Fractures of the Spine in Children Timothy Moore


- Slides: 47
Fractures of the Spine in Children Timothy Moore, MD Original Author: Steven Frick, MD; March 2004 Revised: Steven Frick, MD; August 2006 Timoth Moore, MD; November 2011
Important Pediatric Differences • • Anatomical differences Radiologic differences Increased elasticity Periosteal tube fractures – apparent dislocations • Surgery rarely indicated • Immobilization well tolerated
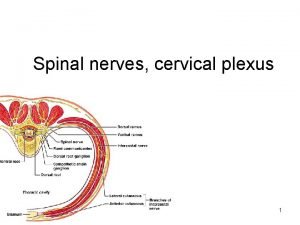
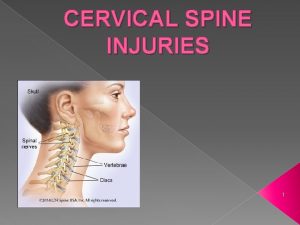
Cervical Spine Injuries • Rare in children - < 1% of children’s fractures • Quoted rates of neurologic injury in children’s C spine injuries vary from “rare” to 44% in large series • Age less than 7 – Majority of C spine injuries are upper cervical, esp. craniocervical junction • Age greater than 7 – Lower C spine injuries predominate Jones. Pediatric cervical spine trauma. J Am Acad Orthop Surg. 2011; 19: 600.
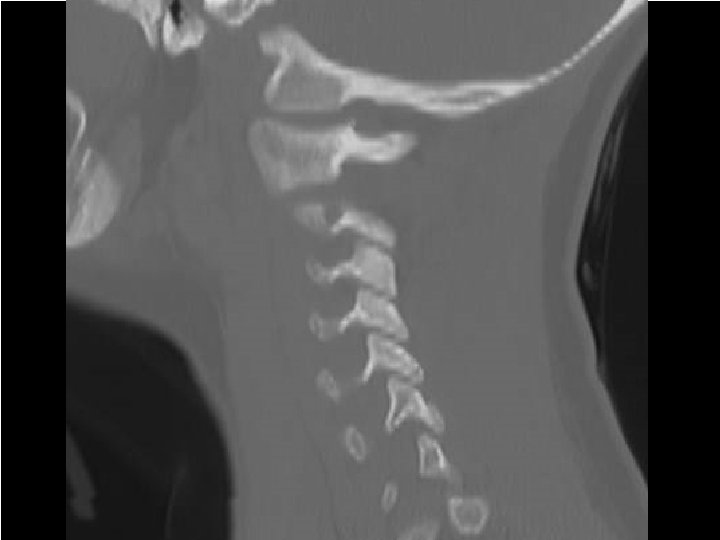
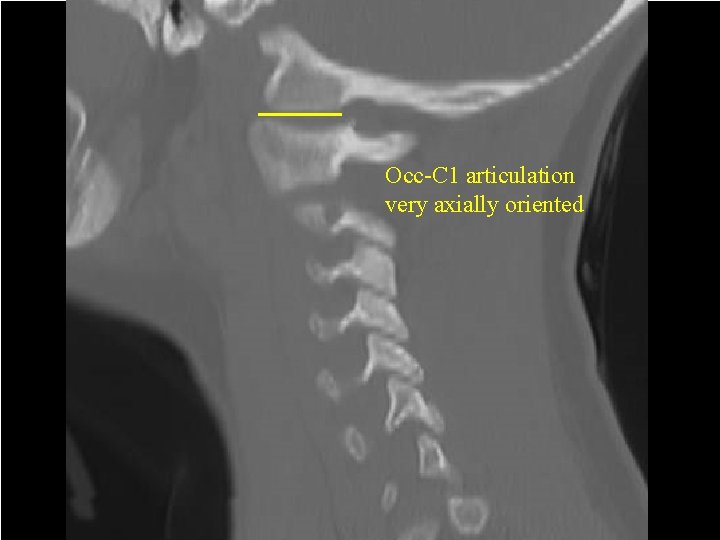
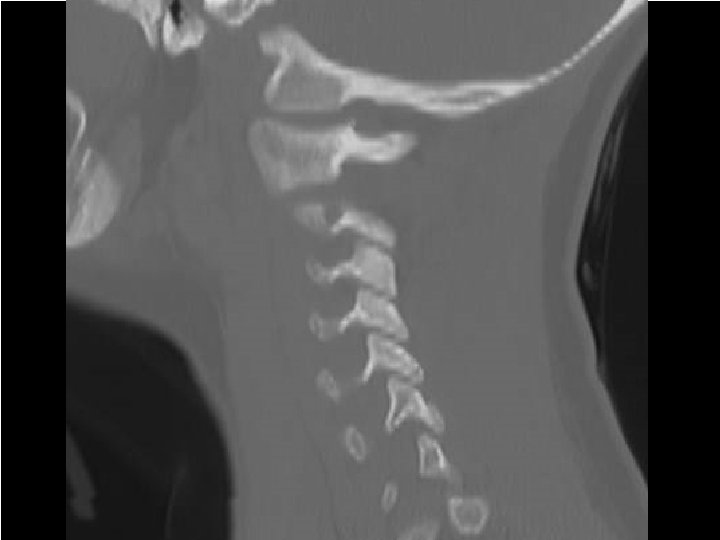
Cervical Spine Injuries • Upper cervical anatomy – Occiput-C 1 articulation – Axially oriented – Prone to occiput-C 1 injury
Multiple Small Diameter Pin Child’s Halo for Displaced C 2 Fracture Note bolster behind neck to maintain lordosis and reduce angulation
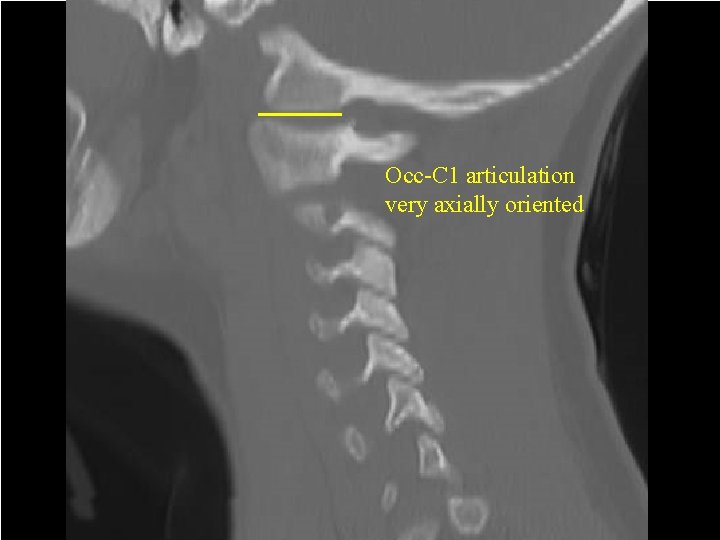
Multiple Small Diameter Pin Child’s Halo for Displaced C 2 Fracture Occ-C 1 articulation very axially oriented Note bolster behind neck to maintain lordosis and reduce angulation
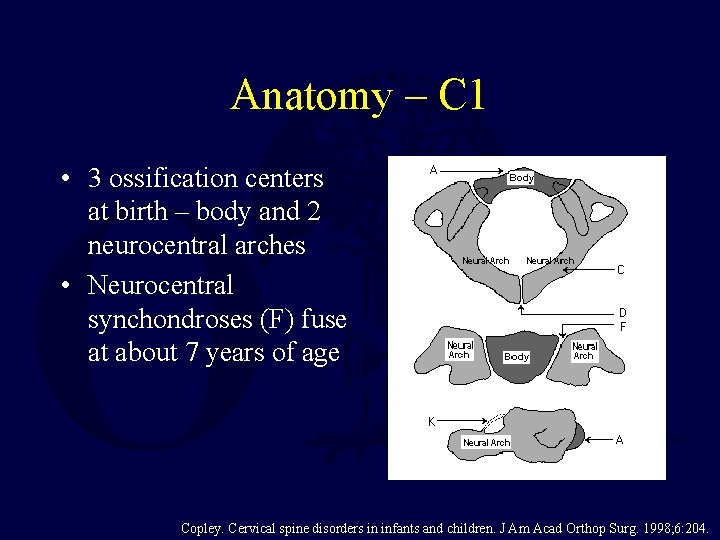
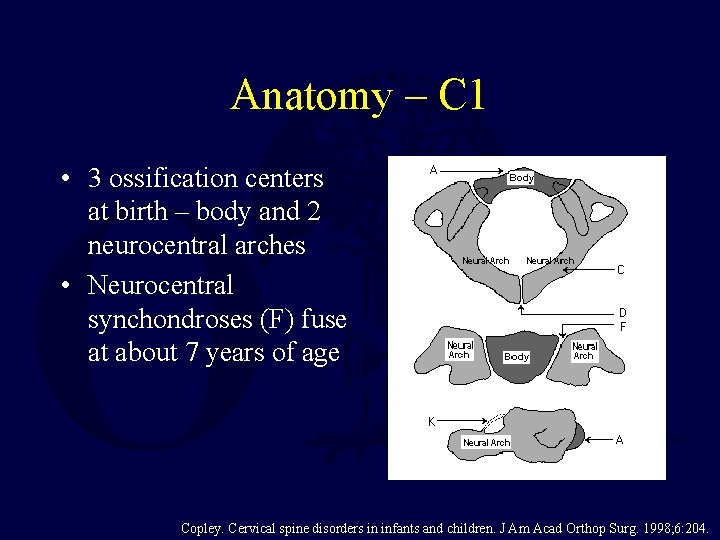
Anatomy – C 1 • 3 ossification centers at birth – body and 2 neurocentral arches • Neurocentral synchondroses (F) fuse at about 7 years of age Copley. Cervical spine disorders in infants and children. J Am Acad Orthop Surg. 1998; 6: 204.
