Evaluation of Renal Function Mohamed O Ezwaie MD



- Slides: 33
Evaluation of Renal Function Mohamed O. Ezwaie, MD Associate professor and consultant of medicine and nephrology 2020 mohamed. ezwaie@uob. edu. ly
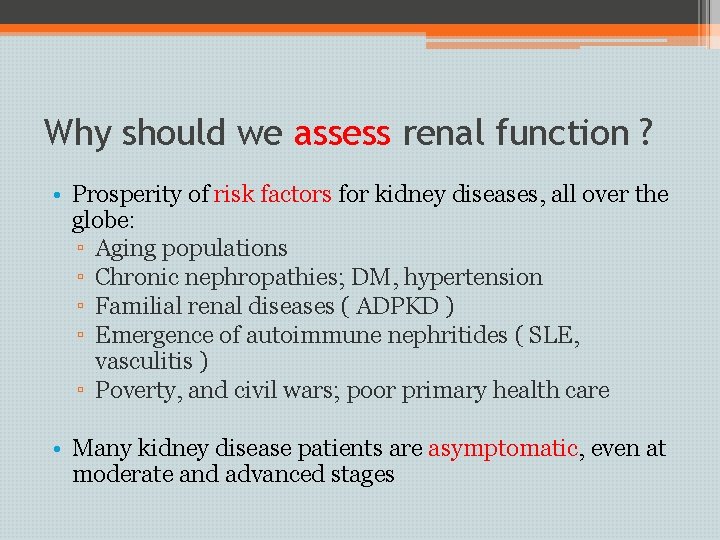
Why should we assess renal function ? • Prosperity of risk factors for kidney diseases, all over the globe: ▫ Aging populations ▫ Chronic nephropathies; DM, hypertension ▫ Familial renal diseases ( ADPKD ) ▫ Emergence of autoimmune nephritides ( SLE, vasculitis ) ▫ Poverty, and civil wars; poor primary health care • Many kidney disease patients are asymptomatic, even at moderate and advanced stages
Why should we monitor renal function • To monitor disease progression and efficacy of therapy • To adjust drug dosage to avoid nephrotoxicity ( antibiotics, chemotherapy )
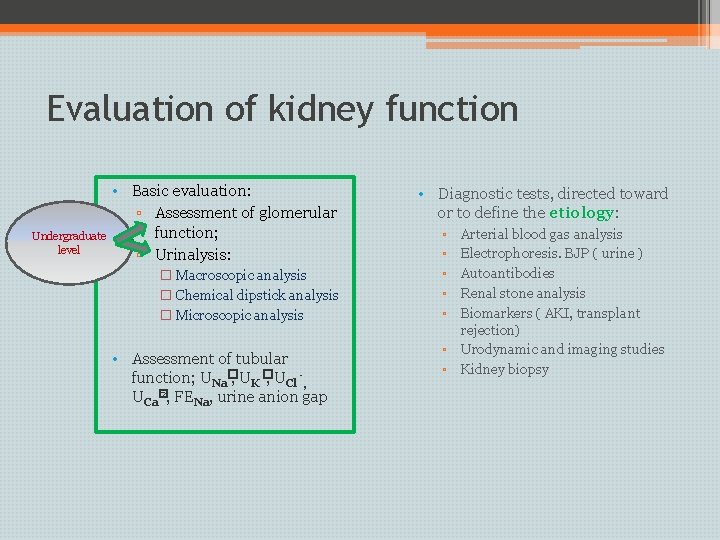
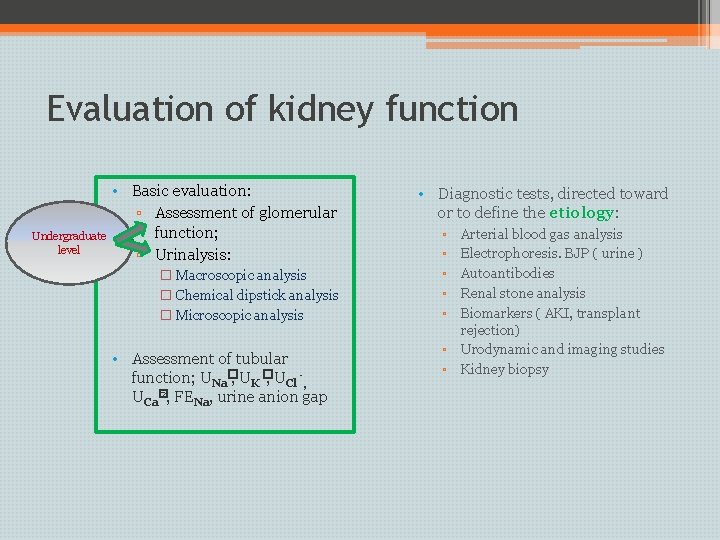
Evaluation of kidney function Undergraduate level • Basic evaluation: ▫ Assessment of glomerular function; ▫ Urinalysis: � Macroscopic analysis � Chemical dipstick analysis � Microscopic analysis • Assessment of tubular function; UNa�, UK �, UCl -, UCa� 2, FENa, urine anion gap • Diagnostic tests, directed toward or to define the etiology: ▫ ▫ ▫ ▫ Arterial blood gas analysis Electrophoresis. BJP ( urine ) Autoantibodies Renal stone analysis Biomarkers ( AKI, transplant rejection) Urodynamic and imaging studies Kidney biopsy
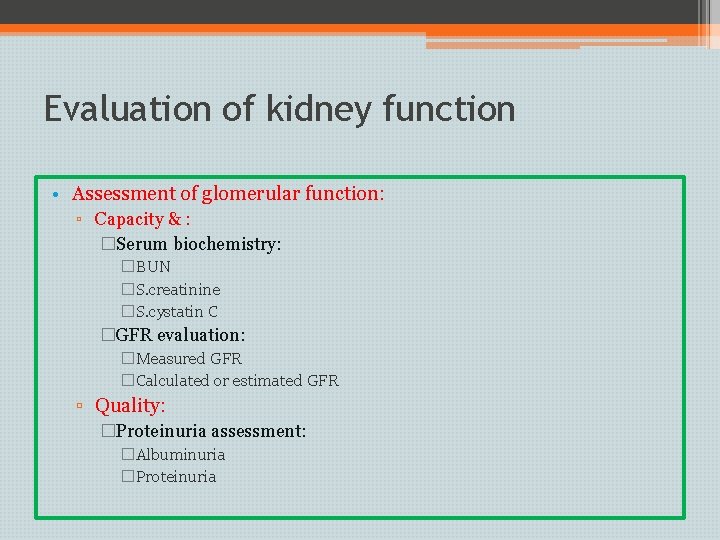
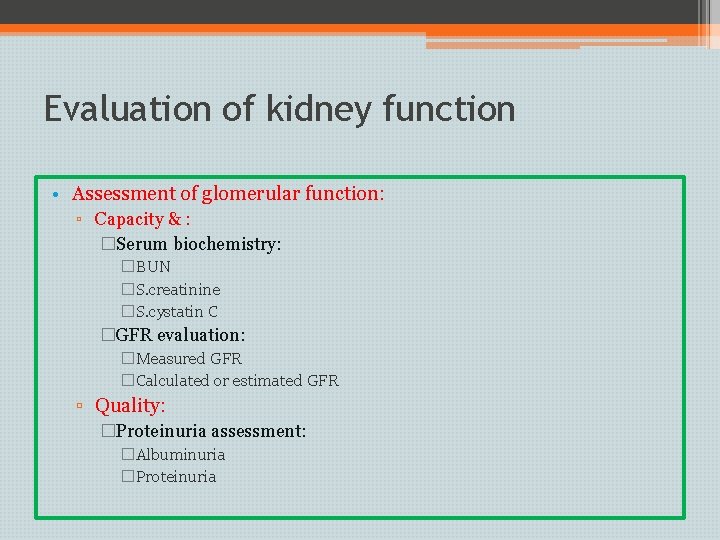
