In the name of God Congenital Laryngeal Anomalies

- Slides: 55
In the name of God
Congenital Laryngeal Anomalies M. H. Baradaranfar M. D professor of otolaryngology Head and Neck surgery Rhinologist
Introduction n n Wide range of problems Anatomy Embryology Diagnosis Types: supraglottis, subglottis n n Presentation/diagnosis Management
Normal Anatomy n Larynx n n Ventilates and protects lungs Clears secretions Voice Differences in adults and infants n n 1/3 size at birth Narrow dimensions (subglottis vs. glottis) Higher in neck and more pliable Epiglottis narrower
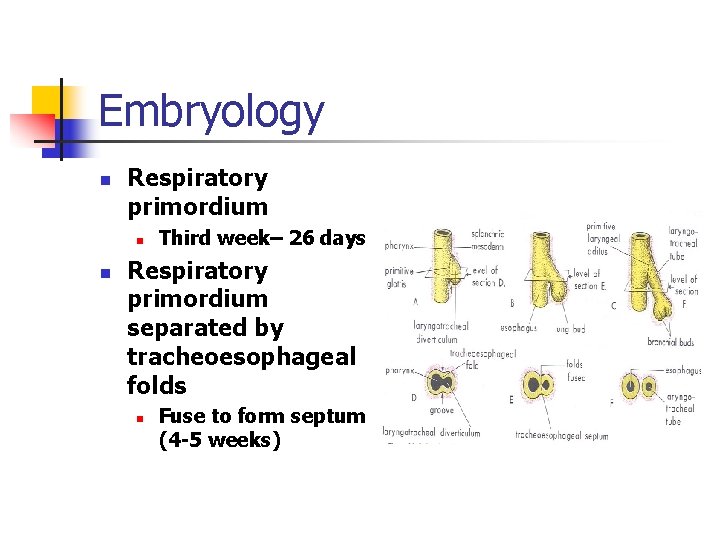
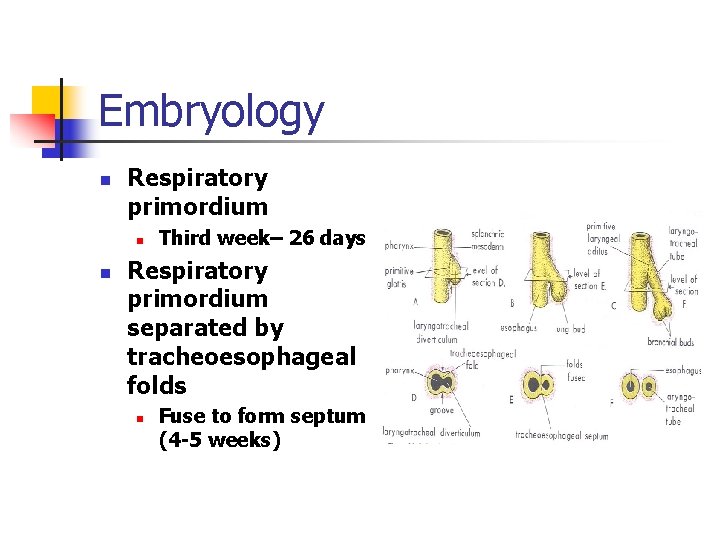
Embryology n Respiratory primordium n n Third week– 26 days Respiratory primordium separated by tracheoesophageal folds n Fuse to form septum (4 -5 weeks)
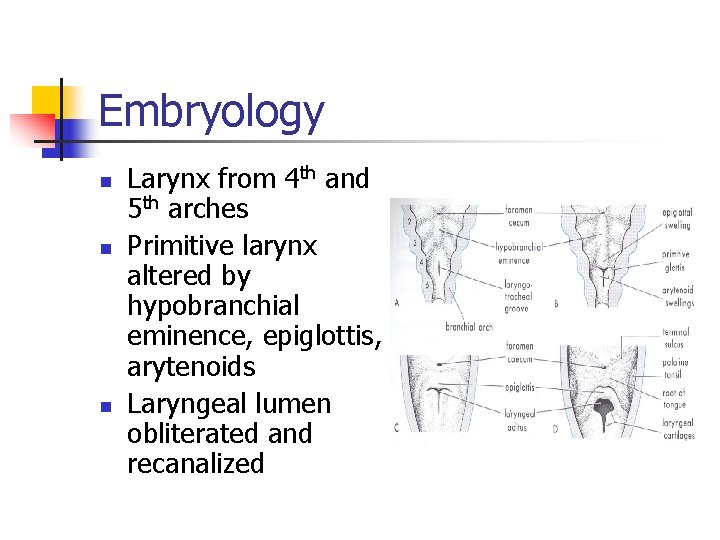
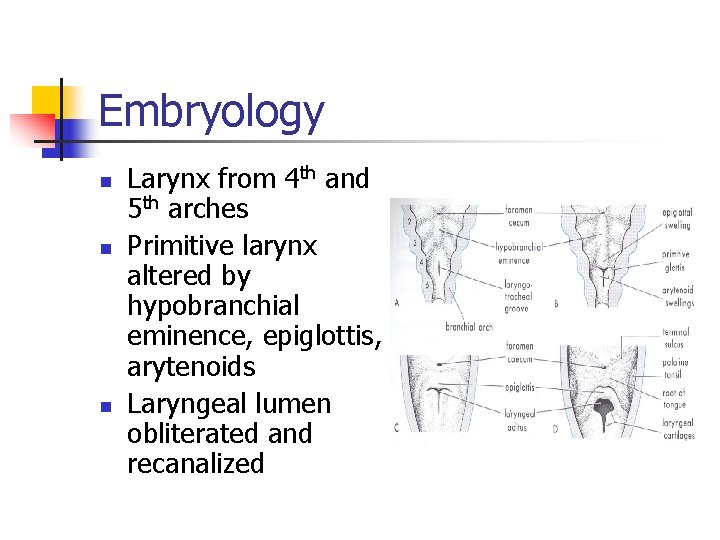
Embryology n n n Larynx from 4 th and 5 th arches Primitive larynx altered by hypobranchial eminence, epiglottis, arytenoids Laryngeal lumen obliterated and recanalized
Clinical Manifestations n n n n Respiratory obstruction Stridor Weak cry Dyspnea Tachypnea Aspiration Cyanosis Sudden death
Clinical Diagnosis n History n n Premature, medical problems Birth records, intubation history Symptom frequency, feeding Physical exam n n n Observation Voice Flexible exam
