Gout Pharmacotherapy Ryan L Crass Pharm D PGY



- Slides: 48
Gout Pharmacotherapy Ryan L. Crass, Pharm. D PGY 1 Pharmacy Resident UK Health. Care ryan. crass@uky. edu
Learning Objectives 1. Understand the pathophysiology of and risk factors for the development of gouty arthritis 2. Recognize clinical and laboratory findings consistent with the diagnosis of gout and how they are modified by treatment 3. Explain the different treatment modalities for acute gout attacks and long-term prophylaxis 4. Discuss the mechanisms, major adverse effects, and key drug-drug interactions for the primary medications used in the treatment and prevention of gout
“The Disease of Kings”
Characterizing the Disease PATHOPHYSIOLOGY, MANIFESTATIONS, AND DIAGNOSIS
Characterizing Gout • Gout is a spectrum of clinical features related to an excess total body burden of uric acid • One of the most common adulthood rheumatic diseases – about 4% of U. S. adults (~ 8. 3 million people) Khanna D, et al. Arthritis Care Res. 2012; 64(10): 1431 -1446.
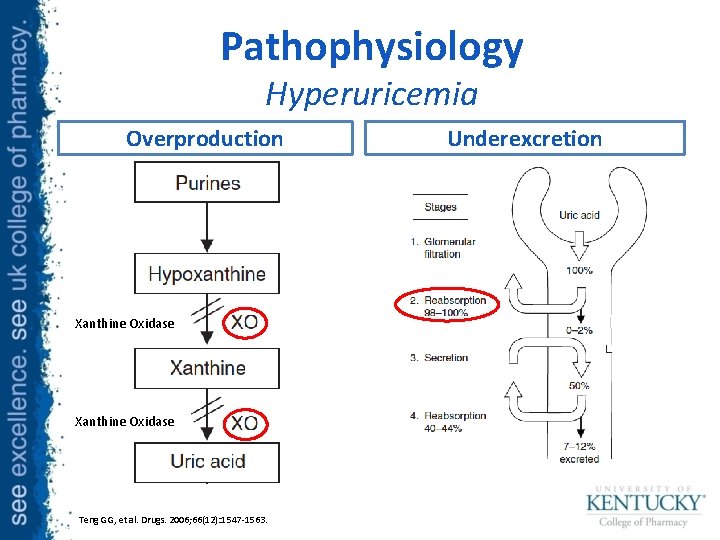
Pathophysiology Hyperuricemia • Uric acid is byproduct of purine metabolism • Hyperuricemia occurs when there is an imbalance in uric acid production and excretion – Defined as serum uric acid > 7 mg/d. L Teng GG, et al. Drugs. 2006; 66(12): 1547 -1563.
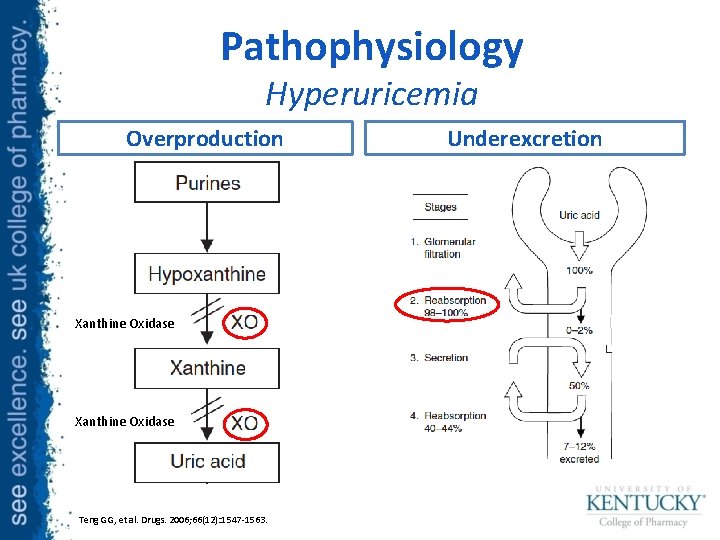
Pathophysiology Hyperuricemia Overproduction Xanthine Oxidase Teng GG, et al. Drugs. 2006; 66(12): 1547 -1563. Underexcretion
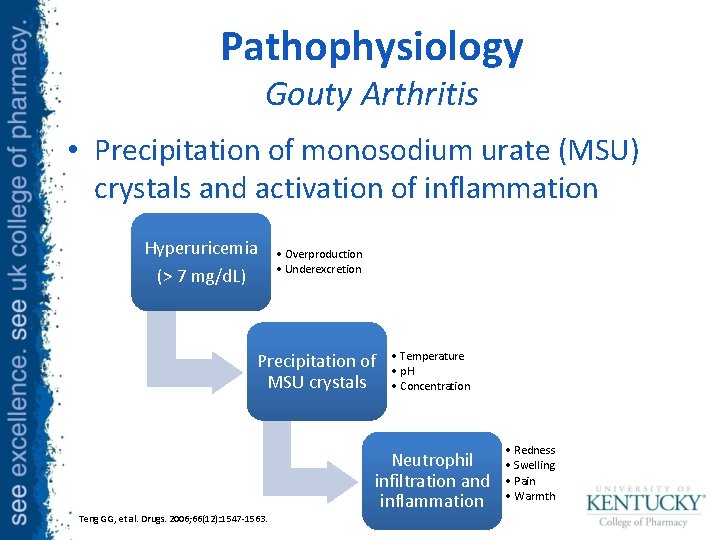
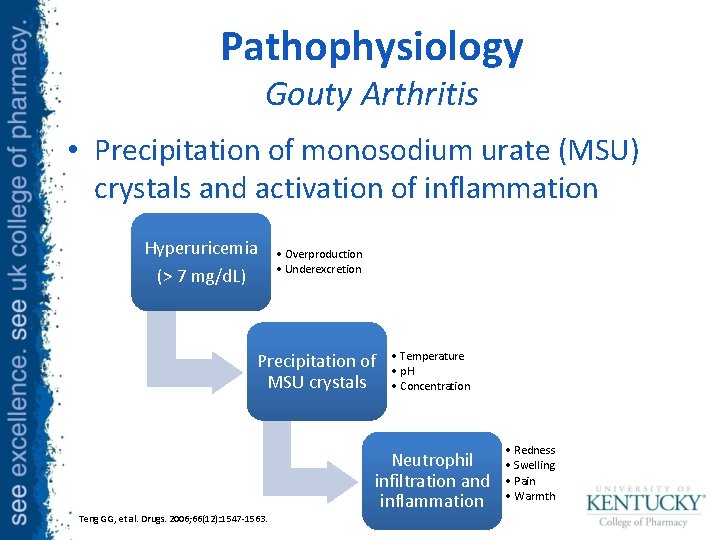
Pathophysiology Gouty Arthritis • Precipitation of monosodium urate (MSU) crystals and activation of inflammation Hyperuricemia (> 7 mg/d. L) • Overproduction • Underexcretion Precipitation of MSU crystals • Temperature • p. H • Concentration Neutrophil infiltration and inflammation Teng GG, et al. Drugs. 2006; 66(12): 1547 -1563. • Redness • Swelling • Pain • Warmth
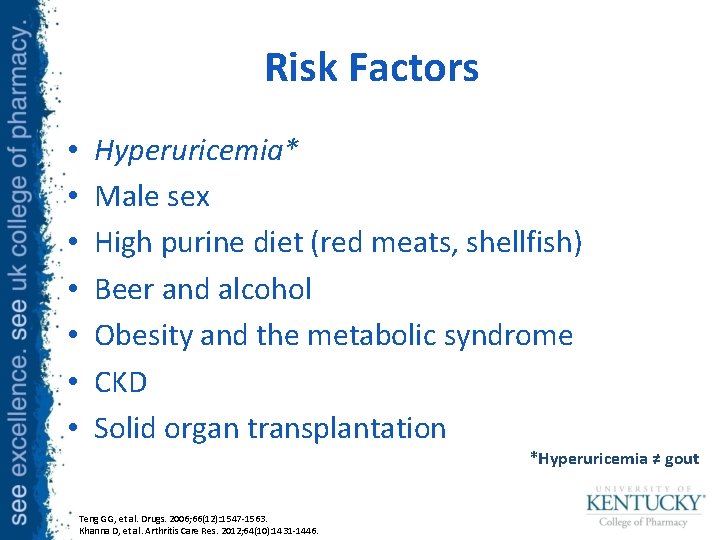
Risk Factors • • Hyperuricemia* Male sex High purine diet (red meats, shellfish) Beer and alcohol Obesity and the metabolic syndrome CKD Solid organ transplantation *Hyperuricemia ≠ gout Teng GG, et al. Drugs. 2006; 66(12): 1547 -1563. Khanna D, et al. Arthritis Care Res. 2012; 64(10): 1431 -1446.
