Faculty of Medicine Health Economics and Policies 31505391

- Slides: 87
Faculty of Medicine Health Economics and Policies (31505391) Economic Evaluation By Hatim Jaber MD MPH JBCM Ph. D 2 + 4 - 04 - 2018 1
World Health Day - 7 April 2018
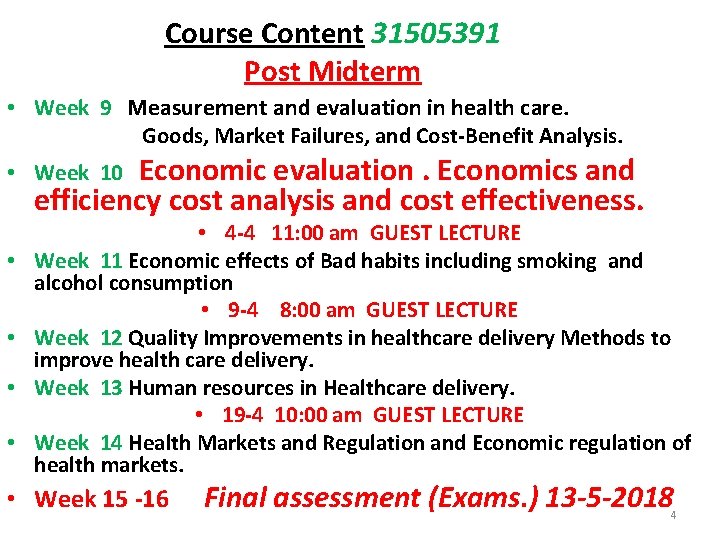
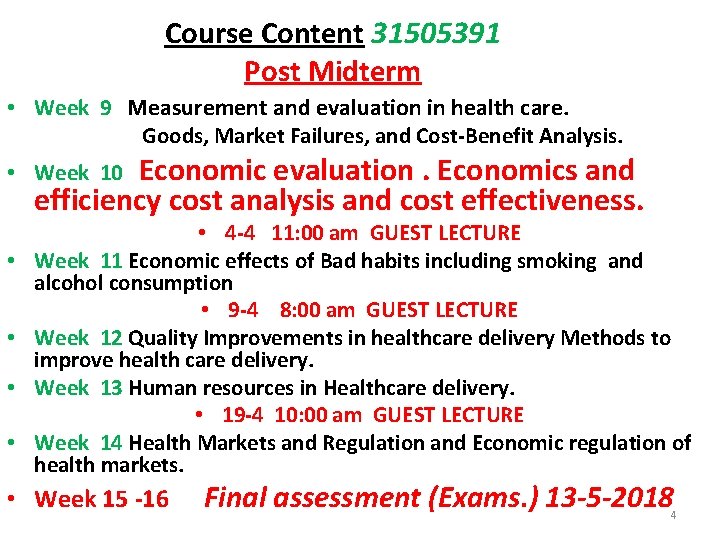
Course Content 31505391 Post Midterm • Week 9 Measurement and evaluation in health care. Goods, Market Failures, and Cost-Benefit Analysis. Economic evaluation. Economics and efficiency cost analysis and cost effectiveness. • Week 10 • • • 4 -4 11: 00 am GUEST LECTURE Week 11 Economic effects of Bad habits including smoking and alcohol consumption • 9 -4 8: 00 am GUEST LECTURE Week 12 Quality Improvements in healthcare delivery Methods to improve health care delivery. Week 13 Human resources in Healthcare delivery. • 19 -4 10: 00 am GUEST LECTURE Week 14 Health Markets and Regulation and Economic regulation of health markets. • Week 15 -16 Final assessment (Exams. ) 13 -5 -2018 4
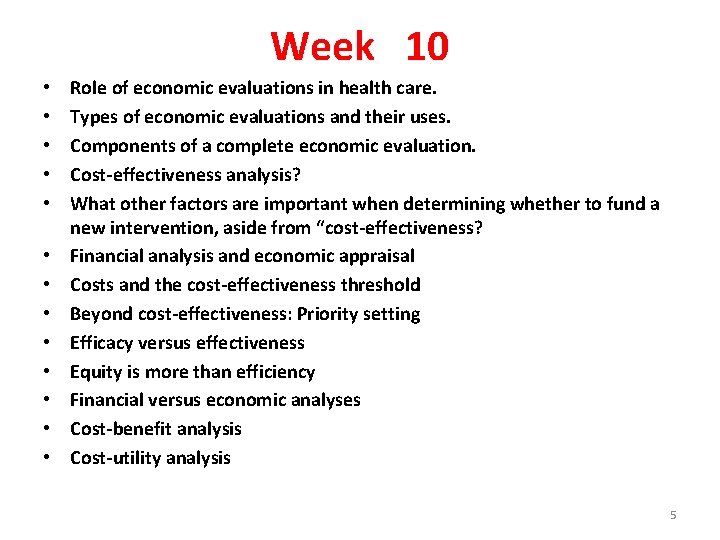
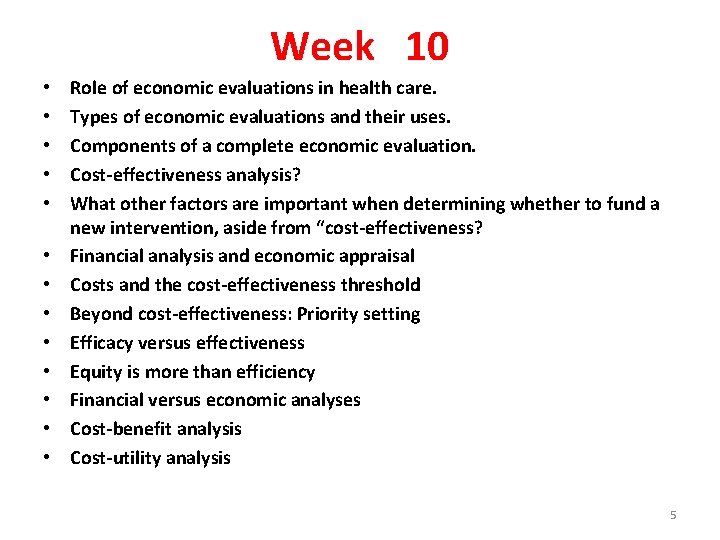
Week 10 • • • • Role of economic evaluations in health care. Types of economic evaluations and their uses. Components of a complete economic evaluation. Cost-effectiveness analysis? What other factors are important when determining whether to fund a new intervention, aside from “cost-effectiveness? Financial analysis and economic appraisal Costs and the cost-effectiveness threshold Beyond cost-effectiveness: Priority setting Efficacy versus effectiveness Equity is more than efficiency Financial versus economic analyses Cost-benefit analysis Cost-utility analysis 5
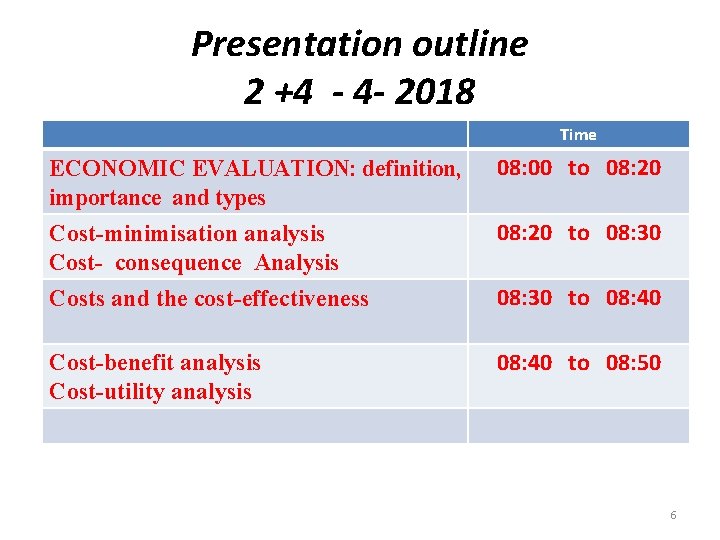
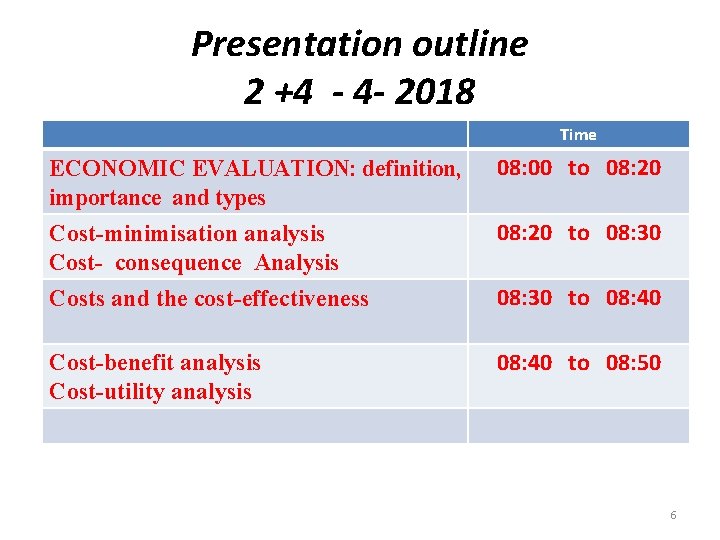
Presentation outline 2 +4 - 4 - 2018 Time ECONOMIC EVALUATION: definition, importance and types 08: 00 to 08: 20 Cost-minimisation analysis Cost- consequence Analysis 08: 20 to 08: 30 Costs and the cost-effectiveness 08: 30 to 08: 40 Cost-benefit analysis Cost-utility analysis 08: 40 to 08: 50 6
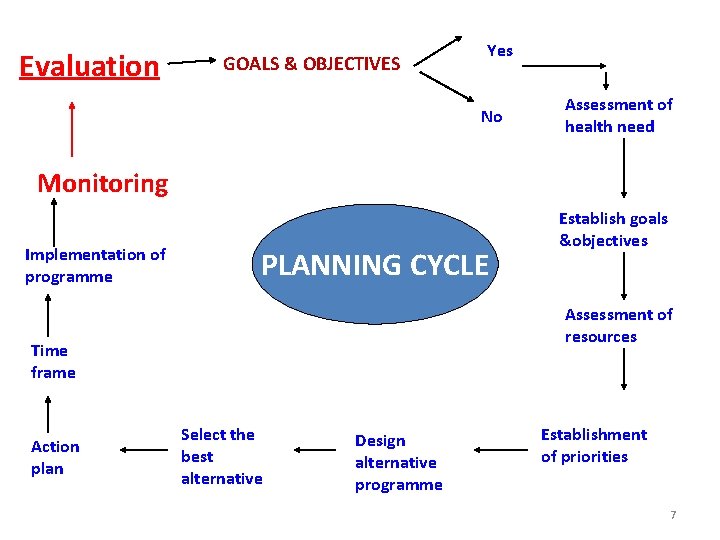
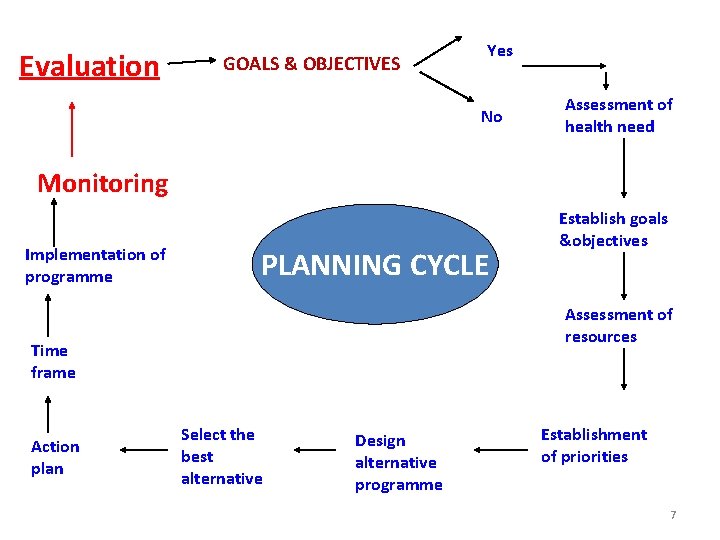
Evaluation GOALS & OBJECTIVES Yes No Assessment of health need Monitoring Implementation of programme PLANNING CYCLE Assessment of resources Time frame Action plan Establish goals &objectives Select the best alternative Design alternative programme Establishment of priorities 7
EVALUATION It is a systematic way of: - learning from experience and -using the lessons learnt to: improve current activities and promote better planning by careful selection of alternatives for future action 8
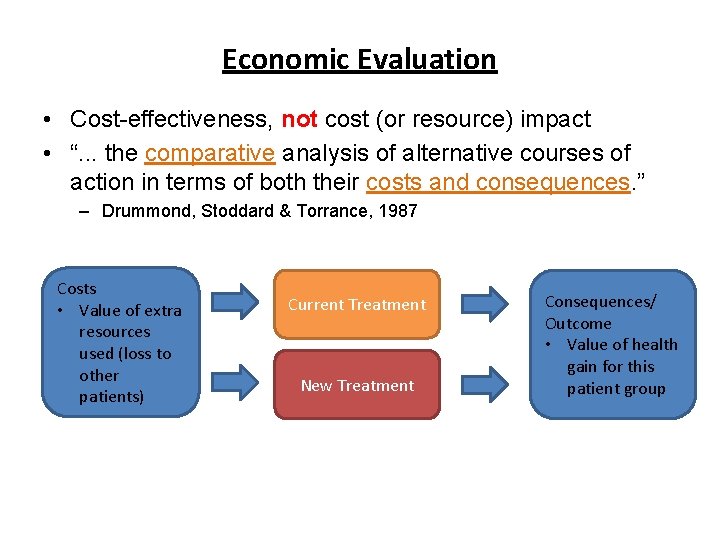
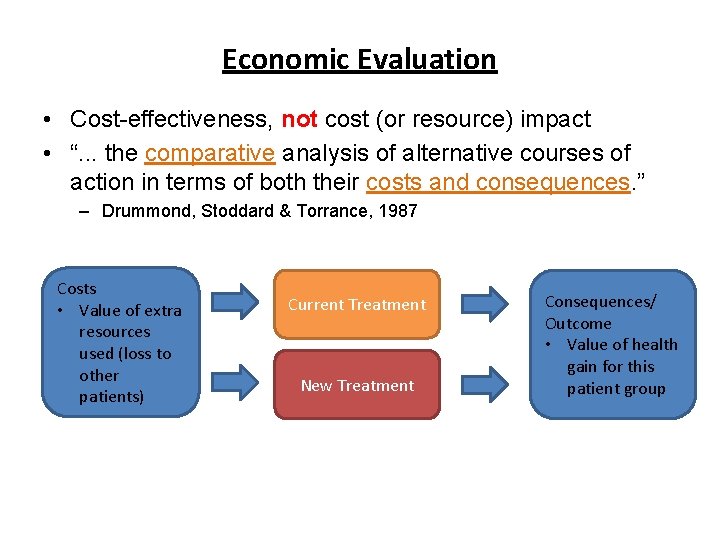
Economic Evaluation • Cost-effectiveness, not cost (or resource) impact • “. . . the comparative analysis of alternative courses of action in terms of both their costs and consequences. ” – Drummond, Stoddard & Torrance, 1987 Costs • Value of extra resources used (loss to other patients) Current Treatment New Treatment Consequences/ Outcome • Value of health gain for this patient group