Evaluation of kidney function • Assessment of glomerular function: ▫ Capacity & : �Serum biochemistry: �BUN �S. creatinine �S. cystatin C �GFR evaluation: �Measured GFR �Calculated or estimated GFR ▫ Quality: �Proteinuria assessment: �Albuminuria �Proteinuria
Plasma Urea is the major nitrogen-containing metabolic product of protein catabolism in humans • Its elimination in the urine represents the major route for nitrogen excretion • More than 90% of urea is excreted through the kidneys, with losses through the GIT and skin ( sweat)
Plasma Urea • Urea is filtered freely by the glomeruli, but subject to tubular reabsorption , depending on urea excretion may underestimates GFR • Urea production and excretion is increased by a high protein intake and it is decreased in patients with a low protein intake • Blood urea levels are reduced in patients with liver disease, and pregnancy, but increased with dehydration
Plasma Urea • Plasma concentrations also tend to be slightly higher in males than females (normal adults is level 10 -40 mg/dl) • Non-renal factors can affect the urea level like: • Dehydration • High protein diet • Increased protein catabolism • Reabsorption of blood proteins after a GIT haemorrhage • Treatment with corticosteroids
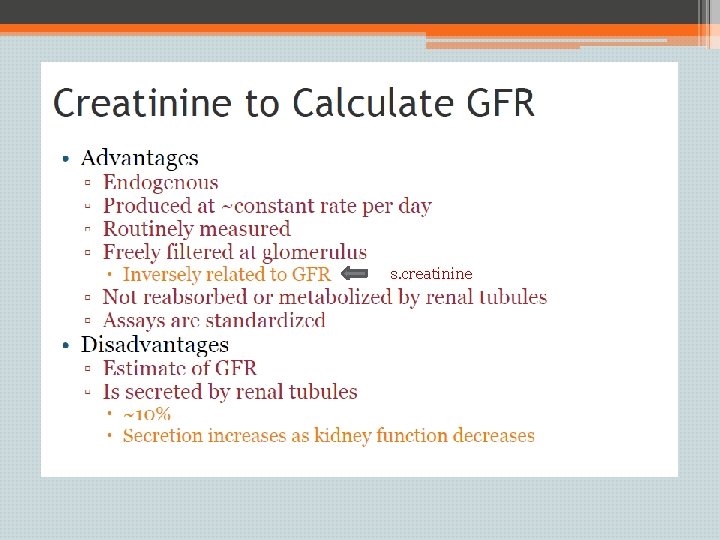
Creatinine • Non-enzymatic breakdown of phosphocreatine in muscle fibers • Produced at a relatively constant rate based on age, gender, race, and muscle mass; so decreased with aging, females, whites and patients with neuromuscular disease • Not affected by diet ( protein intake ) or hydration state • Measurement of plasma creatinine provides a more accurate assessment than urea because there are many factors that affect urea level.
