Drugs in Gout uric acid Gout Rx of

- Slides: 66
Drugs in Gout ↑ uric acid → Gout Rx of gout: 1. Rx of acute attack Colchicine, orally 2. Control of ↑ uric acid levels by: a. ↑ excretion of uric acid Uricosuric agents: Pobenecid, given orally; Sulphinpyrazone, given orally
b. ↓ uric acid synthesis: Allopurinol, given orally MOA: Inhibition of the enzyme xanthine oxidase Hypoxanthine acid xanthine oxidase xanthine uric
Hypnotics Sleep producing drugs Major clinical uses: Insomnia (inability to sleep)… could be due to: anxiety, depression, disease, pain or excessive drinking of coffee or tea
Chloral hydrate Given orally Considered safe drug Has an unpleasant taste Widely used in children and old people with insomnia Dosage forms: Caps. & Syrup
Paraldehyde Given orally, rectally or I. M Has mild hypnotic effect May be used in patients with status epilepticus to quieten the patient Chlormethiazole Related to Vit. B 1. Effective sedative-hypnotic used in old patients to control alcohol withdrawal symptoms Given orally & I. V. It may lead to addiction
Antihistamines e. g. Promethazine… Produce sedation May be used as hypnotics in children Major side effect: Anticholinergic side effects e. g. dry mouth, blurred vision…
Benzodiazepines Diazepam; Nitrazepam; Lorazepam; Temazepam. . . Known as minor sedatives Have long t 1/2 and active metabolites Relatively safe and usually given orally M. O. A: ↑ GABA levels in the brain (an inhibitory neurotransmitter) They lead to addiction Temazepam has short t 1/2 and does not produce active metabolites
Zopiclone Has similar M. O. A to benzodiazepines but has different structure Given orally Has short t 1/2 It may lead to addiction
Barbiturates e. g. Phenobarbitone; Secobarbital… No more used as hypnotics because of their great potential to produce addiction and fatal withdrawal manifestations Phenobarbitone is an inducer (universal) to drug metabolism and has antiepileptic effect Barbiturates are used before general anaesthesia
Drugs used in psychiatry I. Drugs in schizophrenia (psychosis) Neuroleptics; major tranquilizers; antipsychotics Biochemical defect: Excess dopamine in certain areas of the CNS Diagnosis depends mainly on clinical manifestations Management: ↓ dopamine levels in CNS
1. Phenothiazines Chlopromazine; Promazine; Thioridazine; Fluphenazine… n General effects: - Block dopamine receptors in the brain - Have antipsychotic effect - Produce sedation - Have antiemetic effect
- Have anticholinergic effect - Some block α-adrenergic receptors → postural hypotension - They lead to addiction Phenothiazines are effective orally & parenterally n Clinical uses: - Schizophrenia - Vomiting (Chlorpromazine) - Persistent hiccup (Chlorpromazine)
Phenothiazines side effects: - Parkinsonian- like syndrome; extrapyramidal signs and symptoms (major limitation in their use) - Sedation - Allergy - Jaundice especially with Chlorpromazine - Weight gain and postural hypotension - Anticholinergic effect (dry mouth; blurred vision…) n
2. Thioxanthines e. g. Flupenthixol Similar to phenothiazines but produce less sedation 3. Buterophenones - Haloperidol… mainly used to treat schizophrenia and given orally & I. M - Droperidol… mainly used as an antiemetic before, during or after surgery
