Hypertension HTN A Nephrologists Perspective Disclaimer Some of



- Slides: 47
Hypertension (HTN) A Nephrologist’s Perspective
Disclaimer • Some of the information is from the Canadian Hypertension Education Program (CHEP) guidelines – guidelines. hypertension. ca • Excellent BP related resource for internists, family doctors, nephrologists
Agenda • • • Definition Management of emergencies Causes Investigations Treatment
Case: SB (1) • 33 y African Canadian Male • Presents to ER: – Chest Pain, Shortness of breath – BP 250/150 – Troponin: 86 – Creatinine: 211
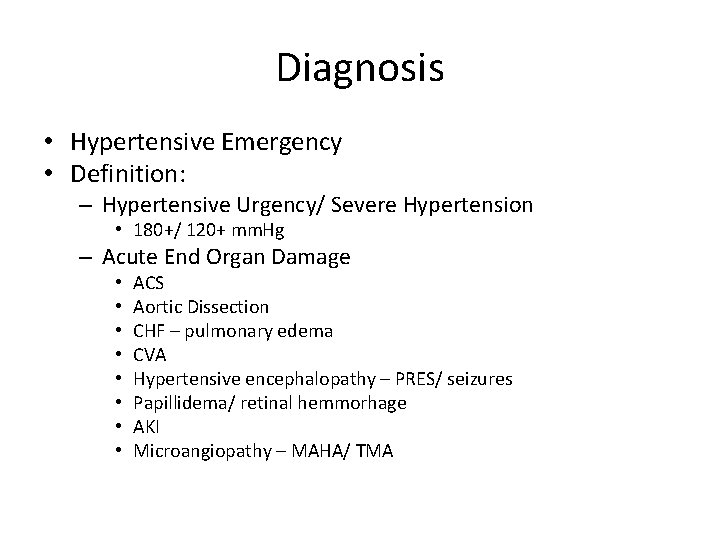
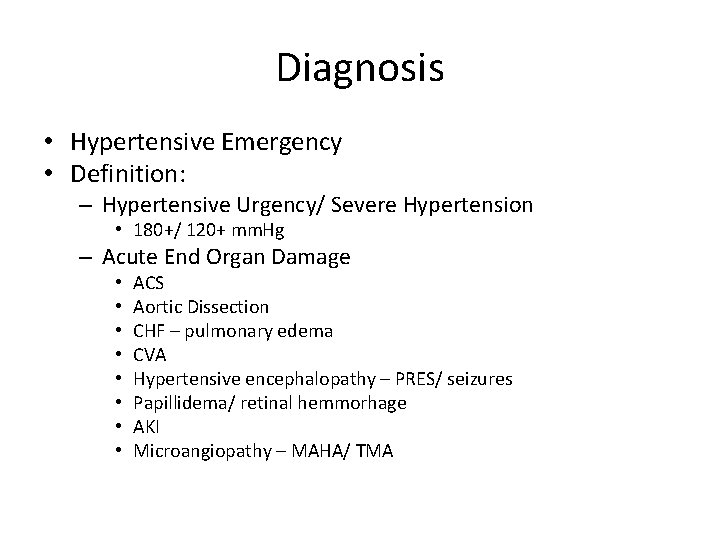
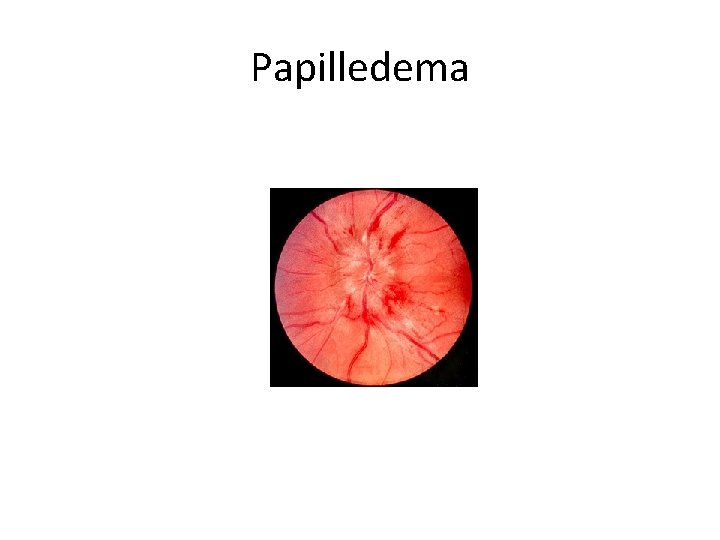
Diagnosis • Hypertensive Emergency • Definition: – Hypertensive Urgency/ Severe Hypertension • 180+/ 120+ mm. Hg – Acute End Organ Damage • • ACS Aortic Dissection CHF – pulmonary edema CVA Hypertensive encephalopathy – PRES/ seizures Papillidema/ retinal hemmorhage AKI Microangiopathy – MAHA/ TMA
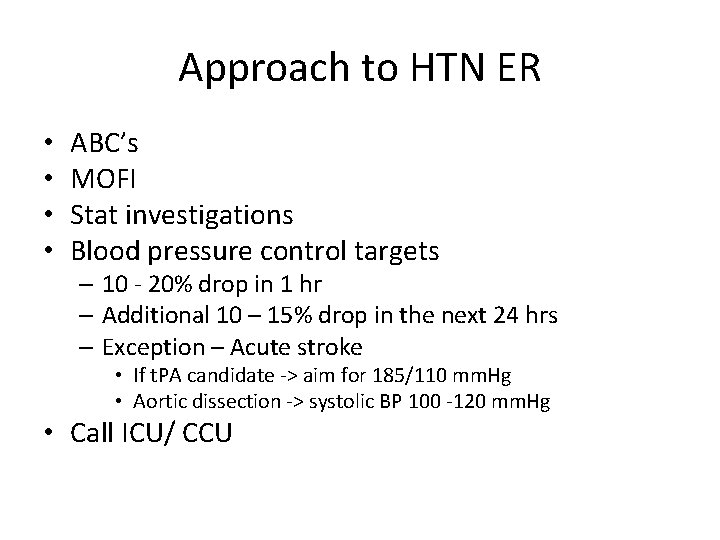
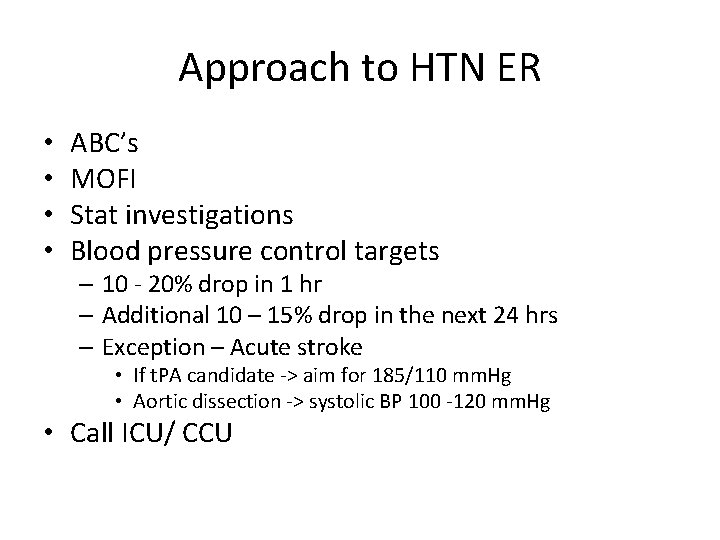
Approach to HTN ER • • ABC’s MOFI Stat investigations Blood pressure control targets – 10 - 20% drop in 1 hr – Additional 10 – 15% drop in the next 24 hrs – Exception – Acute stroke • If t. PA candidate -> aim for 185/110 mm. Hg • Aortic dissection -> systolic BP 100 -120 mm. Hg • Call ICU/ CCU
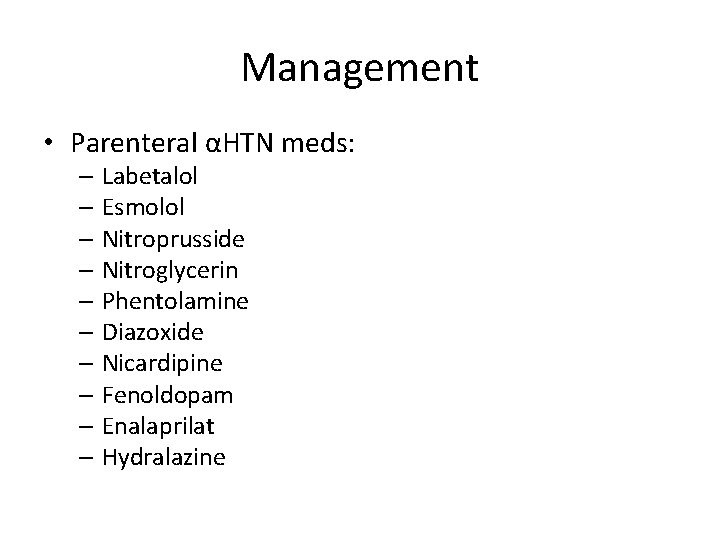
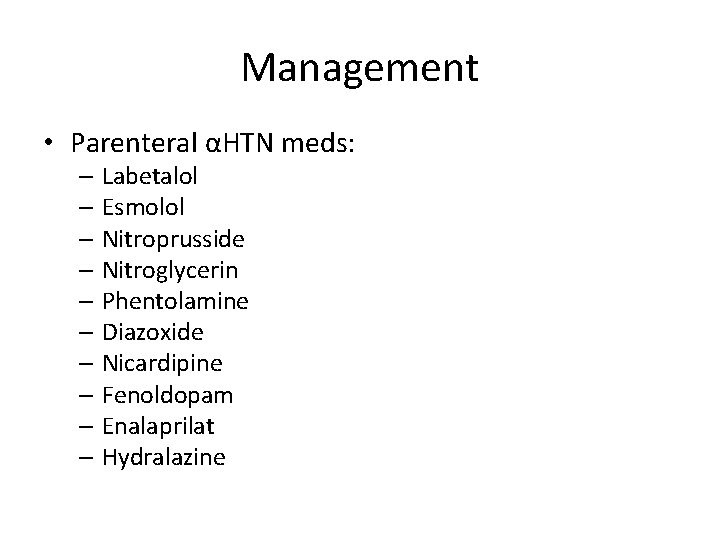
Management • Parenteral αHTN meds: – Labetalol – Esmolol – Nitroprusside – Nitroglycerin – Phentolamine – Diazoxide – Nicardipine – Fenoldopam – Enalaprilat – Hydralazine

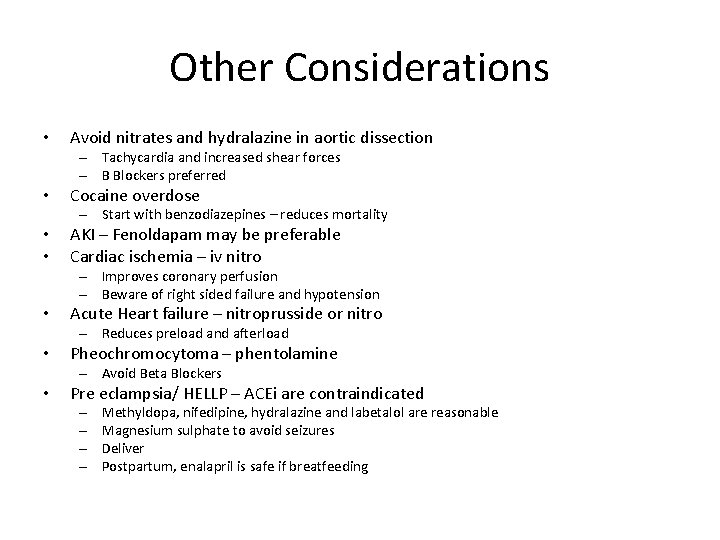
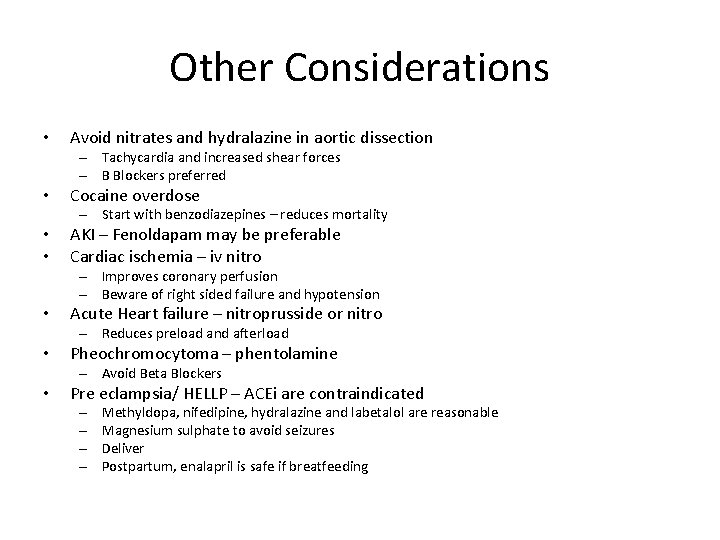
