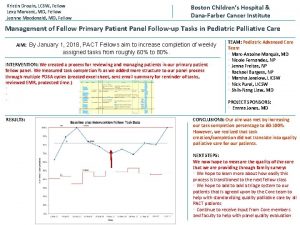
GI Grand Rounds Johanna Chan MD PGY6 Fellow









- Slides: 68
GI Grand Rounds Johanna Chan, MD PGY-6 Fellow, Gastroenterology Baylor College of Medicine 2/19/2014 Mentor: Joseph Sellin, MD
No conflicts of interest No financial disclosures
HPI Reason for consult: screening colonoscopy 50 yo Hispanic woman (originally from El Salvador) referred for screening colonoscopy Brother had colorectal cancer diagnosed in his mid-50’s No anemia, change in stool, constipation, diarrhea, nor blood in stool Remainder of GI ROS negative: no abdominal pain, dyspepsia, nausea, vomiting, weight loss, bloating, early satiety, etc.
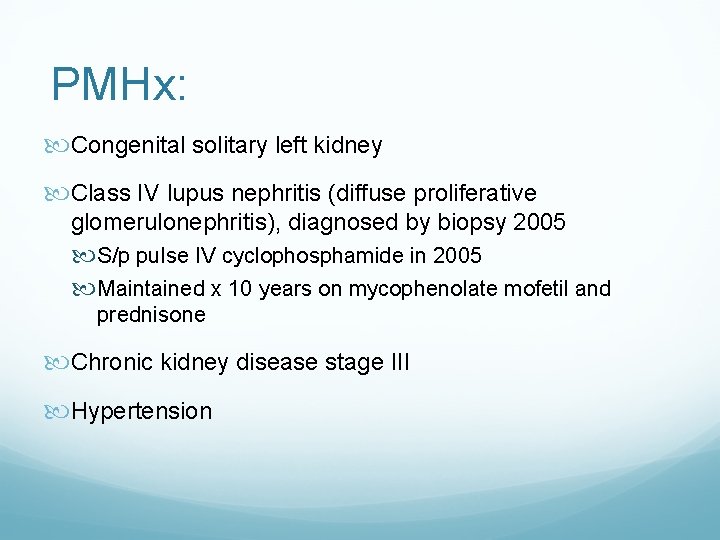
PMHx: Congenital solitary left kidney Class IV lupus nephritis (diffuse proliferative glomerulonephritis), diagnosed by biopsy 2005 S/p pulse IV cyclophosphamide in 2005 Maintained x 10 years on mycophenolate mofetil and prednisone Chronic kidney disease stage III Hypertension
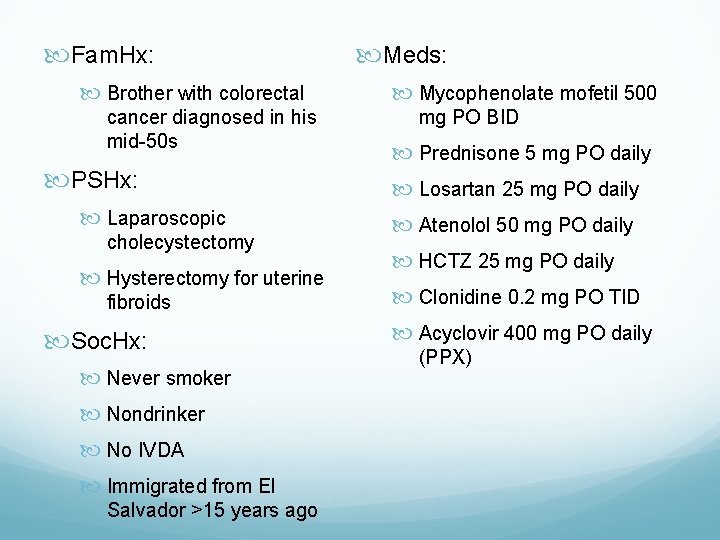
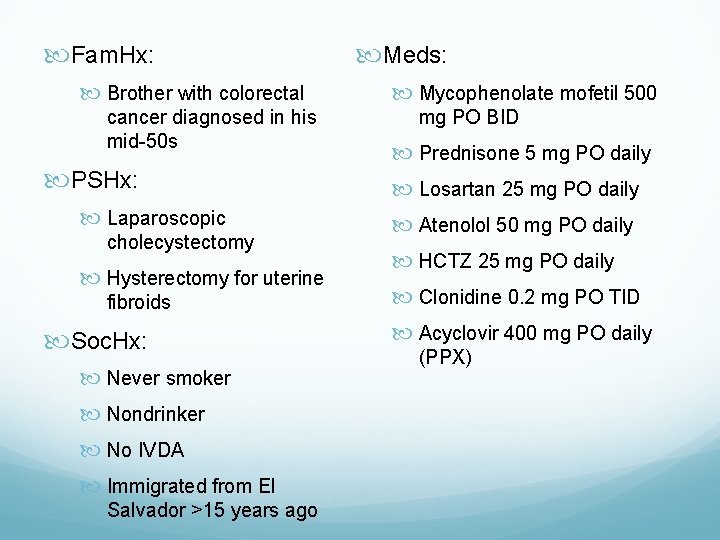
Fam. Hx: Brother with colorectal cancer diagnosed in his mid-50 s PSHx: Laparoscopic cholecystectomy Hysterectomy for uterine fibroids Soc. Hx: Never smoker Nondrinker No IVDA Immigrated from El Salvador >15 years ago Meds: Mycophenolate mofetil 500 mg PO BID Prednisone 5 mg PO daily Losartan 25 mg PO daily Atenolol 50 mg PO daily HCTZ 25 mg PO daily Clonidine 0. 2 mg PO TID Acyclovir 400 mg PO daily (PPX)
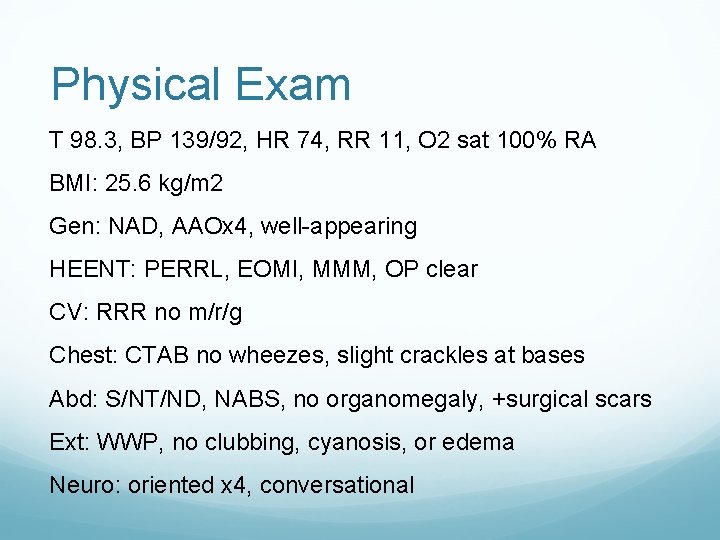
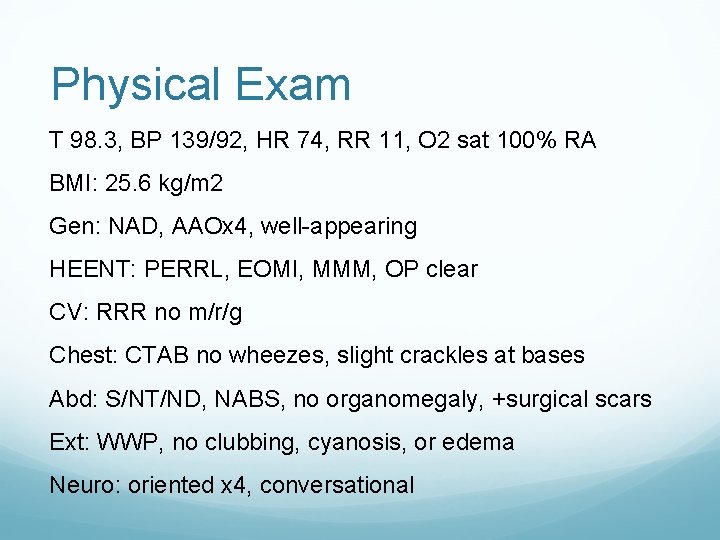
Physical Exam T 98. 3, BP 139/92, HR 74, RR 11, O 2 sat 100% RA BMI: 25. 6 kg/m 2 Gen: NAD, AAOx 4, well-appearing HEENT: PERRL, EOMI, MMM, OP clear CV: RRR no m/r/g Chest: CTAB no wheezes, slight crackles at bases Abd: S/NT/ND, NABS, no organomegaly, +surgical scars Ext: WWP, no clubbing, cyanosis, or edema Neuro: oriented x 4, conversational
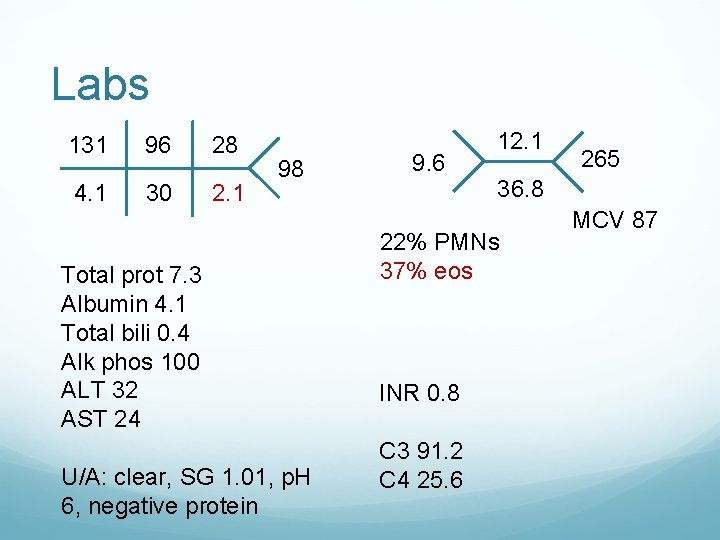
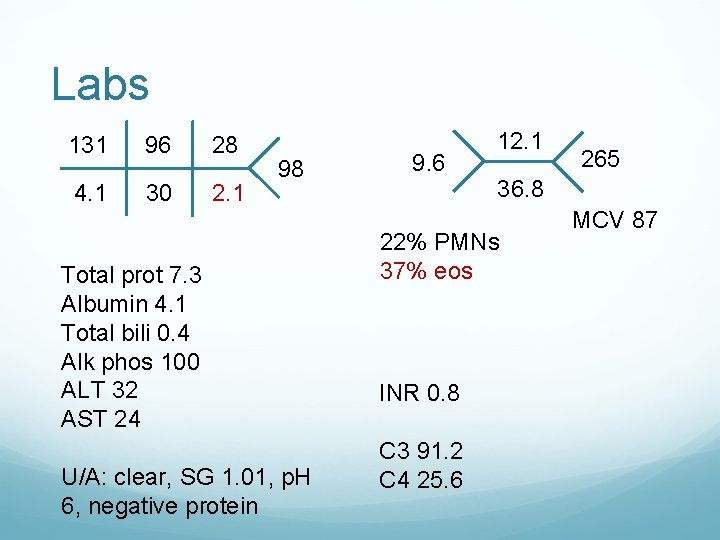