4. Other neuroleptics - Pimozide Produces less side effects than phenothiazines - Sulpiride - Clozapine. . .
II. Drugs in anxiety 1. Benzodiazepines (minor tranquillizers) Diazepam; Lorazepam; Medazolam; Clonazepam; Chlodiazepoxide. . . n Major effects: - Antianxiety-sedative effect - Hypnotic effect (larger doses) - Muscle relaxant effect (Diazepam) - Antiepepileptic (anticonvulsant) effect (Diazepam or Clonazepam given I. V in patients with status epilepticus)
Benzodiazepines have similar MOA but differ in DOA (t 1/2); metabolic fate. . . They are metabolized in the liver and some produce active metabolites n Side effects: - Sedation; drowsiness - Memory difficulties - Addiction
- Withdrawal manifestations which may include tremors; abdominal pain and insomnia - Benzodiazepines overdosage: Leads to respiratory depression → death R x: - Gastric lavage - Specific benzodiazepines antagonist Flumazenil I. V
2. β-blockers Have anxiolytic effect Widely used as an antianxiety agents (in stage phobia; before exam; overactive animals…) Reverse overactivity of sympathetic system that accompany anxiety They, unlike benzodiazepines, don’t lead to sedation or addiction
III. Drugs in depression (antidepressants) Common disorder Biochemical defect: Low levels of Noradrenaline (NE) or Serotonin(5 -HT) or both Diagnosis depends mainly on clinical manifestation Management: ↑ levels of NA (NE) and/or Serotonin
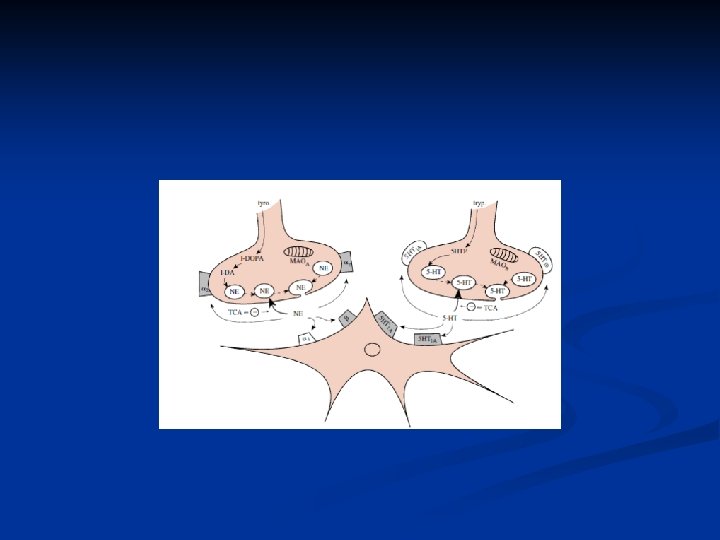
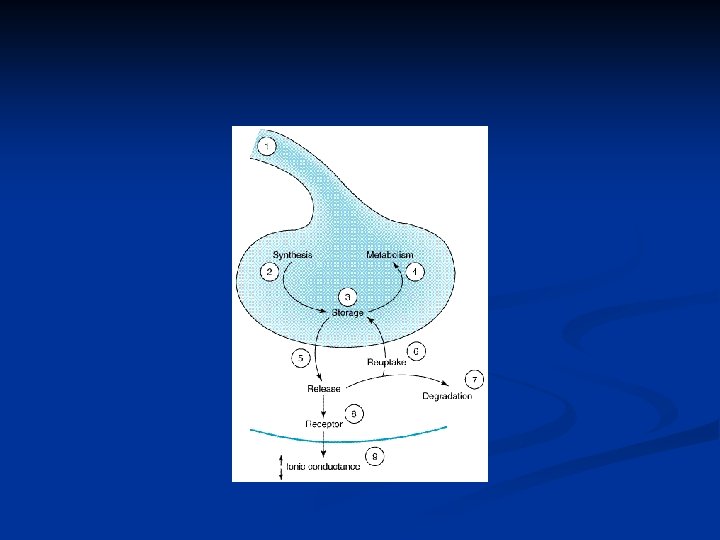
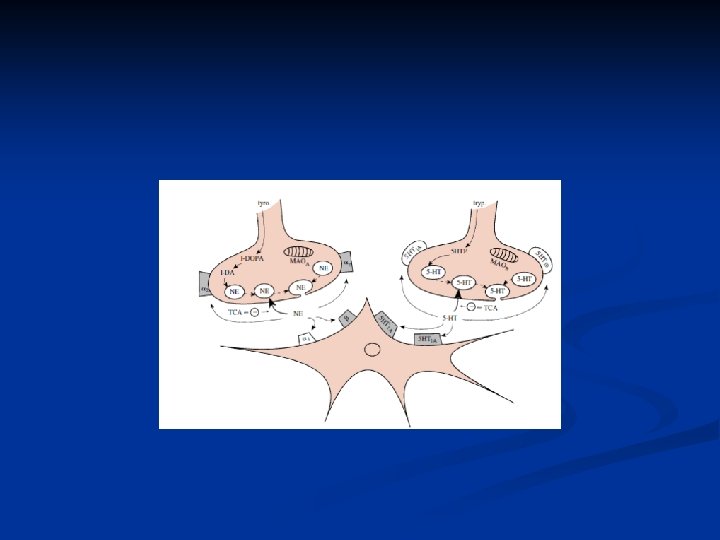
1. Tricyclic antidepressants(TCA’s): Imipramine; Amitriptyline; Nortriptyline… MOA: Inhibit reuptake of NA & serotonin (5 -HT) General effects: - Antidepressant effect - Sedative effect
Clinical uses to tricyclic antidepressants: - Depression - Nocturnal enuresis (Imipramine) Given orally n Side effects: - Anticholinergic effects - Postural hypotension - Depression of conduction in the heart - Addiction (dependence) - Weight gain n
2. Selective serotonin reuptake inhibitors (SSRI): Fluoxetine; Sertraline; Citalopram; Escitalopram; Paroxetine. . . Have similar efficacy to tricyclic antidepressants but produce no anticholinergic effects; no weight gain and no cardiotoxicity Given orally
3. Monoaminoxidase (MAO) inhibitors: Phenelzine; Isocarboxazid; Selegiline; Tranylcypromine ↓ breakdown of A; NA and serotonin Given orally n Side effects: - Insomnia - Jaundice