Limitations of Creatinine • Creatinine excretion is due not only to filtration (90%– 95%) by the kidney but also to secretion (5%– 10%) by the proximal tubule • If the patient with advanced CKD takes a substance that blocks tubular secretion of creatinine (eg, trimethoprim, cimetidine, cefoxitin), to avoid overestimation of GFR Stevens NEJM. 2006
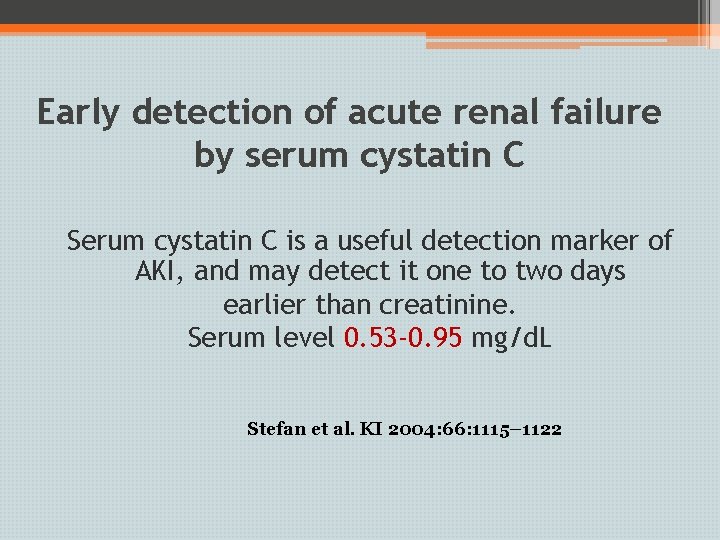
Cystatin C • 13 Kd protein • Produced by all nucleated cells at a constant rate and freely filtered at the glomeruli, no tubular reabsorption or secretion • Minimally affected by diet, gender, ethnicity, age and muscle mass • Affacted by glucocorticoids and thyroid hormone
Early detection of acute renal failure by serum cystatin C Serum cystatin C is a useful detection marker of AKI, and may detect it one to two days earlier than creatinine. Serum level 0. 53 -0. 95 mg/d. L Stefan et al. KI 2004: 66: 1115– 1122
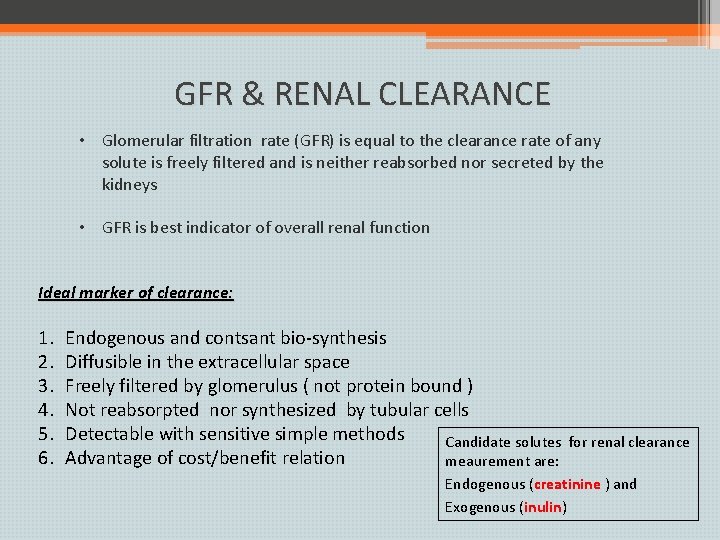
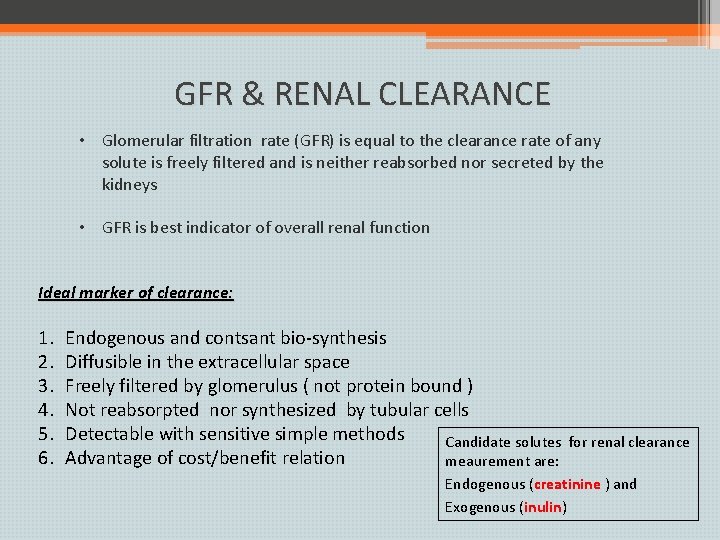
GFR & RENAL CLEARANCE • Glomerular filtration rate (GFR) is equal to the clearance rate of any solute is freely filtered and is neither reabsorbed nor secreted by the kidneys • GFR is best indicator of overall renal function Ideal marker of clearance: 1. 2. 3. 4. 5. 6. Endogenous and contsant bio-synthesis Diffusible in the extracellular space Freely filtered by glomerulus ( not protein bound ) Not reabsorpted nor synthesized by tubular cells Detectable with sensitive simple methods Candidate solutes Advantage of cost/benefit relation meaurement are: for renal clearance Endogenous (creatinine ) and Exogenous (inulin)