Labs 131 96 28 4. 1 30 2. 1 98 Total prot 7. 3 Albumin 4. 1 Total bili 0. 4 Alk phos 100 ALT 32 AST 24 U/A: clear, SG 1. 01, p. H 6, negative protein 9. 6 12. 1 36. 8 22% PMNs 37% eos INR 0. 8 C 3 91. 2 C 4 25. 6 265 MCV 87
Colonoscopy


Colonoscopy Patulous ileo-cecal valve Normal terminal ileum Diffuse nodularity throughout entire colon, with mild erythema and loss of vascularity Random biopsies in right colon, left colon, and rectum were taken and submitted separately
Biopsies
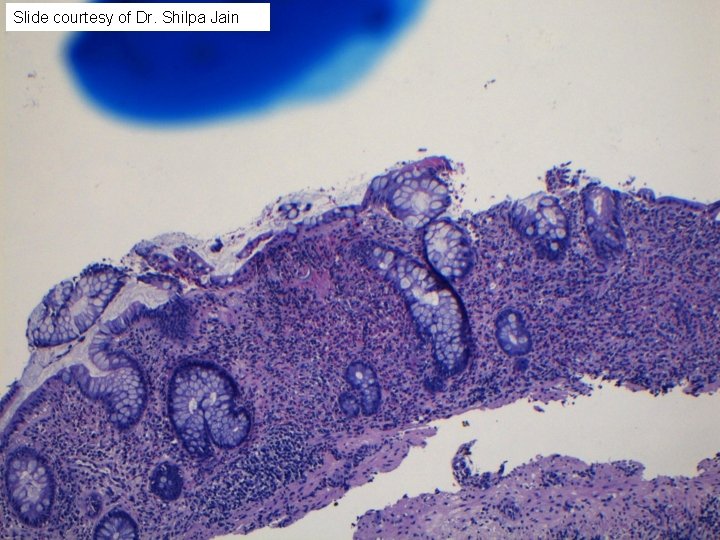
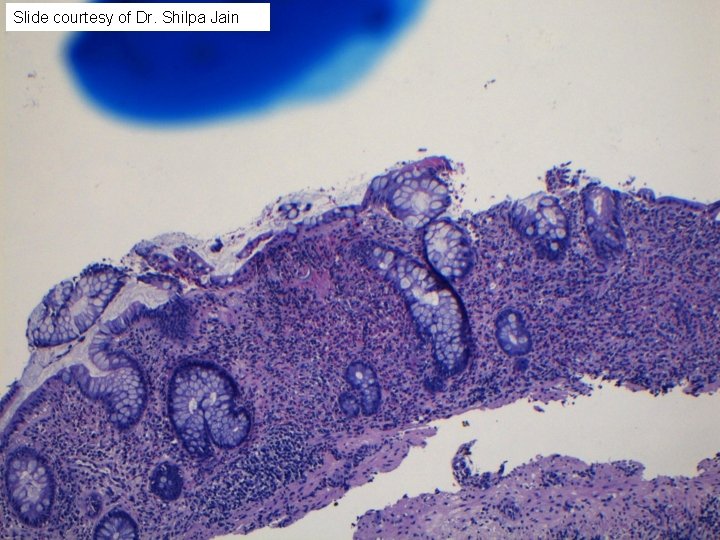
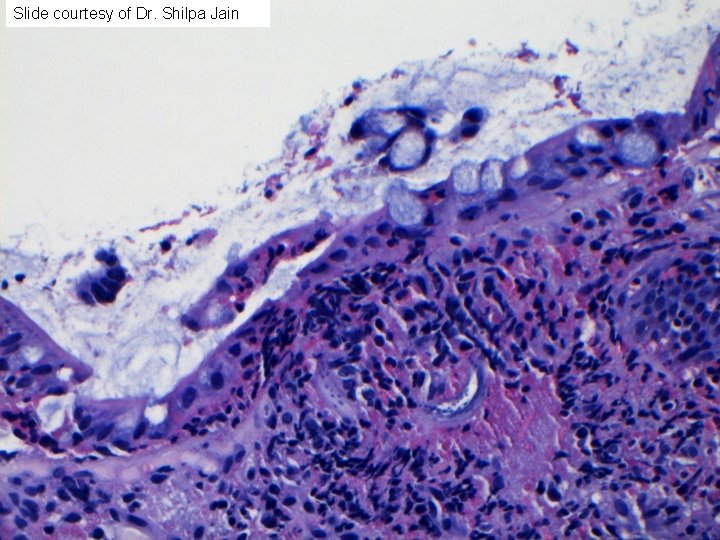
Slide courtesy of Dr. Shilpa Jain

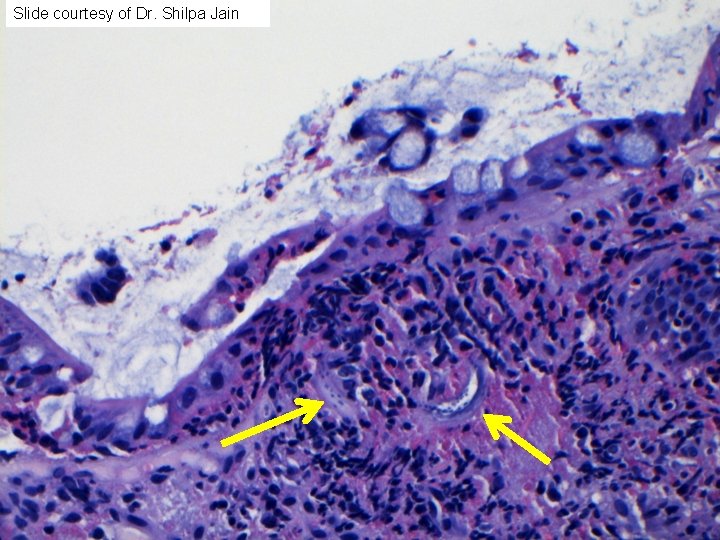
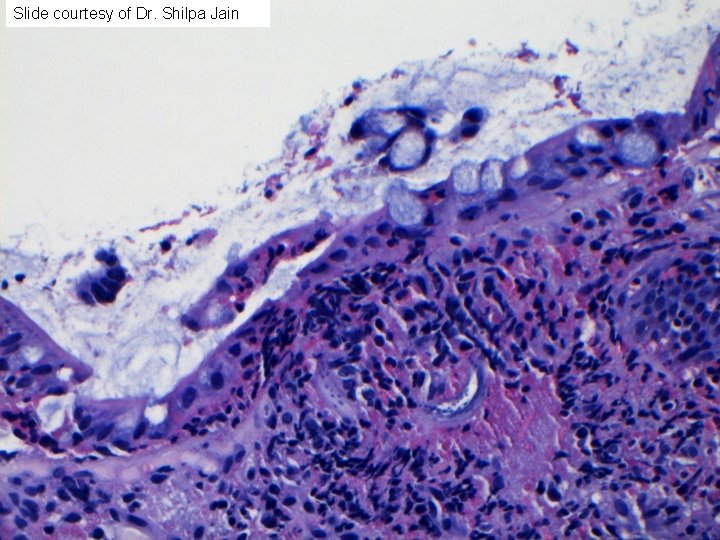
Slide courtesy of Dr. Shilpa Jain
Slide courtesy of Dr. Shilpa Jain
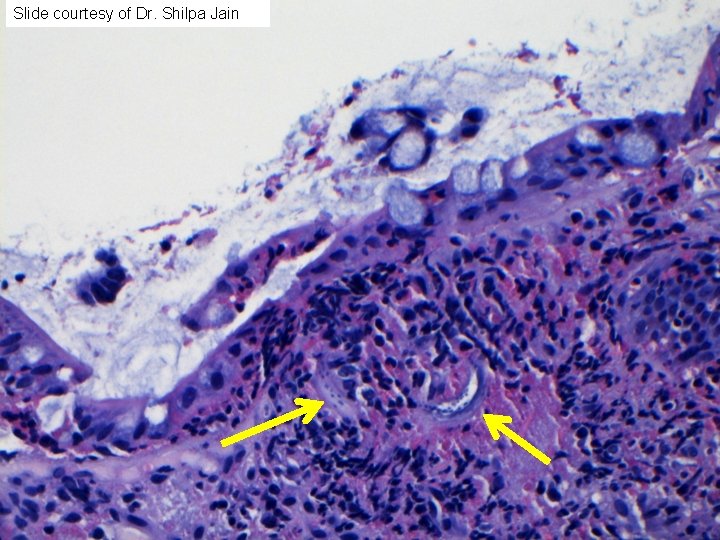
Slide courtesy of Dr. Shilpa Jain
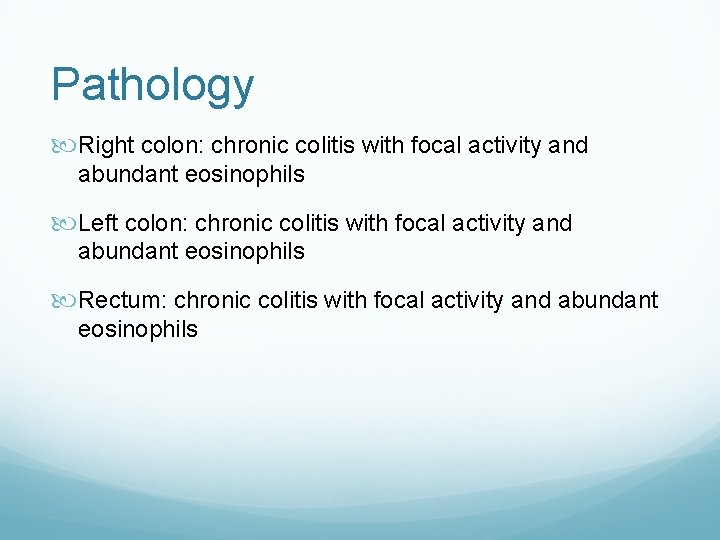
Pathology Right colon: chronic colitis with focal activity and abundant eosinophils Left colon: chronic colitis with focal activity and abundant eosinophils Rectum: chronic colitis with focal activity and abundant eosinophils
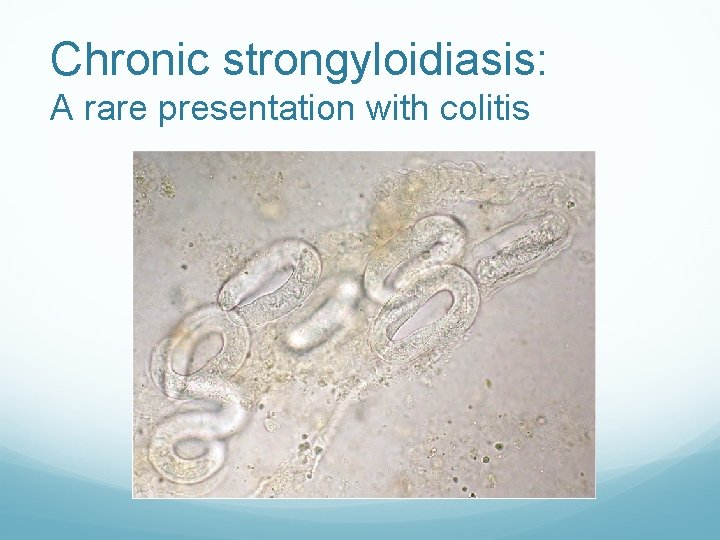
Pathology ADDENDUM (one week later) Colon, right, biopsies: An organism consistent with strongyloides larva is identified in the lamina propria on additional levels
Chronic strongyloidiasis: A rare presentation with colitis
Clinical questions Brief background review (epidemiology, S. stercoralis life cycle, and clinical presentation) What is the spectrum of endoscopic findings in strongyloidiasis? What are the available diagnostic modalities for S. stercoralis, and how do they compare? What is the optimal treatment and follow up for S. stercoralis?
Clinical questions Brief background review (epidemiology, S. stercoralis life cycle, and clinical presentation) What is the spectrum of endoscopic findings in strongyloidiasis? What are the available diagnostic modalities for S. stercoralis, and how do they compare? What is the optimal treatment and follow up for S. stercoralis?