Other Considerations • Avoid nitrates and hydralazine in aortic dissection – Tachycardia and increased shear forces – B Blockers preferred • Cocaine overdose – Start with benzodiazepines – reduces mortality • • AKI – Fenoldapam may be preferable Cardiac ischemia – iv nitro – Improves coronary perfusion – Beware of right sided failure and hypotension • Acute Heart failure – nitroprusside or nitro – Reduces preload and afterload • Pheochromocytoma – phentolamine – Avoid Beta Blockers • Pre eclampsia/ HELLP – ACEi are contraindicated – – Methyldopa, nifedipine, hydralazine and labetalol are reasonable Magnesium sulphate to avoid seizures Deliver Postpartum, enalapril is safe if breatfeeding

• Oral antihypertensives can be started 8 – 12 hours later • Therapy will depend on cause and clinical picture
Case: SB (2) • Admitted to CCU • Started on iv nitro drip, lasix, and labetalol • Eventually transitioned to amlodipine, metoprolol, hydralazine and a nitropatch • RAAS blockade and diuretics were held so that testing could be done • After investigations, ramipril and chlorthalidone were started, and hydralazine and nitropatch were discontinued
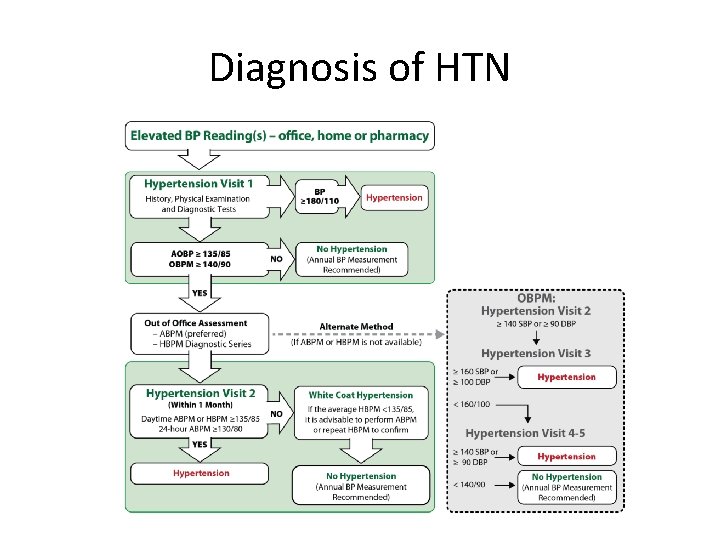
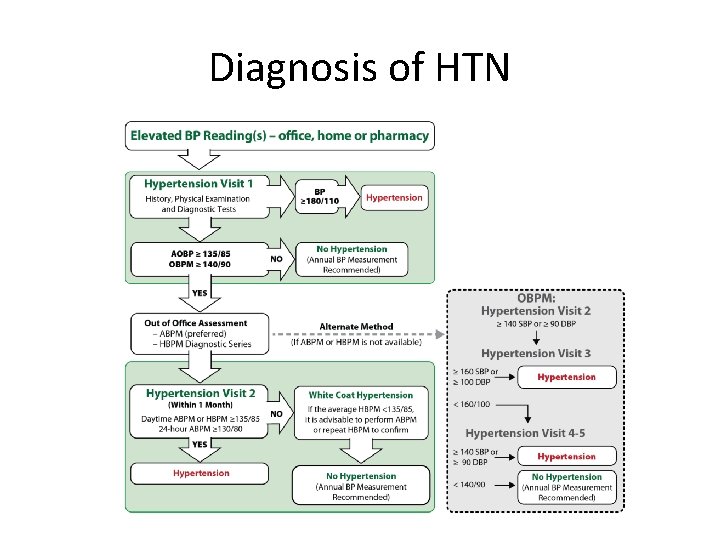
Diagnosis of HTN
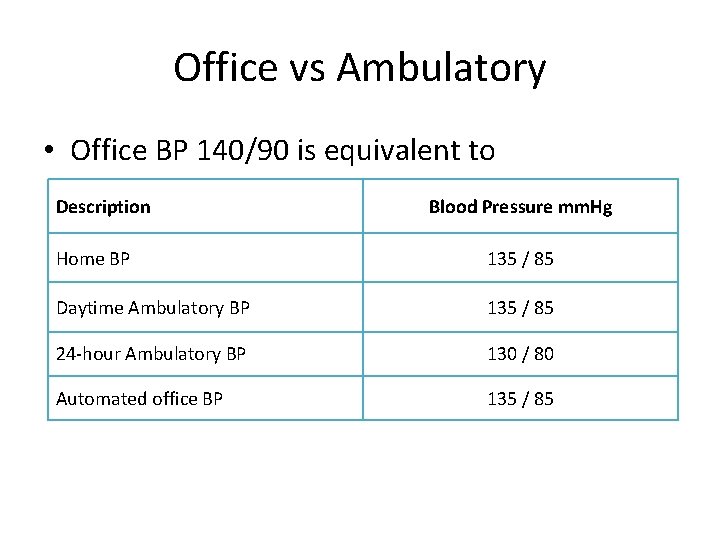
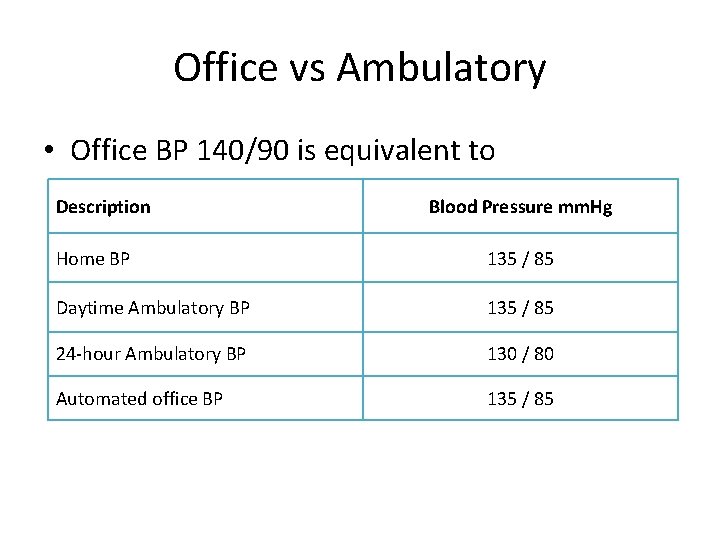
Office vs Ambulatory • Office BP 140/90 is equivalent to Description Blood Pressure mm. Hg Home BP 135 / 85 Daytime Ambulatory BP 135 / 85 24 -hour Ambulatory BP 130 / 80 Automated office BP 135 / 85
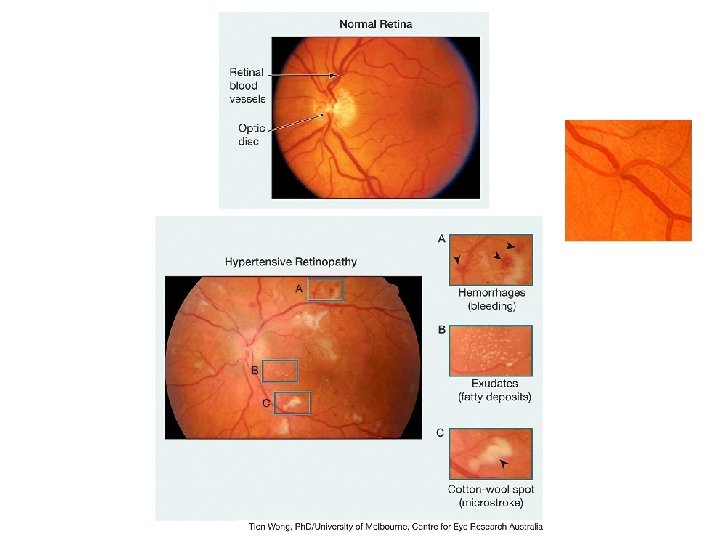
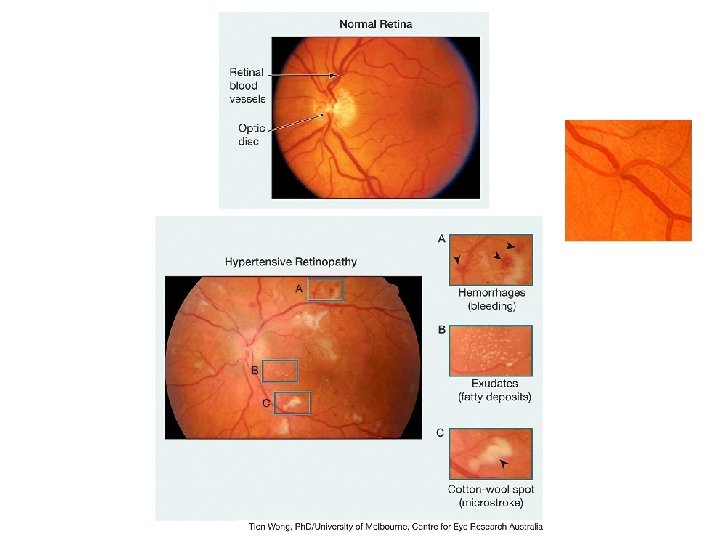
End organ damage • LVH/ CAD/ CHF (LV dysfunction) • CKD and/ or proteinuria • Vascular dementia – Clinical history/ symptoms – Microangiopathic changes on brain imaging – CVA • PVD (AAA, claudication) • Hypertensive retinopathy
