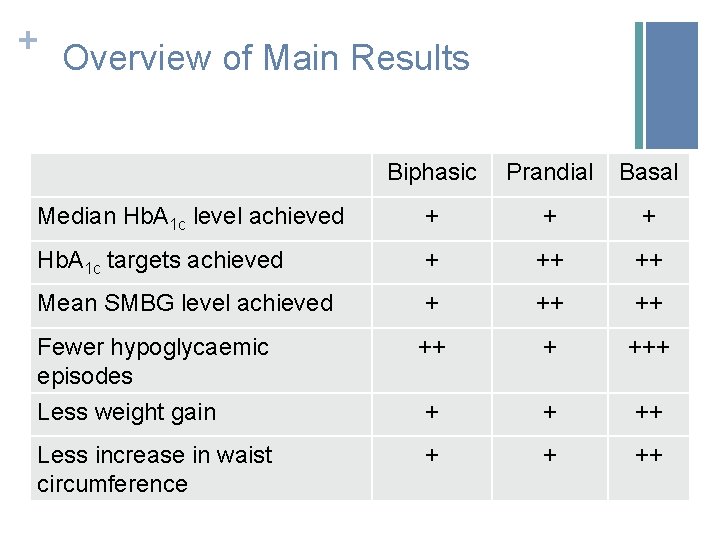
+ Overview of Main Results Biphasic Prandial Basal Median Hb. A 1 c level achieved + + + Hb. A 1 c targets achieved + ++ ++ Mean SMBG level achieved + ++ ++ Fewer hypoglycaemic episodes Less weight gain ++ + + ++ Less increase in waist circumference + + ++
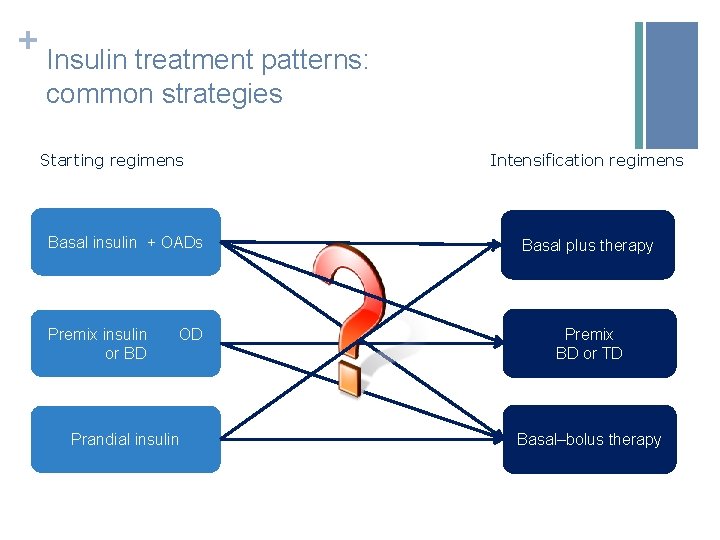
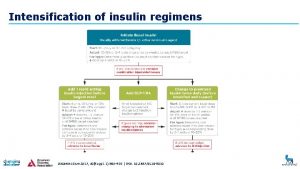
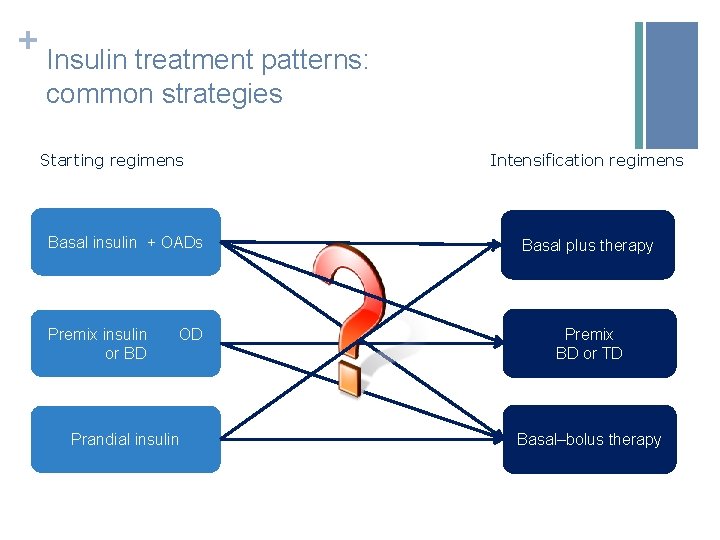
+ Insulin treatment patterns: common strategies Starting regimens Intensification regimens Basal insulin + OADs Basal plus therapy Premix insulin OD or BD Premix BD or TD Prandial insulin Basal–bolus therapy
+ Overview n What to do for follow-up n Titration, hypoglycemia, achieving targets
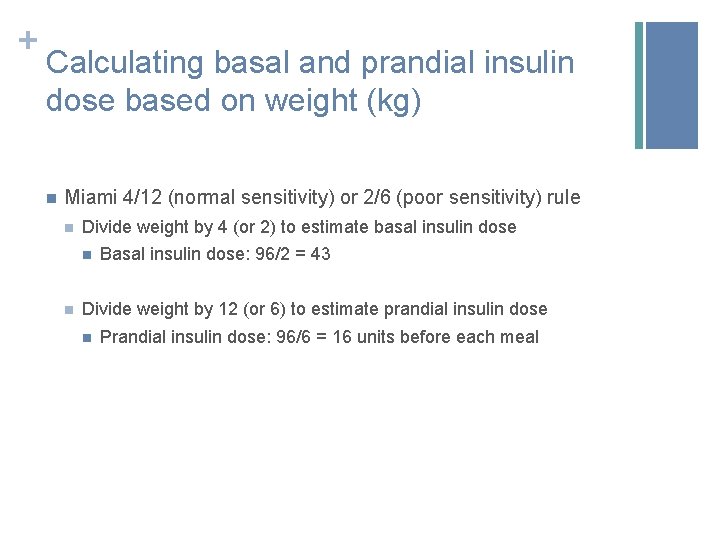
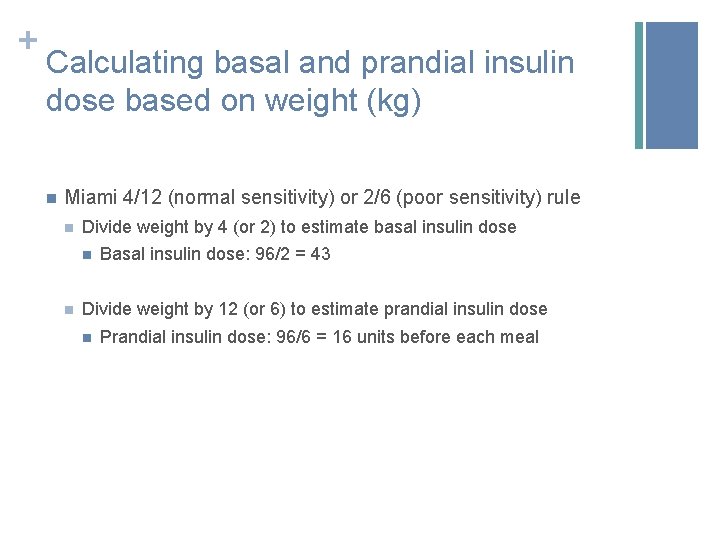
+ Calculating basal and prandial insulin dose based on weight (kg) n Miami 4/12 (normal sensitivity) or 2/6 (poor sensitivity) rule n Divide weight by 4 (or 2) to estimate basal insulin dose n n Basal insulin dose: 96/2 = 43 Divide weight by 12 (or 6) to estimate prandial insulin dose n Prandial insulin dose: 96/6 = 16 units before each meal