Background
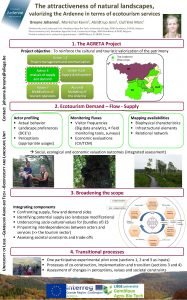
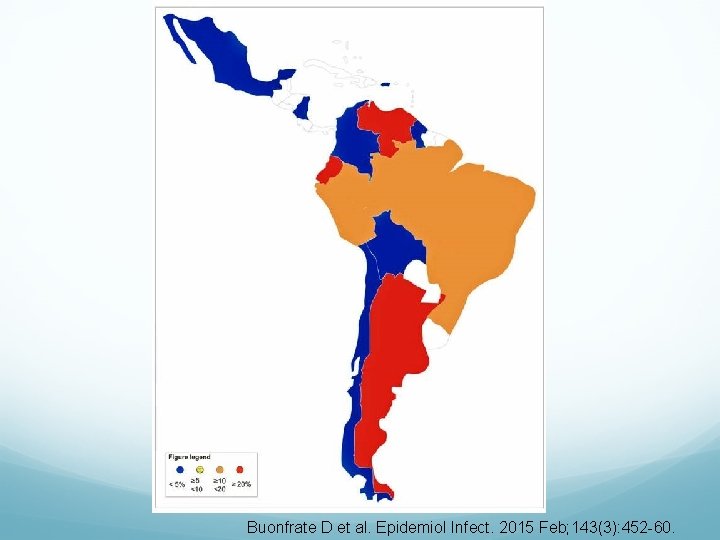
S. stercoralis epidemiology 30 to 100 million infected persons worldwide (likely underestimated) Endemic worldwide More prevalent in tropics and subtropics, especially in resource-poor countries with poor sanitation In U. S. : highest association with WW II veterans returning from Southeast Asia / South Pacific, immigrant populations, and rural Appalachia http: //www. cdc. gov/parasites/strongyloides/ Dreyer G et al. 1996 Oct; 34(10): 2569 -71. Greaves D. BMJ 2013 Jul 30; 347: f 4610. Mejia R, Nutman TB. Curr Opin Infect Dis. 2012 Aug; 25(4): 458 -63. Requena-Mendez A et al. PLo. S Negl Trop Dis. 2013; 7(1): e 2002. Schar et al. PLo. S Negl Trop Dis. 2014 Jun 12; 8(6): e 2854.

Schar et al. PLo. S Negl Trop Dis. 2014 Jun 12; 8(6): e 2854.
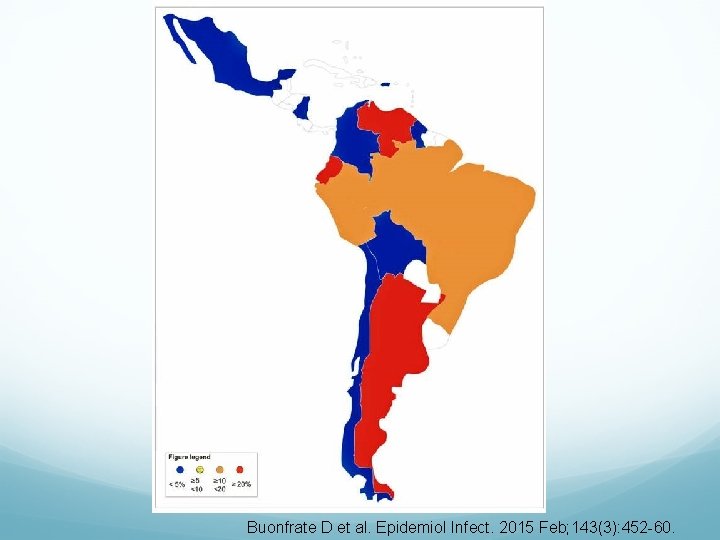
Buonfrate D et al. Epidemiol Infect. 2015 Feb; 143(3): 452 -60.
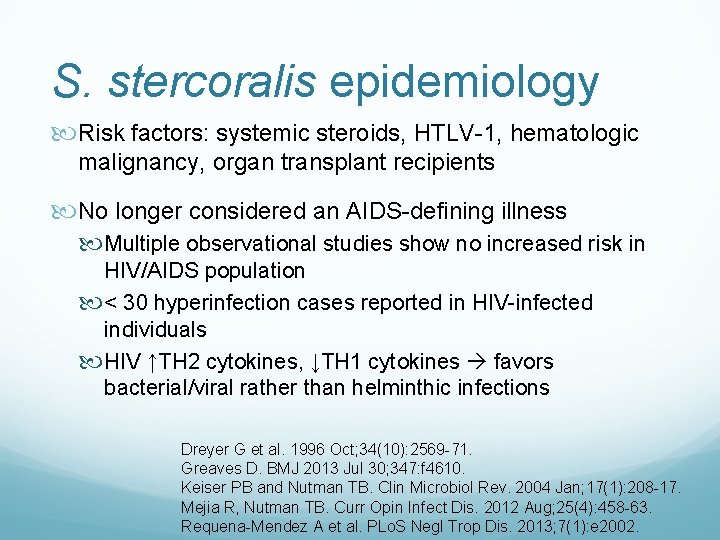
S. stercoralis epidemiology Risk factors: systemic steroids, HTLV-1, hematologic malignancy, organ transplant recipients No longer considered an AIDS-defining illness Multiple observational studies show no increased risk in HIV/AIDS population < 30 hyperinfection cases reported in HIV-infected individuals HIV ↑TH 2 cytokines, ↓TH 1 cytokines favors bacterial/viral rather than helminthic infections Dreyer G et al. 1996 Oct; 34(10): 2569 -71. Greaves D. BMJ 2013 Jul 30; 347: f 4610. Keiser PB and Nutman TB. Clin Microbiol Rev. 2004 Jan; 17(1): 208 -17. Mejia R, Nutman TB. Curr Opin Infect Dis. 2012 Aug; 25(4): 458 -63. Requena-Mendez A et al. PLo. S Negl Trop Dis. 2013; 7(1): e 2002.
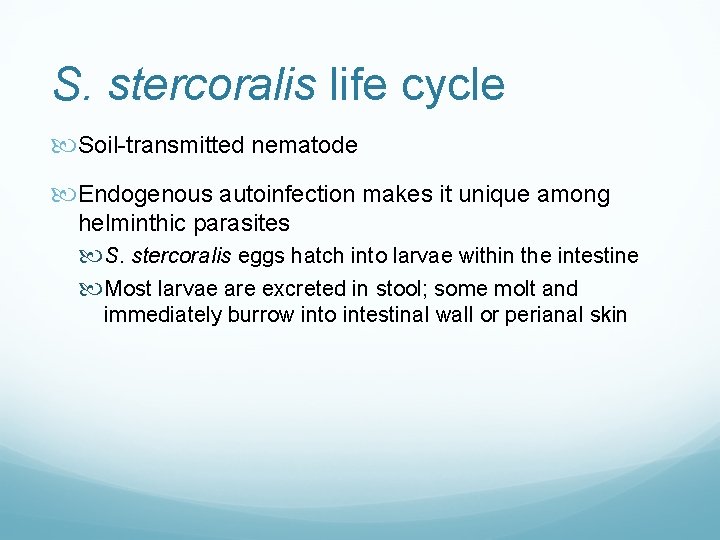
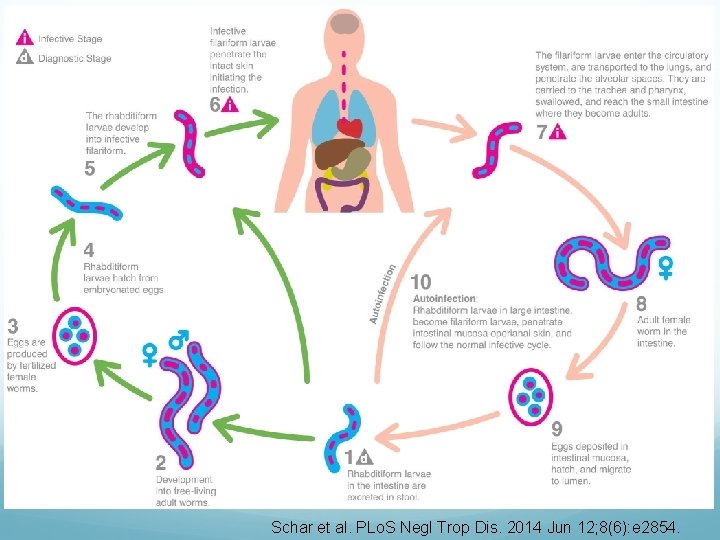
S. stercoralis life cycle Soil-transmitted nematode Endogenous autoinfection makes it unique among helminthic parasites S. stercoralis eggs hatch into larvae within the intestine Most larvae are excreted in stool; some molt and immediately burrow into intestinal wall or perianal skin
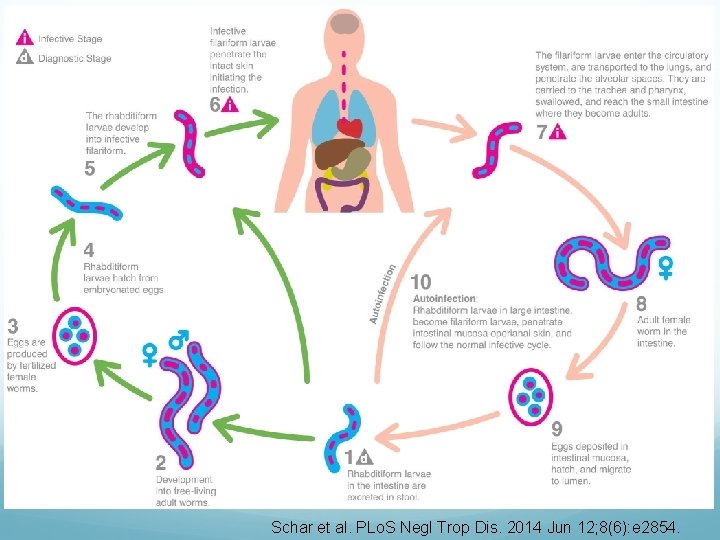
Schar et al. PLo. S Negl Trop Dis. 2014 Jun 12; 8(6): e 2854.
Clinical presentation Asymptomatic in up to 64% of cases (70 patients from metropolitan Barcelona 2003 -2012) Symptoms are due to larval form migrating through various organs of the body Clinical presentations: Acute strongyloidosis Chronic strongyloidosis Hyperinfection syndrome Disseminated strongyloidosis Greaves D. BMJ 2013 Jul 30; 347: f 4610. Valerio L et al. Trans R Soc Trop Med Hyg. 2013 Aug; 107(8): 465 -70.

Acute strongyloidosis Localized pruritic erythematous rash (site of skin penetration) Tracheal irritation and dry cough (larvae migrate from lungs up through trachea) Larvae swallowed into GI tract may have abdominal pain, bloating, heartburn, diarrhea or constipation, or abdominal pain http: //www. cdc. gov/parasites/strongyloides/ Greaves D. BMJ 2013 Jul 30; 347: f 4610. Valerio L et al. Trans R Soc Trop Med Hyg. 2013 Aug; 107(8): 465 -70.
Chronic strongyloidosis Chronic low intensity infection, larvae limited to lungs and GI tract, often asymptomatic Cutaneous symptoms: chronic urticaria, larva currens GI symptoms present in 23% (70 patients in the Barcelona case series) Most common: epigastric pain, postprandial fullness, heartburn, episodic diarrhea or constipation Rarely: fecal occult blood, massive GI hemorrhage, IBD/UC, pseudopolyposis Mild peripheral eosinophilia or ↑ Ig. E in up to 75% of cases http: //www. cdc. gov/parasites/strongyloides/ Greaves D. BMJ 2013 Jul 30; 347: f 4610. Valerio L et al. Trans R Soc Trop Med Hyg. 2013 Aug; 107(8): 465 -70.
