HORMONE AND CARDIOVASCULAR SYSTEM dr Sri Lestari Sulistyo












- Slides: 46

HORMONE AND CARDIOVASCULAR SYSTEM dr. Sri Lestari Sulistyo Rini, MSc
Introduction Ø Various hormones, chemicals Ø Start at a low pace, Ø Have long-lasting influences on cardiovascular function. Ø Hormones and chemicals are classified into two groups Ø Vasoconstrictors Ø Vasodilators


Posterior Pituitary Hormone • Anti diuretic hormone or VASOPRESSIN • Stimulate the contraction of smooth muscle in the arterioles, small blood vessels that connect the arteries to capillaries – blood pressure rises • Oxytocin – induces natriuresis and causes a fall in mean arterial pressure – oxytocin triggers ANP release in vivo
Vasopressin Ø Also called antidiuretic hormone (ADH), Ø formed in the hypothalamus (mainly) Ø secreted through the posterior pituitary gland. Ø even more powerful than angiotensin as a vasoconstrictor. Ø The high concentration of vasopressin during hemorrhage can raise the arterial pressure as much as 40 to 60 mm. Hg.
Vasopressin Ø The amount of endogenous vasopressin in the circulation of normal individuals does not normally affect blood pressure. Ø it does not increase blood pressure when small doses are injected in vivo Ø Acts on the brain to cause a decrease in cardiac output. Ø (in the area of postrema, one of the circumventricular organs) Ø Acts on the kidney
Anterior Pituitary Hormone • GROWTH HORMONE – The physiological nature of cardiac growth is accounted by • the increment in cardiomyocyte size occurs prevalently at expense of the short axis. – This is the basis for the concentric pattern of left ventricular (LV) hypertrophy, • improved contractility and relaxation, and a favorable energetic setting; • the capillary density of the myocardial tissue
Anterior Pituitary Hormone – balanced growth of cardiomyocytes and nonmyocyte elements, which accounts for the lack of interstitial fibrosis – myocardial energetics and mechanics are not perturbed – the growth response is not associated with the gene re-programming that characterizes pathologic cardiac hypertrophy and heart failure
Anterior Pituitary Hormone • Prolactin – Increasing blood pressure – In collaboration with noradrenalin
• INSULIN : – insulin and leptin cooperate in the modulation of vascular tone • through enhancement of endothelial NO release. • A major impact on the regulation of the cardiovascular system, characterized by endothelial NO dysfunction and metabolic disorders, – such as arterial hypertension.

• SEX HORMONE – The greater incidence of hypertension and coronary artery disease in men and postmenopausal women compared with premenopausal women has been related, in part, to gender differences in vascular tone and possible vascular protective effects of the female sex hormones estrogen and progesterone

• Estrogen, progesterone, and testosterone receptors have been identified in blood vessels and cardiomyocytes of human and other mammals and have been localized in the plasmalemma, cytosol, and nuclear compartments of various vascular cells, including the endothelium and the smooth muscle.
• The sex hormone-induced stimulation of the endothelium-dependent mechanisms of vascular relaxation and inhibition of the mechanisms of vascular smooth muscle contraction
• ESTROGEN – Inflammation plays an important role in the response to endoluminal vascular injury. Estrogen (17 beta-estradiol, E 2) inhibits neointima formation in animal models – E 2 may limit the neointimal response to endoluminal vascular injury, at least in part, by limiting leukocyte entry from adventitial/periadventitial tissues into injured vessels early in the injury response.