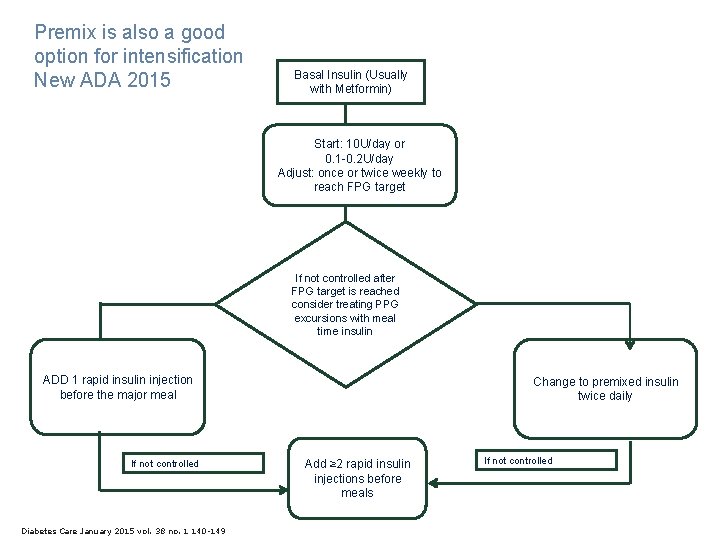
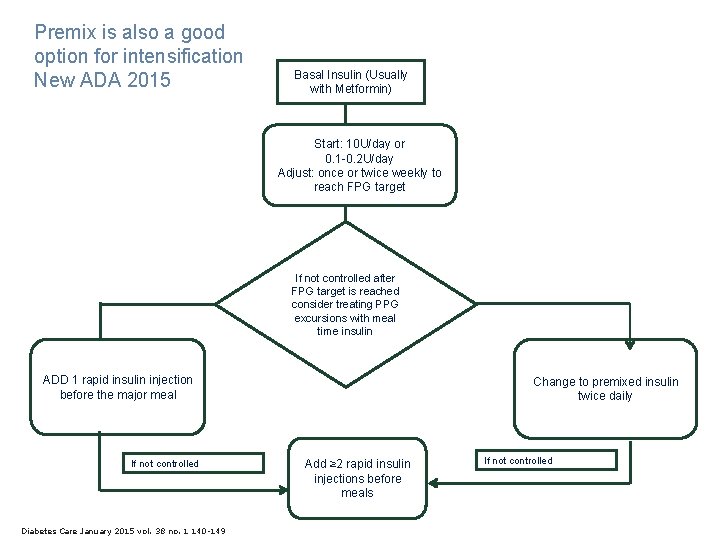
Premix is also a good option for intensification New ADA 2015 Basal Insulin (Usually with Metformin) Start: 10 U/day or 0. 1 -0. 2 U/day Adjust: once or twice weekly to reach FPG target If not controlled after FPG target is reached consider treating PPG excursions with meal time insulin ADD 1 rapid insulin injection before the major meal If not controlled Diabetes Care January 2015 vol. 38 no. 1 140 -149 Change to premixed insulin twice daily Add ≥ 2 rapid insulin injections before meals If not controlled
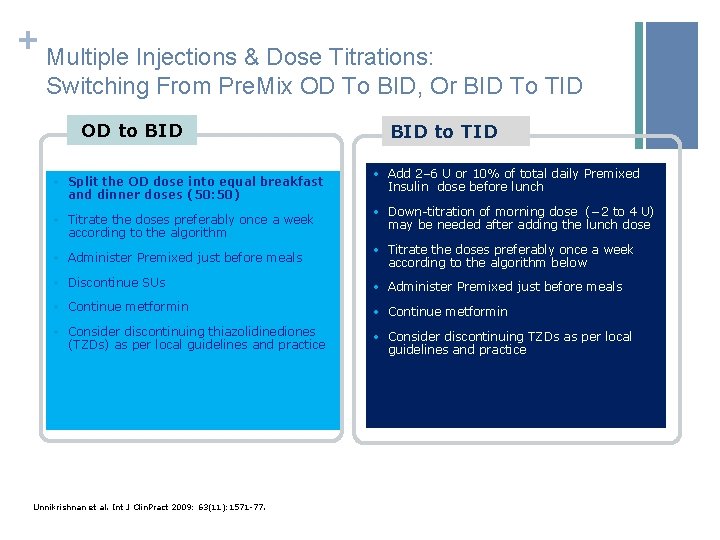
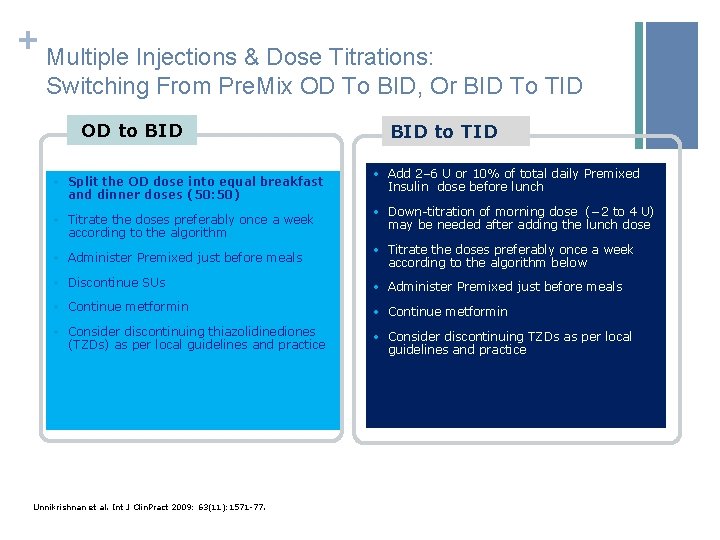
+ Multiple Injections & Dose Titrations: Switching From Pre. Mix OD To BID, Or BID To TID OD to BID • Split the OD dose into equal breakfast and dinner doses (50: 50) • Titrate the doses preferably once a week according to the algorithm BID to TID • Add 2– 6 U or 10% of total daily Premixed Insulin dose before lunch • Down-titration of morning dose (− 2 to 4 U) may be needed after adding the lunch dose • Administer Premixed just before meals • Titrate the doses preferably once a week according to the algorithm below • Discontinue SUs • Administer Premixed just before meals • Continue metformin • Consider discontinuing thiazolidinediones (TZDs) as per local guidelines and practice • Consider discontinuing TZDs as per local guidelines and practice Unnikrishnan et al. Int J Clin. Pract 2009: 63(11): 1571 -77.
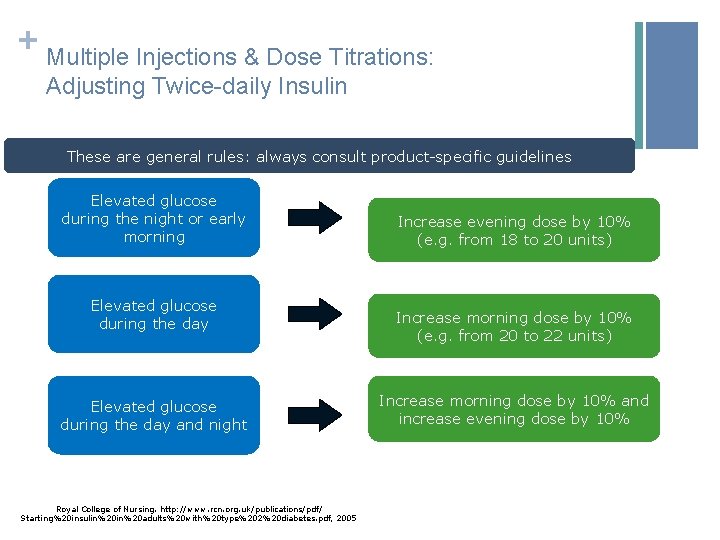
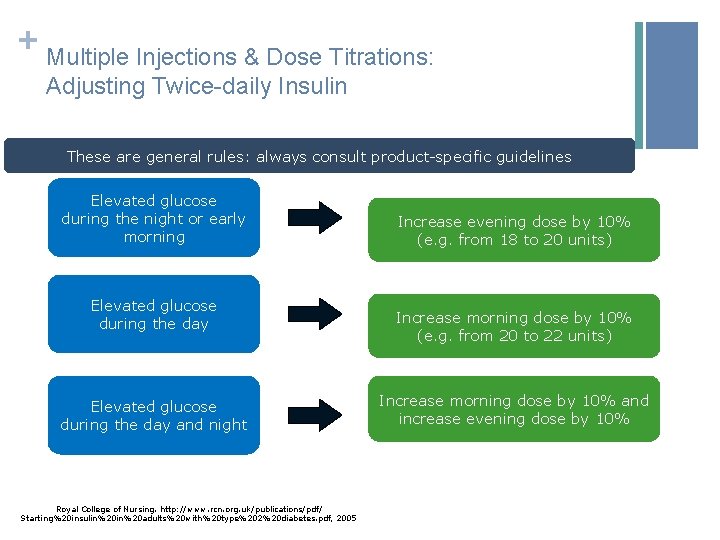
+ Multiple Injections & Dose Titrations: Adjusting Twice-daily Insulin These are general rules: always consult product-specific guidelines Elevated glucose during the night or early morning Elevated glucose during the day and night Royal College of Nursing. http: //www. rcn. org. uk/publications/pdf/ Starting%20 insulin%20 adults%20 with%20 type%202%20 diabetes. pdf, 2005 Increase evening dose by 10% (e. g. from 18 to 20 units) Increase morning dose by 10% (e. g. from 20 to 22 units) Increase morning dose by 10% and increase evening dose by 10%
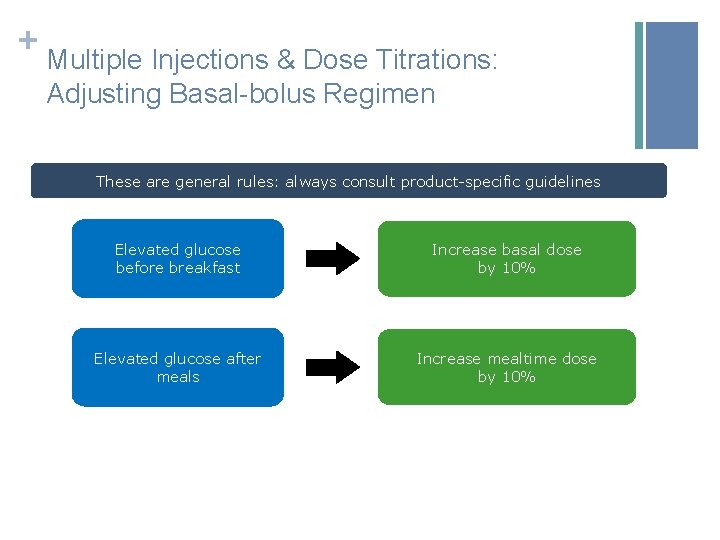