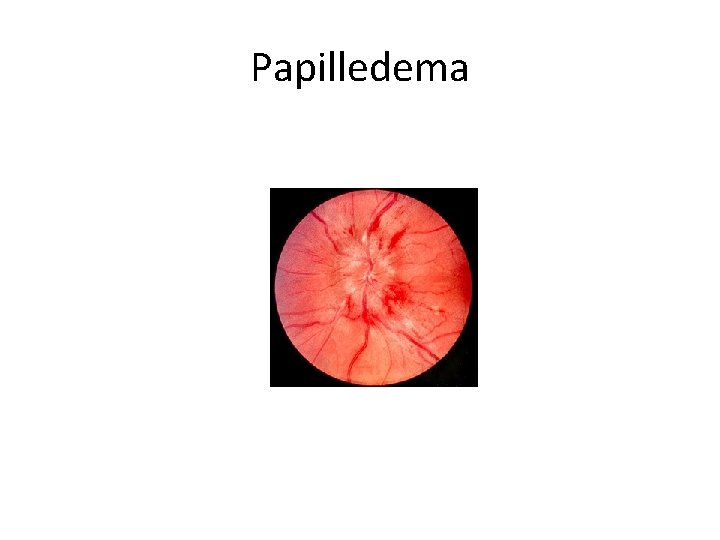
Papilledema
Secondary HTN • When should you suspect 2⁰ HTN? – – – Age: <30 or >55 Sudden or new onset (or worsening of previously well controlled HTN) Refractory HTN ER Associated symptoms/ signs of systemic conditions (or history) • • • Cushingoid appearance Abnormal pulses Connected tissue disease manifestations Intermittent palpitations, headache, pallour History of snoring Family history – Biochemical abnormalities • hypokalemia, • hypercalcemia • abnormal urine
Resistant HTN • BP not controlled on optimal doses of 3 αHTN of different classes, one of which is a diuretic
Refractory HTN • BP still not controlled on optimal doses of 4 or more αHTN of different classes, one of which is a diuretic
Causes • • Renal Endocrine Drugs Metabolic Structural Neurologic Pregnancy
Causes • Renal – – – – • • • Primary hyperaldosteronism* Renovascular Disease (atherosclerotic or fibromuscular dysplasia)* CKD and Hypervolemia* Primary GN’s – Ig. A Nephropathy PCKD Scleroderma renal crisis Erythropoeitin secreting tumour (RCC) Endocrine Drugs Metabolic Structural Neurologic Pregnancy
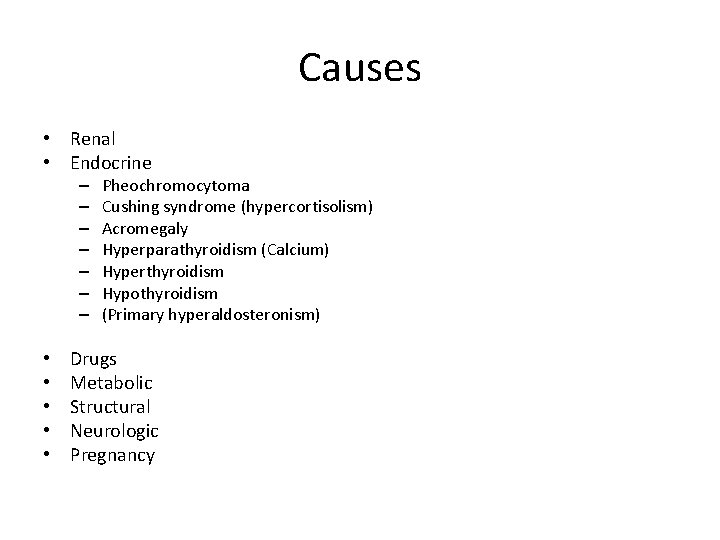
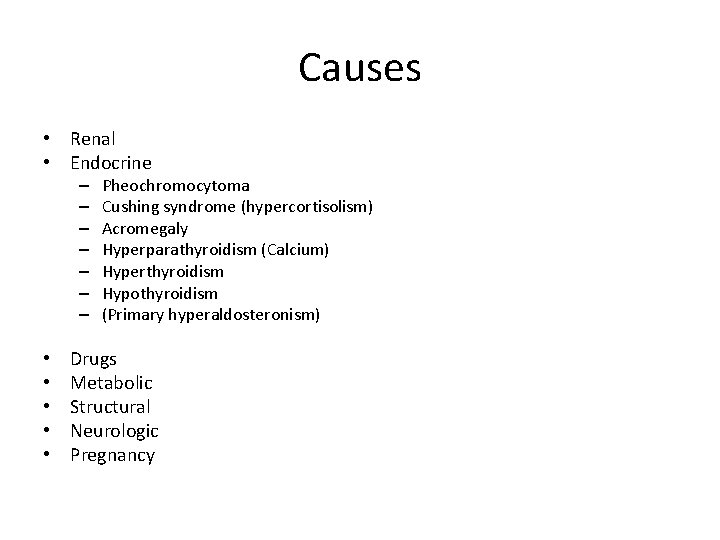
Causes • Renal • Endocrine – – – – • • • Pheochromocytoma Cushing syndrome (hypercortisolism) Acromegaly Hyperparathyroidism (Calcium) Hyperthyroidism Hypothyroidism (Primary hyperaldosteronism) Drugs Metabolic Structural Neurologic Pregnancy
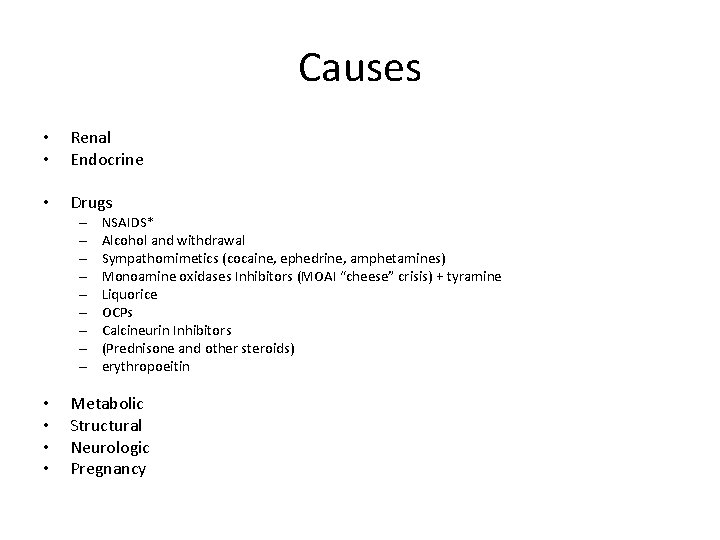
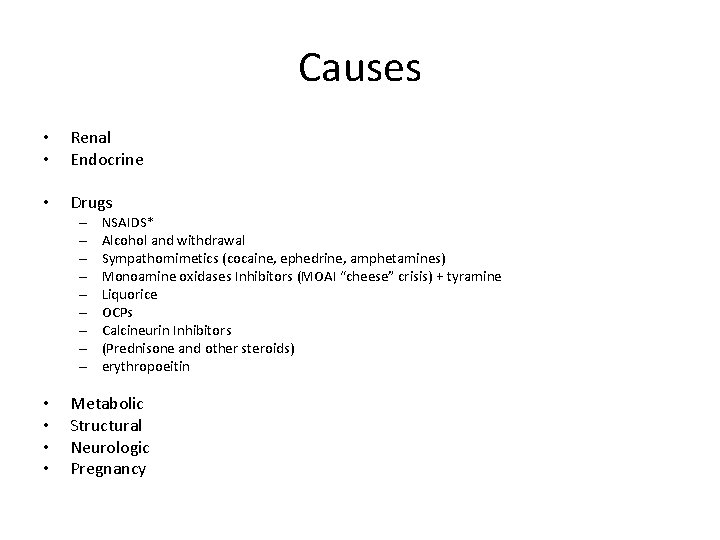
Causes • • Renal Endocrine • Drugs – – – – – • • NSAIDS* Alcohol and withdrawal Sympathomimetics (cocaine, ephedrine, amphetamines) Monoamine oxidases Inhibitors (MOAI “cheese” crisis) + tyramine Liquorice OCPs Calcineurin Inhibitors (Prednisone and other steroids) erythropoeitin Metabolic Structural Neurologic Pregnancy