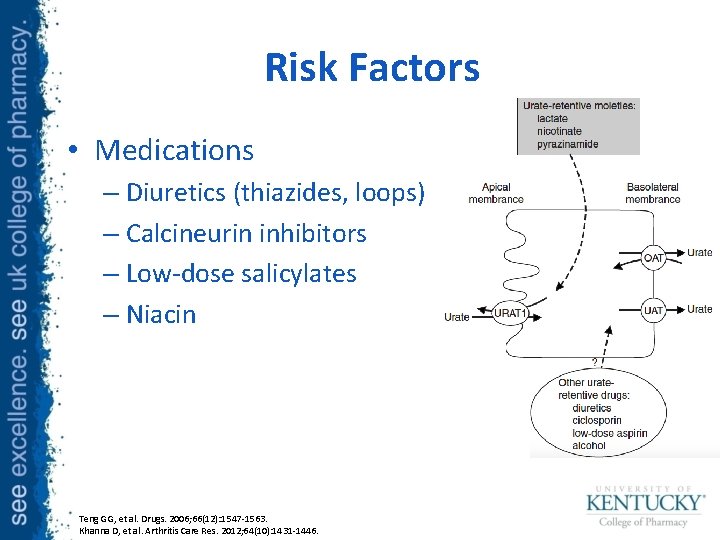
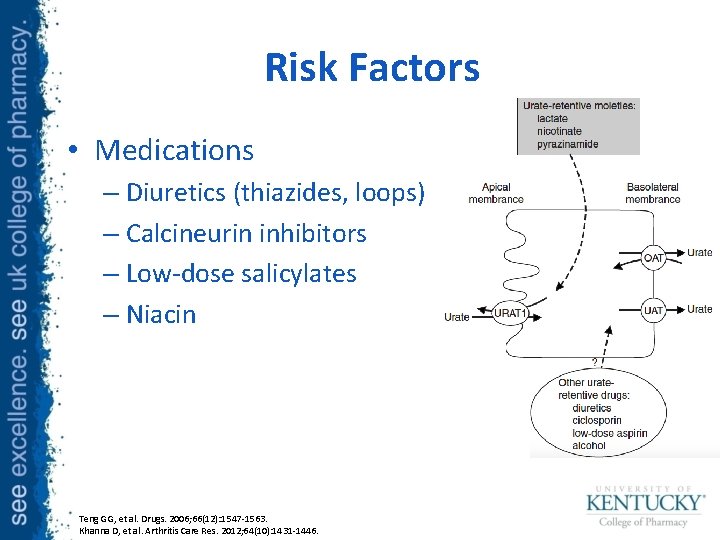
Risk Factors • Medications – Diuretics (thiazides, loops) – Calcineurin inhibitors – Low-dose salicylates – Niacin Teng GG, et al. Drugs. 2006; 66(12): 1547 -1563. Khanna D, et al. Arthritis Care Res. 2012; 64(10): 1431 -1446.

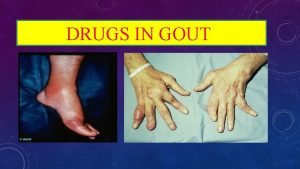
Clinical Manifestations Acute Gouty Arthritis (“Flare”) • Symptoms – Warmth/swelling – Severe Pain – Fever, leukocytosis • Location: – Usually monoarticular • Time course – Onset: Rapid – Peak: 8 -12 hours – Duration: 3 -10 days Teng GG, et al. Drugs. 2006; 66(12): 1547 -1563. Khanna D, et al. Arthritis Care Res. 2012; 64(10): 1431 -1446. Chronic Gouty Arhritis • Chronic Gout – Polyarticular involvement – Tophi = urate crystal aggregates – Nephropathy
Summary Disease Characteristics • The pathophysiology of gout is a dysregulation of the production and/or excretion of uric acid • Gout commonly manifests as an acutely painful monoarticular arthritis with or without tophi formation • Modifiable risk factors include diet, lifestyle, medications, and hyperuricemia

Treatment ACUTE GOUTY ARTHRITIS
General Principles • Maintenance ULT should be continued during attacks • Timing – Therapy should be initiated within 24 hours AND – Continued until resolution of symptoms *ULT = Urate lowering therapy Khanna D, et al. Arthritis Care Res. 2012; 64(10): 1447 -1461.
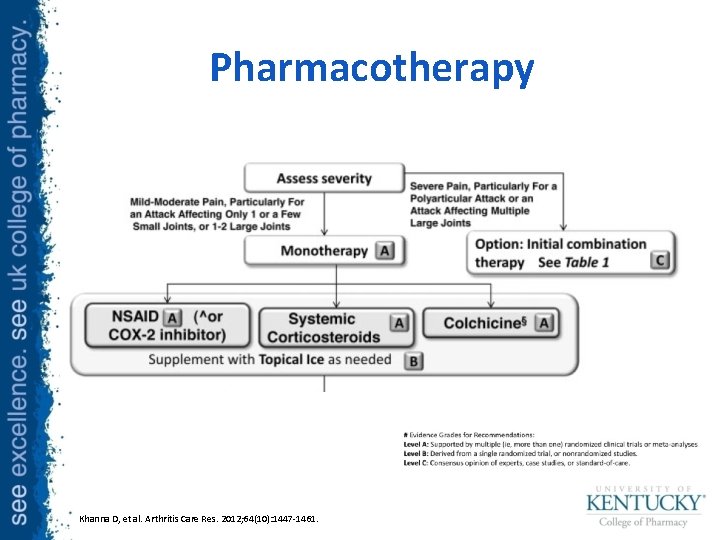
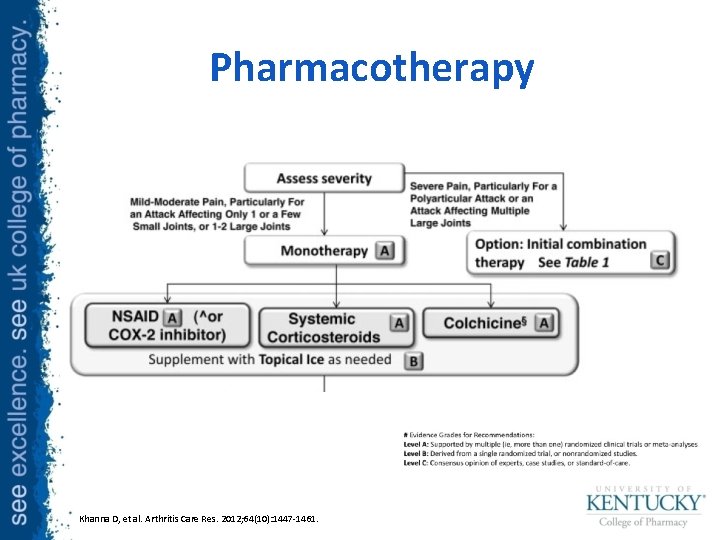
Pharmacotherapy Khanna D, et al. Arthritis Care Res. 2012; 64(10): 1447 -1461.
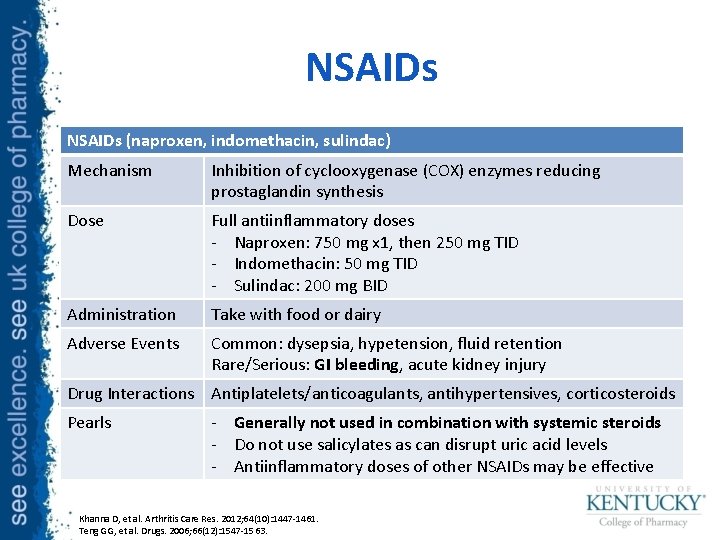
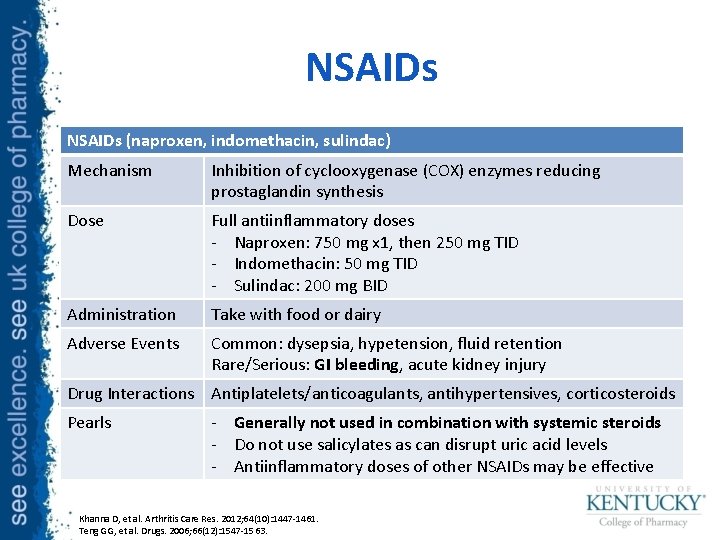
NSAIDs (naproxen, indomethacin, sulindac) Mechanism Inhibition of cyclooxygenase (COX) enzymes reducing prostaglandin synthesis Dose Full antiinflammatory doses - Naproxen: 750 mg x 1, then 250 mg TID - Indomethacin: 50 mg TID - Sulindac: 200 mg BID Administration Take with food or dairy Adverse Events Common: dysepsia, hypetension, fluid retention Rare/Serious: GI bleeding, acute kidney injury Drug Interactions Antiplatelets/anticoagulants, antihypertensives, corticosteroids Pearls - Generally not used in combination with systemic steroids - Do not use salicylates as can disrupt uric acid levels - Antiinflammatory doses of other NSAIDs may be effective Khanna D, et al. Arthritis Care Res. 2012; 64(10): 1447 -1461. Teng GG, et al. Drugs. 2006; 66(12): 1547 -1563.