Clinical Diagnosis n Radiography n n Neck films, chest films Barium swallow CT/MRI Endoscopy in OR n Gold standard
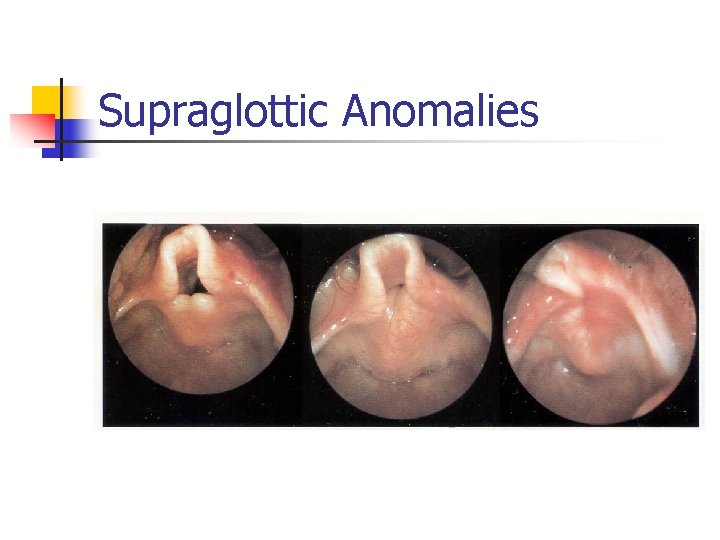
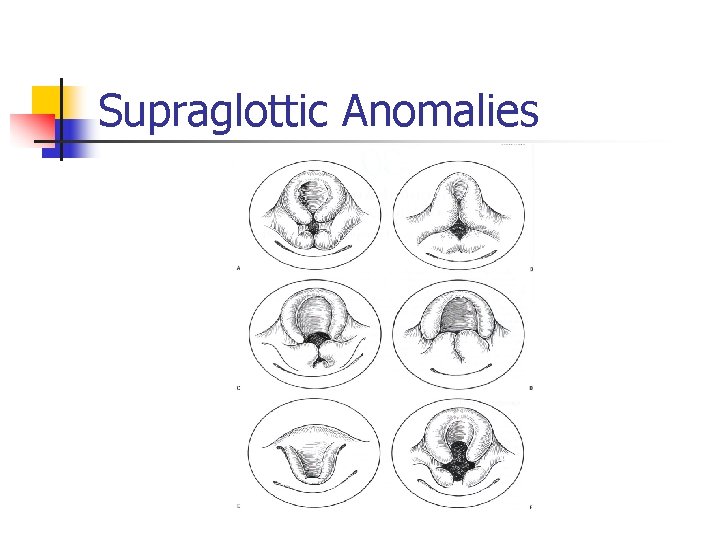
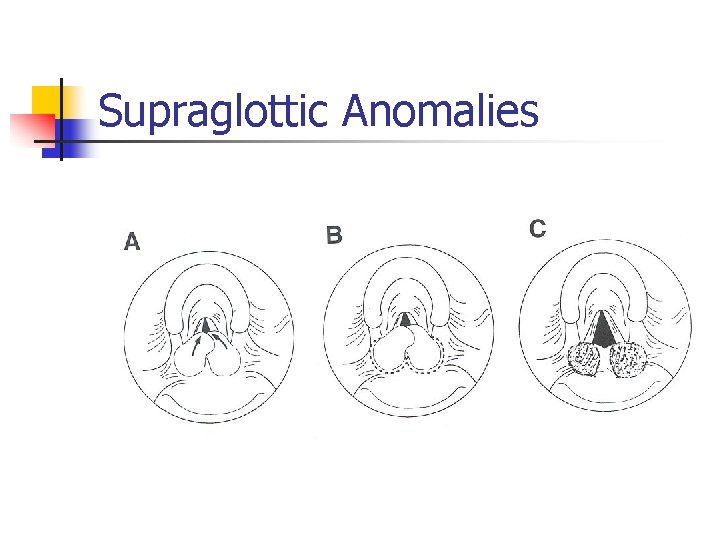
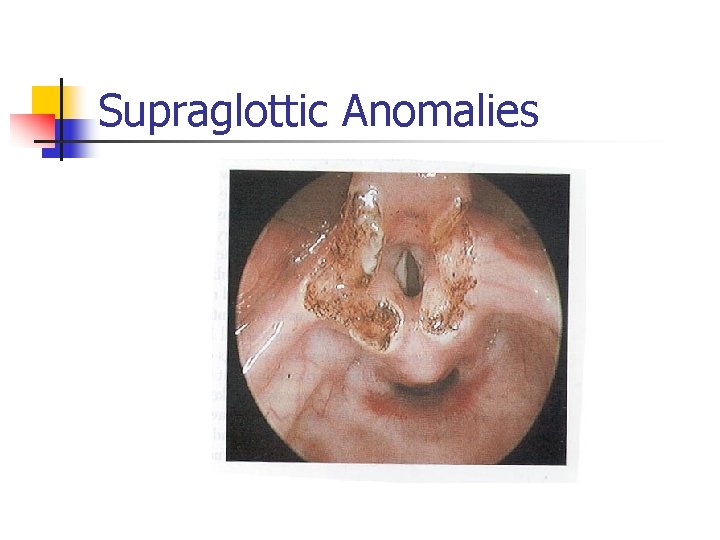
Supraglottic Anomalies n Laryngomalacia n n n Most common (60%) Boys>girls Inspiratory stridor: *not always at birth Benign, self-limiting May be severe Immature larynx
Supraglottic Anomalies n Laryngomalacia n n n Diagnosis: flexible laryngoscopy Occasional endoscopy Treatment= expectant, reassurance n n n Position changes Close follow up Severe cases= surgery
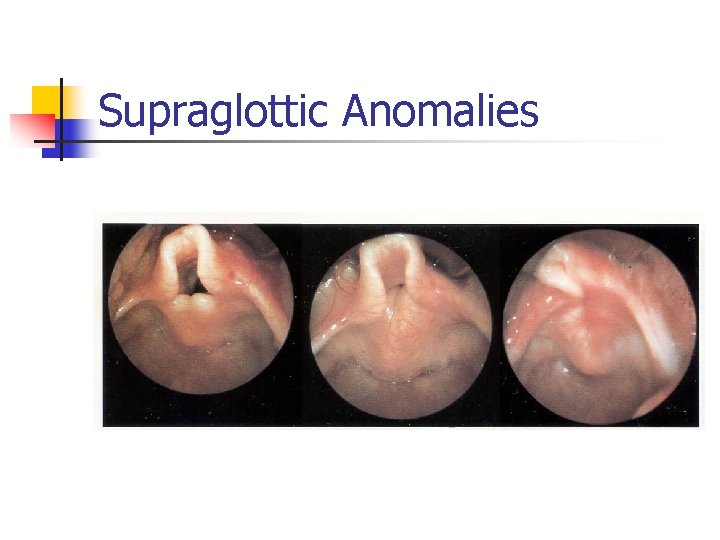
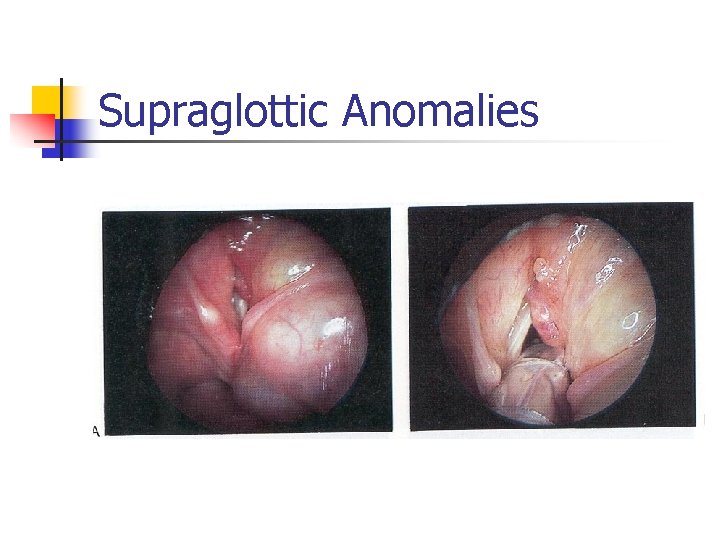
Supraglottic Anomalies
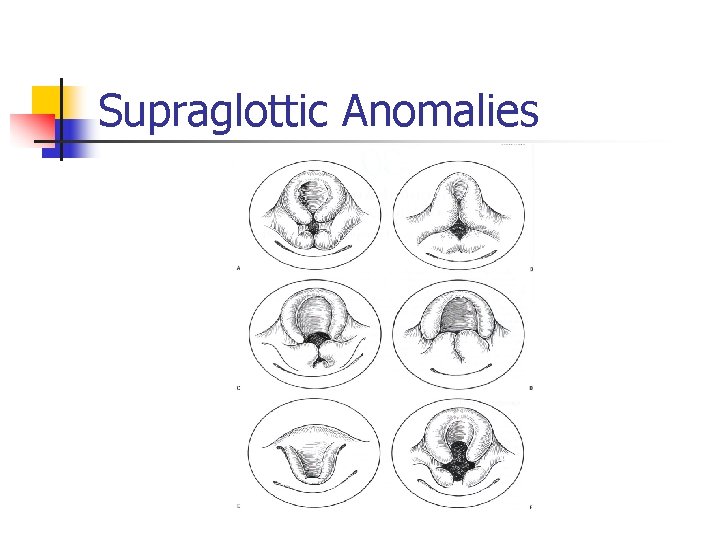
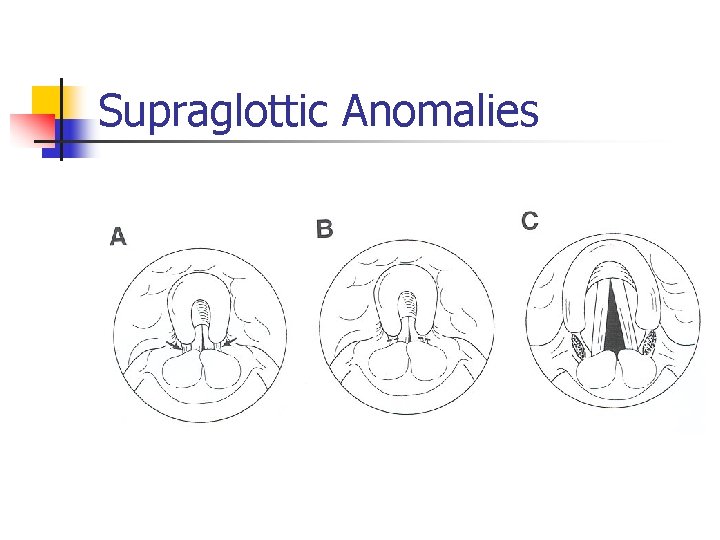
Supraglottic Anomalies
Supraglottic Anomalies
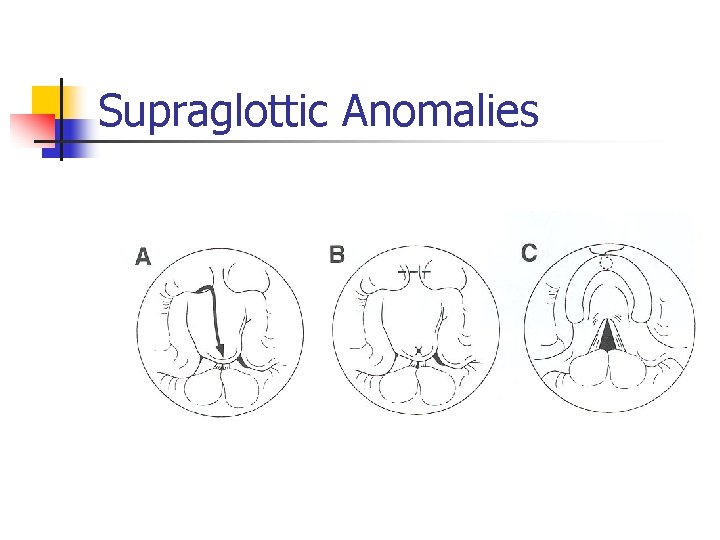
Supraglottic Anomalies
Supraglottic Anomalies
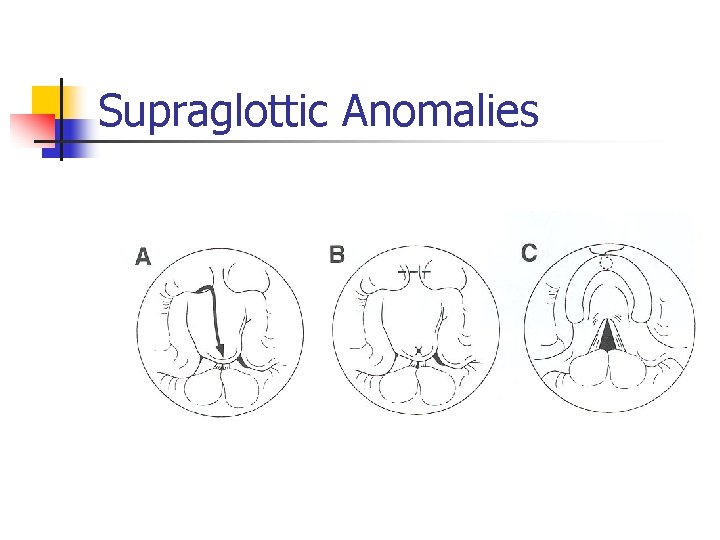
Supraglottic Anomalies
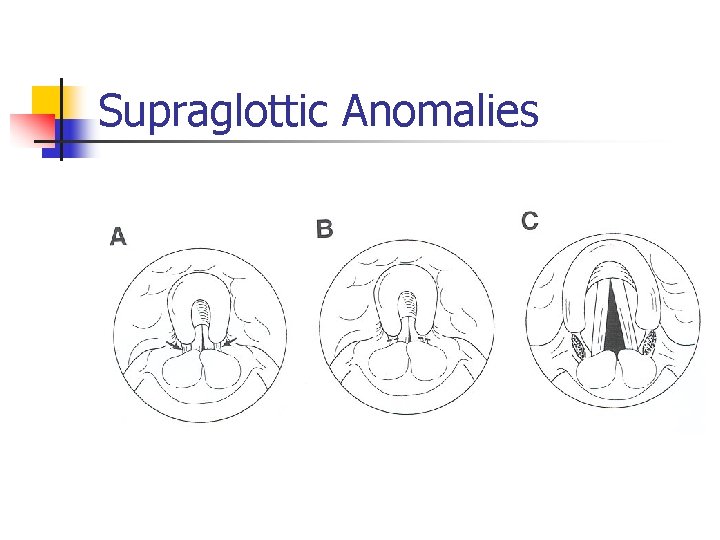
Supraglottic Anomalies n Results of supraglottoplasty n Largest series: 53% complete regression n n 2 needed tracheotomy, pharyngomalacia ? Bi. PAP Other studies: 77 -100% Complications: stenosis, CA fixation, PGS GERD association?