Causes • Renal • Endocrine • Drugs • Metabolic – Calcium • Structural • Neurologic • Pregnancy
Causes • • Renal Endocrine Drugs Metabolic • Structural – Coarctation of Aorta – OSA* • Neurologic • Pregnancy
Causes • • • Renal Endocrine Drugs Metabolic Structural • Neurologic – Autonomic Instability – Guillame Barre Syndrome – Serotonin syndrome – Increased ICP – Cushings triad • Pregnancy
Causes • • • Renal Endocrine Drugs Metabolic Structural Neurologic • Pregnancy – Pre-eclampsia
Renovascular HTN • When to suspect RAS – Clinical Suspicion of 2⁰ HTN (Age, refractory HTN) • More specifically – Significant AKI with ACEi – Flash pulmonary edema – Abdominal Bruit (systolic and/ or diastolic) – Asymmetric kidney sizes
Investigations • captopril-enhanced radioisotope renal scan • doppler sonography • magnetic resonance angiography • CT-angiography (for those with normal renal function)
Management • Medical vs interventional (Renal artery angioplasty with stenting) – Multiple RCT’s (Astral, Coral, STAR) – all show no benefit – May be of benefit in select population that is not well controlled on medications, and has worsening creatinine, flash pulmonary edema – ACEi may be tried, but with caution • Contraindicated if bilateral RAS
Hyperaldosteronism • State of excess hyperaldosteronism or mimicking hyperaldo state • Most commonly Primary hyperaldosteronism – excess aldosterone that is under adequate feedback control – Adrenal hyperplasia – Adrenal adenoma – Conn Syndrome – Adrenal carcinoma (very rare) • When to suspect – Hypokalemia or profound hypokalemia if on diuretic (K+ < 3) • Investigations – Renin: Aldosterone levels • Aldosterone antagonists, ARBs, beta-blockers and clonidine should be discontinued prior to testing – Oral salt loading test – 3 – 5 days of Na > 200 meq/ day (5 g/ day) – Imaging – CT/ MRI – Adrenal vein sampling

Hypertension and hypokalemia Condition Renin Aldosterone Primary hyperaldosteronism (Conn Syndrome) LOW HIGH Renovascular disease HIGH Malignant HTN HIGH Reninoma HIGH Apparent Mineralocorticoid Excess (AME) LOW Liddle’s syndrome LOW Cushing’s disease LOW Glucocorticoid Remediable hyperaldosteronism LOW HIGH
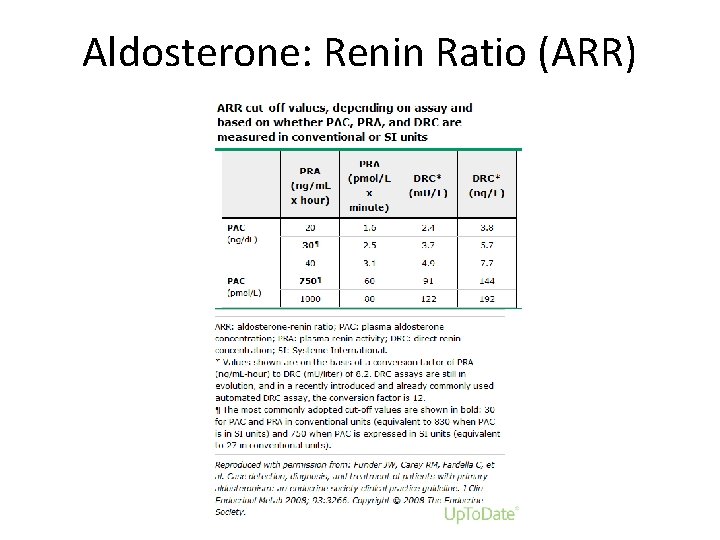
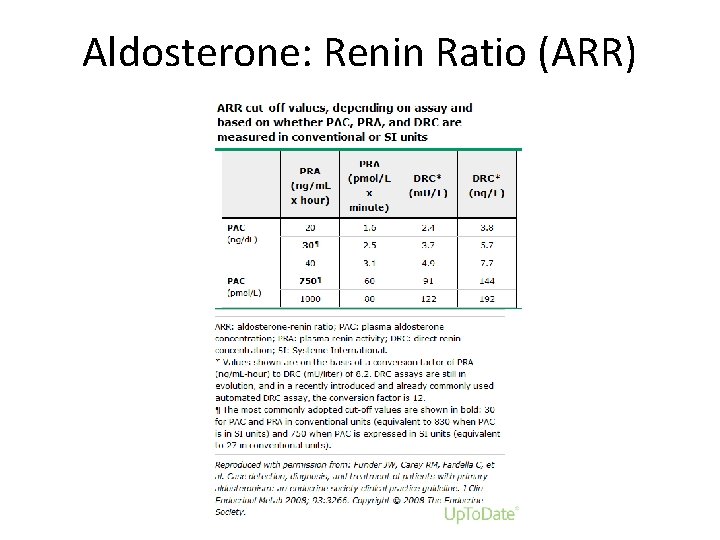
Aldosterone: Renin Ratio (ARR)
Management • If Adenoma found – biopsy may be necessary to assess malignant potential – depending on size • Surgery – if poorly controlled BP, young, malignant • Need to test for pheochromocytoma – especially if going for OR
Treatment • • ACEi ARBs aldosterone antagonists Potassium sparing diuretics – Amiloride – Triamterene • Other antihypertensives –avoid diuretics if hypo. K • Potassium
Pheochromocytoma • Catecholamine secreting tumour – adrenal medulla – chromaffin cells • Very rare, but can be dangerous • Associated with MEN 2, Von Hippel Landau and Neurofibromatosis (NF) 1 • When to suspect: – Intermittent hypertension associated with headache, diaphoresis, palpitations/ tachycardia
Other Manifestations • May present with heart failure – similar to tako-subo cardiomyopathy, and flash pulmonary edema • May also cause orthostatic hypotension • Hyperglycemia • Lactic acidosis • Weight loss