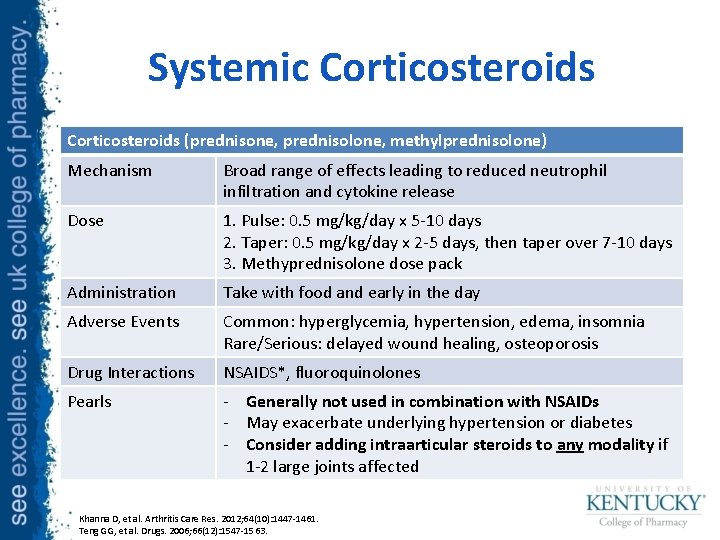
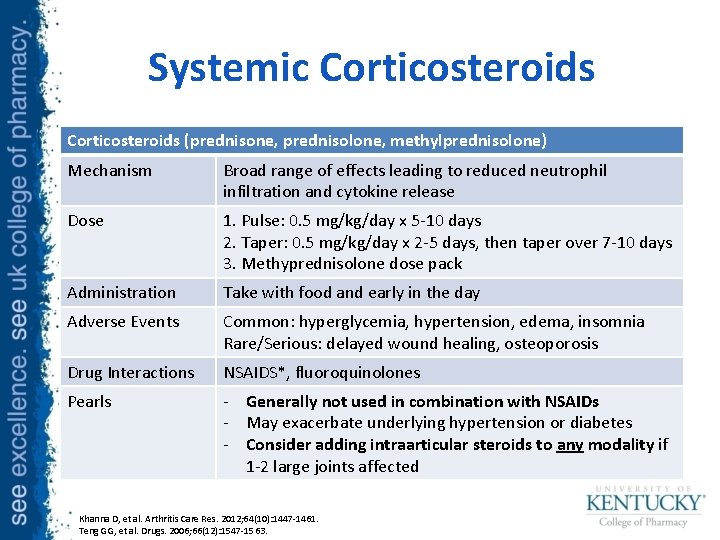
Systemic Corticosteroids (prednisone, prednisolone, methylprednisolone) Mechanism Broad range of effects leading to reduced neutrophil infiltration and cytokine release Dose 1. Pulse: 0. 5 mg/kg/day x 5 -10 days 2. Taper: 0. 5 mg/kg/day x 2 -5 days, then taper over 7 -10 days 3. Methyprednisolone dose pack Administration Take with food and early in the day Adverse Events Common: hyperglycemia, hypertension, edema, insomnia Rare/Serious: delayed wound healing, osteoporosis Drug Interactions NSAIDS*, fluoroquinolones Pearls - Generally not used in combination with NSAIDs - May exacerbate underlying hypertension or diabetes - Consider adding intraarticular steroids to any modality if 1 -2 large joints affected Khanna D, et al. Arthritis Care Res. 2012; 64(10): 1447 -1461. Teng GG, et al. Drugs. 2006; 66(12): 1547 -1563.
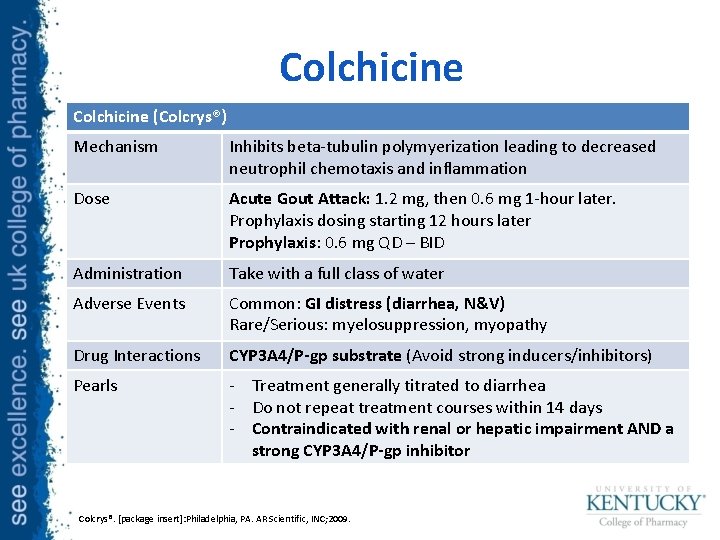
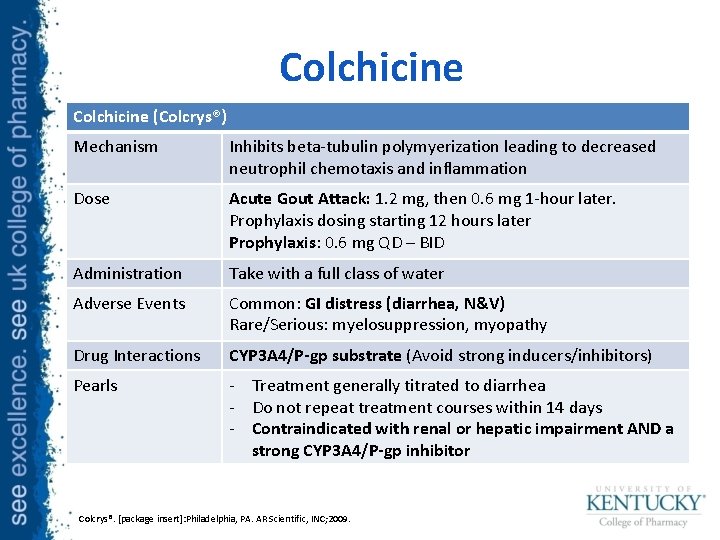
Colchicine (Colcrys®) Mechanism Inhibits beta-tubulin polymyerization leading to decreased neutrophil chemotaxis and inflammation Dose Acute Gout Attack: 1. 2 mg, then 0. 6 mg 1 -hour later. Prophylaxis dosing starting 12 hours later Prophylaxis: 0. 6 mg QD – BID Administration Take with a full class of water Adverse Events Common: GI distress (diarrhea, N&V) Rare/Serious: myelosuppression, myopathy Drug Interactions CYP 3 A 4/P-gp substrate (Avoid strong inducers/inhibitors) Pearls - Treatment generally titrated to diarrhea - Do not repeat treatment courses within 14 days - Contraindicated with renal or hepatic impairment AND a strong CYP 3 A 4/P-gp inhibitor Colcrys®. [package insert]: Philadelphia, PA. AR Scientific, INC; 2009.