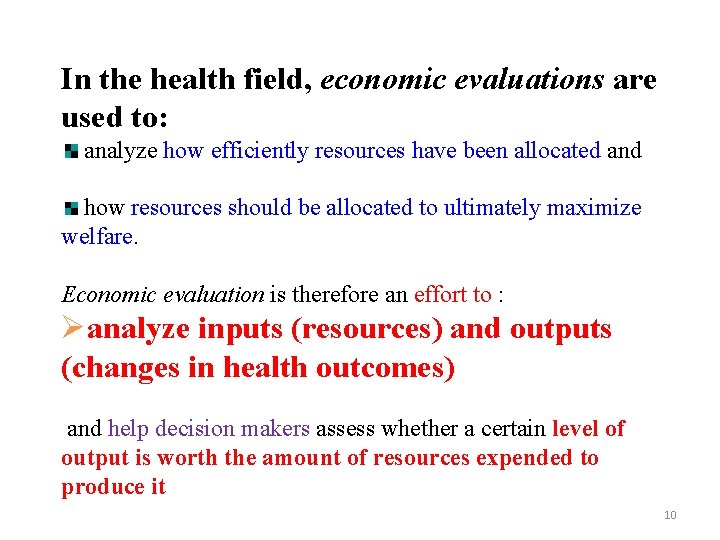
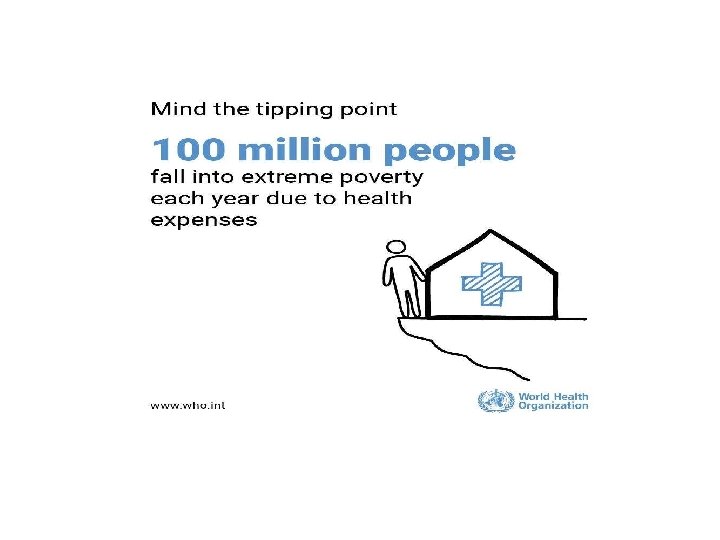
In the health field, economic evaluations are used to: analyze how efficiently resources have been allocated and how resources should be allocated to ultimately maximize welfare. Economic evaluation is therefore an effort to : Øanalyze inputs (resources) and outputs (changes in health outcomes) and help decision makers assess whether a certain level of output is worth the amount of resources expended to produce it 10
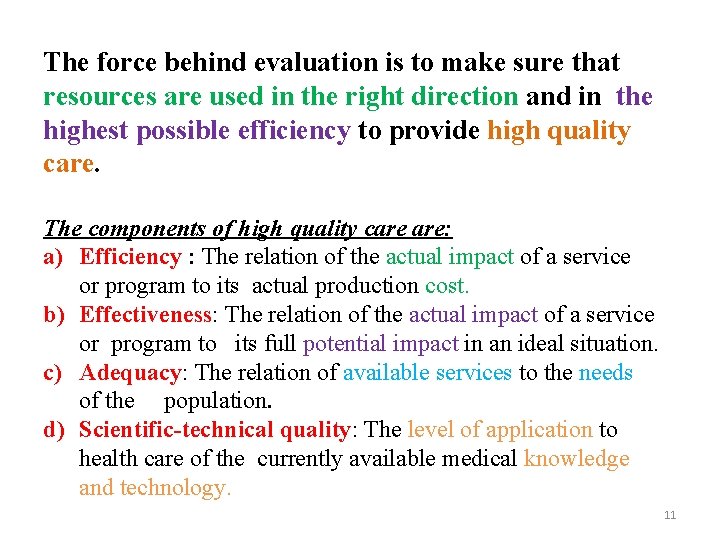
The force behind evaluation is to make sure that resources are used in the right direction and in the highest possible efficiency to provide high quality care. The components of high quality care are: a) Efficiency : The relation of the actual impact of a service or program to its actual production cost. b) Effectiveness: The relation of the actual impact of a service or program to its full potential impact in an ideal situation. c) Adequacy: The relation of available services to the needs of the population. d) Scientific-technical quality: The level of application to health care of the currently available medical knowledge and technology. 11
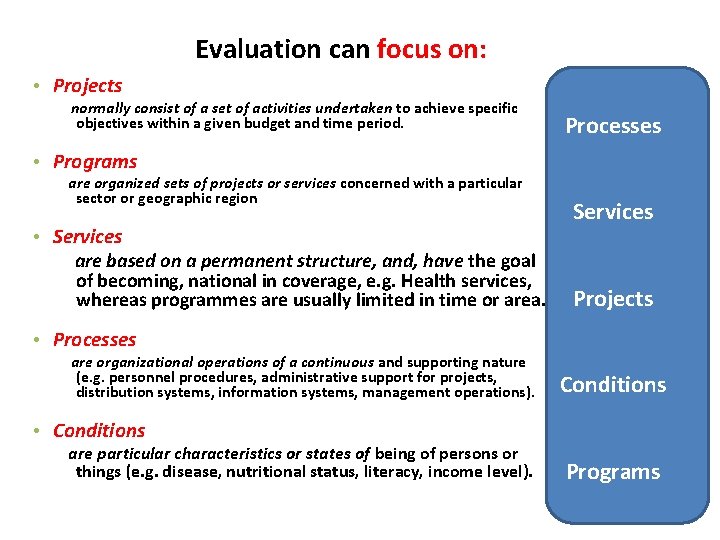
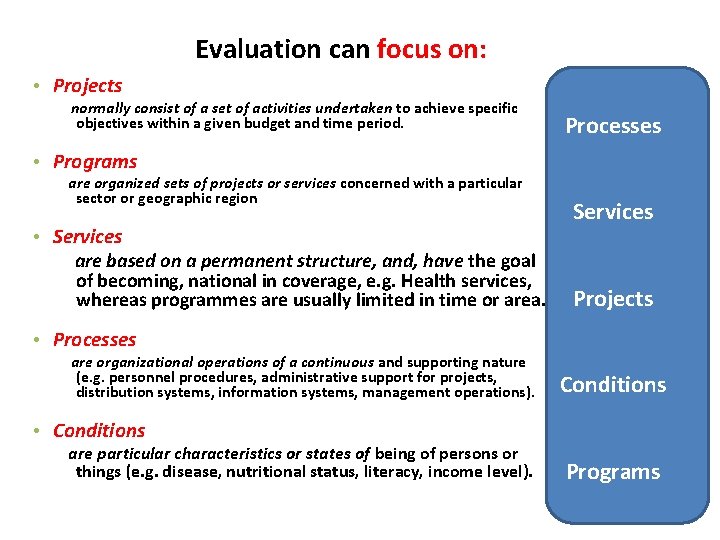
Evaluation can focus on: • Projects normally consist of a set of activities undertaken to achieve specific objectives within a given budget and time period. Processes • Programs are organized sets of projects or services concerned with a particular sector or geographic region • Services are based on a permanent structure, and, have the goal of becoming, national in coverage, e. g. Health services, whereas programmes are usually limited in time or area. Services Projects • Processes are organizational operations of a continuous and supporting nature (e. g. personnel procedures, administrative support for projects, distribution systems, information systems, management operations). Conditions • Conditions are particular characteristics or states of being of persons or things (e. g. disease, nutritional status, literacy, income level). Programs
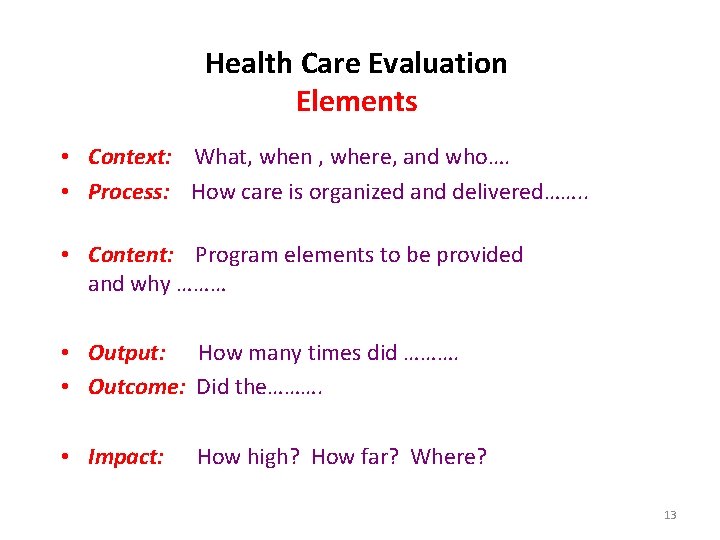
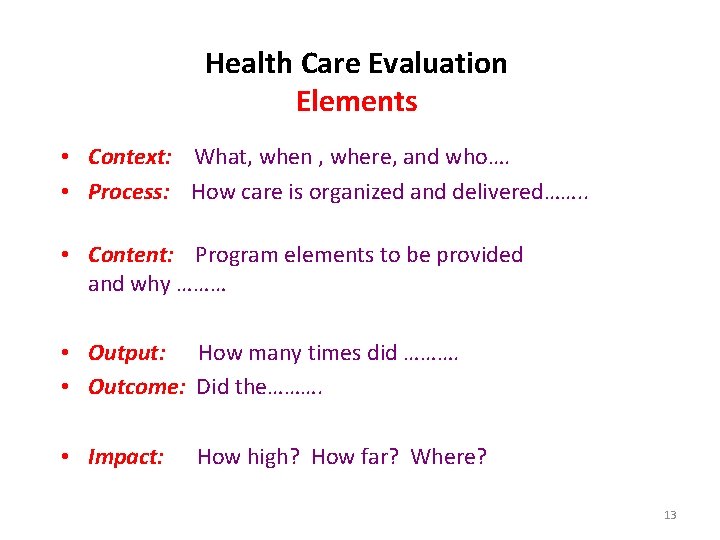
Health Care Evaluation Elements • Context: What, when , where, and who…. • Process: How care is organized and delivered……. . • Content: Program elements to be provided and why ……… • Output: How many times did ………. • Outcome: Did the………. • Impact: How high? How far? Where? 13
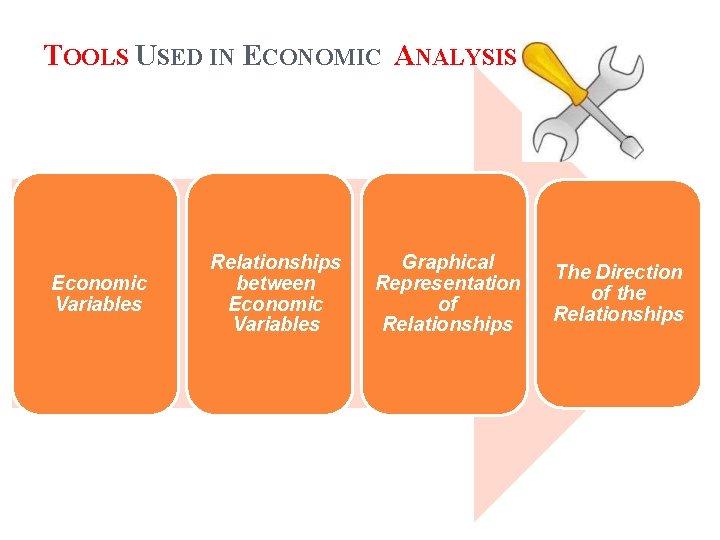
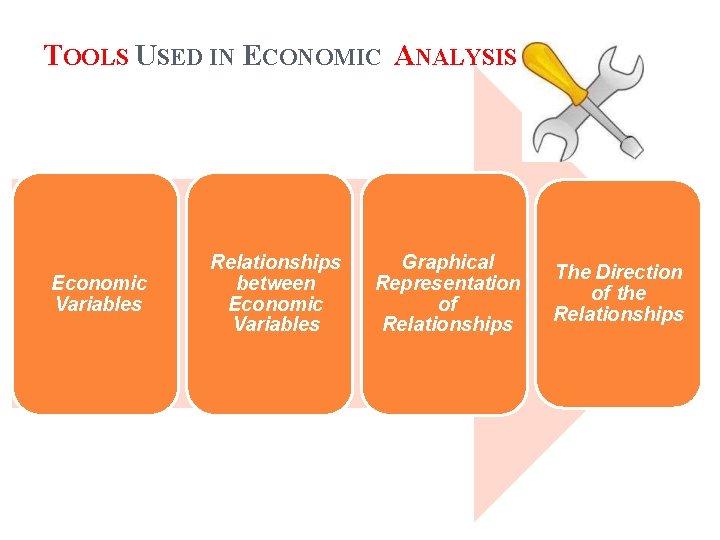
TOOLS USED IN ECONOMIC ANALYSIS Economic Variables Relationships between Economic Variables Graphical Representation of Relationships The Direction of the Relationships
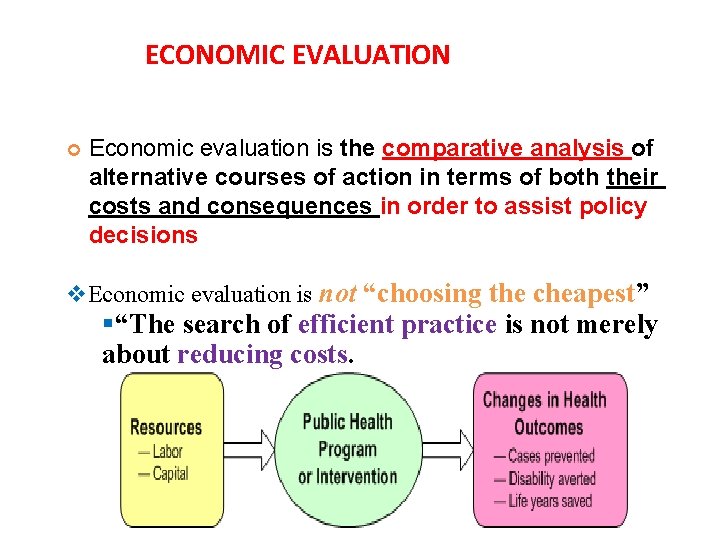
ECONOMIC EVALUATION Economic evaluation is the comparative analysis of alternative courses of action in terms of both their costs and consequences in order to assist policy decisions v. Economic evaluation is not “choosing the cheapest” §“The search of efficient practice is not merely about reducing costs.