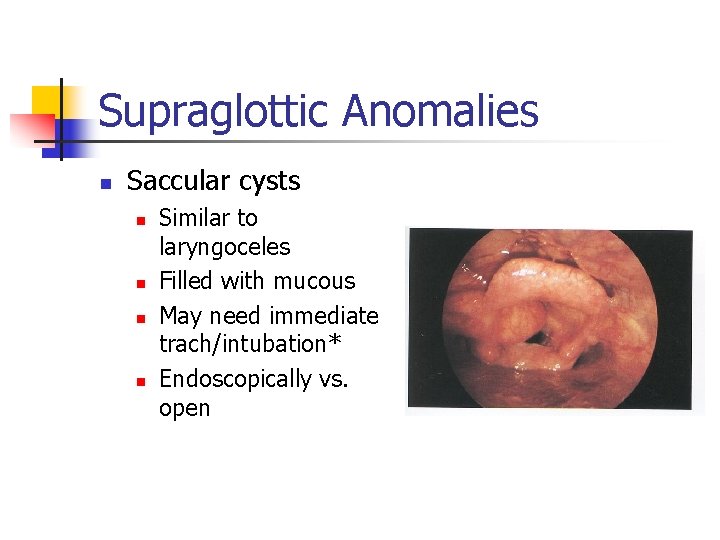
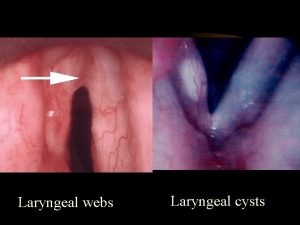
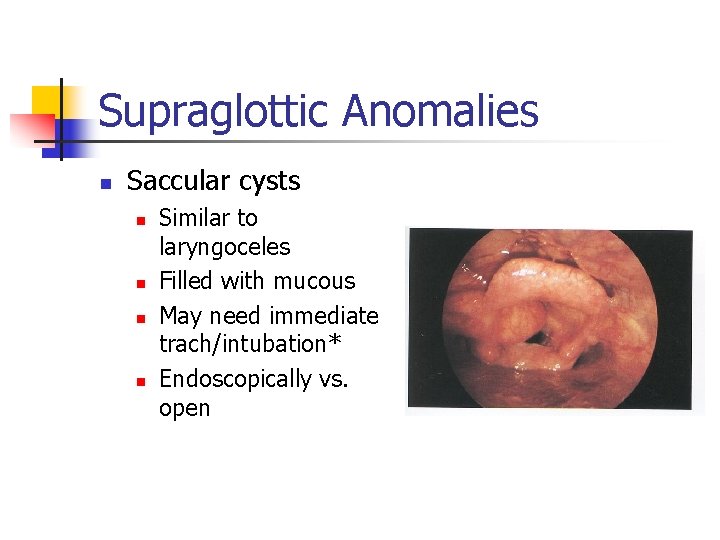
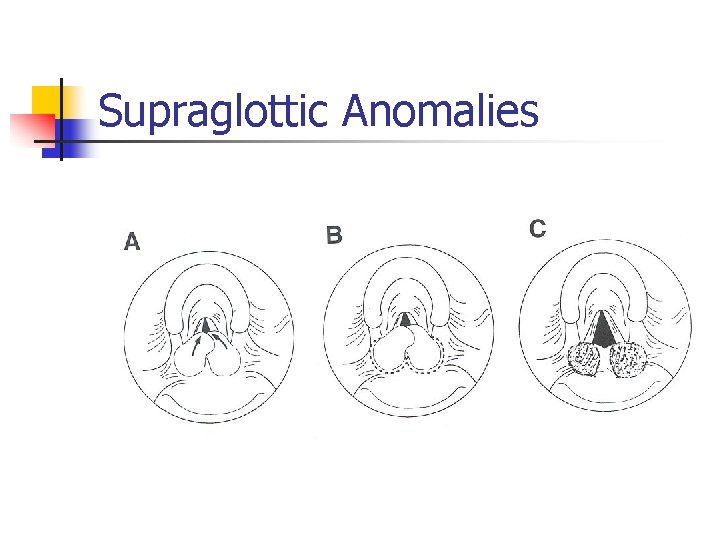
Supraglottic Anomalies n Saccular cysts n n Similar to laryngoceles Filled with mucous May need immediate trach/intubation* Endoscopically vs. open
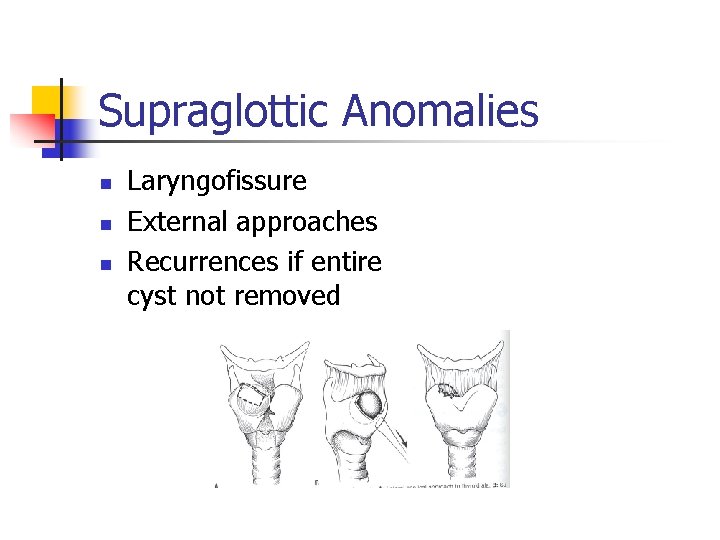
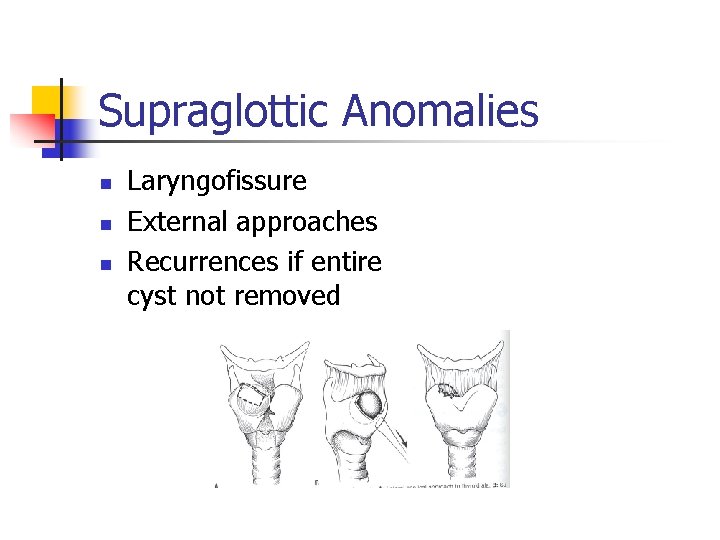
Supraglottic Anomalies n n n Laryngofissure External approaches Recurrences if entire cyst not removed
Supraglottic Anomalies n Laryngocele n n n Dilated sac filled with air (ventricle) Internal vs. external May present at birth– stridor* Difficult to diagnose– CT? Endoscopic or open procedures Recurrences low
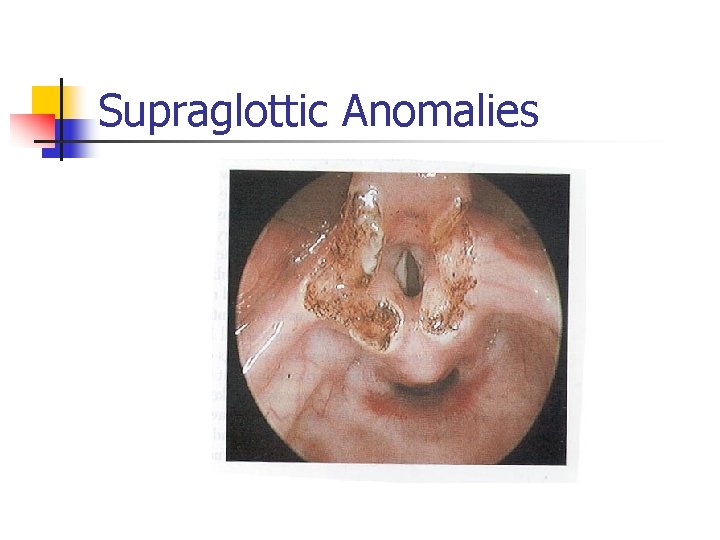
Supraglottic Anomalies n Vascular and lymphatic malformations n Hemangiomas n n n 30% birth– grow in first 6 -18 months Dyspnea, stridor, feeding problems later* Endoscopic evaluation Multiple treatment options Lymphangiomas n n n Compress epiglottis– airway distress at birth* Symptoms varied Endoscopic evaluation: CO 2 laser
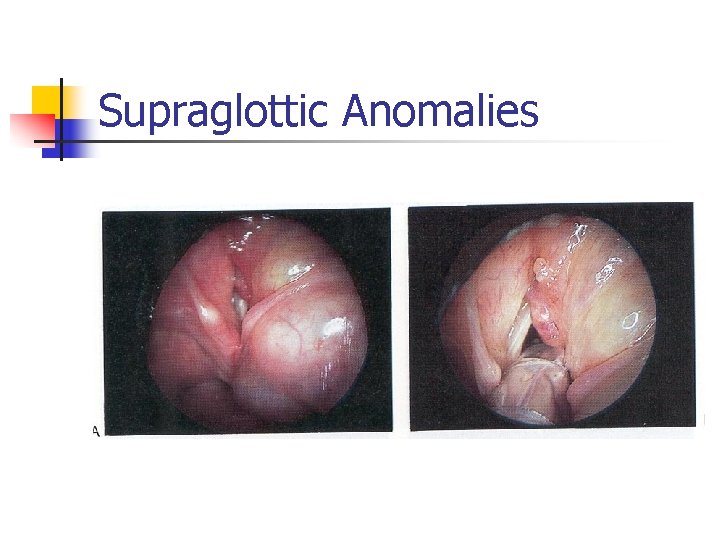
Supraglottic Anomalies
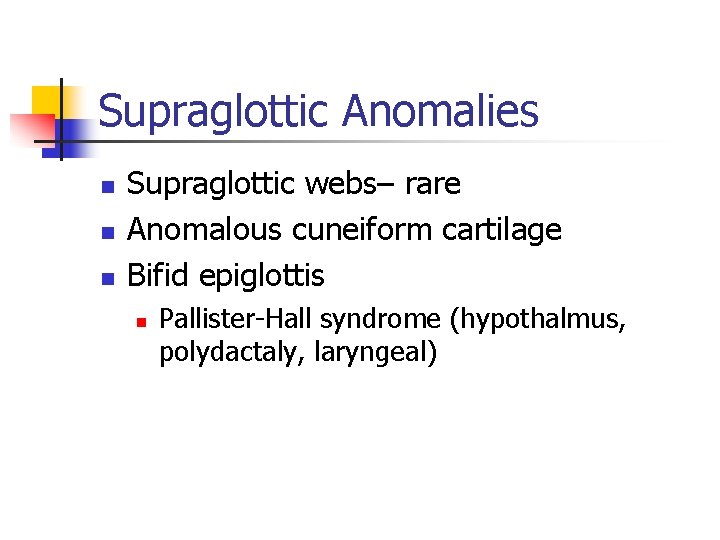
Supraglottic Anomalies n n n Supraglottic webs– rare Anomalous cuneiform cartilage Bifid epiglottis n Pallister-Hall syndrome (hypothalmus, polydactaly, laryngeal)
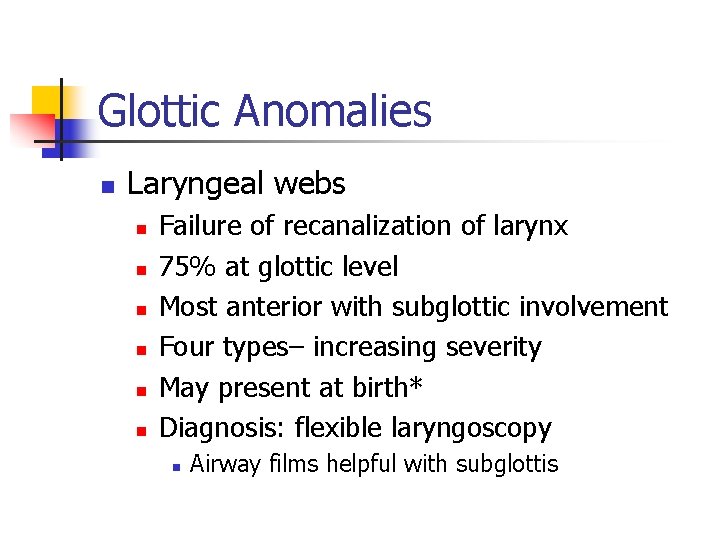
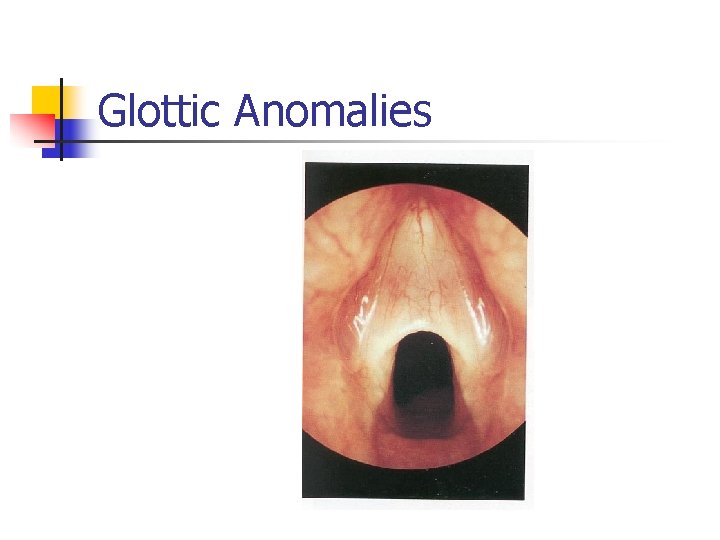