- Important interaction to MAO inhibitors: Cheese reaction or MAO + food containing tyramine (cheese; figs; wine; beer; liver. . . ) could lead to severe hypertensive crisis MAO inhibitors are contraindicated to be given with tricyclic antidepressants
4. Antianxiety antidepressants: Doxepin As compared to tricyclic antidepressants they have less antidepressant effect but better antianxiety action 5. Other antidepressants: Mianserine; Trazodone. . . MOA: ↑ NA release in the brain
6. Lithium carbonate: The drug of choice to treat manic depressive psychosis (a condition in between schizophrenia and depression) Has narrow therapeutic window (drug monitoring is important) Given orally n Side effects: - Hypothyroidism - Diabetes insipidus - Weakness; weight gain
General anaesthetics Drugs that produce reversible loss of consciousness, analgesia, muscle relaxation, and amnesia to perform general anaesthesia n Characteristics of an ideal anaesthetic: - Not to be an irritant to respiratory passages - To be rapidly acting (rapid induction) - To be acting long enough for duration required for the surgery - To have rapid recovery - To be free of side effects
Stages of anaesthesia: - Stage I: Stage of analgesia or induction stage Analgesia → loss of consciousness (analgesia; little muscle relaxation; impaired consciousness) - Stage II: Stage of delirium & excitement Loss of consciousness → rhythmic respiration n
- Stage III: Stage of surgical anaesthesia Rhythmic respiration → apnea - Stage IV: Stage of medullary paralysis Apnea → complete failure of circulation & loss of all vital signs A good general anaesthetic is that one which produces rapid induction (no differentiation into stages) & rapid recovery (occurs in reverse)
Preparation of the patient for surgery is important to avoid postoperative complications e. g. control of high B. P or diabetes or infection…etc and giving some drugs I. Preanaesthetic medications: 1. Anticholinergics Atropine, oral or I. M n
2. Analgesics Opioids; Morphine, I. M or Pethidine, I. M To ↓ pre- & postoperative pain and to ↓ dose of the general anaesthetic 3. Antianxiety agents Diazepam, oral or I. M or I. V 4. Antiemetic Droperidol, I. M
II. Muscle relaxants: Tubocurarine; Gallamine; Pancuronium… Given I. V before general anaesthetic and may be repeated during surgery III. Induction agents: I. V. anaesthetics a. Barbiturate anaesthetics Thiopentone sodium; Methohexitone. . .