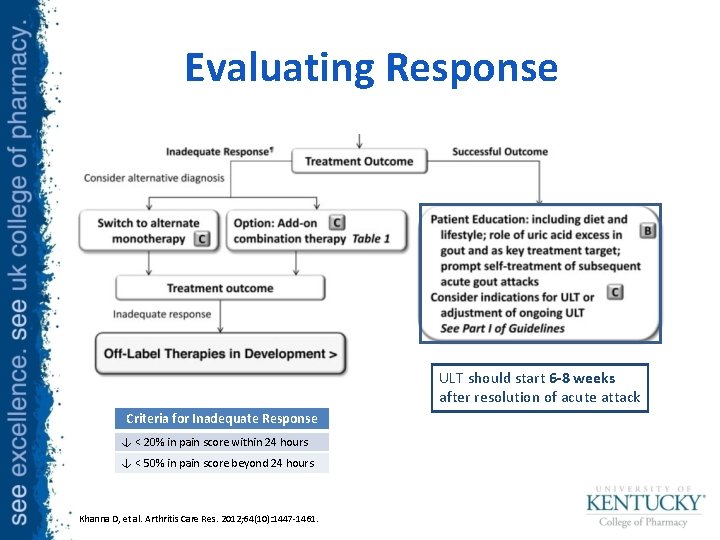
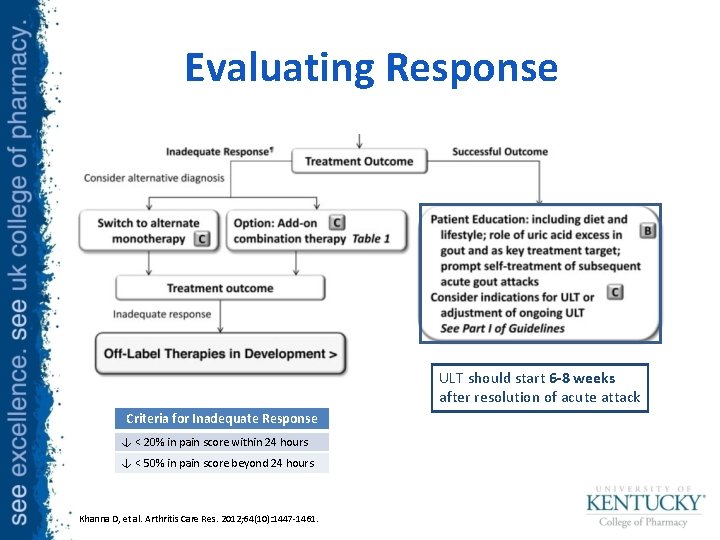
Evaluating Response ULT should start 6 -8 weeks after resolution of acute attack Criteria for Inadequate Response ↓ < 20% in pain score within 24 hours ↓ < 50% in pain score beyond 24 hours Khanna D, et al. Arthritis Care Res. 2012; 64(10): 1447 -1461.
Summary: Acute Gouty Arthritis • Pharmacotherapy is the mainstay of acute gout treatment • NSAIDs, systemic cortiocosteroids, and colchcine are all first line options and choice of agent should be guided by patient-specific factors • Combination therapy can be used for severe attacks

Treatment MAINTENANCE URATE LOWERING THERAPY
Non-pharmacologic Therapy • Dietary and lifestyle modifications – Consume in moderation • Alcohol, red meat, shellfish, sweets – Weight loss – Tobacco cessation – Appropriate hydration • Minimize non-essential medications that may induce hyperuricemia Khanna D, et al. Arthritis Care Res. 2012; 64(10): 1431 -1446.
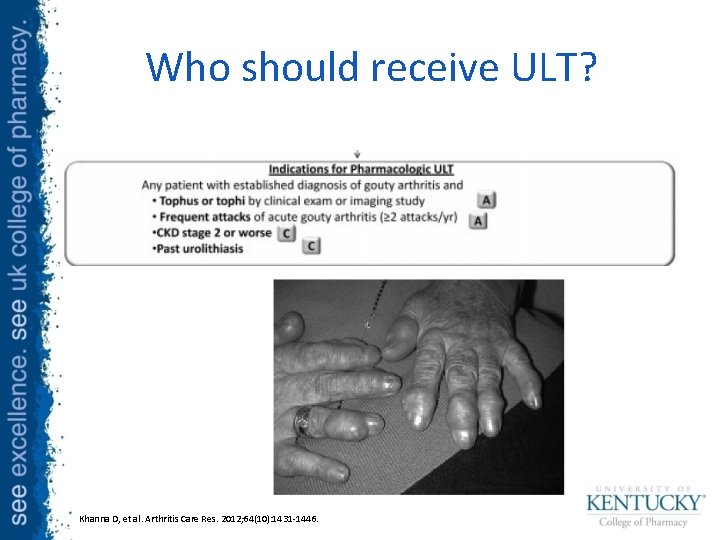
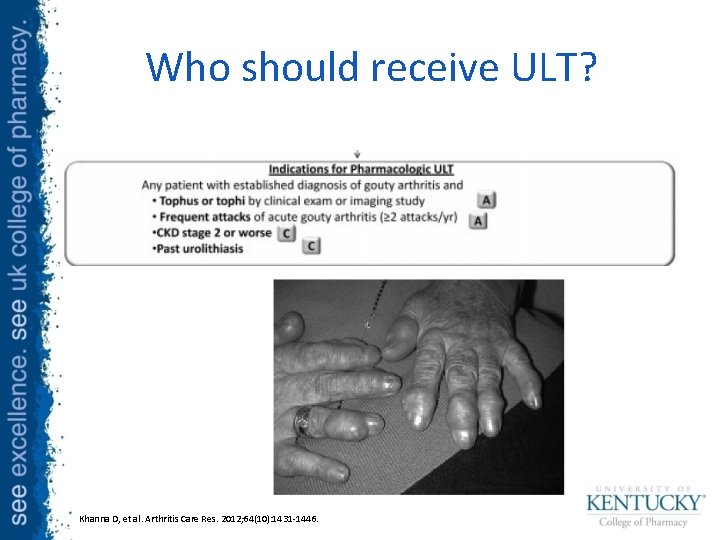
Who should receive ULT? Khanna D, et al. Arthritis Care Res. 2012; 64(10): 1431 -1446.
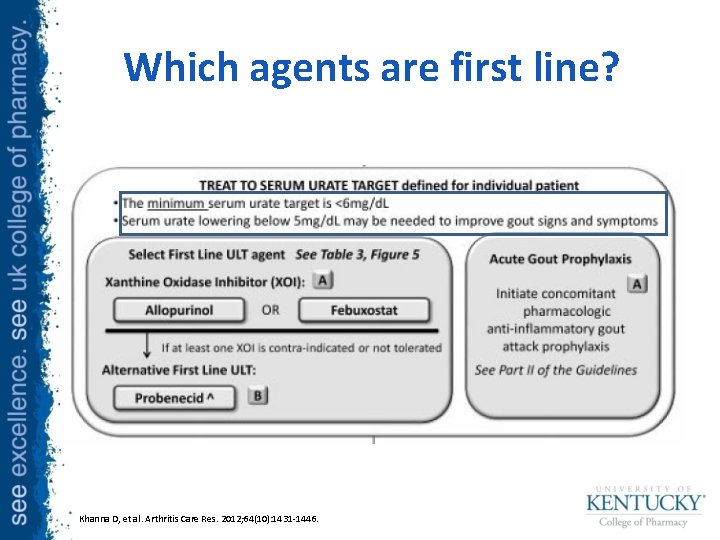
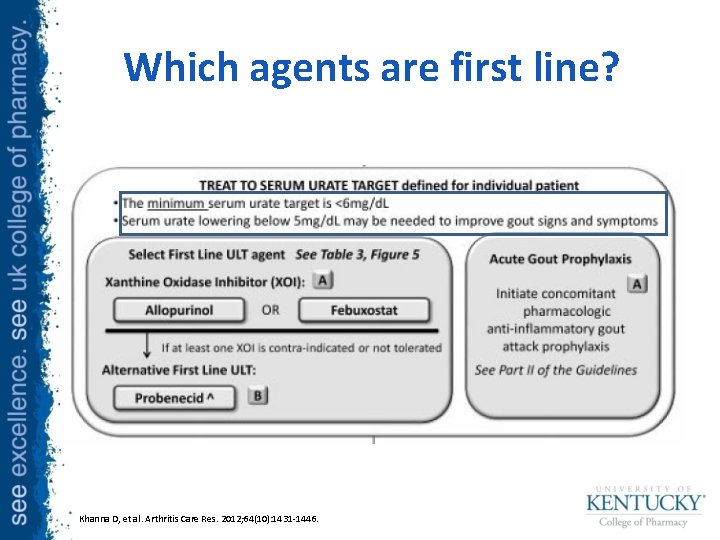
Which agents are first line? Khanna D, et al. Arthritis Care Res. 2012; 64(10): 1431 -1446.