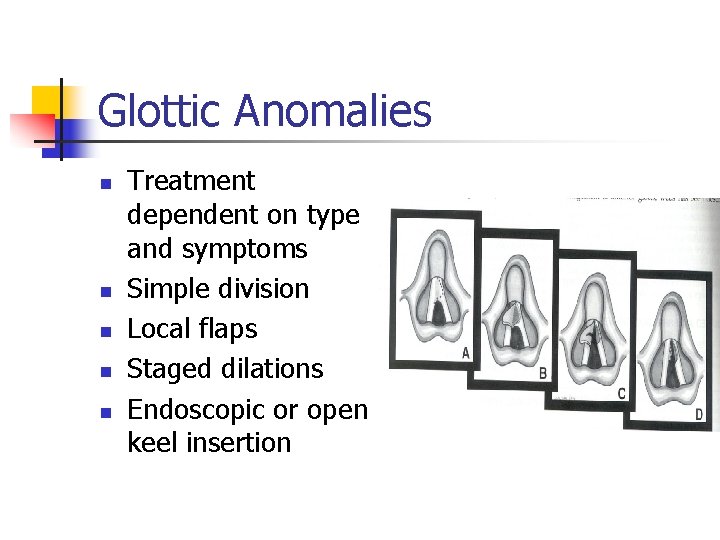
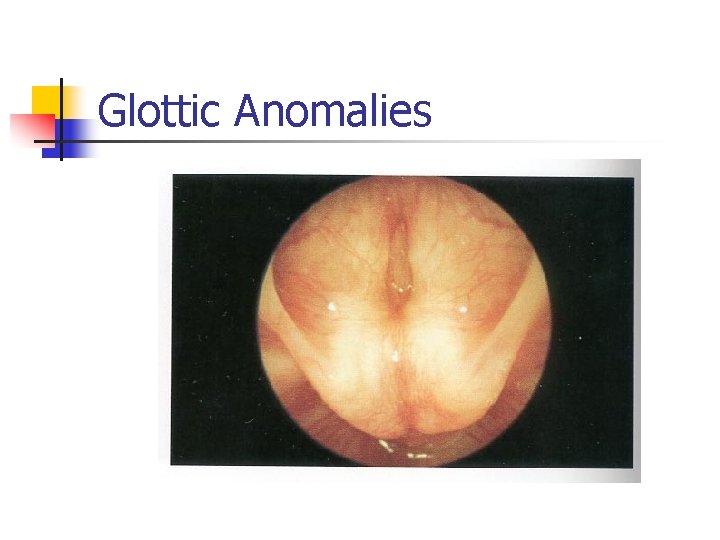
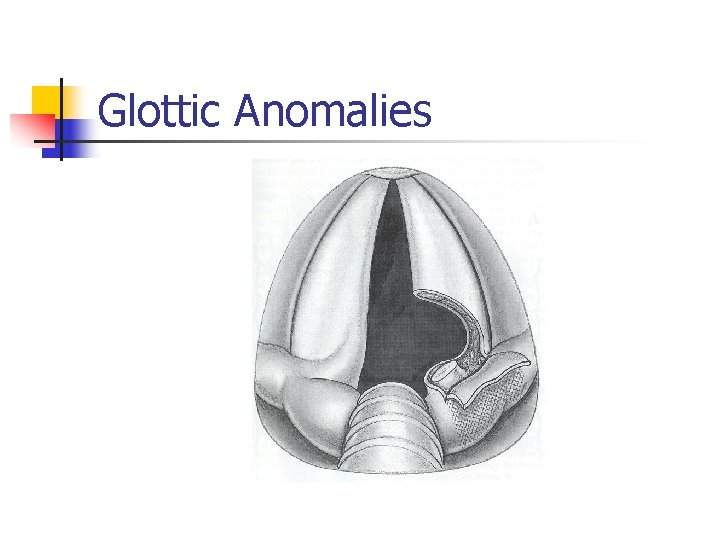
Glottic Anomalies n Laryngeal webs n n n Failure of recanalization of larynx 75% at glottic level Most anterior with subglottic involvement Four types– increasing severity May present at birth* Diagnosis: flexible laryngoscopy n Airway films helpful with subglottis
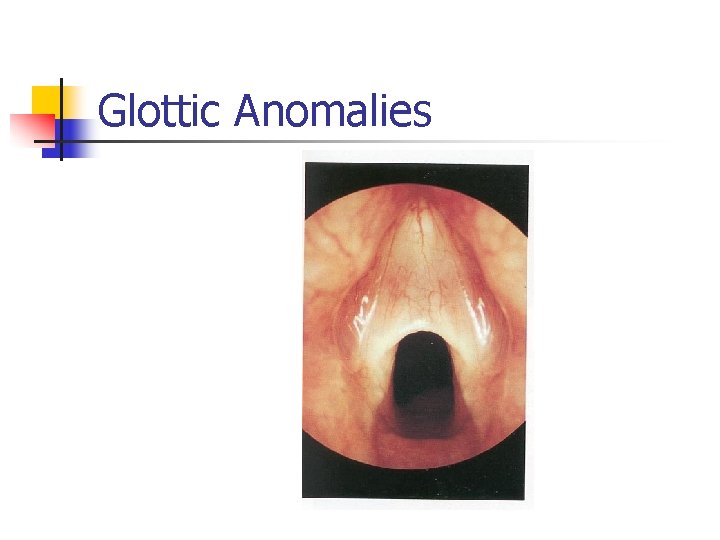
Glottic Anomalies
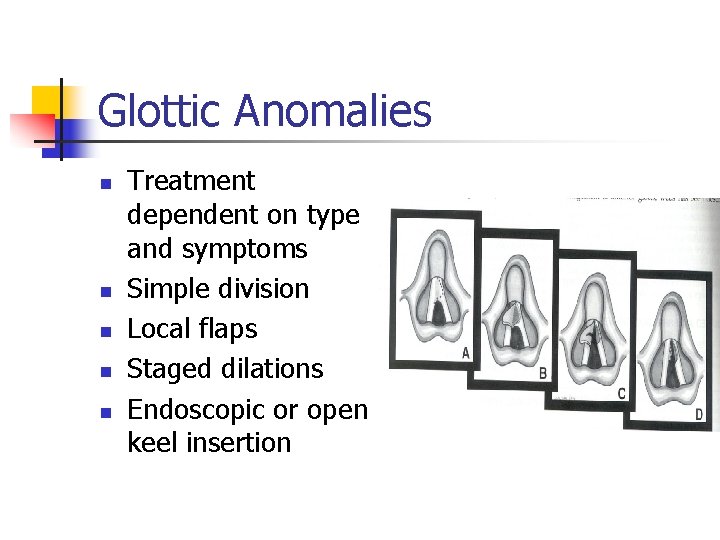
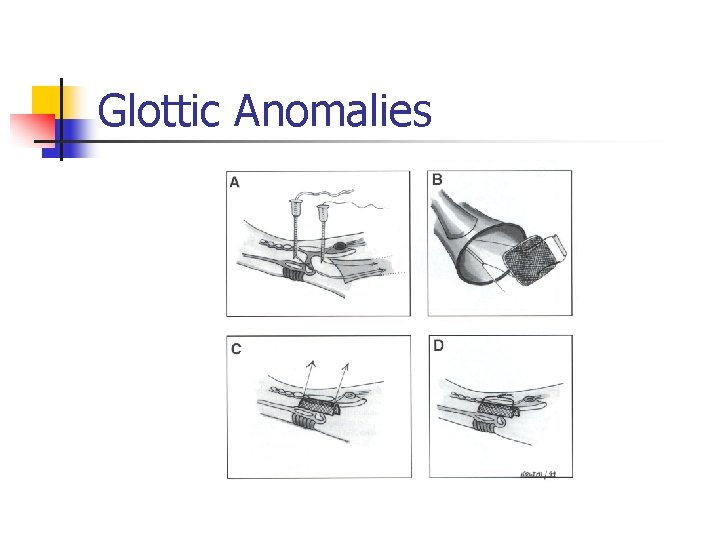
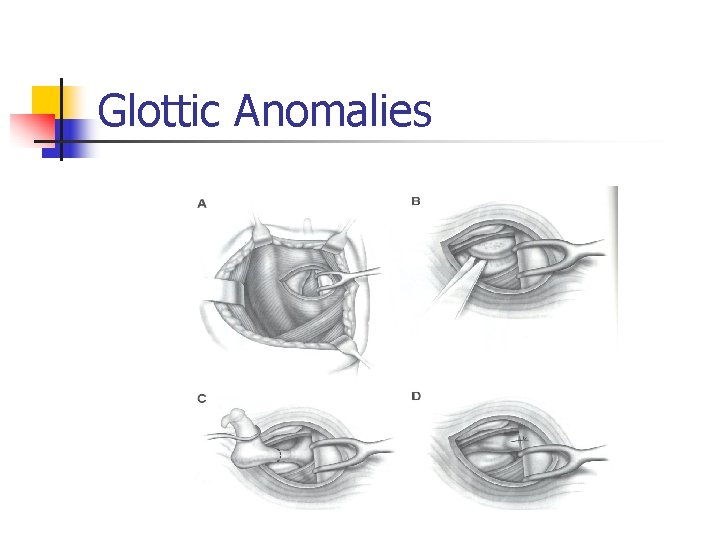
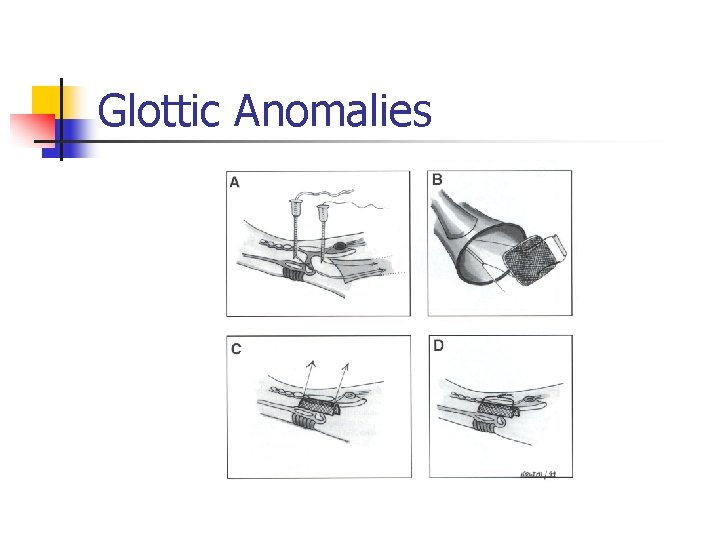
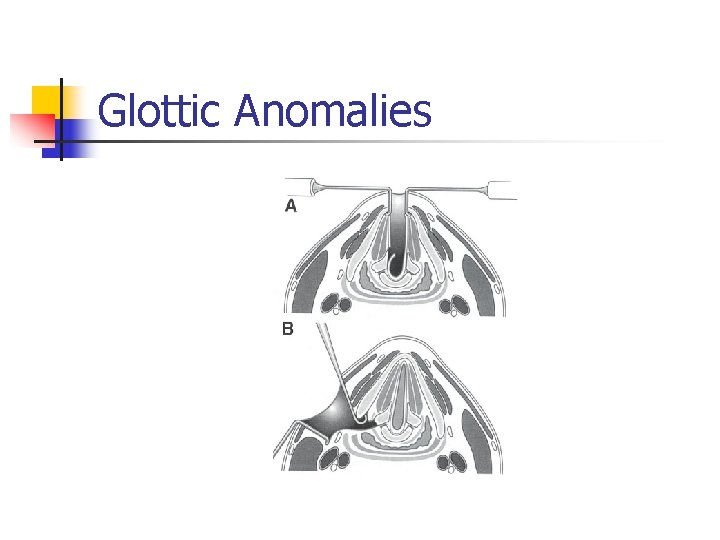
Glottic Anomalies n n n Treatment dependent on type and symptoms Simple division Local flaps Staged dilations Endoscopic or open keel insertion
Glottic Anomalies
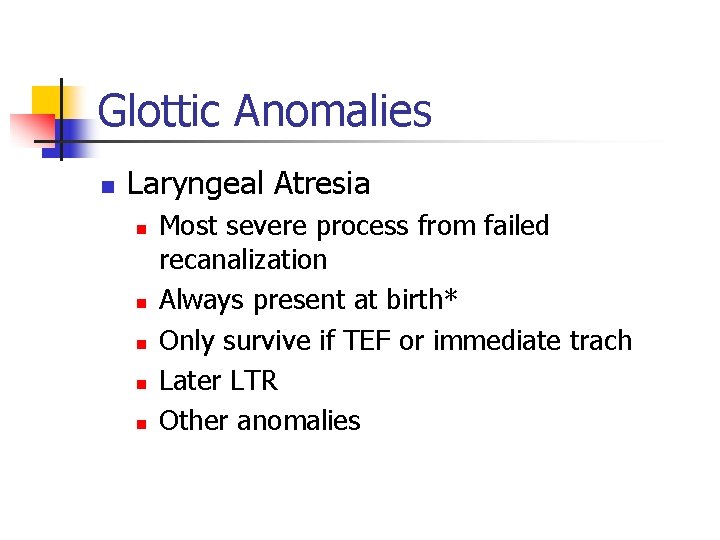
Glottic Anomalies n Laryngeal Atresia n n n Most severe process from failed recanalization Always present at birth* Only survive if TEF or immediate trach Later LTR Other anomalies
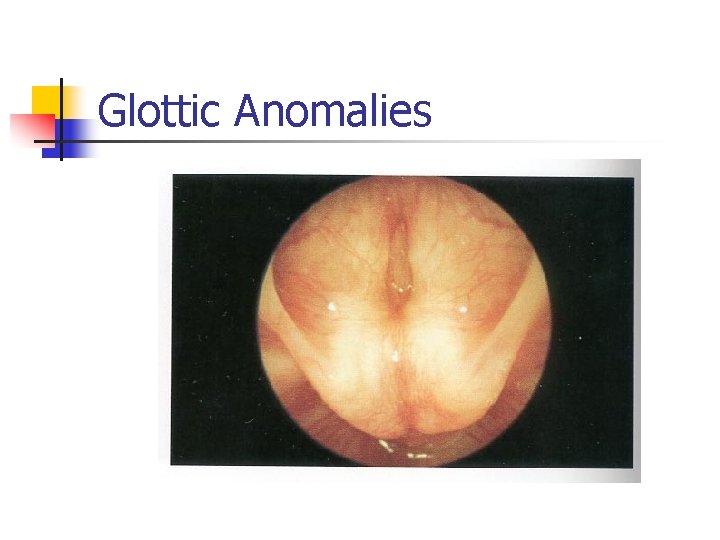
Glottic Anomalies
Glottic Anomalies n Congenital High Upper Airway Obstruction (CHAOS) n n n 1994– ultrasound with large lungs, flat diaphragms, dilated airways, fetal ascites EXIT procedure (ex utero intrapartum treatment) Multidisciplinary team n C-section, maintain placental blood flow, quick tracheotomy