- I. V barbiturates produce rapid induction or anaesthesia - They have long t 1/2 but their effects is terminated quickly by redistribution (getting out of the brain very quickly) - Highly lipid soluble drugs b. Nonbarbiturate I. V anaesthetics - Etomidate Has more rapid effect than barbiturates and produces no effect on B. P
- Propofol Produces rapid induction and recovery faster than any of the other induction agents It can be used as an I. V infusion to provide prolonged anaesthesia or sedation for hours or even days in intensive care wards
- Ketamine Unique induction agent effective I. V and I. M It has strong analgesic effect and produces superficial sleep (not complete sleep) This is known as “dissociative anaesthesia” (the patient can help during the anaesthesia) Widely used during burn dressing
Maintenance of anaesthesia=Inhalational anaesthesia - Gases. . . Nitrous oxide - Volatile liquids. . . Halothane; Desflurane; Enflurane; Isoflurane; Sevoflurane; Methoxyflurane. . . n Other drugs: - During anaesthesia: Neuroleptanalgesia or neuro leptanaesthesia (Neuroleptic=Droperidol + narcotic analgesic=Morphine or Fentanyl) - After anaesthesia: Pethidine; Promethazine; Bethanechol. . . n
MOA of general anaesthetics: Unclear; theories: - General anesthetic dissolve in neurones or cell membrane lipids → alter cell membrane function → expansion of membranes → ↑ threshold for cell firing → anaesthetic effect - ? Affect ionic (Na+; K+) movement - ? Interfere with membrane proteins or affect neurotransmitter release n
Dose of a general anaesthetic: Depends totally on the physical property of the GA & it is based on the partial pressure of the gas or volatile liquid & expressed in alveolar tension required at equilibrium to produce defined depth of anaesthesia n