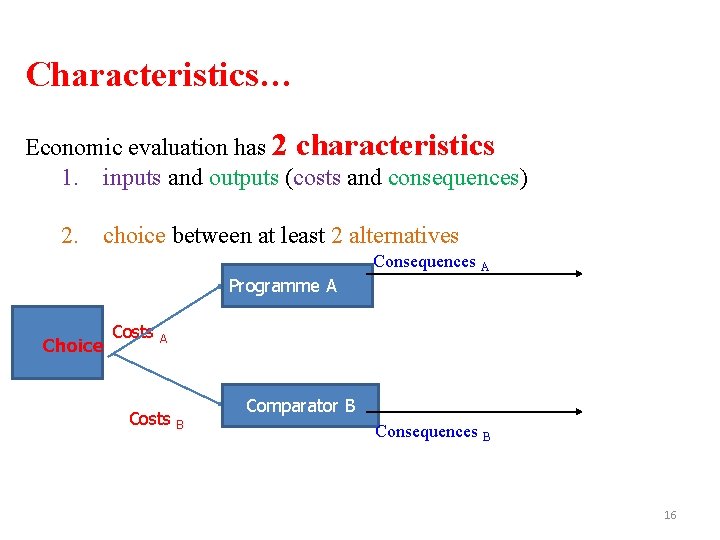
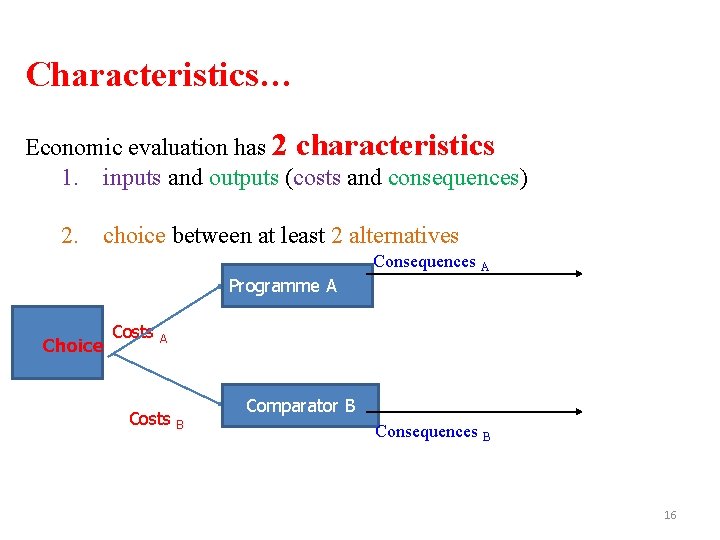
Characteristics… Economic evaluation has 2 characteristics 1. inputs and outputs (costs and consequences) 2. choice between at least 2 alternatives Consequences A Programme A Choice Costs A Costs Comparator B B Consequences B 16
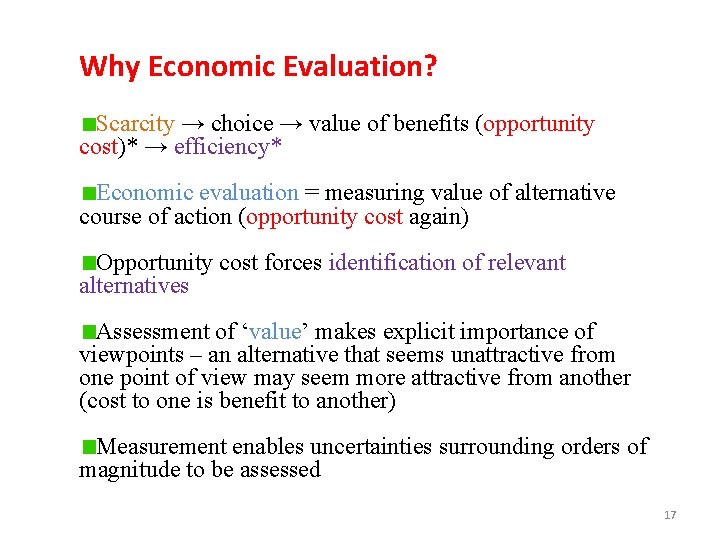
Why Economic Evaluation? Scarcity → choice → value of benefits (opportunity cost)* → efficiency* Economic evaluation = measuring value of alternative course of action (opportunity cost again) Opportunity cost forces identification of relevant alternatives Assessment of ‘value’ makes explicit importance of viewpoints – an alternative that seems unattractive from one point of view may seem more attractive from another (cost to one is benefit to another) Measurement enables uncertainties surrounding orders of magnitude to be assessed 17
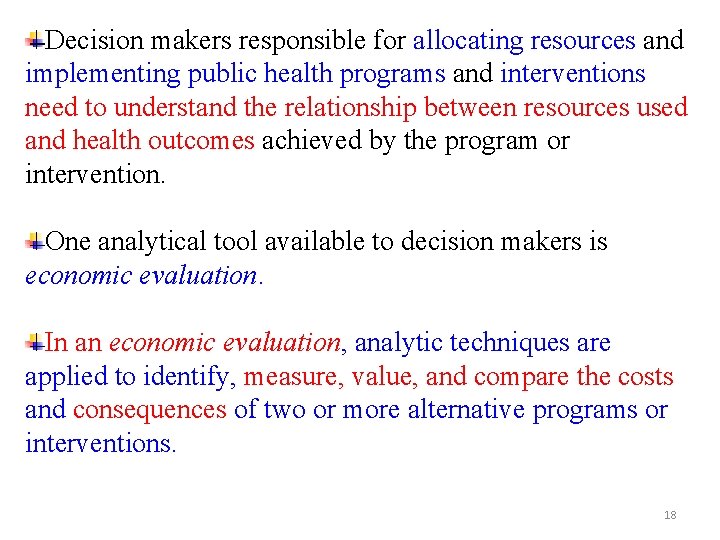
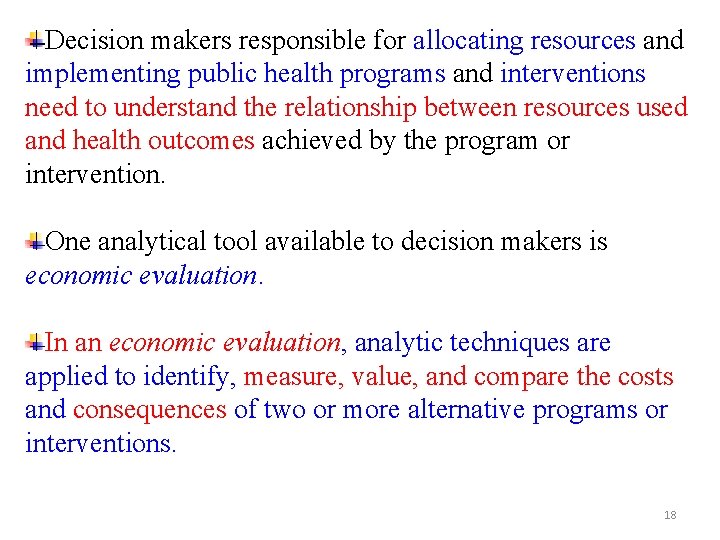
Decision makers responsible for allocating resources and implementing public health programs and interventions need to understand the relationship between resources used and health outcomes achieved by the program or intervention. One analytical tool available to decision makers is economic evaluation. In an economic evaluation, analytic techniques are applied to identify, measure, value, and compare the costs and consequences of two or more alternative programs or interventions. 18
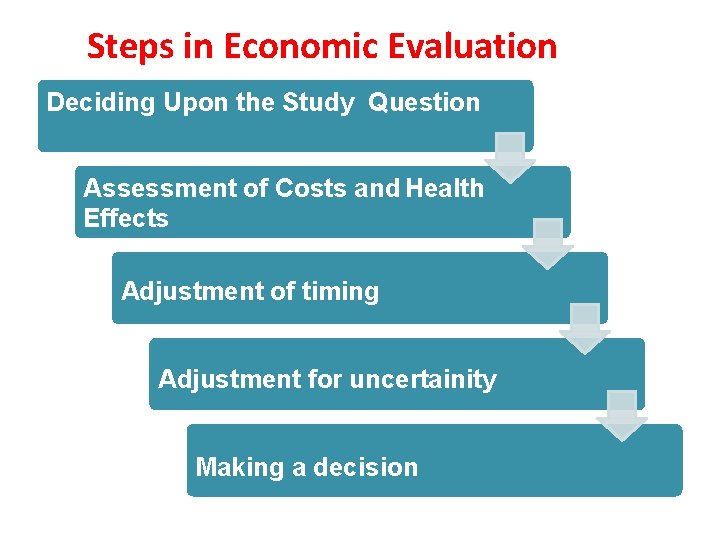
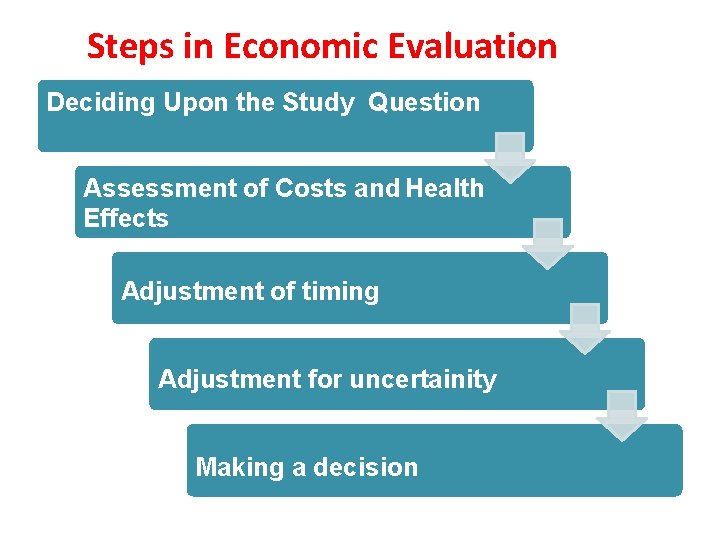
Steps in Economic Evaluation Deciding Upon the Study Question Assessment of Costs and Health Effects Adjustment of timing Adjustment for uncertainity Making a decision
Cost analysis • Cost analysis is a resource tool for financial management in hospital or department. • It is an economic evaluation technique that involves the systematic collection, categorization, and analysis of program or intervention costs, and cost of illness.
When to Use Cost Analysis? Cost analysis can be used as an evaluation method when: • -Only one program is being assessed, • -Information about program effectiveness is not available, • or the interventions being assessed and compared are equally effective.
Objectives of Cost Analysis �To assess the efficiency and effectiveness of function and their cost implication. �To improve the policy relevance and utility through assessment, planning and avoidance of wasteful expenditure in the hospital. �To allow researchers to achieve cost minimization for the programs under consideration.