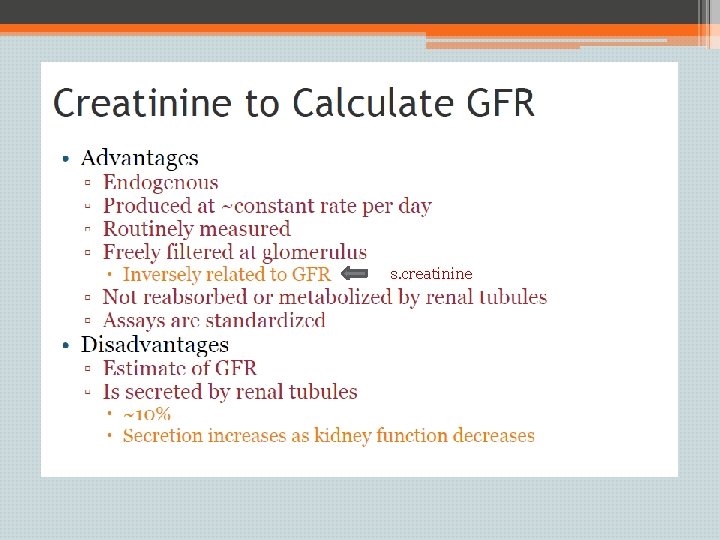
s. creatinine

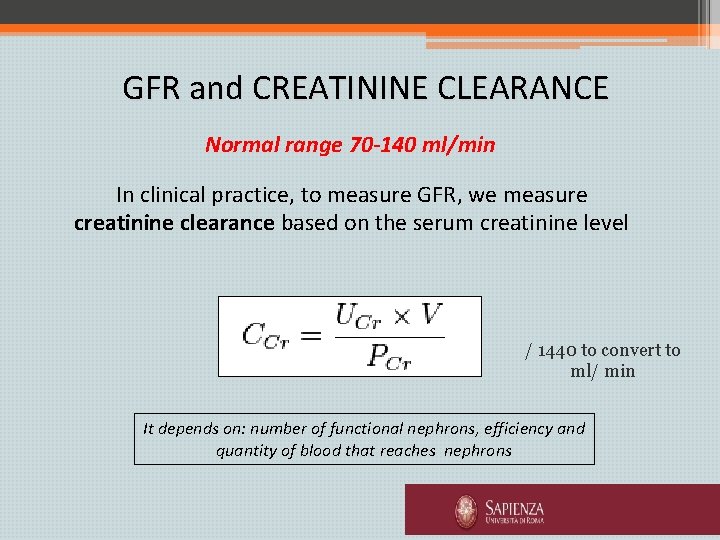
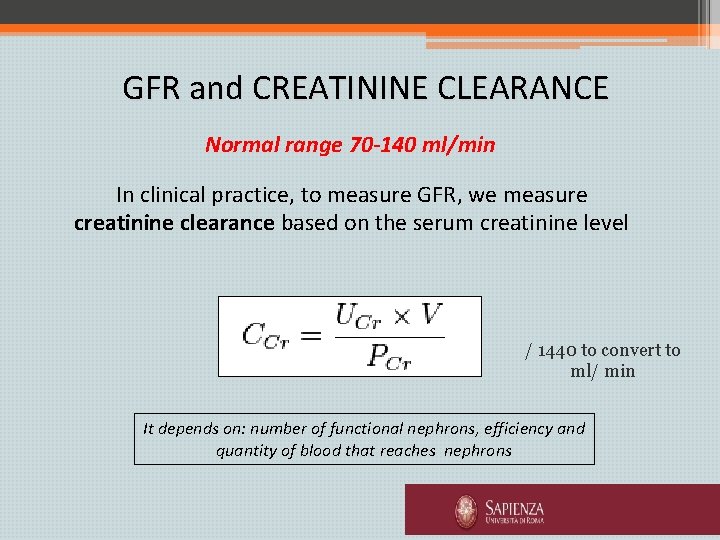
GFR and CREATININE CLEARANCE Normal range 70 -140 ml/min In clinical practice, to measure GFR, we measure creatinine clearance based on the serum creatinine level / 1440 to convert to ml/ min It depends on: number of functional nephrons, efficiency and quantity of blood that reaches nephrons
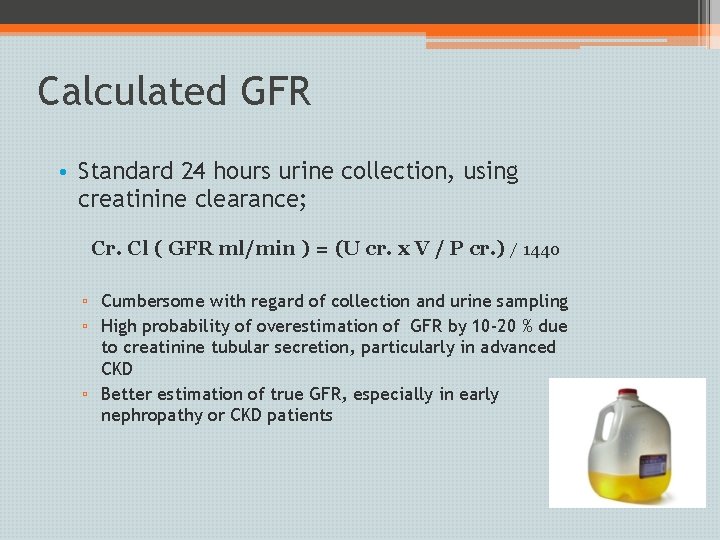
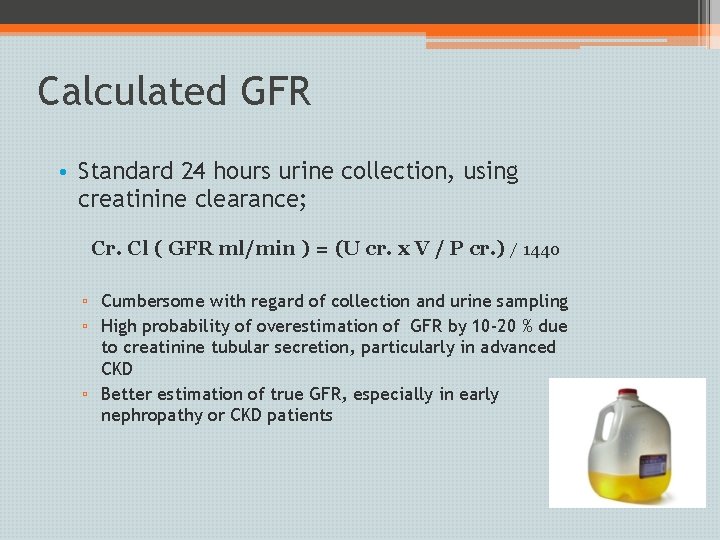
Calculated GFR • Standard 24 hours urine collection, using creatinine clearance; Cr. Cl ( GFR ml/min ) = (U cr. x V / P cr. ) / 1440 ▫ Cumbersome with regard of collection and urine sampling ▫ High probability of overestimation of GFR by 10 -20 % due to creatinine tubular secretion, particularly in advanced CKD ▫ Better estimation of true GFR, especially in early nephropathy or CKD patients
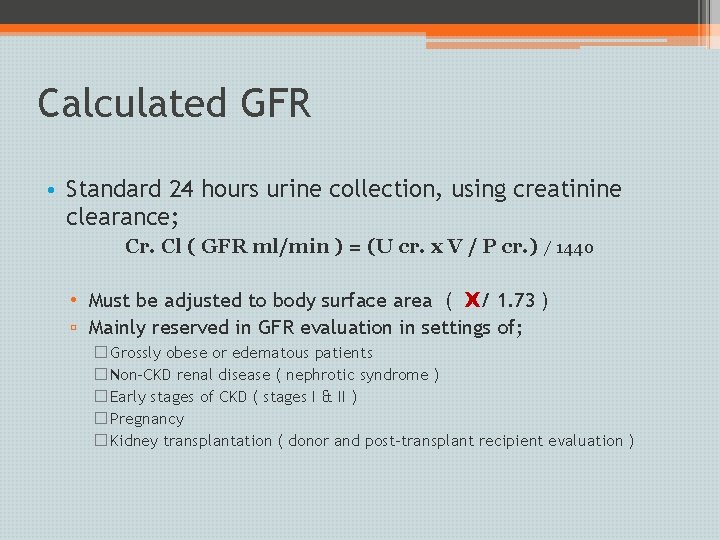
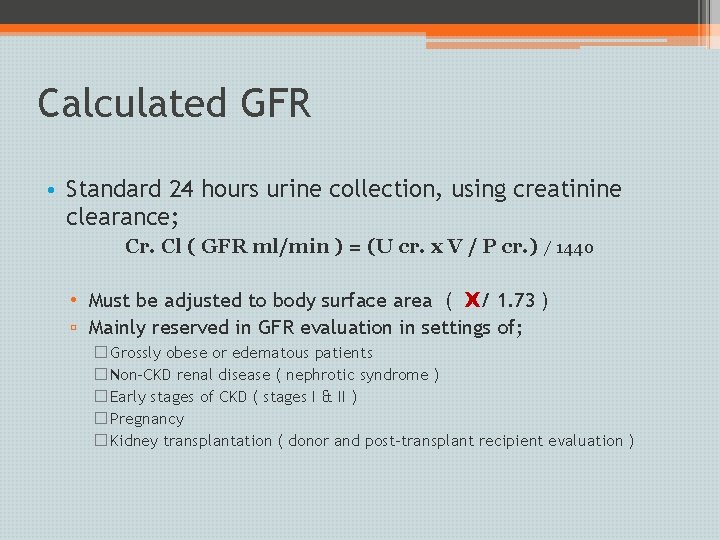
Calculated GFR • Standard 24 hours urine collection, using creatinine clearance; Cr. Cl ( GFR ml/min ) = (U cr. x V / P cr. ) / 1440 • Must be adjusted to body surface area ( X/ 1. 73 ) ▫ Mainly reserved in GFR evaluation in settings of; � Grossly obese or edematous patients � Non-CKD renal disease ( nephrotic syndrome ) � Early stages of CKD ( stages I & II ) � Pregnancy � Kidney transplantation ( donor and post-transplant recipient evaluation )