Volatile liquid or gas ↓↑ Alveoli ↓↑ Blood CNS ↓↑ Tissues
Generally: - More lipid soluble GA’s are more potent - The more the blood solubility of a gas the slower the induction & recovery (GA’s with low blood : gas partition coefficient equilibrate quickly and enter readily the CNS) - MAC=Minimum Alveolar Concentration is another measure of potency and defined as the minimum concentration of GA in alveolar air needed to eliminate movement or produce immobility in 50% of patients exposed or challenged with standardized skin incision or a painful stimulus (the lower MAC the more potent the GA) n
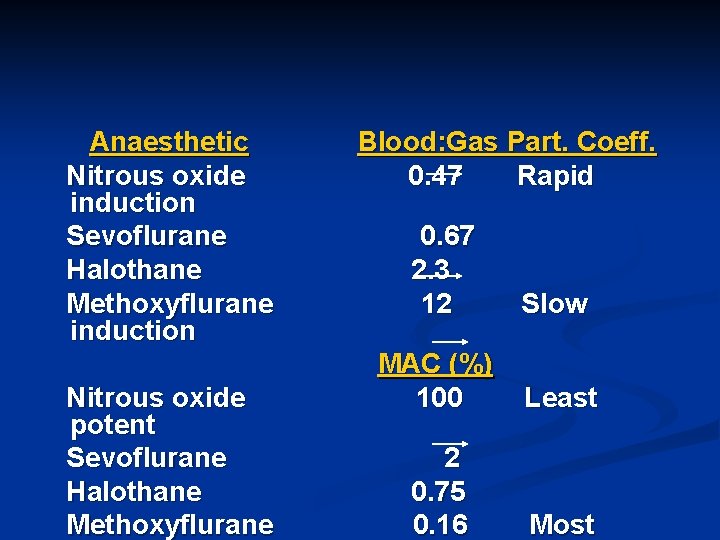
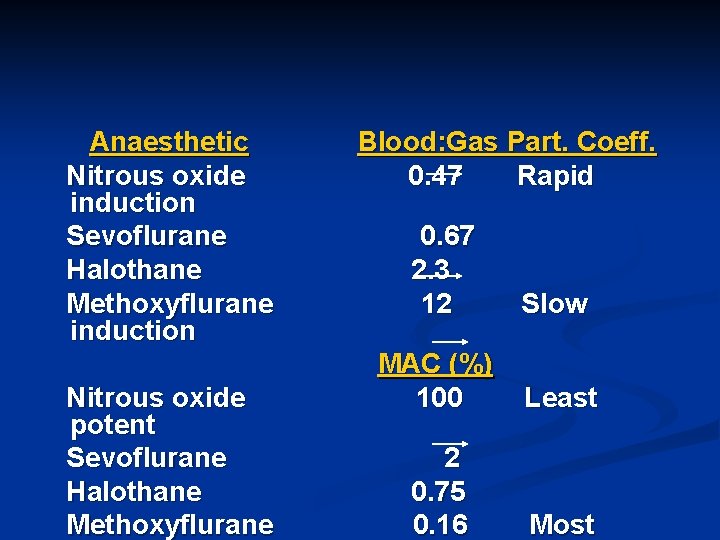
Anaesthetic Nitrous oxide induction Sevoflurane Halothane Methoxyflurane induction Nitrous oxide potent Sevoflurane Halothane Methoxyflurane Blood: Gas Part. Coeff. 0. 47 Rapid 0. 67 2. 3 12 Slow MAC (%) 100 Least 2 0. 75 0. 16 Most
IV. Maintenance of anaesthesia: 1. Inhalational anaesthesia a. Gases Nitrous oxide (N 2 O) Known as “laughing gas” because it leads to very rapid induction and recovery (advantage) Has good analgesic properties (advantage) but weak muscle relaxant effect (disadvantage)
Nitrous oxide is not potent and usually combined with other inhalational anaesthetic + muscle relaxant + antianxiety agent + hypnotic. . . etc This is known as “ balanced anaesthesia” Nitrous oxide side effects: Tissue hypoxia, so it is combined with O 2
b. Volatile liquids - Halothane Most widely used anaesthetic Not irritant to respiratory passages Analgesic effect is not strong n Side effects: - Hepatitis - Cardiac arrhythmias - Malignant hyperthermia