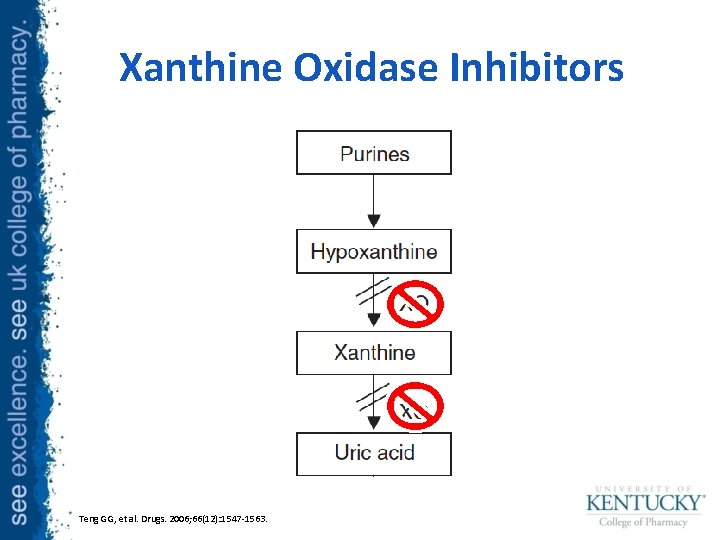
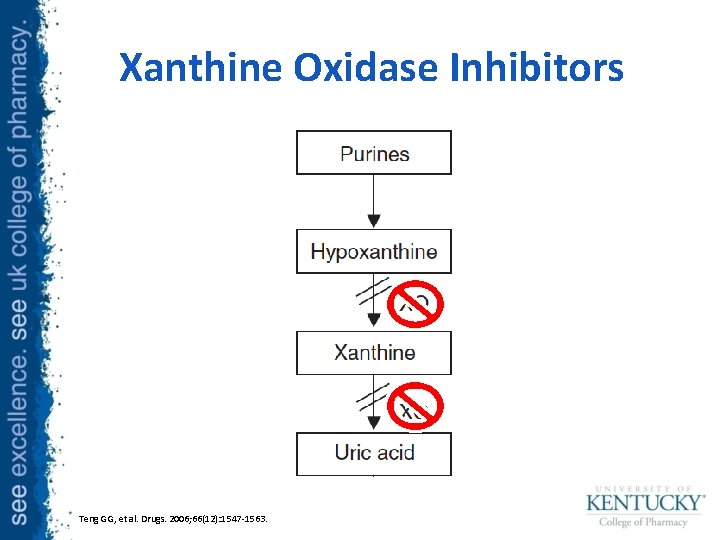
Xanthine Oxidase Inhibitors Teng GG, et al. Drugs. 2006; 66(12): 1547 -1563.
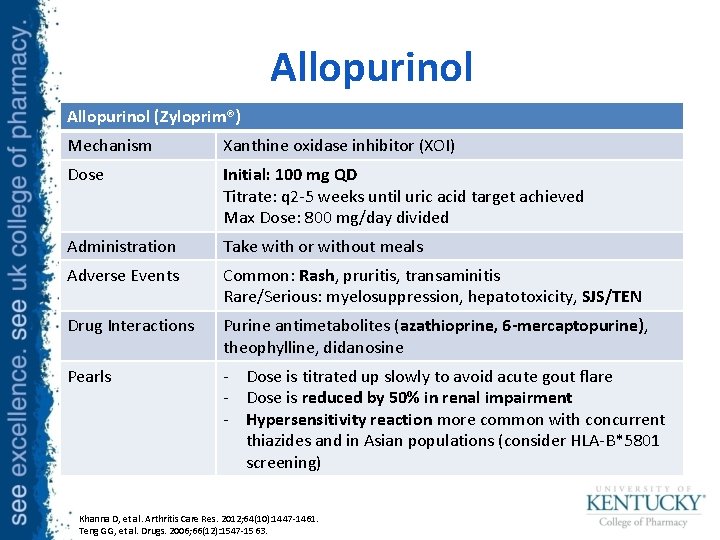
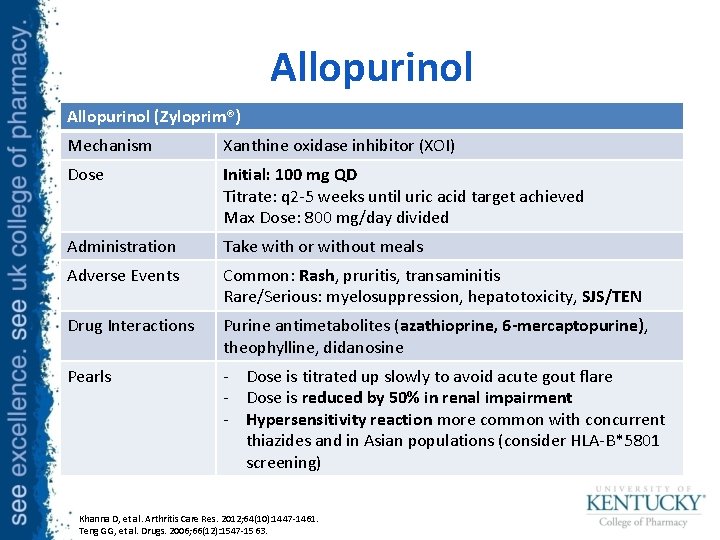
Allopurinol (Zyloprim®) Mechanism Xanthine oxidase inhibitor (XOI) Dose Initial: 100 mg QD Titrate: q 2 -5 weeks until uric acid target achieved Max Dose: 800 mg/day divided Administration Take with or without meals Adverse Events Common: Rash, pruritis, transaminitis Rare/Serious: myelosuppression, hepatotoxicity, SJS/TEN Drug Interactions Purine antimetabolites (azathioprine, 6 -mercaptopurine), theophylline, didanosine Pearls - Dose is titrated up slowly to avoid acute gout flare - Dose is reduced by 50% in renal impairment - Hypersensitivity reaction more common with concurrent thiazides and in Asian populations (consider HLA-B*5801 screening) Khanna D, et al. Arthritis Care Res. 2012; 64(10): 1447 -1461. Teng GG, et al. Drugs. 2006; 66(12): 1547 -1563.
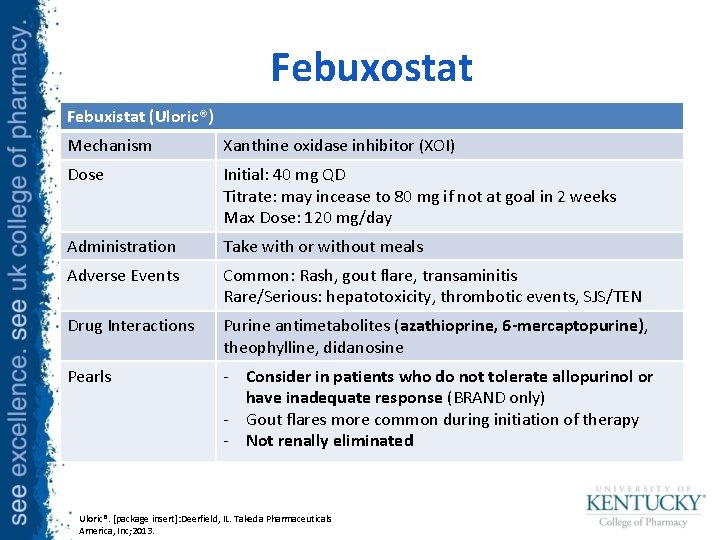
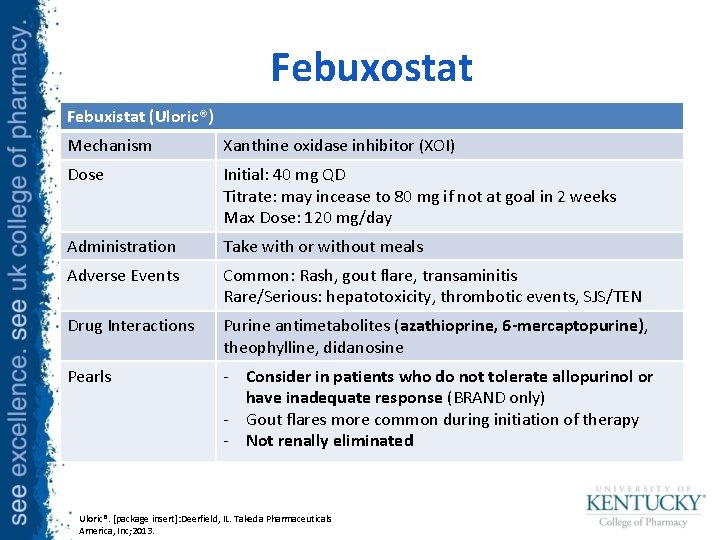
Febuxostat Febuxistat (Uloric®) Mechanism Xanthine oxidase inhibitor (XOI) Dose Initial: 40 mg QD Titrate: may incease to 80 mg if not at goal in 2 weeks Max Dose: 120 mg/day Administration Take with or without meals Adverse Events Common: Rash, gout flare, transaminitis Rare/Serious: hepatotoxicity, thrombotic events, SJS/TEN Drug Interactions Purine antimetabolites (azathioprine, 6 -mercaptopurine), theophylline, didanosine Pearls - Consider in patients who do not tolerate allopurinol or have inadequate response (BRAND only) - Gout flares more common during initiation of therapy - Not renally eliminated Uloric®. [package insert]: Deerfield, IL. Takeda Pharmaceuticals America, Inc; 2013.