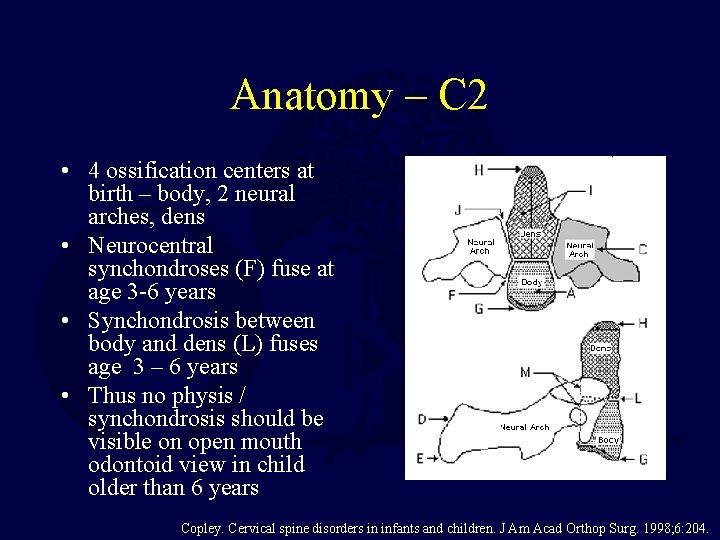
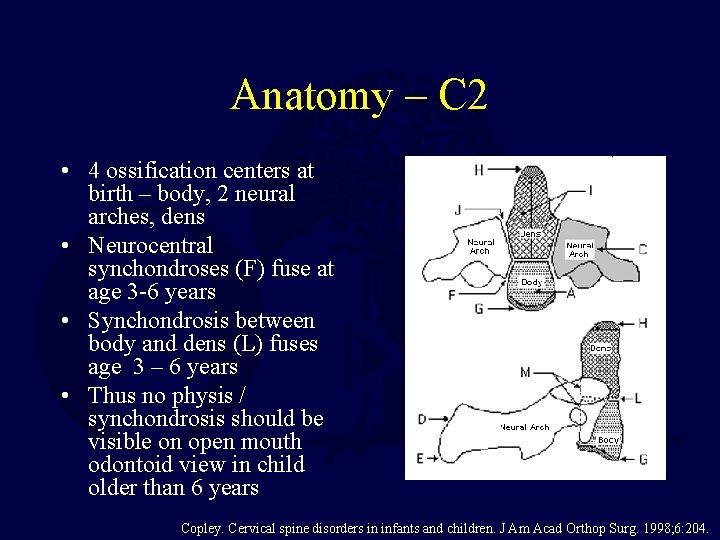
Anatomy – C 2 • 4 ossification centers at birth – body, 2 neural arches, dens • Neurocentral synchondroses (F) fuse at age 3 -6 years • Synchondrosis between body and dens (L) fuses age 3 – 6 years • Thus no physis / synchondrosis should be visible on open mouth odontoid view in child older than 6 years Copley. Cervical spine disorders in infants and children. J Am Acad Orthop Surg. 1998; 6: 204.
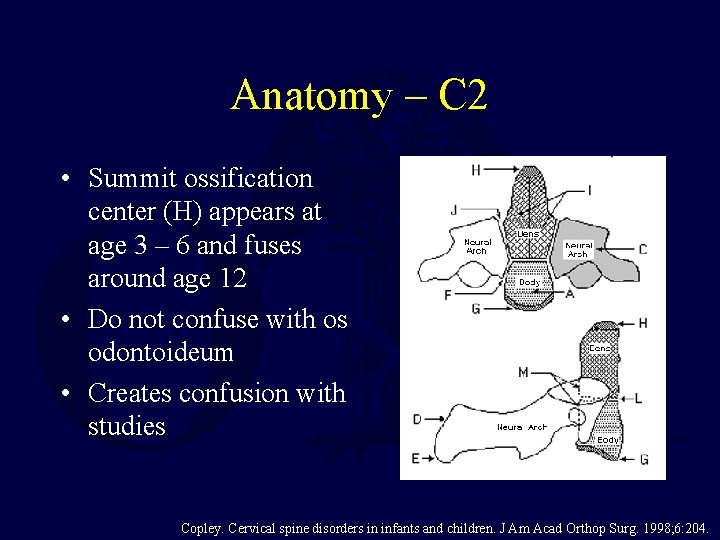
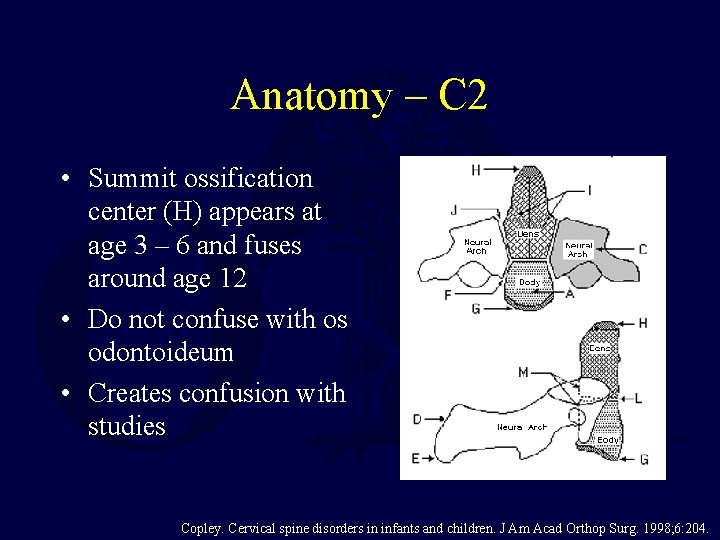
Anatomy – C 2 • Summit ossification center (H) appears at age 3 – 6 and fuses around age 12 • Do not confuse with os odontoideum • Creates confusion with studies Copley. Cervical spine disorders in infants and children. J Am Acad Orthop Surg. 1998; 6: 204.
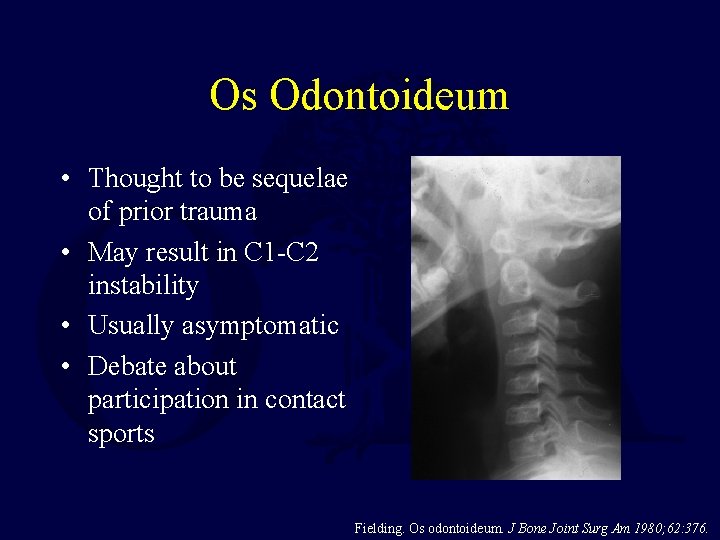
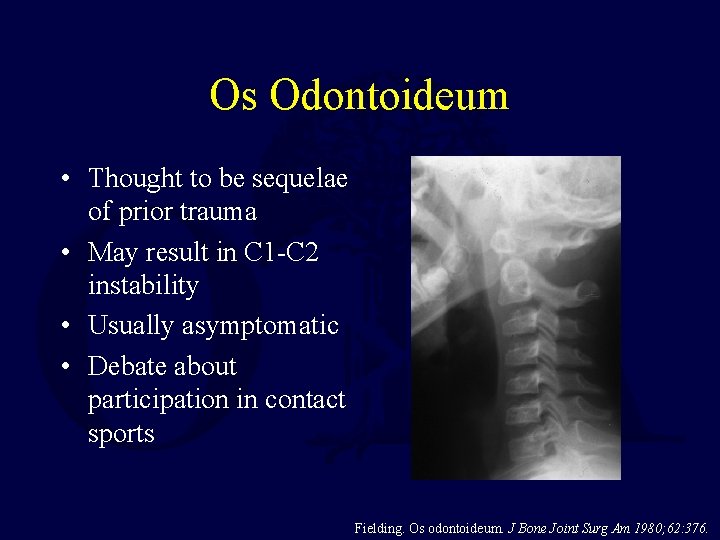
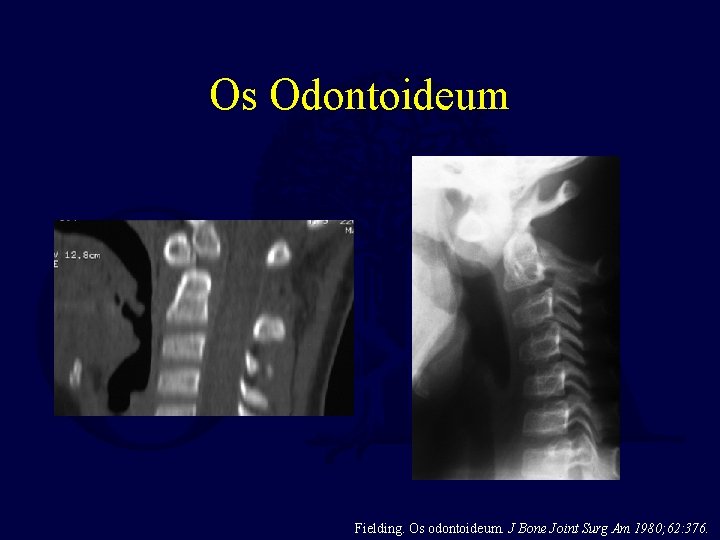
Os Odontoideum • Thought to be sequelae of prior trauma • May result in C 1 -C 2 instability • Usually asymptomatic • Debate about participation in contact sports Fielding. Os odontoideum. J Bone Joint Surg Am 1980; 62: 376.
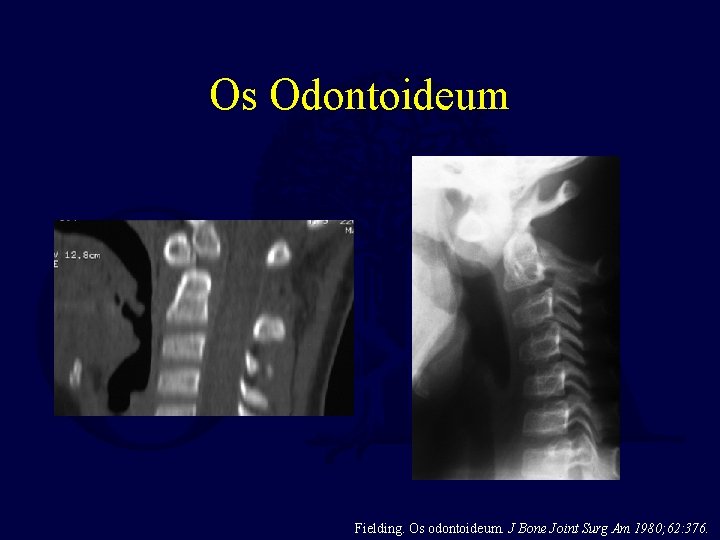
Os Odontoideum Fielding. Os odontoideum. J Bone Joint Surg Am 1980; 62: 376.