Hyperinfection syndrome Larvae limited to lungs and GI tract, with accelerated life cycle, overproliferation, and excessive worm burden Occurs in the following situations: Chronic strongyloidosis + new immunosuppression Immunosuppressed patients + new acute strongyloidosis Most frequently associated with systemic steroids (as low as 20 mg/day and as short as 6 days) GI symptoms include abdominal pain, N/V, diarrhea, weight loss, protein-losing enteropathy http: //www. cdc. gov/parasites/strongyloides/ Greaves D. BMJ 2013 Jul 30; 347: f 4610. Valerio L et al. Trans R Soc Trop Med Hyg. 2013 Aug; 107(8): 465 -70.
Disseminated strongyloidosis Larvae invade numerous organs; mortality 85 -100% Systemic symptoms: hypoalbuminemia, GNR bacteremia/sepsis (larvae carry bacteria as they penetrate bowel wall), eosinophilia often absent Neurologic symptoms: aseptic or GNR meningitis Pulmonary symptoms: cough, hemoptysis, pneumonitis, respiratory failure, diffuse interstitial infiltrates GI symptoms: N/V, abdominal pain, diarrhea, ileus, bowel edema, obstruction, mucosal ulceration, massive hemorrhage, protein-losing enteropathy http: //www. cdc. gov/parasites/strongyloides/ Greaves D. BMJ 2013 Jul 30; 347: f 4610. Mejia R, Nutman TB. Curr Opin Infect Dis. 2012 Aug; 25(4): 458 -63. Valerio L et al. Trans R Soc Trop Med Hyg. 2013 Aug; 107(8): 465 -70.
Clinical questions Brief background review (epidemiology, S. stercoralis life cycle, and clinical presentation) What is the spectrum of endoscopic findings in strongyloidiasis? What are the available diagnostic modalities for S. stercoralis, and how do they compare? What is the optimal treatment and follow up for S. stercoralis?
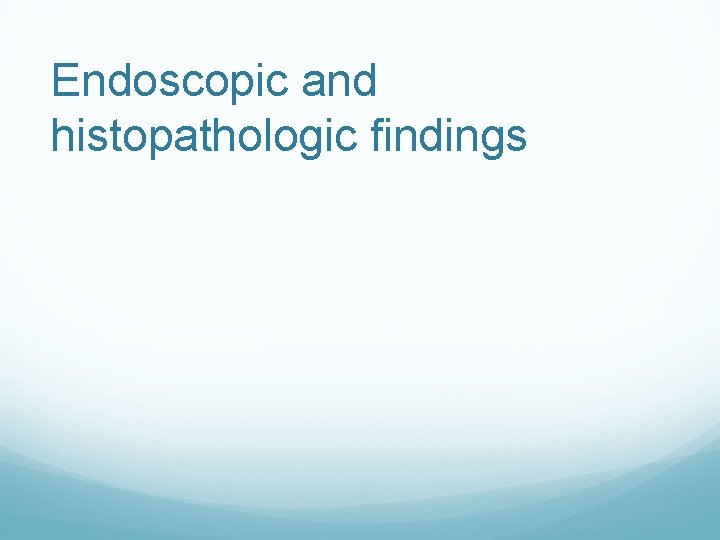
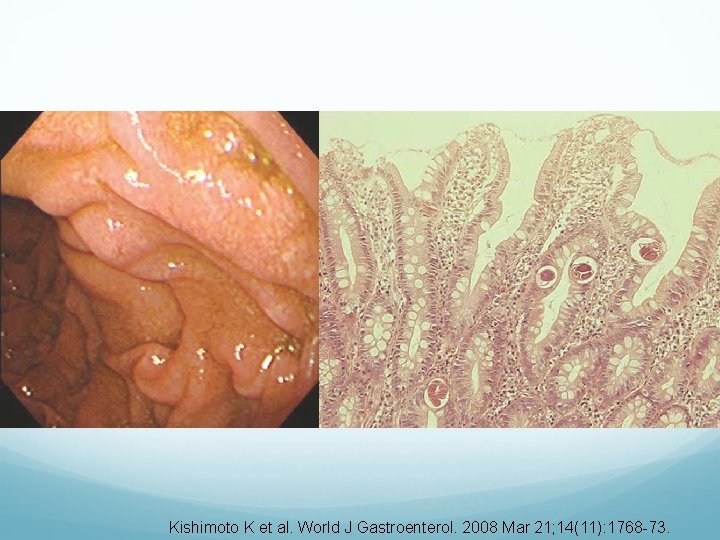
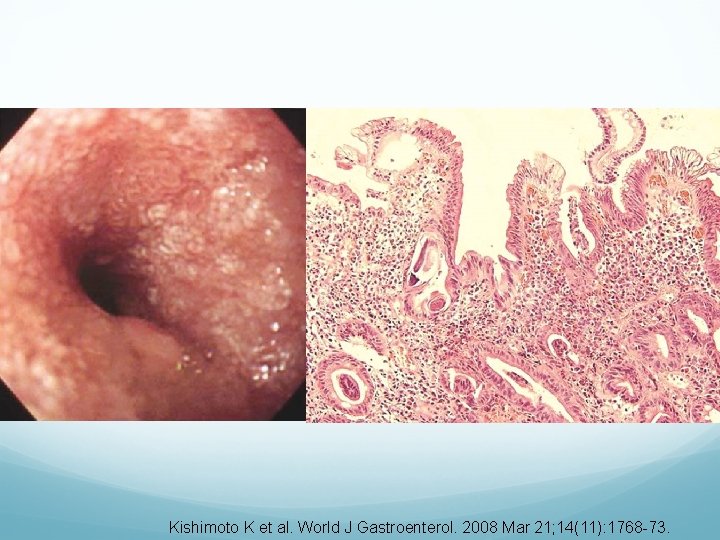
Endoscopic and histopathologic findings
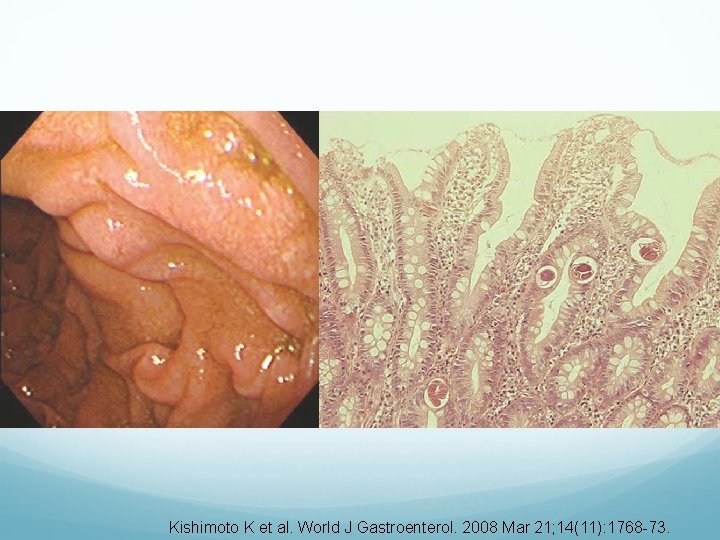
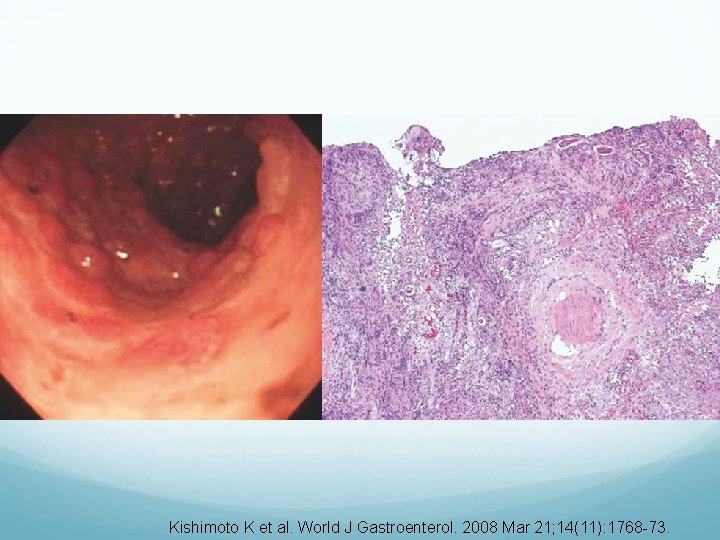
Kishimoto K et al. World J Gastroenterol. 2008 Mar 21; 14(11): 1768 -73.
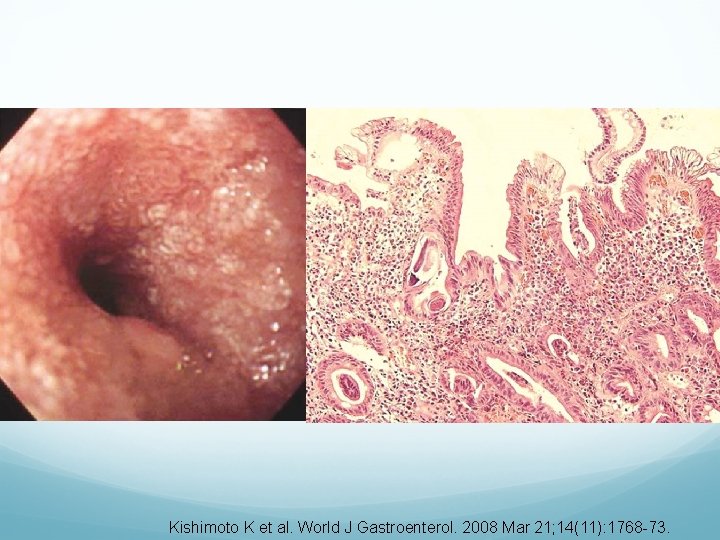
Kishimoto K et al. World J Gastroenterol. 2008 Mar 21; 14(11): 1768 -73.
Kishimoto K et al. World J Gastroenterol. 2008 Mar 21; 14(11): 1768 -73.
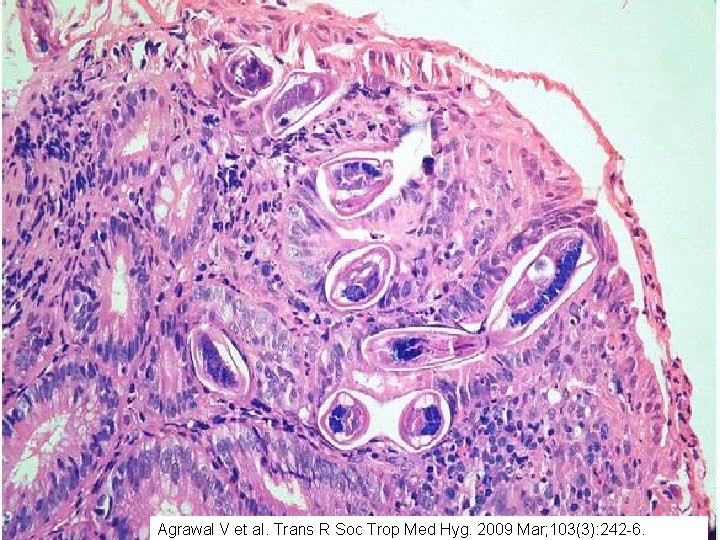
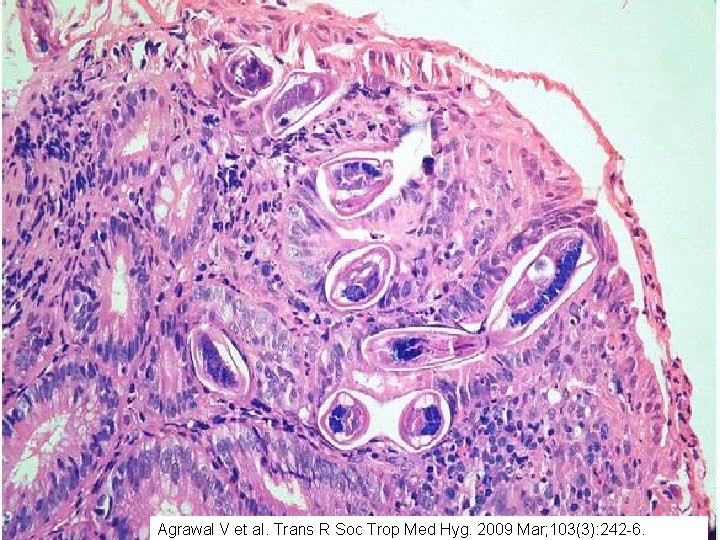
Agrawal V et al. Trans R Soc Trop Med Hyg. 2009 Mar; 103(3): 242 -6.