Investigations • 24 hr urine for metanephrines or catecholamines Or • • Plasma fractionated metanephrines (supine) Clonidine Suppression test - confirmatory Urinary VMA is not a good screening test Interfering drugs: – – – TCA’s Beta Blockers Calcium channel Blockers (CCBs) Buspirone pseudophederine
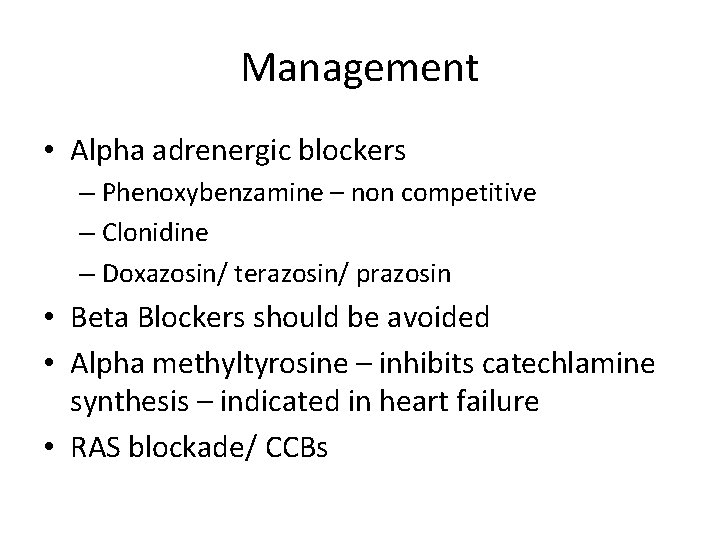
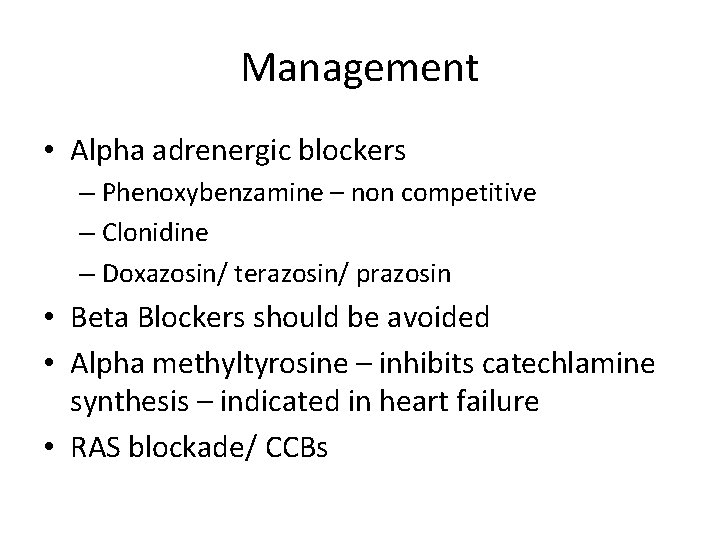
Management • Αlpha adrenergic blockers – Phenoxybenzamine – non competitive – Clonidine – Doxazosin/ terazosin/ prazosin • Beta Blockers should be avoided • Alpha methyltyrosine – inhibits catechlamine synthesis – indicated in heart failure • RAS blockade/ CCBs
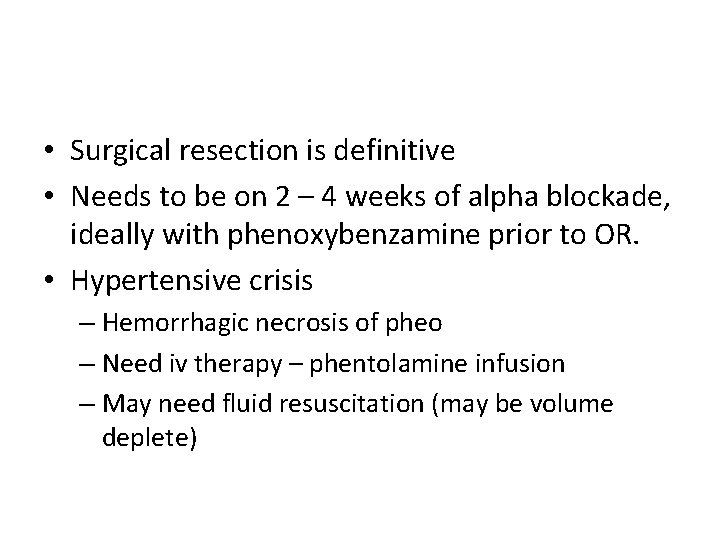
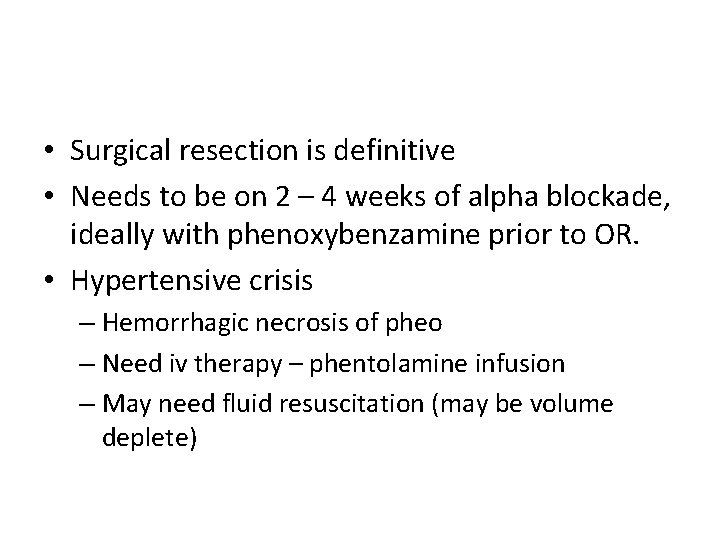
• Surgical resection is definitive • Needs to be on 2 – 4 weeks of alpha blockade, ideally with phenoxybenzamine prior to OR. • Hypertensive crisis – Hemorrhagic necrosis of pheo – Need iv therapy – phentolamine infusion – May need fluid resuscitation (may be volume deplete)
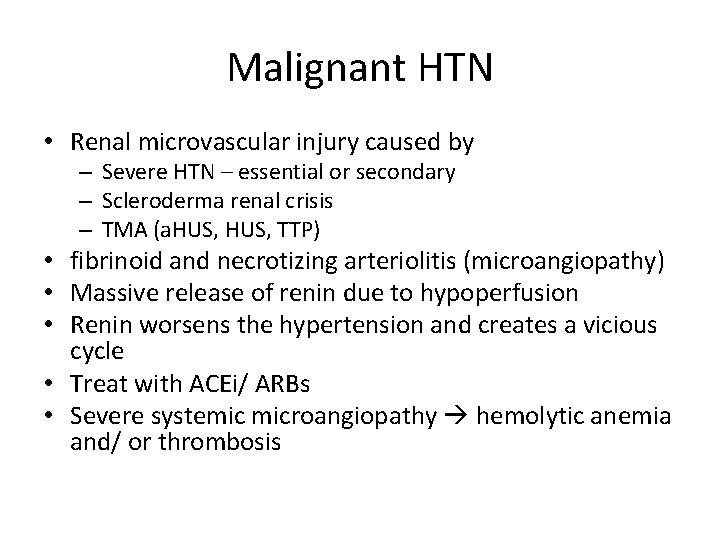
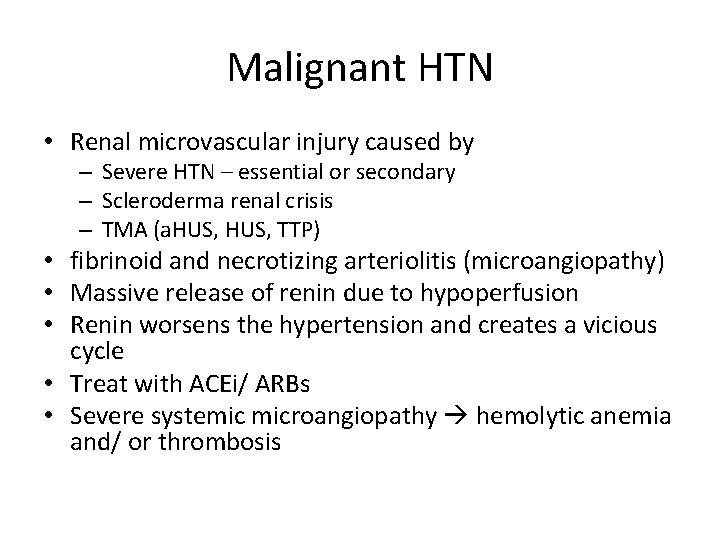
Malignant HTN • Renal microvascular injury caused by – Severe HTN – essential or secondary – Scleroderma renal crisis – TMA (a. HUS, TTP) • fibrinoid and necrotizing arteriolitis (microangiopathy) • Massive release of renin due to hypoperfusion • Renin worsens the hypertension and creates a vicious cycle • Treat with ACEi/ ARBs • Severe systemic microangiopathy hemolytic anemia and/ or thrombosis
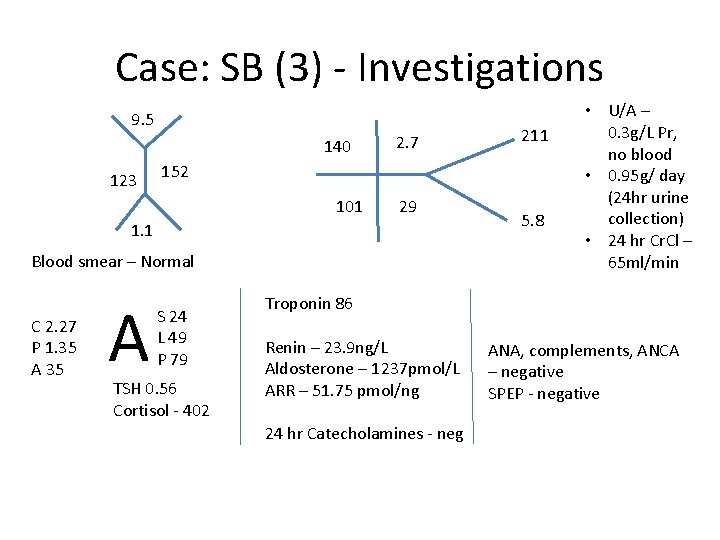
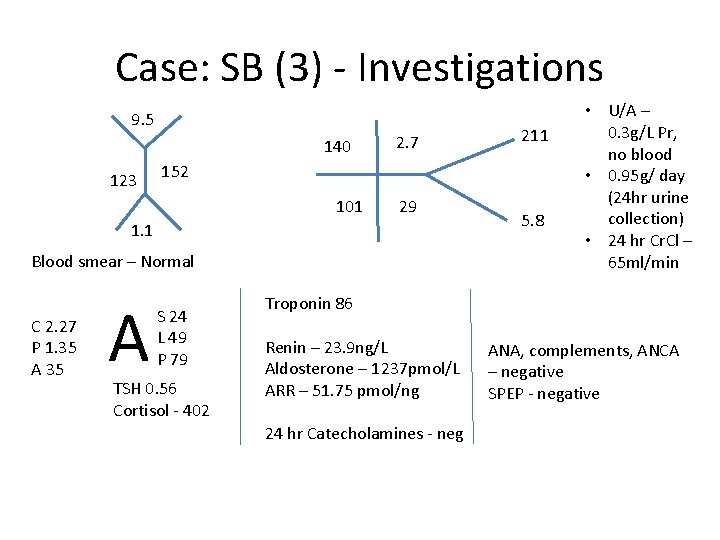
Case: SB (3) - Investigations 9. 5 140 123 2. 7 152 101 29 1. 1 Blood smear – Normal C 2. 27 P 1. 35 A 211 S 24 L 49 P 79 TSH 0. 56 Cortisol - 402 5. 8 • U/A – 0. 3 g/L Pr, no blood • 0. 95 g/ day (24 hr urine collection) • 24 hr Cr. Cl – 65 ml/min Troponin 86 Renin – 23. 9 ng/L Aldosterone – 1237 pmol/L ARR – 51. 75 pmol/ng 24 hr Catecholamines - neg ANA, complements, ANCA – negative SPEP - negative