• Estrogen also has anti-clot function Avoid the formation of thrombus and thus can slow down the hardening of arteries • Microvascular endothelial cells -- cells in the lining of the smallest blood vessels -- produce estrogen and express estrogen receptor
• Estrogen may derive part of its known cardiovascular protective effect by increasing production of nitric oxide in microvascular endothelial cells • Decreasing of Estrogen may induce arrhythmia
Progesterone • postmenopausal women, higher blood levels of progesterone are associated with less of an increase in blood pressure and less blood vessel constriction in response to angiotensin II, one of the naturally occurring substances in the body which causes the blood vessels to constrict

• TESTOSTERONE – Male sex is an acknowledged risk factor for many forms of cardiovascular disease, and vascular disease prevalence patterns appear to be different in men versus women. The vascular properties of the principal mammalian androgen, testosterone, are complex and linked to dose, duration of exposure, presence of underlying vascular disease, and, possibly, biological sex
– lower levels of testosterone in men are associated with higher blood pressure, left ventricular mass, and left ventricular hypertrophy. – Data from isolated vessels and animal models suggest that pharmacological doses of testosterone, or its potent intracellular metabolite dehydrotestosterone, produce vasodilatation.
– Testosterone's endothelium-dependent effects are likely mediated at least in part through nitric oxide (NO) elaboration, whereas mechanisms of endothelium-independent effects involve 1 or more types of smooth muscle ion conductance channels – Clinical studies indicate that, in men, androgen replacement may provide beneficial effects when coronary artery disease is present
• High-dose testosterone significantly increased the circulating plasma testosterone concentration, and was associated with a dramatic increase in brachial artery vasodilatation
• Males with CAD and associated low serum levels of testosterone, is the population in which testosterone replacement therapy may be clinically advantageous – in women, testosterone may augment existing hypertension, increase risk for cardiovascular events, or promote atherogenesis. – there is a relationship between endogenous androgen levels and arterial stiffness in older men.
• Minor endocrine gland – Atriopeptin (atrialnatriuretic factor) • Helps maintain homoestatic balance of fluids, electrolytes. • Lowers blood pressure, blood volume • Target areas are blood vessel, kidneys and adrenal glands
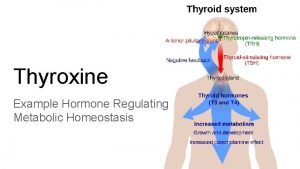
Effects of Thyroid Hormones on the Cardiovascular System • • • Increase heart rate Increase force of cardiac contractions Increase stroke volume Increase Cardiac output Up-regulate catecholamine receptors
• Thyroid have chronotropic effect (increase number and affinity of adrenergic receptors) and inotropic effect (enhance response to circulating catecholamines and increase proportion of myosin heavy chain) on the heart as a target tissue
Autonomic Pacemaker Regulation • Sympathetic and parasympathetic stimulation: – greatest at SA node (heart rate) • Membrane potential of pacemaker cells: lower than other cardiac cells • Rate of spontaneous depolarization depends on: – resting membrane potential – rate of depolarization • ACh (parasympathetic stimulation): – slows the heart • NE (sympathetic stimulation): – speeds the heart
Hormonal Effects on Heart Rate • Increase heart rate (by sympathetic stimulation of SA node): – epinephrine (E) – norepinephrine (NE) – thyroid hormone
Vasoconstrictors and Vasodilators Ø Vasoconstrictors Ø Epinephrine and Norepinephrine Ø Angiotensin II Ø Vasopressin Ø Vasodilators Ø EDRF (NO)(endotelial dilated releasing factor / nitric oxide)
Epinephrine and Norepinephrine Ø The adrenal medulla secrete both epinephrine (80%) and norepinephrine (20%) Ø carried by blood flow to everywhere in the body. Ø In the blood, only a little norepinephrine comes form the endings of the adrenergic fibers.