Estimated GFR; prediction equations • Creatinine-based prediction equations: ▫ Cockcroft- Gault formula ( CGF ), 1976 ▫ Modification of Diet in Renal Disease ( MDRD ) equation, 2005 ▫ Chronic kidney disease- epidemiology ( CKD-EPI ) equation, 2009
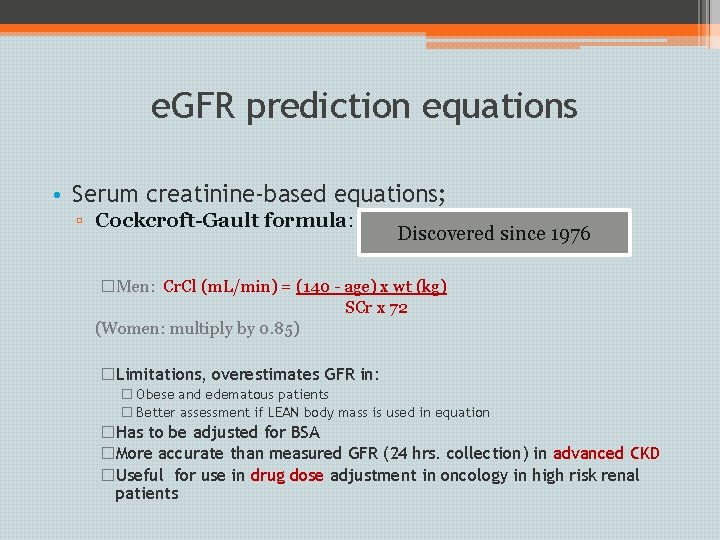
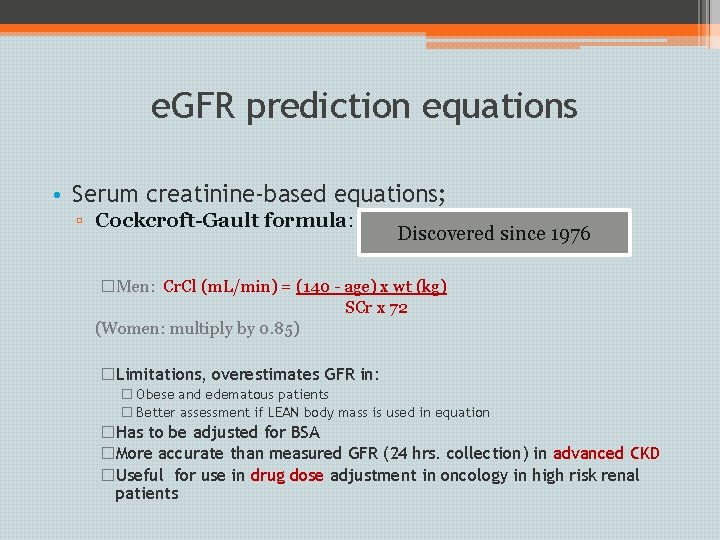
e. GFR prediction equations • Serum creatinine-based equations; ▫ Cockcroft-Gault formula: Discovered since 1976 �Men: Cr. Cl (m. L/min) = (140 - age) x wt (kg) SCr x 72 (Women: multiply by 0. 85) �Limitations, overestimates GFR in: � Obese and edematous patients � Better assessment if LEAN body mass is used in equation �Has to be adjusted for BSA �More accurate than measured GFR (24 hrs. collection) in advanced CKD �Useful for use in drug dose adjustment in oncology in high risk renal patients
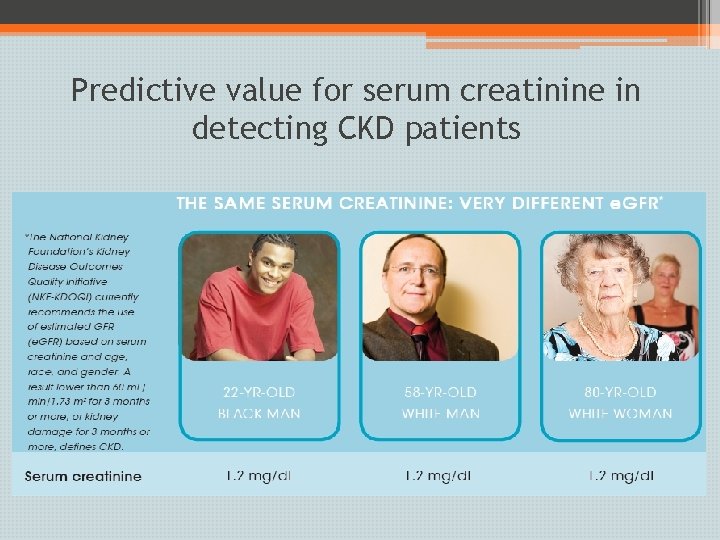
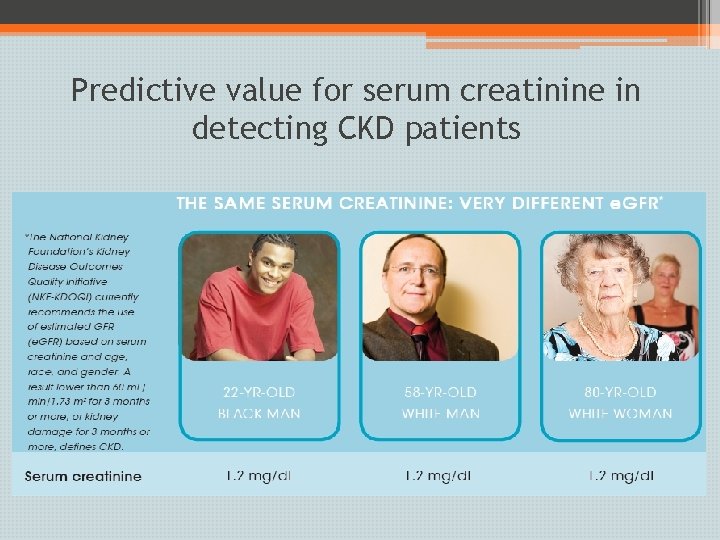
Predictive value for serum creatinine in detecting CKD patients
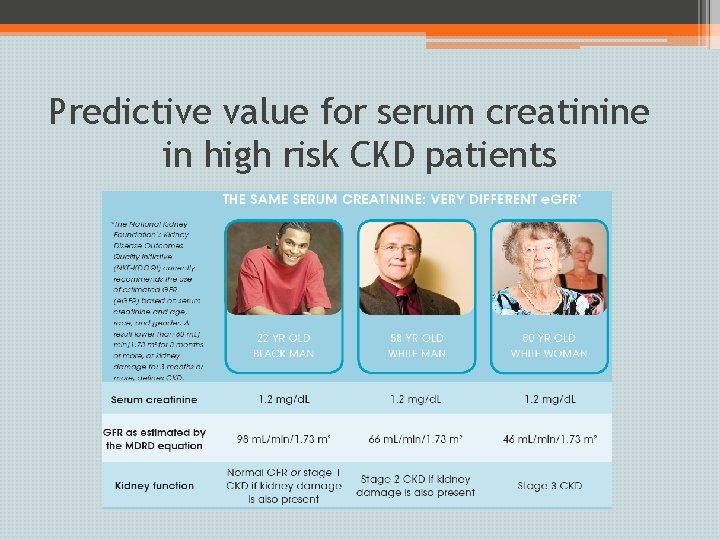
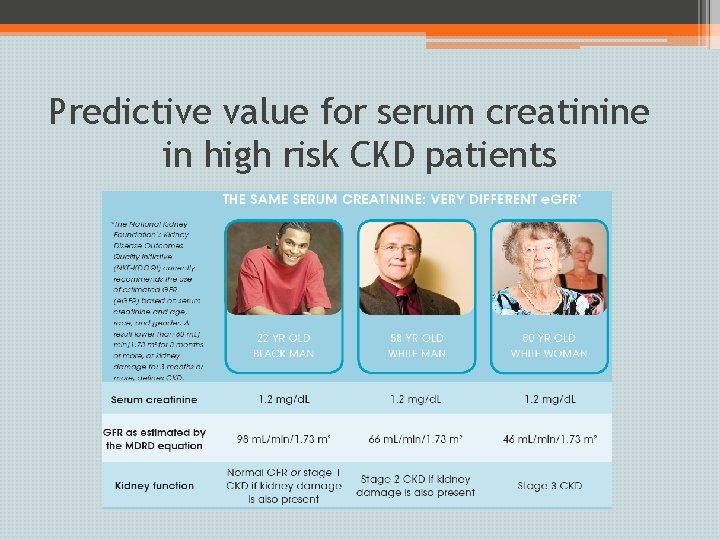
Predictive value for serum creatinine in high risk CKD patients
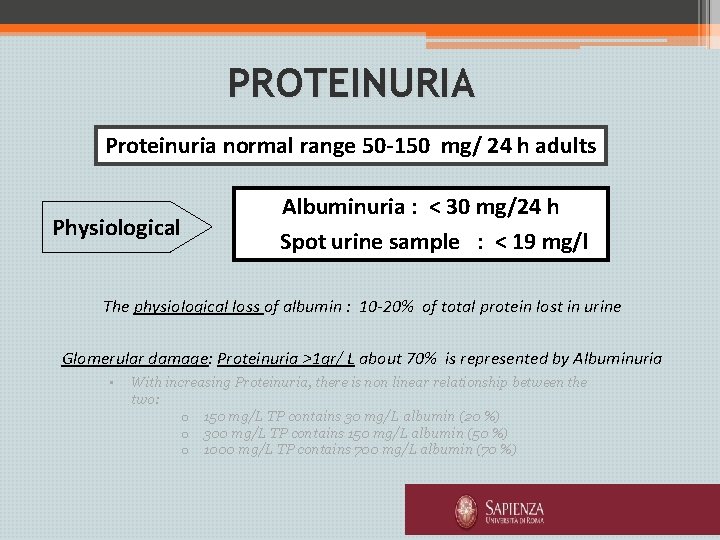
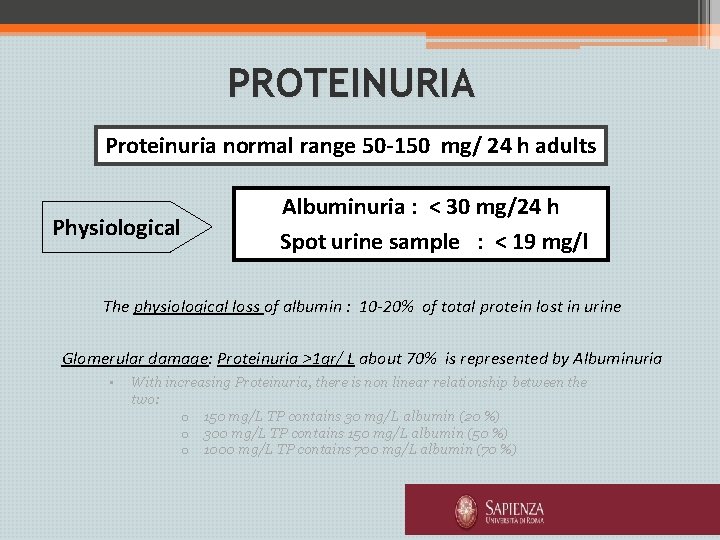
PROTEINURIA Proteinuria normal range 50 -150 mg/ 24 h adults Physiological Albuminuria : < 30 mg/24 h Spot urine sample : < 19 mg/l The physiological loss of albumin : 10 -20% of total protein lost in urine Glomerular damage: Proteinuria >1 gr/ L about 70% is represented by Albuminuria • With increasing Proteinuria, there is non linear relationship between the two: o 150 mg/L TP contains 30 mg/L albumin (20 %) o 300 mg/L TP contains 150 mg/L albumin (50 %) o 1000 mg/L TP contains 700 mg/L albumin (70 %)