Case: SB (4) • Investigations – MRI abdomen – No significant RAS • Echo and cardiac MRI – Borderline increase in LV mass
Case: SB (5) • Remained hypokalemic – but on diuretic • Discontinued chlorthalidone, and started olmesartan, continued KCl tabs • May add spironolactone, amiloride • BP improved • Creatinine stable at 198 - ~ 70 ml/min
Conclusions • Have suspicion of secondary cause of HTN in appropriate situations • Most common cause is hyperaldosteronism (primary or secondary) • Specific conditions require specific treatments
Bogged down by questions? contact: asad. merchant@uhn. ca
 Htn urgency vs emergency
Htn urgency vs emergency Htn statis dan dinamis
Htn statis dan dinamis Hubungan htn dengan ilmu lainnya
Hubungan htn dengan ilmu lainnya Cad htn
Cad htn Hypertensive emergency vs urgency
Hypertensive emergency vs urgency Htn vs goap
Htn vs goap Hypertensive emergency vs urgency
Hypertensive emergency vs urgency Malignant hypertension treatment
Malignant hypertension treatment One point perspective lettering
One point perspective lettering Silo perspective vs business process perspective
Silo perspective vs business process perspective Circles of my multicultural self
Circles of my multicultural self Cake è countable or uncountable
Cake è countable or uncountable Some say the world will end in fire some say in ice
Some say the world will end in fire some say in ice Contact vs noncontact forces
Contact vs noncontact forces Sometimes you win some
Sometimes you win some Some say the world will end in fire some say in ice
Some say the world will end in fire some say in ice They say it only takes a little faith to move a mountain