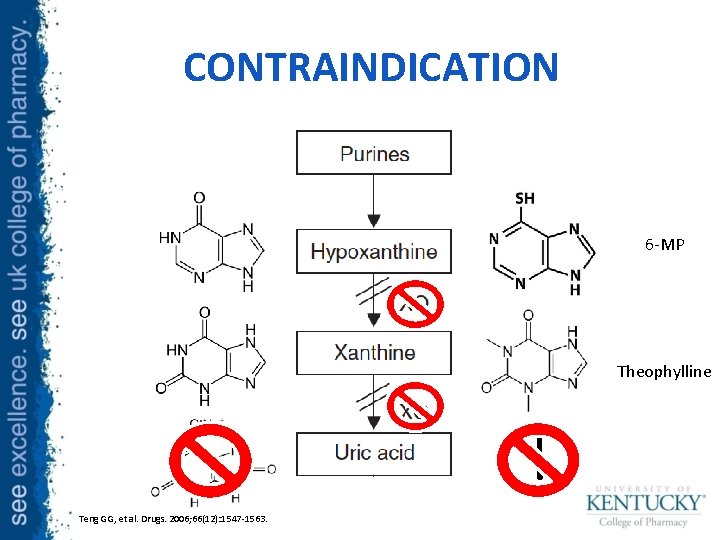
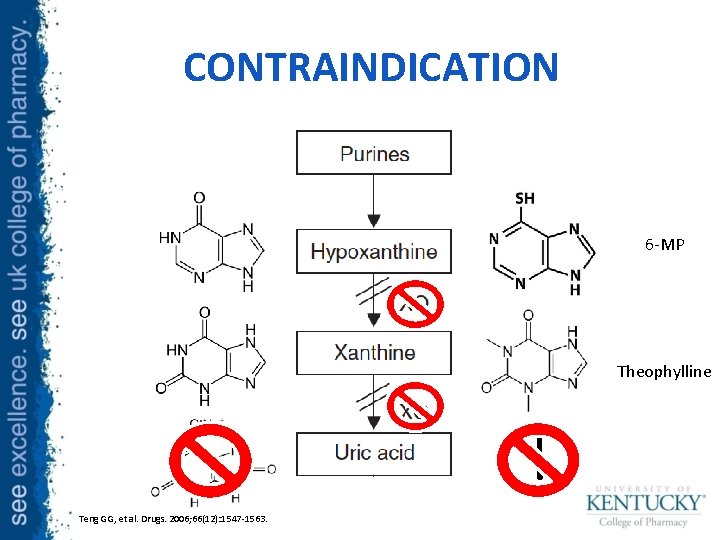
CONTRAINDICATION 6 -MP Theophylline Teng GG, et al. Drugs. 2006; 66(12): 1547 -1563.
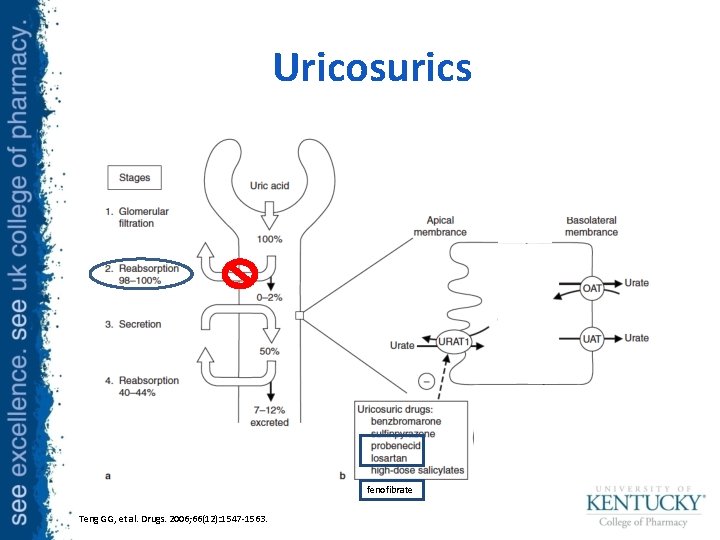
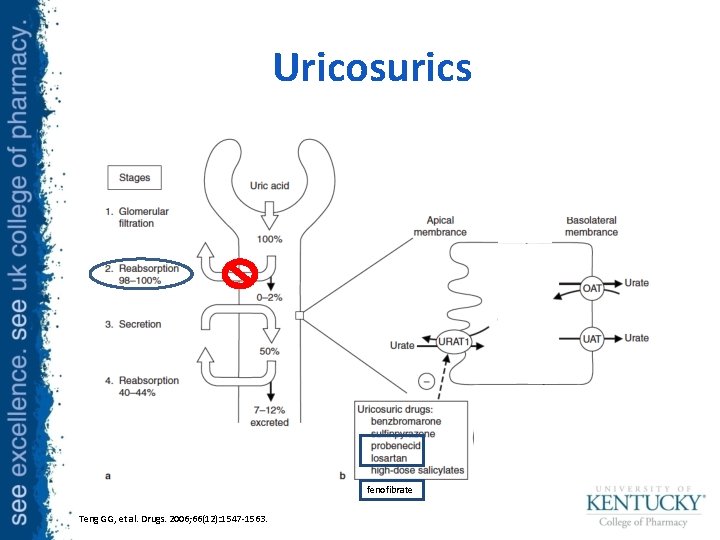
Uricosurics fenofibrate Teng GG, et al. Drugs. 2006; 66(12): 1547 -1563.
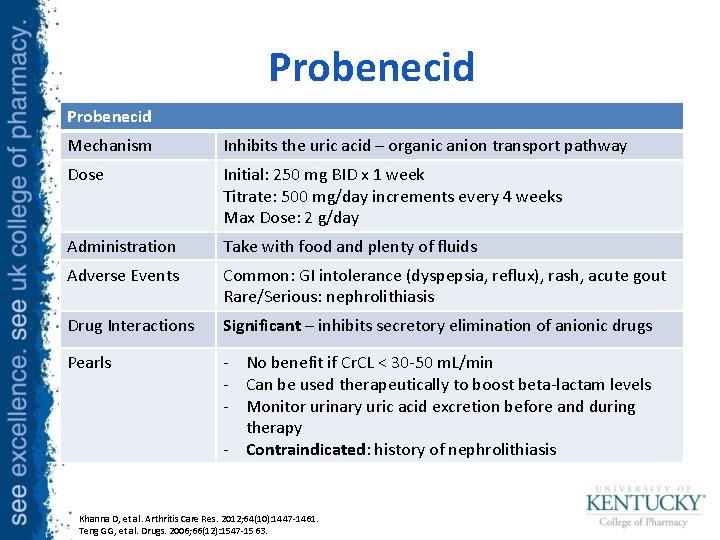
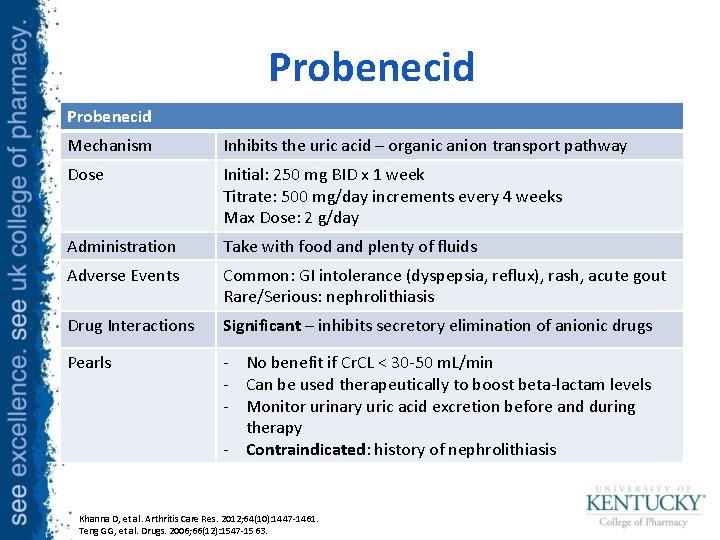
Probenecid Mechanism Inhibits the uric acid – organic anion transport pathway Dose Initial: 250 mg BID x 1 week Titrate: 500 mg/day increments every 4 weeks Max Dose: 2 g/day Administration Take with food and plenty of fluids Adverse Events Common: GI intolerance (dyspepsia, reflux), rash, acute gout Rare/Serious: nephrolithiasis Drug Interactions Significant – inhibits secretory elimination of anionic drugs Pearls - No benefit if Cr. CL < 30 -50 m. L/min - Can be used therapeutically to boost beta-lactam levels - Monitor urinary uric acid excretion before and during therapy - Contraindicated: history of nephrolithiasis Khanna D, et al. Arthritis Care Res. 2012; 64(10): 1447 -1461. Teng GG, et al. Drugs. 2006; 66(12): 1547 -1563.