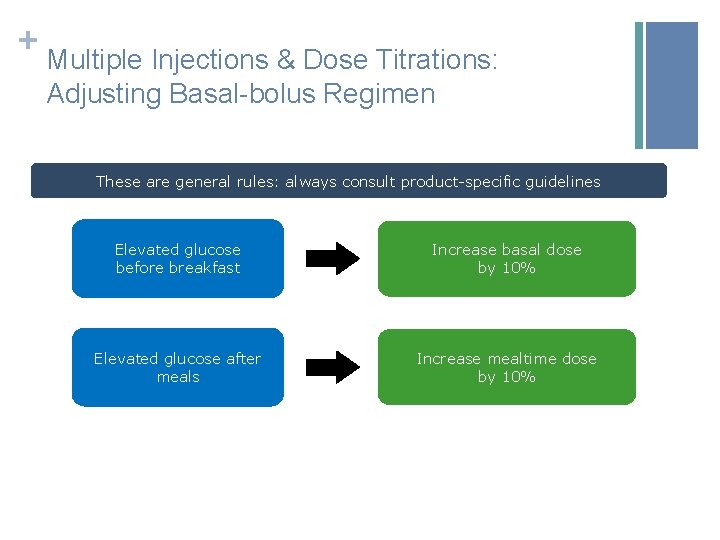
+ Multiple Injections & Dose Titrations: Adjusting Basal-bolus Regimen These are general rules: always consult product-specific guidelines Elevated glucose before breakfast Increase basal dose by 10% Elevated glucose after meals Increase mealtime dose by 10%
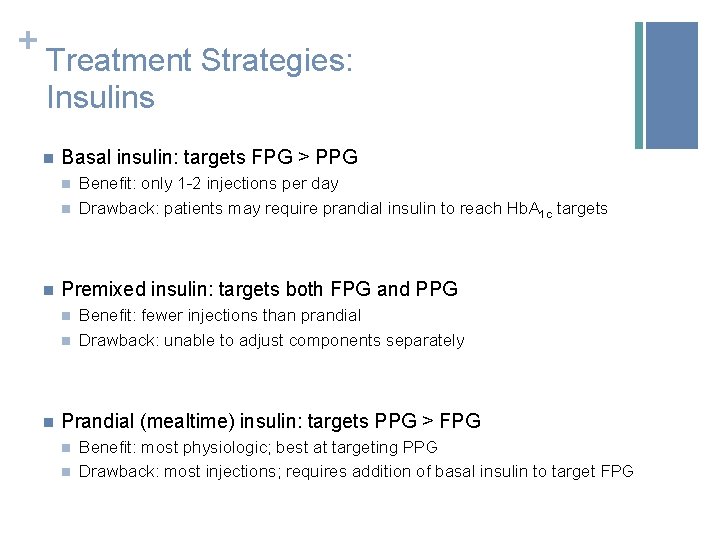
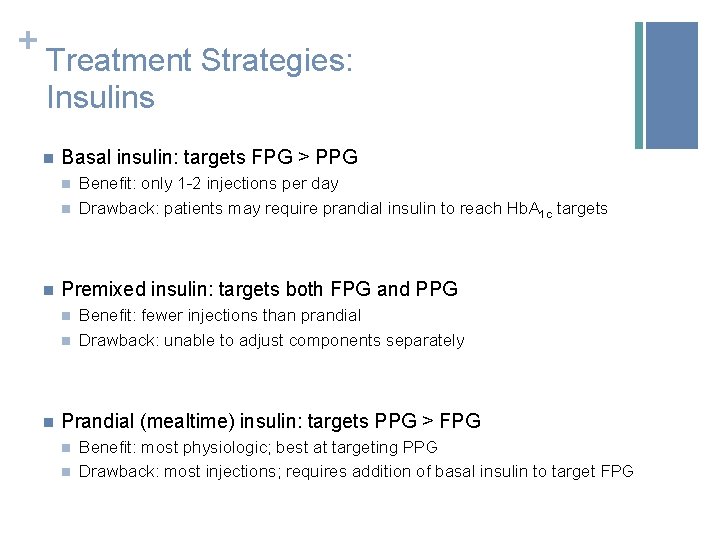
+ Treatment Strategies: Insulins n Basal insulin: targets FPG > PPG n n n Premixed insulin: targets both FPG and PPG n n n Benefit: only 1 -2 injections per day Drawback: patients may require prandial insulin to reach Hb. A 1 c targets Benefit: fewer injections than prandial Drawback: unable to adjust components separately Prandial (mealtime) insulin: targets PPG > FPG n n Benefit: most physiologic; best at targeting PPG Drawback: most injections; requires addition of basal insulin to target FPG Lasserson DS, et al. Diabetologia. 2009; 52(10): 1990 -2000.
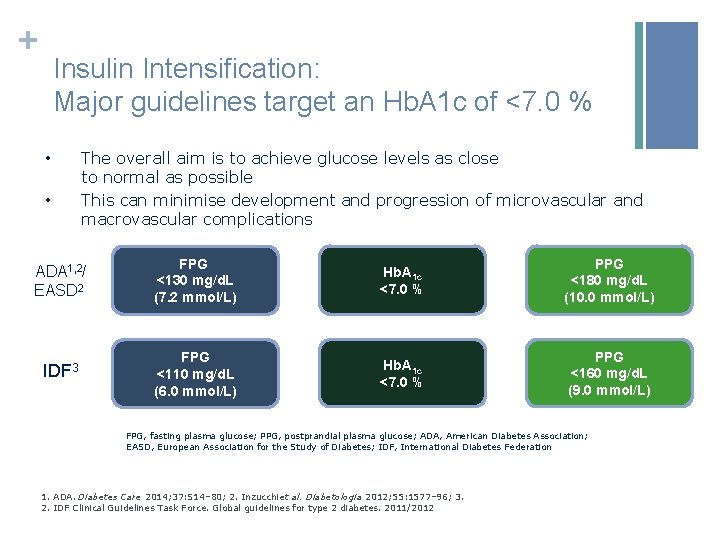
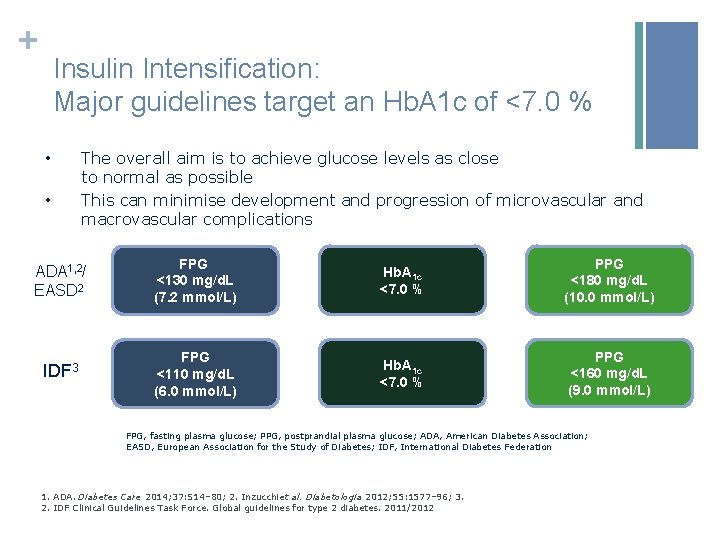