They say it only takes a little faith to move a mountain Some trust in horses
Some trust in horses Health coaches for hypertension control
Health coaches for hypertension control Jnc7
Jnc7 Nursing management of portal hypertension
Nursing management of portal hypertension Diagnosing hypertension
Diagnosing hypertension Conclusion of hypertension
Conclusion of hypertension Pulmonary hypertension
Pulmonary hypertension Definition of hypertension
Definition of hypertension Malignant hypertension ppt
Malignant hypertension ppt Causes of secondary hypertension
Causes of secondary hypertension Jnc 8 hypertension classification
Jnc 8 hypertension classification Diagnosis hypertension
Diagnosis hypertension Chd pulmonary hypertension
Chd pulmonary hypertension Diueritique
Diueritique Hypertensive crisis classification
Hypertensive crisis classification Hypertensive encephalopathy
Hypertensive encephalopathy Dr douglas simonetto
Dr douglas simonetto Symptoms of portal hypertension
Symptoms of portal hypertension Antihypertensive drugs
Antihypertensive drugs Definition of hypertension
Definition of hypertension Traitement hypertension
Traitement hypertension Stage 1 hypertension
Stage 1 hypertension Rules of halves in hypertension
Rules of halves in hypertension Signe de kernig
Signe de kernig Presenting complaints of hypertension
Presenting complaints of hypertension Pulmonary hypertension definition
Pulmonary hypertension definition Gestational hypertension symptoms
Gestational hypertension symptoms Conclusion of hypertension
Conclusion of hypertension Classification of hypertension
Classification of hypertension American heart association 2020
American heart association 2020 Difference between cld and dcld
Difference between cld and dcld