Slide courtesy of Dr. Shilpa Jain
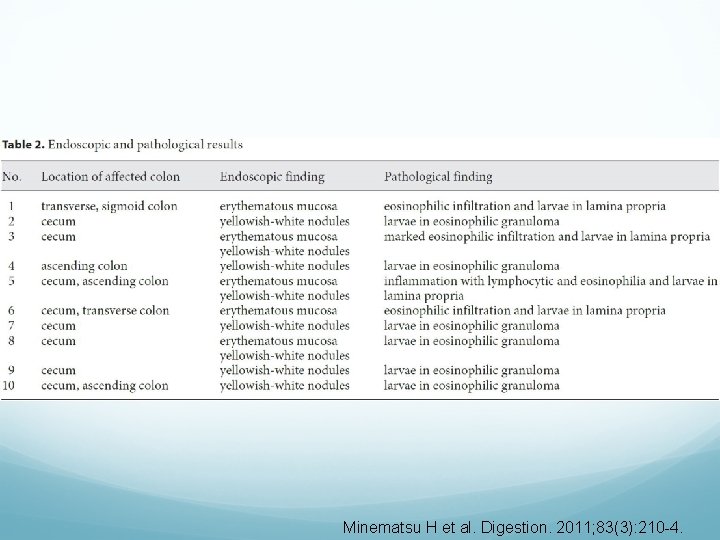
Minematsu H et al. Digestion. 2011; 83(3): 210 -4.
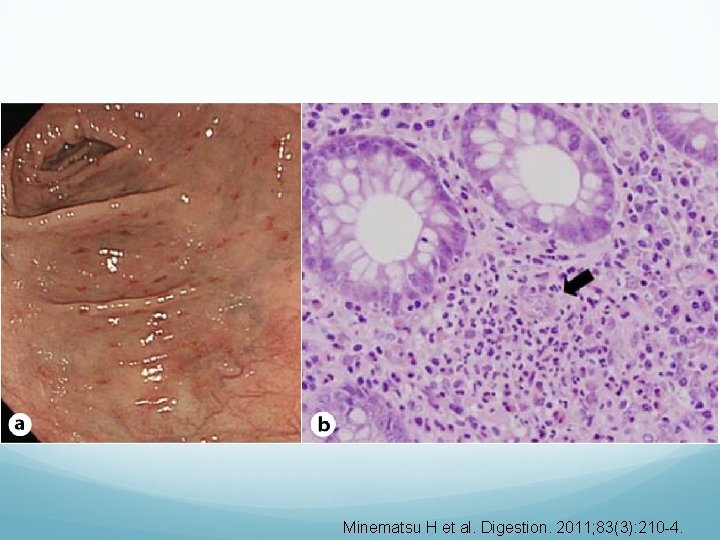
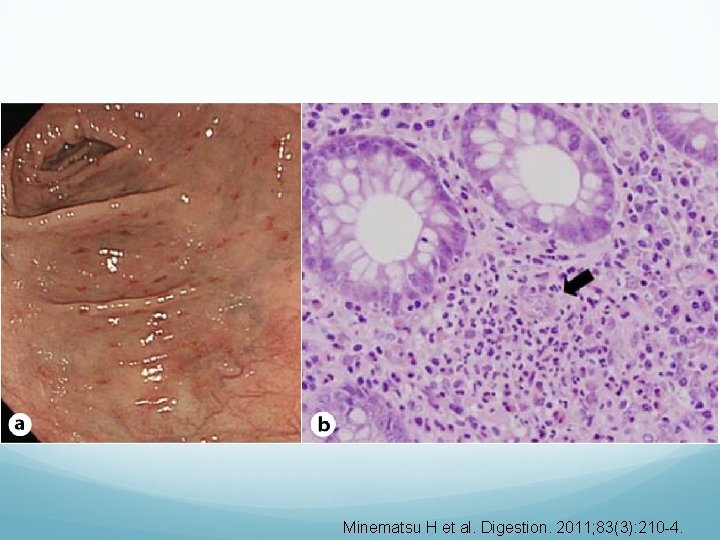
Minematsu H et al. Digestion. 2011; 83(3): 210 -4.

Minematsu H et al. Digestion. 2011; 83(3): 210 -4.
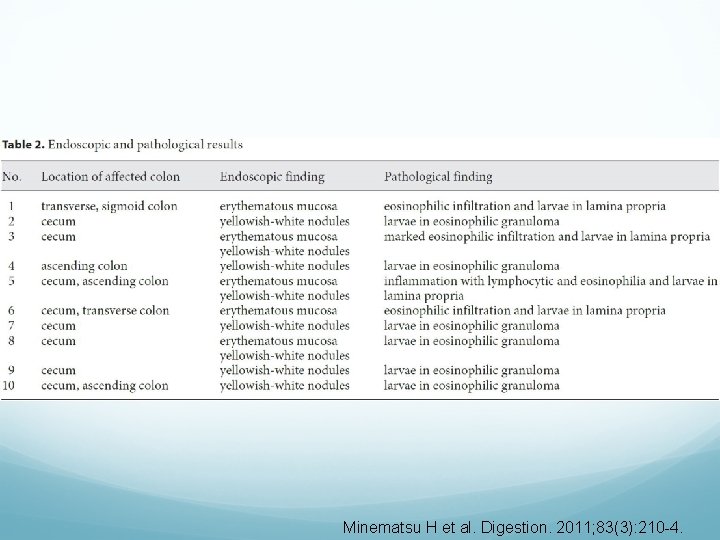
Minematsu H et al. Digestion. 2011; 83(3): 210 -4.
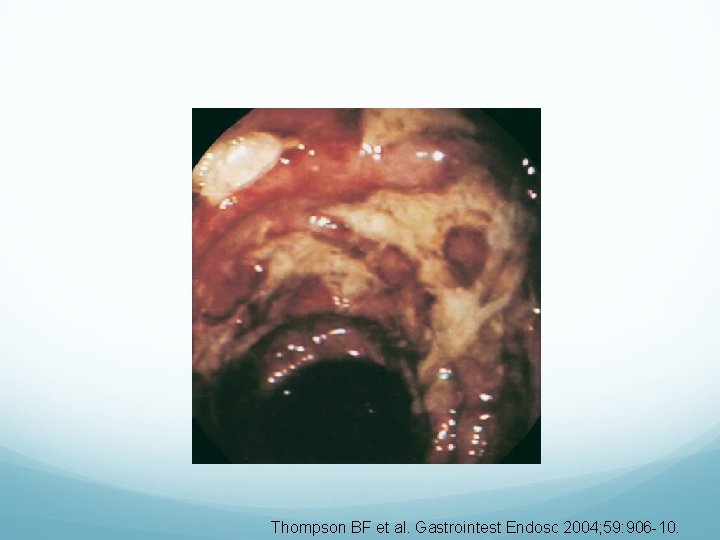
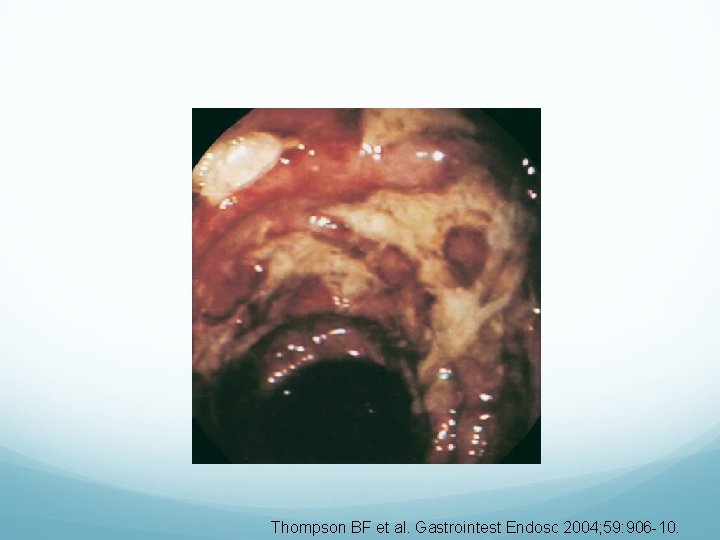
Thompson BF et al. Gastrointest Endosc 2004; 59: 906 -10.
Clinical questions Brief background review (epidemiology, S. stercoralis life cycle, and clinical presentation) What is the spectrum of endoscopic findings in strongyloidiasis? What are the available diagnostic modalities for S. stercoralis, and how do they compare? What is the optimal treatment and follow up for S. stercoralis?
Diagnostic modalities Fecal-based diagnosis Serology-based diagnosis Direct pathologic diagnosis via endoscopy, bronchoalveolar lavage, or other body fluid such as ascites
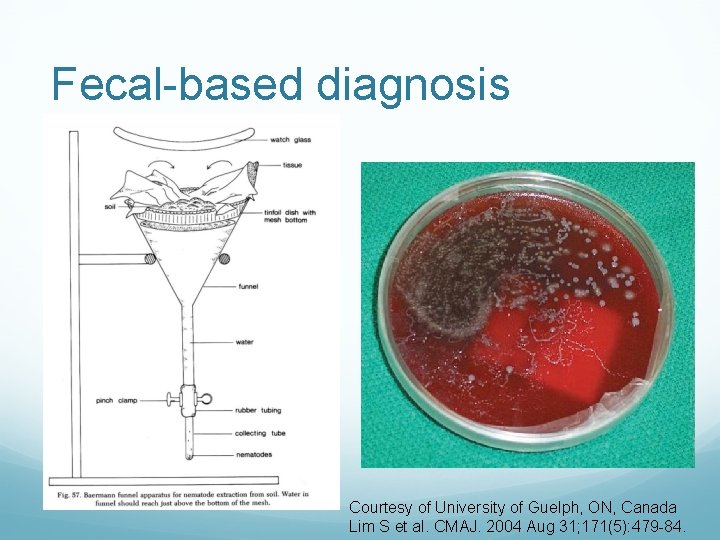
Fecal-based diagnosis Gold standard = serial stool examination Insensitive due to low infectious burden and intermittent larvae excretion Single stool specimen 30% to 50% sensitive 3 stool exams < 46% to 76% sensitive May require up to 7 stool exams to reach sensitivity >90% Specialized stool exams such as Baermann method (3. 6 to 4 x more sensitive) or agar plate culture Anderson NW et al. Clin Vaccine Immunol. 2014 May; 21(5): 732 -6. Greaves D. BMJ 2013 Jul 30; 347: f 4610. Kassalik M, Monkemuller K. Gastroenterol Hepatol. 2011 Nov; 7(11): 766 -8. Levenhagen MA, Costa-Cruz JM. Acta Trop. 2014 Jul; 135: 33 -43. Requena-Mendez A et al. PLo. S Negl Trop Dis. 2013; 7(1): e 2002.