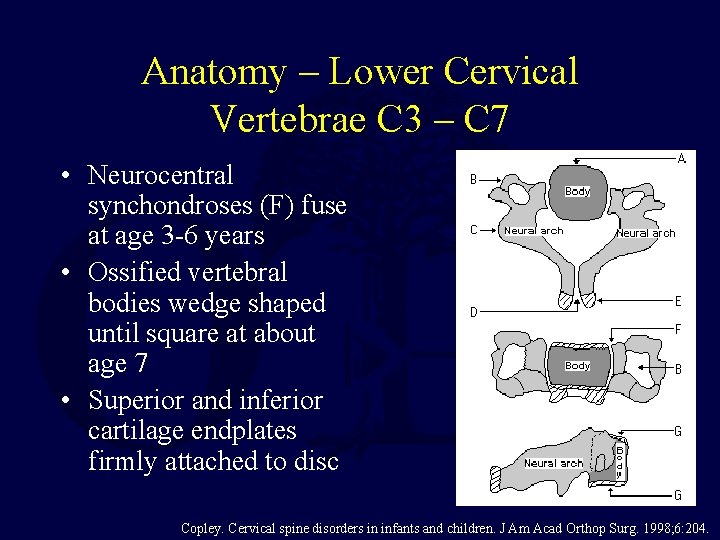
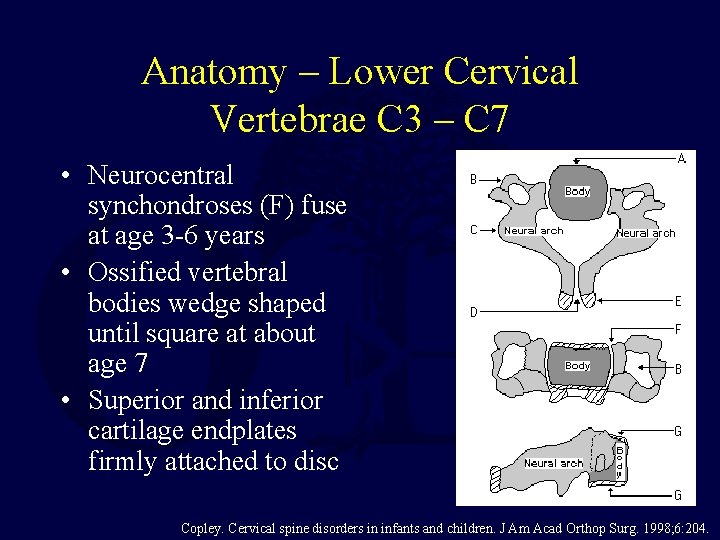
Anatomy – Lower Cervical Vertebrae C 3 – C 7 • Neurocentral synchondroses (F) fuse at age 3 -6 years • Ossified vertebral bodies wedge shaped until square at about age 7 • Superior and inferior cartilage endplates firmly attached to disc Copley. Cervical spine disorders in infants and children. J Am Acad Orthop Surg. 1998; 6: 204.
Mechanism of Injury • Child’s neck very mobile – ligamentous laxity and shallow angle of facet joints • Relatively larger head • In younger patients this combination leads to upper cervical injuries • Falls and motor vehicle accidents most common cause in younger children
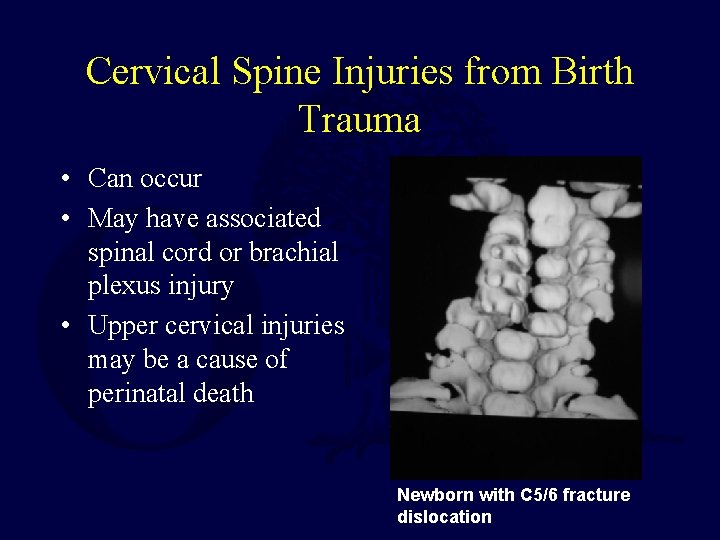
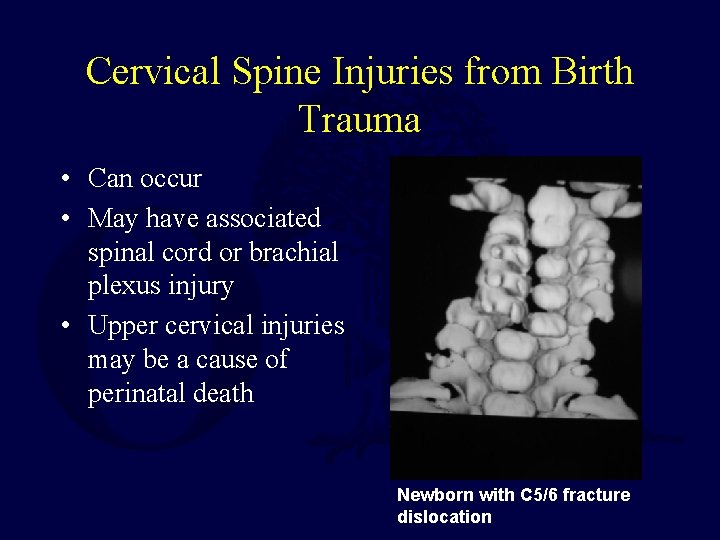
Cervical Spine Injuries from Birth Trauma • Can occur • May have associated spinal cord or brachial plexus injury • Upper cervical injuries may be a cause of perinatal death Newborn with C 5/6 fracture dislocation
Typical Fracture Pattern • Fractures tend to occur within the endplate between the cartilaginous endplate and the vertebral body • Clinically and experimentally fractures occur by splitting the endplate between the columnar growth cartilage and the calcified cartilage • Does not typically occur by fracture through the endplate – disc junction Jones. Pediatric cervical spine trauma. J Am Acad Orthop Surg. 2011; 19: 600.
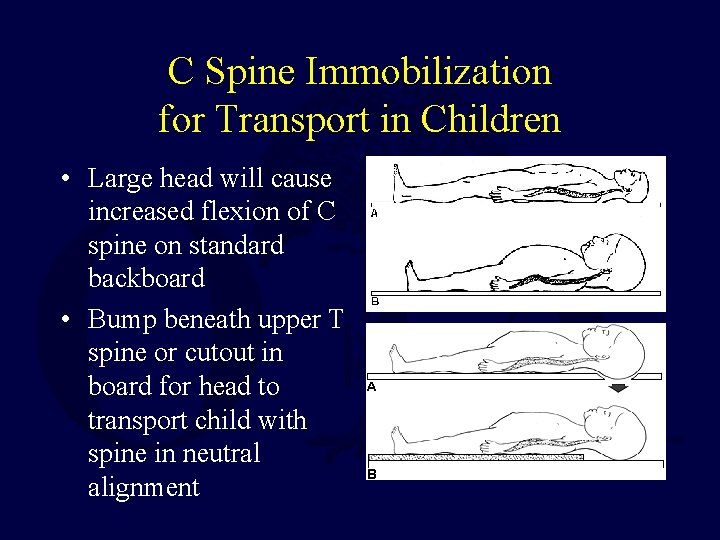
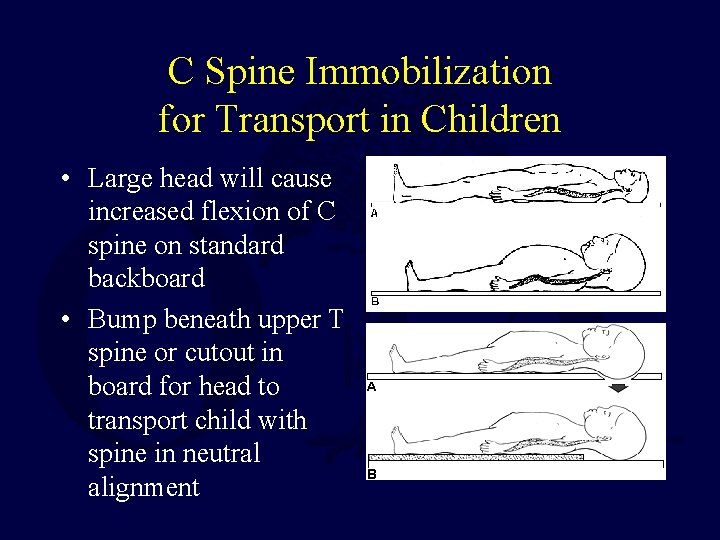
C Spine Immobilization for Transport in Children • Large head will cause increased flexion of C spine on standard backboard • Bump beneath upper T spine or cutout in board for head to transport child with spine in neutral alignment
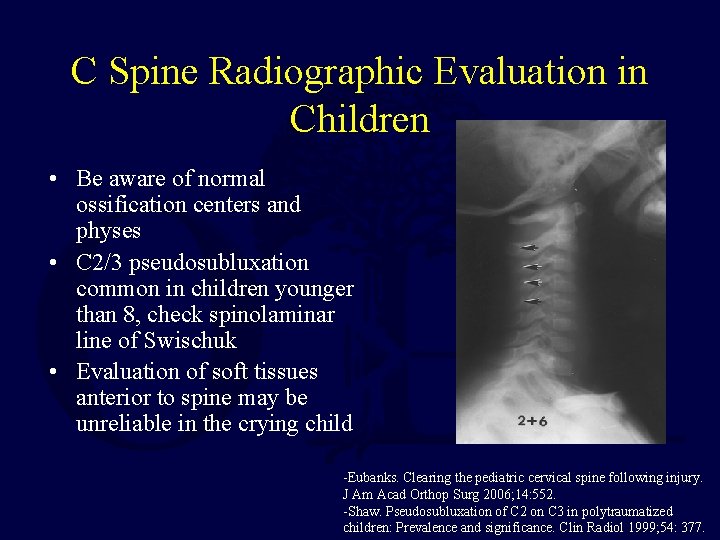
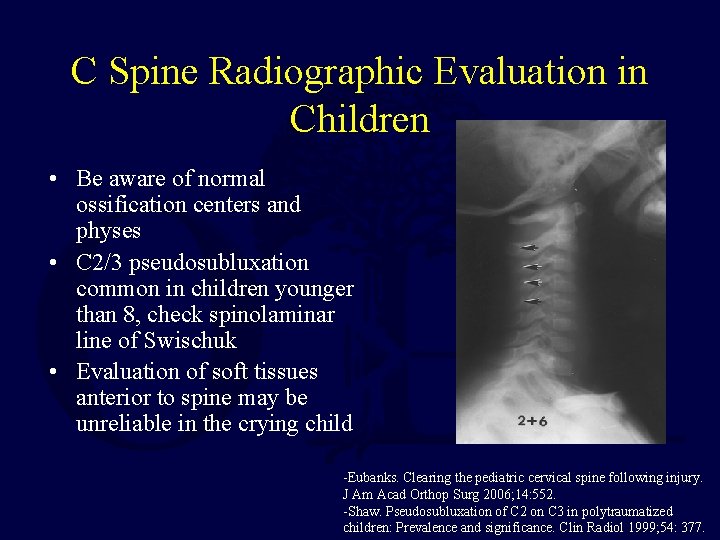
C Spine Radiographic Evaluation in Children • Be aware of normal ossification centers and physes • C 2/3 pseudosubluxation common in children younger than 8, check spinolaminar line of Swischuk • Evaluation of soft tissues anterior to spine may be unreliable in the crying child -Eubanks. Clearing the pediatric cervical spine following injury. J Am Acad Orthop Surg 2006; 14: 552. -Shaw. Pseudosubluxation of C 2 on C 3 in polytraumatized children: Prevalence and significance. Clin Radiol 1999; 54: 377.