Glottic Anomalies n Vocal cord paralysis n n n Second most common cause of stridor 10 -15% of laryngeal pathology Unilateral vs. bilateral Vagus nerve damage Idiopathic (47%) ACM, hydrocephalus, trauma, cardiac problems
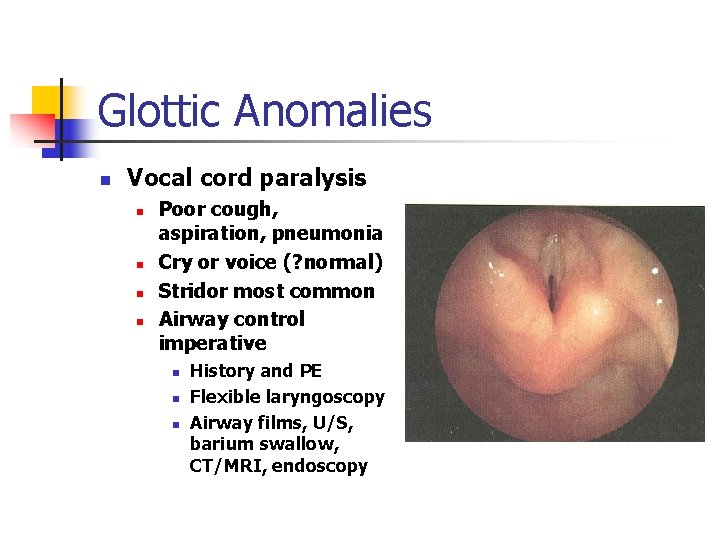
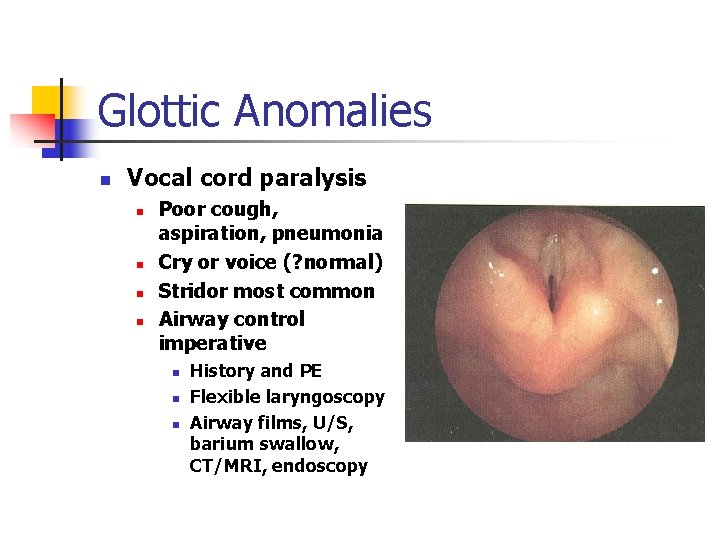
Glottic Anomalies n Vocal cord paralysis n n Poor cough, aspiration, pneumonia Cry or voice (? normal) Stridor most common Airway control imperative n n n History and PE Flexible laryngoscopy Airway films, U/S, barium swallow, CT/MRI, endoscopy
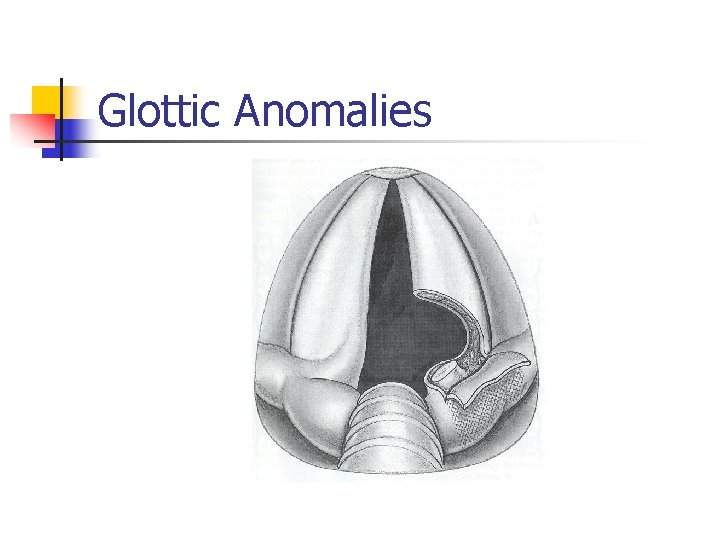
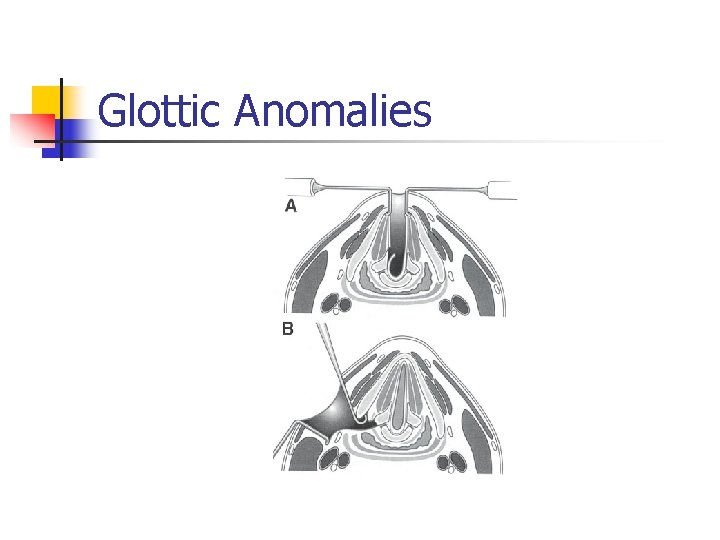
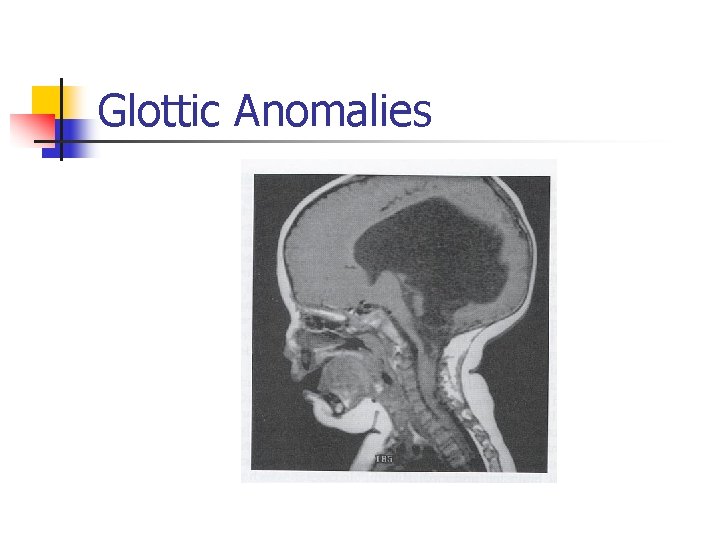
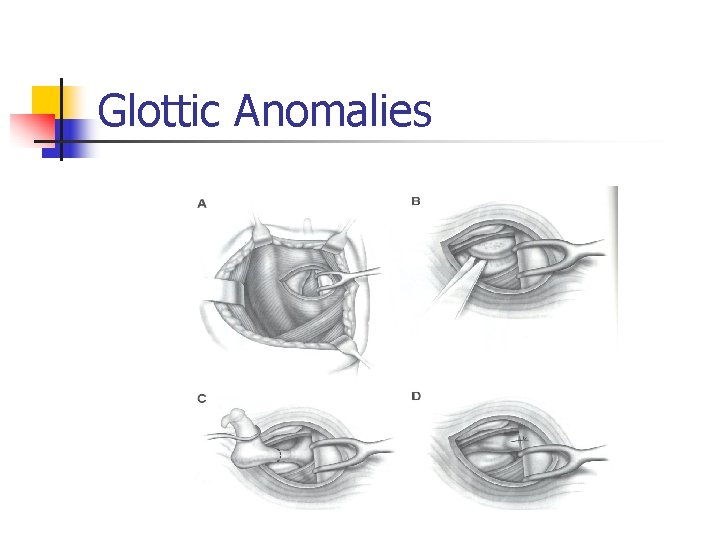
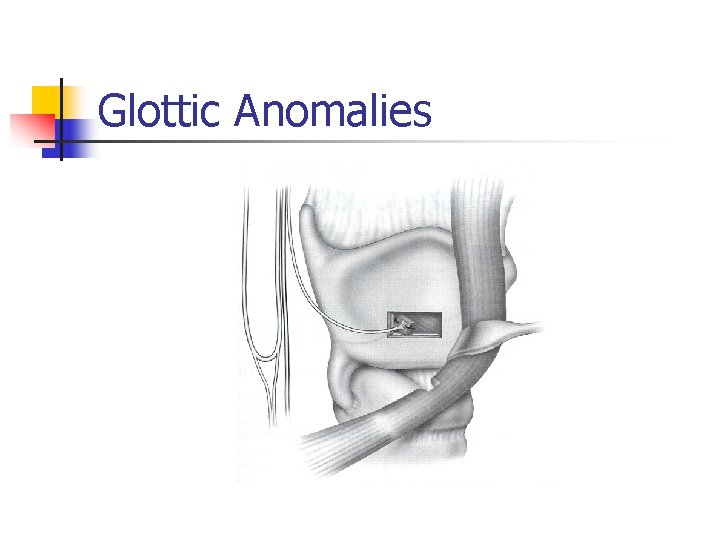
Glottic Anomalies n Bilateral vocal cord paralysis n n n Tracheotomy in 50% Present at birth* ACM– posterior fossa decompression/shunt Serial endoscopy/EMG 60% return with ACM If not, lateralization procedures (over one year)– Woodman arytenoidectomy, laser cordotomy/arytenoidectomy/cordectomy, open procedures, reanimation, electrical pacers
Glottic Anomalies
Glottic Anomalies
Glottic Anomalies
Glottic Anomalies
Glottic Anomalies
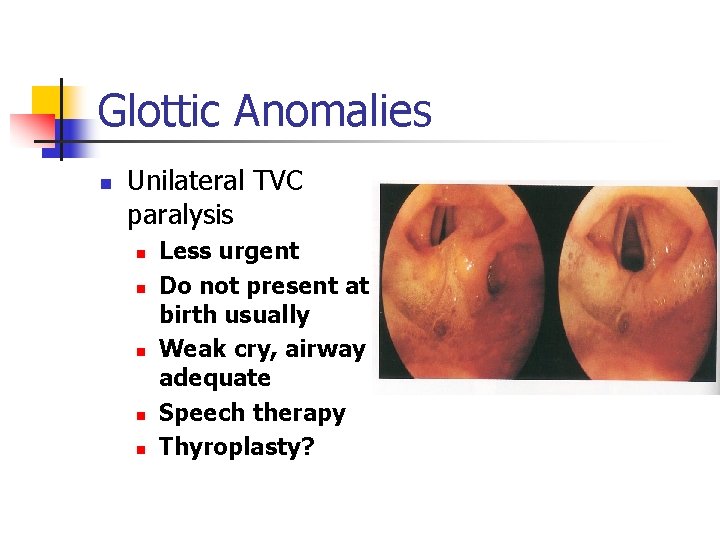
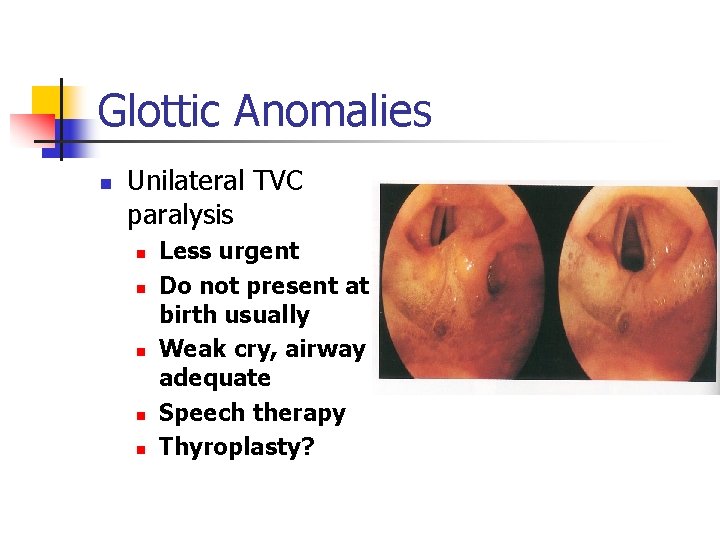
Glottic Anomalies n Unilateral TVC paralysis n n n Less urgent Do not present at birth usually Weak cry, airway adequate Speech therapy Thyroplasty?