Purposes of Cost Analysis �A tool for planning and cost projection �To assess the efficiency of a programme �To assess the priorities �Accountability �To assess equity
Principles of Cost Analysis �Make explicit the analytic perspective �Describe the anticipated benefits �Specify the components of costs �Discount to adjust for differential timing �Perform a sensitivity analysis �Calculate measurement of efficiency
1. Identify and define the problem 2. Defining the alternatives 3. Defining the audience 4. Define the perspective 5. Define time frame 6. Determine the time frame and analytic horizon 7. Choose a format/methodology

�Apply principles of cost analysis �Describe study outcomes �Development of cost inventory �Preparation of cost summary
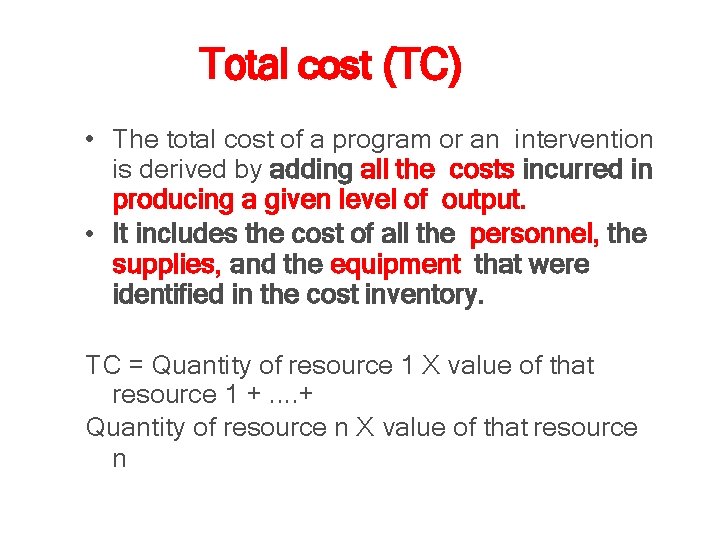
Total cost (TC) • The total cost of a program or an intervention is derived by adding all the costs incurred in producing a given level of output. • It includes the cost of all the personnel, the supplies, and the equipment that were identified in the cost inventory. TC = Quantity of resource 1 X value of that resource 1 +. . + Quantity of resource n X value of that resource n
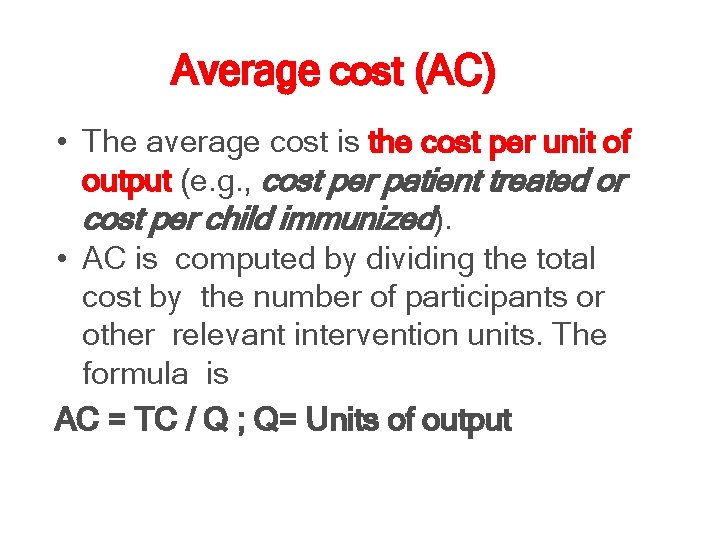
Average cost (AC) • The average cost is the cost per unit of output (e. g. , cost per patient treated or cost per child immunized). • AC is computed by dividing the total cost by the number of participants or other relevant intervention units. The formula is AC = TC / Q ; Q= Units of output
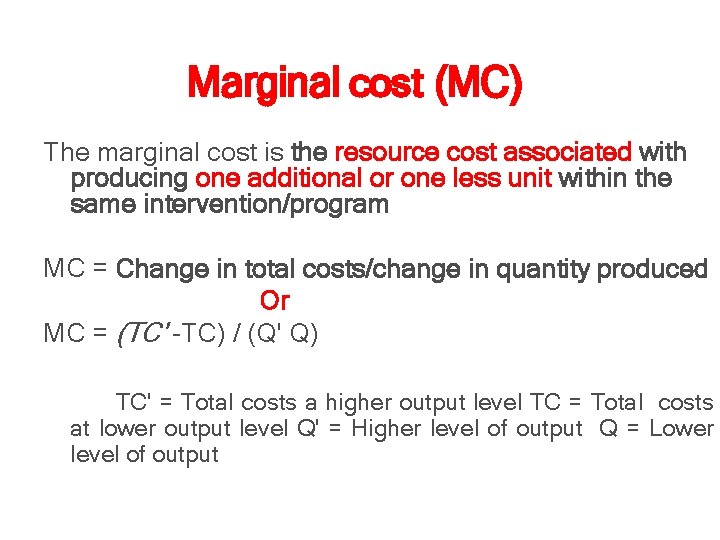
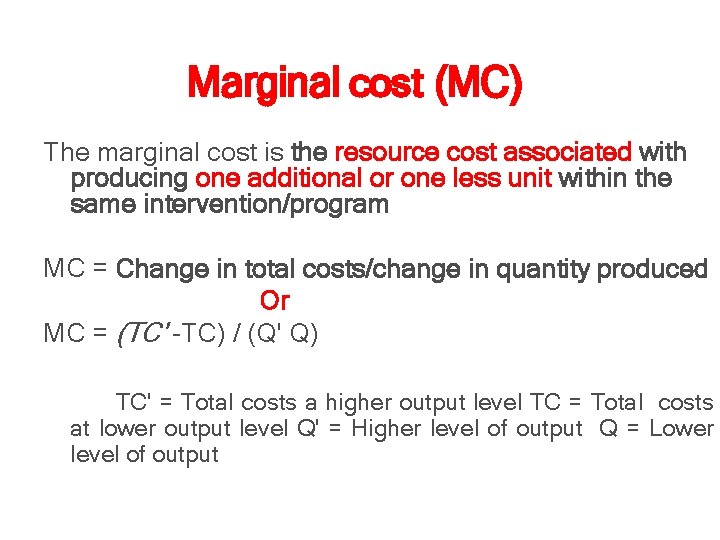
Marginal cost (MC) The marginal cost is the resource cost associated with producing one additional or one less unit within the same intervention/program MC = Change in total costs/change in quantity produced Or MC = (TC' -TC) / (Q' Q) TC' = Total costs a higher output level TC = Total costs at lower output level Q' = Higher level of output Q = Lower level of output
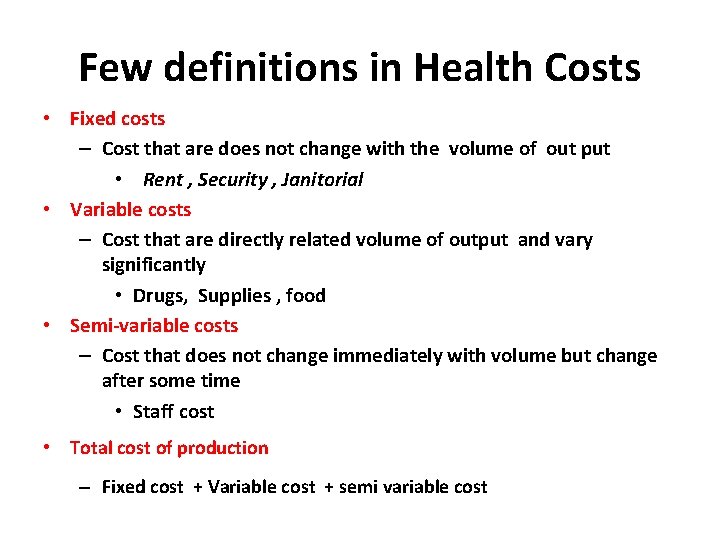
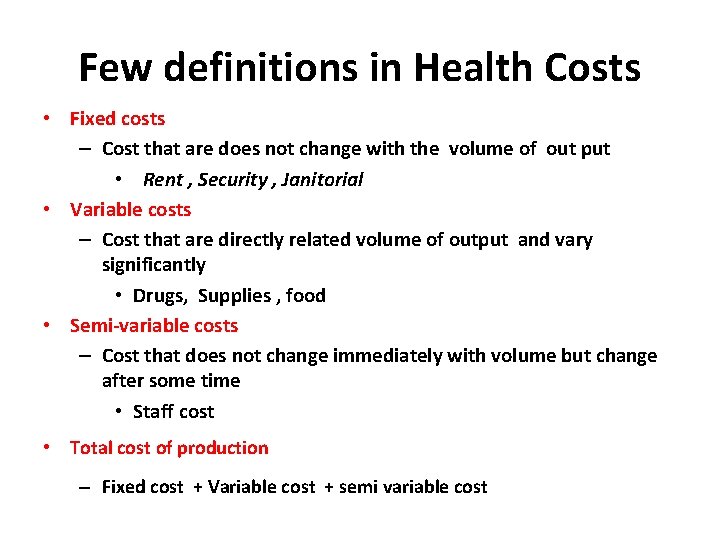
Few definitions in Health Costs • Fixed costs – Cost that are does not change with the volume of out put • Rent , Security , Janitorial • Variable costs – Cost that are directly related volume of output and vary significantly • Drugs, Supplies , food • Semi-variable costs – Cost that does not change immediately with volume but change after some time • Staff cost • Total cost of production – Fixed cost + Variable cost + semi variable cost
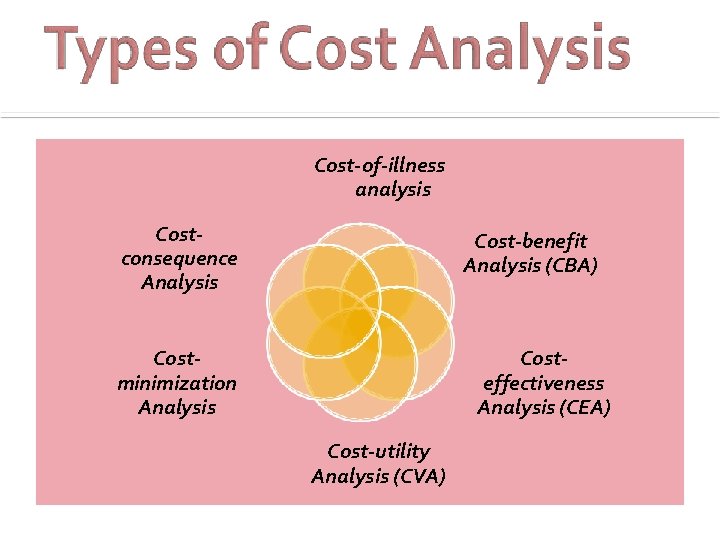
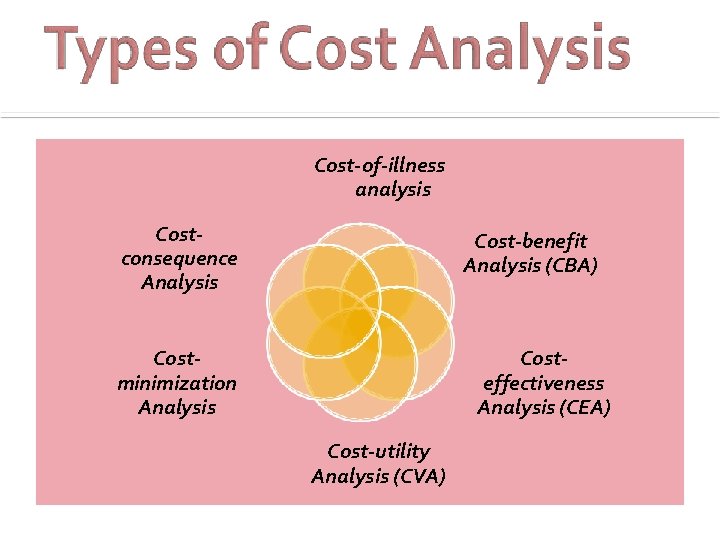
Cost-of-illness analysis Costconsequence Analysis Cost-benefit Analysis (CBA) Costeffectiveness Analysis (CEA) Costminimization Analysis Cost-utility Analysis (CVA)
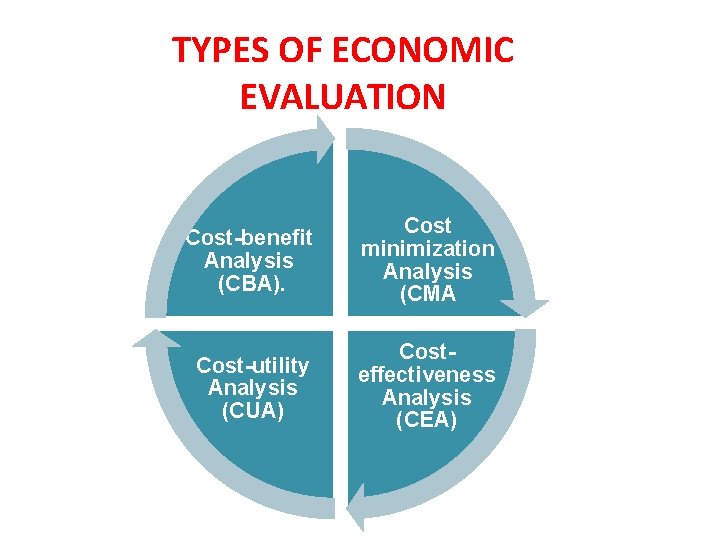
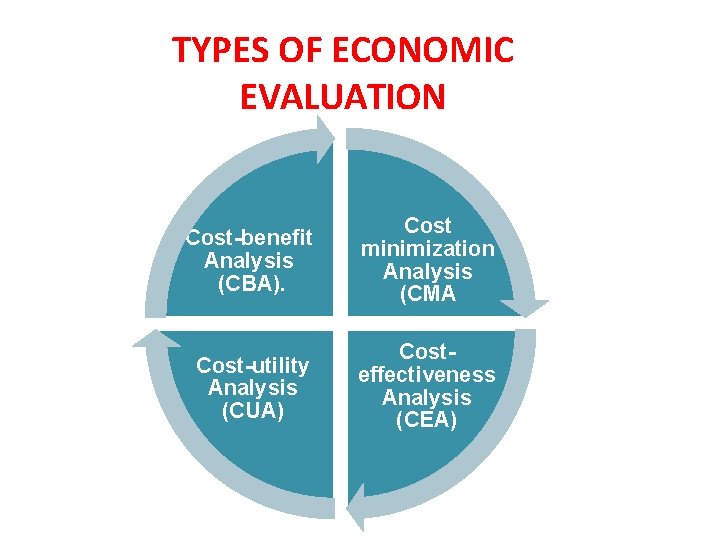
TYPES OF ECONOMIC EVALUATION Cost-benefit Analysis (CBA). Cost minimization Analysis (CMA Cost-utility Analysis (CUA) Costeffectiveness Analysis (CEA)
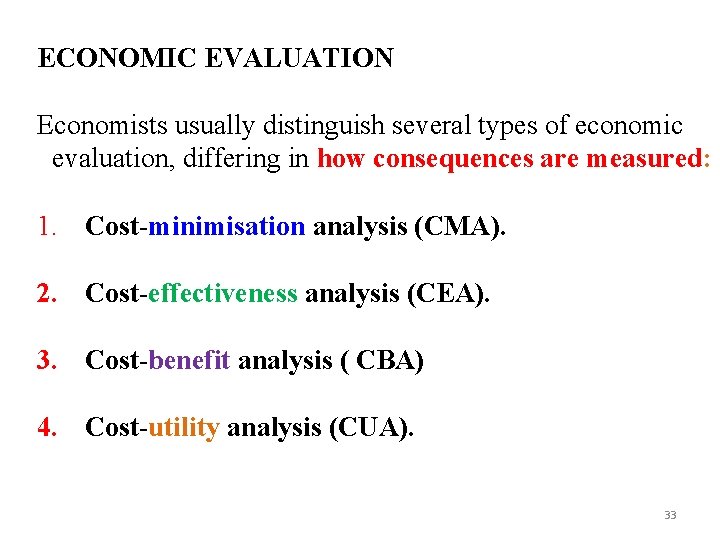
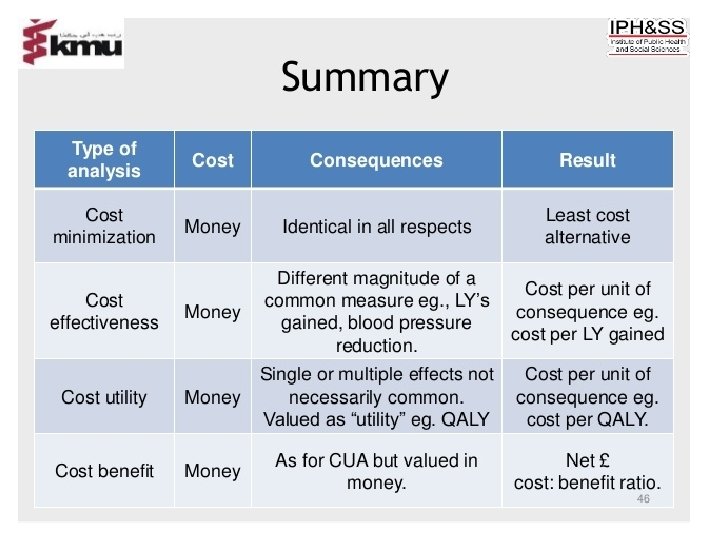
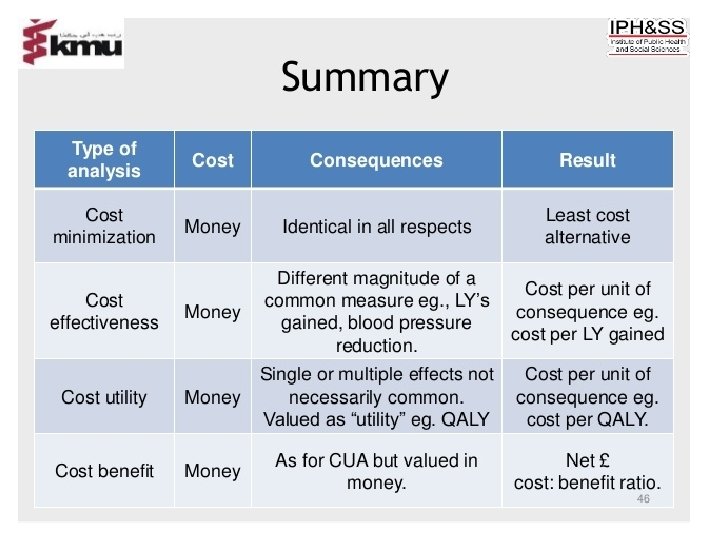
ECONOMIC EVALUATION Economists usually distinguish several types of economic evaluation, differing in how consequences are measured: 1. Cost-minimisation analysis (CMA). 2. Cost-effectiveness analysis (CEA). 3. Cost-benefit analysis ( CBA) 4. Cost-utility analysis (CUA). 33
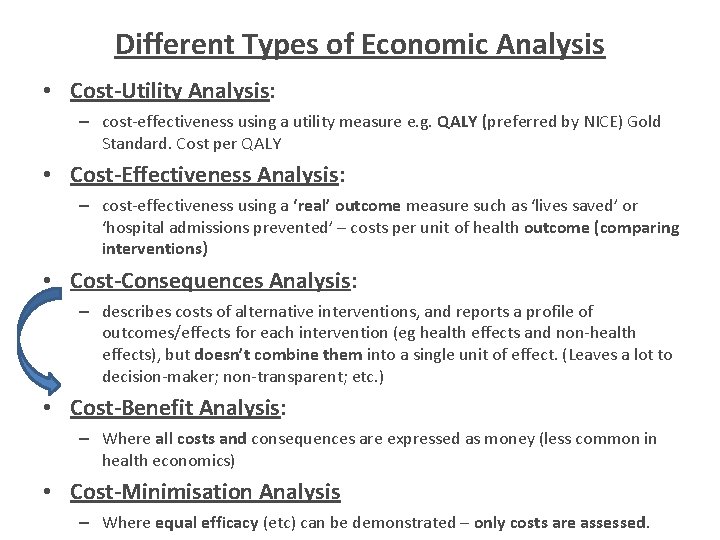
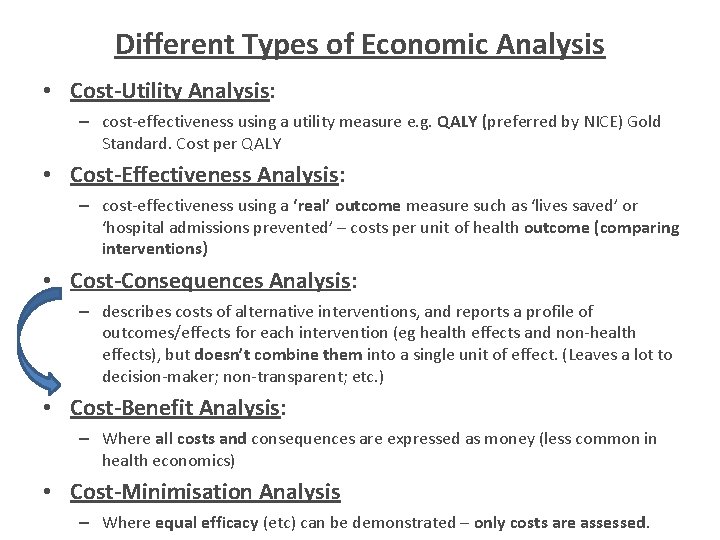
Different Types of Economic Analysis • Cost-Utility Analysis: – cost-effectiveness using a utility measure e. g. QALY (preferred by NICE) Gold Standard. Cost per QALY • Cost-Effectiveness Analysis: – cost-effectiveness using a ‘real’ outcome measure such as ‘lives saved’ or ‘hospital admissions prevented’ – costs per unit of health outcome (comparing interventions) • Cost-Consequences Analysis: – describes costs of alternative interventions, and reports a profile of outcomes/effects for each intervention (eg health effects and non-health effects), but doesn’t combine them into a single unit of effect. (Leaves a lot to decision-maker; non-transparent; etc. ) • Cost-Benefit Analysis: – Where all costs and consequences are expressed as money (less common in health economics) • Cost-Minimisation Analysis – Where equal efficacy (etc) can be demonstrated – only costs are assessed.