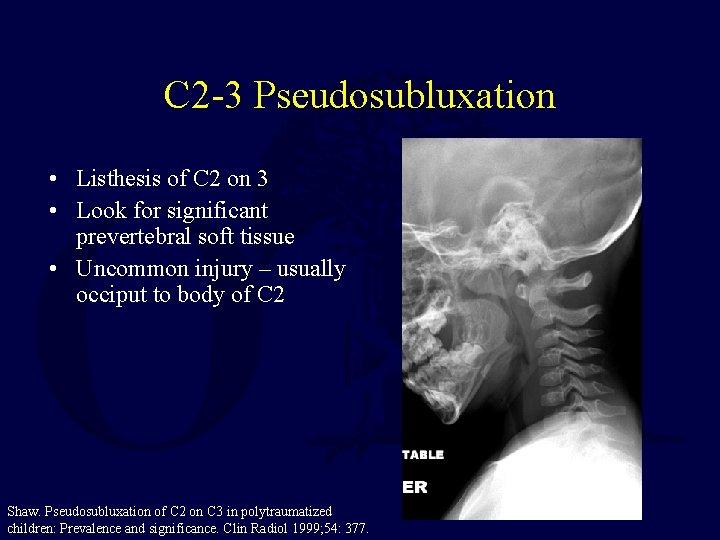
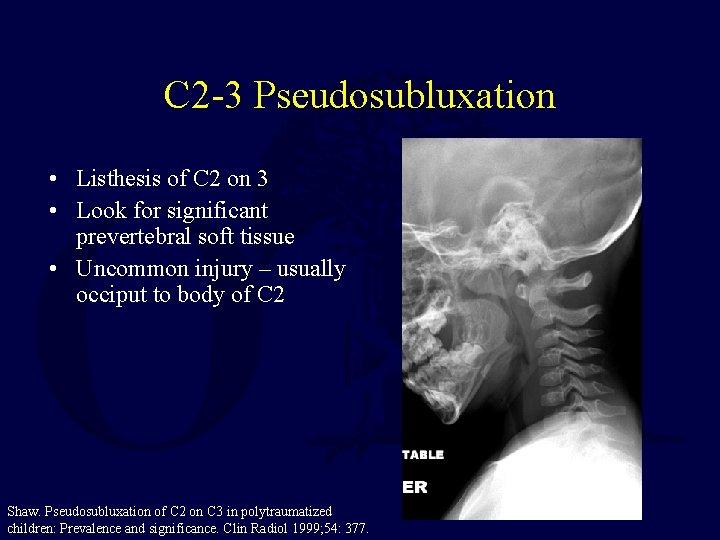
C 2 -3 Pseudosubluxation • Listhesis of C 2 on 3 • Look for significant prevertebral soft tissue • Uncommon injury – usually occiput to body of C 2 Shaw. Pseudosubluxation of C 2 on C 3 in polytraumatized children: Prevalence and significance. Clin Radiol 1999; 54: 377.
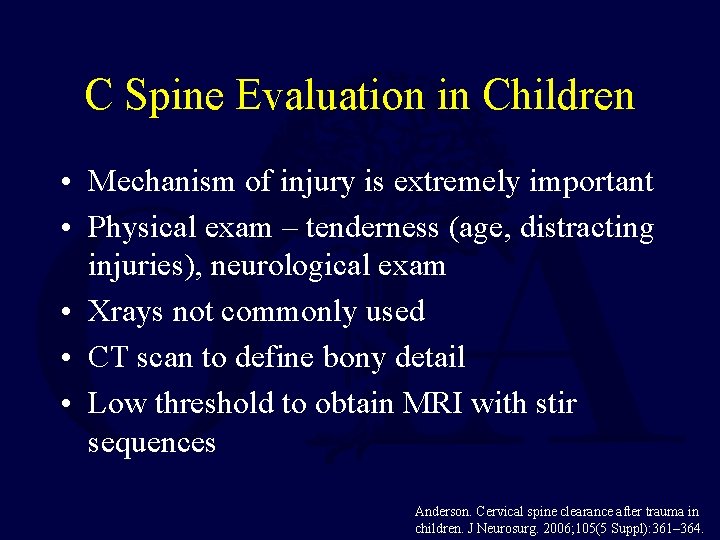
C Spine Evaluation in Children • Mechanism of injury is extremely important • Physical exam – tenderness (age, distracting injuries), neurological exam • Xrays not commonly used • CT scan to define bony detail • Low threshold to obtain MRI with stir sequences Anderson. Cervical spine clearance after trauma in children. J Neurosurg. 2006; 105(5 Suppl): 361– 364.
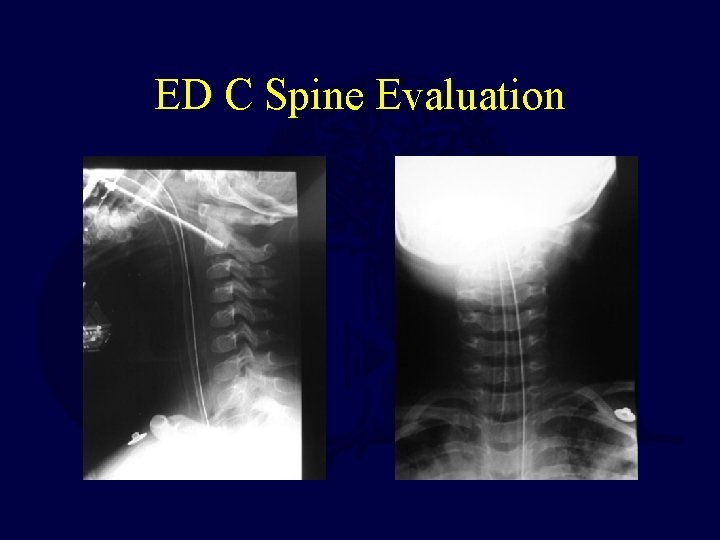
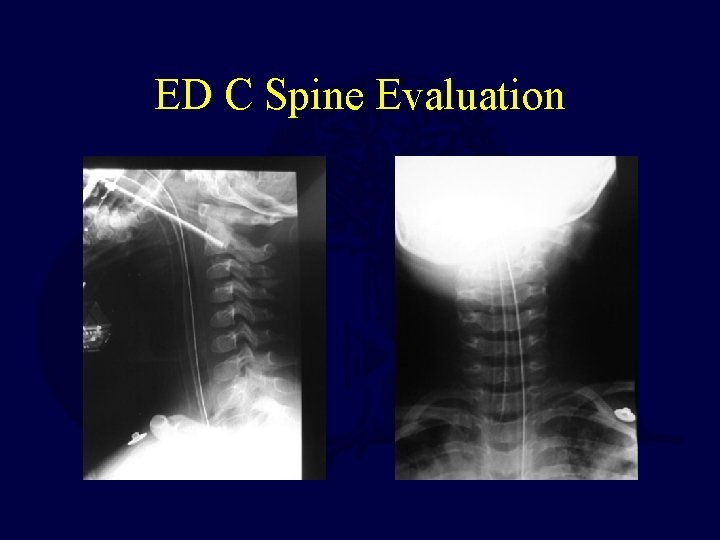
ED C Spine Evaluation
Traumatic Spinal Cord Injury • Rare in children • Better prognosis for recovery than adults • Treat aggressively with immobilization +/decompression • Late sequelae = paralytic scoliosis (almost all quadriplegic children if injured at less than 10 years of age) Parent. Spinal cord injury in the pediatric population: a systematic review of the literature. J. Neurotrauma. 2011; 28: 1515.