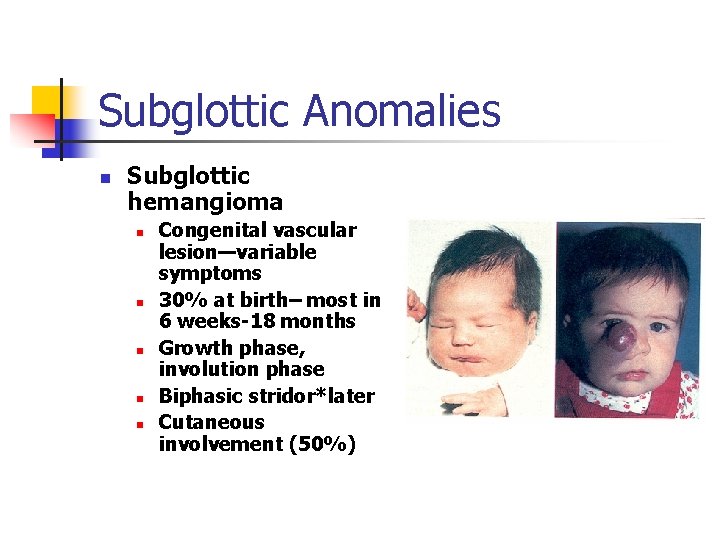
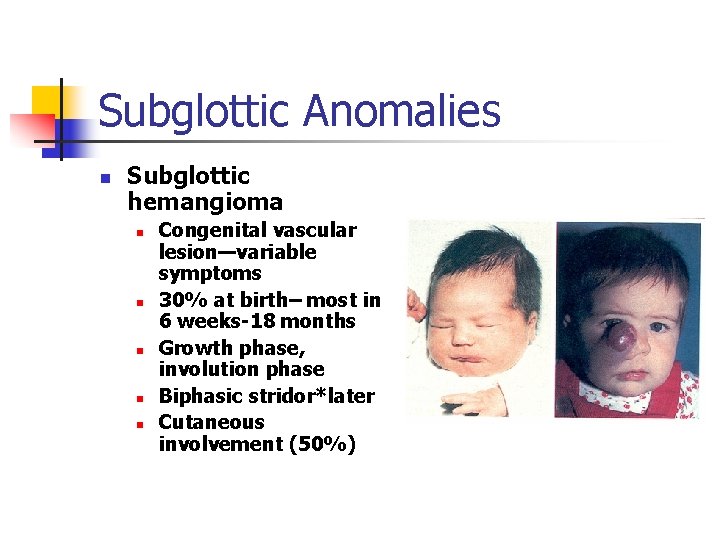
Subglottic Anomalies n Subglottic hemangioma n n n Congenital vascular lesion—variable symptoms 30% at birth– most in 6 weeks-18 months Growth phase, involution phase Biphasic stridor*later Cutaneous involvement (50%)
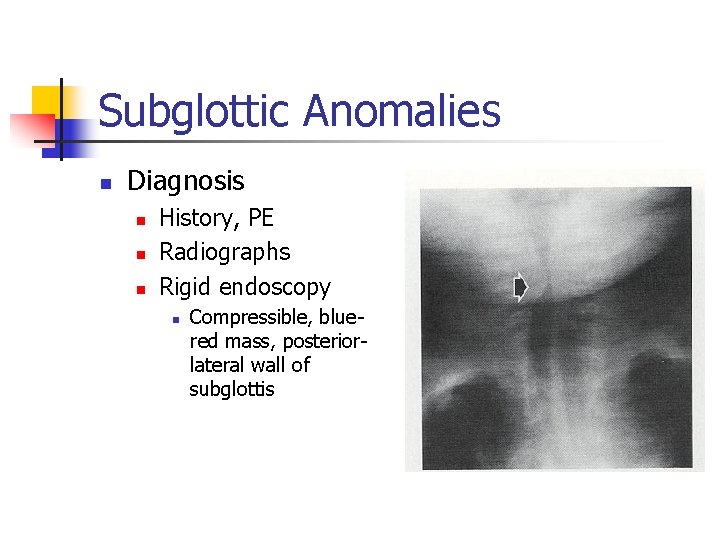
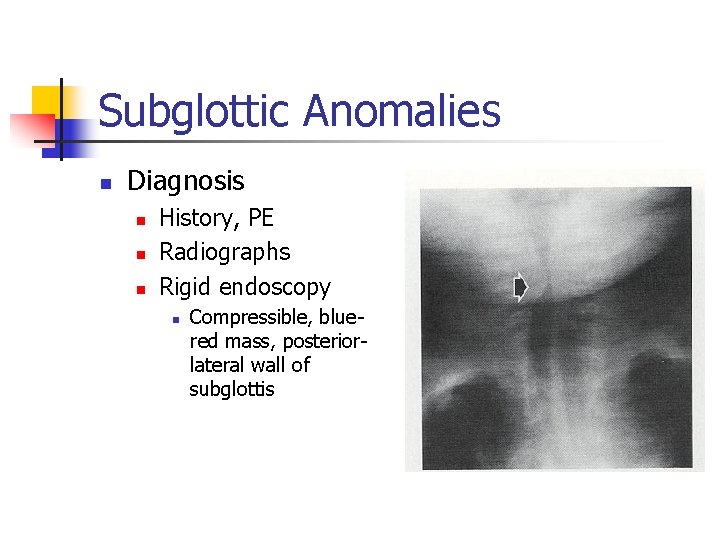
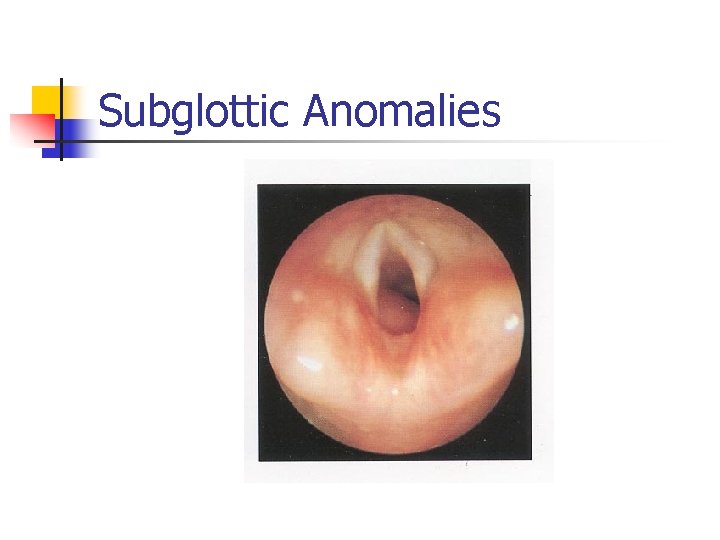
Subglottic Anomalies n Diagnosis n n n History, PE Radiographs Rigid endoscopy n Compressible, bluered mass, posteriorlateral wall of subglottis
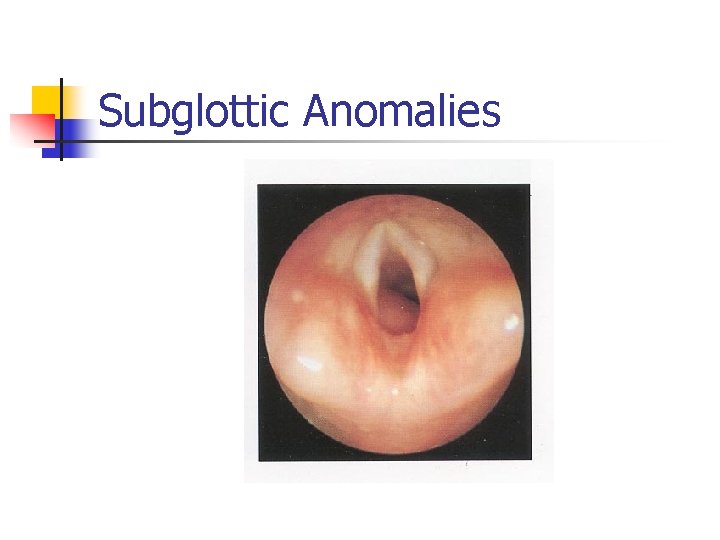
Subglottic Anomalies
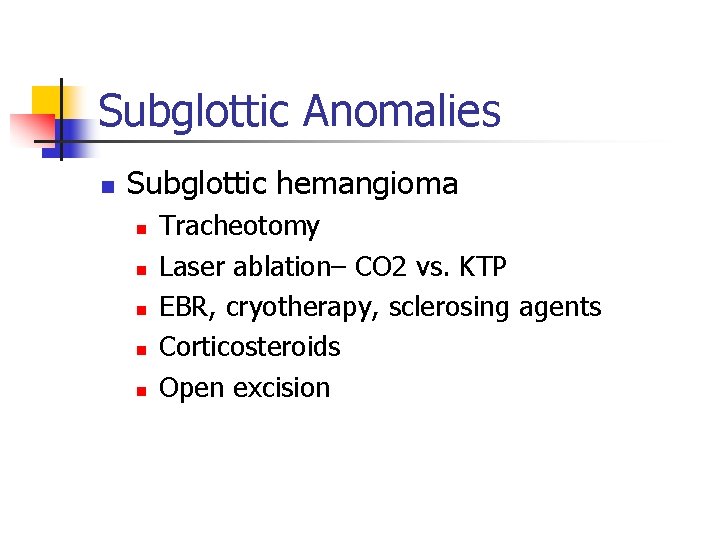
Subglottic Anomalies n Subglottic hemangioma n n n Tracheotomy Laser ablation– CO 2 vs. KTP EBR, cryotherapy, sclerosing agents Corticosteroids Open excision
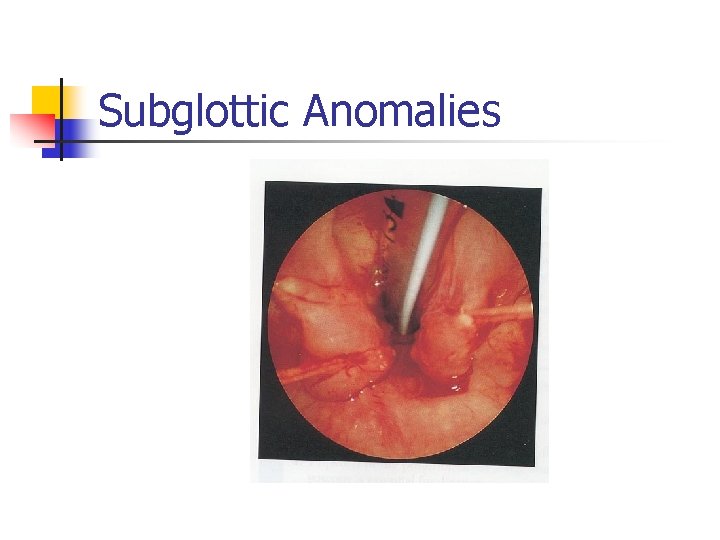
Subglottic Anomalies n Posterior laryngeal cleft n n n Failure of tracheoesophageal septum development (rostral portion) 6% with TEF have PLC Pallister-Hall syndrome May present at birth* Respiratory distress with feeds, cyanosis Aspiration, pneumonia, death
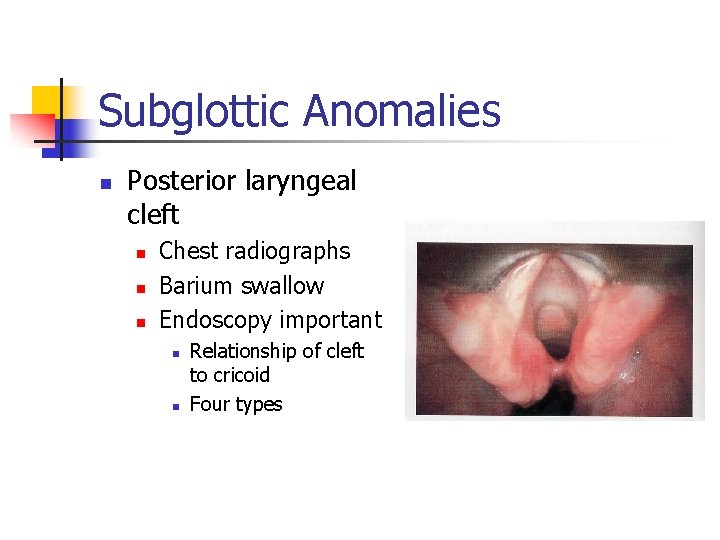
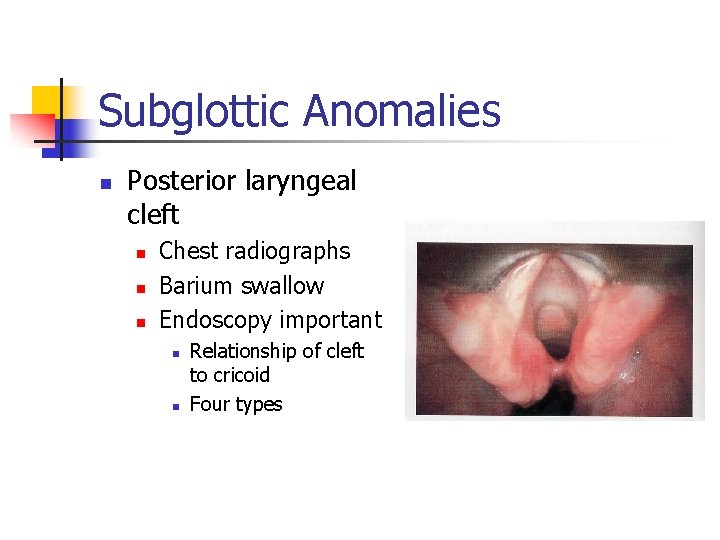
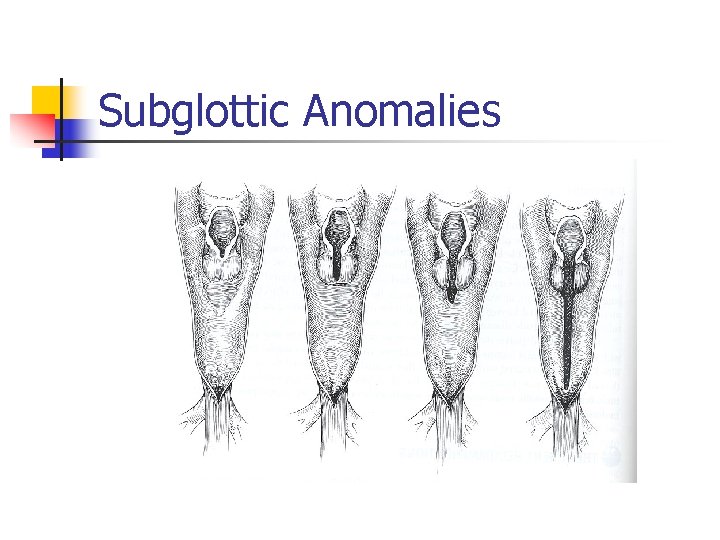
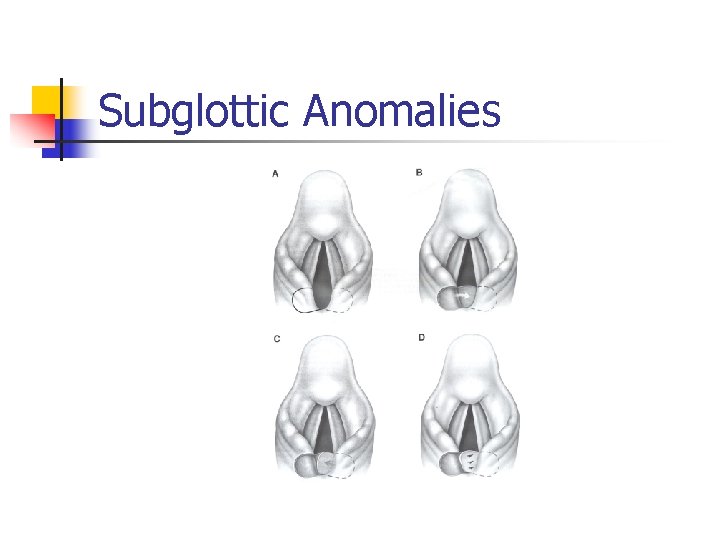
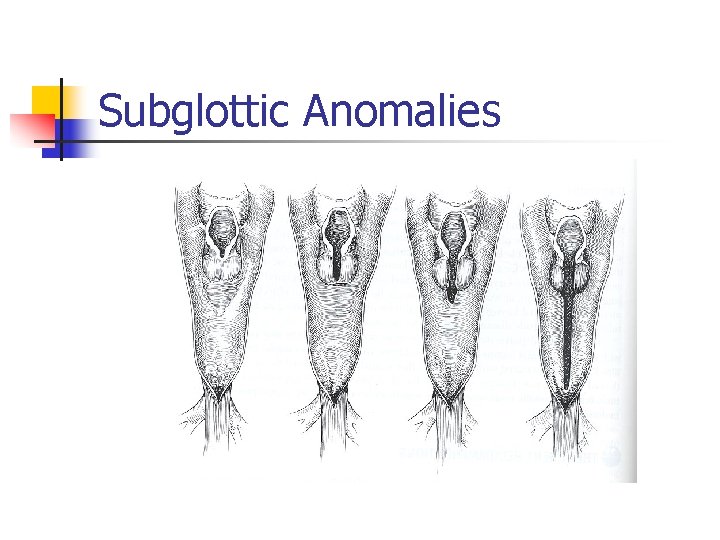
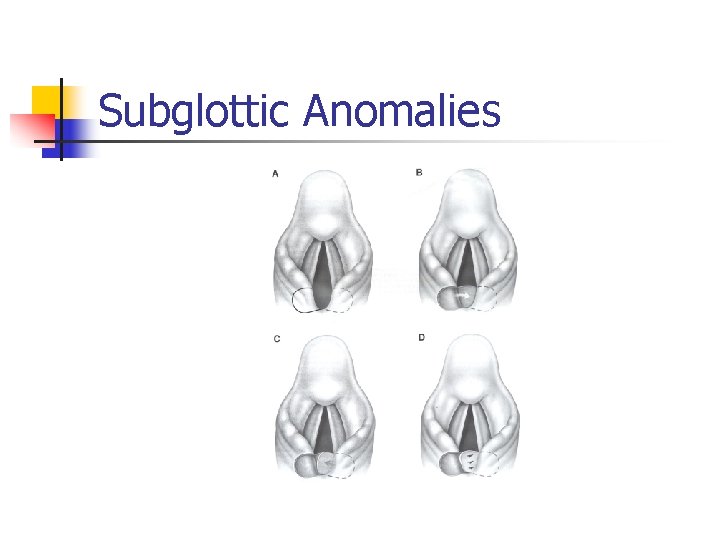
Subglottic Anomalies n Posterior laryngeal cleft n n n Chest radiographs Barium swallow Endoscopy important n n Relationship of cleft to cricoid Four types
Subglottic Anomalies
Subglottic Anomalies
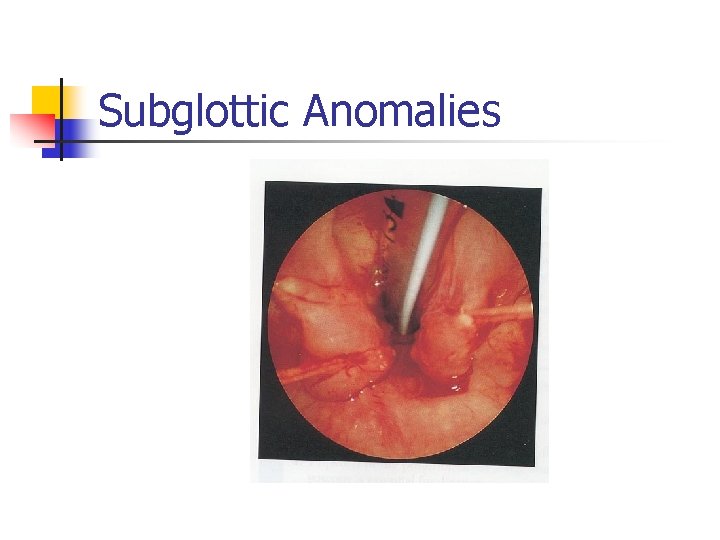
Subglottic Anomalies
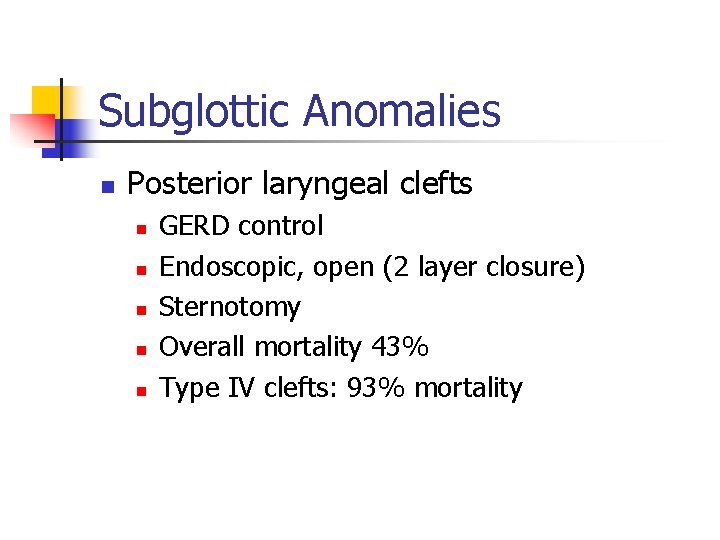
Subglottic Anomalies n Posterior laryngeal clefts n n n GERD control Endoscopic, open (2 layer closure) Sternotomy Overall mortality 43% Type IV clefts: 93% mortality
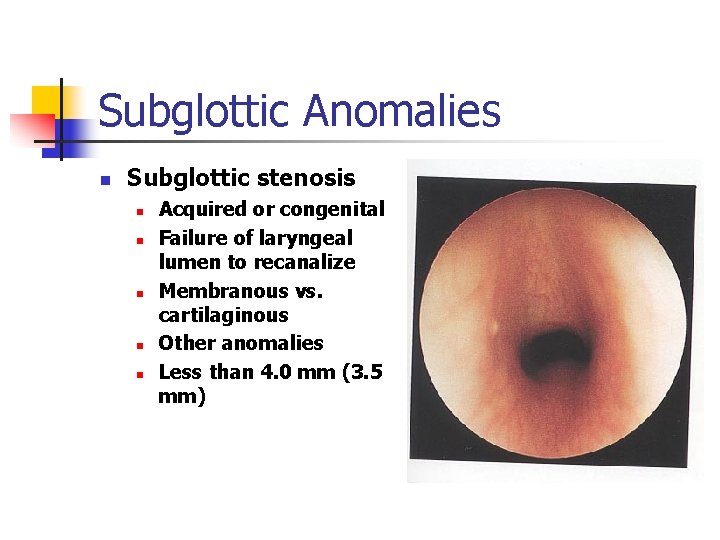
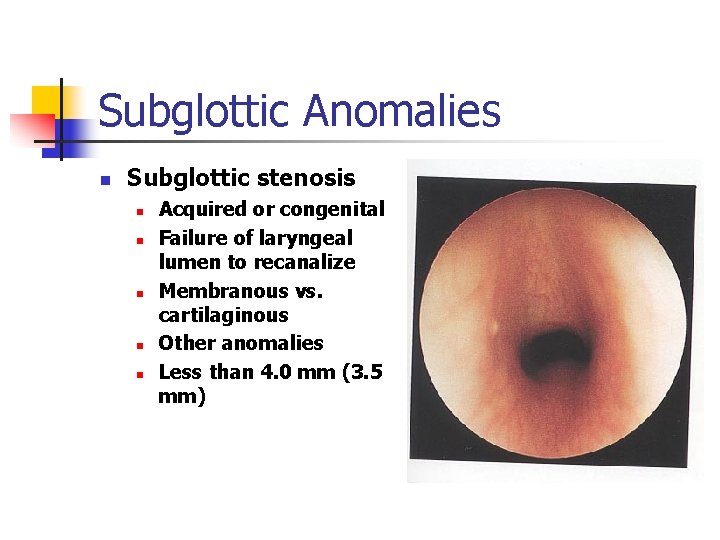