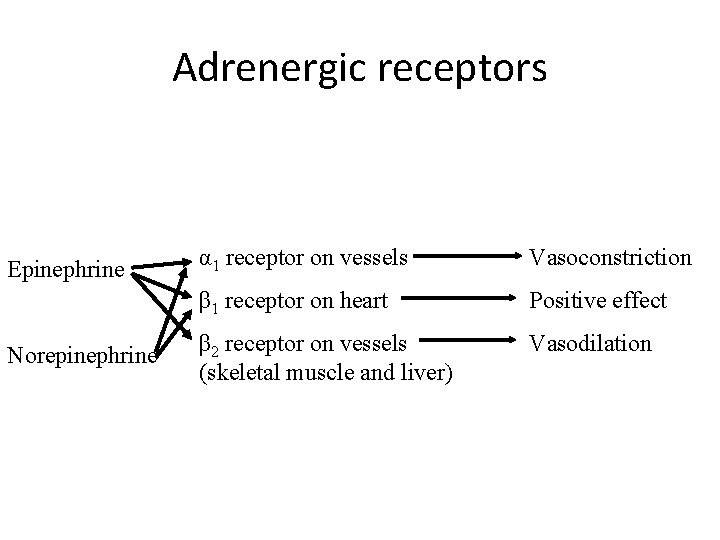
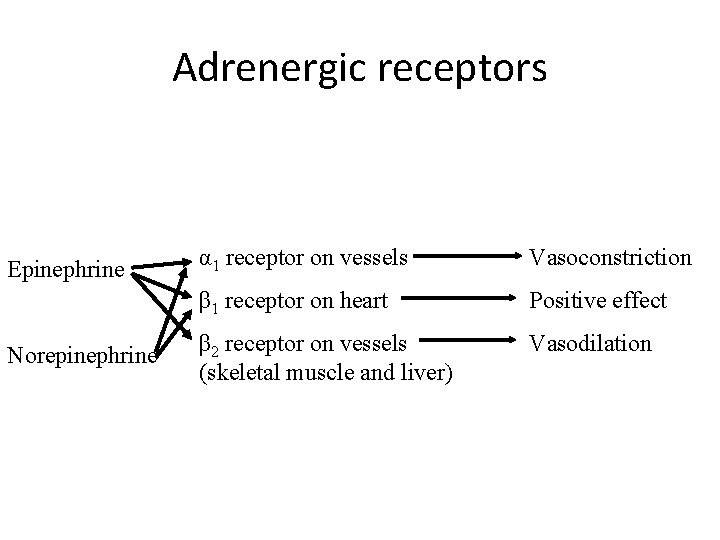
Adrenergic receptors Epinephrine Norepinephrine α 1 receptor on vessels Vasoconstriction β 1 receptor on heart Positive effect β 2 receptor on vessels (skeletal muscle and liver) Vasodilation

Effect Ø On heart in vitro (contractility and automaticity). Ø both increase the force and rate of contraction of the isolated heart. Ø mediated by β 1 receptors.
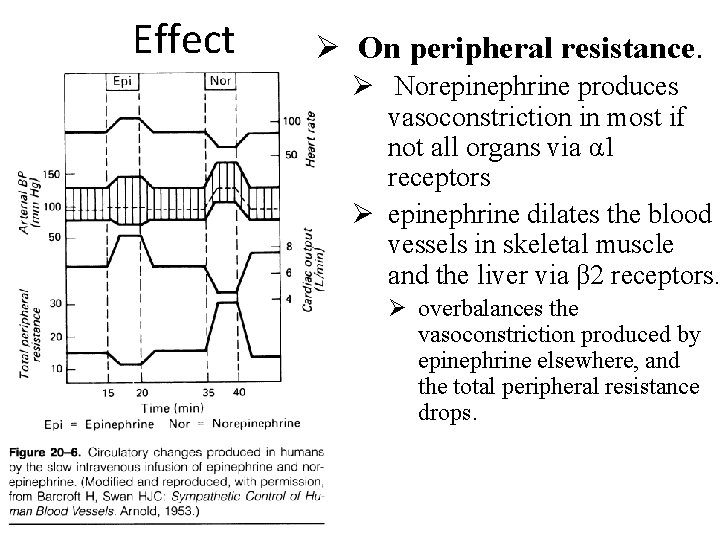
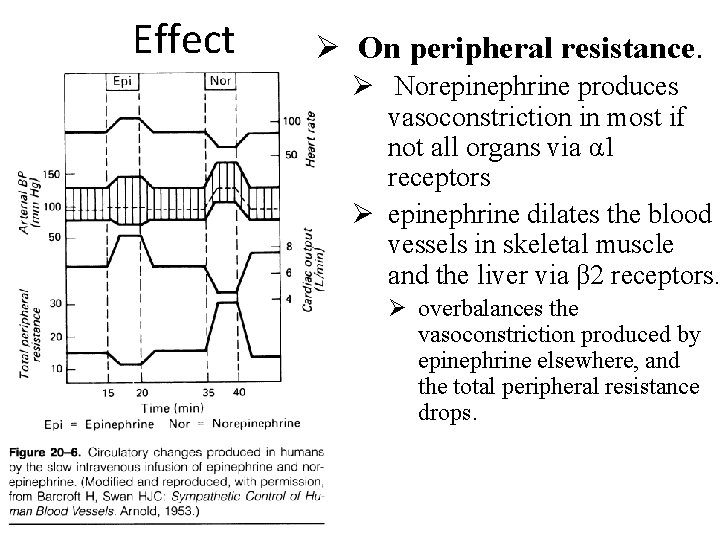
Effect Ø On peripheral resistance. Ø Norepinephrine produces vasoconstriction in most if not all organs via α 1 receptors Ø epinephrine