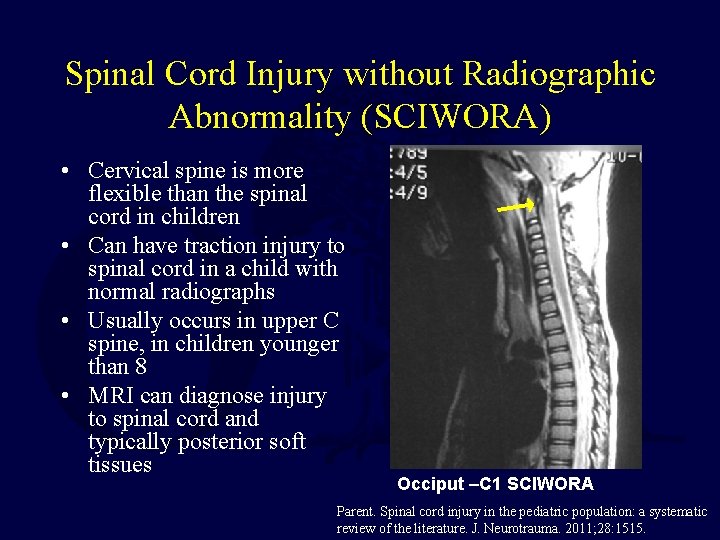
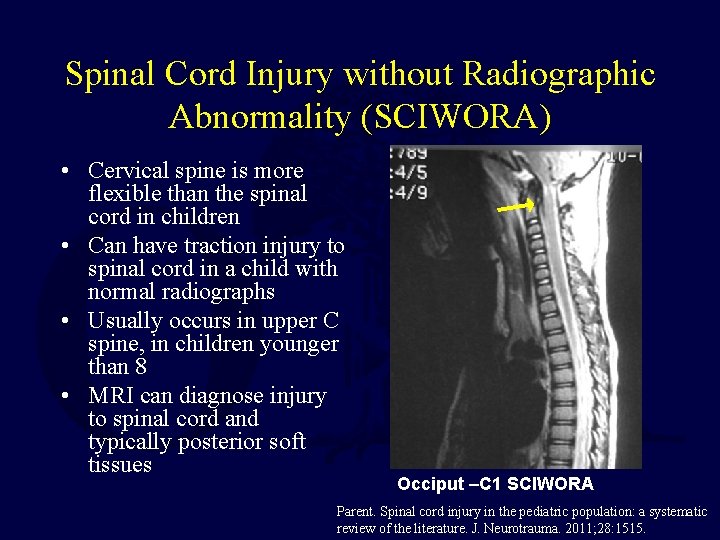
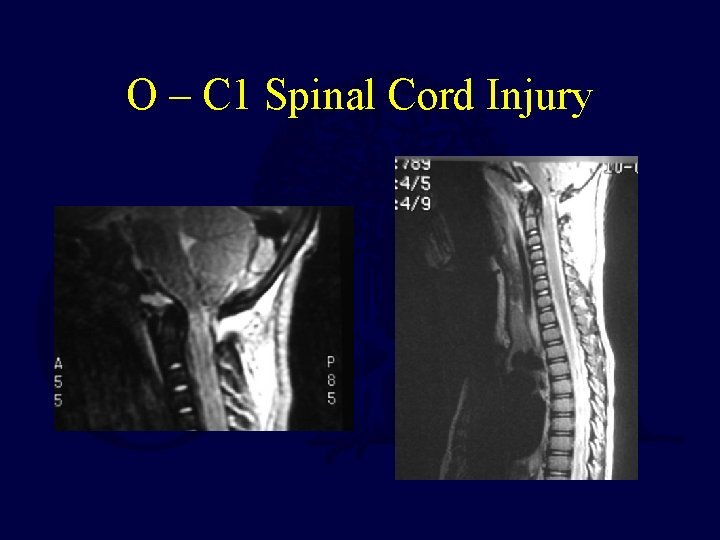
Spinal Cord Injury without Radiographic Abnormality (SCIWORA) • Cervical spine is more flexible than the spinal cord in children • Can have traction injury to spinal cord in a child with normal radiographs • Usually occurs in upper C spine, in children younger than 8 • MRI can diagnose injury to spinal cord and typically posterior soft tissues Occiput –C 1 SCIWORA Parent. Spinal cord injury in the pediatric population: a systematic review of the literature. J. Neurotrauma. 2011; 28: 1515.
SCIWORA • Spinal cord injury without radiographic abnormality – Plain x-rays, not MRI • Distraction mechanism of injury • Spinal cord least elastic structure • Young children less than 8 yrs • Be aware in patient with GCS 3 and normal CT head there may be upper cervical spinal cord injury!
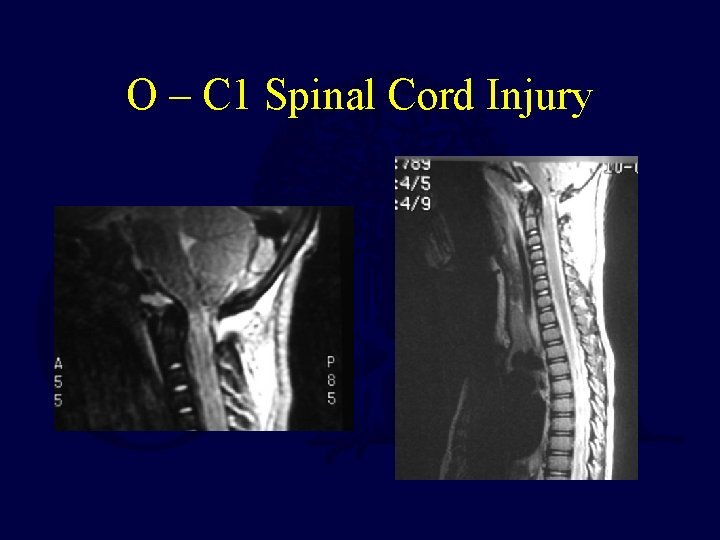
O – C 1 Spinal Cord Injury
Imaging • • 3 view plain film series still used Low threshold for further imaging CT scan upper C-spine (O-C 2) Consider MRI if intubated or obtunded Sharma. Assessment for additional spinal trauma in patients with cervical spine injury. Am Surg. 2007; 73: 70.
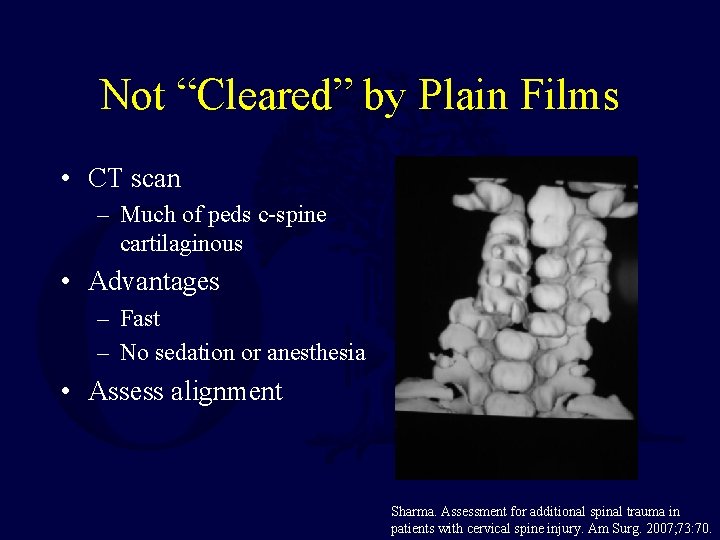
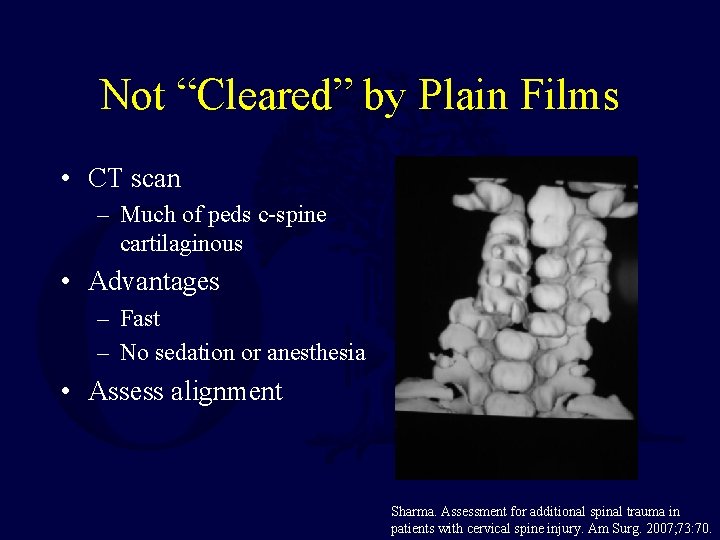
Not “Cleared” by Plain Films • CT scan – Much of peds c-spine cartilaginous • Advantages – Fast – No sedation or anesthesia • Assess alignment Sharma. Assessment for additional spinal trauma in patients with cervical spine injury. Am Surg. 2007; 73: 70.
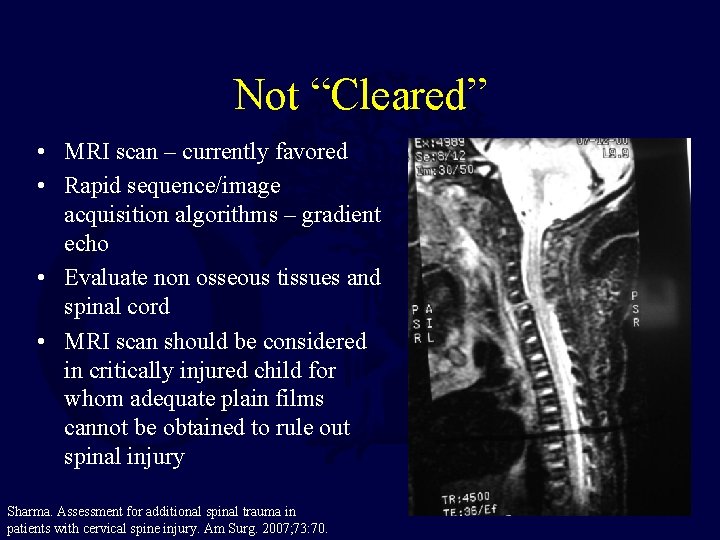
Not “Cleared” • MRI scan – currently favored • Rapid sequence/image acquisition algorithms – gradient echo • Evaluate non osseous tissues and spinal cord • MRI scan should be considered in critically injured child for whom adequate plain films cannot be obtained to rule out spinal injury Sharma. Assessment for additional spinal trauma in patients with cervical spine injury. Am Surg. 2007; 73: 70.
If not “Cleared” within 12 Hours • Switch to pediatric Aspen or Miami J collar • Consider CT or MRI Mc. Call. Cervical spine trauma in children: a review. Neurosurg Focus. 2006; 20(2): E 5.