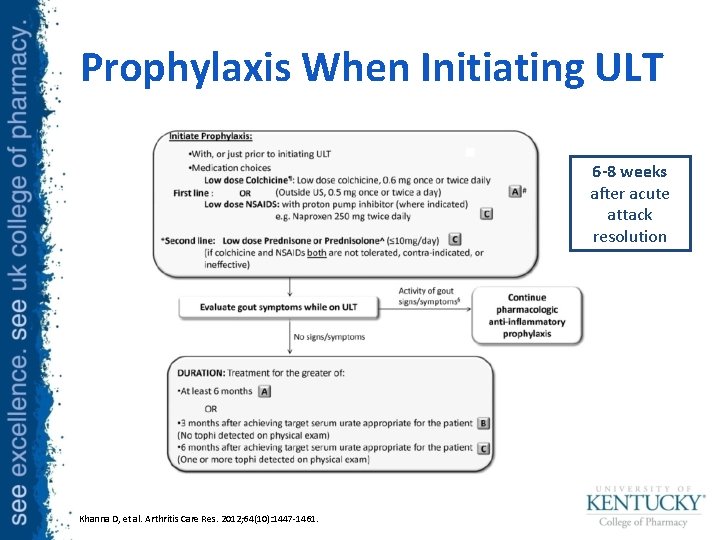
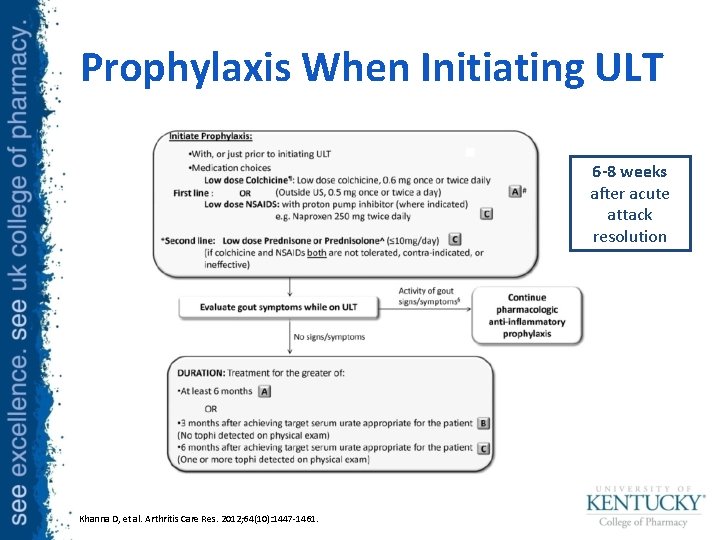
Prophylaxis When Initiating ULT 6 -8 weeks after acute attack resolution Khanna D, et al. Arthritis Care Res. 2012; 64(10): 1447 -1461.
Treatment-Resistant Gout • Referral to a rheumatologist – Refractory signs and symptoms – Difficulty reaching serum uric acid target, particularly with renal impairment and trial of XOI – Multiple/serious adverse effects to treatment Khanna D, et al. Arthritis Care Res. 2012; 64(10): 1431 -1446.
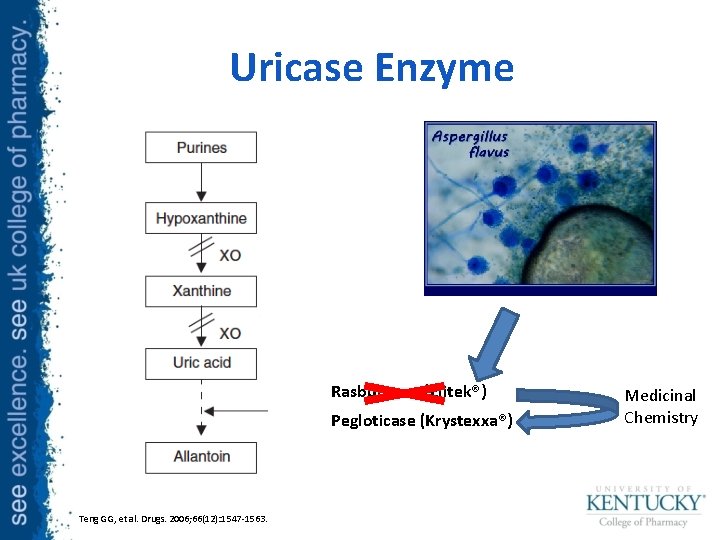
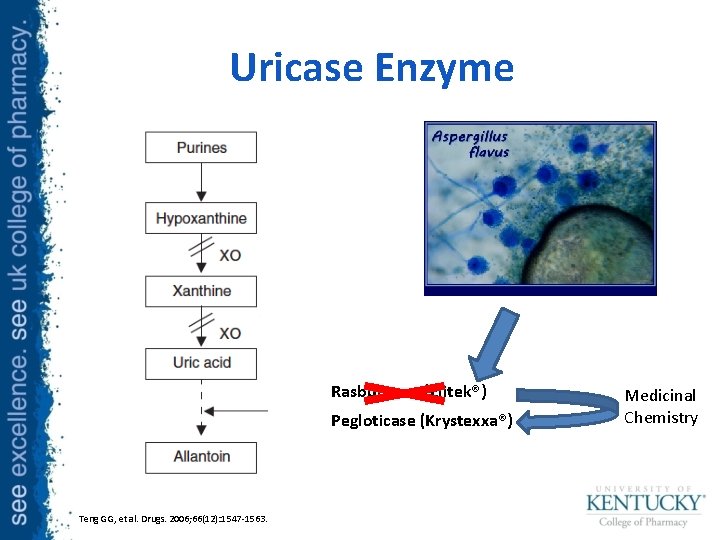
Uricase Enzyme Rasburicase (Elitek®) Pegloticase (Krystexxa®) Teng GG, et al. Drugs. 2006; 66(12): 1547 -1563. Medicinal Chemistry
Hot Off the Press http: //www. fda. gov/News. Events/Newsroom /Press. Announcements/ucm 478791. htm
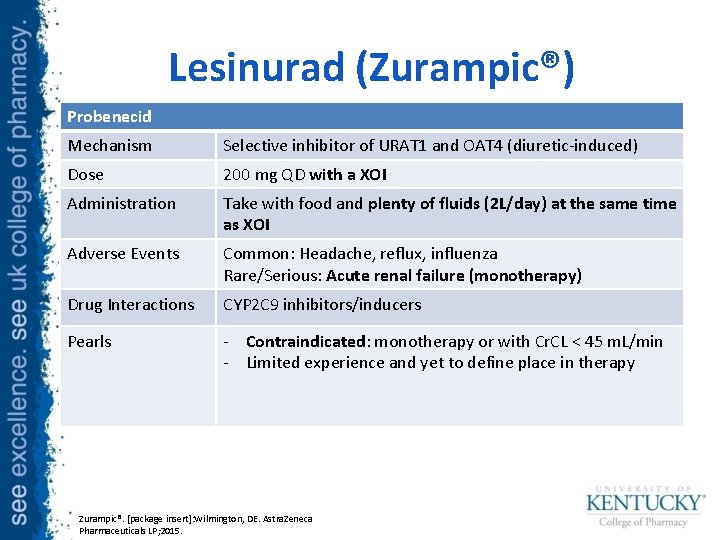
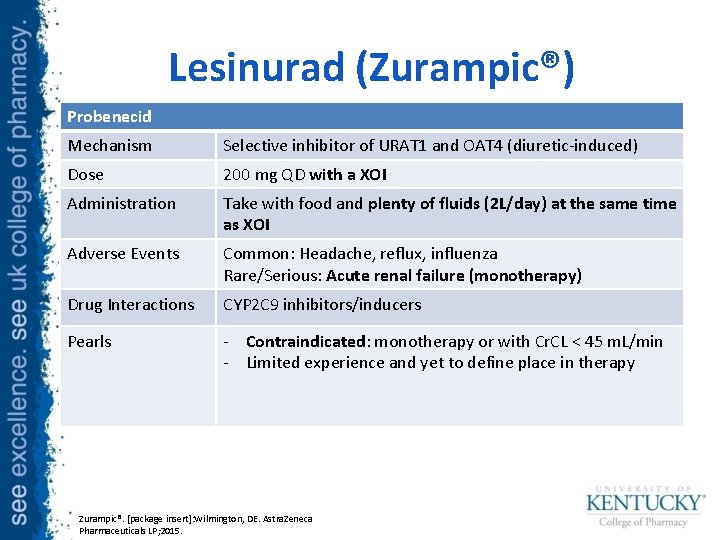
Lesinurad (Zurampic®) Probenecid Mechanism Selective inhibitor of URAT 1 and OAT 4 (diuretic-induced) Dose 200 mg QD with a XOI Administration Take with food and plenty of fluids (2 L/day) at the same time as XOI Adverse Events Common: Headache, reflux, influenza Rare/Serious: Acute renal failure (monotherapy) Drug Interactions CYP 2 C 9 inhibitors/inducers Pearls - Contraindicated: monotherapy or with Cr. CL < 45 m. L/min - Limited experience and yet to define place in therapy Zurampic®. [package insert]: Wilmington, DE. Astra. Zeneca Pharmaceuticals LP; 2015.