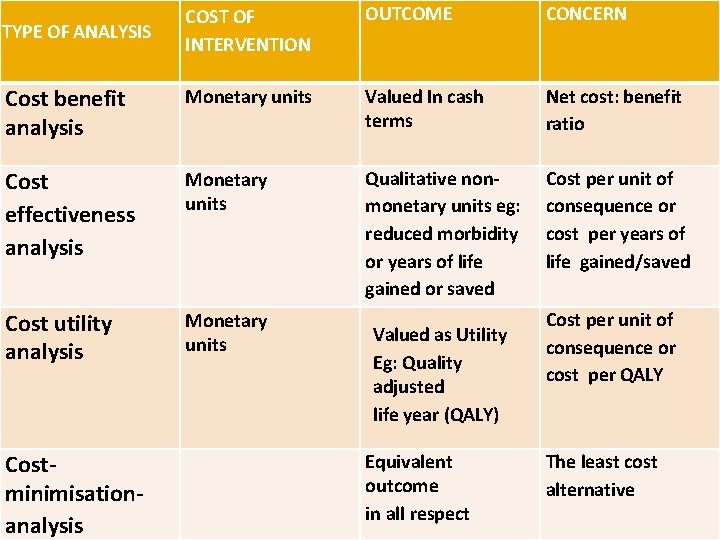
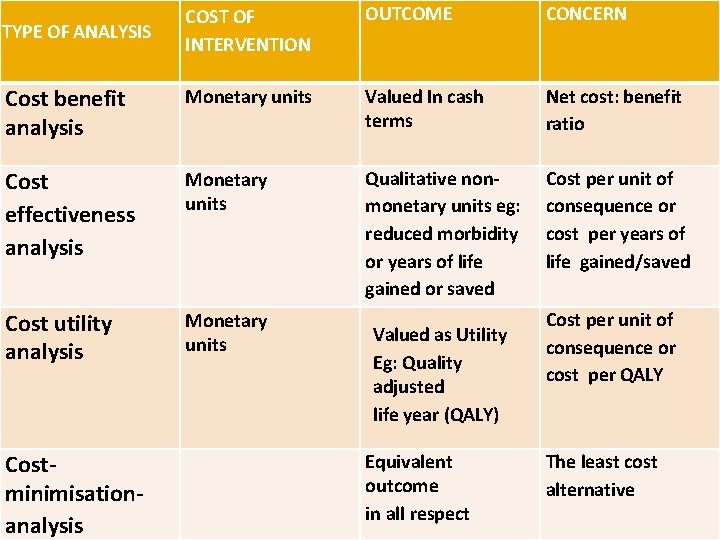
COST OF INTERVENTION OUTCOME CONCERN Cost benefit analysis Monetary units Valued In cash terms Net cost: benefit ratio Cost effectiveness analysis Monetary units Qualitative nonmonetary units eg: reduced morbidity or years of life gained or saved Cost per unit of consequence or cost per years of life gained/saved Cost utility analysis Monetary units TYPE OF ANALYSIS Costminimisationanalysis Valued as Utility Eg: Quality adjusted life year (QALY) Equivalent outcome in all respect Cost per unit of consequence or cost per QALY The least cost alternative
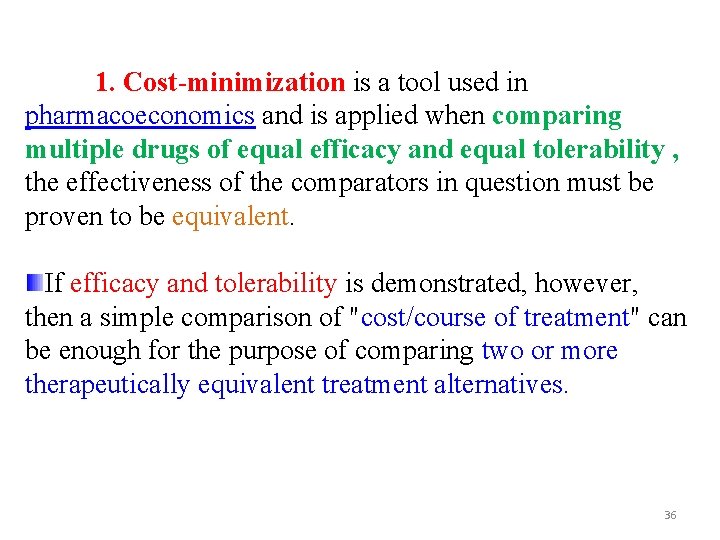
1. Cost-minimization is a tool used in pharmacoeconomics and is applied when comparing multiple drugs of equal efficacy and equal tolerability , the effectiveness of the comparators in question must be proven to be equivalent. If efficacy and tolerability is demonstrated, however, then a simple comparison of "cost/course of treatment" can be enough for the purpose of comparing two or more therapeutically equivalent treatment alternatives. 36
When conducting a cost-minimization study, the author needs to measure all costs (resource expenditures) inherent to the delivery of therapeutic intervention and that are relevant to the pharmacoeconomic perspective. It is used to compare costs of alternative therapies that have: identical clinical effectiveness (including adverse reactions, complications and duration of therapy), BUT Different costs. Choose the least cost alternative among equivalent or equally effective alternatives 37
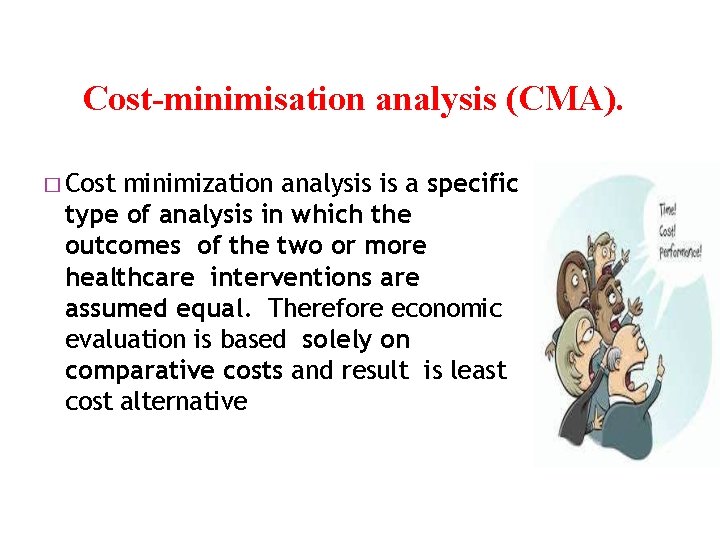
Cost-minimisation analysis (CMA). � Cost minimization analysis is a specific type of analysis in which the outcomes of the two or more healthcare interventions are assumed equal. Therefore economic evaluation is based solely on comparative costs and result is least cost alternative
Cost–benefit analysis (CBA)
Cost–benefit analysis (CBA) 2. Cost–benefit analysis (CBA), sometimes called benefit–cost analysis (BCA), is a systematic process for calculating and comparing benefits and costs of an action. CBA has two purposes: 1. To determine the justification/feasibility, 2. To provide a basis for comparing actions. It involves comparing the total expected cost of each option against the total expected benefits, to see whether the benefits outweigh the costs, and by how much. 40
Cost benefit analysis • This is more expanded version than cost effectiveness analysis. Here the monetary values of benefits of a project are compared with monetary costs of the project. It enables comparisons between projects and is vital in decision-making. • Project cost Vs Project outcomes Source : Jones, . I. R. (1998): Costing Health Services
Cost–benefit analysis (CBA) In CBA, benefits and costs are expressed in money terms, and are adjusted for the time value of money, so that all flows of benefits and flows of costs over time are expressed on a common basis in terms of their "net present value. “ Example , when deciding how to allocate the limited funding, policy makers might have to choose between implementing : • screening program for tuberculosis infection or • a job-training program for the unemployed. 42
Cost–benefit analysis (CBA) When do we use CBA? The prominent features differentiate CBA from other forms of economic evaluation are: • CBA adopts a broad community perspective (thus it includes all costs and all benefits), and • CBA measures the outcomes in monetary terms. • CBA is the appropriate form of economic evaluation to assess the economic efficiency (maximum amount of output [e. g. , persons screened, cases prevented, or cases treated] is produced from the given level of inputs). 43
Cost–benefit analysis (CBA) CBA It is a particularly helpful tool for the following purposes: A. Deciding Whether To Implement a Specific Program: For example, research indicates that a vaccine protects against human papillomavirus (HPV). (HPV is the virus that is responsible for the majority of cervical cancer cases. ) A CBA might indicate that, even if the price of the vaccine is relatively high, the savings from : Øthe averted HPV infection, Øthe resulting cervical cancer treatment, and Øthe averted productivity losses outweigh the costs of vaccination and Ø generate a net gain in community welfare. This provides an additional argument for public decision makers to support an HPV vaccination program that can prevent thousands of deaths. 44
Cost–benefit analysis (CBA) CBA It is a particularly helpful tool for the following purposes: B. Choosing Among Competing Options: health policy makers might have to choose between : 1. funding a program of free Pap smear testing for women at high risk of infection and 2. HPV vaccination program. The results of a CBA might indicate that the net gain in community welfare equals : • $521 million for Pap smear testing and • $987 million for HPV vaccination programs. The evident preferable alternative would be the HPV vaccination program. 45
Cost–benefit analysis (CBA) CBA It is a particularly helpful tool for the following purposes: C- Choosing and Setting Priorities from a Group of Potential Programs The benefit maximization rule can also guide decisions on allocating a fixed resources among a group of potential programs. The combination of programs that has the largest net gain in community benefit is the preferred choice. 46
Cost–benefit analysis (CBA) CBA It is a particularly helpful tool for the following purposes: D. What are costs and benefits? Benefits are the economic values of desirable consequences of economic policies and decisions. Together with costs they reflect the changes in individual and social welfare that result from implementing alternative programs. Benefits are generally classified as direct, indirect, and indescribable: 1. Direct benefits are the values of desirable health and non-health outcomes directly related to the implementation of proposed interventions that can be estimated from data. 2. Indirect benefits are the averted costs and savings resulting from the interventions but not related directly to them. 3. indescribable benefits include the values of positive outcomes (e. g. , reductions in health risk, pain, and suffering), which cannot be estimated from data. 11/29/2020 47
Cost–benefit analysis (CBA) Benefits �Direct Benefits �Indirect Benefits �Intangible Benefits (B) > Costs (C) or Net Benefits (NB) = B -C > O.
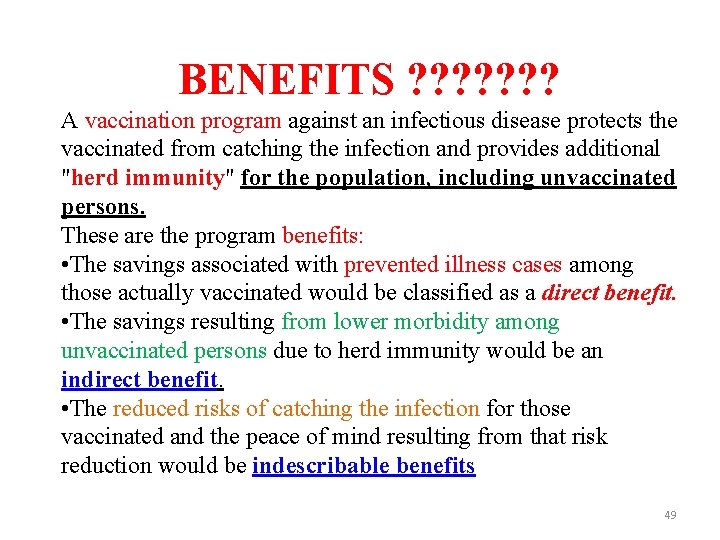
BENEFITS ? ? ? ? A vaccination program against an infectious disease protects the vaccinated from catching the infection and provides additional "herd immunity" for the population, including unvaccinated persons. These are the program benefits: • The savings associated with prevented illness cases among those actually vaccinated would be classified as a direct benefit. • The savings resulting from lower morbidity among unvaccinated persons due to herd immunity would be an indirect benefit. • The reduced risks of catching the infection for those vaccinated and the peace of mind resulting from that risk reduction would be indescribable benefits 49
Cost–benefit analysis (CBA) �Cost-benefit analysis is a practical way of assessing the desirability of projects, where it is important to take a long view (looking at the repercussion in the future as well as in the near future and a wide view in the sense of allowing side effects of many decisions) Le. it implies the enumeration and evaluation of all the relevant cost and benefits. -Prest and Terkey
Cost–benefit analysis (CBA) �Cost Benefit Analysis (CBA) is an economic evaluation technique that measures all the positive (beneficial) and negative (costly) consequences of an intervention or program in monetary terms.