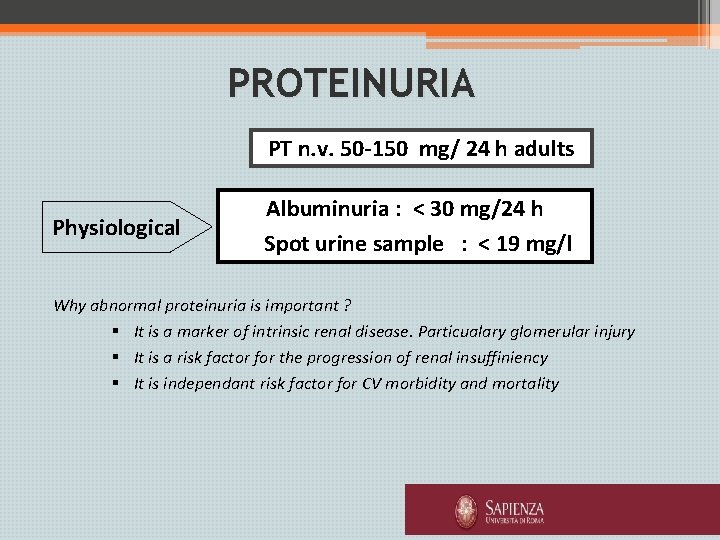
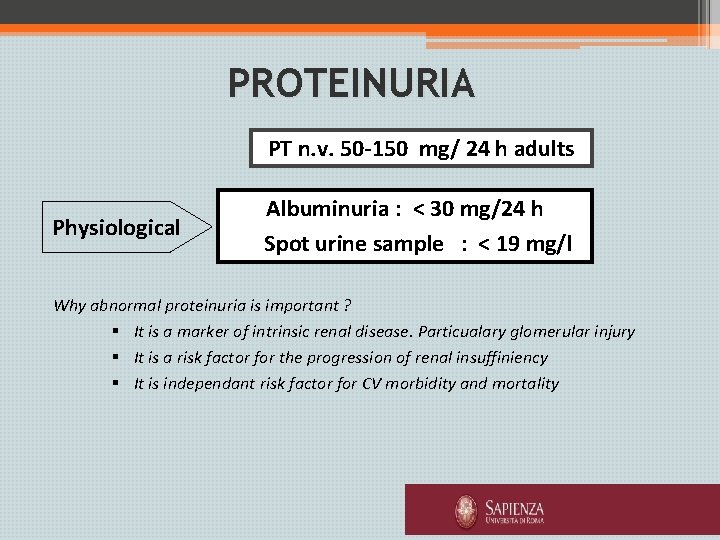
PROTEINURIA PT n. v. 50 -150 mg/ 24 h adults Physiological Albuminuria : < 30 mg/24 h Spot urine sample : < 19 mg/l Why abnormal proteinuria is important ? § It is a marker of intrinsic renal disease. Particualary glomerular injury § It is a risk factor for the progression of renal insuffiniency § It is independant risk factor for CV morbidity and mortality
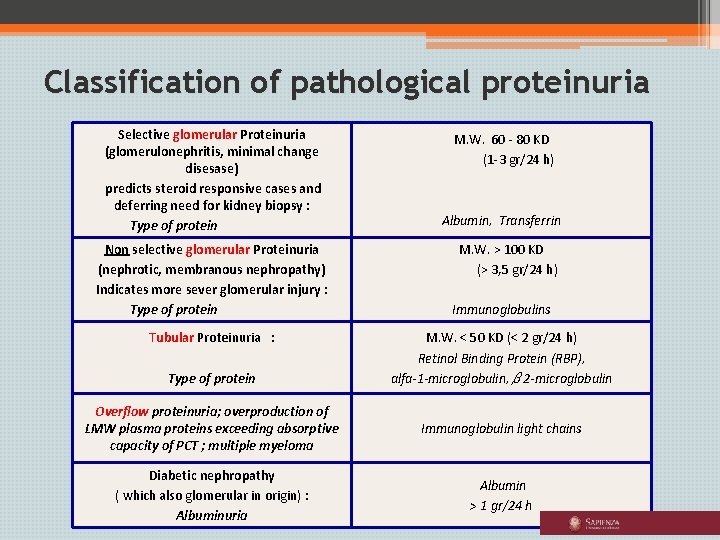
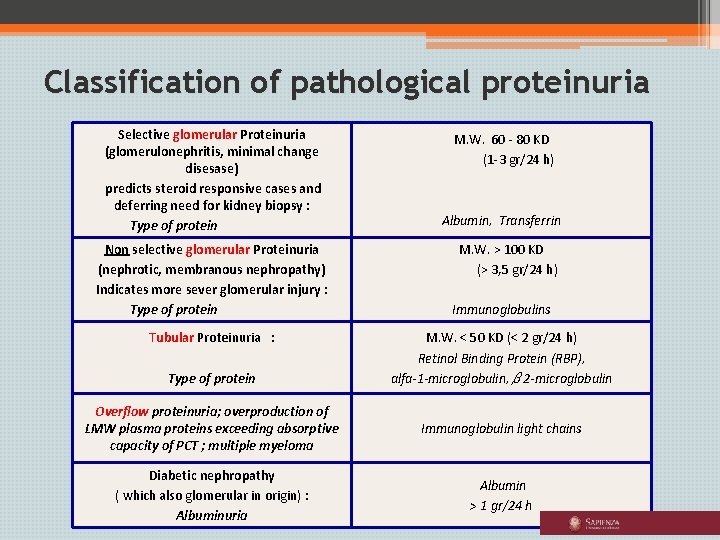
Classification of pathological proteinuria Selective glomerular Proteinuria (glomerulonephritis, minimal change disesase) predicts steroid responsive cases and deferring need for kidney biopsy : Type of protein Non selective glomerular Proteinuria (nephrotic, membranous nephropathy) Indicates more sever glomerular injury : Type of protein Tubular Proteinuria : Type of protein M. W. 60 - 80 KD (1 -3 gr/24 h) Albumin, Transferrin M. W. > 100 KD (> 3, 5 gr/24 h) Immunoglobulins M. W. < 50 KD (< 2 gr/24 h) Retinol Binding Protein (RBP), alfa-1 -microglobulin, β 2 -microglobulin Overflow proteinuria; overproduction of LMW plasma proteins exceeding absorptive capacity of PCT ; multiple myeloma Immunoglobulin light chains Diabetic nephropathy ( which also glomerular in origin) : Albuminuria Albumin > 1 gr/24 h
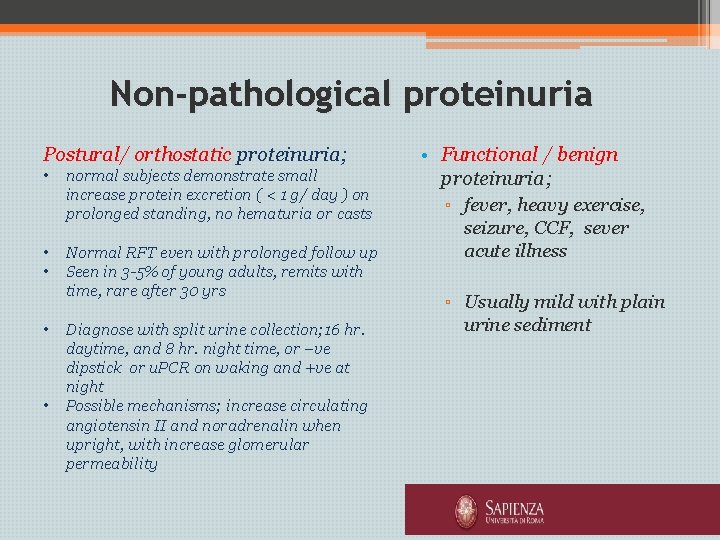
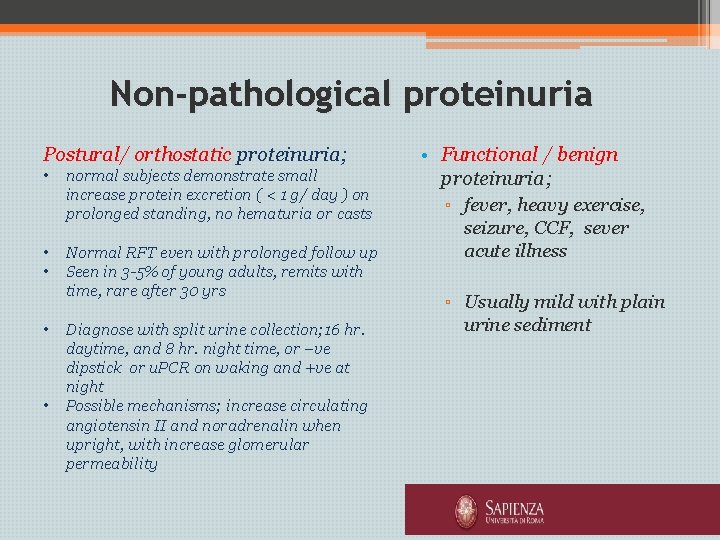