+ Insulin Intensification: Major guidelines target an Hb. A 1 c of <7. 0 % • • The overall aim is to achieve glucose levels as close to normal as possible This can minimise development and progression of microvascular and macrovascular complications ADA 1, 2/ EASD 2 FPG <130 mg/d. L (7. 2 mmol/L) Hb. A 1 c <7. 0 % PPG <180 mg/d. L (10. 0 mmol/L) IDF 3 FPG <110 mg/d. L (6. 0 mmol/L) Hb. A 1 c <7. 0 % PPG <160 mg/d. L (9. 0 mmol/L) FPG, fasting plasma glucose; PPG, postprandial plasma glucose; ADA, American Diabetes Association; EASD, European Association for the Study of Diabetes; IDF, International Diabetes Federation 1. ADA. Diabetes Care 2014; 37: S 14– 80; 2. Inzucchiet al. Diabetologia 2012; 55: 1577– 96; 3. 2. IDF Clinical Guidelines Task Force. Global guidelines for type 2 diabetes. 2011/2012
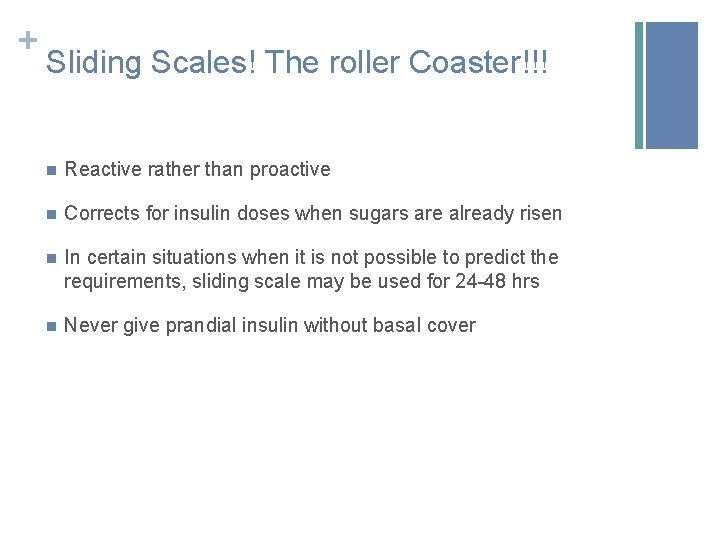
+ Sliding Scales! The roller Coaster!!! n Reactive rather than proactive n Corrects for insulin doses when sugars are already risen n In certain situations when it is not possible to predict the requirements, sliding scale may be used for 24 -48 hrs n Never give prandial insulin without basal cover