Cost–benefit analysis (CBA) �CBA is a practical approach of appraising the desirability of an intervention involving public expenditure in terms of net social gain society. �CBA is the use of analytical techniques involving a monetary assessment to identify the total costs and benefits of a specific intervention
�Cost Benefit Analysis is used for determining priorities among various alternative programs or interventions. �It provides an estimate of the potential value of undertaking a course of action, i. e. instituting a new program or intervention or revising the old one. �It can also be used to compare health-related interventions to those in other economic sectors.
�It enables policy makers to determine whether the value of its positive consequences exceeds the value of societal resources required to implement the program. �It estimates and totals up the equivalent money value of the benefits and costs of projects to establish whether they are worthwhile. . �It is a powerful and relatively easy tool for deciding whether to make a change or not.
�CBA adopts a broad societal perspective as it includes all costs and all benefits �CBA measures the outcomes in monetary terms. �It assess the desirability of program/intervention
Advantages of Cost Benefit Analysis • It helps to allocate scarce resources to programs that maximize societal economic benefit • It studies the full economic impact of all potential outcomes of an intervention. • It makes possible to compare different programs having different health outcomes, or health programs to non health programs. • lt allows analysts to examine its distributional aspects; who will receive these benefits and who will bear the costs.
Drawbacks of Cost Benefit Analysis • It measures costs and outcomes in monetary terms and not disease specific • There is difficulty in assigning monetary values to all pertinent outcome including changes in the length or quality of human life. • The results of CBA are only as good as the assumptions and valuations on which they are based.
Cost-effectiveness analysis
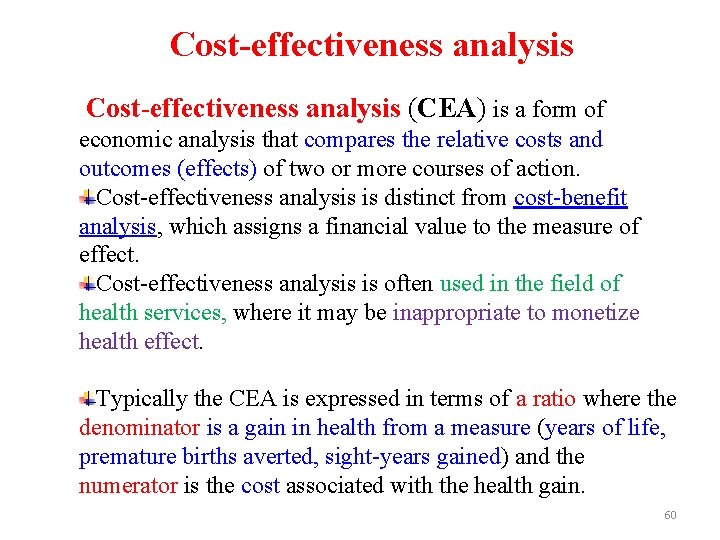
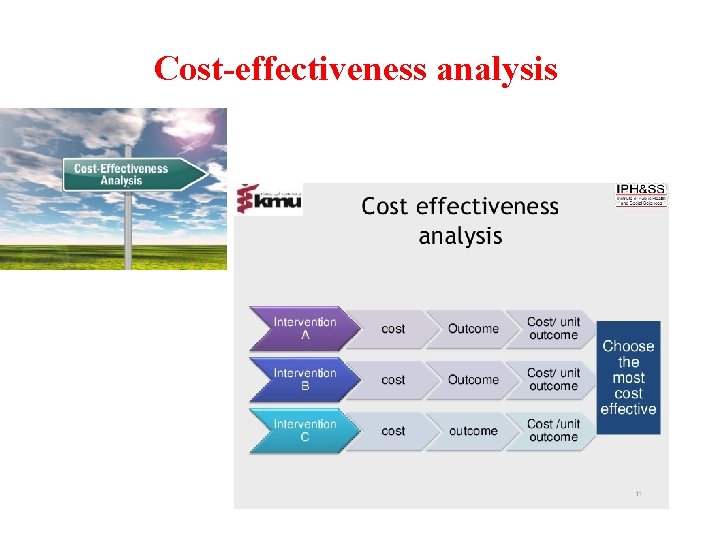
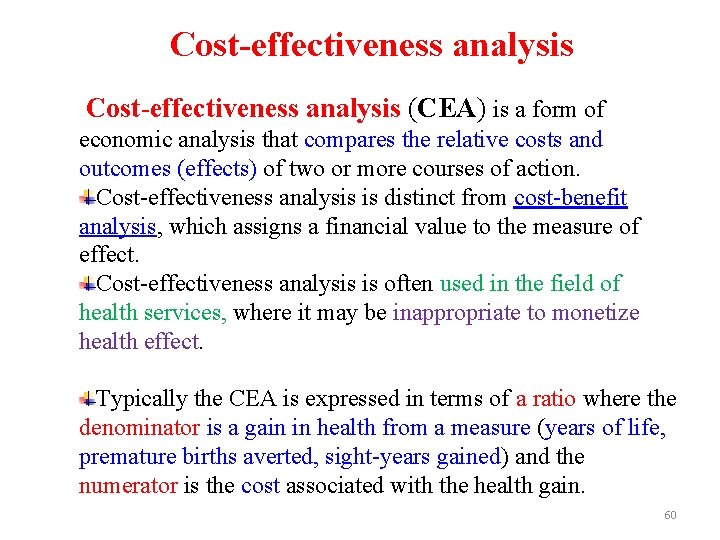
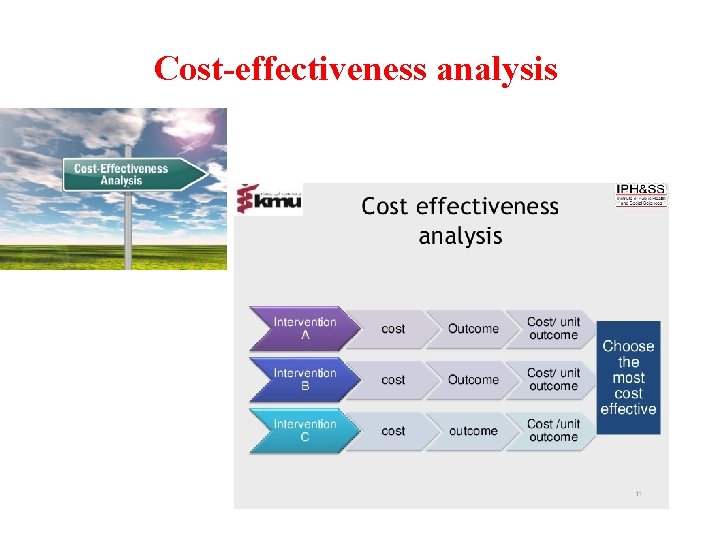
Cost-effectiveness analysis (CEA) is a form of economic analysis that compares the relative costs and outcomes (effects) of two or more courses of action. Cost-effectiveness analysis is distinct from cost-benefit analysis, which assigns a financial value to the measure of effect. Cost-effectiveness analysis is often used in the field of health services, where it may be inappropriate to monetize health effect. Typically the CEA is expressed in terms of a ratio where the denominator is a gain in health from a measure (years of life, premature births averted, sight-years gained) and the numerator is the cost associated with the health gain. 60
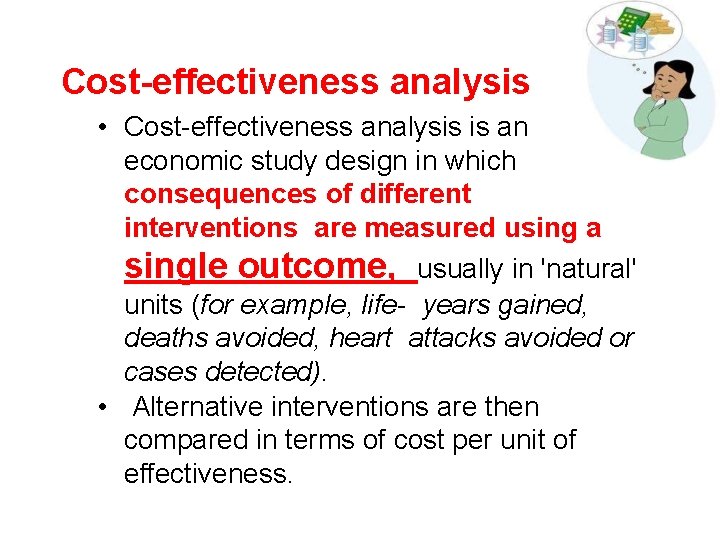
Cost-effectiveness analysis • Cost-effectiveness analysis is an economic study design in which consequences of different interventions are measured using a single outcome, usually in 'natural' units (for example, life- years gained, deaths avoided, heart attacks avoided or cases detected). • Alternative interventions are then compared in terms of cost per unit of effectiveness.
Cost-effectiveness analysis as tool decisionmakers can use to assess and potentially improve the performance of their health systems. It indicates which interventions provide the highest 'value for money' and helps them choose the interventions and programmes which maximize health for the available resources.
Cost-effectiveness analysis Cost Effectiveness Analysis (CEA) is a type of economic evaluation that examines both the costs and health outcomes of alternative intervention strategies. Aim of Cost Effectiveness Analysis • To maximize the level of benefitshealth effects-relative to the level of resources available
Cost-effectiveness analysis These options have a common health outcome: the number of cases of a disease prevented by the vaccine. CEA can be used to identify the option that prevents the most cases at the least cost. Cost-effectiveness analysis for immunization program for poliomyelitis: cost CBA= -------------------------------- number of cases of a disease prevented by the vaccine 64
Cost-effectiveness analysis Why Is CEA Important? Decision makers are often faced with the challenges of resource allocation. Resources are scarce; therefore, they must be allocated wisely. CEA is used to identify the most cost-effective strategies from a set of options that have similar results. For example, the government might have to allocate scarce resources to: • provide a new facility to assist in the development and procurement of vaccines, or • enhance the current public health vaccine delivery. 65
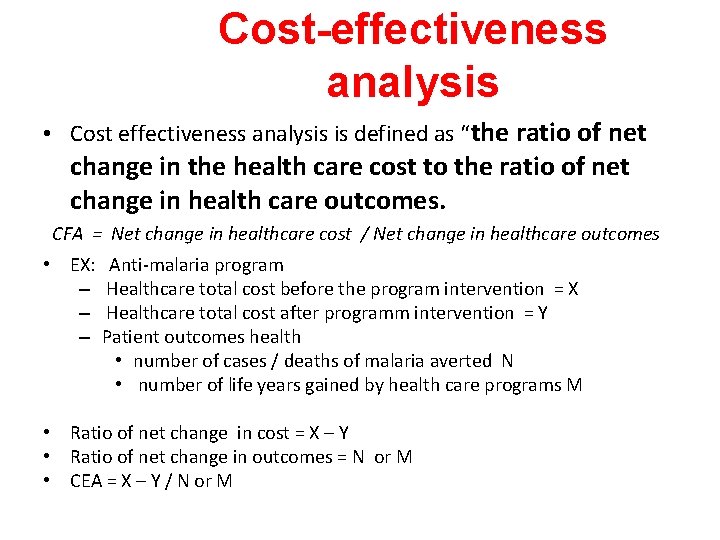
Cost-effectiveness analysis • Cost effectiveness analysis is defined as “the ratio of net change in the health care cost to the ratio of net change in health care outcomes. CFA = Net change in healthcare cost / Net change in healthcare outcomes • EX: Anti-malaria program – Healthcare total cost before the program intervention = X – Healthcare total cost after programm intervention = Y – Patient outcomes health • number of cases / deaths of malaria averted N • number of life years gained by health care programs M • Ratio of net change in cost = X – Y • Ratio of net change in outcomes = N or M • CEA = X – Y / N or M
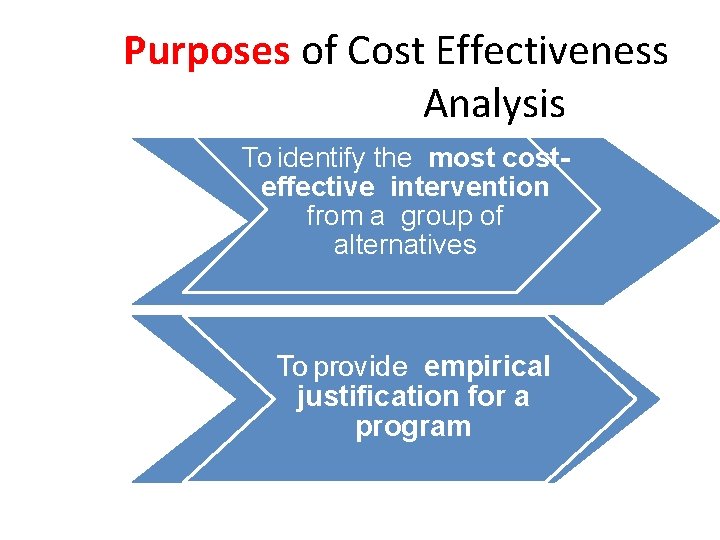
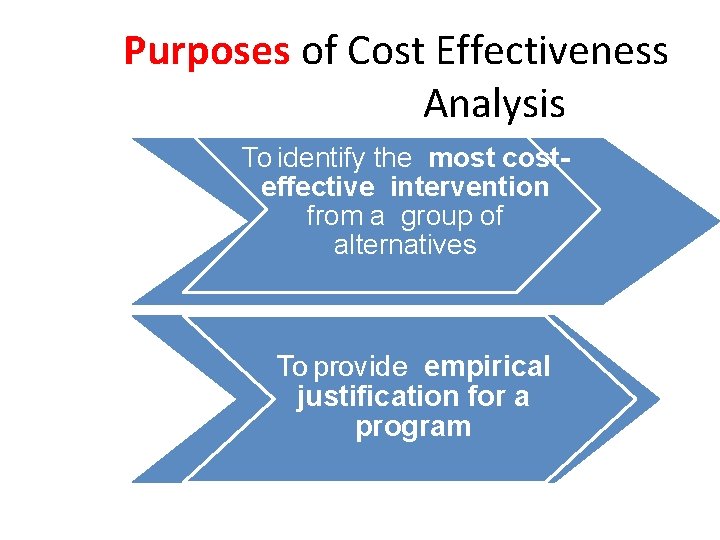
Purposes of Cost Effectiveness Analysis To identify the most costeffective intervention from a group of alternatives To provide empirical justification for a program
Drawbacks of Cost Effectiveness Analysis • The data regarding direct costs such as doctors' or nurses' time and supplies used; indirect costs such as a portion of administrative costs, the cost of equipment are usually not readily available. • It does not facilitate comparisons across different diseases when different outcomes have been used. • Cost-effectiveness is the only one criterion for judging whether an intervention is effective or not.