Summary: Urate Lowering Therapy • Maintenance ULT is indicated in significant disease burden and renal comorbidities • Xanthine oxidase inhibitors are the mainstay of therapy to target uric acid levels of at least < 6 mg/d. L • Uricosuric agents are alternatives to XOIs and useful adjuncts in resistant disease
Take Away Points • Gout is a common rheumatic disease that can be largely “cured” with pharmacotherapy • Medication selection during acute attacks should be guided by patient-specific factors • Maintenance ULT is largely well tolerated by some significant drug-drug interactions exist and most medications should be adjusted for renal dysfunction
Patient Case • Doran Martell is a 58 YOM with PMHx HTN, HLD, T 2 DM, DVT who presents with a chief complaint of swelling and excruciating pain in his right foot.
Patient Case • Doran Martell supplies the following history – Diet: Eats shellfish frequently due to proximity to the sea, red meat on weekends – Et. OH: Drinks 3 -4 ales/day – Exercise: Little physical activity
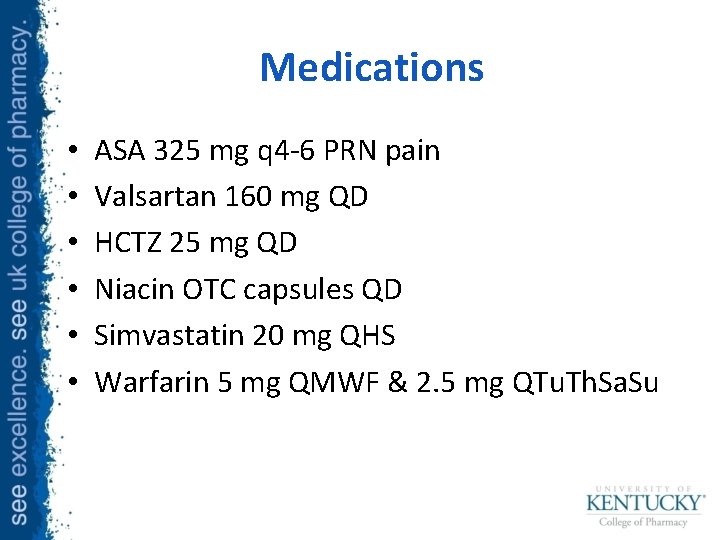
Medications • • • ASA 325 mg q 4 -6 PRN pain Valsartan 160 mg QD HCTZ 25 mg QD Niacin OTC capsules QD Simvastatin 20 mg QHS Warfarin 5 mg QMWF & 2. 5 mg QTu. Th. Sa. Su
Patient Counseling • What modifiable risk factors could you counsel this patient on? • Which medications may exacerbate gout?
Physical Exam Findings Erythema, tenderness, and swelling in the right great toe
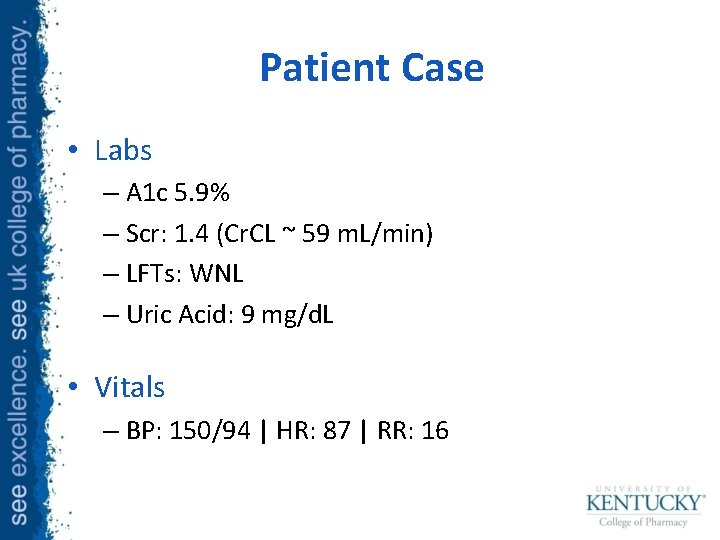
Patient Case • Labs – A 1 c 5. 9% – Scr: 1. 4 (Cr. CL ~ 59 m. L/min) – LFTs: WNL – Uric Acid: 9 mg/d. L • Vitals – BP: 150/94 | HR: 87 | RR: 16
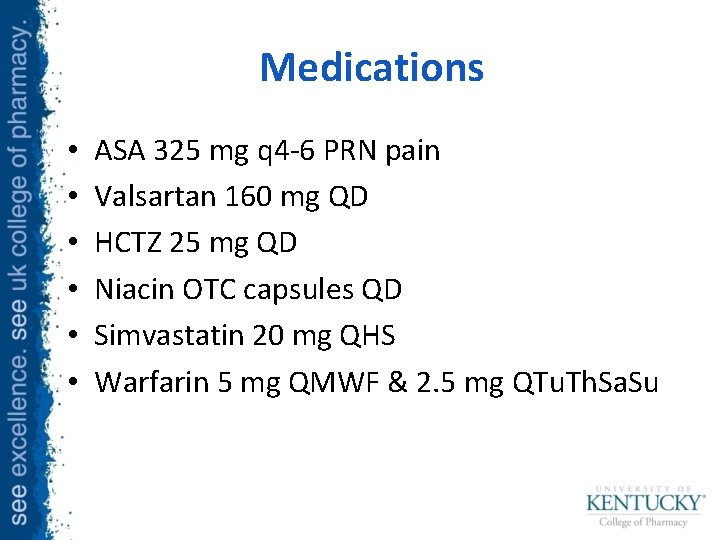
Medications • • • ASA 325 mg q 4 -6 PRN pain Valsartan 160 mg QD HCTZ 25 mg QD Niacin OTC capsules QD Simvastatin 20 mg QHS Warfarin 5 mg QMWF & 2. 5 mg QTu. Th. Sa. Su
Patient Case • With your neighbor discuss: – Which laboratory/physical exam findings are consistent with acute gout? – Which medication(s) you want initiate for Doran Martell’s acute gout attack? Why?
Patient Case • One year later, Prince Doran returns to clinic for follow up (he was swept away in wars and intrigue and missed his other follow ups). This is his physical exam today:
Patient Case • He is asymptomatic but has tophi on examination. He has made the dietary and lifestyle modifications you discussed previously. What therapy would you like to initiate?
Questions?
 Pharmacotherapy workup
Pharmacotherapy workup Pharmacotherapy
Pharmacotherapy Pharmacotherapy
Pharmacotherapy Habit in human acts
Habit in human acts Crass
Crass Crass
Crass Pharm d means
Pharm d means Ambio pharm
Ambio pharm Pharm gkb
Pharm gkb Library.med.utah.edu/kw/pharm/hyper heart.html
Library.med.utah.edu/kw/pharm/hyper heart.html Klucel exf pharm
Klucel exf pharm Pharm406
Pharm406 Purdue retail pharmacy
Purdue retail pharmacy Secur pharm
Secur pharm Library.med.utah.edu/kw/pharm/hyper heart.html
Library.med.utah.edu/kw/pharm/hyper heart.html Pharm
Pharm Bc bio-pharm
Bc bio-pharm Pharm degree
Pharm degree Outfield pharm
Outfield pharm Pharm id
Pharm id Pharmlinks
Pharmlinks Pharm
Pharm Sakita 1m45
Sakita 1m45 Underweight pes statement
Underweight pes statement Gout
Gout Gout treatment
Gout treatment Spinal dysraphism
Spinal dysraphism Gout criteria
Gout criteria Analglesia
Analglesia Hydrocodone and gout
Hydrocodone and gout Kode icd 10 dystonia
Kode icd 10 dystonia Over the counter gout medication boots
Over the counter gout medication boots Anatomi fisiologi asam urat
Anatomi fisiologi asam urat 2015 gout classification criteria
2015 gout classification criteria Gout
Gout Gout
Gout Nursing diagnosis of gout
Nursing diagnosis of gout Dr ryan fernandes
Dr ryan fernandes Thinkers keys examples
Thinkers keys examples Ryan o'donnell cmu
Ryan o'donnell cmu Marta ryan
Marta ryan Svxc turkey chase
Svxc turkey chase Ryan varick
Ryan varick Ryan gorski
Ryan gorski Deci en ryan
Deci en ryan Tidal energy assignment
Tidal energy assignment Ryan weiler
Ryan weiler Ryan dombrowski
Ryan dombrowski Ryan van wyk at&t
Ryan van wyk at&t