dilates the blood vessels in skeletal muscle and the liver via β 2 receptors. Ø overbalances the vasoconstriction produced by epinephrine elsewhere, and the total peripheral resistance drops.
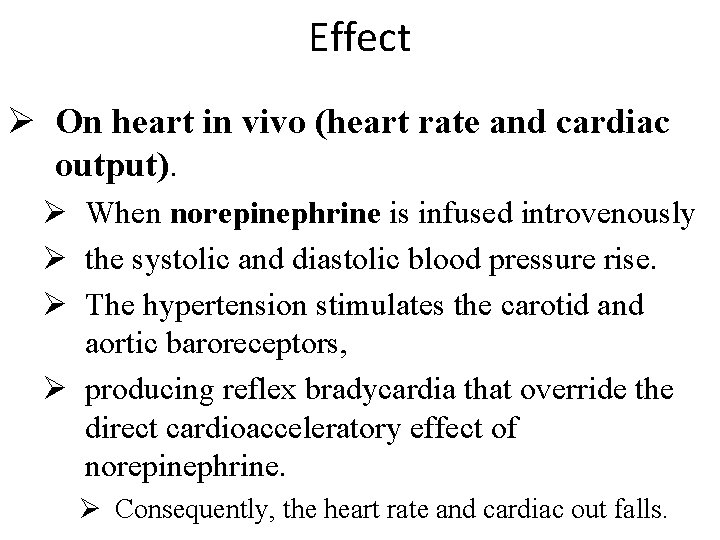
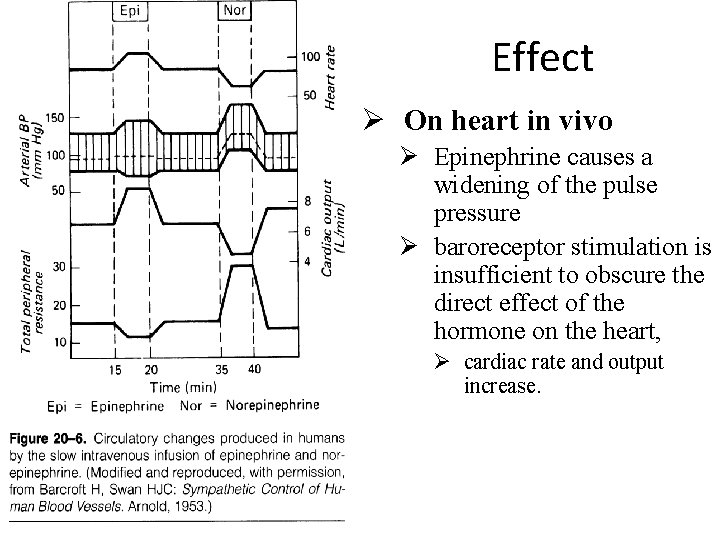
Effect Ø On heart in vivo (heart rate and cardiac output). Ø When norepinephrine is infused introvenously Ø the systolic and diastolic blood pressure rise. Ø The hypertension stimulates the carotid and aortic baroreceptors, Ø producing reflex bradycardia that override the direct cardioacceleratory effect of norepinephrine. Ø Consequently, the heart rate and cardiac out falls.