Non-pathological proteinuria Postural/ orthostatic proteinuria; • • • normal subjects demonstrate small increase protein excretion ( < 1 g/ day ) on prolonged standing, no hematuria or casts Normal RFT even with prolonged follow up Seen in 3 -5% of young adults, remits with time, rare after 30 yrs Diagnose with split urine collection; 16 hr. daytime, and 8 hr. night time, or –ve dipstick or u. PCR on waking and +ve at night Possible mechanisms; increase circulating angiotensin II and noradrenalin when upright, with increase glomerular permeability • Functional / benign proteinuria; ▫ fever, heavy exercise, seizure, CCF, sever acute illness ▫ Usually mild with plain urine sediment

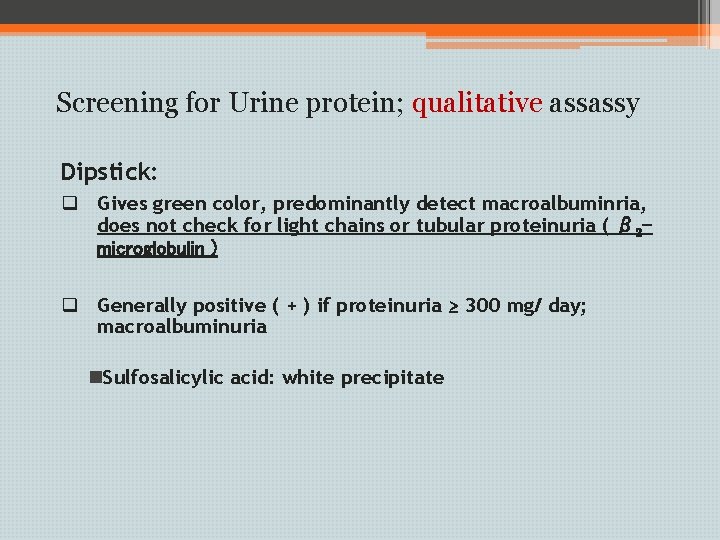
Screening for Urine protein; qualitative assassy Dipstick: q Gives green color, predominantly detect macroalbuminria, does not check for light chains or tubular proteinuria ( β 2 microglobulin ) q Generally positive ( + ) if proteinuria ≥ 300 mg/ day; macroalbuminuria n. Sulfosalicylic acid: white precipitate
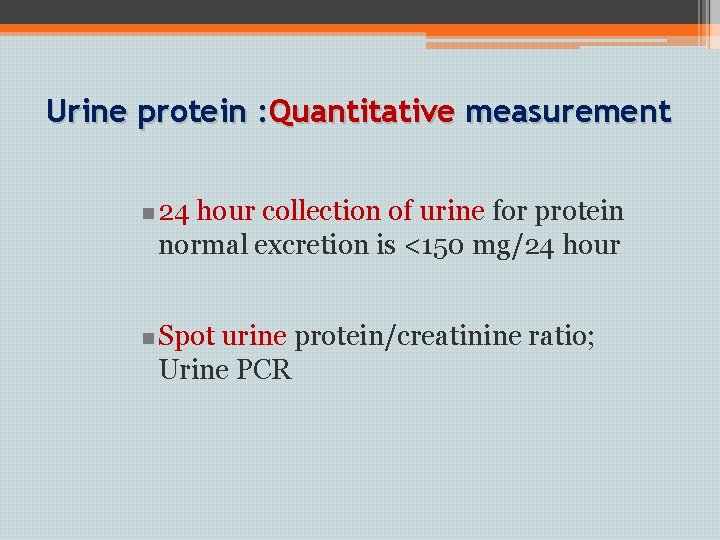
Urine protein : Quantitative measurement n 24 hour collection of urine for protein normal excretion is <150 mg/24 hour n Spot urine protein/creatinine ratio; Urine PCR
Protein: creatinine ratio ( PCR ) • Morning spot urine sample • Urine gram protein / gram creatinine • Mainly used in evaluation of protein excretion in glomerulonephritis ▫ Normally < 0. 2 ; nearly correlates with 200 mg protein per day ▫ Nephrotic range >3. 5
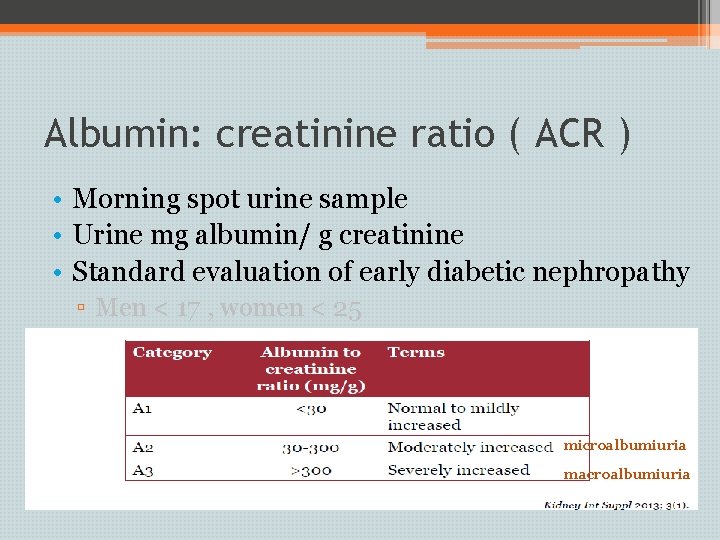
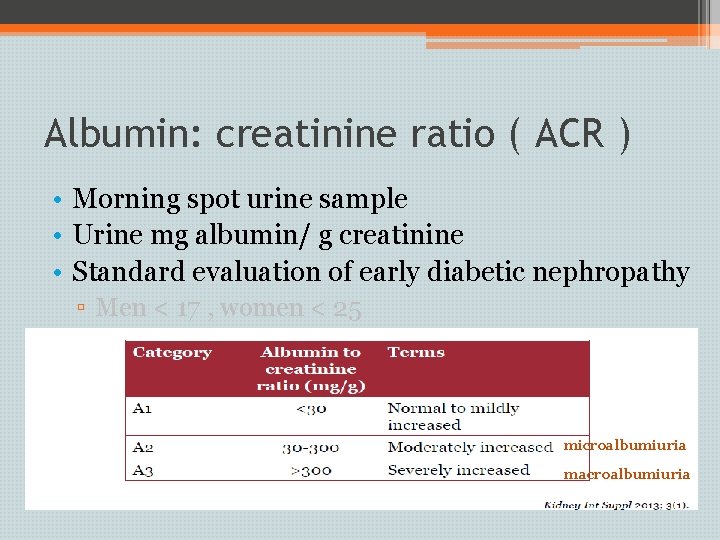
Albumin: creatinine ratio ( ACR ) • Morning spot urine sample • Urine mg albumin/ g creatinine • Standard evaluation of early diabetic nephropathy ▫ Men < 17 , women < 25 microalbumiuria macroalbumiuria