+ What about OADs while initiating insulin n Metformin, AGIs, DPP 4 i & SGLT 2 i therapy may be continued n SUs may be continued when basal insulin alone is used n Usually SUs should be discontinued when initiated on basalbolus or premix insulins
+ Clinical pearls while writing prescription n Do not add basal and premix on same prescription n Write clearly the relation between insulin timing and meals n Specify insulin administration sites and frequency of insulin needle change n Explain clearly about expectations regarding glycemic control n Address patient concerns regarding insulin
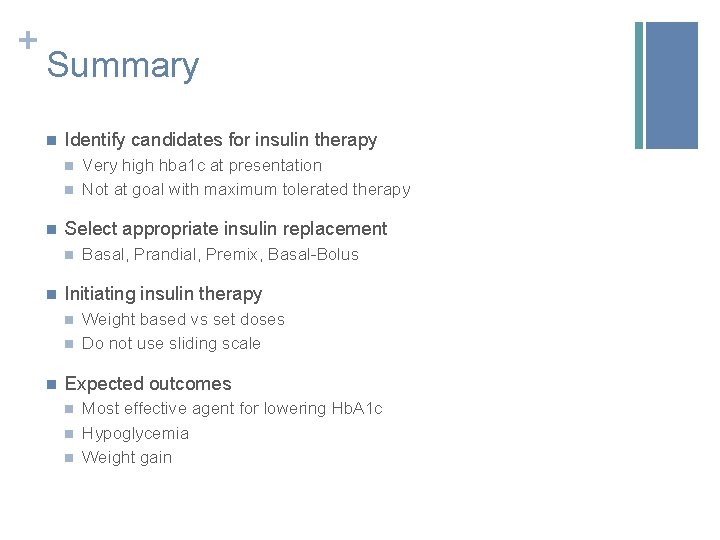
+ Summary n Identify candidates for insulin therapy n n n Select appropriate insulin replacement n n Basal, Prandial, Premix, Basal-Bolus Initiating insulin therapy n n n Very high hba 1 c at presentation Not at goal with maximum tolerated therapy Weight based vs set doses Do not use sliding scale Expected outcomes n n n Most effective agent for lowering Hb. A 1 c Hypoglycemia Weight gain
 Mechanism of action of insulin
Mechanism of action of insulin Insulin and insulin receptor
Insulin and insulin receptor Rapid intensification