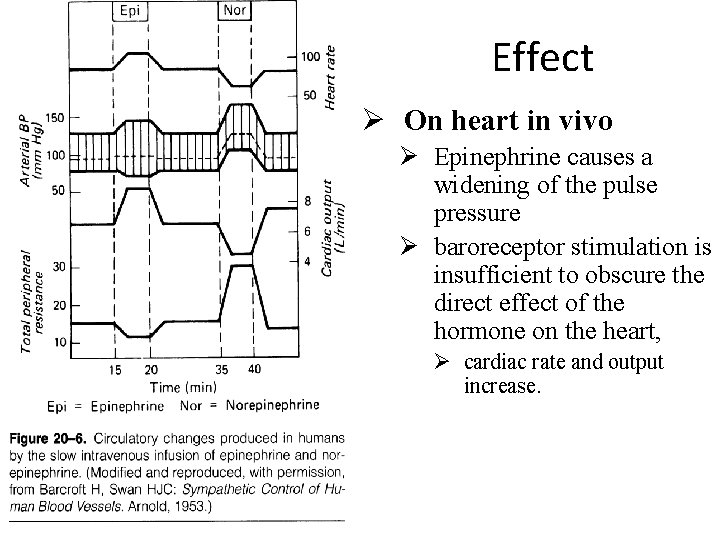
Effect Ø On heart in vivo Ø Epinephrine causes a widening of the pulse pressure Ø baroreceptor stimulation is insufficient to obscure the direct effect of the hormone on the heart, Ø cardiac rate and output increase.




Angiotensin II Ø very potent vasoconstrictor Ø formed in the plasma through a chain reaction. Ø The chain is triggered by a substance, renin, released form kidneys. Ø Renin is released from kidneys in response to renal ischemia, which may be due to a fall in blood pressure.
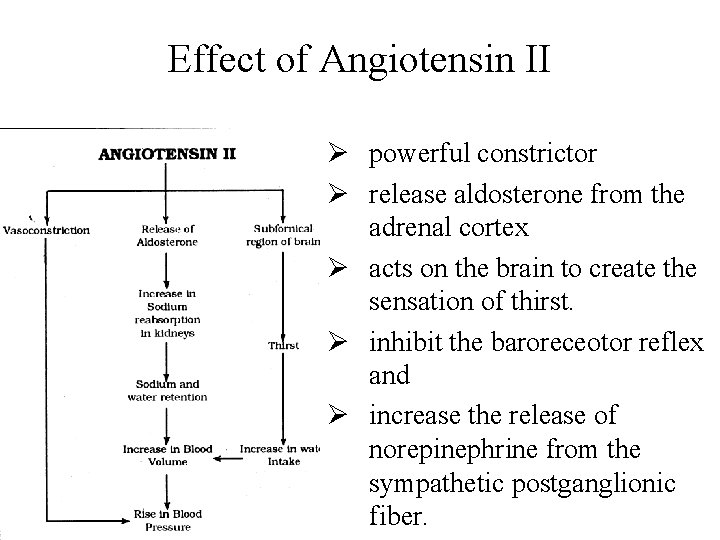
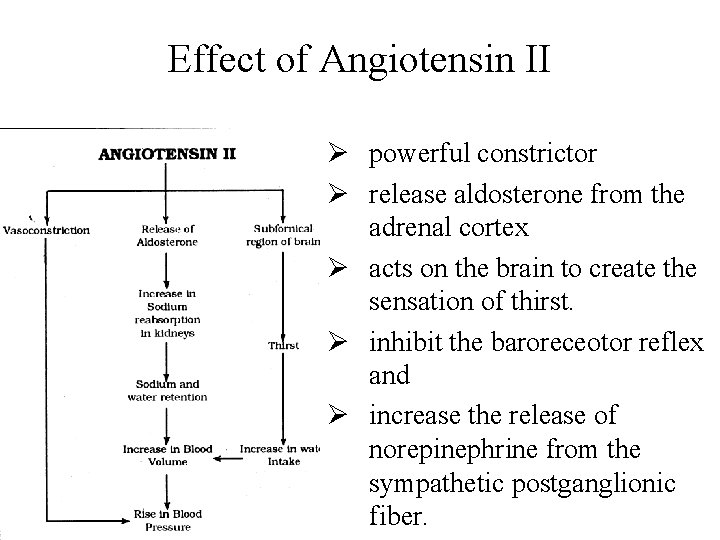
Effect of Angiotensin II Ø powerful constrictor Ø release aldosterone from the adrenal cortex Ø acts on the brain to create the sensation of thirst. Ø inhibit the baroreceotor reflex and Ø increase the release of norepinephrine from the sympathetic postganglionic fiber.
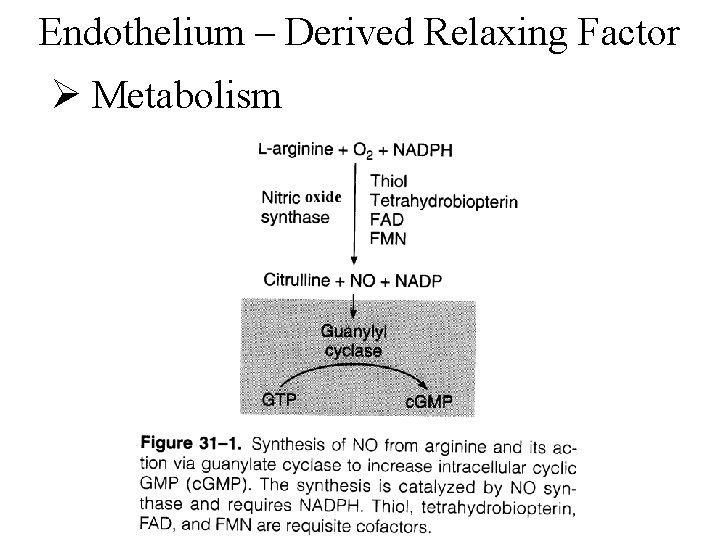
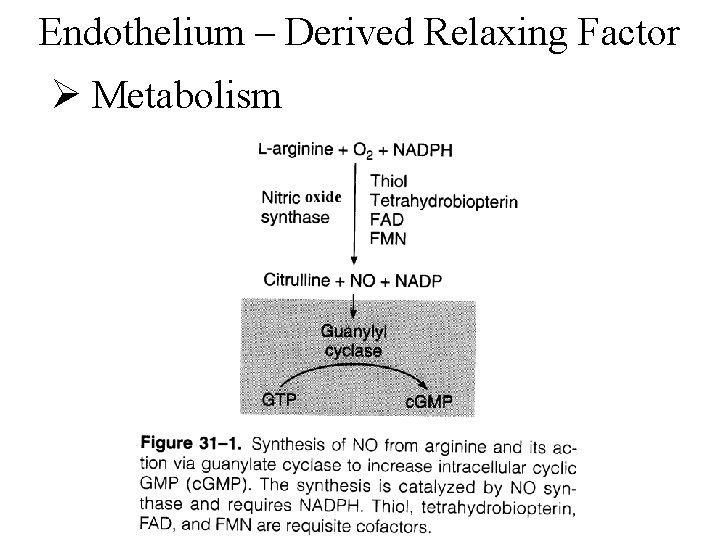
Endothelium – Derived Relaxing Factor Ø Metabolism
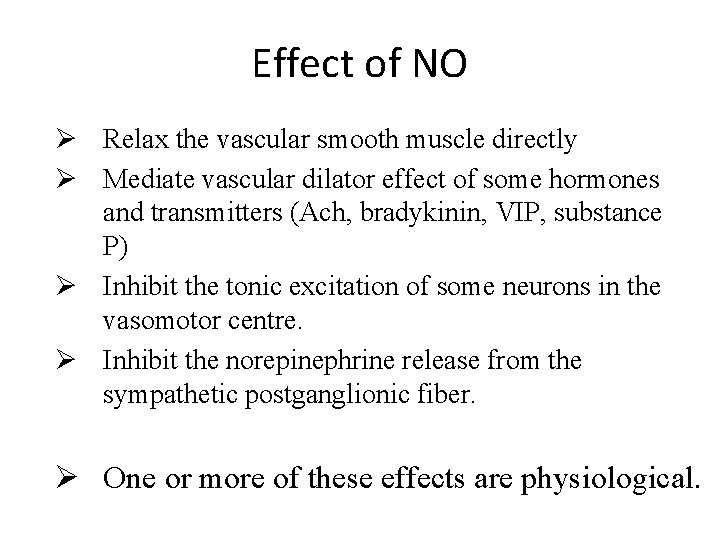