- Isoflurane Doesn’t lead to cardiac arrhythmia Leads to very rapid recovery Recently replaces halothane because it produces less side effects - Enflurane Similar to halothane but causes mild reversible renal tubular damage
2. Opioids Fentanyl Most widely used opioid to maintain anaesthesia Produces profound analgesia, sedation and in large doses hypnosis and respiratory depression (in this situation it is a useful effect) The action of opioids could be easily reversed by Naloxone
Drugs in epilepsy n Types of epilepsy: 1. Generalized seizures Grand mal- tonic-clonic Petit mal=absence seizures 2. Focal seizures Partial; psychomotor seizures
Antiepileptic or anticonvulsant drugs - Phenytoin Effective in all types of epilepsy except petit mal Drug of choice for Rx of grand mal epilepsy Also effective in Rx of trigeminal neuralgia Given orally; has narrow therapeutic window n Major side effects: - Hyperplasia of gums (most important) - Sedation, anemia, allergy
- Carbamazepine Similar to Phenytoin and has similar clinical uses n Side effects: - Dizziness - Leucopenia Given orally
- Phenobarbitone n Clinical uses: - Grand mal tonic-clonic convulsions - Febrile convulsions ↑ body temperature especially in children could lead to convulsions Recent management: Diazepam rectally to terminate seizures followed by Phenobarbitone to prevent recurrence of attacks
- Primidone; sodium Valproate Effective in grand mal and petit mal epilepsies - Vigabatrin; Lmotrigine Effective in focal and tonic-clonic seizures - Ethosuximide Drug of choice to treat petit mal epilepsy