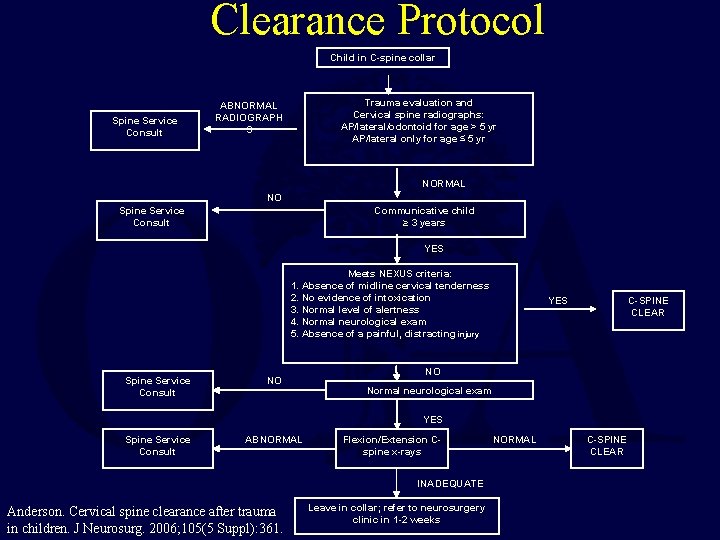
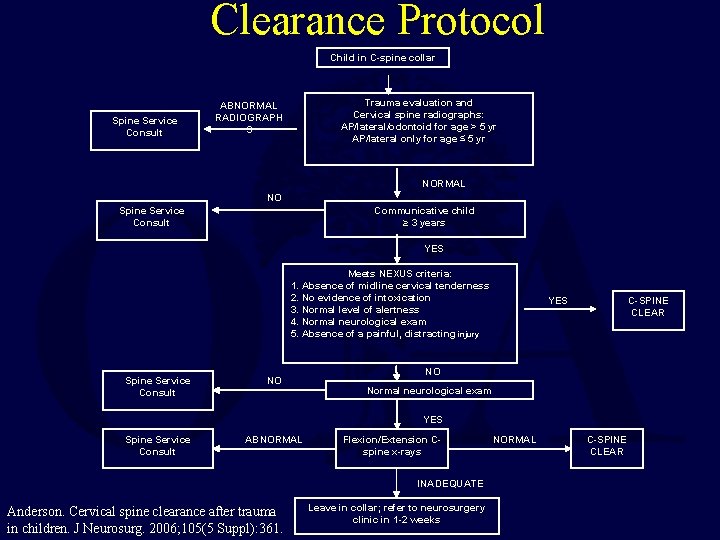
Clearance Protocol Child in C-spine collar Spine Service Consult Trauma evaluation and Cervical spine radiographs: AP/lateral/odontoid for age > 5 yr AP/lateral only for age ≤ 5 yr ABNORMAL RADIOGRAPH S NORMAL NO Spine Service Consult Communicative child ≥ 3 years YES Meets NEXUS criteria: 1. Absence of midline cervical tenderness 2. No evidence of intoxication 3. Normal level of alertness 4. Normal neurological exam 5. Absence of a painful, distracting injury Spine Service Consult NO YES C-SPINE CLEAR NO Normal neurological exam YES Spine Service Consult ABNORMAL Flexion/Extension Cspine x-rays INADEQUATE Anderson. Cervical spine clearance after trauma in children. J Neurosurg. 2006; 105(5 Suppl): 361. Leave in collar; refer to neurosurgery clinic in 1 -2 weeks NORMAL C-SPINE CLEAR
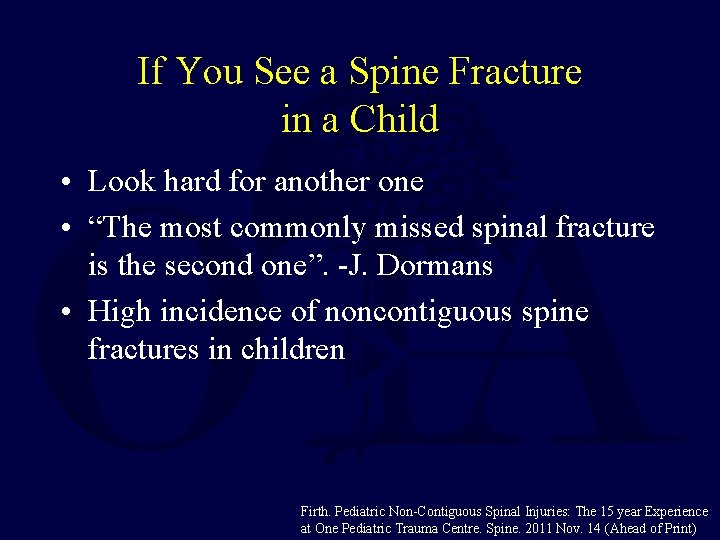
If You See a Spine Fracture in a Child • Look hard for another one • “The most commonly missed spinal fracture is the second one”. -J. Dormans • High incidence of noncontiguous spine fractures in children Firth. Pediatric Non-Contiguous Spinal Injuries: The 15 year Experience at One Pediatric Trauma Centre. Spine. 2011 Nov. 14 (Ahead of Print)
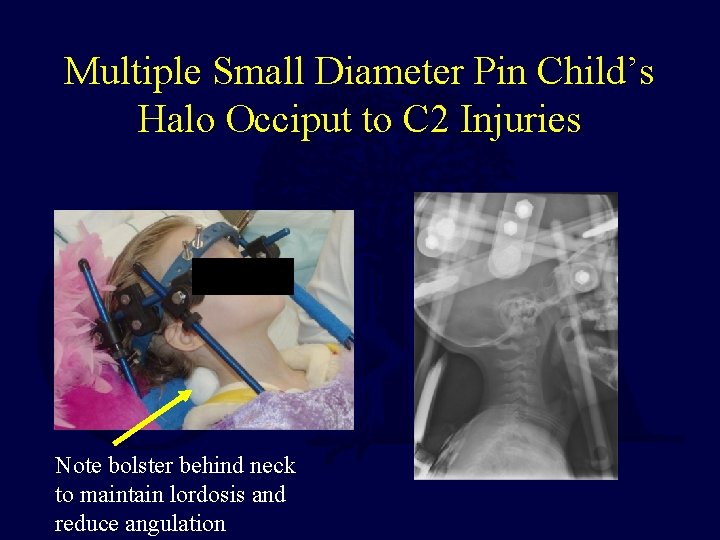
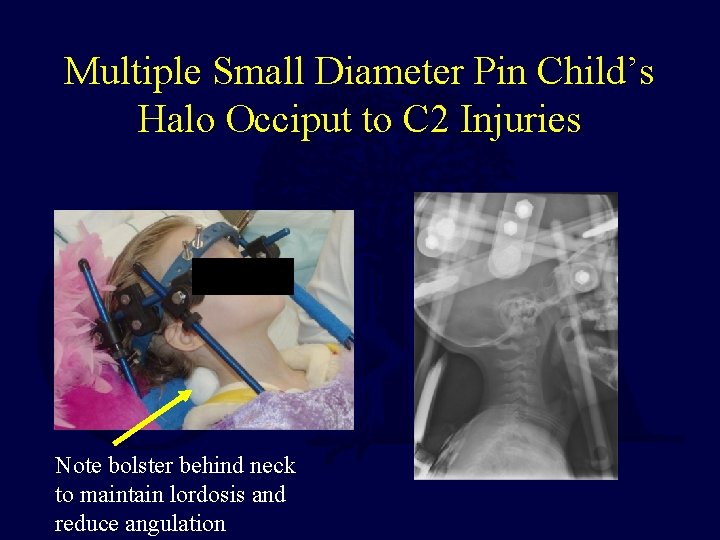
Multiple Small Diameter Pin Child’s Halo Occiput to C 2 Injuries Note bolster behind neck to maintain lordosis and reduce angulation
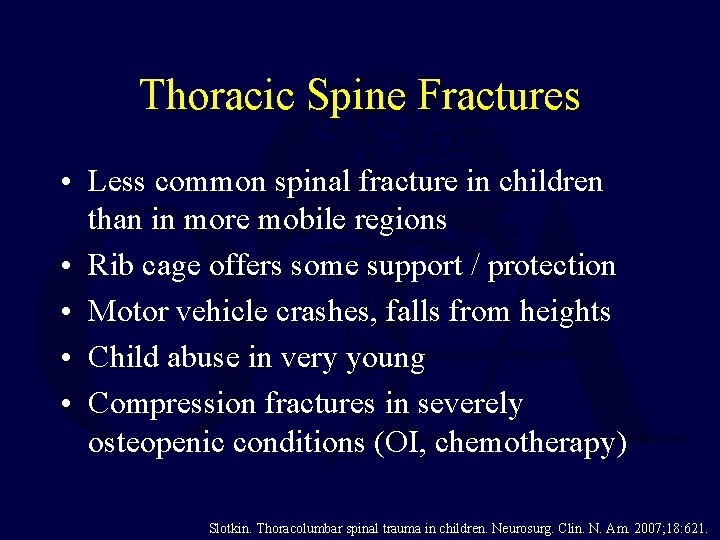
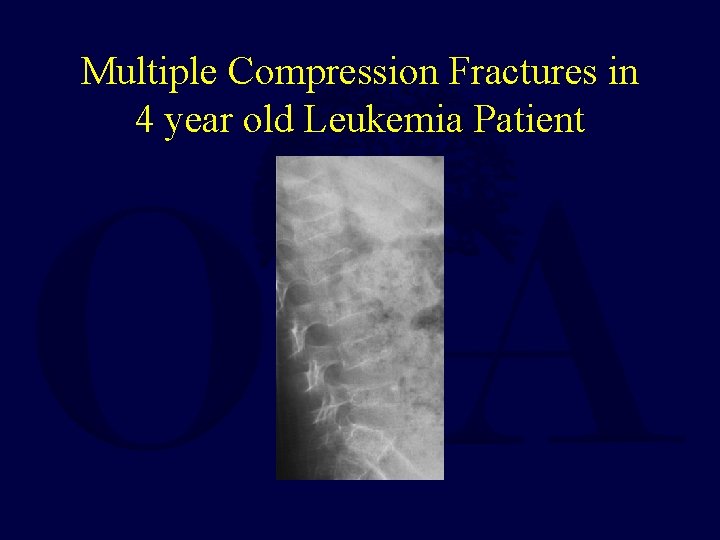
Thoracic Spine Fractures • Less common spinal fracture in children than in more mobile regions • Rib cage offers some support / protection • Motor vehicle crashes, falls from heights • Child abuse in very young • Compression fractures in severely osteopenic conditions (OI, chemotherapy) Slotkin. Thoracolumbar spinal trauma in children. Neurosurg. Clin. N. Am. 2007; 18: 621.
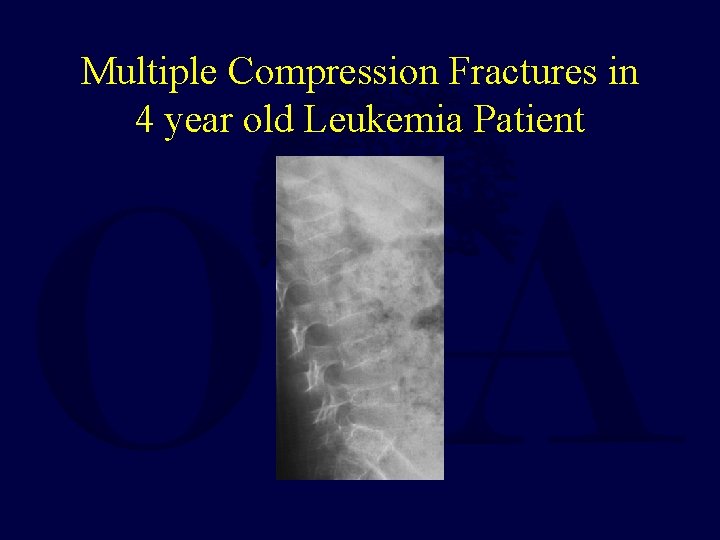
Multiple Compression Fractures in 4 year old Leukemia Patient
Thoracic Spine Fracture Dislocations • High energy mechanisms • Often spinal cord injury, can be transected • Prognosis for recovery most dependent on initial exam – complete deficits unlikely to have recovery • Infarction of cord (artery of Adamkiewicz) may play some role –especially in delayed paraplegia Slotkin. Thoracolumbar spinal trauma in children. Neurosurg. Clin. N. Am. 2007; 18: 621.