Take home message • Assessment of renal function should be included in routine evaluation of all patients; outpatient/ inpatient • Be aware of conditions that raise BUN and creatinine other than kidney disease ? • The current use of estimation/ prediction equations for GFR assessment • Evaluation for proteinuria and albuminuria

 Ira pré renal renal e pós renal
Ira pré renal renal e pós renal Sindrome nefrótica
Sindrome nefrótica Peritubular capillaries and vasa recta difference
Peritubular capillaries and vasa recta difference Function of renal cortex
Function of renal cortex Disequilibration syndrome
Disequilibration syndrome Kidney function test
Kidney function test Riham mohamed aly
Riham mohamed aly Mohamed dahoui
Mohamed dahoui Dr elsayed mohamed
Dr elsayed mohamed Mohamed kossentini
Mohamed kossentini Aya moughni
Aya moughni Discovering computer
Discovering computer Mohamed el merouani
Mohamed el merouani Mohamed seghir nekkache
Mohamed seghir nekkache Dr mohamed bashar shala
Dr mohamed bashar shala Dr qazi omar
Dr qazi omar Dr nasser mohamed
Dr nasser mohamed Dr mohamed eldeib
Dr mohamed eldeib Power rating
Power rating Bouhicha mohamed
Bouhicha mohamed Abdelrahman mohamed
Abdelrahman mohamed Dr mohamed bashar shala
Dr mohamed bashar shala Dr alboushi
Dr alboushi Mohamed salah
Mohamed salah Zofinopril
Zofinopril Mohamed akel
Mohamed akel Mohamed akel
Mohamed akel Zahran nyu
Zahran nyu Henintsoa georges
Henintsoa georges Mohamed zahran nyu
Mohamed zahran nyu Mohamed merchant
Mohamed merchant Mohamed akel
Mohamed akel Mohamed akel
Mohamed akel Mohamed younis umbc
Mohamed younis umbc