Effect of NO Ø Relax the vascular smooth muscle directly Ø Mediate vascular dilator effect of some hormones and transmitters (Ach, bradykinin, VIP, substance P) Ø Inhibit the tonic excitation of some neurons in the vasomotor centre. Ø Inhibit the norepinephrine release from the sympathetic postganglionic fiber. Ø One or more of these effects are physiological.
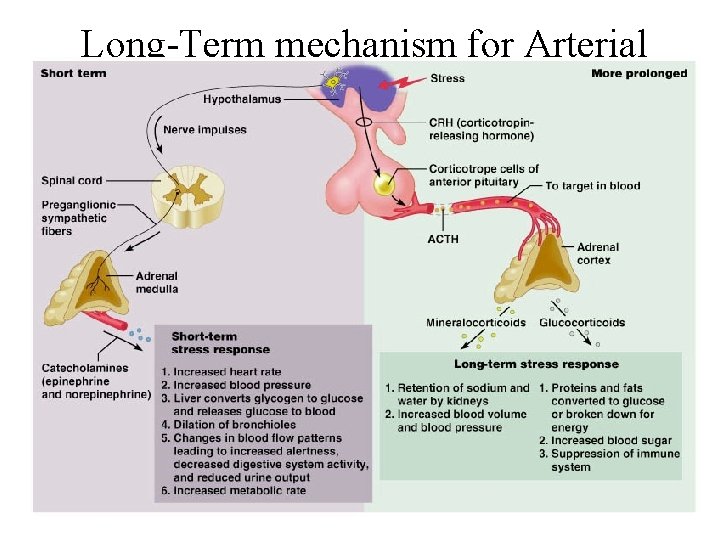
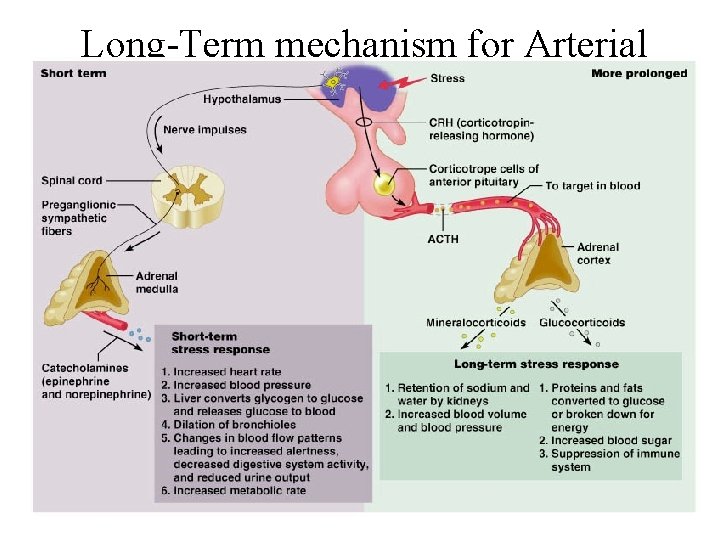
Long-Term mechanism for Arterial Pressure Regulation ØRenal –body Fluid Mechanism

Terima kasih
 Sri rama sri rama sri manoharama
Sri rama sri rama sri manoharama Dr sri lestari
Dr sri lestari Budi sulistyo kkp
Budi sulistyo kkp Dina ayu lestari
Dina ayu lestari Drg dwi imbang lestari
Drg dwi imbang lestari Drg dwi imbang lestari
Drg dwi imbang lestari Pt hutan amanah lestari
Pt hutan amanah lestari Dina lestari enterprise
Dina lestari enterprise Pt strawberindo lestari
Pt strawberindo lestari Pamuji lestari
Pamuji lestari Batang
Batang Desi lestari
Desi lestari Albe lestari
Albe lestari Pt asia pratama walindo
Pt asia pratama walindo Pt. indobamboo lestari