Subglottic Anomalies n Subglottic stenosis n n n Acquired or congenital Failure of laryngeal lumen to recanalize Membranous vs. cartilaginous Other anomalies Less than 4. 0 mm (3. 5 mm)
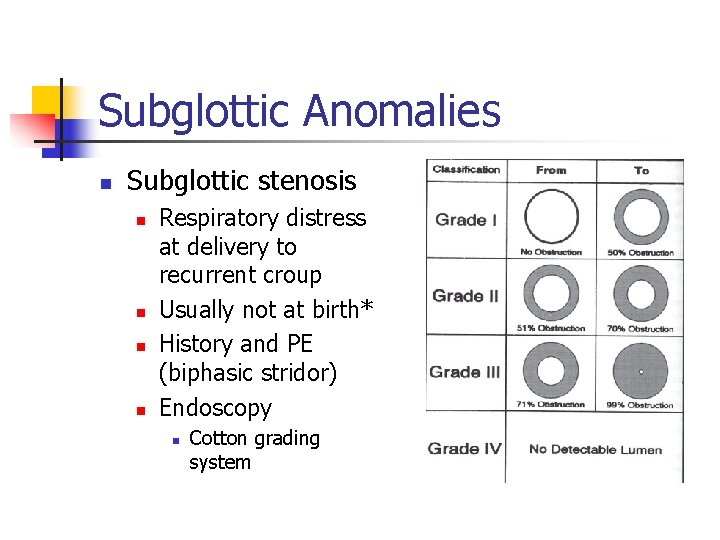
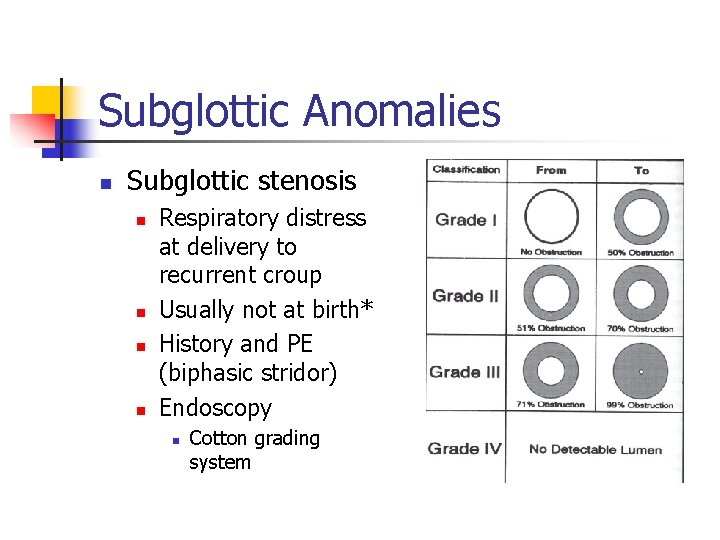
Subglottic Anomalies n Subglottic stenosis n n Respiratory distress at delivery to recurrent croup Usually not at birth* History and PE (biphasic stridor) Endoscopy n Cotton grading system
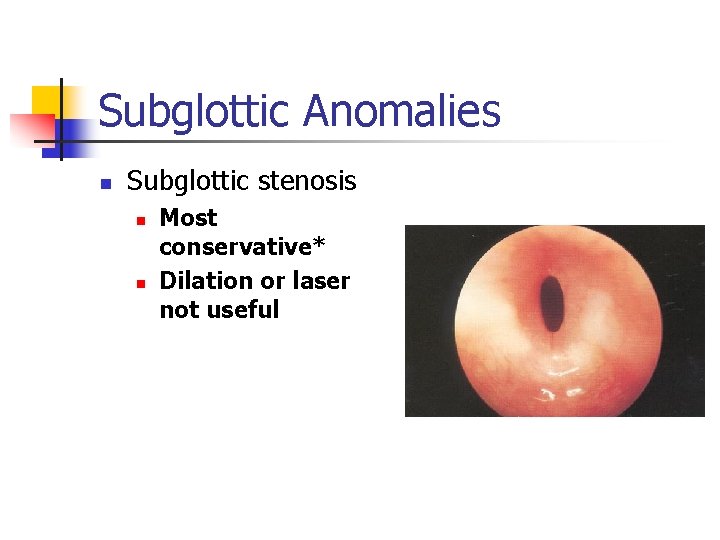
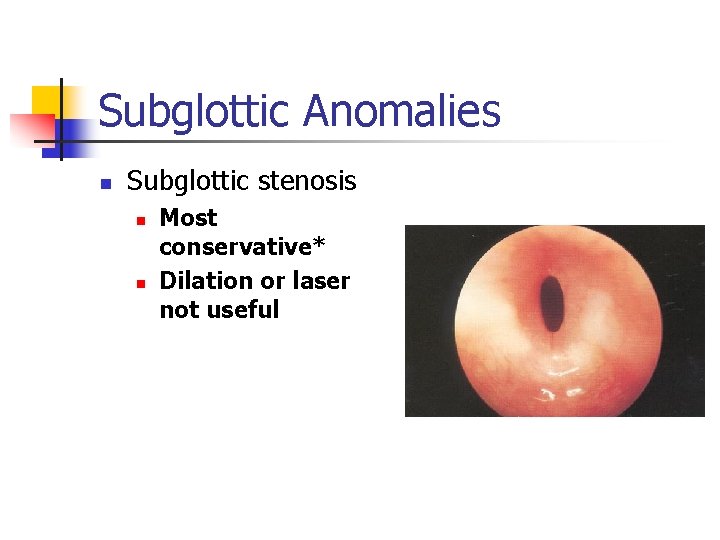
Subglottic Anomalies n Subglottic stenosis n n Most conservative* Dilation or laser not useful
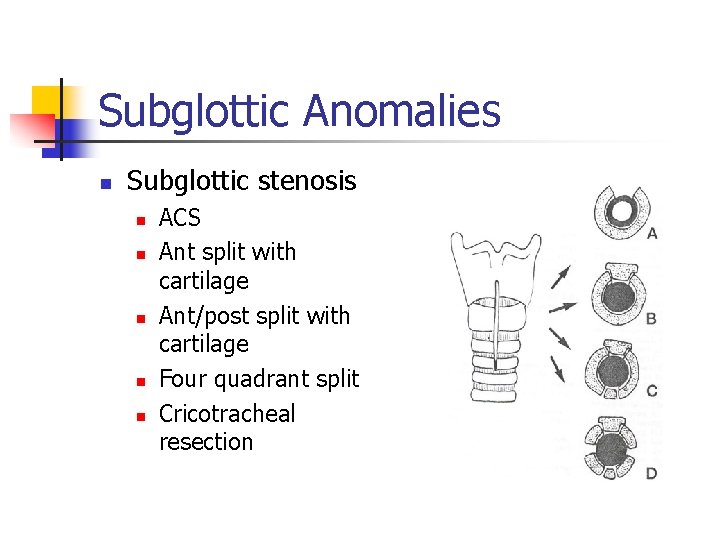
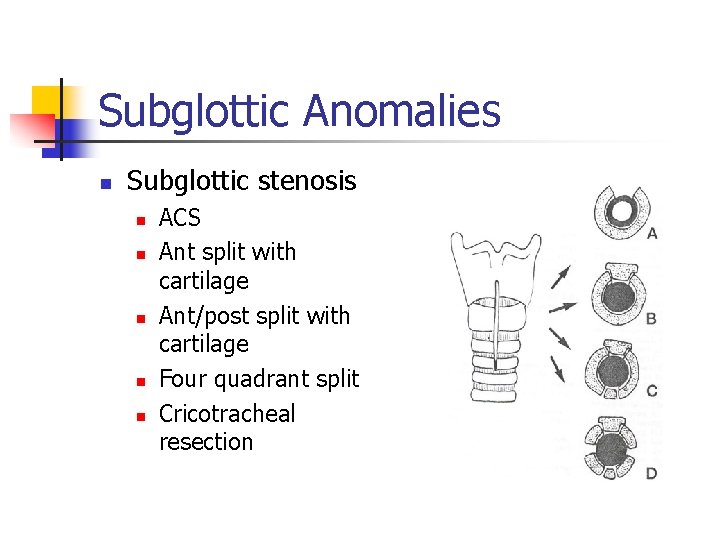
Subglottic Anomalies n Subglottic stenosis n n n ACS Ant split with cartilage Ant/post split with cartilage Four quadrant split Cricotracheal resection

 Mcgovern nipple
Mcgovern nipple Larynx
Larynx Icd 10 multiple congenital anomalies
Icd 10 multiple congenital anomalies Micrognathia definition
Micrognathia definition Causes of congenital anomalies
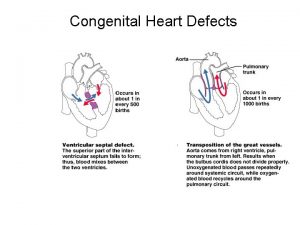
Causes of congenital anomalies Congenital anomalies
Congenital anomalies Unilateral superior laryngeal nerve injury
Unilateral superior laryngeal nerve injury Cricothyroid muscle.
Cricothyroid muscle. What is the function of the tongue
What is the function of the tongue Laryngeal surface of epiglottis
Laryngeal surface of epiglottis Laring berbentuk omega
Laring berbentuk omega Semon law
Semon law Alternatives to surgery for laryngeal paralysis in dogs
Alternatives to surgery for laryngeal paralysis in dogs Laryngeal orifice embryology
Laryngeal orifice embryology Pho nation
Pho nation Intrinsic laryngeal muscle
Intrinsic laryngeal muscle Laryngeal inlet
Laryngeal inlet Corniculate
Corniculate Laryngeal prominence
Laryngeal prominence Rima glottidis
Rima glottidis Recurrent laryngeal nerve
Recurrent laryngeal nerve 5th pharyngeal pouch
5th pharyngeal pouch Cadaveric position of vocal cord