Benefits of Cost Effectiveness Analysis • This method is easy to understand more readily suited to decision making. • It provides empirical decision results for the makers to compare the costs and consequences associated with alternative programmes.
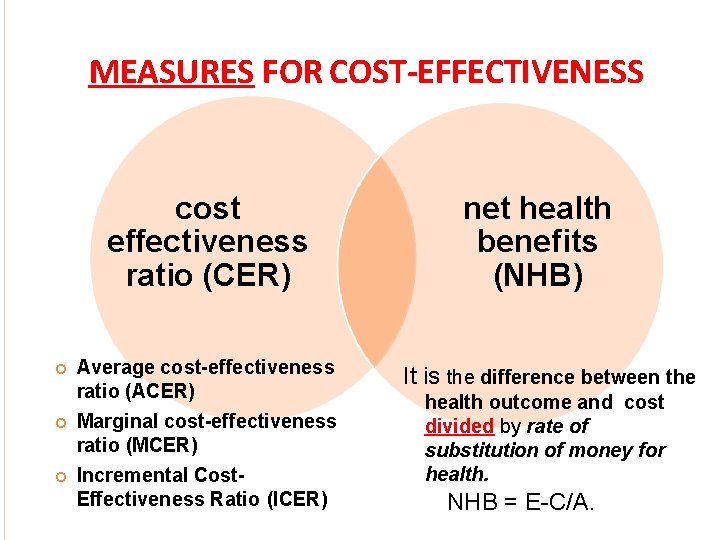
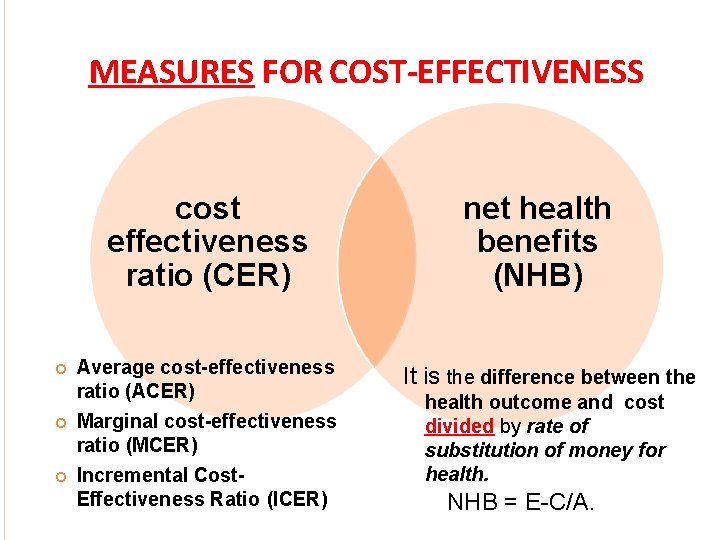
MEASURES FOR COST-EFFECTIVENESS cost effectiveness ratio (CER) Average cost-effectiveness ratio (ACER) Marginal cost-effectiveness ratio (MCER) Incremental Cost. Effectiveness Ratio (ICER) net health benefits (NHB) It is the difference between the health outcome and cost divided by rate of substitution of money for health. NHB = E-C/A.
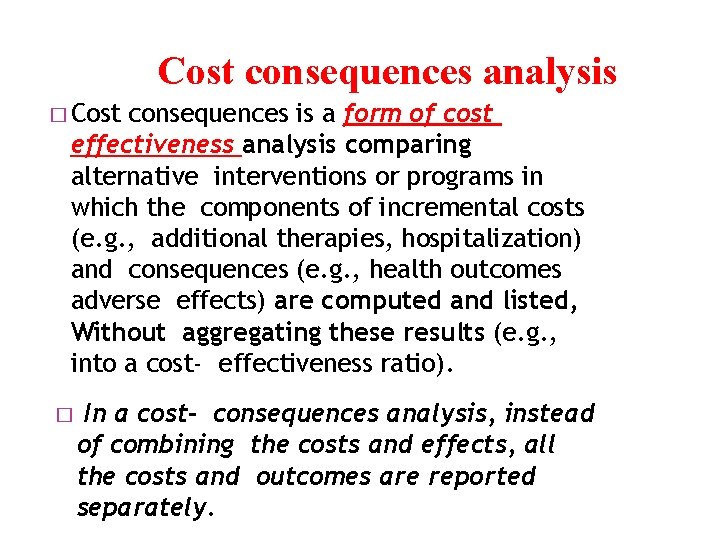
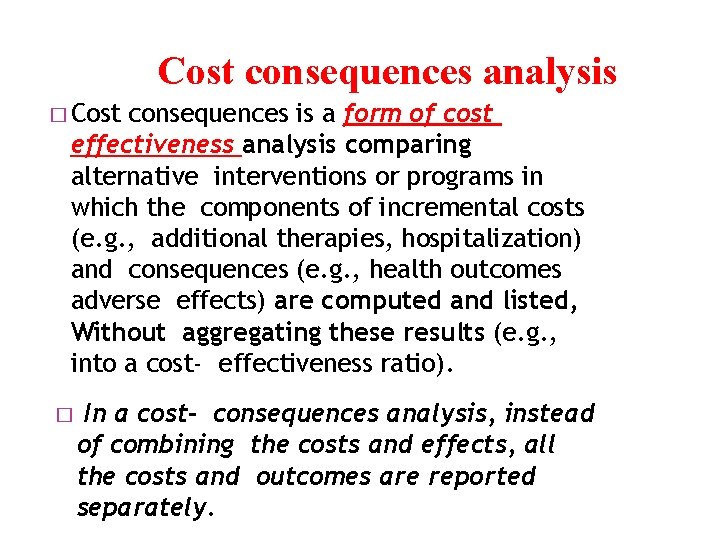
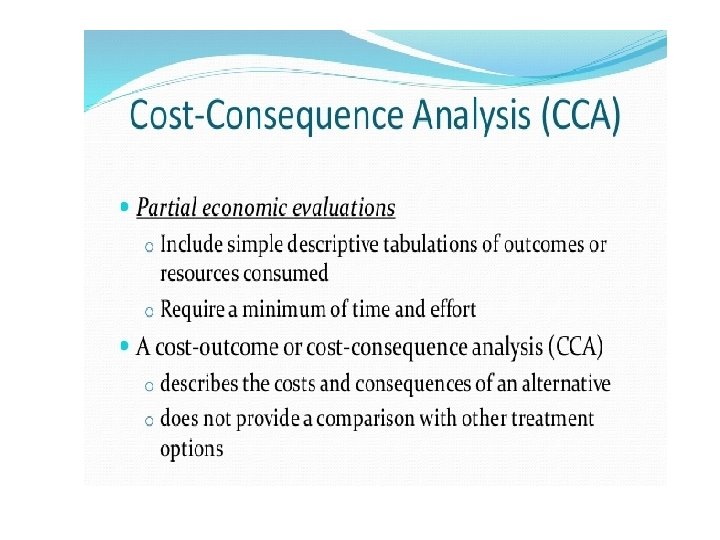
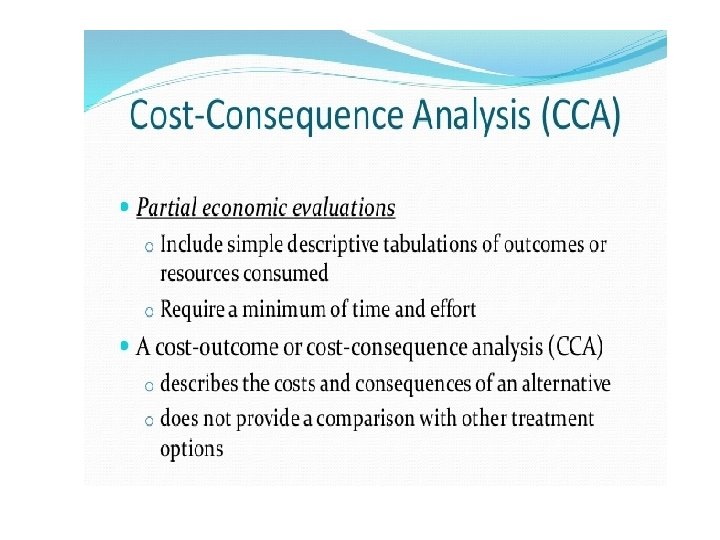
Cost consequences analysis � Cost consequences is a form of cost effectiveness analysis comparing alternative interventions or programs in which the components of incremental costs (e. g. , additional therapies, hospitalization) and consequences (e. g. , health outcomes adverse effects) are computed and listed, Without aggregating these results (e. g. , into a cost- effectiveness ratio). � In a cost- consequences analysis, instead of combining the costs and effects, all the costs and outcomes are reported separately.
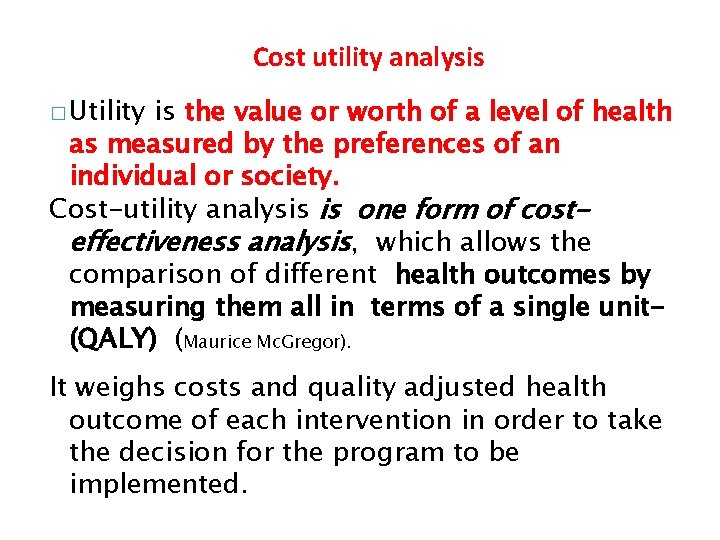
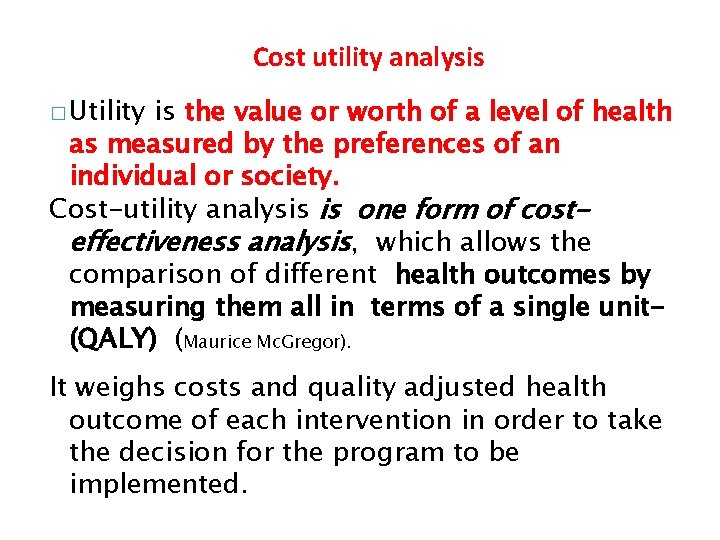
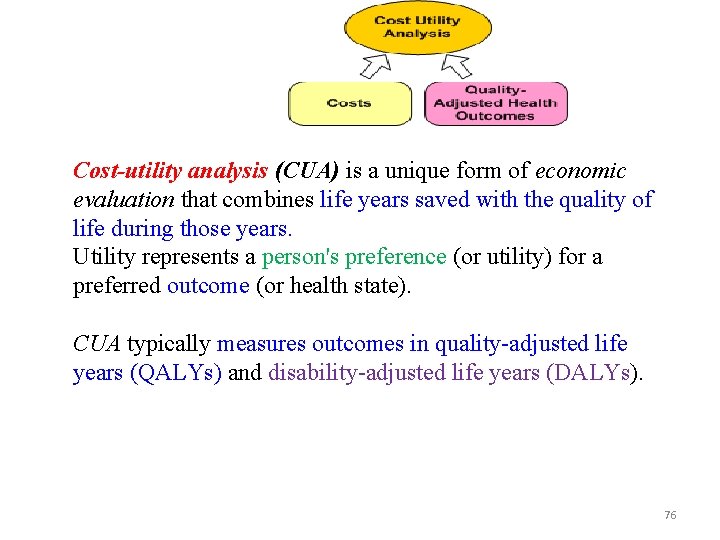
Cost utility analysis � Utility is the value or worth of a level of health as measured by the preferences of an individual or society. Cost-utility analysis is one form of costeffectiveness analysis, which allows the comparison of different health outcomes by measuring them all in terms of a single unit(QALY) (Maurice Mc. Gregor). It weighs costs and quality adjusted health outcome of each intervention in order to take the decision for the program to be implemented.