Rapid intensification Western intensification
Western intensification Sri system of rice intensification
Sri system of rice intensification Sri system of rice intensification
Sri system of rice intensification Process intensification example
Process intensification example Sri system of rice intensification
Sri system of rice intensification System of rice intensification
System of rice intensification Stages of rice plant
Stages of rice plant Sri system of rice intensification
Sri system of rice intensification Ethics beauchamp and childress
Ethics beauchamp and childress Psychoanalytic vs humanistic
Psychoanalytic vs humanistic Bioness bits cost
Bioness bits cost Psychoanalytic therapy is to as humanistic therapy is to
Psychoanalytic therapy is to as humanistic therapy is to Is responsible for all file i/o initiation and termination
Is responsible for all file i/o initiation and termination Initiation and maintenance of callus culture
Initiation and maintenance of callus culture Project identification and selection
Project identification and selection Clozapine titration chart
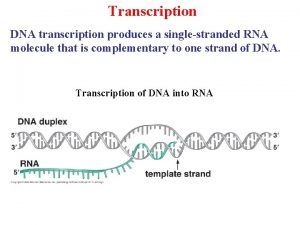
Clozapine titration chart Rna polymerase
Rna polymerase Separation initiation return
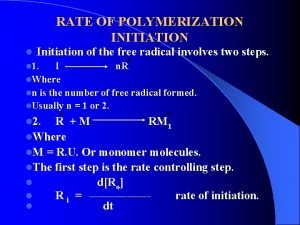
Separation initiation return Initiation radical reaction
Initiation radical reaction Raci 차트
Raci 차트 Importance of project initiation
Importance of project initiation Initiation à la recherche en soins infirmiers
Initiation à la recherche en soins infirmiers Site initiation visit in clinical trials ppt
Site initiation visit in clinical trials ppt Contoh inisiasi proyek sistem informasi
Contoh inisiasi proyek sistem informasi Home visiting meaning
Home visiting meaning Divergent diagram
Divergent diagram The creature of nightmare archetype examples
The creature of nightmare archetype examples Site initiation visit
Site initiation visit Sensibilisation et initiation à la cybersécurité
Sensibilisation et initiation à la cybersécurité Knapp's model of relational stages
Knapp's model of relational stages Initiation à la qualité
Initiation à la qualité L'initiation
L'initiation Initiation à la démonstration 5ème
Initiation à la démonstration 5ème