Drugs in status epilepticus - Diazepam or Clonazepam I. V (drug of choice). In children given by a rectal tube - Phenytoin I. V to prevent relapse - Chlormethiazole I. V if above Rx fails - Thiopentone sodium I. V if above Rx fails n
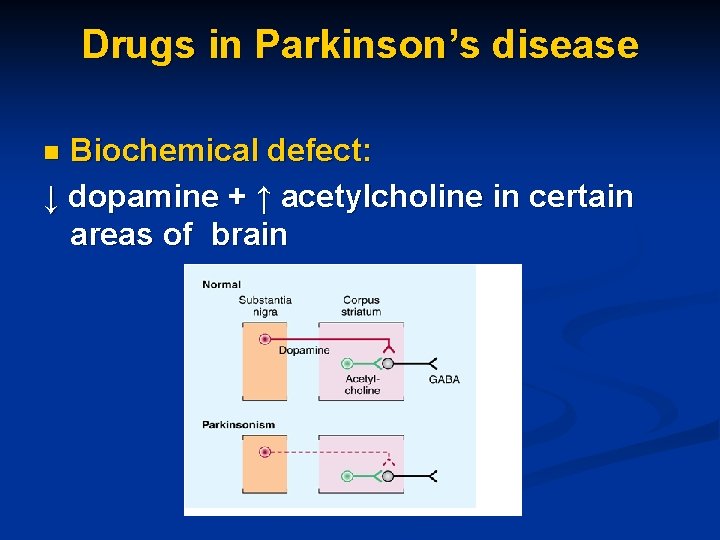
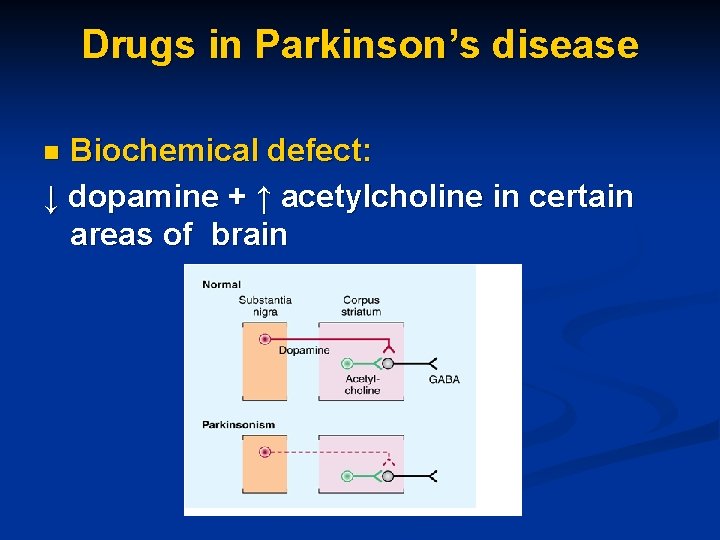
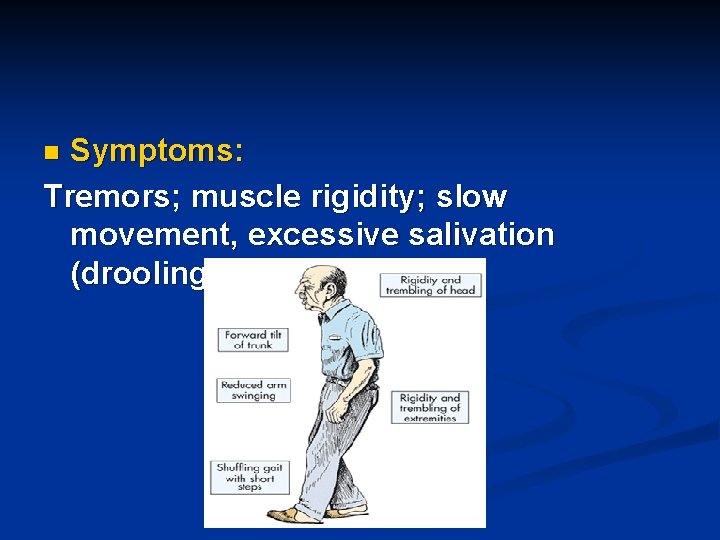
Drugs in Parkinson’s disease Biochemical defect: ↓ dopamine + ↑ acetylcholine in certain areas of brain n
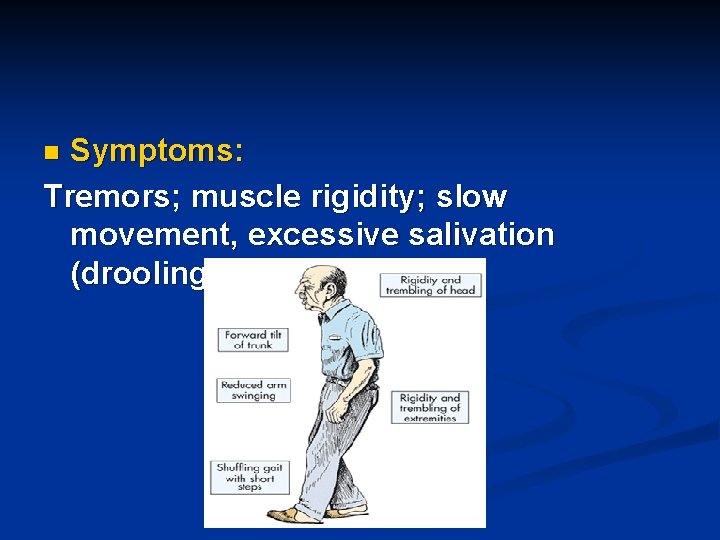
Symptoms: Tremors; muscle rigidity; slow movement, excessive salivation (drooling). . . n

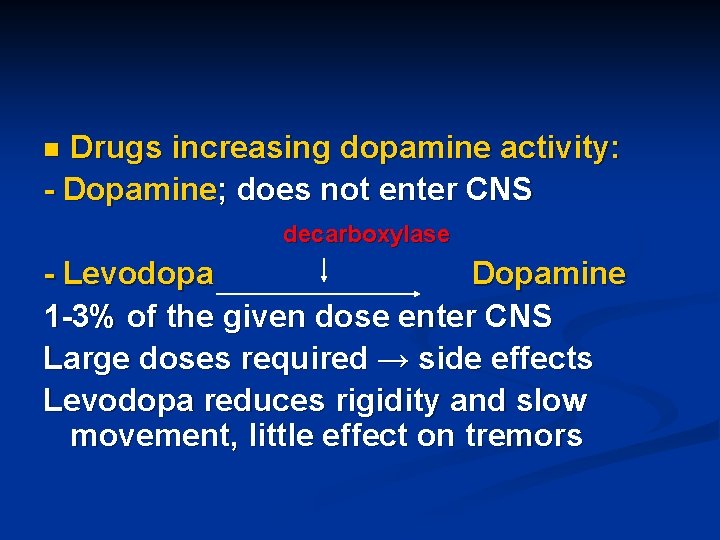
Treatment: ↑ dopamine + ↓ acetylcholine activities in brain n
Drugs decreasing cholinergic activity: - Benzhexol Synthetic Atropine-like drug given orally; relieves rigidity and tremors Has better effect on tremors - Benztropine Similar to atropine highly effective in relieving salivation n Side effects to anticholinergics: Dry mouth; constipation; blurred vision; urine retention hallucinations. . . n
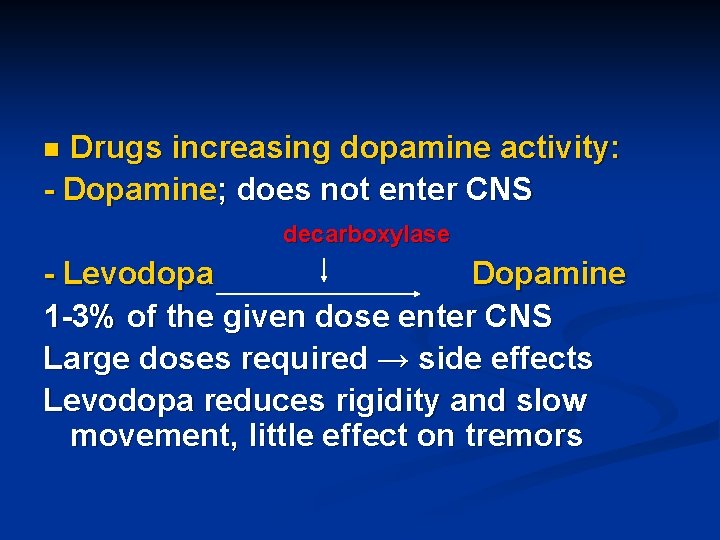
Drugs increasing dopamine activity: - Dopamine; does not enter CNS n decarboxylase - Levodopa Dopamine 1 -3% of the given dose enter CNS Large doses required → side effects Levodopa reduces rigidity and slow movement, little effect on tremors
Levodopa is an alpha, β 1 and D 2 (presynaptic inhibitory to NE release) agonist n Levodopa side effects: Nausea, vomiting, postural hypotension, tachycardia, extrasystoles, atrial fibrillation, hypertension with high doses or with MAO inhibitors n Levodopa interactions: Levodopa + Halothane ↑ risk of cardiac arrhythmias Levodopa should not be combined with MAO inhibitors (hypertension) n