Cost utility analysis • This is a similar to cost effectiveness analysis but it considers the alternative strategies to improve the quality of life as well as morbidity. • Net change in health outcomes = Disability adjusted life years ( DALY) is taken as a measure and compared between alternative strategies for intervention ! Source : Witter, S. , Ensor, T. . Jowett, M. & Thomson, R. (2000) Health Economics in Developing countries
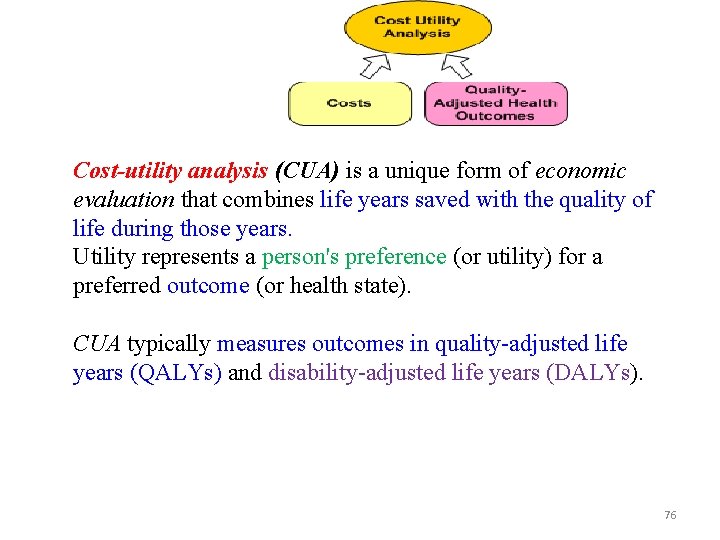
Cost-utility analysis (CUA) is a unique form of economic evaluation that combines life years saved with the quality of life during those years. Utility represents a person's preference (or utility) for a preferred outcome (or health state). CUA typically measures outcomes in quality-adjusted life years (QALYs) and disability-adjusted life years (DALYs). 76
quantity of life years / QALY disability-adjusted life years /DALY
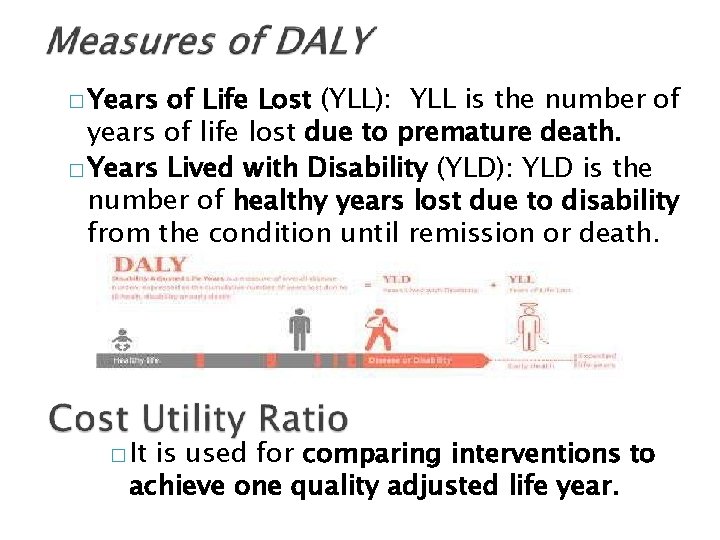
� The World Health Organization defines disabilityadjusted life years (DALY) as 'a health gap measure that extends the concept of potential years of life lost due to premature death to include equivalent years of healthy life lost by virtue of being in states of poor health or disability'. In other words, one DALY is one lost year of healthy life. � DALY is a combined measure of years in disability and years of life lost due to premature death (from the disability).
Quality Adjusted Life Years -QALY • What is a QALY? – QALYs combine both quantity and health-related quality of life (Qo. L) into a single measure of health gain – Use a self reported preference-based questionnaire score (like EQ 5 D or SF-36) – The amount of time spent in a health state is weighted by the Qo. L score attached to that health state – Qo. L scores (utilities) should reflect people’s preferences over health – Utilities usually scored with ‘perfect health’=1 and death=0 – Some states can be ranked as being worse than death (-) 79
Quality Adjusted Life Years • Why use QALYs? – Can weigh up net effect of treatment for patients – Survival vs Qo. L (e. g. for cancer chemotherapy) – Long-term Qo. L for chronic & recurrent conditions (e. g. arthritis) – Benefits versus harms (e. g. COX II inhibitors) – Allows broader comparisons between patient groups The QALY is the preferred measure when conducting costeffectiveness analysis (mostly in clinical and technology appraisals). However, not always possible for social care and public health so look to other methods. 80
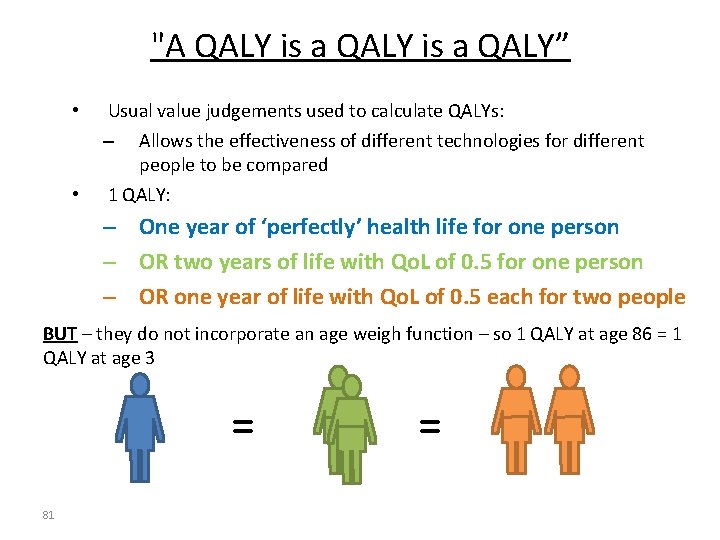
"A QALY is a QALY” • Usual value judgements used to calculate QALYs: Allows the effectiveness of different technologies for different people to be compared 1 QALY: – • – One year of ‘perfectly’ health life for one person – OR two years of life with Qo. L of 0. 5 for one person – OR one year of life with Qo. L of 0. 5 each for two people BUT – they do not incorporate an age weigh function – so 1 QALY at age 86 = 1 QALY at age 3 = 81 =
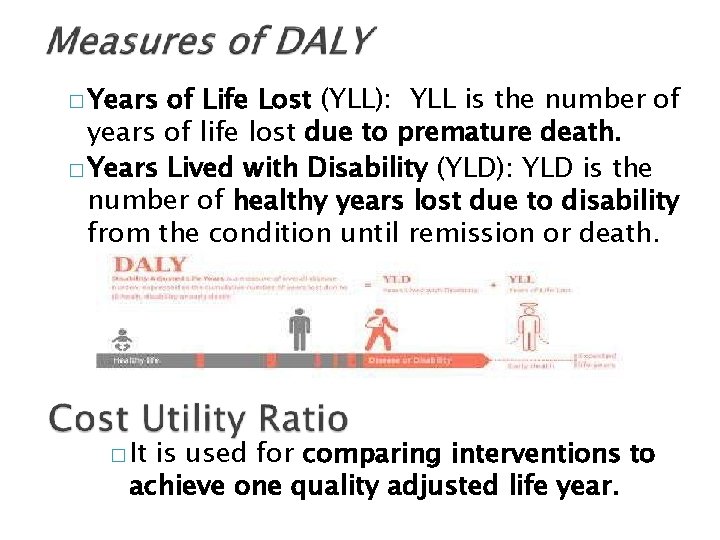
� Years of Life Lost (YLL): YLL is the number of years of life lost due to premature death. � Years Lived with Disability (YLD): YLD is the number of healthy years lost due to disability from the condition until remission or death. � It is used for comparing interventions to achieve one quality adjusted life year.
Cost is measured in monetary (financial) units. Benefits needs to be expressed in a way that allows health states that are considered less preferable to full health to be given quantitative values. However , unlike cost- benefit analysis, the benefits do not have to be expressed in monetary terms. In health technology assessment (HTA) , it is usually expressed in quality –adjusted life years ( QALY) 83
When acting on the results of cost effectiveness and cost utility studies, if two treatments A and B are compared and costs are lower for A and outcomes better, then treatment A will be preferable. If, as is more commonly the case with a new drug, costs are higher for one treatment, but benefits are higher too, it is necessary to calculate how much extra benefits is obtained for the extra cost. A decision then needs to be made as to whether this addition in benefit is worth paying for. 84
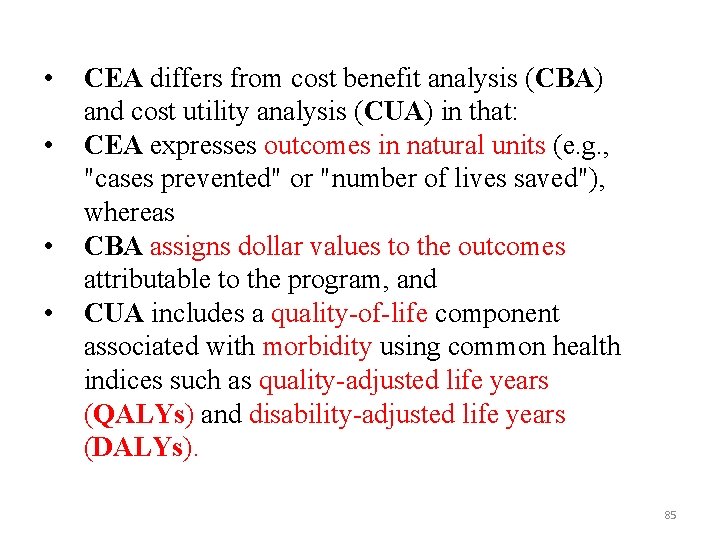
• • CEA differs from cost benefit analysis (CBA) and cost utility analysis (CUA) in that: CEA expresses outcomes in natural units (e. g. , "cases prevented" or "number of lives saved"), whereas CBA assigns dollar values to the outcomes attributable to the program, and CUA includes a quality-of-life component associated with morbidity using common health indices such as quality-adjusted life years (QALYs) and disability-adjusted life years (DALYs). 85
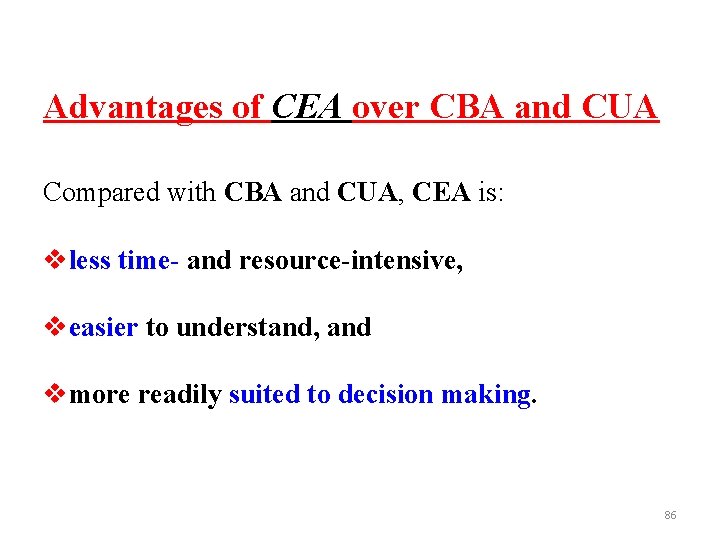
Advantages of CEA over CBA and CUA Compared with CBA and CUA, CEA is: vless time- and resource-intensive, veasier to understand, and vmore readily suited to decision making. 86
 Faculty of medicine nursing and health sciences
Faculty of medicine nursing and health sciences Faculty of medicine dentistry and health sciences
Faculty of medicine dentistry and health sciences Mendel university faculty of business and economics
Mendel university faculty of business and economics University of debrecen faculty of economics and business
University of debrecen faculty of economics and business Faculty of economics and business zagreb
Faculty of economics and business zagreb Mendel university faculty of business and economics
Mendel university faculty of business and economics Hubert kairuki memorial university faculty of medicine
Hubert kairuki memorial university faculty of medicine Solid thyroid nodule
Solid thyroid nodule King abdulaziz university faculty of medicine
King abdulaziz university faculty of medicine Agnes csaki semmelweis
Agnes csaki semmelweis Faculty of veterinary medicine cairo university logo
Faculty of veterinary medicine cairo university logo Hacettepe university faculty of medicine
Hacettepe university faculty of medicine Dosrsal
Dosrsal Semmelweis university faculty of medicine
Semmelweis university faculty of medicine Department of medicine mcgill
Department of medicine mcgill Faculty of veterinary medicine cairo university
Faculty of veterinary medicine cairo university Emory anticoagulation clinic
Emory anticoagulation clinic Cairo university faculty of veterinary medicine
Cairo university faculty of veterinary medicine National policy and legislation
National policy and legislation Economics and business economics maastricht
Economics and business economics maastricht Faculty of public health mahidol university
Faculty of public health mahidol university Facultad de ciencias de la salud uma
Facultad de ciencias de la salud uma Non mathematical economics
Non mathematical economics School of public health and preventive medicine monash
School of public health and preventive medicine monash National center for disaster medicine and public health
National center for disaster medicine and public health Duke medicine grand rounds
Duke medicine grand rounds Security program and policies principles and practices
Security program and policies principles and practices Bsbhrm506
Bsbhrm506 Security program and policies principles and practices
Security program and policies principles and practices Security program and policies principles and practices
Security program and policies principles and practices Security program and policies principles and practices
Security program and policies principles and practices Security program and policies principles and practices
Security program and policies principles and practices Ecology of human performance model
Ecology of human performance model Dr marina flecha
Dr marina flecha Meritus definition
Meritus definition Health and social component 3
Health and social component 3 Health economics lecture notes
Health economics lecture notes Manuel roxas programs and policies
Manuel roxas programs and policies Classroom policies and procedures
Classroom policies and procedures Lending policies and procedures managing credit risk
Lending policies and procedures managing credit risk Antidumping laws
Antidumping laws Modifying principles of accounting
Modifying principles of accounting Chapter 11 school policies and their functions
Chapter 11 school policies and their functions Importance of policies
Importance of policies Policies and procedures presentation
Policies and procedures presentation Configuration policies and procedures
Configuration policies and procedures Hr policies and practices
Hr policies and practices Hr policies and practices
Hr policies and practices Hr policies
Hr policies Who was babur
Who was babur Conservative policies under reagan and bush
Conservative policies under reagan and bush Chapter 6 supply demand and government policies
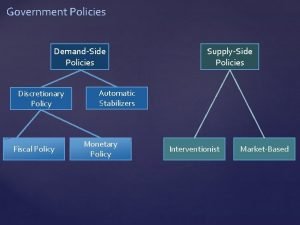
Chapter 6 supply demand and government policies Tricker corporate governance
Tricker corporate governance Lee kong chian faculty of engineering and science
Lee kong chian faculty of engineering and science Motivated energized and capable faculty
Motivated energized and capable faculty Lee kong chian faculty of engineering and science
Lee kong chian faculty of engineering and science It basics
It basics Difference between health education and promotion
Difference between health education and promotion Chapter 3 health wellness and health disparities
Chapter 3 health wellness and health disparities Health education and health propaganda
Health education and health propaganda Chapter 1 lesson 2 what affects your health
Chapter 1 lesson 2 what affects your health Glencoe health chapter 1 understanding health and wellness
Glencoe health chapter 1 understanding health and wellness Nps management policies
Nps management policies Nixons foreign policies
Nixons foreign policies Crime control policies
Crime control policies What are policies
What are policies Disk scheduling policies
Disk scheduling policies Natalist policies
Natalist policies Macroeconomics lesson 2 activity 45
Macroeconomics lesson 2 activity 45 Step migration ap human geography
Step migration ap human geography Mao's domestic policies
Mao's domestic policies Macroprudential policies
Macroprudential policies Crime control policies
Crime control policies Policies largely dictate how structure will be established
Policies largely dictate how structure will be established Demand side policies
Demand side policies Interventionist supply side policies
Interventionist supply side policies Dwight d eisenhower domestic policy
Dwight d eisenhower domestic policy Lesson 4 eisenhower's cold war policies
Lesson 4 eisenhower's cold war policies Demand side policies
Demand side policies Crime control policies
Crime control policies Database security policies
Database security policies Lingua franca project 1999 to 2003
Lingua franca project 1999 to 2003 Classical and neoclassical theory criminology
Classical and neoclassical theory criminology What is working capital cycle
What is working capital cycle Crime control policies
Crime control policies Crime control policies
Crime control policies Crime control policies
Crime control policies Castro's domestic policies
Castro's domestic policies