Pt. indobamboo lestari Anggi lestari
Anggi lestari Anatomy and physiology unit 7 cardiovascular system
Anatomy and physiology unit 7 cardiovascular system Chapter 8 cardiovascular system
Chapter 8 cardiovascular system Chapter 19 the cardiovascular system blood vessels
Chapter 19 the cardiovascular system blood vessels What makes up the cardiovascular system
What makes up the cardiovascular system Pithed rat meaning
Pithed rat meaning Cardiovascular/lymphatic system it's totally tubular
Cardiovascular/lymphatic system it's totally tubular Structure of blood vessels
Structure of blood vessels Chapter 5 learning exercises medical terminology
Chapter 5 learning exercises medical terminology Chapter 11 the cardiovascular system figure 11-3
Chapter 11 the cardiovascular system figure 11-3 Chapter 11 the cardiovascular system figure 11-10 answers
Chapter 11 the cardiovascular system figure 11-10 answers Chapter 11 the cardiovascular system
Chapter 11 the cardiovascular system Lesson 11 cardiovascular system
Lesson 11 cardiovascular system Tissues in circulatory system
Tissues in circulatory system Anatomy blood vessels
Anatomy blood vessels Introduction to cardiovascular system
Introduction to cardiovascular system Ptca
Ptca Chapter 13 cardiovascular system
Chapter 13 cardiovascular system Chapter 11 the cardiovascular system figure 11-2
Chapter 11 the cardiovascular system figure 11-2 The cardiovascular system includes the
The cardiovascular system includes the Blood vessels
Blood vessels True capillaries
True capillaries Reproductive physiology
Reproductive physiology Payment and settlement system in sri lanka
Payment and settlement system in sri lanka Lanka settle system
Lanka settle system Payment and settlement system in sri lanka
Payment and settlement system in sri lanka Sri system of rice intensification
Sri system of rice intensification Tsunami early warning system sri lanka
Tsunami early warning system sri lanka Sri system of rice intensification
Sri system of rice intensification Sri system of rice intensification
Sri system of rice intensification Stages of palay
Stages of palay Allegro productivity toolbox
Allegro productivity toolbox