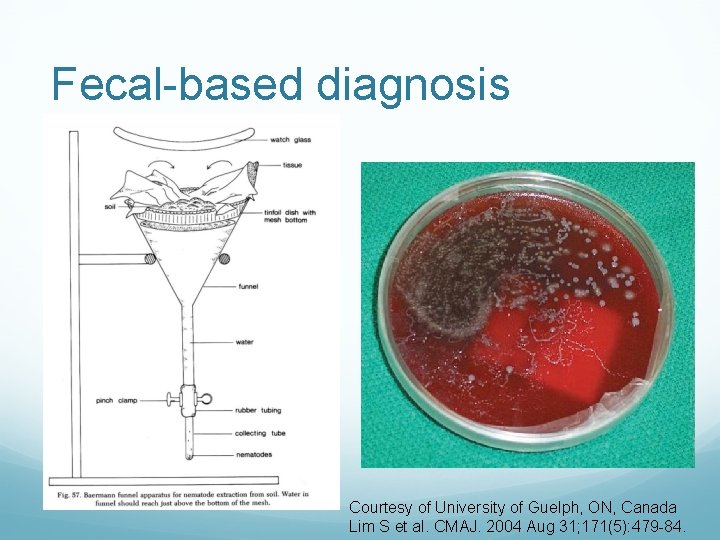
Fecal-based diagnosis Courtesy of University of Guelph, ON, Canada Lim S et al. CMAJ. 2004 Aug 31; 171(5): 479 -84.
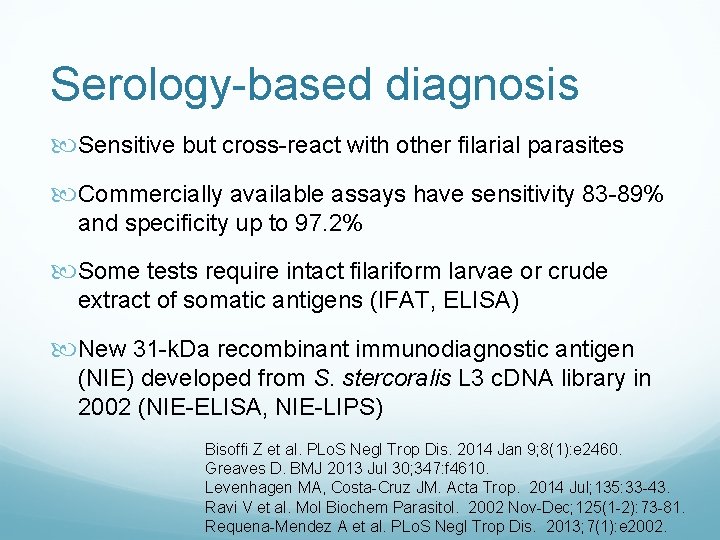
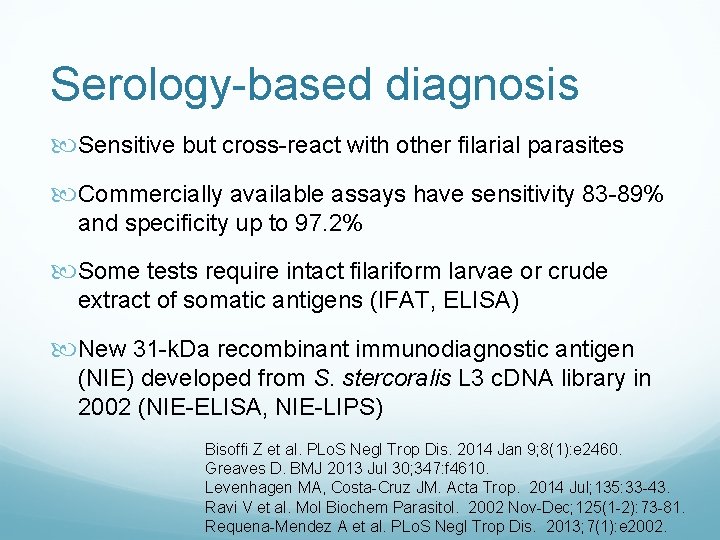
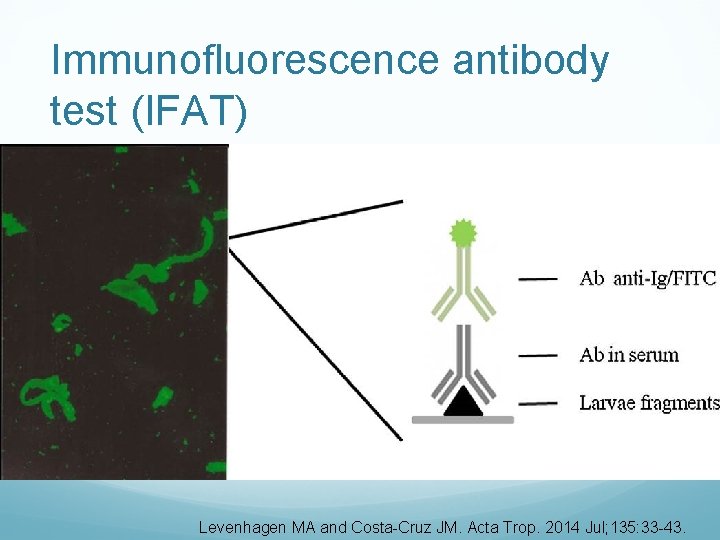
Serology-based diagnosis Sensitive but cross-react with other filarial parasites Commercially available assays have sensitivity 83 -89% and specificity up to 97. 2% Some tests require intact filariform larvae or crude extract of somatic antigens (IFAT, ELISA) New 31 -k. Da recombinant immunodiagnostic antigen (NIE) developed from S. stercoralis L 3 c. DNA library in 2002 (NIE-ELISA, NIE-LIPS) Bisoffi Z et al. PLo. S Negl Trop Dis. 2014 Jan 9; 8(1): e 2460. Greaves D. BMJ 2013 Jul 30; 347: f 4610. Levenhagen MA, Costa-Cruz JM. Acta Trop. 2014 Jul; 135: 33 -43. Ravi V et al. Mol Biochem Parasitol. 2002 Nov-Dec; 125(1 -2): 73 -81. Requena-Mendez A et al. PLo. S Negl Trop Dis. 2013; 7(1): e 2002.
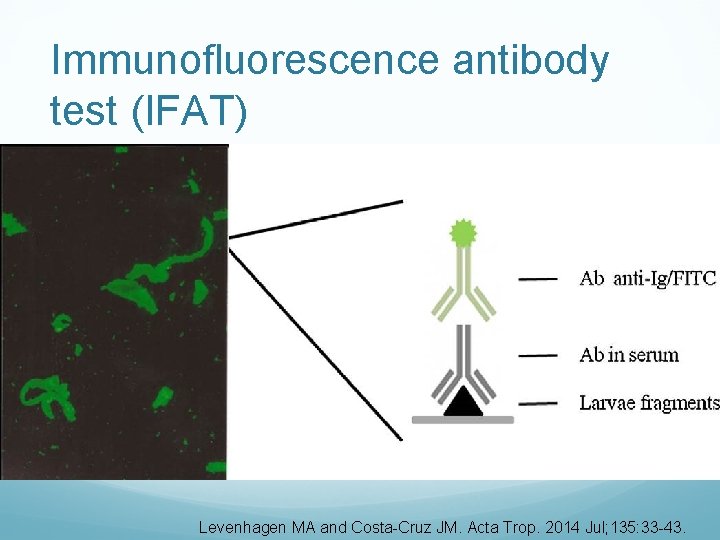
Immunofluorescence antibody test (IFAT) Levenhagen MA and Costa-Cruz JM. Acta Trop. 2014 Jul; 135: 33 -43.
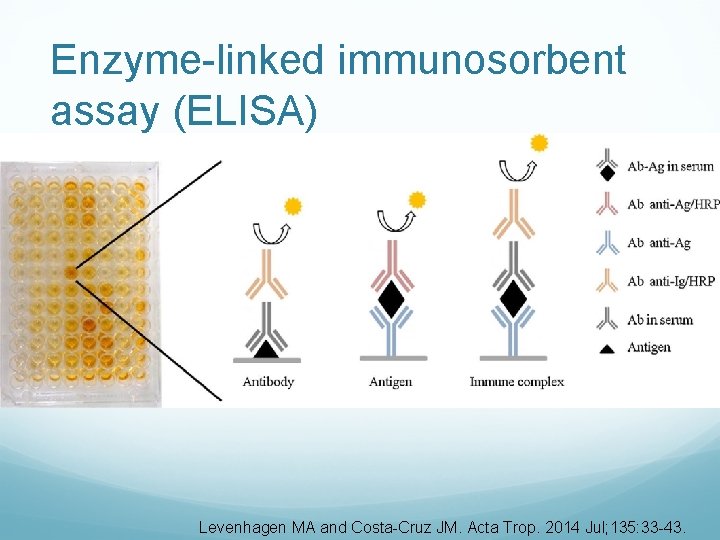
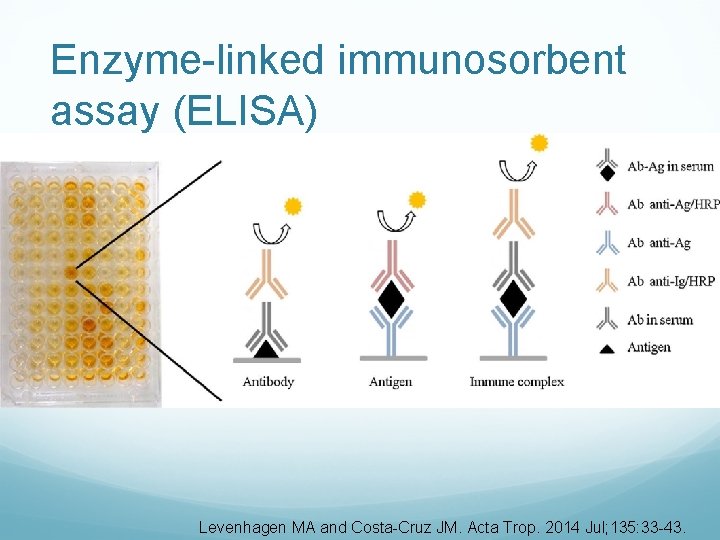
Enzyme-linked immunosorbent assay (ELISA) Levenhagen MA and Costa-Cruz JM. Acta Trop. 2014 Jul; 135: 33 -43.
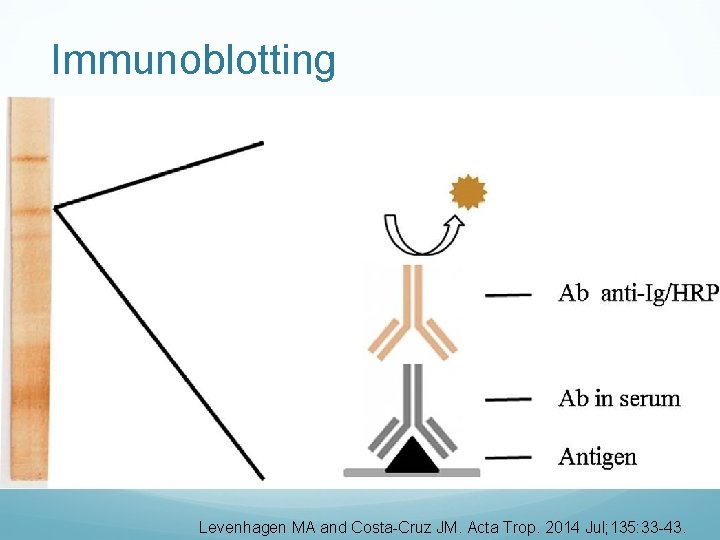
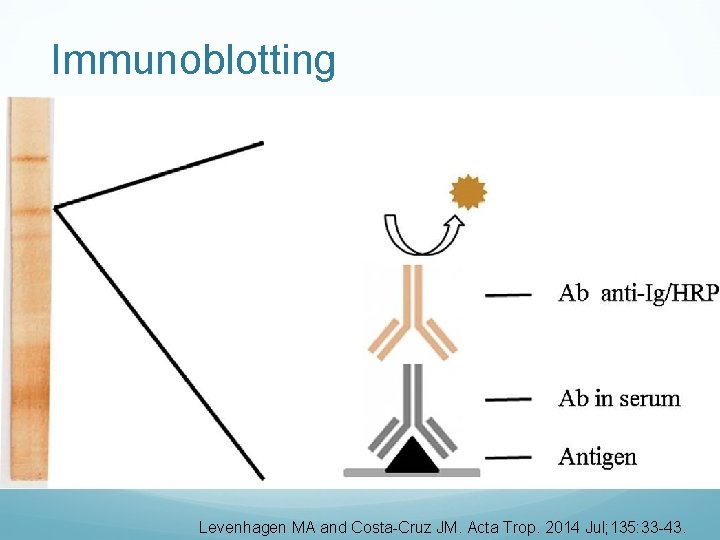
Immunoblotting Levenhagen MA and Costa-Cruz JM. Acta Trop. 2014 Jul; 135: 33 -43.