Cadaveric position of vocal cord Muscular process of arytenoid
Muscular process of arytenoid Type 1 resp failure
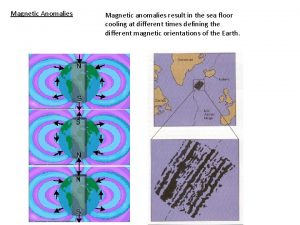
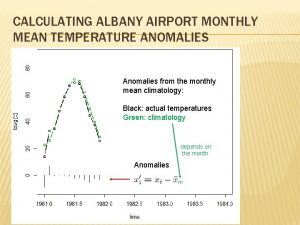
Type 1 resp failure Database anomalies
Database anomalies Vitelline fistula
Vitelline fistula Modification anomalies
Modification anomalies Attention anomalies finance
Attention anomalies finance Gynerisq
Gynerisq Accommodation anomalies
Accommodation anomalies Irregularities in population pyramids
Irregularities in population pyramids Anomalies du rcf pendant le travail
Anomalies du rcf pendant le travail Oddball: spotting anomalies in weighted graphs
Oddball: spotting anomalies in weighted graphs Ferri
Ferri Roulure bois
Roulure bois Andrea frazzini aqr
Andrea frazzini aqr Data redundancy and update anomalies
Data redundancy and update anomalies Cfsv2 monthly prec anomalies
Cfsv2 monthly prec anomalies Pbs platelet count
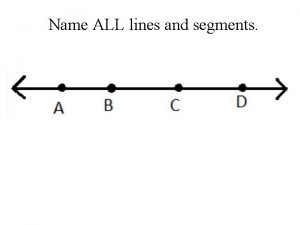
Pbs platelet count Name all the rays
Name all the rays Pathophysiology of pneumonia
Pathophysiology of pneumonia Congenital pneumonia
Congenital pneumonia Picior equin definitie
Picior equin definitie Trabeculodysgenesis meaning
Trabeculodysgenesis meaning Eisenmenger syndrome
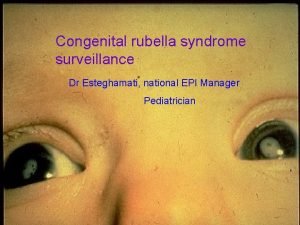
Eisenmenger syndrome Congenital rubella syndrome
Congenital rubella syndrome Congenital malformations
Congenital malformations Congenital voice disorders
Congenital voice disorders Congenital hypothyroid
Congenital hypothyroid 5 cyanotic congenital heart disease
5 cyanotic congenital heart disease Egg on a string heart
Egg on a string heart Congenital fibrosis of the extraocular muscles
Congenital fibrosis of the extraocular muscles Congenital adrenal hyperplasia electrolytes
Congenital adrenal hyperplasia electrolytes Congenital rubella syndrome triad
Congenital rubella syndrome triad Complete endocardial cushion defect
Complete endocardial cushion defect