Thoracolumbar Junction Injuries T 11 -L 2 • Classically lap-belt flexion-distraction injuries • Chance fractures and variants • High association with intraabdominal injury (50 -90%) • Neurologic injury infrequent but can occur Arkader. Pediatric chance fractures: a multicenter perspective. J Pediatr Orthop. 2011; 31: 741.
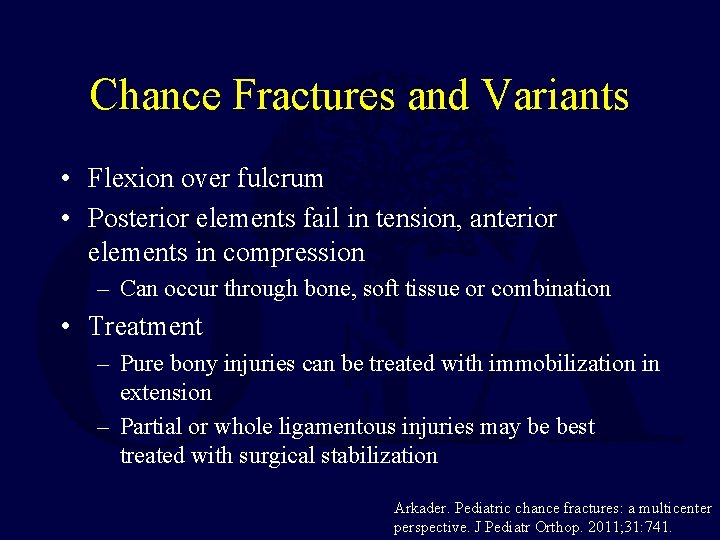
Chance Fractures and Variants • Flexion over fulcrum • Posterior elements fail in tension, anterior elements in compression – Can occur through bone, soft tissue or combination • Treatment – Pure bony injuries can be treated with immobilization in extension – Partial or whole ligamentous injuries may be best treated with surgical stabilization Arkader. Pediatric chance fractures: a multicenter perspective. J Pediatr Orthop. 2011; 31: 741.
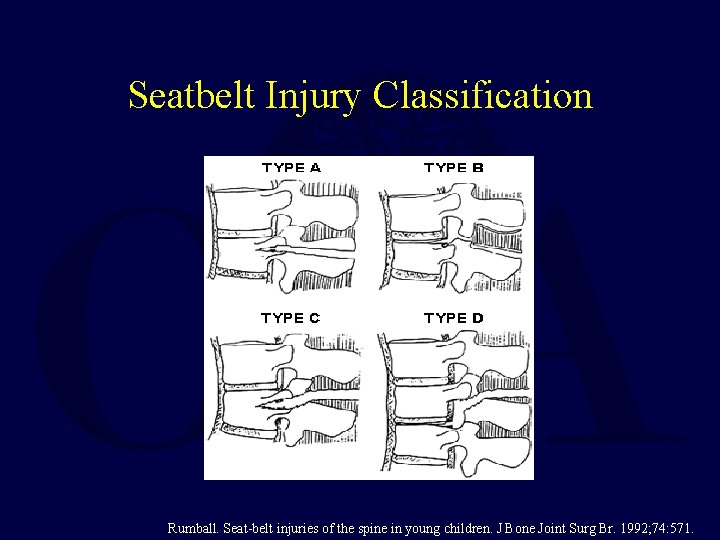
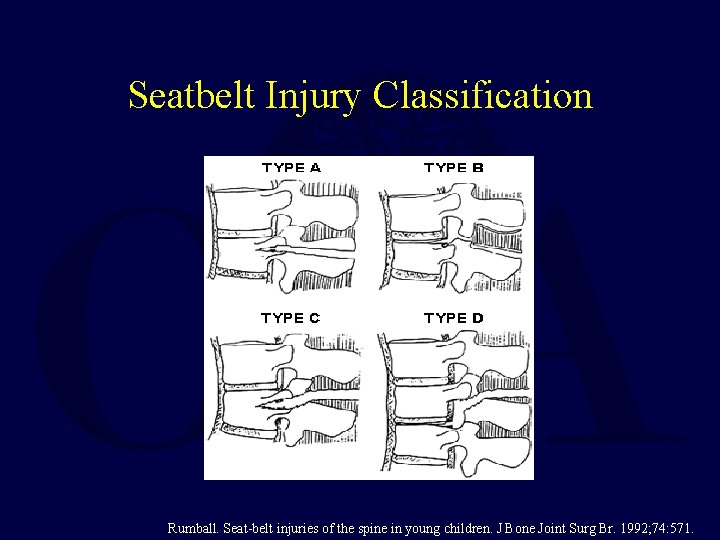
Seatbelt Injury Classification Rumball. Seat-belt injuries of the spine in young children. J Bone Joint Surg Br. 1992; 74: 571.
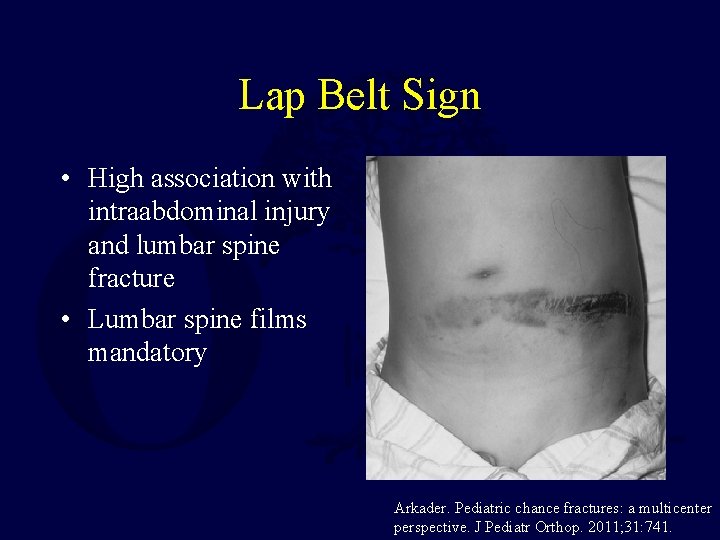
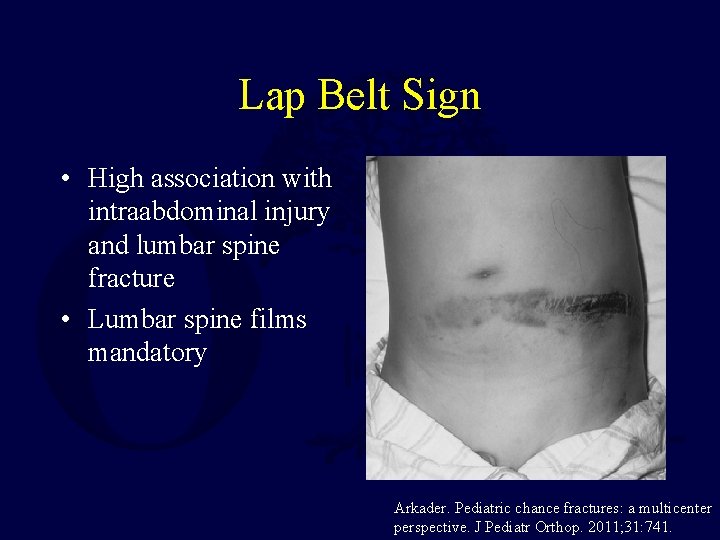
Lap Belt Sign • High association with intraabdominal injury and lumbar spine fracture • Lumbar spine films mandatory Arkader. Pediatric chance fractures: a multicenter perspective. J Pediatr Orthop. 2011; 31: 741.

4 yo Lap Belt Restrained Passenger Intraabdominal Injuries, Paraplegic
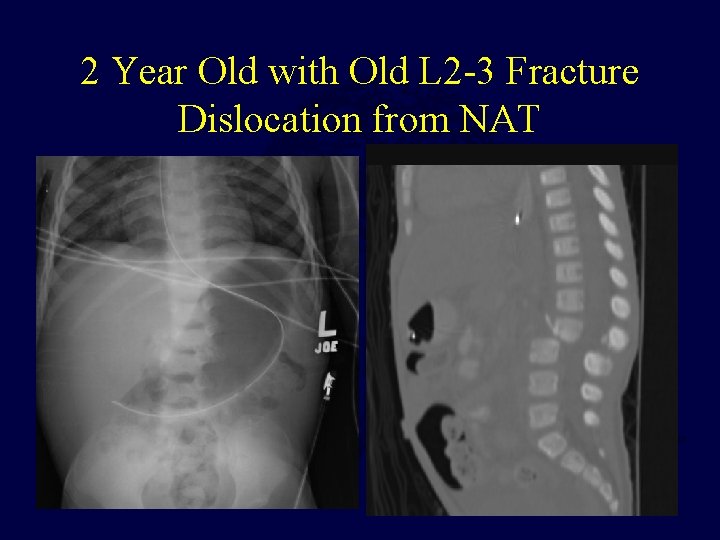
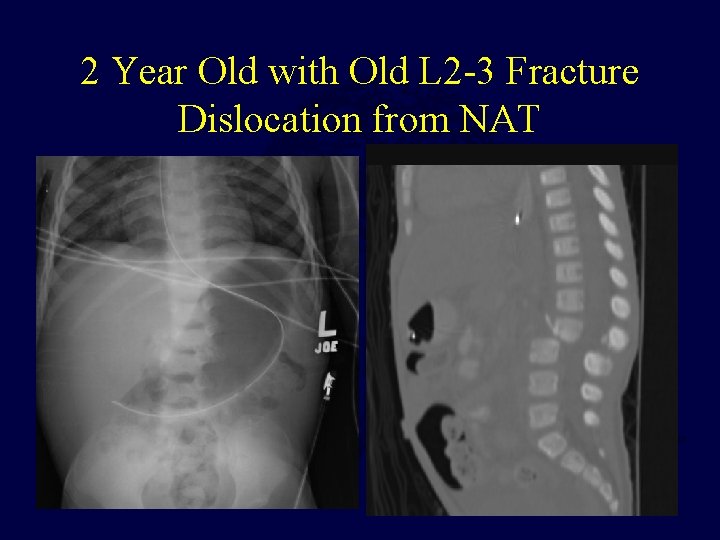
2 Year Old with Old L 2 -3 Fracture Dislocation from NAT
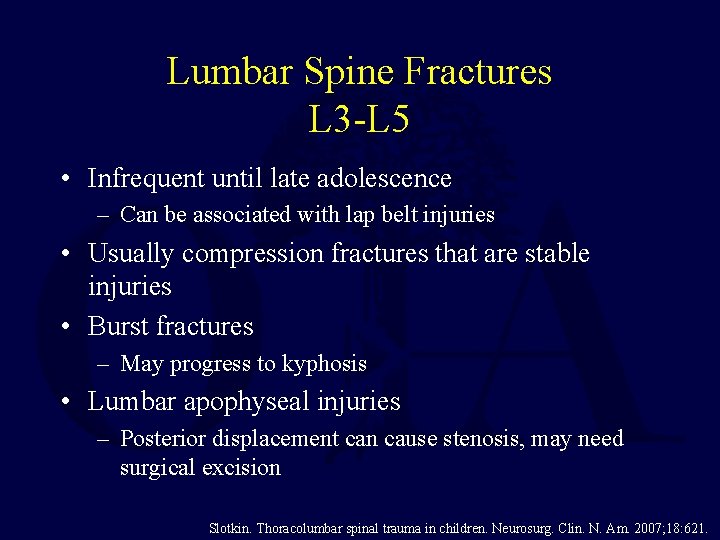
Lumbar Spine Fractures L 3 -L 5 • Infrequent until late adolescence – Can be associated with lap belt injuries • Usually compression fractures that are stable injuries • Burst fractures – May progress to kyphosis • Lumbar apophyseal injuries – Posterior displacement can cause stenosis, may need surgical excision Slotkin. Thoracolumbar spinal trauma in children. Neurosurg. Clin. N. Am. 2007; 18: 621.