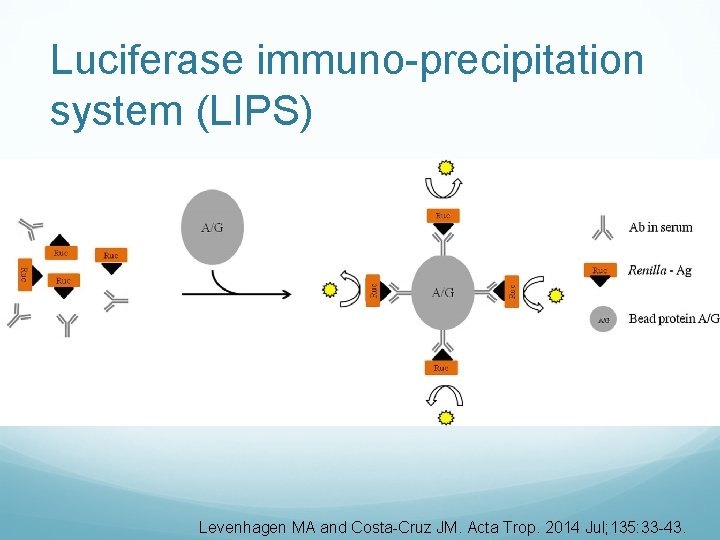
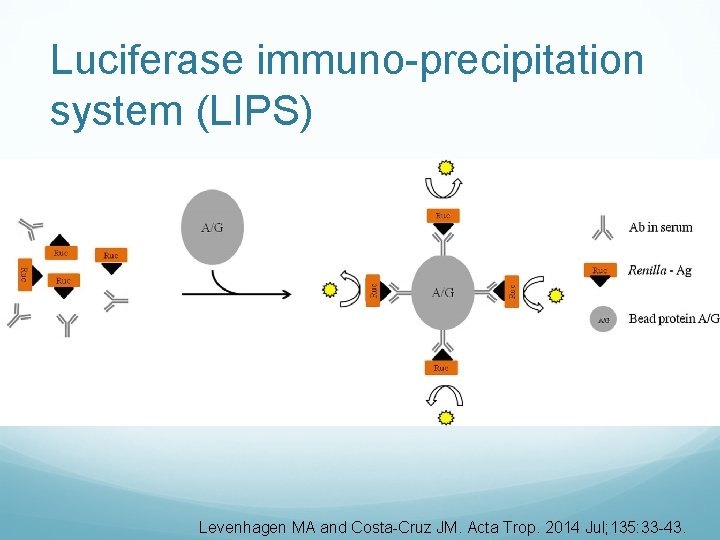
Luciferase immuno-precipitation system (LIPS) Levenhagen MA and Costa-Cruz JM. Acta Trop. 2014 Jul; 135: 33 -43.

Serology-based diagnosis Bisoffi Z et al. PLo. S Negl Trop Dis. 2014 Jan 9; 8(1): e 2460.
Pathologic diagnosis Examples shown Invasive: bronchial fluid, endoscopy or colonoscopy (especially duodenal biopsy), ascites Impractical for screening asymptomatic populations
Clinical questions Brief background review (epidemiology, S. stercoralis life cycle, and clinical presentation) What is the spectrum of endoscopic findings in strongyloidiasis? What are the available diagnostic modalities for S. stercoralis, and how do they compare? What is the optimal treatment and follow up for S. stercoralis?
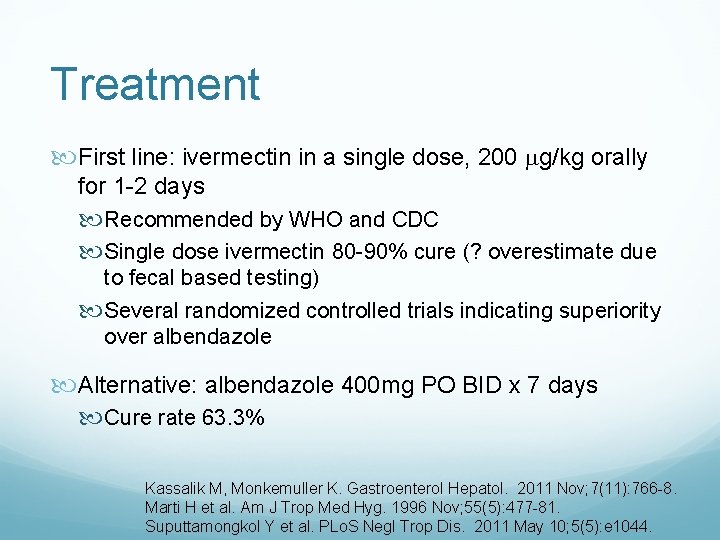
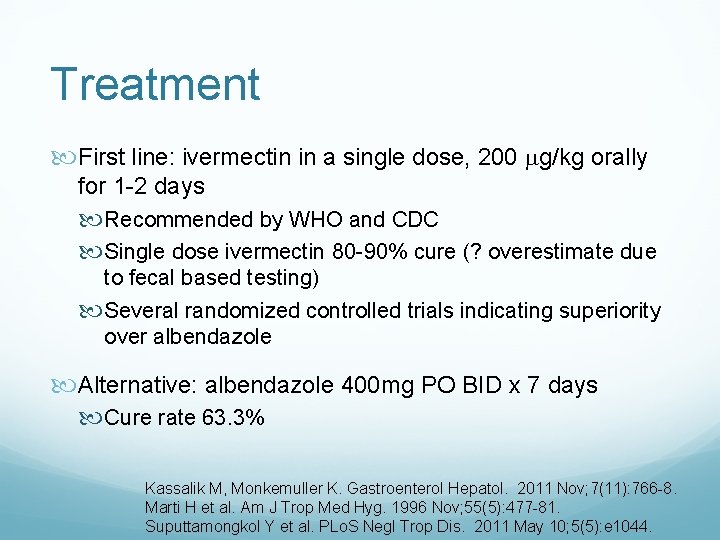
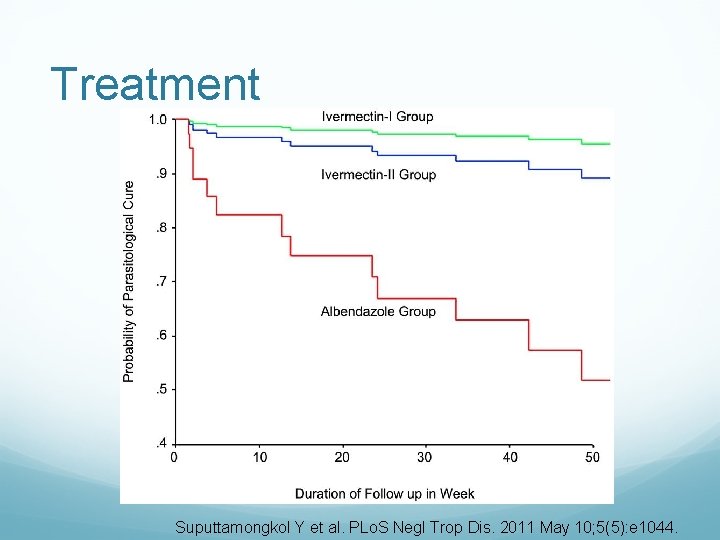
Treatment First line: ivermectin in a single dose, 200 g/kg orally for 1 -2 days Recommended by WHO and CDC Single dose ivermectin 80 -90% cure (? overestimate due to fecal based testing) Several randomized controlled trials indicating superiority over albendazole Alternative: albendazole 400 mg PO BID x 7 days Cure rate 63. 3% Kassalik M, Monkemuller K. Gastroenterol Hepatol. 2011 Nov; 7(11): 766 -8. Marti H et al. Am J Trop Med Hyg. 1996 Nov; 55(5): 477 -81. Suputtamongkol Y et al. PLo. S Negl Trop Dis. 2011 May 10; 5(5): e 1044.
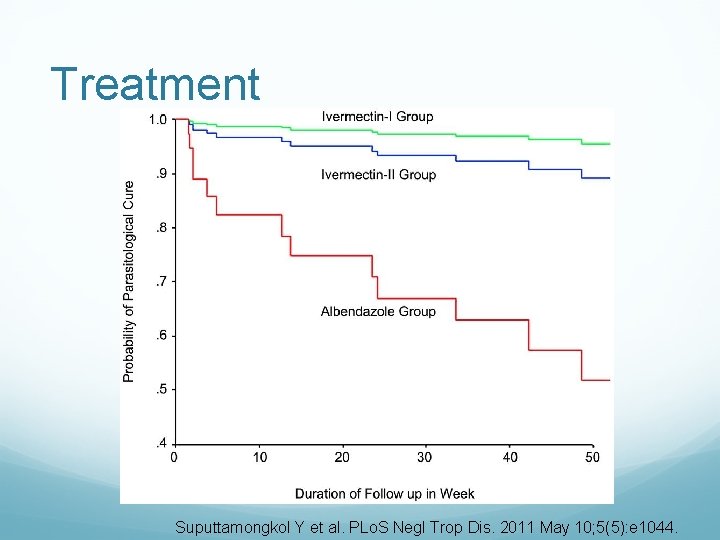
Treatment Suputtamongkol Y et al. PLo. S Negl Trop Dis. 2011 May 10; 5(5): e 1044.