- Levodopa + decarboxylase inhibitor: Levodopa + Carbidopa (Sinemet®) Levodopa + Benserazide (Madopar®) This combination allows the use of smaller doses of levodopa. Decarboxylase inhibitors do not enter CNS but inhibit peripheral conversion of levodopa to dopamine (10% of Levodopa dose enter CNS) so daily required dose of Levodopa is reduced by 75% and its peripheral toxicity is reduced
- Dopamine receptor agonists: Bromocriptine; Pergolide; Lysuride, Ropinirole… Have similar effects to Levodopa used if patients develop intolerance or resistance to Levodopa - Selegiline Specific selective DA-MAO inhibitor. Inhibits breakdown of DA. If combined with Levodopa, lower doses required - Entacapone; Tolcapone COMT inhibitors. Inhibit breakdown of DA; if combined with Levodopa they inhibit its peripheral metabolism and hence lower doses required
Amantadine Antiviral drug found to be effective in Parkinson’s disease Its effects are not due to its antiviral activity MAO: Unclear n β-blockers Relieve tremors could be used in Parkinson’s patients n Antihistamines Have anticholinergic effect could be used in Parkinson’s patients n
CNS stimulants Used in cases of respiratory depression irrespective of its causes, in addition to the use of other drugs + O 2 + suction to get rid of secretions in respiratory passages - Doxapram Given in an I. V infusion
- Methylxanthines Aminophylline; Theophylline Given orally and I. V Rarely used as respiratory stimulants; mainly used to manage bronchial asthma, pulmonary edema and bronchitis to relieve bronchospasm (good bronchodilators) - Caffeine A xanthine similar to Aminophylline but not used clinically