Flexion-Distraction Injury L 2 -L 3 6 Months after Compression Fixation, Posterolateral Fusion
Lumbar Apophyseal Injuries Slipped Apophysis • Compression-shear injuries • Same age group as SCFE • Typically adolescent males, inferior endplates of L 4 or L 5 • Traumatic displacement of vertebral ring apophysis and disc into spinal canal • If causes significant compression of cauda equina, treatment is surgical excision Chang. Clinical significance of ring apophysis fracture in adolescent lumbar disc herniation. Spine. 2008; 33: 1750.
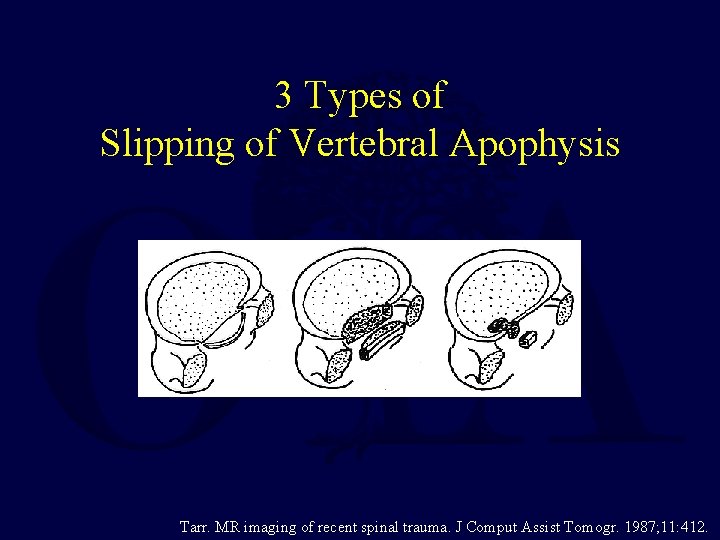
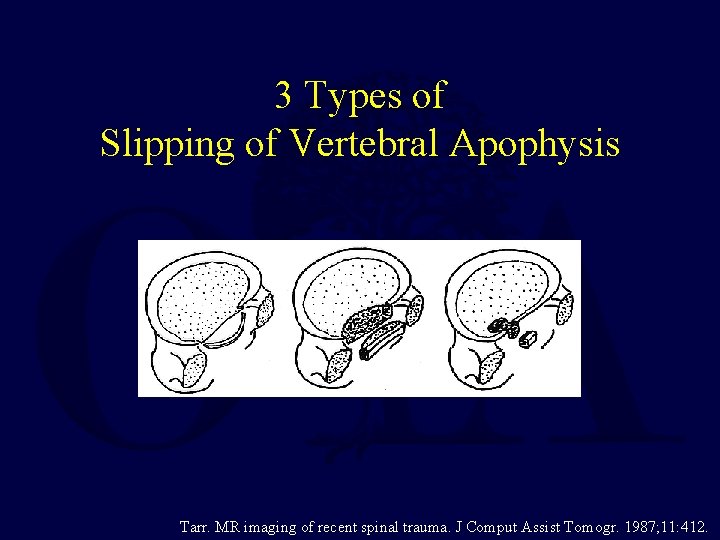
3 Types of Slipping of Vertebral Apophysis Tarr. MR imaging of recent spinal trauma. J Comput Assist Tomogr. 1987; 11: 412.
Burst Fractures • Usually in older adolescents • Treatment similar to adults • May not need surgery in neurologically intact patient • Injuries at thoracolumbar junction higher risk for progressive kyphosis Slotkin. Thoracolumbar spinal trauma in children. Neurosurg. Clin. N. Am. 2007; 18: 621.
Bibliography • • • Anderson RCE, Scaife ER, Fenton SJ, Kan P, Hansen KW, Brockmeyer DL. Cervical spine clearance after trauma in children. J Neurosurg. 2006 Nov. ; 105(5 Suppl): 361– 364. Arkader A, Warner WC, Tolo VT, Sponseller PD, Skaggs DL. Pediatric chance fractures: a multicenter perspective. J Pediatr Orthop. 2011 Sep. ; 31(7): 741– 744. Chang C-H, Lee Z-L, Chen W-J, Tan C-F, Chen L-H. Clinical significance of ring apophysis fracture in adolescent lumbar disc herniation. Spine. 2008 Jul. 15; 33(16): 1750– 1754. Copley LA, Dormans JP. Cervical spine disorders in infants and children. J Am Acad Orthop Surg. 1998 Jun. ; 6(4): 204– 214. Eubanks JD, Gilmore A, Bess S, Cooperman DR: Clearing the pediatric cervical spine following injury. J Am Acad Orthop Surg 2006; 14(9): 552 -564. Fielding JWHensinger RN, Hawkins RJ: Os odontoideum. J Bone Joint Surg Am 1980; 62: 376 -383. Firth GB, Kingwell S, Moroz P. Pediatric Non-Contiguous Spinal Injuries: The 15 year Experience at One Pediatric Trauma Centre. Spine. 2011 Nov. 14 (Ahead of Print) Jones TM, Anderson PA, Noonan KJ. Pediatric cervical spine trauma. J Am Acad Orthop Surg. 2011 Oct. ; 19(10): 600– 611. Mc. Call T, Fassett D, Brockmeyer D. Cervical spine trauma in children: a review. Neurosurg Focus. 2006; 20(2): E 5. Parent S, Mac-Thiong J-M, Roy-Beaudry M, Sosa JF, Labelle H. Spinal cord injury in the pediatric population: a systematic review of the literature. J. Neurotrauma. 2011 Aug. ; 28(8): 1515– 1524.
Bibliography • • • Rumball K, Jarvis J. Seat-belt injuries of the spine in young children. J Bone Joint Surg Br. 1992 Jul. ; 74(4): 571– 574. Sharma OP, Oswanski MF, Yazdi JS, Jindal S, Taylor M. Assessment for additional spinal trauma in patients with cervical spine injury. Am Surg. 2007 Jan. ; 73(1): 70– 74. Shaw M, Burnett H, Wilson A, Chan O: Pseudosubluxation of C 2 on C 3 in polytraumatized children: Prevalence and significance. Clin Radiol 1999; 54(6): 377 -380. Slotkin JR, Lu Y, Wood KB. Thoracolumbar spinal trauma in children. Neurosurg. Clin. N. Am. 2007 Oct. ; 18(4): 621– 630. Tarr RW, Drolshagen LF, Kerner TC, Allen JH, Partain CL, James AE. MR imaging of recent spinal trauma. J Comput Assist Tomogr. 1987 Apr. ; 11(3): 412– 417. If you would like to volunteer as an author for the Resident Slide Project or recommend updates to any of the following slides, please send an email to ota@ota. org Return to Pediatrics Index
 Timothy moore md
Timothy moore md Dr sukhpal singh
Dr sukhpal singh Ao classification of fractures
Ao classification of fractures Ilioposas
Ilioposas Bone cancer fractures
Bone cancer fractures Bobine d andrieu
Bobine d andrieu Irving olecranon fractures
Irving olecranon fractures Open fracture treatment
Open fracture treatment Fracture sus condylienne
Fracture sus condylienne Acetabulum ossification
Acetabulum ossification Panfacial fractures sequencing
Panfacial fractures sequencing Weber classification
Weber classification Concentric fractures
Concentric fractures Lisa cannada md
Lisa cannada md Classification tile bassin
Classification tile bassin Types of glass fractures
Types of glass fractures Daniel tibia
Daniel tibia Glass analysis in forensic science
Glass analysis in forensic science Tubular shaft of a long bone
Tubular shaft of a long bone Canthatomy
Canthatomy Chest tube placement
Chest tube placement Late complications of fractures
Late complications of fractures Pqrst pain scale
Pqrst pain scale Spine vs thorn
Spine vs thorn Schober's test positive
Schober's test positive Peripheral nerves
Peripheral nerves Spine meninges
Spine meninges Frankel a b c d e
Frankel a b c d e Lumbar referral patterns
Lumbar referral patterns Pubic arch
Pubic arch Chapter 20 worksheet the spine
Chapter 20 worksheet the spine Boney spine
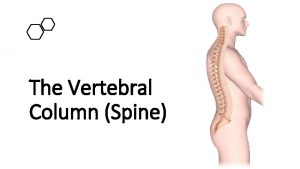
Boney spine 7 12 5 spine
7 12 5 spine Harborside spine and sports
Harborside spine and sports Maxillary sinus
Maxillary sinus Emory spine center
Emory spine center Mental spine of mandible
Mental spine of mandible Interalveolar septa mandible
Interalveolar septa mandible Rattle spine nms
Rattle spine nms Strickler spine and sport
Strickler spine and sport Spine blood spatter definition
Spine blood spatter definition Mental spine
Mental spine Spine palpation landmarks
Spine palpation landmarks Spine store layout
Spine store layout Trunk extensors
Trunk extensors Fabrics on ethernet
Fabrics on ethernet Who made the griffin ford model
Who made the griffin ford model Iliac tubercle
Iliac tubercle