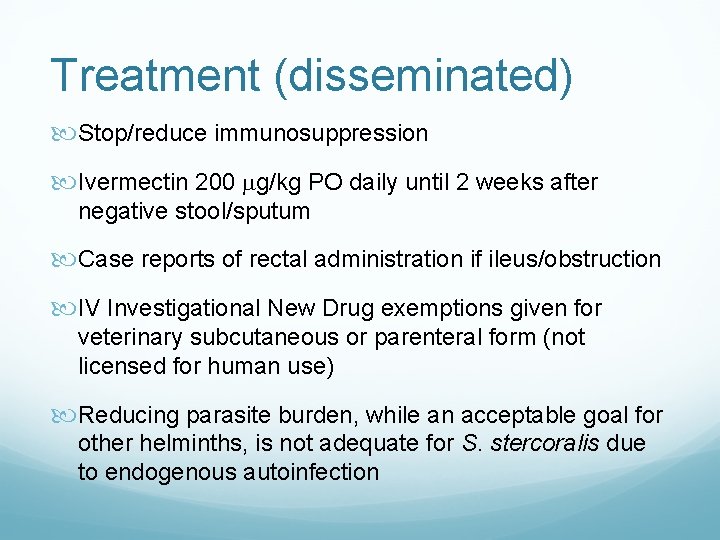
Treatment (disseminated) Stop/reduce immunosuppression Ivermectin 200 g/kg PO daily until 2 weeks after negative stool/sputum Case reports of rectal administration if ileus/obstruction IV Investigational New Drug exemptions given for veterinary subcutaneous or parenteral form (not licensed for human use) Reducing parasite burden, while an acceptable goal for other helminths, is not adequate for S. stercoralis due to endogenous autoinfection
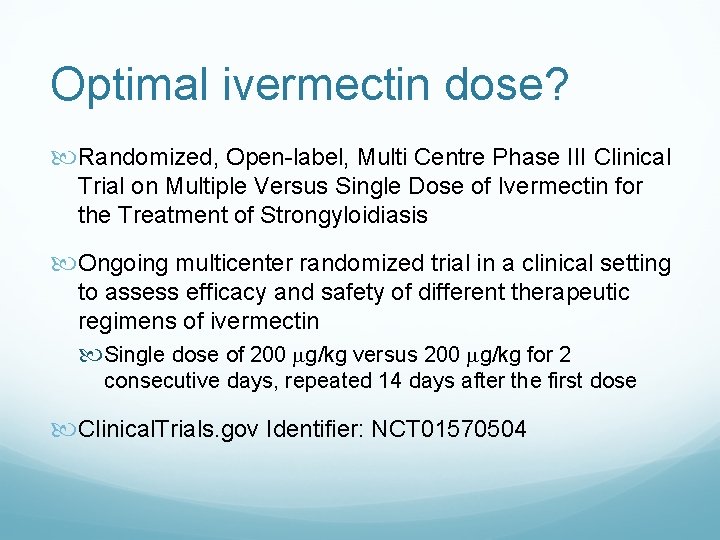
Optimal ivermectin dose? Randomized, Open-label, Multi Centre Phase III Clinical Trial on Multiple Versus Single Dose of Ivermectin for the Treatment of Strongyloidiasis Ongoing multicenter randomized trial in a clinical setting to assess efficacy and safety of different therapeutic regimens of ivermectin Single dose of 200 g/kg versus 200 g/kg for 2 consecutive days, repeated 14 days after the first dose Clinical. Trials. gov Identifier: NCT 01570504
Follow up If initial positive stool exam and persistent symptoms, may repeat stool exam 2 -4 weeks after treatment Dreyer et al. study of stool test reproducibility: 75. 9% of 108 asymptomatic patients with positive stool exam were negative on next four samples despite no treatment If initial serologic-based diagnosis, seroreversion or decline in antibody titer observed at 6 -12 months ? eosinophilia trend: decline at an average of 96 days in two referral centers in Switzerland 1998 -2002 Buonfrate D et al. PLo. S Negl Trop Dis. 2015 Feb 10; 9(2): e 0003491. Dreyer G et al. J Clin Microbiol. 1996 Oct; 34(10): 2569 -71. Kassalik M, Monkemuller K. Gastroenterol Hepatol. 2011 Nov; 7(11): 766 -8. Marti H et al. Am J Trop Med Hyg. 1996 Nov; 55(5): 477 -81. Nuesch R et al. J Travel Med. 2005 Mar-Apr; 12(2): 80 -4. Suputtamongkol Y et al. PLo. S Negl Trop Dis. 2011 May 10; 5(5): e 1044.
Our patient Completed ivermectin 12 mg PO once Prednisone was decreased to 2. 5 mg PO daily (unrelated to strongyloidiasis; SLE nephritis doing well) Specialized serologic testing for S. Stercoralis is not available at Ben Taub Options for follow up: trend eosinophilia, serial stool exams, or blood agar culture (BAL fluid only)
Take home points Difficult diagnosis and fatal if unrecognized; maintain high level of suspicion! New/improved serology-based diagnostic tests are not all commercially available Best therapeutic regimen of ivermectin is undergoing investigation in ongoing clinical trial There are more questions than answers… WEAR SHOES WHEN TRAVELING!!
References Agrawal V et al. Intestinal strongyloidiasis: a diagnosis frequently missed in the tropics. Trans R Soc Trop Med Hyg. 2009 Mar; 103(3): 242 -6. Anderson NW et al. Comparison of three immunoassays for detection of antibodies to Strongyloides stercoralis. Clin Vaccine Immunol. 2014 May; 21(5): 732 -6. Bisoffi Z et al. Diagnostic accuracy of five serologic tests for Strongyloides stercoralis infection. PLo. S Negl Trop Dis. 2014 Jan 9; 8(1): e 2460. Bisoffi Z et al. Strongyloides stercoralis: a plea for action. PLo. S Negl Trop Dis. 2013 May 9; 7(5): e 2214. Buonfrate D et al. Accuracy of five serologic tests for the follow up of Strongyloides stercoralis infection. PLo. S Negl Trop Dis. 2015 Feb 10; 9(2): e 0003491. Buonfrate D et al. Prevalence of strongyloidiasis in Latin America: a systematic review of the literature. Epidemiol Infect. 2015 Feb; 143(3): 452 -60. Dreyer G et al. Patterns of detection of Strongyloides stercoralis in stool specimens: implications for diagnosis and clinical trials. J Clin Microbiol. 1996 Oct; 34(10): 2569 -71. Greaves D. Strongyloides stercoralis infection. BMJ 2013 Jul 30; 347: f 4610. Kassalik M and Monkemuller K. Strongyloides stercoralis hyperinfection syndrome and disseminated disease. Gastroenterol Hepatol. 2011 Nov; 7(11): 766 -8. Keiser PB and Nutman TB. Strongyloides stercoralis in the immunocompromised population. Clin Microbiol Rev. 2004 Jan; 17(1): 208 -17.
References Kishimoto K et al. Endoscopic and histopathologic study on the duodenum of Strongyloides stercoralis hyperinfection. World J Gastroenterol. 2008 Mar 21; 14(11): 1768 -73. Krolewiecki AJ et al. A public health response against Strongyloides stercoralis: time to look at soil-transmitted helminthiasis in full. PLo. S Negl Trop Dis. 2013 May 9; 7(5)e 2165. Levenhagen MA and Costa-Cruz JM. Update on immunologic and molecular diagnosis of human strongyloidiasis. Acta Trop. 2014 Jul; 135: 33 -43. Lim S et al. Complicated and fatal Strongyloides infection in Canadians: risk factors, diagnosis, and management. CMAJ. 2004 Aug 31; 171(5): 479 -84. Marti H et al. A comparative trial of a single-dose ivermectin versus three days of albendazole for treatment of Strongyloides stercoralis and other soil-transmitted helminths in children. Am J Trop Med Hyg. 1996 Nov; 55(5): 47781. Mejia R and Nutman TB. Screening, prevention, and treatment for hyperinfection syndrome and disseminated infections caused by Strongyloides stercoralis. Curr Opin Infect Dis. 2012 Aug; 25(4): 458 -63. Minematsu H et al. Colonoscopic findings and pathologic characteristics of strongyloides colitis: a case series. Digestion. 2011; 83(3): 210 -4. Nuesch R et al. Imported strongyloidosis: a longitudinal analysis of 31 cases. J Travel Med. 2005 Mar-Apr; 12(2): 80 -4. Prendki V et al. Strongyloidiasis in man 75 years after initial exposure. Emerg Infect Dis. 2011 May; 17(5): 931 -2.
References Ravi V et al. Characterization of a recombinant immunodiagnostic antigen (NIE) from Strongyloides stercoralis L 3 stage larvae. Mol Biochem Parasitol. 2002 Nov-Dec; 125(1 -2): 73 -81. Requena-Mendez A et al. The laboratory diagnosis and follow up of strongyloidiasis: a systematic review. PLo. S Negl Trop Dis. 2013; 7(1): e 2002. Santiago M and Leitao B. Prevention of strongyloides hyperinfection syndrome: a rheumatological point of view. Eur J Intern Med. 2009 Dec; 20(8): 744 -8. Schar et al. Strongyloides stercoralis: Global distribution and risk factors. PLo. S Negl Trop Dis. 2014 Jun 12; 8(6): e 2854. Suputtamongkol Y et al. Efficacy and safety of single and double doses of ivermectin versus 7 -day high dose albendazole for chronic strongyloidiasis. PLo. S Negl Trop Dis. 2011 May 10; 5(5): e 1044. Thompson BF et al. The spectrum of GI strongyloidiasis: an endoscopic-pathologic study. Gastrointest Endosc 2004; 59: 906 -10. Valerio L et al. Strongyloides stercoralis, the hidden worm. Epidemiological and clinical characteristics of 70 cases diagnosed in the North Metropolitan Area of Barcelona, Spain, 2003 -2012. Trans R Soc Trop Med Hyg. 2013 Aug; 107(8): 465 -70. WHO (2006). Preventive chemotherapy in human helminthiasis. Coordinated use of antihelminthic drugs in control interventions: a manual for health professionals and programme managers. Geneva: World Health Organization. 62 p.
Questions or comments?
 Johanna chan pack
Johanna chan pack Dr johanna chan
Dr johanna chan Nursing grand rounds presentation example
Nursing grand rounds presentation example Utmb grand rounds
Utmb grand rounds Duke medicine grand rounds
Duke medicine grand rounds Bé thì chăn nghé chăn trâu
Bé thì chăn nghé chăn trâu Readiness rounds
Readiness rounds Tabular dimensioning
Tabular dimensioning Schwartz rounds facilitator training
Schwartz rounds facilitator training Guns
Guns Layers of neurosis in gestalt therapy
Layers of neurosis in gestalt therapy Sam rounds
Sam rounds What is 75 rounded to the nearest ten
What is 75 rounded to the nearest ten Harvard instructional rounds
Harvard instructional rounds A is an odd number which rounds to 100 000
A is an odd number which rounds to 100 000 Red, white & blue bite size rounds tortilla chips
Red, white & blue bite size rounds tortilla chips Quality teaching rounds coding sheet
Quality teaching rounds coding sheet What do you call a stubborn angle
What do you call a stubborn angle Maintenance rounds
Maintenance rounds Ieee fellow nomination
Ieee fellow nomination Fellow lpkia
Fellow lpkia Importance of fellow customers in service delivery
Importance of fellow customers in service delivery Ieee fellow requirements
Ieee fellow requirements Microsoft technical fellow
Microsoft technical fellow Fellow lpkia
Fellow lpkia Cisco fellow
Cisco fellow Poor little black fellow summary
Poor little black fellow summary Policy statement mun example
Policy statement mun example Asme fellow nomination
Asme fellow nomination Odd fellow orden
Odd fellow orden Trish livingston deakin
Trish livingston deakin Little fellow
Little fellow Paul harris fellow certificate template
Paul harris fellow certificate template Odd fellow medlemsregister
Odd fellow medlemsregister Insurgent characters
Insurgent characters Johanna bobrowski
Johanna bobrowski Keppinukke
Keppinukke Johanna laisaari
Johanna laisaari Heidi personajes
Heidi personajes Johanna biemans
Johanna biemans Avanne ja alkoholi
Avanne ja alkoholi Johanna snickars
Johanna snickars Johanna marroig
Johanna marroig Johanna nguyen
Johanna nguyen Alkylerare
Alkylerare Johanna urm
Johanna urm Power semiconductor devices
Power semiconductor devices Johanna sonntag
Johanna sonntag Dutrion tabletid
Dutrion tabletid Prof. johanna haberer
Prof. johanna haberer Johanna eia
Johanna eia Johanna waldau
Johanna waldau Johanna will-orava
Johanna will-orava Abrufvertrag rahmenvertrag
Abrufvertrag rahmenvertrag Johanna wyn
Johanna wyn Mircea oprica
Mircea oprica Johanna breyne
Johanna breyne Johanna rönn
Johanna rönn Johanna monti
Johanna monti Johanna ungerstedt
Johanna ungerstedt Paramalignt syndrom
Paramalignt syndrom Johanna koti porvoo
Johanna koti porvoo Emilia galotti 5 aufzug 1 auftritt
Emilia galotti 5 aufzug 1 auftritt Johanna lattu
Johanna lattu Johanna londoño modelo
Johanna londoño modelo Johanna luomala
Johanna luomala Sơ đồ chân arduino nano
Sơ đồ chân arduino nano Một nhà thơ chân chính
Một nhà thơ chân chính Wake forest opcd
Wake forest opcd